An overview of this resource
Referral pathways from ambulance providers into urgent community response (UCR) services are in place in many areas of the country, but there is variation in approach.
Although there has been continued growth from 999 into UCR over the last 12 months, there are still opportunities to increase referral activity, supporting individuals in need of rapid support as well as system pressures.
This document outlines:
- a variety of referral models between 999 and UCR services, and associated benefits/limitations
- pathways and case studies to illustrate what the different models look like ‘on the ground’.
The different types of referral models described are:
- portal transfer (with or without automated referral)
- interoperability toolkit (ITK) transfer
- telephone transfer
- referral via a single point of access (SPoA) or similar.
How to use this document
This document can support places/integrated care boards (ICBs) to:
- Implement referral pathways from 999 into UCR, where these are not already in place
- Review existing arrangements, and support pathway transformation where needed to ensure optimal management of ambulance referrals across a system.
When reading through this document, it can be helpful to reflect on the below indicators for testing the maturity of any pathway in place:
- Ambulance providers are identifying appropriate caseload to pass to UCR services
- UCR services accept all appropriate referrals, and where capacity allows, proactively identify caseload
- UCR services have the digital capability to communicate with and accept referrals from ambulance providers
- Audits on both rejected referrals and missed opportunities to refer into UCR are carried out, and identified issues are resolved
- Evaluations occur to understand the impact the pathway is having and to actively target priority population groups (e.g. those experiencing health inequalities).
UCR and 999: the current picture
Overview
11 ambulance services (including Isle of Wight) operate in England, receiving around 12-14m calls annually.
Not all these incidents will require an emergency response. Through developing pathways between ambulance providers and other community-based services, it’s expected that:
- people will still receive timely, safe clinical care in their homes
- systems will be able to maximise their limited resource, deploying 999 crews only when needed.
These ambitions are supported by the 2023 Delivery plan for recovering urgent and emergency care services, with systems/providers asked to transfer patients who do not need a face-to-face 999 response into services that more appropriately meet their needs, including UCR.
In May 2023, 4,430 UCR referrals (8.4%) were from ambulance services, around 56% more referrals than May 2022. There is a national average of approximately 400 referrals per month by ambulance trusts across England. Part of this increase is due to better data quality/ reporting. There are also significant variations among trusts, with high referrers having over 1000 referrals per month and low referrers having less than 200 per month.
Ambulance services are currently the fourth highest referrer into UCR services, behind self-referral, GPs and other community services.
150 Day Challenge
Part of the reason for a 48% increase in referrals from ambulance services to UCR over the period from October 2021 to March 2022 was due to the 150 Day Challenge – see slides 12 and 13 on the UCR FutureNHS platform, which encouraged ambulance and UCR services to work together to:
- help manage ambulance demand and where clinically appropriate, have UCR take on category 3 and 4 calls
- build networks and enable collaboration between UCR services and ambulance trusts.
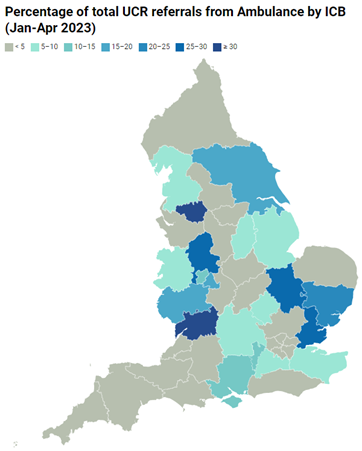
Percentage of total UCR referrals from ambulance by ICB, January to April 2023
The above map of England shows the percentage of total UCR referrals from ambulance providers from January to April 2023, by integrated care board (ICB). Greater Manchester and Gloucestershire ICBs report the largest percentage of referrals from ambulance services, whereas South East London and Northamptonshire ICBs are reporting the lowest percentage of UCR referrals.
Referral models
An overview of referral models, and where this is occurring
Overview of referral process
Who should refer
UCR services can accept 999 activity via:
- ambulance control rooms, also known as Emergency Operations Centres (EOC)
- 999 crews on scene, who can refer via telephone, or through Directory of Services (DoS)/MiDoS (versatile and widely used service finding app in the NHS)
- Single point of access (SPoA)/Clinical Assessment Service (CAS), where a range of 999 incidents (not just UCR appropriate) are passed and validated for onward referral; or a 999 clinician (in the SPoA) is ‘pulling’ incidents for referral.
UCR services should accept non-clinician to clinician referrals, where this is supported by the NHS Pathways algorithm/clinical decision support system. This could be supported by the agreement of ‘pre-determined code sets’ (see more information in the ‘Pre-determined code sets and automation’ section of this document).
How to refer
Some 999 incidents on the EOC incident stack can be considered for alternative response by the ambulance service and, where appropriate, referred onto UCR by one of the below models:
- Portal transfer
- Interoperability toolkit (ITK) transfer
- Telephone transfer
- Referral via a SPoA, which can occur with or without an automated referral
- 999 to SPoA, or;
- SPoA ‘pull’ from 999 (via a 999 approved clinician e.g. paramedic working in a MDT).
Although distinct, the referral models can be linked solutions. Data shows that ICBs with one consistent referral model into UCR have a higher number of ambulance referrals on average than areas utilising a mix of models.
Appropriate 999 incidents can also be referred from ‘at scene’ by a clinician. This can happen via various routes:
- telephone referral into UCR
- referral into SPoA
- referral via DoS/MiDoS.
It is imperative that strong clinical governance surrounds any transfer of care between 999 and UCR. Key features include: the selection of appropriate incidents to refer; patient safety netting (i.e. ensuring timeliness of response is not compromised, and that escalation back to 999 is available if needed); consideration of cyber/information governance principles; and conducting regular audits.
In line with the Delivery plan for recovering urgent and emergency care services, NHS England encourages the use of electronic referral methods that enable the quick transfer of appropriate incidents into community services.
Referral models for consideration
While each model has benefits and limitations, engagement across the country suggests model A is best for ensuring a high volume of appropriate referrals into UCR. See the annex of this document for case studies for various referral models outlined below.
Model A: Portal transfer (with or without automated referral)
Key features:- The portal is a web-based platform that can be accessed by alternative providers, who can go into the portal and select appropriate 999 cases to manage.
- The portal is external to the computer-aided dispatch (CAD) system, which is the software used within Emergency Operations Centres (EOC) to triage calls and deploy ambulance resources.
- If an incident is rejected in the portal by an alternative provider, then the original position of the case in the 999 incident queue is retained.
- The portal enables a streamlined referral route across an area. It supports a system-led, collaborative approach by ensuring all partners have an opportunity to ‘pick up’ referrals.
- It shows potential to maximise referral numbers (i.e. two of the top three regions with the most referrals are using portals).
- The portal facilitates improved data monitoring and auditing as a portal system provides the functionality to accept/reject referrals and outline reasons for referral status.
- Pre-determined code sets can enable patient information to be moved across seamlessly.
- The portal is unavailable to frontline 999 crews.
- It requires large scale, system wide buy-in and collaboration to maximise benefits.
Model B: ITK transfer
Key features:- Interoperability toolkit (ITK) is a set of national standards, frameworks and implementation guides to support interoperability within local organisations.
- Appropriate incidents are identified/validated by navigators or clinicians in an EOC who can make a referral via ITK messaging.
- An ITK transfer involves a trusted assessor model, as in ‘trusted’ of assessment of patient, and ‘decision’ of what is the best treatment and place as outcome of the assessment.
- The ITK transfer process can be made more efficient with the use of administration staff, given the manual elements that are involved.
- The ITK transfer is a manual process.
- There is variation in who receives the referral and their confidence in accepting referrals, which can be difficult to navigate for the referrer.
Model C: Telephone transfer
Key features:- A telephone transfer requires having a dedicated number for a specific UCR team or going through the Directory of Services (DoS) to access a UCR service.
- Clinicians/navigators in EOC (or 999 crews on scene) can directly contact a UCR team and make a patient referral.
- A telephone transfer can facilitate clinician-to-clinician discussions, if the pathway is designed with this in mind.
- The process can be made more efficient with the use of administration staff, given the manual elements that are involved.
- This is a manual process, risking different interpretations of inclusion/exclusion criteria. There is also a lack of an audit trail.
- A telephone transfer will not always allow for clinician-to-clinician discussions.
Model D: Referral via a SPoA or similar
Key features:- A single point of access (SPoA) coordinates care more effectively by maximising the use of non-ED pathways.
- Appropriate incidents are identified by clinicians/ navigators in EOC (or by 999 crews on scene), who can utilise a dedicated number to call a SPoA and refer an incident or can access the SPoA via the DoS.
- A SPoA reduces the complexity caused by multiple referral points and criteria, enabling a streamlined referral route.
- It incorporates co-location and MDT working – UCR is available as ‘one of many’ services, providing ease of access to wider care options.
- It maximises referral numbers (e.g. several ICBs report greater numbers of referrals when a SPoA model is used).
- There can be multiple SPoA’s – with different criteria and operating hours, resulting in confusion.
- It requires large scale, system wide buy-in and collaboration to maximise benefits.
Additional information
An overview of challenges, solutions and principles areas should be aware of.
Pre-determined code sets and automation
What is it?
Pre-determined code sets refers to a list of codes (agreed locally among services) that can be sent from 999 to UCR by ambulance control room staff, without full clinical validation. Calls go through initial telephone triage and call coding (AMPDS or NHS Pathways) but are then quickly identified to staff for onward referral.
Automation refers to the automatic referral of appropriate incidents (based on the pre-determined code set) without the need for staff to manually complete the referral. Currently, the East of England via the ‘Cleric Digital Portal at East of England Ambulance Service NHS Trust (EEAST)’ project are set to trial this concept in September 2023.
How is it beneficial?
Pre-determined code sets and automation aim to improve referral efficiency due to fewer touch points, and ensure patients get to the right point of care quickly.
What needs to happen to make it a reality?
A joint memorandum of understanding (MoU), operational policy or similar, should be developed and signed off by all parties involved in the 999 to UCR referral pathway. This should include governance and detail on patient safety netting arrangements within the pathway. The MoU could include a pre-determined code set.
Cross-system engagement is key to maintaining patient safety and should include regular meetings. Setting up communication channels for daily touch-points – Microsoft Teams Chat, Cleric Portal Chat (EEAST and WMAS) – is also recommended.
Regular monitoring, auditing and sharing of referral data (i.e. referral numbers, acceptance rates, reasons for rejections and timeliness of referrals) should occur. This could involve reviewing recent data, missed opportunities, DATIX incidents and patient safety incidents:
- East of England conducted ‘Learning Lab’ audits which investigated missed opportunities for UCR to accept calls that had been rejected. This was done in partnership across the region, with both UCR and ambulance providers in attendance. For more detail see Learning Labs Outcomes on the East of England FutureNHS page.
Accurate and timely reporting should occur – this will support audits, analysis and monitoring.
What are some good practice examples?
Several ambulance services are already using locally agreed code sets. For more information, or to set up a call with a service who has agreed pre-determined code sets, please contact england.ambulance@nhs.net or england.communitycare@nhs.net.
Key challenges and principles for developing solutions
Challenge 1: Data
Description:- Inaccurate Community Services Data Set (CSDS) submissions impact data quality.
- There is a lack of standardisation across systems and teams (e.g. what constitutes a 2-hour UCR response, variance in capture of out of hospital activity, etc.).
- There are challenges regarding identifying all 999 activity as some activity is diverted to falls providers outside of an organisation or a specific UCR team.
- Data sharing agreements must be in place between ambulance services and relevant teams, with the responsibility for arranging these shared across all partners (including the ICB).
- ICBs should work with their regional Urgent and Emergency Care/Digital teams to identify data quality issues and resolve them. This could include improving data recording and reporting to incorporate capture of UCR referrals from 999 separately to general CAS referrals.
- Where possible, insight on UCR referrals should be captured regarding learning from time of day/day of week, rejected referrals, key reasons for referral, and where referral was not possible due to service constraints/lack of specific service provision.
Challenge 2: Inconsistency of offer for UCR teams within a system
Description:- There are different referral acceptance times within a system.
- There are varying levels of skills (e.g. Advanced Clinical Practitioner training/availability, capability to respond to falls) and capacity among UCR teams.
- There is inconsistency among UCR teams regarding accepting referrals without GP/medical triage or C2C conversation.
- There is varied care home engagement for reducing 999 calls.
- Have regular service to service conversations and enable the sharing of learning, good practice and discussions challenges and solutions through regional/local learning events (webinars, workshops, community of practice, etc.). See the following examples: 1) Learning Hours on the North West Region Ageing Well FutureNHS page and 2) Learning Labs – missed opportunity audits on the East of England Region FutureNHS page (from rejected 999 to UCR referrals).
- Work with NHS England Improvement and ambulance service colleagues to develop data requirements around rejected cases from 999.
- Share good practice regarding care home support for alternatives to 999 pathways.
Challenge 3: Ambulance reporting requirements
Description:- Ambulance services are required to report on various standards, indicators and measures as part of Ambulance Quality Indicator (AQI) reporting.
- An issue was raised to NHSE regarding the recording of referrals sent through to alternative care providers via 999 without clinical validation taking place in the ambulance control room – how should this activity be recorded and does it meet the definition of a 999 hear and treat (H&T)?
- If the case is picked up by a UCR team from either a direct referral or via a ‘portal’, it counts as H&T.
- If a case sits on the portal and either is ‘not accepted’ or ‘times out’, it is returned to the EOC stack for one of the following:
- EOC clinical validation, and/ or referral to another service (counts as H&T).
- Ambulance response (which could either count as See and Treat or See and Convey).
Challenge 4: Communication/lack of awareness of UCR service
Description:- There is varying confidence from primary care providers regarding the ability of UCR teams to defer/manage a 999 call.
- There are different levels of knowledge of UCR by crews on the scene, including the speed and ability for UCR teams to respond to a need.
- Awareness of UCR services by pathway partners (e.g. SDEC, ED, Urgent Treatment Centres) varies.
- Support systems to communicate their UCR offer.
- Ensure cross-organisational education occurs across services.
- Engage with wider teams on the pathway.
- Have shared oversight of community urgent caseload.
- Establish links with clinical leads at ambulance services.
- Define a UCR and 999 strategy that aligns to relevant regional and national strategies as well as the wider strategy for alternative pathways to ED.
Challenge 5: Variability of Single Point of Access (SPoA)
Description:- There is a lack of a standardised pathway to access UCR.
- There are varying levels of SPoA maturity and clinical oversight.
- There are multiple SPoA opportunities (e.g. CAS/Care Co-ordination Centre, etc.).
- Support systems through critical challenge to ensure the use of one SPoA for accessing community services.
- Define what good looks like for a SPoA.
Annex
Case study for Model A: West Midlands Ambulance Service integrated referral portal, enabling the transfer of patients to alternative providers
Overview
- In response to increasing emergency activity from July 2021, compounded by significant increases in lost operational hours through extended hospital turnaround, West Midlands Ambulance Service (WMAS) introduced the clinical validation team to better manage category 3 and 4 emergency patients.
- An external trust website/portal was also developed that can be accessed by alternative providers across the WMAS footprint. Incidents suitable for UCR are transferred to providers (via the external stack) by clinical staff in the 999 control room. This is for a specific NHS Pathways code DX124 (2-hour UCR).
Situation
When reviewing which community services are most likely targeted by the Clinical Validation Team, only 9.25% of services had a means of electronic referral available and almost all were email-based. Having few electronic referrals was identified as a limiting factor to referrals and likely increases the handling time to complete a referral, as patient details have to be shared verbally or an email receipt must be confirmed.
The CAD/’integrated referral portal’ was developed to increase the efficiency of referrals into community teams.
Action
The Trust developed the integrated referral portal to streamline referrals to community services, with functionality to receive an SMS text prompt for new referrals and the ability to confirm acceptance of the patient. When a case is ‘rejected’, it goes back to the ambulance stack in its original position.
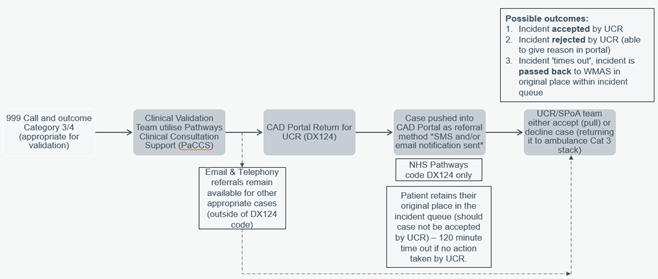
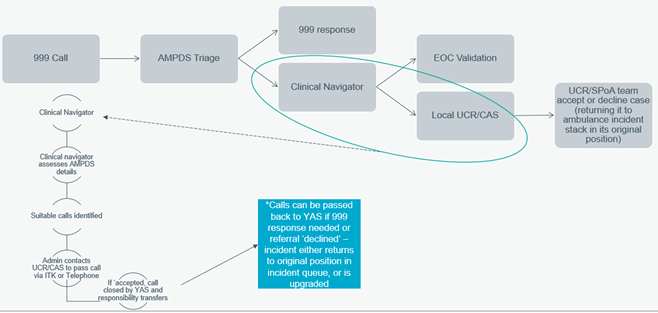
The process is outlined as:
- 999 call and outcome category 3/4 (appropriate for validation)
- Clinical validation team use pathways clinical consultation support (PaCCS)
- CAD portal return for UCR (DX124)
- Case pushed into CAD portal as referral method *SMS and/or email notification sent*
- UCR/SPoA team either accept (pull) or decline case (returning it to ambulance cat 3 stack).
Results
Since implementation in Feb/March 2022*, over 9000 cases have been passed via the Integrated Referral Portal. ~5900 of those have been accepted by UCR teams, with just over 3000 rejected due to referrals not being clinically appropriate or no capacity available within the UCR team (among other reasons). *Note: only two ICB areas were live during the initial phases of the portal launch, all other ICBs were onboarded from July 2022.
For more information, see Ambulance (999) and Urgent Community Response Webinar Series – Part 1, Episode 1 Digital Opportunities.
Detailed guidance for Model A: 999 to UCR portal pathway
The below outlines a pathway for the WMAS integrated portal. The Trust developed the integrated referral portal to streamline referrals to community services, with functionality to receive an SMS text prompt for new referrals and the ability to confirm acceptance of the patient. When a case is ‘rejected’, it goes back to the ambulance stack in its original position.
Steps in the pathway include:
- 999 call and outcome category 3 or 4 (appropriate for validation)
- Clinical Validation Team utilise Pathways Clinical Consultation Support (PaCCS)
- Computer-aided dispatch (CAD) portal return for UCR (DX124) [Alternatively, email and telephony referrals remain available for other appropriate cases (outside of DX124 code) and the UCR/single point of access (SPoA) team either accept (pull) or decline case (returning it to ambulance category 3 stack)]
- Case pushed into CAD portal as referral method *SMS and/or email notification sent* – this is for NHS Pathways code DX124 only. The patient retains their original place in the incident queue (should case not be accepted by UCR) – there is a 120 minute time out if no action is taken by UCR.
- UCR/SPoA team either accept (pull) or decline case (returning it to ambulance category 3 stack)
- Possible outcomes include the following:
- Incident accepted by UCR
- Incident rejected by UCR (able to give reason in portal)
- Incident ‘times out’, incident is passed back to WMAS in original place within incident queue
For detailed external user guidance to the WMAS integrated portal, see the UCR FutureNHS page. See video explanation on the Ambulance (999) and Urgent Community Response Webinar Series – Part 1, Digital Opportunities.
Case study for Model A: Cleric Digital Portal at East of England Ambulance Service NHS Trust, enabling transfer of patients to alternative providers
Overview
ICBs in the East of England (EOE) aimed to create an autonomous, interoperable and digital solution across the region.
In October 2022, a web-based platform was developed that can be accessed by alternative providers across all six ICB areas and enables incidents from the ambulance control rooms to be directly streamed and clinically handed over (pre or post clinical validation) to UCR providers.
Patients suitable for UCR are transferred to providers (via the external stack) by clinical staff in the 999 control room, and autonomously (pre-clinical validation) for some pre-determined code sets.
Situation
Although delivering some good outputs and improving MDT working, the manual process that was in place for referring from 999 into UCR (including patient flow huddles) was not sustainable or sufficient for the required pace for referrals.
As part of demand management and shared system risk discussions, colleagues from the regional UEC team, East of England Ambulance Service NHS Trust (EEAST) and the Integrated Care Systems (ICSs) agreed that a model – similar to that utilised by West Midlands Ambulance service – should be adopted.
However, concerns and resistance remained regarding the building of the ‘portal’ and potential issues with cybersecurity, information governance (IG) and clinical governance.
Action
The ICBs across the EOE agreed to pool the region’s funding to build a digital portal/platform to enable UCR providers to directly review and accept appropriate referrals from the ambulance service.
Cybersecurity experts and analysts worked together to address concerns, overcoming IG barriers.
A web-based platform that can be logged into by alternative providers was developed. This allowed incident details to be reviewed and accepted or rejected (while maintaining clinical safety netting back to the patient’s original position in the 999 incident queue).
UCR and EEAST reached an agreement regarding Advanced Medical Priority Dispatch System (AMPDS) codes to be passed onto UCR providers as well as those clinically reviewed and deemed appropriate, including 111 calls.
Results
Agreement on funding from all system partners, the design of the technical product and the rollout of the product to the first three providers were all achieved within 100 days. After eight weeks of the first providers going live, the whole region was live (6 ICSs comprising 14 UCR teams) and able to accept and reject referrals digitally.
There is a stable transfer of calls from all three EEAST EOC, with an average acceptance rate of ~60%.
Referral and acceptance rates are the following: 68 per day (56% accepted in April 2023), 64 per day (56% accepted in May 2023), and 82 per day (60% accepted in June 2023).
For more information, see Ambulance (999) and Urgent Community Response Webinar Series – Part 1, Episode 2 Digital Opportunities.
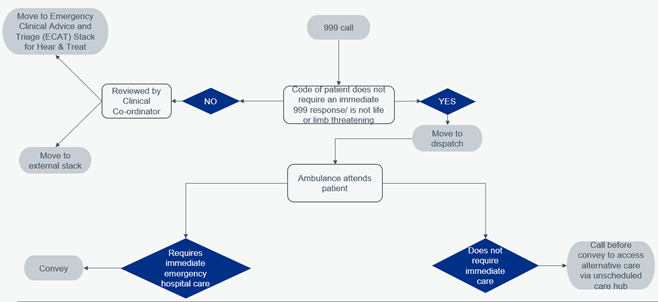
Detailed guidance for Model A: 999 Category 3 to 5 calls to UCR ‘external stack’
The below outlines a pathway for the Cleric Digital Portal at EEAST project, showing 999 call demand management. If calls do not require immediate care, then call before convey can occur to access alternative care via an unscheduled care hub.
The pathway below includes further details on how UCR teams can manage appropriate 999 incidents that are transferred to them via a digital portal.
For more details, see Ambulance (999) and Urgent Community Response Webinar Series – Part 1, Episode 2 Digital Opportunities.
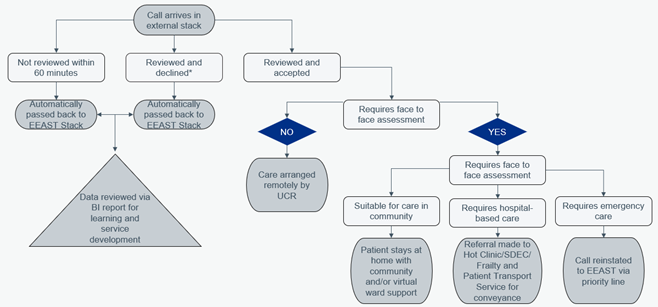
Detailed guidance for Model A: 999 to UCR ‘external stack’
The below outlines a pathway for the Cleric Digital Portal at EEAST project, showing the process utilised for the portal and external stack.
The ICBs across the East of England agreed to pool the region’s funding to build a digital portal/platform to enable UCR providers to directly review and accept appropriate referrals from the ambulance service. Patients suitable for UCR are transferred to providers (via the external stack) by clinical staff in the 999 control room, and autonomously (pre-clinical validation) for some pre-determined code sets.
If a call is not reviewed within 60 minutes or if it is reviewed and declined, then it is automatically passed back to the EEAST stack. If the call is reviewed and accepted, in-person or virtual care can be arranged by UCR teams. Additionally, if hospital-based care or emergency care is required, then UCR teams can ensure the incident is escalated appropriately.
*Note: Any CAD requiring clinical upgrade is phoned back into the Clinical Control Desk via a dedicated line.
For more details, see Ambulance (999) and Urgent Community Response Webinar Series – Part 1, Episode 2 Digital Opportunities.
Case study for Models C and D: Yorkshire Ambulance Service UCR model for Category 3 and 4
Overview
The aim of the pilot was to have quick and easy access to UCR services across the region for the three unplanned care services lines within Yorkshire Ambulance Service (YAS): ambulance crews, EOC and Integrated Urgent Care (IUC).
Situation
YAS receives around 3500 calls per day and covers a population of 5 million over 6,000 square miles.
There are three ICSs and 15 UCR providers – with varying service models and access routes – across the YAS footprint. This results in barriers for YAS when managing roughly 2,000 category 3 and 4 incidents per month that are received and appropriate for UCR.
Action
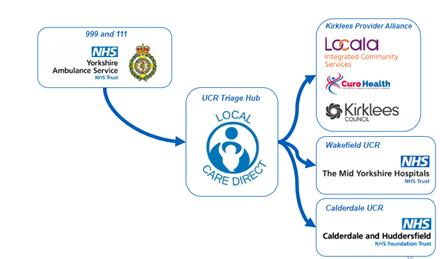
It was agreed that the Yorkshire Ambulance Service would work in collaboration with a GP-led ‘out of hours care provider’ to act as a single point of access for UCR referrals across one ICS area. As a result, a SPoA/‘UCR triage hub’ was established via Local Care Direct, who serve as the access and navigation point between YAS and UCR providers. The hub is staffed by senior clinicians who review calls passed to them by EOC and navigate patients to an appropriate local service. They are also accessible via 111 and provide an advice and referral line for ambulance crews at scene.
Three out of five places in West Yorkshire were a part of the pilot, along with Kirklees, Calderdale and Wakefield UCR teams.
The following were in place to ensure a successful single point of access for UCR teams:
- Infrastructure, networks and staffing – required a hub with strong networks and relationships with local services and the ability to review cases passed to them in a timely manner.
- Approach to clinical risk – required experienced clinicians and a supportive clinical governance structure.
- Clear responsibilities – required understanding of each other’s roles and careful design of clinical handover.
Guiding principles for the pilot included:
- Right care for the patient (not just focusing on volume)
- Collaborative working (dependent on strong professional relationships, trust and respect among teams)
- Adding value to the patient journey (ensuring patient needs are met as early as possible, not just shifting demand)
- Patient safety and reducing risk (calls are kept under clinical oversight at each stage and there is a clear transfer of responsibility between agencies and a mechanism for transferring calls back if required)
As part of the pilot, a ‘no wrong door’ policy was implemented as well to ensure the right actions for the patient could be identified.
Results
As a result, the model is showing acceptance rates of 75% when incidents are passed from 999 into the SPoA across West Yorkshire, with onward acceptance rates of between 55-70% for the three UCR teams using this model.
The average acceptance rates for other UCR services in the YAS footprint are between 10-45%. Additionally, there is a steady increase in referral numbers into the three UCR teams – over 20 per month in November 2021 compared to over 140 per month in February 2023.
For more information, see Ambulance (999) and Urgent Community Response Webinar Series – Part 4 Maximising referrals and Single Point of Access.
Detailed guidance for Models C and D: 999 to UCR pathway (telephone/ ITK)
The below outlines a pathway for the UCR model for category 3 and 4 incidents for Yorkshire Ambulance Service (YAS). YAS worked in collaboration with a GP-led ‘out of hours care provider’ to act as a single point of access for UCR referrals across one ICS area. As a result, a SPoA/‘UCR triage hub’ was established via Local Care Direct, who serve as the access and navigation point between YAS and UCR providers. The hub is staffed by senior clinicians who review calls passed to them by EOC and navigate patients to an appropriate local service.
In a local clinical advice/SPoA model, UCR is ‘one of many’ services available. The below is an example of the SPoA model, which outlines how YAS connects with the UCR triage hub, which provides further connections to local UCR services and provider alliances (Kirklees Provider Alliance – Kirklees Council; CuroHealth; Locala Integrated Community Services. Wakefield UCR (The Mid Yorkshire Hospitals NHS Trust). Calderdale UCR (Calderdale and Huddersfield NHS Foundation Trust).
Some elements in this document are not fully accessible. If you have any issues please contact england.communitycare@nhs.net.
Publication reference: PRN00805