About this guidance
This guidance has been developed by NHS England with the following partners:
- Care Quality Commission
- Centre for Governance and Scrutiny
- Department of Health and Social Care
- Healthwatch England
- Local Government Association
- National Voices
- NHS Confederation
- NHS Providers
- Patients Association
- The Health Creation Alliance
- Integrated Care Systems in Dorset, North East and North Cumbria, Sussex and West Yorkshire.
It also had input from NHS England’s public participation networks and forums. NHS England undertook a public consultation on this guidance during May 2022.
This statutory guidance is made up of a suite of documents – the main body and two annexes:
- Guidance on working with people and communities: this sets out how the guidance should be used; the main legal duties; reasons for working with people and communities; and the leadership needed to realise these benefits. It gives 10 principles to follow to build effective partnerships with people and communities.
- Annex A gives the detail on putting it into practice. It describes the approaches to take for different contexts and how organisations can work together to create genuine and authentic relationships with local communities.
- Annex B explains the public involvement legal duties in more detail and organisations’ responsibilities for working with people and communities.
Further information about all the case studies can be found on the NHS England website. It links to other relevant guidance on integrated care and to further resources on working effectively with people and communities.
Forewords
Edward Argar, Minister of State for Health
People and communities are at the heart of everything the NHS does. Working with people and communities is critical if we are to create a health and care service which offers personalised care, is tailored to the needs of each individual, and which works for everyone.
The Health and Care Act 2022 is designed to enable a more joined up, collaborative system. System leaders from across health and local government told us they wanted to work better together to tackle the big challenges in health and care. The Act ensures that every part of England is covered by an Integrated Care System, which brings together NHS, Local Government and wider system partners to empower them to put collaboration and partnership at the heart of planning. To achieve real impact, we need systems to look beyond those who are typically involved – building partnerships across traditional boundaries and working with people, communities and those who represent them to create real change.
The Act also introduces a new duty on NHS organisations to have regard to the effects of their decisions on the ‘Triple Aim’ of the health and wellbeing for the people of England, quality of services provided or arranged by NHS bodies, and sustainable use of NHS resources. The previous legislative framework directed organisations to work primarily in the best interest of their own organisations and their own immediate patients – but this does not fully support the delivery of integrated, patient-centred care. The new duty requires organisations to think about the interests of the wider system and provides common, system-wide goals that need to be achieved through collaboration. We expect NHS organisations to draw on the knowledge and experience of wider partners, including the voluntary, community and social enterprise (VCSE) sector, local authorities and Healthwatch, alongside their communities when considering how to meet this duty.
By working with people across places, we can better tailor services to meet their needs and preferences, so that they are designed and delivered more effectively. This ensures that locations, opening times, models of care, and patient information are suitable for the communities we serve. Involvement helps us prioritise resources to have the greatest impact; and helps us make better decisions about changing services. Information from involvement activities can be used alongside financial or clinical information to ensure that services are delivered in a way that works for patients and their carers, and can be tailored to the needs of a particular area.
This guidance has been developed in partnership with organisations with experience of working with communities and ensuring their voices are heard in health and care services. It is intended to support health and care systems to build positive and enduring partnerships with people and communities in order to improve services and outcomes for everyone. It is an important next step in realising the benefits of the changes brought about by the Health and Care Act 2022.
Amanda Pritchard, Chief Executive, NHS England
The NHS has always been at the heart of communities. Our hospitals, primary care and community health services provide services to millions of people every week, and a reassuring physical and psychological presence for many more. And never has the NHS been a source of more reassurance and more pride for communities than during the COVID-19 pandemic.
The NHS response to the pandemic – both the initial efforts to protect people from the virus, and especially our delivery of the vaccine programme – has depended in large part on our ability to work with and through communities, not just to spread broadcast messages, but more importantly to understand and overcome barriers to accessing services.
As we move into a new phase, our mission now is to continue recovery and tackle Covid backlogs, reform for the future and build resilience to future pressures. But we must also do so with respect for our patients and communities, ensuring their needs and opinions are central to how we plan, deliver and improve services.
Through Integrated Care Systems (ICSs) – particularly now they are underpinned by statutory Integrated Care Boards (ICBs) and Integrated Care Partnerships (ICPs) – we have an opportunity to further strengthen the relationship with the communities we serve collaboratively, with our Local Government and Voluntary Sector partners. The involvement of our people and communities sits right at the heart of this relationship; we can’t achieve the best outcomes in the most effective way, without working with the people we treat and care for.
The public rightly have high expectations of the NHS. But equally they understand the challenges we face, and want ways to be involved in finding solutions. They have knowledge, skills, experiences and ideas to develop solutions that best meet their needs and support their health and wellbeing. Without insight from people who use, or may use, services, it is impossible to make truly informed decisions about service design, delivery and improvement.
This is particularly important in addressing the health inequalities highlighted by the pandemic; we need to take this opportunity to address the barriers and challenges people experience and ensure we improve the health and wellbeing of the people who need care and support the most. And sometimes this means having the courage to be challenged on our current and historic performance.
Fortunately, we are not starting from scratch. As this guidance sets out, we can build on examples of existing collaboration already taking place in ICSs and on the benefits we have already seen and are seeing from working with communities this way.
Sam Allen, Chief Executive, North East & North Cumbria Integrated Care Board
Listening and involving the communities and citizens we serve through open conversations, to truly make a difference together, and with the aim of reducing inequalities is at the heart of our Integrated Care System. People and communities are why we are here, and we are in service to them. We will draw on their lived experience, wisdom and expertise and involve them as partners in our work.
Adam Doyle, Chief Executive, Sussex Integrated Care Board
I am very pleased to support the guidance for all ICBs and ICSs. The communities that we serve are best placed to help shape and co-produce health and care services that are meaningful to them. I encourage all colleagues to consider this guidance in as they take forward their 5-year strategy in each of their systems.
Patricia Miller, Chief Executive, Dorset Integrated Care Board
I am very privileged to confirm my support for a new approach to involving communities. If we are going to fulfil the ambition of integrated care systems around reducing inequalities, we need to understand the lived experience of our communities and design solutions with them that enable them to live their best lives and thrive. Our citizens should be at the centre of every decision we take.
Kate Shields, Chief Executive, Cornwall Integrated Care Board
Our view about person voice is really clear. Without the voices of our people and our communities we will fail from the start. What we do and how we do it has to be aligned with what matters to the people we serve.
People and their communities will increasingly be engaged in our services re-design across our system and we’ll ensure their voice is heard in our ICB and be at the heart what we do in Cornwall and the Isles of Scilly.
Executive summary
The Health and Care Act 2022 mobilises partners within Integrated Care Systems (ICSs) to work together to improve physical and mental health outcomes. These new partnerships between the NHS, social care, local authorities and other organisations will only build better and more sustainable approaches if they are informed by the needs, experiences and aspirations of the people and communities they serve.
This is statutory guidance for Integrated Care Boards (ICBs), NHS trusts and foundation trusts, and is adopted as policy by NHS England. It supports them to meet their public involvement legal duties and the new ‘triple aim’ of better health and wellbeing, improved quality of services and the sustainable use of resources. It is relevant to other health and care organisations, including local government, to ensure that we work collaboratively to involve people and communities, in ways that are meaningful, trusted and lead to improvement.
The public involvement legal duties require arrangements to secure that people are ‘involved’, and this can be in a variety of ways. ICBs, trusts and NHS England need to be able to demonstrate that they assess whether that the duties apply to decisions about services and, where they do, that they are properly followed. NHS England’s assessment of ICBs’ performance will include how they meet their legal duties. There are also policy requirements for Integrated Care Boards (ICBs), Integrated Care Partnerships (ICPs), place-based partnerships and provider collaboratives to involve people, including in their membership and when developing plans and strategies. Involvement is a contractual responsibility for Provider organisations, including General Practice, as set out in the NHS Standard Contract.
While involving people and communities is a legal requirement, working with them also supports the wider objectives of integration including population health management, personalisation of care and support, addressing health inequalities and improving quality. The legal duties provide a platform to build collaborative and meaningful partnerships that start with people and focus on what really matters to our communities. However, the ambition is for health and care systems to build positive, trusted and enduring relationships with communities in order to improve services, support and outcomes for people.
There are clear benefits to working in partnership with people and communities. It means better decisions about service changes and how money is spent. It reduces risks of legal challenges and improves safety, experience and performance. It helps address health inequalities by understanding communities’ needs and developing solutions with them. It is about shaping a sustainable future for the NHS that meets people’s needs and aspirations.
Senior leaders have a particular role in making this happen. They should ensure that they:
- understand and act on what matters to people
- demonstrate how their organisations meet met the legal duties to involve
- work with partners to put people are at the centre of everything they do
- ensure there are resources for their organisations to do this work effectively
- spend time personally listening to and understanding their local communities.
Accessible diagram text:
The 10 principles for working with people and communities are:
- Centre decision-making and governance around the voices of people and communities
- Involve people and communities at every stage and feed back to them about how it has influenced activities and decisions
- Understand your community’s needs, experiences, ideas and aspirations for health and care, using engagement to find out if change is working
- Build relationships based on trust, especially with marginalised groups and those affected by health inequalities
- Work with Healthwatch and the voluntary, community and social enterprise sector
- Provide clear and accessible public information
- Use community-centred approaches that empower people and communities, making connections what works already
- Have a range of ways for people and communities to take part in health and care services
- Tackle system priorities and service reconfiguration in partnership with people and communities
- Learn from what works and build on the assets of all health and care partners – networks, relationships and activity in local places.
This guidance is structured around 10 principles. These have been developed from good practice already taking place, and will help organisations achieve the benefits of effective working with people and communities:
Applying the principles means taking a variety of approaches to working with people and communities, depending on context and objectives. Regardless of the approach used, organisations should start with existing insight about the needs and experiences of their communities, and work with partners that already have links to them. They should also consider taking community-centred approaches – ones that recognise the strengths within communities and that build on existing assets that support people’s health.
To ensure legal duties are met, all approaches should be fair, proportionate and have regard to equalities, so that all relevant groups can take part. They should be designed to take account of the contexts that people live their lives in. This means building trust, safety, and shared understanding.
Integrated care gives an opportunity for the NHS to collaborate with partners on working with communities. This is both within the NHS (for example, commissioners and providers coordinating their involvement activities so they do not duplicate), and between the NHS and other partners – including local authorities, social care providers, Healthwatch and voluntary, community and social enterprise (VCSE) sector organisations that already have links to and knowledge of communities.
Terminology
In this guidance we talk about working in partnership with people and communities. We use this phrase to cover a variety of approaches such as engagement, participation, involvement, co-production and consultation. These terms often overlap, mean different things to different people, and sometimes have a technical or legal definition too.
By people we mean everyone of all ages, their representatives, relatives, and unpaid carers. This is inclusive of whether or not they use or access health and care services and support. Communities are groups of people that are interconnected, by where they live, how they identify or shared interests. They can exist at all levels, from neighbourhood to national, and be loosely or tightly defined by their members.
Community-centred approaches recognise that many of the factors that create health and wellbeing are at community level, including social connections, having a voice in local decisions, and addressing health inequalities.
We refer to health and care systems as all organisations working to improve people’s physical and mental health, nationally and locally, including the NHS, local authorities and social care providers. We use the term trusts to refer to NHS trusts and NHS foundation trusts.
Integrated care systems (ICSs) are partnerships of health and care organisations that come together to plan and deliver joined up services, and to improve the health of people who live and work in their area.
Each ICS consists of an:
- Integrated care board (ICB): a statutory organisation that brings the NHS together locally to improve population health and care
- Integrated care partnership (ICP): a statutory committee (established by the ICB and relevant local authorities) that is a broad alliance of organisations and representatives concerned with improving the care, health and wellbeing of the population.
- ICSs also include place-based partnerships and provider collaboratives. The King’s Fund animation explains more about the new organisations in the NHS and how they can collaborate with partners to deliver joined-up care.
Introduction
This new guidance sets the ambition and expectations for how integrated care boards (ICBs), NHS trusts and foundation trusts should work in partnership with people and communities in this new collaborative environment. It is also adopted as policy by NHS England and will be useful for local authorities and other partners to understand the statutory duties on NHS England, ICBs and trusts.
Many colleagues across these organisations already recognise the value of working with people and communities, and the experiences and knowledge that they contribute to improving health and care services. People and communities have the skills and insight to transform how health and care is designed and delivered. Working with them as equal partners helps them take more control over their health and is an essential part of securing a sustainable NHS.
This guidance aims to spread effective practice across all systems by building on the expertise and experience that exists and approaches already being applied (Health and wellbeing: a guide to community-centred approaches, Community-centred public health: taking a whole system approach). It provides practical advice and signposts to further information including training and resources. It also shares learning from areas where partnership is already making the vision a reality and makes clear the difference that working with people and communities makes.
The response to COVID-19 saw communities mobilise themselves to support family, friends and neighbours including those self-isolating and to encourage vaccine take-up; developing approaches that fitted local circumstances and needs (UKHSA: The community response to coronavirus (COVID-19), Health Creation Alliance: Learning from the community response to COVID19; how the NHS can support communities to keep people well). Communities worked alongside health and care partners to find innovative solutions to new challenges (National Voices: Unlocking the digital front door – keys to inclusive healthcare). There was agreement between communities and the organisations that provide services about the shared priorities. This led to joint working often with communities leading and systems responding to the needs and preferences voiced by people.
This learning should be transferred to help meet other challenges that health and care services face by listening to people and working with them to decide what will work best for them. The pandemic brought into sharp focus the disproportionate impact on certain population groups. A key part of how we address physical and mental health inequalities is to begin by listening to diverse communities and working with their knowledge, commitment and resources to improve access, experience and health outcomes.
Who is this guidance for?
This is statutory guidance issued by:
- NHS England for ICBs under section 14Z51 of the National Health Service Act 2006 in relation to their ‘public involvement’ duty under section 14Z45
- the Secretary of State for Health and Social Care for NHS trusts and NHS foundation trusts under section 242(1G) in relation to their ‘public involvement’ duty under section 242(1B).
It replaces the 2017 statutory guidance for commissioners, the 2008 statutory guidance for trusts and the 2021 implementation guidance for ICSs.
As statutory guidance, this means that ICBs and trusts must have regard to this guidance. They must consciously consider the guidance and, where appropriate, be able to explain any substantial departure from it.
NHS England has its own ‘public involvement’ duty (section 13Q of the National Health Service Act 2006). It is NHS England’s policy to have regard to this guidance in the same way that ICBs and trusts are required to as statutory guidance.
NHS England is also required under section 14Z59 to conduct a performance assessment of ICBs that must (amongst other things) include how well the ICB has discharged its public involvement duty.
While it is statutory guidance for the ICBs and trusts, it supports the vision of integrated care where organisations work in genuine partnership. It is therefore relevant to the entire health and care system.
Accessible diagram text:
This guidance has the status of:
- Policy for NHS England, under its public involvement duty in the NHS Act 2006, as amended by the Health and Care Act 2022
- Statutory guidance for Integrated Care Boards, under its public involvement duty in the NHS Act 2006, as amended by the Health and Care Act 2022
- Statutory guidance for NHS trusts and foundation trusts, under their public involvement duty in the NHS Act 2006, as amended by the Health and Care Act 2022
- Good practice for other partners in Integrated Care Systems.
For ICS partners it will be used by:
- Integrated care partnerships (ICPs) to help inform their strategies, during the development of which they must involve people
- place-based partnerships as a guide on how they involve people in decision-making processes and engage them on plans for change
- provider collaboratives, clinical networks and cancer alliances, as it supports working with people on improving whole care pathways across multiple places and systems
- health and care partners involved in research, as the guidance supports working with communities to identify research needs (both locally and across care pathways), and to be involved in shaping research studies that align with what matters to communities
- Primary care networks for their work at neighbourhood level with local communities, to understand local needs and reduce health inequalities.
It will also be of interest to other partners within health and care systems as good practice, including local authorities – in particular health overview and scrutiny committees (HOSCs), health and wellbeing boards (HWBs) and other local democratic structures – voluntary community and social enterprise (VCSE) sector organisations, social care providers, local Healthwatch and patient groups. Finally, it is relevant to people interested in how their NHS should work with them.
This guidance complements separate guidance on involving people in their own health and care (there are legal duties on involving people in their own health and care, covered in separate guidance. An update to this guidance will be published in 2022).
Setting the ambition
The ambition is for health and care systems to build positive, trusted and enduring relationships with communities to improve services, support and outcomes for people.
This means a health and care system that:
- listens more and broadcasts less
- undertakes engagement which is ongoing and iterative, not only when proposing changes to services
- is focussed on and responds to what matters to communities and prioritises hearing from people who have been marginalised and those who experience the worst health inequalities
- works with and through existing networks, community groups and other places where people identify and feel comfortable
- develops plans and strategies that are fully informed and understood by people and communities
- learns from people and communities, using insight, data and a range of approaches to understand whether their needs are being met and what their priorities, ambitions and ideas are
- provides clear feedback about how people’s involvement leads to improvement
- invests in different approaches to working with people and communities, enabling them to contribute meaningfully in ways that are safe and accessible for them
- shares power with communities so they have a greater say in how health services are shaped and can take responsibility to improving their health.
Legal duties and responsibilities
Public involvement legal duties
The legal duties on public involvement require organisations to make arrangements to secure that people are appropriately ‘involved’ in planning, proposals and decisions regarding NHS services.
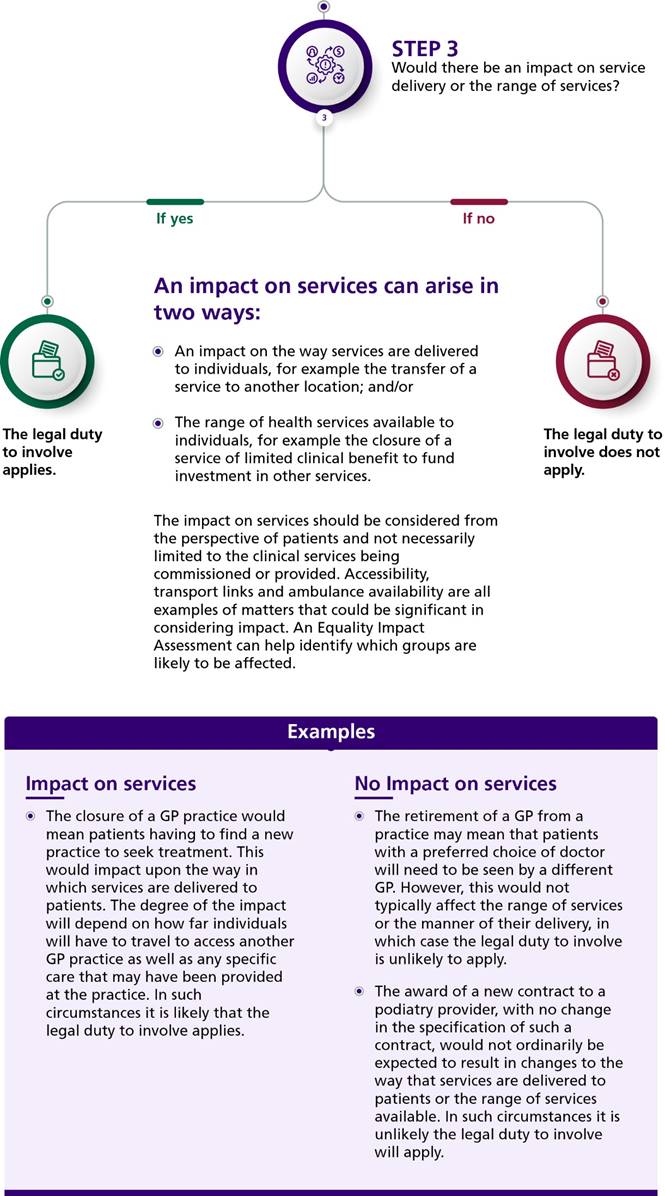
Annex B provides the detail on these legal duties, when they are likely to apply and how they can be met. Key requirements of ICBs, trusts and NHS England include that they:
- assess the need for public involvement and plan and carry out involvement activity
- clearly document at all stages how involvement activity has informed decision-making and the rationale for decisions
- have systems to assure themselves that they are meeting their legal duty to involve and report on how they meet it in their annual reports.
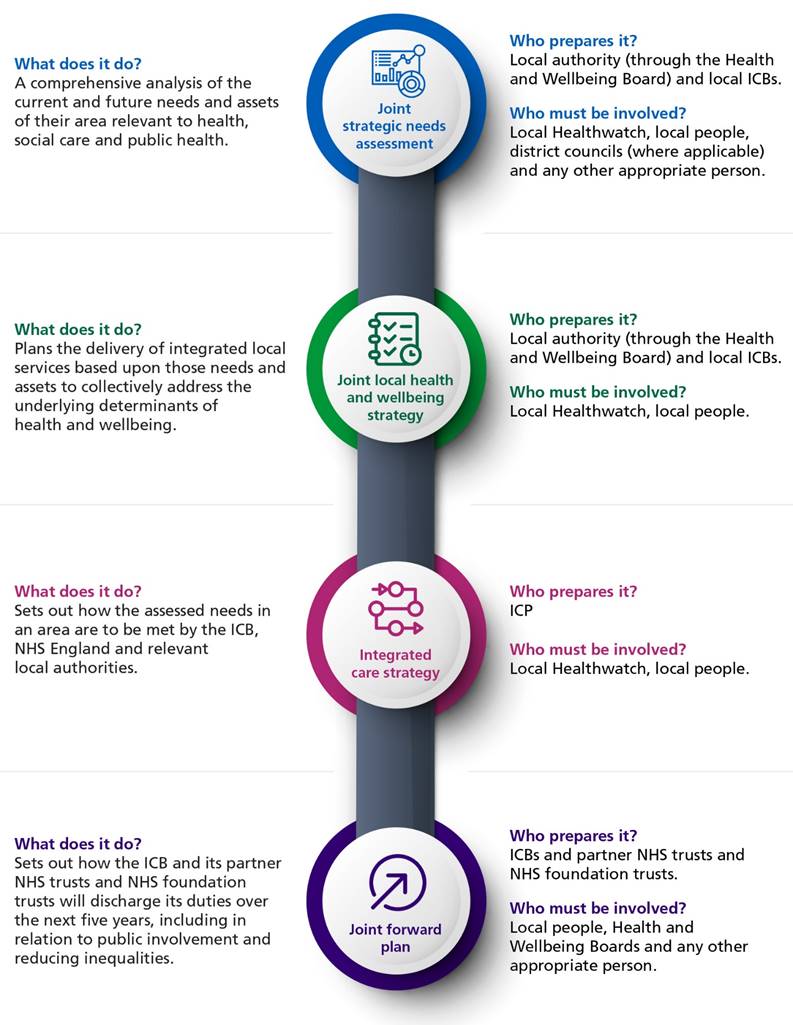
ICPs, place-based partnerships and provider collaboratives also have specific responsibilities towards participation, summarised below. There are statutory requirements for ICBs and ICPs to produce strategies and plans for health and social care, each with minimum requirements for how people and communities should be involved (see Annex B).
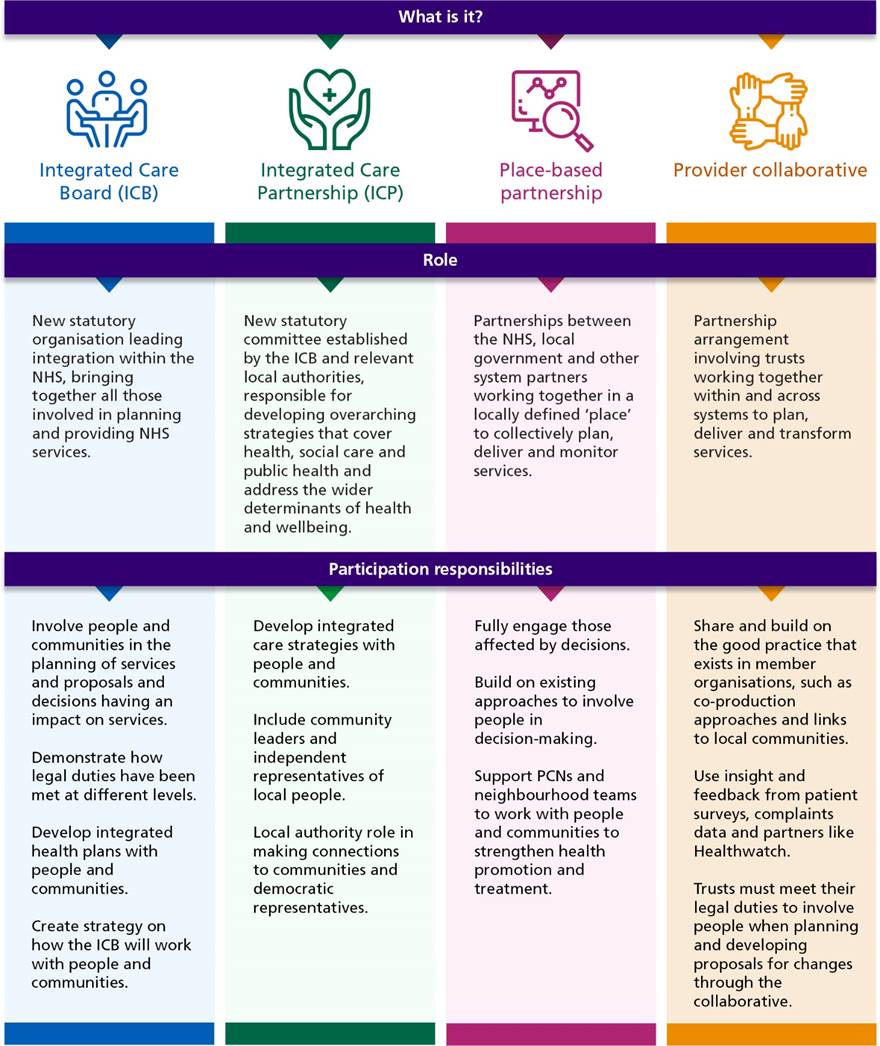
Accessible diagram text:
Different parts of the ICS have their own participation responsibilities. The roles of the new organisations and partnerships are described in this diagram along with their participation responsibilities.
Integrated care board (ICB)
Role: New statutory organisation leading integrating within the NHS, bringing together all those involved in planning and providing NHS services.
Participation responsibilities:
- Involve people and communities in the planning of services and proposal and decisions having an impact on services
- Demonstrate how legal duties have been met at different levels
- Develop integrated health plans with people and communities
- Create strategy on how the ICB will work with people and communities
Integrated care partnership (ICP)
Role: New statutory committee established by the ICB and relevant local authorities, responsible for developing overarching strategies that cover health, social care and public health and address the wider dominants of health and wellbeing.
Participation responsibilities:
- Develop integrated care strategies with people and communities
- Include community leaders and independent representatives of local people
- Local authority role in making connections to communities and democratic representatives
Place-based partnership
Role: Partnerships between the NHS< local government and other system partners working together in a locally defined ‘place’ to collectively plan, deliver and monitor services
Participation responsibilities:
- Fully engage those affected by decisions
- Build on existing approaches to involve people in decision-making
- Support PCNs and neighbourhood teams to work with people and communities to strengthen health promotion and treatment
- Provider collaborative: Partnership arrangement involving trusts working together within and across system to plan, deliver and transform services
Participation responsibilities:
- Share and build on the good practice that exists in member organisations, such as co-production approaches and links to local communities
- Use insight and feedback from patient surveys, complaints data and partners like Healthwatch
Trusts must meet their legal duties to involve people when planning and developing proposals for changes through the collaborative
The triple aim duty
NHS England, ICBs, NHS trusts and NHS foundation trusts are subject to the new ‘triple aim’ duty in the Health and Care Act 2022 (sections 13NA, 14Z43, 26A and 63A respectively). This requires these bodies to have regard to ‘all likely effects’ of their decisions in relation to three areas:
- health and wellbeing for people, including its effects in relation to inequalities
- quality of health services for all individuals, including the effects of inequalities in relation to the benefits that people can obtain from those services
- the sustainable use of NHS resources.
Effective working with people and communities is essential to deliver the triple aim, as shown in the diagram below.
Other relevant legal duties
Effective working with people and communities will also inform and support organisations in meeting other legal duties:
- Equalities: The Public Sector Equality Duty (PSED) of the Equality Act 2010
- Health inequalities: The National Health Services Act 2006
- Social value: Public Services (Social Value) Act 2012.
Annex B explains how working with people and communities can help meet these duties.
The triple aim duty and participation
Accessible diagram text:
Working with people and communities will help to meet the triple aim duty:
1. Better population health and wellbeing:
- Health inequalities: Improve understanding of the experiences, perspectives and needs of people and communities that experience the worst health inequities, including inclusion health groups, and working together, beyond clinical boundaries, to develop solutions
- Data and Insight: Accessing data and insight including qualitative data from communities and the VCSE sector, to build knowledge of the communities we service, and the impact of wider dominants of health
- Assets: Understanding the assets in our communities that will help to improve population health and wellbeing and to strengthen understanding of community needs and perspectives
2. Better quality of services for individuals:
- Designing services: Designing services in partnership with people so they meet their needs and preferences and reflect experience
- Approaches and solutions: Jointly develop improvement approaches and solutions to concerns about quality, including patient safety and experience
3. Improved efficiency and sustainability:
- Prioritising resources: Prioritising resources to where they have the greatest impact based on the needs, knowledge and experience of communities
- Understanding barriers: Understanding the barriers to access which impact on the efficiency and sustainability of services and work together in solutions to address them.
Why work in partnership?
Accessible diagram text:
There are several benefits of partnership with people and communities, shown in this diagram:
- Improved health outcomes
- Value for money
- Better decision-making
- Improved quality
- Accountability and transparency
- Participating for health
- Meeting legal duties
- Addressing health inequalities
The benefits of partnership
Improved health outcomes
Working in partnership with people and communities creates a better chance of creating services that meet people’s needs, improving their experience and outcomes. People have the knowledge, skills, experiences and connections services need to understand in order to support their physical and mental health. Partnership working contributes to defining ‘shared outcomes’ that meet the needs of their communities (GOV.UK: Health and social care integration: joining up care for people, places and populations. This is particularly relevant in the context of population health management and reducing health inequalities.
Value for money
Services that are designed with people and therefore effectively meet their needs are a better use of NHS resources. They improve health outcomes and reduce the need for further, additional care or treatment because a service did not meet their needs first time.
Better decision-making
We view the world through our own lens and that brings its own judgements and biases. Business cases and decision-making are improved when insight from local people is used alongside financial and clinical information to inform the case for change. Their insight can add practical weight and context to statistical data, and fill gaps through local intelligence and knowledge. Challenge from outside voices can promote innovative thinking which can lead to new solutions that would not have been considered had the decision only been made internally.
Improved quality
Partnership approaches mean that services can be designed and delivered more appropriately, because they are personalised to meet the needs and preferences of local people. Without insight from people who use, or may not use, services, it is impossible to raise the overall quality of services. It also improves safety, by ensuring people have a voice to raise problems which can be addressed early and consistently.
Accountability and transparency
The NHS Constitution states: ‘The system of responsibility and accountability for taking decisions in the NHS should be transparent and clear to the public, patients and staff.’ Organisations should be able to explain to people how decisions are made in relation to any proposal – and how their views have been taken onboard. Transparent decision-making, with people and communities involved in governance, helps make the NHS accountable to communities. Engaging meaningfully with local communities build public confidence and support as well as being able to demonstrate public support for proposals.
Participating for health
Being involved can reduce isolation, increase confidence and improve motivation towards wellbeing. Individuals’ involvement in delivering services that are relevant to them and their community can lead to involvement at a service level and to more formal volunteering roles and employment in health and care sectors. It is well recognised that doing something for others and having a meaningful role in your local community supports mental health. Getting involved can be health creating – being part of a community and being in control is good for our health.
Meeting legal duties
Although this should not be the primary motivation, failure to meet the relevant legal duties risks legal challenge, with the substantial costs and delays that entails, and damage to relationships and trust and confidence between organisations, people and communities.
Reducing health inequalities
Joint solutions
Tackling the causes and consequences of health inequalities is a central priority for health and care systems. It is one that has been given new momentum by the disproportionate impact of the COVID-19 pandemic on those people and communities who already face the worst inequalities (Public Health England: COVID-19: review of disparities in risks and outcomes).
Health inequalities can be reduced by jointly identifying solutions, developed in partnership with people using community-centred approaches. This builds on the approach of CORE20PLUS5 – a national framework that helps define the population groups in each system experiencing health inequalities. Hearing their experiences and understanding the barriers these groups face in accessing care and treatment is an important part of addressing unequal access to services. From there we can work with them to co-create community-centred solutions.
Focussing engagement on groups who have been marginalised and excluded helps tackle the inverse care law, whereby those with the most need for services are the least likely to receive them and least likely to feel safe to participate. By building engagement approaches that include people who are currently not well supported by existing services, systems can design models of care that meet the needs of all their communities and address inequalities. This includes recognising that some communities may require different approaches to meet their needs. Population groups facing the worst health inequalities are often the most disempowered, with the lowest levels of various markers for control, belonging and wellbeing. Working with the most marginalised groups needs to be based on building trust and connection as an important foundation for improving their health outcomes.
Collaborative approaches
The NHS cannot do this alone. Wider determinates of health – for example, poverty, discrimination, educational attainment, employment and housing – relate to barriers that the NHS by itself cannot overcome. Collaboration brings an opportunity to capture a holistic picture of inequalities and work with people and communities on joined up solutions. Local authorities and other partners are well placed to understand the social determinants of health and how they can be addressed together.
There is also an opportunity to share power and strengthen relationships with people that experience inequalities. They can be involved in agreeing ambitions, shared outcomes and plans to improve health outcomes through commissioning and service delivery. For example, they could work with the groups identified through CORE20PLUS5 to make decisions collaboratively on how to address their specific health and care needs. This helps ensure intended objectives are relevant, achievable, and based on skills, experiences and what really matters to the people they are intended to help. This means proactively seeking their participation and using approaches that enable diverse communities to contribute and take more control.
It is important to recognise that boosting the power of communities to make decisions and encouraging them to take more responsibility has a strong health creating effect. If the NHS can support people and communities to take more control, they will be helping to improve health and address inequalities (NHS England will publish guidance on addressing health inequalities in 2022/23).
Building a culture of partnership
Leadership is vital to achieving these benefits. Communities and staff will look to system leaders to role model a culture of partnership, to demonstrate that their views are taken seriously and that they prioritise giving people a genuine part in decisions about how services are designed and delivered (Kings Fund: Understanding integration: How to listen to and learn from people and communities. Leadership can be a joint endeavour, with leaders from systems and from within communities working together.
Collaborative and inclusive leadership means seeing participation as everybody’s business and fundamental to meeting shared objectives. This means leadership teams that value participation as part of all their roles and seeking assurance that it is happening within their organisation, rather than being delegated to one individual who is accountable for ensuring it happens. This sets the tone for practitioners and communities to work, learn, and improve together. It creates the culture to enable staff to innovate and collaborate in new ways and gives them permission and autonomy to try things out, to learn and to celebrate success.
This requires a commitment for sufficient funding, resources, training and support to do so effectively, and allowing time to build trust and relationships. This will support working with all groups of people and communities, including those whose voices are not currently heard in a meaningful way.
Senior leaders and decision-makers will want to make sure that they understand and take action on what matters to people in the decisions that they are responsible for and to work with partners to really make sure that people are at the centre of everything they do. Spending time with local communities, listening to and building understanding about their experiences is essential. This visible leadership helps to unlock potential and demonstrates that working in partnership with people is everyone’s business.
Ten principles for working with people and communities
The guidance is based on ten principles that will help health and care organisations develop their ways of working with people and communities, depending on local circumstances and population health needs.
They are intended to be a golden thread running throughout systems, whether activity takes place within neighbourhoods, in places, across system geographies or nationally.
They have been developed from good practice already taking place and are intended to support existing approaches which may exist locally. They will form the basis of NHS England’s assessment of how well integrated care boards meet their legal duties (see 12.1 below). However, they can be used by all organisations to develop effective ways of working in partnership.
1. Ensure people and communities have an active role in decision-making and governance
- Build the voices of people and communities into governance structures so that people are part of decision-making processes
- Recognise the collective responsibility at board level for upholding legal duties, bringing in lay perspectives but avoiding creating isolated, independent voices
- Make sure that boards and communities are assured that appropriate involvement with relevant groups has taken place (including those facing the worst health inequalities); and that this has an impact on decisions.
- Ensure that effective involvement is taking place at the appropriate level, including system, place and neighbourhood, and that there is a consistency and coordination of approaches
- Support people with the skills, knowledge and confidence to contribute effectively to decision-making and governance
- Make sure that senior leaders role model inclusive and collaborative ways of working.
Case study: Building a consistent approach to involvement across North West London integrated care system (ICS)
In December 2019, North West London ICS launched the EPIC (Engage – Participate –Involve – Collaborate) programme to try to address some of the challenges around how it works with residents. A key strand of the programme was co-production of a future, best practice approach to resident involvement in the CCG and future ICS. Despite some very good practice, the public had not previously been involved systematically in shaping the ICS’s work and many communities were not being effectively engaged. The ICS’s approach now includes:
- ‘Collaborative spaces’ -open meetings where health and care colleagues come together with people to discuss health and care issues
- Outreach with all our communities including targeted involvement of groups we have not successfully involved in the past
- Lay partners to sit on key programmes/workstreams as appropriate.
This approach is assured via North West London’s involvement charter.
2. Involve people and communities at every stage and feed back to them about how it has influenced activities and decisions
- Take time to plan and budget for participation and start involving people as early as possible so that it informs options for change and subsequent decision-making
- Involve people and communities on a continual basis, as part of meaningful partnerships, rather than taking a stop-start approach when decisions are required. As a result, there will be much greater, ongoing awareness of the issues, barriers, assets and opportunities
- Be clear about the opportunity to influence decisions; what taking part can achieve; and what is out of scope
- Record and celebrate people’s contributions and give feedback on the results of involvement, including changes, decisions made and what has not changed and why
- Keep people informed of changes that take place sometime after their involvement and maintain two-way dialogue so people are kept updated and can continue to contribute
- Take time to understand what works and what could be improved.
3. Understand your community’s needs, experiences, ideas and aspirations for health and care, using engagement to find out if change is working
- Use data about the experiences and aspirations of people who use (and do not use) health and care services, care and support; and have clear approaches to using this information and insight to inform decision-making and quality governance
- Work with what is already known by partner organisations, from national and local data sources, and from previous engagement activities including those related to the wider determinants of health
- Share data with communities and seek their insight about what lies behind the trends and findings. Their narrative can help inform about the solutions to the problems that the data identifies
- Understand what other engagement might be taking place on a related topic and take partnership approaches where possible, benefiting from your combined assets. This will also help avoid ‘consultation fatigue’ amongst communities, by working together in an ongoing dialogue that is not limited by organisation boundaries
- Build on existing networks, forums and community activities to reach out to people rather than expecting them to come to you. Be curious and eager to listen; don’t assume you know what people will say or what matters to them
- Involve people in designing evaluation frameworks and deciding what ‘good’ looks like, using measures of change that matter to them. Include evidence collection in engagement plans to demonstrate the impact that working with people and communities has had.
Case study: Community conversations on public mental health
Poor mental health is a major challenge facing London, and the prevalence of mental health problems is often much higher in the communities facing the deepest inequalities.
Recognising this, in 2017/18 the Mental Health Foundation and Thrive LDN co-ordinated 17 community conversations across half of the city’s boroughs, involving more than 1000 Londoners, with the aim of finding out how local systems could best implement a public mental health approach.
These conversations went far beyond the consultations that communities had previously seen on mental health services: as well as getting ideas for providing ‘services when and where needed’ they were designed to find ways of improving the determinants of mental health to enable prevention for everyone, early intervention for those at risk, and effective support for those who need it.
Evaluation of these conversations by the Mental Health Foundation found several ways that they tangibly influenced public mental health initiatives in the areas where they were held. For example:
- in Hackney, they brought together public health and planning teams around the design of a new leisure centre to ensure high quality community space
- in Enfield, the community conversation influenced the plans for a major regeneration, prompting greater focus on creating ‘mentally healthier’ places with better access to green and community space.
The community conversations also led to the development of a network of mental health champions across London and new job roles, including a specialist public mental health position and a voluntary sector liaison post.
More information on the process and results are in the Londoners Said and Londoners Did reports from the Mental Health Foundation.
4. Build relationships based on trust, especially with marginalised groups and those affected by inequalities
- Proactively seek participation from people who experience health inequalities and poorer health outcomes, connecting with trusted community leaders, organisations and networks to support this
- Consider how to include people who do not use services, whether because they do not meet their needs or are inaccessible, and reach out to build trust and conversations about what really matters to them
- Work with people and communities from the outset, taking time to build trust, listen and understand what their priorities are
- Be honest and realistic about what is in scope and where they can set the agenda for change
- Tailor your approach to engagement to include people in accessible and inclusive ways so you include those who have not taken part before. This includes recognising that some communities will not feel comfortable discussing their issues and needs within wider meetings, so may need bespoke approaches. They may need additional support to take part including reimbursements for their time
- When reporting on engagement activity, explain the needs and solutions for different communities rather than simply aggregating all data and feedback together. This also supports equality impact assessments.
Case study: Embedding Cultural Awareness in Maternity and Neonatal Care
For over 10 years, the East of England Local Government Association via the Strategic Migration Partnership has been delivering a wide range of engagement and integration projects with ethnic minority groups in the East of England.
They understand the challenges health and care staff can experience when supporting a wide range of culturally diverse and dynamic groups. This can include language barriers, a reluctance to engage with professionals and a mistrust of the NHS system because of past relationships with authorities in countries of origin. They also understand that for many ethnic minority groups, healthcare in the UK can be seen as confusing and often inaccessible due to a lack of appropriate information and a reliance on people having access to digital devices.
In response to the challenges faced by the healthcare professionals and ethnic minority groups, they have worked to create cultural awareness workshops, which are both effective and efficient at ensuring the development of sustainable maternity and neonatal care pathways for different groups across the region.
The workshops were an opportunity to identify engagement issues specific to the East of England and delivered by members and advocates of ethnic minority groups considered hard to engage with across the region, including LGBTQ+ groups, African groups, Orthodox Jewish groups, Gypsy and Traveller groups, Roma groups, South Asian groups, Eastern European groups, Asylum Seekers and Refugees.
5. Work with Healthwatch and the voluntary, community and social enterprise sector as key partners
- Build strong partnerships with Healthwatch and the Voluntary Community and Social Enterprise sector to bring their knowledge and reach into local communities. Work with them to facilitate involvement from different groups and develop engagement activities
- Understand the various types of Voluntary Community and Social Enterprise sector organisations in your area, from larger national charities to local user-led groups, their links to different communities and how the NHS can connect with them
- Recognise that resources can be limited and that organisations may need financial support and capacity building to take on partnership roles
- When commissioning other organisations to work with communities, ensure that decision-makers remain personally involved and hear directly what people or their representatives have to say.
6. Provide clear and accessible public information
- Develop information about plans that is easy to understand, reflecting the communication needs of local communities and testing information where possible
- Where accessible formats such as easy read and translations into other languages are used, these should be ready at the same time as other materials
- Providers of NHS care must meet their requirements under the Accessible Information Standard for the information and communication needs of people in their own care. The same principles can be applied for public information so that it is clear and easy to understand, for example, taking steps to ensure that people receive information which they can access and understand, and receive communication support if they need it
- Be open and transparent in the way you work, being clear about where decisions are made and the evidence base that informs them. Provide people with an honest picture of the health and care landscape, along with resource limitations and other relevant constraints. Where information must be kept confidential, explain why
- Make sure you describe how communities’ priorities can influence decision-making, including how people have influenced research priorities or planning for future health care ambitions; and how people’s views are considered. Also ensure that you regularly feedback to those who shared their views and others about the impact this has made
- Provide feedback in inclusive and accessible ways, that suit how people want or are able to receive it
- Make sure information on opportunities to get involved is clear and accessible and encourage a wide range of people to take part; including targeting information at particular communities who might traditionally not be involved.
7. Use community-centred approaches that empower people and communities, making connections to what works already
- Support and build on existing community assets, such as activities and venues which already bring people together such as faith communities, schools, community centres, local businesses and community-centred services, including those that involve link workers, community champions and peer support volunteers.
- Adopting asset based approaches to community development to understand how these assets can support people’s physical and mental health. Link with local authorities where they already have approaches in place and consider jointly funding.
- Build trust and meaningful relationships in a way that people feel comfortable sharing ideas about opportunities, solutions and barriers. Design, deliver and evaluate solutions together that are built around existing community infrastructure.
- Recognise existing volunteering and social action that supports physical and mental health and create the sustainable conditions for them to grow (for example, by providing places to meet, small grants or community development support).
Case study: working at neighbourhood level in Morecambe Bay to reduce health inequalities
This project was designed to explore what access issues and inequalities were being experienced by a range of health inclusion and other key groups. It started with the primary care networks (PCNs) using population health management approach to identify groups of patients that may experience health inequalities. There was then an asset mapping process with each PCN group supported to identify local people and organisations that could potentially support with the work. Next, engagement took place with groups of patients and local people including young people, adults with learning disabilities and their carers and workers from migrant communities. A workshop supported people to plan how they would share what they had found and what they planned to do next with the communities they had focused on.
The PCNs have changed their services based on what they found through this work. For example, for people with learning disabilities, annual learning disability health checks are being reassessed to improve uptake and providing care in a way that makes patients feel comfortable, cared for and listened to.
Overall, participants report feeling more confident around how to engage with their local communities, and how the process can be applied to other groups experiencing health inequalities to inform other improvement initiatives.
It was undertaken by Morecambe Bay CCG, North Cumbria ICS, Morecambe Bay PCNs, Co-create and other local partners.
8. Have a range of ways for people and communities to take part in health and care services
- Choose the ways of working with people and communities depending on the specific circumstances, ensuring they are relevant, fair and proportionate. Use a combination of approaches where appropriate. The approach that gives the greatest opportunity for people to take part in decision-making should be used that is suitable for the situation.
- Design activities to take place at times and in ways that encourages participation and consider the support people may need to take part, including reimbursements for their time and expenses
- Recognise that people are busy and have other priorities such as work and caring responsibilities. Ensure that there are different ways to get involved with varying levels of commitment
- Include approaches such as co-production where professionals share power and have an equal partnership with people to plan, design and evaluate together
- Using different approaches can bring in a wider range of voices beyond those who already contribute and ensure findings are more representative of the whole population
- Have clear, achievable and actionable goals that can comprise both quick wins to inspire people, as well as longer term goals that may be more challenging to achieve but may ultimately be more transformative
- Where decisions are genuinely co-produced, then people with lived experience work as equal partners alongside health and care professionals (those with learnt experience), jointly agreeing issues and developing solutions.
Case study: Co-producing a new model of community mental health support
In Somerset, the NHS, local authority and Voluntary Community and Social Enterprise sector partners have worked with people with lived experience of mental illness to co-produce community mental health services. The involvement of experts by experience as equal partners has been embedded across the programme from the beginning, and the lived experience perspective they represent has influenced key decisions about the service. They co-designed the Open Mental Health model, whereby 24/7 support is available to adults in Somerset who are experiencing mental health issues. Provision is offered through an alliance of provider organisations from the Voluntary Community and Social Enterprise sector, NHS and social care working in partnership. Experts by experience have an ongoing role as partners in the governance, continuous development and evaluation of the service.
There is more about Open Mental Health on the Rethink Mental Illness website.
9. Tackle system priorities and service reconfiguration in partnership with people and communities
- People who use health and care services have knowledge and experience that can be used to help make services better. They can put forward cost-effective and sustainable ideas that clinicians and managers have not thought of, which inform planning for future healthcare development
- Communities often have longer memories than the professionals who may change roles and move. Understanding the local history of change that communities have experienced helps to learn and build trust with people
- When people better understand the need for change, and have been involved in developing the options, they are more likely to advocate the positive outcomes and involve others in the process.
10. Learn from what works and build on the assets of all health and care partners – networks, relationships and activity in local places
- Collaborate with partners across your system to build on their skills, knowledge, connections and networks
- Reduce duplication by understanding what is already known and what has already been asked, before designing the approach to engagement.
- Learn from approaches taken elsewhere in the country and how they can be adapted and applied locally
- Plan together across systems so that partnership work with people and communities is co-ordinated, making the most of partners’ skills and networks.
Annex A: Implementation
A1 – Different ways of working with people and communities
This chapter sets out a variety of approaches to working with people and communities however there is no ‘one size fits all’. The options for doing so will vary depending on the context and objectives, and there needs to be flexibility depending on the aims and scale of the programme.
A blended approach can also work well, with different approaches and ways of working used at different stages of a project to build a more detailed picture of what matters to people and what improvements can be made.
Some of the main ways to work with people are set out below. They each offer different levels of involvement, from sharing information through to more extensive ways of working such as co-design and co-production, where there is a greater opportunity for people to have influence. As a general principle, partnership should be achieved by using the most effective approach (or combination of approaches) as is feasible and suitable in any given situation.
Starting with people means going to the neighbourhoods and places where they already are and begin by listening to them about their priorities. From this we can design approaches that should ensure relevant communities can take part, recognising that different approaches work better for different groups.
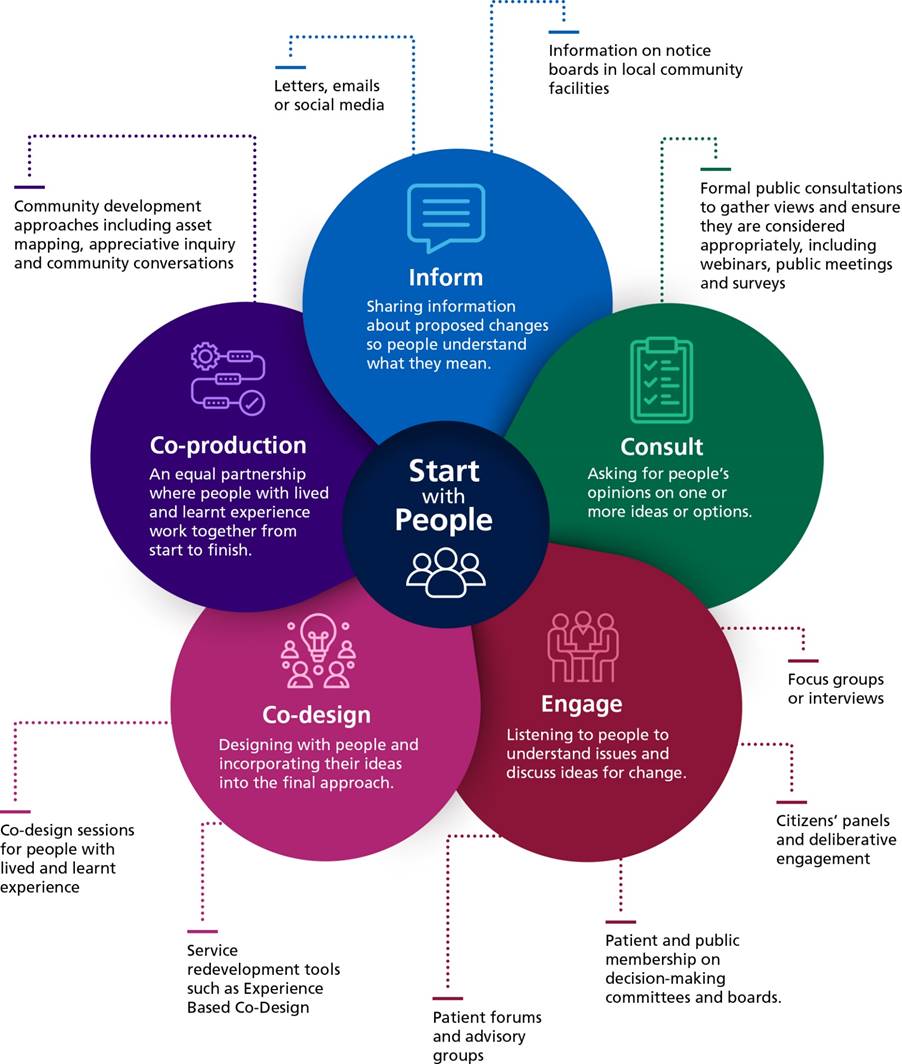
Different ways of working with people and communities
Accessible diagram text:
This diagram shows some of the different ways of working with people and communities, with examples for each
- Inform: Sharing information about proposed changes so people understand what they mean. Examples are Letters, emails or social media, and information on notice boards in local community facilities
- Consult: Asking for people’s opinions on one or more ideas or options. An example is a formal public consultation to gather views and ensure they are considered appropriately, including webinars, public meetings and surveys
- Engage: Listening to people to understand issues and discuss ideas for change. Examples are focus groups or interview, citizens’ panels and deliberative engagement, patient and public membership on decision-making committees and boards, and patient forums and advisory groups
- Co-design: Designing with people and incorporating their ideas into the final approach. Examples are service redevelopment tools such as Experience Based Co-Design and co-design sessions for people with lived and learnt experience
- Co-production: An equal partnership where people with lived and learnt experience work together from start to finish. An example is community development approaches including asset mapping, appreciative inquiry and community conversations.
For all the approaches used, there are three main pitfalls to avoid:
- Tick box exercises. Involvement is not an obstacle to overcome on the way to achieving a predetermined outcome. Any perception that it is tokenistic or that a strategy or service change has not been informed by insight from the public, will not only undermine trust, it is unlikely to be supported at local, regional or national level.
- Unrealistic timescales. Service design and service changes should be planned to achievable timescales that allow for early, ongoing and effective public involvement, including careful consideration and discussion of the views expressed by people and communities.
- Limiting public dialogue to service change proposals. While consultations necessarily focus on the proposals being consulted on, involvement should not only take place when a system wants to make changes – it should be part of how every system operates, with insights from community conversations informing and driving policy decisions. Systems should be in regular dialogue with people and communities; enabling them to also influence the agenda.
Case study: Northern Cancer Alliance’s work with communities in the recovery of urgent cancer referrals
The COVID-19 pandemic had a dramatic effect on the rate of cancer referrals across England. At the start of the pandemic the Northern Cancer Alliance saw referral rates across the region drop to 40.9% of pre-pandemic levels (April 2020). The Alliance decided to build on the national ‘Help Us to Help You’ campaign with locally produced material. This local campaign focussed on health inequalities by focussing on specific tumour groups and communities where recovery levels were slowest.
Key to all aspects of the Northern Cancer Alliance work plan is the effective involvement of the public. The Alliance value to ‘always involve the right people at the right time’ was a fundamental aspect of the design and delivery of the campaign. With a focus on health inequalities, the Cancer Alliance brought together the Alliance Lay Representatives, people with lived experience, the Be Cancer Aware team and community groups to co-produce the campaign.
The campaign produced short films made by people with lived experience of cancer, people with a learning disability and people from minority ethnic groups in different languages. There was also patient information and campaign webpages produced by the Northern Cancer Alliance Lay Representatives.
To reach as many people as possible, the campaign worked with community assets, for example, by distributing leaflets, posters and magazines via food banks and other venues in the most deprived areas across the region. This element of the campaign was supported by local community organisations who already had links to wider groups of people and the Alliance Cancer Community Awareness Workers. As a result, the campaign contributed to a recovery of urgent cancer referrals.
Existing sources of feedback and insight
The starting point for any involvement is to consider existing sources of insight about the needs and experiences of different groups of people – what do you already know, what have people already told you? A review of existing information can save time and money and point to gaps in insight, while also avoiding asking people to repeat themselves. This helps to ensure that involvement is focused, meaningful and avoids duplication. This may be information held by partner organisations, including patient feedback, complaints, needs assessments and insights collected during previous activities. Consider whether the context of this previous work has changed significantly and when it took place to understand whether it is still relevant.
Involving partners in the planning process helps identify what is already known and also where the gaps are. Some people, such as those in inclusion health groups (see next chapter) and others who face social exclusion, may be systematically missed in feedback, qualitative and quantitative data sources. For example, if existing ways to give feedback are not accessible for people with learning disabilities, then their views are more likely to be missing.
One source of insight into population health needs are the intelligence functions that ICSs are building. These are system-wide, multi-disciplinary collaborations which share data and provide analytical support to help understand their local contexts. A key purpose of the intelligence function will be to support a population health management approach to care, including by pooling information and data held by partners on a local population’s health and care needs, such as granular intelligence on inequalities across different population groups (see NHS England resources for more on population health management). Intelligence functions should work with patient experience and engagement colleagues to ensure that qualitative and quantitative insights about the population are informing the interpretation of other analyses and are given equal weight in decision-making. Contextualising this intelligence with people and communities is essential and needs to be undertaken in sensitive and accessible ways.
ICBs and trusts can work in partnership with local authorities (in particular local health scrutiny functions and public health, social care and housing teams), other ICS partners and local communities to share insight and develop a detailed understanding of population health needs. A combination of national data tools, insight collected by partners and local engagement can be used to understand what works for different communities. Combined with insights drawn from the community, data can support primary care and neighbourhood teams to increase uptake of preventative services while also tackling health inequalities by identifying those groups that may currently be underserved (Next steps for integrating primary care: Fuller Stocktake report, NHS England, May 2022). One approach some ICSs are taking is to set up a network of engagement colleagues across partner organisations to share insight and coordinate engagement (see case study below).
Examples of insight and feedback sources:
- ·National patient surveys
- Friends and Family Test
- Local surveys and engagement by the NHS and local authorities
- Social media and review websites
- Local Healthwatch reports and Healthwatch England national reports
- Intelligence from the VCSE sector and local authorities
- Care Quality Commission (CQC) reviews, surveys and reports
- Patient Participation Groups (PPGs)
- Complaints and compliments
- Patient Experience Library
- Patient Safety Specialists
- Patient experience discussions at System Quality Groups
- Staff feedback including their own views
- Mapping of previous consultation and engagement activities including those by partner organisations
- Local Health Profiles
- ICS intelligence functions
- Local authority reports including Director of Public Health annual report, joint strategic needs assessment and joint health and wellbeing strategy and reviews by scrutiny committees.
Case study: System insight group and patient and public insight library at Derby and Derbyshire integrated care system
During the early stages of COVID-19, partner organisations within the Derby and Derbyshire ICS wanted to gather insights on how people were experiencing the pandemic and how it affected their lives. Residents in Derby and Derbyshire began to get inundated with separate requests to share their experiences and fill in surveys.
To avoid duplication, these efforts needed to be co-ordinated, so the ICS set up a System Insight Group, bringing together patient and public experience and engagement leads from NHS trusts, the local authorities and the VCSE sector. Its vision is to develop a culture of making insight-led decisions across the ICS. Insight could be from evidence, research, reflections, conversations, observations, and from any number of different sources. The aim of the System Insight Group was to link the types of insight together.
The System Insight Group has developed a Patient and Public Insight Library set up on the NHS Future platform. New insight is being added to the library on a regular basis, and any member of staff can join. The aim is to assist decision-makers to find current insight in the system, with the aim of avoiding duplication and consultation fatigue.
The group has also produced a report on Remote Access to Health and Care during the pandemic. The report pulled together a large proportion of insight and summarised the key themes. The report is being used by ICS partners when making decisions about the recovery of services, meaning that additional engagement will only be needed if it fills a gap in insight within the report. A digital inclusion checklist was developed using the report and will be promoted to all service providers to ensure good practice in remote access implementation programmes.
Patient participation groups
It is a contractual requirement for every GP practice to have a Patient Participation Group (PPG). The form a PPG takes is not specified and this provides flexibility for practices to work in partnership with people and communities in ways that best support the practice populations. While the PPG is one of the main ways General Practice have used to engage with patients, it should not be the only approach if it does not reach diverse groups, people with the worst health inequalities or people not accessing the services. These groups are more likely to be hesitant about getting involved in traditional PPG models. However, PPGs do not need to be limited to the meeting style group which has become the most common. Primary care networks (PCNs) and practices need to consider if the form of the present PPG supports people to take part or if other approaches are also needed to widen participation. This animation has some useful principles to use as a starting point to think through how practices currently hear the voice of their community and where the gaps are. While the main focus of a PPG is on making improvements to its local practice, their insight and experiences can be relevant to its PCN. PCNs can also learn from their practices’ PPGs about how different structures can effectively engage diverse groups.
Co-production
Co-production is a way to involve people by sharing power with them. The Coalition for Personalised Care defines co-production as:
‘a way of working that involves people who use health and care services, carers and communities in equal partnership; and which engages groups of people at the earliest stages of service design, development and evaluation.’
Co-production can be used strategically, to design services, make quality improvements, design and undertake research and innovation, and develop participatory budgets. At an individual level, it is the cornerstone of person-centred care such as personal health budgets. As well as being well suited to designing services in places and neighbourhoods, it can also be applied strategically for systems and national organisations.
The starting principle is that people with ‘lived experience’ are often best placed to advise on what support and services will make a positive difference to their lives. When done well, co-production helps to ground discussions and to maintain a person-centred perspective.
Where partnerships are genuinely equal, professionals are comfortable with not having the answers and with sharing resources, responsibility and power. This can be difficult to achieve without cultural change and support for staff and people to share power and take on co-production roles.
The Coalition for Personalised Care sets out the values and practical steps to make this ambition a reality. These includes:
- senior leaders supporting co-production through culture and behaviour
- identifying areas of work where co-production can have a genuine impact and involving people at the earliest stages
- investing in training and development so that people with lived experience and people working in the system know what co-production is and how to work in ways that enable this.
Case study: Building people’s skills and knowledge to take part in co-production
The Peer Leadership Development Programme was launched in 2014 by NHS England with the purpose of enabling people with lived experience to develop their knowledge, skills and confidence to co-produce. Over 200 peer leaders have now been trained.
The programme provides people with an opportunity to learn about how the health and care system works, about local and national policy and about how to share good information. It also teaches about change management theory and communication styles and preferences, and how people can use their personal story to create a narrative for change. This programme enables people with lived experience to access up-to-date information and support, in the same way that people working in the health and care system do. This ultimately enables people with lived experience to co-produce on a level playing field.
Case study: The difference made to the NHS England Musculoskeletal Services (MSK) programme by the Musculoskeletal Lived Experience Group (MSK LEG)
The first COVID-19 pandemic lockdown had a devastating effect on the provision of Musculoskeletal Services (MSK) services. Face-to-face consultations became a rarity, replaced by telephone and video consultations. MSK clinicians had to quickly learn new skills to assess and treat patients in these unfamiliar formats. The number of patients treated by MSK clinicians was significantly reduced as therapists were re-deployed to care for COVID patients.
It was quickly clear that going forward MSK services would need to be remodelled, not only to cope with pandemic times, but also to move into the future. The pandemic created challenges but also opportunities for new and better MSK services.
For such large-scale re-modelling to be successful it was evident that all partners would need to play a part in the development process including, perhaps most importantly, people using the services and their carers. Without their involvement it could easily result in services that people didn’t want or were not sufficiently accessible to them.
In June 2020, a MSK Recovery Group was established with lived experience partners alongside healthcare professionals. The intention was to work together collaboratively to assist with restoring and improving MSK services in the wake of the pandemic lockdowns. It evolved into MSK Lived Experience Group (MSK LEG). Each member of the new MSK LEG has experience of a relevant MSK condition and were rigorously interviewed and appointed after an open and accessible selection process.
MSK LEG have already co-produced its own terms of reference and engaged in providing feedback on various MSK pieces of work. The group have helped shape the evolution of the #BestMSKHealth Collaborative programme and some members have presented alongside the National Clinical Director and various MSK clinicians to a range of audiences at events. The MSK LEG team has been developed from strong principles of co-production and has already made a difference to the recovery and advancement of MSK services throughout the UK.
Community-centred approaches
Community-centred approaches build on existing assets to support communities to take more control over their lives and their areas. The diagram below shows the different types of assets that can contribute to creating health. These approaches (which include community development, asset and strength-based approaches) help identify the issues that matter to local people and support them in tackling them, working with the relevant public sector organisations.
Accessible diagram text:
There are different types of community health assets which are shown in the diagram:
- The resources and facilities within the public, private and VCSE sectors
- Physical, environmental and economic resources that enhance wellbeing
- Friendships, good neighbours, local groups and community and voluntary associations
- The skills, knowledge and commitment of individual community members.
Recognising assets rather than deficits is an important aspect of how to tackle health inequalities. It builds on strengths and ensures that health action co-produced between communities and services so that it effectively meets local needs. Identifying community assets also reduces the possibility that new interventions inadvertently override what already works well or are not fully used because people still defer to preferred and trusted community initiatives
This can require a shift in how health services view their communities and, like co-production, requires leadership and support to make a reality. It can need time and sustained effort before communities can take collective control. Asset based approaches are already well established in parts of local authorities and social care so there may be opportunities to learn from local authority partners (Evidence for strengths and asset-based outcomes, Social Care Institute of Excellence, August 2019).
People often relate closely to their neighbourhood where links between communities and services can be strongest. Neighbourhoods contain a wide range of roles which work closely with their communities including community nurses, GPs, pharmacists, community and mental health teams, Social Prescribing Link Workers, social workers, housing workers and VCSE sector organisations. There are also community-led services, such as peer support workers and community champions whose roles are designed to address local needs and health inequalities.
Primary care networks that are most effective in improving population health and tackling health inequalities are those that work in partnership with their people and communities and local authority colleagues (Next steps for integrating primary care: Fuller Stocktake report, NHS England, May 2022; Health Creation: How can Primary Care Networks succeed in reducing health inequalities? The Health Creation Alliance, February 2020). This includes using co-production to work with marginalised groups to break down barriers to accessing healthcare. In some neighbourhoods general practice is the hub through which many relationships are built between the community and the health and care system. In other neighbourhoods, partnerships are led by others, so it is important that health supports and builds on these existing networks rather than reinventing something new. There is an opportunity to leverage the knowledge and expertise of different workforce groups, including general practice, housing, policing and schools about the concerns and priorities of their communities, including its most vulnerable members whose voices are less likely to be heard.
Communities organise themselves in many ways and understanding where and how they do this is crucial to reaching and hearing diverse voices. An integral part of building a system-wide approach to involvement is to start at neighbourhood level with understanding what matters to people’s health and the assets they have. It means that engagement should start with where people are already and aggregate findings to make the links to wider geographies.
Community-centred approaches help understand the specific local context where people live their lives and so design more integrated and preventative interventions that are tailored to local needs. These early public physical and mental health responses can prevent the need for acute services. These can be co-delivered by communities, employing local people and making the best use of the assets in each neighbourhood. This boosts the power of communities to take responsibility and set an agenda for change which has a strong health creating effect.
While for many people their community is at the level of neighbourhood, they may also belong to wider communities. For example, as a member of a national support group for a rare condition, where peers help each other to understand treatment options.
Case Study: Local Area Coordination in Derby
Since 2011, Derby City Council and its system partners have been developing an evidence-led approach called Local Area Coordination. They work alongside other areas in England and Wales who have come together to form the Local Area Coordination Network (supported and convened by Community Catalysts CIC). Local Area Coordination sees ‘Local Area Coordinators’ working closely alongside people, families and communities at a hyperlocal level with populations of around 8,000-10,000. Rooted in community, Local Area Coordinators take the time to build and nurture supportive relationships and partnerships with people and families.
Many of the people they are alongside have pressing concerns around their health and wellbeing. With no eligibility criteria, referral pathway or barriers to access, Local Area Coordinators across Derby can help people identify and build on their strengths and find practical, local (ideally non-service) solutions to any barriers that are preventing them from achieving good lives and making their contribution.
Through a dedicated ‘Custodian Group’ of system leaders, the approach is offering the Derby system rich insights into all aspects of people and community life including things that need to change. It also provides greater opportunities for reducing siloes, promoting working together and ongoing co-production and collaboration with local people around what good health and wellbeing really looks like and means.
Recently Local Area Coordination Derby has received investment from health programme partner “Team Up” (Derbyshire / Derby). Team Up is an ambitious programme in that aims to create one team across health and social care who see all housebound patients in a neighbourhood. This accounts for 29 practices across five PCNs serving a population of almost 400,000. The investment represents the growing recognition in the value of Local Area Coordination, not least in how it helps areas think and view patient and public involvement through a very different lens.
You can find more about Local Area Coordination here www.lacnetwork.org
A2. Key considerations for all approaches
While the approaches to working with people and communities depend on the specific context, there are some universal considerations that apply. These help meet the legal duties and ensure that people are supported to take part safely.
Fair and proportionate approaches
Whichever approach is taken, it needs to be fair and proportionate. Judgement is needed and it is not an area where definitive advice can be offered without knowledge of the specific circumstances. Where staff need to make a particularly complex or potentially contentious judgement, they may wish to consider seeking legal advice.
The courts have established guiding principles for what constitutes a fair consultation exercise, known as the Gunning principles:
- consultation must take place when the proposal is still at a formative stage
- sufficient information and reasons must be put forward for the proposal to allow for intelligent consideration and response
- adequate time must be given for consideration and response
- the product of consultation must be conscientiously taken into account.
For more information, see Annex B5. These four principles relate to formal consultation but can be informative for other approaches.
The approach should also be proportionate. NHS organisations need to meet their duties to involve the public alongside their duties to act effectively, efficiently and economically and make sustainable use of NHS resources.
Staff will need to consider the impact of proposals on the different groups of people who may be affected. Generally, the greater the extent of changes and number of people affected, the greater the level of activity that is likely to be necessary. However, the nature and extent of public involvement required will always depend on the specific circumstances.
Decisions in urgent situations
In an urgent situation, it may be necessary to consider the duty to involve the public alongside the public interest in maintaining continuity of care and protecting the health, safety or welfare of patients or staff.
It will only be reasonable to justify carrying out a limited (or no) public involvement exercise on grounds of urgency when the lack of time was genuinely caused by an urgent situation or where there is a genuine risk to the health, safety or welfare of patients or staff. These can arise from staff shortages, estate issues or other causes. It does not permit commissioners or providers to leave public involvement until the last moment without enough time to carry out a fair and proportionate exercise, when the public could and should have been involved earlier or to a greater extent.
Where urgent changes are made on a temporary basis, the legal duties still apply if organisations subsequently consider whether to make them permanent. This equally applies when changes were introduced because of the COVID-19 pandemic; public involvement should be undertaken if there are plans to make them permanent.
ICBs, Provider collaboratives and Trusts are encouraged to maintain an open and ongoing dialogue with ICP members and Health Overview and Scrutiny Committees on the services it regards as at risk and the actions it may need to take in order to maintain patient and staff safety. This can fulfil a valuable function in anticipating and evaluating the impact on patients of urgent changes made in these circumstances and ensuring that health inequalities are not increased. Of course, organisations that have in place ongoing mechanisms of working with people and communities will be in a much better position to undertake rapid engagement as an interim measure.
Equality considerations
Public authorities including ICBs, trusts and NHS England are required to comply with the public sector equality duty of the Equality Act 2010. When it comes to proposals for changes to services, carrying out an equality and health inequality impact assessment can help identify people who experience the greatest health inequalities, including socio-economic groups and those people with protected characteristics under the Equality Act 2010 who may be affected by a particular plan or decision.
The Health Equity Assessment Tool can also help identify what action needs to be taken to reduce health inequalities and promote equality and inclusion.
These can be used alongside the Equality Delivery System for the NHS, a framework to help local NHS organisations, in discussion with local partners including local communities, to review and improve their performance for people who share protected characteristics.
Approaches to working with people should be designed to include these groups and planned to ensure that they are fair and equitable. Involvement plans should consider how to include all groups affected by proposals for changes to services and prioritise hearing from those affected by the greatest inequalities. In practical terms this means recognising that not every type of involvement works for everyone and that there can be additional complexities to work effectively with some groups, so you may have to carry out a range of activities. This can mean:
- using accessible venues, making reasonable adjustments or specific effort to ensure disabled people, autistic people and people with a learning disability can participate
- working with peer support workers to facilitate the involvement of people who may be struggling with their mental health
- targeting resources and approaches at ethnic minority groups to provide the additional support that some of their members will need because of the health disparities that they experience
- recognising that deprivation and poverty can prevent people taking part in activities unless financial support and resources are in place that enable their involvement
- considering health literacy levels and language. Content should be relatable rather than using NHS terms and acronyms. Jargon can be a barrier for everyone
- accounting for digital literacy and access to digital systems in areas of socioeconomic deprivation
- building people’s knowledge of how different parts of the health and care system fit together and where their input will make a difference. People will be at different levels of understanding about the NHS structures.
Auditing and monitoring the participation of certain groups, for example in events and formal governance roles, should be undertaken. This will help identify any gaps in engagement requiring attention; and supports staff to promote the involvement of people who are more reflective of the population in question.
Whilst the Equality Act refers specifically to the protected characteristics, there are also other communities such as inclusion health groups that should be considered and included within engagement.
Inclusion Health Groups
These groups often experience the worst health inequalities through being at risk or living with extremely poor health because of poverty, marginalisation, multi-morbidity and social exclusion, and further impacted by discrimination and stigmatisation, and are not consistently accounted for in electronic records (such as healthcare databases). These can overlap with protected characteristic groups. These are any socially excluded population including, but not limited to:
- Gypsies, Roma, Travellers, Showmen and Liveaboard Boaters
- people experiencing homelessness
- people experiencing alcohol and/or drug dependence
- sex workers
- vulnerable migrants and refugees
- young carers
- victims of modern slavery
- people in contact with the criminal justice system.
There are other groups that experience barriers to accessing services, like people with a learning disability and autistic people, and people with severe mental illness. They can also belong to inclusion health groups.
It is essential to understand the barriers that the system inadvertently creates to the involvement of inclusion health groups. Approaches should be developed in partnership with trusted organisations and people with lived experience and seek to ensure that involvement means that people’s voices are heard and understood. These may be national organisations where there is not the local expertise of working with specific groups. Approaches must be trauma informed (see box below), culturally aware and provide a psychologically informed environment for people to take part safely.
PCNs can use a self-assessment tool to assess their engagement with inclusion health groups. Further guidance on inclusion health is on the GOV.UK website.
Case study: Making sure vulnerable groups are not left behind
To support the COVID-19 vaccine rollout, Bury Council and CCG worked with its PCNs, Healthwatch and VCSE sector organisations to make sure vulnerable groups did not get left behind. They focussed on proactive outreach to groups which the vaccine data, equality impact assessment and community insight showed were at risk of low uptake. This included Gypsy, Roma, Travellers, people experiencing homelessness and people with disabilities.
The partners worked together to engage these groups to see what the potential problems were, making use of their existing links with the communities. For example, the local authority team that works with Gypsy, Roma and Travelling people visited traveller sites to discuss what the issues were.
The response to COVID-19 and delivery of the vaccination programme has been a single endeavour between the council and NHS in partnership with the wider system, for example by working together to identify locations for vaccination centres and pop-up clinics that would meet their different communities’ needs.
More information is on the Local Government Association website.
The impact of wider experiences
Approaches to involvement should be designed to take account of the contexts that people live their lives in and should recognise that everyone experiences health services differently. It should start from a position of building trust, safety, and shared understanding.
This means recognising and reflecting the wider lived experiences of the people we work with and how this can affect how they participate. We should also involve people and communities in a way that considers how social determinants (such as racism, stigma, discrimination, poverty, access to greenspace and healthy food, poor housing, employment and education) affect physical and mental health. It means recognising intersectionality – that people are affected by several overlapping characteristics and experiences. They can face multiple sources of exclusion, discrimination and disadvantage, which will affect how they want to participate and their perceptions of health and care services.
It is also important to consider that previous involvement experiences, both good and bad, can affect how someone wants to be involved. For example, a bad hospital appointment where someone feels like they have not been listened to, could influence how they respond to invitations to get involved. These things may not seem directly relevant to the conversation you want to have but can matter a lot to those you are wanting to engage.
There is a responsibility to keep people who get involved safe. Being asked repeatedly to go back over bad or even traumatic experiences so professionals can learn how to improve services, will cause distress and increase lack of trust. One way to keep people safe is not to create isolated positions of ‘lay representation’ which can burden people with the responsibility of bringing a public perspective to a large group of professionals. Instead it can be better to work with groups who can continue to support each other outside of meetings and help each other to take part effectively. Depending on the context, it may be necessary to arrange therapeutic support at activities and afterwards.
Trauma informed approaches
Working with people and communities should start from a position of building trust, physical and psychological safety, and shared understanding. It acknowledges what may be difficult. Trauma informed approaches are often partnership based, working with people and organisations that are trusted, well informed and specifically trained. VCSE sector organisations can have a particular role to work with people who have often experienced significant trauma in their life or who have been excluded by society. Working with community leaders, experts by experience and others who already hold people’s trust is often a more appropriate way of reaching people. Acknowledging and validating people’s previous and current negative experiences are a key part of this, alongside building shared understanding and authentic relationships.
West Yorkshire Health and Care Partnership has collated resources on trauma informed approaches.
Case study: Improving engagement through online communities
With the move to online working during the pandemic, Shine Cancer Support found that this enabled them to reach people who would not necessarily have engaged with their services or community previously as physical barriers no longer existed. For example, attending in-person retreats was not possible for some due to their treatment, their physical health, or the travel time.
During the pandemic Shine developed several online programmes with shorter sessions over several weeks that enabled people from across the country and at different stages of their treatment to attend at the same time.
Through these programmes people developed strong peer support, shared information and participated in a community that could support them. This has been particularly important for young adults with incurable cancer who are increasing in number but less likely to find someone physically nearby who shares a similar experience. They have been brought together virtually through the Shine Circles programme and they usually continue their support and sharing via WhatsApp groups after the programme ends.
These and other online support groups show how people get information and support for their health and from communities that exist at different levels.
Supporting people to take part
It is important to have a consistent approach to recruiting, training and supporting the range of people who get involved in different roles. This helps ensure they have the knowledge, skills and confidence to contribute effectively, and that opportunities are equally accessible to people on low incomes and those with health and social care needs or disabilities.
The level of support needed will partly depend on the role. Those with ongoing involvement or which include decision-making activities as part of co-production approaches may require specific training, for example to help people to understand their own lived experience in the wider context and have the skills and confidence to influence professionals. This could also include having pre-meetings to help people explore the issues and check their understanding, as well as follow-up debriefs.
It is good practice for organisations to have a written policy giving details about their approach to reimbursing and paying people. A policy helps to clarify the situation for everyone and avoids people being treated differently on different occasions. There are advantages to developing a consistent approach across organisations within an ICS so that people can easily understand whether and how they will be reimbursed. Any policy on payments will need to be compliant with HMRC rules.
Consider the resources required to take part, including the cost to an individual of travelling to a meeting or attending online, especially where they may have limited income or no recourse to public funds. Payments can support participation from more diverse groups and helps recognise the value that organisations place on people contributing their experiences, knowledge and skills. Organisations paying people for their time as part of involvement activities have a responsibility to ensure that people who receive benefits are supported with independent welfare rights advice.
Beyond financial means, there are many ways to recognise people’s contributions including receiving an acknowledgement in writing, support to develop skills and experience, and seeing the improvements made because of their input. Ask people what form of recognition they would value and would support them to take part.
It is important to recognise that there can be a cost to partner organisations such as VCSE organisations or Local Healthwatch. This can be in terms of staff time to provide insight or to take part in advisory groups as well as arranging for communities to participate in engagement activities.
There are also practical considerations to ensure different people can take part by making activities accessible, such as when and where they take place, making reasonable adjustments so everyone can take part, provision of British Sign Language and community language interpretating, and providing accessible information. This links to the recognition that a range of approaches are likely to be needed to involve relevant groups, and that we should go to where they are already, rather than expect them to come to us.
NHS England has a patient and public voice partners policy that sets out how it supports people to be involved in its work. It sets out the different types of roles people can do and includes support and training. There is also a policy on reimbursements and payments.
Case study: Working with young people to develop keyworking in the Black Country
The NHS Long Term Plan includes a commitment that by 2023/24 children and young people with a learning disability and/or who are autistic with the most complex needs will have a designated keyworker. Keyworkers make sure that these children, young people and families get the right support at the right time. They make sure that local systems are responsive to fully meeting the young people’s needs in a joined up way.
Black Country Healthcare NHS Foundation Trust worked with children, young people and families from the outset to design its keyworker service. The parents, carers and young people with lived experience knew what they needed and the impact it would make.
Co-production was at the heart of the approach from day one. A steering group was co-chaired by a young expert by experience. Young people were helped by Dudley Voices for Choice to take part with pre-meetings and debriefs; resources and papers were written in plain English, and support was provided for the emotional nature of the work. They worked on all stages of the pilot, including the bid for funding, communications and job descriptions for key workers. A peer support model was also developed alongside as a step down from the key worker model.
The approach is being evaluated by the Challenging Behaviour Foundation. Feedback shows the positive impact keyworkers are having for young people, their families and the wider health and care network – for example there has been a significant reduction in Tier 4 hospital admissions.
A3. Collaboration between the NHS and other partners
This chapter sets out how different organisations can collaborate on how they work with people and communities. Collaboration is about building relationships with partner organisations and local communities, treating all partners equitably with a valid and useful contribution to make to the health and care system.
The partners highlighted in the diagram below can help systems to work with people and communities in terms of contributing views, sharing insights and providing outreach. It is not an exhaustive list and systems should map the different partners in their areas to understand how they can work with them.
Local authorities, social care providers and the Voluntary Community and Social Enterprise (VCSE) sector may already have well-established mechanisms for including people in decision-making and, where possible, NHS organisations should use the insights from these and work through existing forums and activities, rather than setting up new ones.
There is also an opportunity to coordinate working with people and communities. For example, an integrated care board (ICB) and a trust can work together on engagement over changes to hospital services for which they both may have public involvement duties. Their approach could include working with existing forums run by the local authority, or commissioning Healthwatch and the VCSE sector to engage the communities they already have links with.
Joining up conversations across sectors and coming together to involve people about what matters to them can lead to significant improvements and reduces the need for people to contribute separately to each organisation.
Partners for the NHS on working with people and communities

Accessible diagram text:
Different partners shown in the diagram are: local authorities and councillors, social care providers, Healthwatch, the voluntary, community and social enterprise sector, Social Prescribing Link Workers, volunteer and peer roles, non-executive roles, workforce, other health and care partners
Local authorities and councillors
Local authorities are important partners in working with people and communities. Their membership of integrated care system’s (ICSs) brings their experience of working with people to design and deliver services that meet local needs and build community assets.
The Boards of each ICB must include at least one ‘partner member’ jointly nominated by the local authorities within the area of the ICB. The ICB, and each responsible local authority wholly or partly within the ICB’s area, must establish an integrated care partnership (ICP) as a statutory committee of the ICB.
All local authorities have a role in delivering better health and care and influencing people’s health outcomes through the operation of a wide range of statutory powers and duties. These include those relating to children and young people, health and wellbeing, adult social care, housing, environment protection and planning, to name just a few. As such they are all important partners in working with people and communities. Partnerships should exist with councils, including district and other councils such as town or parish councils, and beyond the formal membership of the ICB and ICP.
Local authorities are key partners in designing and commissioning person-centred services. They also have expertise in co-production – especially in relation to direct payments for social care.
They often employ community development workers with experience of community-centred approaches. They are also significant funders of local VCSE sector organisations providing care and support to communities.
Council public health teams work closely with their diverse communities to provide information and support to improve population health and address health inequalities.
Councillors are elected to represent their local communities at ward level. They have detailed knowledge of the communities they serve, including their concerns around health services and the wider determinants of health. They have links to community resources and networks, including neighbourhood forums, and a reach into their communities.
County council and unitary authorities are responsible for health and wellbeing boards – inclusive place-based forums in which political, clinical, professional and community leaders agree shared priorities to improve the health and wellbeing of their communities. The boards have a statutory duty to develop and publish joint strategic needs assessments (JSNA), an invaluable source of information on an area’s demographics and the profiles of local communities. The boards are required to publish joint health and wellbeing strategies (JHWS) that identify the priorities for improving health and wellbeing and the actions needed to achieve this. ICBs and their partner trusts must involve the boards in producing the new joint forward plan for each ICS (see Annex B5). In many cases, the JSNA and JHWS are developed with extensive collaboration and co-production with communities and with people who use services.
Unitary and county councils have powers and duties in respect of Health Overview and Scrutiny. This role is usually carried out by a Health and Overview Scrutiny Committee (HOSC) of the local authority for its local area or a joint HOSC appointed by two or more local authorities to cover a larger area. Working with scrutiny can help systems take a wider perspective and develop effective partnership working.
More information on when consultation with HOSC is required and the role of HOSCs more generally is contained in Annex B.
Case study: Vibrant Communities Partnership Board
Bournemouth, Christchurch and Poole (BCP) Council have a strong track record of working with communities, but acknowledges that to be better, it must involve the VCSE sector into decision-making positions within the council.
The vast majority of public sector organisations work using traditional, deficit-based approaches. This means they are set up to focus on perceived issues or weaknesses of a particular community that, it is believed, require a professional approach to solving. While there are some reasons why this approach may be useful, it can inadvertently take power and responsibility away from the community.
In order to reverse deficit-based public services, BCP Council has developed the ‘vibrant communities’ approach which focuses on developing strength-based ways of working within individual communities and within council services.
To do this, the Council set up the Vibrant Communities Partnership Board, which is a partnership between the council, the local VCSE sector and the NHS and other partners. The broad overall objective is to deliver strength-based approaches and interventions that focus on the inherent assets of people, communities and organisations. The Board has two co-chairs, one elected by the council and the other by the voluntary sector, so a mixture of community and council priorities are covered; and to empower non-public sector partners by devolving responsibility.
The Board avoids discussing strategic priorities of Board members, but instead focuses solely on operational needs of the community. This is deliberate as a key objective of the Board was to avoid it becoming a smaller ‘health and wellbeing board’.
Social care providers
Social care is the term used to describe the personal care given by public or private organisations to help people in society who need specialised assistance to live a comfortable, healthy, fulfilling life. Services aim to provide care for and protect society’s most vulnerable and this could include children, young people, adults or older people.
Social care providers can bring an understanding of the needs of the people they support, with advocacy and insight into their experience in the current systems and what will make those better. Social care providers often have frequent and long-lasting connections with the people they work with and can support connections and relationship-building with them. Social care providers can also be experienced at working with co-production so that people can actively shape their care and support they receive.
Healthwatch
Healthwatch is the independent body responsible for understanding the needs, experiences and concerns of people who use health and social care services, and to ensure their views are put at the heart of their care.
Its activities include:
- promoting the involvement of local people in health and care services
- enabling people to monitor standards of care and how services can be improved
- obtaining their views and experiences of services.
At a national level, Healthwatch England provides leadership and support to local Healthwatch organisations. Its other statutory functions include escalating concerns raised by local Healthwatch to the CQC, and to provide advice to Secretary of State for Health and Social Care, NHS England and English local authorities, especially where they hold the view that the quality of services provided are not adequate.
The Health and Social Care Act 2012 put the focus of local Healthwatch at top-tier local authority level. The development of ICSs means that Healthwatch will need to work at both system and place levels if local voices are to be property represented where decisions are made. As local Healthwatch are not ordinarily funded to do this work at system level, ICBs and ICPs will need to consider what additional support Healthwatch will need to make an effective contribution.
Providers of health and social care services are under a duty to allow entry by local Healthwatch. This power to ‘enter and view’ services, offers a way for Healthwatch to undertake their activities and allows them to identify what is working well with services and where they could be improved. Healthwatch can use this evidence to make recommendations and inform changes both for individual services and across the system. There are requirements for the service providers to respond to a Healthwatch report and its recommendations within a set timeframe.
Through their role in obtaining views of local people about their needs and experiences of care, local Healthwatch can provide insight about the breadth of health and care, particularly picking up on issues which go beyond a single service such as integration and the impact on people. ICSs should build on the existing statutory activities of local Healthwatch in their geographies, working with the organisations to resource the co-ordination and analysis of user experience data. This will complement insight collected by commissioners and providers.
Systems can also work with local Healthwatch to involve local people. One of their functions is to support the involvement of local people in the commissioning, provision and scrutiny of care services. Their scrutiny function means they can make recommendations of service improvements to commissioners, providers, Healthwatch England and the CQC. These functions help them have knowledge of how to work effectively with local communities and how services can be improved to meet local needs.
Local Healthwatch must be involved in developing joint strategic needs assessments and integrated care strategies (see Annex B5). Healthwatch organisations may provide views, reports and recommendations on decisions and decision-making processes based on the evidence available. This includes the option to refer issues to overview and scrutiny where they feel it is appropriate (see Annex B3).
Local Healthwatch organisations have a place on their local Health and Wellbeing Boards, so they can present people’s views in strategic discussions. They can have strong relationships with local authorities, working with both service delivery and elected members.
Many ICSs already have some system-level arrangements in place with their local Healthwatch. Arrangements for how Healthwatch can work at both system and place level will vary depending on the geography of the system and different local authority commissioning arrangements. ICSs should consider how they can invest in these partnerships in order that Healthwatch has the resource to take on their roles effectively, including commissioning them to undertake engagement or fulfil the roles at system level.
While Healthwatch have different roles from VCSE sector organisations, their shared values mean they should be seen as complementary rather than competing (and many Healthwatch are hosted by VCSE sector organisations). Strong relationships with both will help ICSs hear the voices of people at all levels.
Case study: Bringing local people’s voices to the ICS – Healthwatch in North East London
To ensure that local people’s experiences are at the heart of the North East London ICS, the eight local Healthwatch are working together. By combining their knowledge of their local areas, the experiences that people share with them and the different barriers they face, they have been able to identify trends, variations and differences in health and care – helping to tackle and reduce inequalities.
Together the local Healthwatch have been working with the ICS on its engagement strategy and the principles it will follow. They meet regularly with the ICS as a forum for dialogue and a space to highlight local issues. They are actively involved in their place-based partnerships and will participate in ICS governance.
They have been commissioned by the ICS to deliver community insights through a single database across North East London, particularly in relation to COVID-19. The eight local Healthwatch combined their data, using a system already in use by some local Healthwatch to provide ICS level insight. The Community Insights Repository collates feedback for providers from different sources, such as NHS Choices, Care Opinion, Google reviews, website feedback, surveys and complaints
For local Healthwatch, there have been significant benefits too. They now have more evidence to base their work on; they’re more quickly able to identify critical issues people are experiencing and have better relationships with communities facing health inequalities.
Healthwatch activities for the ICS are funded through the ICS engagement budget. More information is on the Healthwatch website.
The voluntary, community and social enterprise (VCSE) sector
Organisations within the VCSE sector have many different roles. They are often providers of services (both commissioned and funded through voluntary or charitable income) to the most disadvantaged communities and consequently can have an excellent understanding of the health and care issues faced by those communities. The sector has a key role in tackling the wider determinants of health by reaching people who experience health inequalities and removing barriers to accessing services. At both national and local levels, the VCSE sector has an important contribution to make in shaping and providing health and care services, and in developing and implementing plans to tackle wider determinants of health.
VCSE sector organisations can bring their knowledge of how to work with people and communities:
- they are often trusted, accessible and skilled at outreach and engagement
- they have routes into and established relationships with different groups, especially those that experience health inequalities, and can help communicate with them
- they provide expertise in directly working with people and communities in service planning and delivery, including experience of community-centred approaches
- they have knowledge of the needs and strengths of those they work with and can support them to be more directly involved in health and care strategies and plans.
Within ICSs, VCSE sector partnerships should be embedded in how they operate (see the 2021 integrate care system implementation guidance on partnerships with the VCSE sector). All ICBs should have a formal agreement to work with the VCSE sector in governance and decision-making, building on their existing involvement in place and neighbourhood level forums, and where they have well-established relationships with other NHS organisations and partnerships such as Cancer Alliances. This agreement should consider the role of infrastructure organisations including the new VCSE Alliances or leadership groups that can bring strategic voice to governance of ICSs.
Depending on the engagement taking place, it may mean working with national VCSE sector organisations. For example, if redesigning the pathway for a rare condition, there may not be relevant groups in the system, but a national organisation could advise on what approaches to take and help contact people.
At the other end of the scale, health inequalities manifest at highly localised levels, such as wards. Community organisations are close to the ground and with strong intelligence about their communities. These organisations may not be members of system level partnerships. As such, it is vital that they are factored into the design of engagement and co-production processes to reduce the risk of unintentionally excluding local voices.
It is also important to work with informal groups and networks such as user-led organisations, peer support groups and advocacy organisations. Many people who are excluded or stigmatised by society are often involved in their own community group or user-led organisation.
VCSE sector capacity and infrastructure will vary between areas and some organisations will have only limited resources to facilitate and support engagement. They may need financial support to meet the costs of staff time, training or the direct costs of carrying out engagement with communities. Commissioning VCSE organisations to lead engagement with the groups they work with supports investment in community assets and can secure wider benefits by strengthening local organisations. Building longer-term partnerships beyond short-term projects can support financial planning and build the sector’s resilience so that they can help tackle health challenges.
The COVID-19 response saw organisations across the VCSE sector support people and communities. Through ICSs there is an opportunity to deepen partnerships with VCSE sector organisations and, if this does not already exist, to amplify the voices of the communities they work with in decisions about health and care. For more information see Creating Partnerships for Success, NCVO, January 2020 and How health and care systems can work better with the VCSE sector, NHS Confederation, August 2020.
Case study: Embedding the VCSE sector in the planning and design of systems in Humber Coast and Vale integrated care system
There has been close working between the health and care system and the VCSE sector for over 18 months, building strong foundations so that the sector is a key strategic partner in the planning, design and delivery of health and care services.
A well-established VCSE leadership programme has meant that the system has got a mechanism to speak to the sector and the leaders around the table to understand their place. From the outset the approach has always been to make the connections with the partnership and ensure the sector is embedded. This has led to investment in the sector and its involvement in the partnership’s governance and strategic planning. It has resulted in the system embracing the value of the VCSE sector and is proactively involving it at the earliest opportunity.
This early engagement with the VCSE sector has many benefits and being part of the design of services rather than ‘just’ delivery, allows for wider perspectives and different ideas being formed through co-design. Work with the Cancer Alliance has seen the sector shaping proposals around early cancer detection and having a greater reach into targeted communities, which can be delivered by the VCSE. As a result of this increased understanding of the capabilities of the sector, the proportion of the budget allocated for the VCSE is more in line to that for the statutory services, meaning it is seen much more of an equal partnership, rather than an add on.
Social prescribing link workers
Social prescribing link workers (SPLWs) support people with practical, social or emotional needs that affect their physical and mental health. As part of primary care networks, SPLWs work with people to co-produce a simple personalised care and support plan (PCSP) which includes medical needs alongside psycho-social needs. It is a planning process which leads to activities or solutions of care which support the person’s goals, and works with the person’s skills, strengths, and preferences. It addresses the things that are not working in the person’s life and identifies outcomes and actions to resolve these. This could include connecting people to a range of activities, groups and services in their local community, including supporting people to access statutory services, volunteering activities and peer support.
Through their role, SPLWs develop detailed knowledge of their neighbourhood, both in terms of the physical and mental health needs of residents, and the community assets available that can support them. Their local knowledge means that SPLWs may have specific expertise in community-centred approaches and can help facilitate co-production. SPLWs can help identify whose voices need to be heard, and support and facilitate access to engagement opportunities for diverse groups. They can also help identify local community organisations and map existing insight, particularly in relation to health inequalities. In some areas, specialist SPLWs work alongside community development roles to reach specific inclusion health groups and so can act as intermediaries.
Case study: Co-designing a new green social prescribing project to improve people’s mental health and wellbeing and reduce health inequalities
In South Yorkshire and Bassetlaw integrated care system, a green social prescribing project has started to test how connecting with nature, green spaces and the outdoors can improve people’s mental health and wellbeing and reduce health inequalities across the community. The project is also looking at how green space can be accessible to everyone, focusing on people negatively affected by the pandemic, including people from ethnic minority communities.
Co-design, which included working with VCSE sector organisations, community groups and people with lived experience was at the centre of the development of new green social prescribing activities to make sure that they are what people want and need and are accessible.
The project team engaged with local communities in a variety of ways, helping people to get involved in the project in the way that worked best for them. This included working with local voluntary and community organisations, attending local green activities and groups to talk to people, workshops, questionnaires, and offering individual meetings and calls.
The project team and community worked in partnership to reach a set of criteria for new services, such as agreeing that referral pathways to social prescribing projects needed to be expanded to help people less likely to go to the NHS for support connect to social prescribing through trusted community connectors and groups. The group also agreed that working through trusted community leaders would help some ethnic minority communities connect with activities and suggested that promoting case studies featuring people from ethnic minority backgrounds and using communication channels favoured by local communities would increase visibility of support on offer.
People with lived experience of mental ill-health sat on panels to assess grant applications for new green projects and made joint decisions about funding. Working together has helped to form trusting relationships between green spaces and social prescribing services and communities, and funded projects are what people want them to be; accessible, inclusive, and safe to use.
Volunteer and peer roles
These roles provide advice, information and support or organise activities around physical and mental health. They are often part of community-centred services, designed to meet specific local needs and assets. Examples include community champions, research champions, care navigators, health walk leaders and breastfeeding support peers. These are active community members who draw on their local knowledge, skills and experiences to promote physical and mental health. Alongside health improvement and building connections between services and communities, they can support involvement through an in-depth understanding of the different communities’ they work with. Like SPLWs, they can have detailed knowledge of health needs and inequalities, and how engagement approaches can be designed to include diverse groups.
Non-executive roles
The Health and Care Act 2022 requires ICB boards to consist of a chair, chief executive and ‘ordinary members’, appointed by the ICB. Ordinary members can include ‘non-executive members’ defined as members who bring a perspective independent of local health and care organisations (Guidance to Clinical Commissioning Groups on the preparation of Integrated Care Board constitutions – Annex, NHS England, May 2022). The ICB’s constitution must set out how many of these members will be on the board and any qualifying expertise or experience so they can bring different perspectives to the ICB board. There is a requirement that at least one of the ordinary members has knowledge of services relating to mental illness. These can be directors of public health, VCSE sector representatives, or people with lived experience. Non-executive members can provide knowledge of community involvement in prevention and advocate for it across their system. More broadly, the appointment of non-executive members is an opportunity to reflect the diversity of communities and bring their voice to ICB decisions especially where they have been recruited for their knowledge and experience of local communities.
All NHS trusts and NHS foundation trusts have non-executive directors (NEDs) on their Boards. In addition, NHS foundation trusts have a range of governors who represent staff, patients, unpaid carers and service users, and the public, and are elected by the ‘constituencies’ they serve.
NEDs are appointed for their wider board experience and independence. They have a key role in accountability and bringing a different viewpoint to deliberations. NEDs can also support Boards and systems to think strategically about how they connect with local people, having often worked in different sectors, and can be active in and well-connected to the local community.
Public governors provide an important link to local communities, which works in two ways: to help a trust to understand the views of the public; and to help a trust engage with them. They can act as a conduit between patients, the public and trust leadership. However, councils of governors are not restricted to representing members or the interests of a narrow section of the public served by the foundation trust – that is, patients and the public local to the trust or those from governors’ own electorates. Instead, governors are expected to take account of the interests of the ‘public at large’. This includes the population of the ICS that the trust belongs to. The membership system also provides foundation trusts with a ready pool of people who can be more directly engaged in decision-making, with established routes for communication.
Workforce
In many areas, the local authority and the organisations which make up the local NHS are together the biggest local employer (or at least one of the biggest) – which gives them a significant (and in some cases unique) position within the community. NHS organisations can have a positive impact locally as ‘anchor institutions’ – contributing to people’s sense of local identity, and what defines and makes them proud of where they are from. This also enables organisations to have significant impact on the physical and mental health of the immediate community they serve, for example by reducing congestion and pollution by adopting green transport initiatives for staff.
In thinking about working in partnership with local people, organisations should take care to include their employees as part of this group. Staff members will also be users, or potential users, of services, as well as unpaid carers and supporters of family members, friends and neighbours. They will have views of their own about what could improve the health of local people, and about how services could be improved – so it is important to consider how these can be captured. Unions, professional bodies and staff networks can also bring their members’ perspectives.
In addition, staff (particularly in patient-facing clinical and non-clinical roles, such as receptionists, drivers and porters) can be communicators to the public, through informal conversations with people using services. ‘Word of mouth’ remains the most powerful communication tool, especially when those speaking directly to local people are in the most trusted of all professions (nurses and doctors), so it is essential that staff understand initiatives and the rationale behind them. If staff have been actively involved, they are more likely to become ambassadors for local change processes and encourage other local people to get involved and have their say. Staff can have an important role here given that they are more likely to live in the local area and can be powerful influencers within their communities.
Other health and care partners
Other public bodies and organisations may also be active locally in improving health and care. These might include health and care research collaboratives and local social enterprise and entrepreneur networks, as well as Academic Health Science Networks who work to improve health and generate economic growth.
ICBs have a duty to ‘facilitate or otherwise promote research’ and to ‘promote innovation’, and duties around reporting these activities. There is an expectation that communities are involved in these activities (Shared commitment to improve public involvement in research – UKRI). People and communities should be directly involved in identifying unmet health needs and shaping the future research, innovations and health services for their communities. Local and regional research and innovation partnerships often have strong networks with local communities and are a good source of insight into people’s current experience of care as well as aspirations for the future of healthcare.
Organisations should coordinate their healthcare delivery and research work with people and communities. Many health and care organisations that deliver services also undertake research, and the findings can be relevant to how services can be commissioned and provided to tackle inequalities most effectively, improve health outcomes and people’s experiences. This reduces the risk of communities being excluded or overburdened by many different organisations trying to work with them. A coordinated approach across healthcare delivery and research will make it more likely that research will reflect what matters to people and communities and be put into practice to improve health and care delivery. The appendix contains links to relevant resources and initiatives that support the research community to work effectively with people and communities.
Annex B: Legal duties and responsibilities
B1. Public involvement legal duties
This guidance encourages the involvement of people and communities as an ongoing approach, providing opportunities for people to raise the issues and ideas that matter to them, and make decisions with them about their health and care services. As well as best practice, there are specific legal duties for commissioners and providers of health and care services.
Involvement duties on commissioners and providers
To reinforce the importance and positive impact of working with people and communities, NHS England, ICBs and trusts all have legal duties to make arrangements to involve the public in their decision-making about NHS services.
The main duties on NHS bodies to make arrangements to involve the public are all set out in the National Health Services Act 2006, as amended by the Health and Care Act 2022:
- section 13Q for NHS England
- section 14Z45 for integrated care boards
- section 242(1B) for NHS trusts and NHS foundation trusts.
A requirement to involve the public is also included as a service condition in the NHS Standard Contract for providers.
Each of the organisations listed above is accountable and liable for compliance with their public involvement obligations. However that does not mean that each organisation should carry out its public involvement activities in isolation from others within the ICS and beyond. Plans, proposals or decisions will often involve more than one organisation, particularly in respect of integration and service reconfiguration, in which case it is usually desirable to carry this out in an joined up and co-ordinated way, reducing the burden on both the public and the organisations themselves.
The legal duties require arrangements to secure that people are ‘involved’. This can be achieved by consulting people, providing people with information, or in other ways. This gives organisations a considerable degree of discretion as to how people are involved, subject to the below requirements.
Neither the legal duties, nor this statutory guidance, seek to prescribe exactly how to involve people in any given case. Indeed, what is necessary will always depend upon the circumstances. Therefore, while this guidance is ambitious in its intent, it is not intended to place additional legal obligations on organisations and does not mandate that organisations may only discharge their duties in a particular way.
Public bodies are required to act rationally, and this applies to the arrangements they make to involve people. Public bodies can demonstrate that they are acting rationally by keeping good records of decisions taken about when and how to involve the public.
Statutory duties, such as the involvement duties set out above, are not the only circumstances in which a duty to consult may arise. Under common law, a duty to consult may also arise where there has been a promise to consult, where there has been an established practice of consultation, or, in exceptional cases, it would be conspicuously unfair not to consult. There will also be circumstances in which working with people and communities would be beneficial even if doing so is not legal requirement. Therefore, whether or not the involvement duties apply is not the only consideration when deciding whether and how to work with people and communities.
Individuals, carers and representatives
These public involvement duties have applied to commissioners and providers for many years and are largely unchanged. However, a significant change introduced by the Health and Care Act 2022 is that, in respect of NHS England and ICBs, the description of people they must make arrangements to involve has been extended from ‘individuals to whom the services are being or may be provided’ to also include ‘their carers and representatives (if any)’. While it is already common practice to involve carers and their representatives – and to do so is in line with previous statutory guidance on the public involvement duties – this change makes it a legal requirement for arrangements for public involvement to secure the involvement of carers and representatives (if any), as well as service users themselves.
The legislation does not include a definition of carers or representatives. However relevant carers[1] and representatives should be identified by reference to the individuals who use, or may use, the services in question. It is up to local organisations to identify who to involve – depending upon the circumstances, nature of the services and decision-making process in question – but relevant carers and representatives could include young carers, individual patients’ advocates or family members who help organise their care, as well as councillors and community leaders, VCSE sector organisations, local Healthwatch and other organisations able to represent the interests of the individuals who use, or may use, the services in question.
A stakeholder analysis can help determine which groups are relevant representatives depending on the context. More than one of these representative groups may need to be involved alongside people with lived experience to ensure that the full range of views can be considered.
A process for assessing whether the legal duty to involve applies
NHS England has developed a three-step process for assessing whether the legal duty to involve applies. ICBs and trusts may use their own process or adopt this one. They should be able to demonstrate that they assess whether the duties apply to plans, proposals and decisions about services and, where they do, that they are properly followed.
Accessible diagram text:
The diagram shows the three steps for assessing whether the legal duty to involve applies.
Step 1: Does the activity relate to services the organisation is responsible for commissioning or that the provider is responsible for delivering?
If yes: Go to Step 2
If no: The legal duty to involve does not apply
Examples are:
- A decision about the relocation of a community diabetes service commissioned by an ICB and delivered by a trust does
- A decision about the relocation of an ICB’s or trust’s administrative offices does not
Step 2: What type of activity is it? The duty applies to three types of activities:
- Planning: Commissioners are required to always have arrangements in place to involve the public in the planning of commissioning arrangements; trusts must have them in place in the planning of provision of those services. If the activity relates to planning then the legal duty applies regardless of the impact it may have at step 3
Example: The development of an ICB policy for the commissioning of diabetes services.
- Proposals for change: This activity includes not only the consideration of proposals to changes to how services are commissioned or delivered, but also the development of such proposals. If the activity relates to proposals for change, go to step 3.
Example: Development of options for the reconfiguration of urgent and emergency care and the subsequent consideration of any developed options or model.
- Operational decisions: This activity relates to decisions made by the commissioner or trust that change or affect the way a service operates. If the activity relates to operational decisions, go to step 3
Examples: Making changes to the opening hours or locations of a service, or the closure of a clinic for operational reasons
While the legislation distinguishes between these different types of activity, as can be seen by the examples opposite they often overlap and sometimes a plan, proposal or decision can fall into more than one category. Where the duty sits with commissioners and providers also overlaps and the duty can apply to both. In these cases there is an opportunity for commissioners and trusts to work jointly with people and communities and meet their legal duties without duplicating effort and activities.
Step 3: would there be an impact on service delivery or the range of services?
An impact on services can arise in two ways:
- An impact on the way services are delivered to individuals, for example the transfer of a service to another location; and/or
- The range of health services available to individuals, for example the closure of a service of limited clinical benefit to fund investment in other services.
If yes – the legal duty to involve applies
If no, the legal duty to involve does not apply
The impact on services should be considered from the perspective of patients and not necessarily limited to the clinical services being commissioned or provided. Accessibility, transport links and ambulance availability are all examples of matters that could be significant in considering impact. An Equality Impact Assessment can help identify which groups are likely to be affected.
Examples:
Impact on services
- The closure of a GP practice would mean patients having to find a new practice to seek treatment. This would impact upon the way in which services are delivered to patients. The degree of the impact will depend on how far individuals will have to travel to access another GP practice as well as any specific care that may have been provided at the practice. In such circumstances it is likely that the legal duty to involve applies.
No impact on services
- The retirement of a GP from a practice may mean that patients with a preferred choice of doctor will need to be seen by a different GP. However, this would not typically affect the range of services or the manner of their delivery, in which case the legal duty to involve is unlikely to apply.
- The award of a new contract to a podiatry provider, with no change in the specification of such a contract, would not ordinarily be expected to result in changes to the way that services are delivered to patients or the range of services available. In such circumstances it is unlikely the legal duty to involve will apply.
The Gunning principles
Commissioners and trusts must ensure that their arrangements to involve people are fair.
The courts have established guiding principles for what constitutes a fair consultation exercise, known as the Gunning principles. These four principles relate to public consultation processes and do not create a binding legal precedent for how other ways of involving the public should be carried out. However, they will still be informative when making arrangements to involve the public, whatever the form of those arrangements.
1. Consultation must take place when the proposal is still at a formative stage.
Meaningful consultation cannot take place about a decision that has already been made. There is no requirement, and it would be misleading, to consult on options which are not genuinely under consideration, or are undeliverable – but it may be necessary to provide some information about realistic alternatives.
2. Sufficient information and reasons must be put forward for the proposal to allow for intelligent consideration and response.
Those being consulted should be provided with sufficient information to enable them to understand what the proposal is and the reasons why it is being considered. They should be made aware of the criteria against which proposals have been or will be judged. This may involve providing information about realistic alternatives and the reasons why they are not also being considered. The level of detail provided will depend on the circumstances such as the complexity and impact of the proposal.
3. Adequate time must be given for consideration and response.
People must have enough time to properly consider and respond to the consultation. What is adequate will depend upon the circumstances and is not prescribed by law. However, a time period may be inadequate if it is during a holiday period or only allows a short time for the public to consider complex proposals.
4. The product of consultation must be conscientiously taken into account.
Decision makers must be able to show that they have given consideration to what they have heard during the consultation and that they have borne this in mind when the ultimate decision is taken.
B2. Other relevant legal duties
The Equality Act 2010
The Equality Act 2010 prohibits unlawful discrimination in the provision of services on the grounds of protected characteristics. These are: age; disability; gender reassignment; marriage and civil partnership; pregnancy and maternity; race; religion or belief; sex and sexual orientation.
As well as these prohibitions against unlawful discrimination the Equality Act 2010 requires public sector organisations to have ‘due regard’ to the need to:
- eliminate unlawful discrimination, harassment and victimisation and other conduct prohibited by the Act
- advance equality of opportunity between people who share a protected characteristic and those who do not
- and foster good relations between people who share a protected characteristic and those who do not.
This is known as the ‘public sector equality duty’ (section 149 of the Equality Act 2010).
Working with people with characteristics protected under the Act means understanding how decisions or policies can affect them and whether they will be disproportionately affected. Following this guidance will be an important part of meeting the equality duty.
Health inequalities
NHS England and ICBs are also under a separate statutory duty to have regard to the need to reduce health inequalities of access to health services and the outcomes achieved (sections 13G and 14Z35 of the National Health Service Act 2006, respectively). By understanding the needs of people experiencing health inequalities, services can work with them to reduce barriers to access and design improvements.
Duty to promote innovation and research
ICBs have statutory duties in relation to innovation and research (sections 14Z39 and 14Z40 respectively of the Health and Care Act 2022). These cover how ICBs must promote innovation and facilitate or promote research in the provision of health services. ICBs should explain in joint forward plans how they propose to discharge their innovation and research duties and include in annual reports an assessment of how the ICB has discharged its research and innovation duties. Working with people and communities will play a key role in discharging these duties. NHS England will publish specific guidance in 2022/23 for ICBs on how they can support and facilitate research, including further information on the involvement of people and communities.
Public Services (Social Value) Act 2012
This requires people who commission public services to think about how they can also secure wider social, economic and environmental benefits. There are several benefits to local communities in embedding social value in commissioning, including improved service delivery, health creation and an increase in the resilience of communities. Working with a range of VCSE organisations on new approaches to engaging diverse communities in service planning is an example of how NHS organisations can bring social value to their commissioning. This links to the role of the NHS as anchor institutions, using their assets to promote the physical and mental health of their local communities and harnessing their spending power to address health inequalities and invest in health (Anchor institutions and how they can affect people’s health, The King’s Fund, September 2021).
B3. Service reconfiguration and public consultation
The Secretary of State’s functions in relation to service reconfiguration introduced by the Health and Care Act 2022 will commence at a later date. The Department of Health and Social Care will publish statutory guidance on these functions, alongside updating the 2014 Local Authority Health Scrutiny guidance. NHS England will also update its guidance on substantial service change to reflect the new functions.
Applying the principles to major service change
Changing how services are planned and delivered will happen for several reasons. These include to improve the quality of services and patient experience to address prevailing inequalities in health outcomes in a community, or to adapt to changing clinical practice.
A critical success factor is open community and stakeholder involvement from the first stage of considering change (Insight on effective NHS service change from the Independent Reconfiguration Panel, February 2020). This means involving people at the earliest opportunity in co-designing what the future health and care services for their area looks like. It means building on the conversations that systems should already be having with people about what a health community might look like and using their existing approaches as a starting point for producing service change proposals.
Service change proposals can be subject to judicial review or be referred by the local Health Overview Scrutiny Committee (HOSC) to the Secretary of State for Health and Social Care, particularly if they have not been sufficiently involved. In undertaking service change, systems must comply with their legislative duties to engage the public, consult their HOSC where required and have regard to the need to reduce health inequalities, and to have due regard to the Equality Act and the Public Sector Equality Duty. In carrying out these duties, consistent and meaningful involvement from people and communities is fundamental.
One of the most important early steps to take is to build long-term relationships and invest resources in developing partnership approaches with key community and political leaders, including politicians, faith leaders and VCSE sector organisations. Clinical Senates also bring a public perspective to significant service reconfiguration. They bring together clinicians, patients and other partners to assist commissioners and providers to make the best decisions about healthcare for the populations they represent. Clinical Senates will assure the contents of a service change’s Pre-Consultation Business Case (PCBC), including approving the involvement of patients and the public in any clinical modelling that has been undertaken.
Every effort should be made to include local Healthwatch organisations in the decision-making process at an early stage, where they may offer support and advice as to the best way to engage with the groups affected by the change, as well as sharing existing relevant insight. Where a proposal is likely to have an impact across a wide geographical area, it will be necessary to work with all the individual Healthwatch organisations to ensure that all areas are appropriately represented.
Every system that plans to change how its services are delivered should undertake an Integrated Impact Assessment (IIA) to understand pre-existing access to and understanding of the services available. This assessment can support commissioners to identify and reach diverse communities that may be affected by these changes. Local Healthwatch and VCSE sector organisations can support commissioners to engage these communities, and to develop meaningful long-term relationships with them in the design and delivery of reconfigured services.
Inevitably, some transformation proposals will be so contentious that any amount of good planning, relationship building, and mitigation will not prevent significant local opposition. In these circumstances, systems should consider the following core principles:
- maintaining a civil discourse: All partners should work hard to maintain a civil discourse throughout the process and avoid disengaging from dialogue or publicly criticising other partners
- ongoing and continuous dialogue with communities: Engagement even from the early planning stages, before formal service change proposals are made, can support understanding about the process and rationale for decisions, including how people have been included and their views considered. This needs visible leadership from Board level
- learn from previous proposals: Communities often have longer memories than the professionals who may change roles and move. Understanding the local history of change that communities have experienced helps to learn and build trust with people
- scope of proposals: All engagement must have a clearly defined scope and the ability to have some influence. For example, it is not appropriate to consult on options that are not genuinely under consideration or are unviable or unrealistic
- length of consultation: When planning a public consultation, consideration should be given to the amount of time necessary – a longer consultation is not always best. Government advice is that consultations should last for a proportionate amount of time. Shorter consultations backed by significant evidence of engagement beforehand may be most effective. Long and unpopular consultation processes, however well meaning, can negatively impact on the long-term relationship with communities and partner organisations. However, in all circumstances you should ensure that the consultation is long enough so that interested parties have the time to respond. This may include giving them time to consult within their membership. Through demographic monitoring, you may also need to factor in time to undertake additional engagement with communities that have not previously been adequately involved. The length and timing of the consultation and other engagement activities can be affected by pre-election periods, during which consultation should generally not be launched
- access to information: As part of the consultation process you should ensure that people have access to the information that they need. This should be accessible, timely and easy to understand with potential benefits and drawbacks clearly set out. This will allow them to give an informed opinion that may take account of significant factors about which they may not have been aware previously. Alternative formats (such as easy read documents) must be ready at the same time. Good practice indicates that public-facing versions of business cases, such as the plan for public consultation, will help communities to understand proposals more easily. Certain documents, such as the Pre-Consultation Business Case, and the Decision-making Business Case, will be publicly available and systems should ensure these are clear, succinct and easy for everyone to access
- continuing dialogue throughout consultation: The consultation process should not close all other communication with stakeholders. You should consider whether it is it is appropriate to share information openly and to maintain an ongoing dialogue
- addressing issues raised by all groups: Significant service change will often arouse a lot of public interest, including from campaign groups. Any public consultation needs to ensure that all opinions provided as part of the consultation are heard, but also must consider that there may be a range of views. Responses to public consultation should address significant issues raised by all groups and show how they have been considered. This underlines the importance of involving all groups affected by the change but who may be less likely to take part in public consultations
- public-facing decision-making: Once consultation has completed, and responses have been independently consolidated and considered, a decision regarding the agreed way forward should be made in public and communicated clearly.
Finally, it should be emphasised that systems that have ongoing, meaningful involvement of people and communities, are more likely to develop proposals where issues, barriers, opportunities and solutions have been thought through together. This gives them a firm basis before going out for wider consultation.
Case Study: Community hospital change
The NHS in Gloucestershire used a Citizens’ Jury to decide the location of a new community hospital instead of having two hospitals. The change had been proposed and firmly rejected more than 10 years previously by a very vocal and well-organised opposition.
Communicating to the public that it was not possible to deliver high quality care across two sites comprised of older buildings was seen as challenging as the local population have experienced high-quality care in both hospitals over time and may not understand the benefit that a new site would bring to the quality of their care.
To involve the public in the change process and gather strong public evidence, the team needed to recognise the strength of local feelings and emotions rooted in the area.
The presence of local staff at involvement events who understood the history of the two hospitals helped to acknowledge the significance of the change for local identity. Their presence helped support residents to provide views about quality of care. They also reported that showing the experience of new community hospitals elsewhere in the county helped highlight the increased quality of care that could be delivered at a new site. This approach helped the public navigate the tension between local access to services and quality of care.
A combination of traditional and deliberative involvement informed decision-making and design at each stage. Qualitative evidence gathered through public events and discussions helped answer the question, ‘what good looks like’ at the pre-consultation business case stage. It highlighted issues around access and the potential impact of inequalities that the team would need to consider in more depth in the design of options.
The site selection stage of options development used an independent Citizens’ Jury to make a recommendation from three possible locations. A Citizen’s Jury is an involvement method where a small group of the public are selected to deliberate over a policy issue and asked to make a recommendation based on evidence presented. The Jury has no decision-making power as it is not a legal entity, and instead makes a recommendation to the local NHS as accountable decision-makers. Neither the Trust nor the CCG had a preferred option out of three possible locations – all were understood to have the potential to deliver high quality care. The local population did have preferred options – it was a highly contentious local decision.
The jury was run by an independent company that recruited a mix of residents through public advertisement where residents applied to take part. This ensured a geographical spread across the area and as well as selecting people who were genuinely interested to take the recommendation-making responsibility.
The system accepted the Citizens’ Jury recommendation because they trusted the process that had created more neutral, clinically framed public evidence.
Health overview and scrutiny
Where changes are proposed which are a substantial development of the health service in the local area, or a substantial variation in the provision of the service, commissioners and providers of NHS services (including NHS England, ICBs, trusts and private providers) are under a duty to consult all relevant local authority Health Overview and Scrutiny Committees (HOSCs) on the change. Ordinarily, the commissioners (ICBs or NHS England) will carry out this exercise on behalf of providers.
HOSCs contribute constructively, in the interests of their communities, to plans. Councillors can highlight potential risks which might not otherwise be apparent – their unique perspective and insight, derived from their role in the local community, provides vital intelligence for policymakers and a particular credibility in giving voice to public concerns. They will expect to see how NHS commissioners and providers have engaged people in developing plans and that equalities issues have been considered. Where relationships are positive, the management of proposals for substantial variations or other major changes will be easier.
Where there are concerns about proposals for reconfiguration then local authorities can formally refer them to the Secretary of State, for example if the HOSC does not view the proposal as in the interests of the health service of its area or that consultation with the HOSC on the proposal was inadequate. Early and transparent engagement can minimise the likelihood of referrals to the Secretary of State and any damage to the relationship between the NHS, local authorities and communities.
Judicial review
If a person with sufficient interest in the matter disagrees with either the proposals or the Secretary of State’s decision in relation to a referral, they can seek the court’s permission to bring a Judicial Review (JR). It is important to note that under a JR the court will not typically scrutinise the merits of a decision made by a public body, or substitute its own decision. Rather, the court will scrutinise the process by which the public body has come to this decision, and may ‘quash’ the decision if it finds it to be unlawful. This scrutiny may include whether legal duties regarding public involvement and equality have been met. Strong, consistent and continuous involvement of the public, and good records to demonstrate that this has been done in compliance with legal duties, will reduce the risk of an application for JR materialising, being granted permission by the courts, or ultimately succeeding.
B4. Integrated Care Systems’ responsibilities
Integrated care systems (ICSs) have been set up to improve outcomes in population health and healthcare, and to support and promote partnership working to address broader health inequalities. The underlying principles to achieve these aims are collaboration between partners within and outside the NHS, and that decisions are taken as close as possible to the people they affect. ICSs are encouraged to identify the best way to improve the physical and mental health of their populations, address health inequalities, and provide joined-up, efficient and effective services. ICSs should build on existing work with people and communities. For example, the approaches and networks of the Clinical Commissioning Group (CCG) predecessors and other partners within the ICS.
There is separate guidance for integrated care partnerships, place-based partnerships and provider collaboratives which includes how they should work with people and communities. They can use the 10 principles in Chapter 4 to develop their approaches, ideally collaboratively with all partners, for working with people and communities.
Specific opportunities and minimum expectations for each are detailed below.
Integrated care boards (ICBs)
ICBs have a legal obligation to include in their constitutions
- provision about the arrangements to be made by them for discharging their public involvement duty, and
- a statement of the principles to be followed by them in implementing those arrangements (paragraph 14 of Schedule 1B to the National Health Service Act 2006).
In addition they should:
- have a process for updating and reviewing progress on its strategy for working with people and communities (see Annex B5)
- adopt clear and transparent mechanisms for developing joint forward plans with people and communities, and include in these details of how they will meet their statutory duties on public involvement, research and innovation
- work with partners across the ICS to develop arrangements for ensuring that ICPs and place-based partnerships have representation from local people and communities in priority-setting and decision-making forums
- give workforce the time, resources and support to deliver on working with people and communities.
Where a process to involve people has already started by one of its legacy CCGs, ICBs will need to be assured that this meets the legal duty for which they are now responsible. Where good arrangements are already in place, ICBs should continue and build on the work already underway.
Under section 14Z59 of the National Health Service Act 2006, NHS England has a duty to assess the performance of ICBs on various duties, including those under section 14Z45 for public involvement. This will be included in the new System Oversight Framework, building on the approach that took place for CCGs where a specific indicator was included in their oversight framework. The process will include providing evidence of the how the ICB meets the 10 principles in this guidance and the difference that working with people and communities has made. It will look for evidence of meaningful involvement taking place consistently across the ICB’s places and neighbourhoods.
NHS England will work with partners including ICBs to design the new indicator and will issue specific guidance for ICBs as part of the overall system oversight framework in 2022/23.
Integrated care partnerships (ICPs)
ICPs should:
- be open and transparent, agreeing arrangements for accountability, including meeting in public and providing accessible information about their plans and strategies
- build on the expertise, governance arrangements and engagement forums that already exist, such as Health and Wellbeing Boards, and so avoid duplication and ensure joined-up decision-making
- develop a structured and meaningful approach to how they work with people which brings accountability. This could include engagement on its strategy, co-producing sections with people with relevant lived experience, and collecting quantitative and qualitative evidence
- include membership from the VCSE sector, Healthwatch and people with lived experience who can bring expertise on how the ICP can engage its population and provide scrutiny that it takes place effectively.
Working with people and communities at place level
It is at place level that many engagement activities will happen. It contains health and care services that people use frequently, including those provided by councils and the VCSE sector, and so is a level that people can often recognise more easily than a system. It is also to places that some commissioning will be delegated by ICBs and NHS England.
Place-based partnerships
Place-based partnerships should:
- have clear and transparent mechanisms for ensuring strategies and changes are developed with people with lived experience of health and care services and wider communities
- Work with their coterminous Health and Wellbeing Boards to identify priorities to improve the health of their communities
- build on existing approaches and networks for engaging and co-producing with people and communities, including those run by providers and the former CCGs
- support PCNs and neighbourhood teams to work with people and communities using community-centred approaches to strengthen health improvement and treatment. This might mean working with existing neighbourhood provision such as from the local authority or housing associations, networking Practice Participation Groups so they share insight and learning across the PCN, and leveraging the links that GPs and primary care staff already have into their communities. Resourcing this work at neighbourhood level can support place and system level engagement.
Provider collaboratives
Provider collaboratives should:
- share and build on the good practice that exists in their member organisations, such as co-production approaches and partnerships with experts by experience
- draw on the community connections of foundation trust governors, and use insight and feedback from patient surveys, complaints data and partners like Healthwatch
- each provider organisation within the collaborative will need to meet its own legal duties on public involvement where programmes result in changes that impact how patients receive services
- explore community-centred approaches to enable both better decision-making and new approaches to outreach for communities of both geography and experience (for instance, people with the same condition).
System quality groups
ICSs have responsibilities for quality to ensure services are consistently safe, effective and provides a personalised experience. Working with people and communities forms part of how systems can achieve these aims.
All ICSs must have a System Quality Group (SQG) to engage and share intelligence and improvement for quality. These groups provide an important strategic forum within ICSs at which partners can share and triangulate intelligence, insight and learning on quality matters across the ICS and identify actions for improvement.
Guidance on SQGs is available here: National Guidance on System Quality Groups. Part of their scope is to improve the safety of NHS care and people’s experience of care through co-design and co-production. This includes involving people with relevant lived experience as equal partners in the full range of SQG activities, including co-designing improvements. Membership must include at least two patient safety partners (see below) and two members with lived experience or from local Healthwatch. It is possible that the patient safety partners may also have lived experience and work for Healthwatch. The groups are therefore an important source of insight into what matters to patients and a forum which works with people to make quality improvements.
The guidance also covers place-based quality groups which are expected to include two people with lived experience. It is also expected that people with lived experience are on any task and finish groups reporting to SQGs. Examples established to date include maternity, children and young people, and safeguarding.
Patient safety partners
The NHS Patient Safety Strategy recognises the importance of involving patients, their families and carers and the public in improving the safety of NHS care. One way this is achieved is through the new role of Patient Safety Partners (PSPs) which is required in all NHS organisations. PSPs are patients, carers, family members or other people who work in partnership with staff to influence and improve the governance and leadership of safety within an NHS organisation.
PSPs’ roles include involvement in patient safety improvement projects, membership of safety and quality committees and participation in investigation oversight groups. They therefore offer unique insight into safety from a patient perspective and as potential partners in quality improvement projects. Further guidance is available here: Framework for involving patients in patient safety.
B5. Strategies and reports
There are statutory requirements for organisations in integrated care systems (ICSs) to produce strategies and plans for health and care. These are the minimum requirements for who must be involved:
Accessible diagram text:
The diagram shows the minimum requirement for who must be involved in each ICS strategy and plan.
Joint strategic needs assessment
- What does it do? A comprehensive analysis of the current and future needs and assets of their area relevant to health, social care and public health
- Who prepares it? Local authority (through the Health and Wellbeing Board) and local ICBs
- Who must be involved? Local Healthwatch, local people, district councils (where applicable) and any other appropriate persons
Joint local health and wellbeing strategy
- What does it do? Plans the delivery of integrated local services based upon those needs and assets to collectively address the underlying determinants of health and wellbeing
- Who prepares it? Local authority (through the Health and Wellbeing Board) and local ICBs
- Who must be involved? Local Healthwatch, local people
Integrated care strategy
- What does it do? Sets out how the assessed needs in an area are to be met by the ICB, NHS England and relevant local authorities
- Who prepares it? ICP
- Who must be involved? Local Healthwatch, local people
Joint forward plan
- What does it do? Sets out how the ICB and its partner NHS trusts and NHS foundation trusts will discharge its duties over the next five years, including in relation to public involvement and reducing inequalities
- Who prepares it? ICBs and partner NHS trusts and NHS foundation trusts Who must be involved? Local people, Health and Wellbeing Boards and any other appropriate person.
Other reports and strategies which should demonstrate how organisations are working with people and communities are included below.
Annual reports
Integrated care boards (ICBs) and NHS England have a duty to produce annual reports that must show how their public involvement duties have been met (sections 14Z58 and 13U of the National Health Service Act 2006 respectively). The reports must also explain how they discharged a variety of their duties, including their duties in relation to improvement in quality of services, research, reducing inequalities, the triple aim and public involvement.
Organisations can take different approaches to how they do this – they can incorporate it in their main annual report or produce a separate one dedicated to public involvement. However the following should typically be included:
- governance and assurance information: an overview of the structures and processes that support working with people and communities, and how these work at different levels of the organisations, including place-based partnerships and primary care networks
- how the strategy on working with people and communities has been put into practice: how the role of the public in governance structures have been achieved, how it has worked with people in priority setting and decision-making, and examples of approaches used to work with people and communities
- the key involvement activities that have taken place: what the changes have been for service delivery and health outcomes, how activities were designed to reach specific groups and the voices of those experiencing health inequalities were heard
- patient insight and data: how intelligence about people’s needs and experiences was gathered and how this informed decision-making and quality governance
- information presented in an accessible and appealing way for a public audience. This applies to the main annual report and to any separate one covering involvement
- the evidence that equality and inclusion principles were considered when with working with diverse communities.
The information accessible and appealing, considering the needs of the diverse groups of people in the area. NHS England is producing new guidance in 2022/23 which explains these requirements in detail, and updates Annual reporting on the legal duty to involve patients and the public from 2016.
ICB strategies on working with people and communities
Although not a statutory requirement, each ICB has prepared a strategy for working with people and communities. The strategy should describe the ICB’s:
- principles and approaches to working with people and communities
- approach to working with partners so people and communities are involved in priority-setting and decision-making forums across the ICS
- arrangements for gathering intelligence about the experience and aspirations of people who use care and support, and its approach to using these insights to inform decision-making and quality governance.
The strategy helps promote consistency of approaches across systems. It is an important element in how ICBs demonstrate to people they intend to work with them, and one which will develop over time. NHS England’s assurance of ICBs’ public involvement duties will include how the strategy is monitored and reviewed, and how further iterations are developed with people and communities.
Provider quality accounts
A Quality Account is a report published annually about the quality of services offered by an NHS healthcare provider, including trusts. It reports on patient safety, the effectiveness of treatment and patient feedback, so is an important way to demonstrate how providers are acting on insight to improve continuously its services.
Drafts must be shared with NHS England and relevant ICBs, local Healthwatch and HOSCs, with any comments included in the final version. Healthwatch and HOSCs are best placed to provide meaningful comment when there has been continuous engagement with them by the provider on their priorities.
Producing a Quality Account should not be a one-off exercise, but rather a year-round process of engagement with the public, including with foundation trust governors and members, local Healthwatch and patient groups. Providers may organise specific engagement on their Quality Accounts to agree with people the actions that it will take improve the services it delivers.
Quality Accounts must be published by the trust. The language and layout should be accessible and appealing to the public to improve accountability.
Case study: Co-producing a patient and public involvement strategy
East of England Ambulance Service NHS Trust (EEAST) needed to develop a Patient and Public Involvement Strategy to provide clear direction to how it works with its communities. It was decided that the strategy should be approached as a co-production project and to effectively start from a blank page.
The Trust understood the importance of co-production to produce the strategy but had not previously had much experience working in this way, especially for such a large project. Co-production was a move away from the traditional consultation process, and collectively led by the people who would be affected by the strategy. The Trust reached out to Healthwatch Suffolk, who then delivered comprehensive co-production training, with these sessions explaining the culture of co-production, the underpinning principles, and the benefits of using co-production for such a project.
With support from their Healthwatch partners, the strategy was developed through a series of 16 co-production workshops, with 70 attendances by patients, community representatives, volunteers, and specialist groups. Each session took an open approach but included key questions which were used to build foundations for the strategy. Co-production sessions were as inclusive as possible and were offered at a variety of times to suit the needs of individuals and community groups.
All the feedback received was collated and a thematic review was then undertaken, which identified five key themes (Ethos, involvement and engagement, accessibility, networking and communication). In true co-production style, further sessions were organised to feedback and sense check in relation to the themes identified, concluding with strategy writing workshops with the patients and the public, to decide on the language used within strategy.
The strategy is currently into the process of being officially launched, although both the strategy on a page and easy read version are available on the Trust’s public website.
B6. Resources and learning
NHS England offers a range of learning and resources to help put this guidance into practice. More information is available on the Start with People network.
The following are some other resources and guides on different ways of working effectively with people, including groups with specific needs.
Benefits of working with people and communities
- Building trusted relationships with partners and communities, resources for NHS leaders, NHS Leadership Academy, 2022
- Community Power: The Evidence New Local, 2022
- Community engagement: improving health and wellbeing and reducing health inequalities National Institute of Health and Care Excellence, 2016
- Understanding integration: how to listen to and learn from people and communities King’s Fund, 2021
Community-centred approaches
- Community-centred public health: taking a whole system approach, Public Health England, 2020
- Health and wellbeing: a guide to community-centred approaches, Public Health England, 2015
- Asset-Based Community Development for Local Authorities, NESTA, 2020
- Evidence for strengths and asset-based outcomes, Social Care Institute of Excellence, 2019
Supporting different groups to take part
- West Yorkshire Health and Care Partnership has collated resources on trauma informed approaches
- Integrated health and social care for people experiencing homelessness, National Institute of Health and Care Excellence, 2022
- Seldom Heard – Engaging young people in health services research and service design, Challenging Behaviours Foundation
- Engaging young people in health services research and service design The Association of Young People’s Health, 2022
- Valuing the Views of Children with a Learning Disability Challenging Behaviour Foundation and Mencap, 2021
Involvement in health and care research
The National Institute of Health and Care Research (NIHR) has several resources to support involvement in research including:
- UK Standards for Public Involvement which support the research community to work effectively with people and communities
- People in Research website which links people and communities to opportunities to shape research
- Include Ethnicity framework to help the research community become more inclusive.