Enhanced Therapeutic Observations and Care programme
What is Enhanced Therapeutic Observations and Care (ETOC)?
Enhanced Therapeutic Observation and Care (ETOC), often referred to as enhanced care, enhanced therapeutic observations, 1:1s or specialling, is an intervention which contributes to safe and effective care of patients. The intervention should promote recovery and preserve dignity. Typically, ETOC is undertaken by a Healthcare Support Worker (HCSW), Registered Nurse (RN) or a Registered Mental Health Nurse (RMN).
Background to the programme
The NHS is caring for more patients with complex needs who require ETOC. The NHS must ensure the workforce is effectively engaged, trained and deployed to provide innovative, patient centred solutions that promote therapeutic and safe care.
In August 2024, NHS England launched the ETOC programme, which supports trusts to make local, clinically led, and patient centred approaches that improve their care provision.
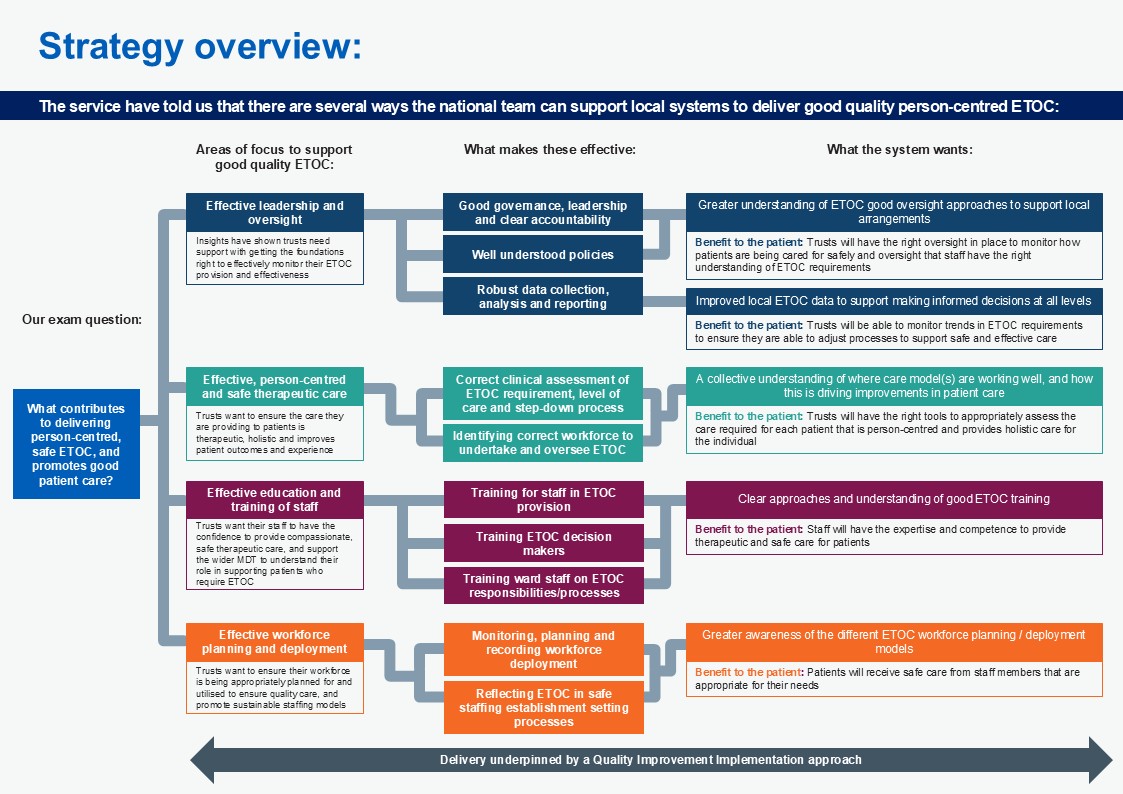
Co-designed with clinical leaders, frontline staff and wider stakeholders four main pillars have been identified to support systems to provide quality patient care. These four pillars inform the programme strategy:
- effective leadership and oversight – including governance, data, local assurance, clinical policy making.
- effective person-centered and safe therapeutic care – including identifying the need for ETOC, monitoring and stepdown.
- effective education and training – ensuring that that staff are trained in reviewing, providing and overseeing ETOC.
- effective workforce planning and deployment – planning for levels of ETOC, ensuring that ETOC is considered during safe staffing establishment setting processes.
Programme aims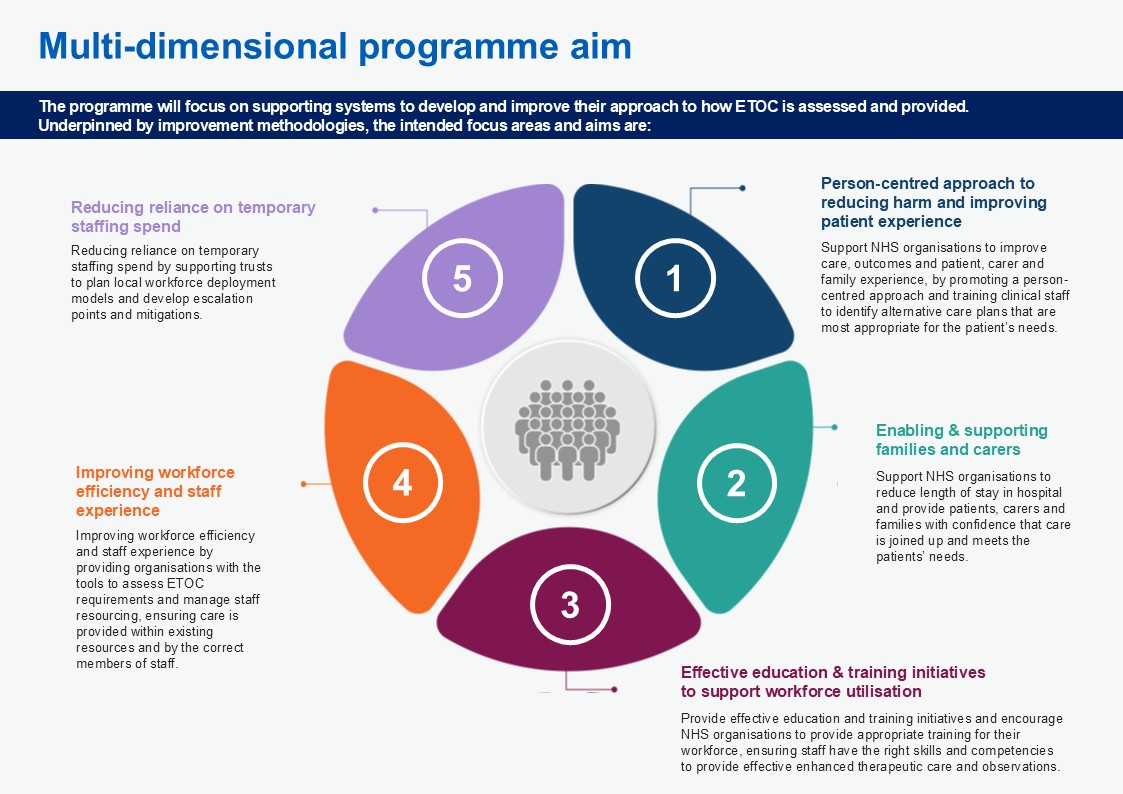
The aims of the programme are listed below.
- Support NHS organisations to improve care, outcomes and patient, carer and family experience, by promoting a person-centred approach and training clinical staff to identify alternative care plans that are most appropriate for the patient’s needs.
- Support NHS organisations to reduce length of stay in hospital and provide patients, carers and families with confidence that care is joined up and meets the patients’ needs.
- Provide effective education and training initiatives and encourage NHS organisations to provide appropriate training for their workforce, ensuring staff have the right skills and competencies to provide effective enhanced therapeutic care and observations.
- Improving workforce efficiency and staff experience by providing organisations with the tools to assess ETOC requirements and manage staff resourcing, ensuring care is provided within existing resources and by the correct members of staff.
- Reducing reliance on temporary staffing spend by supporting trusts to plan local workforce deployment models and develop escalation points and mitigations.
The program aims to create a holistic, compassionate approach to healthcare delivery, focusing on continuous improvement and human-centered care.
ETOC strategy
Working with nurse leaders, NHS England has co-developed a programme strategy focusing on high-quality, patient-centred ETOC.
Each pillar has been supported by a co-design advisory group and task and finish groups with the aim of helping organisations with their ETOC provision.
The diagram below outlines what the system has told us links to good-quality ETOC and what support the system needs to make these 4 pillars effective.
This diagram shows how national support for local ETOC systems flows from left to right through 3 stages:
- Focus areas: Leadership, commissioning frameworks, staff training and workforce management.
- Effective practices: These include governance structures, needs assessment, staff training programs and workforce planning.
- System outcomes: Each focus area leads to specific improvements, including better oversight, data-informed decisions, consistent training and appropriate staffing models.
Each outcome includes a patient benefit, such as better monitoring of service delivery, safer care processes, person-centred support and appropriately skilled staff.
The elements interconnect rather than existing in isolation. For example, effective leadership supports appropriate training, while good workforce planning depends on strong leadership and commissioning.
All activities are underpinned by a quality improvement transformation approach to deliver better patient care.
The output of the strategy has several resources which have been co-developed by clinical leaders with the aim to support organisations in the delivery of enhanced therapeutic observations and care.
- a guide to improving data collection and reporting
- developing a local policy
- embedding therapeutic practice
- education and training
Programme delivery
There are two key mechanisms to deliver the ETOC programme: a bespoke support offer and a universal support offer.
The bespoke support offer
NHS England’s Nursing Workforce Policy and Implementation Team is initially working with 14 organisations from across England to review their ETOC provision following a 90-day improvement cycle.
Two trusts from each region have been selected, following an expression of interest process. The bespoke offer provides engaged trusts with clinical insights and a peer network to help them to learn and share, whilst honing their improvement plans. The insights from this cohort will support the production of the wider programme.
Effective leadership and oversight case study-
East and North Hertfordshire NHS Trust
In 2015 the decision was made to build an in-house specialist, substantive enhanced care team. Specialist training was provided to the team, drawing from various areas of expertise, including critical care outreach and moving and handling, to equip them with the necessary skills for enhanced patient care.
The team developed a process and policy for enhanced care, ensuring daily reviews of patients by team leaders and establishing a central point for all enhanced care requirements, which removed the capacity for ward leaders and managers to independently allocate shifts. The enhanced nursing care team manager became the sole authority for shift allocation, with the support of duty matrons or site matrons in their absence, to ensure proper review and assignment of enhanced care requirements. Monthly audits of risk assessments were introduced, allowing for data comparison and the introduction of ‘bay watching’ and the ‘John’s campaign’ to further enhance patient care.
The digitisation of documentation and the adoption of a virtual roster have led to more efficient operations, with a behavioural observation chart introduced to monitor patient activity and identify patterns for enhanced care needs. Enhanced care assessments are now completed on the EPR system, with care plans and acuity assessments required to be filled out, ensuring real-time support and proper patient care planning. The digitised system allows for proactive redeployment of staff, with a communication system in place to ensure staff can be reassigned as needed, enhancing flexibility and responsiveness to patient needs.
The enhanced care team’s efforts have led to a notable reduction in patient falls and associated harm, contributing to improved patient safety and care quality. Improved compliance with care plans and risk assessments has been achieved through the digitisation of documentation, ensuring patients are assessed in real-time and receive the necessary support promptly. Staff training and engagement have been key factors in the team’s success, with a focus on providing comprehensive care, including basic care and activities, to enhance the patient experience.
Feedback from staff and patients is actively sought and used to refine and improve the service, with a focus on ensuring the team’s responsiveness to the evolving needs of patients and the healthcare environment.
The universal support offer
The universal support offer supports all organisations across England with a review of their ETOC provision, including good practice case studies, resources and access to deep-dive webinars.
To stay up to date with the latest events, you can:
- join our FutureNHS community
- access our programme forum to ask questions and network with other organisations:
- subscribe to receive notifications about upcoming webinars, new case studies and other opportunities:
- join the conversation on X by following the @Team_CNO account and using the hashtag #ETOCP
Email England.NursingWorkforce@nhs.net to create a good practice case study about your approach to ETOC provision.
Effective education and training case study
Somerset NHS Foundation Trust
In 2022, the trust reviewed their ETOC approach and found that there were unnecessary costs in their provision, where staff were often being used in areas which didn’t require Enhanced Care.
The trust adopted a Quality Improvement (QI) approach and piloted three components:
- a poster for escalation process
- a decision-making tool
- a 5-day ETOC training programme for healthcare support workers) across 6 wards.
The training component provides support workers with the necessary skills and knowledge to support enhanced care. The programme consists of a mixture of online learning, specialist training, immersive experience and reflection time. The training is patient focused, providing training on patient rights and freedom of movement while maintaining a safe environment.
Following the immersion day, 60% of staff join the Mental Health Bank. 12-15 staff are trained at a time, reducing the requirement of external help. Bank staff are only used to cover non-enhanced care shifts if needed by the wards.
Feedback from staff so far has been fantastic around improvements to their wellbeing following this approach.
Pilot 1 data has showed a clear reduction in spend with explanations of high spend where this has occurred (patients requiring more observations etc). Average spend on one of the pilot wards dropped from around £5,000 to £960 per week. Similar percentage decreases were seen on all the pilot wards.