Introduction
1. The NHS Long-Term Plan made a commitment to improve the quality of care within mental health inpatient settings for people with a learning disability and autistic people. To support this, we need to have robust and effective systems in place to identify and address concerns relating to quality of care and safety at the earliest opportunity.
2. Where mental health inpatient services are commissioned by integrated care boards (ICBs) and spot purchased, this can lead to care for people in a single location being commissioned by, and originating from, multiple and dispersed ICBs.
3. It can also lead to ICBs having people from their local system receiving assessment, treatment and support across multiple areas and regions.
4. Responsibility for the oversight of each person’s care is held by placing commissioners. However, historically there has been little opportunity to share intelligence between placing commissioners about care quality or concerns, or to triangulate any issues identified.
5. For this reason, Minister of State for Care Caroline Dinenage, announced in May 2019 that there would be new responsibilities for the host clinical commissioning group (CCG) (now replaced by integrated care boards) to oversee and monitor the quality of care:
“Where it is essential that someone is supported at distance from home, we will make sure that those arrangements are adequately supervised. We cannot have people out of sight and out of mind. That is why we are introducing stronger oversight arrangements.
“Where someone with a learning disability or an autistic person is an inpatient out of area, they will [be] visited every six weeks if they are a child and every eight weeks if they are an adult, on site.
“The host CCG will also be given new responsibilities to oversee and monitor the quality of care.”
6. Following this announcement, NHS England issued guidance in January 2021 to help CCGs and NHS regional teams to deliver this increased oversight. The Learning disability and autism – host commissioner guidance supported this oversight by enabling host commissioner arrangements to be put into place.
7. This guidance has been updated to reflect the host commissioner arrangements as ‘business as usual’, and in light of the transition from CCGs to ICBs.
Defining the role of the host integrated care board
8. The key roles of the host ICB, in respect of mental health inpatient care commissioned for people with a learning disability and autistic people are to:
- be the point of contact for placing commissioners and for the Care Quality Commission (CQC) for issues relating to quality and safety, in respect of commissioner oversight, for units where mental health care is delivered to people with a learning disability and autistic people, including acute mental health settings.
- ensure that placing commissioners are aware of the key contact in the host ICB should they become aware of issues of concern.
- establish a mechanism for sharing intelligence between commissioners who are placing people (or considering placing people) with a learning disability, or autistic people within each unit.
- gain understanding of and monitor overall patient experience within the particular unit(s) including having mechanisms to gain feedback from patients and families and this may include links with the relevant advocacy provider(s).
- ensure that there is an interface with the relevant local authority adult social care safeguarding service, and with the local safeguarding adult board (SAB) so that any safeguarding concerns are raised with the host local authority and dealt with as directed under the Care Act (2014).
- work with colleagues in contracting and quality teams, both within the ICB and the provider, and be the key point of contact from these teams with the provider for issues relating to quality and safety, including those that impact multiple commissioners.
- work alongside other host commissioners for that same unit, for example the NHS led specialised mental health, learning disability and autism provider collaborative.
- work with colleagues in contracting and quality teams, both within the ICB and the provider, to develop actions that will deliver required quality improvements, and seek assurance that necessary improvements have been made.
- work in conjunction with place, system, regional and national quality governance arrangements – including the relevant system quality group (SQG), taking a lead role in coordinating the response required if there are serious and/or multiple quality concerns
- ensure the SQG has strong and formal links with the local SAB, so that concerns discussed at SQG can also be discussed with SAB chairs.
- work with the relevant NHS local, regional and national communications teams, alongside placing commissioners, to develop clear and consistent communication materials in light of significant quality concerns or unit closures, for example, ensuring any materials produced are patient-focused and available in easy read.
- Work with NHS England regional leads where concerns about units are identified as needing an escalation to the regional or national NHS England team.
9. To deliver these roles, each ICB should ensure there is dedicated capacity for the host commissioner role relevant to population size and risk.
10. The host ICB does not:
- replace the role of a person’s Placing Commissioner. The placing commissioner is responsible for:
- commissioning and overseeing the person’s placement and pathway of care back into the community.
- undertaking regular commissioning reviews of the person, including commissioning oversight visits, as described in section 94.
- take responsibility for the quality of care received at an individual level.
- have responsibility for persons’ care plans or discharge.
Identifying units which require a host integrated care board
11. Any mental health inpatient unit which provides care commissioned by ICBs to people with a learning disability, or autistic people, will need an identified host ICB. This includes units which provide assessment and treatment, long-term rehabilitation, and other specialist inpatient care). This includes both NHS and independent sector provision.
12. ICB’s should be aware that host commissioner and placing commissioner arrangements are also in place for specialised mental health, learning disability and autism services, eg secure inpatient provision, and should work together with these colleagues to ensure a comprehensive approach to quality oversight for the population.
13. Mental health inpatient settings commissioned by ICBs may have wards or beds either designated for or occupied by autistic people or people who have a learning disability. The host commissioner arrangements also apply in these settings and must be implemented. Collaborative work between mental health, learning disability and autism commissioners to identity roles and responsibilities is advised in these situations to ensure adherence to this Host commissioner guidance. This will support safe care and the best outcomes for people in these settings.
Determining the host integrated care board
14. It is important that the host commissioner model is considered alongside NHS contracting arrangements so that there is an appropriate framework for the host ICB to work with the provider and on behalf of individual ICBs.
15. We recognise there will be different scenarios in which these arrangements are implemented, which may mean the host commissioner arrangement differs from the default position. For example, an ICB may hold a contract for the unit in its area and could be the only ICB to place people in that unit. Alternatively, a unit may have no block contract in place, and people could be placed by multiple and dispersed commissioners on spot contracts.
16. The default position is that the ICB in whose geographic patch the unit is located in, is the host commissioner and fulfils the role as described within this guidance.
17. On occasion, the host commissioner may choose to delegate operational oversight to another ICB or provider collaborative (through mutual agreement). It should be noted that whilst operational oversight can be delegated, the accountability for quality oversight for any units in its geographic footprint still remains with the host ICB.
18. An example of when it may be deemed more appropriate for operational oversight to be delegated is if the unit has a block NHS contract in place that is held by an ICB, ie as identified lead commissioner for contracting purposes, then it may be deemed more appropriate for that ICB to be the Host Commissioner – even if the ICB and provider are not located in the same geographic area. This would ensure a consistent approach to quality oversight and grant the ICB the authority to work with the provider on any required actions.
19. Where there are regularly a number of patients within a unit whose care is commissioned by a number of different ICBs, it is recommended that a co-ordinating commissioner contracting arrangement be put in place (if this has not been done already). This will provide a framework for the host commissioner to act on behalf of the other ICBs,who would be associates to the lead provider contract, if any actions are required with the provider following any quality concerns raised(Section 13 of NHS Standard contract 2022/23 technical guidance provides further information relating to collaborative commissioning arrangements).
20. Should disputes arise, or if identification of the host ICB is unclear, arrangements will need to be determined on a case-by-case basis, with the NHS England regional lead for learning disability and autism taking overall responsibility for ensuring the most appropriate host ICB is identified, in collaboration with the regional chief nursing officer (see Appendix 1 for details of regional leads).
21. In mediating any dispute between ICBs, the NHS England regional lead will take into account the local arrangements in place for quality oversight, and which commissioning organisation is best placed to carry out the roles and responsibilities described within this guidance.
22. On the rare occasion when disputes between ICBs cannot be resolved at a regional level, these should be escalated to NHS England’s national learning disability and autism programme team.
23. Where there is a cross regional dispute, this will be mediated by the two relevant regional SROs for learning disability and autism.
24. Irrespective of which ICB is identified as host, the relevant local safeguarding adults board (SAB) (and therefore, the relevant local authority and other partners such as Health Watch and emergency services representatives) will be those where the unit is geographically located.
25. The host ICB must inform the NHS England regional lead for learning disability and autism of the details of the person who will act as the host commissioner for each of the units for which they have host commissioner responsibility.
26. The final list of identified host ICBs will be agreed with the NHS England regional lead for learning disability and autism (Appendix 1) and shared with the NHS England’s national learning disability and autism team.
27. The regional lead for learning disability and autism will ensure there is a named host ICB and commissioner (including email address and telephone number) for all units within their region.
28. The regional lead for learning disability and autism must establish a mechanism for keeping an up-to-date register of this information, refreshing this on at least a quarterly basis
29. The National Learning Disability and Autism team will continue to hold a central list of host ICBs and the inpatient units for which they have host commissioner responsibility and seek to update this on a quarterly basis, through intelligence from regional leads. This list will be made available to the other regional leads for learning disability and autism, as well as to ICBs across the country.
Establishing key commissioning and provider relationships
30. The host ICB will need to make sure that there is internal corporate knowledge of which units it is the host ICB for. It is recommended that this is identified at a minimum of annually to its Board in writing. This should align with the final list identified in point 26.
31. Host ICBs must ensure they are aware of any units within their boundary and should put arrangements in place with their local Care Quality Commission (CQC) service relationship owner to ensure they are notified of any mental health inpatient facilities newly registered within their boundaries. This will include all types of mental health inpatient units whether providing specific assessment and treatment for autistic people and people with a learning disability, or acute mental health hospitals.
32. There may be a unit within an ICB’s area that is dual registered to provide both mental health and learning disability services, but which currently does not support any people with a learning disability or autistic people. A host ICB and a host commissioner should still be identified for such units, and relationships should still be made within local partners, including the provider. However, there will be no requirement for the host commissioner to undertake routine quality surveillance until someone with a learning disability or autism is admitted to that unit (it is the responsibility of the placing commissioner to notify the relevant host commissioner of any new placements within a unit.
33. The host ICB must identify a named person within the ICB who can act as the host commissioner, and undertake the responsibilities described within this document.
34. This person should be of sufficient seniority, and with the appropriate skill set to carry out all required duties within this guidance, including liaison with senior management within provider units, other ICBs and local authorities, and with regional and national teams as appropriate. They must conduct visits to provider units and respond to any escalation of serious quality and safety concerns.
35. It will be for each ICB to determine who this person should be, but it is suggested that this could be a director with responsibility for quality and/or nursing, or a medical director.
36. While there will need to be a single, named person identified as the host commissioner, it is important to note that this commissioner works as part of a system (which incorporates health, education social care and housing) and not in isolation. To provide resilience and timely action it may, on occasion, be appropriate to make arrangements including delegation of duties described within this guidance.
37. The host commissioner must work with the provider(s) to obtain a full list of people with a learning disability and autistic people placed in any units for which it has host commissioner responsibility, and which ICBs and placing commissioners are responsible for those people. Please note that this must not include patient identifiable information, rather, a pseudonymised identifier for the person should be used.
38. For any people from outside of England, if the provider is unable to provide contact details for the relevant commissioner, the host ICB should contact their regional lead for learning disability and autism for assistance.
39. Each regional team will provide host commissioners with a list of lead learning disability and autism commissioners for each ICB (the list of placing commissioners) and should make sure that this is updated on a quarterly basis.
40. Placing commissioners have a responsibility to notify the host commissioner if the person is discharged, and if they no longer have any people placed at that unit.
41. The host commissioner must contact each of the placing commissioners so that they are aware of the host ICB, and provide their contact details and the duty on call number for the host ICB and host commissioner in case of emergency (ie if there is an immediate risk to individual safety which would require other placing commissioners to be notified.
Establishing local and relevant stakeholders
42. The host commissioner should make sure that they know the local stakeholders who will play a role in ensuring the quality and safety of care for people with a learning disability and autistic people. These will include:
- local Care Quality Commission service relationship owners.
- local authority heads of service for learning disability and autism (sometimes joint NHS/ social care posts).
- local adult safeguarding leads – this will be the local authority where the unit is based.
- local advocacy provider(s) for the hospital, eg local authority and/or hospital commissioned providers.
- ICB designated professionals for adult safeguarding.
- local Healthwatch representatives.
- representative from local emergency services, including ambulance trusts.
- local NHS providers – including physical health services.
- local education providers and SEND teams for children and young people.
43. In addition to the above, the host commissioners should ensure that, where applicable, they identify relevant contacts responsible for commissioning highly specialised and secure services that are outside of the scope of this document but where the services may be co-located with non-secure services, as well as relevant contacts outside of England.
Identifying relevant contacts for specialised services, including secure provision
44. In April 2020, NHS led provider collaboratives were established to take on the commissioning and provision of the majority of specialist inpatient mental health, learning disability and autism provision within a geographical footprint. The NHS led provider collaboratives are a collective of both NHS and independent sector providers and are overseen by an NHS lead provider. Currently the services that sit within the remit of the NHS led provider collaboratives include adult low secure, medium secure, children and young people’s inpatient services and adult eating disorder inpatient services.
45. Lead providers deliver some of the commissioning and quality oversight and assurance tasks on behalf of NHS England regional teams, who still maintain overall accountability. The lead provider will play a similar role to the ICB host commissioner, triangulating intelligence received and ensuring that this is acted upon.
46. It is particularly important that when there are multiple commissioners for a single unit, commissioners work together to agree a local Responsible Accountable Supporting Consulted Inform (RASCI) framework. This may include regional specialised teams, host lead providers and host ICBs. The local RASCI should outline roles and responsibilities and enable the sharing of intelligence locally.
47. In addition, NHS regional leads should share intelligence between themselves, for example where a unit is in enhanced quality surveillance, or when the Unit is provided by a multisite independent sector provider. Regional leads for learning disability and autism are responsible for ensuring that there is a mechanism for receiving and sharing intelligence across regions.
48. Further detail is provided in points 60 to 70 on sharing intelligence and acting in a way that is proportionate and appropriate to the intelligence received.
Identifying relevant contacts outside of England
49. There are some people from outside England placed within English units The priority will be for placing commissioners to maintain oversight of the people for whom they have commissioning responsibility and ensuring continued quality of care.
50. There are some units in Wales where there is a small but consistent flow of people from England, particularly from ICBs within the North-West, West Midlands and South-West regions. Host ICBs in England should be identified for these units. These host ICBs will take a lead role in liaising with the units and relevant Welsh commissioners to provide a single point of contact. They will ensure that people in these units (who are the commissioning responsibility of ICB’s in England) receive the same oversight and co-ordination as they would if they were in a unit in England.
Acting as the central point for concerns relating to quality of care
51. One of the key responsibilities of the host commissioner is to act as a central point to receive any issues relating to quality and safety that are escalated from individual commissioners, people, family members, carers or their advocates. They are not responsible for resolving individual patients’ quality issues and concerns as this is the role of the placing commissioner, but they have a role in resolving issues where themes arise. An example could be where there is an impact on numerous people or the culture and safety within a unit.
52. In most circumstances, it will be sufficient to share pseudonymised information relating to people. This should be the default unless there is a legitimate reason why more information should be shared.
53. It is vital that any professional sharing information relating to a person (as opposed to the overall environment, for example) does so in line with Caldicott Principles and General Data Processing Regulations (GDPR), gaining the person’s consent wherever possible, through use of a best interests decision for a person without capacity, or where there is a legitimate reason to share without consent. Commissioners should not share personal identifiable information unless, due to safety concerns, there is legitimate reason to do so a clear need to do so that is in the person’s best interest due to safety concerns overriding the need for consent. If so, this should be logged within the Caldicott Guardian log of the ICB responsible for the person (that is, the placing ICB).
54. The host ICB will need to establish and use a system to log individual issues raised in line with its usual practice and governance. Although it will contain pseudonymised data, the host ICB will need to make every effort to ensure the security and integrity of this information. The host ICB should seek advice from their information governance lead or data protection officer if there is any doubt as to what can and cannot be shared.
55. It is important to note that placing commissioners will continue to retain responsibility for people in an inpatient setting. They are also responsible for:
- oversight of that inpatient placement.
- or ensuring that the care being provided is reviewed.
- and for ensuring that intelligence is shared.
The role of the host commissioner is not to replace this but to act as a single point of escalation for a particular unit and to ensure that intelligence is shared across the relevant system.
56. The placing commissioner should use their professional judgement in determining what to escalate to the host commissioner, and use a range of sources of intelligence, such as:
- Care (Education) and Treatment Reviews (C(E)TRs).
- Care Programme Approach meetings, where applicable.
- multidisciplinary team meetings and care co-ordination as described in the Community Mental Health Framework, which supersedes Care Programme Approach in some treatment pathways
- commissioner oversight visits.
- complaints or feedback from the person and/or their family.
- advocacy feedback.
- serious incidents, including deaths of people.
- Healthwatch reports.
- information received through Ask Listen Do.
57. Intelligence shared should include (but not limited to):
- concerns of immediate risk of harm to people or staff which must also be escalated to local authority safeguarding services.
- use of restrictive practices outside national policy.
- death of a patient.
- concerns about lack of, or inappropriate, application of Liberty Protection Safeguards.
- concerns relating to staffing ratios.
- concerns relating to treatment of people by individual or multiple staff and a lack of person-centred care.
- concerns raised by families.
- repeated failure to deliver agreed actions as part of C(E)TRs or Care Programme Approach meetings.
- poor use of documentation for example care planning, failure to personalise care, or to involve the person or their family in the care planning process.
- concerns about the inpatient environment, for example health and safety.
- medication concerns.
- lack of involvement of families or of incidences where families are regularly being excluded from units.
- concerns about whether a person’s human rights are being upheld (see What is the Human Rights Act on the British Institute of Human Rights website for health and social care professionals).
- concerns about the level of meaningful activity for people.
- concerns about a person’s hydration and nutrition.
- concerns about the management of physical health conditions.
- Lack of/poor formulation of assessed needs and outcomes-focussed treatment plan.
58. This list is by no means exhaustive, and the placing commissioner will need to use their professional judgement to determine what is appropriate to share with the host commissioner.
59. Beyond this, the placing commissioner also has their own responsibility, and duty of care, to take appropriate and proportionate action. This will depend on, and be relative to, the concerns they identify, for example raising issues with the provider or making a safeguarding referral. This will support continued oversight of the person’s care and treatment and help make sure that any concerns relating to quality or individual safety can be identified and escalated at the earliest opportunity.
Taking an appropriate response to quality/safety issues raised
Routine quality surveillance
60. The host commissioner should ensure that arrangements are in place for routine quality surveillance. This is an opportunity to speak to commissioners with people placed within the unit, as well as other local partners including families, community health providers and advocacy services. This will ensure all quality and safety concerns have been escalated as appropriate, and safeguarding concerns appropriately referred.
61. The routine quality surveillance implemented by the host commissioner should be locally appropriate. This should take account of factors such as the number of placing commissioners and current arrangements already in place to oversee quality of care. Arrangements put in place should ensure there is the mechanism for intelligence to be shared on a regular basis and include the following organisations:
- placing commissioners.
- local authority head of service and/or adult safeguarding lead – this is the local authority where the unit is located.
- host ICB adult safeguarding leads.
- local CQC service relationship owner.
- local emergency services representatives.
- representative from the provider including ambulance trusts.
- experts by experience.
- Healthwatch.
- commissioned advocacy service(s).
62. This list is not exhaustive, and the host commissioner may wish to invite other relevant people.
62. The host commissioner should develop a good understanding of the care being delivered at the unit and the organisation’s culture. This will require visiting the unit as well as using information gained from other methods such as speaking with the hospital advocacy provider(s) or additional methods to understand patient experience of care.
63. The host commissioner should note that the Winterbourne View Concordat (Department of Health, 2012) highlighted the importance of robust safeguarding arrangements, and the role of local safeguarding adults board’s (SAB) in ensuring the safety of vulnerable people. There is significant interface between the role of the host commissioner and the role of the local SAB in respect of safeguarding vulnerable adults. It is important that respective responsibilities are well understood to avoid duplication, and/or important intelligence being missed through miscommunication.
65. All professionals have a duty of care to people service users. Should they have a safeguarding concern, they should raise this via the relevant local authority, in line with the Care Act 2014, and with the host commissioner. Systems should ensure that the chair of the local SAB includes the host commissioner as a partner when the board investigates any concerns that have been raised.
66. The following is taken from the Care Act 2014, S43 and S42(1) and clarifies the role of the local SAB:
“When adults who have care and support needs are experiencing or are at risk of abuse and neglect, and because of their needs are unable to protect themselves, local SABs are responsible for co-ordinating and seeking assurance on and supporting the effectiveness of what partner agencies do.”
67. Host commissioners must ensure they are familiar with local adult safeguarding referral processes, and that there are defined routes for regular liaison with ICB and local authority safeguarding leads regarding care provided at the specialist inpatient unit.
Enhanced quality surveillance
68. There may be quality concerns of such a scale or nature that it is deemed necessary to take further action and escalate concerns. These issues should be escalated to the local system quality group (SQG).
69. The National Guidance on System Quality Groups from the National Quality Board sets out how the SQG will assess the risks and how they will either seek further information or put in place enhanced quality surveillance as appropriate. It is likely that the host commissioner will be required to play a lead/ co-ordinating role in undertaking any actions agreed by the SQG.
70. Depending on the nature of the concerns raised, local adult safeguarding processes may run alongside actions initiated by the host commissioner and partners to review and address any quality concerns highlighted.
71. As per the national SQG guidance, the SQG will determine at what point a unit can revert to routine quality surveillance.
72. See figure 1 below for levels of quality risk guidance:
Figure 1: National Quality Board (NQB) Quality Risk Guidance
The NQB’s Guidance on Risk response and escalation is based on the premise that all risks should be managed as close to the point of care as possible.
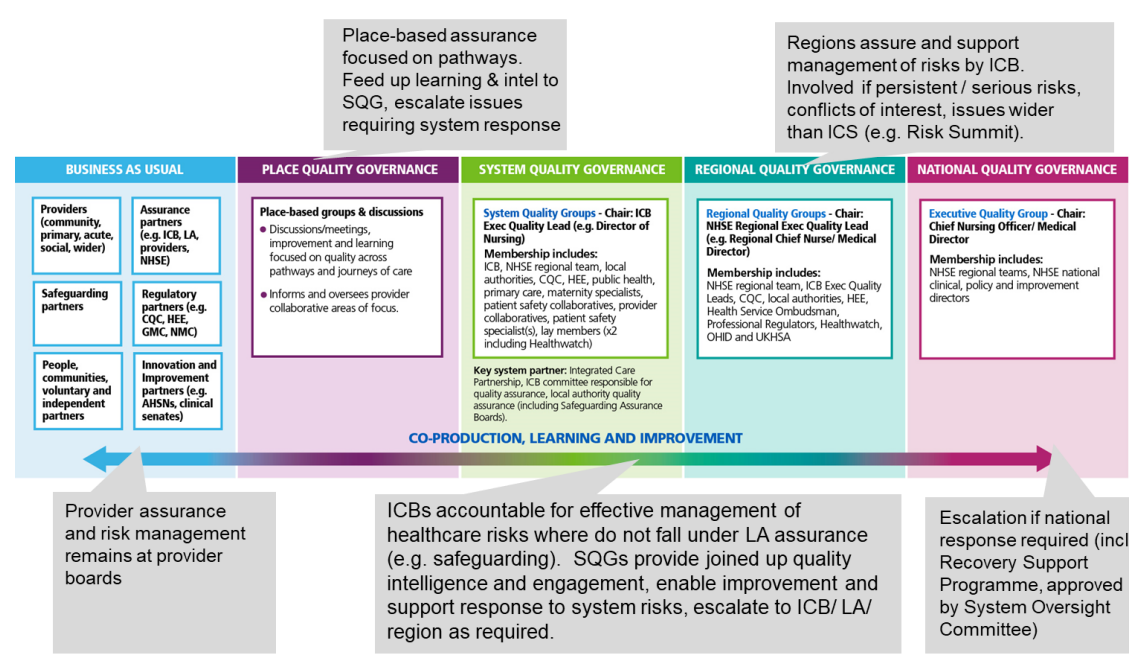
Image text: This diagram shows an overview of quality governance. It is taken from the National Guidance on Quality Risk Response and Escalation in Integrated Care Systems, which was published by the National Quality Board in June 2022. It shows how issues are escalated across different levels. This includes beginning from business as usual, to place level, system level, regional level and then to national level quality governance. It provides detail on who should be involved in the System Quality Group at each level of assurance. It outlines high level tasks at each level of governance. The diagram also shows that across all levels of governance there should be co-production, learning and improvement.
Wards or units rated as inadequate by the Care Quality Commission (CQC)
73. Host commissioners may be aware of quality concerns in a ward or unit that is providing care for autistic people or people with a learning disability that may lead to a rating of inadequate following inspection by the CQC. Usual quality assurance and oversight processes should be followed in relation to quality concerns and issues when such a rating is given.
74. In the Building the Right Support Action Plan NHS England makes a commitment that the NHS will strive to ensure that no autistic person or person who has a learning disability will be placed in a unit rated as inadequate by the CQC other than in exceptional circumstances. It is the placing commissioner’s responsibility to uphold this commitment or, following appropriate safeguards and steps, to seek agreement from their relevant ICB for any exceptions. As part of an exceptions process, we would expect host commissioners to be consulted and contribute to relevant information or intelligence to support the exception’s decision-making process.
Hearing the voice of people, family carers and advocates
75. The views of the person and their family/carers must always be sought and responded to when considering the quality of care provided. The host commissioner should have mechanisms in place to ensure that this takes place including good links with the advocacy service in the hospital.
76. Families and carers who have concerns regarding the quality of care provided in an inpatient setting should raise their concern via existing mechanisms including through the placing commissioner, with the provider, via a safeguarding team or with CQC Equally. Placing commissioners have a responsibility to ensure that they communicate openly with families and carers of those placed in inpatient care.
77. Placing commissioners must make family members, carers and the commissioned advocacy service(s) aware of the role of the host commissioner and how they can be contacted to raise any concerns.
78. NHS England regional leads for learning disability and autism should ensure that the role and contact details of the host commissioner is promoted and made available to families and carers, for the purposes of raising concerns regarding the quality of care.
79. The host commissioner should note that a number of Safeguarding Adult Reviews and NHS England’s Safe and Wellbeing Reviews have continued to highlight how important the voice of people, families, and advocates are in identifying concerns, often at an early stage
80. Should any person in hospital, family member or carer contact a host commissioner regarding a person in a unit, it is important that:
- the host commissioner takes the time to listen to and acknowledge concerns raised, and follows local safeguarding processes as applicable.
- patient identifiable information is only shared in line with General Data Protection Regulation (GDPR) and with the consent of the person where this is possible.
- concerns are recorded, as per section 53 above, and in line with GDPR.
- family members, carers and advocacy providers are encouraged to discuss concerns with the placing commissioner if they have not already done so.
- regardless of whether the family member or carer wishes to raise concerns directly with the placing commissioner, they should be made aware that any concerns will be discussed by the host commissioner with the placing commissioner, and whether this will be anonymised.
- feedback should be provided to families following any concerns raised in a timely way.
Communication and engagement while overseeing quality concerns
81. The host commissioner will play a vital role in ensuring local stakeholders are involved in and kept up to date with any surveillance or actions being undertaken with a provider.
82. ICBs are responsible for ensuring a mechanism is in place to allow host commissioners within their area to communicate regularly to any relevant stakeholders whilst overseeing any quality concerns.
83. Regional leads for learning disability and autism must ensure that they communicate at a regional and national level regarding any units that are placed in enhanced quality surveillance, or where there is evidence of, and a response underway to, serious risk of harm to a person(s) or staff.
84. While overseeing quality concerns, it is important that the host commissioner does so in collaboration with the ICB’s quality and contracting teams to make the most of any existing arrangements in place for quality oversight and management of any quality concerns.
85. In certain circumstances, it is particularly important that intelligence is shared between regional leads. These include where a unit is in enhanced quality surveillance, or where there is evidence of, and a response underway to, serious risks of harm, and the unit is provided by a multi-site independent sector provider.
86. Regional leads for learning disability and autism and the host commissioner should share intelligence with the relevant NHS lead providers of mental health, learning disability and autism provider collaboratives, where there are concerns regarding sites that are co-located with secure provision, or where there are concerns relating to multi-site independent sector providers.
87. Communication should be proportionate and appropriate to the level of quality surveillance in place. Those sharing intelligence with other regional leads and NHS lead providers should also consider GDPR – particularly when sharing information regarding people, or where it is possible to identify a person due to their high profile.
Host Commissioner Forum
88. The National Host Commissioner Forum has been established to support the successful and timely delivery of the host commissioner arrangements. It meets regularly and focuses on supportive discussions and engagement amongst commissioners especially when there are issues associated with people and units of concern.
89. The Forum provides a platform on which to share intelligence relating to both the NHS and independent sector providers. The Forum is also a place to share good practice and inform ongoing implementation and actively consider how commissioners can best discharge their responsibilities particularly when challenges are raised. We recommend that all host commissioners attend this forum on a regular basis.
90. The Forum is an active part of the quality surveillance process and host commissioners should consider this a key vehicle to share intelligence. The Forum does not replace communication with placing commissioners or host commissioners, as described within this document.
Having an ongoing awareness of the autistic people and people with a learning disability in each mental health inpatient setting
91. It is the responsibility of all commissioners to ensure they know who the host ICB and commissioner are for any inpatient unit where they are planning to admit a person. Before a placing commissioner places a person into a unit out of area, they must contact the host commissioner to understand any current concerns or issues associated with that provider. The only exceptions to this may be in exceptional emergency circumstances, or where a person is admitted, outside office hours.
92. If a person with a learning disability or an autistic person is admitted to a mental health hospital, placing commissioners will be required to notify the host commissioner by email within 48 hours of any admission. This should contain the pseudonymised patient identifier and contact details of the responsible/placing commissioner. This must not contain any patient identifiable information. The host commissioner will then be able to ensure that they include that commissioner in any communication regarding individual quality or safety at that unit.
Support for the host commissioner role
93. Each ICB should ensure there is dedicated capacity for the host commissioner role relevant to population size, number of units and size of these, and quality assurance underway.
94. For the role to be fulfilled effectively, there needs to be dedicated resource with appropriate support. Support needs may vary and will increase significantly if a unit of concern is closed or requires extensive monitoring and support. ICBs may wish to consider what these arrangements may look like and how they will be fulfilled in timely way particularly if extra resource is required.
95. Host commissioners should also, particularly in cases of serious incidents or unit closures, work closely with NHS England regional and national colleagues. Areas should not, in these situations, work independently, as cross system collaboration is essential to ensure intelligence is shared and to inform future learning.
Interdependencies and helpful documents
96. The role of the host commissioner is one that will exist amongst several other national, regional and local initiatives designed to ensure oversight of quality and safety for people in inpatient care with a learning disability and autistic people.
97. It is therefore important that the host commissioner familiarises themselves with existing structures and processes in place locally, in particular any existing forums established to share intelligence or to bring local partners together for the purposes of quality assurance. Care should be taken to ensure that the role of the host commissioner and their responsibilities can be aligned with existing local processes – where these are working well – wherever possible.
98. In addition, there are nationally mandated processes in place that will interface with the role of the host commissioner including, but not limited to, CETRs, CPAs and commissioner oversight visits.
Review of the host commissioner model
99. We will continue to engage with host commissioners and ICBs on the implementation of this guidance and will review it as appropriate. Feedback on the guidance in practice should be shared via the national host commissioner forum, or via the relevant regional lead for learning disability and autism.
Appendix 1: Regional leads for learning disability and autism
North East and Yorkshire
- Eamonn Harrigan: Eamonn.Harrigan@nhs.net
- Julie Bates: juliebates2@nhs.net
North West
- Claire Swithenbank: Claire.Swithenbank@nhs.net
East of England
- Sue Fox: Susan.Fox11@nhs.net
Midlands
- Robert Ferris-Rogers: R.Ferris-Rogers@nhs.net
South East
- Adanna Williams: Adannawilliams@nhs.net
South West
- Graham Carr: Graham.Carr@nhs.net
London
- Heidi Peakman: H.Peakman@nhs.net
Definitions
- Care (Education) and Treatment Reviews: A Care and Treatment Review (CTR) for adults and a Care (Education) and Treatment Review (C(E)TR) for children and young people is a review for a child, young person or adult with a learning disability or autistic child, young person or adult who is in a mental health inpatient setting or is at risk of being admitted to hospital.
- Commissioner oversight visit: A visit undertaken by the commissioner (placing commissioner). Visits take place for autistic people and people with a learning disability at least every eight weeks for adults, and at least every six weeks for children and young people.
- ICB contracting and quality teams: Teams working within the integrated care board (ICB) that have responsibility for managing the contract with providers, including delivery of any quality standards, and working with the provider to address any identified issues.
- Host commissioner: The host ICB must identify a named person within the ICB who can act as the host commissioner, and undertake the responsibilities described within this document. The default position will be that the host commissioner will be the ICB in whose geographic patch the mental health inpatient unit is located.
- Integrated care board (ICB): A statutory NHS organisation responsible for developing a plan for meeting the health needs of the population, managing the NHS budget and arranging for the provision of health services in the integrated care system.
- Integrated care system (ICS): Integrated care systems (ICSs) are partnerships of organisations that come together to plan and deliver joined up health and care services, and to improve the lives of people who live and work in their area.
- Placing commissioner: The placing commissioner is a commissioner from the patient’s originating integrated care system (ICS) – where the patient is ordinarily resident. The placing commissioner is the person who has agreed the contract with the unit to support the individual patient. Sometimes this is referred to as the responsible commissioner, as outlined in ‘Who Pays’ (NHS England, 2022). The placing commissioner’s responsibilities include, but are not limited to:
- commissioning and overseeing the person’s placement and pathway of care back into the community
- undertaking regular commissioning reviews of the person’s care, including commissioning oversight visits
- taking responsibility for the quality of care received on an individual basis.
- having responsibility for people’s care plans or discharge planning
- Care (Education) and Treatment Reviews (C(E)TRs)
- identifying concerns from C(E)TRs, Care Programme Approach meetings and commissioner oversight visits which relate to the care delivered by a provider
- notifying the host commissioner and any other agency as required (eg safeguarding) of any intelligence which they believe should be shared in relation to care delivered by the provider
- notifying the host commissioner if the person is discharged, and if they no longer have any people placed at that unit.
- Regional lead (NHS England): Refers to the NHS England regional lead for learning disability and autism, in a particular NHS region. The list of these contacts is provided within Appendix 1.
- Spot purchasing: Means when a service is purchased for an individual person, rather than being provided through existing contractual arrangements. In this policy it means purchasing an individual hospital service in another locality, rather than using a local mental health inpatient hospital where an existing contract is in place which covers all, or most, of the beds there. This is usually because the required service is not available locally.
- System quality group: A strategic forum within an integrated care system (ICS), with partners from across health, social care, which:
- routinely and systematically shares and triangulates intelligence, insight and learning on quality matters across the ICS
- identifies ICS quality concerns/risks and opportunities for improvement and learning, including addressing inequalities. This includes escalating to the ICB, local authority assurance (eg safeguarding assurance boards) and regional NHS England teams as appropriate
- develops ICS responses and actions to enable improvement, mitigate risks (respecting statutory responsibilities) and demonstrate evidence that these plans have had the desired effect. This includes commissioning other agencies and using ICS resources to deliver improvement programmes/solutions to the intelligence identified above (eg academic health science networks (AHSNs)/provider collaboratives/clinical networks)
- tests new ideas, sharing learning and celebrating best practice.
- Unit: For the purposes of this document a Unit is any mental health inpatient service, or part of a service, which is commissioned by an ICB, and which provides mental health assessment, treatment and support to people with a learning disability and autistic people.This includes, but is not limited to:
- acute learning disability and autism units
- assessment and treatment units
- long-term rehabilitation units
- other specialist inpatient units (including those delivering care to people with/or mental illness)
- both NHS and independent sector provision
- mental health inpatient settings which have wards or beds designated for autistic people or people who have a learning disability
- mental health inpatient settings which have wards or beds occupied by autistic people or people who have a learning disability.
Publications approval reference: PRN0931

