Guidance for emergency departments: initial assessment
Introduction
The 2022 to 2023 NHS planning guidance specifies the need for more structured streaming arrangements between urgent treatment centres (UTCs) and emergency departments (EDs), and as such they must have robust processes that match patients with the service most suited to meet their clinical need; for example, a UTC (which may or may not be co-located with an ED) or same day emergency care (SDEC) service.
The rationale for changing the way in which we look at and understand the performance of UEC was set out in the interim report of the clinically led review of access standards (March 2019) and subsequently in transformation of urgent care: models of care and measurement (December 2020) makes it clear that UEC needs to identify the sickest patients early and their treatment begun as soon as possible after arrival. Urgent and emergency care (UEC) attendances continue to increase across England. Effective patient flow that supports early senior clinical decision-making is therefore imperative.
This guidance makes recommendations for models of initial assessment of patients arriving at EDs and provides standard definitions of the processes that classify as initial assessment: streaming, triage, and rapid assessment and treatment. It recognises that initial assessment and flow from the front door of a hospital are a crucial first step on a patient’s journey. Decisions made at the first point of interaction can frame much of the subsequent process of care and are an essential component in managing risk and ensuring a high quality service.
It builds on and replaces clinical streaming in the accident and emergency department (2017) and initial assessment of emergency department patients (RCEM 2017), which recommended beginning initial assessment of patients presenting to ED within 15 minutes . This document has been developed with the Royal College of Emergency Medicine (RCEM) after consultation with key stakeholders (NHS England, RCEM, Royal College of Nursing (RCN), Care Quality Commission, regional UEC clinical advisors, Society of Acute Medicine, emergency department clinicians across England), and agreed for England. RCEM will consult the other UK nations to achieve consistency wherever possible.
‘ED’ in this document refers to the location where the initial patient assessment takes place. Assessment can be performed by a type 1 (ED) or type 3 (UTC) service. Hospitals may have a UTC at the front door which performs the streaming function.
The following are not within the scope of this document:
- initial assessment of patients presenting during a major incident
- initial assessment processes used by NHS111.
In partnership with The Royal College of Emergency Medicine. Document first published: 12 August 2022.
Contents
- patient flow into emergency departments
- initial assessment
- clarification of definitions of activity that constitutes initial assessment
- counting and coding
- training and assessment
Patient flow into emergency departments
The core principle is that on arrival at hospital, patients are directed to a treatment area or service staffed with appropriate healthcare practitioners to manage their clinical needs.
Patient arrival
Most patients who arrive at emergency departments (EDs) self-present (they are unheralded). Since the COVID-19 pandemic, hospitals have changed the way that patients access services due to increased infection prevention and control (IPC) measures, including rapid testing of patients for COVID-19. Consequently, a proportion of patients who attend ED may have had earlier contact with a clinician in another setting, such as NHS 111.
Heralded patients
These patients have contacted NHS 111 and been advised to go to hospital. NHS 111 books them into ED arrival slots. Providers should use the NHS national standard for booking and referral and should make the ED aware of the patient’s attendance in advance of their arrival.
Patients who are conveyed by ambulance are also heralded.
Ambulance handover
Ambulances will pre-alert the ED if they are conveying a patient who needs to be received by a clinical team. These patients must be received by the appropriate team immediately on arrival.
Handover of non-pre-alerted patients from an ambulance crew to the ED should be completed following locally agreed processes within 15 minutes of arrival, as per NHS ambulance services pre-alert criteria guidance. Responsibility for patient clinical assessment and treatment lies with the hospital from the point the ambulance arrives at the department. Ambulance clinicians need to return to their vehicle immediately after handover to prepare and makes themselves available for patients needing an ambulance response in the community.
Unheralded patients
These patients are not expected by the ED. They include patients who self-present with no previous contact with a clinician in another healthcare setting and those advised to attend ED by a clinician in 999, primary or community care.
Initial assessment
Patients should be assessed promptly by locally agreed processes within 15 minutes of arrival. However, patients who have a booked appointment via NHS 111 at a co-located UTC are not required to have a further assessment on arrival if they are seen within 30 minutes of their appointment time. An exception to this would be if the patient’s clinical condition has deteriorated before arrival and in this case further clinical assessment would be of value.
Clinical governance of any assessment must be unambiguous. The service assessing and directing the patient should ensure joint governance arrangements are in place for clinical responsibility, until the patient is next assessed by a clinician.
Patients should be assessed according to two main factors:
- chief complaint or suspected diagnosis: the chief complaint is the primary problem the patient is presenting with, as initially assessed by a clinician
- acuity: acuity is a measure of the severity of the patient’s condition and the urgency with which they need to be seen and assessed by a clinician qualified to do this through training and experience. Defined in the data dictionary.
In the Emergency Care Data Set (ECDS) acuity is assigned a score of 1 to 5. If an explicit (formal) triage system is not used, implicit triage that flows patients to resus (1), majors (3) or minors (4) is currently used.
Table 1: Acuity coding in ECDS
ECDS |
A&E coding |
| 1 Immediate emergency care | 1 Resuscitation |
| 2 Very urgent emergency care | 3 Majors |
| 3 Urgent emergency care | 4 Minors |
| 4 Standard emergency care | |
| 5 Low acuity emergency care |
Initial assessment must add value to the patient’s journey and not cause inappropriate clinical duplication. Although initial assessment models may differ across the country and be based on one or more of the processes defined below. They should encompass the recommendations in Table 3 below.
The main objectives of initial assessment are to:
- identify patients with potentially life-threatening conditions and injuries to ensure those with the most time-critical conditions are prioritised
- accurately assess non-life-threatening conditions and injuries so that appropriate prioritisation occurs for these patients and they are seen by the right service within appropriate timeframes
- prevent ED crowding and support infection prevention and control (IPC)
- recognise potentially vulnerable patients and consider their immediate safeguarding concerns.
Initial assessment recommendations
- Identify patients with life-threatening conditions/injuries and ensure they are prioritised.
- Identify patients with non-life-threatening conditions/injuries and ensure appropriate service allocation and prioritisation occurs.
- Identify immediate clinical care needs (e.g. medication administration/diagnostics) and deliver care or enable prompt transfer to an area that can deliver care.
- Identify potentially vulnerable patients including those with safeguarding concerns, learning disabilities, acute mental health illness and high risk of absconding.
- Initial assessment should begin at soon as possible after a patient arrives.
- Patients should be made aware of who is responsible for their care.
- Initial assessment processes should be resourced to meet variation in demand.
- There must be clear signage and processes to ensure patients know where they can access care.
- When patients are advised to attend ED by other providers, the initial assessment process must account for this.
- Where clinicians from other providers work within an initial assessment system, service development and governance structures should be shared.
- Initial assessment areas must facilitate confidential conversations, enable access to patients with disabilities and their careers, and maintain patient dignity.
- Staff should have support to assess patients who do not speak or understand English.
- Initial assessment processes must support IPC measures, including minimising crowding in ED.
Clarification of definitions of activity that constitutes initial assessment
The terminology surrounding patient flow – pre-hospital and from the ED front door – is inconsistent, with terms such as streaming, assessment and triage used interchangeably. Since national implementation of streaming models in EDs in 2017/18, providers have said clearer definitions of initial assessment would be helpful.
On arrival at an ED, patients undergo an initial clinical assessment. This includes one or more of the processes described in Table 2. While navigation, redirection and referral are also defined and described to clarify terminology around flow, they are not classed as part of the initial assessment but could be an output.
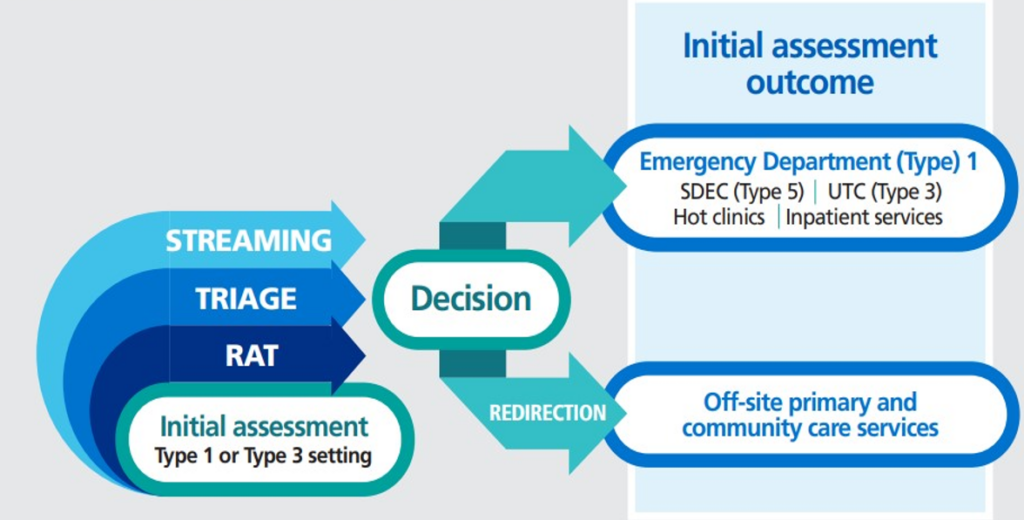
Figure: Initial assessment flow
This diagram describes how initial assessment can include triage, streaming and Rapid assessment and Treatment. It highlights that clinical decisions made through initial assessment conclude in either the patient being redirected off site to an appropriate service or remaining in hospital within the Emergency Department or another service such as and Urgent Treatment Centre.
Definitions of initial assessment and context in which terms should be used
Streaming
Definition
A clinical activity to direct patients to the most appropriate service based on their presenting symptoms, chief complaint and acuity.
Context
Streaming manages queues and matches patients’ needs to the practitioner and area with the right clinical skills and diagnostic and treatment capabilities at the earliest opportunity.
Streaming of patients is carried out within an ED (type 1) or a co-located UTC (type 3) and is likely to be the first clinical activity the patient experiences when arriving. It focuses on determining who will see the patient next, and results in a transfer of care.
It is based on a clinical assessment that typically involves taking a brief medical history and may include performing basic observations. Some sites may include other measures such as NEWS (National Early Warning Score) or PEWS (Paediatric Early Warning Score), basic first aid measures, simple analgesia and simple tests. It is not appropriate to perform complex investigations at this point in the patient journey.
Streaming should be done only by clinicians who are registered and trained in local guidelines and bound by local clinical governance. Patients may also be asked to use digital streaming tools (digital enablers) and where they are staff should be available to support them to do so if required; the clinical governance and accountability remain with the clinical service.
Streaming is the first clinical activity the patient is likely to experience when arriving at the ED. The streaming activity should be brief, to avoid queues developing, and completed as soon as possible. However, the overall system must incorporate safeguards to ensure the further assessment of those patients who require this
Streaming environments must be conducive to a patient’s needs, with sufficient privacy to allow the exchange of confidential information. They should be situated close to clinicians who can provide support if needed, and as close to the main entrance and waiting room as possible.
Outcomes of streaming are likely to be varied and can include:
- UTC (if present on-site)
- ED clinical assessment (resuscitation room, majors, minors)
- streaming to another service such as SDEC, or a specialty assessment unit (medial, surgical, gynaecology, children’s, etc)
- redirection off-site.
Streaming explicitly assumes protocols are in place that allow patients to be immediately transferred to the ED if clinically required and appropriate.
Streaming allows rapid referral into services such as SDEC but pre-hospital referral to services such as SDEC is recommended at an integrated care system (ICS) level, to avoid presentation at the ED where appropriate. Patients arriving by ambulance may be suitable for streaming and there should be joint working and governance between ED, the ambulance service and any streaming provider.
Triage
Definition
The clinical process to prioritise patients, completed before a full assessment to support effective management of demand and flow, identifying time critical requirements for patients.
Context
Triage is part of the process to prioritise patient treatment so that the most acutely unwell patients are seen first. Triage may be done in isolation from streaming or completed after a patient has been initially streamed on arrival. This process and model of care will depend on capacity and demand. When EDs are under pressure, triage may be used to help clinicians identify the order in which patients should be seen, but it can also be part of normal business to support the flow of patients within the ED.
Triage is a meaningful face-to-face clinical assessment which may include observations and the use of triaging tools to support decision-making. It typically takes longer than streaming. The outcome is a priority assigned to the patient, thus helping manage workload and ensuring the sickest patients are seen first.
Triage should be performed by a clinician who is trained and competent in using the specific triage system being applied. Its correct use ensures robust and reproducible assessment. The triage process should start as soon as possible after the patient arrives in the department, and if the patient has not already been streamed will also be the patient’s initial assessment. Sufficient resources need to be allocated to triage to cope with variations in demand (both in numbers and time taken to complete triage), not average demand.
Triage should be performed in an environment that is sufficiently private for exchange of confidential information but not isolated from the department.
Several validated triage systems are in use across England, such as the Manchester Triage System, Canadian Triage and Acuity Scale and the Emergency Severity Index
Rapid assessment and treatment (RAT)
Definition
Rapid assessment and treatment is the initiation of investigations and treatment as determined by a team including senior decision-makers.
Context
RAT is the most complex form of initial assessment and incorporates both streaming and triage. It is commonly but not exclusively used for the most unwell patients arriving to the ED.
A RAT process requires a team that includes a senior decision-making clinician, nursing, and support staff. Clinicians are usually senior doctors such as consultants, middle grades or advanced clinical practitioners who can make decisions about care, order investigations and prescribe early treatments.
It takes longer than streaming or triage (often 20 to 30 minutes, depending on the patient) and therefore, if insufficiently resourced, could create a queue to access it. However, it can improve the overall emergency care episode by initiating investigations and treatments early.
Note on digital enablers
External providers and NHS England have developed digital tools across England to support the initial assessment process and they are becoming a key part of the initial assessment process. More tools are emerging and being implemented to help reduce overcrowding in waiting rooms and to offer patients the ability to self-triage as they enter a type 1 or type 3 site. These tools are clinically designed and governed by the site where they are used.
Definitions of activity that is associated with flow and may be an outcome of initial assessment (but is not part of the initial assessment)
Redirection
Definition
Patients may be redirected to an appropriate service after streaming or triage contact with a clinician or digital clinical tool. Redirection is a choice offered to patients with the full awareness that there is no transfer or formal handover of care.
Context
Redirection involves signposting the patient to services that are suitable for their care needs after a clinician or digital tool has streamed or triaged them. It is different from streaming, navigation, and triage as it involves directing patients to off-site care.
The patient should be able to access the services offered within an appropriate timescale. This is not a direct transfer of care as it is for the patient to decide if they should act on. The responsibility to utilise the advice lies with the patient, and there is not a direct transfer of care.
Technical streaming tools used in EDs may assist in this process. Redirection options are agreed by the hospital on implementing the digital enablers. Examples are community pharmacies, dental services, or other specialist services in primary and community care.
Referral
Definition
Occurs when a patient has been assessed by an appropriately qualified practitioner in an emergency care facility and the decision made to refer them to another specialty for further care. In this case, a full ECDS ED episode has occurred.
Context
To differentiate streaming from referral, it is important to understand that referral happens after a patient has been assessed by an appropriately qualified practitioner in an emergency care facility and the decision made to refer them to another specialty for further care. The ECDS ED episode has been completed.
The clinical governance of this process is subject to local agreements; that is, it may be a negotiated or non-negotiated transfer of care. In the case of streaming there is not a full ECDS ED episode for the attendance, just an ECDS streaming episode. The clinical governance of this process is subject to local agreements: i.e. may be a negotiated or non-negotiated transfer of care.
Navigation
Definition
A process to direct patients to services that may be suitable for their care needs. It is not based on clinical judgement or assessment.
Context
Navigation typically happens before the patient comes under the responsibility of the ED and is not a counted activity in the patient’s journey. This activity, at an early point of a patient’s experience, may not involve a clinician and therefore is not based on clinical judgement. Navigation should not be confused with redirection, which is conducted by a clinician.
Positive or adverse outcomes as a consequence of navigation cannot be recorded. This has clinical governance issues, specifically an absence of accountability or ability to recognise good practice. This process lacks an ability to be counted.
Counting and coding
Initial assessment activity should be recorded using the Emergency Care Data Set v3 regardless of whether the streaming episode occurs in a type 1 or 3 ED. Consistent data supports management of demand and capacity, enables comparisons between sites and supports improved processes for patients. Streaming does not currently attract a national tariff under payment by result; however, local arrangements may apply.
- To record an initial assessment episode in ECDS these fields need to be completed: arrival mode,
- attendance source
- date/time of attendance
- date/time of initial assessment
- chief complaint
- acuity, including NEWS-2 score if relevant, injuries fields if relevant.
If the patient is streamed to another service (eg SDEC or UTC), the episode would include discharge status, discharge destination and, if relevant, safeguarding should also be recorded.
Treatments, investigations, or diagnosis would be necessary.
Providers should refer to the most up-to-date technical standards in the data dictionary for the clock start and stop times for any patient’s journey. Policy guidance should be followed when recording the patient journey on ECDS.
It is critical that patient registration is the first step in any patient journey, so that ECDS can then accurately record all episodes of care whether the outcome of initial assessment is for the patient to remain in the ED, be streamed to a UTC or an SDEC, or to flow into another part of the hospital or offsite.
| Example | Streamed to co-located UTC | Streamed to co-located SDEC |
| Acuity | 4 or 5 | 3, 4 or 5 |
| Chief complaint | From the standard ECDS list | From the standard ECDS list |
| Discharge status | Streamed to primary care | Streamed to ambulatory emergency care (now referred to as SDEC, but this change has still to be made in some systems) |
The NHS UEC Daily SitRep uses the same definitions for streaming and acuity, and submissions to this collection should be consistent with those made to ECDS.
Training in initial assessment
Staff undertaking initial assessment should be registered healthcare professionals who are competent in UEC and have received appropriate training. They will need to demonstrate well-developed interpersonal skills so they can communicate effectively with patients and their families in what is often a stressful situation. Individual departments should have an agreed and documented auditable training process for staff that includes a competency framework.
Experienced reception staff have always had a role in identifying extremely unwell patients presenting to an ED or UTC and will often alert a clinical colleague if they are concerned about a patient who has yet to have a formal clinical assessment. However, their role must be viewed as an adjunct to safety mechanisms in place and never a replacement for a timely initial assessment by a trained registered clinician.
When digital tools are used to support initial assessment, staff trained in using them should be available to support their use by patient using the tools.