Foreword
My name is David Gill and I am a learning disability and autism advisor in the Children and Young People’s Team at NHS England. My role is a lived experience role as I am autistic. As an autistic adult I would like to write a few words about my experiences of going to the dentist when I was a young person and why this is important to me.
I have always taken a lot of pride in how I look after myself and this has included my teeth. I have always made sure I brush my teeth every morning and night and am proud of the fact that I have never had a filling. Going to the dentist can cause some sensory issues though. Things like sitting in the waiting room with people I don’t know and the dentist coming close to my face to check my teeth could be major issues. What helped me was that my Mum took me to the same dentist from a very young age, so I got used to the building. The waiting room always had loads of Beano comics to read so I could ignore the noise of different people. Mum also made sure I was booked in with the same dentist every time so that I got used to her and felt comfortable going back every 6 months. This dentist has since retired but as I am now used to the building, I just take myself for my appointments.
These reasonable adjustments have helped me have good oral care. Making small changes like visiting the same dentist, going at quieter times for appointments, having something else to read or focus on in the waiting room and planning something nice to do after the appointment could really help more young people have a good experience. Get it wrong for people while they are young and this could result in poor dental hygiene all through life, another health inequality for people with a learning disability and autistic people. That is why at a young age it is important we get it right!
David Gill Learning disability and autism advisor, Children and Young People’s team, NHS England
The NHS Long Term Plan (LTP) outlines a commitment to bring hearing, sight and dental checks to autistic children and young people and/or those with a learning disability in special residential schools.
All children and young people deserve a smile for life, and we all have a role to play. I am particularly proud that we have exceeded the ambition outlined in the LTP by not only describing the clinical standard, but also offering training and evidence-based resources for all carers. This will ensure that every child and young person receives effective, daily mouthcare and that non-dental professionals are empowered to “lift the lip” and make every contact count. This strong focus on prevention is not only ethically the right thing to do, it is also a financially astute intervention to deliver return on investment and prevent our children and young people experiencing preventable dental disease.
Sara Hurley Chief Dental Officer England
Equality and health inequalities statement
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. The reduction of inequalities in access and outcomes should be central to the development of dental services. Local commissioners should make explicit in their plans how they have taken into account the duties placed on them under the Equality Act 2010, and also their duties with regard to reducing health inequalities as set out in the Health and Social Care Act 2012. Service design and communications should be appropriate and accessible to meet the needs of diverse communities.
Throughout the development of the policies and processes cited in this document, we have:
Given due regard to the need to reduce inequalities between persons in access to, and outcomes from, healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it.
Given regard to the wider effects of this Clinical Standard in relation to the health and well-being of people and the quality of services provided to individuals including in relation to equality.
Executive summary
There are around 440,000 autistic children and young people and/or those with a learning disability in England. The NHS Long Term Plan (LTP) published in 2019 set out a commitment to provide oral health, sight and hearing checks for autistic children and young people and/or those with a learning disability in residential special education settings (SES). Individuals in these settings reportedly experience poorer oral healthcare outcomes than the general population, which go beyond tooth decay.
Engagement work with children and young people and their carers has been central to the development of the care model and our understanding of the reasonable adjustments to oral healthcare services for autistic children and young people and/or those with a learning disability (aged 4-25 years) with particular reference to the residential special educational setting. Alongside carer representation on the clinical standard working group, two bespoke pieces of engagement work were commissioned from Professor Zoe Marshman at the University of Sheffield and the Challenging Behaviour Foundation.
The co-produced clinical standard and accompanying resources provide greater consistency in delivering improvements in oral health. Oral health checks are a vital starting point but as we heard, without informed support, timely access to appropriate care pathways and sustaining good oral health behaviours can be problematic.
Consequently, the clinical standard provides structured guidance, reasonable adjustments and resources for a streamlined care pathway, clarifying responsibilities with daily mouthcare integral to the delivery on the LTP commitment. The standard supports the vision of universal access whereby everyone receives quality health services that meet their needs. It is designed to be utilised by all those involved in improving health outcomes and quality of life for autistic children and young people and/or those with a learning disability in England.
Delivery of programmes of oral health care and support to residential special education settings currently falls to the community dental services (CDS). However, in certain geographical areas the option to use the CDS may not be appropriate for a number of factors such as existing capacity levels and travel times. Necessary oral health and clinical support has successfully been commissioned from local general dental services (GDS) teams, with the relevant additional competencies or skills. Supported by the Consultant led Managed Clinical Network, these GDS practice teams remain key providers, integral to the on-going multi-disciplinary care planning and vital to ensuring universal access to quality healthcare.
Activities not covered in this clinical standard:
- Population needs assessment and oral epidemiology programmes; these activities are out with the scope of this clinical standard but may be found in the Clinical Guide to Dentistry .
- Procurement of services and contractual/commissioning guidance are not within the scope of this clinical standard.
Who is this for?
This clinical standard is principally aimed at oral health care teams by supporting carers and families in access to dental care for Children and Young People (CYP), to improve oral health and reduce the detrimental impacts of dental disease experienced by autistic children and young people and/or those with a learning disability in England. It includes collaboratively designed evidence-based resources to support a more holistic oral health care model for autistic children and young people and/or those with a learning disability.
The publication outlines the minimum clinical standard for oral health care services for autistic children and young people and/or those with a learning disability (aged 4-25 years) with particular reference to the residential special educational setting. The complementary and supporting CYP patient pathways and services are detailed in the Clinical Standards for Paediatric and Special Care Dentistry and should be read in conjunction this document.
Clinicians and providers of services including dental teams from the General, Community and Hospital Dental Services will be able to draw on several aspects of this document and will also find the Oral Health in Special Educational Settings Clinicians’ toolkit valuable. Complementary toolkits have also been produced for special educational setting staff, and parents/carers of autistic children and young people and/or those with a learning disability in special educational settings.
Local Authorities will find this guidance useful given their responsibilities for oral health and public health. The standard will also be of use to Dental Public Health teams, dental commissioners and other NHS England staff, in particular Integrated Care System staff as they assume their statutory responsibilities.
Service designers and commissioners are offered a benchmark against which existing services may be reviewed and modified. Local Dental Networks and their Paediatric Dentistry and Special Care Dentistry Managed Clinical Networks should consider this clinical standard and the options for reasonable adjustments when reviewing and aligning their service provision and/or re-designing their commissioned services for autistic children and young people and/or those with a learning disability in their local population. Whilst commissioned dental provision in some NHS regions may already meet these requirements others may not.
Whilst the standard is focussed on autistic children and young people and/or those with a learning disability in residential special educational settings, the model and reasonable adjustments could equally be applied to non-residential special educational settings and also to all children and young people in residential special educational settings, regardless of whether they have been identified as having a learning disability and/or autism. It is recommended that oral health programmes should embrace a whole school approach to reduce the risk of inadvertently increasing oral health inequalities.
The NHS Accessible Information Standard and relevant legislative frameworks such as the Human Rights Act 1998, the Mental Capacity Act 2005 and the Equality Act 2010 should also be consulted.
What is a Residential Special Educational Setting?
Residential special educational schools (RSES) and colleges have dual registration and accommodation for their schools and care provision. Children and Young People attend school or college usually on site (registered and regulated by Ofsted as a school or college) and then live in separate accommodation (usually on site) before and after school and at weekends. Definitions are:
- Boarding school is a residential school where children and young people up to the age of 18 live on site for up to 38 weeks a year (going home for holidays).
- Children’s home (boarding school) means there are children and young people up to the age of 18 living on site 52 weeks a year (i.e., full time). They may or may not go home for holidays and some of these Children and Young People (CYP) may have been removed from their families for child protection reasons. These Children’s Homes have a special legal status and are differently regulated by Ofsted (they must be a Children’s Home for children and young people to stay 52 weeks a year). The children and young people who are there for 52 weeks will likely have a legal status known as being ‘looked after’ under Section 20 of the Children Act 1989 (this means their care is shared between the Local Authority and the family and there are additional checks and support that must be in place for these children and young people).
- College/further education (FE) residential accommodation means the same as the above, except that the care (living) provision is now regulated by the Care Quality Commission (CQC). The population here will be over 18 (up to aged 25). The College and FE teaching provision is still regulated by Ofsted.
Designing for clinical delivery
Patient, carer, clinical and commissioner collaboration in designing services is vital. In addition to patient and public engagement a thorough understanding of the population need, with an appreciation of any limitations and constraints created by, factors such as location, logistics of access, infrastructure, school timetable is essential. Guidance for conducting a thorough health needs assessment is detailed in the Clinical Guide to Dentistry for Dental Specialties.
In designing a local service or amending local service provision, the needs assessment should be complemented with clinical advice from the Managed Clinical Networks for Paediatric dentistry and Special Care dentistry. Managed Clinical Networks under the Integrated Care System (ICS) will provide local clinical leadership and work collaboratively with stakeholders, whilst providing quality assurance to their local systems.
There should be regular communication between all stakeholders, including Local Dental Networks, ICS commissioning teams, Consultants in Dental Public Health, Local Authority representatives, Children’s Universal Services, Oral Health Promotion Teams, as well as special residential schools and colleges.
To provide effective continuity of care for CYP at the 16 years of age transition point it is vital that the Managed Clinical Networks in Paediatric Dentistry work closely with Managed Clinical Networks in Special Care Dentistry. This must be done in close liaison with the CYP, their carers and RSES to ensure patient choice and patient voice is integral to the continuing care pathway.
In designing clinical support for the RSES, a pathway for urgent dental care and telephone advice should be in place in line with the Clinical Standard for Urgent Dental Care. A review of the reasonable adjustments is recommended to ensure that this pathway is sufficiently robust, provides timely access and is appropriate for children and young people attending RSES.
Care model
The care model, primarily designed for residential special education settings, has considered the scale, unique logistics, infrastructure as well as the potential impact on educational timetables, caring priorities and daily routines.
Collaborative planning of the timing and format of visit programmes will be key. The initiation of the care pathway commences with the necessary liaison with CYP, their carers and school management teams to plan; access, locations for clinical/visit session and assess requirement for reasonable adjustments. The recommended components of the care model:
- An initial oral health “check-in” for all children and young people with valid consent ensuring reasonable adjustments are made where necessary, e.g. face to face or virtual/remote oral health check.
- A clinical assessment of an individual’s oral health needs, a determination and record of the patient’s oral health risk status.
- Collaborative review of current mouthcare plan/provision of routine oral healthcare for CYP with a co-designed tailored mouth care plan placing an emphasis on prevention.
- Shared decision making for optimal next steps in the CYP’s oral health care pathway with any existing providers and/or hurdles in accessing dental care.
- With relevant consent, liaison with CYP’s team of health care professionals and families to ensure all are aware of oral health care needs and agreed next steps.
- Reinforcing existing health behaviours and prevention measures assessed as delivering good oral health outcomes.
- Establishing mouth care plans with carers with advice on daily routines to improve oral health.
- Referral (urgent and routine) and provision of appropriate clinical interventions in line with the established care pathways described in the Clinical Standards for Paediatric and Special Care Dentistry.
- Organising continuing care; accepting patient for care and/or arranging onward referral to existing provider and/or specialist care.
- With the agreement of the CYP and their carers, the CYP’s existing dental provider remains the default receiving provider to ensure continuity of care.
- Where a child or young person does not have an identified dental care provider; following the initial dental check the service provider should ensure the CYP is accepted for continuing care with an appropriate local dental team.
- Where specialist care is required, the dental teams should manage referrals in line with local pathways overseen by the regional Managed Clinical NetworkChairs. Where applicable, and only with CYP/carer consent, a referral should be copied to the CYP’s own dentist.
- Subsequent visit programmes will need to be co-ordinated around risk based dental check-ups tailored to individual needs, depending on the child or young person’s level of risk, in line with the NICE 2021 guidance Dental checks: intervals between oral health reviews.
A check list of actions and considerations is at Appendix 1, supporting templates and links to resources are at Appendix 2
Reasonable adjustments
Oral health care teams will need to consider reasonable adjustments to ensure appropriate access for individual children and young people.
Lessons identified from COVID-19 and the provision of virtual/remote consultations across primary care with protocols for conduct, consent and record keeping provides evidence and a rationale for this reasonable adjustment to the traditional care model. The “remote consultation” provides an opportunity to operate at scale, whilst developing rapport and a familiarisation with the individual and their carers. The Remote Oral Health Check (ROHC) protocol and methodology as a reasonable adjustment is summarised at Appendix 3.
Compliance with consent, record keeping, referral and information governance for the ROHC are no different to the clinical standard expected for a “face to face “consultation.
The inclusion of a ROHC may ease anxiety levels both for the children and young people and their carers with the potential to lead to a more positive experience. The ROHC also has potential to be deployed within the programme of bespoke risk-based recall with interim care remote “dental check-ins” key to maintaining regular contact and access to professional support without the logistic burden on the CYP, their family and/or the school.
Where face to face visits in a dental practice/clinic are required, consideration must be given to the individual needs of the patient with regards to:
- Time of the appointment when the practice may be quieter.
- Time allowed for CYP to become accustomed to surroundings.
- Length of appointment.
- Private area to recover after appointment.
Consideration may also be given for a visit to the clinical setting where no clinical work is undertaken but is utilised to welcome the individual child or young person to the clinical staff, sights, sounds and surroundings before their first clinical visit.
It is essential that any requirements are considered and planned for ahead of the consultation, treatment or appointment. Discussion should be had with the child/young person and their parent/carer or residential school or college to determine how best to accommodate their needs.
Mouthcare at the residential special educational setting
Staff and parents/carers are to be offered a tailored mouth care plan to support daily mouthcare for the children and young people in their residential special educational setting in line with Delivering Better Oral Health. The oral health care team attached to the residential special educational setting should ensure that the SES are accessing /signposted to the appropriate resources available. Further advice and links to resources are contained in Appendix 2
Workforce
Everyone involved in the provision of oral health care must be appropriately trained and experienced. As part of this, they must have successfully completed the Mini Mouth Care Matters (MMCM) e-learning module on the e-Learning for Healthcare (eLfH) website ‘Caring for the Oral Health of Children and Young People in Special Education Settings’.
The oral health services provided must fall under the clinical leadership of a GDC registered dentist with appropriate skills and training determined by the local Managed Clinical Network in Paediatric Dentistry. Face to face oral health assessments should be completed by dentists supported by other members of the dental team. Remote oral health checks may be completed by any GDC registered member of the dental team.
Appendix 1 – check list for oral health team
1. Training
- Complete e-learning module on e-LfH website: Caring for the Oral Health of Children and Young People in Special Education Settings e-Learning for Healthcare (eLfH)
- Score >80% on multiple choice questions to successfully pass the e-Learning module
2. Planning and Preparation: Establish a point of contact with the residential special education school setting to propose and discuss arrangements for oral health programme, any pre-visits and timetable of supporting events, and potential for remote oral health check (ROHC) where it is agreed that this is a reasonable adjustment.
3. Key information requirements and preliminary actions:
- How many children and young people in RSES?
- Timeframes and dates for the visit(s) and/or RHOC
- Assess how many children and young people’s oral health checks can be done per session?
- Ensure enough clinical time allocated for face to face/remote oral health check with children and young people and arrange timeslots and relay these back to RSES support staff (suggest at least 30 minutes per consultation as a minimum)
- Agree consent process (Appendix 4)
- Discuss reasonable adjustments with support staff at the RSES prior visit or to remote oral health checkg., use of a social story prior to the check. Consider the production of picture books/social story of dental setting.
- Set up visit programme +/- online platform (Resource 1/2), ensure all digital technology functioning correctly.
- Distribute and agree information governance and timeframe for return of medical history, mouth check and pre-check form, e.g. secure on-line platform under NHS IT Governance and Assurance.
- Review relevant consent, medical history, mouth check and pre-check form (Resource 11) for each child or young personin advance of allocated time for the child or young person. Consider reasonable adjustments (Resource 23) which may be required to support the oral health check on the day.
Delivery of the oral health check
- Guidance and complete oral health check form (Resource 16)
- Assessment of Risk use of the Red, Amber Green (RAG) rating (Resource 18)
- Provide tailored oral hygiene and prevention advice based on dental findings, patient factors e.g., co-operation, likes and dislikes (demonstrate oral hygiene tools as required- can direct support staff to the product information guide for instructions on how to use specific recommended oral hygiene tools – (Resource 17)
- Review mouth care plan, (if one already in place) and adapt accordingly or create individualised mouth care (Resource 6)
- Make decision regarding further face-to-face care, recall/assessment, discuss options/arrangements that may already be in place (Resource 18)
- Action all areas of risk classification and decide on next steps/ face-to-face visit / onward referral (Resource 19)
- Follow local referral guidelines, if unsure which dental setting appropriate, use ‘Planning care guide’ resource (i.e. case-mix complexity chart) (Resource 19)
- Arrange follow-up oral health check at an appropriate recall interval
- Write a letter to the child or young person’s parent/guardian, school, social worker (where necessary) and to the young person themselves if they wish, GDP/GP with findings from oral health check, mouth care plan and follow-up arrangements (Resource 22).
Appendix 2 – resources
The Long Term Plan committed to improving health outcomes and to “work with partners to bring hearing, sight and dental checks to children and young people with a learning disability, autism or both in special residential schools” The key to prevention and improved oral health is an awareness of the importance of daily mouthcare and any reasonable adjustments or adaptations that may be required in supporting good oral health in autistic children and young people and/or those with a learning disability.
A package of tools and resources have been adapted and designed as an adjunct to the delivery of the oral health assessment (either face to face/remote) and to support teams in the development of complementary tailored mouthcare plans.
Resources
1. Programme information leaflets for parents/guardians/carers
This leaflet is to be distributed to the parents/ guardians of children and young people within the Residential Special Education Setting. This may be the first point of contact with the parents/ guardians to explain the programme, their role within it and the opportunity to contact the appropriate team to ask any questions. This can be distributed in print or digital form.
For children under 16 years of age, staff should first judge whether the young person is Gillick competent. If not, consent should be sought from those who have parental responsibility. For those young people over 16 years of age, capacity to consent to the procedure should be assumed in line with the Mental Capacity Act 2005. If staff judge that a young person does not have the capacity to consent to the procedure, then they should follow the process outlined in the current Mental Capacity Code of Practice. Moving forward, consent for the remote oral health check process should be obtained during enrolment to the RSES and an opt-in/ out-out scheme may be considered.
2. Programme information leaflets for special educational setting staff
- Staff residential programme leaflet – This leaflet is to be distributed to the relevant care support staff within the SES. It outlines their role and invites any questions. This can be distributed in print/ digital form.
- Staff day programme leaflet – This leaflet is to be distributed to the relevant care support staff within the SES. It outlines their role and invites any questions. This can be distributed in print/ digital form.
3. The consent process
For children under 16 years of age, staff should first judge whether the young person is Gillick competent. If not, consent should be sought from those who have parental responsibility.
For those young people over 16 years of age, capacity to consent to the procedure should be assumed in line with the Mental Capacity Act 2005. If staff judge that a young person does not have the capacity to consent to the procedure, then they should follow the process outlined in the current Mental Capacity Code of Practice.
Moving forward, consent for the remote oral health check process should be obtained during enrolment to the RSES and an opt-in/ out-out scheme may be considered.
4. Mouth check
A mouth check should be completed for each child or young person at regular intervals by a support worker (intervals to be defined by oral healthcare team) usually approximately once a month, unless more frequent attention is required e.g., dry mouth care which may need to be re-evaluated.
It is important the RSES staff identifies:
- The child or young person’s current oral hygiene status
- Whether they are suffering from any obvious oral health problems
- Whether their current mouth care routine needs to be modified e.g., adding dry mouth care
- Any reason why they may need to be seen by a dentist sooner than planned ROHC e.g., any changes to eating, sleeping, behaviour patterns which may be attributed to dental problems
5. Mouth care guide
This RAG mouth care guide provides a visual aid for what to look for inside the mouth during the mouth check, and can be used to advise on changes to mouth care routine and actions going forward e.g. involving senior staff and/or oral health team.
6. Mouth care plan
Can be used in the daily care plan as visual representation of mouth care routine to aid support staff with incorporating mouth care into daily routine.
7. Mouth care recording log
When appropriate, the daily mouth care log should be updated by support staff with every attempt to give mouth care – even if not possible , to attempt at an alternative time. After the mouth check is completed monthly, this may need updating according to the actions found from the mouth care guide. It can also be modified as per direction from the oral health team.
8. Teeth brushing chart
A visual aid which can be used to show toothbrushing attempts, motivating the child or young person to brush their teeth.
9. Product order information guide
Contains information for the oral health team about specialised oral hygiene tools a child or young person may require, and where these can be purchased.
10. Medical history form
This is to be completed prior to the remote oral health check by the child or young person’s parent/carer and sent back to the oral health team.
11. Pre-remote oral health check-in form
12. Assessing e-learning for healthcare
1. SES staff e-learning module: ‘Improving mouth care for children and young people in residential special education setting – designed for training of residential SES staff in mouthcare in residential special educational settings.
2. Dental teams e-learning module: ‘Caring for the Oral Health of Children and Young People in Residential Special Education Settings’ – designed for training of oral healthcare teams in the provision of oral care in special education settings.
3. Allied health professionals e-learning module: Caring for the oral health of children and young people in special education settings – designed for training of allied health professionals in the provision of oral care in special educational settings.
4. Non- residential SES staff e-learning module: Improving mouth care for children and young people in non-residential special education settings – designed for training of non- residential SES staff in mouthcare in special educational settings.
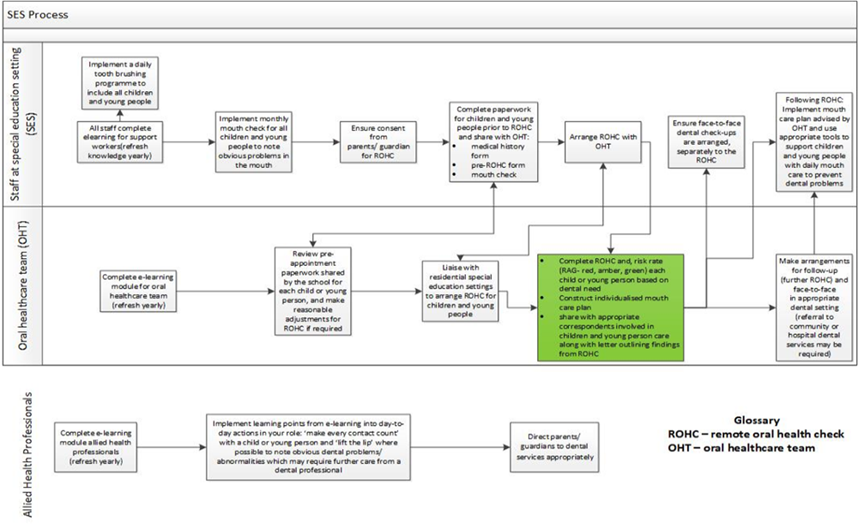
13. Oral Health process
- Oral Health process – Visual diagram of SES oral health process
14. A step-by-step guide to completing a remote oral health check
The purpose of this video is to explain the process of completing a remote oral health check-in for CYP with learning disabilities, autism or both in a special education setting.
15. Remote oral health check flow chart
Outlines entire remote oral health check process for the oral health team in a step-by-step format.
16. Remote oral health check form
For completion by the oral health team containing information about previous dental history, findings from mouth check, future actions and recommended mouth care plan.
17. A user guide for mouth care products
A detailed how-to guide on specialised oral hygiene tools which may be recommended for a child or young person’s daily mouth care routine. This guide contains a step-by-step in pictorial format of how to use each product.
18. Outcome of remote oral health check-in
Visual diagram – outcome of remote oral health check-in.
19. Planning care guide
Visual diagram – planning care guide to inform appropriate outcome of Remote Oral Health Check-in.
20. Social story – having a remote oral check-in
Can be used by support staff with a child or young person in preparation for remote oral health check – created in collaboration with Widgit Health.
21. Role of Residential special educational staff
Visual diagram – role of residential special educational staff.
22. Template letter
Remote oral health check template to GDP/Parents/Guardians regarding findings from remote oral health check.
23. Making reasonable adjustments in dentistry
The video demonstrates how to make reasonable adjustments for patients with learning disabilities, autism or both in your place of work.
24. How to complete a mouth check
The video demonstrates how to complete a mouth check
25. Dental pain communication sheet
Can be used to record dental pain and symptoms using an accessible format developed by Widgit Health.
26. Mouth care plan – widgit
27. Pre Mini MCM Baseline knowledge and school scoping interview template
To be used by oral health care teams and prevention leads to establish baseline knowledge of oral health within SES, and scope the demographic of the CYP to assess needs and tailor delivery of intervention appropriately.
28. Dental passport
A Dental Passport that can be taken with the CYP to any setting which should allow an understanding of their current oral health care regime and needs to ensure standardisation and bespoke care for the individual.
29. Mini MCM Poster on resistance to toothbrushing
Visual aid for care and support staff offering strategies to help children cope with the sensory challenges of toothbrushing.
Training for clinicians
- NHS England » Ask Listen Do – Making conversations count in health, social care and education: Tips for health, social care and education organisations and practitioners
- What is challenging behaviour? – Challenging Behaviour Foundation
- e-Learning for Health Programmes. A number of programmes are relevant including:
- Autism Awareness
- Delivering Sensory Health Services
- Children’s Emotional and Additional Health Needs
- Mouthcare Matters
- Widgit Health – Communication boards and easy read sheets for professionals (widgit-health.com)
Other relevant guidance
- Dental checks: intervals between oral health reviews. National Institute of Clinical Excellence (NICE). 2004
- Delivering Better Oral Health : an evidence-based toolkit for prevention. Public Health England 2017
- NG43 Transition from children to adults’ services for young people using health or social care services National Institute of Clinical Excellence (NICE). 2016
- CG89 Child maltreatment: when to suspect maltreatment in under 18s National Institute of Clinical Excellence (NICE). 2009
- NG76 Child abuse and neglect National Institute of Clinical Excellence (NICE) 2017
- PH28 Looked after children and young people National Institute of Clinical Excellence (NICE). 2010
- Guidance for health services for children and young people with Special Educational Needs and Disability (SEND). NHS England
- The learning disability improvement standards for NHS trusts. NHS England
- Accessible Information Standard. NHS England
Appendix 3 – remote oral health check – a reasonable adjustment
Oral health checks with the oral healthcare team may be organised either as a face to face or as a ‘remote oral health check’ (ROHC). Following on from the initial contact appropriate provisions will be made for the child or young person to be seen face-to-face, in a dental clinical setting suited to their needs (e.g., general dental services, community dental services or hospital services).
The potential for the inclusion of a remote oral health care check as a reasonable adjustment in special education settings has been recognised. This overview of the ROHC and its conduct and place within the process is designed to offer uniformity in application of the reasonable adjustment. Remote oral health checks may be completed by any appropriately trained GDC registered member of the dental team.
Preparation and planning considerations (resource 13/15)
- Ensure there is an appropriate location for remote oral health check to take place – ideally a quiet room where internet/video call access is available. Ensure all digital technology is adequate and functioning prior to commencing ROHC
- When planning allocation of timeslots to children and young people ensure support staff are available, consideration should be made for the use of a social story (resource 20) or any other reasonable adjustments that may assist in this process
- Plan for sufficient allocation of clinical time and relay these back to residential setting. At least 30 minutes per consultation as a minimum and factor in change over time between consultations.
- Ensure appropriate consent completed for ROHC (NB for some residential CYP consent is implied for all medical/dental interventions)
- Complete medical history form (resource 10) – may require assistance from parents/guardians to complete this
- Complete pre-ROHC form (resource 11) – may require assistance from parents/guardians to complete this
- Complete mouth check (resource 4).
- Sharing the information collected with the dental team via online platform prior to the check. The following completed documents should be shared in advance:
- Relevant consent form
- Medical history form (resource 10)
- Pre- check form (resource 11)
- Mouth check (resource 4) with RAG rating.
Supporting the child or young person during ROHC
- At pre-arranged time, accompany and support both with IT (setting up device) and in answering questions if the child or young person is unable to do so. You may also need to support them to open their mouth so that oral healthcare team can assess any obvious concerns or confirm findings from the completed mouth-check
- Discuss the child or young person’s current mouth care routine and need for adaptations. This will help to develop a tailored mouth care plan
- Discuss with oral healthcare team the need for a face-to-face appointment (in appropriate dental setting to suit the child or young person’s needs) Arrange next remote oral health check at appropriate interval- this should be done for the purposes of a safety net in case further referral not actioned and also ensure follow up in place.
Provide prevention advice given during remote oral health check
- Continue supporting CYP to individual level of assistance required with daily mouth care
- Advise on individual mouth care plan and recommendations (resource 6)
- Recommend maintenance of monthly mouth checks or at more frequent intervals as advised by the oral health team (resource 4)
- Motivate the individual child or young person to implement mouth care plan (see rewards toothbrushing chart on completion of daily mouthcare (resource 8)
- Ensure supply of appropriate oral hygiene tools for child or young person which are disposed of and replaced regularly in line with infection control guidance – see product information guide (resource 9)
After the remote oral health check
Ensure correspondence and outcome of the check is documented in the individual’s notes and shared with relevant healthcare professionals alongside parent/carer.
NB: For children or young people with urgent dental needs e.g., facial swelling or uncontrolled bleeding, do not wait for the ROHC. Follow local protocol and arrange urgent dental care immediately.
Oral health process
Appendix 4 – consent
For children under 16 years of age, staff should first judge whether the young person is Gillick competent. If not, consent should be sought from those who have parental responsibility.
For those young people over 16 years of age, capacity to consent to the procedure should be assumed in line with the Mental Capacity Act 2005. If staff judge that a young person does not have the capacity to consent to the procedure, then they should follow the process outlined in the current Mental Capacity Code of Practice.
Moving forward, consent for the remote oral health check process should be obtained during enrolment to the RSES and an opt-in/ out-out scheme may be considered.
Publication reference: PAR1514