Version 3
1. Service background
1.1 The NHS Long Term Plan, highlights the need to boost out-of-hospital care and to reduce pressure on emergency hospital services. It also commits to make greater use of community pharmacists’ skills and opportunities to engage patients.
1.2 Against this background, the NHS Community Pharmacist Consultation Service (CPCS) was commissioned by NHS England as an advanced service from 29 October 2019. A patient referred into the service will undergo a confidential consultation with a community pharmacist to assess their need for an urgent repeat medication or to assess acuity of minor illness symptoms and provide advice to support next steps. At that time, the referrals to community pharmacies were made by telephony services for NHS 111 or Integrated Urgent Care Clinical Assessment Services (IUC CAS) for patients presenting to these services, with low acuity minor illnesses or urgent repeat medicines supply requests, which could be seen by a community pharmacist at a location closer to their home. The service was later extended to cover referrals for low acuity minor illness from general practice settings and referrals from 999 services and 111Online for minor illness and urgent repeat medication.
1.3 From April 2023, referrals from other urgent and emergency (UEC) settings are now included as part of the NHS CPCS. These additional UEC settings include, for example, urgent treatment centres (UTC), emergency departments (ED) and urgent care centres (UCC). This enables patients presenting at these UEC sites with low acuity, minor illness conditions and urgent repeat medication supply requests, to be referred to the NHS CPCS in a comparable way to those made by NHS 111 and IUC CAS services.
1.4 Extending the NHS CPCS to cover referrals from other UEC settings is in line with the ambitions set out in the NHS Long Term Plan, supports relieving pressure on access to general practice (GP) services, and the delivery plan for recovering urgent and emergency care services following the impact of the Covid pandemic. It also helps to tackle elements of existing health inequalities by providing urgent access to patients who are not registered with a GP.
2. Service objectives
2.1 The objectives of the NHS CPCS advanced service are:
- To offer patients who contact either,
- NHS 111 (by telephone or on-line), or
- 999 service, or
- their own GP practice, or
- A primary care out-of-hours service, or
- A UEC setting (e.g.an ED, UTC, UCC), the opportunity to access appropriate urgent care services in a convenient and easily accessible community pharmacy setting.
- To free up clinician capacity in the above settings, for the treatment of patients with higher acuity conditions.
- To identify ways that individual patients can self-manage their health more effectively with the support of community pharmacists and to recommend solutions that could prevent inappropriate use of UEC services in the future.
- To provide urgent access to patients who are not registered with a GP for treatment of low acuity minor illnesses, and to ensure equity of access to the emergency supply provision, regardless of the patient’s ability to pay for the cost of the medicine requested.
3. Requirements for service provision
3.1 Prior to provision of the service, the pharmacy contractor must:
- Be satisfactorily complying with their obligations under Schedule 4 of the NHS (Pharmaceutical and Local Pharmaceutical Services) Regulations (Terms of Service of NHS pharmacists) in respect of the provision of essential services and an acceptable system of clinical governance.
- Notify NHS England that they intend to provide the service by completion of an electronic registration declaration through the NHS Business Services Authority (NHSBSA) Manage Your Service (MYS) platform.
3.2 Where IT solutions which meet the minimum digital requirements of the service (as specified within the NHS CPCS Technical Toolkit and including an application programming interface (API) to facilitate transfer of data into the NHSBSA MYS platform) are available, contractors must utilise one of these systems within the timeframe agreed by NHS England, the Department of Health and Social Care (DHSC) and the Pharmaceutical Services Negotiating Committee (PSNC). When choosing an IT supplier, contractors should refer to the NHS CPCS IT Buyers Guide.
3.3 The data which is submitted to the MYS platform via the API will be used by the NHSBSA for payment and post-payment verification Some of this data, which has been anonymised, will be shared with NHS England for monitoring and service evaluation purposes.
3.4 The pharmacy contractor must have a business continuity plan (BCP) and standard operating procedure (SOP) in place covering the provision of the service. The SOP must include the process for escalation of issues identified, signposting details, staff training and the key contact details for the service (see the template in Annex D).
3.5 The pharmacy contractor must ensure that all pharmacy staff involved in the provision of the service, are familiar with and adhere to the SOP. Both the BCP and SOP should be reviewed regularly, including following any significant incident or change to the service.
3.6 Pharmacies must have a consultation room that will be used for the provision of the service which meets the requirements of the terms of service. Where a face-to-face consultation is the preferred access model for the person, these consultations must be delivered from the consultation room at the pharmacy. There must be IT equipment accessible within the consultation room to allow contemporaneous records of the consultations provided as part of this service to be made within the CPCS IT system.
3.7 Remote consultations are also permitted to be used to provide the service. When undertaking remote consultations, the contractor must ensure that there are arrangements in place at the pharmacy which enable staff to communicate confidentially with the person receiving the service by telephone or another live audio link or a live video link. NHS Guidance to support community pharmacy teams can help to plan for this.
3.8 The pharmacy contractor must participate in any local audit of integrated urgent care service provision organised by NHS 111 or the local urgent care commissioner.
Service availability
3.9 The pharmacy contractor must ensure that the service is available throughout the pharmacy’s full opening hours (i.e., core and supplementary).
3.10 If the service must be temporarily withdrawn by the pharmacy contractor due to unforeseen circumstances, they must inform the NHS Directory of Services (DoS) Provider and Commissioner Helpline (0300 0200 363) as soon as possible to stop referrals being made to the pharmacy. GP practices and UEC settings within the local primary care network (PCN) should also be contacted to prevent them making further direct referrals. The pharmacy contractor must also inform the Commissioner of their temporary withdrawal from the service.
3.11 The pharmacy contractor must ensure the service is accessible, appropriate, and sensitive to the needs of all service users. No eligible person shall be excluded, or experience difficulty, in accessing and effectively using this service due to their race, gender, disability, sexual orientation, religion or belief, gender reassignment, marriage or civil partnership status, pregnancy or maternity, or age.
4. Service description
4.1 The service pathway is outlined in Annex A.
4.2 Patients will access the NHS CPCS by one of the following routes:
- Referred by NHS 111 telephony.
- Referred by NHS 111 on-line.
- Referred by an integrated urgent care clinical assessment service (IUC CAS).
- Referred by 999.
- Referred by general practice.
- Referred by other urgent and emergency care provider (e.g., UTC, ED, UCC).
N.B. for the purposes of this specification, these providers are collectively referred to as the “referring organisation.”
Referral to the community pharmacy
4.3 The referring organisation will refer appropriate patients, who are presenting with low acuity minor illness conditions, or a request for an urgent supply of repeat medicines, to a community pharmacy of the patient’s choice.
4.4 The referring organisation will offer patients a choice of pharmacies which are participating in the CPCS. The referring organisation should use the Directory of Services (DoS) to offer patients a choice of pharmacies for the service, based on location and availability at that time. If the DoS is not available, then a choice of pharmacies must be offered to the patient by the referring organisation that includes the list of local pharmacies offering the service.
4.5 The referring organisation will provide the telephone number of the selected pharmacy to the patient, advising them to either call the pharmacist or attend in-person at the pharmacy.
4.6 A secure, electronic referral that complies with the standards laid out in the NHS CPCS Technical Toolkit, will be sent to the selected pharmacy. The referral will be made into the contractor’s chosen CPCS IT system and/or via NHSmail into the pharmacy NHSmail shared mailbox.
4.7 If no electronic referral message has been received, the pharmacist will contact the referring organisation to confirm whether a referral has been made and, where appropriate, to confirm the patient’s NHS number and GP details and to request that the electronic referral message is resent.
4.8 Where a pharmacy has received a referral but has not been contacted by the patient within 30 minutes of the referral, the pharmacy must make a reasonable attempt to contact the patient using the contact details set out in the referral message as soon as possible. If the patient has not made contact before the next working day, then the pharmacist can close the referral as ‘no intervention or no supply made’. No payment is due where there is no consultation (remotely or face-to-face) with the patient.
4.9 If an electronic referral has not been made by the referring organisation and the patient has self-presented at the pharmacy, treatment is outside the scope of the NHS CPCS. Only patients who have been referred by a referring organisation are eligible to receive advice and treatment under this service. Patients presenting in the pharmacy with a low acuity condition / minor illness or a request for an emergency supply of medicines cannot be diverted into the service. Those who usually manage their own conditions through self-care and the purchase of over the counter (OTC) medicines should continue to self-manage and treat their conditions.
4.10 During the pharmacy’s opening hours, the CPCS IT system must be checked with appropriate regularity, to pick up referrals in a timely manner. This includes checking the pharmacy’s shared NHSmail mailbox when a pharmacy opens and before the pharmacy closes each day to ensure that no messages have been missed.
Referrals for low acuity, minor illnesses
4.11 Where a face-to-face consultation is the preferred access model for the person, these consultations must be provided from the consultation room at the pharmacy. The pharmacist must, using the CPCS IT system, view any available clinical record with the patient’s consent before collecting information on the patient’s condition and then make appropriate records, during the consultation.
4.12 The pharmacist will ensure that any relevant ‘Red Flags’ are recognised and responded to as part of the consultation process.
4.13 The pharmacist will identify any concurrent medication or medical conditions, which may affect the treatment of the patient.
4.14 The outcome of the referral received in relation to low acuity/minor illness may include:
- Self-care advice to the patient.
- Self-care advice and the sale of an OTC medicine.
- Referral to a separately commissioned pharmacy service delivered in the pharmacy.
- Referral to the patient’s GP or relevant out of hours service for an urgent appointment.
- Routine referral to other appropriate services (including other health professionals).
4.15 If it is known that a patient has used the service more than twice within a month, with the same symptoms and there is no indication for urgent referral, the pharmacist should consider referring the patient to their general practice.
Onward referral for an urgent appointment
4.16 There will be times when the pharmacist will need additional advice or will need to escalate the patient to a higher acuity care location (e.g., a GP, UTC or ED).
4.17 The pharmacist should use their clinical judgement to decide the urgency, route and need for referral and then choose one of the options below:
- Option A – Refer the patient for an urgent in-hours appointment with their own GP. After agreeing this course of action with the patient, the pharmacist should telephone the patient’s general practice to secure them an appointment.
- Option B – Call the NHS 111 service when the patient’s own general practice is not available. The pharmacist should call NHS 111 using the healthcare professionals’ line for access to a clinician, to seek advice.
- Option C – Signpost the patient to A&E or call 999. If the patient presents with severe symptoms indicating the need for an immediate medical consultation, the pharmacist should tell the patient to attend A&E immediately or call an ambulance on behalf of the patient.
Referrals for urgent repeat medicines supply
4.18 Referrals can be made into this element of the service from the referring organisations apart from general practice, who can only refer patients with low acuity minor illnesses into the NHS CPCS.
4.19 Patients contacting the eligible referring organisations to request access to urgently needed medicines, will be referred to a pharmacy that is providing this service for assessment and the potential supply of a medicine previously prescribed for that patient on an NHS prescription.
4.20 For the emergency supply to be made, the pharmacist must have interviewed the person requesting the prescription-only-medicine (POM) and satisfied themselves that there is an immediate need for it to be supplied and that it is impracticable in the circumstances for the patient to obtain a prescription without undue delay. They will also assess the suitability and legality of making an emergency supply and confirm that they have the medicine requested in stock.
4.21 With the patient’s consent, their SCR, or an alternative clinical record for the patient, must be checked by the pharmacist unless there is good reason not to do so.
4.22 Where it is appropriate for an emergency supply to be made, and the medicine is in stock at the pharmacy, the pharmacist will arrange for the patient or their representative to come to the pharmacy to collect the medicine.
4.23 If a prescription is available on the EPS tracker, this should be downloaded and used to fulfil the urgent supply need and complete the consultation.
4.24 The pharmacist should apply their professional judgement to determine the most appropriate quantity of medicine to supply, in line with the provisions of the Human Medicines Regulations 2012.
4.25 An NHS prescription charge per item should be collected, unless the patient is exempt from prescription charges, in accordance with the National Health Service (Charges for Drugs and Appliances) Regulations 2015. Any NHS prescription charges collected from patients will be deducted from the sum payable to the pharmacy.
4.26 The pharmacist will advise the patient or their representative on the importance of ordering prescriptions in a timely manner from their GP practice in order that they may change future behaviours and prevent the future need for emergency supplies.
4.27 If the medicine is not in stock at the pharmacy, with the agreement of the patient, the pharmacist will identify another pharmacy that provides the service and forward the electronic referral to the other pharmacy via NHSmail or the CPCS IT system. In this instance, both pharmacies are eligible for the service completion fee.
4.28 If it is not possible to make an emergency supply due to prohibitions within the legislation or other patient factors, the pharmacist will ensure the patient is able to speak to another appropriate healthcare professional by either:
- referring the patient to their own general practice; or
- by contacting a local out of hours provider.
N.B. Pharmacists must not refer a patient back to NHS 111 or the IUC CAS by asking the patient to call back directly.
4.29 If the patient (or representative) is unable to get to the premises, then the pharmacist must ensure the patient is able to obtain the supply in a timely manner by discussing with the patient (or representative) all reasonable options for accessing their medicines, e.g., the pharmacy referring the patient to the out of hours service.
Records and documentation for the CPCS consultations
4.30 Details and the outcome of each CPCS referral must be recorded on the CPCS IT
4.31 Appropriate data from the CPCS IT system may also be shared to support contract management, service monitoring and evaluation.
4.32 A blank FP10DT EPS dispensing token must be used to record any medicines provided to the patient, where they are claiming exemption from prescription charges. This dispensing token must include the following information:
- Full name, address, and date of birth of the patient.
- Patient’s NHS number.
- Name, strength, and form of medicines requested (using DM+D name or shortened DM+D name in both cases).
- The quantity supplied.
- Date of supply.
- Name and address of patient’s GP (for those who are registered with one).
- Referral ID number.
Post event messaging to the patient’s general practice
4.33 The pharmacy contractor will ensure that a notification of the provision of the service is sent to the patient’s general practice on the day of provision or on the following working day. Where possible, this should be sent as a structured message in real-time, however in the absence of an automated digital solution, this should be sent via NHSmail or hard copy.
4.34 If secure electronic data interchange is used and a problem occurs with this notification system, the pharmacy contractor must ensure a copy of the paperwork is sent or emailed to the general practice.
4.35 The information which must be sent to the patient’s general practice is set out in Annex B for urgent medicines supply and Annex C for low acuity, minor illness referrals.
4.36 All relevant records must be managed in line with the Records Management Code of Practice for Health and Social Care.
5. Governance
5.1 The contractor is required to report any patient safety incidents in line with the Clinical Governance Approved Particulars for pharmacies.
5.2 In addition to 5.1 above:
- Any patient safety incident should be logged on the NHS CPCS IT system.
- Where an incident is related to a referral, the referring organisation should be notified of the incident with appropriate details provided.
- The contractor must participate in any reasonable activities associated with the patient safety incident, as deemed necessary by the referring organisation’s local governance group.
6. Payment arrangements
6.1 A consultation fee of £14 will be paid for each completed referral (both urgent medicines supply and low acuity/minor illness).
6.2 Claims for payments for this service will automatically be added to the MYS portal using the Application Programme Interface (API) between the CPCS IT system and the NHSBSA. Contractors will need to submit the claims within the MYS portal, as part of the normal month end claims process.
6.3 For urgent medicines supply, a referral is completed when either:
- the pharmacist has a consultation with the patient (remotely or face-to-face) and confirms no supply is required, or
- the patient is given advice, the patient purchases the required product, or an emergency supply is made, or
- the patient is referred on to another healthcare provider, or
- an EPS prescription is downloaded and dispensed, or
- an item is not available, and the patient is referred to a second pharmacy.
6.4 For low acuity/minor illness, a referral is completed when either:
- the pharmacist has a consultation with the patient (remotely or face-to-face) and the patient is given self-care advice.
- the patient receives self-care advice and purchases an OTC
- the patient is referred to a minor ailments scheme locally (where one exists).
- the patient is referred to an appropriate
- the pharmacist makes the decision that the presenting condition is not minor in nature and the patient is referred onwards to higher acuity services, or
- the patient is contacted and the patient refuses to undergo a full consultation but receives safety-netting advice i.e., pharmacist provides the following advice “if symptoms worsen, please call the pharmacy or NHS 111 for advice”.
6.5 No consultation fee can be claimed where the pharmacist cannot make any contact with the referred patient.
6.6 The cost of medicines supplied under the CPCS urgent medicines provision will be reimbursed using the basic price specified in Drug Tariff Part II Clause 8 – Basic Price. No other elements of the Drug Tariff in relation to reimbursement of medicines apply to this service. An allowance at the applicable VAT rate will be paid to cover the VAT incurred when purchasing the supplied medicine.
6.7 The cost of medicines supplied via the service will be recharged to Integrated Care Board (ICB) medicines budgets on a fair-share basis.
6.8 Claims for payment should be submitted within one month of, and no later than three months from the claim period for the chargeable activity provided. Claims which relate to work completed more than three months after the claim period in question, will not be paid.
7. Withdrawal from the Service
7.1 If the pharmacy contractor wishes to permanently stop providing the service, they must notify NHS England that they are no longer going to provide the service via the MYS platform, giving at least one month’s notice prior to cessation of the service. Contractors will be asked for a reason as to why they wish to stop providing the service.
7.2 The contractor must continue to provide the service for the duration of the notice period.
8. Monitoring and post payment verification
Monitoring
8.1 Pharmacies may be required to provide additional reports for service evaluation and monitoring purposes. These criteria and evaluation periods will be agreed nationally with the Pharmaceutical Services Negotiating Committee (PSNC) and communicated to contractors when any submission is required. The core datasets collected via the API that are required for ongoing service monitoring and evaluation purposes are detailed at Annex E.
8.2 In the event of a referring organisation under this service not being able to make a referral through to the pharmacy, or patients reporting that they have been unable to speak to the pharmacist, the commissioner will investigate this issue and action may be taken in line with the local dispute resolution policy.
8.3 In the event of problems with service provision by a pharmacy contractor, the commissioner will assess the ongoing ability of the pharmacy to provide the service. In the intervening period, the DoS will be amended to stop referrals to the pharmacy until the issue is resolved. Other local providers who may also refer into the pharmacy through this service will also be notified.
Post payment verification
8.4 NHS England has a duty to be assured that where contractors make claims for payment for activity in services, that they meet all the specified requirements of the service. NHS England will work with the NHSBSA Provider Assurance Team to undertake pre- and post-payment verification checks on claims made.
8.5 Additional evidence may be requested directly from contractors. The verification checks include comparing the information provided by contractors in their claims against datasets and evidence sources that are available to the NHSBSA Provider Assurance Team.
8.6 It is the contractor’s responsibility to be able to provide evidence of claims when requested by the NHSBSA for post-payment verification.
8.7 In cases where evidence is not available or does not demonstrate that the service activity was delivered, and so these claims cannot be verified, they may be referred to the Pharmaceutical Services Regulations Committee to decide whether an overpayment has been made.
8.8 In such cases, where the PSRC decides that an overpayment has been made, and will need to be recovered, contractors will be contacted by the NHSBSA and notified of the overpayment recovery process.
8.9 Any overpayment recovery would not prejudice any action that the NHS may also seek to take under the performance related sanctions and market exit powers within The National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013.
8.10 Accurate record keeping is an essential part of the service provision. The necessary records for reimbursement must be kept for a period of three years to demonstrate service delivery in accordance with the service specification, and to assist with post-payment assurance These records must be provided by a contractor when requested by the NHSBSA Provider Assurance Team.
Annex A: service pathway
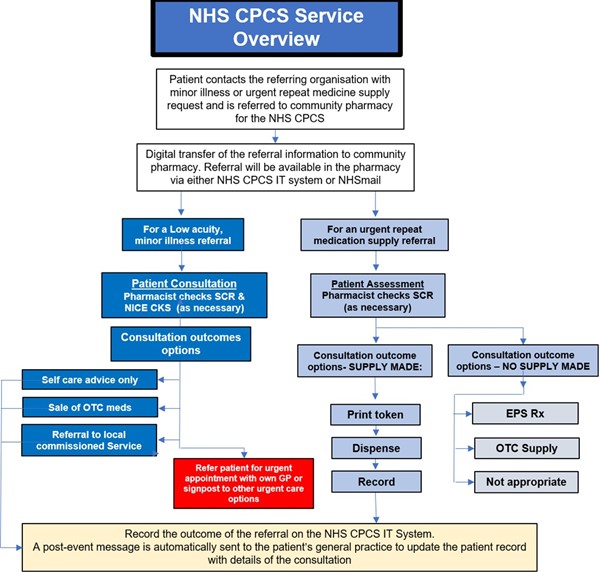
Annex A is a flowchart showing the referral pathway for patients contacting a referring organisation for minor illness or urgent repeat medicines supply and referred to community pharmacy for the NHS Community Pharmacy Consultation Service (CPCS)
Annex B: sending information to general practice (urgent repeat medicines supply referrals)
For an urgent repeat medicines supply referral, where consent is provided, information on the consultation must be sent via NHSmail or other secure digital process to the person’s general practice for entry into the patient record. The following information should be sent:
- System ID
- Person full name
- Date of birth
- Person address
- Postcode
- NHS number
- GP name
- GP Practice details
- GP practice identifier
- Organisation identifier
- Organisation name
- Organisation address
- Organisation contact details
- Date
- Service e., urgent medicines supply
- Clinician name
- Reason for supply request
- Medicine supplied
- Quantity of medication supplied
- Days supplied
- Consultation outcome
- Clinical narrative
- Referral Date
- Urgency of referral
- Referral to (organisation name)
- Referral to (organisation identifier)
- Reason for referral
Annex C: sending information to general practice (low acuity/minor illness referrals)
For a low acuity, minor illness referral, where consent is provided, information on the consultation must be sent via NHSmail or other secure digital process to the person’s general practice for entry into the patient record. The following information should be sent:
- System ID
- Person full name
- Date of birth
- Person address
- Postcode
- NHS number
- GP name
- GP Practice details
- GP practice identifier
- Organisation identifier
- Organisation name
- Organisation address
- Organisation contact details
- Date
- Service ie., minor illness
- Clinician name
- Medicine supplied
- Quantity of medication supplied
- Days supplied
- Dose directions instructions
- Presenting complaint or Issue
- Consultation outcome
- Clinical narrative
- Referral Date
- Urgency of referral
- Referral to (organisation name)
- Referral to (organisation identifier)
- Reason for referral.
Annex D: Key contact details
|
Name of organisation | |
|
Address | |
|
Postcode | |
|
Health professional’s telephone number |
(Note – this number must NOT be shared with the public) |
|
Key contact | |
Directory of Services (DoS) search tool | |
|
Local DoS search tool |
NHS Service Finder (https://finder.directoryofservices.nhs.uk) |
|
Login details |
Username: |
NHS DoS provider and commissioner helpline | |
|
0300 0200 363 | |
Local NHS England team contact | |
|
Key contact | |
|
Telephone | |
|
Email address | |
Copies of this contact sheet can be downloaded from https://psnc.org.uk/cpcs.
Annex E: List of symptoms groups identified for referral to a community pharmacist
This list is not exhaustive but reflects the expected case mix based on current NHS 111 calls.
- Acne, spots, and pimples
- Allergic reaction
- Ankle or foot pain or swelling
- Athlete’s foot
- Bites or stings, insect, or spider
- Blisters
- Constipation
- Cough
- Cold and ‘flu
- Diarrhoea
- Ear discharge or ear wax
- Earache
- Eye, red or irritable
- Eye, sticky or watery
- Eyelid problems
- Hair loss
- Headache
- Hearing problems or blocked ear
- Hip, thigh, or buttock pain or swelling
- Knee or lower leg pain
- Lower back pain
- Lower limb pain or swelling
- Mouth ulcers
- Nasal congestion
- Pain and/or frequency passing
- Rectal pain
- Scabies
- Scratches and grazes
- Sinusitis
- Shoulder pain
- Skin, rash
- Sleep difficulties
- Sore throat
- Teething
- Tiredness
- Toe pain or swelling
- Vaginal discharge
- Vaginal itch or soreness
- Vomiting
- Wound problems – management of dressings
- Wrist, hand, or finger pain or swelling.
Annex F: Core dataset to be captured in the CPCS pharmacy IT system
Core data sets that will be extracted from the CPCS IT system for monitoring and evaluation purposes are:
- System ID
- Person full name
- Date of birth
- Gender
- Person address
- Person postcode
- NHS number
- GP practice identifier
- GP practice details (GP address and postcode)
- Referrer organisation type
- Referrer organisation
- Referrer case ID
- Referrer case reference
- Disposition code
- Organisation identifier (organisation providing the service)
- Date
- Service: minor illness or urgent medicines
- Consultation method
- Reason for supply request (urgent medicines)
- Medicine supplied (urgent medicines)
- Quantity of medication supplied (urgent medicines)
- No supply reason (urgent medicines)
- Prescription charge exemption charge category (urgent medicines)
- Presenting complaint or issue (minor illness)
- Medicine supply type (minor illness)
- Consultation outcome
- Urgency of referral
- Reason for onward referral
- Receiving organisation identifier
- Onward referral date
- Incident.
This data will be obtained using a direct data feed from any CPCS IT system in operation at the time of the extract.
Publication approval reference: PR00361