Statement on reducing health inequalities
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and technical guidance defined in this document we have given:
- due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it.
- regard to the need to reduce inequalities between patients in equity of access to, and outcomes from, healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
Summary
From 1 July 2020 urgent community response (UCR) data has been collected through the Community Services Data Set (CSDS). The UCR Technical Guidance was first published in November 2020 and was updated in May 2021 to reflect changes in policy following the pandemic response and the delivery of community services.
The updates set out in this guidance address changes to the scope of UCR policy, including the prioritisation of the two-hour UCR standard and removal of the two-day reablement UCR standard. Two-day reablement has been superseded by the hospital discharge policy during the pandemic and developments in wider recovery services for intermediate care, which will take forward the ambition for reablement.
As part of the NHS Operational Planning and Contracting Guidance requirements, Integrated Care Systems (ICSs) and providers are expected to deliver two-hour UCR, providing consistent service at scale, from 8am to 8pm, seven days a week (at a minimum) across their full geography. UCR providers should accept referrals from all key routes and should be working to improve outcomes by achieving and exceeding the minimum threshold of responding to at least 70 percent of clinically appropriate demand in two hours or less. Additionally, providers and ICSs should be working to improve capacity in post urgent community response services to support flow and patient outcomes, including avoiding deterioration into crisis again or unnecessary admission. Meeting patients’ urgent care needs at home is key to improving patient outcomes, preventing avoidable hospital admissions, and delivering NHS strategic priorities.
This technical guidance supports collection and recording of the relevant data to ensure a standardised approach for two-hour UCR across England. All providers of publicly-funded community health services, including those funded through the Better Care Fund, are legally mandated to collect and submit community health data, as provided for by section 250 of the Health and Social Care Act 2012.
Please contact the Data and Analytics Team at NHS England for technical and data-related queries.
- For dedicated support around submission reports and provider-specific challenges and support on data quality improvement, contact the Data Liaison Team dataliaison@nhs.net
- For technical submission and registration support with contact CSDS Data Quality dq@nhs.net
- For generic queries relating to reporting to CSDS, including any issues on uploading to SDCS cloud system, contact the National Service Desk nationalservicedesk@nhs.net
For queries relating specifically to this guidance and the UCR national standard for two-hour, please contact the national team at NHS England england.communityservices1@nhs.net
1. Definitions and context
1.1 Urgent Community Response service definitions
Urgent community response services provide urgent care to people in their own homes or usual place of residence, which helps to avoid hospital admissions and enables people to live healthy independent lives for as long as possible. The Community health services two-hour urgent community response standard guidance should be read alongside this technical guidance and should be referred to for information regarding the operational and clinical requirements for NHS-funded UCR services. The national requirements for ICSs to implement two-hour UCR at scale are set out in the NHS Operational Planning and Contracting Guidance. Two-hour urgent community response services should adopt a ‘no wrong door’ ethos and work flexibly based on need to reduce the need for escalation of care to non-home settings. This approach builds on National Institute of Health and Care Excellence (NICE) guidelines.
Two-hour urgent community response
- A two-hour urgent community response is delivered by a community-based service typically provided by a multidisciplinary team to adults in their usual place of residence with an urgent care need (required within two hours) and involves an assessment and short-term intervention(s) (typically lasting up to 48 hours). This is a national standard.
- UCR is typically required when a person is at risk of admission (or re-admission) to hospital due to a ‘crisis’. In these instances, it is likely the person will attend hospital within the following 0-to-24 hour period without interventionto prevent further deterioration and the response can keep the person safe at home/usual place of residence. The referral source will typically be from general practice, self-referral, carer referral, ambulance services, NHS 111, or community-based health and social care (including care homes).
1.2 Major changes to the guidance
There may be other urgent care services (e.g. GP-out-of-hours) or other planned care teams (e.g. district nursing services, mental health services or hospice at-home services) that are not part of an urgent community response service, but may refer in where other support is unable to prevent further deterioration. In other instances, there may be planned care teams that work in an interdisciplinary way to deliver care that meets the requirements of two-hour UCR, despite not being a standalone service with the namesake. Where the criteria for a two-hour UCR standard referral is met as set out in the national guidance, this will be counted as part of the national standard. This guidance has been updated to enable more accurate reporting of the operational delivery of UCR. In parts of the country, UCR services are delivered by different teams through a matrix approach (as opposed to standalone UCR teams), yet this data has not always been counted as part of the national standard. Consequently, additional service types have been included so community teams delivering care that meets the standard for two-hour UCR are now included.
The nature of two-hour UCR is that it is unplanned care. As set out in this guidance, two-hour UCR data should include care contacts of those in crisis and should not be counting ongoing planned care activity. Each UCR should be a new referral, even where people are on a pre-existing caseload or known to the service. As UCR should be delivered in shorter timescales, the recommendation is to collect UCR data as a single referral, rather than add UCR clocks to a pre-existing open referral. This will support improved data completeness and alignment of local delivery with national datasets.
1.3 National waiting time response standard
The two-hour urgent community response standard is 120 minutes or less between clock start and clock stop.
Building on the National Institute of Health and Care Excellence (NICE) guidelines, services should deliver urgent community response care for adults in crisis who need it within a maximum of two hours to prevent further deterioration and to keep them safe at home.
However, where the person being referred requires an urgent community response, but delivery of this care within two hours is not clinically or socially appropriate and the person is supported to remain safely at home with appropriate services for more than two hours, the person should receive care at the earliest opportunity. The associated data should be collected but these responses are not counted as part of the national two-hour urgent community response standard. Full submission of all UCR data to CSDS will enable the volume of this activity to be understood.
Achievement of this standard is defined as: clock stop time is earlier than or equal to clock start time plus two hours.
1.4 Clock starts
Clocks should start at the time at which the referral for the person being referred is received by the provider of urgent community response services. The clock starts are required for the main types of referral routes into urgent community response services:
- Community-based health or social care worker (such as GP, community nurse, care homes, or social care worker)
- Urgent and emergency care sources (such as paramedics, 999 clinical hubs and NHS 111 clinical assessment teams)
- Self/carer/relative-referral (from the person themselves, a family member, neighbour, or a carer, where appropriate):
The two-hour UCR is intended to keep people safe at home and referrals should not be made where the person in crisis is already at an alternative healthcare setting. Referrals from acute or community hospital ward/bed have been excluded from the national two-hour UCR standard.
1.5 Clock stops
For all referral routes, the clock stop is the time at which urgent community response is delivered by the appropriate health or social care worker. While care is usually delivered face to face, or via telemedicine/virtual means in rare instances, regardless of how the care is delivered, the clock should only be stopped once the required intervention to safely address the crisis has been provided. The clock stop for the delivery of care, delivered face to face or via telemedicine/virtual means, will count towards the national standards. Zero-minute waiting times are included in the national standard.
In cases where care is cancelled by the provider (AttendOrNot / AttendanceStatus = 4 Cancelled or postponed by Provider), the date and time of the cancellation should be recorded, as cancellations by provider are still assessed for the two-hour standard.
1.6 Why data is important
The accurate collection, recording and reporting of data are critically important for ensuring that people are benefitting from effective urgent community response services, and will support:
- monitoring of the achievement of the two-hour urgent community response standard
- health and social care commissioners and providers to understand how responsive their local services are, which will lead to improvement of patient experience and outcomes
- reduced reliance on other, less appropriate NHS services
- alignment with the discharge to assess model in the hospital discharge operating model
- learning and continuous quality improvement
- identifying gaps in capacity and capability which may be affecting consistent delivery of the standards.
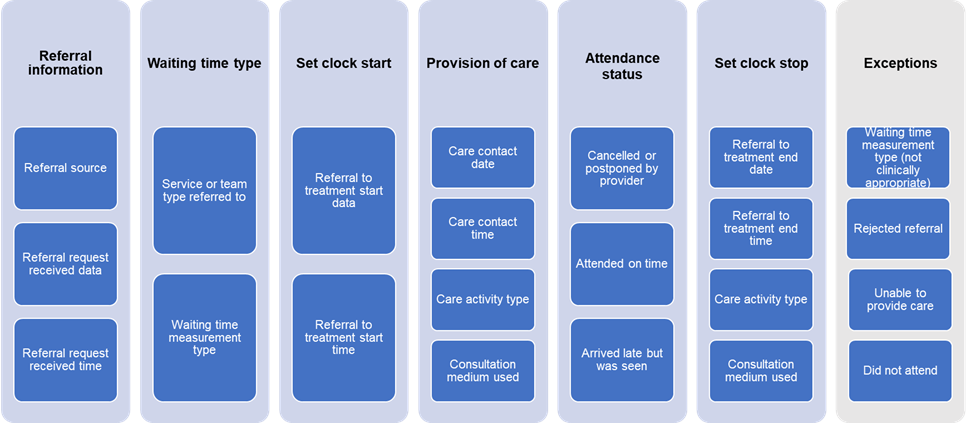
The reported data should include clock starts and clock stops to enable measurement against the response standards, but further data should also be recorded:
- referral into urgent community response service
- the care delivered
- how care was delivered
- onward discharge from urgent community response services.
1.7 Mechanism for reporting data
The urgent community response standards require systematic collection of new data items. Commissioners and providers should ensure that this mandated data is reported to the CSDS and in Electronic Patient Record systems.
The CSDS is a national, patient-level, output-based, mandatory dataset for all providers of publicly funded urgent community response services (including NHS and/or local authority funded). The ability and expectation to submit to CSDS was made on 1 July 2020 when version 1.5 went live. It allows for reporting of urgent community response waiting times data, which will be used in conjunction with existing data items such as patient information, reason for referral, duration of care activities, procedures, observations and findings.
Providers need to make one CSDS submission at provider level to cover all relevant services; it is not possible to make separate submissions for different aspects of the provider’s services. If a provider does not currently submit data to CSDS, they will need to register for SDCS Cloud; further information and contact details can be found on the SDCS Cloud webpage on NHS England’s website.
The information standard DCB1069 (CSDS), under section 250 of the Health and Social Care Act 2012, mandates providers to ensure all data outlined in the CSDS requirements specification, and relevant to the community health services provided, is collected, recorded and reported. NHS England has published comprehensive information about CSDS, the changes brought in through version 1.5 onward and wider background information.
Multiple health and social care organisations, working in partnership, will contribute to achieving the urgent community response standards. Cultures, systems and referral processes within and across commissioners and providers will need to be updated to support this achievement and to allow the collection and transfer of the corresponding data outlined in Sections 2.6 and 2.7 below.
Commissioners will need to consider referral processes for direct referrals between organisations, and referrals made via an interface service/intermediary organisation (that is, a single point of access (SPA) or NHS 111).
2. Recording response times
2.1 Overview of data collection
Wider Community Services Dataset (CSDS) data
Includes wider useful data items such as patient information, reason for referral, duration of care activities, procedures, observations and findings.
2 hour UCR Response standards data
CSDS Data items needed for UCR measurement – quick guide from NHS Digital.
This table lists all CSDS fields needed by NHS England to compile future UCR measures, alongside the mandatory tables and data items needed to make a submission to the CSDS.
More information can be found in the CSDS user guidance and Technical Output Specification (TOS)
Official statistics on UCR will be made available within the monthly Community Services Statistics for Children, Young People and Adults publication.
This guide is subject to change and updates following future developments around UCR data and reporting.
Mandatory tables
|
Table |
Why populate |
|
CYP000 |
Uniquely identifies each CSDS submission made by the provider |
|
CYP001 |
Uniquely identify every patient and record personal details of each patient |
|
CYP002 |
To record details of the GP practice of every patient |
The data needed for recording UCR activity in CSDS
| Table | Field | Notes specific to UCR |
| CYP101 | SourceOfReferral | The most appropriate referral source should be recorded Used to determine if in scope. |
| CYP102 | TeamType | Previously only the following codes were included in UCR: 51: Crisis response intermediate care service 52: Reablement intermediate care service 53: Home-based intermediate care service 54: Community bed-based intermediate care service 45: Integrated multidisciplinary team (jointly commissioned) This has been opened to include other team types to reflect the services that provide a UCR response. Used to determine if in scope. |
| CYP104 | WaitingTime_MeasurementType | Use one of the following codes: 05: Crisis response intermediate care within 2 hours waiting time measurement 07: Crisis response intermediate care waiting time measurement |
| – | RTT_StartDate | Used for Clock start |
| – | RTT_EndDate | Used for Clock stop |
| – | RTT_StartTime | Used for Clock start |
| – | RTT_EndTime | Used for Clock stop |
| CYP201 | Consultation_Medium Used (v1.5) ConsMechanism (v1.6) | The most appropriate consultation mechanism should be recorded. Used to understand what consultation type is stopping the clock. |
| CYP201 | AttenOrNot (v1.5) AttendanceStatus (v1.6) | Used to determine whether the patient has attended or not for the purposes of counting 2hr standard referrals and whether the target has been achieved or not. The following statuses are included in counts of standard referrals and assessment of the 2hr standard 4 – Cancelled or postponed by Provider 5 – Attended on time. 6 – Arrived late but was seen The following statuses are excluded from counts of standard referrals and assessment of the 2hr standard as they are outside the control of the provider 2 – Appt cancelled by the patient 3 – Did not attend – no advance warning given 7 – Patient arrived late and could not be seen NULL values are also excluded as it is not possible to determine whether the patient has attended or not. |
| CYP202 | CYP202 Activity_Type | Any care activities associated with the contact for UCR should be recorded, with the most appropriate care activity type Used to understand what activity type is stopping the clock |
2.2 NHS Data Dictionary
The information in this section should be considered in conjunction with the NHS Data Dictionary which gives definitions for all the data tables, fields and options referred to.
2.3 Service types
The appropriate service type should be reported in the following field in CSDS:
- CYP102 Service or Team Type Referred To Table (CYP102): SERVICE OR TEAM TYPE REFERRED TO (COMMUNITY CARE) / TeamType.
There are four main service types that are most commonly referred to for a two-hour urgent community response:
- 51: Crisis response intermediate care service
- 52: Reablement intermediate care service
- 53: Home-based intermediate care service
- 45: Integrated multidisciplinary team (jointly commissioned)
Additionally, the service types that are applicable for accepting two-hour UCR referrals have been expanded to account for the interdisciplinary nature of UCR teams. It is recognised that some planned care or non-crisis care teams can be referred to deliver an urgent community response to avoid hospital admission. As part of this guidance refresh, two-hour UCR referrals into other service types will no longer be excluded from the national waiting time standard where the referrals meet the other requirements set out in this guidance and the operational guidance.
For all referrals, providers should ensure they are recording the appropriate service type for the two-hour UCR care provided, and the appropriate waiting time measurement type. As required by the CSDS Information Standards Notice, regardless of whether the data is applicable to the national standard, other community data information (e.g. on referral, care contacts and care activities) should still be collected and submitted to the CSDS.
2.4 Waiting time measurement type
As outlined in Section 1.2, urgent community response care has a two-hour response time standard. The appropriate waiting time measurement type should be reported in the following field in CSDS:
- Referral to Treatment Table (CYP104): WAITING TIME MEASUREMENT TYPE / WaitingTime_MeasurementType.
Two-hour urgent community response
Two waiting time measurement types are applicable to urgent community response services:
- 05: Crisis response intermediate care within 2 hours waiting time measurement
- 07: Crisis response intermediate care waiting time measurement.
Providers must consider the definitions of urgent community response to ensure that the correct waiting time measurement type is recorded and acted on when planning the delivery of care.
Where the person being referred requires a two-hour urgent community response as set out in the national operational and clinical community health services two-hour urgent community response standard guidance, the waiting time measurement type should be recorded as:
- 05: Crisis response intermediate care within two-hours waiting time measurement
Referrals with this waiting time measurement type are included in the national standard
Where the person being referred requires urgent community response care which would normally be delivered within two hours but in this exceptional circumstance delivery within two hours is not clinically or socially appropriate, they should receive care within the timescales required and be supported to remain safely at home with appropriate services. In this instance, care should be delivered at the earliest appropriate opportunity and the waiting time measurement type should be recorded as:
- 07: Crisis response intermediate care waiting time measurement.
Referrals with this waiting time measurement type are excluded from the national standard
Providers are encouraged to use the two-hour UCR code 05 for all referrals that meet the national standard requirements. Code 07 should not be used to exclude referrals from the national standard and prevent lower achievement rates of UCR, such as in instances where service capacity or demand pressures.
Other service types
Other community health services may provide a rapid response or provide ongoing care that is delivered within two hours but does not otherwise meet the requirements for two-hour UCR as set out in the guidance (e.g. a District Nurse delivering care that would not prevent a hospital admission in the next two to 24 hours if left untreated). These services may wish to monitor response times but should not use the two-hour UCR code 05 in this instance. The most appropriate waiting time measurement type should be recorded as:
- 07: Crisis response intermediate care waiting time measurement
- 08: Other intermediate care waiting time measurement.
2.5 Referral to treatment period status
The referral to treatment period status field is not applicable for the recording and reporting of urgent community response times. However, providers may choose to use this for referral management purposes.
- Referral to Treatment Table (CYP104): REFERRAL TO TREATMENT PERIOD STATUS / RTT_Status.
2.6 Clock start and corresponding data
Referral source
As outlined in Section 1.3, the clock should start at the time at which the referral for the person being referred is received by the provider of urgent community response services and data for the source of the referral will need to be collected and accurately recorded.
Referral source should be reported in the following field in CSDS:
- Service or Team Referral Table (CYP101): SOURCE OF REFERRAL FOR COMMUNITY / SourceOfReferral.
The most appropriate referral source should be used so that flow and demand across organisations and services can be understood locally and nationally, and quality improvements made.
Where the person needing care is being referred from a community hospital ward/bed, the referral source should be recorded as:
- 07: Community health service (same or other healthcare provider).
Where the person needing care is self-referring, the referral source should be recorded as either of the following options, as appropriate:
- 02: Self-referral
- 03: Carer/relative.
Where the person needing care is being referred from a community-based health or social care worker (that is, GP, paramedic, community nurse or social care worker), the referral source should be recorded as the most appropriate of the 24 available options. Likely examples are:
- 01: General medical practitioner practice
- 07: Community health service (same or other healthcare provider)
- 11: Local authority social services
- 13: Care home
- 19: Telephone or electronic access service (including NHS 111 referrals and Technology Enabled Care services)
- 20: Voluntary sector
- 21: Independent sector
- 22: Ambulance service
- 23: Mental health service.
Where referrals are made through a single point of access, providers are encouraged to collect the original referral source and use supplementary data tables to indicate additional data about the method of referral (i.e. instead of using Code 19: Telephone or electronic access service in place of Code 02: Self referral)
As the two-hour urgent community response is intended for people to receive care in their own home, it is unlikely that referrals from acute settings (such as accident and emergency department or acute hospital inpatient/outpatient department) will be applicable.
Clock start
The clock start should be recorded in the following fields in CSDS:
- Referral to Treatment Table (CYP104): REFERRAL TO TREATMENT PERIOD START DATE / RTT_StartDate.
- Referral to Treatment Table (CYP104): REFERRAL TO TREATMENT PERIOD START TIME / RTT_StartTime.
As the clock start is the time the referral is received for two-hour UCR, providers should consider using the same data collected for and reported in the following fields in CSDS:
- Service or Team Referral Table (CYP101): REFERRAL REQUEST RECEIVED DATE / ReferralRequest_ReceivedDate.
- Service or Team Referral Table (CYP101): REFERRAL REQUEST RECEIVED TIME / ReferralRequest_ReceivedTime.
2.7 Clock stop and corresponding data
Clock stop
The clock stop for all referral sources is defined in Section 1.4. The necessary information for clock stop should be collected/recorded by the health or social care worker delivering the first care activity relevant to the referral when delivery of care starts.
Clock stop dates and times should be reported in the following fields in CSDS:
- Referral to Treatment Table (CYP104): REFERRAL TO TREATMENT PERIOD END DATE / RTT_EndDate.
- Referral to Treatment Table (CYP104): REFERRAL TO TREATMENT PERIOD END TIME / RTT_EndTime.
Providers should consider using the same data collected for the first care contact which meets the care activity type criteria and consultation mechanism used criteria outlined below. These should be reported in the following fields in CSDS:
- Care Contact Table (CYP201): CARE CONTACT DATE / Contact_Date.
- Care Contact Table (CYP201): CARE CONTACT TIME / Contact_Time.
Care activity type
The clock stop requires the provision of care to have started. To identify whether the provision of care has started, the following field in CSDS should be used:
- Care Activity Table (CYP202): COMMUNITY CARE ACTIVITY TYPE / Activity_Type.
Any care activities associated with the contact for UCR should be recorded, with the most appropriate care activity type recorded; five care activity types are applicable to the clock stop and available for selection:
- 01: Administering tests
- 02: Assessment
- 03: Clinical intervention
- 04: Counselling, advice, support
- 05: Patient specific health promotion.
Consultation mechanism
Virtual is increasingly being used to supplement, or be used in place of, face-to-face contact as a consultation mechanism. In these instances, the activity delivered virtually should stop the crisis and escalation of the person’s care to hospital.
While consultation medium is not applicable to the clock stop, it will be useful to record the increasing use of virtual contact and, more generally, how care is being delivered. To record this, the following field in CSDS should be used:
- Care Contact Table (CYP201): CONSULTATION MECHANISM (COMMUNITY CARE)/ ConsMechanism
The most appropriate consultation mechanism should be recorded; ten care activity types are available for selection: In CSDS version 1.6 ‘03 telemedicine’ and ‘06-SMS text messaging’ were retired and replaced by a wider range of telemedicine codes.
- 01: Face-to-face communication
- 02: Telephone
- 03: Telemedicine
- 04: Talk type for person unable to speak
- 05: Email
- 09: Text Message (Asynchronous)
- 10: Instant messaging (Synchronous)
- 11: Video consultation
- 12: Message Board (Asynchronous)
- 13: Chat Room (Synchronous)
- 98: Other (not listed).
For more information or definitions of the above, please refer to the CSDS user guidance.
3. Additional useful data
The CSDS collects data on community health service provision in general, not just waiting times for the provision of these services. This includes, among other things, data about the people who are in contact with community health services and the nature of care provided.
Examples of particularly useful information for commissioners (for commissioning) and providers (for quality improvement) are:
- Service or Team Referral Table (CYP101): PRIMARY REASON FOR REFERRAL (COMMUNITY CARE) / PrimaryReferralReason
- Care Contact Table (CYP201): CLINICAL CONTACT DURATION OF CARE CONTACT / CareContact_Duration
- Care Activity Table (CYP202): PROCEDURE SCHEME IN USE/ Procedure_Scheme, AND; CODED PROCEDURE (CLINICAL TERMINOLOGY) / CodedProcedure
- Care Activity Table (CYP202): FINDING SCHEME IN USE/ Finding_Scheme, AND; CODED FINDING (CODED CLINICAL ENTRY) / FindingCode
- Care Activity Table (CYP202): OBSERVATION SCHEME IN USE/ Observation_Scheme, AND; CODED OBSERVATION (CLINICAL TERMINOLOGY) / CodedObservation
- Onward Referral (CYP105): ORGANISATION IDENTIFIER (RECEIVING)/ OrgID_Receiving, AND; ONWARD REFERRAL REASON / Onward_ReferralReason.
These fields can provide an understanding of health and care need for community health services across the population served. Additionally, understanding resource use and resource use by need is extremely useful for service planning and design.
4. Exceptions and exclusions
All the below exceptions and exclusions should be monitored by commissioners and providers to understand any potential issues with service provision, and efforts should be made to reduce their prevalence where appropriate. Exceptions and exclusions will be monitored by NHS England.
Rejected referrals
Urgent community response services should be inclusive, and all people being referred into these services should receive the most appropriate care. If a referral is rejected, providers should endeavour to re-direct the referral to an appropriate service in keeping with the ‘no wrong door’ ethos of urgent community response care. Where a referral is inappropriate, providers should ensure that rejected referrals are properly recorded using the following fields in CSDS:
- Service or Team Type Referred To Table (CYP102): REFERRAL REJECTION DATE / Referral_RejectionDate.
- Service or Team Type Referred To Table (CYP102): REFERRAL REJECTION REASON / Referral_RejectionReason.
The most appropriate referral rejection reason code should be recorded; there are three available for selection:
- 01: Duplicate referral request (patient already undergoing treatment for the same condition at the same or other healthcare provider)
- 02: Inappropriate referral request (referral request is inappropriate for the services offered by the healthcare provider)
- 03: Incomplete referral request (incomplete information on referral request).
Where any of these options are selected, the applicable referral will be excluded from measurement of the response standard.
Closing referrals
By default, all referrals should be closed when and where it is appropriate to do so. There may be times, outside the influence of the provider, when it is not possible to deliver care. Where this does happen, providers should ensure that referrals are properly closed and recorded using the following fields in CSDS:
- Service or Team Type Referred To Table (CYP102): REFERRAL CLOSURE DATE / Referral_CloseDate.
- Service or Team Type Referred To Table (CYP102): REFERRAL CLOSURE REASON / Referral_ClosureReason.
The most appropriate referral closure reason code should be recorded; there are nine available for selection:
- 01: Admitted elsewhere (at the same or other Healthcare Provider)
- 02: Treatment completed
- 03: Moved out of the area
- 04: No further treatment appropriate
- 05: Patient did not attend
- 06: Patient died
- 07: Patient requested discharge
- 08: Referred to other speciality/service (at the same or other healthcare provider)
- 09: Patient refused to be seen.
Where an urgent community response was delivered virtually, providers are encouraged to differentiate between the time of referral or clock start and the clock stop as to provide useful operational data on the duration of virtual/telemedicine delivery of care. Providers are encouraged to use their community data to drive improvement in appropriate closures of referrals.
No access visit/did not attend (DNA)
No access visits and DNAs should be rare occurrences. However, where the person requiring care is not in their own home when the need for care is identified, there may be issues and delays with transporting that person home to receive care.
Urgent community response services should ensure that the risk of no access visits and DNAs is minimised as far as reasonably possible. Where this does happen, providers should ensure that no access visits and DNAs are recorded using the following field in CSDS:
- Care Contact Table (CYP201): ATTENDANCE STATUS / AttendanceStatus
The most appropriate attendance status code should be recorded; there are six available for selection:
- 2: Appointment cancelled by, or on behalf of, the patient
- 3: Did not attend – no advance warning given
- 4: Appointment cancelled or postponed by the healthcare provider
- 5: Attended on time or, if late, before the relevant care professional was ready to see the patient
- 6: Arrived late, after the relevant care professional was ready to see the patient, but was seen
- 7: Patient arrived late and could not be seen.
No access visits and DNAs will only be regarded as an exclusion where the clock stop criteria outlined in Section 2.7 (‘Care activity type’ and ‘Consultation mechanism’) are met.
Where options 2, 3 or 7 are selected, the applicable care contact will be excluded from measurement of the response standard.
Option 7 should be reported where issues with transporting the person requiring care home meant that care could not be provided.
Providers should then attempt to contact the patient/referring organisation and, when the person’s need for care has been reviewed, consider:
- recording the new, appropriate clock start (the time the need was re-conveyed) against the same referral, and ensuring the date and time of the next care contact are used for the clock stop (following the clock stop guidance outlined in Section 2.7), or
- closing the existing referral (Following the ‘Unable to provide care’ guidance outlined earlier in this section) and recording a new referral with the appropriate service type and waiting time measurement type, and appropriate new clock start.
Not appropriate clinically or for social care, family or carers support – for a two-hour response
Urgent community response should be inclusive, and all people being referred into these services should receive the most appropriate care within the relevant timescale, taking into consideration co-morbidities and the complexity of a person’s needs. The national guidance set out the typical inclusion and exclusion criteria but this list is not meant to be exhaustive. While clinicians should always use professional judgement to decide if a person needs an urgent community response, there may be exceptional cases where it is judged that a person requiring care should not receive care within two hours and thus be excluded from measurement of the response standard.
This should be recorded and this data should be reported in the following field in CSDS:
- Referral to Treatment Table (CYP104): WAITING TIME MEASUREMENT TYPE / WaitingTime_MeasurementType.
The waiting time measurement type for these exceptional circumstances should be recorded as:
- 07: Crisis response intermediate care waiting time measurement.
Clock starts and stops should still be recorded, following the guidance outlined in Sections 2.6 and 2.7.
Publications reference: PRN00200
Version 3