What is digital maturity?
Digital maturity refers to an organisation’s ability to respond to changes and trends in technology. It can also be viewed as an organisation’s ‘state of readiness’ to be able to adapt to, and integrate with, these technologies.
A digitally mature organisation will be able to demonstrate a clear link between their digital strategies and their core business objectives.
Advanced levels of digital maturity can be achieved by:
- developing an advanced digital infrastructure
- involving knowledgeable and committed individuals
- using data for learning and continuous improvement
Why digital maturity matters
Adopting digital health technology is at the centre of the NHS England’s long-term plan which is fundamental to transforming and redesigning health services within the NHS.
Studies have shown that patients are more likely to benefit from technologies that have been carefully designed to support newer ways of working, rather than being ‘add-ons’ to existing systems and structures.
Organisations therefore need to be able to assess their levels of digital maturity in order to identify gaps in service provision, support finance and procurement decisions, understand opportunities for growth and development and to help enable the future planning and delivery of health services.
Digital health technologies can also help reduce workforce pressures, target inequalities in patient access and outcomes, shrink the health sector’s carbon footprint and potentially improve organisational resilience to the effects of climate change and future pandemics.
Digital maturity assessment timeline
2015 | As part of the NHS Five Year Forward View, NHS providers were invited to undertake digital maturity self-assessments, in order to obtain baseline data regarding the effective use of information, technology, and systems within the health service.
2016 | The General Practice Forward View was published, which committed funding to support primary care, including a £45 million to increase online consultation uptake.
2019 | The NHS Long Term Plan provided a further £4.5 billion in funding for primary and community care. A key part of the Long Term Plan was to make better use of data and digital technologies for NHS providers to ‘do things differently.’
Digital maturity assessments
A digital maturity assessment (DMA) is a self-assessment tool that allows an organisation to determine their readiness for the integration of digital technologies. These assessments are designed to help organisations understand their own digital capabilities and the capabilities and compatibilities of information systems across other organisations.
A DMA will tend to focus on the following themes:
- Readiness: an assessment of the organisation’s ability to plan, deliver and optimise the digital systems it needs to operate paper-free at the point of care
- Capabilities: an assessment of the digital capabilities available to that organisation and the extent to which those capabilities are available and being optimised across the organisation
- Infrastructure: an assessment of the extent to which the underpinning infrastructure is in place to support delivery of these capabilities
There are various assessment tools and methods for assessing digital maturity, and consultancy firms can support organisations and businesses wishing to understand their levels of digital maturity.
The NHS Digital Journey Planner can be used to help staff complete this self-assessment process, so that they have an understanding of what is required to deliver high-quality, effective and safe online services.
The Digital Journey Planner starts with a checklist of questions to help provide an assessment, before offering guidance, hints and tips on how to improve effective team working and service delivery for patients.
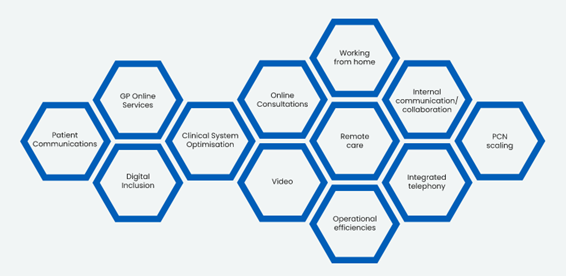
Figure 1: Modules included in the Digital Journey Planner
- Patient communications
- GP online service
- Digital inclusion
- Clinical system optimisation
- Online consultations
- Video
- Working from home
- Remote care
- Internal communication/collaboration
- Integrated telephony
- Operational efficiencies
- PCN scaling
What good looks like
In June 2022, the UK Government published a Plan for digital health and social care which comprised 3 key elements over the next 3 years:
- Digitise
- Connect
- Transform
These are detailed in the What good looks like (WGLL) framework which sets out seven measures of success for organisations:
- Well led: there should be a clear strategy for digital transformation and collaboration
- Ensure smart foundations: digital, data and infrastructure operating environments should be reliable, modern, secure, sustainable and resilient
- Safe practice: organisations should maintain standards for safe care, as set out by the Digital technology assessment criteria for health and social care (DTAC) and will routinely review system-wide security, sustainability and resilience
- Support people: the workforce should be digitally literate and able to work optimally with data and technology. Digital and data tools and systems will be fit for purpose and support staff to do their jobs well
- Empower citizens: citizens should be at the centre of service design and have access to a standard set of digital services that suit all literacy and digital inclusion needs. Citizens will access and contribute to their healthcare information, taking an active role in their health and well-being
- Improve care: the Integrated Care System (ICS) should be embedding digital and data within their improvement capability to transform care pathways, reduce unwarranted variation and improve health and wellbeing
- Healthy populations: data should be used to design and deliver improvements in population health and wellbeing, making best use of collective resources. Insights from data will be used to improve outcomes and address health inequalities
The COVID-19 pandemic accelerated levels of digitalisation throughout the NHS, but levels of digital maturity still vary significantly between healthcare providers.
The WGLL framework is vital in evaluation of digital maturity and may be used by organisations such as the Care Quality Commission (CQC) as part of future assessment criteria.
The WGLL framework is designed to help frontline leaders plan their digital transformation through a peer review process. An online WGLL hub, containing a number of tools and resources, can be used to help support NHS staff and their organisations in achieving WGLL.
The model reflects the unique arrangements in the GP contract where a managed GPIT infrastructure is provided to enable general practice to deliver patient care. It includes a digital primary care maturity assurance tool that continues to evolve to underpin the tracking of local and national progress in meeting the mandated, enhanced and transformational digital requirements.
Click on the following links for more information about the success measures for:
Digital primary care maturity assessment tool (DPCMA)
The DPCMA tool is used to support and assess the effectiveness of the GPIT Operating Model and is reviewed regularly. The data is not a compliance tool, it assures commissioners of their progress towards transformation in primary care as well as help identify areas requiring future investment and/or improvement to support the delivery of their local digital ambitions.
The DPCMA is derived from different data sources including Integrated care board (ICB) questionnaire, General practice annual self-declaration (eDEC) returns, Patient online management information (POMI) and Data security and protection toolkit (DSPT) reports.
Digital primary care maturity assurance tool indicators provide an overview of key indicators and whether it is the practice or commissioning body that should be taking responsibility for these.
Each indicator can be mapped to the different domains of national digital maturity frameworks such as WGLL.
Support for primary care
The Primary Care (GP) Services Operating Model 2021-2023, (also known as the GP IT Operating Model) aims to support the provision of digital services within the primary care setting.
This model:
- reflects on the lessons learned and digital transformation advances made in the pandemic response
- acknowledges establishment of integrated care systems/integrated care boards with roles and responsibilities reflecting forthcoming changes
- seeks to strengthen patient choice of digital access channels
- continues to address the challenges for digitally enabled general practice
The model, along with a Kings Fund Report published in 2021, highlights the importance of reducing health inequalities, stating that digital health solutions can potentially widen health inequalities due to factors such as digital literacy and access.
The NHS Digital Primary Care team help to oversee the support and guidance which is offered to digital services delivered in primary care and individual practices should be urged to work collaboratively with system partners and NHS leaders to invest effectively.
It is important to ensure that technologies are aligned with primary care strategies and transformation plans at both local and national levels. Meeting with relevant stakeholders will be an important part of the development process, and health leaders should consider whether the decommissioning of other services is required to free up additional funding for any new technologies.
Information sharing can be a barrier to successful digital maturity and therefore developing strong levels of trust and accountability between system partners will be essential.
Primary care services may also have access to patient participation groups (PPGs) that may be able to provide valuable support to practices when developing their digital strategy.
It is essential that there is a process of continued monitoring and evaluation in order to ensure continued development of these digital systems.
Further information about integration of primary care services can be found in the Fuller stocktake report.
Related GPG content
Other helpful resources
- NHS England, What good looks like including case studies and stories
- GOV.UK, Data maturity model