1. Introduction
This guidance supports integrated care boards (ICBs) and their partner NHS trusts and foundation trusts (referred to collectively in this guidance as partner trusts) to develop their first 5-year joint forward plans (JFPs) with system partners. The National Health Service Act 2006 (as amended by the Health and Care Act 2022) requires ICBs and their partner trusts (the ICB’s partner NHS trusts and foundation trusts are named in its constitution) to prepare their JFP before the start of each financial year.
This guidance sets out a flexible framework for JFPs to build on existing system and place strategies and plans, in line with the principle of subsidiarity. It also states specific statutory requirements that plans must meet.
It should be read alongside guidance on NHS priorities and operational planning. Specific JFP supporting resources will be available on our FutureNHS collaboration platform (this platform requires you to register and log in).
1.1 Action required of integrated care boards (ICBs) and their partner trusts
ICBs and their partner trusts have a duty to prepare a first JFP before the start of the financial year 2023/24 – i.e. by 1 April. For this first year, however, NHS England is to specify that the date for publishing and sharing the final plan with NHS England, their integrated care partnerships (ICPs) and Health and Well-being Boards (HWBs), is 30 June 2023. We therefore expect that the process for consulting on a draft (or drafts) of the plan, should be commenced with a view to producing a version by 31 March, but recognise that consultation on further iterations may continue after that date, prior to the plan being finalised in time for publication and sharing by 30 June.
ICBs and their partner trusts must consult with those for whom the ICB has core responsibility (people who are registered with a GP practice associated with the ICB, or unregistered patients who usually reside in the ICB’s area, as described in the ICB constitution) and anyone else they consider appropriate. This should include the ICP and NHS England (with respect to the commissioning functions that have been and will be delegated to ICBs). A draft JFP should be shared with the relevant ICP and NHS England; see section 4.1.
ICBs and their partner trusts must involve relevant HWBs in preparing or revising the JFP. This includes sharing a draft with each relevant HWB, and consulting relevant HWB’s on whether the JFP takes proper account of each relevant joint local health and wellbeing strategy (JLHWS); see section 4.1.
ICBs and their partner trusts should agree processes for finalising and signing off the JFP. The final version must be published, and ICBs and their partner trusts should expect to be held to account for its delivery – including by their population, patients and their carers or representatives – and in particular through the ICP, Healthwatch and the local authorities’ health overview and scrutiny committees. JFPs must be reviewed and, where appropriate, updated before the start of each financial year; see section 4.2.
1.2 Purpose of the joint forward plan
Systems have significant flexibility to determine their JFP’s scope as well as how it is developed and structured. Legal responsibility for developing the JFP lies with the ICB and its partner trusts. However, we encourage systems to use the JFP to develop a shared delivery plan for the integrated care strategy (developed by the ICP) and the JLHWS (developed by local authorities and their partner ICBs, which may be through HWBs) that is supported by the whole system, including local authorities and voluntary, community and social enterprise partners.
As a minimum, the JFP should describe how the ICB and its partner trusts intend to arrange and/or provide NHS services to meet their population’s physical and mental health needs. This should include the delivery of universal NHS commitments (for the purposes of this guidance, universal NHS commitments are those described in the annual NHS priorities and operational planning guidance and NHS Long Term Plan) address ICSs’ four core purposes and meet legal requirements (this includes the National Health Service Act 2006 and the requirements of the Public Sector Equality Duty, section 149 of the Equality Act 2010).
1.3 Relationship with NHS planning
ICBs and their partner trusts will continue to separately submit specific operational and financial information as part of the nationally co-ordinated NHS planning process. We will work with systems to avoid duplication and ensure alignment between NHS planning submissions and the public-facing JFP.
2. Principles
Three principles describing the JFP’s nature and function have been co-developed with ICBs, trusts and national organisations representing local authorities and other system partners.
JFP principles
Principle 1: Fully aligned with the wider system partnership’s ambitions.
Principle 2: Supporting subsidiarity by building on existing local strategies and plans as well as reflecting the universal NHS commitments.
Principle 3: Delivery focused, including specific objectives, trajectories and milestones as appropriate.
3. Legislative requirements
Statute describes the purpose of the JFP, the NHS mandate, the integrated care strategy, JLHWSs, joint strategic needs assessments (JSNAs) and system capital plans. For the relationship between the various requirements, see Appendix 1.
Appendix 2, Table 1 describes each statutory requirement the JFP must meet.
4. Developing the joint forward plan
4.1 Consultation
Close engagement with partners will be essential to the development of JFPs (this relates to the general duty of ICBs to involve the public (s14Z45 of the NHS Act 2006), the duty of NHS trusts to involve the public (s242 of the NHS Act 2006) and the ICB duty to consult with the public and other relevant persons when developing the JFP (s14Z54 of the NHS Act 2006)). This includes working with:
- the ICP (ensuring this also provides the perspective of social care providers) – see guidance on adult social care principles for ICPs; this advises on how ICPs and adult social care providers should work together.
- primary care providers (this includes the full breadth of primary care services, including general practice, community pharmacy, optometry and dental services)
- local authorities and each relevant HWB
- other ICBs in respect of providers whose operating boundary spans multiple ICSs
- NHS collaboratives, networks and alliances
- the voluntary, community and social enterprise sector
- people and communities that will be affected by specific parts of the proposed plan, or who are likely to have a significant interest in any of its objectives, in accordance with the requirement to consult described below.
Where an ICB and its partner trusts are developing their JFP or revising an existing plan in a way they consider to be significant (see section 4.2 for revision of plans), there is a statutory duty to consult:
- people for whom the ICB has core responsibility: i.e. those registered with a GP practice associated with the ICB or unregistered patients who usually reside in the ICB’s area (as described in the ICB constitution).
- anyone else they consider it appropriate to consult: e.g. specific organisations with an interest in the plan or whose views it would be useful to obtain, and out-of-area patients who receive treatment funded by the ICB.
The approach should be determined by the ICB and its partner trusts but could involve working with people to understand how services can better meet local needs, developing priorities for change and gathering feedback on draft JFPs.
As JFPs will build on and reflect existing JSNAs, JLHWSs and NHS delivery plans, we do not anticipate their development will require full formal public consultation, unless a significant reconfiguration or major service change is proposed (see also Cabinet Office guidance on consultation principles and Local authority health scrutiny guidance, which provides guidance on service reconfigurations and scrutiny by health overview and scrutiny committees).
Previous local patient and public engagement exercises and subsequent action should inform the JFP. The ICB and its partners will need to consider how this is managed to maximise the benefits from engagement and fulfil these statutory duties efficiently.
The JFP must be reviewed and either updated or confirmed annually before the start of each financial year. For consistency and to avoid duplication of effort, we recommend ICBs and their partner trusts develop a standard approach to consulting on the JFP, while recognising this may need to change over time.
In developing the JFP, ICBs and their partner trusts should consider other relevant duties: e.g. seeking the views of underserved groups (such as inclusion health and vulnerable populations) as part of the duty to reduce inequalities. They must also show they have discharged their legal duty under the Public Sector Equality Duty (s.149, Equality Act 2010).
ICBs and their partner trusts must include in their JFP a summary of the views expressed by anyone they have a duty to consult and explain how they have taken them into account.
Further guidance on public engagement and consultation for ICBs is on our website.
Role of NHS England
We will support ICBs and their partner trusts to develop JFPs – please engage early with us. This will be of particular importance, for example, in relation to the services that we will delegate in future to ICBs.
We will review and comment on the draft JFP, and we recommend this is done in parallel with the review by HWBs (see below). This will not be a formal assurance process but an opportunity to support ICBs and their partner trusts to develop their plans.
Separately we will continue to conduct formal assurance of the information submitted in operational planning returns.
Role of health and wellbeing boards
In preparing or revising their JFPs, ICBs and their partner trusts are subject to a general legal duty to involve each HWB whose area coincides with that of the ICB, wholly or in part. The plan itself must describe how the ICB proposes to implement relevant JLHWSs (a joint local health and wellbeing strategy (JLHWS) is defined as a strategy under section 116A of the Local Government and Public Involvement in Health Act 2007, as amended by the Health and Care Act 2022).
ICBs and their partner trusts must send a draft of the JFP to each relevant HWB when initially developing it or undertaking significant revisions or updates. They must consult those HWBs on whether the draft takes proper account of each JLHWS published by the HWB that relates to any part of the period to which the JFP relates. A HWB must respond with its opinion and may also send that opinion to us, telling the ICB and its partner trusts it has done so (unless it informed them in advance that it was planning to do so) -we may discuss this opinion with the ICB and its partner NHS trusts and foundation trusts.
If an ICB and its partner trusts subsequently revises a draft JFP, the updated version should be sent to each relevant HWB, and the consultation process described above repeated.
The JFP must include a statement of the final opinion of each HWB consulted.
4.2 Revision of joint forward plans
Annual updates
ICBs and their partner trusts should review their JFP before the start of each financial year, by updating or confirming that it is being maintained for the next financial year. They may also revise the JFP in-year if they consider this necessary.
We recognise that 2022/23 is a transition year for ICSs and that it will require time and extensive engagement to fully develop integrated care strategies. The annual refresh of JFPs allows plans to be iterated and provides the opportunity for further engagement and collaboration, as well as the opportunity to continue to reflect the most appropriate delivery mechanisms and partners’ actions.
Where an ICB and its partner trusts update the JFP, in a way they consider to be significant, the same requirements regarding engagement and consultation apply.
Available support
Supporting resources providing further content recommendations will be available soon.
NHS England regional teams can offer support and advice and should be engaged early.
Please direct any technical queries to england.nhs-planning@nhs.net.
Appendix 1: Legislative framework – further detail
Figure 1 shows the statutory framework relating to the joint forward plan (JFP). Please note, it does not show interaction with wider system partners.
Figure 1: Relationship of the JFP with other strategies and plans
In some systems, Health and Well-being Boards’ (HWBs) geography is coterminous (or nearly coterminous) with the system footprint and therefore the relationships may be different.
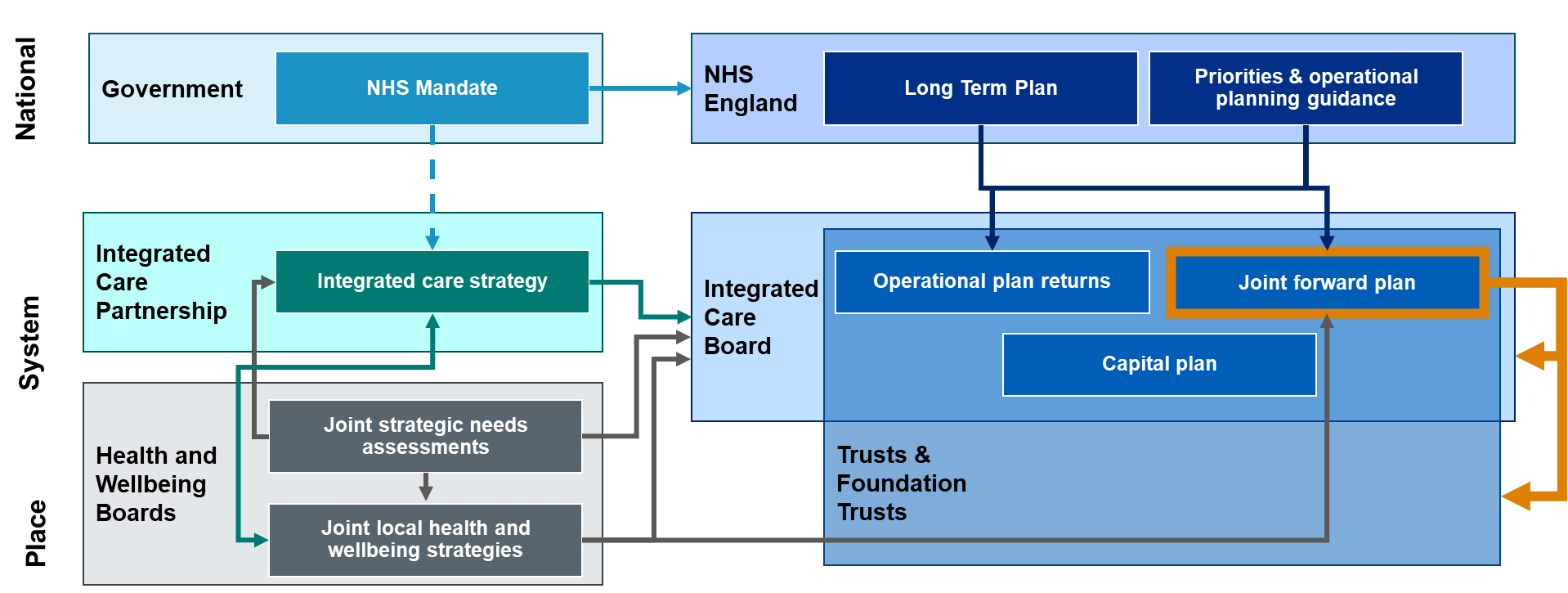
Figure 1 accessible text:
National
- Government: NHS Mandate – NHS England: Long term plan, priorities and operational planning guidance
System
- Integrated care partnerships: Integrated care strategy – Integrated care board: Operational plan returns, Joint forward plan, Capital plan.
Place
- Health and Wellbeing Boards: Joint strategic needs assessments, joint local health and wellbeing strategies.
NHS mandate
The government’s mandate to NHS England sets out our objectives, revenue and capital resource limits. This informs both our guidance on priorities and planning requirements and the integrated care strategy.
The JFP will address objectives in the government mandate regarding the ambitions in the NHS Long Term Plan and NHS planning guidance. It will also deliver on the integrated care strategy, which must have regard to the mandate.
Integrated care strategy
The Department of Health and Social Care has issued guidance on the development of integrated care strategies.
The Local Government and Public Involvement in Health Act 2007, as amended by the Health and Care Act 2022, requires the ICP to produce an integrated care strategy. This should describe how the local population’s assessed needs will be met through the exercise of functions by the ICB, local authorities and NHS England. It must address integration of health and social care and should address integration with health-related services.
In addition, the ICP must have regard to the NHS mandate in developing the integrated care strategy. As such, it should reflect both NHS priorities described in the mandate and the local population’s assessed needs.
The ICB has a statutory duty to have regard to the relevant integrated care strategy in exercising its functions. The JFP is expected to set out steps for delivering the integrated care strategy.
Capital plan
Before the start of each financial year, ICBs and their partner trusts must set out their planned capital resource use. We will publish separate guidance on preparing capital plans.
The content of the JFP should be consistent with this capital plan.
Joint strategic needs assessments (JSNA)
JSNAs, developed by each responsible local authority and its partner ICBs, assess needs that can be met or be affected by the responsible local authority, its partner ICBs or NHS England. These include the local community’s current and future health, care and wellbeing needs, as well as the wider determinants of health which affect those needs, to inform local decision-making and collaboration on development of JLHWSs and the integrated care strategy.
The ICB has a statutory duty to have regard to JSNAs when exercising any relevant functions. The JFP is expected to describe delivery plans to meet the population health needs of people in the ICB’s area.
Joint local health and wellbeing strategies
Each responsible local authority and its partner ICBs will have produced a JLHWS. This is a strategy to meet the needs identified in JSNAs and is unique to each local area. The ICP is expected to build on the JLHWS, which may be facilitated by shared membership across HWBs and the ICP.
Each responsible local authority and its partner ICBs are required to consider whether JLHWSs need to be updated in response to any new or updated integrated care strategy.
The ICB has a statutory duty to have regard to JLHWSs in exercising any relevant functions. The steps that the ICB proposes to take to implement any JLHWS must be described in the JFP.
Appendix 2: Legislative requirements – further detail
Legislative requirement: Describing the health services for which the ICB proposes to make arrangements.
The plan must describe the health services for which the ICB proposes to make arrangements in the exercise of its functions.Implications for the JFP:
The plan should set out how the ICB will meet its population’s health needs. As a minimum, it should describe how the ICB and its partner trusts intend to arrange and/or provide NHS services to meet the physical and mental health needs of their population.Legislative requirement: Duty to promote integration
Each ICB must exercise its functions with a view to ensuring that health services are delivered in an integrated way and that their provision is integrated with that of health-related or social care services, where this would:- improve quality of those services
- reduce inequalities in access and outcomes.
Implications for the JFP:
Plans should describe how ICBs will integrate health services, social care and health-related services to improve quality and reduce inequalities. This could include organisational integration (e.g. provider collaboratives), functional integration (e.g. non-clinical functions), service or clinical integration (e.g. through shared pathways, multidisciplinary teams, clinical assessment processes). This must include delivery on the integration ambitions described in the relevant integrated care strategy and joint local health and wellbeing strategies (JLHWSs).Legislative requirement: Duty to have regard to wider effect of decisions
In making decisions about the provision of healthcare, an ICB must consider the wider effects of its decisions, also known as the ‘triple aim’ of (a) health and wellbeing of the people of England (including by reducing inequalities with respect to health and wellbeing), (b) quality of healthcare services for the purposes of the NHS (including by reducing inequalities with respect to the benefits obtained by individuals from those services) and (c) sustainable and efficient use of resources by NHS bodies.Implications for the JFP:
The plan should articulate how the triple aim was considered in its development. It should also describe approaches to ensure the triple aim is embedded in decision-making and evaluation processes.Legislative requirement: Financial duties
The plan must explain how the ICB intends to discharge its financial duties.Implications for the JFP:
The plan must describe how the financial duties under sections 223GB to 223N of the NHS Act 2006 will be addressed. This includes ensuring that the expenditure of each ICB and its partner trusts in a financial year (taken together) does not exceed the aggregate of any sums received by them in the year, and complying with NHS England financial objectives, directions and expenditure limits.It should also set out how the efficiency and productivity of NHS services will be improved in line with the core purpose to ‘enhance productivity and value for money’.
This should include the key actions the ICB will take to ensure that the collective resources of the health system are used effectively and efficiently. This could include specific plans to support the effectiveness of financial governance and controls; address unwarranted variation; strengthen understanding of the cost of whole care pathways; maximise consolidation and collaboration opportunities across corporate services; unlock efficiency through capital investment; and improve use of NHS estate.
Legislative requirement: Implementing any JLHWS
The plan must set out the steps that the ICB proposes to take to implement any JLHWSs to which it is required to have regard under section 116B(1) of the Local Government and Public Involvement in Health Act 2007.Implications for the JFP:
The plan must set out steps the ICB will take to deliver on ambitions described in any relevant JLHWSs, including identified local target outcomes, approaches and priorities.Legislative requirement: Duty to improve quality of services
Each ICB must exercise its functions with a view to securing continuous improvement in:- the quality of services provided to individuals for or in connection with the prevention, diagnosis or treatment of illness
- outcomes including safety and patient experience.
Implications for the JFP:
The plan should contain a set of quality objectives that reflect system intelligence. It should include clearly aligned metrics (on processes and outcomes) to evidence ongoing sustainable and equitable improvement. Quality priorities should go beyond performance metrics and look at outcomes and preventing ill-health, and use the Core20PLUS5 approach to ensure inequalities are considered. Plans should align with the National Quality Board principles.Legislative requirement: Duty to reduce inequalities
Each ICB must have regard to the need to (a) reduce inequalities between persons with respect to their ability to access health services and (b) reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services. There is also a duty to have regard to the wider effects of decisions on inequalities. The duty to promote integration requires consideration of securing integrated provision across health, health-related and social services where this would reduce inequalities in access to services or outcomes achieved.Implications for the JFP:
The plan should set out how the ICB intends to deliver on the national vision to ensure delivery of high-quality healthcare for all, through equitable access, excellent experience and optimal outcomes. ICBs must also be mindful of, and comply with, the requirements of the Public Sector Equality Duty, section 149 of the Equality Act 2010.Legislative requirement: Duty to promote involvement of each patient
Each ICB must promote the involvement of patients, and their carers and representatives (if any), in decisions that relate to (a) the prevention or diagnosis of illness in the patients or (b) their care or treatment.Implications for the JFP:
The plan should describe actions to implement the Comprehensive model of personalised care, which promotes the involvement of each patient in decisions about prevention, diagnosis and their care or treatment.Legislative requirement: Duty to involve the public
ICBs and partner trusts have a duty to involve people and communities in decisions about the planning, development and operation of services commissioned and provided.Implications for the JFP:
The plans should describe how:- the public and communities were engaged in the development of the plan
- the ICB and partner trusts will work together to build effective partnerships with people and communities, particularly those who face the greatest health inequalities, working with wider ICS stakeholders to achieve this
- activity at neighbourhood and place level informs decisions by the system and how public involvement legal duties are met and assured.
Legislative requirement: Duty to patient choice
Each ICB must act with a view to enabling patients to make choices with respect to aspects of health services provided to them.Implications for the JFP:
The plan should describe how ICBs will ensure that patient choice is considered when developing and implementing commissioning plans and contracting arrangements, and delivering services. The plan should also describe how legal rights are upheld and how choices available to patients are publicised and promoted.Legislative requirement: Duty to obtain appropriate advice
Each ICB must obtain appropriate advice to enable it to effectively discharge its functions from persons who (taken together) have a broad range of professional expertise in (a) the prevention, diagnosis or treatment of illness and (b) the protection or improvement of public health.Implications for the JFP:
The plan should outline the ICB’s strategy for seeking any expert advice it requires, including from local authority partners and through formal governance arrangements and broader engagement.Legislative requirement: Duty to promote innovation
Each ICB must promote innovation in the provision of health services (including in the arrangements made for their provision).Implications for the JFP:
The plan should set out how the ICB will promote local innovation, build capability for the adoption and spread of proven innovation and work with academic health science networks and other local partners to support the identification and adoption of new products and pathways that align with population health needs and address health inequalities.Legislative requirement: Duty in respect of research
Each ICB must facilitate or otherwise promote (a) research on matters relevant to the health service and (b) the use in the health service of evidence obtained from research.Implications for the JFP:
The plan should set out how the ICB will facilitate and promote research, and systematically use evidence from research when exercising its functions. This could include considering research when commissioning, encouraging existing providers to support and be involved in research delivery, recognising the research workforce in workforce planning, and supporting collaboration across local National Institute for Health and Care Research (NIHR) networks. Plans should address the research needs of the ICB’s diverse communities.Legislative requirement: Duty to promote education and training
Each ICB must have regard to the need to promote education and training (this duty relates specifically to persons mentioned in section 1F(1) National Health Service Act 2006. They are “persons who are employed, or who are considering becoming employed, in an activity which involves or is connected with the provision of services as part of the health service in England”) so as to assist the Secretary of State and Health Education England (HEE) (subject to the parliamentary passage of the required Regulations, it is intended that HEE will merge with NHS England in April 2023) in the discharge of the duty under that section.Implications for the JFP:
The plan should describe how the ICB will apply education and training as an essential lever of an integrated workforce plan that supports the delivery of services in the short, medium and long term. The plan should articulate the role of education and training in securing healthcare staff supply and responding to changing service models, as well as the role of trainees in service delivery.Legislative requirement: Duty as to climate change, etc.
Each ICB must have regard to the need to (a) contribute towards compliance with (i) section 1 of the Climate Change Act 2008 (UK net zero emissions target) and (ii) section 5 of the Environment Act 2021 (environmental targets), and (b) adapt to any current or predicted impacts of climate change identified in the most recent report under section 56 of the Climate Change Act 2008.Implications for the JFP:
The plan should describe how the ICB and its partner trusts will deliver against the targets and actions in Delivering a ‘Net Zero’ NHS, including through aligning the JFP with existing green plans.Legislative requirement: Addressing the particular needs of children and young persons
The plan must set out any steps that the ICB proposes to take to address the particular needs of children and young persons under the age of 25.Implications for the JFP:
This could include using data and gathering insights to ensure the plan identifies and sets steps for delivery of the longer-term priorities and ambitions for the ICB’s population of children, young people and families.Legislative requirement: Addressing the particular needs of victims of abuse
The plan must set out any steps that the ICB proposes to take to address the particular needs of victims of abuse (including domestic and sexual abuse, whether children or adults). It must have due regard to the provisions of the Domestic Abuse Act 2021 and accompanying statutory guidance, and relevant safeguarding provisions.Implications for the JFP:
This should include related health inequalities and access to, and outcomes from, services. The plan should also cover the needs of staff who are victims of abuse. This should include the use of data and lived experience to ensure the plan identifies and sets out steps for the delivery of longer-term priorities and ambitions for supporting victims, tackling perpetrators and the prevention of abuse, including through the commissioning of services.Other content
Other recommended content.
- Workforce: Evidence-based, integrated, inclusive workforce plans that ensure the right workforce with the right skills is in the right place to deliver operational priorities aligned to finance and activity plans.
- Performance: Specific performance ambitions with trajectories and milestones that align with NHS operational plan submissions and pay due regard to the ambitions of the NHS Long Term Plan, as appropriate.
- Digital/data: SSteps to increase digital maturity and ensure a core level of infrastructure, digitisation and skills. These actions should contribute to meeting the ambition of a digitised, interoperable and connected health and care system as a key enabler to deliver more effective, integrated care. This could include reducing digital inequity and inequalities and supporting net zero objectives.
- Estates: Steps to create stronger, greener, smarter, better, fairer health and care infrastructure together with efficient use of resources and capital to deliver them. This should align with and be incorporated within forthcoming ICS infrastructure strategies.
- Procurement/supply chain: Plans to deliver procurement to maximise efficiency and ensure aggregation of spend, demonstrating delivery of best value. This could include governance and development of supporting technology and data infrastructure to align or ensure interoperability with procurement systems throughout the ICS.
- Population health management: The approach to supporting implementation of more preventative and personalised care models driven through data and analytical techniques such as population segmentation and financial demand modelling. This could include: developing approaches to better understand and anticipate population needs and outcomes (including health inequalities); using population health management approaches to understand future demand and financial risk; support redesign of integrated service models based on the needs of different groups; and putting in place the underpinning infrastructure and capability to support these approaches.
- System development: How the system organises itself and develops to support delivery. This could include: governance; role of place; role of provider collaboratives; clinical and care professional leadership; and leadership and system organisational development.
- Supporting wider social and economic development: How the ICB and NHS providers will support the development and delivery of local strategies to influence the social, environmental and economic factors that impact on health and wellbeing. This could include their role as strategic partners to local authorities and others within their system, as well as their direct contribution as planners, commissioners and providers of health services and as ‘anchor institutions’ within their communities.

