Labour ward co-ordinators
Who are labour ward co-ordinators?
Labour ward co-ordinators (LWCs) are a group of midwifery leaders who are passionate about and committed to leading maternity teams, to ensure the highest quality care is delivered for women, birthing people, and babies.
They are skilled practitioners who use their in-depth knowledge and intrapartum experience to role-model great leadership and develop others, including learners. They work with integrity, creating psychologically safe environments in which the maternity team feel safe, respected, cared for and able to learn. They aspire to always deliver a consistent and compassionate organisational culture, building and sustaining professional relationships with all members of the team.
By being supernumerary they maintain an overview of the service during their shift. They allocate resources to match the needs of the individual woman and baby. They critically record, appraise, and evaluate maternity safety data via systems such as the Maternity Dashboard and the Intrapartum Forum to consistently lead and improve quality and safety.
The labour ward co-ordinators framework
Why a framework is needed
Labour ward co-ordinators (LWCs) are integral in setting the culture and leading safety standards within the birthing environment and for the wider maternity team. To date, this group of midwifery leaders has not had a recognised pathway of development; as recommended in the Workforce planning and sustainability immediate and essential actions (IEAs) (Ockenden, 2022), a nationally recognised LWC development and educational framework is required.
While the LWC role is like other advanced and enhanced practitioner roles in some ways, it is unique in having a wide remit that incorporates leadership, clinical practice, and operational management.
The Framework is therefore designed to reflect this special nature of the LWC role; and it can be used as ongoing career development for midwives and other groups of staff more generally. This framework should be considered as part of the completion of the Maternity self-assessment tool (see Appendix 7).
How the framework was developed
The framework is informed and designed using a national, collaborative, multi-professional approach. This enabled input from service users and representatives across the maternity system. The process included the following:
- A systematic literature review of current evidence.
- A cross-sectional survey representing 728 members of neonatal, maternity teams, student midwives and educators across England.
- Focus groups conducted with LWCs, maternity improvement advisors (MIAs), midwifery learners, heads and directors of midwifery, service users and professional midwifery advocates (PMAs).
- A matrix was constructed based on the thematic analysis and was cross-checked with other relevant frameworks.
- Live webinars with maternity teams in England were held to develop and refine the required standards for each domain in the framework.
Who the framework is for
This framework provides LWCs – and midwives aspiring to the role – with a pathway of continuous development and supports the workforce to develop their skills and proficiencies to provide high-quality care. The framework also provides the opportunity for senior educators, neonatal and maternity leaders to assess and evaluate the development needs of their midwifery workforce.
Individual and service mapping tools can be found in appendices 5 and 6 respectively.
Professional registration and regulation
LWCs (and those aspiring to the role) remain subject to the registration requirements, and so must continue to meet:
- NMC Standards of Proficiency for Midwives (NMC 2019)
- The Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC 2018)
- regulatory body revalidation requirements.
It is expected that all LWCs will acquire the knowledge, skills, and behaviours to meet all the proficiencies across the framework. LWCs will demonstrate leadership in a range of clinical experiences and act as a credible support for other members of the maternity team to practice safely.
Role descriptors should reflect the level of skills and experience and not be task focused. An example role descriptor can be found in Appendix 1.
Development plans should include time for restorative clinical supervision (A-EQUIP, NHS England 2017) and be representative of the proficiencies stated in the framework.
Organisational readiness
The LWC development framework readiness checklist (see Appendix 3) has been developed to help directors and heads of midwifery and other senior maternity leaders, to assess, implement and evaluate the framework.
Organisations should rate their readiness on a scale of 1 to 4 for each domain: where 1 signifies there is no evidence; and 4 signifies that the factor is fully embedded within the organisational infrastructure and governance.
Appendix 4 provides a list of some key questions to help shape an evidence-based business case to address the areas identified for improvement.
Strengths-based profiling
Strengths-based profiling enables the identification of character strengths using a person-centred approach. This supports an individual to be more aware of their personal strengths and promotes psychological wellbeing. Strengths-based profiling enables the right work environment, the right team, and the right manager to bring out an individual’s strengths, helping them to thrive.
Research conducted so far indicates that people who are in a job that fits their strengths are happier, more engaged, less stressed, more successful and are more effective at their jobs. A strengths-based profile (Bibb, Hogg and Whitaker, 2023) may also include those strengths you get from your professional and social networks. Given the high-pressure of nature birthing environments, being connected to networks is important for LWCs.
Equality, diversity and inclusion
Every member of staff across the NHS has a responsibility to ensure that equality, diversity and inclusion (EDI) is part of their everyday working practice. EDI is key to the delivery of safe, high-quality care for women and babies, as well as staff feeling valued and respected, as outlined in the NHS equality, diversity and inclusion improvement plan (NHS, 2023). EDI is the golden thread that runs throughout this framework.
Governance
The framework will only be as successful as the other parts of the system in which it will operate (see Appendix 2). The role of senior maternity safety champions and neonatal leaders (QUADs) within trusts will set the direction around organisational cultures.
The trust’s quality assurance and governance processes, as well as the local quality and safety forums led by the local maternity and neonatal system (LMNS) and integrated care boards (ICBs), will ensure that LWCs have quality training, supervision, and support to perform to the best of their abilities.
As part of the whole-system commitment to support LWCs, trusts and systems must work together to ensure that their supernumerary status – as defined in the NHS Resolution CNST Maternity incentive scheme safety action 5 (having no caseload of their own during their shift”) – is always maintained (NHS Resolution).
The domains of the framework
The learning outcomes for this framework are structured around six domains (see figure 1 below) and include the necessary technical and non-technical requirements required to perform the role of a LWC to a high standard. The standards of proficiencies for each domain can be found in the next section.
Technical domain requirements:
- Core proficiencies.
Non-technical domain requirements:
- Leadership
- Knowledge
- Communication
- Quality, governance, and safe service
- Operational management.
Figure 1: LWC framework domains
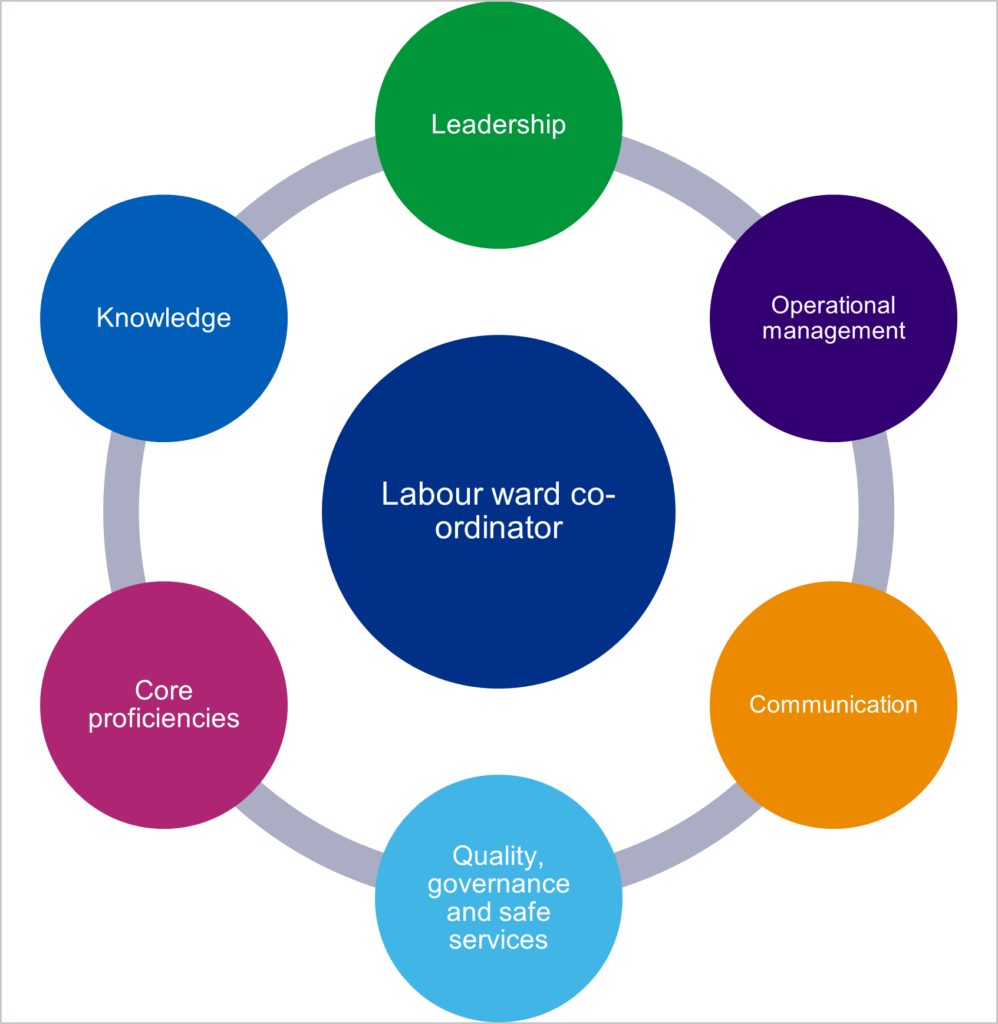
Labour ward co-ordinator
- Leadership
- Operational management
- Communication
- Quality, governance and safe services
- Core proficiencies
- Knowledge
Aims
The framework provides a nationally recognised set of standards and a development process which meets the requirement of the Workforce planning and sustainability IEA (Ockenden, 2022), to improve care, safety, culture, and leadership in maternity services. It aims to enhance the existing knowledge and skills of current LWCs and those aspiring to the role.
How to use the framework
The framework can be implemented at both an individual and organisational level. A set of initial self-assessments (see Appendix 6) should be completed, which will assist with the identification of gaps in knowledge and skill across the domains.
A resource toolkit (see Appendix 7) gives examples of resources that can assist LWCs to address any gaps in knowledge across the domains.
We recognise and respect that there are various ways to gain and develop the requirements within the domains. However, this document outlines clear routes by which evidence of achievement of capabilities for LWCs can be provided, as set out in the framework. This could be by way of:
- mapping previous experience, knowledge, and skills, against the framework
- completing a credit bearing level 6 or level 7 module or course provided by higher education institutes (HEIs), which meet part or all of the framework
- undertaking non-credit-bearing training which meets part of the framework
- developing a portfolio of evidence of the requirements of the framework to support recognition of prior learning (RPL).
It is recommended that LWCs are provided with mentors or coaches and networks to support their development as they acquire the necessary proficiencies.
For LWCs to meet the core proficiencies and standards of the role, they must work in partnership with their organisation. To obtain the most benefit from this framework, it is essential that LWCs, as leaders of maternity services, champion their continued development.
For this reason, the use of the term ‘your’ in some core proficiencies and standards is to reinforce the responsibility of LWCs to ensure their knowledge and skills are current and that their development is sustained over the long-term.
Competencies and standards
The following competencies and standards reflect what is expected of the LWC across each of the six domains:
Domain 1: Clinical, technical and digital skills
Midwives working as a labour ward co-ordinator will be able to:
1. Antenatal, intrapartum and postnatal core proficiencies
1.1 Demonstrate advanced skills in areas such as, but not limited to: foetal surveillance; maternal care pathways; maternal and neonatal life support and assessment; management of clinical risk and escalation.
1.2 Draw upon experience and evidence-based skills to inform assessments to provide safe care.
1.3 Support and lead the team in complex and challenging clinical situations in the birthing environment.
1.4 Use leadership skills to direct the team in the provision of safe care, informed by clinical information and evidence.
2. Digital skills
2.1 Apply with confidence, and support others to use digital skills to ensure safe, timely and effective provision of care.
2.2 Critically examine patient records to identify risks that could impact care and support the team to undertake continual holistic risk assessments.
2.3 Retrieve information from digital systems such as the Maternity Dashboard, to provide safe care, and for audit purposes.
2.4 Maximise patient safety using digital skills to update and maintain patient records in a precise and timely manner in accordance with legal requirements.
2.5 Ensure the GDPR legislation is applied when patient records are accessed.
3. Technical skills
3.1 Use technical skills to operate, maintain and escalate faults in medical devices needed to provide safe and effective care.
3.2 Lead/support the team to identify appropriate local medical devices to support safe practice.
Domain 2: Leadership
Midwives working as a labour ward co-ordinator will be able to:
1. Critically reflect on own leadership style and how this impacts on the safety culture and performance of the multidisciplinary team (MDT)
1.1 Role model behaviours that are consistent with the NMC values and principles expected of a midwifery leader during all interactions with the MDT.
1.2 Recognise own values and principles and acknowledge how these may differ from others in the MDT.
1.3 Identify how conscious and unconscious biases and emotions can affect your judgement and management of behaviours.
1.4 Actively seek feedback from a variety of sources including service users, on leadership style and behaviours.
1.5 Analyses own professional conduct, including civility, and its impact on the maternity team.
1.6 Evaluate the implications of not safeguarding the supernumerary status of the LWC and escalate when this becomes a risk.
2. Evaluate the impact of your behaviours as a leader on the experience and wellbeing of colleagues
2.1 Develop a critical awareness of your personal impact on staff.
2.2 Actively seek out, monitor, and evaluate feedback from staff.
2.3 Proactively reflect and act upon nonverbal signs that the team dynamics are affecting wellbeing and safety.
2.4 Critically evaluate your fitness to practice and be present at work.
2.5 Advocate and promote a culture which rewards positive behaviour.
3. Create a culture where psychological safety and quality improvement is achieved and maintained in a well led maternity service
3.1 Foster collaboration to enable the team to engage in decision-making.
3.2 Identify solutions and constructively challenge where required.
3.3 Ensure the team is consistently focused on the delivery of safe services and quality improvement.
3.4 Create a psychologically safe environment where team members are encouraged to raise concerns and share learning.
3.5 Facilitate a working environment where behaviours such as mutual respect, compassionate care and attention to detail are reinforced at every opportunity.
3.6 Manage hot debriefs immediately after an emergency, ensuring any identified safety actions are implemented and escalated in a timely manner.
4. Evaluate the impact of your behaviours as a leader on service user outcomes
4.1 Critically lead reflection on the language used to communicate with service users.
4.2 Ensure all service users are treated with dignity, care, compassion, and respect and acknowledge their different perspectives.
4.3 Identify and act when behaviour does not align with, or undermines the principles of equality, diversity and civility.
4.4 Actively seek user feedback regarding the impact of behaviour.
5. Role model and foster a culture of continuous learning in others
5.1 Be a role model and support the MDT and learners through career conversations and development opportunities.
5.2 Coach and mentor members of the team, particularly those who lack confidence to seek out development opportunities.
5.3 Positively promote the role of the LWC and inspire others.
5.4 Lead learning from incidents, patient feedback, live drills, and examples of good clinical practice to develop confidence and capabilities of the MDT.
6. Lead the resolution of challenging conversations with compassion, integrity, and confidence
6.1 Apply conflict resolution skills to de-escalate and resolve challenging conversations.
6.2 Take action to manage staff performance and behaviour and escalate if needed.
6.3 Advocate for the use of conflict resolution styles and promote models of professionalism that help to break the pattern of poor behaviours.
6.4 Critically evaluate own role in creating and mitigating conflict.
6.5 Lead compassionately to find solutions to resolve distress for staff and service users.
Domain 3: Knowledge
Midwives working as a labour ward co-ordinator will be able to:
1.1 Demonstrate knowledge of how local and regional maternity and neonatal systems operate
1.2 Assess knowledge and gain understanding of how operational delivery networks (ODNs), integrated care systems (ICSs), LMNSs and regional teams support intrapartum and neonatal care.
1.3 Understand the flow of movement outside the organisation which may occur during escalation.
1.4 Articulate the relationship between the different organisations that make up the LMNSs.
1.5 Critically evaluate knowledge of community and antenatal services outside your unit and how they interact with each other.
2. Use evidence-based knowledge to critique the technical skills of all team members and manage any gaps that could impact safe service delivery
2.1 Critically assess the clinical, digital, and technical skills required by the MDT to ensure safe service delivery.
2.2 Take a systematic approach to identify gaps in the clinical and technical skills of the team.
2.3 Effectively apply knowledge and act to manage any gaps to support the provision of a safe service.
2.4 Continuously monitor and evaluate the outcomes of any interventions to manage identified gaps in clinical, digital or technical skills of the MDT including learners.
3. Create a learning culture within the birthing environment so that members of the MDT can address gaps in practice that impacts safe service delivery
3.1 Facilitate time for reflection and learning to encourage and support others to make realistic self-assessments of their knowledge and skills, so that the right person is in the right place at the right time to deliver safe and effective care.
3.2 Advocate for the continuous monitoring and evaluation of the quality of care provided within the birthing environment and the wider maternity service.
4. Appraise and implement the principles of human factors when leading the MDT
4.1 Understand the key principles of human factors and their impact on service delivery.
4.2 Critically assess own needs and those of the team for training in human factors and take action to resolve this.
4.3 Critically lead and apply the principles of human factors to achieve quality improvement.
4.4 Critically evaluate the impact of human factors on team performance, quality, and safe service delivery.
5. Exercise professional judgement and clinical credibility gained from a range of experience obtained within the birthing environment
5.1 Demonstrate a critical understanding of the broadened level of responsibility and autonomy when caring for users with additional needs that may be complex, high risk, uncertain, and with incomplete information.
5.2 Act on professional judgement about when to escalate, demonstrating critical reflection on own practice, self-awareness, emotional intelligence, and openness to change.
6. Evaluate their knowledge of policies, procedures and processes which influence decision-making and impact safe service delivery
6.1 Exercise professional judgement to identify own role in implementing strategy, policies, guidelines, and processes within your sphere of practice to keep the unit safe.
6.2 Work collaboratively with the team and line manager to ensure that policies and strategies support service users, their families, and staff when making decisions.
6.3 Critically review policies, processes, and guidelines to contribute to and embed new learning to support quality improvement.
6.4 Deploy expert knowledge to ensure that the team works in alignment with agreed strategies, policies, guidelines and processes.
6.5 Work in partnership with women whose personalised care plans sit outside of agreed guidelines, supporting MDT to facilitate this.
7. Critically reflect on individual preparedness for the demands of the role of and your impact on others
7.1 Formulate your own personal development plan reflecting feedback from others.
7.2 Evaluate your knowledge and skills against the standards of the LWC framework.
7.3 Proactively seek out opportunities to improve own knowledge and skills to remain effective in the role of LWC.
7.4 Demonstrate knowledge of current national guidelines, key reports and objectives relating to the maternity landscape
7.5 Critically apply learning from national reports to your area of practice, including benchmarking activities.
7.6 Proactively identify areas for improvement within your sphere of practice informed by knowledge of national reports and strategies.
7.7 Actively promote learning from national guidelines, reports, and objectives.
Domain 4: Communication
Midwives working as a labour ward co-ordinator will be able to:
1. Prioritise confident, communication skills as a leader during an emergency, while maintaining a calm approach
1.1 Clearly articulate to the MDT their roles in an emergency.
1.2 Provide the optimum level of calm and clear communication required during an emergency to support a positive outcome.
1.3 Demonstrate empathy and compassion while communicating to the MDT following an emergency.
1.4 Use hot debriefs to create opportunities for immediate learning from emergencies.
2. Be approachable, trustworthy, and professional to foster effective and kind communication with the team and service users
2.1 Role model the values of the organisation to reflect kindness, trustworthiness, and approachability.
2.2 Use communication styles which are compatible with civil and professional behaviours.
3. Use emotional intelligence to recognise and manage with compassion non-verbal signs of distress in the team, yourself, and service users
3.1 Proactively develop positive working relationships with members of the MDT.
3.2 Demonstrate recognition and ensure appropriate action of non-verbal signals that are impacting the MDT.
3.3 Actively seek feedback to maintain psychological safety.
3.4 Proactively initiate interventions to develop and maintain a psychologically safe environment.
3.5 Critically evaluate own response to non-verbal signs of stress within the team.
4. Compose high quality constructive feedback and use a kind and supportive manner
4.1 Actively promote the workplace as a learning environment and encourage the MDT to learn from sources of recognised good practice.
4.2 Actively lead the use of quality Improvement principles to positively progress workplace culture.
4.3 Facilitate constructive feedback to enable others to develop and apply their knowledge and skills.
4.4 Support individuals who are focusing on specific learning to improve their practice.
4.5 Be receptive to receiving and responding to constructive feedback from colleagues and service users.
5. Develop and maintain highly effective communication with people on complex issues
5.1 Identify the professionals within your network with whom highly effective communication is essential.
5.2 Proactively utilise different methods of communication to maintain effective working relationships.
5.3 Ensure communication is clear and consistent with the recipient’s understanding, culture, background, and preferred methods of communication.
5.4 Anticipate barriers to communication and facilitate actions to find solutions to these.
5.5 Take action to achieve an appropriate level of response to facilitate safe and effective care.
6. Exhibit highly effective, inclusive, and timely communication skills with all members of the MDT
6.1 Actively communicate in ways that demonstrate inclusion, equality, and values diversity.
6.2 Communicate in a manner that is consistent with legislation, policy, and procedures.
6.3 Manage barriers to communication by modifying personal style.
6.4 Proactively monitor the effectiveness of own communication style.
6.5 Initiate clear communication to enable decisions to be made in a timely manner.
7. Use language and resources to enable effective communication with service users
7.1 Appropriate involvement of professional interpreters to ensure safe and personalised care.
7.2 Make resources available to reduce barriers to communication for vulnerable service users.
7.3 Advocate for vulnerable service users.
7.4 Actively engage in clear communication with specialist teams who care for vulnerable service users.
Domain 5: Quality, governance and safe service
Midwives working as a labour ward co-ordinator will be able to:
1. Critically appraise and implement quality improvement processes and evaluate the outcomes
1.1 Understand the underlying principles, and access references for, quality improvement processes, such as PDSA cycle or Lean Six Sigma.
1.2 Implement and lead changes based on quality improvement and change management processes.
1.3 Critically evaluate the impact of the improvement or change.
1.4 Continually monitor change using quality improvement processes.
2. Initiate and maintain a culture of continuous quality improvement across maternity services, to improve outcomes and experiences for all women and babies in response to health inequalities
2.1 Use local data, for example from the Maternity Dashboard and Intrapartum Forum, to identify risks and promote continuous service improvement.
2.2 Use audit to measure, appraise and interpret data on service users’ experiences and feedback.
2.3 Critically examine feedback from service users and/or their advocates and take personal action to lead improvements in quality and safety.
2.4 Work collaboratively with the MDT, service users and their advocates to design and implement solutions to improve service quality and safety.
3. Actively participate in and promote audit and research to improve quality and safety
3.1 Engage and encourage the MDT to participate in the local maternity audit programme.
3.2 Take a critical approach to identify gaps in the evidence base and its application to improve the quality and safety of care.
3.3 Disseminate local and national learning identified through research findings, national maternity reports such as Health Services Safety Investigations Body (HSSIB), Early Notification Scheme, and Perinatal Mortality Reporting Tool (PMRT).
3.4 Lead quality improvement projects to provide safe and personalised care that reflect the findings of local and national reports at 3.3.
Domain 6: Operational management
Midwives working as a labour ward co-ordinator will be able to:
1. Determine and evaluate available resources, to deliver safe and effective care during each shift
1.1 Take personal responsibility to secure and maintain own supernumerary status.
1.2 Take action to develop personal knowledge and skills relating to implementation of your local escalation plans.
1.3 Critically evaluate the risk of gaps in the quantity and quality of resources, staff, and equipment, in the birthing environment.
1.4 Accurately identify the appropriate type and level of resources required to deliver safe and effective maternity care.
1.5 Critically prioritising and adjusting resources to ensure right person, right time, right place, including when awaiting the continuity of carer midwife.
1.6 Manage oversight and assurance of equipment checks to ensure a safe and effective birthing environment.
1.7 Monitor and maintain agreed level of resources (staffing, equipment, and environment) to sustain a safe birthing environment.
2. Implement with confidence, and critically analyse, the local escalation plan
2.1 Take action to develop personal knowledge and skills relating to implementation of your local escalation plans.
2.2 Critically assess your role as an LWC in the escalation process including out of hours responsibilities.
2.3 Actively seek opportunities to be involved in, and gain confidence with, the operationalisation of the local escalation plan, for example, shadowing.
2.4 Proactively use local networks to seek help, support and learning when utilising your local escalation plan.
2.5 Critically evaluate the effectiveness of the local escalation plan and take personal action to collaborate to make improvements as needed.
3. Apply health, safety and security legislation, policies and processes which align to the birthing environment
3.1 Take responsibility to critically identify and assess the potential risks and hazards within the birthing environment.
3.2 Take personal action to record and report actual or potential problems which may compromise the health and safety of staff and service users.
3.3 Manage and mitigate risks, actual or potential by ensuring staff comply with health and safety policy and procedures.
3.4 Proactively identify processes and systems that promote your own and others health, safety, and security.
4. Actively promote and implement local equality, diversity, inclusion and social justice (EDISJ) legislation, policies, and processes
4.1 Know the legislation and your personal, professional responsibility in promoting a kind and inclusive EDISJ culture.
4.2 Actively challenge individual and organisational discrimination.
4.3 Actively facilitate equitable access to development opportunities.
5 Understand the maternity budget and the implications of spending decisions
5.1 Understand the financial management required to resource the birthing environment.
5.2 Seek opportunities to learn about NHS resource allocation, principles, and practice.
5.3 Provide evidence to influence spending decisions regarding the allocation of resources necessary to sustain a safe maternity service within the birthing environment.
6. Manage and ensure responsible and sustainable use of equipment and single-use items
6.1 Critically review current service delivery and identify opportunities to introduce change for more efficient and effective working.
6.2 Identify and report areas of potential waste to senior colleagues within the trust.
Appendix 1: Example of a role descriptor
Labour ward co-ordinators:
- must demonstrate a high level of clinical expertise and sound knowledge of all birthing environments; when supporting others, they will ensure evidence-based practice is upheld to help staff and service users to inform their decision making
- lead with confidence and act with compassion for service users and all members of their team; they act as champions for, and protect a culture of, an inclusive and psychologically safe birthing environment
- will take responsibility for their own professional development to be the best they can be
- communicate calmly, clearly and kindly, including during challenging situations; they can build and maintain trusted and respectful relationships with all colleagues across the MDT
- strive to consistently deliver high quality, safe care by adopting the principles of quality improvement and advocating for a continuous learning environment to improve maternity services; this incorporates learning from intrapartum incidents, and staff/service user feedback
- can manage resources to ensure safe staffing, adequate skill mix and appropriate equipment are available to match the needs of the service; they can escalate appropriately and with confidence; have an awareness of, and take responsibility for departmental spending; and ensure compliance with birthing environment policies and processes.
Appendix 2: Suggested governance of labour ward co-ordinator framework
Figure 2: LWC suggested governance
Appendix 3: Organisational readiness tool*
* Adapted from Advanced practice in midwifery implementation guide (HEE, 2023)
| Factors suggesting readiness to implement LWC framework | Examples of evidence | Extent to which these are in place | Action plan |
|---|---|---|---|
|
The LWC must have supernumerary status to ensure there is an oversight of all birth activity within the service, and structures and processes are in place to sustain this. |
Rota and safe staffing documentation, regular feedback from LWCs |
|
|
|
We have surveyed our staff to establish current competency level within LWC workforce and have mapped these against the Framework to establish where development is needed for develop LWCs |
Workforce reviews, local LWC database, mapping tool |
|
|
|
We have standardised, equitable and transparent processes for recruitment, and selection to LWC roles. |
LWC strategy/governance document |
|
|
|
The title of LWC is consistently used and the framework is actively promoted by DOMS/HOMS/LMNS. |
Communication and engagement planned, support forum for LWCs |
|
|
|
We have opportunities for aspiring LWCs to develop capability across the framework by offering; placements to shadow, individual development plans and career conversations |
Examples of rotations or placements, communication, minutes of meetings |
|
|
|
There is a planned approach to supporting those seeking LWC status via portfolio or credentialling |
Individual learning plans, business cases |
|
|
|
There is clear support, governance, and commitment for LWCs role at board level. |
Named executive sponsor eg, head of directorate or safety champion |
|
|
|
There is an understanding of LWCs role across maternity systems and the value placed on these roles |
Sharing stories workshop to highlight complexity and emotional resilience needed for the role. Highlighting the importance of teamwork to achieve a safe culture |
|
|
|
We have discussed our plans with our ICB/LMNS and HEIs and have designed a business case for investment in LWCs. |
Communications, minutes of meetings, business case, workforce plans |
|
|
Key:
- No evidence of this.
- Limited evidence in place.
- Evidence is in place but not embedded across the whole organisation.
- Fully embedded within the organisation.
Please see the full PDF version of this document for a printable version of the above table.
Appendix 4: Key indicators for organisations to evidence a robust business case
Key indicators that should be evidenced in a robust business case:
- What outcomes are expected from an LWC?
- When will these outcomes be achieved and how will these be measured pre and post implementation of the LWC Framework?
- What risks and unintended consequences might there be to the introduction of the LWC Framework and how may they be mitigated?
- What resources and support are required for development of LWCs (clearly include any work based and educational supervision requirements) and succession planning?
- Is the workforce optimised to ensure implementation of the LWC Framework and to make certain clinical and financial benefits are maximised?
- How will on-going competence and capability of the LWC be reviewed and enabled?
- What reporting and line management structure will be in place?
- What processes will identify gaps in performance and/ or shortfalls in implementation and how will these be addressed?
- Has a quality assurance model been considered to measure gaps and/or shortfalls eg, the NHS Resolution CNST maternity incentive scheme safety action 5, CQC’s five key lines of enquiry which will support inspection?
- Costing and risk statement.
Appendix 5: Maternity unit LWC workforce assessment
| Our ambition to implement the framework to achieve outstanding LWCs: | On a score of 1-10 where are we now? | On a score of 1-10 where do we need to be in 12 months? |
|---|---|---|
| Clinical, technical and digital skills |
|
|
|
Leadership |
|
|
|
Knowledge |
|
|
|
Communication |
|
|
| Quality, governance and safe service |
|
|
| Operational management |
|
|
| What is working well? (Things we can build on to make our ambitions a reality) | Even better if …… (What has prevented us or may prevent us from achieving our ambitions?) |
|
|
|
Signed and agreed by…………………………………………………
Please see the full PDF version of this document for a printable version of the above table.
Appendix 6: Individual LWC self-assessment
| My ambition to implement the framework to become an outstanding labour ward co-ordinator: | On a score of 1-10 where am I now? | On a score of 1-10 where do I need to be in 12 months? |
|---|---|---|
| Clinical, technical and digital skills |
|
|
| Leadership |
|
|
| Knowledge |
|
|
| Communication |
|
|
| Quality, governance and safe service |
|
|
| Operational management |
|
|
| What is working well? (Things I can build on to make my ambitions a reality) | Even better if …… (What has prevented me or may prevent me from achieving our ambitions?) |
|
|
|
Signed and agreed by …………………………………………………
Please see the full PDF version of this document for a printable version of the above table.
Career conversations are a valuable way to identify current and future development needs. These conversations can be utilised during appraisals to design a development plan: Review and career conversations – Leadership Academy
Self-assessment tools can help manage own learning by allowing reflection on which areas for personal and professional development is required: CLCF Self Assessment_Layout 1 (leadershipacademy.nhs.uk)
If you would like further access to career tools, please register via this link for the Leadership academy career portal: Self-assessment tool – Leadership Academy
Appendix 7: Resource toolkits
Core proficiencies
- NMC proficiencies: standards-of-proficiency-for-midwives.pdf (nmc.org.uk)
- Training Packages | PROMPT Maternity Foundation
- Advanced Life Support in Obstetrics (ALSO) | AAFP
- NLS (Newborn Life Support) Course | Resuscitation Council UK
- Advanced Clinical Practice (ACP): capability framework
- Core competency framework for midwives
Leadership
- NHS Leadership Academy (NHSLA): LeadershipModel-colour.pdf
- NHS England » NHS Workforce Race Equality Standard
- Compassion in practice: cip-yr-3.pdf (england.nhs.uk)
- Michael West on compassionate and inclusive leadership | The King’s Fund
- Improving NHS culture | The King’s Fund
- Survey documents related to conducting the survey | NHS Staff Survey (nhsstaffsurveys.com)
- Review and career conversations – NHS Leadership Academy
- Leadership self-assessment tool – NHS Leadership Academy
- Podcast (RCNI) – What to do with uncivil behaviour
- NHS England » Three-year delivery plan for maternity and neonatal services
- Psychological safety – Amy Edmondson (YouTube)
- NHSLA: Clinical leadership competency framework (CLCF) – Self Assessment Layout 1
- Brene Brown: The power of vulnerability (YouTube)
Knowledge
- FutureNHS platform – information and shared learning hub
- Maternal medicine network national service specification
- Newly qualified midwives framework – national preceptorship framework
- Digital Maternity Leaders training course – digital leadership development
- NICE guidance – national maternity guidelines
- Maternity services dataset (MSDS) guidance hub
- My first labour ward co-ordinators post…by Gabby | Personal story of a labour ward co-ordinator (HEE)
- The Phillips Ives Nursing and Midwifery Review – digital health practice (YouTube)
Communication
- NHSLA: How to have confident conversations with members of your team (SE confident conversations toolkit)
- NHS Employers: VBR behaviour framework
- How to plan personalised care: Personalised care and support planning guidance
- Equity and Equality guidance for LMNSs
- Learning after review handbook (NHS England)
- SHARE: A hot debrief tool to use following incidents (NHS England)
- NHS England » Towards a unified vision of nursing and midwifery documentation
- Talking with women: RCM rebirth report
- Civility Saves Lives: The impacts of civility at work
Appendix 8: Suggested reading
- Arnold, R. et al (2023) ‘I might have cried in the changing room, but I still went to work’. Maternity staff balancing roles, responsibilities, and emotions of work and home during COVID-19: An appreciative inquiry – ScienceDirect
- Bunford, DJ, (2019) What makes an excellent Delivery Suite Co-ordinator? Views of the Multidisciplinary Team, a constructivist grounded theory study. University of Teesside.
- Edmondson, A (2023), Right Kind of Wrong: Why Learning to Fail Can Teach Us to Thrive. Cornerstone Press
- House of Commons Woman and Equality Committee, (2023) Black Maternal Health, Third Report of Session 2022–23 https://publications.parliament.uk/pa/cm5803/cmselect/cmwomeq/94/report.html
- Lencioni, PM. (2002) The Five Dysfunctions of a Team: A Leadership Fable. John Wiley & Sons
- Liberati, EG et al (2020) Seven features of safety in maternity units: a framework based on multisite ethnography and stakeholder consultation. British Medical Journal. https://qualitysafety.bmj.com/content/30/6/444
- National Perinatal Epidemiology Unit, (2018) Perinatal Mortality Review Tool https://www.npeu.ox.ac.uk/mbrrace-uk/pmrt
- NHS England (2022) Combatting racial discrimination against minority ethnic nurses, midwives and nursing associates https://www.england.nhs.uk/long-read/combatting-racial-discrimination-against-minority-ethnic-nurses-midwives-and-nursing-associates
- NHS England Equality Objectives Programme; Specific Equality Duties (2023) https://www.england.nhs.uk/publication/specific-equality-duties-reports
- NHS England (2023) NHS equality, diversity, and inclusion improvement plan NHS England (2017) Advocating for Education and Quality Improvement (A-EQUIP) Non-Statutory Model of Midwifery Supervision. NHS England » A-EQUIP a model of clinical midwifery supervision
- NHS England (2023) NHS Long-term Workforce Plan NHS England » NHS Long Term Workforce Plan
- NHS Institute for Innovation and Improvement (2017) Lean Six Sigma: some basic concepts https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Lean-Six-Sigma-Some-Basic-Concepts.pdf
- NHS Workforce Race Equality Standard (2022) https://www.england.nhs.uk/publication/nhs-workforce-race-equality-standard-2022
- Schein EH. (1985) Career Anchors: Discovering Your Real Values Workbook. John Wiley & Sons
- Schein, EH. (2023) Career Anchors Reimagined: Finding Direction and Opportunity in the Changing World of Work. Jossey-Bass Leadership Series
Glossary
- Accountable: To be responsible and answerable to your employer and yourself for the decisions you make and for your actions or omissions.
- A-EQUIP: An acronym for Advocating for Education and Quality Improvement
- Advocacy: Doing your best for individuals by speaking on behalf of another.
- Aspiring: Having Ambition towards a certain goal.
- Board: Senior executive directors of a trust or ICS who make decisions about funding and take responsibility for governance of a trust or maternity system.
- Maternity incentive scheme: A programme of maternity safety actions which promote commitment and action to reduce risk, and if complete, reward trusts financially.
- Competence: The knowledge, skills, attitudes, and ability to practise safely and effectively.
- Complexity: The presence of one or more clinical, psychological, social, or medical complications or further needs that require input and collaborative care by the multidisciplinary and multi-agency team.
- Consent: Explaining what you intend to do with/ to someone and listening carefully to what they say about it. For consent to be valid, it must be current and given voluntarily by an appropriately informed person who has the capacity to consent to the intervention in question. Agreement where the person does not know what the intervention entails is not ‘consent.’
- Consultant midwife: Can be an ally or mentor to the LWC.
- Continuity of carer: A continuous relationship with a named midwife and small team, who provide maternity care for the continuum of the maternity journey.
- Continuous development: A process by which an individual or organisation regularly review their core values and need for improvement.
- Director of midwifery (DOM): Senior Midwifery leader who is professionally accountable for women’s health services.
- Early notification scheme (ENS): Investigates serious brain injuries that happen to children at birth.
- Equality, diversity, inclusion and social justice (EDISJ): Refers to a concept of fairness, where individuals from diverse backgrounds are accepted and welcomed and their unique differences are respected. Social justice is a recognition the systems perpetuate the power and influence of select groups and require conscious effort to change this.
- GDPR: A European Union regulation on Information privacy in the European Union and the European Economic Area.
- Heads of midwifery (HOMs): Senior midwifery leaders who take responsibility for a maternity service within a trust.
- Health Services, Safety Investigations Body (HSSIB): A non-departmental public body that conducts patient safety investigations in England.
- HEI: Highter Education Institute
- Human factors: Human factors refer to environmental, organisational and job factors, and human and individual characteristics, which influence behaviour at work in a way which can affect health and safety.
- Integrated care system (ICS): A partnership of organisations with collaborate to deliver health and care services to improve the lives of their local community.
- Immediate and essential action (IEA): Mandated actions from the Ockenden Inquiry (2022)
- Labour ward co-ordinators (LWCs): Specialist midwifery leaders, who co-ordinate the clinical workload and activity in birthing environments while maintaining situational awareness of other parts of the service.
- Local maternity and neonatal systems (LMNSs): A team of individuals who work strategically across the locality to provide support and steer to maternity and neonatal organisations.
- Mapping tool: A process that can be used to help a team visualise and understand where the problems are and identify opportunities for improvement.
- Maternity journey: The individual’s experience of care and support pertaining to childbearing over time. May be current or historical relating to aspects of the childbearing process from pre-pregnancy, pregnancy, labour, birth, the immediate postpartum, and the early days and weeks of life.
- Maternity improvement advisors (MIAs): A team of professional, senior midwifery leaders who support Trusts to improve culture, safety, and outcomes.
- Mentoring: A work-based method of training using existing experienced staff to transfer their skills informally or semi-formally to learners.
- Multidisciplinary team (MDT): Practitioners providing care and support to individuals at all levels and areas of practice.
- Non-technical: Interpersonal skills such as communication and leadership. Also known as ‘soft skills’
- Nursing and Midwifery Council (NMC): Is the independent regulator for nurses and midwives in the UK, and nursing associates in England, who govern registration.
- Operational delivery network (ODN): A network of neonatal services providers.
- Operational management: The management of those functions that an organisation needs to run effectively daily.
- Organisational culture: Represents the shared ways of thinking, feeling, and behaving in healthcare organisations.
- Perinatal mortality review tool (PMRT): The tool supports standardised perinatal mortality reviews across the NHS.
- Practitioner: An appropriately qualified person in the practice of an occupation.
- Professional midwifery advocate (PMA): Is a title given to a midwife who has undergone additional training to deliver the A-EQUIP model.
- Proficiencies: Competence derived from training and practice.
- Psychological safety: Is a belief that an individual will not be punished or humiliated for speaking up with ideas, questions, concerns, or mistakes.
- Recognition of prior learning (RPL): A method to assess how previous learning or qualifications meet learning outcomes for a course or module.
- Role descriptors: Is an informative document detailing the scope, duties, tasks, responsibilities and working conditions related to a role in addition to their substantive job.
- Single delivery plan: Sets out how the NHS will make maternity and neonatal care safer, more personalised, and more equitable for women, babies, and families.
- Situational awareness: A critical that involves understanding what is happening around you and anticipating their potential consequences.
- Strengths-based profiling: A holistic approach to finding the best person for a role, by identifying their key strengths.
- Supernumerary status: Having no caseload of their own during their shift.
- Technical skills: Are the specialised knowledge and expertise required to perform specific tasks and use specific tools and programs in real world situations.
- Thematic analysis: Is the study of patterns to uncover meaning from qualitative data.
Acknowledgements
We would particularly like to thank our dedicated labour ward co-ordinator colleagues for their support during the development of this work.
A national working group collaborated to design this nationally recognised labour ward co-ordinators education and development framework, and their contributions were invaluable.
Representation from:
- regional teams
- the Workforce, Training and Education team, NHS England
- higher education institutions (HEIs)
- Royal College of Midwives (RCM)
- Nursing and Midwifery Council (NMC)
- student midwives
- service users
- maternity improvement advisors (MIAs)
- labour ward co-ordinators
- local maternity and neonatal systems (LMNS)
- integrated care boards (ICBs)
- obstetrics
- neonatologists
- anaesthesiologists.
Publication reference: PRN00730


