Publication reference: PR2103
Introduction
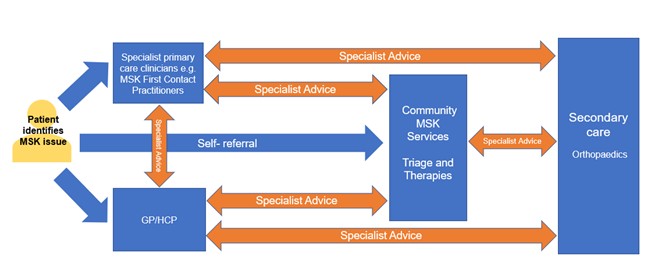
This guidance describes the benefits of referral optimisation in adult services managing musculoskeletal (MSK) conditions, focusing on the use of specialist advice to enable people to be seen by the right person, at the right time and in the right place.
Demand for the treatment of MSK conditions is increasing across the system and there is unwarranted variation in patient management and outcomes (Musculoskeletal health: a 5 year strategic framework for prevention across the lifecourse).
This guidance makes the case for change to sustain high quality care, manage risk and optimise capacity across primary, community and secondary care MSK services.
It recommends the use of specialist advice services to improve access, outcomes and experience for patients; and highlights the value of using the MSK expertise already well placed in primary care and community MSK services as defined in the Community MSK Improvement Framework, as well as having direct access to consultant orthopaedic surgeons in secondary care for those who need surgery or a discussion about their surgery.
This guidance was developed by the Outpatient Recovery and Transformation Programme (OPRT) and BestMSK Health Collaborative, with the involvement of key stakeholders, including:
- patients
- clinicians
- implementation managers
- an MSK subject matter expert from the Health Education England (HEE) National Workforce Transformation team
- relevant professional bodies such as:
- and organisations which represent the views and interests of people with lived experience, including:
- Arthritis and Musculoskeletal Alliance (ARMA)
- Versus Arthritis
- NHS England’s national lived experience group.
This guidance should be considered alongside the other resources available on the FutureNHS platform to support MSK referral optimisation.
National context
MSK conditions affect bones and joints in the axial and peripheral skeleton, cartilage, tendons, ligaments and muscles (collectively known as connective tissues). They range from minor injuries to long-term conditions; some are present from birth and some occur suddenly at any age, whereas others progress gradually and are more common in older age.
In the UK an estimated 20.3 million people are affected by MSK conditions, accounting for 21% of years of life lived with disability, and the demand on NHS services is increasing as the population ages (Versus Arthritis: The State of Musculoskeletal Health 2021).
MSK conditions now account for up to 30% of general practice consultations in England (NHS England » Musculoskeletal); and before the COVID-19 pandemic, orthopaedic referrals were increasing by 7–8% a year (GIRFT (2015) A national review of adult elective orthopaedic services in England) – in part because of changing demographics, but also inappropriate referral.
Around 2.7 million of the 7.6 million outpatient appointments for trauma and orthopaedic services in 2019/20 were first appointments and almost a third of patients were discharged after their first attendance (NHS Digital, Hospital Outpatient Activity 2019-20).
Most MSK conditions can be diagnosed and managed well in primary and community care with advice, appropriate analgesics and physical therapies. A few need timely referral to secondary care orthopaedic services to consider surgical intervention.
The pandemic has had an unprecedented impact on secondary care orthopaedic services and waiting times have increased significantly for most. New ways of working are needed to optimise demand, maximise capacity and mitigate risk.
As part of this we need to optimise the quality of referrals to consultant orthopaedic surgeons, making best use of specialist primary care clinicians, for example MSK first contact practitioners (FCPs), MSK specialist doctors, such as sport and exercise medicine (SEM) consultants and GPs with extended roles (GPwER), specialists from community MSK services delivering a triage function, eg MSK advanced practitioners (MSK APs), MSK consultant practitioners (MSK CPs), alongside and working closely with consultant orthopaedic surgeons.
Reducing community musculoskeletal waits and understanding how the broader primary and community workforce, eg pharmacists, pharmacy technicians, health and wellbeing coaches, social prescribing link workers and care co-ordinators, can support the management of MSK conditions also needs consideration.
The NHS Long Term Plan recognises that many patients could have a better experience by avoiding asking them to attend hospital unnecessarily. The 2023/24 priorities and operational planning guidance prioritises the reduction of outpatient follow up activity by 25% by March 2024 by working collaboratively to improve service delivery models.
Referral optimisation is an essential component for this and also a core recommendation in the BestMSK Health Collaborative High Impact Restoration Strategy.
By ensuring people with MSK orthopaedic conditions are seen in the right place by the right person first time, referral optimisation will also contribute to the NHS reducing its carbon footprint.
What is referral optimisation?
Referral optimisation is the improvement of system-wide pre-referral pathways to ensure that:
- Primary and community services have the support they need to diagnose, treat and support more patients closer to home, without the need for onward referral and thereby make best use of primary, community and secondary care capacity.
- For MSK orthopaedic management, this support may be delivered by MSK FCPs, MSK APs, MSK CPs and MSK specialist doctors within primary care and community MSK services working closely with consultant orthopaedic surgeons.
- Outpatient diagnostic pathways are efficient, ensuring that if a referral is required, specialist clinicians have the information they need, including all relevant investigations, to determine the correct treatment plan, one that minimises inconvenience for patients.
- For MSK orthopaedic management, this support may be delivered by MSK FCPs, MSK APs, MSK CPs and MSK specialist doctors within primary care and community MSK services working closely with consultant orthopaedic surgeons.
- People with long-term conditions are enabled to build their knowledge, skills and confidence, and provided with proactive, holistic and preventative self-management support from the wider primary and community workforce who manage MSK conditions, eg pharmacists, pharmacy technicians, health and wellbeing coaches, social prescribing link workers and care co-ordinators.
Referral optimisation can cover a wide range of interventions in MSK orthopaedic management, from providing specialist advice and strengthening primary care teams through to supporting the self-care of patients.
What is specialist advice?
Specialist advice is an umbrella term for a range of specialist-led models that can be provided in primary, community or secondary care settings.
They allow relevant clinical information to be shared, including patient preferences and values (elicited through a process of shared decision-making), so that:
- before or instead of referral the referring clinician can seek advice from a specialist, eg NHS e-RS (electronic referral service) advice and guidance (A&G) or telephone advice line
- where a referral has been made the specialist can review the clinical information and return the referral with guidance where appropriate, or where necessary direct the referral to the most appropriate clinician, clinic and/or diagnostic pathway first time, eg e-RS Referral Assessment Services (RAS), triage services.
Specialist advice may be provided by appropriately trained clinicians from both consultant and non-consultant commissioned services in primary, community and secondary care providers, interface or intermediate services, and referral management systems.
This gives those who see patients with MSK orthopaedic conditions in primary and community services the support they need to assess, diagnose and provide treatment options (in line with evidence-based interventions guidance and the patient’s preferences and values) and self-management support.
This enables care closer to home to improve patient experience and outcomes, and helps avoid unnecessary outpatient attendances.
Some level of specialist advice may already exist as part of the normal clinical journey. Formalising this clinical practice, where advice is often informally sought between clinicians, is important so that services can be appropriately resourced and factored into the wider planning of MSK activity; and can strengthen an integrated and multidisciplinary approach to care, especially where there may be diagnostic uncertainty.
Specialist advice has a key role in maximising primary and secondary care capacity, supporting recovery and the sustainability of MSK services.
It will aid clinical communication and decision-making early in a patient’s pathway, supporting equitable access to the right care, at the right time, in the right place. It should be the foundation of every system’s referral optimisation strategy.
Benefits of specialist advice in MSK orthopaedic management
Specialist advice is not a new concept in MSK orthopaedic management. Some level of specialist advice will exist in every system across England between primary care and secondary care orthopaedic services through the e-RS A&G platform.
However, use is variable and frequently bypasses the expert MSK specialist advice available in primary care and community MSK services (from MSK FCPs, MSK APs, MSK CPs and MSK specialist doctors).
There are therefore significant opportunities for all systems to optimise its use from within primary and community care:
- supporting timely access to specialist care outside hospital services where appropriate
- promoting both primary and secondary prevention of MSK conditions
- helping patients avoid unnecessary trips to hospital for low clinical value outpatient appointments
- reducing unnecessary demand on secondary care.
Specialist advice should not be used in all instances, particularly the management of emergency and certain urgent MSK conditions.
Serious pathology as a cause of MSK conditions is considered rare and needs to be managed either as an emergency or urgent onward referral as directed by local pathways, and as such should not be directed through specialist advice services.
Guidance on urgent and emergency musculoskeletal conditions requiring onward referral supports primary and community care practitioners in recognising serious pathology that requires emergency or urgent referral to secondary care.
Access to specialist advice across the MSK orthopaedic pathway can:
- improve the interface and clinical communication between primary, community and secondary care clinicians
- ensure equitable access and timely patient care is delivered in the most appropriate setting and by the right person
- improve patient experience and outcomes
- support management of more patients outside hospital
- strengthen shared decision-making and enhance personalised care
- provide opportunities for education and sharing of MSK specialist knowledge
- deliver efficiencies by ensuring appropriate diagnostics are requested, including those for secondary prevention
- deliver efficiencies by ensuring the right patients are referred from primary care
- reduce the environmental impact of services.
The reasons a clinician may wish to seek specialist advice in MSK orthopaedic management include:
- Diagnosis:
- early specialist opinion from MSK experts within primary care and community MSK services on patient management/treatment options
- identifying the most clinically appropriate MSK expert to refer a patient to
- securing rapid digital clinical communication to obtain specialist advice on MSK orthopaedic and diagnostic management
- enabling access to specialist advice where there is diagnostic uncertainty.
- Investigations:
- identifying which diagnostics are appropriate
- clarification on further management options after receiving investigation reports, such as bloods, X-ray/MRI, if this advice is not available from primary care clinicians with MSK expertise
- where there is diagnostic uncertainty/an anomaly in clinical presentation, eg widespread pain/paraesthesia, visceral referral, systemic disease, or for advice on alternative diagnostics if the usual investigation cannot be used.
- Management:
- appropriateness of a referral (who to refer, when to refer, who not to refer) if this advice is not available from primary care clinicians with MSK expertise, enabling patients to be seen in the most appropriate setting, by the right person, at the right time and through the right modality for care
- for patients who do not meet the evidenced-based interventions criteria but for whom there is concern that delaying care may result in a poorer outcome
- on a treatment plan and/or the ongoing care and treatment options for a patient
- which conditions are appropriate for injections in the community setting and secondary care setting
- to highlight a change in a patient’s condition since the initial referral and change their priority, and receive advice about management in the interim
- to optimise referral management in primary and community care for high volume MSK orthopaedic pathways
- shared decision-making, to ensure all appropriate options have been explored.
- Pathways:
- on the appropriateness of a patient referral, and whether there is a more appropriate care pathway, eg for osteoporosis and fragility fracture, physiotherapy, podiatry, osteopathy, rheumatology, orthopaedics, pain, health coaching, self-management education
- to optimise referral management in primary and community care for high volume MSK orthopaedic pathways where appropriate
- to build relationships and trust, and strengthen links between clinical professionals by sharing resources, experience and knowledge to improve healthcare equality for patients.
Specialist advice models in MSK orthopaedic management
Specialist advice must be delivered before a booking is made, but this can be pre or post referral:
- Pre-referral models, eg:
- specialist advice services delivered by secondary care (such as the e-RS A&G model)
- virtual review services offered by specialists/experts working in community or primary care (eg GPwERs or other suitably trained/qualified healthcare professionals such as FCPs)
- independently provided platforms delivering specialist advice to primary care colleagues.
- Post-referral models, eg specialist-led referral assessment or triage services that review a patient’s clinical referral information to identify which is the best onward clinical pathway to refer them to, or return the referral with advice to support further management in primary care. This will enable and support a shared decision-making conversation with the patient/carer about appropriate treatment options.
The model(s) used across a system is for local determination. It should complement standardised referral pathways and should not prevent or delay a referral if this is in the patient’s best interest.
Providing potential urgent and emergency conditions are excluded, local systems may want to consider a ‘specialist advice first’ approach to further enhance and streamline MSK care: rapid expert advice can avoid the booking of an inappropriate referral.
This practice can support the optimum and safe management of patients and ensure patients are presented with treatment options tailored to their clinical needs, preferences and values.
Current MSK orthopaedic service models offer opportunities to use specialist advice within the pre and post-referral pathway:
- Depending on local arrangements, varying MSK service models in primary, community and secondary care involve a wider team assessing MSK conditions, such as MSK FCPs, MSK APs, MSK specialist doctors and practitioners from community MSK services. These may all benefit from using specialist advice along the MSK pathway so that the patient is managed by the right clinician in the right setting.
- Referrals can be made to community MSK services, rheumatology, pain and diagnostic services, thereby using the appropriate MSK expertise across the pathway and helping make best use of secondary care capacity.
- Where there is diagnostic uncertainty, the use of specialist advice services by primary care clinicians, MSK FCPs, MSK APs, MSK specialist doctors and community MSK services into radiology services to access rapid specialist advice will streamline referrals.
- In addition, the use of radiology clinical decision support tools, eg iRefer, can help referrers in primary and community care request the best and safest imaging investigations, alongside all other opportunities that support MSK referral optimisation in primary and community care to ensure optimal patient experience and outcomes, as well as avoid unnecessary outpatient appointments.
Specialist advice can potentially be of most value in the MSK orthopaedic pathway between:
- primary care and specialist primary care clinicians eg MSK FCPs / MSK APs / MSK specialist doctors
- primary care/specialist primary care clinicians and community MSK services
- community MSK services, secondary care orthopaedic outpatients and fracture liaison services
- primary care/specialist primary care clinicians and secondary care orthopaedic outpatients.
Involving people with lived experience in co-designing MSK orthopaedic specialist advice services ensures patient and carer views are represented.
Trusts have a legal responsibility to complete their own equality and health inequalities impact assessment (EHIA) for the services they offer. This will help them better understand the potential impacts of specialist advice for patients and identify effective interventions to address any inequalities that could emerge.
Who can provide specialist advice in MSK orthopaedic management?
Systems should optimise the use of all available specialist advice within primary, community and secondary care.
Current MSK orthopaedic service models involve the wider primary and community care team of healthcare professionals assessing MSK conditions.
Therefore, specialist advice can be provided by medical doctors or other appropriately qualified and experienced healthcare professionals, including: consultant orthopaedic surgeons; specialist registrars; GPwER; MSK FCPs; MSK APs or CPs; or specialist nurses, depending on local governance arrangements.
Formalising specialist advice where an informal approach may already exist will enable safe and timely access to specialist care, streamlining those patients needing outpatient appointments to the correct service and optimising their care and experience.
Who can submit a request for specialist advice in MSK orthopaedic management?
The requesting clinician has traditionally been a GP. However, a wider primary and community care team of healthcare professionals now assess MSK conditions and may also need to access specialist advice.
They may access this from specialist primary care clinicians eg MSK FCPs, MSK APs and MSK specialist doctors, but if a query cannot be resolved at primary care level, any of these clinicians can request specialist advice from community MSK services or consultant orthopaedic surgeons as appropriate.
What are the expected turnaround times for specialist advice in MSK orthopaedic management?
The recommended response time should be within two working days to ensure timely clinical decision-making and minimise delays to onward referral if this is required. However, the timeframe should be agreed locally to reflect local service needs and systems, and adequate time allocated in providers’ job plans to deliver this.
Serious pathology as a cause of MSK conditions should not be managed through specialist advice services, but by following the guidance set out in Urgent and emergency musculoskeletal conditions requiring onward referral.
Can specialist advice be used for follow-up of MSK orthopaedic patients?
Specialist advice provides rapid MSK support for patients who have not yet been referred, and may not require referral, to secondary care orthopaedic outpatient services.
Local systems may agree to provide rapid digital access to specialist advice to support earlier and appropriate discharge of patients by provider teams.
However, patients receiving ongoing orthopaedic follow-up should continue to be supported by the clinician who knows them and their condition best and has overall responsibility for their care.
Can generic MSK advice be accessed via specialist advice services?
The service is intended to provide rapid MSK specialist clinical advice on the care of individual patients, based on the information their referring clinician provides.
The exception is the provision of advice on serious pathology as a cause of MSK conditions, which needs to be managed as an emergency or an urgent onward referral as directed by local pathways.
Guidance on urgent and emergency musculoskeletal conditions requiring onward referral supports primary and community care practitioners in recognising serious pathology.
How do referral triage/assessment services differ from specialist advice services?
Referral triage/RAS provides specialist-led assessment of a patient’s clinical referral information to support a decision on primary care management or the most appropriate onward clinical pathway.
Referrals may be returned to the original referrer with advice to continue to manage the patient in the community; this is similar to specialist advice but differs in that a referral will have been created with the implicit expectation that onward care will be managed by the service receiving the referral.
Providers can undertake referral triage through e-RS RAS, clinical assessment and triage services (CATS) and referral management centres (RMCs), to provide an intermediate level of clinical assessment and treatment between traditional primary and secondary care, or within primary care.
This is non-face-to-face activity, but the RTT clock will have started as a referral has been made. However, no booking will have been made, or appointment slot issued in lieu of a booking, and the episode/patient is not automatically registered on the provider’s patient treatment list.
In general, most community MSK services have a triage function to support diagnosis and divert unnecessary referrals away from secondary care where clinically appropriate.
Enabling specialist advice service referrals complements and enhances referral optimisation within primary and community care.
Resourcing considerations
Specialist advice services must be formalised and adequately resourced to respond to requests in a safe, effective and timely manner; and the need for this resource factored into the wider planning of MSK and diagnostic activity.
This is for local consideration and agreement, and should reflect the best use of resource to deliver a robust specialist advice service.
There is currently wide variation in the extent to which specialist advice for MSK orthopaedic services is resourced and planned. Any changes to referral pathways will need engagement with and agreement between primary, community and secondary care clinical and management teams alongside commissioning and contracting colleagues.
Primary care resourcing considerations
It is important to consider as part of workforce and resource planning that specialist advice may result in a significant shift of the work traditionally carried out by secondary care to primary (and potentially community) care teams.
Therefore, close communication is needed between primary and secondary care services when establishing these services, to determine which patients can be appropriately managed outside a secondary care setting and what access to services and diagnostic provision is in place, supported by appropriate commissioning.
MSK orthopaedic specialist advice resourcing considerations for requesting clinicians may include:
- reviewing previous referral letters and other appropriate documentation
- (potentially) ordering tests and following up results
- reviewing medications and imaging if/as needed
- explaining to the patient how the specialist advice process works, including that the outcome may be a referral (where appropriate), and addressing any questions or concerns
- logging into the appropriate platform, creating the request or dictating the request for a member of the administrative team to send
- contact with the patient or carer to share the outcome/response of the specialist advice request, remotely or in person, where appropriate
- any ongoing management of the patient as appropriate.
Job planning considerations
MSK orthopaedic services may wish to estimate the number of specialist advice requests in a session based on the service casemix and the balance between new and ongoing requests.
For example, 25 requests in a four-hour session allows 8–10 minutes per case, depending on the activities expected to be undertaken (see below).
Job planning should include:
- reviewing referral letters and attachments/imaging
- where required, reviewing additional information in the patient record, including diagnostic results and relevant medical history
- reviewing literature/evidence-based search for cases where there is uncertainty on how to manage a patient
- typing or digitally dictating a suggested diagnosis and management plan where this is appropriate or recommending specific investigations
- converting the specialist advice to a referral where appropriate and indicating the priority of this
- attaching documents/guidelines/web links
- phone calls to GPs, other clinical teams or patients for cases requiring urgent clinical intervention.
Patient contact and experience
Pre-referral specialist advice services are designed to support the reduction in unwarranted variation seen in MSK referral management and the inequalities that can ensue from this, and provide information to support clinicians and patients/carers to make shared decisions about care.
Careful consideration should be given to how services could impact on vulnerable groups, ensuring health inequalities are being identified and addressed.
Shared decision-making is a collaborative process that involves the patient/carer and their healthcare professional working together to reach a joint decision about care. To achieve this the patient/carer/family member needs to understand the risks, benefits and any consequences of the care management options available.
Specialist advice can help manage the expectations that come with this process and shared decision-making should be embedded in any specialist advice service. Decision support tools will also support this process. Further resources to support shared decision-making can be found in the further information section.
If systems are using NHS e-RS A&G, the receiving clinician can convert a specialist advice conversation to a referral as well as provide advice to the referring clinician. This removes the need to return the request to the referrer for them to take this action.
Once the referring clinician has received advice, if they intend to refer onwards, the available treatment options and potential outcomes, and choice of provider should be discussed and agreed with the patient/carer as part of a shared decision-making discussion, before authorising the conversion to referral function on the e-RS A&G request.
Further information about this e-RS functionality is provided on the NHS Digital website.
Patients do not routinely have direct access to the NHS e-RS specialist advice conversation but can request this from their GP practice.
Co-designing specialist advice services with patients/carers and people with lived experience ensures all aspects of embedding personalised care and shared decision-making, enhancing patient experience and outcomes are considered and included in service redesign.
Monitoring and evaluation
Measuring and evaluating specialist advice services can highlight good practice, support benchmarking and inform opportunities for system improvement. This helps develop sustainable services and improves outcomes for patients. Specialist advice services should be regularly reviewed to ensure they meet local requirements and quality standards.
The Elective Recovery Outpatients Collection (EROC) supports assurance of elective recovery in line with the 2023/24 priorities and operational planning guidance. It allows systems to establish a rich flow of information that can be used as a system improvement tool.
The System EROC includes any interactions that facilitate the seeking and/or provision of specialist advice, both before or instead of a referral and through referral assessment services that provide specialist advice post referral but pre booking.
System EROC FAQs and support guides can be found on the System EROC page on the OPRT FutureNHS platform.
The System EROC dashboard supports systems to monitor and evaluate specialist advice services. A registered OKTA account is required to access the dashboard; you can register for this at NHS England applications.
As well as analysis of use and outcome data through system EROC and the national dashboard, review and evaluation of specialist advice services should also include:
- periodic, internal qualitative review/audit of specialist advice responses by the provider to ensure clinicians across the team are giving consistent and comprehensive advice
- review and reporting of high volume and/or repeated specialist advice requests with incomplete clinical information or seeking advice that is readily available from accessible and recognised national referral resources
- user satisfaction (with outcomes) and experience (of process) – for both requesting and responding clinicians
- patient feedback
- shared decision-making measures.
Benefits realisation should also include measurement and evaluation of the carbon footprint. Greener NHS is currently developing a carbon calculator to help systems do this and make reducing carbon emissions part of business as usual.
Innovation and good practice
We are collecting ‘best practice’ case studies and will shortly make these available on the NHS FutureNHS collaboration platform.
Following publication of the National evaluation: advice & guidance services – an evaluation of demand-side factors, commissioned in England to evaluate how A&G is functioning, 46 recommendations were identified across nine broad areas:
- service standards
- governance
- systems
- elective care pathways
- widening access
- resourcing
- staff engagement
- patient involvement
- outcome monitoring.
Systems, commissioners, primary care networks, specialist advice provider organisations and patients/carers may want to refer to these as part of service redesign.
NHS England’s OPRT and BestMSK Health Collaborative programmes have developed high level MSK orthopaedic best practice clinical guidance toolkits for osteoarthritis hip and knee, spinal and radicular, and shoulder pain, which identify where specialist advice should be considered, as well as incorporating relevant quality standards and agreed best practice guidance to support all opportunities for transformation and innovation in these pathway.
Further information
Generic specialist advice FAQs can be found on the OPRT FutureNHS specialist advice page alongside a selection of other support tools and resources.
For further information on the measurement and evaluation of these services please visit the System EROC page on the OPRT FutureNHS platform.
NHS Digital provides information, support and a range of training materials on the use of specialist advice through e-RS.
The National evaluation: advice & guidance services – an evaluation of demand-side factors presents evidence and shares learning to support the ongoing development of A&G within the referral optimisation agenda.
The following information and tools support shared decision-making:
- A three-talk model for shared decision making: multistage consultation process
- Choosing Wisely UK: BRAN – make the most of your appointment
- Personalised Care Institute training on shared decision-making
- HEE Shared decision-making e-learning programme
Glossary
Consultant practitioner
An expert in clinical practice, bringing innovation and influence to clinical leadership as well as strategic direction in a particular field for the benefit of patients/clients (HEE: Multi-professional consultant-level practice capability and impact framework).
First contact practitioner (FCP)
A diagnostic clinician working in primary care at the top of their clinical scope of practice at master’s level Agenda for Change Band 7 or equivalent and above (First contact practitioners and advanced practitioners in primary care: (musculoskeletal) A roadmap to practice).
MSK FCPs can come from a range of allied health professions including physiotherapy, osteopathy, podiatry and occupational therapy.
MSK advanced practitioner
A clinician working at an advanced level (master’s level) across all four pillars of advanced practice (research, leadership and management, education and clinical practice)l (First contact practitioners and advanced practitioners in primary care: (musculoskeletal) a roadmap to practice).
MSK advanced practitioners can come from a range of allied health professions including physiotherapy, osteopathy, podiatry and occupational therapy.
MSK specialist doctors
- GP with extended role: a GP with a UK licence to practise who maintains a primary care medical role but also undertakes activity that is beyond the scope of general practice and requires further training (Royal College of General Practitioners guide to GP clinical extended roles, 2021).
- Sport and exercise medicine (SEM) consultants: specialists skilled in the delivery of MSK medicine, exercise medicine and team care (The Faculty of Sport and Exercise Medicine (fsem.ac.uk).
Specialist
Someone with expert MSK skills.

