1. Context
This national elective access policy aligns with the referral to treatment (RTT) rules and covers the core principles that all providers and systems should include in their local elective access policies, to support consistent application of waiting times rules and guidance. Local policies should reflect local pathways and implementation plans.
Trusts, wider health system leads and other key stakeholders should read this national policy to ensure they understand the principles of elective access and can identify where local policy adaptation is required.
Local elective access policies must be signed off by the provider and system board.
This policy should support the delivery of local training and understanding around RTT rules to both clinical and non-clinical staff, ensuring consistent application of RTT rules.
1.1. Policy structure
This national elective access policy covers:
- general principles (section 2)
- RTT and diagnostic standards and rules application (section 3)
- pathway-specific milestones (section 4)
From section 2 onwards general policy statements form the text, with supporting text outlining what trusts may wish to include in grey boxes. These boxes do not feature in those sections that are self-explanatory.
Alongside the trust’s elective access policy, we recommend that supporting standard operating procedures (SOPs) are in place to underpin the access policy principles and a RTT training strategy.
1.2. Equality health impact assessment
It is important to carry out an equality health impact assessment (EHIA) on an elective access policy. Start this when you start writing the elective access policy, not afterwards.
Please check your trust’s EHIA policy and template for further information. The EHIA should be kept up to date in line with the elective access policy and updated when the policy is changed.
An EHIA has been completed for this document.
2. General principles for referral to treatment (RTT) and diagnostic pathways
2.1. Introduction and purpose
The trust is committed to delivering high quality and timely elective care to patients.
This elective access policy:
- sets out the rules and principles under which the trust manages elective access to outpatient appointments, diagnostics and elective inpatient or day case treatment
- is designed to ensure that elective patient access to services is managed in a transparent, fair and equitable way, and according to clinical priorities
- gives staff clear direction on the application of the NHS Constitution and NHS Choice Framework in relation to elective waiting times
It was developed following consultation with staff, integrated care boards (ICBs), GPs and clinical leads. It will be reviewed and ratified at least annually or earlier if national elective access rules or locally agreed principles change.
This policy will be read by all applicable staff once they have successfully completed the relevant elective care training. It will not be used in isolation as a training tool.
It is underpinned by a comprehensive suite of detailed standard operating procedures (SOPs). All clinical and non-clinical staff must ensure they comply with both the principles in this policy and the specific instructions in the SOPs.
The trust is committed to promoting and providing services that meet the needs of individuals and do not discriminate against any employee, patient or visitor.
2.2. Roles and responsibilities
The staff roles involved in the delivery of elective pathways should reflect local delivery models. The below list is not exhaustive.
Although responsibility for achieving standards lies with the divisional directors and ultimately the trust board, all staff with access to and a duty to maintain elective care information systems are accountable for their accurate upkeep. For example:
- divisional directors are accountable for implementing, monitoring and ensuring standardised compliance with the policy within their divisions
- the chief information officer is responsible for the timely production of patient tracking lists (PTLs) that support the divisions in managing waiting lists and RTT standards
- waiting list administrators, clinic staff, secretaries and booking clerks are responsible to operational managers for standardising the application of and compliance with all aspects of the trust’s elective access policy
- waiting list administrators for outpatients, diagnostics and elective inpatient or day care services are responsible for the day-to-day management of their waiting lists and are supported in this function by the operational managers
- operational managers are responsible for ensuring the NHS e-Referral Service Directory of Services (DoS) is accurate and up to date, and are supported by divisional directors in achieving access standards
- the business intelligence team is responsible for producing and maintaining regular reports to enable divisions to accurately manage elective pathways and ensure compliance with this policy
- GPs and other referrers play a pivotal role in ensuring patients are fully informed during their consultation of the likely waiting times for a new outpatient consultation. They should outline expectations to the patient when they are referred, explaining that, if they are subsequently unable to attend their appointment, they should contact the hospital to rearrange it. GPs should ensure quality referrals are submitted to the appropriate provider first time
- clinicians with responsibility for patient pathways must have an appropriate level of understanding of RTT rules and their application, with specific focus on clinic outcoming
- ICBs are responsible for ensuring all patients are aware of their right to treatment at an alternative provider and the support available to them in the event that their RTT wait goes beyond 18 weeks or is likely to. In this instance ICBs must take all reasonable steps to offer the patient a suitable alternative provider(s) that can see or treat them more quickly than the provider to which they were referred. A suitable alternative provider is one that can provide clinically appropriate treatment and is commissioned by an ICB or NHS England. ICBs are responsible for ensuring there are robust communication links for feeding information back to GPs
2.3. Staff competency and compliance
Trusts should have a RTT training strategy that articulates the detail for the below.
Competency
As a key part of their induction programme, all new trust starters will undertake mandatory contextual elective care training applicable to their role.
All existing staff will undertake mandatory contextual elective care training on at least an annual basis.
All staff will carry out competency tests that are clearly documented to provide evidence that they have the required level of knowledge and ability.
This policy, along with the supporting suite of SOPs, will form the basis of contextual training programmes.
Compliance
Functional teams, specialties and staff will be performance managed against key performance indicators (KPIs) applicable to their role. Role-specific KPIs are based on the principles in this policy and specific aspects of the trust’s SOPs.
In the event of non-compliance, a resolution should initially be sought by the team, specialty or individual’s line manager. If it cannot be, the matter should then be dealt with via the trust’s disciplinary or capability procedure.
2.4. Governance
Trusts should describe their elective governance structures. An example is shown below. The trust’s board should have assurance through the governance framework that RTT core principles are being applied consistently by both clinical and non-clinical staff.
An example governance structure:
Weekly specialty-based access meeting
reports to:
Weekly divisional access meeting (trust only)
reports to:
Monthly access meeting (trust only)
reports to:
Monthly system-wide planned care board
Considerations when developing governance arrangements are:
- structure of the governance framework, including specific groups and sub-groups with deliverables relating directly to recovery goals
- board sign-off
- documented governance structure with agreed reporting lines to the senior oversight forum, including for KPIs and exception reporting
- key attendees and stakeholders with specific roles and deliverables relating to elective recovery. These include clinical leads to ensure risks of clinical harm to patients are being mitigated effectively
- fixed standard agenda items with clear escalation criteria for unresolved issues supported by review at the beginning of each meeting of a concise action report
2.5. Patient rights
The NHS Constitution for England sets out pledges and rights stating what patients, the public and staff can expect from the NHS.
Section 3 of the NHS Choice Framework states that a patient can choose where they go for their first appointment as an outpatient and section 4 states they can ask to be referred to a different hospital if:
- they have to wait, or have already waited, more than 18 weeks before starting treatment or assessment for a condition following non-urgent referral to a consultant-led service or
- following urgent referral for suspected cancer or breast symptoms, the provider is satisfied that the patient will not receive a diagnosis or ruling out of cancer within 28 days of referral, and an appointment with a suitable alternative provider may expedite a diagnosis or ruling out of cancer
Patients should be made aware of the support available to them, such as the travel reimbursement scheme, so they can make an informed decision.
Patient choice is a legal right for patients, but there are exceptions to be aware of. These are detailed in the NHS Choice Framework.
Military veterans
In line with the Armed Forces Covenant (2016), all veterans and war pensioners should receive priority access to NHS care for any conditions related to their service, subject to the clinical needs of all patients.
Prisoners
All elective standards and rules apply to prisoners. Delays to treatment because it is difficult for prison staff to escort patients to appointments or for treatment do not affect the recorded waiting time for the patient.
2.6. Patient eligibility
The trust has an obligation to identify patients who are not eligible for free NHS treatment and, specifically, to assess liability for charges in accordance with Department of Health and Social Care guidance and rules.
All staff have a responsibility to identify patients who are overseas visitors and to refer them to the overseas visitors office for clarification of status regarding entitlement to NHS treatment before their first appointment is booked or date to come in (TCI) agreed.
Further information for tailoring this part of the policy is given in:
2.7. Patients moving between NHS and private care
Patients can choose to move between NHS and private status at any point during their treatment without prejudice.
Where it has been agreed, for example, that a surgical procedure is necessary, the patient can be added directly to the elective waiting list if clinically appropriate. The RTT clock starts at the point the hospital receives the GP or original referrer’s letter. Should the patient notify the trust of their decision to seek private care, their RTT pathway will be closed with a clock stop applied on the date the patient notifies the trust.
2.8. Commissioner approved procedures and evidence-based interventions
Patients referred for treatments for which there may be only limited evidence of clinical effectiveness or which might be considered cosmetic can only be accepted with the prior approval of the relevant ICB. Clinicians should be aware of the list of procedures to ensure it is appropriate to offer the procedure before listing the patient.
If a patient is referred to a consultant-led service and funding approval is required before treatment, the RTT clock will continue to tick during the approval process. Where commissioners are asked to approve funding before a referral is made, then an 18-week clock would start once funding has been approved and the subsequent referral is received by the provider.
Local information and processes should be inserted in this section and further national information can be found in Evidence-based interventions programme.
2.9. Communication
All communications with patients and anyone else involved in the patient’s care pathway (for example, GP or a person acting on the patient’s behalf), whether verbal or written, must be informative, clear and concise. All providers should ensure compliance with the Accessible Information Standard so patients receive communications in the format they request, for example easy read or translated. Copies of all correspondence with the patient must be kept in their clinical notes or stored electronically for auditing purposes.
GPs or the relevant referrer must be kept informed in writing of the patient’s progress.
Regular two-way communication with the patient is key to ensuring they are fully informed and aware of any appointments for their care.
Patients should be made aware of their responsibility to attend agreed appointments.
Where a patient misses an appointment, locally agreed processes should be used to explore the causes and the responsible clinician informed, so they can decide whether it is appropriate to offer the patient further appointments.
Further information for good communication with patients waiting for care is provided in Good communication with patients waiting for care.
Reasonableness
A reasonable offer for any appointment or admission for any service is one that is made with at least 3 weeks’ notice. When made verbally or via email, the patient should be given 2 or more dates with at least 3 weeks’ notice to choose from.
If other dates become available at short notice, these will be offered to patients but can only be considered reasonable if the patient accepts them. If they decline these short notice offers, there is no impact on the patient’s pathway.
Uncontactable
Trusts should define ‘uncontactable’ when offering routine appointments and ensure there are SOPs with clear two-way communication channels. The below example adopts the ‘best practice’ definition.
A patient’s demographics and communication preferences should always be checked and updated at any appointment or when contact is made. Where a patient cannot be reached in the initial phone call, 3 further attempts on different days at different times (ideally one out of hours) should be made to contact the patient. Efforts should also be made to contact the original referrer (for example, GP) to confirm the patient’s demographics and communication preferences. If the patient still cannot be reached, they should be sent a letter informing them they have 3 weeks to make contact to book their appointment. If the patient does not make contact within those 3 weeks, they will be returned to their referrer.
2.10. Non-activity related RTT decisions
Where clinicians review test results in an office setting and make a clinical decision not to treat, the RTT clock will be stopped on the day this decision is communicated in writing to the patient.
2.11. Attendance and outcomes (new and follow-up clinics, diagnostics and admissions)
Every patient, whether they attend or not, will have an attendance status and outcome recorded on the patient administration system (PAS) at the end of the appointment.
2.12. Chronological booking
Patients will be selected for booking appointments or admission dates according to clinical priority. Patients of the same clinical priority will be offered an appointment or treatment date in RTT chronological order; that is, patients who have been waiting longest will be seen first.
Patients will be selected using the trust’s PTLs. They will not be selected from any paper-based systems.
3. National referral to treatment and diagnostic standards and rules application
The elective care standards are:
- referral to treatment: 92% of patients on an incomplete pathway (that is, still waiting for treatment) to be waiting no more than 18 weeks (or 126 days)
- diagnostics: 99% of patients to undergo the relevant diagnostic investigation within 5 weeks and 6 days (or 41 days) from the date of decision to refer to appointment date
In addition to these standards, separate cancer standards must be adhered to.
While the aim is to treat all elective patients within 18 weeks, the national elective access standards are set at <100% to allow tolerance for the following scenarios:
- clinical exceptions: when it is in the patient’s best clinical interest to wait more than 18 weeks for their treatment
- choice: when patients choose to extend their pathway beyond 18 weeks by declining reasonable offers of appointments, rescheduling previously agreed appointment dates or admission offers, or specifying a future date for an appointment or admission (in some situations a clock stop for active monitoring may be appropriate for patients choosing to wait longer)
- co-operation: when patients miss previously agreed appointment or admission dates (TCI) and this prevents the trust from treating them within 18 weeks
3.1. Overview of national referral to treatment rules
Figure 1 shows the key steps of a typical RTT pathway.
Figure 1: The key steps of a typical RTT pathway
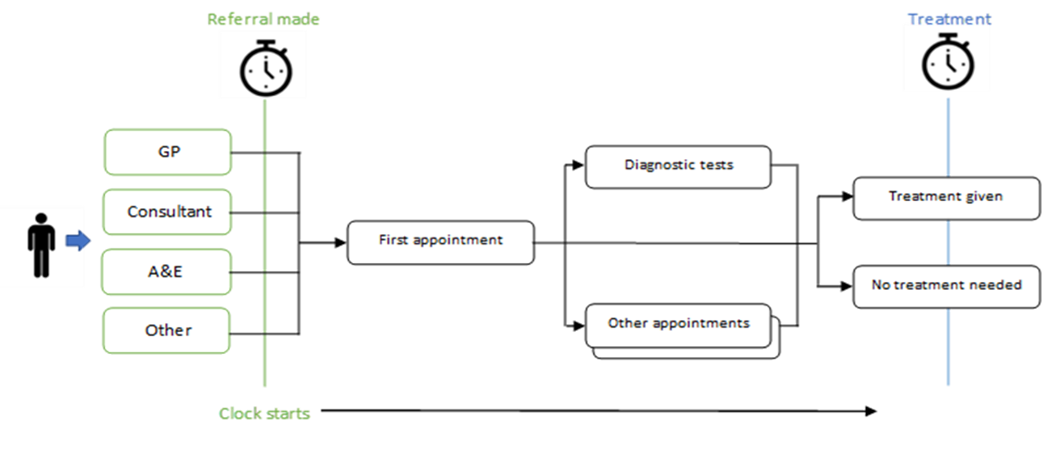
Click here to access explanatory text for figure 1
Step 1: A patient attends a GP appointment, A&E or another healthcare setting, or self-refers to a consultant, and is referred for a first appointment. The receipt of this request (or UBRN conversion) starts the RTT clock. Step 2: At the first appointment the patient could be referred for diagnostic tests or other appointments, or alternatively treatment is given or a decision that no treatment is needed is made; this is when the clock stops. Patients may have multiple diagnostic tests and/or appointments before a treatment decision is made. A patient may be added to the inpatient waiting list for treatment and the clock would stop when treatment starts.
Clock starts (Rules 1 to 3)
The RTT clock starts when any healthcare professional (or service permitted by an English NHS commissioner to make such referrals) refers a patient to a consultant-led service. The RTT clock start date is the date the trust receives the referral. For referrals received through the NHS e-Referral Service (e-RS), the RTT clock starts on the day the patient converts their unique booking reference.
Rule 1: Referrals by healthcare professionals or services
a. a referral is received into a consultant-led service, regardless of setting, with the intention that the patient will be assessed and, if appropriate, treated before clinical responsibility is transferred back to the referrer
b. a referral is received into an interface or referral management assessment centre. This may result in an onward referral to a consultant-led service before clinical responsibility is transferred back to the referrer
Rule 2: Self-referrals
A patient self-refers into a consultant-led service for pre-agreed services agreed by providers and commissioners.
Rule 3: The need for a new clock
On completion of a consultant-led RTT period, a new waiting time clock only starts:
a. when a patient becomes fit and ready for the second of a consultant-led bilateral procedure
b. on the decision to start a substantively new or different treatment that does not already form part of that patient’s agreed care plan
c. on a patient being re-referred into a consultant-led, interface or referral management or assessment service as a new referral
d. when a decision to treat (DTT) is made following a period of active monitoring. Some clinical pathways require patients to undergo regular monitoring or review diagnostics as part of an agreed programme of care. These events would not in themselves indicate a DTT or a new clock start. If a decision is made to treat after a period of active monitoring or watchful waiting, a new RTT clock would start on the date of DTT
e. when a patient rebooks their appointment following a first appointment did not attend (DNA) that stopped and nullified their earlier clock
RTT clock stops (Rules 4 and 5)
Rule 4: clock stops for treatment
a. first definitive treatment starts. First definitive treatment is defined as an intervention intended to manage a patient’s disease, condition or injury and avoid further intervention
This could be:
- treatment provided by an interface service
- treatment provided by a consultant-led service
- therapy or healthcare science intervention provided in secondary care or at an interface service, if this is what the consultant-led or interface service decides is the best way to manage the patient’s disease, condition or injury and avoid further interventions
b. a clinical decision is made to add the patient to a transplant list and this decision has been communicated to the patient and subsequently their GP or other referring practitioner without undue delay
Rule 5: Clock stops for non-treatment
A waiting time clock stops when it is communicated to the patient and subsequently their GP or other referring practitioner without undue delay that:
a. it is clinically appropriate to return the patient to primary care for any non-consultant led treatment in primary care
b. a clinical decision is made to start the patient on a period of active monitoring
c. a patient declines treatment having been offered it
d. a clinical decision is made not to treat
e. a patient misses their first appointment following the initial referral that started their waiting time clock, provided that the provider can demonstrate that the appointment was clearly communicated to the patient (DNAs for a first appointment following the initial referral that started a waiting time clock nullify the patient’s clock; that is, it is removed from the numerator and denominator for RTT time measurement purposes)
f. a patient misses any other appointment and is subsequently discharged back to the care of their GP, provided that:
- the provider can demonstrate that the appointment was clearly communicated to the patient (according to their preferences)
- discharging the patient is not contrary to their best clinical interests
- discharging the patient is carried out according to local, publicly available or published policies on missed appointments
- these local policies are clearly defined and specifically protect the clinical interests of vulnerable patients (for example, children), and are agreed with clinicians, commissioners, patients and other relevant stakeholders
3.1.3. Exclusions
A referral to most consultant-led services starts an RTT clock but the following services and types of patients are excluded from RTT reporting:
- obstetrics and midwifery
- planned patients
- referrals to a non-consultant led service
- referrals for patients from non-English commissioners
- genitourinary medicine services
- emergency pathway non-elective follow-up clinic activity
3.2 Non-consultant led pathway and RTT clocks
Referrals to therapy or healthcare science interventions (for example, physiotherapy, dietetics, orthotics and surgical appliances) can be:
- directly from GPs where an RTT clock would not be applicable
- during an open RTT pathway where the intervention is intended as first definitive treatment or interim treatment
Depending on the particular pathway or patient, therapy or healthcare science interventions could constitute an RTT clock stop. Equally the clock could continue to tick. It is critical that staff in these services know if patients are on an open pathway and if the referral to them is intended as first definitive treatment.
Physiotherapy
For patients on an orthopaedic pathway referred for physiotherapy as first definitive treatment, the RTT clock stops when the patient begins physiotherapy.
For patients on an orthopaedic pathway referred for physiotherapy as interim treatment (as surgery will definitely be required), the RTT clock continues when the patient has physiotherapy.
Surgical appliances
Patients on an orthopaedic pathway can be referred for a surgical appliance with no other form of treatment agreed. In this scenario, the fitting of the appliance constitutes first definitive treatment and therefore the RTT clock stops when this occurs.
Dietetics
If patients are referred to the dietitian and receive dietary advice with no other form of treatment, this would constitute an RTT clock stop. Equally, patients could receive dietary advice as an important step of a particular pathway (for example, bariatric surgery). In such a pathway, the clock could continue to tick.
3.3. Missed appointments
Trusts need to agree their own procedures and processes for managing missed appointments. It is imperative that such arrangements are founded on individual patients’ best clinical interests and that they do not include blanket rules for stopping the clock. Additional information can be found in Did not attends (DNAs)
A clinical review must occur for any missed appointment. A clinician can decide to discharge the patient back to the original referrer (stopping the clock) where this is not contrary to the patient’s best clinical interests. Where a patient misses a subsequent appointment and another appointment is offered, the RTT clock continues to tick.
Section 8.1 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care may become relevant if patients could come to harm by repeatedly failing to attend appointments.
Outpatients
The clinician will review all missed appointments at the end of their clinic to make a clinical decision regarding next steps. Appointments missed by paediatric and other vulnerable patients should be managed with reference to the trust’s safeguarding policy.
Missed first appointments
The RTT clock is stopped and nullified in all cases (Rule 5e), as long as the trust can demonstrate the appointment was clearly communicated to the patient.
If the patient subsequently contacts the trust to rebook their first appointment, this will start a new RTT clock. The clock starts on the date that the patient contacts the trust to rebook their new appointment. If the clinician indicates another first appointment should be offered before the patient contacts the trust to rebook, a new RTT clock will be started on the date this decision is made. If it is not possible to book an appointment due to capacity pressures or lack of available appointment slots, the clock should still start from the decision to offer another appointment and the patient should be added to a waiting list as an alternative to booking their appointment.TT
Further information can be found in sections 3.4.5 and 4.4.1.3 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
Missed subsequent (follow-up) appointments
The RTT clock is stopped if the clinician, following engagement with the patient, decides it is in their best clinical interest to be discharged back to their GP or referrer, as long as the trust can demonstrate the appointment was booked in line with the criteria listed in Rule 5f.
The RTT clock continues if the clinician indicates that a further appointment should be offered. If patients wait more than 18 weeks as a result of such delays, the 8% tolerance within the RTT standard is in place to account for this.
If the subsequent appointment is with a support service, for example preoperative assessment or diagnostics, and is missed, the decision about rebooking should be made by the requesting clinician.
Admissions
Patients who do not attend for admission will have their pathway reviewed by their consultant. If the patient’s consultant decides that they should be offered a further admission date, the RTT clock continues to tick. If the patient’s consultant decides that it is in the patient’s best clinical interest to be discharged back to their GP, the RTT clock is stopped.
3.4. Cancelled appointment or admission dates
Appointment cancellations initiated by the patient
The trust should ensure that the policy does not include blanket rules such as a maximum number of cancellations or default to discharge. It is important that clinicians make all decisions on an individual patient basis. Clinicians should strike a balance between the trust’s responsibility for acting in the patient’s best clinical interests and the fact that patients have a right to choose to delay. Further information can be found in section 4.4.2. of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
Patients should be made aware of their responsibility to do what they can to attend the appointment. If the patient gives any notice that they cannot attend their appointment (even if this is on the day of the clinic), this should be recorded as a cancellation and not a missed appointment.
Cancellations in themselves do not stop clocks. A clock should only be stopped following a clinical review and decision to discharge (where this is in the patient’s best clinical interest) or where there is agreement between the clinician and the patient to initiate a period of active monitoring (see section 3.6. Active monitoring).
Where a patient cancels at short notice (<48 hours before appointment) or has cancelled 2 appointments on the same pathway, providers should ensure that the patient’s reasons for this are understood and a clinical review is undertaken.
Appointment changes initiated by the hospital
Hospital-initiated changes to appointments for reasons such as staff availability, suspension of services or equipment failure will be avoided as far as possible as they are poor practice and cause inconvenience to patients.
Furthermore, clinicians are actively encouraged to book annual leave and study leave as early as possible. Clinicians must provide 6 weeks’ notice if a clinic has to be cancelled or reduced.
Patients will be contacted immediately if the trust identifies it needs to cancel their appointment or admission and they will be offered an alternative date(s) that will allow patients on open RTT pathways to be treated as quickly as possible. Equally, this will allow patients not on open RTT pathways to be reviewed as close to the clinically agreed timeframe as possible.
Hospital-initiated changes to appointments do not affect the RTT waiting time and the clock should continue to tick.
Further information can be found in section 4.4.2.2 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
3.5. Patients who decline appointment or admission date offers
If patients decline the appointment or TCI dates they are offered or contact the trust to cancel a previously agreed appointment or admission date, this will be recorded on the PAS. The RTT clock continues to tick until a clinical decision is made about the next steps.
When a patient declines 2 reasonable offers of dates (which may be at different sites) that are within 6 weeks of each other and wishes to delay their pathway, the consultant should review the patient. The consultant may agree a period of active monitoring with the patient, which should include an appropriate timeframe for further follow-up or review (see section 3.6. Active monitoring). If at the point the patient indicates their availability or at the agreed follow-up review there is agreement to proceed to treatment, a new decision to treat will be recorded and a new RTT clock will start. Although the patient’s clock will start from 0 as normal, the service will offer a new appointment or TCI date in line with clinical prioritisation and act as if the patient is on the waiting list at the point they were before active monitoring started.
3.5.1. Patients who decline earlier appointments or treatment at an alternative provider
It may be necessary to offer patients the option to be seen or treated at another provider. This may be at a private provider as part of an outsourcing arrangement.
The same process and clock rules apply as for patients who cancel or decline appointment or admission offers. However, offers at alternative providers must state date, provider and team and meet reasonableness criteria.
It is important to fully understand a patient’s social as well as clinical factors to best assist them in deciding whether or not to move to an alternative provider. Considerations may include access to transport and carer assistance.
Further information can be found in section 8.3 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
3.6. Active monitoring
Active monitoring is where the clinician, following engagement with the patient, decides the patient may not require treatment at this time but should be monitored in secondary care. When a decision by a clinician to begin a period of active monitoring is made, agreed and communicated to the patient, the RTT clock stops.
It is important that the policy is consistent with national rules and that no blanket rules are stated or applied.
Stopping a patient’s clock for a period of active monitoring requires careful consideration on a case-by-case basis and needs to be consistent with the patient’s perception of their wait. Each decision should be made on an individual patient basis.
Active monitoring may be appropriate in the following situations:
Hospital initiated:
- when the most clinically appropriate option is for the patient to be actively monitored over a period of time, rather than to undergo any further tests, treatments or other clinical interventions at that time
- when a patient wishes to delay their pathway and declines 2 offers of reasonable dates, the clinician may decide to start a period of active monitoring, following a clinical conversation with and the agreement of the patient. Where a patient declares a period of unavailability (for example, a teacher wishes to wait until the school holidays for treatment), it may not be appropriate to offer specific dates within this period (as it is known that the patient will not be able to attend). In this situation, active monitoring should not be considered unless 2 reasonable dates could have been offered during the period of declared unavailability
- when a patient declines 2 reasonable offers of dates for earlier appointment or admission at an alternative provider, the clinician may decide to start a period of active monitoring, following a clinical conversation with and the agreement of the patient. Before offering dates at an alternative provider, the trust should have determined that it would be clinically and socially appropriate for the patient to be seen at the alternative provider. A reasonable alternative provider should be agreed on a case-by-case basis, recognising geographical and social factors, and offers must state details of the date, provider and team. Pragmatic application of active monitoring guidance is encouraged
Patient initiated:
- patients may also initiate a period of active monitoring – for example, by choosing to decline treatment to see how they cope with their symptoms
Where a patient declines reasonable offers of dates and indicates that they wish to delay their pathway, or where a patient communicates a period of unavailability for social reasons (for example, holidays, exams) in which 2 reasonable dates could have been offered, this should be recorded on the PAS. The clinician should arrange a discussion with their patient to ensure the patient fully understands the clinical implications of the delay and allow a clinical decision to be taken on next appropriate step, which may be a period of active monitoring. Any decision that affects the RTT status of the pathway should be discussed and agreed with the patient.
It is not possible to be specific about compulsory timescales within a national elective access policy and each decision is individual. However, initiating a period of active monitoring and stopping a clock for a few days is unlikely to make clinical sense or sense to a patient. Conversely, where a patient wishes to delay their pathway for a longer period, trusts should ensure ongoing clinical review to consider whether the best option is to start a period of active monitoring or whether the patient’s clock should continue to tick.
As a guide, where a patient wishes to delay their pathway by more than 6 weeks, they should have a clinical review to assess the potential impact on their condition and treatment plan and support the clinical decision on next steps. The following next steps may be considered:
- clinically safe for the patient to delay: continue planning for the patient’s treatment if only a short delay is requested or active monitoring where agreed with the patient, including regular review
- clinically unsafe length of delay: clinician to contact the patient with a view to persuading them not to delay. In exceptional circumstances where the clinician believes the patient’s decision to delay their pathway will have a consequential impact on the patient’s treatment plan, it may be appropriate to place the patient on active monitoring (clock stop). If the clinician and the patient make a shared decision to start active monitoring, this decision should include a date for review within a maximum of 12 weeks, so that the patient’s condition and treatment options can be reassessed following the period of active monitoring
- clinically unsafe length of delay: clinical assessment that it is in the patient’s best clinical interests to return them to their GP. The patient is discharged and their RTT clock stops on the day this decision is communicated to the patient and their GP
At the point a decision to start a period of active monitoring is made, the RTT clock will stop. In most cases, it will be clear how the rules should apply. However, where there is doubt or where decisions on the application of the RTT rules are finely balanced, then local clinical decisions should be made within the guidance of national rules. The discussion with the patient about starting a period of active monitoring should include an appropriate timeframe for further follow-up or review. Patients can request delays of any length but should be regularly reviewed in case their condition deteriorates. Where patients are placed on active monitoring due to their request to delay their pathway, a clinical review must take place at least every 12 weeks. Where active monitoring extends past 12 weeks, a clinical review should be undertaken to check the patient’s condition and confirm that active monitoring remains appropriate. The pathway should be visible on a relevant PTL or waiting list report for non-RTT pathways.
When a patient is placed on active monitoring they should be given written contact details and a clear process for two-way communication between them and the clinician in the event that their condition or circumstances change. In all scenarios a new waiting time clock will start when a new decision to treat is made with the patient following a period of active monitoring. For patients who have been placed on active monitoring due to their unavailability, once the patient wishes to go ahead the provider should offer a new appointment or admission date, acting as if the patient is on the waiting list at the point they were before active monitoring started.
Further information on the application of active monitoring can be found in sections 4.4.1.4 and 8.3 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
Patients should be signposted to relevant information or organisations, such as those in the voluntary, community and social enterprise sector, for social issues and any resources that may help them self-manage their condition.
3.6.1. Patients who require thinking time
Patients may wish to think about the recommended treatment options before confirming they would like to proceed. They should be signposted to any support they need to make an informed decision.
The RTT clock should not be stopped where the patient takes only a few days to think about their decision. Where a patient states that they anticipate they will need longer to make a decision, such as months, it may be appropriate to agree a period of active monitoring with them. This decision can only be made by a clinician and on an individual patient basis with their best clinical interests in mind.
Where more than 14 days elapse without next steps being agreed, trusts are encouraged to ensure the patient is contacted so options can be discussed with them.
Where active monitoring has been appropriately applied and the patient decides to proceed, a new RTT clock should start from the date of the decision to admit (DTA).
Further information is given in sections 4.4.1.4 and 8.3 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
4. Pathway-specific milestones
Trusts may wish to add or remove sections of the patient pathway into or from their preferred way of managing stages of treatment.
4.1. Non-admitted pathways
The non-admitted part of the patient pathway comprises the outpatients and diagnostic stages. It starts from the clock start date (that is, the date the trust receives the referral) and ends when a clock stop happens in outpatients (this could at the first, second or a further appointment) or when a decision to admit for treatment is made and the patient transfers to the admitted pathway. This is shown in Figure 2.
Figure 2: Non-admitted stages of the patient pathway
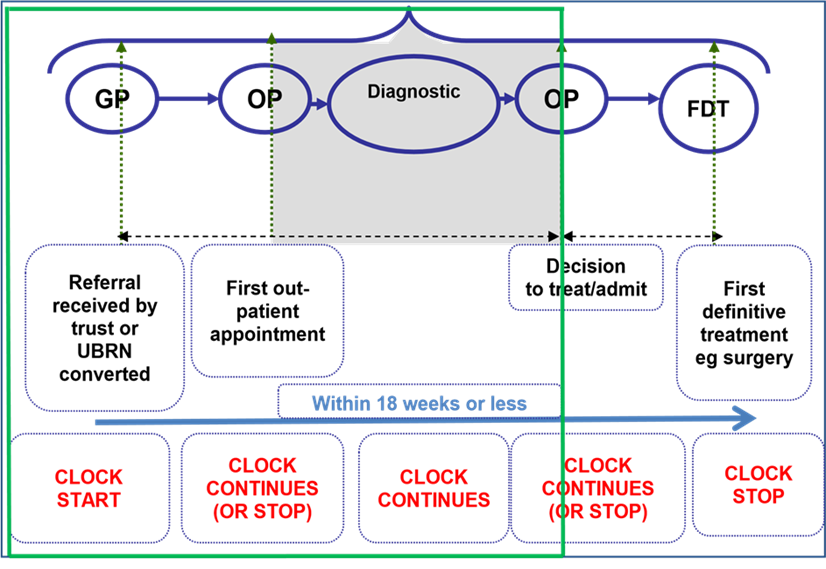
UBRN, unique booking reference number; FDT, first definitive treatment
4.2. Methods of receipt
All referrals from GPs to consultant-led services should be made electronically through the national e-Referral Service (e-RS).
A SOP should detail how the different methods of receipt should be processed onto the trust’s PAS and the expected turnaround time, including how this will be monitored. The different methods should include:
- NHS e-referrals (via e-RS)
- paper-based referrals (including via email)
4.3. Referral types
Trusts should ensure they detail any unique local referral types or services that may have different processes and ensure that sufficient guidance is given in a SOP. This section provides examples.
Referral management centres (RMCs) and referral assessment centres (RAS)
A referral to an RMC or RAS starts an 18-week RTT clock from the day the referral is received in the RMC or RAS. If the patient is referred on to the trust having not received any treatment in the service, the trust inherits the 18-week RTT wait for the patient.
A minimum data set (MDS) form must be used to transfer 18-week information about the patient to the trust.
This is different to advice and guidance (A&G), which does not start an 18-week RTT clock unless the consultant converts the request or receives notice of the referral.
A clinician may wish to seek A&G to:
- ask for advice on a treatment plan and/or the ongoing management of a patient
- ask for clarification regarding a patient’s test results
- seek advice on the appropriateness of a referral for their patient
Inter-provider transfers (IPTs)
Incoming IPTs
All IPT referrals will be received electronically via the trust’s secure generic NHS.net email account in the central booking office.
The trust expects to receive an MDS pro forma with the IPT, detailing the patient’s current RTT status (the trust will inherit any RTT wait already incurred at the referring trust if the patient has not yet been treated) and whether the patient has been referred for a new treatment plan for the same condition (where a new RTT clock will start on receipt at the receiving trust). The patient’s pathway identifier (PPID) should also be provided.
If the IPT is for a diagnostic test only, the referring trust retains responsibility for the RTT pathway.
If any of the above information is missing, the referral should be recorded on the PAS and the information chased by the booking office.
Outgoing IPTs
The trust will ensure that outgoing IPTs are processed as quickly as possible to avoid any unnecessary delays in the patient’s pathway.
An accompanying MDS pro forma will be sent with the IPT, detailing the patient’s current RTT status (the receiving trust will inherit any RTT wait already incurred if the patient has not yet been treated). If the patient has been referred for a new treatment plan for the same condition, a new RTT clock will start on receipt at the receiving trust. The patient’s PPID will also be provided.
If the outgoing IPT is for a diagnostic test only, the referring trust retains responsibility for the RTT pathway.
Referrals and the accompanying MDS will be emailed securely from the specialty NHS.net account to the generic central booking office NHS.net account. The central booking office will verify (and correct if necessary) the RTT status for the patient. If the patient has not yet been treated, the RTT clock will be nullified at this trust. This trust will then forward this information to the receiving trust within 1 working day of receipt into the generic email inbox.
RTT waits should be reported by the provider that has overall clinical responsibility for the patient. Where the transfer of responsibility and reporting may affect acceptance of the pathway – for example, due to the time the patient has waited – arrangements should be discussed and agreed with all relevant providers and commissioners. Referring and receiving providers should ensure clear processes are in place to support the clinical management of the patient, with timely updates to allow pathway data to be accurately reported.
Further information about the reporting of waiting times for patients who transfer between organisations can be found in section 11 of Recording and reporting referral to treatment (RTT) waiting times for consultant-led elective care.
4.4. Appointment slot issues (ASIs)
ASIs present a clinical risk as an RTT clock does not start on a trust’s PAS while the patient’s referral is on an ASI worklist, and patients may not be visible on the trust’s PTL.
Referrals should be either resolved or added to the PAS within 48 hours with the date the unique booking reference number (UBRN) was created as the RTT clock start. It is important to resolve these ASIs promptly as they will be removed from the worklist if not actioned after 26 weeks and will then only be visible on another report within e-RS. They should be monitored closely so that action can be taken to prevent referrals being lost, supported by a SOP.
When patients are unsuccessful in directly booking their first outpatient appointment via e-RS, the RTT clock should be started from the date the patient attempted to book their appointment – for example, when the hospital receives the referral on its ASI worklist.
4.5. Multiple RTT periods on the same pathway
A patient can have multiple RTT periods along the patient pathway for the same original referral. This is where a patient is treated for a condition and then has further treatment for the same underlying condition (for example, chronic or recurrent). The patient pathway will continue beyond the point the first definitive treatment starts, to include further treatment for the same condition. The RTT clocks for these treatments are sequential, not concurrent, as new treatment decisions and plans are made. There may also be periods of active monitoring between these decisions.
Figure 3: Multiple RTT periods on the same pathway
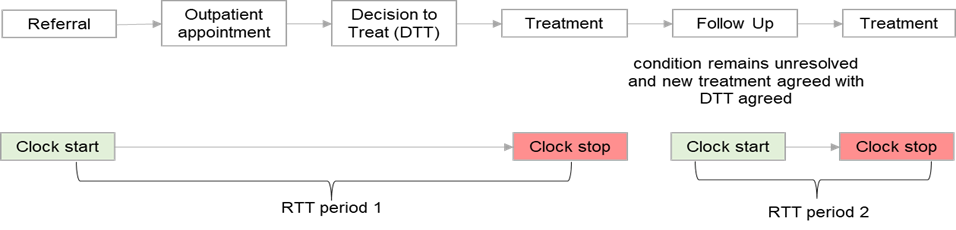
Click here to access explanatory text for figure 3
This diagram shows 2 RTT periods on the same pathway:
RTT period 1:
- referral (clock start)
- outpatient appointment
- decision to treat (DTT)
- treatment (clock stop)
RTT period 2:
4.6 Multiple RTT pathways
Where a patient has more than one referral for unrelated clinical reasons, each referral will have its own patient pathway and RTT clock. It is important to understand any impact the management of one condition has on that for another – for example, where treatment for one condition affects the planning of another treatment or where a patient needs a period of recovery before they can be treated for another condition.
Clinical and operational teams should co-ordinate care pathways as appropriate for patients on multiple pathways. It may be appropriate to agree a period of active monitoring for one pathway while the patient undergoes and recovers from treatment on another pathway that is considered to be the clinical priority.
Figure 4: Multiple RTT pathways
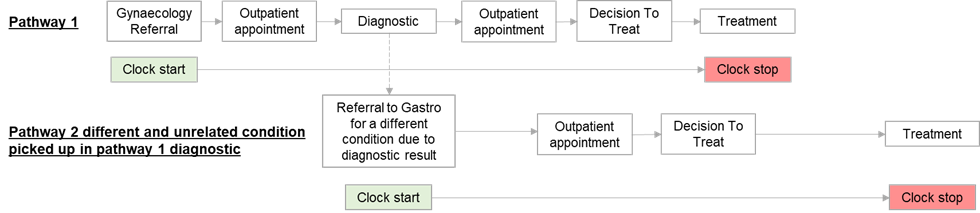
Click here to access explanatory text for figure 4
This diagram shows 2 pathways for the treatment of different conditions and their co-ordination.
Pathway 1:
1. gynaecology referral (clock start)
2. outpatient appointment
3. diagnostic – referral to gastro for a different condition due to diagnostic result
4. outpatient appointment
5. decision to treat
6. treatment (clock stop)
Pathway 2 (for a different unrelated condition picked up in pathway 1 diagnostic):
1. referral to gastro for a different condition due to diagnostic result (clock start)
2. outpatient appointment
3. decision to treat
4. treatment – after treatment and recovery from pathway 1 treatment (clock stop)
Both pathways continue to run – that is, the planning of treatment for pathway 1 does not affect the continuation of pathway 2.
4.7. Diagnostics
This section concerns the diagnostic phase of the patient pathway. Although some patients will already be known to the hospital from outpatients, it is important that the trust details any other referral routes. As examples, the following sections cover patients with an RTT and diagnostic clock, straight to test and diagnostic only patients.
The diagnostic stage of the RTT pathway forms part of the non-admitted pathway (see figure 2). It starts at the point a decision is made to refer a patient for a diagnostic test and ends when the result or report from the diagnostic procedure is available to the requester.
Where a patient is referred to another provider for a diagnostic test while on an active RTT pathway, the host trust will retain overall and reporting responsibility.
4.8. Patients with a diagnostic and RTT clock
Many patients referred for a diagnostic test will also be on an open RTT pathway. In these circumstances, the patient will have both clock types running concurrently:
- their RTT clock – started at the point the trust received the original referral
- their diagnostic clock – starts at the point the decision is made to refer for a diagnostic test
Where the patient is solely waiting for a therapeutic procedure – for example, in the radiology department – there is no 6-week diagnostic standard. However, for many patients there is also a diagnostic element to their admission or appointment, and so they will need to have their procedure within 6 weeks.
4.9. Straight-to-test arrangements
For patients who are referred for a diagnostic test for which one of the possible outcomes is review and, if appropriate, treatment within a consultant-led service (without first being reviewed by their GP), an RTT clock will start on receipt of the referral. These are called straight-to-test referrals.
The trust should appendix an agreed list of straight-to-test services.
4.10. Direct access diagnostics
Patients who are referred directly for a diagnostic test (but not consultant-led treatment) by their GP – that is, clinical responsibility remains with the GP – will only have a diagnostic clock running. These are called direct access referrals.
The trust should appendix an agreed list of direct access services.
4.11. National diagnostic clock rules
All patients referred for a diagnostic test that is not planned or part of a screening programme are expected to be dated within 6 weeks of referral.
Diagnostic clock start: the clock starts at the point the GP or consultant decides to refer for a diagnostic test (day 0).
Diagnostic clock stop: the clock stops at the point the patient has the test.
Patients referred for planned diagnostics must be offered a date by their due date. A diagnostic 6-week clock will start on the due date for patients who have not been dated by this date.
If a patient declines a reasonable offer, cancels an appointment offered with reasonable notice or misses an appointment offered with reasonable notice, the diagnostic 6-week waiting time clock can be reset to 0 and the waiting time will start again from the date the appointment is declined, cancelled or missed. This has no effect on the RTT clock and so all patients should be offered the next available appointment.
4.12. Preoperative assessment (POA)
This section should identify at what stage in the pathway patients can expect to be preoperatively assessed. This may include at walk-in appointments on the same day as the decision to admit and telephone assessment for non-complex patients or procedures. This section also describes the principles and RTT clock rules for the management of the patient’s fitness.
All patients with a decision to admit (DTA) requiring a general anaesthetic will require a POA. A patient’s fitness for surgery should be assessed or as a minimum they should have initial screening, as soon as possible after the DTA. Where necessary, patients should be made aware in advance of their outpatient appointment that they may need to stay longer on the day of their appointment for POA.
Many patients can be assessed by the trust’s dedicated POA nurse specialists. For patients with complex health issues requiring a POA appointment with a nurse consultant or anaesthetist, the trust will aim to agree the date for this with the patient before they leave the clinic. The trust will aim to agree a POA appointment no later than 7 working days from the DTA.
If additional tests are required to ascertain a patient’s fitness, the RTT clock continues while these are arranged.
4.12.1. Patients who are unfit for surgery
If the patient is assessed as unfit for the procedure, the nature and duration of the clinical issue should be ascertained.
Short-term illnesses
If the clinical issue is short-term and has no impact on the original clinical decision to undertake the procedure (for example, cough, cold), the RTT clock continues.
Longer-term illnesses
If the clinical issue is more serious and the patient requires optimisation or treatment for it, clinicians should indicate to administration staff:
- that the patient requires optimisation within secondary care or treatment for another condition or a period of recovery before proceeding, and if they will be placed on active monitoring. If a clinical decision is made to stop the RTT clock for active monitoring, the patient’s next steps should be agreed, including timescale for further review or follow-up to assess their condition. The pathway should remain visible on the relevant PTL or waiting list report to support ongoing management
- that the patient is being optimised or otherwise managed within primary care and will be discharged back to the care of their GP (clock stop)
4.13. Admitted pathways
The trust should ensure that patients with a DTA for treatment are captured and monitored on waiting lists. It is worth noting the difference between active RTT patients and planned patients (awaiting admission at a specific clinically defined time).
4.14. Active waiting list
Ideally patients will be fit, ready and available before being added to the admitted waiting list. However, they will be added to the admitted waiting list without delay following a DTA, regardless of whether they have undergone POA or declared a period of unavailability at the point the DTA is made.
The active inpatient or day case waiting lists or PTLs include all patients who are awaiting elective admission. The only exceptions are planned patients, who are awaiting admission at a specific clinically defined time.
Adding a patient to the inpatient or day case waiting list will either:
- continue the RTT clock from the original referral received date
- start a new RTT clock if the surgical procedure is a substantively new treatment that was not part of the original treatment package, providing that another definitive treatment or a period of active monitoring has already occurred
- start a new RTT clock if the patient’s previous clock had been stopped for active monitoring
The RTT clock will stop on admission.
4.15. Patients requiring more than one procedure
If more than one procedure will be performed in the same scheduled slot by the same surgeon, the patient should be added to the waiting list with all the procedures noted. If different surgeons will work together to perform more than one procedure, the patient will be added to the waiting list of the consultant surgeon for the priority procedure, with the additional procedures noted.
Where a patient requires more than one procedure performed on separate occasions, such as first definitive treatment followed by a new decision to treat for a second or subsequent treatment or bilateral procedures that are completed separately, this is an example of multiple RTT periods on the same patient pathway; see section 4.5.
The patient:
- will be added to the active waiting list for the primary (first) procedure
- when the first procedure is complete and the patient is fit and able to proceed with the second procedure, will be added (as a new waiting list entry) to the waiting list and a new RTT clock will start
Note: RTT clocks for bilateral procedures are sequential and not concurrent (nor listed as ‘planned’) as stated in Rule 3a.
Figure 5: Bilateral pathway
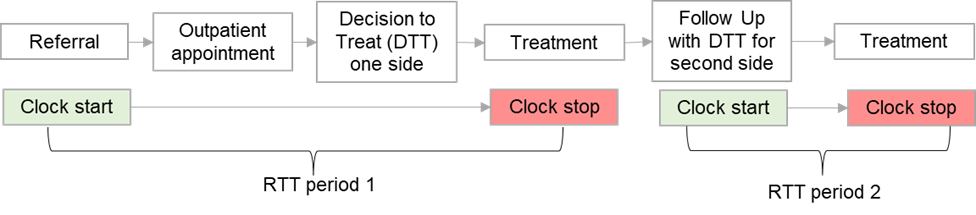
Click here to access explanatory text for figure 5
This diagram shows 2 RTT periods on a bilateral pathway:
RTT period 1:
1. referral (clock start)
2. outpatient appointment
3. decision to treat (DTT) one side
4. treatment (clock stop)
RTT period 2:
1. follow-up with DTT for other side (clock start)
2. treatment (clock stop)
4.16. Planned waiting lists
Patients will only be added to an admitted planned waiting list if there is a clinical reason they need to have a procedure at a specific time or repeated at a specific frequency, such as a repeat colonoscopy. Patients who are on an RTT pathway should not be placed on a planned list if they are unfit or unavailable for a procedure or operation.
A patient’s due date [sometimes locally known as the guaranteed admission date (GAD)] for their planned procedure will be included in the planned waiting list entry. Patients on planned waiting lists will be scheduled for admission at the clinically appropriate time and they should not have to wait any longer after this time has elapsed.
When patients on planned lists awaiting admission for treatment are clinically ready for their treatment to begin and reach their due date for their planned procedure, they will either be admitted for the procedure or transferred to an active waiting list and a new RTT clock will start.
Patients who require a diagnostic test at a specific point in time for clinical reasons (such as for post-treatment surveillance) are exempt from the diagnostic clock rules and will be held on a planned waiting list with a clinically determined due date identified. However, if the patient’s wait goes beyond their due date for the test, they will be transferred to an active waiting list and a new diagnostic clock will start.
4.17. Clinical prioritisation
When a patient is added to the waiting list the clinician should assign them a clinical prioritisation code.
Clinical prioritisation criteria for each elective specialty should be agreed by clinical leads following guidance from respective Royal Colleges. These follow a standard format as detailed below:
|
P code |
Booking timescale |
Review timescale |
|
P1a |
Emergency procedures to be performed in <24 hours – would not usually apply to patients awaiting elective admission |
|
|
P1b |
Procedures to be performed in <72 hours – would not usually apply to patients awaiting elective admission |
|
|
P2 |
Procedures to be performed in <1 month |
1 month |
|
P3 |
Procedures to be performed in <3 months |
3 months |
|
P4 |
Procedures to be performed in >3 months |
6 months |
All patients, including those who have chosen to delay treatment, should be reviewed to make sure their condition or preference has not changed. The maximum time between reviews is 6 months. Reviews should be undertaken in line with the timescale indicated by the patient’s priority category or sooner if appropriate (for example, if a change in the patient’s condition has been highlighted).
4.18. On-the-day cancellations
Where a patient is cancelled on the day of admission or day of surgery for non-clinical reasons, they will be rebooked within 28 days of the original admission date and must be given reasonable notice of the rearranged date. The patient may choose not to accept a date within 28 days.
If it is not possible to offer the patient a date within 28 days of the cancellation, the trust will offer to fund the patient’s treatment at the time and hospital the patient chooses, where appropriate.
5. Glossary
A glossary of terms and acronyms will need to be included for readers unfamiliar with NHS terms. The trust will need to include any cultural or local terminology and ensure the descriptions are based on national or common understanding between trusts.
Active monitoring: where a clinical decision is made to start a period of monitoring in secondary care without clinical intervention or diagnostic procedures. Often referred to as ‘watchful wait’.
Advice and guidance (A&G): by providing a digital communication channel, A&G allows a clinician (often in primary care) to seek advice from another (usually a specialist) before or instead of a referral.
Active waiting list: the list of elective patients who are fit, ready and able to be seen or treated at that point in time. Applicable to any stage of the RTT pathway where patients are waiting for hospital resource reasons.
Appointment slot issue (ASI): a list of patients who have attempted to book their appointment through the national e-Referral Service but have not been successful due to lack of clinic slots.
Bilateral procedures: where a procedure is required on both the right and left sides of the body.
Breach: a pathway where the waiting time to be seen or receive treatment exceeds the access standard, national or local target time.
Clinic outcome form (COF): used to record the RTT outcome and other clinical information after an outpatient appointment.
Consultant-led service: a service where a consultant retains overall responsibility for the care of the patient. Patients may be seen in nurse-led clinics, which come under the umbrella of consultant-led services.
Day case: patients who require admission to hospital for treatment and will need the use of a bed but are not expected to need to stay overnight.
Decision to admit (DTA): where a clinical decision is made to admit the patient for either day case or inpatient treatment.
Direct access: where GPs refer patients to hospital for diagnostic tests only. These patients will not be on an open RTT pathway.
Elective care: any pre-scheduled care that is not within the scope of emergency care.
First definitive treatment (FDT): an intervention intended to manage a patient’s disease, condition or injury and avoid further intervention. What constitutes first definitive treatment is a matter of clinical judgement in consultation with the patient.
Fixed appointments: where an appointment or admission date is sent to the patient without the opportunity to agree a data.
Full booking: where an appointment or admission date is agreed either with the patient at the time of the decision or within 24 hours of the decision.
Incomplete pathways: patients who are waiting for treatment on an open RTT pathway, either at the non-admitted or admitted stage.
Inpatients: patients who require admission to the hospital for treatment and will remain in hospital for at least 1 night.
Integrated care board (ICB): an organisation that brings NHS and care organisations together locally to improve population health and establish shared strategic priorities within the NHS.
Minimum data set (MDS): minimum information required to process a referral either into a trust or out of another trust.
Missed appointment: patients who give no notice of their non-attendance. Also known as did not attends (DNAs).
Nullified: where the RTT clock is discounted from any reporting of RTT performance.
Partial booking: where an appointment or admission date is agreed with the patient close to the time it is due.
Patient administrative system (PAS): records the patient’s demographics (for example, name, home address, date of birth) and details all patient contacts with the hospital, both outpatient and inpatient.
Patient-initiated delay: where the patient declines offers or cancels or does not attend an appointment or admission. This in itself does not the stop the RTT clock. A clinical review must always take place.
Patient initiated follow-up (PIFU): PIFU is when a patient initiates an appointment when they need one, based on their symptoms and individual circumstances.
Patient pathway identifier (PPID): a unique identifier that together with the provider code uniquely identifies a patient pathway.
Patient tracking list (PTL): a tool used for monitoring, scheduling and reporting on patients on elective pathways (covering both RTT and cancer).
Planned waiting list: patients who are to be admitted as part of a planned sequence of treatment or they have to wait for treatment or investigation at a specific time. Patients on planned lists should be booked in for an appointment or treatment at the clinically appropriate time. They are not counted as part of the active waiting list or on an RTT pathway.
Reasonable offers: an offer of an appointment or admission date with 3 weeks’ notice. It is good practice to offer patients 2 reasonable dates.
Referral management centre (RMC): provides a single point of access for professionals to make referrals into providers.
Referral to treatment (RTT): the NHS Constitution sets out that patients should wait no longer than 18 weeks from GP referral to treatment.
Straight to test (STT): arrangements where patients can be referred straight for diagnostics as the first appointment as part of an RTT pathway.
To come in (TCI): the date of admission for an elective surgical procedure or operation.
6. References and further reading
Referral to treatment consultant-led waiting times rules suite (October 2022)
Referral to treatment (RTT) statistics
Evidence-based interventions programme
The NHS Constitution (August 2023)
The NHS Choice framework (August 2023)
Handbook to the NHS Constitution for England (January 2025)
Diagnostics waiting times and activity
Guidance on completing the ‘diagnostic waiting times & activity’ monthly data collection (March 2015)
Frequently asked questions on completing the ‘diagnostic waiting times & activity’ monthly data collection (February 2015)
Supplementary diagnostics FAQs (October 2022)
Equality Act 2010 (June 2015)
Armed Forces Covenant (June 2016)
NHS cost recovery – overseas visitors (December 2024)
Did not attends (DNAs)
Good communication with patients waiting for care (October 2023)
Publication reference: PRN01045

