NHS England has developed a Fit and Proper Person Test (FPPT) Framework in response to recommendations made by Tom Kark KC in his 2019 review of the FPPT (the Kark Review). This also takes into account the requirements of the Care Quality Commission (CQC) in relation to directors being fit and proper for their roles.
In the foreword to his review, Tom Kark KC stated that “The culture and management of each hospital Trust flows from the management team. Thus, the quality and culture of the management team is of the greatest significance to the ethos and success of the hospital, the effectiveness, and the working conditions (in the widest sense) of its staff, and ultimately the care, comfort, and safety of the patients to whom the Trust provides health services.”
The framework will introduce a means of retaining information relating to testing the requirements of the FPPT for individual directors, a set of standard competencies for all board directors, a new way of completing references with additional content whenever a director leaves an NHS board, and extension of the applicability to some other organisations, including NHS England and the CQC.
This framework should be read in conjunction with associated guidance documents.
1. Introduction
1.1 Background
The Kark Review (2019) was commissioned by the government in July 2018 to review the scope, operation and purpose of the Fit and Proper Person Test (FPPT) as it applies under the current Regulation 5 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
This included looking at how effective the FPPT is:
“… in preventing unsuitable staff from being redeployed or re-employed in the NHS, clinical commissioning groups, and independent healthcare and adult social care sectors.”
The review highlighted areas that needed improvement to strengthen the existing regime.
The specific recommendations from the Kark Review (2019) have been detailed in Appendix 1.
1.2 Purpose and benefits
This document supports the implementation of the recommendations from the Kark Review, and promotes the effectiveness of the underlying legal requirements by establishing a Fit and Proper Person Test Framework (also known as the ‘Framework’). The purpose is to strengthen/reinforce individual accountability and transparency for board members, thereby enhancing the quality of leadership within the NHS.
The Framework is effective from 30 September 2023 and should be implemented by all boards going forward from that date. NHS organisations are not expected to collect historic information to populate ESR or local records, but to use the Framework for all new board level appointments or promotions and for annual assessments going forward.
The Framework should be read in conjunction with the NHS Constitution, NHS People Plan, People Promise and NHS Leadership Competency Framework for leaders at board level. This Framework supports transparency and should be the start of an ongoing dialogue between board members about probity and values. It should be seen as a core element of a broader programme of board development, effective appraisals and values-based (as well as competency-based) appointments – all of which are part of the good practice required to build a ‘healthy’ board.
The aim of strengthening the FPPT is to prioritise patient safety and good leadership in NHS organisations. The Framework will help board members build a portfolio to support and provide assurance that they are fit and proper, while demonstrably unfit board members will be prevented from moving between NHS organisations.
The Framework will be fair and proportionate and has been developed with the intention to avoid unnecessary bureaucratic burden on NHS organisations.
Ensuring high standards of leadership in the NHS is crucial – well-led NHS organisations and better-led teams with both strong teamwork and strong governance translate into greater staff wellbeing and better clinical care. This requires accountable board members with both outstanding personal conduct and professional capabilities to effectively oversee NHS organisations that are often under significant financial restraint and operating in a highly regulated environment with public and political scrutiny.
As the FPPT assessment is on an individual basis, rather than in relation to the board as a whole, it is envisaged that aspirant board members who can demonstrate the characteristics described above should not be deterred from seeking to join the board of a more challenged NHS organisation. The FPPT assessment is one of general competence to act as a board member, and situational context should therefore be taken into account.
Ensuring that board members are demonstrating the right behaviours will help the NHS drive its cultural initiatives: namely, to foster a culture of compassion, respect and inclusion, and a feeling of belonging; as well as setting the tone at the top to encourage a listening and speaking up culture.
1.3 Applicability
The Framework applies to the board members of NHS organisations. Within this guidance, the term ‘board member’ is used to refer to:
- both executive directors and non-executive directors (NEDs), irrespective of voting rights
- interim (all contractual forms) as well as permanent appointments
- those individuals who are called ‘directors’ within Regulation 5 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
Those individuals who by virtue of their profession are members of other professional registers, such as the General Medical Council (GMC) or Nursing and Midwifery Council (NMC), should still be assessed against this Framework if they are a board member at an NHS organisation.
The Framework is designed to assess the appropriateness of an individual to effectively discharge their duties in the capacity of a board member.
It is recognised that some organisations may want to extend the FPPT assessment to other key roles, for example, to those individuals who may regularly attend board meetings or otherwise have significant influence on board decisions. The annual submission requirement is, however, limited to board members only.
Within this guidance, the term ‘NHS organisations’ refers to those institutions to which the Framework will apply; for the purposes of this Framework, this includes:
- NHS trusts
- NHS foundation trusts
- integrated care boards (ICBs)
- the following arm’s length bodies in the first instance:
- Care Quality Commission (CQC)
- NHS England.
ICB chairs will need to consider FPPT assessment on a member-by-member basis and take into account assurance received from other recruiting/appointing organisations, for example, in the case of partner members.
1.4 Personal data
Personal data relating to the FPPT assessment will be retained in local record systems and specific data fields in the NHS Electronic Staff Record (ESR). The information contained in these records will not routinely be accessible beyond an individual’s own organisation. There will be no substantive change to the data controller arrangements from those already in place for ESR.
Although, as set out below, NHS England will not have day-to-day access to the system or its content, NHS England recognises that it may be considered a (joint) controller of the ESR fields because as the commissioner of the ESR module and author of the Framework, it has a role in determining the nature and purposes of processing.
The organisations that are uploading the content (and determining what is said about each board member), and the NHS Business Services Authority (as the main commissioner of ESR), will also each be a data controller. For the purposes of Article 26 UK GDPR, NHS England has put in place ‘transparent arrangements’ to set out its responsibilities in this respect.
NHS England has established that the most relevant lawful basis for processing the FPPT data contained in ESR is set out in Article 6(1)(e) UK GDPR. This is on the basis that the processing of personal data is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller (that is, the employer, or indeed NHS England in connection with any role it fulfils as a joint controller).
The aim of the maintaining a record of FPPT outcomes in ESR is to significantly improve the management of the NHS, and ultimately the experience and outcomes for patients, and is therefore in the public interest and done as part of the exercise of the functions of the organisation concerned.
As special category data would be processed as part of the maintenance of the ESR FPPT data fields, controllers will also rely on one of the lawful bases for processing set out in Article 9 UK GDPR: Articles 9(2)(b) – employment; 9(2)(g) – statutory/public functions; and 9(2)(h) (read with Schedule 1, paragraph 2 of the Data Protection Act 2018). This covers processing that is ‘necessary for the management of the health service.’
NHS England recognises the requirements of Article 5(1) UK GDPR, and that personal data should be processed lawfully, fairly and transparently. In line with all other ESR data fields, fair processing information will be available to the users of the ESR system. Current ESR fair processing information can be found in the NHS Electronic Staff Record (ESR) privacy notice. The Framework and related guidance documents also help discharge transparency-related obligations.
Information that is the personal data of the applicant is exempt from the Freedom of Information Act under section 40(1) and any request should be processed under section 7 of the DPA. Regulation 5(3) of the EIR is the equivalent provision and has the same effect.
Arrangements for dispute resolution or request for review of content of data (in ESR and local records), or relating to the FPPT assessment outcome, are set out in the guidance document for chairs.
The launch of the Framework will involve NHS England and participating data controllers (NHS trusts, foundation trusts and integrated care boards) communicating to all board members in their organisation whose details will be included in ESR, in advance of the FPPT Framework (and standard reference tools) going live on 30 September 2023. By doing so directors will be afforded the opportunity to object if they have concerns regarding the proposed use of their data, and NHS England and participating data controllers will be able to consider these concerns and amend their approach if necessary. An example of a board member FPPT privacy template is attached at Appendix 6. Organisations should ensure that an appropriate policy document is in place in relation to special category data.
2. Context
2.1 Current fit and proper persons regulations
In 2014, the government introduced a ‘fit and proper person’ requirement, via Regulation 5 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (the ‘Regulations’).
This sets out the requirements for a FPPT which applies to directors and those performing the functions of, or functions equivalent or similar to the functions of, a director in all NHS organisations registered with the CQC, which includes all licence holders and other NHS organisations to which licence conditions apply. For the purposes of this guidance, we have referred to these individuals as ‘board members’.
Regulation 5 recognises that individuals who have authority in NHS organisations that deliver care are responsible for the overall quality and safety of that care. The regulation requirements are that:
- the individual is of good character
- the individual has the qualifications, competence, skills and experience that are necessary for the relevant office or position or the work for which they are employed.
- the individual is able by reason of their health, after reasonable adjustments are made, of properly performing tasks that are intrinsic to the office or position for which they are appointed or to the work for which they are employed.
- the individual has not been responsible for, contributed to or facilitated any serious misconduct or mismanagement (whether unlawful or not) while carrying out a regulated activity or providing a service elsewhere which, if provided in England, would be a regulated activity.
- none of the grounds of unfitness specified in part 1 of Schedule 4 apply to the individual.
The grounds of unfitness specified in Part 1 of Schedule 4 to the Regulated Activities Regulations are:
- the person is an undischarged bankrupt or a person whose estate has had sequestration awarded in respect of it and who has not been discharged
- the person is the subject of a bankruptcy restrictions order or an interim bankruptcy restrictions order or an order to like effect made in Scotland or Northern Ireland
- the person is a person to whom a moratorium period under a debt relief order applies under Part VIIA (debt relief orders) of the Insolvency Act 1986
- the person has made a composition or arrangement with, or granted a trust deed for, creditors and not been discharged in respect of it
- the person is included in the children’s barred list or the adults’ barred list maintained under section 2 of the Safeguarding Vulnerable Groups Act 2006, or in any corresponding list maintained under an equivalent enactment in force in Scotland or Northern Ireland
- the person is prohibited from holding the relevant office or position, or in the case of an individual from carrying on the regulated activity, by or under any enactment.
The good character requirements referred to above in Regulation 5 are specified in Part 2 of Schedule 4 to the Regulated Activities Regulations, and relate to:
- whether the person has been convicted in the United Kingdom of any offence or been convicted elsewhere of any offence which, if committed in any part of the United Kingdom, would constitute an offence
- whether the person has been erased, removed or struck off a register of professionals maintained by a regulator of health care or social work professionals.
Integrated care boards (ICBs) are statutory bodies with the general function of arranging for the provision of services for the purposes of the health service in England and are NHS bodies for the purposes of the 2006 Act. The main powers and duties of ICBs are to commission certain health services as set out in sections 3 and 3A of the 2006 Act.
ICBs, together with the CQC and NHS England, are within scope of this Framework. One of the recommendations made by Tom Kark KC was to extend the scope of the FPPT into certain arm’s length bodies (ALBs) to:
“…bolster the strength and width of the test, as well as to put a stop to ‘the revolving door,’ the FPPT should be extended to commissioners as well as other arms-length bodies. It was described as ‘incongruous’ that it did not apply to commissioners.”
2.2 Related principles and values
This section summarises relevant principles and values that underpin the Framework and provide additional context to understand its aims.
2.2.1 NHS Constitution
The NHS Constitution states:
The NHS belongs to the people.
It is there to improve our health and wellbeing, supporting us to keep mentally and physically well, to get better when we are ill and, when we cannot fully recover, to stay as well as we can to the end of our lives.
It works at the limits of science – bringing the highest levels of human knowledge and skill to save lives and improve health. It touches our lives at times of basic human need when care and compassion are what matter most.
The NHS is founded on a common set of principles and values that bind together the communities and people it serves – patients and public – and the staff who work for it.
2.2.2 NHS guiding principles
The seven guiding principles that govern the way the NHS operates, and define how it seeks to achieve its purpose:
- The NHS provides a comprehensive service, available to all.
- Access to NHS services is based on clinical need, not an individual’s ability to pay.
- The NHS aspires to the highest standards of excellence and professionalism.
- The patient will be at the heart of everything the NHS does.
- The NHS works across organisational boundaries and in partnership with other organisations in the interest of patients, local communities, and the wider population.
- The NHS is committed to providing best value for taxpayers’ money and the most effective, fair, and sustainable use of finite resources.
- The NHS is accountable to the public, communities, and patients that it serves.
2.2.3 NHS values
These principles are underpinned by the core NHS values, which have been derived from extensive discussions with staff, patients and the public. The values are integral to creating a culture where patients come first in everything the NHS does.
These values are not intended to be limiting. Individual NHS organisations should use them as a basis on which to develop their own values, adapting them to local circumstances. The values should be taken into account when developing services with partner NHS organisations, patients, the public and staff.
The 6 core values are:
- Working together for patients.
- Respect and dignity.
- Commitment to quality of care.
- Compassion.
- Improving lives.
- Everyone counts.
2.2.4 The Nolan Principles of Standards in Public Life
NHS board members, in their capacity as public office holders, are expected to abide by the ‘Nolan Principles’ as defined by the Committee on Standards in Public Life:
1. Selflessness
- Holders of public office should act solely in terms of the public interest.
2. Integrity
- Holders of public office must avoid placing themselves under any obligation to people or organisations that might try inappropriately to influence them in their work. They should not act or take decisions in order to gain financial or other material benefits for themselves, their family or their friends. They must declare and resolve any interests and relationships.
3. Objectivity
- Holders of public office must act and take decisions impartially, fairly and on merit, using the best evidence and without discrimination or bias.
4. Accountability
- Holders of public office are accountable to the public for their decisions and actions and must submit themselves to the scrutiny necessary to ensure this.
5. Openness
- Holders of public office should act and take decisions in an open and transparent manner. Information should not be withheld from the public unless there are clear and lawful reasons for so doing.
6. Honesty
- Holders of public office should be truthful.
7. Leadership
- Holders of public office should exhibit these principles in their own behaviour. They should actively promote and robustly support the principles and be willing to challenge poor behaviour wherever it occurs.
3. FPPT Framework
The Framework sets out:
- When the full FPPT assessment is needed, which includes self-attestations (see sections 3.2 and 3.3).
- New appointment considerations (section 3.4).
- Additional considerations in specific situations such as joint appointments, shared roles and temporary absences (section 3.5).
- The role of the chair in overseeing the FPPT (section 3.6).
- The FPPT core elements to be considered in evaluating board members (section 3.7).
- The circumstances in which there will be breaches to the core elements of the FPPT (regulation 5) (section 3.8).
- The requirements for a board member reference check (section 3.9).
- The requirements for accurately maintaining FPPT information on each board member in the ESR record (section 3.10) – for the purpose of the FPPT framework, ‘ESR’ refers to the FPPT data fields in ESR.
- The record retention requirements (section 3.11).
- Dispute resolution (section 3.12).
- Quality assurance over the Framework (section 4).
Ultimate accountability for adhering to this framework will reside with the chair of an NHS organisation.
Throughout this document and the associated guidance, the term ‘ESR’ refers to the FPPT data fields in ESR. It is important to note that:
- Information held in ESR about board members is accessible by a limited number of senior individuals within their own organisation only.
- There is no access to FPPT information about board members in one organisation by another organisation or individual.
ESR provides a tool for individual organisations to record that testing has been carried out for the chair, who has overall accountability for the FPPT within their organisation. It also records that testing is complete and enables reports to be run at local level as an audit trail of completed testing and sign off.
ESR is not a public register – there is no access to it by the public/externally. It provides a tool to help support chairs record some of their key FPPT requirements and provides a sign-off facility in one place. It is good practice for NHS organisations to report on the high-level outcome of the FPPT assessments in the annual report or elsewhere on their websites.
3.1 FPPT overview
The duty to take account of ‘fit and proper person’ requirements is pervasive, continuous and ongoing. However, for the purposes of the Framework, NHS England considers it appropriate for NHS organisations to be able to consistently demonstrate, on an annualised basis, that a formal assessment of fitness and properness for each board member has been undertaken. NHS organisations should consider carrying out the assessment alongside the annual appraisal.
Chairs should ensure that their NHS organisation can show evidence that appropriate systems and processes are in place to ensure that all new and existing board members are, and continue to be, fit and proper (that is, the board members meet the requirement of Regulation 5), and that no appointments breach any of the criteria set out in Schedule 4 of the regulations.
Such systems and processes include (but are not limited to) recruitment, induction, training, development, performance appraisal, governance committees, disciplinary and dismissal processes.
As such, the chair in each NHS organisation will be responsible for ensuring that their organisation conducts and keeps under review a FPPT (in line with the list in section 3.2 below) to ensure board members are, and remain, suitable for their role.
In evaluating a board member’s fitness, a decision is expected to be reached on the fitness of the board member that is in the range of decisions that a reasonable person would make. NHS England recognises that chairs will need to make judgements about the suitability of board members and will support balanced judgements made in the spirit of the Framework.
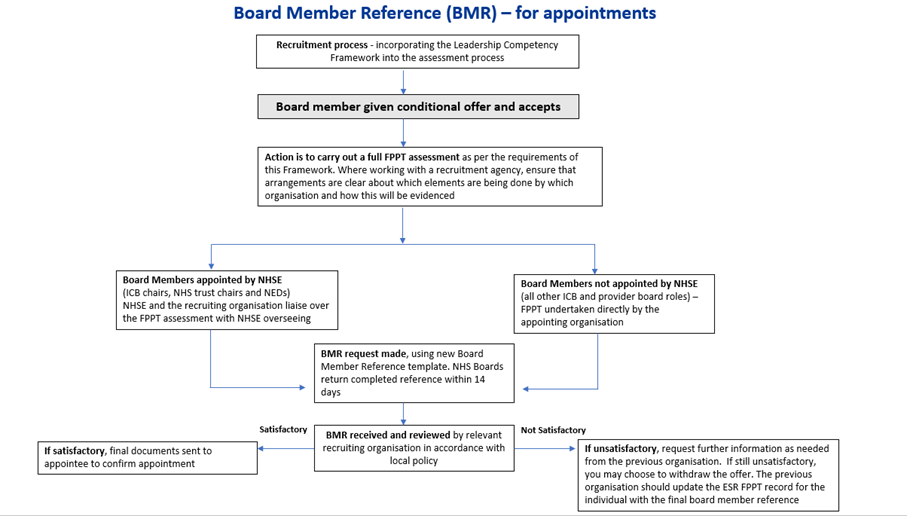
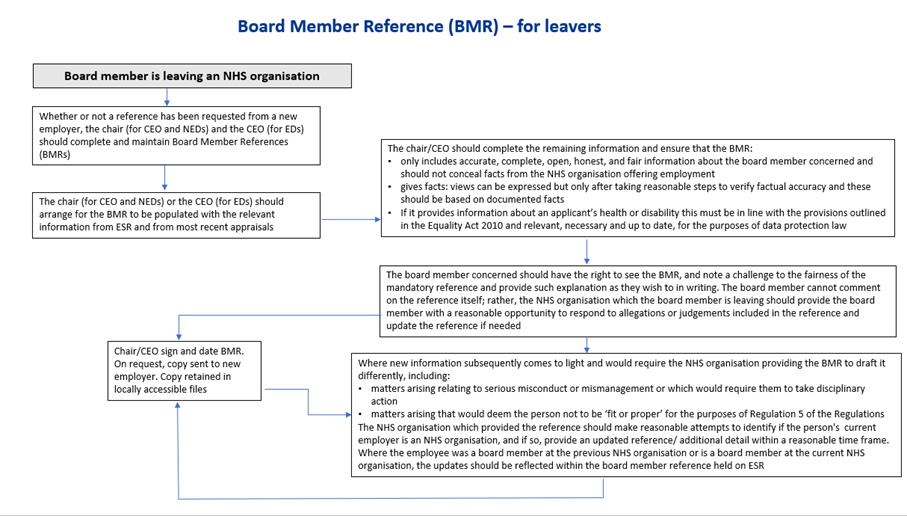
The suggested approach to the assessment, including the Board Member Reference process, is set out in the three flow charts below and is also described in more detail in the supporting chairs’ guidance document.
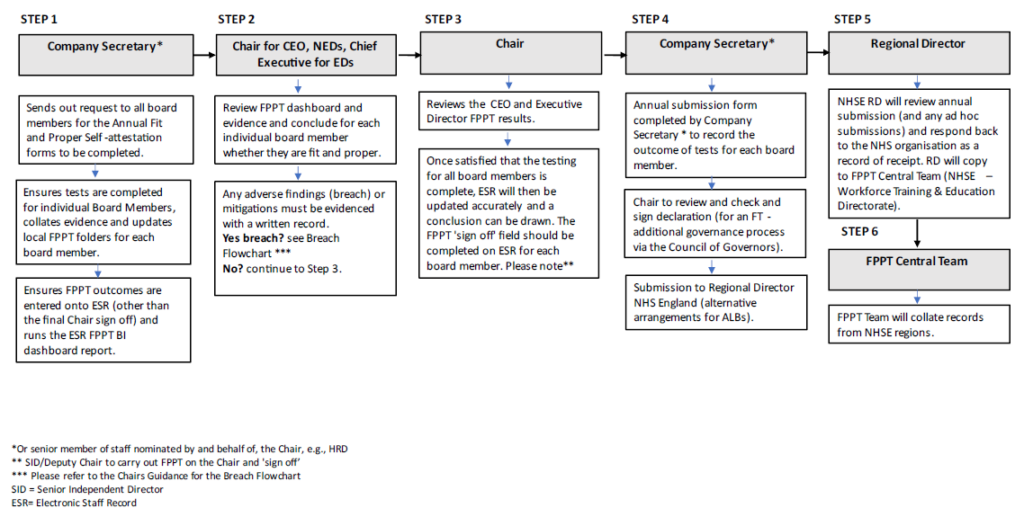
Board members reference (BMR) – for appointments
Board members reference (BMR) – for leavers
3.2 Full FPPT assessment
A documented, full FPPT assessment – a complete assessment by the employing NHS organisation against the core elements (detailed in section 3.7) – will be needed in the following circumstances:
1. New appointments in board member roles, whether permanent or temporary, where greater than six weeks, this covers:
- new appointments that have been promoted within an NHS organisation
- temporary appointments (including secondments) involving acting up into a board role on a non-permanent basis
- existing board members at one NHS organisation who move to another NHS organisation in the role of a board member
- individuals who join an NHS organisation in the role of board member for the first time from an organisation that is outside the NHS.
2. When an individual board member changes role within their current NHS organisation (for instance, if an existing board member moves into a new board role that requires a different skillset, eg chief financial officer).
3. Annually; that is, within a 12-month period of the date of the previous FPPT to review for any changes in the previous 12 months.
Note: for points 1a – 1d above (new appointments) the full FPPT will also include a board member reference check (see section 3.9).
For points 2 and 3 above, the board member reference check will not be needed.
The exact requirements for the initial FPPT assessment versus the annual FPPT assessment thereafter are detailed in section 3.10.1.
3.3 Self-attestation
Every board member will need to complete an annual self-attestation, to confirm that they are in adherence with the FPPT requirements. Self-attestations will be a necessary step that forms a part of the full FPPT assessment (see Appendix 3).
3.4 New appointments
NHS organisations should be able to demonstrate that appointments of new board members are made through a robust and thorough appointment process.
As such, no new appointments should be made to the post of board member unless the appointee concerned can demonstrate they have met the FPPT requirements as detailed in section 3.7 of this document.
As part of conducting the initial appointment process for a board member, an inter-authority transfer (IAT)* could be submitted to identify any of the applicant’s previous or current NHS service/employment history. Alternatively, other arrangements could be made to collate the relevant information. This should also help identify any potential duplicate employment accounts for the appointee, eg when someone has more than one NHS role on ESR.
For the initial appointment of NHS trust chairs and ICB chairs only, once the NHS organisation has obtained board member references and completed the fit and proper person assessment, FPPT approval should be sought from the NHS England Appointments Team before they commence their role.
* An IAT is an electronic way of gathering information from an employer for an applicant’s previous or current NHS service using the ESR system. How to complete an Inter Authority Transfer (IAT) check in NHS Jobs user guide (nhsbsa.nhs.uk)
3.5 Additional considerations
There will be additional considerations when applying the FPPT for joint appointments across NHS organisations, shared roles within the same NHS organisation and periods of temporary absence. These additional considerations have been detailed below.
3.5.1 Joint appointments across different NHS organisations
Additional considerations are needed where there are joint appointments to support closer working between NHS organisations in the health and care system.
For instance, where joint appointments of a board member can help foster joint decision-making, enhance local leadership and improve the delivery of integrated care. Joint appointments may occur where:
- two or more NHS organisations want to create a combined role
- two or more NHS organisations want to employ an individual to work across the different NHS organisations in the same role.
In the scenario of joint appointments, the full FPPT would need to be completed by the designated host/employing NHS organisation and in concluding their assessment they will need input from the chair of the other contracting NHS organisation to ensure that the board member is fit and proper to perform both roles.
The host/employing NHS organisation will then provide a ‘letter of confirmation’ (Appendix 4) to the other contracting NHS organisation to confirm that the board member in question has met the requirements of the FPPT.
The chair of the other contracting NHS organisation has the responsibility to keep the host/employing NHS organisation abreast of changes and any matters that may impact the FPPT assessment of the board member.
Where there is a joint appointment, the host/employing NHS organisation responsible for the FPPT should also lead on conducting the joint appraisal and ensure adequate input from the other contracting NHS organisation.
Where the joint appointment results in a new board member (for the NHS organisation in question), it will constitute a new appointment and as such, the host/employing NHS organisation should provide a ‘letter of confirmation’ to the other NHS organisation(s).
For the avoidance of doubt, where two or more organisations employ or appoint (in the case of a chair or NED) an individual for two or more separate roles at the same time, each organisation has a responsibility to complete the FPPT.
If the FPPT assessment at one organisation finds an individual not to be FPP, the chair should update their counterpart of any other NHS organisation(s) where the individual has a board-level role and explain the reason. To note, the issue at one organisation may be one of role-specific competence, which may not necessarily mean the individual is not FPP at the other organisation.
3.5.2 Shared roles within the same NHS organisation
Where two individuals share responsibility for the same board member role (eg a job share) within the same NHS organisation, both individuals should be assessed against the FPPT requirements in line with sections 3.2 and 3.3.
3.5.3 Temporary absence
For the purpose of the FPPT process, a temporary absence is defined as leave for a period of six consecutive weeks or less (eg sick leave, compassionate leave or parental leave) and where the NHS organisation is leaving the role open for the same board member. As such there is no requirement to approve another permanent individual for the role of board member.
Where there is a temporary absence, it is expected that the HR director/company secretary will liaise with the chair and chief executive to ensure temporary cover is provided; and to ensure that local internal systems are adequately updated to record the start and projected end date of the temporary absence.
Where an individual is appointed as temporary/interim cover and is not already assessed as fit and proper, the NHS organisation should ensure appropriate supervision by an existing board member.
A full FPPT assessment should be undertaken for an individual in an interim cover role exceeding six weeks. Therefore, if the interim cover is expected to be in post for longer than six weeks, the NHS organisation should look to commence the FPPT assessment as soon as possible. Where the period of temporary absence is extended beyond six weeks, the FPPT assessment should commence as soon as the NHS organisation is aware of the extension. This FPPT assessment should be carried out in line with the requirements under section 3.2.
3.6 Role of the chair in overseeing FPPT
Chairs are accountable for taking all reasonable steps to ensure the FPPT process is effective and that the desired culture of their NHS organisation is maintained to support an effective FPPT regime. As such, chairs’ responsibilities are as below:
- Ensure the NHS organisation has proper systems and processes in place so it can make the robust assessments required by the FPPT.
- Ensure the results of the full FPPT, including the annual self-attestations for each board member, are retained by the employing NHS organisation.
- Ensure that the FPPT data fields within ESR are accurately maintained in a timely manner.
- Ensure that the board member references/pre-employment checks (where relevant) and full FPPT (including the annual self-attestation) are complete and adequate for each board member.
- Ensure an appropriate programme is in place to identify and monitor the development needs of board members.
- On appointment of a new board member, consider the specific competence, skills and knowledge of board members to carry out their activities, and how this fits with the overall board.
- Conclude whether the board member is fit and proper.
- Chairs will also complete an annual self-attestation that they themselves are in continued adherence with the FPPT requirements. On an annual basis, chairs should confirm that all board members have completed their own FPPT self-attestation and that the FPPT is being effectively applied in their NHS organisation.
- Ensure that for any board member approved to commence work or continue in post despite there being concerns about a particular aspect of the FPPT, they document the reason(s) as to why there has been an issue about whether a board member might not be fit and proper and the measures taken to address this. A local record of this should be retained. A summary of this should also be included in the annual FPPT submission form (Appendix 5) to the relevant NHS England regional director.
Accountability for ensuring a new board member meets the FPPT assessment criteria will reside with the chair. In making such decisions the chair will be supported by existing processes and committees.
In considering their overall assessment of board members, chairs should confirm points d) and g) are adequately addressed, and where relevant for point i), appropriate action has been taken to address any concern.
It is good practice for the chair to present a report on completion of the annual FPPT in accordance with local policy, to the board in a public meeting and, where applicable, to the Council of Governors for Non-Executive Directors, for information.
3.6.1 Overseeing the role of the chair
Chairs will be subject to the same FPPT requirement, as per sections 3.2 and 3.3. In completing their own annual self-attestation, chairs will effectively be confirming that they have adequately addressed points a), b), c), e), f) and h) of section 3.6 above.
The accountability for ensuring that chairs in NHS trusts, foundation trusts and ICBs meet the FPPT assessment criteria will reside with NHS England regional directors, as is also the case for the chairs’ annual appraisals.
For the chairs of NHS England and the CQC, this accountability will reside with the Department of Health and Social Care (DHSC).
Annually, the senior independent director (SID) or deputy chair will review and ensure that the chair is meeting the requirements of the FPPT.
If the SID and deputy chair are the same individual, another NED should be nominated to review the chair’s FPPT on a rotational basis.
Once the NHS organisation has completed their annual FPPT assessment of the chair, they should sign this off within ESR. The annual FPPT submission, which summarises the results of the FPPT for all board members in the organisation, is then sent to the relevant NHS England regional director.
In relation to foundation trusts, there are no proposed changes to the Council of Governors’ responsibilities in relation to the chair’s FPPT assessment as it is not within the scope of the Framework to do so. However, as the chairs’ annual appraisals are presented to the Council of Governors for information, the same should be the case for a summary of the outcome of the FPPT for non-executive board members.
This information can be retained by the Council of Governors as part of future considerations for any reappointments. Similarly, the Council of Governors should be informed of a satisfactory initial FPPT assessment for new chair and NED appointments.
3.7 FPPT assessment – core elements
This section of the Framework details the core elements that should be included in an FPPT assessment. The checks that underpin the core elements reflect the assessment criteria per Regulation 5 and Schedule 4 of the Regulations.
The full FPPT assessment will constitute an assessment against each of the core elements detailed below and should be conducted in accordance with section 3.2. Individual board members should complete self-attestations to confirm they are fulfilling the core elements of the FPPT assessment, as described below.
NHS organisations should assess board members against the following three core elements when considering whether they are a fit and proper person to perform a board role:
- Good character.
- Possessing the qualifications, competence, skills required and experience.
- Financial soundness.
Note: the FPPT checks relating to these core elements will be in addition to standard employment checks, as per the NHS organisation’s recruitment and selection procedures and NHS Employers’ pre-employment check standard. This can include CV checks, self-attestations, internet searches, proof of qualifications, proof of identity, right to work, etc.
The section below, which considers both Regulation 5 and Schedule 4 of the Regulations, explains matters that the NHS organisation should take account of in relation to the three core elements.
When an NHS organisation assesses a board member against these core elements in relation to being a fit and proper person, they should consider the nature, complexity and activities of their NHS organisation.
3.7.1 Good character
There is no statutory guidance as to how ‘good character’ in Regulation 5 of the 2014 Regulations should be interpreted. Chairs should be aware of the elements to consider when assessing good character (as detailed below).
To encourage openness and transparency, these should not be considered as a strict checklist for compliance, but rather as points for a conversation between the chair (or chief executive for executive board members) and a prospective board member during the appointment process. This will in turn emphasise the ongoing benefits of openness and transparency among board members.
When assessing whether a person is of good character, NHS organisations should follow robust processes to make sure that they gather appropriate information, and must have regard to the matters outlined in Part 1 and Part 2 of Schedule 4, namely:
- Convictions of any offence in the UK.
- Convictions of any offence abroad that constitutes an offence in the UK.
- Whether any regulator or professional body has made the decision to erase, remove or strike off the board member from its register, whether in the UK or abroad.
As such, NHS organisations should conduct:
- A search of the Companies House register to ensure that no board member is disqualified as a director.
- A search of the Charity Commission’s register of removed trustees.
- A Disclosure and Barring Service (DBS) check in line with their local policy requirements:
- each NHS organisation should outline, within their local policy, the relevant DBS check (basic, standard, enhanced, or enhanced with barred lists) required for each individual board member roles; while a 3-year DBS check cycle is a recommended best practice, it is not a mandatory requirement unless specified by local policy
- in defining the required DBS level, NHS organisations should identify those board roles that fall within the definition of a ‘regulated activity’, as defined by the Safeguarding Vulnerable Groups Act 2006, as required barred list checks
- A check with the relevant professional bodies where appropriate.
It is not possible to outline every character trait that a person should have, but it is expected that processes followed take account of a person’s honesty, trustworthiness, reliability, integrity, openness (also referred to as transparency), respectfulness and ability to comply with the law.
Furthermore, in considering that a board member is of ‘good character,’ the relevant NHS organisation should also consider the following in relation to the individual in question:
- Compliance with the law and legal processes.
- Employment tribunal judgements relevant to the board member’s history.
- Settlement agreements relating to dismissal or departure from any healthcare-related service or NHS organisation for any reason other than redundancy.
- A person in whom the NHS organisation, CQC, NHS England, people using services and the wider public can have confidence.
- Adherence to the Nolan Principles of Standards in Public Life.
- The extent to which the board member has been open and honest with the NHS organisation.
- Whether the person has been the subject of any adverse finding or any settlement in civil proceedings, particularly in connection with investment or other financial business, misconduct, fraud or the formation or management of a body corporate.
- Whether the person has been involved – as a director, partner or concerned in management – with a company, partnership or other organisation that has been refused registration, authorisation, membership or a licence to carry out a trade, business or profession.
- Whether the person has been a director, partner or concerned in the management of a business that has gone into insolvency, liquidation or administration while the person has been connected with that organisation or within one year of that connection.
- Whether the person involved as a director, partner or concerned with management of a company has been investigated, disciplined, censured, suspended, or criticised by a regulatory or professional body, a court or tribunal, whether publicly or privately.
- Any other information that may be relevant, such as an upheld/ongoing or discontinued (including where a board member has left the NHS organisation prior to an investigation being completed):
- disciplinary finding
- grievance finding against the board member
- whistleblowing finding against the board member
- finding pursuant to any trust policies or procedures concerning board member behaviour.
3.7.1.1 Serious mismanagement or misconduct
To comply with Regulation 5, consideration of good character should also ensure, as far as possible, the individual has not been responsible for, contributed to or facilitated any serious misconduct or mismanagement (whether unlawful or not) in the course of delivering CQC-regulated activity, in England or equivalent activities elsewhere.
In determining what amounts to ‘serious misconduct or mismanagement,’ beyond the decision by a court or professional regulators regarding individuals, context is paramount. Normally these would require to be findings of serious misconduct or mismanagement that are upheld after a disciplinary process.
NHS organisations should consider the mismanagement and misconduct behaviours in relation to the services they provide, the role of the board member/individual and the possible adverse impact on the NHS organisation or confidence in its ability to carry out its mandate and fulfil its duties in the public interest.
As part of reaching an assessment as to whether any actions or omissions of the board member amount to ‘serious misconduct or mismanagement’, NHS organisations should consider whether an individual board member played a central or peripheral role in any wider misconduct or mismanagement.
The NHS organisation should also consider whether there are any aggravating or mitigating factors; for instance (including but not limited to):
- The extent to which the conduct was deliberate and reckless.
- The extent to which the conduct was dishonest.
- Whether the issues are frequent or have continued over a long period of time.
- If lack of experience contributed to the issue that has been remediated through training.
- The extent to which the board member (or aspirant board member) demonstrates insight and self-reflection in relation to the conduct/issues identified.
Although NHS organisations have information on when convictions, bankruptcies or similar matters are to be considered ‘spent’, there is no time limit for considering serious misconduct or responsibility for failure in a previous role, for the purposes of Regulation 5.
Below are some examples of misconduct and mismanagement that NHS organisations would be expected to conclude as amounting to serious misconduct or mismanagement, unless there are exceptional circumstances that make it unreasonable to determine that there is serious misconduct or mismanagement.
It is impossible to produce a definitive list of all matters that would constitute serious misconduct or mismanagement and, as such, the list below is not exhaustive.
This list sets the minimum expectations and should be read in conjunction with local policy expectations/requirements to determine whether or not a board member has been involved in serious misconduct or mismanagement:
- Fraud or theft.
- Any criminal offence other than minor motoring offences at work (although this and the issues set out in this section may be relevant to assessing whether an individual is of good character more generally).
- Assault.
- Sexual harassment of staff.
- Bullying or harassment.
- Discrimination as per the Equality Act 2010.
- Victimisation (which falls within the scope of the Equality Act 2010) of staff who raise legitimate concerns.
- Any conduct that can be characterised as dishonest, including:
- deliberately transmitting information to a public authority or to any other person, which is known to be false
- submitting or providing false references or inaccurate or misleading information on a CV.
- Disregard for appropriate standards of governance, including resistance to accountability and the undermining of due process.
- Failure to make full and timely reports to the board of significant issues or incidents, including clinical or financial issues.
- Repeated or ongoing tolerance of poor practice, or failure to promote good practice, leading to departure from recognised standards, policies or accepted practices.
- Continued failure to develop and manage business, financial or clinical plans.
In assessing whether misconduct or mismanagement was ‘serious’, regard should be had to all the circumstances. For instance, an NHS organisation could consider isolated incidences of the following types of behaviour to amount to misconduct or mismanagement that does not reach the threshold of seriousness:
- Intermittent poor attendance.
- Failure to follow agreed policies or processes when undertaking management functions where the failures had limited repercussions or limited effects or were for a benevolent or justifiable purpose.
Note: For the purpose of the FPPT Framework, reference to serious misconduct and serious mismanagement should be read in the context of upheld, ongoing and discontinued investigations relevant to FPPT. All misconduct and mismanagement issues that are relevant to other elements of the FPPT Framework such as good character, should be considered.
3.7.2 Qualifications, competence, skills required and experience
NHS organisations need to have appropriate processes for assessing and checking that the candidate holds the required qualifications and has the competence, skills and experience required.
For instance, where possible, checking the websites of the professional bodies to confirm that where required the board member holds the relevant and stated qualification.
Where NHS organisations consider that a board member role requires specific qualifications (for example, the chief financial officer being an accredited accountant, or the chief medical officer being a GMC-registered doctor), they should make this clear and should only appoint those candidates who meet the required specification, including any requirements to be registered with a professional body.
As such, job descriptions and person specifications should be clear in detailing required skills and relevant qualifications and/or memberships. These should be reviewed to ensure that they are appropriate and tailored for each board role.
In assessing competence, skills and experience for the purposes of the FPPT, the NHS organisation should look to use the outcome of their appraisal processes for board members, which will be based on the NHS Leadership Competency Framework (LCF) for board level leaders: a framework that will apply to all NHS organisations.
Given the appraisal process will feed into the full FPPT assessment, the appraisal process should be of an appropriate frequency and should give due consideration to assessing good character and conduct (that is, a behavioural assessment).
The NHS LCF provides guidance for the competence categories against which a board member should be appointed, developed and appraised. The LCF covers the following six competence categories:
- Setting strategy and delivering long term transformation.
- Leading for equality.
- Driving high quality, sustainable outcomes.
- Providing robust governance and assurance.
- Creating a compassionate and inclusive culture.
- Building trusted relationships with partners and communities.
In assessing whether a board member has the competence, skills and experience to be considered fit and proper, the FPPT assessment will:
- not just consider current abilities, but also have regard to the formal training and development the board member has undergone or is undergoing
- take account of the NHS organisation (its size and how it operates) and the activities the board member should perform
- consider whether the board member has adequate time to perform and meet the responsibilities associated with their role.
Regarding formal training:
- NHS organisations should ensure any necessary training is undertaken by board members where gaps in competency have been identified.
- As such, a tailored learning development plan and training framework should support board members.
- Both the development plan and training should be updated and delivered respectively with an appropriate frequency.
- Training constitutes continued development for board members.
- Those consistently failing to undergo required training in a timely manner should be deemed to have missed an important obligation, and appropriate action should be taken in line with the NHS organisation’s policies and procedures.
- In turn, this may mean that a board member is not fit and proper.
3.7.2.1 Reasonable adjustments
In assessing if a board member can properly perform tasks to the requisite level of competence and skill for the office or position for which they are appointed, consideration will be given to their physical and mental health in accordance with the demands of the role and good occupational health practice.
This means all reasonable steps must be made to make adjustments for people to enable them to carry out their role. As a minimum, these must be in line with requirements to make reasonable adjustments for employees under the Equality Act 2010; to prevent discrimination as defined by the Act.
Hence when appointing a person to a role, NHS organisations should have processes for considering their physical and mental health in line with the requirements of the role.
As such, NHS organisations should undertake occupational health assessments (OHA) for potential new board member appointments, in circumstances where the individual in question has indicated a physical or mental health condition as part of pre-employment checks (eg medical assessment questionnaire).
The results of the OHA should be evaluated, and relevant reasonable adjustments should be made in line with the requirements under the Equality Act 2010, so an individual can carry out their role.
While the OHA will not form part of the annual FPPT, it is an integral component of the recruitment process checks to ensure that the NHS organisation can demonstrate that they have taken account of and made any such reasonable adjustments for those in board member roles. This obligation is ongoing in relation to those with disabilities for the purposes of the Equality Act 2010.
The statutory duty to make reasonable adjustments must be considered on an ongoing basis and applies where a disabled person is put at a substantial disadvantage.
3.7.3 Financial soundness
NHS organisations must seek appropriate information to assure themselves that board members do not meet any of the elements of the unfit person test set out in Schedule 4 Part 1 of the regulations.
Robust processes should be in place to assess board members in relation to bankruptcy, sequestration, insolvency and arrangements with creditors. This, as a minimum, will include search of the insolvency and bankruptcy register and checks over county court judgement (CCJ) or high court judgement for debt.
3.8 Breaches to core elements of the FPPT (Regulation 5)
1. A board member is unfit on the grounds of character, such as:
- an undischarged conviction
- being erased, removed or struck-off a register of professionals maintained by a regulator of healthcare, social work professionals or other professional bodies across different industries
- being prohibited from holding a relevant office or position (see section 3.7.1).
2. A board member is also unfit on the grounds of character if they have been responsible for, contributed to or facilitated any serious misconduct or mismanagement (whether lawful or not) in the course of carrying out a regulated activity.
3. A board member is unfit should they fail to meet the relevant qualifications or fail to have the relevant competence, skills and experience as deemed required for their role.
4. A board member is unfit on grounds of financial soundness, such as a relevant undischarged bankruptcy or being placed under a debt relief order.
5. An NHS organisation does not have a proper process in place to make the robust assessments required by the Regulations.
6. On receipt of information about a board member’s fitness, a decision is reached on the board member that is not in the range of decisions a reasonable person would be expected to reach.
With regards to the above points, it is acknowledged that there could be circumstances where, for instance, board members are deemed competent but do not hold relevant qualifications.
In such circumstances there should be a documented explanation, approved by the chair, as to why the individual in question is deemed fit to be appointed as a board member, or fit to continue in role if they are an existing board member. This should be recorded in the annual return to the NHS England regional director (Appendix 5 part 2).
Furthermore, there may be a limited number of exceptional cases where a board member is deemed unfit (that is, they failed the FPPT) for a particular reason (other than qualifications) but the NHS organisation appoints them or allows them to continue their current employment as a board member.
In such circumstances there should be a documented explanation as to why the board member is unfit and the mitigations taken, which is approved by the chair. This should be submitted to the relevant NHS England regional director for review, either as part of the annual FPPT submission for the NHS organisation, or on an ad hoc basis as a case arises.
The NHS organisation shall determine breaches based on points 1 to 4, whereas any regulatory inspections, such as a CQC inspection will determine breaches of points 5 and 6.
3.9 Board member references
3.9.1 Content of the references
A standardised board member reference is being introduced to ensure greater transparency, robustness and consistency of approach when appointing board members within the NHS.
The aim of this is to help foster a culture of meritocracy, ensuring that only board members who are fit and proper are appointed to their role, and that there is no recycling of unfit individuals within the NHS.
The Leadership Competency Framework will help inform the ‘fitness’ assessment in FPPT. This is in line with the Kark Review’s (2019) recommendations on professional standards.
The Leadership Competency Framework references six competency domains which should be incorporated into all senior leader job descriptions and recruitment processes. It will also form the core of board appraisal frameworks, alongside appraisal of delivery against personal and corporate objectives.
The competency domains in the Leadership Competency Framework should be taken into account when the board member reference is written. It is recognised that no board director will be able to demonstrate how they meet all the competencies in the framework. What is sought as part of the board member reference is evidence of broad competence across each of the six competency domains, and to ensure there are no areas of significant lack of competence which may not be remedied through a development plan.
Board level leaders will be asked to attest to whether they have the requisite experience and skills to fulfil minimum standards against the six competency domains. This attestation will be reviewed by the board director’s line manager and overseen by the organisation’s chair. The attestation record will be captured on ESR.
The annual attestation by board members is expected to be undertaken at the same time as the annual appraisal process and assessment of competence against the six competency domains will also be used to guide the board member’s development plan for the coming year. The line manager will also capture stakeholder feedback as part of the appraisal process and summarise competence against each of the six competency domains. (A board member appraisal framework will be published ahead of the 2023/2024 appraisal process to support this process.) The annual appraisals of the past three years will then be used to guide the board member’s reference.
NHS organisations will need to request board member references, and store information relating to these references (see section 3.10) so that it is available for future checks; and use it to support the full FPPT assessment on initial appointment.
NHS organisations should maintain complete and accurate board member references at the point where the board member departs, irrespective of whether there has been a request from another NHS employer and including in circumstances of retirement. Both the initial and board member references should be retained locally.
Board member references will apply as part of the FPPT assessment when there are new board member appointments, either internal to a particular NHS organisation, internal to the NHS, or external to the NHS. This applies whether permanent or temporary where greater than six weeks; specifically:
- New appointments that have been promoted within an NHS organisation.
- Existing board members at one NHS organisation who move to another NHS organisation in the role of a board member.
- Individuals who join an NHS organisation in the role of board member for the first time from an organisation that is outside of the NHS.
- Individuals who have been a board member in an NHS organisation and join another NHS organisation not in the role of board member, that is, they take a non-Board level role.
It is important that board member references checks are carried out in accordance with the data protection principles, as set out within data protection law. In particular, the process should be undertaken fairly, and the information generated should be accurate and up to date.
Requests for board member references should not ask for specific information on whether there is a settlement agreement/non-disclosure agreement in place.
The board member reference request instead asks for any further information and concerns about an applicant’s fitness and propriety, relevant to the FPPT to fulfil the role as a director, be it executive or non-executive.
Information on settlement agreements should be retained locally (where applicable) and included in the overall consideration of the fit and proper status of the individual in question.
If there is a historical settlement agreement/non-disclosure agreement already in place which includes a confidentiality clause, NHS organisations should seek permission from all parties prior to including any such information in a board member reference.
Going forward, NHS organisations should consider inclusion of a term in any proposed settlement agreement to state that information about the settlement agreement can be included in ESR, and in doing so will not be a breach of confidence.
The existence of a settlement agreement does not, in and of itself determine that a person is not fit or proper to be a board member.
The board member reference is based on the standard NHS reference and includes additional requests for information as follows (relevant to the FPPT):
Discontinued investigations are included in the reference request to identify issues around serious misconduct and mismanagement and to deliberately separate them from issues around qualifications, competence, skills, and experience (which it is believed can be remedied) and health (which it is believed can improve), unless such competence and/or health issues could potentially lead to an individual not meeting the requirements of the FPPT.
Investigations (irrespective of reason for discontinuance) should be limited to those which are applicable and potentially relevant to the FPPT, and examples are as follows (this is not an exhaustive list and consideration will be needed on a case-by-case basis):
- Relating to serious misconduct, behaviour and not being of good character (as described in the FPPT Framework).
- Dishonesty.
- Suppression of the ability of people to speak up about serious issues in the NHS, eg whether by allowing bullying or victimisation of those who speak up or blow the whistle, or any harassment of individuals.
- Any behaviour contrary to the professional Duty of Candour which applies to health and care professionals, eg falsification of records or relevant information.
The reason for discontinuing (including not commencing) an investigation should be recorded, including whether an investigation was not started or stopped because a compromise, confidentiality or settlement agreement was then put in place (recognising that such an agreement is not necessarily a conclusion that someone is not fit and proper for the purposes of the FPPT).
It will be necessary as a matter of fairness for the employee to have had an opportunity to comment on information that is likely to be disclosed as part of any reference request i.e., as part of any disciplinary procedures/action. NHS organisations should develop local policy about who provides references, when they are provided and what will/will not be included.
NHS organisations should take any advice that they deem necessary in an individual case where they have assessed that the employee or prospective employer is likely to bring a claim.
3.9.2 Obtaining references
At least one board member reference should be obtained when an NHS organisation is appointing a board member.
- For board members:
- An NHS organisation should obtain a minimum of two board member references (using the board member reference template) where the individual is from outside the NHS, or from within the NHS but moving into the board role for the first time.
- These two references should come from different employers, where possible.
- For an individual who moves from one NHS board role to another NHS board role, across NHS organisations:
- Where possible one reference from a separate organisation in addition to the board member reference for the current board role will suffice.
- This is because their board member reference template should be completed in line with the requirements of the framework so that NHS organisations can maintain accurate references when a board member departs.
- For a person joining from another NHS organisation:
- The new employing/appointing NHS organisation should take reasonable steps to obtain the appropriate references from the person’s current employer as well as previous employer(s) within the past six years.
- These references should establish the primary facts as per the board member reference template.
- Where an employee is entering the NHS for the first time or coming from a post which was not at board member level:
- The new employing NHS organisation should make every practical effort to obtain such a reference which fulfils the board member reference requirements.
- In this scenario, the NHS organisation will determine their own reasonable steps to satisfy themselves they have pursued relevant avenues to obtain the information on potential incoming individuals through alternative means.
- For example, if a chief financial officer is joining from financial services, they can check the financial services register, or request for a mandatory reference under the financial services regulations.
It is acknowledged that where the previous employer is not an NHS organisation, there may be greater difficulty in obtaining a standardised NHS board member reference.
Nonetheless, for new appointments from outside of the NHS, employers should seek the necessary references to validate a period of six consecutive years of continuous employment (or provide an explanation for any gaps), or training immediately prior to the application being made.
In such cases where references from previous employers are unattainable for the previous six years, additional character or personal references should be sought. Character and personal references should be sought from personal acquaintances who are not related to the applicant, and who do not hold any financial arrangements with that individual.
References should never be used as the sole grounds for assessing an applicant’s suitability for a post. Where negative issues are included in a reference, information should be carefully considered and weighed up against the wider range of evidence gathered as part of the recruitment process.
NHS organisations should aim to investigate negative information by sensitively raising it with the individual concerned, giving them the opportunity to explain the situation in more detail and/or, where appropriate, give them a chance to outline any learning from past mistakes or experiences to obtain the necessary assurances about their suitability for a role.
If a reference reveals something which is incompatible with the requirements of Regulation 5 of the Regulations, the individual should not be appointed to the role.
An NHS organisation should obtain references before the start of the board member’s appointment. The NHS organisation requesting the reference should make it clear that this is being requested in relation to a person being appointed to the role of board member, or for other purposes linked to the board member’s current employment.
The obligation to obtain a reference for a potential candidate for employment/
appointment in the role of board member applies irrespective of how the previous employment ended, for instance, resignation, redundancy, dismissal or fixed term work or temporary work coming to an end.
Where a potential candidate for employment/appointment in the role of board member has a gap between different employments, all reasonable efforts should be made to ensure that references covering those periods/gaps are obtained.
References should be obtained in writing (either via hardcopy or email) and NHS organisations will need to satisfy themselves that both the referee and the organisation are bona fide.
From time to time the information provided in a reference may contradict the information provided by board members.
There may be a reasonable explanation for apparent discrepancies and NHS organisations should proceed sensitively to seek the necessary assurances directly with the board member. In exceptional circumstances where there is serious misdirection, employers may feel it appropriate to report their concerns to the NHS Counter Fraud Authority.
Where an NHS organisation is unable to fully evidence that the incoming board member is fit and proper because of gaps in the board member reference, they may continue to hire the individual but should clearly document within ESR the gaps in relation to the board member reference and the reasons/mitigations for being comfortable with employing/appointing the board member.
In this scenario, the employing NHS organisation also should be able to demonstrate that they have exercised all reasonable attempts to obtain the missing information.
3.9.3 Providing references
An NHS organisation should aim to provide a reference to another NHS organisation within a 14-day period, which starts from the date that the reference request was received. However, it should be acknowledged thar there are occasions of exceptional circumstances, and references may take more than 14 days to provide.
The references referred to above are for a request made in relation to the individual being appointed to the role of board member, or for other purposes linked to the board member’s current employment.
Where a current board member moves between different NHS organisations, a board member reference form following a standard format (Appendix 2) should be completed by the employer and signed off by the chair of that NHS organisation.
The previous NHS organisation should provide information in relation to that which occurred:
- in the six years before the request for a reference
- between the date of the request for the reference and the date the reference is given
- in the case of disciplinary action, serious misconduct and/or mismanagement at any time (where known).
NHS organisations should also consider when providing the reference:
- That the process captures accurate, complete, open, honest and fair information about the board member concerned.
- As such, references should not conceal facts from the NHS organisation offering employment.
- References should give established facts that are part of the history of the person.
- It is unfair to give partial facts if those result in the offer being withdrawn, for example where this causes the recipient NHS organisation to assume the information is missing because it is negative, so the offer is withdrawn.
- Views can be expressed but only after taking reasonable steps to verify factual accuracy and should be based on documented facts.
- The reference should be fair, such that the employee concerned should have the right to note a challenge to the fairness of the mandatory reference and provide such explanation as they wish to in writing.
- This does not mean that the board member can comment on the reference itself; rather, that the NHS organisation (which the board member is leaving) has provided those board members with a reasonable opportunity to respond to allegations or judgements upon which the reference is based.
- Hence a board member’s opinions are not required to be included within the reference, but should be appropriately considered when drafting them.
- Where the NHS organisation providing the reference has not offered the employee the opportunity to previously (at the time the matter occurred) comment on the allegation, they ought to do so before including that allegation within the reference, rather than leaving the allegation out of the reference.
- Where the reference provides information about an applicant’s health or disability this must be in line with the provisions outlined in the Equality Act 2010 and be relevant, necessary, and up to date, for the purposes of data protection law.
3.9.4 Revising references
If an NHS organisation has provided a reference to another NHS organisation about an employee or former employee, and has subsequently:
- become aware of matters or circumstances that would require them to draft the reference differently
- determined that there are matters arising relating to serious misconduct or mismanagement
- determined that there are matters arising which would require them to take disciplinary action
- concluded there are matters arising that would deem the person not to be ‘fit or proper’ for the purposes of Regulation 5 of the Regulations,
The NHS organisation that provided the reference should make reasonable attempts to identify if the person’s* current employer is an NHS organisation and, if so, provide an updated reference/additional detail within a reasonable timeframe.
Where the employee was a board member at the previous NHS organisation or is a board member at the current NHS organisation, the updates should be reflected within the board member reference.
Revised references between NHS organisations should cover a six-year period from the date the initial board member reference was provided, or the date the person ceased employment with the NHS organisation, whichever is later. The exception to this are matters that constitute serious misconduct or mismanagement: details of such events should be provided irrespective of time period.
* For the avoidance of doubt, this refers to executive board members employed by an NHS organisation and non-executive board members who have been appointed.
3.9.5 Board member reference template
The board member reference template provided should be used by NHS organisations.
This Framework, along with the board member reference template, sets out the minimum requirements for a reference. An NHS organisation can provide information in relation to additional matters if it deems it necessary to do so.
If references are provided for the role of board member, or for other purposes linked to the board member’s current employment, the NHS organisation providing the reference should look to complete all sections of the template even where the NHS organisation requesting the reference does not specifically ask for it.
As mentioned previously, NHS organisations should maintain board member references at the point where the board member departs, irrespective of whether there has been a request from another NHS employer.
Therefore, the template should be completed, and retained locally in an accessible archive, for departing board members even where they have indicated they are moving onto a non-NHS role and/or performing a role that is not on the board, or where they have indicated they are to retire.
Often in these circumstances the individual may go on to act in the capacity of a board member at a future date, even if it is just on a temporary basis, for example to cover staff shortages.
The BMR template can be accessed via the HR Forms Dashboard on ESR A manual copy can be located here. This template is to be used should there be a technical issue with ESR or for external recruitment where there is no information held on ESR for the newly appointed board member. The completed form is to be retained locally.
3.10 Electronic Staff Record (ESR)
NHS Business Services Authority (NHSBSA) hosts ESR on behalf of the NHS, as commissioned by the Department for Health and Social Care.
New data fields in ESR will hold individual FPPT information for all board members operating in the NHS and will be used to support recruitment referencing and ongoing development of board members. The FPPT information within ESR is only accessible within the board member’s own organisation and there is no public register.
ESR will hold information about each board member in line with the criteria detailed below in section 3.10.1.
NHS England will use its network of regional directors in a direct oversight role to ensure that individual NHS organisations (within the designated regions) are completing their FPPT, via annual submissions to the NHS England regional directors.
The CQC will continue in its regulatory role and as such may determine that reviews are required over the data integrity and controls that a particular NHS organisation has in relation to the records held in ESR.
There should be limited access to ESR in accordance with local policy and in compliance with data protection law. It is reasonably expected that the following individuals have access to the FPPT fields in ESR:
- chair
- chief executive officer (CEO)
- senior independent director (SID)
- deputy chair
- company secretary
- human resources director (HRD)/chief people officer (CPO).
Access will also be provided to relevant individuals within the CQC at a local level, where this information is necessary for their roles, noting the CQC’s ability to require information to be provided to it under Regulation 5(5) of the Regulations.
The ESR FPPT data fields need to be maintained to ensure information about the serving board member is current. This will mean that ESR is specifically updated for:
- all board members within an NHS organisation
- new board members who have been appointed within an NHS organisation
- whenever there has been a relevant change to one of the fields of FPPT information held in ESR (as per section 3.10.1 below)
- updates for annual completion of the full FPPT
- annual completion of FPPT confirmed by chairs.
It will be the responsibility of each NHS organisation to ensure that ESR remains current and is updated for relevant changes in a timely manner. As a minimum it is expected that each NHS organisation conducts an annual review to verify that ESR is appropriately maintained.
The chair will be accountable for ensuring that the information in ESR is up to date for their organisation.
NHS organisations will need to establish policies and procedures for collating the relevant information in an accurate, complete and timely manner for updating ESR.
NHS organisations will need to establish a process for individuals to access and exercise their rights in connection with the information held about them, in accordance with the requirements of data protection law.
3.10.1 Information held in ESR
The information that ESR will hold about board members is detailed below and also summarised in the FPPT checklist.
The supplementary guidance document provides specific step-by-step instructions for NHS organisations to update and maintain ESR.
The FPPT assessment on initial appointment of a board member will cover all points mentioned below:
- First name*
- Second name/surname*
- Organisation* (that is, current employer)
- Staff group*
- Job title* (that is, current job description)
- Occupation code*
- Position title*
- Employment history:*
- This would include detail of all job titles, organisation departments, dates, and role descriptions.
- Any gaps that are because of any protected characteristics, as defined in the Equality Act 2010, would not need to be explained.
- Training and development
- References:*
- Available references from previous employers, board member references, including resignations or early retirement.
- Last appraisal and date
- Disciplinary findings
- That is, any upheld finding pursuant to any trust policies or procedures concerning employee behaviour, such as misconduct or mismanagement, this includes grievance (upheld) against the board member, whistleblowing claims against the board member (upheld) and employee behaviour upheld finding.
- Any ongoing and discontinued investigations relating to Disciplinary/ Grievance/Whistleblowing/Employee behaviour should also be recorded.
- Type of DBS disclosed* †
- Date DBS received* †
- Disqualified directors register check
- Date of medical clearance* (including confirmation of OHA)
- Date of professional register check (eg membership of professional bodies)
- Insolvency check
- Settlement agreements
- Self-attestation form signed
- Social media check
- Employment tribunal judgement check
- Disqualification from being a charity trustee check
- Board member reference*
- Sign-off by chair/CEO.
It should also be noted that the national insurance number is an additional check where there may have been a change of name highlighted in the initial or annual assessment.
The annual FPPT requires an NHS organisation to validate all fields above – except for:
Fields marked with an asterisk (*) – these do not require validation as part of the annual FPPT unless a specific reason arises. However, these fields should still be updated in the event of a change to the information held.
DBS check requirements should align with the organisation’s local policy, as outlined in section 3.7.1.
3.11 Record retention
The ESR FPPT data fields will retain records of completed tests to support the FPPT assessments. All supporting documents/records in relation to the FPPT will be held locally by each individual NHS organisation.
As such, an NHS organisation should establish, implement and maintain adequate policies and procedures to comply with GDPR and the NHS Records Management Code of Practice.
The NHS Records Management Code of Practice sets out expectations in relation to retaining actual staff documents/records for a period of six years.
However, NHS organisational case documents/records may be retained for longer than the standard six years, based on the facts of the case. This will be a local decision for each NHS organisation.
When determining how long to retain documents/records in relation to disciplinary and similar cases and where applicable, NHS organisations should make an assessment as to the severity of the misconduct and/or mismanagement and its impact to the FPPT. The more serious the issue the longer the retention period should be.
In relation to ESR, the information and accompanying references should be kept career long, which at a minimum should be until the 75th birthday of the board member.
3.12 Dispute resolution
1. Data and information
Where a board member identifies an issue with data held about them in relation to the FPPT, they should request a review which should be conducted in accordance with local policies in the first instance.
Where this does not lead to a satisfactory resolution for the board member, the following options are available:
- For NHS England-appointed board members (NHS trust chairs and NEDs and ICB Chairs) – the matter should be escalated to the NHS England Appointments Team.
- For chairs not appointed by NHS England – a further request for review can be made to the SID or deputy chair who would establish a process proportionate to the matter being considered; for example, establishing a panel with at least one independent member.
- For all other board members (including NHS England-appointed board members, and chairs not appointed by NHS England where the above processes have not led to a satisfactory conclusion), the options could include:
- referring the matter to the ICO
- (For executive director roles only*) taking the matter to an employment tribunal (ET)
- instigating civil proceedings.
2. Outcome of FPPT assessment
Where a board member disagrees with the outcome of the FPPT assessment and they have been deemed ‘not fit and proper,’ the following options are available:
- For NHS England-appointed board member roles – the matter should be escalated to the NHS England Appointments Team for investigation in accordance with extant policy and procedure.
- Where this results in a board member being terminated from their appointed role, a BMR** must be completed and retained by the local organisation in accordance with the Framework.
- For non-NHS England-appointed roles (executive and non-executive) – local policy and constitution arrangements should be followed first.
- NHS organisations may wish to take their own legal advice or seek advice from NHS England.
At any point, employees have the right to take the matter to an ET*.
* Chair and non-executive board members cannot take their organisation to ET unless in relation to discrimination, but they can instigate civil proceedings.
** Exit BMR to be drafted by local chair for non-executive directors [NEDs] (with support from the NHS England Appointments Team), and by the NHS England Appointments Team for chairs.
4. Quality assurance and governance
To ensure that the FPPT is being adequately embedded within NHS organisations there will need to be quality assurance checks conducted by the CQC, NHS England and an external/independent review. The quality assurance checks over the various parts of the FPPT Framework have been detailed below.
4.1 CQC quality assurance
The CQC’s role is to ensure NHS organisations have robust processes in place to adequately perform the FPPT assessments, and to adhere to the requirements of Regulation 5 of the Regulations. As such, as part of the Well Led reviews, CQC will consider the:
- quality of processes and controls supporting the FPPT
- quality of individual FPPT assessments
- board member references, both in relation to the new employing NHS organisation but also in relation to the NHS organisation which wrote the reference
- collation and quality of data within the database and local FPPT records.
In doing so the CQC will have regard to the evidence that exists as to whether the board members meet the FPPT. For example, this includes, but is not limited to, checking the following forms of evidence:
- That the NHS organisation in question is aware of the various guidelines on recruiting board members and that they have implemented procedures in line with this best practice.
- Personnel files of recently appointed board members (including internal appointments of existing staff).
- Information or records relating to appraisals for board members.
- References and personal development plans.
The CQC may intervene where there is evidence that proper processes have not been followed or are not in place for FPPT. While the CQC does not investigate individual board members, it will pass on all information of concern that is received about the fitness of a board member to the relevant NHS organisation.
The CQC will notify NHS organisations of all concerns relating to their board member and ask them to assess the information received. The board member to whom the case refers will also be informed.
NHS organisations should then detail the steps they have taken to assure the fitness of the board member and provide the CQC with a full response within 10 days. The CQC will then carefully review and consider all information.
Where the CQC finds that the NHS organisation’s processes are not robust, or an unreasonable decision has been made, they will either:
- contact the NHS organisation for further discussion
- schedule a focused inspection
- take regulatory action in line with their enforcement policy and decision tree if a clear breach of regulation is identified.
4.2 NHS England quality assurance
NHS England will have oversight through receipt and review of the annual FPPT submissions to the relevant NHS England regional director from NHS organisations.
4.3 Internal audit/external review
Every three years, NHS organisations should have an internal audit to assess the processes, controls and compliance supporting the FPPT assessments. The internal audit should include sample testing of FPPT assessment and associated documentation.
NHS organisations should consider inclusion of FPPT process and testing in the specification for any commissioned Well-Led/board effectiveness reviews.
4.4 Governance
For good governance, organisations should be clear about the reporting arrangements across the FPPT cycle. This is likely to include:
- an update to a meeting of the board in public to confirm that the requirements for FPPT assessment have been satisfied at least annually
- consideration by the Audit Committee, for example where there is a related internal or external audit review included in the audit programme
- relevant information to the Council of Governors (CoG) in an NHS foundation trust as described in section 4.5 below.
4.5 NHS foundation trusts – appointment and removal of the chair and non-executive directors
The document ‘Your statutory duties- A reference guide for NHS foundation trust governors’ refers to the role of the CoG in appointing and removing the chair and NEDs. The FPPT Framework should be considered alongside this document and the local trust constitution. The CoG in an NHS foundation trust:
- Should continue to make chair and NED appointments in accordance with their statutory duties and local constitution. These continue to be subject to satisfactory recruitment checks, and this will now include consideration of the initial FPPT assessment.
- Should continue to ‘…receive performance information for the chair and other non-executive directors as part of a rigorous performance appraisal process …’ in accordance with their local constitution. Performance appraisals will now include application of the LCF in accordance with the Framework.
- Should be advised of any outcome from a non-executive board member (including the chair) FPPT assessment as ‘not fit and proper.’ Dependent on the circumstances and in accordance with the local constitution, the CoG would be involved as appropriate with any subsequent removal process, where applicable.
The CoG should receive support from the SID and/or the company secretary and use the governance arrangements already in place in their trusts, such as the nomination committee.
4.6 Integrated care boards
ICBs should apply the Framework alongside relevant statutory requirements and the existing requirements of their organisation’s constitution.

