Equality and health inequalities statement
This operational guidance sets out the principles that should underpin the planning, design and delivery of an autism assessment pathway that works for everyone irrespective of where they live, their background, age, ethnicity, sex, gender, sexuality, disability, or health conditions. Implementation of this operational guidance will include taking actions to reduce known sources of health inequality that exist in access to, or experiences of, an autism assessment across England.
Overview
This operational guidance sits alongside the national framework to deliver improved outcomes in all-age autism assessment pathways. It provides an overview of common roles and responsibilities that autism assessment services have. These include conducting autism assessments, as well as providing training, consultation and liaison, and supervision, to a range of local and regional services and organisations.
Part 1 of this operational guidance outlines key components of the autism assessment pathway. These are underpinned by ten key principles that should guide decision making about the design, procurement, delivery and evaluation of all services that comprise the autism assessment offer within the area, notably that this is:
- ethical
- evidence based
- respectful
- delivered by an appropriately skilled multidisciplinary workforce
- a comprehensive, coherent offer
- accessible to everyone
- co-designed by clinicians and people who access the services
- based on shared and current conceptualisation of autism
- transparent
- described in, and informed by, national statistical data.
Part 2 of this operational guidance outlines considerations for conducting autism assessments that differ from standard service delivery, such as using telehealth or seeing people who are in hospital or a forensic setting.
Part 3 focuses on the provision of autism-relevant training, consultation and liaison, and supervision.
For more information about the design, procurement, delivery and evaluation of accessible and effective autism assessment services, please refer to the national framework, which should be read in conjunction with this operational guidance. The national framework document outlines a brief overview of the most relevant policy context, general principles underpinning autism assessment service and how to apply these principles when commissioning.
Part 1.The autism assessment pathway
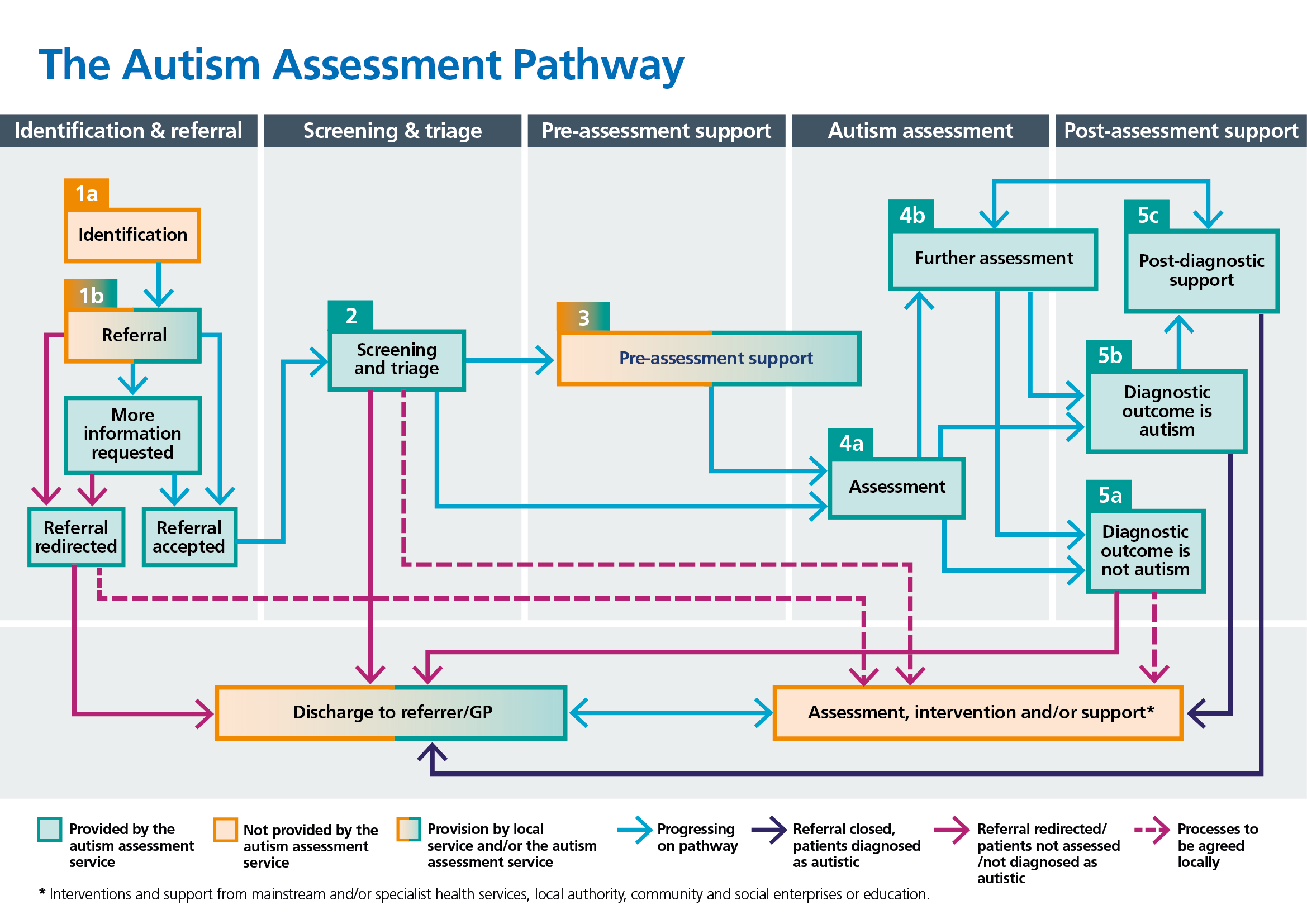
Five stages of the autism assessment pathway
People and their family/carers seek an autism assessment for a range of reasons. Confirmation of an autism diagnosis can be a validating experience (1–3) and facilitate access to services and support (4). Establishing if a person is not autistic is also important as it offers the opportunity for them to be referred into an alternative pathway, receive signposting to support or be directed to social prescribing link workers, depending on need.
Autism assessments routinely take place in different services, including child development centres, neurodevelopmental assessment teams and autism assessment services. In this guideline, and based on extensive stakeholder engagement, the autism assessment pathway (that is, from the point at which possible traits are identified and a referral for an autism assessment is first considered, through to discharge after an assessment has taken place) is seen to comprise five distinct stages, specifically:
- identification and referral
- screening and triage
- pre-assessment support
- autism assessment
- post-assessment support
Some services solely provide an autism assessment (stages 1, 2 and 4), whereas other services also provide pre- and post-assessment support (stages 1 to 5). For many people, sequential delivery of each stage of the autism assessment pathway is ideal. This recognises that people and their family/carers can benefit from signposting and support before and after the autism assessment, rather than simply focusing on the assessment element of the pathway (3,5–7). At the same time, there should be flexibility in service provision. For example, it is important to consider the needs, preferences and other time or work commitments of people, as well as their family/carers, a proportion of whom may themselves be autistic.
Importantly, the autism assessment pathway should be viewed in the context of other services (including health, social care and education) that a person or their family/carers may be receiving or could benefit from. This is because referral for an autism assessment does not preclude input from other services if there are identified needs that warrant support.
The five stages of the autism assessment pathway are outlined in Figure 1. It is recommended that a range of stakeholders in each Integrated Care System (ICS) and Integrated Care Board (ICB) collaboratively develop accessible autism assessment services for people of all ages and all abilities residing in that area. See Appendix B for a list of suggested stakeholders.
Reach, acceptability and effectiveness of these pathways should be evaluated periodically, including through service evaluation, audit or research, as well as feedback, concerns or complaints received. This should involve particular focus on any gaps in provision, such as for people who are approaching transitions (for example, from children and young people’s services to adult services), and people who are members of marginalised groups, have atypical presentations, and people with additional needs (for example, an intellectual disability, or visual or hearing impairment). Consideration should also be given to gaps between different services, including adult mental health and learning disability services, to ensure that people do not fall between service eligibility criteria.
Personalisation
There may be opportunities to use personalised approaches throughout the autism assessment pathway. More information on the comprehensive model for universal personalised care can be found in the national framework and on the NHS England website.
Two elements of universal personalised care may be especially relevant to the autism assessment process. Firstly, social prescribing link workers can offer signposting to local services and support networks when someone is early in the pathway and may provide continuity of care throughout a person’s journey on the assessment pathway, including when onward referrals are made. It is important link workers are appropriately skilled and trained to best support autistic and possibly autistic people (8). Social prescribing link workers form part of local personalised care offers across ICBs.
Secondly, decision making can be used to ensure that the person understands the risks, benefits and possible consequences of different care and support options. NICE has developed a shared decision making learning package to support healthcare professionals develop skills and knowledge to apply the clinical guideline on shared decision making (9).
Consent
In places throughout this document, we refer to the person’s consent, for example to taking part in the assessment, or to involving others in that process or sharing information that would otherwise be confidential. That consent is essential if they have capacity to make those decisions (as should be presumed if they are over 16, unless established otherwise, per the Mental Capacity Act 2005), or if they are under 16 years but are “Gillick competent” (that is, they have sufficient maturity and understanding to make those decisions). Where the person is a child who does not yet have Gillick competence to make those decisions for themselves, the decision may be made by the exercise of parental responsibility, where this is in the best interests of the child.
For someone over 16 who lacks capacity for the relevant decisions, the decision must be made in the person’s best interests, per the Mental Capacity Act.
Stage 1: Identification and referral
The first stage of the autism assessment pathway involves identification of potential autistic traits and subsequent referral for an assessment. While autism is a neurodevelopmental disorder of childhood onset, the possibility that a person is autistic can become evident at any age. It may be that people self-identify traits they associate with autism, or these may be observed by family/carers, professionals, friends or colleagues (6,7,10–13). A formal referral for an autism assessment may be sought when traits are first identified or when there are concerns about the impact these appear to have. Importantly, perceived stigma around an autism diagnosis or cultural stigma may present concerns to people or their family/carers, potentially serving to delay obtaining a referral (14–17). Cultural factors such as differences in knowledge, awareness and descriptions of autism may also contribute to delays (18–20).
Services can minimise the impact of these factors by ensuring referrers have up to date information that is clear and accessible to inform discussion with people and their family/carers, such as regarding the options for accessing an autism assessment within the area and what this may involve. While the latter screening and triage stage is a fact-finding process (stage 2), initial conversations with a referrer can also focus on preparing the person and their family/carers about possible outcomes of a referral and an autism assessment. Information should be tailored to the needs of different groups, including people of all ages, some of whom may have a possible or confirmed intellectual disability.
Identification
There can be a significant lag between the identification of possible autistic traits, a referral being made, and the autism assessment taking place (5,7). This is partly because some people and their family/carers experience barriers and bottlenecks at this early stage of the autism assessment pathway (21,22). See Appendix C for examples of barriers. This can result in a delay in people and their family/carers obtaining the right support when they need it. Consequently, routes into the autism assessment pathway need to be transparent and easy to access, irrespective of age or ability.
Facilitating sensitive conversations about a possible autism assessment
Discussions with professionals involved in a person’s care and support, for example, a GP or teacher, are often the first step in the process for requesting a referral for an autism assessment (23). Some people feel comfortable talking about why they would like to have this, but others may not. It may be difficult for them to articulate their thoughts, or they may find the professionals they approach dismissive and unsupportive (12,15).
Therefore, initial conversations with people and their family/carers should be conducted sensitively and with compassion (15), focusing on aspects including:
- Ensuring they have time to talk about possible autistic traits that have been identified and potential impact on day-to-day functioning. Offering a longer appointment than usual or follow up meetings may be appropriate.
- Broadly clarifying the range of difficulties or needs the person experiences – and the order of priority – to establish whether an autism assessment or referral for another type of assessment is necessary (for example, of mental health or intellectual ability). This can include clarifying if the priority areas of need or difficulties identified are the same for the person and their family/carers, or distinct.
- Identifying the drivers for, potential advantages with and any concerns about having an autism assessment.
- Considering any cultural differences that may make it difficult for some people and their family/carers to seek or accept a referral, such as perceived stigma about autism specifically or healthcare use more generally.
- Noting any contextual factors that may influence a referral being made (for example, for people and their family/carers who are from travelling communities or who have no current fixed abode).
- Making a plan to address needs and risks in the short term, if necessary.
The outcome of these initial discussions should be formally noted in the clinical records, including whether the person would like to proceed with a referral. This can help with continuity of care, for example if the person discusses this with a different clinician at a follow up appointment.
Referral
Some people and their family/carers report that information about the autism assessment pathway is inaccessible (6). There can be a lack of clarity about who can make a referral, when, how, and what will happen next. Understandably, this can be distressing for people and their family/carers and contributes to delay in obtaining support.
For each ICS, the following information should be publicly available and proactively shared across multiple locations, for example, social media and local authority publications, as well as all service provider websites:
- Accurate and up-to-date information about the autism assessment offer in each area, including details for services providing autism assessments (including name, address, contact details, general remit, eligibility criteria, referral process and documentation).
- An indication of waiting times for an autism assessment at each service.
- Information on Legal Rights to Choice of provider and team, and information to facilitate informed choice including waiting times, quality of assessment that would facilitate access to local services and any known limitations as a result of accessing an external pathway.
Suggested actions for the ICB:
- Check that people of all ages can access an autism assessment in the area.
- Address gaps in autism assessment provision for particular groups (for example, people with an intellectual disability, or people in inpatient NHS or independent hospitals or services, at residential schools and colleges, or in prison).
- Decide at an ICS level whether standardised referral processes across services have merit (for example, single point of access, an online form, shared templates).
- Develop protocols for how people and their family/carers can access pre- and post-assessment support if seen for an autism assessment by an external provider, including independent providers.
- Indicate what types of autism-relevant training is available for professionals working across services in the ICS.
- Identify who holds responsibility for periodically evaluating that information listed remains up to date.
A transparent referral process
People and family/carers report they would like to know more about the potential reasons for choosing to proceed with an autism assessment (or not), the process for referral, which services can provide this, and any differences in this according to age or ability. They want to know what the main components of the autism assessment pathway are and what they can expect as potential outcomes (7,24). From the outset, conversations about expectations are essential to encourage the person and their family/carers to approach the process as an assessment for autism, rather than anticipating a specific assessment outcome. At the point of referral, people should be made aware of their rights to choose a provider and provided with accurate and up-to-date information to inform these choices. This may include average wait time and where opportunities to access local pre- and post- assessment support after an assessment differs by service.
Autism assessment services have responsibility for providing referrers, people and family/carers with accurate and detailed information about the autism assessment pathway; ideally, this information is co-produced. This should be available in multiple formats. This can include leaflets (for example, placed at GP practices, mental health and learning disability services, and in education settings as part of the Special Educational Needs and Disabilities (SEND) agenda), and on the internet (for example, websites for health and social care services, and parent groups such as Parent Carer Forums). This should also be tailored for different audiences, including young people, adults and family/carers. Translation into other languages may be appropriate for people who use English as a second language. Similarly, easy read versions and plain English versions can be more accessible for some. Referral processes should be accessible, with services addressing possible barriers, including literacy levels and access to technology.
Developing easier routes into the autism assessment pathway
Referral routes for an autism assessment can vary according to the person’s age and availability of services. In some areas, the GP can refer directly to autism assessment services. However, there can be stipulations about what assessments or input are needed after possible autistic traits have been identified, but before a formal referral for an autism assessment is made. For example, people may first need to be seen for a more general assessment of difficulties, functioning or mental health, such as by a clinician in secondary care. Alternatively, people or family/carers may be asked to complete autism screening questionnaires, the scores of which may be used to help determine whether onward referral is deemed appropriate.
People and their family/carers may experience stress or distress in learning how to navigate these processes. While some areas may adopt an ‘all age, no wrong door’ referral system, good practice would be for each ICB area to have one accessible source of information about autism assessment services for all ages and the routes to these.
Additionally, it is sometimes suggested that family/carers of children and young people attend classes or courses focused on training in parenting skills while waiting for an autism assessment. This can delay input for children and young people. The research evidence for training in parenting skills in this context is limited (25,26), and the potential harm to family/carers by recommending they attend these courses is rarely considered (27).
There is some evidence for the success of parent mediated interventions (that may be delivered in a course format) targeting communication skills in young children, with improvements found in parent/carer and child interaction (28). Recommending interventions is appropriate only if clinically indicated. It should be based on the need for support, and not tied to the autism assessment pathway. However, parents should not be excluded from receiving support on the basis that their child is waiting for an autism assessment if they could derive benefit from this.
Taken together, decisions to delay referral for an autism assessment must be underpinned by a clinical rationale.
Making a referral for an autism assessment
Referrals for an autism assessment are usually made by professionals working in health services, social care and in education, or by professionals in the criminal justice system. Table 1 shows a summary of these settings and the roles of professionals who commonly instigate referrals. Some areas also accept self-referrals or referrals from family/carers.
Table 1. Examples of professionals who may make referrals for autism assessments, and the setting in which they may work.
| Setting | Professional |
| Health | GPs Paediatricians Psychiatrists Nurses Clinical, counselling or forensic psychologists Occupational therapists Speech and language therapists Health visitors |
| Social care | Social workers Occupational therapists Speech and language therapists |
| Education | Educational psychologists Speech and language therapists Special Educational Needs Co-ordinators Teachers at schools or colleges Nursery teachers |
| Criminal justice | Probation officers Professionals working in court Forensic psychologists |
A joint referral from two or more professionals who know the person enhances the specificity of this. For example, this could be contributed to by the GP and either the Special Educational Needs Co-ordinator (SENCo) or the clinical psychologist offering intervention at that time. When joint referrals are made, clarity is needed about which professional and service has primary responsibility for the person while they are on the waiting list for an autism assessment, and for actioning onward referrals and recommendations.
Self-referrals for an autism assessment, and direct referrals from family/carers, are less common in NHS services. If autism assessment services accept these, there must be operational protocols about what information is needed so that appropriateness (that is, eligibility for the service) can be clinically evaluated. There also needs to be an agreement that the person’s GP be kept informed about the referral and outcome to ensure continuity of care. Careful consideration must be given to factors such as which professional and service has responsibility for ongoing risk management and can initiate further referrals if indicated at subsequent stages of the autism assessment pathway. If the person is formally referred by a professional, for example, they may be more easily signposted to other services during and after the autism assessment.
Preparing a detailed referral letter
Some autism assessment services require a general referral letter while others have a standardised referral form. The latter can reduce duplication and effort on the part of people and their family/carers. Submission of referrals via an online portal can be particularly efficient.
Referrals should be comprehensive and, at the very least, summarise:
- Past and current clinical information (including about possible autistic traits and any other physical or mental health-related symptoms).
- Concerns, as described by the person and family/carers, and order of priority, whether these differ between the person and their family/carers, and how these concerns are currently being managed.
- Contextual factors (such as about who the person lives with, any dependents, their day-to-day activities).
- If known, information about adverse childhood experiences.
- Identified risks to or from self/others, including a risk management plan.
- Any requirements for adapting the autism assessment pathway if known (for example, as the person has an intellectual disability).
A referral should indicate whether the person has been referred for assessment for another developmental condition, including Attention Deficit Hyperactivity Disorder (ADHD) or possible intellectual disability. See Appendix D for a summary of suggested focal points for inclusion in an autism assessment referral.
The more detailed a referral is, the more informed the decision making can be regarding eligibility for an autism assessment and any adaptations the person or family/carers may benefit from along the autism assessment pathway. This can reduce inefficiencies at this initial stage, such as undue administrative and clinical time addressing inappropriate referrals and retrieving missing information. However, it is important that referrals are not declined based on omitted information that is not crucial for the referral, as this can cause unnecessary delay and frustration.
Information that may be relevant to include in a referral for children and young people:
- Clarity about whether the child or young person met developmental milestones at the expected age or whether there were any noted delays.
- Details about the education settings the child or young person attends and the current year or stage of education that they are in or specifying if they are not currently in education settings.
- A copy of the current Education, Health and Care Plan, plans put in place at SEN Support, or details of other access requirements at education settings, or other services if the child or young person is not in education.
- Whether the child or young person is due to move education settings within the following calendar year.
- A summary of concerns raised by teachers, along with examples of strengths and difficulties observed within the classroom and less structured education settings contexts (for example, break times, after school clubs).
- Details of any assessments conducted by professionals such as an educational psychologist, a speech and language therapist, an occupational therapist.
- An overview of any additional support the child or young person has or is receiving (for example, one to one support in lessons, referral for additional classes), including details of teachers and SENCo to input into the process and as points of contact post-assessment.
- If any siblings or parents have been diagnosed with a developmental condition or are awaiting an autism assessment.
- Whether the child or young person has some understanding of autism and the purpose of the assessment.
Information that may be relevant to include in a referral for adults:
- Age on leaving education.
- Any notable difficulties in education (for example, dropping out of education settings or university).
- A summary of the person’s independent living skills or requirement for social care or support.
- Any noted concerns in the context of employment (for example, a history of difficulties within the workplace).
- A description of the person’s current social circumstances.
- The person’s expectations of the autism assessment.
- Information about who is able to provide additional information, such as a parent or partner.
Information that may be relevant to include in a referral for people approaching transition:
- The age at which people are discharged from the service they may be referred to.
- If and how referrals can be transferred from services for children and young people to an adult service, without the person being placed at the bottom of the waiting list (that is, they should not wait disproportionately longer if their referral is transferred to an adult service).
- If and how referrals can be transferred to a service in another area if the young person moves from the family home for university.
- Which service will keep the person and their family/carers updated about the potential transfer of a referral to adult services.
Stage 2: Screening and triage
Streamlined and accessible referral processes help to ensure that the second stage of the autism assessment pathway – screening and triage – is efficient and effective at identifying people who are eligible for the service and will potentially benefit from an autism assessment. This process should also identify what components will be included in the assessment (such as via a differentiated pathway). Equally, timely decisions about people who are not eligible or are more likely to benefit from assessment by another service is essential for facilitating onward referral or signposting to another service.
Different services use the terms screening and triage interchangeably, or to refer to distinct aspects of the autism assessment pathway. Some services use these steps to determine eligibility for an autism assessment. This means some people may not be offered input beyond triage if this does not appear to be clinically indicated.
Each autism assessment service should, therefore, define screening and triage processes as per commissioning agreements (for example, what the service is commissioned to provide, for whom, in what circumstances and with any additional requirements noted, such as for children and young people approaching transition age). Additionally, there should be clarity about when screening and triage take place (for example, the number of days from the point of receipt of a referral), and the range of potential outcomes from these processes. This information should be available for people and family/carers.
Screening
Screening processes require input from administrative staff and clinicians. On receipt, referrals are usually reviewed in the first instance by administrative staff against pre-agreed eligibility criteria for the service, such as the age of the person and whether they live in the relevant catchment area, unless the referral has been made through Patient Choice. The sensitivity and specificity of these criteria or checklists should be evaluated periodically, for example, in relation to conversion rates (the proportion of people diagnosed with autism relative to the total number of people seen for an autism assessment). The criteria should also be reviewed if commissioning arrangements for the service change, or if there are changes to eligibility criteria for other autism assessment services in the area that may impact on the flow of referrals elsewhere.
Screening necessitates clinical input to determine if an autism assessment is appropriate based on the referral letter/form, with or without additional information being obtained in the interim. The focus here is on ascertaining whether the person may have traits indicative of autism, which is why comprehensive and detailed information is required.
A further aspect of screening involves noting any reasons why the referral cannot be accepted, for example because the person does not meet the age criteria for the service. Alternatively, a person may have specific additional diagnoses or difficulties that are outside the remit of the autism assessment service. Decisions to decline a referral are ordinarily made by senior clinicians responsible for screening these or the multidisciplinary team (MDT). In either instance, the referral should be promptly returned to the referrer or forwarded on to a more appropriate service if this is possible (depending on relevant service level agreements).
Some areas may have comparable processes for reviewing referrals across children, young people and adult services. This can make it simpler and more efficient for referrals to be passed on, such as in the instance a person is referred for an autism assessment during the transition period from children and young people to adult services.
In some instances, screening can take substantial time. For example, if the referral lacks information required to make a decision about appropriateness for the service, or when there is evidence of clinical complexity. Autism assessment services may choose to conduct audits periodically on the amount of time and input required at this stage, and by whom (for example, by administrative staff and clinicians), including the processing of clearly inappropriate referrals. Sharing information about the screening process with people in a commissioning role can highlight whether there are adequate resources available for this stage of the autism assessment pathway.
Triage
Triage helps autism assessment services to better understand a person’s presenting needs and difficulties, gather comprehensive information about possible autistic traits and traits suggestive of other conditions (for example, anxiety or ADHD), and potentially ascertain what the autism assessment should comprise.
Different approaches to triage
Triage can comprise one or more standardised or semi-structured methods, including:
- paper-based questionnaires or forms
- review of relevant correspondence (such as from health, social care, education, or the criminal justice system)
- meeting with the person, their family/carers, partners or friends
- liaising with professionals the person is in contact with or has recently been in contact with.
Any paper-based methods of triage should be accessible for people and family/carers, such as translated in other languages, easy read or Plain English versions if the service is an all-ability service, and age appropriate. Questionnaires, for example, are potentially easily completed online, but there should be options for people and family/carers to receive and return hard copies in the post if they prefer.
For more information about different types of triage, see Appendix E.
People and their family/carers may also be supported with triage in some areas by local authority, voluntary, community and social enterprises or education.
Clinical decision making after screening and triage
Information gathered by screening and triage processes should ideally be evaluated within ten working days. In some services, a senior or more experienced clinician who has reviewed paper-based information or met the person decides what the outcome of screening and triage is. Other services hold meetings – attended by the MDT – to discuss the information obtained and to form a consensus view about whether an autism assessment is indicated. Another option is for the decision-making approach to vary. For example, people who have more complexity or atypicality in presentation are discussed at dedicated MDT referrals/triage meetings and single clinicians reach a decision for people who appear, at triage, to present with less complexity.
Setting up an internal audit system, whereby clinicians discuss a proportion of decisions they have made with the MDT, their clinical supervisor or a peer can contribute to standardisation in practice. Additionally, a peer supervision process can be developed across autism assessment services within the area, to enhance parity in clinical decision making and provision.
The decision to progress to an autism assessment should be made based on the available information, while balancing the impact of any gaps. For example, there may be no one identified to complete an informant-based questionnaire about childhood or to support the autism assessment. However, this should not preclude the person having this if the available information suggests this is clinically indicated. Alternatively, a person may have a high score on an autism self-report screening questionnaire, yet in-person triage with an experienced or senior clinician, along with information from family/carers and clinical records, may indicate autism is highly unlikely. In this instance, it may be that the person is discharged without being seen for an autism assessment (that is, they are discharged back to the referrer as the information gathered until that point indicates they do not need an autism assessment). Conversely, differential or co-occurring diagnoses can obscure the (underlying) clinical presentation. Decisions to discharge people at this stage of the autism assessment pathway should therefore be discussed with the MDT and include appraisal of all the information available about the person.
Outcomes of screening and triage
A fundamental aim of screening and triage is to establish what the next clinical step is for the person, with regards to proceeding through the autism assessment pathway (that is, whether an autism assessment is indicated, at this time, with or without additional input or support from another service).
The most common outcomes following screening and triage are listed below.
- Discharge the person from the service if they are not considered to require an autism assessment. Signposting the person to other services may be appropriate.
- Recommend a ‘wait and see’ (or ‘watch and wait’) approach with the option of review or re-referral in the future. There should be an agreement about when this period will end, how the person can be seen for review (that is, will they need a re-referral or stay open to the autism assessment service) and who will provide a written summary of traits or difficulties for the referrer during this interim period. The person should maintain their place on the waiting list, so that they are not disadvantaged if there is a ‘watch and wait’ period.
- Recommend the person is offered assessment or intervention by another service to address acute symptoms or difficulties they present with that appear to take priority over an autism assessment (for example, psychotic symptoms or hypomania). Review by the autism assessment service (further screening or triage) takes place either after an agreed period or when symptoms or difficulties have been adequately addressed, to facilitate the person’s participation in the autism assessment. The person should maintain their place on the waiting list, so that they are not disadvantaged by the need for more urgent support by another service.
- Recommend the person is referred to a national specialist service for an autism assessment (for example, when the constellation or complexity of needs and difficulties warrants more specialist input).
- Offer the person an autism assessment without recommendations for interim input by another service. This may be tailored to their specific needs or difficulties and may also involve jointly conducting the assessment with clinicians based at another service, such as an ADHD or secondary care mental health service.
- Offer the person an autism assessment with recommendations for interim input by another service. Recommendations could include intervention for mental health symptoms (for example, low mood, anxiety), or ongoing assessment and support of special educational needs and disability within an education context. The autism assessment may be tailored to the person’s specific needs or difficulties. This may also involve jointly conducting the assessment with clinicians working at another service, such as an ADHD assessment or secondary care mental health service. Information about actioned recommendations should be shared with the autism assessment service while the person is on the waiting list.
Communicating screening and triage outcomes
A summary of the information gleaned at screening and triage should be communicated to people, their family/carers and professionals at different times, such as after this has been obtained or after the autism assessment has been completed. Services may adopt different approaches to this stage. Feedback can be summarised succinctly (for example, an overview of scores on self- and informant-report standardised questionnaires), or described comprehensively (for example, in depth description of responses to questions posed during an appointment with the person). All information should be presented in a manner and format that is accessible to the person, their family/carers and professionals.
The amount and detail of information shared at this stage also potentially depends on the outcome and next steps. Recommendations for interim or alternative assessment, or intervention by other services should be explicitly outlined, including clarification about what processes are already in place and which professional or service is being asked to make onward referrals or to assess the person.
Addressing concerns about screening and triage outcomes
Sometimes a person is discharged from the service without being seen for an autism assessment. They or their family/carers may feel disappointed about this outcome or concerned about how their perceived needs will be met. Similarly, professionals working in health, social care or in education may disagree with the clinical opinion. This means there should be an option for the person, their family/carers or professionals to discuss screening and triage outcomes. Discussion should include the rationale for how and why particular clinical conclusions have been reached (that is, what information was used to inform decision making), with emphasis on signposting to other services when feasible.
Expediting referrals
There are likely to be instances when people on the waiting list – whether already in receipt of support or not – are deemed to require an expedited (faster) assessment. Autism assessment services should outline the process for requesting an expedited assessment, criteria for reviewing these requests (such as an MDT discussion about new/current concerns) and the possible outcomes (for example, agreeing or declining the request). Criteria employed to support expediting of referrals may vary between services. Therefore, consistency and transparency are essential for ensuring parity in decision making. It may be that children and young people and adult services within the area develop shared criteria that are reviewed periodically.
Information that may be relevant when screening and triaging referrals for children and young people include:
- Using age-appropriate self-report questionnaires of autistic traits and traits of other conditions.
- Reviewing the My Personal Child Health Record and any medical correspondence from very early years.
- Asking for copies of reports from education settings, reports by educational psychologists, SENCOs and Education, Health, and Care Plans.
- Asking teachers to complete informant-rated screening questionnaires or to provide more general information.
- Establishing if there are other informants who can contribute information (for example, grandparents, childminders, nannies).
- Seeking information from support providers, for example if the person is a ‘Looked After Child’.
Information that may be relevant when screening and triaging referrals for adults include:
- Establishing if there are others who can contribute to the assessment as an informant for childhood and adult years (e.g., family, friends, partners) and the period during which they have been in contact.
- Obtaining information about further and higher education, such as end of year reports.
- Reviewing any correspondence relating to employment, such as occupational health reports.
Information that may be relevant when screening and triaging referrals for people approaching transition include:
- Seeking consent to share information gathered at a children and young person’s service with an adult service, rather than the person and family/carers needing to re-start the process.
- Determining what data sharing arrangements are in place if the person is moving to another area.
- Considering whether the person will need to complete additional screening questionnaires if they step up into an adult service.
Stage 3: Pre-assessment support
There is often a gap between screening and triage and the autism assessment taking place. This may be due to waiting times, preference, or clinical factors (for example, if the person is experiencing significant mental health symptoms) that warrant being addressed first. Pre-assessment support is described as important by people and their family/carers but has traditionally seldom been available.
Keeping people and their family/carers informed about their autism assessment pathway
People, and where consent allows, their family/carers and professionals they are in contact with should be updated about the estimated waiting time for the assessment regularly (for example, every three months). There should, however, be an opt out option for the person if they do not wish to receive these updates.
Updates should:
- Highlight the reason for the waiting time (for example, due to demand for the service or that the person requires prior assessment or intervention elsewhere).
- Indicate the approximate waiting time at that point.
- Provide contact details for a professional working at the service (for example, an administrator or clinician) who they can contact if they have questions while they are waiting, or if they need to advise about a change in circumstances (for example, a new home address or telephone number).
- Specify which service to contact if the person or family/carers become more acutely concerned about risk or acuity of presenting symptoms or difficulties.
- Confirm the next steps to be taken by the autism assessment service and how and when this will happen.
- Correspondence should be copied to the referrer so that they know when the autism assessment is likely to take place.
Providing resources for people and family/carers while they wait
Some people or their family/carers require support or input from health or social care services or education while the person is waiting for the autism assessment.
Needs identified can be related to possible autism (for example, social communication difficulties, problems with managing change and transition) or broader issues (for example, anxiety, disrupted sleep). Similarly, family/carers can benefit from signposting, advice or support at this time, in relation to supporting their child, other family members and in terms of their own wellbeing.
Needs and difficulties may have been highlighted in the initial referral letter/form or during screening and triage processes. For health-related needs, the referrer or local primary or secondary care services must not omit providing assessment or interventions relevant to the person’s needs while they are waiting for an autism assessment. Clarity about a possible autism diagnosis, in almost all instances, does not negate input for current needs, symptoms or difficulties that appear linked to physical or mental health. If a person’s needs are particularly complex, a link worker or equivalent can provide helpful oversight and coordination between services.
The autism assessment service may share resources or offer input while people are on the waiting list. This can include:
- Contact details for general local health and social care services, education support, voluntary, community and social enterprises, and social prescribing.
- Information about what will happen at the autism assessment and how, potential outcomes and a list of answers to frequently asked questions about the autism assessment pathway and process.
- General psychoeducational information about autism, such as what autism is and is not. This may include tips and strategies for addressing the possible impact of autistic traits.
- General psychoeducational information and evidence-based tips and strategies about symptoms and conditions commonly experienced by people referred for an autism assessment (including autistic and non-autistic people), such as low mood, general or specific anxiety, or disrupted sleep.
- General information and evidence-based tips and strategies for family/carers, such as around reducing stress and enhancing wellbeing.
- Peer support sessions or groups. Peer support sessions can include support from people or family/carers of people who have been through the autism assessment pathway.
- Information can be provided in written, audio-visual formats or via group approaches and should be accessible for people and their family/carers using the service (for example, translations, different versions for people with all abilities, and of different ages). Information should also be conveyed using an autism-informed approach (29), such as combining prose and images.
Education support – delivered outside of the autism assessment service
Some children and young people will benefit from support within an education setting while awaiting an autism assessment. Support for children in these settings should not be dependent on an autism diagnosis; education staff are expected to work collaboratively with external professionals and family/carers to ensure good quality support is in place when needed. Education settings are required to plan support in response to a child or young person’s individual profile of SEND through reasonable adjustments, SEND support or through an Education, Health and Care Plan (EHCP).
This should include how schools, while waiting for an assessment, can a) identify special educational needs linked to possible autism, and b) meet those needs. It could also include training and advice for schools, colleges and universities on the likely presentation of traits and needs of people while they are on the waiting list and how students can be supported.
Autism assessment services should provide information about a point of contact for queries while the person and family/carers are waiting, keep education settings informed of the anticipated waiting time for an assessment and signpost to other sources of advice and support when possible.
Informing professionals about pre-assessment support
Referrers and local services should be informed about any provision of resources or input to people while they are on the waiting list for an autism assessment. This may be via a template checklist or letter, or a more comprehensive letter for people or family/carers who have been offered more specific pre-assessment support.
Clinical records should be updated in a timely way, to reflect what resources or input has been offered to the person and their family/carers, when, and by which professionals. Scores on any outcome measures administered should also be provided.
Factors that may be relevant for pre-assessment support for children and young people include:
- Providing age-appropriate information for children and young people, and parallel information for family/carers.
- Considering the age and developmental stage mix of children and young people attending for group interventions.
- Providing clarity for family/carers about differences between parent-mediated interventions and training in parenting skills. Any interventions offered to family/carers should be delivered based on an emerging or robust evidence-base.
- Offering family/carers information about how to access support in education settings and in further or higher education.
- Signposting family/carers to social care support and options for breaks from caring.
- Undertaking stakeholder engagement to clarify what resources and sources of support for family/carers would like.
Factors that may be relevant for pre-assessment support for adults include:
- Providing information about access to support in higher education and at work.
- Putting together a list of links to different benefits and financial support options, with some supporting notes about completing application forms.
- Considering the age and life stage mix of adults attending for group interventions.
- Running group interventions at times people working full time will also be able to access.
- Giving examples of anonymised communication passports that adults may wish to edit for their own use.
- Undertaking stakeholder engagement to clarify what resources and sources of support family/carers would like.
Factors that may be relevant for pre-assessment support for people approaching transition include:
- Setting up protocols that outline which service (that is, the children and young people or adult service) will provide pre-assessment support if the young person is due to transition to adult services while awaiting an autism service.
- Providing information about adult services and adult-focused third sector organisations within the local area.
- Developing written resources, podcasts or blogs about cohesive transitions.
- Clarifying, for family/carers, the age at which young people transition to adult medical, mental health and neurodevelopmental services in the local area. For example, for some services this will be at aged 18, at others this may be at 21. Listing contact details for adult services commonly accessed by people seen by the autism assessment service.
- The GP becoming the coordinator of care from the age of 18 years, unless there are additional provisions available.
Stage 4: Autism assessment
Following screening and triage, people are either discharged from autism assessment services, offered a review appointment after a specified period to determine whether an assessment is clinically indicated (a ‘watch and wait’ approach) or placed on the waiting list for an autism assessment.
Clear aims for the autism assessment
An autism assessment has several aims. Broadly, these are to:
- Establish whether autistic traits are currently present, appear to have been lifelong and have contributed to impairment in different areas of daily life. For example, in education, occupation and social relationships (30).
- Screen for or assess common differential (that is, alternative) or co-occurring diagnoses.
- Understand the person’s strengths and goals, as well as their current needs and difficulties.
- Consider whether further medical, psychological, cognitive, sensory, skills-based or functional assessment is warranted and, if so, which service is best placed to provide this.
- Reach a clinical conclusion about whether the person is autistic and communicate this.
- Provide written recommendations to address current difficulties and needs, and to maximise well-being.
People, their family/carers and professionals should be aware of these aims prior to this stage in the autism assessment pathway – ideally at the point of referral, as well as in public-facing materials about the service (for example, documented in leaflets in written and diagrammatic form and on the organisation’s website). They should also know how information they provide will be used within correspondence (that is, in interim letters or an assessment report), if there will be opportunities to comment on the report before the final draft is shared with the referrer and other professionals involved, and what steps they can take if they do not agree with the assessment outcome or recommendations.
Additionally, the triage stage of the process may have provided the person and their family/carers with an opportunity to meet with clinicians and find out more about what the autism assessment could comprise.
The parameters of the assessment must be explicit, including which structured, semi-structured and unstructured measures may be used in the autism assessment (for example, autism assessment tools, or questionnaires), other neurodevelopmental and mental health conditions that will be screened for and assessed, and common outcomes from the assessment.
The National Institute for Health and Care Excellence (NICE) clinical guidelines (31–33) and Quality Standards (34) set out evidence for good practice in autism assessments. This includes which professionals may be involved and the recommended autism assessment tools and processes employed.
A multidisciplinary team approach to autism assessment
The workforce configuration of autism assessment services differs between settings. At a minimum, this should comprise an MDT, with substantial collective experience and expertise in assessing both autism and the range of neurodevelopmental and mental health conditions that can commonly be differential or co-occur with autism (33).
Owing to the nature of core training, paediatricians, psychiatrists and clinical psychologists are well placed to conduct autism assessments and reach diagnostic opinions, both independently, and as part of an MDT (22). Clinicians from other professional disciplines often undertake components of the assessment, but do not tend to routinely conduct these as sole practitioners.
Some clinical professionals may have additional training and qualifications to practise at multi-professional consultant or at multi-professional advanced clinical practice level to increase the number and diversity of professions represented in leadership roles. When these include training and assessed capability to conduct components of autism assessments, such as, for example, the autism credential, this may increase capability in relation to assessment components a professional can undertake. Some clinical professionals may have some additional non-clinical qualifications (for example diplomas, undergraduate or postgraduate degrees in research or other non-applied areas), this does not change their qualification to conduct each component of clinical autism assessment. Some components of assessment can be undertaken by staff under clinical supervision.
Given the possibility of clinical complexity and differential co-occurring diagnoses, it is not advisable for non-clinically trained professionals to conduct autism assessments independently (for example, research assistants, teachers), but they may make helpful contributions to aspects of the assessment or post-assessment support offered.
A differentiated approach to autism assessment based on clinical presentation and need
Based on information gathered from screening and triage, autism assessment planning should consider which components to include alongside the clinical interview. Planning should consider assessment tools, possible further assessments and which professional disciplines should be involved. The assessment can be differentiated in two main ways: standard or enhanced.
A standard autism assessment
- An assessment conducted by one or two clinicians (for example, a consultant psychiatrist and a mental health nurse or trainee psychologist).
- This may be indicated when information attained at screening and triage suggests an autism diagnosis is probable with no evidence of likely mental health considerations for the person. Furthermore, the circumstances may lend themselves to a straightforward process of gathering developmental and corroborative information. For example, the person is able to participate in the regular assessment format (including the clinical interview) and family/carers are available for interview.
- Consistent with NICE guidelines (31,32) the assessment should include, at a minimum, a clinical interview, behavioural observation, integration of developmental and corroborative information and consideration of possible differential and co-occurring diagnoses not identified at triage (especially when there has been a delay between initial referral, triage and main assessment).
An enhanced autism assessment
- An assessment conducted by two or more clinicians.
- This may be indicated when the screening and triage information suggests an autism diagnosis is possible but there is the possibility of other health considerations (for example, differential or co-occurring diagnoses). The circumstances may not lend themselves to a straightforward process of gathering developmental and corroborative information, such as parents being unavailable for interview or the person not being able to participate in the regular assessment format, such as the clinical interview.
- Consistent with NICE guidelines (31,32) assessment should include, at a minimum, a clinical interview, behavioural observation, integration of developmental and corroborative information, use of validated assessment tools, a broader assessment of clinical presentation (such as estimated intellectual functioning or sensory processing) and additional liaison with referrers and other involved service(s). Siblings, partners or friends may provide corroborative information.
Components of a good clinical assessment
The components of an autism assessment can vary according to the age and developmental stage of the person. As noted previously, the early indications from triage may direct the nature and breadth of the assessment, but not always. This means the autism assessment service should facilitate flexibility as needed, including having the option to incorporate additional components into the assessment, when clinically indicated.
The autism assessment must include a clinical interview with the person, conducted by a clinician with a medical background or a qualified mental health professional (for example, clinical psychologist or mental health nurse)(31,32). This is distinct from an assessment with family/carers or conversations with siblings (for example, developmental history taking or asking for descriptions of current concerns). This is also distinct from semi-structured behavioural observation assessments that specifically focus on traits associated with autism (for example, the Autism Diagnostic Observation Schedule – 2; ADOS-2 (35)). The clinical interview is pivotal for putting into context scores obtained on standardised questionnaires that may be used for screening or triage, or scores on semi-structured assessment tools. This also helps to address the question as to whether the person may have differential or co-occurring diagnoses; crucial for formulation and reaching clinical conclusions.
Themes for discussion at a clinical interview with the person include:
- Reason(s) for referral and the person’s, their family/carers and referrer’s expectations of the assessment
- the impact of past and current traits associated with autism (according to the International Classification of Diseases, eleventh edition; ICD-11 (30), or the Diagnostic and Statistical Manual of Mental Disorders, fifth edition; DSM-5 (36)), and any modifiers for these
- current concerns, and the onset and trajectory of these
- developmental history
- information about what life was like growing up
- general day-to-day functioning
- education and occupation
- hobbies and passions
- needs and difficulties
- strengths, resilience factors and personal (coping) resources
- social circumstances, friendships and relationships
- physical and mental health and emotional wellbeing
- mental state assessment
- risk (to self/others including self-harm and suicidal ideation, and from others).
The assessment must include screening or assessment of common differential or co-occurring diagnoses, as part of the clinical interview conducted by a clinician with a medical background or a qualified mental health professional. This includes consideration of other neurodevelopmental conditions such as ADHD and intellectual disability, mental health conditions (including mood disorders, anxiety disorders, obsessive compulsive disorder and related disorders, disordered eating, traumatic stress) and attachment-based difficulties.
The person and family/carers may also complete screening questionnaires about mental health and wellbeing. In this instance, responses should be followed up if clinically indicated. This is because it is important to ascertain whether low or high scores on questionnaires are consistent with information gathered during screening, triage and the autism assessment from the person. Information about other potential neurodevelopmental traits or mental health symptoms is crucial for developing a formulation and thereby the diagnostic opinion, as well as informing recommendations for post-assessment support or intervention.
Some services incorporate behavioural observation assessments (for example, the ADOS-2 (35)). These should be conducted by appropriately trained professionals, ideally with expertise in mental health and development. There must be clinical oversight if the professionals conducting these are not clinicians, and they should have regular supervision. These assessments may take place in clinic, at education settings or at home and can be structured, semi-structured or unstructured.
Importantly, behavioural observation assessments do not replace the need for a clinical interview. This is because scores cannot be meaningfully interpreted without the contextual information gathered during a clinical interview (scores below and above the indicative threshold suggested for autism may be due to the presence of autistic traits, differential diagnosis, or both autistic traits and co-occurring conditions).
Any deviations in the administration of standardised and licensed assessments (for example, conducting the ADOS-2 online) should be reported in the outcome documentation (for example, what adaptations were introduced, which, if any, activities or tasks were omitted or added), with clarity about how this may be relevant for any clinical conclusions reached.
Corroborative information is important for reaching clinical conclusions. This should be sought when feasible, and the person has consented to this. This may be obtained using a standardised semi-structured assessment (for example, the Autism Diagnostic Interview – Revised (ADI-R; 37)) or an unstructured interview. Some services gather this information as part of the triage process, whereas other services may do this as part of the autism assessment. It can be more challenging with older adults as parental information may not be readily available or may be less reliable owing to time passed since childhood.
As with behavioural observation assessments, interviews conducted with family/carers, such as the ADI-R, do not replace the need for a clinical interview that asks the person directly about their experiences growing up. Additionally, developmental information obtained in semi-structured assessments needs to be considered alongside all other information gathered, to discern whether scores below or above the threshold are attributable to the presence of autistic traits, differential diagnosis, or a combination of autistic traits and co-occurring conditions. Other information, such as from siblings, partners, close friends or professionals the person is in contact with, should be gathered when possible.
Development of service or area-wide templates for systematic gathering and recording of information can be useful for ensuring that key focal points for an autism assessment are addressed before or during Stage 4 of the autism assessment pathway. Using a consistent template for an area also makes it easier to transfer information, for example, if people have had a triage at a children and young people service, but are likely to transition to an adult service for the autism assessment.
Formulating a view about diagnosis
Clinical formulation of individual presentation, developmental patterns, strengths and needs, resources and difficulties, contributes to the clinical conclusions and provides the first step to generic and focused post-assessment support. Formulation is based on the integration of information gathered from a clinical interview, behavioural observation, developmental and corroborative accounts, clinical and educational records and liaison with other professionals. It must be viewed as more than just the scores on any given screening questionnaires or assessment tools.
At times, it may be necessary to consider all the information available and, on balance, to agree that the scores on standardised assessments do not present an accurate picture of the person. In other words, while specific assessment tools tapping traits associated with autism may yield scores above or below the indicative threshold suggested for autism, this remains a clinical decision – that is, made by clinicians on the basis of all available information and in light of their clinical experience.
Consensus diagnosis meetings provide opportunities to:
- present information gathered about a person.
- identify potential gaps in information before completing the assessment and determine how this can be best obtained.
- consider multidisciplinary perspectives about the formulation, including views about whether the person is autistic.
- outline recommendations to be shared with the person.
Communicating the assessment outcome clearly
The lead clinician or clinical team (depending on the protocol of the autism assessment service) shares the outcome with the person and their family/carers (as appropriate). Consideration needs to be given regarding the nature and format of this feedback to ensure this is accessible and clear, and that recipients can feel confident in the outcome, irrespective of what this is.
Some young people and adults participating in the assessment process may be expecting an autism diagnosis. Parents may be hoping for an autism diagnosis if they believe this is essential for securing necessary services to meet their child’s needs (38). Sharing the assessment outcome is never neutral, whether expected or not (3,6,11,13,39). A lengthy wait for assessments can make the outcome more important to people and their family/carers. If the standard protocol for the service includes sharing the outcome at the end of the main assessment appointment (usually involving a clinical interview), due time and attention should be given to this aspect of the process; this should not be rushed.
The following considerations are needed for the sharing the outcome of the autism assessment verbally:
- The person may benefit from more than one appointment to discuss this, whether diagnosed as autistic or not.
- Feedback may need to be offered face-to-face, even if the main assessment took place via a telehealth platform, particularly if the person or family/carers have difficulty understanding or accepting the outcome.
- Consider the skill set that clinicians require to share the formulation and assessment outcome.
- Feedback should be provided by a lead clinician or qualified clinician who participated in the assessment process and is known to the person and their family/carers.
- Local protocols for providing feedback can be developed in consultation with people and family/carers to ensure this is shared in a personalised manner.
- Check consent (from earlier consent processes) and current wishes for sharing the outcome with others, including the referrer or professionals in other contexts. (Consider that some information may be shared with GPs via local recording and reporting processes, such as System One, and the person and their family/carers should be made aware of this. See earlier section about consent.)
- Signpost people and their family/carers to information concerning their rights if an autism diagnosis is made, such as information to help someone understand how their diagnosis help them to seek reasonable adjustments in the workplace under the Equality Act 2010.
- Inform people and their family/carers that details of the assessment and the discussion will also be provided in writing.
The following considerations are needed for sharing the outcome of the autism assessment in written form:
- Develop local protocols for efficient and effective written communication of the assessment outcome and recommendations.
- Agree on integral components of each document. See Appendix G for the core components of an autism assessment report.
- Determine an optimal time within which to complete the autism assessment documentation and share with the person and their family/carers.
- Consider the option of a staged process of sharing the documentation (brief statement with headlines and evidence prepared within one week of the outcome, followed by a more detailed report including recommendations and next steps. Further documents might be provided at a later stage depending on the post-assessment support offered. (The function of the brief statement is to provide evidence of the diagnostic outcome and how this was reached. This also serves the purpose of a short statement that can be used by the person or family/carers for a wide range of purposes without the need to share the detailed clinical report that contains highly personal information.)
- Establish local systems to support the integration of clinical notes and electronic patient records to reduce duplication when producing outcome documentation.
- Where multiple authors contribute to the document, consider using shared documents to enable clinical professionals to work concurrently, rather than waiting for sections to be completed independently.
- When possible and sufficient administrative resources are available, consider dictation of letters and statements.
- Develop templates for assessment statements, reports and letters.
- Consider relevant recipients – documents may need to be available in the future so that a copy can be held by the person, family/carers or Primary Care, irrespective of who the referrer is.
- Consider privacy rules and sharing information, such as when reporting information about extended family members who are not part of the autism assessment process.
- Include, when appropriate, the comments and contributions of the person in the process, outcome and recommendations.
Recording assessment outcomes in clinical records
Clinicians are responsible for recording the assessment outcome in the clinical records system. This is essential for maintaining contemporaneous and accurate information about a person and ensures other health professionals in contact with them are aware of the diagnosis.
This is also an important step in the submission of regional recording and coding of the referrals for autism assessment, waiting times and assessment outcomes that are monitored nationally via the Mental Health Services Data Set (MHSDS) and Community Services Data Set (CSDS) respectively.
Specific considerations for conducting an autism assessment with children and young people can include:
- Offering flexibility around appointment times to accommodate days and times spent in education and family/carer commitments.
- Considering the age and developmental stage of the person and which semi-structured assessment measures are appropriate to their needs.
- Recognising that good practice for autism assessments in children and young people includes assessment/observation in at least two settings, such as clinic and education setting, irrespective of the service (child development centres or children and young people mental health services).
- Facilitating opportunities for parents/carers to speak with clinicians independently of the child or young person, if appropriate.
- Offering information about diagnosis in an accessible way for both children and young people and family/carers.
- Making recommendations about which service may be able to update the assessment report over time, to reflect any changes in strengths and needs.
Specific considerations for conducting an autism assessment with adults can include:
- Identifying whether there are informants who can take part in the autism assessment, to provide, for example, developmental or corroborative information.
- Offering flexibility around appointment times to accommodate higher education, work, or care commitments the person may have.
- Providing a shorter assessment letter that the person can share with an employer if they wish to.
Specific considerations for conducting an autism assessment with people approaching transition can include:
- Considering the age and developmental stage of the person and which semi-structured assessment measures are appropriate to their needs.
- Considering joint autism assessments between the children and young people, and adult services.
- Developing protocols for sharing information between services if the person is due to transition to adult services after screening and triage processes have taken place at a children and young people service.
Stage 5: Post-assessment support
Receiving or not receiving an autism diagnosis can mean different things to different people. Some people experience a sense of validation. For others, the clinical assessment conclusion can come as a surprise and feel unsettling or upsetting, at least initially. Family/carers and partners can similarly experience a range of emotions about this. Members of a family can have shared or unique responses; not all will feel able to have open and in-depth conversations about this (3,6,11,13,39). Therefore, having time to talk through the assessment outcome (and formulation) and to ask questions is important.
Some people and their family/carers can benefit from further support or intervention after an autism assessment. Post-assessment input can be offered by health, social care, education and voluntary, community and social enterprises. Some people benefit from short-term support by one service, while others may require several types of input either sequentially or concurrently.
Autism assessment services can be well placed to provide targeted interventions for autistic people and signposting for people who are not diagnosed as autistic.
Offering post-assessment support for people who are not autistic
Some people seen for an autism assessment are not diagnosed as autistic. Whether they receive an alternative (differential) diagnosis can depend on factors including:
- The skill set of the clinicians who assess the person (for example, whether they have the training and expertise required to assess other conditions).
- The scope of the assessment (that is, whether other conditions have been sufficiently investigated in order to be able to reach a firm clinical conclusion).
- Commissioning arrangements (for example, whether the service is commissioned to provide clinical conclusions about diagnoses other than autism).
Signposting and referral for further assessment or support
Many people who are not diagnosed as autistic may benefit from further signposting and provision of resources, support or intervention after being seen for an autism assessment. If these are available, it can be useful to share a list of resources, pertaining to health, social care, education, occupation or third sector organisations, locally and nationally. Some people who are not diagnosed as autistic will require a referral for further assessment or support by another team (for example, specific mental health service, an ADHD service). To avoid unnecessary delays, there should be a standardised policy about which service can make onward referrals. For example, this could be the GP, or a clinician at a mental health service, who may be better placed to make referrals or has a gatekeeping function within referral pathways. Assessment outcome documentation can be a useful appendix to any further referrals.
Offering post-assessment support for autistic people
Post-assessment support for autistic people can comprise:
- further assessment
- enhanced understanding of strengths
- development of a passport or self-disclosure tools
- signposting and provision of resources
- individual or group psychoeducational interventions focused on autism
- individual or group psychosocial interventions focused on mental health and emotional wellbeing
- individual or group interventions for family/carers
- peer support and mentorship
- personalised care and recommendations for social prescribing
- crisis intervention
- liaison with other services.
Further assessment
During the autism assessment, it may become evident that the person presents with needs that have not been sufficiently investigated, but that are likely to benefit from greater understanding and support. This can include specific difficulties, such as in relation to speech and language, sensory processing or functional skills. Alternatively, a more global assessment of the person’s needs can lead to tailored recommendations for education, occupation and independent living. While these focal points are slightly aside from clarifying whether a person is autistic, they can inform more individualised support offered by health and social care services or within education settings.
Enhanced understanding of strengths
While people are often referred to health services based on presenting needs (including for an autism assessment), it is paramount to also understand a person’s strengths, resilience factors and personal (coping) resources. This can be a focus of individual and group-based post-assessment support.
Development of a passport or self-disclosure tools
Some autistic people benefit from having a health passport (summarising preferences and needs relating to health and health care), an autism passport (summarising preferences and needs relating to autism) or self-disclosure tools (for example, assessment statements or a summary of key information they would like to share with others, including professionals).
The amount and type of information people choose to document varies, as can the format and layout. Some autistic people prefer to compile this alone, whereas others may like support to develop these as part of a post-assessment support offer. These are not static documents. Autistic people and family/carers should be encouraged to update these as appropriate (such as, if the person would like to share this with new people or in a new context, or as preferences and needs change over time).
Signposting and provision of resources
Many autistic people and family/carers find it useful to have access to resources about:
- psychoeducation about autism (psychoeducation is the provision of a focused programme of information-sharing and advice for diagnosed individuals, families and carers.)
- recognising and regulating emotions
- understanding and improving mental health conditions
- strategies for improving eating
- strategies for enhancing sleep
- health and social care provision in the local area (including acute and general services, and how these can be accessed)
- employment rights
- third sector organisations.
This list of topics is indicative rather than exhaustive. Provision and signposting of the most clinically helpful services will depend, to some extent, on the age of people seen and available services within the area.
Resources are more commonly provided in written form (for example, leaflets, posters and worksheets), but complementing these with podcasts or workshops can be helpful. The input of autistic people and family/carers into resource development is key, including ensuring that there are versions tailored according to age, ability and additional needs (for example, dyslexia).
Individual or group psychoeducational interventions focused on autism
Research suggests that access to psychoeducational interventions following an autism diagnosis can be beneficial and contribute to improved understanding and acceptance of autism, and improved mental health (40). These sessions can be delivered in groups or individually and may involve input from autistic people who have previously gone through the autism assessment pathway.
Overall, psychoeducational interventions – delivered individually or via groups – should aim to:
- normalise and validate experiences
- support a person’s understanding about autism, what this means to them and their autism identity
- reduce perceived stigma and build confidence.
Individual or group psychosocial interventions focused on mental health and emotional wellbeing
A substantial proportion of autistic people experience one or more co-occurring mental health conditions, including anxiety disorders and depression (41–44). They can benefit from (adapted) evidence-based psychosocial interventions. The autism assessment service may offer time-limited individual or group psychosocial interventions to target mental health and emotional wellbeing. This does not, however, replace the remit of primary and secondary mental health and psychological therapies services that are expected to make reasonable adjustments to routine care, so this is more accessible for autistic people.
Locally, there should be clarity about which service will provide psychosocial interventions, to whom (that is, the eligibility criteria) and what the referral process is.
Individual or group interventions for family/carers
Family/carers can benefit from individual and group interventions after people have received an autism diagnosis. These groups may occur alongside parallel groups for autistic people or separately and may be for family/carers of children and young people as well as adults. While more research into these types of interventions is required, initial evidence (25,26,45) demonstrates feasibility, effectiveness and acceptability for interventions designed to:
- increase knowledge and understanding of autism and associated conditions
- validate experiences and reduce perceived stigma
- improve emotional wellbeing and self-efficacy
- enhance communication, interaction and relationships between parents/carers and their autistic child
- teach skills and strategies flexibly for supporting an autistic child.
General principles for developing and delivering individual and group interventions
Some general principles underpin provision of individual/group psychoeducation and psychosocial interventions for autistic people and family/carers.
Intervention design should:
- Involve co-production – autistic people and family/carers who have used this or a similar service should be invited to contribute to decision-making about what interventions are offered, as well as developing materials.
- Be evidence-based – there is emerging evidence for varied interventions for autistic people and family/carers. Novel interventions offered should be underpinned by a clinical rationale.
- Have clear parameters – interventions offered by autism assessment services are intended to complement, rather than replace or replicate those offered within mental health or other settings.
- Emphasise strengths – a focus on strengths and unique abilities is key.
- Reduce perceived stigma – interventions should seek to normalise and validate experiences and reduce perceived stigma.
- Be accessible – the needs and abilities of autistic people and family/carers vary. Interventions should accommodate different requirements (for example, with parallel materials developed for autistic people with and without an intellectual disability).
- Demonstrate cultural sensitivity – interventions should be accessible to the people living in the local area. Resources may require translation into other languages and may need to consider cultural norms for different groups.
The following factors are important for intervention delivery:
- Location – some people may wish to attend sessions in person, and others may prefer to use telehealth. Sometimes, a hybrid of in-person and telehealth sessions may be suitable. If clinically appropriate, autistic people and their family/carers should choose which they prefer; see the personalised care section in the national framework document for more information about choice.
- Mode of delivery – some autistic people and family/carers will prefer to be offered sessions individually, and others may wish to attend a group session. Developing a process for assessing eligibility for individual versus group interventions can help to ensure parity in provision while balancing available resources.
- Duration of sessions – some autistic people benefit from having a longer time to process information. Others may experience attentional impairments, such as those associated with ADHD. It can be helpful to build in regular breaks and to provide a summary of information discussed or contemporaneous notes that people can refer to between sessions.
- Clinical considerations – potential delivery of post-assessment support involves clinical considerations around issues, such as whether the person seems able to engage in the intervention at that time and whether there are any known risks to self or others that could influence participation or engagement in individual or group sessions.
- Audit and service evaluation – the accessibility, feasibility, acceptability and effectiveness of post-assessment support options should be regularly audited or evaluated. This can include summary and analysis of routinely collected information (for example, any systematic differences in characteristics of people or family/carers who decline to attend versus those who participate) and qualitative exploration of the views and experiences of people who have had post-assessment support, as well as the clinicians who delivered this. Providing autistic people with answers to frequently asked questions or worries about interventions (for example, “what will happen in a session?”, “will I have to speak in a group?”, “what if I change my mind and want to come to a group rather than having sessions individually?”) can be useful.
Further assessment and individual and group interventions can result in internal referrals and waiting lists. It is important to let people and their family/carers, professionals based in other settings and colleagues within the service know about these processes and the likely waiting time for input. It is also crucial that referrers and the GP are aware of the parameters of ongoing work by the autism assessment service. For example, this does not replace the need for risk assessment and management by local health services, or requests for referral for psychological therapy.
Peer support and mentorship
Peer support roles are becoming more commonplace in mental health services, and these are intended to be paid positions. Health Education England (HEE) has been developing a new Autism Peer Support Worker role. To this end, HEE has commissioned the development of a framework of core skills and capabilities required by Autism Peer Support Workers. Training will be provided for these roles to enable people with lived experience of autism to provide support to other autistic people who are experiencing health difficulties. Peer support (carers) could also be provided to family/carers of autistic people. The training and implementation of these roles will be piloted in 2023.
Crisis intervention and prevention
According to the Building the Right Support National Plan (46), autistic people who are experiencing a mental health crisis, who are at risk of admission to hospital or who are admitted to hospital have a right to have a Care (Education) and Treatment Review. They should also be placed on the Dynamic Support Register if they are in or at risk of admission to a mental health inpatient setting. Key working services are also available in every area funded through the NHS Long Term Plan (4).
Some people seen for an autism assessment may potentially be eligible for input under the Building the Right Support National Plan. In this instance, there should be clarity about which service will make the referral to the person in a commissioning role (that is, the referrer, a mental health team, or the autism assessment service).
In some instances, the autism assessment service may be asked to attend a Care (Education) and Treatment Review if the autism assessment has been completed very recently and, for example, the outcome documentation has not yet been finalised and circulated. Within this forum, there should be clarity about the remit and parameters of each professional and service involved. For example, it may be that post-assessment support can be postponed until such time that the person is able to attend this.
Liaising with other services after the assessment
Following the autism assessment, it may be beneficial for a designated clinician to offer information, consultation or feedback to external professionals involved in providing ongoing care, further assessment or education to the person. The person and family/carers may also be involved in this. Regular meetings between services offering autism assessments and other services should be arranged to ensure people and their family/carers are supported through the respective pathways, especially at times of transition.
Supporting people who relocate prior to or during delivery of post-assessment support
Some people and their family/carers may move out of the area prior to post-assessment support being fully delivered. The autism assessment service should provide clarity about whether it can honour the offer of post-assessment support in this instance and for what time period this extends to (for example, if a person moves abroad for an extended period). Conversely, the service should operationalise whether it can provide post-assessment support to autistic people and their family/carers if the diagnosis was made by another NHS service or independent provider.
Specific considerations for developing post-diagnostic support for children and young people diagnosed as autistic can include:
- Considering the age and developmental stage mix of children and young people attending group interventions.
- Running group interventions at times that fit with the education settings day and other childcare responsibilities family/carers may have.
- Providing a quiet space for family/carers to use while their child is attending individual or group interventions.
- Offering family/carers adjunctive post-diagnostic support sessions.
Specific considerations for developing post-diagnostic support for people approaching transition diagnosed as autistic can include:
- Setting up protocols that outline which service will provide post-diagnostic support if the young person is due to transition to adult services before this has been offered (that is, the children and young people or adult service).
- Noting any differences in eligibility criteria for post-diagnostic support for children and young people and adults, across services.
- Developing resources focused on issues relating to transitions (for example, coping with exam stress, starting university, moving out of the family home).
Specific considerations for developing post-diagnostic support for adults diagnosed as autistic can include:
- Considering the age and life stage mix of adults attending group interventions.
- Providing clarity about the remit and parameters of group interventions.
- Running group interventions at times that fit with higher education and occupational responsibilities adults may have.
- Developing a protocol regarding whether group interventions can be offered via telehealth, and if so, what the eligibility criteria for this are.
Discharge from the services providing autism assessments
Discharge from the service conducting the autism assessment takes place after the clinical assessment conclusions have been reached and the letter has been sent, or after post-assessment support or intervention have been delivered. People may be discharged back to the care of the professional who initially referred them for an autism assessment (for example, the community psychiatrist), or to the GP if they are no longer open to the referring service.
Sometimes it can be useful to give a verbal handover to the referrer or other services and any professionals involved in the person’s care and support.
Sending a formal discharge letter is standard practice for all people seen for an autism assessment, whether or not they are diagnosed as autistic, unless this has already been documented in the assessment outcome letter. This should include the following information at a minimum:
- Updated personal information if there have been any recent changes (for example, to the person’s name, contact details).
- A concise summary of what input the service conducting the autism assessment has provided and when (for example, seen for an autism assessment, attended a post-assessment group).
- A statement indicating the clinical assessment conclusions.
- An outline of any pertinent clinical issues that warrant short-term consideration or input by the referrer or GP (for example, relating to risk).
- A list of requests for other professionals to action, if needed (for example, please refer for further occupational therapy input or a medication review).
- Clarity about the date the person is being discharged from the service.
People and their family/carers should be made aware of the discharge date and what this means for them in terms of any further contact (for example, whether they will be asked to provide anonymous feedback about their experiences). They should also be made aware of which service or professional they should contact if they have questions about the assessment outcome or further assessment or intervention.
Clinical records should be updated to reflect the date the person is discharged and by whom promptly.
Part 2. Common variations in how the autism assessment is conducted
Many people will have a standard or enhanced autism assessment at a local autism assessment service, but some people will have a different experience. For example, they may be assessed jointly with another service or require adaptations to usual practice.
There should be eligibility criteria for different types of autism assessment by each service. This information should be communicated to people and their family/carers as part of the identification and referral, or screening and triage stages of the autism assessment pathway.
Telehealth
The COVID-19 pandemic impacted service provision across the NHS. Many autism assessment services introduced telehealth to conduct components of, or the entirety of an autism assessment.
Telehealth refers to digital healthcare practices for the purpose of delivering health-related services and information, using methods including video calling, telephone services (voice- or text-based) and apps or web portals. There is preliminary empirical support for using this approach in terms of autism assessments and primary care interventions for autistic people from research studies conducted before and during the pandemic (47–49).
At the time of preparing this document in early 2023, COVID-19 restrictions have been lifted. However, there continues to be variation in routine service provision by autism assessment services across England, with some working exclusively in person, some exclusively offering telehealth assessment and others using a mix of both.
In 2021, the autism team at NHS England commissioned Autistica to produce a briefing report outlining considerations for using telehealth methods in healthcare delivery for autistic people (50). Autism assessment services via telehealth methods should consider the following.
- Telehealth autism assessments should be conducted in accordance with current organisational policy and guidance (for example, using the approved e-platform, and ensuring security settings are switched on during an appointment to limit the possibility of anyone else joining the meeting).
- Clinical and risk issues permitting (see below), people and their family/carers should be able to indicate their preference for being seen in person, via telehealth or with a hybrid approach. For example, people and their family/carers could provide this detail, including their email address, as part of the referral or screening and triage process.
- People and their family/carers should be provided with an information sheet about telehealth (for example, at the point of referral, or at screening and triage). This may be developed by the autism assessment service or the organisation more generally and outline:
- Issues for people and family/carers to think about in terms of the range of advantages and considerations with having the autism assessment via telehealth (such as, no need to travel, but a lack of privacy at home)
- What happens during in-person and telehealth assessments, so that people and family/carers can effectively ‘walk through’ the process before making a decision about which to opt for
- Practicalities associated with using telehealth (for example, how to log on to the platform and access the meeting link)
- Answers to troubleshooting questions (including who to contact if the meeting link is not working)
- Environmental considerations (for example, optimal set up for the appointment such as being in a quiet location, with privacy, good internet access)
- Clinical considerations (such as what to do if the person or family/carers become highly distressed or agitated during a telehealth appointment).
- Ideally, telehealth should be accessible to everyone on a waiting list for an autism assessment and their family/carers, if this is clinically appropriate, and including people who do not have access to internet-enabled devices or require an interpreter service.
- Each autism assessment service or all services doing so collectively in the area offering at least some autism assessments via telehealth, should develop clinical guidelines indicating:
- Reasons for offering people an in-person versus telehealth autism assessment, or giving the option for either (for example, some people may present with significant mental health issues or risk or systemic factors within the home that seem to clinically warrant an in-person appointment)
- An outline of factors that suggest people should be seen in person rather than via telehealth after they have attended for a first appointment or if new information comes to light
- Any additional considerations for assessment and management of risk or safeguarding when seeing people and family/carers off site
- How to manage unanticipated situations that could occur during a telehealth appointment (such as if the internet connection fails, or the person discloses imminent risk)
- If and how post-assessment interventions require adaptation if they are delivered via telehealth as opposed to in person.
- Use of telehealth methods of service delivery should be evaluated regularly by the autism assessment service to establish factors, including what is working well or not, or whether any specific sub-groups of people are waiting disproportionately longer for the autism assessment or post-assessment support (for example, due to digital poverty or substantial risk).
Joint assessments with clinicians from another service
Sometimes, the autism assessment is conducted by clinicians from the autism assessment service in collaboration with clinicians working in another service (such as mental health, learning disability or ADHD assessment services). This might be because the person is well known to the other team and there is consensus that a joint assessment by both services will be clinically appropriate and, potentially, an efficient use of resources. Alternatively, it may be that the person has several areas of need, and concurrent assessment by two services could result in a more complete formulation/clinical assessment conclusion and better support for the person. In this event, it is useful for the clinicians involved in the process to meet prior to the autism assessment commencing. This is an opportunity to:
- Share relevant background and contextual information about the person.
- Consider whether there is a need to embed reasonable adjustments or adaptations into the assessment process, so that this is more tailored for the person’s needs or preferences (for example, in relation to previously identified sensory sensitivities, use of communication aids, attentional impairments).
- Clarify what, if any, components of the autism assessment have already been conducted, when, by whom and the outcomes.
- Establish which MDT clinicians are best placed to conduct the assessment based on the person’s identified difficulties or needs (for example, including a clinician with a medical background or a speech and language therapist).
- Identify focal points for the joint assessment, which methods will be used (for example, autism assessment tools) and who will have responsibility for administering these.
- Decide about practicalities such as which service will arrange appointments, who will coordinate preparation of the assessment letter and upload information to the clinical records, and how post-assessment support will be organised.
Working jointly in this way can reduce the likelihood of people falling through gaps between services, such as when a person with a borderline or mild intellectual disability is not eligible to access a Learning Disability service, but whose needs may not readily be met by autism assessment services to people who do not have an intellectual disability.
Assessment of people in mental health inpatient settings
Some people may be admitted to a mental health or forensic ward at the time they are due to be offered an autism assessment. They may be admitted on a voluntary basis or detained under the Mental Health Act 1983.
Ideally, autism assessment services should be informed in advance if there has been a change in the person’s mental health or emotional well-being or risk, such that they are deemed to require an inpatient admission. Furthermore, if the person has been admitted to an establishment far from home, clarity will be needed about whether they will be seen by the initial autism assessment service that they were referred to or if a local autism assessment service may offer this instead. The referrer should also be kept up to date.
The appropriateness of undertaking an autism assessment when people are in hospital depends on several factors, including:
- clinical symptomatology (for example, what mental health symptoms they are experiencing, acuity of these and degree of impairment)
- current circumstances (for example, how settled the person is)
- engagement (for example, whether the person will be able to participate in all the components of an autism assessment if there are factors that substantially impact attention, concentration or memory)
- level of distress (for example, whether conducting an autism assessment will increase the person’s level of distress, even if unintentional)
- risk (for example, imminent risk to self, very high risk to others)
- timing (that is, considerations, advantages and disadvantages with conducting the autism assessment now versus waiting until the person is less symptomatic)
- potential imminent utility of outcomes (for example, that an autism diagnosis would mean the person is eligible to have a Care (Education) and Treatment Review, can be placed on the Dynamic Support Register)
- the likelihood that the range of factors highlighted above will impact on completion of the autism assessment and the possibility of drawing meaningful clinical conclusions about diagnosis.
Decisions to proceed with, or delay, the autism assessment should be discussed with the person, their family/carers if appropriate, and informed by discussions with the referrer, the clinical team providing inpatient care and potentially other professionals who are involved.
If a decision is made to delay the autism assessment, there should be agreement about when this decision will be reviewed and by whom (that is, which professionals), what factors are deemed to need to change so that this can proceed (for example, what a reduction in mental health symptoms looks like, what the threshold is for attention and concentration capability in order for the person to engage with the process) and who will be measuring these factors and updating professionals in the system, including the referrer.
If a decision is made to proceed with the autism assessment while the person is in hospital, this is likely to require some additional planning beyond the standard and enhanced autism assessments taking place in the community. Factors to consider include identifying:
- What information has been obtained during the hospital admission that is relevant to review prior to commencing (for example, initial assessment by the psychiatrist, assessments or progress notes by MDT clinicians).
- Which MDT clinicians from services conducting autism assessments are best placed to be involved in the process (for example, a psychiatrist or clinical psychologist).
- Which professionals in the clinical team providing inpatient care may be able to be involved in the process (for example, gathering information about particular themes, supporting completion of self-report screening questionnaires).
- Who (which professional from which service) will discuss the autism assessment with the person and assess capacity to participate in this, as well as liaising with family/carers if appropriate.
- How to set up assessment appointments in a way that suits the person and the ward (for example, what time of day and which days of the week do not interfere with the person’s structured activities and are easier for the ward to accommodate, including environmental adjustments for sensory differences).
- What caveats there are to undertaking the autism assessment at that time (for example, if the person becomes floridly unwell, or risk substantially increases).
- When, how and to whom the clinical assessment conclusions should be communicated.
- Which service will provide post-assessment support relevant to the outcome.
A summary of discussions and decisions made should be recorded on the clinical records.
Outreach assessments
Some people may have moved out of the catchment area for the autism assessment service between the point of referral and the autism assessment taking place. For example, they may reside in a residential education setting, residential social care setting or have been admitted to a specialist inpatient service in another area. Ideally, the service providing the autism assessment will be kept updated about any changes in contact details for people on the waiting list and clinical factors relevant for decision making about optimal times to do the autism assessment, and what this should comprise (for example, the skill set of clinicians meeting the person).
Depending on commissioning agreements, some services will provide outreach autism assessments, with clinicians visiting the person if they are unable to come to in-person appointments and telehealth is not viable. The reasons for and remit of outreach autism assessments should be explicit for referrers, people and their family/carers.
Assessment of people with additional needs
Depending on commissioning agreements and autism and wider service pathway arrangements, autism assessment services may accept referrals based on clear criteria, such as people who do not have additional needs (including intellectual disability). When autism is considered a possible diagnosis for a person with a known intellectual disability, the appropriate learning disability service should be well placed to conduct the autism assessment. MDT professionals should have knowledge and expertise of assessment of features of autism in the context of features and behaviours consistent with an intellectual disability. Screening and assessment tools appropriate for a person’s cognitive and communication differences should be available and used routinely. Communication aides should be employed as needed, to support the inclusion of the person in the process. Careful gathering of corroborative information from family/carers is essential for forming a comprehensive a picture of the person and their strengths, needs and aspirations as possible.
There are some instances when a person does not meet the formal criteria for an intellectual disability, but the referral should be made or transferred to the learning disability team. For example, if cognitive testing indicates a highly mixed cognitive profile with borderline intellectual disability in verbal or non-verbal domains, or functional assessment suggests their needs would be better understood and supported by the expertise available in the learning disability service.
Alternatively, a joint assessment with the learning disability service may be indicated. Post-assessment support and psychoeducation will likely need tailoring to the person’s needs as the standard group psychoeducation programme on offer may not be appropriate.
Assessment of people in residential education settings
In some instances, children and young people in residential special education settings (who should all be in receipt of an EHCP) may be identified as needing an autism assessment while they are placed in residential education settings. While circumstances and presentation may be complex, a clear clinical rationale must be provided if an autism assessment is not conducted at this time, such as the child or young person is due to relocate or return home and the process cannot be completed during this time. A request for an autism assessment or annual review would follow the same process as for any child or young person in the community.
The period for which the child or young person is resident (38-52 weeks) may have an impact on their legal status. Some children and young people will be looked after under different sections of The Children Act 1989, in which case parental responsibility may be shared between parent carers and the local authority. When children have a looked after status – either under s.20, s.31 (or other section of the Children Act 1989) the local authority will have other responsibilities as a corporate parent. Consideration needs to be given as to who holds the legal responsibility to make decisions for the child or young person. However, the child or young person should be involved in decision making and the referral process for an autism assessment.
The needs of children and young people in these settings are likely to be complex and an enhanced assessment should be conducted with close collaboration between clinical, educational and support staff to reach a diagnostic outcome and comprehensive formulation of the child or young person’s strengths and needs.
However, some young people may not wish to proceed with an assessment or may be reluctant to involve their parents or carers. Care must be taken to provide information that is accessible and transparent with respect to the purpose of the assessment, the process and likely outcomes. If a child or young person is diagnosed as autistic, their EHCP plan and any other relevant plan (such as Looked After Child) should be revised to ensure it reflects the diagnosis and recommendations for care and support.
If a diagnosis of autism is made, post-diagnostic support and intervention should address needs across education and residential domains, potentially including consultation for education, therapeutic and residential staff in supporting the child or young person. Reasonable adjustments and consideration of transitions would be as relevant as for children and young people in the community.
Assessment of people in the criminal justice system
Some children, young people and adults are identified as needing an autism assessment while they are in secure and detained settings. Such settings include prisons, secure facilities for children and young people and immigration removal centres.
The national framework and operational guidance may be helpful to consider when commissioning and delivering autism assessment pathways. However, there is already guidance from NHS England best practice guidance concerning meeting the healthcare needs of adults with a learning disability or autistic people in prison (51) and best practice guidance for those accessing Liaison and Diversion services (52). In all guidance, the importance of identification, screening, assessments, appropriate support, pathways and partnership working is emphasised.
The Ministry of Justice published an action plan to address the issues raised by a 2021 Inspectorate report on neurodiversity in the criminal justice system (53).
Assessment of people by national specialist services
Many people are seen by an autism assessment service in the area within which they live. However, for a proportion of people, referral to a national specialist service may be considered appropriate. This may be for several reasons. For example, there may be no existing autism assessment service that the person can access in their area. Alternatively, the person may present with a high level of clinical complexity and a more in-depth assessment of autism, and differential and co-occurring diagnoses is being sought. On some occasions, it may be that the person has previously had an autism assessment but there is no clear assessment outcome due to clinical complexity, and therefore, an opinion from another service is deemed pragmatic.
Routes to a national specialist service can vary (such as, whether a GP or clinician working in secondary care setting can instigate the referral and whether the person needs to have already had an autism assessment in the area they live).
Information about the autism assessment pathway for people, their family/carers and professionals should outline the process for making referrals for an autism assessment to a national specialist service. This should include whether the person will first need to be seen by an autism assessment service in the area they live and whether they need to be open to a specific health service concurrently (for example a secondary care mental health service).
Referrals to national specialist services should be detailed and include copies of any correspondence reports from health and social care services or education settings that may be relevant for informing decisions about whether the national specialist service accepts the referral and the subsequent autism assessment. National specialist services may not have access to the same clinical records, and so the referrer or professional who knows the person well may need to amalgamate relevant information.
There should also be clarity about which service has responsibility for risk assessment and management while the person is awaiting an autism assessment. There should also be clarity about which professional or service will be expected to action any outcomes or recommendations following the autism assessment (such as for referring for or overseeing further assessment or post-assessment support).
Second opinion referrals
Some professionals, or people or their family/carers, may seek a second or even third opinion, to clarify whether a person meets diagnostic criteria for autism, with or without co-occurring conditions.
Second opinions may be sought when a person or their family/carers disagree with the existing clinical assessment conclusion(s), or when there is clinical uncertainty about initial clinical assessment conclusion (for example, that this was made some time ago, or the person had symptoms from another condition that substantially impacted their clinical presentation). Further opinion about possible autism diagnosis may also be sought at a different point in time (for example, some years after an initial autism assessment, and if the person’s autistic traits have become more apparent). It is important that the rationale for seeking a second opinion is clarified for each person.
ICBs should have a local policy regarding second opinion autism assessments, focusing on issues including:
- Operationalisation of criteria used to decide whether to accept or decline second opinion autism assessments.
- Whether people can be seen by a second clinician at the service that conducted the initial autism assessment.
- Whether it is helpful to have reciprocal agreements with other services in the area, as part of the autism assessment offer, that may be able to provide a second opinion assessment.
- The process of referring people to a service outside their local area or to a national/specialist service and for what reasons.
- The rationale and protocols for removing diagnoses (such as an autism diagnosis being queried during an inpatient admission, or a previous diagnosis of personality disorder being queried when a new diagnosis of autism is made).
In instances when a second opinion autism assessment is offered or there is a question about removing an existing autism diagnosis, the clinician(s) should have access to previous correspondence, including the original autism report as well as the write up of specific methods of assessment (for example, of autism assessment tools).
Consideration is needed regarding which clinicians will conduct the assessment (that is, representing which professional disciplines, with what level of experience or seniority, and expertise in autism). As with all autism assessments, there should be emphasis on gathering sufficient current, contextual, developmental and historic information, in order for clinicians to be able to develop a clinical formulation and reach a decision about autism diagnosis. Completion of self-report screening questionnaires or standalone behavioural observation assessments is insufficient. The parameters of the assessment should be clear for people, their family/carers and professionals (that is, what the specific remit of the appointments is, and that the outcome may not be different from the previous clinical assessment conclusions).
Assessments by independent providers
Sometimes, independent providers are commissioned to conduct autism assessments, either as part of a block contract or per person (for example, through referrals where patients have exercised their legal rights to choice of provider/team). Independent providers may be based in the local area, regionally or nationally. People, their family/carers may also seek and self-fund an independent assessment.
Issues that inform decision making about whether to commission an independent provider include the following:
- Parity of provision – service provision should be comparable to the local NHS offer with respect to quality standards, flexibility and experience for people and their family/carers.
- Parity of regulation – at present some providers of autism assessments are registered with the CQC and others, especially independent sector providers, are not. While that remains the case, ICBs commissioning autism assessments should consider the extent to which any provider that is not CQC registered can offer reassurance that this will not be to the detriment of the person assessed, and the way in which this distinction and its implications will be communicated to the person and their family/carers as appropriate.
- Accessibility – the service should be accessible to all people who could potentially be referred from the area.
- MDT representation – some autism assessments require input from different professional disciplines (for example, psychiatry, psychology and occupational therapy, see Second opinion referrals for more information). The clinicians best placed to see a person for the autism assessment may be known at the point of referral. Alternatively, this may become more apparent during the screening and triage stages, or once the assessment has commenced. Services need an MDT workforce, with options for different clinicians to become involved, as indicated. At least one clinician conducting the autism assessment should be a mental health professional (for example, psychiatrist, clinical psychologist, mental health nurse), given the high possibility that people may have differential or co-occurring diagnoses.
- Differentiated pathway – components of the autism assessment can vary slightly, depending on the needs and difficulties of each person. For example, some people will need to meet one experienced clinician, whereas others will benefit from seeing several clinicians. The service should be flexible and be able to offer the components of the assessment that are relevant to each person.
- Location of assessment – some services offer in-person appointments, whereas others use telehealth, or a hybrid approach of both methods. There is preliminary evidence of feasibility and reliability of telehealth autism assessments (49,54). However, there is insufficient research to date indicating what the optimum components of telehealth appointments are (for example, in terms of structure, process and methods of assessment) and whether this is a sufficient approach for all people (that is, does it affect the rate of false negative and false positive diagnoses when compared with in-person appointments). Additionally, telehealth may not be feasible for some people and their family/carers, due to factors including digital poverty, risk or safeguarding issues, or personal preference. The service, therefore, should be able to offer in-person appointments if these are clinically indicated or this is the person’s preference.
- Components of assessment – the autism assessment should include a clinical interview with the person, augmented with information obtained in other ways such as observation in education settings for children and young people. Use of screening questionnaires and assessment tools (such as the ADOS-2 and ADI-R) are insufficient on their own. Assessments must include core components outlined in the components of a good clinical assessment section of this document.
- Conversion rates – the proportion of people diagnosed as autistic following an autism assessment, versus those who are not, differs between services. Conversion rates should be made available to those in a commissioning role and the local or regional NHS services that provide autism assessments. These should be considered alongside the conversion rates for other services in the area and would be expected to be broadly comparable.
- Outcome documentation – assessment documentation should be shared in a timely way with people attending for the appointment, their family/carers and professionals involved in the person’s care and support.
- Post-assessment support – evidence indicates that many people diagnosed as autistic benefit from post-assessment support (40,55). This can include signposting and interventions, offered individually or in groups, in person or via telehealth. To promote parity of provision, comparable post-assessment support should be offered that is similar to other services in the area.
- Audit and service evaluation – evaluation of services provided is key to ensuring that people and their family/carers are offered high quality, accessible and effective care. Services should conduct regular audit and service evaluation and findings should be shared with those in a commissioning role.
People and their family/carers should be informed at the outset of the autism assessment pathway, as to whether there are any implications of accessing an assessment via an independent provider, rather than an NHS service. For example, whether the person and their family/carers will have access to local support while waiting for an assessment (that is, pre-assessment support) and post-assessment support.
Part 3. Training, consultation and liaison, and supervision
Autism assessment services also offer support to professionals working with autistic people and people who may be autistic. General types of support include autism-relevant training, consultation and liaison, and supervision.
Training
In some areas, autism assessment services organise autism-relevant training for other professionals, including MDT trainees and students. Doing this can enhance the knowledge, skills and confidence of professionals working in mainstream services, so that they can work more effectively with autistic and possibly autistic (but not yet assessed) people. National Frameworks are available to support staff and managers in considering the core competencies required when working with autistic people (22).
The type of training delivered will depend on the requirements of other services, the professional skill mix of clinicians in the autism assessment service, as well as time and resources. Working jointly with other autism assessment services to develop a local area training offer can help to reduce duplication.
Training can be formal or informal, and generic or bespoke. This must also fit with the organisation’s training strategy and policy and may take place alongside the Oliver McGowan Mandatory Training on Learning Disability and Autism. Ideally, training materials are co-produced and delivered by autistic people and family/carers.
Key considerations regarding training delivery are:
- Determining whether the autism assessment service is the right service to deliver this.
- Having clarity about the purpose of the training, and who (which professional disciplines and level of experience) will attend this.
- Providing the trainers with access to up-to-date research and clinical guidelines so that this can be embedded in teaching materials.
- Delivering training to professionals from different services concurrently, if appropriate.
- Identifying the learning outcomes and objectives in advance.
- Considering the appropriateness of training relating to autistic people of all ages, with the needs of young people and family/carers being different to those of adults.
- Choosing methods of training delivery that are accessible, efficient and effective (for example, delivering training online).
- Evaluating outcomes before and after training.
- Ensuring there is scope for training attendees to offer qualitative feedback.
- Maintaining a log of training requests and sessions delivered to avoid duplication.
- Providing the necessary training and support for professionals, and autistic people and family/carers so that they can contribute to the design, delivery and evaluation of training provision.
Consultation and liaison
Colleagues working in mainstream and specialist services can benefit from consultation and liaison with clinicians working at the service conducting autism assessments. For example, to discuss the possible needs of autistic people, and people with possible autism who are awaiting an autism assessment, who are accessing other services (for example, adjustments to sensory environments or accounting for communication preferences). Consultation is one way that clinicians working in non-autism services can become more knowledgeable, skilled up and confident to work with autistic people.
Key considerations regarding provision of consultation and liaison are:
- Clarifying what the aims of this are, what outcomes are expected, and for whom.
- Establishing which clinicians (that is, representing which professional disciplines) are best placed to provide this.
- Obtaining the person’s consent for this to go ahead.
- Deciding who can attend.
- Documenting a summary of the discussion, aims, outcomes and action points in the clinical records, including ensuring there is clarity about which service holds clinical responsibility for the person.
- Obtaining quantitative and qualitative feedback about the process.
Clinical supervision
All professionals using standardised assessment tools should only do so after they have completed relevant training and gained sufficient experience to be signed off to administer using these.
Professional and accrediting bodies for each of the clinical disciplines (for example, General Medical Council, Health and Care Professions Council, Nursing and Midwifery Council) provide guidance on the key characteristics of effective supervision for professionals registered with the Health and Care Professions Council (56). This includes how often meetings should take place, the level of seniority and clinical experience of supervisors and requirements for them to be signed off as competent in this role.
In some autism assessment services, the supervisor will have the same professional background as the supervisee. When this is not possible, it is important that the supervisee can access supervision that will allow them to continue meeting requirements for revalidation of their professional pin number.
Some autism services provide a combination of individual, group and peer clinical supervision. Each of these forums have merit. Combined group or peer supervision with clinicians working at similar services in the area can also be a useful means for exploring issues pertinent to the area. Formal terms of reference and clear governance are essential to ensure the agreed remit and scope of supervision and discussion groups are clear and confidentiality is maintained in relation to any clinical discussions. Local and regional discussions may highlight common areas of concern and identify learning needs across services and professional disciplines.
While professionals in autism assessment services may be well placed to offer supervision and training to practitioners working in generic and specialist services (mental and physical health settings), highly specialist knowledge and skills will be in evidence within certain teams where autism co-occurs with mental health conditions, for example, psychosis and opportunities for shared learning should be facilitated.
Appendix A. Glossary
Table 2. This shows the abbreviations and definitions used throughout this document.
| Abbreviation | Definition |
| ADHD | Attention deficit hyperactivity disorder |
| ADI-R | Autism Diagnostic Interview – Revised |
| ADOS-2 | Autism Diagnostic Observation Schedule-2 |
| CSDS | Community Services Dataset |
| DISCO | Diagnostic Interview for Social and Communication Disorders |
| DSM-5 | Diagnostic and Statistical Manual for Mental Disorders, fifth edition |
| EHCP | Education, Health, and Care Plan |
| GP | General Practitioner |
| HEE | Health Education England |
| ICD-11 | International Classification of Diseases and Related Health Problems, eleventh edition |
| ICS/ICB | Integrated Care System and Integrated Care Board |
| MDT | Multidisciplinary team |
| MHSDS | Mental Health Services Dataset |
| NICE | The National Institute of Health and Care Excellence |
| SENCO | Special Educational Needs Coordinator |
| SEND | Special Educational Needs and Disabilities |
| SPA | Single point of access |
Appendix B. Suggested autism assessment services development stakeholders (ICS and ICB)
- Representatives from the ICB and ICS
- Operational managers, service leads and MDT clinicians for autism assessment services and allied primary, secondary and tertiary developmental and mental health services
- Operational managers, service leads and multidisciplinary team clinicians from primary and secondary medical health services, including General Practitioners, paediatricians and health visitors
- Transition workers
- Operational managers and service leads working in the criminal justice system and forensic services
- Autistic people and family/carers
- Representatives from third sector organisations providing advice or support to people who may access the autism assessment pathway
- Operational managers and service leads who have responsibility for social care support
- Educational psychologists, SENCOs, Local Authority SEND Leads, teachers and representatives leading on the SEND agenda
Appendix C. Examples of common barriers to treatment
Table 3. This shows examples of barriers to accessing the initial stages of the autism assessment pathway, split by type of barrier.
| Category | Barriers to accessing initial stages of the autism assessment pathway |
| Service-related | • Fragmented and inflexible services. • Lack of clarity about which service provides autism assessments. • The need for review by multiple people. • Long waiting times. |
| Professional-related | • Mainstream professionals’ lack of knowledge or understanding of autism and its heterogeneity. • Inaccurate or biased preconceptions about autism. • Lack of support to proceed with an autism assessment. • Diagnostic overshadowing. |
| Family/carer-related | • Perceived stigma associated with autism. • Lack of knowledge or understanding of autism. • Difficulties knowing where and how to access help. • Negative previous experiences with professionals, and apprehension about approaching them again. |
Appendix D. Information to be included in a referral letter
Referrals for an autism assessment can include the following information, when known:
- Full name of the person, and the name they prefer to be called if this is different (for example, Steven Jones, preferred name Steve).
- Their date of birth and age.
- Gender and preferred pronouns.
- Current contact details and the person’s preferred mode of contact (for example, letter, telephone, email).
- A summary of past and current developmental, medical and mental health diagnoses.
- A list of pending medical, mental health or developmental assessments or investigations.
- An overview of current and past treatment for developmental, physical or mental health conditions, including what treatment was offered and a summary of the treatment response.
- Copies of relevant developmental or mental health letters or reports written by other professionals.
- Reason for the referral, including examples of autistic traits, symptoms or behaviours the person has, or others have noticed and the context(s) within which these manifest (for example, only at home or at home, education settings and social situations).
- Scores of any developmental or mental health screening questionnaires or standardised tests used.
- Clarity about whether any risks have been identified at the time the referral is made, including directly or indirectly to the person or to others. If there are known risks, a copy of the risk assessment and crisis safety plan should be provided
- Any past or current contact with the criminal justice system.
- Information relevant to the practicalities of arranging an autism assessment, such as whether the person is agoraphobic, has access to the internet or is due to move home.
- Clarity about whether the person has additional needs (for example, an intellectual disability, visual or hearing impairment) that may require adaptations to an autism assessment.
- A note about whether there are any known impending transitions or changes (for example, parents separating or divorcing, a house move).
- A statement indicating whether the person is aware the referral has been made and has consented to this. If the person is not aware of this or they have not provided consent, the rationale for making the referral should be clearly documented.
Appendix E. Triage
Standardised screening strategies
- Self-report questionnaires are completed by the person. These may screen for autistic traits, traits of other developmental conditions (for example, ADHD), mental health symptoms (for example, low mood, anxiety, emotion regulation), or the impact of current difficulties on daily functioning. Care must be taken in the interpretation of questionnaires, particularly where people may have speech and language or literacy difficulties.
- Informant-report questionnaires are completed by someone who knows the person well now, or knew them well as a child, such as family/carers, a partner or a professional. These may screen for traits associated with autism or other developmental conditions, mental health symptoms, as well as general behavioural difficulties and the impact of these for the person and possibly others around them. For children and young people these may be completed by professionals in education settings such as colleges. For some adults, it may be difficult to identify reliable informants to provide developmental and personal information. Also, care must be taken to obtain up-to-date written consent prior to contacting informants, and to protect confidentiality in the process of gathering third-party information.
Semi-structured screening questionnaire developed in-house by the autism assessment service
- Some services develop a document to collect information from the person, their family/carers or significant others in their lives (such as a partner) and professionals the person is currently in contact with or has been recently. Ideally, these documents are developed in collaboration or consultation with people who use the service and their family/carers, to ensure these are structured and phrased meaningfully.
- It can be advantageous for autism assessment services within the area to collect similar information or to use the same document (with age and stage relevant additions and omissions). This makes it easier for referrals to be passed between services (for example, in the case of people transitioning from children and young people to adult services). It also limits the need for the same information to be sought on repeated occasions.
- These questionnaires commonly collate factual historical information (for example, about mother’s health during pregnancy, age at which developmental milestones were met), family context (for example, health and wellbeing of family members), schooling (for example, details about attendance, additional support provided) and health and wellbeing history (for example, art therapy or access to community support).
Review of correspondence relating to medical and mental health history
- Some people have had regular or substantial contact with medical or mental health services, in the past or at the time of the referral for an autism assessment.
- At the very least, a summary of the history should accompany the referral letter. Review of correspondence is integral to screening, particularly letters and reports that summarise history, treatment plans and progress.
Review of correspondence relating to contact with other developmental services
- Some people may have been seen by other developmental services, including ADHD assessment services or services for people with an intellectual disability.
- Correspondence from these appointments, such as an overview of what the assessment comprised, test results (for example, IQ and functional ability scores) and overall clinical assessment conclusions, is highly informative. This can reduce the likelihood of repeating tests unnecessarily.
Information about contact with the criminal justice system
- Some people may have had past or current contact with the criminal justice system, either as a victim or perpetrator of a crime (or alleged crime).
- Review of information relating to cautions and convictions is important, as this can inform decision making about risk and vulnerability.
In-person triage
Some services offer people an initial triage appointment. The purpose can vary. For example, this can be an opportunity to more formally determine whether an autism assessment is clinically indicated, or to gather general information that can be used to inform the autism assessment. People and their family/carers should know what the aims and possible outcomes of the appointment are.
Meeting with family/carers, partners or friends
Significant others (typically family/carers of adults) are sometimes invited to attend an appointment as part of the triage process, most commonly to provide background information about childhood history and development, and additional context (for example, the person’s current difficulties from their perspective). Consent to speak to someone else should normally be obtained from the person. If consent is not granted, but others are contacted nevertheless, the rationale for doing so should be documented in the clinical records. Family and carers of children and young people under the age of 16 should be included in triage and assessment since they have parental responsibility.
Some services use validated standardised semi-structured interviews to gather information, whereas others develop a bespoke interview. As with other forms of triage, reasons for offering this appointment, and how the information will be used, should be clear from the outset.
Liaison with professionals the person is in contact with
When feasible, and consent-permitting, it can be useful to speak with professionals who are currently or have recently been in contact with the person, such as professionals working in health and social care, education, the criminal justice system or third sector organisations. This can help to clarify information about parameters of their involvement, approaches or interventions offered, to or the effectiveness of these and anticipated next steps.
Appendix F. Data reporting
Autism assessment services are an important element of the Government’s National Strategy for Autistic Children, Young People, and Adults (21). This emphasises a focus on ensuring ‘demonstrable progress on reducing diagnosis waiting times and improving assessment pathways for children, young people and adults across the country’. For adults and children and young people referred for assessment to mental health services, this will be monitored through the monthly submissions mental health care providers make to the MHSDS. For children and young people assessed through paediatric services it is likely that it will be monitored mainly through submissions to the CSDS.
At present referrals to autism diagnosis services in mental health services are identified through the Primary Reason for Referral specified in MHSDS table MHS101. This should be coded ’25 – Suspected Autistic Spectrum Disorder’. This code should not be used for any other referrals. If a person has been referred to the provider for another reason, but clinicians initially assessing them consider an autism assessment is appropriate, a second referral should be made for this.
Contacts between clinical staff and the referred person are normally recorded in the Care Contacts (MHS201) and Care Activity (MHS202) tables. The clinical discipline and grade of staff undertaking contacts is of interest. This should be recorded in the Staff Details (MHS901) table and providers should ensure that links between this and the Care Activity table, through the Care Professional Local Identifier field, are intact.
During the course of an assessment, an autism diagnosis or other diagnoses may be made. These should be recorded in the Primary Diagnosis (MHS604) and Secondary Diagnosis (MHS605) tables.
The Referral Request Received Date and Service Discharge Date in the Referrals table, along with the dates of contacts and of recording of diagnoses provide the basis for assessment of waiting times.
Further work is currently under way:
- To develop additional Systematized Nomenclature of Medicine to record the method of termination of autism diagnosis assessments, structured tools used in the assessment process, whether the process was conducted face to face or through tele-consultation, whether an autism diagnosis made was the first the person has received, and the outcome of the assessment. The last is needed in part to allow recording of the negative clinical conclusion that a person is not autistic.
- To assess the developments needed in the CSDS to allow similar monitoring of autism assessments undertaken by paediatric services.
Appendix G. Core components of autism assessment report
Core components of an autism assessment report:
- reason and background to referral
- dates seen and format (face-to-face, telehealth or hybrid)
- professionals involved
- sources of information, including parents, teachers, partners, employers etc.
- screening tools used and results
- autism assessment tools
- assessment system, for example, ICD-11 or DSM-5
- summary of current functioning
- summary of health and wellbeing, including risk
- summary of developmental and personal history
- assessment formulation
- consideration of the impact of strengths and needs
- recommendations and next steps.
Core components of brief autism assessment statement (optional):
- reason and background to referral
- dates seen and format (face-to-face, telehealth or hybrid)
- professionals involved
- sources of information, including parents, teachers, partners, employers etc.
- screening tools used and results
- autism assessment tools
- assessment system, for example, ICD-11 or DSM-5
- summary assessment formulation
- reference to recommendations and next steps:
- including Equality Act 2010
- reasonable adjustments
Acknowledgements
The national autism team would like to thank all internal and external colleagues who provided feedback and expertise during the writing of this document. In particular, we would like to acknowledge all those who participated in meetings such as the steering group, the oversight group and various task and finish group meetings over the past 2 years.
References
1. Lewis LF. Realizing a diagnosis of autism spectrum disorder as an adult. Int J Ment Health Nurs [Internet]. 2016 Aug 1 [cited 2023 Mar 7];25(4):346–54. Available from: https://doi.org/10.1111/inm.12200
2. Raymond-Barker P, Griffith GM, Hastings RP. Biographical disruption: Experiences of mothers of adults assessed for autism spectrum disorder. J Intellect Dev Disabil [Internet]. 2018 Jan 2 [cited 2023 Mar 7];43(1):83–92. Available from: https://doi.org/10.3109/13668250.2016.1262011
3. Powell T, Acker L. Adults’ experience of an Asperger Syndrome diagnosis: Analysis of its emotional meaning and effect on participants’ lives. Focus Autism Other Dev Disabl [Internet]. 2016 Mar 1 [cited 2023 Mar 7];31(1):72–80. Available from: https://doi.org/10.1177/1088357615588516
4. NHS England. The NHS Long Term Plan [Internet]. Leeds; 2019. Available from: https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/
5. Crane L, Chester JW, Goddard L, Henry LA, Hill E. Experiences of autism diagnosis: A survey of over 1000 parents in the United Kingdom. Autism [Internet]. 2016 Feb 1 [cited 2023 Mar 7];20(2):153–62. Available from: https://doi.org/10.1177/1362361315573636
6. Crane L, Batty R, Adeyinka H, Goddard L, Henry LA, Hill EL. Autism diagnosis in the United Kingdom: Perspectives of autistic adults, parents and professionals. J Autism Dev Disord [Internet]. 2018 Nov 1 [cited 2023 Mar 7];48(11):3761–72. Available from: https://doi.org/10.1007/s10803-018-3639-1
7. Jones L, Goddard L, Hill EL, Henry LA, Crane L. Experiences of receiving a diagnosis of autism spectrum disorder: A survey of adults in the United Kingdom. J Autism Dev Disord [Internet]. 2014 Dec 1 [cited 2023 Mar 7];44(12):3033–44. Available from: https://doi.org/10.1007/s10803-014-2161-3
8. Charlton RA, Crompton CJ, Roestorf A, Torry C. Social prescribing for autistic people: A framework for service provision. AMRC Open Res [Internet]. 2020 Apr 27 [cited 2023 Mar 8];2:19. Available from: https://doi.org/10.12688/amrcopenres.12901.2
9. NICE. Shared decision making [Internet]. 2021 [cited 2023 Mar 8]. Available from: https://www.nice.org.uk/guidance/ng197
10. Lewis LF. “We will never be normal”: The experience of discovering a partner has autism spectrum disorder. J Marital Fam Ther [Internet]. 2017 Oct 1 [cited 2023 Mar 7];43(4):631–43. Available from: https://doi.org/10.1111/jmft.12231
11. Abbott M, Bernard P, Forge J. Communicating a diagnosis of Autism Spectrum Disorder – A qualitative study of parents’ experiences. Clin Child Psychol Psychiatry [Internet]. 2013 Jul [cited 2023 Mar 7];18(3):370–82. Available from: https://doi.org/10.1177/1359104512455813
12. O’Reilly M, Nina Lester J, Muskett T, Karim K. How parents build a case for autism spectrum disorder during initial assessments: ‘We’re fighting a losing battle.’ Discourse Stud [Internet]. 2017 Feb 1 [cited 2023 Mar 7];19(1):69–83. Available from: https://doi.org/10.1177/1461445616683590
13. Potter CA. “I received a leaflet and that is all”: Father experiences of a diagnosis of autism. Br J Learn Disabil [Internet]. 2017 [cited 2023 Mar 3];45(2):95–105. Available from: https://doi.org/10.1111/bld.12179
14. Russell G, Norwich B. Dilemmas, diagnosis and de-stigmatization: Parental perspectives on the diagnosis of autism spectrum disorders. Clin Child Psychol Psychiatry [Internet]. 2012 Apr [cited 2023 Mar 7];17(2):229–45. Available from: https://doi.org/10.1177/1359104510365203
15. Lewis LF. A mixed methods study of barriers to formal diagnosis of Autism Spectrum Disorder in adults. J Autism Dev Disord [Internet]. 2017 Aug 1 [cited 2023 Mar 7];47(8):2410–24. Available from: https://doi.org/10.1007/s10803-017-3168-3
16. Khowaja MK, Hazzard AP, Robins DL, Khowaja M. Sociodemographic barriers to early detection of autism: screening and evaluation using the M-CHAT, M-CHAT-R, and Follow-Up HHS Public Access. J Autism Dev Disord [Internet]. 2015 [cited 2023 Feb 7];45(6):1797–808. Available from: https://doi.org/10.1007%2Fs10803-014-2339-8
17. Burkett K, Morris E, Manning-Courtney P, Anthony J, Shambley-Ebron D. African American families on autism diagnosis and treatment: the influence of culture. J Autism Dev Disord [Internet]. 2015 Oct 22 [cited 2023 Feb 7];45(10):3244–54. Available from: https://doi.org/10.1007/s10803-015-2482-x
18. Bailey B, Arciuli J. Indigenous Australians with autism: A scoping review [Internet]. Vol. 24, Autism. SAGE Publications Ltd; 2020 [cited 2023 Mar 7]. p. 1031–46. Available from: https://doi.org/10.1177/1362361319894829
19. Fox F, Aabe N, Turner K, Redwood S, Rai D. “It was like walking without knowing where I was going”: A qualitative study of autism in a UK Somali migrant community. J Autism Dev Disord [Internet]. 2017 [cited 2023 Feb 7];47:305–15. Available from: https://doi.org/10.1007/s10803-016-2952-9
20. Mandell DS, Ittenbach RF, Levy SE, Pinto-Martin JA. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. J Autism Dev Disord [Internet]. 2007 [cited 2023 Feb 7];37:1795–802. Available from: https://doi.org/10.1007/s10803-006-0314-8
21. Department of Health and Social Care. The national strategy for autistic children, young people and adults: 2021-2026 [Internet]. 2021 [cited 2022 Nov 30]. Available from: https://www.gov.uk/government/publications/national-strategy-for-autistic-children-young-people-and-adults-2021-to-2026/the-national-strategy-for-autistic-children-young-people-and-adults-2021-to-2026
22. Skills for Health, Skills for Care, Opening Minds the NAS. Core capabilities framework for supporting autistic people [Internet]. London; 2019. Available from: https://www.skillsforhealth.org.uk/images/services/cstf/Autism Capabilities Framework Oct 2019.pdf
23. Happé FG, Mansour H, Barrett P, Brown T, Abbott P, Charlton RA. Demographic and cognitive profile of individuals seeking a diagnosis of autism spectrum disorder in adulthood. J Autism Dev Disord [Internet]. 2016 Nov 1 [cited 2023 Mar 7];46(11):3469–80. Available from: https://doi.org/10.1007/s10803-016-2886-2
24. Crane L, Lui LM, Davies J, Pellicano E. Autistic parents’ views and experiences of talking about autism with their autistic children. Autism [Internet]. 2021 May 1 [cited 2023 Mar 7];25(4):1161–7. Available from: https://doi.org/10.1177/1362361320981317
25. Deb S, Retzer A, Roy M, Acharya R, Limbu B, Roy A. The effectiveness of parent training for children with autism spectrum disorder: A systematic review and meta-analyses. BMC Psychiatry [Internet]. 2020 Dec 1 [cited 2023 Mar 7];20(1). Available from: https://doi.org/10.1186/s12888-020-02973-7
26. O’Donovan KL, Armitage S, Featherstone J, McQuillin L, Longley S, Pollard N. Group-based parent training interventions for parents of children with autism spectrum disorders: A literature review [Internet]. Vol. 6, Review Journal of Autism and Developmental Disorders. Springer New York LLC; 2019 [cited 2023 Mar 7]. p. 85–95. Available from: https://doi.org/10.1007/s40489-018-00155-6
27. Fang Z, Lachman JM, Zhang C, Qiao D, Barlow J. A virtuous circle: Stakeholder perspectives of a short-term intensive parent training programme delivered within the context of routine services for autism in China. Autism [Internet]. 2022 Nov 24 [cited 2023 Mar 7];26(8):1973–86. Available from: https://doi.org/10.1177/13623613211070869
28. Oono IP, Honey EJ, Mcconachie H. Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews [Internet]. 2013 Apr 30 [cited 2023 Mar 7];2013(4). Available from: https://doi.org/10.1002/14651858.cd009774.pub2
29. NHS England. Making information and the words we use accessible [Internet]. 2022 [cited 2022 Nov 30]. Available from: https://www.england.nhs.uk/learning-disabilities/about/get-involved/involving-people/making-information-and-the-words-we-use-accessible/#autism
30. World Health Organisation. ICD-11: International classification of diseases [Internet]. 11th edition. 2019 [cited 2022 Nov 21]. Available from: https://icd.who.int/
31. NICE. Autism spectrum disorder in adults: Diagnosis and management (NICE clinical guideline, CG142) [Internet]. 2012 [cited 2023 Mar 7]. Available from: https://www.nice.org.uk/guidance/cg142
32. NICE. Autism spectrum disorder in under 19s: Recognition, referral and diagnosis (NICE Clinical Guideline CG128) [Internet]. 2017. Available from: https://www.nice.org.uk/guidance/cg128
33. NICE. Autism spectrum disorder in under 19s: support and management (NICE Clinical Guideline CG170) [Internet]. 2014 [cited 2023 Mar 7]. Available from: https://www.nice.org.uk/guidance/cg170
34. NICE. Autism: Quality standard [Internet]. 2014. Available from: nice.org.uk/guidance/qs51
35. Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule – 2nd edition (ADOS-2) [Internet]. Los Angeles, CA: Western Psychological Corporation; 2012 [cited 2023 Mar 8]. Available from: https://www.pearsonclinical.co.uk/store/ukassessments/en/Store/Professional-Assessments/Behavior/Autism/Autism-Diagnostic-Observation-Schedule%2C-Second-Edition/p/P100009202.html
36. American Psychiatric Association. Diagnostic and statistical manual of mental disorders [Internet]. 5th ed. Washington: American Psychiatric Association; 2013 [cited 2023 Mar 8]. Available from: https://doi.org/10.1176/appi.books.9780890425787
37. Rutter M, Le Couteur A, Lord C. Autism diagnostic interview-revised. Los Angeles, CA: Western Psychological Services [Internet]. 2003 [cited 2023 Mar 8];29(2003):30. Available from: https://www.pearsonclinical.co.uk/store/ukassessments/en/Store/Professional-Assessments/Behavior/Autism/Autism-Diagnostic-Interview%2C-Revised/p/P100009201.html
38. Rogers CL, Goddard L, Hill EL, Henry LA, Crane L. Experiences of diagnosing autism spectrum disorder: A survey of professionals in the United Kingdom. Autism [Internet]. 2016 Oct [cited 2023 Mar 7];20(7):820–31. Available from: https://doi.org/10.1177/1362361315611109
39. Huang Y, Arnold SRC, Foley KR, Trollor JN. Choose your own adventure: Pathways to adulthood autism diagnosis in Australia. J Autism Dev Disord [Internet]. 2022 Jul 1 [cited 2023 Mar 7];52(7):2984–96. Available from: https://doi.org/10.1007/s10803-021-05169-4
40. Beresford B, Mukherjee S, Mayhew E, Heavey E, Park AL, Stuttard L, et al. Evaluating specialist autism teams’ provision of care and support for autistic adults without learning disabilities: The SHAPE mixed-methods study. Health Services and Delivery Research [Internet]. 2020 [cited 2023 Mar 7];8(48):1–200. Available from: https://doi.org/10.3310/hsdr08480
41. Hossain MM, Khan N, Sultana A, Ma P, Lisako Mckyer E, Ahmed HU, et al. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: An umbrella review of systematic reviews and meta-analyses. Psychiatry Res [Internet]. 2020;112922. Available from: https://doi.org/10.31124/advance.11497014.v1
42. Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. J Autism Dev Disord [Internet]. 2013 Jun [cited 2023 Mar 7];43(6):1314–25. Available from: https://doi.org/10.1007/s10803-012-1679-5
43. Lai MC, Kassee C, Besney R, Bonato S, Hull L, Mandy W, et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry [Internet]. 2019 Oct 1 [cited 2023 Mar 7];6(10):819–29. Available from: https://doi.org/10.1016/s2215-0366(19)30289-5
44. Rydzewska E, Hughes-Mccormack LA, Gillberg C, Henderson A, Macintyre C, Rintoul J, et al. Prevalence of sensory impairments, physical and intellectual disabilities, and mental health in children and young people with self/proxy-reported autism-observational study of a whole country population. Autism [Internet]. 2019 [cited 2023 Mar 2];23(5):1201–9. Available from: https://doi.org/10.1177/1362361318791279
45. Rutherford M, Singh-Roy A, Rush R, McCartney D, O’Hare A, Forsyth K. Parent focused interventions for older children or adults with ASD and parent wellbeing outcomes: A systematic review with meta-analysis [Internet]. Vol. 68, Research in Autism Spectrum Disorders. Elsevier Ltd; 2019 [cited 2023 Mar 7]. Available from: https://doi.org/10.1016/j.rasd.2019.101450
46. NHS England, Local Government Association, ADASS. Building the Right Support: A national plan to develop community services and close inpatient facilities for people with a learning disability and/or autism who display behaviour that challenges, including those with a mental health condition [Internet]. 2015. Available from: https://www.england.nhs.uk/wp-content/uploads/2015/10/ld-nat-imp-plan-oct15.pdf
47. Dahiya A V., McDonnell C, DeLucia E, Scarpa A. A systematic review of remote telehealth assessments for early signs of Autism Spectrum Disorder: Video and mobile applications. Practice Innovations [Internet]. 2020 [cited 2023 Mar 7];5(2):150–64. Available from: https://doi.org/10.1037/pri0000121
48. Ali D, O’Brien S, Hull L, Kenny L, Mandy W. ‘The key to this is not so much the technology. It’s the individual who is using the technology’: Perspectives on telehealth delivery for autistic adults during the COVID-19 pandemic. Autism [Internet]. 2022 [cited 2023 Mar 7]; Available from: https://doi.org/10.1177/13623613221108010
49. Alfuraydan M, Croxall J, Hurt L, Kerr M, Brophy S. Use of telehealth for facilitating the diagnostic assessment of Autism Spectrum Disorder (ASD): A scoping review. PLoS One [Internet]. 2020 Jul 1 [cited 2023 Mar 7];15(7 July). Available from: https://doi.org/10.1371%2Fjournal.pone.0236415
50. Spain D, Stewart GR, Mason D, Milner V, Fairhurst B, Robinson J, et al. Telehealth autism diagnostic assessments with children, young people, and adults: Qualitative interview study with England-wide multidisciplinary health professionals. JMIR Ment Health [Internet]. 2022 Jul 20 [cited 2023 Mar 7];9(7):e37901. Available from: https://doi.org/10.2196/37901
51. NHS England. Meeting the healthcare needs of adults with a learning disability and autistic adults in prison [Internet]. 2021 [cited 2023 Mar 8]. Available from: https://www.england.nhs.uk/publication/meeting-the-healthcare-needs-of-adults-with-a-learning-disability-and-autistic-adults-in-prison/
52. NHS England. Provision or people with a known or suspected learning disability, autism or both [Internet]. 2020 [cited 2023 Mar 8]. Available from: https://www.england.nhs.uk/publication/provision-for-people-with-a-known-or-suspected-learning-disability-autism-or-both/
53. HMICFRS. Neurodiversity in the criminal justice system: A review of evidence [Internet]. 2021 [cited 2023 Mar 8]. Available from: https://www.justiceinspectorates.gov.uk/hmicfrs/publications/neurodiversity-in-the-criminal-justice-system/
54. Matthews NL, Skepnek E, Mammen MA, James JS, Malligo A, Lyon A, et al. Feasibility and acceptability of a telehealth model for autism diagnostic evaluations in children, adolescents, and adults. Autism Research [Internet]. 2021 Dec 1 [cited 2023 Mar 7];14(12):2564–79. Available from: https://doi.org/10.1002/aur.2591
55. Wigham S, Ingham B, Le Couteur A, Wilson C, Ensum I, Parr JR. Consensus statements on optimal adult post-autism diagnosis support and services: Delphi process following a UK survey of autistic adults, relatives and clinicians. Autism [Internet]. 2022 [cited 2023 Mar 7]; Available from: https://doi.org/10.1177/13623613221097502
56. Health and Care Professions Council. Key characteristics of effective supervision [Internet]. 2021 [cited 2023 Feb 9]. Available from: https://www.hcpc-uk.org/standards/meeting-our-standards/supervision-leadership-and-culture/supervision/approaching-supervision/key-characteristics-of-effective-supervision/
Publication reference: PAR1806
Version: 1.0

