Version 2, 16 May 2023
Introduction
This document details the clinical standards for paediatric dental treatment in primary, community and specialist care settings. However, it is important to remember that some patients require treatment in a shared care approach, across more than one setting.
The majority of children access care and treatment from general dental practitioners (GDPs), but those with severe disease and or complicating health or social factors may need dentists with specialist skills and/or specialist facilities. This clinical standard explains what specialist paediatric care is, when it is needed, how it can be accessed and how it should be delivered to ensure a consistent quality and outcomes. It complements the commissioning of programmes at a population or community level to monitor and improve the oral health of children.
This document defines the NHS England minimum clinical standards and dental care pathway for children and young people (CYP) that all providers of paediatric dental services must adhere to. Careful individual patient assessment for each treatment episode is crucial.
- Chapter 2 of the document focuses on what paediatric dentistry is, and the current provision.
- Chapter 3 considers the future commissioning of paediatric dentistry
- Chapter 4 outlines referral for treatment
- Chapter 5 reviews quality and outcome measures
1 What is paediatric dentistry?
1.1 Description and scope of the specialty
Paediatric dentistry is the provision of oral healthcare to CYP from birth until their 16th birthday. Care may be provided across primary, secondary and tertiary care settings.
Specialists in paediatric dentistry provide oral healthcare for CYP:
- with extensive oral disease,
- whose oral health care is complicated by intellectual, medical, physical, social, psychological and/or emotional factors/disability,
- with developmental disorders of the teeth and mouth,
- who are either too anxious or too young to accept routine dental treatment,
with diagnosed special educational needs,
- who have sustained complex traumatic dental injuries.
The age range covered by the specialty is normally regarded as 0-16 years; however, young people should start the transition process to adult oral health services some time before their 16th year. For patients whose care may require specialist support from 16 years of age the specialist in paediatric dentistry will liaise with local specialists such as special care dentists, maxillofacial surgeons, orthodontists and restorative dentists to facilitate a smooth and appropriate transition. This may involve a period of joint care.
1.2 Provision of care
1.3 Description of the national picture
The most common non communicable disease affecting children in England is dental decay which is largely preventable. Poor oral health has a significant impact on the quality of life, causing pain and embarrassment and limitation of function. Children’s pain and sleep disturbance also affects parents and carers, often disturbing home, educational and work routines. The social consequences of poor oral health have a significant effect on the child and their families.
Most dentistry delivered to children is provided in primary care by dentists, therapists, hygienists, and dental nurses as part of general dental service arrangements (GDS). To support general dental services, NHS England issued an avoidance of doubt notification (1) to provide clarity for dentists about examining and treating very young children.
1.4 Specialist care
Some children may also need access to specialist facilities as well as seek care from professionals with additional competencies. Specialists in paediatric dentistry should work in multidisciplinary teams (MDTs) with other appropriate dental specialties, including orthodontics, restorative dentistry, maxillofacial and oral surgery and oral medicine. Specific multidisciplinary clinics need to be established to ensure holistic provision.
1.5 Anxiety management
Anxiety management techniques can allow comprehensive care to be provided for children who suffer anxiety or need potentially distressing dental procedures such as minor oral surgery. Availability of dental treatment under sedation (especially inhalation sedation with nitrous oxide and oxygen) is an essential component of paediatric clinical care pathways. Commissioners and providers are directed to view the ‘Clinical guide for dental anxiety management’ (2) alongside this guide when considering anxiety management provision in all settings.
All patients should be managed with the simplest and safest anxiety management technique which is considered likely to be successful.
For some anxious / phobic patients, including ‘pre-co-operative’ children, dental treatment may not be possible using behavioural and / or conscious sedation techniques alone. General anaesthesia may be indicated if dental treatment is required, because of anxiety and / or the complexity of the dental procedure.
Referrals for paediatric patients for dental treatment using sedation or general anaesthesia must indicate that the reason for referral and the referral process has been explained to the patient or their carers. There are a large number of tools available for the measurement of anxiety in children e.g., the Dental Fear Survey (DFS), CEDAM, the Venham Picture Test (VPT), Modified Child Dental Scale (MCDAS) and its faces version (MCDASf). Reliability and validity estimates for the most widely used are good, however, many questionnaires have a limited focus on the aspects of anxiety they assess (3, 4). Equally none can discount the influence of parental / carer impact, especially in the younger age groups who may/ will rely on parents/carers to complete the assessment form. The measurement/description of anxiety will need discussion at the Managed Clinical Network (MCN) so that all local referrals use a regionally agreed and shared approach.
Careful consideration of all less restrictive anxiety management techniques, including behavioural therapies and inhalation sedation must be undertaken before referring a patient for specialist led sedation (in secondary or tertiary settings) or general anaesthesia.
[1] Porritt J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children’s dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol 2013; 41; 130–142
[2] Porritt J, Morgan A, Rodd H, Gilchrist F, Baker S, Newton T, Marshman Z. A Short Form of the Children’s Experiences of Dental Anxiety Measure (CEDAM): Validation and Evaluation of the CEDAM-8. Dent J (Basel) 2021 Jun; 9(6):71
1.5.1 Dental care under general anaesthesia
Dental treatment under general anaesthesia (GA) is an essential adjunct to providing care where the surgical intervention is complex or to those children who are cognitively immature, highly anxious or who have a medical condition where GA is the most appropriate or only way to deliver dental treatment.
Children undergoing GA should receive the same standard of assessment and preparation as children admitted for any other procedure under GA, as set out in the Guidelines for the Provision of Paediatric Anaesthesia Services 2020 (5). Comprehensive dental care, such as cases where restorative care is being provided, should be led by specialists and/or consultants.
1.6 Safeguarding
All healthcare professionals contribute towards safeguarding children by working with social care and other agencies as set out in the overarching guide Working Together to Safeguard Children (6).
Clinical input to safeguarding children by dental teams falls into three domains:
- Making child protection referrals to children’s social care where a child is thought to be experiencing or at risk of significant harm because of maltreatment
- Communication with other professionals (including writing reports) regarding children already identified as at risk or maltreated (identifying persistent failure to bring children for dental care should be considered a safeguarding issue)
- Communication with other professionals (including writing reports) regarding children already identified as at risk or maltreated:
(a) Children who are undergoing medical examination for suspected neglect.
(b) Children subject to a child protection plan.
(c) Some looked after children (annual dental visits for looked after children are a requirement and are already subject to monitoring).
1.7 Looked After Children
The provision of oral healthcare to children in care is described in the statutory guidance document, Promoting the health and well- being of looked- after children (7). Specifically, looked after children must ensure the following occurs:
The Initial Health Assessment (IHA) should identify the existing arrangements for the child’s dental care appropriate to their needs, which must include information regarding:
- Routine checks… including dental health treatment and monitoring for identified health…or dental care needs;
- Relevant information drawn together beforehand and fast-tracked by all involved to the health professional undertaking the assessment…
- The child’s personal and family history if known (8)
The guidance also states that NHS England should ensure looked-after children always have access to dentists near to where they are living. This is a shared responsibility with the local authority for the children it looks after. All decisions must be shared to ensure there is clarity for carers, dentists and the child, about what care decisions have been delegated to carers; shared through a delegated authority document. Where children are Fraser / Gillick competent they should lead the decision-making process.
Dental recalls for all children, including those in care, are guided by the NICE guideline (9) for dental recalls; appropriate to their needs (NICE October 2004 Dental checks: intervals between oral health reviews – cg 19).
The IHA should identify any dental concerns, outline any modifying factors that may affect delivery and, where possible, provide any past history including active referrals e.g., medical comorbidity, behavioural conditions and their management. This will inform the dental assessment and subsequent management. A typical pathway for a child in care is shown in Appendix 1.
1.8 Transition to adult services
Where children are likely to require on-going specialist oral and dental care through adolescence and into adulthood (usually beyond their 16th birthday) it is important to plan appropriate transition to relevant adult oral health care services.
2 Considerations for paediatric dentistry
2.1 Establishing a paediatric Managed Clinical Network (MCN)
Commissioners should familiarise themselves with the National NHS England requirements for Local Dental Networks (10) and speciality Managed Clinical Networks. There are examples of MCN terms of reference to be found on the NHS England website.
The British Society for Paediatric Dentistry can help to locate local specialists or consultants. They can be contacted by emailing administrator@bspd.co.uk
2.2 Needs assessent
The provision of any services should be supported by an oral health needs assessment described in Appendix 2.
2.3 Provision of care and treatment complexity
Primary care teams are expected to provide comprehensive dental care for children where delivery is not complicated by significant modifying factors. These may include:
- severity of disease
- difficulty in a child being able to co-operate either due to age or severe anxiety
- medical comorbidity
- disability that affects access to or use of GDS that cannot reasonably be adjusted in accordance with the requirements of the Equality Act 2010.
The Department of Health and Social Care has previously defined procedures and modifying patient factors that describe the complexity of a child’s dental care and are detailed at Appendix 3. The descriptors relate to the General Dental Council (GDC) expectations of core and specialist skills.
2.4 Transforming services
Clinicians are expected to work with key partners including local authorities to ensure that their responsibilities are fulfilled. NHS England encourages clinicians and commissioners to work with their local authorities to ensure the development and delivery of services to improve the oral health of children observing the guidance shared by the Office for Health Improvement and Disparities (OHID) and the recommendations of the GIRFT national report for Hospital Dentistry (GIRFT 2021. Hospital Dentistry. GIRFT Programme National Speciality Report).
3 Referral management
All providers must only accept referrals which comply with referral management systems in place, preferably an e-Referral system (12). The referral minimum data sets should include all of the following items:
- A fully recorded medical history (including prescribed and non- prescribed drugs and any known allergies).
- A dental history, including any outstanding acute issues.
- A social history
- The dental treatment plan proposed
- Provision of any dental treatment already provided including radiographs (digital images should be attached to the referral)
- Assessment of anxiety and any tools used
- Any individual patient requirements (e.g. looked after children, safeguarding concerns/issues, need for an interpreter)
- An explanation of the attempts made to manage dental care in a primary care setting.
Referral for the management of anxiety and/or lack of ability to co-operate is comprehensively covered within the Clinical Guide for Dental Anxiety Management (13). Where specialist services such as GA and sedation are needed to deliver dental care additional patient information will be required.
Where patients are referred for treatment under general anaesthesia, robust, holistic, shared patient treatment plans (14) and follow up responsibility between the patient’s general dental practitioner and Paediatric MCNs need to be in place (15).
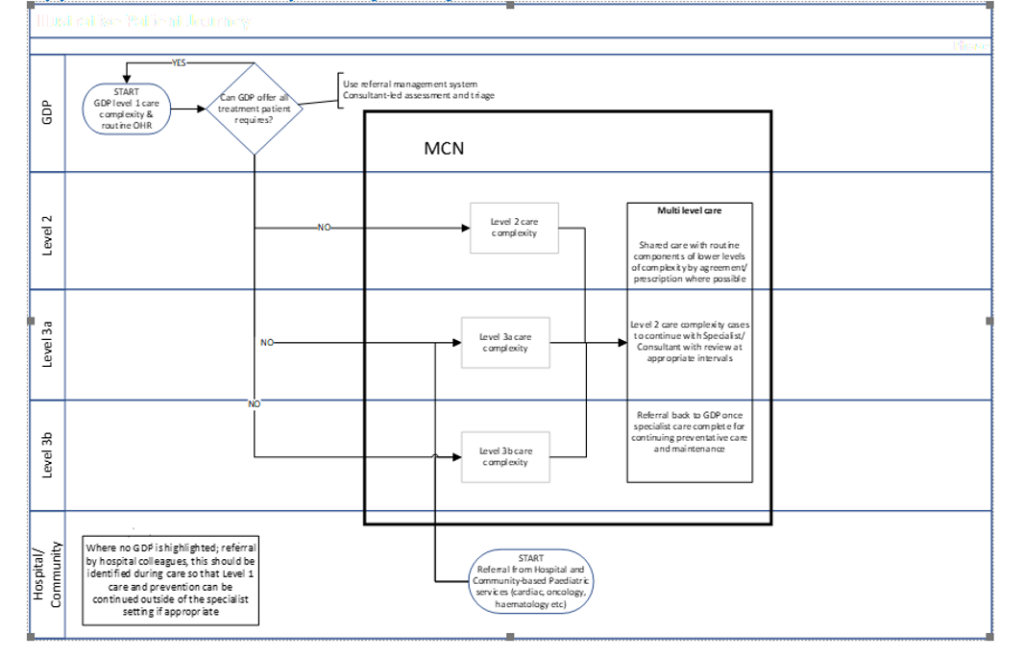
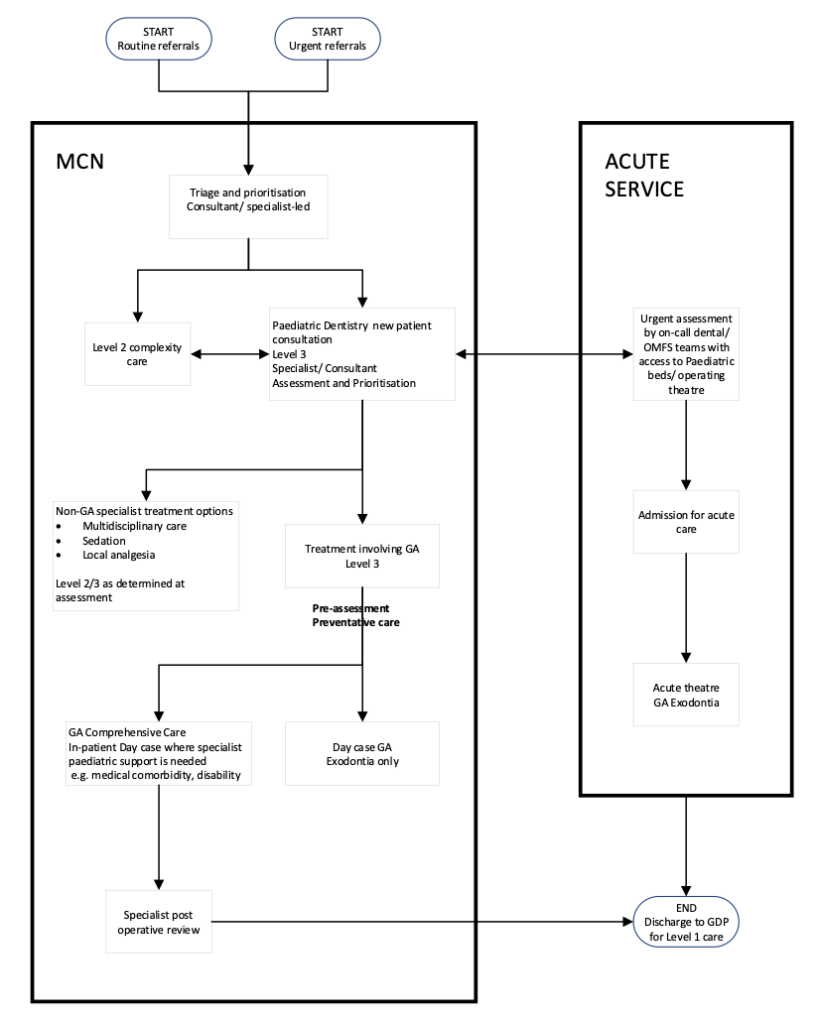
Appendices 5 and 6 indicate possible pathways of care across primary, secondary and tertiary care, including the management of patients under GA.
4 Quality and outcome measures
4.1 Service metrics/data
Key performance indicators for service delivery need to be agreed for each setting. The indicators need to align with the themes of the NHS Long Term Plan (16) and the annual operating plan/framework.
All services providing level 2 and 3 care must be able to demonstrate enhanced skills and facilities. Appendix 7 provides a comprehensive list of expected staff and environmental standards.
Examples of performance indicators are shown in appendix 7.
All performers of care of level 2 and 3 complexity must be members of the associated paediatric MCN and must demonstrate attendance at meetings and participation in audits, peer review and other quality assurance as agreed by the MCN.
4.2 PROMs and PREMs
In addition, each provider will be expected to collect patient related outcome measures (PROMs) and patient related experience measures (PREMs) and report these to commissioners for the purpose of benchmarking.
4.2.1 Patient reported outcomes (PROMs)
These should be able to measure any difference in a patient’s oral health after specialist treatment, irrespective of the presenting condition or treatment. The use of PROMs in children is still the subject of debate and ongoing development. The language and presentation of response does require a full understanding of childhood development (17).
An example of the type of questions possible are shown in appendix 5 (18). Child friendly responses should be considered including pictures and/or computer aided.
4.2.2 Parent/carer reported outcome measures
These are perceptions of parents/carers regarding the oral health quality of life of their children (19). They should complement those being used by children. Examples of questions that may be used are shown in Appendix 8.
4.2.3 Patient Reported Experience Measure (PREMs)
The MCN should review and decide the questions they feel are most appropriate. Examples include:
- How was your experience of our service?
- Were the people looking after you kind?
- Did people help you to understand what was happening?
- Did people listen to you?
- Did you feel safe?
Appendix 1
Looked after child pathway
- Child placed in care
- Foster carer to present delegated authority and arrange for notes to be available if possible
- Initial oral health risk assessment
- LOW: appointment when next available
MEDIUM: advise of issues noted at IHA
HIGH: request urgent appointment
Appendix 2
An oral health needs assessment should explore paediatric provision, and oral health of the child population.
Health needs assessment is a systematic method for reviewing the health issues facing a population, leading to agreed priorities and resource allocation that will improve health and reduce inequalities. Table 2 provides examples of service level provision and indicators that can be used to understand the local level of provision required.
Further details may be obtained from the Office for Health Improvement and Disparities.
Table 2. Example of a systematic approach to assessing need for paediatric dental care
|
|
Level of service complexity to be completed locally |
Indicators used to estimate service provision |
|
Specialist led network to link all levels | Level 1 – Primary Care No additional complexity or setting requirements. | Children who can manage well in mainstream primary care for routine care and most other procedures. Looked after children’s initial oral health assessment where no enhanced needs (social, behavioural, medical) are identified through the medical initial health assessment (IHA).
|
| Level 2 – Primary or secondary care Additional provision includes:· Clinician with additional knowledge and skill. · Extended appointment times are accommodated. · Flexibility with appointments possible. · Inhalation sedation facilities. | Cleft lip and palate. Children with extensive dental disease. Moderate Learning Disability (LD) that affects delivery of oral healthcare.Medical conditions that affect the delivery of oral health care e.g. unstable asthma, cardiac disease requiring antibiotic cover Physical disability affecting access to or use of facilities in GDS.Moderately controlled behavioural conditions e.g., ADHD managed with medication and/or psychological support Looked after children with enhanced needs (social, behavioural, medical) as identified through IHA.
| |
| Level 3 – Primary care setting. Additional provision includes: · Specialist in Paediatric Dentistry leads the provision of care within a team. Additional administrative time to link with partner professionals. · Extended appointment times are accommodated.· Flexibility with appointments possible. · Children who require assessment for general anaesthesia for routine or occasional treatment.· Children under 12 years who may require sedation other than inhalation sedation (assessment only) Level 3 – Secondary or tertiary care setting · Children who require provision of general anaesthesia for routine or occasional treatment. · Children under 12 years who require provision of sedation, other than inhalation sedation, for routine or occasional treatment.
| Severe LD. Profound and multiple LD. Severely medically compromised. Severe behavioural conditions that are poorly controlled Severe dental anxiety. |
Appendix 3
Level 2 services should provide:
- Management of dento-alveolar trauma of increased complexity including:
- complicated crown fracture of permanent teeth.
- injuries to primary teeth not manageable by restoration or extraction.
- root and crown-root fractures of permanent teeth without complicating factors.
- post-emergency follow-up of multi-tooth injuries in the permanent dentition.
- post emergency follow-up of permanent tooth avulsion and significant luxation injuries.
- Management of complex problems affecting the developing dentition or dental hard tissues under the direction of a specialist or consultant in Paediatric Dentistry.
- Extraction of teeth under general anaesthesia.
- Inhalation sedation where appropriate for all ages of children and IV sedation for children of 12 years of age and above.
- Management of children with extensive caries or early childhood caries in pre-cooperative children amenable to care under local analgesia with/without sedation as an adjunct.
- Moderate tooth surface loss in the permanent dentition, with support from a specialist.
- Mild to moderate hypodontia with support from a specialist
- Supernumerary teeth and/or delayed eruption of permanent teeth not requiring complex surgical or multidisciplinary management with support from a specialist
- Treatment planning, support and follow up for children requiring extractions under general anaesthesia with support from a specialist
- Uncomplicated dento-alveolar surgical interventions.
- Assessment and management (or referral to a higher level as appropriate) of children subject to a child protection plan.
Following the item or course of treatment, the child will be discharged to their referring dentist. If referral has come from a community dentist, consultant or specialist, the child will be discharged to their general dental practitioner.
Level 3a services should provide:
Care and procedures that may require the knowledge and skills of a dentist recognised as a specialist in Paediatric Dentistry including:
- Severe early childhood caries or unstable/extensive caries (especially where treatment under general anaesthesia may be necessary).
- Severe tooth surface loss in the permanent dentition.
- Abnormalities of dental development not amenable to simple preventive or restorative management
- Moderate/severe molar incisor hypomineralisation (MIH).
- Amelogenesis imperfecta.
- Dentinogenesis imperfecta.
- Restorative and exodontia treatments for children being managed under the direction of a regional multi-disciplinary team with cleft lip and/or palate.
- Dento-alveolar trauma requiring more specialised management including:
- Avulsion injuries and post-avulsion management, especially where complications have developed.
- Management of injuries to immature permanent incisors where endodontic treatment is required.
- Moderate to severe luxation injuries, especially where injuries involving significant damage to multiple teeth.
- Aggressive periodontitis or other less common periodontal/gingival conditions.
- Uncomplicated dento-alveolar surgical interventions.
- Treatment planning and delivery of comprehensive dental care under general anaesthesia.
- Dental care of children with significant anxiety and/or behavioural conditions.
- Oral health surveillance and or treatment needs where significant medical comorbidity or disability increase the complexity and risks of delivery of care. Such care may be shared with a consultant and many such children will be under the on-going care of a paediatrician. For example:
- significant cardiovascular disease.
- significant abnormalities of haemostasis.
- children undergoing treatment for haematological or organ malignancies.
- children with significant disability or learning difficulties.
- children with significant behavioural problems or communication disorders.
- A clear pathway for acceptance and management of dental emergencies requiring specialist level care. This will include more complex dento-alveolar traumatic injuries and acute dental infection in children with significant disability or co-morbidity.
Level 3b service should provide:
Care delivered by a dentist recognised as consultant in Paediatric Dentistry including:
- Assessment and management of complex dental or cranio-facial conditions which require a multi-disciplinary team input to treatment planning and care or where management of a disturbance in dental development is complicated by features requiring input/active treatment from other dental specialties. Examples include:
- Severe hypodontia, and significant dental hard-tissue developmental defects, especially during transition into orthodontic and definitive adult restorative management and treatment.
- Traumatic dento-alveolar injuries where significant complications have arisen, especially where multidisciplinary planning and care is required.
- Premolar transplantation.
- Patients requiring obturators or other more advanced intermediate restorative management.
- Patients with complex presentations of tooth morphology (macrodontia, double teeth, dens-in-dente, talon teeth).
- Assessment and facilitating management of oral pathology or oral medical conditions in children.
- Assessment, surveillance and treatment of children with significant co-morbidity being managed by other paediatric specialities (for example oncology, cardiology, haematology, hepatology, nephrology, endocrinology. This may include providing urgent dental treatment prior to open heart surgery, organ transplant or prior to commencing chemotherapy, for example.
- Assessment and management of children with a significant disability, co-morbidity, significant behavioural conditions (e.g. children with severe autism) or severe anxiety who require hospital based and/or multidisciplinary work-up and support prior to and/or as an adjunct to delivery of dental treatment.
- Treatment planning and comprehensive care under general anaesthetic, involving more difficult surgical or restorative procedures, or where the child is undergoing joint procedures with another surgical specialty.
- Acute dental emergencies, especially complex dentoalveolar trauma and acute treatment for children with significant disability and/or significant co-morbidity.
The service will provide on-going care for children as follows:
- Management of children with routine oral health surveillance or treatment needs but where behavioural/psychological development or significant anxiety increases the complexity of delivery of care such as those requiring sedation.
- Management of children with routine oral health surveillance or treatment needs but where medical comorbidity or disability increases the complexity of delivery of care.
Appendix 4
|
Descriptor |
Standard |
Additional comments |
|
Location level 2 & 3 |
Provided at a location or locations to minimise travel times for children, parents and carers. |
MCN should advise on appropriate travel time for the locality |
|
Level 2 facilities | · Where manual transfer, hoisting or lifting of patients into the dental chair is not appropriate, equipment should be available to safely recline wheelchair patients in order to carry out dental treatment. · A variety of communication aids should be available, and staff trained to use them · Equipment to support the delivery of conscious sedation to the contemporaneous standard. · Access to intra-oral and panoramic radiography equipment. · Appropriate equipment to perform any Level 2 complexity treatment · Paediatric Resuscitation equipment. · Orthodontic equipment to support treatment of trauma. |
Providers should ensure that they are able to provide in multiple locations to ensure appropriate travel times for service users. |
|
Level 2 staff | · CPD relevant to Paediatric Dentistry · Adherence with the current national guidelines on sedation.· Working knowledge of Mental Capacity Act including consent issues in children.· Ability to undertake treatment under GA.· Safe use of specialised equipment, for example hoists and use of positioning aids.· Range of behavioural management skills and techniques.· Non-verbal communication methods.· Skills in examining the mouth in children with limited ability to cooperate.· Clinical holding skills. · Paediatric Immediate Life Support. |
Staff includes the wider team, utilising a wide skill mix |
|
Level 3a | Include all those noted for level 2 plus: · Access to appropriate dental laboratory to support advanced restorative treatment · Arrangements for transport of patients requiring more than one handler should be available (for example two-man ambulances). · Facilities for the safe treatment of bariatric patients should be available. Access to cone beam tomography facilities. |
|
|
Level 3b | To include Level 2 & 3a facilities plus: · Access to a multi-disciplinary team for any complex care. · Access to facilities for providing treatment under general anaesthesia for children where GA is part of the specification. |
|
Appendix 5
Illustrative patient journey
Appendix 6
Example of specialist paediatric dental care under general anaesthesia
Appendix 7
|
Data item |
Frequency |
|
Waiting times for assessment (weeks). |
Monthly. |
|
Waiting times for treatment (weeks). |
Monthly. |
|
Number waiting for assessment. |
Monthly. |
|
Number waiting for treatment. |
Monthly. |
|
Length of time of longest wait (weeks). |
Monthly. |
|
Number seen for assessment. |
Monthly. |
|
Number seen for treatment. |
Monthly. |
|
New to follow up ratio by performer. |
Monthly. |
|
Number assessed and discharged. |
Monthly. |
|
Number assessed and accepted for L3 care. |
Monthly. |
|
Number discharged complete. |
Monthly. |
|
Number on review. |
Monthly. |
|
DNA/WNB rate (%). |
Monthly. |
|
Cancel by provider rate (%). |
Monthly. |
|
Cancel by patient rate (%). |
Monthly. |
|
PROMs, PREMs. |
Quarterly. |
Appendix 8
CARIES-QC PROMs items (20) as a measure of PROMs
|
How much do your teeth hurt you |
|
Do your teeth make it hard to eat some foods |
|
Do you have to eat on one side of your mouth because of your teeth |
|
Do you get food stuck in your teeth |
|
How much do you get kept awake by your teeth |
|
How much do you get kept awake by your teeth |
|
How much do your teeth hurt when you brush them |
|
Do you have to eat more carefully because of your teeth |
|
Do you have to eat more slowly because of your teeth |
|
Do you feel cross because of your teeth |
|
How much have you cried because of your teeth |
|
Do your teeth make it hard to do your schoolwork |
|
Global question: How much of a problem are your teeth for you |
Parental perceptions reported as outcome measures (21)
|
Global question about impact of oral health on quality of life overall rating | ||||||
|
How much is your child’s overall well-being affected by the condition of his/her teeth, lips, jaws and mouth? |
Very much. |
A lot. |
Some. |
Very little. |
Not at all. | |
|
Global treatment-related change | ||||||
|
Since the treatment of your child’s teeth, has your child’s overall quality of life been: |
Much improved? |
A little improved? |
The same? |
A little worse? |
Much worse? | |
References
1, NHS England. Gateway Reference 07250. 25 September 2017. Avoidance of Doubt: Dental visits for children under the age of 3 years.
2. NHS England. Publication reference PR1483. December 2022 Clinical Guide for Dental Anxiety Management
3. Porritt J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children’s dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol 2013; 41; 130–142
4. Porritt J, Morgan A, Rodd H, Gilchrist F, Baker S, Newton T, Marshman Z. A Short Form of the Children’s Experiences of Dental Anxiety Measure (CEDAM): Validation and Evaluation of the CEDAM-8. Dent J (Basel) 2021 Jun; 9(6):71
5. Royal College of Anaesthetists. 2020. Guidelines for the Provision of Paediatric Anaesthesia Services
6. HM Government 2018 DFE-00195-2018 Working Together to Safeguard Children. A guide to inter-agency working to safeguard and promote the welfare of children.
7. Department of Health & Social Care. August 2022. Promoting the health and well- being of looked- after children. Statutory guidance for local authorities, clinical commissioning groups and NHS England
8. Ibid
9. NICE October 2004 Dental checks: intervals between oral health reviews (cg 19)
10. NHS England What is a local dental network. Available January 2023
11 GIRFT 2021. Hospital Dentistry. GIRFT Programme National Speciality Report
12. ibid
13 NHS England. December 2022. Clinical Guide for Dental Anxiety Management
14 Ibid [footnote 10]
15 NHS England (2018). Commissioning Standard for Dental Specialties – Paediatric Dentistry.
16 NHS England. January 2019. The NHS Long Term Plan
17 Graham A, Knapp R, Rodd H, Marshman Z, Zaitoun H, Gilchchrist F. The Utility and Feasibility of Routine Use of a Patient-Reported Outcome Measure in Paediatric Dentistry. Oral 2021, 1(4), 290-299
18 ibid
19 Jokovic A, Locker D, Stephens M, Kenny D, Tompson B. 2003 Measuring Parental Perceptions of Child Oral Health-Related Quality of Life. Journal of Public Health Dentistry 63, 67-72.
20. Ibid [ref 17]
21. Ibid [ref 19]

