Foreword
The professional nurse advocate (PNA) training programme launched in March 2021, towards the end of the third wave of COVID-19 and the start of a critical point of recovery: for patients, for services and for our workforce.
This programme is the first of its kind for nursing, not just in England but across the world. It is the first clinical model of restorative supervision for nurses in England that equips PNA-trained staff to listen and understand the challenges fellow colleagues and teams are facing, and to provide and deliver quality improvement initiatives in response.
We have seen, through the existing version of this programme for maternity colleagues, that the training and use of the A-EQUIP model has a positive impact on staff wellbeing and retention, supports professional resilience and improves patient outcomes.
It has been incredible to see the response from our nursing workforce to this programme, with thousands already enrolled, in training or qualified as PNAs to support colleagues across a number of specialties, including mental health, community, learning disabilities, safeguarding and international recruitment. I am pleased to see so many of our colleagues taking up this opportunity for further professional development.
I want to offer my thanks to all nurses in England for their continued hard work, and to those who have taken the opportunity to participate in the programme, support their colleagues and make improvements.
I’d also like to thank our national taskforce who have worked to develop and test the employer led A-EQUIP model, the pilot sites that are testing and measuring the impact of the PNA programme, and the higher education institutions that deliver the training.
Ruth May, Chief Nursing Officer for England
Summary
Professional nursing leadership and clinical supervision are essential in enabling nurses to continuously improve the care they provide to patients and their families, as well as to protect their own and their colleagues’ health and wellbeing.
This document describes the A-EQUIP (Advocating and Educating for QUality ImProvement) model of professional nursing leadership and clinical supervision and provides guidance on the implementation of the professional nurse advocate (PNA) role, including key actions for each relevant group. It is of particular relevance to all nurses, student nurses, providers of nursing services and patients. From 1 April 2022, providers of nursing services will support the implementation of the A-EQUIP model and the PNA role.
The A-EQUIP model works for nurses in four ways:
- advocating for the patient, the nurse and healthcare staff
- providing clinical supervision using a restorative approach
- enabling nurses to undertake personal action for quality improvement
- promoting the education and development of nurses.
It supports a continuous improvement process that aims to build on the personal and professional clinical leadership of nurses, enhance the quality of care for patients, and support preparedness for appraisal and professional revalidation. The restorative function has been shown to have a positive impact on the physical and emotional wellbeing of staff as it reduces burnout, stress and absences, and improves job satisfaction and patient experience.
Nursing providers need to prepare for implementation of the PNA role and support the rollout of restorative clinical supervision.
Introduction
This document describes the A-EQUIP (Advocating and Educating for QUality ImProvement) model of professional nursing leadership and clinical supervision, and provides guidance on the implementation of the professional nurse advocate (PNA) role. It is of particular relevance to:
- all nurses and student nurses
- providers of nursing services.
Restorative clinical supervision (RCS) addresses the emotional needs of staff. It provides ‘thinking space’, which, as highlighted in this guidance, reduces stress and burnout and in turn improves staff retention.
The A-EQUIP model has been adapted for the nursing profession to improve and develop nursing professional clinical leadership and advocacy, following the successful implementation of the professional midwifery advocate (PMA) programme in maternity services.
The PNA training programme provides nurses with the skills, competencies and confidence to lead programmes of improvement, fostering a culture of learning and development within their clinical settings, and to deliver RCS to their colleagues.
The A-EQUIP model and PNA role can be applied in different ways and can benefit both clinical and non-clinical nurses within all healthcare settings and across all fields of nursing practice. This is illustrated in various case studies.
This document is organised into three chapters:
Chapter 1 describes the A-EQUIP model and its benefits to nurses, patients and providers of nursing services.
Chapter 2 describes the PNA role.
Chapter 3 gives specific guidance and key actions for:
- PNAs
- providers of nursing services
- higher education institutions (HEIs)/PNA training providers
- regional PNA advisors.
1. A-EQUIP – a new model of nursing supervision
1.1 Developing A-EQUIP
The A-EQUIP model stems from the three functions of clinical supervision in Brigid Proctor’s 1987 clinical supervision model that is commonly used in health services (Ross, 2019):
- normative – managerial aspects concerning practice, learning and core mandatory training
- formative – educational aspects: developing knowledge and skills in professional development and self-reflection
- restorative – supportive aspects, including personal development, improving stress management and mitigating burnout.
Bowles and Young (1999) stated “nurses greatly benefit from clinical supervision from each of the[se] three functions” and that the model provides a framework for using clinical supervision “to change and critically examine nursing practice” (Bowles et al, 1999).
NHS England added a fourth function: personal action and quality improvement (NHS England, 2017). Subsequent to this addition, a new taskforce was convened in England with sponsorship from the Chief Nursing Officer for England to further develop the A-EQUIP model for use in professional nursing leadership and clinical supervision, and for use by PNAs.
The A-EQUIP model is flexible and can be implemented according to organisational requirements to support collaboration between nurses and healthcare colleagues when delivering RCS sessions.
Principles of the model
The taskforce agreed that the model should:
- strategically respond to national initiatives such as the supporting mental health and wellbeing aspect of the NHS People Plan 2020/21 and the NHS Long Term Plan, with a focus on the clinical leadership response to COVID-19 and continuing professional development of the nursing workforce
- be integrated into local governance arrangements
- be consistent – programme standards should be developed nationally, supported regionally and delivered locally through education and training.
1.2 How A-EQUIP and the PNA role support nurses, healthcare staff and patients
The A-EQUIP model benefits nurses, healthcare staff and patients in the following ways:
- advocating for the patient, the nurse and healthcare staff
- providing clinical supervision using a restorative approach
- enabling nurses to undertake personal action for quality improvement
- promoting the education and development of nurses.
PNAs and the use of the A-EQUIP model will help nurses and healthcare staff recognise that the views of patients are integral not only to their personal care but also in shaping service delivery (Degboye et al, 2023).
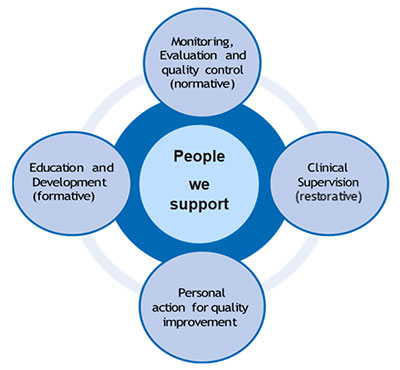
1.3 The four functions of A-EQUIP
The model supports nurses and their supervisors to reflect on the four functions (Figure 1).
- Monitoring evaluation and quality control (normative)
- Clinical supervision (restorative)
- Personal action for quality improvement
- Education and development (formative)
Clinical supervision (restorative)
This function focuses on addressing the emotional needs of the workforce and supporting the development of professional clinical leadership. RCS “involves the development of open discussion space and supporting the professional to undertake reflective conversations and open feedback” (Pettit et al, 2015).
The restorative approach “promotes reflection of personal emotions and practice, has a positive impact on emotional wellbeing, provides a strategy to mitigate workplace stress, enhances retention and assists with the management of personal and professional demands” (Royal College of Nursing, 2021). In particular, the findings from the Restorative Supervision Programme review support the recommendation that RCS improves the mental health and wellbeing of staff: it reduced burnout by 43% (from 42.81 to 24.71) and stress by 62% (from 43.35 to 16.86) from regional baselines.
Box 1: Benefits of the RCS function
For the individual:
- ·feel supported
- experience less stress, burnout and sickness absence
- develop personally and professionally
- be less inclined to leave the profession
- confidence increased
- feel less isolated
- develop clinical competence and knowledge.
For the organisation:
- have a means of developing nursing practice to improve quality of patient care
- improved communication between professional groups, particularly where clinical supervision groups are multi-professional
- dissemination of good practice, shared learning
- reduced turnover of staff/sickness absence
- have a tool for maintaining, monitoring and developing good practice
- innovation encouraged; staff more motivated and have higher job satisfaction.
(Davenport D (2013) The basics of clinical supervision. Nursing in Practice)
Further benefits of the PNA programme are evidenced in the national PNA programme evaluation and the PNA programme rapid literature review.
Monitoring, evaluation and quality control (normative)
The normative function “endeavours to develop management strategies for the professional accountability and quality issues in nursing. Themes emerge such as improving the quality of care which leads to changes of how nursing care is delivered to patients” (Brunero et al, 2008).
It concentrates on supporting individuals to become increasingly effective in their clinical role through undertaking quality activities to improve patient safety and outcomes.
Box 2: Benefits of the normative function
- Promotes professional accountability.
- Promotes involvement in improving quality issues.
- Improves effectiveness in a clinical role.
- Supports service improvement to deliver a high standard of patient care.
Personal action for quality improvement
This function of the A-EQUIP model addresses the need for nurses to be familiar with and contribute to quality improvement, to help improve patient care. Direct contribution to quality improvement and quality assurance systems (Box 3), as well as ensuring the safety of those receiving nursing care, are fundamental aspects of a nurse’s role. This function “ensures that the improvement of quality care becomes part of everyone’s role, every day, across the system”(NHS England, 2017).
Box 3: Nurse’s role in quality improvement
Carry out interdisciplinary processes to:
- meet organisational QI goals
- measure, improve and control nursing-sensitive indicators (NSI) – that is, those specific to nursing practices that affect patient outcomes
- carry out protocols and standards of care shown to improve patient care.
(Barnard C (2010) Ask the expert: Understanding nursing roles in quality improvement. Nurse Leader Insider)
Education and development (formative)
This educational function of the A-EQUIP model “identifies that learning should take place during clinical supervision… [and focuses on] skills and knowledge, learning from experience and competence,” to inform appraisals, revalidation and development of leadership (Proctor B (2000) Group supervision: A guide to creative practice (Counselling Supervision Series). London: Sage Publications).
Guided reflection can support the exploration of self-leadership through examining a nurse’s interactions with others, influence change and improve the delivery and standard of care.
2. The professional nurse advocate role
The PNA is a professional clinical leadership and advocacy role introduced to deploy the A-EQUIP model for registered nurses (see Section 3.4 for the PNA responsibilities as a sessional PNA or a full-time PNA). The role supports staff through a continuous improvement process that builds personal and professional clinical leadership, improves the quality of care delivered and supports professional revalidation. In summary, the PNA role involves:
- deploying the A-EQUIP model
- supporting and developing the nurse advocacy role
- guiding and supporting nurses through actions that will benefit other nurses, patients and families
- facilitating support and feedback to improve, advance and solidify the capabilities of the nursing workforce.
PNAs must demonstrate that they can take actions, link academic learning with their practical settings and experiences, and develop their practice skills to support colleagues to improve the capabilities of the nursing workforce.
2.1 Leadership
The educational programmes to train and prepare PNAs focus on leadership skills.
PNAs demonstrate leadership through emotional intelligence. As expert reflective practitioners they are self-aware and open-minded, and they understand their own emotions alongside recognising and influencing those of others. This provides a platform of psychological safety and promotes an optimal workplace culture for individuals to learn, develop and perform at their best.
Integrity and openness are essential PNA attributes, as is upholding the professional standards of practice and behaviour within The Code.
If PNAs are to advocate for their fellow nurses, other healthcare staff, and patients and their families, it is essential they actively listen and develop confidential relationships with individual nurses.
PNAs support a culture of autonomy, belonging and contribution (The King’s Fund, 2020) to inspire continuous improvement and empower staff in all positions to innovate (NHS Leadership Academy, 2011).
The PNA will have the knowledge and experience to facilitate feedback on themes and learning to influence education and quality improvement initiatives.
2.2 PNA-to-staff ratios
Effective supervision ratios depend on tasks, standards and responsibilities. These will vary for different nursing specialties and the appropriate ratio for deploying effective supervision can range from 1:5 to 1:20. At least one PNA per clinical team/ward will be needed, and to achieve this, nursing providers should commit to training at least 1 in 20 registered nurses for the PNA role by 2025.
In implementing the A-EQUIP model, some healthcare organisations have opted for sessional PNAs and others a combination of one full-time PNA and a small number of sessional PNAs (Smythe et al, 2023).
3. Implementation guidance
This section provides guidance on implementing the PNA role in an organisation and signposts to a suite of resources to support implementation.
From 1 April 2022, providers of nursing services have been encouraged, via the NHS Standard Contract Service Development and Improvement Plan (SDIP), to implement the PNA role within their organisations.
3.1 Governance – data collection and board reporting
As implementation of the PNA role is employer-led, the organisation’s leadership team is responsible for the implementation of the PNA role, including ensuring all nurses have access to restorative clinical supervision. All organisations should ensure the PNA role, and its delivery of RCS, is embedded in current clinical governance arrangements, including board oversight.
Suggested actions to underpin the implementation of the PNA role, collection of data and board reporting for every organisation are:
- Organisation’s chief nurse to identify a senior registered nurse who is responsible for the oversight and implementation of PNAs (within their organisation) and to liaise with the NHS England regional PNA advisor.
- Create a live register of the PNAs employed in the organisation: this will allow succession planning and maintenance of a 1:5 to 1:20 PNA-to-nurse ratio, dependent on setting.
- Establish a PNA community of practice.
- Ensure completion of the provider workforce return (PWR) and that qualitative data from PNAs is reported monthly, to enable local, regional and national oversight and evaluation of the implementation of the PNA role and A-EQUIP model (data collection on PWR started on Monday 1 November 2021).
3.2 PNA application criteria and training
PNA application criteria:
- be a registered nurse with the Nursing & Midwifery Council (hold a current registration)
- Band 5 or above working in a patient-facing clinical role within a healthcare setting providing NHS-commissioned care
- evidence of previous level 6 study (Bachelor’s degree level)
- completed the Professional Clinical Nursing Leadership e-learning modules on the PNA role and the A-EQUIP model.
PNA training offer:
- professional development at master’s level 7 with a national qualification in leadership and advocacy
- virtual classes to measure competency using chosen forms of assessment
- each student PNA will have access to a supervisor (qualified PNA) provided by their employing organisation
- access to booster sessions and national webinars
- designated PNA NHSFutures platform for various communities of practice, examples of best practice and networking.
PNA selection
A registered nurse who fulfils the criteria listed above can be nominated by their line manager or PNA trust lead to apply following the regional process to undertake the PNA training programme.
Hours of restorative clinical supervision
This guidance does not specify how many hours of RCS nurses should be able to access. Each organisation determines this to reflect the needs of its workforce, in line with its current clinical supervision policies and to comply with the NHS Standard Contract.
A nurse can be employed in the PNA role full time or on a sessional basis in addition to their substantive position, but the route to become a PNA is by undertaking a voluntary programme which equips registered nurses with an enhanced skillset to compliment their job role. The employer should choose the approach that meets the needs of the nursing service, but is encouraged for all those in a PNA role to include within their annual Personal Development Plan.
3.3 Regional support for PNAs
The NHS England regional PNA teams will support organisations with local implementation of the PNA role. Each of the seven regions has established a regional PNA nurse advisor role to provide professional leadership and direction. Contact information for the NHS England regional PNA teams can be found .
Each region will establish a network or community of practice to give PNA leads from all nursing providers/organisations the opportunity to meet, learn from each other and share ideas.
3.4 Roles and responsibilities
PNA checklists have been developed setting out the roles and responsibilities of the following:
- PNA
- nursing and healthcare provider
- nurse and healthcare staff (accessing a PNA and RCS)
- HEIs/PNA training providers
- NHS England regional PNA advisor.
Further resources
- Alderwick H, Charles A, Jones B, Warburton W (2017) Making the case for quality improvement: lessons for NHS boards and leaders. King’s Fund.
- Bond M, Holland S (2011) Skills of clinical supervision for nurses: a practical guide for supervisees, clinical supervisors and managers. Supervision in context. 2nd edn. Berkshire: McGraw-Hill Education (UK) Open University Press.
- Griffiths K (2022) Using restorative supervision to help nurses during the Covid-19 pandemic. Nursing Times 118(3).
- Lynch L, Hancox K, Happell B, Parker J (2009) Clinical supervision for nurses. Wiley-Blackwell.
- McCormack B, McCance T (2017) Person-centred practice in nursing and health care, theory and practice. 2nd edn. Oxford: Blackwells.
- Proctor B (2010) Training for the supervision alliance. Routledge Handbook of Clinical Supervision.
- Royal College of Nursing (2023) Professional nurse advocate standards for education and training programmes and modules.
- Wallbank S (2013). Maintaining professional resilience through group restorative supervision. Commun Pract 86(8).
Acknowledgments
The Professional Nurse Advocate taskforce is grateful to the following for their support in developing this implementation guide:
- Dame Ruth May DBE, Chief Nursing Officer for England
- Professor Emma Wadey, Deputy Director of Mental Health Nursing, NHS England
- Sarah Legood, Project Manager for Mental Health Nursing and Professional Nurse Advocate, NHS England
- Allison Meaney, Programme Business Support Officer, NHS England
- Karen Cameron, East of England PNA Regional Lead Advisor, NHS England
- Clare Capito, London PNA Regional Lead Advisor, NHS England
- Joanne Watson, Midlands PNA Regional Lead Advisor, NHS England
- Eileen Aylott, North East and Yorkshire PNA Regional Lead Advisor, NHS England
- Samantha Lungu, South East PNA Regional Lead Advisor, NHS England
- Amanda Shobrook, South West PNA Regional Lead Advisor, NHS England
- Kathryn Currah, Children and Young People’s Mental Health Advisor, NHS England
- Laura Spike, Children and Young People’s Mental Health Advisor, NHS England
- Aatikah Kaba, Staff Nurse, Blackpool Teaching Hospitals NHS Trust
- Alison Wells, Deputy Head of Education, The Royal Wolverhampton NHS Trust
- Amy George, Strategic Health Facilitator, Southern Health NHS Foundation Trust
- Andrea Stebbings, PNA Module Lead, University of Plymouth
- Catherine Gamble, Head of Nursing Practice, South West London and St George’s Mental Health NHS Trust
- Hannah Baker, Senior Sister, Mid and South Essex NHS Foundation Trust
- Helen Gadsby, Staff Nurse, Buckinghamshire Healthcare NHS Trust
- Jayne L Walker, PNA Module Lead, University of Hull
- Michelle Bridger, Community Staff Nurse, East Sussex Healthcare Trust
- Scott Topping, Senior Practice Development Nurse, South West London and St George’s Mental Health NHS Trust
- Stephen Jones, Professional Lead for Mental Health, Royal College of Nursing
- Vanessa Whatley, Deputy Chief Nurse, The Royal Wolverhampton NHS Trust
- Yvette Dimes, Senior Staff Nurse, Birmingham and Solihull Mental Health NHS Foundation Trust
The Professional nurse advocate A-EQUIP model: A model of clinical supervision for nurses has been endorsed by the Royal College of Nursing (RCN).
Publication reference: PRN00698_i