Executive summary and action required
This year marks five years since the NHS became the world’s first health system to commit to reaching Net Zero. The NHS Net Zero Strategy commits the NHS to regular reviews against our targets.
The NHS England Board are invited to note progress made in reducing NHS emissions, the associated benefits in decarbonisation and the improvements made to our carbon footprint methodology, aligning with global carbon accounting best practice
Background/issue and context
1. Climate change has a direct impact on the ability of health systems to deliver care effectively and efficiently. Unless acted upon, it will result in higher temperatures, more frequent and more severe incidences of extreme weather, increased air pollution and a higher risk of transmission of illnesses such as dengue and yellow fever. Total costs of heat-related mortalities from climate change and related socio-economic change in England have been estimated at approximately £6.8 billion per year in the 2020s, rising to £14.7 billion per year in the 2050s. The NHS is responsible for around 4-5% of the country’s carbon footprint and approximately 30%-40% of all public sector emissions.
2. In October 2020, the NHS became the world’s first national health system to commit to net zero. The Delivering a Net Zero National Health Service strategy provides a roadmap to net zero for all aspects of NHS emissions. The strategy was co-produced with an expert panel of climate and health representatives and set two ambitious but feasible targets (against a 1990 baseline):
- net zero by 2040 for the emissions we control directly (the NHS Carbon Footprint), with an 80% reduction by 2028-2032
- net zero by 2045 for the emissions we can influence but don’t directly control (the NHS Carbon Footprint Plus), with an 80% reduction by 2036-2039.
3. The Health and Care Act 2022 introduced legally binding duties on all NHS organisations to have regard to the Climate Change Act 2008 and Environment Act 2021 in the decisions they make, and more recently, Government’s Fit for the Future: 10 Year Health Plan for England reiterated a commitment to our targets and through its overall ambition provides opportunity for future decarbonisation.
4. This year marks five years since the publication of the NHS Net Zero Strategy. The strategy committed the NHS to regularly review the NHS carbon footprint and our progress against its priorities. Since that publication, we have been able to gradually improve and update our footprint methodology. This has allowed us to better understand the NHS emissions profile, improve prioritisation and focus on areas that can deliver the greatest carbon and cost savings.
5. To assess progress, the NHS Net Zero Expert Panel was re-established in May this year, bringing together global leaders and experts in the field of environmental sustainability and healthcare. Their knowledge and guidance has been instrumental in making a fair assessment of progress and updates to the Footprint methodology. Membership of the expert panel is set out at Annex A to this paper.
6. Drawing from the progress report published today and the NHS Carbon Footprint methodology, to be published as an academic paper, this paper outlines key progress made and highlights the excellent work by NHS staff to deliver our ambitions. It summarises methodological improvements and seeks to quantify some of the co-benefits of reducing our footprint.
7. We estimate the NHS has reduced its Carbon Footprint by 14% since 2019 and by 68% since 1990. Core progress has been delivered through a range of interventions made by NHS staff, focusing on the medicines we use, managing our estate effectively and the use of lower carbon travel and transport options within the NHS.
8. We estimate the NHS Carbon Footprint Plus is broadly the same as in 2019. This follows an increase in emissions following the pandemic and an overall increase in NHS activity. Over this five-year period, the NHS Carbon Footprint Plus has reduced by 15% per real pound of the NHS budget, and by 7% per finished admission episode (FAE).
9. The Board is asked to consider progress and note the wider benefits that have been realised as part the interventions to meet our ambitions.
Interdependencies and wider implications
10.Estimating the Carbon Footprint and Carbon Footprint Plus of the NHS is complex. Size and scale are broadly equivalent to that of some countries with modelling, data inputs, assumptions and emissions factors brought together to meet international best practice. Reporting of emissions helps to inform where interventions are most valuable to the NHS and also deliver against other reporting requirements, such as the Task Force on Climate-related Financial Disclosure (TCFD).
11. NHS England’s approach to Climate and Health footprint modelling and healthcare decarbonisation has been commended and considered by notable organisations including The Lancet, The World Health Organisation, the Intergovernmental Panel on Climate Change, and the Climate Change Committee. It has also inspired global action, with over 40 health systems in other countries, setting their own net zero targets and more than 90 countries committing to deliver low carbon, sustainable health systems.
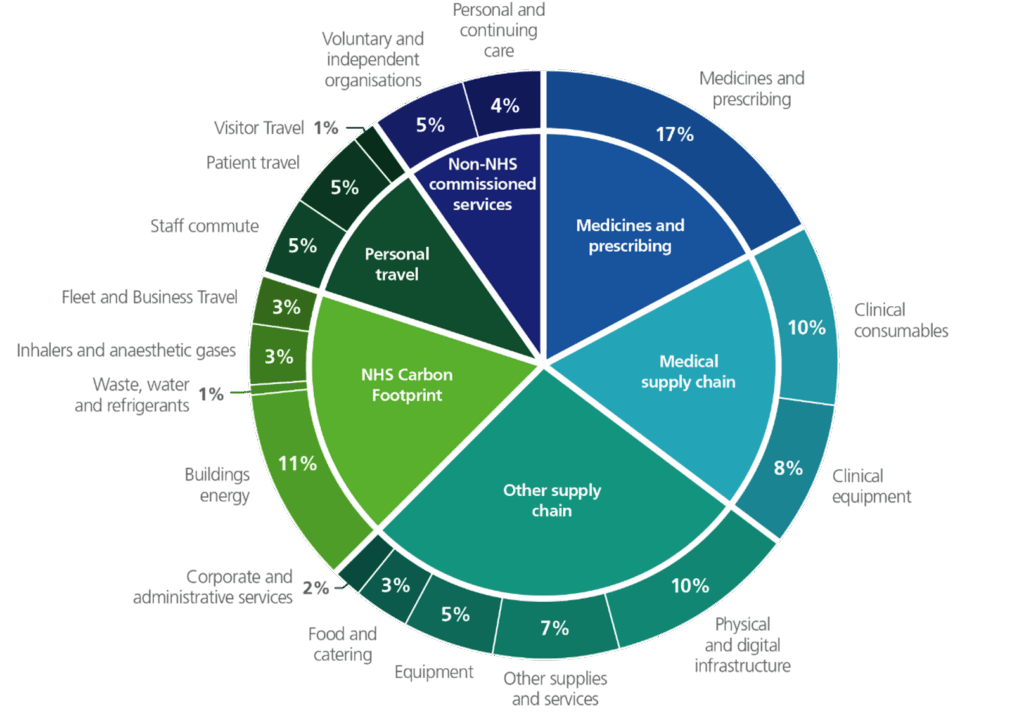
12. The updated methodology builds on the approach used in 2020 but has focussed on the use of new and more granular NHS-specific data, allowing a consistent methodology to be retrospectively applied across all years and allows previously published estimates to be improved and updated. Figure 1 represents an improved understanding of the source and intensity of emissions.
13. Notable improvements include: the addition of refrigerant emissions; estimates of waste treatment and fleet emissions, now based on NHS-specific data; and supply chain emissions are now based on financial data from individual NHS organisations. As such, new emission categories have been identified. Overall, this improved understanding of NHS emissions will help to prioritise and track actions nationally and locally. Like in 2020, a comprehensive overview of the updated methodology will be published as an academic paper to ensure transparency of the approach used.
Figure 1: An updated breakdown of emissions by source
Overall progress
14. Since 2020, significant progress has been made to reduce our emissions, concurrently improving patient health, reducing costs, reducing the NHS’ contribution to air pollution and increasing energy resilience and security.
15. Applying our improved footprinting methodology to carbon emissions calculations from the past five years, we can see that for the NHS Carbon Footprint, emissions in 2024/25 are estimated to be 4.7 MtCO2 Comparing with a revised estimate of 14.5 MtCO2e for 1990 emissions this represents a total reduction of 68%, and a reduction of 14% in just 5 years since 2019/20.
16. The Carbon Footprint Plus increased in 2020/21 and 2021/22, driven by the NHS response to the COVID-19 pandemic, but fell back to pre-COVID levels in 2023/24 and 2024/25. Considered alongside an increase in activity, staff and patient contact, falling back a similar level suggests, relative to activity, the NHS and suppliers are making progress in reducing supply chain emissions.
|
Figure 2 |
2019/20 |
2020/21 |
2021/22 |
2022/23 |
2023/24 |
2024/25 |
|
Total NHS Carbon Footprint (MtCO2e) |
5.5 |
5.2 |
5.3 |
5.0 |
4.8 |
4.7 |
|
Which consists of: | ||||||
|
Buildings energy, waste, water, and refrigerants |
3.5 |
3.3 |
3.3 |
3.2 |
3.2 |
3.1 |
|
Fleet and business travel |
0.7 |
0.7 |
0.7 |
0.6 |
0.7 |
0.7 |
|
Inhalers and anaesthetics gases |
1.4 |
1.2 |
1.2 |
1.1 |
1.0 |
0.9 |
|
The NHS Carbon Footprint is encompassed within the NHS Carbon Footprint Plus: | ||||||
|
Total Carbon Footprint Plus (MtCO2e) |
27.3 |
30.5 |
29.9 |
27.5 |
26.8 |
27.3 |
Figure 2: (table) annual total NHS Carbon Footprint and Carbon Footprint Plus (MtCO2e) for 2019/20 to 2024/25, updating figures published previously to be consistent with improved data and methodology. Please note the figures have been rounded to one decimal place.
17. Meeting the 80% NHS Carbon Footprint reduction target by 2032 would require emissions to fall to 2.9 MtCO2e, a reduction of 1.8 MtCO2e (38%) over the next 8 years, or an average of 225 ktCO2e per year. This will be challenging and dependent on several factors, but the Greener NHS team believes that this is achievable if current momentum is maintained.
18. Key actions will include: improving respiratory care and the introduction of more sustainable inhaler propellants; continuing work to reduce nitrous oxide waste; Government’s mission to make Britain a clean energy superpower and supporting the delivery of a £100m Great British Energy and NHS renewable energy programme; increased roll-out of zero emission vehicles in the NHS fleet, supported by £8m funding from the Department for Transport for Electric Vehicle Charging Points; and the adoption of low-carbon heating with a further £370m secured through Phase 4 of the Public Sector Decarbonisation Scheme (PSDS).
19. Heat decarbonisation is likely to be one of the biggest challenges to meeting our Carbon Footprint ambitions. PSDS has been the primary intervention to provide low carbon heating and cooling but will not provide any additional capital funding beyond Phase 4. However, partnering with Great British Energy, the Greener programme is planning to deliver nearly 200 onsite solar and storage projects across 78 trusts. When invested, it is expected to payback within 7-10 years, providing immediate savings on secondary care energy bills which have nearly doubled since 2019 to over £1.4bn.
20. Progress at a local level has been delivered through NHS staff producing, and delivering against, Green Plans. Recently updated Green Plan Guidance outlines key priorities and best practice to update plans, drive action and monitor progress. More detailed progress in key areas, is set out below.
Medicines
21. Working in collaboration with the NHS and industry, significant progress has been made in reducing medicines emissions. The total emissions from inhalers, nitrous oxide and volatile anaesthetics have reduced by 470 ktCO2e, or 33% since 2019/2020. Actions taken include:
- partnering with the Royal College of Anaesthetists and Association of Anaesthetists to decommission desflurane in favour of safe, and clinically appropriate alternatives has delivered 41 ktCO2e (98%) in emissions reductions. Direct savings are estimated to be up to £4m per year.
- improvements in respiratory care and optimising the use of inhalers is supporting patients to better manage their respiratory conditions, reducing direct emissions from inhalers. Emissions have fallen by over 340 ktCO2e (33%) since 2019/2020 and progress is expected to continue following the publication by NICE of updated asthma clinical guidelines, further supporting better outcomes for asthma patients and lower environmental impact; and
- reducing nitrous oxide waste through leaner supply and stock management has led to cost savings of over £2.3m annually and emissions reductions of around 90 ktCO2e since 2019/20.
Energy
22. The NHS is the UK’s largest single public energy user, supplying energy to over 13,500 buildings spanning 27 million m2. Overall, estates emissions have reduced by 10% since 2019/20. Across the secondary care estate energy consumption has reduced, with emissions associated with the consumption of grid electricity dropping by over 220 ktCO2e (21%). Key actions that have delivered those savings include:
- through the £1.4bn in additional capital funding secured through the PSDS, across over 100 projects which are expected to reduce energy bills, reduce emissions by over 125 ktCO2e, and typically provide a more comfortable ambient temperature environment for patients through building management systems.
- over £135m has been invested in energy efficiency measures, including LED lighting, solar panels, upgrades to building infrastructure, and enhanced building energy management systems. 50% of the secondary care estate is now equipped with LED lighting, and solar generation has tripled since 2019.
- Great British Energy (GBE) solar projects, allocated across 78 Trusts, are expected to deliver savings of around £8.6 million a year, and up to £260 million over their projected lifetime. The £100m capital investment is estimated to deliver around 50-65GWh annual generation and pay back between 7-10 years, equivalent to providing electricity for nearly 20,000 homes a year.
Travel and transport
23. Travel and transport emissions cover fleet and business travel emissions (700 ktCO2e) within the NHS Carbon Footprint, and personal travel (2,820 ktCO2e), representing 13% of the NHS Carbon Footprint Plus, in total. Within fleet and business travel, 140 ktCO2e are associated with the ambulance fleet, 30 ktCO2e with other NHS owned and leased fleet, and 520 ktCO2e associated with other transport and transport services. Personal travel comprises both staff commutating and patient and visitor travel – it is estimated 90% of these emissions relate to travel by car.
24. Whilst overall transport emissions have increased, driven by increased spending in NHS organisations on transport, significant progress has been made in transitioning the NHS fleet in line with the NHS Net Zero Travel and Transport Strategy which, when delivered, is expected to deliver annual operational savings of £59 million and over £270 million a year in wider health and societal benefits. Key areas of progress include:
- wide scale adoption of zero-emission vehicles (ZEVs), across the NHS fleet with one in 10 now being ZEV, compared to one in 100 in 2021.
- twenty-one zero-emission emergency vehicles are being trialled across ambulance trusts, and twelve electric 19-tonne trucks are now in operation across the country.
- in July 2025 the Department for Transport and the Department for Health and Social Care announced the NHS ChargePoint Accelerator scheme. An investment of £8 million will support the installation of on-site electric vehicle chargepoints on NHS sites.
25. Staff continue to be supportive of the NHS taking action on net zero with 9 in 10 staff supporting this ambition. Across the NHS small changes in behaviour have unlocked improved patient outcomes, efficiency, cost savings and greater staff retention. The ambition is to now embed behaviour change at all levels across the workforce, to deliver these demonstrated benefits.
26. Collaboration with the Royal Colleges, clinical associations and societies has seen the development of a range of specialty specific guidance for the clinical workforce. This includes but is not limited to the Royal College of General Practitioners – Net Zero Hub; The Royal College of Emergency Medicine – GreenED framework; Green Impact – Dentistry Toolkit; and the Royal College of Psychiatrists’ Net Zero resources and guidance amongst others– all offer guidance to clinicians and staff on options to deliver greener care, improve patient health, deliver financial savings and reduce emissions.
27. In partnership with the Greener NHS team, NHS England’s Getting It Right First Time (GIRFT) programme has developed ‘GIRFT greener pathways’, a cross-specialty approach to decarbonising clinical care featuring high impact climate recommendations. Implementation can reduce carbon emissions by 2470 tCO2e, as demonstrated by work on the bladder cancer pathway, as well as increasing same-day diagnosis and allowing patients to spend less time in hospital.
28. Greener NHS continue work to implement the Government’s Design for Life roadmap in partnership with the Department of Health and Social Care. Ensuring a transition away from all avoidable single-use medical technology products towards a functioning circular system by 2045 by identifying opportunities to maximise reuse, manufacture, recycling, and resilience.
Supply chain
29. A large proportion of the NHS Carbon Footprint Plus is associated with the supplies and services purchased by NHS organisations, with over 600,000 products purchased from 80,000 national and global suppliers. Supply chain emissions for 2024/25 are estimated to be around 12.4 MtCO2
30. The Net Zero Supplier Roadmap, published in 2021, set expectations for suppliers to help meet the NHS ambition to decarbonise its supply chain and provides useful indicators for supply chain decarbonisation. Progress includes:
- Adoption of a 10% weighting for net zero and social value across all new NHS procurements since April 2022. From April 2023, implementation of the Cabinet Office Procurement Policy Notice 006 began, requiring suppliers for all new contracts above £5 million per annum to publish a Carbon Reduction Plan (CRP). From April 2024, this was proportionately extended to all new procurements.
- under this extended policy, 90% of NHS (non-pay) spend is in scope of Carbon Reduction Plans (CRP) or Net Zero Commitment requirements; and
- over 2000 suppliers have signed up to the Evergreen Sustainable Supplier Assessment, a tool for suppliers to engage on their sustainability journey.
31. The shift from analogue to digital driven by the 10 Year Health Plan will transform the way that care is delivered in the NHS, by putting care into the hands of patients through technology. This digital transformation will need to meet the needs of patients and users efficiently and sustainably; whilst also ensuring that IT systems are resilient to the impacts of climate change.
32. Emissions associated with digital contribute to categories throughout the Carbon Footprint Plus including purchase of hardware, software and MedTech. There are also emissions associated with energy usage – as a result calculating a single total for digital emissions is difficult due to the complexity of purchasing. Despite these challenges we know that a range of interventions to support the switch from analogue to digital have delivered and continue to deliver carbon savings, including:
- the creation of more than 12,000 virtual ward ‘beds’ is allowing patients to get the care they need at home safely and conveniently. The NHS is increasingly introducing virtual wards to support people at the place they call home, including care homes. This is expected to deliver savings of up to 100 ktCO2
- the NHS App outpatient booking service allows patients to quickly and easily book outpatient appointments, the service could save 29 ktCO2e, 63 million sheets of A4 paper and 152 million minutes of staff time each year.
Annex A – NHS Net Zero expert panel members
- Chair – Chris Gromley, Chief Sustainability Officer, NHS England
- Professor Mike Davies, UCL Institute for Environmental Design and Engineering
- Professor Matthew Eckelman, Department of Civil and Environmental Engineering, Northeastern University
- Professor Piers Forster, University of Leeds and Chair of the Climate Change Committee
- Professor Kamila Hawthorne, and later Dr Victoria Tzortziou Brown, Chair Royal College of General Practitioners Council
- Dr Josephine Sauvage, Chief Medical Officer of North Central London Integrated Care Board
- Dr Richard Smith, Chair, UK Health Alliance on Climate Change
- Professor Nick Watts, Director, Centre for Sustainable Medicine
- Chris Naylor and Zoe Abrams, Kings Fund

