How to use this guide
This guide will help boards to consider their approach to handling and acting on the information they receive. It considers the leadership behaviours and culture of the board and how these can affect the information it receives and the actions it takes, as well as metrics that can support the board to better understand the organisation’s performance.
The 6 domains are indicative areas of oversight and should be read as a collective – for example, information about an organisation’s estate could fall within all domains.
The supporting guidance includes further metrics and additional considerations which boards may find useful to provide insight into their trust’s performance. Boards should also consider performance against the objectives set out in the annual priorities and operational planning guidance, as well how it is contributing to its local system plans.
This guide is not an exhaustive governance resource and should be read alongside the Code of governance for NHS providers and guidance on good governance and collaboration. Also, it is not intended to be used as a checklist; it is to support boards to reflect and consider whether the leadership, culture, systems and processes they have in place are using information in the best way to lead their organisations effectively.
The recommendations are best practice advice, not mandatory guidance, and non-compliance is not in itself a breach of any regulatory requirement.
This guide is structured as follows:
- governance and culture: the factors that make it challenging for the right information to flow to the board and the role of effective governance in tackling this; how boards should handle and act on information; and the importance of a curious, problem sensing and open culture
- meaningful information: the principles that govern the flow of information to the board, and tools to report that information; and a strong focus on outcomes rather than actions and processes
- 6 domains for consideration: these areas and illustrative metrics can be used by boards to understand if their organisation has a sufficiently comprehensive framework for reviewing trust performance, making decisions and developing strategy
- putting the framework into practice: a sample integrated performance report (IPR) to illustrate how information can be presented and used effectively
1. Governance and culture
The role of an NHS provider board
The board is responsible for ensuring the healthcare and other services the trust provides for patients are high quality and safe. The board also promotes the long-term sustainability of the trust as part of its integrated care system (ICS) serving the wider population and healthcare system. The board has a collective responsibility for:
- ensuring high-quality and effective care for all patients and service users
- setting strategic direction, ensuring the executive has appropriate capacity and capability to monitor and manage quality of care and operational delivery
- adding value to the success of the organisation and its system
- using prudent and effective controls to lead the organisation
- promoting and adhering to the organisation’s values
- ensuring the organisation’s obligations and duties are met
As set out in the Code of governance, boards are unitary, which means decisions are taken as a single group of executives and non-executive directors, and all members of the board share the same responsibility and liability.
Well-led boards:
- set a challenging but achievable strategic direction
- identify the strategic issues that require discussion or decision and distinguish these from operational detail
- embed the trust’s values throughout the organisation to consistently improve the culture
- provide constructive challenge
- make sure all patients and service users receive a consistently high-quality service
- ensure that innovation and transformational change are being delivered and benefits realised
- focus on improving access to services and reducing health inequalities across all the communities they serve
- make sure taxpayers receive value for money by maximising productivity
- identify unwarranted variation in quality and performance
- triangulate signals from different sources to identify underlying issues
- use benchmarking tools and data such as the Model Health System to regularly compare their performance with similar organisations
- embed continuous quality improvement approaches in all aspects of service delivery
- understand and respond to the needs and views of patients, service users and all the communities they serve, listening to their experiences and using their feedback to improve services
- anticipate the potential impact of policy, technological and socioeconomic developments
- protect board agenda time to regularly reflect on learnings from independent reviews
- assure themselves that the organisation is complying with statutory duties, quality and clinical standards, other regulatory requirements and national priorities
To fulfil these duties, run their organisations well and support their system, boards need to have the appropriate mix of knowledge, skills, experience and diversity to reflect their population.
Boards also need to ensure:
- effective governance arrangements are in place across their organisation
- their trust has an open, curious and transparent culture which supports the sharing of information, provides psychological safety and fosters learning and improvement
- insightful information is used to set strategy, oversee the quality of care and delivery of national standards, and monitor the overall health of the organisation and its people
While the need for robust and relevant information and its effective use and interpretation is the focus of this guidance, the other elements above have a significant impact on how information is cascaded through the organisation. It is good practice for boards to conduct in-depth, independently facilitated developmental reviews every 3 to 5 years to assess how well-led the trust is across all areas, and to identify areas where their leadership and governance can improve.
It is important for boards to continually review and understand their trust’s performance against guidance and good practice. As part of a continuous development ethos, boards should routinely consider what training and other resources they need to have the required skills and experience.
Effective governance arrangements
Effective governance is essential for the quality and timely flow of information to and from the board. This flow is critical for trusts to make the right decisions based on the correct information. As the factors underpinning effective governance can evolve, for example, as services change, people leave or organisations restructure, regular reviews can help to ensure governance remains fit for purpose.
‘Active’ governance means issues are considered by the most appropriate people, relevant information is reviewed in the most useful format and at the right time, and the level of scrutiny produces rigorous challenge and an effective response. Findings with a material importance for the organisation should be identified and reported promptly to the board and analysed through a thematic lens.
The unitary board and collective discussions and decisions
All board members should have sufficient understanding of issues and risks across all aspects of the trust’s operations to make decisions and ensure there is a culture which supports open debate. Appropriate training for board members, including on topics such as finance and clinical and financial governance, can be an effective way to enable this. Reports to the board should be concise with issues, risks and mitigating actions clearly set out.
The unitary board and collective discussions and decisions
All board members should have sufficient understanding of issues and risks across all aspects of the trust’s operations to make decisions and ensure there is a culture which supports open debate. Appropriate training for board members, including on topics such as finance and clinical and financial governance, can be an effective way to enable this. Reports to the board should be concise with issues, risks and mitigating actions clearly set out.
Governance – questions for provider boards to consider:
- Are the chair’s roles and responsibilities clearly set out?
- Are there rigorous skills-based recruitment and appointment processes for non-executives, and are these independent?
- Does the size of the board, the committee structures and processes reflect the size, services and complexity of the organisation?
- Are there regular performance reviews of the board and its individual members?
- Does the board receive the right information, presented in the right way and at the right time?
- Are there robust internal controls across the trust to support organisation-wide transparency and accountability?
- Are the right structures in place to escalate information through the organisation from the point of care to the board?
- Is the board able to hear patients, service users and staff voices in an authentic way as part of its leadership role?
- Are the roles and responsibilities of the Senior Independent Director clear and agreed by the board (as set out in the Code of governance)?
The board’s role in shaping culture
Investigations into care failings continue to highlight the importance of an open culture. Staff, patients and service users should feel able to speak up and share concerns and see them escalated and acted on. Boards need to receive the right information about these to make decisions based on accurate and timely data and intelligence.
Board members need to be regularly visible to provide opportunities for staff to engage and feed back, in addition to Freedom To Speak Up (FTSU) and other channels. It is essential to frequently test whether information presented in board reports matches the reality for patients and staff at service level. Fundamental to good oversight is curiosity and appreciative inquiry and knowing when to seek external review and when to directly address concerns. This is important at all levels of the organisation and especially the board.
The board shapes the culture of its organisation by how it operates and behaves. Boards require diversity of thought to improve decision-making and enable alternative views to be debated and evaluated. No areas should dominate the conversation at the expense of others. In particular, the ‘clinical voice’ (including that of trainees) should always be heard across all remits of the board. Some important areas (such as estates) may not have individual executive representation on the board; for these areas it is even more important that information flows effectively so the board can understand risks, issues, opportunities and progress.
Transparency and candour
The Care Quality Commission’s ‘Regulation 20: Duty of Candour’ is a statutory duty to be open and transparent with people receiving care.
Boards must develop and foster a safe reporting culture so that staff, service users and family members feel able to report incidents or concerns and have assurance these will be listened to and acted on.
Creating a feedback loop is essential for a transparent culture. The board should ensure that staff, patients and service users are told about what is happening or has happened as a result of their feedback. The board should ensure that staff, patients and service users are told about what is happening and has happened as a result of their feedback.
Board members, through their actions and how they govern, should be visible and approachable role models who lead and promote the organisation’s values for their staff and patients and service users.
A positive organisational culture is:
- open and transparent – there is an open and honest reporting culture at all levels. Staff feel psychologically safe to speak up and raise concerns in a just culture which supports continuous The organisation’s information, data and decisions are shared with patients, service users and partners when requested
- compassionate and inclusive – staff understand patient experience and the impact of inequalities on health outcomes and they actively promote equity, equality, diversity and inclusion. The trust has policies and procedures to identify and address behaviours that are inconsistent with NHS values
- fair and just – the board and senior managers consider wider systemic issues when things go wrong, ensuring the organisation and individuals learn without fear of retribution. Boards understand why failings occurred and what has led to staff behaviours and poor patient outcomes. A just culture is one which balances learning from incidents with accountability for their consequences – and where no-one fears blame
- problem-sensing – leaders at all levels proactively seek out and listen, not only to the views of those they lead but also to the experience of patients, service users and their families. The board demonstrates an understanding of their role in detecting early – and preventing – closed cultures. When something goes wrong people are informed and supported, and the duty of candour is followed
- continuously improving – there is a genuine and proactive interest in finding out what has worked elsewhere and examples that have been successfully adopted, as well as local innovation to identify ways to improve. The board seeks assurance that quality improvement has been applied to test ideas to solve complex problems
Problem-sensing
Well-led, successful boards should be scrutinising the information and data presented to them. Crucial to this is having a problem-sensing culture, described by Dixon-Woods & Martin (2023) “Problem-sensing involves actively seeking out weaknesses in systems relating to quality and safety, typically using multiple techniques and sources of organisational intelligence.
[This includes] forms of organisational intelligence that offer challenge, disrupting any incipient risk of complacency…As with the collection of “harder” data, though, it is important not to mistake activity for action.
Simply undertaking listening activities or unannounced visits is no substitute for the hard work of analysing and responding to the issues they unearth. The willingness of those at the “sharp end” [frontline] to speak and of those at the “blunt end” (senior leadership) to listen exist in a reciprocal relationship.”
Culture – questions for provider boards to consider:
- Does the board role-model a culture of open and curious challenge?
- Does the board understand when to seek external review and independent input?
- Is most of the discussion at the public board, and with clear justification for any items discussed in private?
- Are issues appropriately escalated from executives and is information presented transparently?
- Does the board balance operational performance with people performance at all levels of the organisation?
- Do all board members undertake 360-degree feedback?
- Does the board proactively seek views, listen to them and demonstrably follow-up, and promote the value of a ‘speaking up’ culture?
- Is Freedom to Speak Up (FTSU) information discussed at the board and is it considered alongside other sources of information on organisational culture?
Corporate governance – processes and structures
An effective and high-performing board needs to be supported by a robust corporate governance structure that enables the seamless flow of information and decision-making up and down the organisation, supported by independent perspective and challenge from non-executive directors. This structure needs to be complemented with effective policies on risk, and risk escalation, and delegation for the board to operate effectively. In addition, given providers’ requirements to meet the standards of other healthcare regulators, where there are specific regulatory or other roles set by a statutory body in the trust (for example the Human Tissue Authority’s ‘Designated Individuals’ for mortuaries), these have a clearly defined line of sight to the board.
Board committees
Boards should make the best use of committees, delegating where appropriate functions and responsibilities that are best considered in these forums to allow more dedicated time for detailed review and consideration. These can be standing committees (for example, audit, finance, quality) or time-limited, for example, if a board has a particular aim or programme that requires more detailed oversight and scrutiny, such as significant investments in new buildings or whole-organisation digital systems.
Boards should review committees’ effectiveness regularly as well as their structures (at least annually) to ensure they are fit for purpose and support board governance and organisational oversight. Alongside, boards should have clear schemes of delegation and standing financial instructions that clearly set out the functions of these committees and associated responsibilities and accountabilities.
Committees should report regularly to the board in a balanced and insightful way which does not simply repeat the information and discussion that has already taken place at the committee.
Committee reports should be concise and consider the most appropriate metrics and commentary for the performance or issue being considered. The domains included in this guide give an overview of the metrics that should be considered by boards and these should often be reviewed first by a committee.
One of the values non-executive directors (NEDs) can bring to board and committee performance is by providing independent perspectives on how the data and other information are scrutinised. To foster a diverse experience base across NEDs, each NED can sit on multiple committees, for example, quality and finance, so they can gain different perspectives.
The supplement to this guidance outlines additional areas which committees may find useful when trying to understand an issue or improve performance.
Using information
The NHS generates a lot of data. Boards do not need to see every metric every month, otherwise they would be overwhelmed. Information needs to be scrutinised at the right level in the organisation and reviewed or escalated accordingly.
Information presented needs to:
- be timely, reflecting the most recent data available
- cover both improvement – using statistical methods to track trends over time, looking at variation and not just comparing against targets at a point in time – and assurance – looking at whether standards are being met and comparing performance against relevant historical trust data or external benchmarks
- be valid and subject to review – are the measures fit for purpose? How much weight can be placed on the data?
- allow for deep dives to understand care quality and performance within a directorate, department, team, service and at the point of care.
Confidence in information received – assurance vs reassurance
When receiving reports, the board and its committees should ensure there is a balance of assurance and reassurance in the information it receives. Boards need to have confidence that the information is a true reflection of performance and improvement and there are no other issues or considerations arising that warrant further review. The diagram below outlines the questions and lines of enquiry board members should be pursuing.
Figure 1: lines of enquiry board members should be pursuing
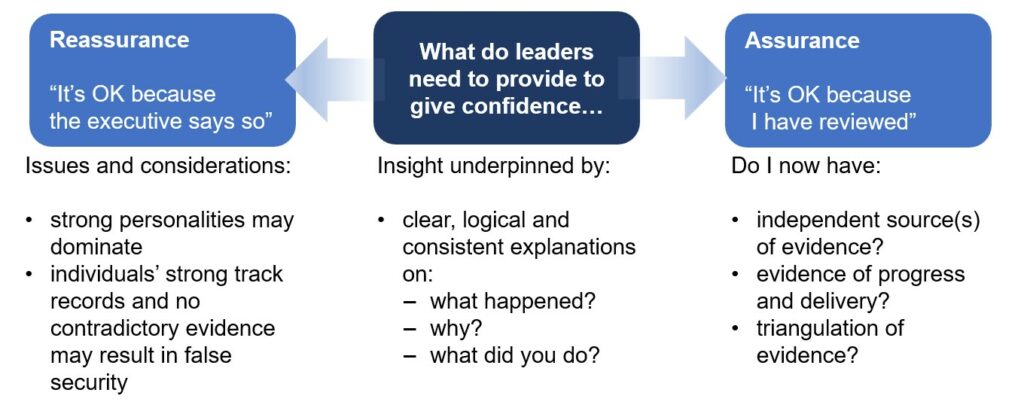
Issues and considerations:
strong personalities may dominate
individuals’ strong track records and no contradictory evidence may result in false security
What do leaders need to provide to give confidence…
Insight underpinned by:
clear, logical and consistent explanations on:
what happened?
why?
what did you do?
Assurance – “It’s OK because I have reviewed”
Do I now have:
independent source(s) of evidence?
evidence of progress and delivery?
triangulation of evidence?
For example, if a trust has identified a safety or quality issue and sought to resolve and address it internally, it must ensure it has seen evidence and independent validation of the actions taken to assure the board the issue has been resolved.
Board and committees – questions for provider boards to consider:
- Is the role of each board committee clear, including what areas and organisational risks it covers and how it reports into the board?
- Are there areas and functions of your trust’s operations that require specific governance groups (for example Mental Health Act)?
- Are board agendas planned in such a way over the year that all relevant areas of the trust’s operations get the appropriate scrutiny?
- Is there the right balance between strategy – developing and delivering it – and day-to-day operations?
Organisational policies and procedures
To validate an organisation’s information, it is essential that policies and procedures are in place and these are well understood across the organisation and kept under regular review. For the purposes of board reporting, this is especially important for risk management policies, schemes of delegations and financial instructions. These policies should clearly set out:
- standing orders for how an organisation carries out its business
- nominated/designated individuals where appropriate
- financial instructions which detail the financial thresholds and limits that apply to the organisation and its budget holders
- schemes of delegation which set out where responsibility and accountabilities lie and where they have been delegated to committees, executives or other forums
Schemes of delegation are especially important when organisations consider new models of collaboration, including across systems, to deliver care differently. Boards must be clear where decision-making and accountability sits when making any changes to the organisation’s delegated functions.
2. Meaningful information
Boards need relevant and insightful information to inform their decision-making. This information needs to cover the organisation’s statutory requirements, quality of care, delivery of services, progress against strategic objectives, use of resources and local intelligence. Boards should look at the organisation’s internal priorities as well as those of their local system and national areas of focus.
The amount of data available to organisations and boards continues to increase. Reducing the risk of information overload requires:
- governance structures including board committees to provide more detailed scrutiny of specific areas
- the board to have confidence in the scope and robustness of these committees and the escalations and reports arising from them
Reports to the board should focus on the outcomes and impact of the board’s actions to deliver change and improvement, and not just report on processes or progress made against a plan.
This section sets out high-level principles for how information can be prepared and shared at board level.
Board-level information
Boards and teams across the organisation need to distinguish between information that:
- needs to be reported routinely – for operational or statutory reasons – to the board with a certain level of detail
- needs to be reported only if there is demonstrably a problem, for example, where performance significantly diverges from that achieved by peer trusts
- changes relatively slowly and that should therefore be looked at only on a quarterly or 6-monthly basis
In planning agendas and structuring reporting, boards should be mindful of these dynamics. Reports to the board from committees must provide a meaningful summary of the issues and risks that have been discussed, rather than simply noting that discussion took place. There should be a clear process with defined criteria by which teams outside of committees can escalate matters to the board as necessary.
Information should not be repeated unnecessarily in board packs (for example repeated provision of background information) so that board attention can be focused on the key messages, updates and actions. In the final board pack, charts and other data should be in a legible and accessible format and units of time should be presented consistently for comparative purposes. For some data, forecasts and trajectories should be included (for example, revised financial run rates). Consideration should be given to how professional views can complement data to provide greater insight into findings and observations. Papers should always be provided with adequate time for members to review and scrutinise the information in advance. Boards should regularly review the quality of the information provided to support board discussions and provide assurance, to ensure the information and format is appropriate.
Aggregation
Some quality and performance information is typically reported in aggregate forms to simplify the volume of information seen by the board and allow for easier triangulation – for instance as part of an overall summary to an integrated performance report, performance on a page or integrated balanced scorecard which provides a high-level overview of organisational performance across specified domains.
While these aggregate metrics can help simplify the complex landscape of data and provide an at a glance picture of the organisation’s performance, they are also by their nature limited and are not designed to highlight emerging issues at site, specialty or clinical business unit level. The risk of issues being masked within aggregate data is likely to increase with the size and complexity of the organisation and the clinical business units within it.
Integrated reporting enables board members to get a clear picture of successes, failures and emerging risks, and prepare insightful questions in advance of a meeting (at a strategic level rather than becoming too operational). It is essential that integrated reporting describes the reasons for unusual patterns in data and the actions being taken. Many integrated performance reports simply describe the data rather than articulating causes and actions being taken in response.
For integrated reporting, many metrics are reported and calculated monthly. Boards should not require reporting which is calculated more frequently than this and some metrics are not updated frequently, for example, annual survey information. Data tools such as Statistical Process Control (SPC – discussed below) should be used to ensure that an organisation does not react unnecessarily to expected variation in regularly reported data.
Data should routinely be considered from a health inequalities perspective and by ethnicity and deprivation, and to determine which population groups might be missing from data.
Exception reporting
Reports by exception are important and boards need a clear process for escalating matters either within or outside the normal reporting cycle, for example, ad hoc information from third parties such as auditors, professional bodies like General Medical Council (GMC) and Nursing and Midwifery Council (NMC) or national clinical audits.
Triangulation
Boards will often be presented with a range of information cutting across multiple areas of activity. Seemingly non-related elements can, when taken together, reflect an underlying issue that otherwise may not have been picked up in time. Other information may highlight unintended consequences of policies or decisions that need drilling into.
Boards should always be aware of potential interlinkages, triangulating where necessary to identify and focus in on potential emerging issues. Examples include:
- considering levels of complaints along with their nature and the appropriate response to them, for example, about maternity settings, and correlating with trainee reports, patient safety incident records and information from medical examiners or national audit findings
- agency pay, productivity measures and safe staffing red flags
- patient and family voice and themes from patient safety incident data
- comparing staff survey information with patient and service user experience
- considering potential linkages between the built environment (for example the condition of the trust’s estate) and quality and safety metrics
- movements in quality and outcomes with operational productivity measures
Boards should gain assurance from board reports and a range of other information (especially patient, service user and staff feedback) and direct observation. Using listening events, walkarounds, patient stories and narrative accompanying quantitative data at board level is best practice. Boards can gain insights via shadowing, ‘mystery shopper’ type data gathering, role swaps and clinical simulation. It is important these are carried out with an improvement mindset rather than as a compliance-based activity. Where different sources appear to contradict each other, further investigation may be necessary.
Triangulation
To understand the factors that may be affecting the quality of care patients receive, boards should look at a variety of indicators and sources. Examples include:
- considering, at unit level, staff turnover, grievances, sickness levels and survey data and correlating these with patient experience and quality issues to identify root causes of problems
- correlating Estates Return Information Collection (ERIC) data, patient and staff experience, and estates related safety incidents as part of a patient safety review across the trust’s estate
It is important to scrutinise trends across multiple indicators to understand the source and drivers of key issues and to then implement evidence-based solutions.
Using national and local data
While most data considered by boards is drawn from local systems, boards must also consider national data and reviews. National dashboards and data sources such as the Model Health System, the Office of National Statistics, clinical audits, the Data Quality Maturity Index (DQMI), those from the Healthcare Quality Improvement Partnership (such as MBRRACE-UK) and others provide opportunities for benchmarking and review of progress against national targets and comparable peer trusts. These may draw out themes such as health inequalities which may be less evident from local data alone. Board members can use these alongside the information in board packs to form a broad understanding and triangulate the information they receive. Improvement tools and approaches such as NHS IMPACT and national and local clinical audits also support trusts to understand their data and focus their improvement resource on patient outcomes.
Establishing a framework for data reporting
Information should be framed and presented in a way that enables board members to understand the relevance of it to the agreed strategic objectives and processes for managing risk and gaining assurance. A consistent style of reporting should be adopted for board and committee reports.
Some boards may choose to structure integrated performance reporting according to thematic domains (for example, quality, workforce, finance) while others choose to structure or align reporting to the Care Quality Commission (CQC) domains or well-led quality statements (plus finance), which enables self-assessment against the domains in an integrated way. For assessing broad areas, such as urgent and emergency care, boards integrate indicators from multiple domains to understand all factors that impact performance.
Reporting can also take the form of a themed dynamic report. This could focus on different, specific areas and themes, for example, across performance data, clinical insight or lived experience. This can be planned periodically through the year as part of a forward plan. This can allow a more holistic view of quality with a limited set of indicators presented.
Analytical tools to guide decision-making
There are several statistical and other analytical tools to guide decision-making. One is Statistical Process Control (SPC), which looks at data over time using a control chart to reveal the type of variation in a process. There is a strong evidence base demonstrating the benefits of SPC.
NHS England’s Making Data Count programme provides training for boards on the benefits of replacing more traditional methods of analysing data such as Red Amber Green (RAG) reporting with SPC. While RAG reporting provides an at a glance method of understanding performance, it can mask important messages in the data, driving unhelpful behaviours, poor decision-making and potentially wasted time and resources. Many trusts now use SPC as the primary method of analysis to understand quality, performance, workforce and finance data. Boards have reported benefits including:
- a strengthened ability to challenge
- reduced time being distracted by insignificant changes in data
- better governance processes
- greater clarity on where the board should focus its attention
Read more about the benefits of SPC. This sample integrated performance report incorporates SPC charts, pareto (also referred to as the 80/20 rule) charts and associated narrative. A pareto chart is a useful analytical tool to demonstrate the key contributors to an issue. It is important to triangulate quantitative data in the integrated performance report with available qualitative data.
Does the trust have, and will keep in place, effective arrangements for the purpose of monitoring and continually improving the quality of healthcare
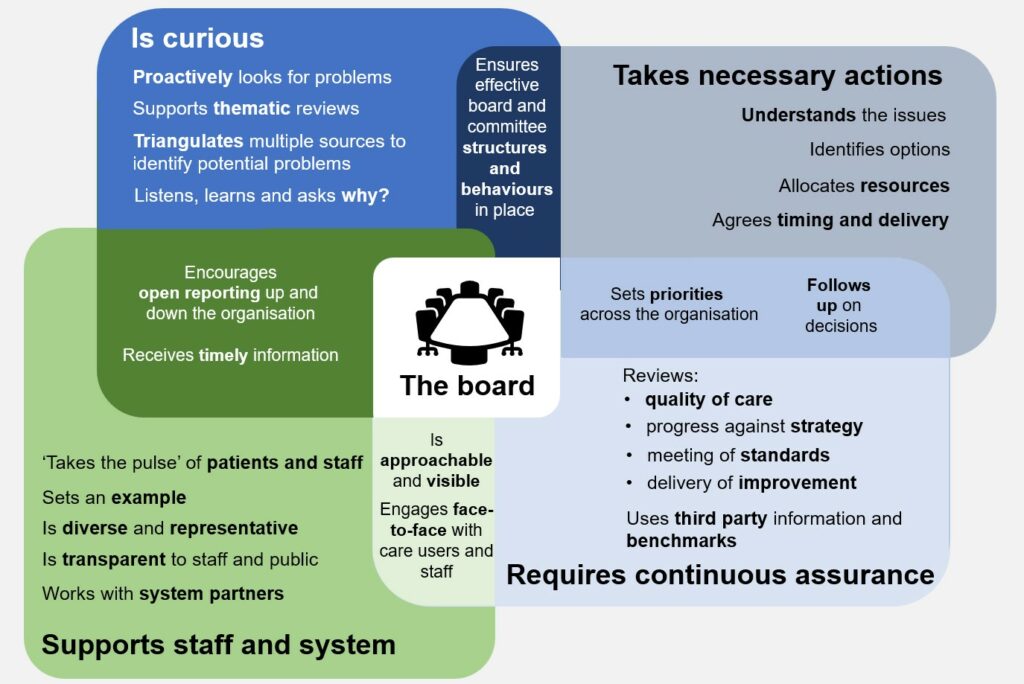
Figure 2: the characteristics of effective NHS provider boards
3. 6 domains to consider
This section provides an overview of the types of information and metrics which may be considered by boards. By its nature it is extensive and although it identifies mandatory reporting, the inclusion of metrics in these domains does not mean they, and all related information, should routinely be reported. Similarly, the domains are not the only or best way to frame information provided to the board.
Information overload is a real risk. Minimising it requires a thoughtful consideration of the organisation’s risks and priorities and the quality of the data available to develop a bespoke approach to reporting, and which allows the board to have meaningful discussions that support learning and decision-making.
I. Strategy
Questions for boards:
- Does the organisation’s strategy reflect shared priorities across the system and an agreed contribution to the Joint Forward Plan and Capital Plan with integrated care board (ICB) and system partners?
- Is the trust working effectively and collaboratively with system partners and its provider collaborative for the overall good of the system and population served?
- Is the board assured that it is overseeing the delivery of its organisational strategy effectively, and that this is responding to the needs of the local system strategy?
- Is the organisation meeting, and will continue to meet, any regulatory directions placed on it or undertakings?
Boards are focused on collaboration and how best they can work with their local systems and partners to deliver the best outcomes for their local population. Each organisation is a partner in at least one integrated care system (ICS) and one provider collaborative, and the organisation’s own strategy needs to support not just the organisation’s own service delivery, but that of its system and provider collaborative(s). When governance operates collaboratively, all parties who have an influence in the delivery of healthcare outcomes recognise, understand and respect each other’s needs, and work together to align their governance arrangements.
The board’s strategy needs to enable the organisation to deliver clinically, financially and operationally sustainable services for the population. Developing strategy involves close consultation with clinical colleagues and staff across the organisation, as well as the ICB and other partners in the local health economy (having regard to the Joint Strategic Needs Assessment), including citizens, patients, and service users, carers, and their families. Boards must set aside time to ensure their strategy is clear and well-developed, with most of their time devoted to strategic objectives that have appropriate goals and ways of measuring progress against their achievement and demonstrating success. Boards also need to ensure they are meeting their organisation’s legal and regulatory requirements.
Board strategies need to take account of national plans for the NHS and associated guidance, priorities set out in operating planning guidance, government commitments such as Net Zero as well as clinical and technological advances which change how care is delivered. The table below outlines some areas of focus and metrics boards should consider when setting their strategy and evaluating the delivery and impact of it.
Area: Trust’s own strategic objectives
Relevant indicators and measures (quantitative and qualitative):
- Locally defined
Area: Local system objectives including forward plans
Relevant indicators and measures (quantitative and qualitative):
- Developed with local ICB
- Whole system measures developed through co-design
Area: Organisational development
Relevant indicators and measures (quantitative and qualitative):
- Assessments of local health needs and inequalities in access and outcomes
- Referral rates by diagnosis and procedure from local GPs to the trust
- Benchmarking analysis from GIRFT and Model Health System
- Strategic development indicators such as:
- o commercial priorities
- o digital and data priorities (such as digital transformation and cyber security threats)
- o technology opportunities
- Progress in delivering transformational change
Area: Pan-organisational activity and resource planning
Relevant indicators and measures (quantitative and qualitative):
- Identifying priorities and converting these into clear and quantifiable targets
- Ensuring capacity and demand projections inform workforce, activity and financial planning
Area: Key trends and forecasts
Relevant indicators and measures (quantitative and qualitative):
- Trends in income and expenditure against budget including run rate analysis
- Projected activity growth by service line
- Cash-flow forecast over 6, 12 and 24-month horizons
Area: National priorities
Relevant indicators and measures (quantitative and qualitative):
- For example, indicators relating to:
- quality oversight and improvement
- national planning guidance
- reducing health inequalities
- Greener NHS (net zero) – progress in delivery (see Annex B of the Green Plan guidance for suggested metrics)
- NHS Long Term Workforce Plan commitments
- patient safety
- Sexual Safety Charter
Area: Statutory duties, regulatory ratings, and compliance with regulatory requirements
Relevant indicators and measures (quantitative and qualitative):
- For example:
- Public Sector Equality Duty
- CQC ratings
- meeting ongoing statutory duties plus any trust-specific regulatory requirements such as CQC improvement notices, statutory undertakings
- compliance with 10% social value weighting across contracts
- Violence prevention and reduction standard
Area: Key external developments
Relevant indicators and measures (quantitative and qualitative):
- Locally defined, but may also include:
- nationally set targets and indicators
- local system targets for local population. These should be aligned with provider collaborative, ICB and public health indicators to avoid inconsistency and duplication
- changes and trends in local health needs, how they are addressed and any impact on future workforce (for example, care closer to home and virtual wards)
Area: Compliance and risk
Relevant indicators and measures (quantitative and qualitative):
- Highest rated estates and facilities compliance risks including analysis of service impact of non-compliance and infrastructure failure
- Premises Assurance Model Self-Assessment
II. Quality
Questions for boards:
- Does the trust have, and will keep in place, effective arrangements for the purpose of monitoring and continually improving the quality of healthcare provided to its patients having had regard to relevant NHS England guidance (supported by Care Quality Commission information, its own information on safety intelligence, patterns of complaints, and including any further metrics it chooses to adopt)?
- Are systems in place to monitor patient experience, and are there clear paths to relay safety concerns to the board?
The quality of care provided, and its continued improvement, is a core responsibility of boards. They must be able to identify and act in response to early warning signs of poor-quality care, and where harm has occurred this needs to be understood and addressed. Over the last 15 years, a series of national reviews and programmes have made recommendations to strengthen boards’ visibility of quality, and the reporting of certain types of quality information to the board is also now mandatory.
Staff, patient and service user feedback and insights are vital indicators about the quality of services and care. To improve patient experience and outcomes, boards need a whole systems approach to collecting, analysing, using and learning from feedback for quality improvement. This feedback should cover the care and the physical environment in which services are delivered. Triangulating data from different sources is vital. All trusts have a legal duty to involve the public in their decision-making about NHS services and boards need to be assured this duty has been met.
Area: Experiences of care
Relevant indicators and measures (quantitative and qualitative):
- All providers:
- Triangulating staff experience at ward and site level with patient experience
- Friends and Family Test
- reviewing the patient experience improvement framework
- Patient-Led Assessments of the Care Environment (PLACE) annual appraisals
- national and local patient and carer survey results
- patient reported experience measures
- availability of advocacy, peer advocacy, culturally competent advocacy
- knowledge of how patients are involved in quality improvement and who takes part, for example in patient forums or advisory groups
- local Healthwatch and the insight it gathers on the provider’s services (for example, Enter and View reports)
- Mental health:
- Patient and carers race equalities framework (PCREF)
- Patient and Carer Feedback Mechanism
Area: Mandatory board information Patient Safety Incidents
Relevant indicators and measures (quantitative and qualitative):
- Learning from Deaths (quarterly)
- Perinatal Quality Surveillance mandatory measures
Area: Safety
Relevant indicators and measures (quantitative and qualitative):
- Selected Patient Safety Incident reporting rates and analysis
- Organisations should use the Framework for Measuring and Monitoring Safety where applicable. The choice of metrics will be informed by the services provided and should link clearly to the local Patient Safety Incident Reporting Plan (PSIRP)
- Boards should consider the timeliness of the intelligence they are reviewing, and ensure historical data is balanced with real-time information including direct engagement between board, staff and patients and service users:
- feedback from board walkarounds and safety huddles (visible leadership)
- patient safety partner feedback
- patient safety specialist engagement
- Generic incident and safety related metrics may include:
- whether all national patient safety alerts are actioned by deadline – particularly those issued by the Central Alerting System (CAS)
- duty of candour compliance percentages
- patient safety incident reporting patterns, paying particular attention to changes over time and looking across harm severity, location, services involved, contributory factors and other relevant information
- patient safety incident investigation and other learning response action implementation and the impact on service safety
- staff survey safety culture metrics
- Relevant outcome metrics linked to safety of care should be used to identify trends which would in turn trigger more thematic reviews
- Mental health providers may wish to consider metrics such as patient self-harm; all forms of Restrictive Practice (including Long Term Segregation); sexual safety incidents; homicides and attempted homicides; crisis response times; up to date risk assessments. This must include reporting against the requirements set out in the Mental Health Units (Use of Force) Act
- Ambulance providers may wish to consider metrics such as:
- quality alerts where partner organisations have raised a concern
- care provided to patients experiencing a cardiac arrest, ST elevation myocardial infarction (STEMI) or stroke – for example call to hospital arrival mean
- Acute and community providers may wish to consider metrics related to:
- healthcare associated infections (HCAI)
- falls
- pressure ulcers
- hospital associated venous thromboembolism (VTE)
- Anti-microbial resistance (AMR)
- medication optimisation and administration
- maternity outcomes
- implementation of physiological scoring and appropriate response
- post-operative outcomes
- readmission rates, for example, within 7 days or 30 days
- unplanned activity, for example, return to theatre, out of hours operating, unplanned admission to ITU
- missed clinical review / ambulance had to be called
- missed therapy or time sensitive medication
Area: Mortality
Relevant indicators and measures (quantitative and qualitative):
- For all trusts:
- Summary Hospital-level Mortality Indicator (SHMI)
- selected standardised mortality rates by specialty, division or pathway as appropriate.
- Ambulance trusts may wish to split mortality into key pathways, for example, cardiac arrest survival rates. As ambulance trusts cover a large geography, boards may wish to consider whether there is unwarranted variation in quality metrics between different ICBs.
- Mental health, learning disability and autism, and community trusts will want to consider:
- premature mortality for the populations they serve
- suicide prevention data including inpatient suicides
- compliance with Learning from lives and deaths – People with a learning disability and autistic people (LeDeR)
- Mortality reporting should draw on and triangulate data from several other sources:
- Medical Examiners intelligence
- Coroners’ Regulation 28 Reports
- mortality related outliers noted in audits, reviews and national programmes
- patient safety incident records where the incident is thought to have contributed to the death, and the subsequent investigation report
- insights from investigations into patient perpetrated homicides
- For trusts operating mortuaries: HTA Reportable Incidents (HTARIs) – incidents which must be reported to the Human Tissue Authority, rather than being captured through the Learn from patient safety events (LFPSE) service.
Area: Infection prevention and control (IPC)
Relevant indicators and measures (quantitative and qualitative):
- Number of healthcare associated infections (HCAI) (for example per 1000 bed days or expressed as total numbers) split out by:
- MRSA
- C.diff
- E Coli
- MSSA
- other gram-negative infections
- nosocomial Covid – relevance to be determined locally
- Ambulance trusts may wish to focus on IPC process measures such as:
- hand hygiene compliance rates
- deep clean compliance
Area: Safeguarding
Relevant indicators and measures (quantitative and qualitative):
- Number of safeguarding referrals subject to:
- CPIS alerts
- Prevent
- Female Genital Mutilation
- Initial and Review
- Health Assessments for Looked After Children
- Child Death Reviews
- Domestic Homicide Reviews
- Safeguarding Adult Reviews
- Deprivation of Liberty Safeguards.
- Percentage of safeguarding training compliance, as per the Royal College intercollegiate competencies and standards for child and adult safeguarding.
- Providers of mental health, learning disability and autism care will want to pay specific attention to safeguarding referrals for all people placed in a hospital setting.
Area: CQC
Relevant indicators and measures (quantitative and qualitative):
- Ratings, regulatory breaches and other activity, including CQC Well Led Rating and findings from CQC surveys (for example, UEC, maternity, adult inpatient, community mental health).
Area: Audits and independent reviews
Relevant indicators and measures (quantitative and qualitative):
- CQC red flags
- Internally commissioned reviews and audits (for example Cancer Patient Experience Survey)
- Externally commissioned reviews and audits, for example:
- any outliers identified through national clinical audits e.g. MBRRACE, NNAP
- National patient safety alerts and reporting
- Health Services Safety Investigations Body
- Maternity and Newborn Safety Investigations programme
- Coroner Regulation 28 notices
- Parliamentary and Health Service Ombudsman complaints and reports
- Medical examiner intelligence
Area: Staff indicators on quality (also covered under People below)
Relevant indicators and measures (quantitative and qualitative):
- Staff survey feedback – including:
- staff engagement
- staff confidence and security in reporting unsafe clinical practice
- violence prevention and reduction performance
- staff reporting unwanted behaviour of a sexual nature
- Staff turnover rate and staff who leave within 12 months of starting – all staff groups (including nurses, midwives, medical and dental, allied health professionals, operational and administrative staff)
- Skill mix of registered to support staff
- Safe staffing levels – red flags and themes in red flags
- Whistleblowing alerts; Freedom to Speak Up – bullying and harassment cases reported to FTSU Guardian per 1,000 whole time equivalent (WTE); percentage of FTSU concerns that have resulted in change
- National Education and Training Survey (NETS) feedback
- Level of quality voice from clinical leaders and people using services at board level, action and improvement plans to mitigate risks and improve services and evidence of their sustainability
- Quality improvement activity – percentage of staff trained leading QI projects; percentage of local improvement projects scaled up; percentage of projects co-produced (staff, service users, carers) based on what matters to people in experiences of care; evidence of QI activity based on safety and other quality intelligence (for example, linked to PSIRF)
- Percentage of staff completing ‘Essentials of Patient Safety, Level 1’ online training
- Percentage of staff completing the ‘Understanding sexual misconduct in the workplace’ training
Area: Mixed sex accommodation breaches
Relevant indicators and measures (quantitative and qualitative):
- Total number of unjustified breaches in the reporting period
Area: Complaints, concerns and compliments
Relevant indicators and measures (quantitative and qualitative):
- Number of PALS concerns received and resolved, and number of complaints received
- Response time for complaints
- Complaints referred to the Parliamentary and Health Service Ombudsman
- Re-opened complaints
- Deeper analysis of complaints:
- themes
- follow-up action
- how learning has been incorporated
- tone and content of responses (experiences of people making a complaint)
- Compliments
III. People
Questions for boards:
- Is staff feedback used to improve the quality of care provided by the trust?
- Do staff have the relevant skills and capacity to undertake their roles, with training and development programmes in place at all levels?
- Are staff able to express concerns in an open and constructive environment?
- Are staff metrics used to improve productivity, staff satisfaction and patient care?
Boards need to:
- listen to their staff and make the best use of their skills and experience
- use information to inform strategic decisions on how to improve employee experience, to retain and attract staff and ensure the trust’s services are sustainable
- gain assurance that staff have the relevant skills and capacity to undertake their roles
- ensure workforce inequalities are identified and addressed
- ensure succession planning is carried out
Board members should routinely consider employee experience, including the health and wellbeing of staff, ensure the working environment is safe and secure, and proactively manage and mitigate risks. They should also listen to and support staff to be appropriately empowered to be advocates for themselves, their colleagues, patients and service users.
Area: Headcount, salary bill, skill mix Total headcount
Relevant indicators and measures (quantitative and qualitative):
- Total WTE
- Gross salary bill
- Staff mix (including volunteers)
- Nurse Staffing Fill rate
- Deployments
- Effective workforce
- Proportion of Apprenticeship Levy spent
Area: Use of agency and bank
Relevant indicators and measures (quantitative and qualitative):
- Total cost by month and area (including off framework and above cap)
- Demographic mix of bank staff
Area: Staff health and wellbeing
Relevant indicators and measures (quantitative and qualitative):
- Percentage sickness absence, presenteeism (percentage reporting coming to work while unwell in staff survey)
- Long term sickness absence
- Average number of sick days per full time equivalent (FTE)
- Reason for sickness (themes)
- Perceived manager and organisational support for staff wellbeing (NHS staff survey)
- Whether staff felt unwell because of work-related stress (NHS staff survey)
Area: Vacancy Number of vacancies by area
Relevant indicators and measures (quantitative and qualitative):
- Vacancy rate (ratio of vacancies to all posts)
- Staff turnover rate
Area: Staff turnover and leaver rates
Relevant indicators and measures (quantitative and qualitative):
- Number of leavers by staff group, ward site, organisation benchmarked vs entire NHS
- Common themes on why people are leaving the organisation (including those leaving within 12 months of joining)
Area: Diversity
Relevant indicators and measures (quantitative and qualitative):
- NHS Equality Delivery System (EDS)
- NHS Workforce Race Equality Standard (WRES) data and responses to returns
- NHS Workforce Disability Equality Standard (WDES) data and responses to returns
- Percentage of staff in senior positions that are Black and Minority Ethnic (BME) or have a disability
- Gender Pay Gap reporting
Area: Staff speaking up (FTSU)
Relevant indicators and measures (quantitative and qualitative):
- Number of Freedom To Speak Up (FTSU) Guardians (including number in senior bands)
- Number of FTSU reports
- Number of FTSU reports that have led to actions being delivered and changes implemented
- Deeper analysis of FTSU data:
- percentage of reports made anonymously vs named
- themes from FTSU and specific divisions and departments they relate to
- time taken to respond to FTSU: initial response and to conclusion
- details of learning and improvement from speaking up
- percentage of staff that have completed the 3 FTSU training modules (if included on MaST)
- percentage of people that would speak up again
- details of actions taken to understand and reduce barriers to speaking up
- analysis of the protected characteristics of those speaking up
- time taken to resolve employee relations issues
Area: Staff engagement
Relevant indicators and measures (quantitative and qualitative):
- NHS Staff Survey results for staff engagement theme and sub-themes of involvement, advocacy and motivation
- National Quarterly Pulse Survey (NQPS) results (staff engagement theme and sub-themes as above)
Area: Employee experience
Relevant indicators and measures (quantitative and qualitative):
- People Promise scores and sub-scores
- Staff engagement and morale theme and sub-theme scores
- Triangulation of staff experience and ward and site level with patient experience
Area: Lived experience workforce
Relevant indicators and measures (quantitative and qualitative):
- Mental health, learning disability and autism trusts may want to consider the number of lived experience staff who are employed to provide peer support, peer advocacy and other roles.
Area: Grievances
Relevant indicators and measures (quantitative and qualitative):
- Internal complaints / staff grievances / disciplinaries open
- Employment tribunal claims
Area: Staff screening
Relevant indicators and measures (quantitative and qualitative):
- NHS Employment check standards: Staff recruited need to have the relevant pre-recruitment checks carried out:
- identity
- criminal record
- work health assessment
- professional registration and qualifications
- right to work
- employment history and reference(s)
IV. Access and targets
Questions for boards:
- Are plans in place to improve performance against the relevant access and waiting times standards?
- Is the trust able to identify and address inequalities in access and waiting times to NHS services across its patients?
- Have appropriate population health targets been agreed with the Integrated Care Board?
Trust boards will need to track how their organisations are delivering against national commitments. In general, this performance should be viewed in conjunction with individual partner providers in the system and across the ICB itself. Board members should look at trends using Statistical Process Control and other appropriate tools to identify situations where there might be significant negative or positive movements. Analysing data with a particular focus on ethnicity and deprivation is key to reducing health inequalities.
This information is likely to change. Trusts should always refer to the latest updates to the relevant NHS England guidance on the specific NHS indicators and targets by which it will be assessed nationally.
Area: Community services
Relevant indicators and measures (quantitative and qualitative) :
- Community service waiting times
- Proportion of Category 4 calls resulting in ambulance response
Area: Urgent and emergency care
Relevant indicators and measures (quantitative and qualitative):
- A&E waiting times, percentage of patients seen within 4 hours
- Category 2 ambulance response times
- 999 call answer mean time
- Number of emergency admissions for ambulatory care sensitive conditions
- Number of emergency admissions for people with multiple long-term conditions
Area: Elective care
Relevant indicators and measures (quantitative and qualitative) :
- Number of long waits (as defined nationally)
- Delivery of local system specific activity targets
- Proportion of outpatient appointments as first or follow-up appointments
- Ambition: Patient experience of choice at referral
- Under 18-year-old elective activity rate compared to baseline
Area: Cancer
Relevant indicators and measures (quantitative and qualitative):
- Performance against national wait standard
- Performance against national diagnosis standard
- Ambition: Proportion of diagnosis at an early stage (1 and 2)
Area: Diagnostics
Relevant indicators and measures (quantitative and qualitative):
- Diagnostic 6-week performance
Area: Maternity
Relevant indicators and measures (quantitative and qualitative):
- Midwifery fill rate in line with Birthrate plus
Area: Mental health (to consider as appropriate as not all of these will apply to all mental health providers)
Relevant indicators and measures (quantitative and qualitative):
- Patient flow performance
- Out of area placement reduction performance
- Number of people accessing:
- adult community mental health services
- perinatal health services
- children and young people’s mental health services
- Number of adults and older people accessing and completing a course of NHS Talking Therapies
- Percentage of people with a severe mental illness receiving a full annual physical health check
- ICB-wide Dementia Diagnosis Rate performance
- Number of mental health patients spending less than 12 hours in an emergency department
Area: People with a learning disability and autistic people
Relevant indicators and measures (quantitative and qualitative):
- Proportion of people aged 14 and over with a learning disability on the GP register receiving a full annual physical health check
- Number of people with a learning disability and number of autistic people in mental health inpatient care
Area: Prevention and health inequalities
Relevant indicators and measures (quantitative and qualitative):
- Percentage of patients with hypertension treated
- Percentage of patients with a CVD risk score greater than 20% on lipid lowering therapies
- Myocardial infarction admission rate deprivation gap
- Proportion of frontline healthcare workers who have had Covid-19 and influenza vaccinations
Area: Workforce
Relevant indicators and measures (quantitative and qualitative):
- Number of clinical placements and apprenticeship pathways provided
V. Productivity
Question for boards:
- Are plans in place to deliver productivity improvements as referenced in, for example, the Model Health System, this guide and other relevant guidance?
In recent years, tools like Getting it Right First Time (GIRFT) and the Model Health System have shone a light on how data can help trusts provide a more effective and consistent quality of care for patients and service users. These tools can also identify opportunities to improve operational productivity and efficiency and reduce unwarranted variation. There are a range of measures – for each type of trust – that boards can look at to assure themselves they are delivering health and care services and using assets as effectively as possible.
Productivity considerations
Consider productivity in terms of how the outputs of healthcare are growing in comparison to the inputs required, or put another way, the total inputs required to get each unit of output. These are typically:
- outputs – the healthcare services provided, such as emergency admissions, outpatient appointments and treatments from waiting lists
- inputs – the resources required to deliver healthcare services, including the number of staff (including bank and agency), direct and indirect staff costs and time, capital required, and goods and services used, such as medicines and equipment
Productivity and efficiency denote different things. Productivity is focused on the quantity of outputs and achieving a greater number of these with the inputs (resources) available. Efficiency measures the quality of the inputs and specifically how well the inputs (resources) are being used, so requiring fewer resources (such as time or money) to achieve the same or greater number of or quality of outputs.
Productivity improvements can be supported by robust demand and capacity modelling, to ensure affordable workforce growth to meet demand, and connected to operational planning (see access and targets section). Boards should refer to the Model Health System for core productivity and efficiency metrics in conjunction with local intelligence to assess the key drivers of productivity, and benchmark performance with peers. Provider collaboratives may also choose to develop their own metrics to measure productivity.
More information to support trusts to assess their productivity is on the Model Health System.
Area: Headline productivity
Relevant indicators and measures:
- Implied Productivity Growth (year-to-date compared to 2019/20)(percentage): Implied Productivity Growth is calculated by comparing output growth (activity) to input growth (based on expenditure costs) against a baseline period. The measure examines a trust’s current year-to-date activity and costs to the same period in 2019/20
Area: Operational and clinical productivity
Relevant indicators and measures:
- Average Length of Stay (ALOS) – non-elective (1+ days): The average length of stay for all non-elective admissions (spells) where the patient has stayed in hospital for at least one night
- Bed occupancy classed as clinically ready for discharge from hospital (percentage): The proportion of acute patients who do not meet the criteria to reside, and therefore are clinically ready for discharge, but continue to reside in acute hospitals against the total occupied beds
- Capped theatre utilisation (percentage): Total touch time within the start and end time of the planned session, in proportion to planned theatre session/list duration
- Day case rates (percentage): Proportion of activity carried out as a day case compared to an overnight admission for British Association of Day Case Surgery procedures
Area: Workforce productivity
Relevant indicators and measures:
- Implied workforce productivity growth (year-to-date compared to 2019/20): This is calculated by comparing output growth (activity) to input growth (workforce) against a baseline period. The measure examines a trust’s current year-to-date activity and costs to the same period in 2019/20
- Outpatient per consultant WTE (whole-time equivalent): Number of outpatient attendances per clinical WTEs (nursing plus consultants)
- Elective admissions per clinical WTE: Number of elective admissions per clinical WTEs (nursing plus consultants)
- Non-elective admissions per clinical WTE: Number of non-elective admissions per consultant WTEs
- A&E attendances (Type 1 and 2) per emergency medicine consultant: Number of A&E attendances per (Type 1 and 2) per emergency medicine consultant
- Care hours per patient day: Care hours per patient day (CHPPD) total nursing and midwifery staff
Area: Workforce drivers
Relevant indicators and measures:
- Overall temporary staff spend as a percentage of total spend: Spend on bank and agency staff as a proportion of total staff spend
- Registered nurses: Sickness absence rate (percentage): Registered nurses who are absent because of sickness
- Percentage of registered medical and dental staff who are absent because of sickness (percentage): Medical and dental sickness absence rate
- All staff: NHS turnover rate (percentage): Staff leaving the organisation – retirement or new job – out of total staff numbers
- Non-pay efficiency Non-pay Efficiency – Medicines (cost): National medicines optimisation opportunity size
- Non-pay Efficiency – Corporate Services (cost): Cost of running corporate services per £100 million turnover
- Non-Pay Efficiency – Estates and Facilities: (£ per m2) The total estates and facilities running costs to the total occupied floor area
VI. Finance
Questions for boards:
- Does the trust have a robust financial governance framework and appropriate contract management arrangements?
- Is financial risk managed effectively, and financial considerations (such as efficiency programmes) do not adversely affect patient care and outcomes?
- Does the trust actively engage with system partners regarding the optimal use of NHS resources and supports the system’s delivery of its planned financial out-turn?
When planning services, improvements, investments or efficiency changes, boards must understand the impact on workforce, quality and financial sustainability, including for the wider health and care system.
Finance should not be considered in a silo – it is a significant factor in how the trust prioritises resources and the impact this has on the services provided for patients and service users, and the wider finances of the system. In addition to the data below, boards should be mindful of other information, such as internal and external audit reports and implications these will have for financial controls.
Area: Organisational performance
- income and expenditure
- cash flow Performance against budget (including filled posts versus total funded establishment)
Relevant indicators and measures (quantitative and qualitative):
- Financial stability (variation from breakeven)
- Financial efficiency
- Variance analysis to planned financial efficiency from current position
- Trust cash flow forecasts and analysis
Area: Business unit information
Relevant indicators and measures (quantitative and qualitative):
- Cash flow
- Gross margin
Area: Debtors and payments to suppliers
Relevant indicators and measures (quantitative and qualitative):
- Value of 30, 60 and 90-day debtors
- Trust compliance with Better Payment Practice Code (BPPC)
Area: Liquidity
Relevant indicators and measures (quantitative and qualitative):
- How many days’ operating cash requirement the trust has available
Area: Interest cover
Relevant indicators and measures (quantitative and qualitative):
- How much headroom the trust has over fixed interest payments (including PFI unitary payments)
Area: Financial run-rate
Relevant indicators and measures (quantitative and qualitative):
- Current financial performance versus plan
Area: Risk and mitigations
Relevant indicators and measures (quantitative and qualitative):
- Risks and mitigations to the reported financial position
Area: Phasing of efficiency schemes
Relevant indicators and measures (quantitative and qualitative):
- Analysis on whether efficiency schemes are phased realistically
Area: Capital
Relevant indicators and measures (quantitative and qualitative):
- High quality and regular reporting on progress toward delivery of capital plan
- Main risk areas for capital projects with associated mitigations and timings
- Variance analysis showing planned capital spend compared to capital allocation per system (CDEL) allowance
Area: System financial performance
Relevant indicators and measures (quantitative and qualitative):
- High quality and regular reporting on:
- the organisation’s contribution to system breakeven
- current system financial projections vs ICB’s Joint Forward Plan
- For mental health trusts this should also include analysis of the system delivery of the Mental Health Investment Standard.
Area: Productivity
Relevant indicators and measures (quantitative and qualitative):
- Productivity trends per WTE
- Cost per weighted activity unit (WAU) outliers (by specialty and staff group [clinical and non-clinical staff])
Area: Estates and facilities management running costs
Relevant indicators and measures (quantitative and qualitative):
- Benchmarked to other organisations
- Analysis of achievable efficiencies
- Annual Estates Return Information Collection (ERIC) returns

