Sir James Mackey, Accounting Officer
21 October 2025
The accountability report sets out how NHS England meets key accountability requirements to Parliament and is comprised of three key sections:
The corporate governance report sets out how the organisation was governed during 2024/25, including membership and organisation of our governance structures and how they support achievement of our objectives. The report includes:
- directors’ report
- statement of accounting officer’s responsibility
- governance statement
The remuneration and staff report sets out our remuneration policies for executive and non-executive directors (NEDs) and how these policies have been implemented for the reporting period, including salary information and pension liabilities. The report provides further detail on remuneration and staff and starts from page 86.
The parliamentary accountability and audit report (from page 113) brings together key information to support accountability to Parliament, including a summary of fees and charges, contingent liabilities and the Certificate and Report of the Comptroller and Auditor General to the Houses of Parliament.
Accountability to Parliament and the public
During 2024/25, NHS England has continued to work closely with the NAO in their work to test whether public bodies are delivering value for money. During this period, the Chief Executive and other senior leaders gave evidence to Public Accounts Committee (PAC) hearings on Addressing the risks of antimicrobial resistance, the DHSC Annual Report and Accounts 2023/24, Fixing NHS dentistry and NHS financial sustainability.
In 2024/25, the NAO published reports on NHS England’s management of elective care transformation programmes, Antimicrobial resistance, NHS dental recovery plan, Progress in preventing CVD, and NHS financial management and sustainability 2024.
This resulted in 34 PAC recommendations involving NHS England, of which 29 were accepted, and 19 NAO recommendations of which 17 were accepted.
The 10-Year Health Plan sets out how the government will deliver an NHS fit for the future and addresses many of these recommendations through the three big shifts (hospital-centred to community-based care, from analogue to digital, and from sickness to prevention), a rigorous approach to financial discipline and shift to longer-term planning, and a relentless focus on delivering value-based healthcare.
In response to the PACs recommendations, NHS England has:
- continued to support the NHS to recover lost productivity caused by the COVID-19 pandemic through increasing clinical and operational productivity training and maximising the use of digital innovations to improve the efficiency of services (Government Response to the Committee of Public Accounts from Session 2024-25)
- continued work to improve access to NHS dental care through working with ICBs to deliver 700,000 extra urgent dental appointments per year from 2025/26 onwards
- continued to implement targeted recruitment and retention initiatives for areas struggling to recruit NHS dentists and developed changes to the current dental contract focussing on supporting access for higher needs patients and encouraging increased use of preventative dentistry (Government Response to the Committee of Public Accounts on the Eighteenth to the Twenty-Second reports from Session 2024-25)
Bi-annual updates are provided to the Government on all open PAC recommendations via HMT’s Treasury Minute progress reports.
Corporate governance report
Directors’ report
The Board
The key responsibility of the Board is to provide strategic leadership to the organisation, including:
- setting the overall direction of NHS England, within the context of the NHS Mandate from government
- approving the business plan, which is designed to support achievement of our strategic objectives and monitor our performance against it
- holding the NHS Executive to account for this performance and for the proper running of the organisation, including operating in accordance with legal and government requirements
- determining which decisions, it will make and which it will delegate to the executive or committee or sub-committee, via the Scheme of Delegation
- ensuring high standards of corporate governance and personal conduct
- monitoring performance against core financial and operational objectives
- providing effective financial stewardship
- promoting effective dialogue between NHS England, government departments, partners, ICSs, providers of healthcare and the communities served by the NHS.
In accordance with paragraph 2 of Schedule A1 to the 2006 Act (also set out in section 4.1 of the Standing Orders), the Board comprises the chair, ten NEDs and five executive directors including the chief executive.
Appointments
The chair and NEDs are appointed by the Secretary of State for Health and Social Care and executive members of the NHS England Board are appointed by the chair and NEDs.
The appointment of the chief executive is subject to the Secretary of State for Health and Social Care’s consent. The Board also approved the appointment of two associate NEDs in April 2024.
Board members
Directors who served on the NHS England Board during the year are listed in the table below, along with their attendance (Biographical details may be viewed on our website).
| Members | Role | Term ends | Number of eligible Board meetings attended |
|---|---|---|---|
| Richard Meddings[1] | Chair | 31 March 2025 | 6/6 |
| Sir Andrew Morris[2] | Deputy Chair | 24 September 2025 | 6/6 |
| Mike Coupe[3] | Non-Executive Director | 31 July 2025 | 5/6 |
| Jeremy Townsend | Non-Executive Director | 30 September 2026 | 4/6 |
| Professor the Baroness Mary Watkins | Non-Executive Director | 31 July 2025 | 5/6 |
| Professor Sir Mark Walport | Non-Executive Director | 24 June 2025 | 5/6 |
| Professor Sir Simon Wessely | Non-Executive Director | 31 July 2025 | 5/6 |
| Professor Sir Robert Lechler | Non-Executive Director | 18 February 2027 | 6/6 |
| Jane Ellison | Non-Executive Director | 31 July 2025 | 6/6 |
| Mark Bailie | Non-Executive Director | 18 February 2027 | 4/6 |
| Suresh Viswanathan | Associate Non-Executive Director | 1 October 2025 | 5/6 |
| Amanda Pritchard | Chief Executive Officer | 31 March 2025 | 6/6 |
| Julian Kelly | Chief Financial Officer | 31 March 2025 | 6/6 |
| Duncan Burton[4] | Chief Nursing Officer for England | 5/5 | |
| Professor Sir Stephen Powis | National Medical Director | 20 July 2025 | 5/6 |
| Dame Emily Lawson | Chief Operating Officer | 31 March 2025 | 5/6 |
[1] Richard Meddings’s term as Chair ended on the 31 March 2025.
[2] Sir Andrew Morris’s term as non-executive director was extended for six months, from 25 March to 24 September 2025.
[3] Mike Coupe, Professor the Baroness Watkins, Professor Sir Mark Walport, Professor Sir Simon Wessely and Jane Ellison resigned and their non-executive directorships ended in July 2025.
[4] Duncan Burton was appointed as Chief Nursing Officer for England on the 25 July 2024.
| Former members | Role | End date |
|---|---|---|
| Sir David Behan | Non-Executive Director | 31 August 2024 |
| Professor Dame Helen Stokes-Lampard[1] | Non-Executive Director | 14 October 2024 |
| Wol Kolade[2] | Deputy Chair | 24 March 2025 |
| Tanuj Kapilashrami[3] | Associate Non-Executive Director | 23 March 2025 |
| Dame Ruth May | Chief Nursing Officer | 24 July 2024 |
[1] Professor Dame Helen Stokes-Lampard resigned and her non-executive directorship ended on 14 October 2024.
[2] Wol Kolade’s term as non-executive director ended on the 24 March 2025.
[3] Tanuj Kapilashrami resigned and her term ended on 23 March 2025.
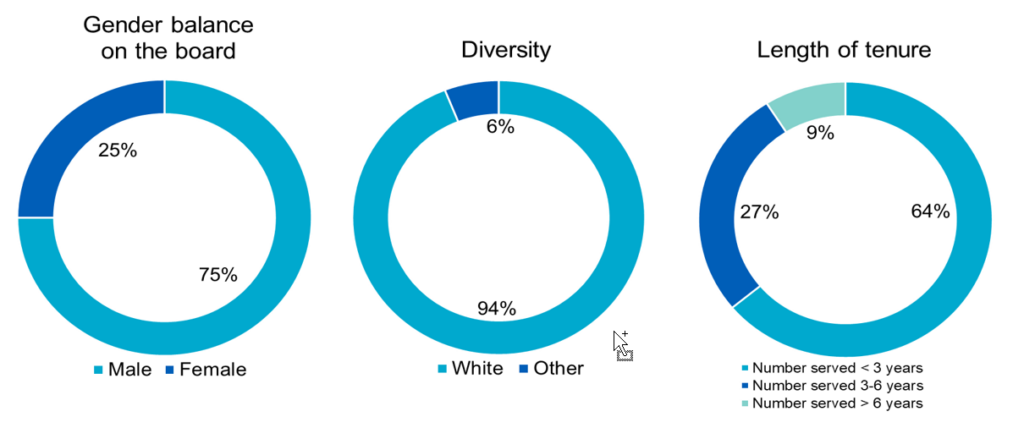
Board diversity
The charts below show the composition of the Board members by gender, diversity, and tenure as of 31 March 2025.
The governance structure
An overview of the Board governance framework is shown on the next page and individual Board committee reports can be found from page 55 to 64. A report detailing the business considered by the board committees is provided for each Board meeting.
Board activity and administration
There were six NHS England Board meetings during the year, each including a public and private session. The option for members of the public to attend public sessions in person was available throughout the year. Public sessions were live video streamed and published on our website along with the agenda, papers, and minutes.
In addition to the six formal meetings, the Board held two strategy sessions and various subject-specific workshops and deep dives.
Throughout the year, the Board focused on ensuring the integrity and effectiveness of NHS England’s strategic, performance, and governance functions. In relation to strategy, it reviewed transformation, innovation and research, strategic priorities for mental health, the future operating model for primary care, transformation of the frailty pathway, the New Hospital Programme, and the NHS productivity programme. It also considered the long-term infrastructure strategy project, the revised NHS Performance and Assessment Framework, and the NHS LTWP.
In terms of performance, the Board received regular updates on operational and financial performance, winter planning and preparedness, and the delivery plan for recovering access to primary care. It reviewed the annual report on healthcare inequalities and the NHS Race and Health Observatory, the learning disability and autism programme, work on the attention deficit hyperactivity disorder pathway, and progress on the Maternity and Neonatal Three-Year Delivery plan.
In relation to governance and risk, the Board conducted the annual board effectiveness review for 2023/24, assessed risk appetite, reviewed delegation of commissioning functions to ICBs, and ensured robust oversight of NHS England’s operations.
Review of Board effectiveness and performance evaluation
In July 2024, the Board received the findings of the 2023/24 NHS England Board governance effectiveness review and endorsed the recommendations and actions. The review identified several areas that had improved, including the operation of the Board committees. Recommendations for improvement were made in relation to duplication of discussions across committees and groups, the role and responsibilities of the Quality Committee including the interaction with other quality fora, and the timely distribution of papers. The review recommendations and actions were implemented during 2024/25.
Events after the reporting period
In addition to the appointment of Dr. Penny Dash as Chair and Sir James Mackey as Chief Executive Officer, several new members joined the executive team on 1 April 2025.
Further executive and non-executive director appointments were made after the reporting period, and our website is updated regularly to reflect these appointments.
Further detail on the changes and mergers for ICBs can be found within Note 20.
Board committees
Audit and Risk Assurance Committee (ARAC)
|
Role |
The committee’s primary role is to provide assurance to the Board about the integrity of NHS England’s financial statements and the comprehensiveness, reliability and integrity of its internal control, risk management and governance processes. |
|
Frequency |
The committee met five times in the financial year. |
|
Membership |
The committee is made up of five NEDs and one non-voting member. Additional attendees are invited to meetings to assist with committee business. The committee can meet with the internal and external auditors without management when required, and the auditors have direct access to the Board Chair and committee chair to support independence. |
|
Principal activities during the year |
ARAC approved the internal audit plan and reviewed regular progress reports, including the annual Head of Internal Audit Opinion. The committee evaluated risk management governance and reviewed NHS England’s principal risks. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Jeremy Townsend (Chair) |
5/5 |
Non-Executive Director |
|
Wol Kolade |
4/5 |
Non-Executive Director |
|
Mark Bailie |
4/5 |
Non-Executive Director |
|
Mike Coupe |
4/5 |
Non-Executive Director |
|
Jane Ellison |
4/5 |
Non-Executive Director |
|
Gerry Murphy |
2/2 |
Non-executive Chair of DHSC’s Audit Committee (non-voting member) |
|
Richard Douglas |
3/3 |
Non-executive Chair of DHSC’s Audit Committee (non-voting member) |
Nominations Committee
|
Role |
The committee oversees succession planning for the NHS England Board and senior management, board composition and board evaluation. |
|
Frequency |
The committee met three times in the financial year. |
|
Membership |
The committee is made up of the Chair of NHS England, three NEDS and the CEO. The Director of Human Resources and Organisational Development is invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The committee considered NHS England Board and board committee composition, recommending changes for Board approval where necessary, received updates on NED recruitment, and reviewed and advised on succession plans for national directors. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Richard Meddings |
3/3 |
Chair of NHS England |
|
Sir Andrew Morris |
3/3 |
Deputy Chair, NHS England |
|
Wol Kolade |
3/3 |
Deputy Chair, NHS England |
|
Michael Coupe |
3/3 |
Non-Executive Director |
|
Amanda Pritchard |
3/3 |
Chief Executive Officer |
Data, Digital and Technology Committee (DDaTC)
|
Role | The role of the committee is to consider and make recommendations on the digital and technology strategy, including cyber strategy, to the Board and oversee its implementation. It advises on the development of data and technology architecture and assures the Board on the discharge of data functions, including compliance with statutory guidance on protecting patient data. |
|
Frequency |
The committee met five times in the financial year. |
|
Membership |
The committee is made up of four NEDs, the Chair of NHS England, one Associate NED and three non-executive members. Additional attendees are routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The committee supported a wide range of strategic initiatives, including the rollout of the FDP, strengthening technical architecture, and efforts to address digital and data challenges in primary care. The committee endorsed the Tech and Digitally Enabled Productivity Plan and contributed to shaping the NHS 10-Year Health Plan through development of the data, digital and technology vision and roadmap. It also reviewed the resilience plan and data, digital and technology operating model aimed at enhancing system sustainability and robustness. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Mark Bailie (Chair) |
5/5 |
Non-Executive Director |
|
Richard Meddings |
5/5 |
Chair of NHS England |
|
Mark Walport |
3/5 |
Non-Executive Director |
|
Michael Coupe |
4/5 |
Non-Executive Director |
|
Robert Lechler |
3/5 |
Non-Executive Director |
|
Suresh Viswanathan |
3/5 |
Associate Non-Executive Director |
|
Steve Woodford |
5/5 |
Non-Executive Member |
|
Daniel Benton |
5/5 |
Non-Executive Member |
|
John Noble |
1/1 |
Non-Executive Member |
|
Jamie Saunders |
4/4 |
Non-Executive Member |
Quality Committee
|
Role |
The primary role of the committee is to support the Board in ensuring that areas concerning patient safety, the quality of care provided to patients and patient experience are continuing to improve and develop to meet the needs of patients in England. |
|
Frequency |
The committee met five times in the financial year. |
|
Membership |
The committee is made up of the Chair of NHS England, four NEDs, six National Directors and up to four Patient and Public Voice (PPV) members. Additional attendees are routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The Quality Committee oversaw the development of an Integrated Quality Report and contributed to the development of an NHS Quality Strategy. The committee received updates on issues and challenges in a number of clinical programmes including; Maternity and Neonatal, Children and Young People, Palliative and End of Life care, Stroke, and Learning Disability and Autism. The committee also reviewed all risks relating to quality of care and patient safety on the risk register, ensuring appropriate mitigations are in place. Members reviewed and approved the updated policy on Working with People and Communities, ahead of Board approval. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Professor Sir Robert Lechler (Chair) |
4/5 |
Non-Executive Director |
|
Professor Sir Simon Wessely (Interim Chair) |
3/5 |
Non-Executive Director |
|
Richard Meddings |
5/5 |
NHS England Chair |
|
Sir David Behan |
1/2 |
Non-Executive Director |
|
Professor the Baroness Mary Watkins (Professor the Baroness Mary Watkins became a member of the Quality Committee in March 2025) |
1/1 |
Non-Executive Director |
|
Dr Aidan Fowler |
5/5 |
National Director of Patient Safety |
|
Emily Lawson (Sarah Jane Marsh (National Director of UEC and Deputy Chief Operating Officer) attended the Quality Committee on behalf of the Chief Operating Officer) |
4/5 |
Chief Operating Officer |
|
Sir Andrew Morris |
3/5 |
Non-Executive Director |
|
Dame Ruth May (Dame Ruth May was a member until 24 July 2024) |
0/2 |
Chief Nursing Officer |
|
Duncan Burton (Duncan Burton was appointed a member on the 25 July 2024) |
2/3 |
Chief Nursing Officer for England |
|
Professor Sir Stephen Powis |
4/5 |
National Medical Director |
|
Amanda Doyle |
3/5 |
National Director for Primary Care and Community Services |
|
Charlotte McArdle |
2/4 |
Deputy Chief Nursing Officer |
|
Andrea Lewis (Andrea Lewis was appointed a member in March 2025) |
1/1 |
Interim Deputy Chief Nursing Officer |
|
Patient and Public Voice members |
4/4 |
|
People and Remuneration Committee
|
Role |
The committee supports the Board in ensuring that NHS England as an employer has appropriate people and workforce strategies in place and is delivering these, provides assurance to the Board on NHS England’s workforce risks and oversees strategic people management and organisational development. It also oversees and determines appointment, and remuneration matters in respect of NHS England employees, ICBs and NHS trusts on behalf of the Board. The exercise of these duties and powers is supported by the Executive HR Group, Appointment Termination Committee and Regional Appointment and Approval Committees, which were established by the People and Remuneration Committee. |
|
Frequency |
The committee met five times in the financial year. |
|
Membership |
The committee is made up of four NEDs and the Chair of NHS England. Additional attendees are routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The committee oversaw significant activity across the People Programme, with a focus on progressing delivery priorities for the newly formed NHS England. This included improving HR services and driving organisational development, culture, and behaviours. The committee reviewed progress on the implementation of the Equality, Diversity and Inclusion Improvement Plan, including work on social mobility and publication of the 2023 Gender Pay Gap report. It also considered updates on staff survey outcomes and internal FTSU activity. Key decisions were made on the revised Appointment Policy for NHS Chairs and NEDs, the proposed pay award for executive and senior medical leaders, and the Board Member Appraisal Framework. The committee continued to oversee Chair and NED talent pipelines, succession planning and senior appointments, while receiving regular updates from the Executive HR Group on pay cases, redundancies, and legal matters. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Sir David Behan (Chair) |
2/2 |
Non-Executive Director |
|
Jane Ellison (Chair) (Jane Ellison was appointed as chair of the People and Remuneration Committee in August 2024) |
5/5 |
Non-Executive Director |
|
Richard Meddings |
3/5 |
Chair of NHS England |
|
Sir Andrew Morris |
3/5 |
Non-Executive Director |
|
Professor the Baroness Watkins |
4/5 |
Non-Executive Director |
Workforce, Training and Education Committee
|
Role |
The committee’s role is to have oversight of all functions that ensure the NHS in England has a workforce with the capacity, knowledge, skills, values and behaviours to deliver compassionate, high-quality health and care to the people it serves. The committee’s work plan ensures that the functions above are aligned to delivering the LTWP and vision for the NHS workforce: more people, working differently, in a compassionate and inclusive culture. |
|
Frequency |
The committee met six times in the financial year. |
|
Membership |
The committee is made up of at least five NEDs, one Associate NED, and three non-executive members. Additional attendees are routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The committee oversaw a workforce, training and education delivery plan that ensured the Board’s priorities were informed by the DHSC mandate and the LTWP. It was also assured on delivery of the Workforce, Training & Education (WT&E) delivery plan and of performance across the system against the WT&E priorities for the NHS. Additionally, and in partnership with the ARAC, it considered and provided assurance to the Board on the management of strategic WT&E risks. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Sir David Behan (Chair) |
3/6 |
Non-Executive Director |
|
Sir Andrew Morris (Chair) |
6/6 |
Non-Executive Director |
|
Professor the Baroness Watkins |
5/6 |
Non-Executive Director |
|
Professor Dame Helen Stokes-Lampard |
2/6 |
Non-Executive Director |
|
Professor Sir Mark Walport |
2/6 |
Non-Executive Director |
|
Dr Harpreet Sood |
2/6 |
Non-Executive Member |
|
John Latham |
5/6 |
Non-Executive Member |
|
Professor Andrew George |
5/6 |
Non-Executive Member |
|
Tanuj Kapilashrami |
4/6 |
Non-Executive Member |
The New NHS England Committee
|
Role |
The New NHS England Committee was a time-limited committee, established to provide leadership and strategic oversight of the delivery of the Creating the New NHS England Programme. |
|
Frequency |
The committee met once in the financial year. It was disbanded in May 2024 at the close down of the Creating the New NHS England Programme. |
|
Membership |
The committee was made up of three NEDs, the Chair of NHS England and three national directors. Additional attendees were routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The only meeting of the New NHS England Committee this financial year oversaw the close down of the programme and transfer of remaining activities. The committee also reviewed lessons learned from the programme. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Wol Kolade (Chair) |
1/1 |
Deputy Chair, NHS England |
|
Richard Meddings |
1/1 |
Chair of NHS England |
|
Sir Andrew Morris |
1/1 |
Deputy Chair, NHS England |
|
Sir David Behan |
1/1 |
Non-Executive Director |
|
Amanda Pritchard |
1/1 |
Chief Executive Officer |
|
Julian Kelly |
1/1 |
Chief Financial Officer |
|
Steve Russell |
1/1 |
Chief Delivery Officer |
The New Hospital Programme (NHP) Delivery Committee
|
Role |
The NHP Delivery Committee’s role is to scrutinise, challenge and assure delivery of the NHP on behalf of the Board. |
|
Frequency |
The committee met four times in the financial year. |
|
Membership |
The committee is made up of the Chair of NHS England, two NEDs, three national directors, the Chief Programme Officer, and two independent advisors. Additional attendees are routinely invited to attend meetings to assist with committee business. |
|
Principal activities during the year |
The committee endorsed the NHP agreement, which formalises the relationship between partners (NHP, NHS England, and relevant NHS provider organisations) in the delivery of the NHP Programme. It also received updates on the Hospital 2.0 system, a central programmatic delivery strategy for the NHP, and programme risks and mitigations. |
| Members | Number of eligible meetings attended | Comment |
|---|---|---|
|
Richard Meddings |
4/4 |
Chair, NHS England |
|
Wol Kolade |
4/4 |
Deputy Chair of NHS England |
|
Michael Coupe |
4/4 |
Non-Executive Director |
|
Julian Kelly |
2/4 |
Chief Financial Officer |
|
Amanda Pritchard |
0/4 |
Chief Executive |
|
Jacqueline Rock (Jacqueline Rock left the organisation in December 2024) |
3/3 |
Chief Commercial Officer |
|
Morag Stuart |
4/4 |
Chief Programme Officer, the New Hospital Programme |
|
Independent Advisers |
4/4 |
|
Board disclosures
Functional conflicts
NHS England maintains a policy on conflicts between functions, to comply with its duty under new section 13SB of the National Health Service Act 2006 (inserted by section 34 of the Health and Care Act 2022), to make arrangements to minimise the risk of conflicts between the exercise of the former Monitor regulatory functions and NHS England’s other functions, and to manage any conflicts that arise. The policy contains arrangements for handling individual conflicts (notifiable to the Board Secretariat) and provides for formal escalation to a non-executive panel. The need to mitigate functional conflicts was considered as part of the setup of the Independent Patient Choice and Procurement Panel, where there are conflicts checks at each panel meeting and when panel members are allocated to cases. During 2024/25, the Board Secretariat were notified of no (zero) conflicts.
Register of Board members’ interests
Personal interests held by Board and committee members are managed in accordance with the NHS England Standing Orders and the Standards of Business Conduct policy. The organisation maintains a register of members’ interests to ensure that potential conflicts of interest can be managed appropriately. Board members and executives are also required at the beginning of each Board and committee meeting to declare any personal interest they might have in any business on the agenda and abstain from relevant Board or committee discussions as required. Where potential conflicts arise, they are recorded in the Board and committee minutes along with any appropriate action to address them. A copy of the register of interests is available on our website. Note that this only reflects Board members currently in post.
Details of related party transactions, where NHS England has transacted with other organisations during the year to which a Board or an executive is connected, are set out in Note 19 on page 171.
Disclosure of personal data breach incidents
For the disclosure of personal data breach incidents, NHS England follows the Data Security and Protection Toolkit (DSPT) Incident Reporting process guidance. This is in line with the UK General Data Protection Regulation (UK GDPR). The DSPT sets out the reporting requirements for NHS organisations where a potential or actual incident may lead to a personal data breach as defined under UK GDPR. All organisations that have access to NHS patient data and systems must use DSPT to provide assurance that they are practising good data security, and where required under UK GDPR, to report a personal data breach to the Information Commissioner’s Office (ICO).
In 2024/25, NHS England reported 246 personal data breaches to the Data Protection Officer. 10 of these were reported to the ICO voluntarily or where they met the threshold for reporting under UK GDPR.
Directors’ third-party indemnity provisions
NHS England has the appropriate director’s and officer’s liability indemnity in place for legal action brought against, among others, its executive and NEDs, by virtue of its membership of the statutory Liabilities to Third Parties Scheme administered by NHS Resolution.
During 2024/25, there was one ongoing legal claim brought against NHS England during 2022/23 (disclosed in our prior year report), concerning alleged conduct of an NHS England director. This claim was indemnified by NHS Resolution.
Directors’ responsibility statement
The Annual Report and Accounts have been reviewed in detail by NHS England’s ARAC and Board. At each point it has been confirmed that the Annual Report and Accounts, taken as a whole, are considered to be fair, balanced, and understandable. They provide the information necessary for NHS England’s stakeholders to assess the business model, performance, and strategy.
Human rights
NHS England supports the Government’s objectives to eradicate modern slavery and human trafficking. The NHS England Slavery and Human Trafficking Statement for the financial year ending 31 March 2025 is available on our website.
Statement of Accounting Officer’s responsibilities
Under the National Health Service Act 2006 (as amended), the Secretary of State for Health and Social Care (with the consent of HM Treasury) has directed NHS England to prepare, for each financial year, a statement of accounts in the form and on the basis set out in the Accounts Direction. The accounts are prepared on an accruals basis and must give a true and fair view of the state of affairs of NHS England and of its income and expenditure, statement of financial position and cash flows for the financial year.
In preparing the accounts, the Accounting Officer is required to comply with the requirements of the Government Financial Reporting Manual (FreM) and in particular to:
- observe the Accounts Direction issued by the DHSC, including the relevant accounting and disclosure requirements, and apply suitable accounting policies on a consistent basis
- make judgements and estimates on a reasonable basis
- state whether applicable accounting standards, as set out in the Government FReM, have been followed and disclose and explain any material departures in the financial statements
- prepare the financial statements on a going concern basis
- confirm that the Annual Report and Accounts are fair, balanced, and understandable,
and take personal responsibility for the Annual Report and Accounts and the judgements required for determining that they are fair, balanced and understandable.
The National Health Service Act 2006 (as amended) schedule A1 paragraph 15(4) states that the Chief Executive shall be the Accounting Officer of NHS England.
The responsibilities of the Accounting Officer, including responsibilities for the propriety and regularity of the public finances for which the Accounting Officer is answerable and for keeping proper records and safeguarding NHS England’s assets are set out in Managing Public Money (HM Treasury, July 2013, as amended May 2023).
As the Accounting Officer for NHS England, I have taken the steps that I ought to have taken to make myself aware of any relevant audit information and to establish that NHS England’s auditors are aware of that information. So far as I am aware, there is no relevant audit information of which the auditors are unaware.
I confirm that there was adequate and sufficient handover from the previous Accounting Officer to provide me with the assurances required to make these statements.
Governance statement
This governance statement covers NHS England, its system leadership role of the NHS, directly commissioned health services, and oversight and assurance of the commissioning system.
Following the government’s announcement in March 2025, NHS England will undergo significant structural reform as part of the wider 10-year health plan to build an NHS fit for the future. The organisation’s functions will be streamlined and integrated into the DHSC to reduce bureaucratic duplication, both nationally and at ICB level. This restructuring is designed to eliminate operational inefficiencies and redirect substantial resources – potentially amounting to hundreds of millions of pounds – towards frontline patient services. This structural transformation represents part of broader healthcare reforms that are necessary to address the critical challenges facing the NHS and ensure its long-term sustainability.
As Accounting Officer, I have responsibility for the system of internal controls supporting and enabling the achievement of NHS England’s aims and objectives, while safeguarding public funds and the assets for which I am personally responsible in accordance with Managing Public Money and as set out in my Accounting Officer appointment letter.
This includes assurance of several organisations which are part of the wider commissioning system, including those organisations hosted by NHS England.
My responsibilities in relation to the oversight of ICBs are set out from page 74.
Board arrangements
Information on our Board and its committees is set out from page 55.
Freedom to Speak Up
Our report on whistleblowing disclosures made by NHS workers is published on our website.
Government functional standards
Functional standards set out what needs to be done, and why, for different types of functional work and were mandated for use in Governmental departments and their ALBs from the end of March 2022. The extent to which these standards are adopted across NHS England varies, and certain elements of the standards are not applicable to the organisation.
Governance arrangements and effectiveness
Governance framework
The Governance Manual brings together all key strands of governance and assurance, including Standing Orders, Standing Financial Instructions (SFIs), Scheme of Delegation, Standards of Business Conduct Policy, Risk Management Framework and the three lines of defence model.
Assessment against the Corporate Governance in Central Governance Departments: Code of Good Practice 2017 Compliance Checklist
As part of implementing best practice, an assessment is undertaken each year against this checklist from HM Treasury. NHS England is compliant (it should be noted that the following provisions in the code do not apply to NHS England: Sections 1, 2.3, 2.11, 3.3a, 3.3b, 3.3c, 3.6e, 3.7, 3.8, 3.9, 3.14, 3.19, 4.9, 4.12, 4.13, 4.14, 5.7, 5.8 and 6) against the provisions of the code, with the following exceptions:
| Ref | Code provision | Exception |
|---|---|---|
|
4.7 |
Through the Board Secretariat, the Department provides the necessary resources for developing the knowledge and capabilities of Board members, including access to its operations and staff |
This responsibility is shared between |
|
4.11 |
The Board Secretary’s responsibilities include arranging induction and professional development of Board Members |
This responsibility is shared between |
|
4.12 |
The lead non-executive board member supports the chair to ensure a board effectiveness evaluation is carried out annually, and is carried out with independent input at least once every three years, |
Effectiveness evaluation takes place annually, due to organisational changes independent input has not been sought in the last three years |
|
5.5 |
The Head of Internal Audit is periodically invited to attend Board meetings, where key issues are discussed relating to governance, risk management, or control issues across the department and its ALBs |
The Head of Internal Audit routinely attends ARAC meetings |
Corporate assurance
The NHS England corporate assurance framework, set out below, helps to provide assurance on organisational stewardship and the management of significant risks to organisational objectives.
| Assurance activity | How does it add value? |
|---|---|
|
Organisational change framework |
The framework provides a consistent approach to thinking about the impact of organisational change, including on people, infrastructure, |
|
Risk management framework |
The framework enables a consistent approach to be taken across the organisation, allowing identification of cross-directorate risks and challenges. It provides a mechanism for managers to identify risks with a route of escalation to those accountable. |
|
SFIs, Scheme of Delegation and |
Together, these documents ensure that our financial transactions, accountabilities and responsibilities are carried out in accordance with the law and government policy in order to achieve probity, accuracy, economy, efficiency and effectiveness. |
|
Programme management framework |
Provides staff with a framework to manage, control and deliver projects and programmes. Provides the organisation with consistency of reporting and monitoring, confidence of delivery of outcomes to enable decision-making and better resource control. |
|
Contract management framework |
Ensures directorates responsible for major contracts assign a contract manager and put arrangements in place to monitor supplier performance. Obtains assurance over the services provided. |
|
Corporate policy framework |
Provides an approach to help ensure policy documents are not developed in isolation, so they are balanced against the priorities of the organisation. |
We work with the support of both our internal and external auditors to strengthen and embed our assurance framework. All directorates and regions have designated leads with responsibility for ensuring that risk management, implementation of internal audit actions and other key assurance activities are properly carried out, including regular reporting and escalation.
During 2024/25, the corporate governance and compliance teams worked across the organisation to improve and embed controls by:
- ensuring that officers declared relevant interests in line with the Standards of Business Conduct Policy
- developing refreshed strategic and operational risk registers (ORRs)
- introducing enhanced risk governance arrangements to support the management of our most significant risks
- carrying out targeted interventions with teams to ensure the timely completion of actions arising from internal audit reviews
- developing and implementing an approach to undertake assurance reviews against NHS England’s statutory functions.
Management assurance
Throughout 2024/25, the Board has been provided with regular performance updates on the implementation of the priorities and programmes committed to in the NHS Long Term Plan and NHS England’s business plan.
Board reporting integrates performance against constitutional standards, the NHS Long Term Plan commitments and workforce and quality metrics.
Individual programme boards and oversight groups, each with responsibility for delivery of their programmes, meet frequently, with representatives from national and regional teams.
Assuring the quality of data and reporting
The Board has agreed the information it requires to carry out its duties. The Board is confident that performance reports have been through appropriate management review and scrutiny, and that reporting continues to evolve to meet changing organisational needs.
Risk governance
The Board sets the organisation’s risk appetite and oversees the organisational risk profile to ensure key risks are mitigated within the agreed appetite level. Risk appetite statements, setting out the amount of risk that we are willing to seek or accept in the pursuit of long-term objectives, were approved in May 2024. The Board discusses the most significant risks and actions identified to mitigate their likelihood and impact.
ARAC is responsible for reviewing the establishment and maintenance of an effective system of risk management. The committee holds the organisation to account on the effectiveness of risk management processes and evaluates the effectiveness of the Risk Management Framework.
It oversees the risk governance activities undertaken by the executive and board committees which consider those strategic risks, and top operational risks, that fall under their remit.
Executive committees are responsible for assessing and challenging the effectiveness of risk mitigation plans, ensuring relevant actions are implemented and escalating as appropriate to the NHS Executive. Board committees seek assurance, including through periodic deep dives, that risks are being effectively mitigated or have adequate plans in place where the current risk score is not within appetite.
Executive Risk Group is responsible for assuring ARAC about how risks across the organisation are being managed in line with the Risk Management Framework. The NHS Executive also periodically reviews the organisation’s most significant risks and, when appropriate, undertakes in-depth review.
The Chief Executive Officer, supported by senior management, provides leadership, and articulates their continued commitment to risk management through the organisational risk management framework.
The executive team collectively owns the Strategic Risk Register (SRR) and ORR and has nominated a responsible officer for each risk within them. Individual executives are responsible for managing risk at a directorate and regional level. Each directorate and region hold its own risk register and is required to regularly review its risks.
Recognising that changing leadership, with a resultant loss of corporate memory and the potential for this to continue as posts are appointed to the new organisation, may have an adverse impact on decision making, accountability or cross-team working. ARAC requested that this risk be considered and added to the ORR. Key controls and mitigations for this risk include: frequent executive meetings to support decision-making; inter-organisational collaboration ensures governance clarity; a governance manual outlining decision-making powers; and a revised terms of reference define responsibilities.
Principal risks
The SRR and ORR together contain over 40 risks to the organisation. The SRR considers the principal risks that could impact delivery of NHS England’s strategic objectives. The ORR contains the key organisational risks which relate to systems, processes and in-year delivery. NHS England’s risk profile changes throughout the course of the year in response to events and emerging priorities. NHS England considers its most significant risks to be those which, once mitigated as far as possible, will remain outside of risk appetite. The five risks detailed below were NHS England’s most significant risks in 2024/25 and will remain under regular review.
Risk: The NHS workforce is not sufficiently skilled or resourced to meet the immediate or future needs of the population.
This includes gaps in skill mix, rising demand, and ongoing challenges in culture, training, and retention. The LTWP was developed to address these issues. However, several planned mitigations have been affected by a change in government direction and funding constraints.
As a result, the workforce capacity risk remains high.
A broad range of controls have been implemented under the LTWP to mitigate this risk.
These include regional pilots of generalist training models, introduction of new roles such as anaesthetic and physician associates, and greater use of digital tools, supported by initiatives like the NHS Digital Academy. To address rising demand, measures have included increased medical school places, targeted international recruitment, and successful delivery of the 50k nursing recruitment target ahead of schedule. Retention has been supported through programmes such as the People Promise exemplar sites and publication of the NHS Equality Diversity and Inclusion Improvement Plan. Governance tools, including the Education Quality Assurance Training Framework and Board-level competency frameworks, have also been established.
Several key milestones originally planned to reduce the risk have not been met. These include the confirmation of apprenticeship funding and the commencement of the Medical Doctor Degree Apprenticeship pilot. The Digital Staff Passport was delayed beyond December 2024 as part of a broader prioritisation review. While the People Promise Exemplar Programme continues to roll out, current data does not yet show sustained improvement. Delays to these milestones—largely due to factors outside NHS England’s control—present a challenge to effective risk reduction. The LTWP is now under review 18 months after publication, with many mitigations yet to be delivered. Delivery plans for other elements of the LTWP are currently in development and will inform future assessments of the risk score once implementation is underway.
Risk: There is a risk to quality care (safety, effectiveness and experience) for patients, carers and families if NHS England does not satisfactorily deliver its statutory functions; commissioning and regulatory duties; implement national policy and strategy that cover assurance, improvement and planning functions.
Due to the cross-cutting nature of quality, assurance and evaluation of this risk occur within the governance of existing programmes, such as the implementation of the Patient Safety Strategy.
A comprehensive set of controls is in place to manage this risk. These include the continued investigation of unsafe care, and implementation of the National Patient Safety Strategy and associated policies, such as Martha’s Rule and initiatives on managing deterioration. NHS England has established clear governance structures and escalation processes, including a revised National Quality Board (NQB) framework, and effective learning mechanisms from coroners’ reports and safety incidents. Work on patient experience has also been prioritised, and public and patient involvement is embedded across programmes. Additionally, national and regional quality and safety teams are in place to support delivery and oversight.
Ongoing mitigation focuses on the development and implementation of a Quality Strategy for the NHS, led by the NQB and aligned with the 10-Year Health Plan and the Dash Review of Quality. This will encompass quality management systems, patient safety, experience, and clinical effectiveness. Planned work includes publication of the Quality Strategy, improvements to internal quality governance structures, and reconstitution of the NQB with updated terms of reference and governance routes. Further action includes development of a quality dashboard, updates to clinical audit governance, and publication of new guidance on QIA and best practice for audits. Efforts are also underway to ensure appropriate resources, expertise, and clarity of roles are in place to support and embed quality across the system.
Risk: There is a risk of national supply disruption in the supply market of non-clinical goods, services, medical devices and clinical consumables; amplified supply chain fragility due to a variety of factors including geopolitical, global economic challenges, cyber threats, lack of processes and capacity to proactively anticipate and manage supply challenges, could have potential adverse consequences for patient outcomes.
Immediate responses to incidents are often effective at preventing short-term harm, however they come at high cost and offer limited support for longer-term patient safety or systemic resilience. In response, an expert working group was convened in November 2024 with cross-organisational stakeholders to assess the resilience landscape, map gaps, and develop a more coordinated approach to risk management.
Several controls are currently in place. The DHSC and NHS Supply Chain manage supply disruptions through structured mechanisms such as the Shortage Management Oversight Group and the use of data tools. NHS Supply Chain has demand management processes and maintains oversight of products in their catalogue, although this only covers around 60% of the NHS market. Clinical expertise is available during incident response, though gaps in resource capacity are recognised. Additional control measures include contingency logistics such as air freight and expedited freight services, compliance with legislation through contract management, and horizon scanning for regulatory changes.
Areas identified for further attention include high-risk categories such as digital, estates, independent sector provision, pharmaceutical devices, and transport. Key next steps include establishing robust clinical and commercial expertise, improving proactive communication with trusts and ICBs, and defining national leadership on supply resilience.
Risk: Due to advancements in technology and improved care pathways, 45% of estates infrastructure (including reinforced autoclaved aerated concrete) is not fit for the services the NHS delivers today. This results in disruption to productive clinical services, significant risks to patient and staff safety and an estate that is located in places not aligned with the populations needs.
While key strategies such as the Long-Term Infrastructure Strategy and Integrated Care Systems (ICS) Estate Strategies are underway, financial and capacity constraints are affecting progress. Work on a supplier resilience strategy has been paused, and some planned developments are delayed or under-resourced, impacting the pace of change.
Infrastructure strategies led by ICBs aim to align estate needs with service models. A Property Companies Delivery Board has been established to coordinate delivery and maximise the NHS property offer. National oversight is improving, supported by the Capital Strategy Programme and ICS Infrastructure work. Early steps are being taken to build an asset management centre of excellence and improve estate guidance. A workforce action plan has been delivered, though it does not yet address structural capability or pay disparities.
Work is ongoing with ICSs to develop first-generation infrastructure and investment strategies, focused on creating an estate that is resilient, efficient, and better aligned with service delivery. Key deliverables include a Primary Care Estates Strategy, a Supplier Resilience Strategy and an Operational Digitalisation Strategy. Some workstreams are paused due to lack of financial support. The publication of an Asset Management Strategy and updated Estate Code is now expected in June 2025.
Risk: There is a risk of significant data breach resulting in accidental or unlawful loss, alteration, unavailability, unauthorised disclosure of, or access to, personal data causing patient and employee harm, poor clinical outcomes, damage to public trust, lost productivity and financial loss.
Given NHS England’s role as a custodian of some of the world’s most comprehensive and sensitive health and workforce data, the impact of a breach could be severe, affecting patients, staff, public trust, clinical outcomes, and leading to productivity loss and financial damage.
The greatest severity of breach would likely result from a cyber-attack, insider threat, or supply chain failure, risks where NHS England has only partial control.
A comprehensive governance framework is in place to ensure appropriate technical, organisational, and security controls. This includes policies and training for records management, data protection by design, and mandatory Data Protection Impact Assessments (DPIAs). Awareness campaigns and training reinforce staff responsibilities and breach response procedures. Breach incidents are actively monitored and investigated by a dedicated team, with 24/7 response capacity and breach-specific playbooks. Legal and regulatory processes are embedded, with external legal support and stakeholder coordination including the ICO. A strong lessons-learned feedback loop ensures that breach causes are analysed, trends identified, and actions taken to reduce recurrence. Information Governance (IG) audits and monitoring support assurance and compliance across the organisation.
Key future deliverables include a breach cause analysis process, and refreshed IG policies including those on Generative AI and international data transfers. IG audit procedures will be implemented to monitor compliance, alongside breach assurance reviews. However, ongoing resource constraints may delay or prevent delivery of several mitigation actions including additional incident capacity, creating a risk of insufficient capacity in the event of multiple data breaches. Further IG awareness activities are planned, with internal campaigns ongoing through 2025/26.
NHS oversight and support
We use the NHS Oversight Framework to assess ICBs’ and providers’ performance against a set of metrics and allocate them into one of four segments, which determine the level of support we provide. NHS England has met regularly with each ICB throughout the year, to review segments and support needs for both the ICB and the providers across their ICS footprint and published segmentation decisions on our website.
To ensure the model of oversight remains relevant and effective we committed in the 2024/25 Priorities and Operational Planning guidance to engage on a new oversight framework. We formally consulted on the principles underpinning our oversight approach in spring 2024 and have engaged with service leaders and the new government to develop an NHS Oversight Framework in line with the government’s 2025 Mandate to NHS England. A draft of this framework underwent public consultation early in 2025/26. We intend to publish the first formal segmentation decisions in quarter two, giving a segment score of 1-4 based on performance against delivery metrics.
Quality oversight and assurance
NHS England understands the importance of viewing quality, finance, workforce and population health matters together as part of the Quadruple Aim, and of managing quality through a combination of planning, improvement, control and assurance activity (a Quality Management System approach).
NHS England develops the strategy for and delivers a range of statutory quality functions, including the NHS Patient Safety Strategy, the National Clinical Audit Programme, the Safeguarding Accountability and Assurance Framework, NICE Guidelines and Quality Standards, Coroners Prevention of Future Death reports, Freedom to Speak Up, Professional Standards and complaints.
The Board’s Quality Committee (see page 59) ensures that NHS England’s strategies are continually improving quality, safety, and experience of care. Executive level quality meetings reporting in are the Quality and Performance Committee to scrutinise quality, performance, workforce and finance issues, and the Executive Quality Group to provide oversight and scrutiny of care quality across regions and receives regional quality insight from ICBs and providers.
Provider collaboratives
NHS England has supported providers to continue to strengthen collaborative arrangements as part of ICSs, to deliver improvements and transform care for patients. The spread of best practice has been encouraged through the delivery of a programme of support – including webinars, case studies, and peer learning. Collaboratives are increasingly leading on key improvement priorities on behalf of the wider system, such as elective care performance, clinical support services, and corporate efficiencies.
Alongside provider collaboratives, shared chair and chief executive arrangements have been put in place across some NHS trusts and foundation trusts where this enables more effective collaboration. NHS England has worked with trusts to understand the opportunities and risks of such arrangements.
Regulating independent providers of NHS services
All independent providers of NHS services are required to hold a provider licence, unless exempt, under the DHSC regulations. The provider licence gives NHS England the ability to safeguard continuity of services for patients if a provider gets into difficulty. As of 31 March 2025, 150 independent providers held a provider licence, as did three NHS-controlled providers.
Under the ‘Commissioner Requested Services’ policy; local commissioners are required to tell NHS England which of their services (commissioned from independent providers) need the protections of the licence’s continuity of services conditions. Under the ‘Hard to Replace Providers’ policy, NHS England can apply the same protections where providers deliver regional or national services of significant scale or complexity. As of 31 March 2025, 55 licensed providers were subject to the license’s continuity of services conditions.
During 2024/25, no formal enforcement action was taken with any independent providers, meaning that as of 31 March 2025, no enforcement undertakings were in place.
Mergers and acquisitions
NHS England is responsible for risk rating statutory transactions. The assurance process for significant transactions includes reviewing trusts’ strategic cases and full business cases to assess the rationale for the transaction, why the transaction is the preferred option, the likely financial and patient benefits associated with the transaction, that the transaction and integration is well planned and that all statutory requirements have been met. These are assessed through review of documentation and discussions with the trusts, ICBs and system leaders.
Transactions completed during the reporting period:
- Transfer of services (community, mental health and learning disability) from Isle of Wight NHS Trust to Southern Health NHS Foundation Trust on 1 May 2024.
- Southern Health NHS Foundation Trust acquired Solent NHS Trust on 1 October 2024, with the newly enlarged trust renamed Hampshire and Isle of Wight Healthcare NHS Foundation Trust.
- Transfer of services and dissolution of Dudley Integrated Health and Care NHS Trust on 1 October 2024.
- Kingston Hospital NHS Foundation Trust acquired Hounslow and Richmond NHS Trust on 1 November 2024, with the newly enlarged trust renamed Kingston and Richmond NHS Foundation Trust.
- Camden and Islington NHS Foundation Trust acquired Barnet, Enfield and Haringey NHS Trust 1 November 2024, with the newly enlarged trust renamed North London NHS Foundation Trust.
- Royal Free London NHS Foundation Trust acquired North Middlesex University Hospital NHS Trust on 1 January 2025, with the newly enlarged trust retaining the Royal Free London NHS Foundation Trust name.
New Hospitals
Three new hospitals were opened through the New Hospital Programme, including the Dyson Cancer Centre (Royal United Hospitals Bath NHS Foundation Trust), the Greater Manchester Major Trauma Hospital (Northern Care Alliance NHS Foundation Trust) and the Midland Metropolitan University Hospital (Sandwell and West Birmingham Hospitals) opened during 2024/25.
Direct commissioning by NHS England and delegation to ICBs
NHS England directly commissions certain clinical services at a national or regional level. During 2024/25, NHS England continued to delegate the responsibility for commissioning suitable services to ICBs, to realise the benefits of integrated commissioning at local level, including improving population health outcomes, reducing health inequalities and achieving better value for money. Where NHS England has delegated responsibility to ICBs for commissioning services, NHS England remains accountable for these services. During the year, a single approach to oversight and assurance of delegated commissioning has been developed, ready to apply to primary care and specialised services in 2025/26, and to any more commissioning services subsequently delegated.
Primary care services
In 2024/25, NHS England followed its Primary Care Commissioning Assurance Framework to oversee ICBs’ delegated commissioning of primary care services (primary medical, dental (primary, secondary and community), general ophthalmic and pharmaceutical services).
Overall, this exercise indicated full or substantial assurance for 35 out of 42 ICBs across all their primary care functions. For the remaining ICBs, there were some individual functions where there was limited evidence, and these were subject to additional assessment and agreed actions where required.
Specialised services
Specialised services support people with a range of rare and complex conditions. They often involve innovative treatments for patients with rare cancers, genetic disorders, complex medical conditions or surgical needs. The specialised commissioning allocation for all specialised services was £27 billion at the end of 2024/25.
In April 2024, commissioning responsibility for 59 specialised services was delegated to all ICBs in the Northwest, Midlands, and East of England regions. ICBs in the remaining regions continued to commission these services via five statutory joint committees, formed between ICB and NHS England regions. Most of the £27 billion allocation is issued to ICBs for delegated services and regional teams for jointly commissioned and retained specialised services, with the balance held centrally to fund national budgets such as the Cancer Drugs Fund and other national programmes. Local ICB governance structures and annual reporting applies to the £5.6 billion spend allocated to ICBs in Northwest, Midlands, and East of England ICBs, in their duty as responsible commissioners.
NHS England acted as the accountable commissioner for both delegated and retained services, maintaining oversight through regional accountability reporting lines. During 2024/25, the Delegated Commissioning Group for Specialised Services continued to provide strategic direction for the 59 delegated services, set national standards, approved key national transformational gateway documents, and brought together the responsible and accountable commissioners from across the country. Correspondingly, the National Commissioning Group for Specialised, Health and Justice Armed Forces Services continued to set strategic direction, set standards and manage gateway approvals, as well as oversee commissioning of those services commissioned by NHS England.
The Clinical Priorities Advisory Group made formal recommendations relating to the commissioning treatments and interventions for adoption across delegated and retained services.
In 2024/25, there was careful assessment and preparations for all suitable specialised services (including an additional 11 services, thus 70 services in total) to be delegated to all ICBs in England, commencing in April 2025.
Health and justice
Health and justice services comprise health services in adult prisons and pre and post custody services, IRC’s, children and young persons secure and detained and sexual assault referral centres. They are supported through the Health and Justice Delivery and Oversight Group nationally, and this feeds into the NCG. NHS England regional teams are the responsible commissioners for health and justice services, working in conjunction with the appropriate national health and justice teams.
Armed forces
Armed Forces directly commissioned services comprise secondary and community care for serving personnel and some families; prosthetics and three bespoke physical and mental health services for veterans. They are the responsibility of the national armed forces commissioning team. This is overseen by the Armed Forces Oversight Group which feeds into the NCG.
Vaccinations and screening – governance and the Section 7A agreement
The annual NHS Section 7A public health functions agreement between NHS England and the DHSC sets out the arrangements under which the Secretary of State delegates responsibility to the NHS England Board for commissioning certain NHS public health services. Under that agreement, NHS England commissions 11 screening programmes, 20 immunisation programmes, and Child Health Information Services (CHIS).
Internal assurance in 2024/25 was provided through the NHS England Vaccinations and Screening Delivery and Transformation Board, informed by programme-specific boards for screening, vaccinations, and CHIS programmes.
In January 2025, following extensive engagement with ICBs and other stakeholders, the NHS England Board approved the delegation of the commissioning of all vaccination services and most screening services, to take place in April 2026 (subject to Ministerial approval and readiness). Following the organisational changes subsequently announced, commissioning accountability for vaccination and screening will now transfer to ICBs. This is likely to take place from April 2027, subject to the passage of legislation.
Other assurance
Information Governance
The Privacy, Transparency & Trust (PTT) function provides operational data protection, confidentiality and records management advice and support to enable NHS England to meet data protection requirements, minimise privacy and confidentiality risks, manage corporate records, respond to, investigate and report personal data breaches (See Director’s Disclosures), and improve transparency over how NHS England uses data. The PTT function also delivers services that support other NHS organisations with IG.
In 2024/25, the PTT function has delivered advice, support and services that have enabled NHS England to:
- deliver national digital, technology and data products, platforms and services to other parts of the NHS e.g. NHS App, NHS Mail, FDP, NHS Notify, National Proxy
- support other NHS organisations to respond to cyber incidents, including supporting the NHS response to the attack on Synnovis, a laboratory service provider in 2024
- collect, analyse, use and share national datasets for operational, planning, commissioning and research purposes. This includes supporting seven new Secretary of State directions (Under section 254 of the Health and Social Care Act 2012) and two statutory requests (under section 255 of the Health and Social Care Act 2012) (from Digital Health and Care Wales) for the collection and analysis of datasets. Those directions and requests are published on our website
- use data internally, for example in relation to Human Resources, use of internal IT systems and management of records, including publishing a new Operational Selection for Preservation Policy relating to records to be preserved under the Public Records Act 1958 and updates to Data Protection, Confidentiality and Records Management Policies
- respond to individual rights requests made under UK GDPR, including requests for access to personal data. During 2024/25 NHS England responded to 808 data access requests
- provide assurance that it is practising good data security, and that personal information is handled correctly, through its annual submission against the standards set out in the Data Protection and Security Toolkit. All mandatory standards were met in 2024/25.
Assessment under section 13U(2)(d) of the National Health Services Act 2006
Under section 13U(2)(d) of the National Health Services Act 2006, the annual report must contain an assessment of how effectively NHS England has discharged its relevant data functions (as defined in section 253(3) of the Health and Social Care Act 2012).
NHS England has published information on our website generally (NHS England » Protecting and safely using data in the new NHS England) about the ways NHS England protects data and has regard to the Statutory Guidance on NHS England’s Protection of Patient Data in the discharge of its function. In addition, during 2024/25:
- NHS England established tailored IG arrangements to support the roll out of the FDP.
This included the development of the FDP Information Governance Framework,
DPIA templates for local FDP products, FDP specific DPIAs for national products, a new FDP Privacy Notice and separate national and local Product Privacy Notices (NHS England » NHS Federated Data Platform national product privacy notices and DPIAs and NHS England » NHS Federated Data Platform local product privacy notices and DPIAs.
The FDP DPIA was also published. - NHS England has several de-identified technical data processing environments where de-identified data is analysed to fulfil its statutory functions. Since March 2024 this included the national instance of the FDP which hosts national products which transitioned from the national data platform.
- During 2024/25, a new privacy enhancing technology service was launched within NHS England, which enhances privacy protection through de-identification and treatment of data to support analysis in de-identified data processing environments, including the national instance of the FDP.
- NHS England seeks advice from its Advisory Group for Data (AGD) on specific data access requests and to support the development and maintenance of precedents, standards, and guidance on data access for planning, commissioning and research.
The AGD minutes containing advice provided and the AGD Terms of Reference are publicly available on the NHS England website. Recruitment of a new Chair and some new members of AGD to replace members whose terms of appointment came to an end began in 2024/25 and will complete early in 2025/26. - NHS England regularly consults and engages with the National Data Guardian (NDG) and the ICO. During 2024/25, NHS England had regular engagement with National Data Guardian and ICO in relation to the development of the IG documentation that supports the FDP. A range of other FDP programme specific expert advisory groups also met regularly to support the implementation of the FDP including the FDP Check and Challenge Group and the FDP Data Governance Group.
- NHS England considers that it is effectively protecting patient data and has effectively discharged its relevant data functions during 2024/25.
Commissioning support units
Four NHS CSUs operate across England, providing essential support to organisations including ICBs, trusts, NHS England, and local authorities. With a workforce of circa 6,500 and income of circa £450 million, CSUs rely on income for services delivered, creating an incentive to offer quality services and value to the NHS at scale.
As an integral part of the NHS, CSUs operate in accordance with good governance principles. In 2024/25, the CSU programme achieved its financial targets.
Supply Chain Coordination Limited (SCCL)
SCCL is the company owned by NHS England which manages the NHS supply chain. It undertakes its procurement services and transacts with customers and suppliers, leveraging the collective buying power of the NHS to support them to achieve their financial, operational and strategic objectives.
NHS England is the sole shareholder of SCCL, a UK incorporated company. SCCL’s Articles of Association include a range of matters reserved for shareholder decision.
NHS England has established a governance framework regarding its shareholdings.
In addition to controls set out in the company’s Articles of Association, NHS England appoints directors who sit on the Board and Committees of SCCL and holds quarterly accountability meetings to review performance against KPIs and financial targets, both of which are agreed by the NHS England board annually.
Counter fraud
NHS England has a dedicated counter fraud team which ensures that appropriate counter fraud arrangements are in place. This includes proactive activities to prevent and detect fraud, as well as reactive investigation of allegations of fraud related to our functions.
The Director of Financial Control has day-to-day operational responsibility for the function, and the Chief Financial Officer provides executive support and direction. We continued to work collaboratively with key partners in both proactive and reactive areas, including the Public Sector Fraud Authority, the DHSC, NHS Counter Fraud Authority, NHS Business Service Authority and law enforcement agencies.
NHS England public Inquiries
NHS England has a legal requirement to comply with Public Inquiries. In 2024/25 NHS England participated in or responded to the following:
- UK COVID-19 Public Inquiry
- Thirlwall Public Inquiry – circumstances around the crimes of Lucy Letby
- Fuller Independent Inquiry – mortuaries/privacy and dignity of the deceased
- Lampard Public Inquiry – investigating mental health inpatient deaths in Essex
- Angiolini Inquiry – safety of women in public spaces after Sarah Everard’s death
- Infected Blood Inquiry – which published its final Report in May 2024.
Inquiry work in NHS England is led by a central team responsible for managing multiple inquiries. The Inquiry Team has developed a successful ‘end to end’ operating model for the lifespan of public inquiries; from their establishment to final reporting. This methodology includes locating and retrieving records from NHS England and legacy ALBs, managing the disclosure of evidence, as well as providing written and oral evidence.
As a Core Participant, NHS England reviews disclosed material, responds to evidence proposals for witnesses to provide insight in live hearings, makes oral submissions and informs the thinking of Inquiry Chairs. The team’s rigorous process has enabled NHS England to provide 73 written statements, support 14 appearing witnesses and participate in over 200 days of public hearings.
The team sets and maintains high professional standards to help ensure that the NHS learns lessons and implements improvements to patient services, whilst making the best use of public funds. As part of our ‘end to end’ approach, we are building on work to support Baroness Thirlwall’s assessment of historic recommendations, as well as learning from the Health Services Safety Investigations Body report on public inquiries “Recommendations but no action”, in order to lead on the tracking and assuring implementation of inquiry recommendations in line with the Government’s approach.
Some of the inquiries listed above will issue warning letters, reports and recommendations in 2025/26. The Inquiry team is therefore preparing for this, alongside supporting individuals through the organisation’s transition, retaining legacy records and advising and supporting current and former staff. Preparatory work is also underway for newly announced inquiries into the events in Southport in Summer 2024 and the crimes committed by Valdo Calocane in Summer 2023.
Control issues
Managing third-party contracts
NHS England’s commercial delivery teams manage 2,800+ active contracts (with an approximate value of £15.5 billion), that are critical to the delivery of services for the NHS. These are managed in line with NHS England’s Contract Management Framework, which is based on Government Commercial Function methodology, which has been updated to reflect recent legislative and policy requirements. All Contract Management team members have either successfully completed the corresponding Government Commercial Function Accreditation or are actively working towards achieving accreditation. In line with the government’s transparency agenda, NHS England comply with notice publication requirements including commercial pipeline publication of contracts above £2 million, and publication of contract award notices above £10k.
Overpayments to medical practitioners
Following the identification of overpayments to medical practitioners in 2021/22 and 2022/23, a new process has been implemented. Since April 2024, all payments to suspended medical practitioners have been centralised and are now processed by the national team.
The new process ensures that a standardised approach to applying the guidance is in place and the monthly assurance process to reconfirm eligibility allows for changes to circumstances to be actioned quickly to prevent overpayments. During 2024/25, one small overpayment of £277 occurred as a result of unique circumstances which do not undermine the new control environment overseeing these payments. An overpayment of £9k in 2024/25 was disclosed in the 2023/24 Annual Report and Accounts, as it was identified prior to the publication of that report.
Recoveries of previously identified overpayments continue to be pursued subject to legal advice.
Review of economy, efficiency and effective use of resources
Allocations
NHS England has responsibility for allocating the NHS funding agreed with the DHSC as part of our mandate. Please see the Chief Financial Officer’s Report on page 43, for information on allocations.
ICB auditor referrals
5 ICBs were subject to 2024/25 referrals (2023/24: 14 referrals) to the Secretary of State by their auditor under Section 30 of the Local Audit and Accountability Act 2014, due to forecasting that expenditure would exceed income during the financial year.
Financial performance monitoring
The financial position across the commissioning system was reported monthly using the Integrated Single Financial Environment (ISFE) system and through provision of supporting information. These collections included key elements of provider reporting which facilitated the focus on overall system reporting. Alongside this, NHS providers continued to report their monthly financial position to NHS England. This reporting has enabled a detailed monthly review by regional and national finance leadership teams and NHS England’s Chief Financial Officer.
Individual ICB, system, direct commissioning and provider financial performance is monitored against KPIs including balance sheet indicators and performance against efficiency plans, in addition to the reported forecast and year-to-date position.
The financial position of commissioners is consolidated and reported in the overall NHS England accounts. NHS England is not the parent entity of NHS trusts and NHS foundation trusts; the financial position of providers is reported separately in the consolidated NHS provider accounts.
Cabinet Office efficiency controls
As part of the Government’s control of expenditure, NHS England are subject to specified expenditure controls. These controls cover a range of expenditure categories and require proposed expenditure to be approved to secure best value for money and ensure efficiency is being maximised. For expenditure above certain thresholds in specified categories (including professional services and consultancy), onward approval is also sought from the DHSC and for some cases this also requires approval from the Minister, Cabinet Office, and/or HM Treasury
Ministerial Directions
The Secretary of State gave 11 directions to NHS England under section 254 of the Health and Social Care Act 2012 to establish and operate information systems i.e. systems for the collection or analysis of information relating to health or social care. In addition, 23 direction specifications, which connected with existing directions, were also issued. The Secretary of state issued the routine financial directions, making provision for NHS England’s budgets and financial limits.
Head of internal audit opinion
Internal audit’s opinion is based on a programme of work designed to address the specific assurance requirements of the NHS England Board and Accounting Officer. It is their opinion of the overall adequacy and effectiveness of the NHS England framework of governance, risk management and internal control as they operated during the year to 31 March 2025.
Results of internal audit work, including remedial actions agreed with management, have been regularly reported to management and ARAC.
The opinion is given following the Prime Minister’s announcement on 13 March that NHS England will be abolished, that a programme of work would bring NHS England back into the Department of Health and Social Care, and that significant organisational changes and uncertainty are to be expected. At the time the announcement was made, the majority of the internal audit work had been completed, and the opinion is expressed in the context of this.
The opinion of internal audit is that the design of the governance and risk management framework for the year were effective, except for the SFIs which had not been fully updated but were being reset at the year-end following announcements in March 2025 on NHS England’s integration into the DHSC. A paper to update the SFIs was approved by the NHS England Board in June 2025, with a full update planned for later in 2025/26.
The advice of internal audit is that it is fundamental that the reset of the governance and risk management frameworks be kept under review during 2025/26 to confirm they remain appropriate during transition.
Internal audit concluded that limited assurance could be provided over the effectiveness and efficiency of the internal control framework, with the exception of four areas where they were unable to provide assurance because either previous actions remained in progress, the areas were not ready to audit, or known historical issues had not been addressed. Actions have been agreed for each of these areas after the reporting period and are being progressed to address the recommendations.
The organisation has continued to be under significant operational pressure and was subject to further change including substantial changes to the executive (see page 55) and delegation of specialised commissioning functions to ICBs. Actions have been agreed throughout 2024/25 to address the issues identified by internal audit. However, implementing actions in a timely manner has been challenging in the context of the ongoing operational pressures, and management continue to focus on this.
Despite the challenging operating environment, internal audit noted that a number of mechanisms have been put in place during the year to confirm compliance with corporate policies and procedures, including travel and expenses monitoring and contingent labour. The agreed management actions from the 2023/24 internal audit of dental contract management, which was given a ‘no assurance’ rating, were addressed during 2024/25.
There remains significant reliance on third party providers of core services, such as payroll processing, and there remains a requirement to further embed the contract management framework to obtain assurance over the delivery of services.
Some of the weaknesses in internal controls for core processes were assessed as being fundamental to the system of controls. Management actions have been agreed to address these observations, not all of which were completed by year end given their nature, but where possible, interim solutions have been put in place.
Remuneration and staff report
Our people
Our NHS People Plan ambitions and values drive our workforce strategy, which aims for more staff working flexibly in a compassionate and inclusive culture. Alongside our People Plan, our NHS People Promise sets out our pledge to one another and describes how we want to improve the experience of working in the NHS for everyone.
Organisational change
The Government announced on 13 March 2025 that NHS England will be abolished as an arm’s length body and integrated into a restructured DHSC, with the total headcount reduced by 50%. We have started conversations with colleagues in Government about the design of the new the DHSC and the timetable for this transition. We appointed Richard Barker in May 2025 as Senior Responsible Owner to lead the joint transformation programme. We continue to work closely with the DHSC to design and implement the new organisation that will bring together many of the existing functions of NHS England and the DHSC.
Our values
Contributions from across the organisation helped define our new values that would shape the culture of NHS England. Over 650 colleagues participated in workshops and gave written feedback. This collaborative effort helped develop and define our new values and set the tone for our new organisation. This saw the introduction of three new organisational values: collaboration, inclusion, and learning and improvement.
Our workforce
Staff numbers
On 31 March 2025, NHS England directly employed 15,978 staff (14,492 WTE). Of these, 15,477 were permanently employed, and 501 were employed on payroll on fixed term contracts of employment.
Staff by grade
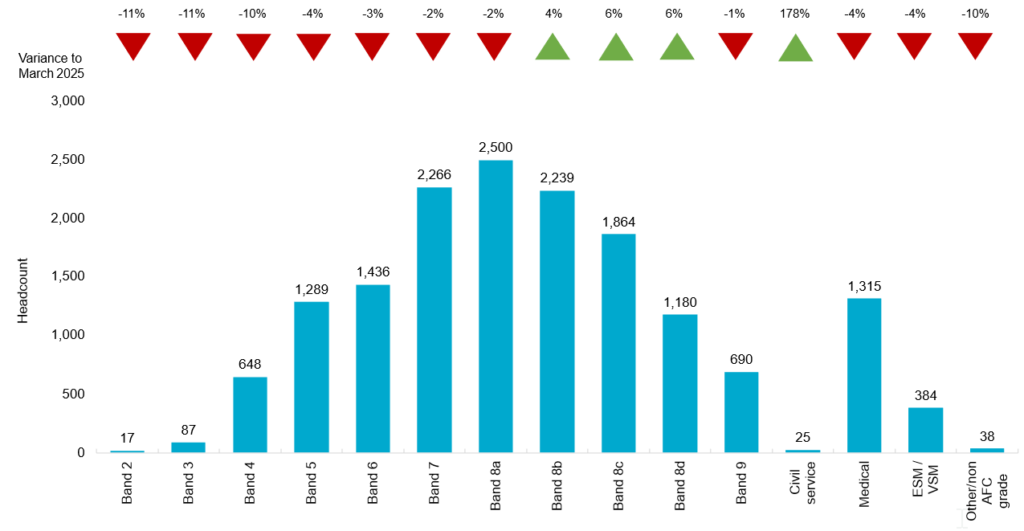
The chart shows the headcount by pay band on 31 March 2025. Detail on staff numbers and costs for NHS England and the consolidated group, including CSUs, are presented from page 94.
The headcount of permanent and fixed term staff in NHS England decreased by 1% since 31 March 2024.
Staff turnover
Turnover decreased in 2024/25 compared to 2023/24. Both the headcount and the number of people leaving the organisation decreased.
| 2018/19 | 2019/20 | 2020/21 | 2021/22 | 2022/23 | 2023/24 | 2024/25 | |
|---|---|---|---|---|---|---|---|
| NHS England | 14.0% | 13.2% | 4.88% | 9.65% | 11.01% | 16.52% | 7.09% |
| NHS TDA | 14.9% | 15.2% | 4.65% | 7.30% | 8.10% | N/A | N/A |
| Monitor | 19.4% | 29.5% | 4.13% | 11.58% | 2.21% | N/A | N/A |
| NHS Digital | – | – | – | 11.79% | 10.17% | N/A | N/A |
| Total | 14.7% | 14.0% | 4.85% | 10.00% | 10.90% | 16.52% | 7.09% |
Equality, diversity, and inclusion
The charts below reflect the proportion of all staff and senior managers who have reported a disability or long-term conditions, in ESR.
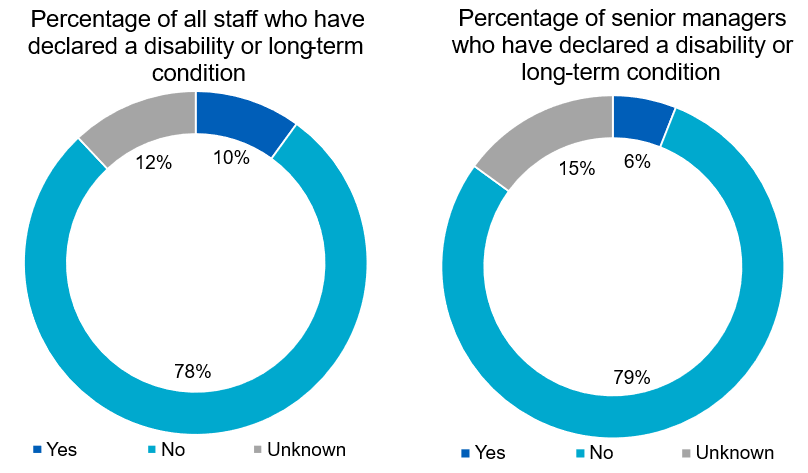
Ethnicity of all staff and senior managers
Figures below show the overall percentage of black or minority ethnic (BME) staff and the change over the last 3 years:
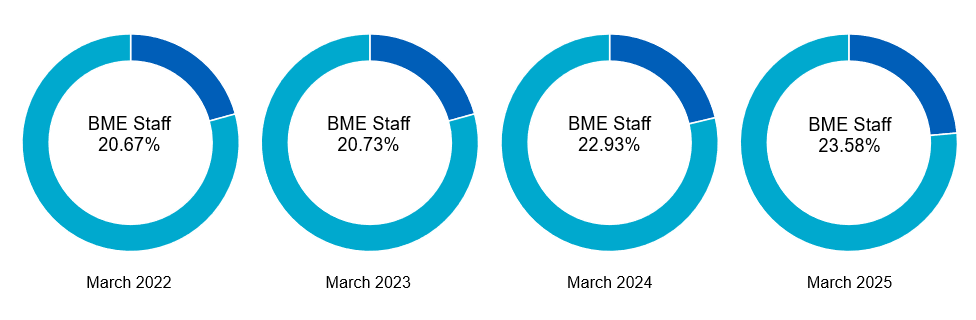
The proportion of people employed by NHS England who consider themselves to be from a BME heritage increased by 0.7 ppts between 31 March 2024 and 31 March 2025.
The graphs below show ethnicity for all staff and senior managers, as reported in ESR.
The proportion of senior managers who identify as BME has increased from 22.7% in 2023/24 to 23.1% in 2024/25.
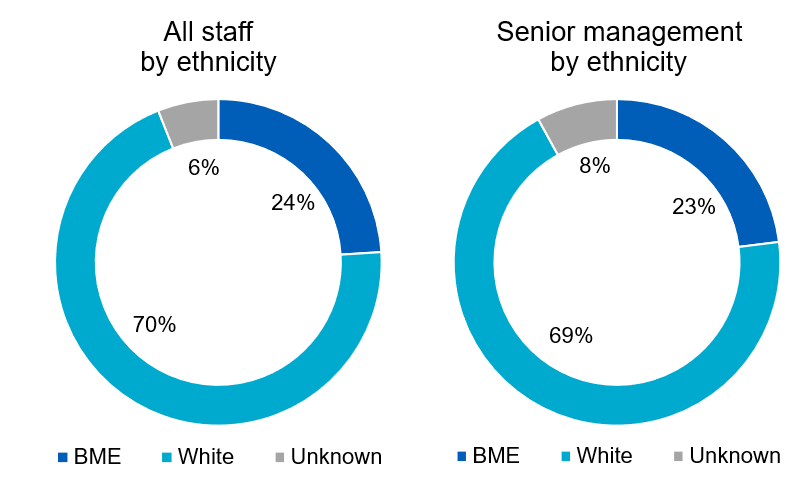
Sexual orientation of staff and senior managers
The percentage of staff who disclose their identity as lesbian, gay and bisexual (LGB) is 4.9% as of March 2025. The breakdown of sexual orientation declaration is detailed below, including an overview of senior managers who have declared as LGB in ESR (4.1%).
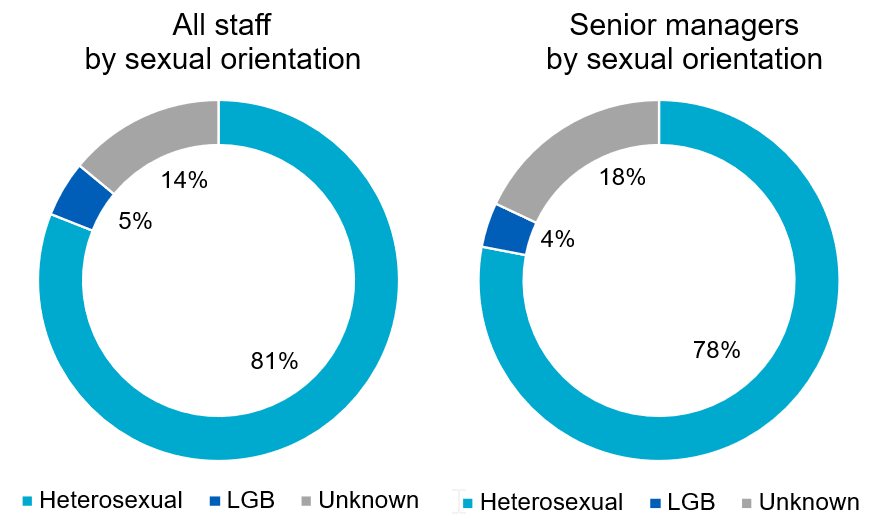
Gender of all staff and senior managers
The female gender profile of the total NHS England ‘on payroll’ workforce decreased by 0.7% between 31 March 2024 and 31 March 2025. There has been an increase in the number of female senior managers from 54.7% on 31 March 2024 to 55.4% on 31 March 2025.
The gender diversity of NHS England Board members is set out on page 54 and the graphs below highlight gender reporting in ESR:
All staff and senior managers by gender
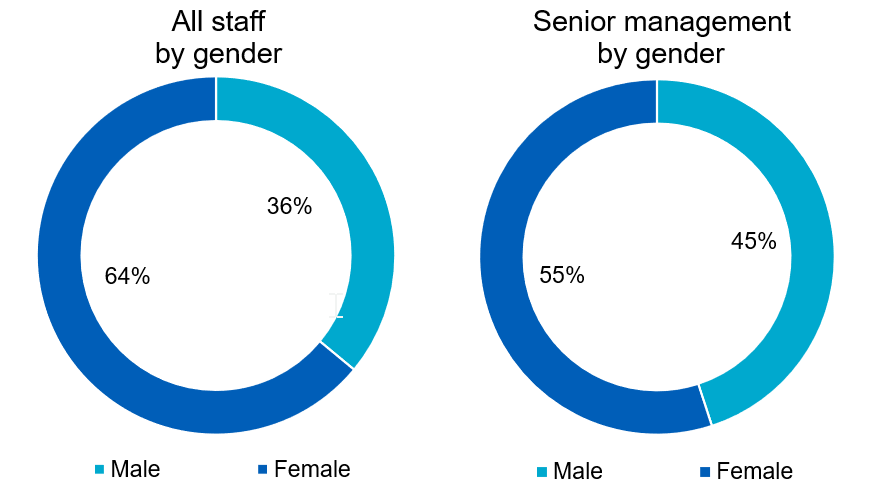
IMAGE
Gender pay gap 2024
We have produced a gender pay gap report as at 31 March 2024. The gender pay gap trend for NHS England is positive, with improvements made from the previous year. The mean gender pay gap was 11.41% in March 2024, representing a reduction in the gap of more than 5% over four years.
| Year | Mean gender pay gap |
|---|---|
|
2024 |
11.4% |
|
2023 |
11.8% |
|
2022 |
14.7% |
|
2021 |
16.2% |
|
2020 |
16.7% |
Pay quartiles by gender in NHS England
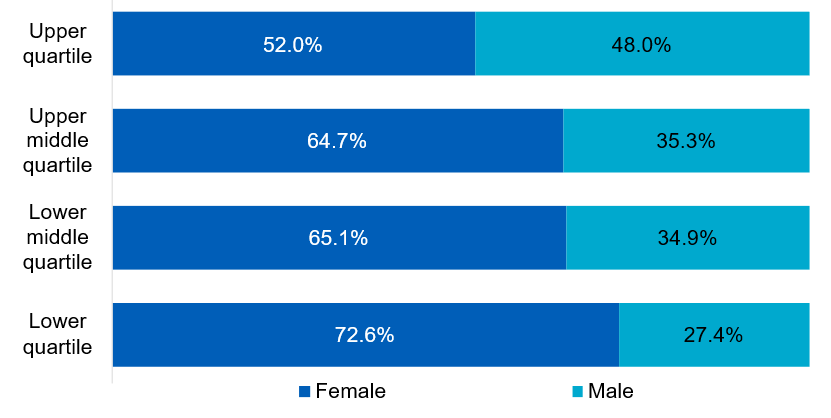
In NHS England 52% of women are in the highest paid jobs compared to 48% men. In contrast, 73% of women are in the lowest paid jobs compared to 27% men.
The pay gap is a result of having a smaller proportion of men in lower pay bands. Although the mean salaries for women across pay bands 2 to 7 are higher, their mean earnings are considerably less than men across bands 8b and above. Similarly, we have the highest proportion of women in pay bands 5 to 8a compared to men who have a higher proportion in bands 8b and above.
Sickness absence
Sickness absence for the period 1 April 2024 to 31 March 2025 was as follows:
| WTE days available | WTE days lost to sickness absence | Sickness absence rate | |
|---|---|---|---|
|
NHS England 2024/25 |
5,217,850 |
158,887 |
3.05% |
|
NHS England 2023/24 |
5,663,098 |
140,459 |
2.48% |
Employment policies
We have a range of employment policies that reflect the culture of NHS England and support our ambition to be an Employer of Choice. Our priorities include:
- Continue to develop effective working relationships with our trade union colleagues on our Policy Subgroup.
- Develop a model to effectively engage with all areas of the business to ensure stakeholder feedback is considered when reviewing policies.
- Harmonise the three legacy policies on attendance management.
- Focus on the review of the policies on our policy schedule.
- Lead on the policy development for the new internal Sexual Misconduct policy, which was launched as part of the National Domestic Abuse and Sexual Violence programme in response to new legal responsibilities.
- Development of policy summaries for the most used HR policies, to support accessibility.
- Continue to work closely with the National Policy team to enable us to adapt and align our policies to the National People Policy Framework.
Partnership working
NHS England fully recognises the vital contribution of trade unions in representing the interests of colleagues and our organisation. We work closely in partnership with our recognised trade unions on important employment matters. Partnership work includes consulting on organisational change, as a legal requirement, as well as developing and refining our policies and discussing and negotiating on a wide range of issues affecting people and the organisation.
To facilitate partnership working, NHS England has a National Partnership Forum that meets every quarter. This forum provides strategic direction for other important sub-groups that focus on specific issues. Sub-groups include policy, organisational change, equality and diversity and the Local Negotiating Committee. In addition, we hold regional and corporate engagement forums to address any local issues, that can be escalated to the national partnership structure(s).
Trade union facility time disclosures
We fulfil our obligations under the Trade Union (Facility Time Publication Requirements) Regulations 2017 for 2024/25 by reporting the information to form part of the government’s public sector trade union facility time data, which is published on the gov.uk website in August each year.
Trade union representatives – the total number of employees who were trade union representatives during 2024/25
| Number of employees who were relevant union officials during the relevant period | WTE employee number |
|---|---|
|
88 |
85.14 |
Percentage of time spent on facility time (duties and activities):
| Percentage of time | Number of employees |
|---|---|
|
0% |
56 |
|
1-50% |
31 |
|
51-99% |
0 |
|
100% |
1 |
Percentage of pay bill spent on facility time:
| Description | Figures |
|---|---|
|
Provide the total cost of facility time |
£193,550 |
|
Provide the total pay bill |
£1,288,700,000 |
|
Provide the percentage of the total pay bill spent on facility time, |
0.02% |
Paid trade union activities:
| Description | Figures |
|---|---|
|
Hours spent on paid facility time |
5469.5 |
|
Hours spent on paid trade union activities |
1068 |
|
Percentage of total paid facility time hours spent on paid Trade Union activities |
19.53% |
Staff networks
We remain committed to building a fairer, more diverse organisation. Our 13 national Staff Networks play a vital role in this, providing safe spaces for colleagues to share lived experiences and helping shape an inclusive culture. We work with them as strategic partners, using their insights to drive meaningful change.
Talent management, learning and development
Data indicates an under representation of some protected characteristics at some grades. An inclusive recruitment handbook and a supporting training package have been designed and delivered to over 2,000 recruiting managers and other staff. A pilot Accelerated Development Programme has also been established to provide development placements of 12 months for colleagues from BME, disabled and LGB communities.
We introduced a mandatory four-module Line Manager Development programme designed to reset, refresh, and upskill our leaders. The programme, rolled out to 6,000 line managers, aims to drive culture transformation in line with our organisational values, with practical tools, models and techniques.
A new approach to one-to-one meetings and appraisals was launched to provide a simple, consistent performance management framework. It focuses on celebrating individual successes, identifying areas for improvement and supporting colleagues to perform at their best.
We have renewed our Learning and Development Managed Service Contract which provides one portal for colleagues to access a wide range of Learning and Development suppliers with opportunities ranging from technical, professional, leadership and management and coaching and skills development. The new contract maintains continuity of provision for NHS England and aims to increase value add by improving the quality and choice of provision.
Employee benefits and staff numbers (subject to audit)
Detail on staff numbers and costs for NHS England and the consolidated group, including CSUs, are presented in the following tables:
Average number of people employed
| Parent 2024/25 | Permanently employed number | CSU employed number | Other number | CSU other number | Total number |
|---|---|---|---|---|---|
|
Total |
14,120 |
5,946 |
939 |
48 |
21,053 |
|
Of the above: |
|
|
|
|
|
|
Number of WTE people engaged on capital projects |
77 |
– |
11 |
– |
88 |
| Parent 2023/24 | Permanently employed number | CSU employed number | Other number | CSU other number | Total number |
|---|---|---|---|---|---|
|
Total |
14,716 |
6,492 |
1,912 |
113 |
23,233 |
|
Of the above: |
|
|
|
|
|
|
Number of WTE people engaged on capital projects |
66 |
– |
31 |
– |
97 |
| Consolidated group 2024/25 | Permanently employed number | CSU employed number | Other number | CSU other number | Total number |
|---|---|---|---|---|---|
|
Total |
37,771 |
5,946 |
2,138 |
48 |
45,903 |
|
Of the above: |
|
|
|
|
|
|
Number of WTE people engaged on capital projects |
77 |
– |
11 |
– |
88 |
| Consolidated group 2023/24 | Permanently employed number | CSU employed number | Other number | CSU other number | Total number |
|---|---|---|---|---|---|
|
Total |
38,512 |
6,492 |
3,720 |
113 |
48,837 |
|
Of the above: |
|
|
|
|
|
|
Number of WTE people engaged on capital projects |
66 |
– |
31 |
– |
97 |
Employee benefits
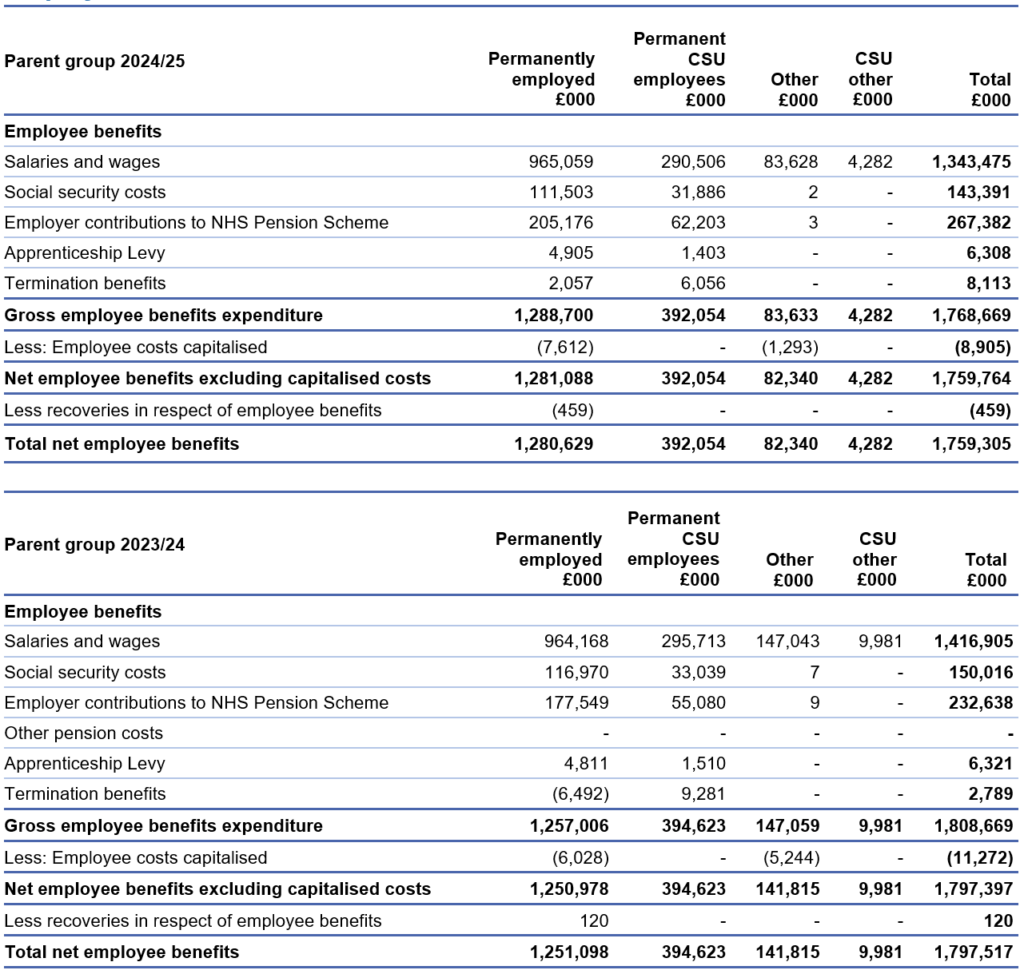
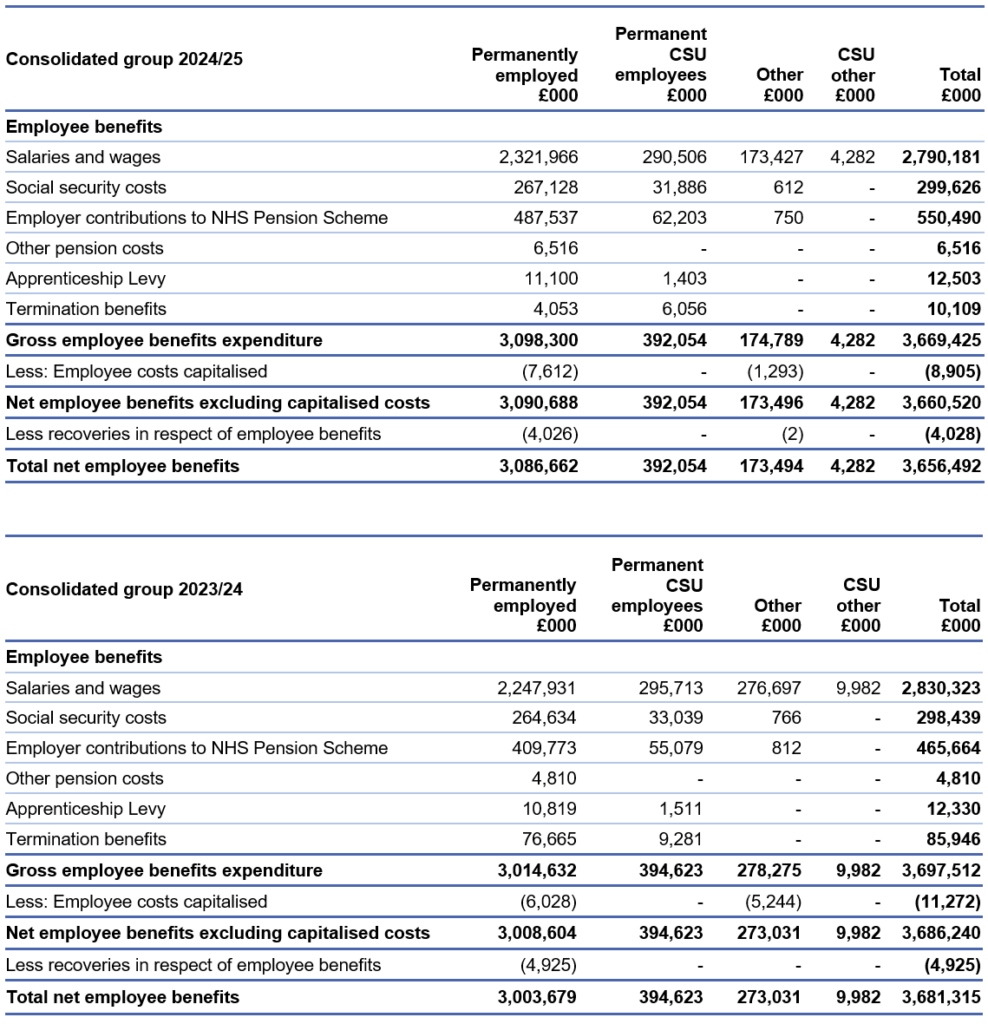
CSUs are part of NHS England and provide services to ICBs and other external bodies.
The employment contracts or secondment of almost all of these staff are held for NHS England on a “hosted basis” by the NHS Business Services Authority.
Exit packages, severance payments and off-payroll engagements
Expenditure on consultancy and contingent labour
Expenditure on consultancy is detailed in the Annual Accounts under Note 4: Operating expenses. NHS England and CSUs procured consultancy services worth £16.9 million during the financial year, a decrease of £260k since the previous year (2023/24: £17.1 million).
Across the group, there was a total spend of £48.4 million on consultancy services during the period, against £56.5 million the previous year.
Expenditure on contingent labour, including agency staff and secondees, is given in the employee benefits table on page 95, under the ‘other’ column.
Net expenditure for NHS England and CSUs in this area was £88 million in 2024/25, against £157 million in 2023/24. Across the group, there was a total spend of £179 million on contingent labour during the year, against £288.3 million the previous year.
Further detail on efficiency controls, and steps we have taken to improve procurement practices and compliance within NHS England during the year, can be found in our governance statement from page 67.
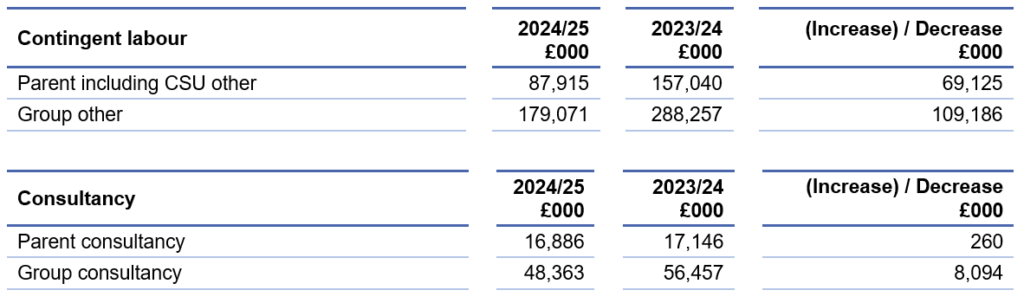
Off-payroll engagements
NHS England is committed to employing a capable, talented, and diverse on-payroll workforce to support the delivery of its business. It is recognised that in some specific circumstances the use of off-payroll workers (OPWs), working alongside our on-payroll workforce, can be helpful. For some of our time-limited programmes, short-term contracts are appropriate. The following tables identify OPWs engaged by NHS England at March 2025. OPWs engaged by ICBs are reported in ICB annual reports and published on their websites (NHS England » Integrated care boards in England).
Off-payroll engagements longer than 6 months
Off-payroll engagements on 31 March 2025, covering those earning more than £245 per day are as follows (the £245 threshold is set to approximate the minimum point of the pay scale for a Senior Civil Servant):
| Off-payroll engagements longer than 6 months | NHS England (number) | CSUs (number) | Total (number) |
|---|---|---|---|
|
Number of existing engagements as of 31 March 2025 |
1,071 |
31 |
1,102 |
|
Of which, the number that have existed: |
|
|
|
|
for less than 1 year at the time of reporting |
403 |
28 |
431 |
|
for between 1 and 2 years at the time of reporting |
356 |
3 |
359 |
|
for between 2 and 3 years at the time of reporting |
299 |
– |
299 |
|
for between 3 and 4 years at the time of reporting |
2 |
– |
2 |
|
for 4 or more years at the time of reporting |
11 |
– |
11 |
The reporting methodology has changed since the previous year to include individuals engaged via third party contracts in addition to agency workers.
The majority of the individuals reported above were engaged via third party contracts mainly undertaking software development and maintenance on the main digital platforms such as the NHS App.
All off-payroll engagements were subject to a risk-based assessment as to whether assurance was required that the individual was paying the right amount of tax and, where necessary, assurance has been sought.
New off-payroll engagements
New off-payroll engagements or those that reached 6 months in duration, between 1 April 2024 and 31 March 2025, for more than £245 per day are as follows (the £245 threshold is set to approximate the minimum point of the pay scale for a Senior Civil Servant):
| New off-payroll engagements | NHS England (number) | CSUs (number) | Total (number) |
|---|---|---|---|
|
Number of OPWs engaged during the year ended 31 March 2025 |
1,789 |
93 |
1,882 |
|
Of which: |
|
|
|
|
Number not subject to off payroll legislation. A worker that provides their services through their own limited company or another type of intermediary to the client will be subject to off-payroll legislation and the Department must undertake an assessment to determine whether that worker is in-scope of Intermediaries legislation (IR35) or out-of-scope for tax purposes. |
– |
– |
– |
|
Number subject to off-payroll legislation and determined as in-scope of IR35131 |
1,789 |
82 |
1,871 |
|
Number subject to off-payroll legislation and determined as out of scope of IR35131 |
– |
11 |
11 |
|
Number of engagements reassessed for compliance or assurance purposes during the year |
– |
– |
– |
|
Of which: |
|
|
|
|
Number of engagements that saw a change to IR35 status following review |
– |
– |
– |
Off-payroll board member/senior official engagement
Off-payroll engagements of Board members and/or senior officials with significant financial responsibility between 1 April 2024 and 31 March 2025 are shown in the table below:
| Off-payroll board member/senior official engagement | NHS England (number) | CSUs (number) | Total (number) |
|---|---|---|---|
|
Number of off-payroll engagements of Board members and/or senior officers with significant financial responsibility, during the financial year |
– |
– |
– |
|
Total number of individuals on-payroll and off-payroll who have been deemed ‘Board members and/or senior officials with significant financial responsibility’ during the financial year |
393 |
29 |
422 |
Details of exit packages agreed over the year are detailed in the following tables.
All contractual severance payments were subject to full external oversight by the DHSC.
Exit packages agreed during the year (subject to audit)
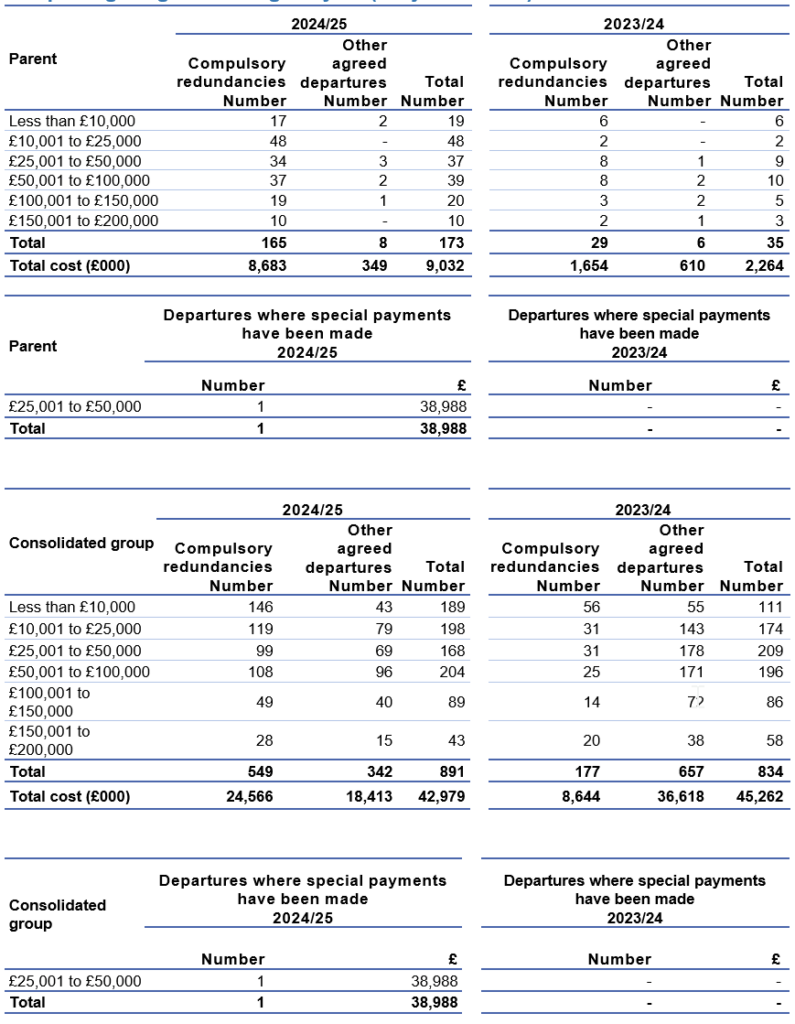
Analysis of other agreed departures (subject to audit)
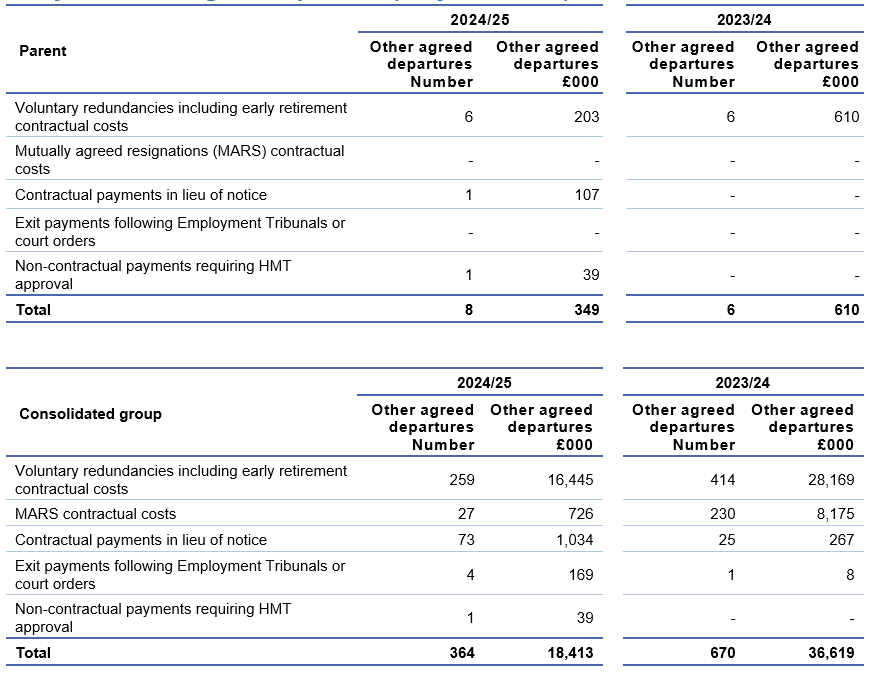
As a single exit package can be made up of several components, each of which will be counted separately in this table, the total number of exit packages will not necessarily match the total number in the table above.
These tables report the number and value of exit packages agreed in the financial year.
The expense associated with these departures may have been recognised in part or in full in a previous period.
Redundancy and other departure costs have been paid in accordance with the provisions of NHS England.
Exit costs are accounted for in accordance with relevant accounting standards and at the latest in full in the year of departure.
Where NHS England and ICBs have agreed early retirements, the additional costs are met by NHS England or the ICB and not by the NHS Pension Scheme and are included in the tables. Ill-health retirement costs are met by the NHS Pension Scheme and are not included in the tables.
The Remuneration Report includes the disclosure of exit payments payable to individuals named in that report.
People and Remuneration Committee
Detail on the role and activity of the People and Remuneration Committee is given in our Directors’ Report on page 52.
Percentage change in remuneration of highest paid director (subject to audit)
| Percentage change in remuneration of the highest paid director | Salary and allowances | Performance pay and bonuses |
|---|---|---|
|
The percentage change from the previous financial year in respect of the highest paid director |
0% |
0% |
|
The average percentage change from the previous financial year in respect of employees of the entity, taken as a whole |
6.88% |
0% |
The average percentage increase in salary and allowances from 2023/24 to 2024/25 can be explained by NHS England undergoing a mass organisational change following the merge with NHS Digital on 01 February 2023 and Health Education England on 01 April 2023.
This organisational change came into effect on 01 April 2024 and resulted in a change to NHS England’s organisational staff profile. In addition to organisational change an AFC pay award of 5% was implemented.
Pay ratio information (subject to audit)
Reporting bodies are required to disclose the relationship between the total remuneration of the highest-paid director/member in their organisation against the 25th percentile, median and 75th percentile of remuneration of the organisation’s workforce. Total remuneration of the employee at the 25th percentile, median and 75th percentile is further broken down to disclose the salary component.
The banded remuneration of the highest paid director/member in NHS England in the financial year 2024/25 was £265,000 to £270,000 (2023/24: £265,000-£270,000). The relationship to the remuneration of the organisation’s workforce is disclosed in the table below.
| 2024/25 | 25th percentile | Median | 75th percentile |
| Total remuneration (£) | 44,806 | 56,698 | 79,616 |
| Salary component of total remuneration (£) | 44,806 | 56,454 | 78,814 |
| Pay ratio information | 5.97:1 | 4.72:1 | 3.36:1 |
| 2023/24 | 25th percentile | Median | 75th percentile |
| Total remuneration (£) | 37,350 | 51,558 | 72,245 |
| Salary component of total remuneration (£) | 37,350 | 50,952 | 70,417 |
| Pay ratio information | 7.16:1 | 5.19:1 | 3.70:1 |
The pay ratio information for the 2024/25 financial year is consistent with the pay, reward and progression policies for the employees taken as a whole, due to applying all nationally mandated pay awards where applicable and adhering to the relevant pay progression principles.
In 2024/25, no employees received remuneration in excess of the highest-paid director/ member (2023/24: none). Remuneration ranged from £7,883 to £270,000 (2023/24: £7,883 to £270,000).
Total remuneration includes salary, non-consolidated performance-related pay, benefits-in-kind, but not severance payments. It does not include employer pension contributions and the cash equivalent transfer value (CETV) of pensions.
Policy on remuneration of senior managers
The framework for the remuneration of executive directors is set by the DHSC through the Executive Senior Mangers (ESM) pay framework for Arm’s Length Bodies (ALBs).
It is NHS England’s policy to pay salaries that are appropriate to recruit senior managers with the necessary skills, capability and experience for the effective running of a more than £191 billion organisation, while recognising the importance of demonstrating pay restraint at a time of considerable pressure on NHS finances. Recommending appropriate remuneration for executive directors was undertaken by the People and Remuneration Committee and the Nominations Committee. Final decisions are made by the DHSC ALB Remuneration Committee and HM Treasury, where appropriate.
Performance-related pay
The PRP arrangements for national (executive) directors are set out in the ESM pay framework for ALBs. They follow guidance prescribed by the DHSC and are in line with HM Treasury requirements. As a local policy decision, NHS England does not currently allocate any funding for PRP non-consolidated bonus payments. In recognition of the current economic climate and the need to provide effective system leadership for the NHS, the decision was taken by the Executive HR Group and the People and Remuneration Committee not to allocate funds for PRP non-consolidated bonus payments for 2024/25.
Secondees are subject to the terms and conditions of their employing organisation.
Policy on senior managers’ contracts
Contracts of employment for senior managers are open-ended and recurrent, unless otherwise specified. Notice periods follow the provisions of the ESM contract of employment, as applied by NHS England, of six months’ contractual notice.
Termination payments can only be authorised where they are contractual and, subject to the value involved, may still require further approval from the DHSC Governance and Assurance Committee.
Any proposed non-contractual special severance payment requires formal approval from the DHSC and HM Treasury.
Payments for loss of office (subject to audit)
No payments were made to any senior manager to compensate for loss of office in 2024/25.
Payments to past directors (subject to audit)
No payments have been made to past directors and no compensation has been paid on early retirement. This is subject to audit.
Senior managers’ service contracts
| Name and title | Date of appointment | Notice period | Provisions for compensation for early termination | Other details |
|---|---|---|---|---|
|
Amanda Pritchard |
1 August 2021 |
6 months |
Option to provide taxable pay in lieu |
Left NHS England 31 March 2025 |
|
Dame Emily Lawson |
1 November 2023 |
6 months |
Left COO post 31 March 2025 | |
|
Stephen Russell |
3 April 2023 |
6 months |
Left CDO post 31 March 2025 | |
|
Jacqueline Rock |
1 January 2022 |
6 months |
Left NHS England 31 December 2024 | |
|
Professor Sir Stephen Powis |
1 March 2018 |
6 months |
| |
|
Julian Kelly |
1 April 2019 |
6 months |
Left NHS England 31 March 2025 | |
|
Dame Ruth May Chief Nursing Officer |
7 January 2019 |
6 months |
Left CNO post 24 July 2024 | |
|
Duncan Burton Chief Nursing Officer for England |
25 July 2024 |
6 months |
| |
|
Dr Vinod Diwakar |
18 September 2023 |
6 months |
| |
|
Christopher Hopson |
13 June 2022 |
6 months |
| |
|
Navina Evans Chief Workforce Officer |
1 July 2022 |
6 months |
|
Remuneration (salary, benefits in kind and pensions) 2024/25 (subject to audit)
Name and title | (a) Salary (bands of £5,000) £000 | (b) Benefits in kind (taxable) to nearest £100 £s | (c) Performance pay and bonuses (bands of £5,000) £000 | (d) Long-term performance pay and bonuses (bands of £5,000) £000 | (e) Pension-related benefits (bands of £2,500)[1] £000 | (f) Total (a to e) (bands of £5,000) £000 |
|
Amanda Pritchard[2] |
385-390 |
0 |
0 |
0 |
10-12.5 |
395-400 |
|
Dame Emily Lawson[3] |
260-265 |
0 |
0 |
0 |
0 |
260-265 |
|
Stephen Russell[4] |
205-210 |
1,000 |
0 |
0 |
0 |
205-210 |
|
Jacqueline Rock[5] |
160-165 |
2,100 |
0 |
0 |
97.5-100 |
260-265 |
|
Professor Sir Stephen Powis |
240-245 |
0 |
0 |
0 |
0 |
240-245 |
|
Julian Kelly[6] |
230-235 |
0 |
0 |
0 |
55-57.5 |
290-295 |
|
Dame Ruth May[7] |
60-65 |
300 |
0 |
0 |
0 |
60-65 |
|
Duncan Burton[8] Chief Nursing Officer for England |
135-140 |
0 |
0 |
0 |
105-107.5 |
240-245 |
|
Dr Vinod Diwakar |
215-220 |
0 |
0 |
0 |
0 |
215-220 |
|
Christopher Hopson Chief Strategy Officer |
215-220 |
0 |
0 |
0 |
52.5-55 |
270-275 |
|
Navina Evans |
205-210 |
0 |
0 |
0 |
0 |
205-210 |
[1] The value of pension benefits accrued during the year is calculated as the real increase in pension multiplied by 20, less the contributions made by the individual. The real increase excludes increases due to inflation or any increase or decrease due to a transfer of pension rights. This value derived does not represent an amount that will be received by the individual. It is a calculation that is intended to provide an estimation of the potential benefit of being a member of the pension scheme.
[2] Amanda Pritchard left NHS England on 31 March 2025 and received a Pay in Lieu of Notice (PILON) payment of £105,000-£110,000 and a Lieu of Annual Leave payment of £5,000-£10,000. The remuneration figure noted in the above table reflects the total of these two payments, plus Amanda’s 2024/25 remuneration of £265,000-£270,000. However, the PILON and Lieu of Annual Leave payments were paid to Amanda during the 2025/26 reporting period.
[3] Dame Emily Lawson left the Chief Operating Officer post on 31 March 2025.
[4] Stephen Russell left the Chief Delivery Officer post on 31 March 2025. Stephen Russell’s benefit in kind relates to a Lease Car.
[5] Jacqueline Rock left NHS England on 31 December 2024. The full year equivalent salary is £215,000-£220,000. Jacqueline Rock’s benefit in kind relates to a Lease Car.
[6] Julian Kelly left NHS England on 31 March 2025 and received a Lieu of Annual Leave payment of £15,000-£20,000. The remuneration figure noted in the above table reflects the total of this payment, plus Julian’s 2024/25 remuneration of £215,000-£220,000. However, the Lieu of Annual Leave payment was paid to Julian during the 2025/26 reporting period.
[7] Dame Ruth May left the Chief Nursing Officer post on 24 July 2024. The full year equivalent salary is £190,000-£195,000. Dame Ruth May’s benefit in kind relates to a Lease Car.
[8] Duncan Burton commenced in post on 25 July 2024. The full year equivalent salary is £195,000-£200,000.
Remuneration (salary, benefits in kind and pensions) 2023/24 (subject to audit)
Name and title | (a) Salary (bands of £5,000) £000 | (b) Benefits in kind (taxable) to nearest £100 £s | (c) Performance pay and bonuses (bands of £5,000) £000 | (d) Long-term performance pay and bonuses (bands of £5,000) £000 | (e) Pension-related benefits (bands of £2,500)[1] £000 | (f) Total (a to e) (bands of £5,000) £000 |
|
Amanda Pritchard |
265-270 |
0 |
0 |
0 |
0 |
265-270 |
|
Sir David Sloman[2] |
95-100 |
0 |
0 |
0 |
0 |
95-100 |
|
Sir James Mackey[3] |
0 |
0 |
0 |
0 |
0 |
0 |
|
Dr Emily Lawson[4] |
110-115 |
0 |
0 |
0 |
0 |
110-115 |
|
Mark Cubbon[5] |
0-5 |
0 |
0 |
0 |
0 |
0-5 |
|
Stephen Russell[6] |
205-210 |
1,000 |
0 |
0 |
0 |
205-210 |
|
Jacqueline Rock[7] |
220-225 |
2,800 |
0 |
0 |
50-52.5 |
275-280 |
|
Professor Sir Stephen Powis |
240-245 |
0 |
0 |
0 |
0 |
240-245 |
|
Julian Kelly |
215-220 |
0 |
0 |
0 |
52.5-55 |
270-275 |
|
Dame Ruth May[8] |
180-185 |
1,600 |
0 |
0 |
0 |
180-185 |
|
Dr Tim Ferris[9] |
90-95 |
0 |
0 |
0 |
0 |
90-95 |
|
Dr Vinod Diwakar[10] |
110-115 |
0 |
0 |
0 |
12.5-15 |
120-125 |
Christopher Hopson Chief Strategy Officer |
215-220 |
0 |
0 |
0 |
50-52.5 |
265-270 |
|
Navina Evans |
205-210 |
0 |
0 |
0 |
0 |
205-210 |
[1] The value of pension benefits accrued during the year is calculated as the real increase in pension multiplied by 20, less the contributions made by the individual. The real increase excludes increases due to inflation or any increase or decrease due to a transfer of pension rights. This value derived does not represent an amount that will be received by the individual. It is a calculation that is intended to provide an estimation of the potential benefit of being a member of the pension scheme.
[2] Sir David Sloman’s salary was recharged to NHS England from the Royal Free London NHS Foundation Trust where he was also formally employed and retained a post. Sir David Sloman left NHS England on 03 September 2023. The full year equivalent salary is £230,000-£235,000.
[3] Sir James Mackey covered this post on an interim basis from 04 September 2023 to 31 October 2023 on an NHS assignment. Sir James Mackey’s salary costs were retained wholly by Northumbria NHS Foundation Trust where he was formally employed and retained a post.
[4] Dr Emily Lawson commenced in post on an interim basis on 01 November 2023. The full year equivalent salary is £250,000-£255,000.
[5] Mark Cubbon’s salary was recharged to NHS England from Portsmouth Hospitals NHS Trust where he was also formally employed and retained a post. Mark Cubbon left NHS England on 02 April 2023. The full year equivalent salary is £220,000-£225,000.
[6] Stephen Russell commenced in post on 03 April 2023. Stephen Russell’s benefit in kind relates to a Lease Car.
[7] Jacqueline Rock’s benefit in kind relates to a Lease Car.
[8] Dame Ruth May’s benefit in kind relates to a Lease Car.
[9] For the period 01 April 2023 to 09 May 2023 80% of the salary costs for Dr Tim Ferris were recharged to NHS England from Mass General Brigham Inc. where is he was also formally employed and retained a post, with NHS England directly funding the remaining 20%. For the period 10 May 2023 to 17 September 2023 NHS England directly funded 100% of the salary costs. Dr Tim Ferris left this post on 17 September 2023. The full year equivalent salary is £190,000-£195,000. NHS England also paid Mass General Brigham Inc. a retirement contribution of $0,000-$5,000.
[10] Dr Vinod Diwakar commenced in post on an interim basis on 18 September 2023. The full year equivalent salary is £205,000-£210,000.
Pension benefits (subject to audit)
Name and title | Real increase in pension at pension age (bands of £2,500) £000 | Real increase in pension lump sum at pension age (bands of £2,500) £000 | Total accrued pension at pension age on 31 March 2025 (bands of £5,000) £000 | Lump sum at pension age related to accrued pension on 31 March 2025 (bands of £5,000) £000 | CETV on 31 March 2025[1] £000 | Real Increase in CETV £000 | CETV on 31 March 2025 £000 | Employer’s contribution to partnership pension £000 |
|
Amanda Pritchard |
0-2.5 |
0 |
90-95 |
220-225 |
1,747 |
11 |
1,907 |
0 |
|
Dame Emily Lawson[2] |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Stephen Russell |
0 |
0 |
65-70 |
165-170 |
1,320 |
0 |
1,395 |
0 |
|
Jacqueline Rock[3] |
5-7.5 |
N/A |
15-20 |
N/A |
153 |
76 |
259 |
0 |
|
Professor Sir Stephen Powis[4] |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Julian Kelly |
2.5-5 |
N/A |
25-30 |
N/A |
331 |
43 |
422 |
0 |
|
Dame Ruth May[5] |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Duncan Burton[6] |
5-7.5 |
15-17.5 |
60-65 |
155-160 |
1,069 |
93 |
1,300 |
0 |
|
Dr Vinod Diwakar National Director of Transformation (Interim) |
0 |
0 |
90-95 |
245-250 |
2,151 |
0 |
2,270 |
0 |
|
Christopher Hopson |
2.5-5 |
N/A |
10-15 |
N/A |
120 |
43 |
197 |
0 |
|
Dr Navina Evans[7] |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
[1] As per previous submissions, the column CETV on 31 March 2025 is the uninflated value whereas the real increase in CETV is the employer-funded increase.
[2] Dame Emily Lawson chose not to be covered by the NHS Pension arrangements during the reporting period.
[3] Jacqueline Rock left NHS England on 31 December 2024, therefore the Pension Benefits disclosed are pro-rata for this period.
[4] Professor Sir Stephen Powis chose not to be covered by the NHS Pension arrangements during the reporting period.
[5] Dame Ruth May chose not to be covered by the NHS Pension arrangements during the reporting period.
[6] Duncan Burton commenced in post on 25 July 2024, therefore the Pension Benefits disclosed are pro-rata for this period.
[7] Dr Navina Evans chose not to be covered by the NHS Pension arrangements during the reporting period.
Cash equivalent transfer values (subject to audit)
A CETV is the actuarially assessed capital value of the pension scheme benefits accrued by a member at a particular point in time.
The benefits valued are the member’s accrued benefits and any contingent spouse’s (or other allowable beneficiary’s) pension payable from the scheme.
A CETV is a payment made by a pension scheme or arrangement to secure pension benefits in another pension scheme or arrangement when the member leaves a scheme and chooses to transfer the benefits accrued in their former scheme.
The pension figures shown relate to the benefits that the individual has accrued as a consequence of their total membership of the pension scheme, not just their service in a senior capacity to which disclosure applies.
The CETV figures and the other pension details include the value of any pension benefits in another scheme or arrangement which the individual has transferred into the NHS Pension Scheme. They also include any additional pension benefit accrued to the member as a result of their purchasing additional years of pension service in the scheme at their own cost. CETVs are calculated within the guidelines and framework prescribed by the Institute and Faculty of Actuaries.
Real increase in CETV
This reflects the increase in CETV effectively funded by the employer. It does not include the increase in accrued pension due to inflation or contributions paid by the employee (including the value of any benefits transferred from another scheme or arrangement) and uses common market valuation factors for the start and end of the period.
Pensions liability
Past and present employees are covered by the provisions of the NHS Pension Schemes. Details of the benefits payable and rules of the schemes can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions. Both the 1995/2008 and 2015 schemes are accounted for, and the scheme liability valued, as a single combined scheme. Both are unfunded defined benefit schemes that cover NHS employers, GP practices and other bodies, allowed under the direction of the Secretary of State for Health and Social Care in England and Wales. They are not designed to be run in a way that would enable NHS bodies to identify their share of the underlying scheme assets and liabilities. Therefore, each scheme is accounted for as if it were a defined contribution scheme: the cost to the NHS body of participating in each scheme is taken as equal to the contributions payable to that scheme for the accounting period.
In order that the defined benefit obligations recognised in the financial statements do not differ materially from those that would be determined at the reporting date by a formal actuarial valuation, the FReM requires that “the period between formal valuations shall be four years, with approximate assessments in intervening years.” An outline of these follows:
a) Accounting valuation
A valuation of scheme liability is carried out annually by the scheme actuary (currently the Government Actuary’s Department) as at the end of the reporting period. This utilises an actuarial assessment for the previous accounting period in conjunction with updated membership and financial data for the current reporting period and is accepted as providing suitably robust figures for financial reporting purposes. The valuation of the scheme liability as at 31 March 2025, is based on valuation data as at 31 March 2023, updated to 31 March 2025 with summary global member and accounting data. In undertaking this actuarial assessment, the methodology prescribed in IAS 19, relevant FReM interpretations, and the discount rate prescribed by HM Treasury have also been used.
The latest assessment of the liabilities of the scheme is contained in the Statement by the Actuary, which forms part of the annual NHS Pension Scheme Annual Report and Accounts. These accounts can be viewed on the NHS Pensions website and are published annually. Copies can also be obtained from The Stationery Office.
b) Full actuarial (funding) valuation
The purpose of this valuation is to assess the level of liability in respect of the benefits due under the schemes (considering recent demographic experience), and to recommend the contribution rate payable by employers.
The latest actuarial valuation undertaken for the NHS Pension Scheme was completed as at 31 March 2020. The results of this valuation set the employer contribution rate payable from 1 April 2024 to 23.7% of pensionable pay. The core cost cap cost of the scheme was calculated to be outside of the 3% cost cap corridor as at 31 March 2020. However, when the wider economic situation was taken into account through the economic cost cap cost of the scheme, the cost cap corridor was not similarly breached. As a result, there was no impact on the member benefit structure or contribution rates.
The 2024 actuarial valuation is currently being prepared and will be published before new contribution rates are implemented from April 2027.
Policy on remuneration of non-executive directors
The remuneration of non-executive directors is set by the DHSC on appointment and is non-pensionable. All non-executive directors are paid the same amount, except the Chair and Chair of ARAC, to reflect the equal time commitment expected from each non-executive director.
The Chair and Chair of ARAC are entitled to higher amounts to reflect the increased time commitment associated with their respective roles.
Some non-executive directors, including one of the Deputy Chairs, have opted to waive their contractual remuneration. Non-executive directors do not receive PRP or pensionable remuneration.
Non-executive director service contracts
| Name and title | Date of appointment | Unexpired term at 31 March 2025 | Notice period | Provisions for compensation for early termination | Other details |
|---|---|---|---|---|---|
|
Richard Meddings |
25 March 2022 |
0 months |
3 months |
None |
Left on |
|
Wol Kolade |
25 March 2022 |
0 months |
3 months |
None |
Waived entitlement to remuneration Left on 24 March 2025 |
|
Jeremy Townsend |
1 October 2020 |
18 months |
3 months |
None |
|
|
Michael Coupe |
1 January 2021 |
21 months |
3 months |
None |
|
|
Sir Andrew Morris |
1 July 2022 |
6 months |
3 months |
None |
Appointment term extended for 6 months |
|
Sir David Behan |
1 September 2022 |
0 months |
3 months |
None |
Left on |
|
Baroness Mary Watkins |
27 January 2023 |
10 months |
3 months |
None |
|
|
Professor Sir Simon Wessely |
27 January 2023 |
10 months |
3 months |
None |
|
|
Sir Mark Walport |
27 January 2023 |
10 months |
3 months |
None |
|
|
Mark Bailie |
19 February 2024 |
22.5 months |
3 months |
None |
|
|
Jane Ellison |
19 February 2024 |
22.5 months |
3 months |
None |
|
|
Sir Robert Lechler |
19 February 2024 |
22.5 months |
3 months |
None |
|
|
Professor Dame Helen Stokes-Lampard |
19 February 2024 |
0 months |
3 months |
None |
Left on 14 October 2024 |
Non-executive director remuneration (including salary entitlements)
Salaries and allowances 2024/25 (subject to audit)
| Name of non-executive director | (a) Salary (bands of £5,000) £000 | (b) Benefits in kind (taxable) rounded to nearest £100 £s | (c) Performance pay and bonuses (bands of £5,000) £000 | (d) Long-term performance pay and bonuses (bands of £5,000) £000 | (e) Pension-related benefits to the nearest £1,000[1] £000 | (f) Total (a to e) (bands of £5,000) £000 |
|---|---|---|---|---|---|---|
|
Richard Meddings[2] |
60-65 |
0 |
0 |
0 |
N/A |
60-65 |
|
Wol Kolade[3] |
0 |
0 |
0 |
0 |
N/A |
0 |
|
Jeremy Townsend |
10-15 |
0 |
0 |
0 |
N/A |
10-15 |
|
Michael Coupe |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Andrew Morris |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir David Behan[4] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Baroness Mary Watkins |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Professor Sir Simon Wessely |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Mark Walport |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Mark Bailie[5] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Jane Ellison |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Robert Lechler |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Professor Dame Helen Stokes-Lampard[6] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
[1] Non-executive directors do not receive pensionable remuneration and therefore have no pension-related benefits
[2] Richard Meddings donated 50% of his non-executive director remuneration to charity via NHS England’s Give As You Earn scheme during the reporting period.
[3] Wol Kolade waived his entitlement to non-executive director remuneration. Wol Kolade left NHS England on 24 March 2025.
[4] Sir David Behan left NHS England on 31 August 2024. The full-year equivalent salary is £5,000-£10,000.
[5] Mark Bailie donated 100% of his non-executive director remuneration to charity via NHS England’s Give As You Earn scheme during the reporting period.
[6] Professor Dame Helen Stokes-Lampard left NHS England on 14 October 2024. The full-year equivalent salary is £5,000-£10,000.
Salaries and allowances 2023/24 (subject to audit)
| Name of non-executive director | (a) Salary (bands of £5,000) £000 | (b) Benefits in kind (taxable) rounded to nearest £100 £s | (c) Performance pay and bonuses (bands of £5,000) £000 | (d) Long-term performance pay and bonuses (bands of £5,000) £000 | (e) Pension-related benefits to the nearest £1,000[1] £000 | (f) Total (a to e) (bands of £5,000) £000 |
|---|---|---|---|---|---|---|
|
Richard Meddings[2] |
60-65 |
0 |
0 |
0 |
N/A |
60-65 |
|
Wol Kolade[3] |
0 |
0 |
0 |
0 |
N/A |
0 |
|
Jeremy Townsend |
10-15 |
0 |
0 |
0 |
N/A |
10-15 |
|
Laura Wade-Gery[4] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Rakesh Kapoor[5] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Susan Kilsby[6] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Michael Coupe |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Professor Sir Munir Pirmohamed[7] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Andrew Morris |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir David Behan |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Baroness Mary Watkins |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Professor Sir Simon Wessely |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Mark Walport |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Mark Bailie[8] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Jane Ellison[9] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Sir Robert Lechler[10] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Professor Dame Helen Stokes-Lampard[11] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
[1] Non-executive directors do not receive pensionable remuneration and therefore have no pension-related benefits
[2] Richard Meddings donated 100% of his non-executive director remuneration to charity via NHS England’s Give As You Earn scheme for the period 01 April 2023 to 31 October 2023, and 50% of his non-executive director remuneration from 01 November 2023.
[3] Wol Kolade waived his entitlement to non-executive director remuneration.
[4] Laura Wade-Gery left NHS England on 30 June 2023. The full-year equivalent salary is £5,000-£10,000.
[5] Rakesh Kapoor left NHS England on 31 December 2023. The full-year equivalent salary is £5,000-£10,000.
[6] Susan Kilsby left NHS England on 31 December 2023. The full-year equivalent salary is £5,000-£10,000.
[7] Professor Sir Munir Pirmohamed left NHS England on 31 December 2023. The full-year equivalent salary is £5,000-£10,000.
[8] Mark Bailie joined NHS England on 19 February 2024. The full-year equivalent salary is £5,000-£10,000. Mark Bailie donated 100% of his non-executive director remuneration to charity via NHS England’s Give As You Earn scheme.
[9] Jane Ellison joined NHS England on 19 February 2024. The full-year equivalent salary is £5,000-£10,000.
[10] Sir Robert Lechler joined NHS England on 19 February 2024. The full-year equivalent salary is £5,000-£10,000.
[11] Professor Dame Helen Stokes-Lampard joined NHS England on 19 February 2024. The full-year equivalent salary is £5,000-£10,000.
Parliamentary accountability and audit report
All elements of this report are subject to audit.
Remote contingent liabilities
There were no remote contingent liabilities.
Notation of gifts over £300,000
NHS England made no political or charitable donations of gifts during 2024/25.
Regularity of expenditure: Losses and special payments
Losses and special payments are items that Parliament would not have contemplated when it agreed funds for the health service or passed legislation. By their nature they are items that ideally should not arise and are therefore subject to special control procedures compared to the generality of payments. They are divided into different categories, which govern the way that individual cases are handled.
Details of any losses and special payments relating to ICBs can be found within individual ICBs annual reports which are published on ICB websites. A list of ICBs along with links to their websites, can be found on the NHS England website.
Losses
The total number of NHS England losses cases, and their total value, was as follows:
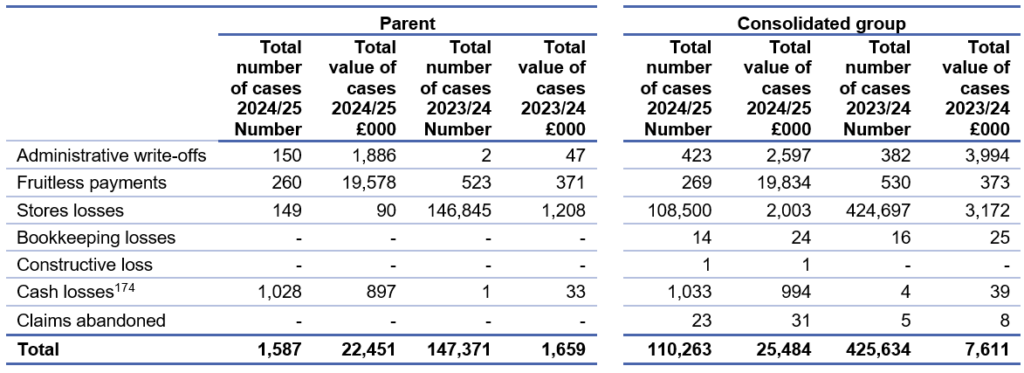
2024/25 Disclosure: Administrative write off
£1 million – This relates to irrecoverable dental debts that were owed due to underperformance on the dental contracts.
£0.5 million – This write off relates to 25 GP irrecoverable aged debts due to being beyond the 6-year recovery period or dissolution of companies following liquidation.
2024/25 Disclosure: Fruitless payments
£17 million – This payment is where continuing health care should have been awarded to individuals and when the payments were made including redress values, the tax liability was not deducted by CCG’s and paid over to HMRC which is now due following various court proceedings.
£2.2 million – This relates to payroll worker tax compliance within the former Health Education England which has now transferred to NHS England upon the Health Education England and NHS England merger.
2024/25 Disclosure: Store losses
£2 million – Of this £1.9 million relates to various stock items that cannot be utilised in healthcare facilities as the stock has reached the manufacturers expiry date and therefore requires writing off.
2024/25 Disclosure: Cash losses
£0.9 million – These debts relate to irrecoverable bursaries that have been paid to eligible medical or dental students to cover costs incurred by students that were due to be paid back from scenarios such as the student leaving the course early.
2023/24 Disclosure: Store losses
£1.2 million – there is one instance comprising of multiple individual items for £1.1 million that relates to various stock items that cannot be utilised in healthcare facilities, as the stock has reached the manufacturer’s expiry date and therefore requires writing off.
Special payments
The total number of NHS England special payments cases, and their total value, was as follows:
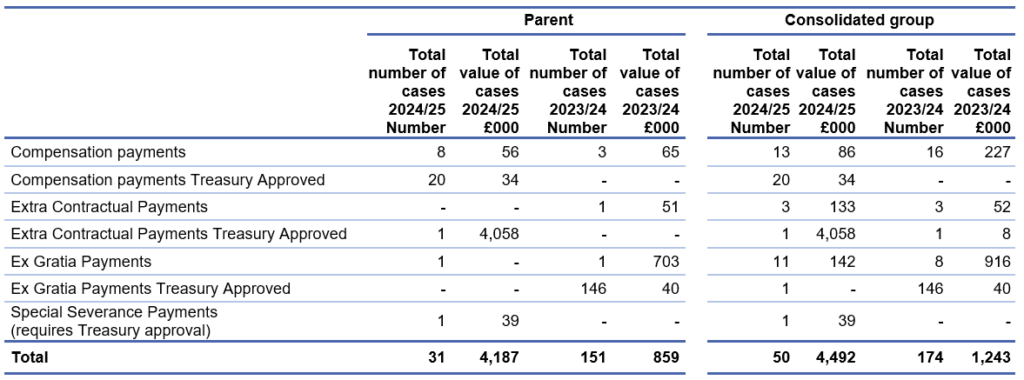
2024/25 Extra Contractual Payments
£4,058k – This is a claim for damages for breach of the General Ophthalmic Services contract brought by a supplier against NHS England.
2024/25 Special Severance Payments
There was 1 special severance payment that did not have HMT approval as follows:
NHS South, Central and West CSU
During 2024/25, the CSU has paid one special severance payment in the parent account for £38,988. It relates to a settlement agreement payment made to the individual. The payment was not approved by NHS England or HMT and is therefore irregular.
The payment noted above is also included in the Exit Package disclosures from page 100.
2023/24 Ex Gratia Payments
£703k – This case relates to the IR35 employment status assessments for all relevant OPWs engagements relating to the financial periods 2017 to 2019. 159 engagements of OPWs were deemed to have been subject to IR35 regulations and the payment due reflects the outcome of the assessment carried out. This payment relates to the negotiated settlement of the sum including interest due to HMRC in relation to those OPWs who based on a more recent understanding of HMRC interpretation of the rules and indicators, may have been incorrectly deemed out-of-scope.
Cost allocation and setting of charges
NHS England certifies that it has complied with the HM Treasury guidance on cost allocation and the setting of charges. The following table provides details of income generation activities whose full cost exceeded £1 million or was otherwise material:
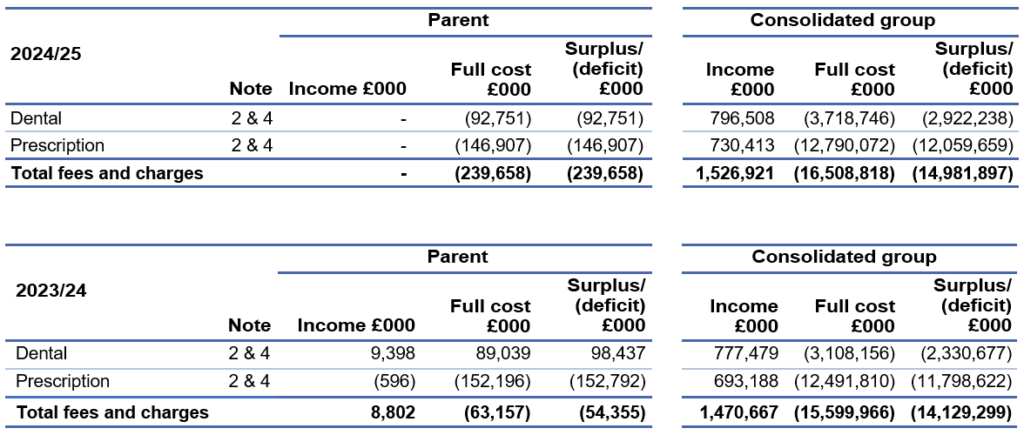
The fees and charges information in this note is provided in accordance with section 6.7.1 of the Government FReM. It is provided for fees and charges purposes and not for IFRS 8 purposes. The financial objective of prescription and dental charges is to collect charges only from those patients that are eligible to pay.
Prescription charges are a contribution to the cost of pharmaceutical services including the supply of drugs. In 2024/25, the NHS prescription charge for each medicine or appliance dispensed was £9.90. However, around 95% of prescription items (Prescription cost analysis – England 2023/24 Additional Tables”, “Table 4A”) are dispensed without charge each year where patients are exempt from charges or hold a pre-payment certificate.
In 2024/25 pre-payment certificates were charged at £32.05 for three months or £114.50 for a year. A number of other charges were payable for wigs and fabric supports.
Those who are not eligible for exemption are required to pay NHS dental charges which fall into three bands depending on the level and complexity of care provided. From 1st April 2024, the charge for Band 1 treatments was £26.80, for Band 2 was £73.50 and for Band 3 was £319.10. Prior to this uplift the charge for Band 1 treatments was £25.80, for Band 2 was £70.70 and for Band 3 was £306.80.
The certificate of the Comptroller and Auditor General to the Houses of Parliament
Opinion on financial statements
I certify that I have audited the financial statements of NHS England and its group for the year ended 31 March 2025 under the National Health Service Act 2006 and the Health and Social Care Act 2012.
The financial statements comprise NHS England and its group’s
- Statement of Financial Position as at 31 March 2025;
- Statement of Comprehensive Net Expenditure, Statement of Cash Flows and Statement of Changes in Taxpayers’ Equity for the year then ended; and
- the related notes including the significant accounting policies.
The financial reporting framework that has been applied in the preparation of the group financial statements is applicable law and UK adopted International Accounting Standards.
In my opinion, the financial statements:
- give a true and fair view of the state of NHS England and its group’s affairs as at 31 March 2025 and their total net expenditure for the year then ended; and
- have been properly prepared in accordance with the National Health Service Act 2006 and the Health and Social Care Act 2012 and Secretary of State directions issued thereunder.
Opinion on regularity
In my opinion, in all material respects, the income and expenditure recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
Basis for opinions
I conducted my audit in accordance with International Standards on Auditing (UK) (ISAs UK), applicable law and Practice Note 10 Audit of Financial Statements and Regularity of Public Sector Bodies in the United Kingdom (2024). My responsibilities under those standards are further described in the Auditor’s responsibilities for the audit of the financial statements section of my certificate.
Those standards require me and my staff to comply with the Financial Reporting Council’s Revised Ethical Standard 2019. I am independent of NHS England and its group in accordance with the ethical requirements that are relevant to my audit of the financial statements in the UK. My staff and I have fulfilled our other ethical responsibilities in accordance with these requirements.
I believe that the audit evidence I have obtained is sufficient and appropriate to provide a basis for my opinion.
Conclusions relating to going concern
In auditing the financial statements, I have concluded that NHS England and its group’s use of the going concern basis of accounting in the preparation of the financial statements is appropriate.
Based on the work I have performed, I have not identified any material uncertainties relating to events or conditions that, individually or collectively, may cast significant doubt on NHS England and its group’s ability to continue as a going concern for a period of at least twelve months from when the financial statements are authorised for issue.
My responsibilities and the responsibilities of the Accounting Officer with respect to going concern are described in the relevant sections of this certificate.
The going concern basis of accounting for NHS England and its group is adopted in consideration of the requirements set out in HM Treasury’s Government Financial Reporting Manual, which requires entities to adopt the going concern basis of accounting in the preparation of the financial statements where it is anticipated that the services which they provide will continue into the future.
Other Information
The other information comprises information included in the Annual Report but does not include the financial statements and my auditor’s certificate thereon. The Board and Accounting Officer are responsible for the other information.
My opinion on the financial statements does not cover the other information and, except to the extent otherwise explicitly stated in my certificate, I do not express any form of assurance conclusion thereon.
My responsibility is to read the other information and, in doing so, consider whether the other information is materially inconsistent with the financial statements or my knowledge obtained in the audit, or otherwise appears to be materially misstated.
If I identify such material inconsistencies or apparent material misstatements, I am required to determine whether this gives rise to a material misstatement in the financial statements themselves. If, based on the work I have performed, I conclude that there is a material misstatement of this other information, I am required to report that fact.
I have nothing to report in this regard.
Opinion on other matters
In my opinion the part of the Remuneration and Staff Report to be audited has been properly prepared in accordance with Secretary of State directions issued under the National Health Service Act 2006 and the Health and Social Care Act 2012.
In my opinion, based on the work undertaken in the course of the audit:
- the parts of the Accountability Report subject to audit have been properly prepared in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012.
- the information given in the Performance and Accountability Reports for the financial year for which the financial statements are prepared is consistent with the financial statements and is in accordance with the applicable legal requirements.
Matters on which I report by exception
In the light of the knowledge and understanding of NHS England and its group’s and its environment obtained in the course of the audit, I have not identified material misstatements in the Performance and Accountability Reports.
I have nothing to report in respect of the following matters which I report to you if, in my opinion:
- adequate accounting records have not been kept by NHS England and its group or returns adequate for my audit have not been received from branches not visited by my staff; or
- I have not received all of the information and explanations I require for my audit; or
- the financial statements and the parts of the Accountability Report subject to audit are not in agreement with the accounting records and returns; or
- certain disclosures of remuneration specified by HM Treasury’s Government Financial Reporting Manual have not been made or parts of the Remuneration and Staff Report to be audited is not in agreement with the accounting records and returns; or
- the Governance Statement does not reflect compliance with HM Treasury’s guidance.
Responsibilities of the Board and Accounting Officer for the financial statements
As explained more fully in the Statement of Accounting Officer’s Responsibilities, the board and Accounting Officer are responsible for:
- maintaining proper accounting records;
- providing the C&AG with access to all information of which management is aware that is relevant to the preparation of the financial statements such as records, documentation and other matters;
- providing the C&AG with additional information and explanations needed for his audit;
- providing the C&AG with unrestricted access to persons within NHS England and its group from whom the auditor determines it necessary to obtain audit evidence;
- ensuring such internal controls are in place as deemed necessary to enable the preparation of financial statement to be free from material misstatement, whether due to fraud or error;
- preparing financial statements which give a true and fair view in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012;
- preparing the annual report, which includes the Remuneration and Staff Report, in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012; and
- assessing NHS England and its Group’s ability to continue as a going concern, disclosing, as applicable, matters related to going concern and using the going concern basis of accounting unless the Accounting Officer anticipates that the services provided by NHS England and its group will not continue to be provided in the future.
Auditor’s responsibilities for the audit of the financial statements
My responsibility is to audit, certify and report on the financial statements in accordance with the National Health Service Act 2006 and the Health and Social Care Act 2012.
My objectives are to obtain reasonable assurance about whether the financial statements as a whole are free from material misstatement, whether due to fraud or error, and to issue a certificate that includes my opinion. Reasonable assurance is a high level of assurance but is not a guarantee that an audit conducted in accordance with ISAs (UK) will always detect a material misstatement when it exists. Misstatements can arise from fraud or error and are considered material if, individually or in the aggregate, they could reasonably be expected to influence the economic decisions of users taken on the basis of these financial statements.
Extent to which the audit was considered capable of detecting non-compliance with laws and regulations including fraud
I design procedures in line with my responsibilities, outlined above, to detect material misstatements in respect of non-compliance with laws and regulations, including fraud. The extent to which my procedures are capable of detecting non-compliance with laws and regulations, including fraud is detailed below.
Identifying and assessing potential risks related to non-compliance with laws and regulations, including fraud
In identifying and assessing risks of material misstatement in respect of non-compliance with laws and regulations, including fraud, I:
- considered the nature of the sector, control environment and operational performance including the design of NHS England and its group’s accounting policies, key performance indicators and performance incentives.
- inquired of management, NHS England’s head of internal audit and those charged with governance, including obtaining and reviewing supporting documentation relating to NHS England and its group’s policies and procedures on:
- identifying, evaluating and complying with laws and regulations;
- detecting and responding to the risks of fraud; and
- the internal controls established to mitigate risks related to fraud or non-compliance with laws and regulations including NHS England and its group’s controls relating to NHS England’s compliance with the National Health Service Act 2006, Health and Social Care Act 2012, Health and Care Act 2022 and Managing Public Money.
- inquired of management, NHS England’s head of internal audit and those charged with governance whether:
- they were aware of any instances of non-compliance with laws and regulations;
- they had knowledge of any actual, suspected, or alleged fraud;
- discussed with the engagement team regarding how and where fraud might occur in the financial statements and any potential indicators of fraud.
As a result of these procedures, I considered the opportunities and incentives that may exist within NHS England and its group for fraud and identified the greatest potential for fraud in the following areas: revenue recognition, posting of unusual journals, complex transactions, bias in management estimates. In common with all audits under ISAs (UK), I am required to perform specific procedures to respond to the risk of management override.
I obtained an understanding of NHS England and its group’s framework of authority and other legal and regulatory frameworks in which NHS England and its group operates. I focused on those laws and regulations that had a direct effect on material amounts and disclosures in the financial statements or that had a fundamental effect on the operations of NHS England and its group. The key laws and regulations I considered in this context included the National Health Service Act 2006, Health and Social Care Act 2012, Health and Care Act 2022, Managing Public Money, employment law, tax legislation, relevant legislation relating to fees charged by the NHS England, and regulations relating to suspension payments to suspended medical practitioners.
Audit response to identified risk
To respond to the identified risks resulting from the above procedures:
- I reviewed the financial statement disclosures and testing to supporting documentation to assess compliance with provisions of relevant laws and regulations described above as having direct effect on the financial statements;
- I enquired of management and the Audit and Risk Assurance Committee concerning actual and potential litigation and claims;
- I reviewed minutes of meetings of those charged with governance and the Board and internal audit reports; and
- I addressed the risk of fraud through management override of controls by testing the appropriateness of journal entries and other adjustments; assessing whether the judgements on estimates are indicative of a potential bias; and evaluating the business rationale of any significant transactions that are unusual or outside the normal course of business.
I communicated relevant identified laws and regulations and potential risks of fraud to all engagement team members and remained alert to any indications of fraud or non-compliance with laws and regulations throughout the audit.
A further description of my responsibilities for the audit of the financial statements is located on the Financial Reporting Council’s website at: www.frc.org.uk/auditorsresponsibilities.
This description forms part of my certificate.
Other auditor’s responsibilities
I am required to obtain sufficient and appropriate audit evidence to give reasonable assurance that the expenditure and income recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
I communicate with those charged with governance regarding, among other matters, the planned scope and timing of the audit and significant audit findings, including any significant deficiencies in internal control I identify during my audit.
Report
I have no observations to make on these financial statements.
Gareth Davies
28 October 2025
Comptroller and Auditor General
National Audit Office, 157-197 Buckingham Palace Road, Victoria, London SW1W 9SP

