Appendix 1: How we delivered against the government’s mandate to the NHS
The government’s mandate to NHS England sets out high-level priorities and objectives the organisation must seek to achieve. For the financial year 2024/25, NHS England had objectives under two mandates: the first originally set in 2023 by the previous government, and the most recent mandate published on 30 January 2025. This assessment covers both the objectives within the 2023 mandate and those included in the current 2025 mandate, using data between April 2024 to March 2025.
The government’s 2023 mandate set out three priorities: to cut NHS waiting lists and recover performance; support the workforce through training, retention and modernising the way staff work; and to deliver recovery using data and technology. The government’s 2025 mandate sets out five priorities: reform to cut waiting lists; reform to improve primary care access; reform to improve UEC; reform to the operating model; and reform to drive efficiency and productivity.
In many cases the priorities and objectives overlapped across the two mandates. In these areas, assessment was consolidated against both, and a summary is included below.
Elective Care and Diagnostics
In 2024/25, NHS England made some progress in tackling the persistent issue of long elective care waiting times. From March 2024 to March 2025, the overall waiting list fell from 7.5 million to 7.4 million, with reductions in long waits: 65-week waiters dropped by 85%, and 52-week waiters by 42% compared to March 2024. Additionally, from March 2024 to March 2025, performance against the 18-week standard improved from 57.2% to 59.8%. However, this has not met the standards set out in the NHS Constitution.
The NHS continued to increase theatre capacity in 2024/25. As of April 2025, there are 116 elective surgical hubs operational across England, including 29 which are Targeted Investment Fund funded. 44 surgical hubs have so far been accredited for clinical and operational excellence. We are currently in the process of running cohorts 7/8 with the expectation of accreditation being awarded in April 2025.
Diagnostic wait times also improved, 18.4% of patients on the diagnostic waiting list in March 2025 had still been waiting more than 6 weeks. This compared to 21.9% in March 2024. The rollout of CDCs exceeded the ambition of 160 set out in the Elective Recovery Plan (February 2022), with 169 CDC sites operational by March 2025. CDCs delivered 6.8 million additional tests in 2024/25. These included over 1 million CT scans and 900,000 physiological tests.
Urgent and Emergency Care
Significant pressures in UEC persisted in 2024/25. In 2024/25 capital incentives supported improvements in high-performing A&Es, the 2024/25 Additional Capacity Targeted Investment Fund scheme distributed £150 million of capital to support improvements, and the Rapid Improvement Offer programme supported challenged acute trusts with the longest A&E delays. A&E and ambulance metrics showed modest improvements despite increased demand.
The 4-hour A&E performance improved marginally to 75% in 2024/25 (2023/24: 74%).
In 2024/25 national category 2 ambulance response times reduced by 1 minute, compared to 2023/24, but remains almost double the 18-minute target at over 35 minutes.
NHS England met its target to add 5,000 extra beds to the permanent bed base to improve capacity and deployed 800 new ambulances. Virtual wards also now provide nearly 13,000 beds. Challenges in delayed discharges were tackled through the Better Care Fund and new discharge metrics.
The 2025/26 UEC Delivery Plan recognises the ongoing challenges in UEC delivery and focuses on improving flow through hospitals, reducing ambulance handover times, and improving patient discharge processes, and is aligned with the 10-Year Health Plan.
Data and technology
By March 2025, 91% of NHS Trusts had implemented an EPR. Over 75% of adult social care providers have a digital care plan and have adopted Digital Social Care Records, covering 85% of CQC registered adult social care recipients.
The NHS FDP enables NHS organisations to bring together operational data. The NHS FDP began roll-out to NHS trusts in April 2024. By March 2025, 108 trusts and 40 ICBs had formally signed up to implement the platform, and 72 trusts and 39 ICBs have been onboarded.
Early benefits within the trusts that have adopted FDP products include 70,000 inpatient and 205,000 outpatients wait list removals and an 18% reduction in long-stay discharge delay days.
Usage of the NHS App by patients to manage prescriptions, access records, manage primary and secondary care appointments and communications all significantly increased this year. Compared to March 2024, in March 2025, the number of prescriptions managed through the NHS App totalled 5.5 million, up 49%, the number of records accessed through the NHS App totalled 24.6 million, up 70%, and the number of primary care appointments managed through the NHS App was 415,000 plus 2.4 million online consultation interactions, up 36% and 56% respectively. In secondary care, the number of secondary care appointments managed through the NHS App totalled 4.5 million, up 98%.
Primary care
Primary care continues to face high demand and workforce pressures. Between March 2024 and March 2025, there was a 3.7% increase in GP appointments (including COVID-19 vaccinations). 88.1% of appointments not usually booked in advance, took place within 14 days and 44.2% of all appointments on the same day. 99.9% of the total GP estate now uses digital telephony and over 98% of practices are using online consultation, appointment booking and messaging systems.
Mental health services
Mental health services access expanded: 655,000 adults, 63,000 perinatal women, and 822,000 children and young people accessed services in 2024/25. Eating disorder referral targets were met for over 73% of cases.
All ICBs have three-year plans for local mental health inpatient redesign in line with an evidence-based Commissioning Framework. 61 providers of NHS-commissioned mental health inpatient services are in receipt of a national culture change improvement programme, the Culture of Care Programme, to support delivery of national standards.
Community-based care
On 30th January 2025, 2025/26, Neighbourhood Health Guidelines were published[1] alongside the 2025/26 NHS Planning Guidance and the 2025/26 Better Care Fund policy framework. These guidelines asked systems to standardise and scale the six core components of Neighbourhood Health in 2025/26, as set out in the guidelines.
Access to community mental health services has improved. In the year to February 2025, 654,679 (February 2024: 599,320) adults accessed community mental health services with two or more care contacts.
Urgent Community Response referrals averaged 154 per 100,000 in 2024/25, with 83% seen within two hours. Self-referrals reached 255,000 in January 2025.
By February 2025 community pharmacy was delivering an increased number of clinical pathway consultations, with the monthly data evidencing performance exceeding Pharmacy First targets for oral contraception consultations and blood pressure checks.
In November 2024, NHS England published Insightful Board guidance[2] for providers and ICBs. ICBs have a unique role in supporting wider primary and community care working to be sustainable, and the Insightful Board documents support that by providing clarity around the critical information boards need to understand their organisations and plan appropriate care for their local population.
Cancer services
One-year survival for people diagnosed with cancer in 2020 is 74.6%, and five-year survival for people diagnosed in 2016 is 55.7%. Performance against the Faster Diagnosis Standard (a person should have cancer ruled out or receive a diagnosis within 28 days of an urgent cancer referral) improved from 77.3% in March 2024 to 78.9% in March 2025, exceeding the 75% standard. Performance against the 62-day treatment standard improved from 68.9% to 71.4% between March 2024 and March 2025.
The proportion of cancers diagnosed at stage 1 and 2 rose to 59.1% by February 2025 which is up from 57.6% as of February 2024 and up from 55.9% in February 2020.[3] This equates to an estimated 8,800 more stage 1 and 2 cancer diagnoses in the 12 months to February 2025 compared to pre-pandemic. NHS lung cancer screening continues to roll out, with over 3,000 lung cancers diagnosed in 2024/25, an increase from 2,000 in 2023/24. 75% of cancers diagnosed through the programme are caught at an early stage, compared to 29% outside of the programme.
The following objective was only included in the 2023 mandate:
Workforce growth and retention
In 2024/25, 7,830 medical school places were offered, with an increase to 8,180 planned for 2025/26.[4] Nursing and midwifery course applications rose by 6% compared to pre-pandemic levels. Over 500 pharmacy technicians were trained through a new apprenticeship. Amendments to regulations in June 2024 enabled dental hygienists and therapists to administer and supply specified medicines.
The following objectives were only included in the 2025 mandate:
Reform to the operating model
The 2025 mandate includes an additional objective to reform the NHS operating model.[5]
Since February 2025, NHS England has replaced the Oversight and Assessment Framework with the National Oversight Framework (previously the NHS Performance Assessment Framework)[6], which segments organisations from one to five based on metrics and benchmarks. Segment scores influence intervention levels and capital freedoms. Specific proposals for capital freedoms were published in the 2025/26 capital planning guidance.[7]
The Very Senior Managers Pay Framework[8] was revised to provider a stronger link between pay and operational performance by rewarding those who successfully improve performance and penalising those who are persistently failing.
Reform to drive efficiency and productivity
In 2024/25 NHS England worked with the DHSC and systems to improve productivity, efficiency and strengthen financial discipline. NHS England refreshed its oversight system to reflect lessons learned from 2023/24 including a revised risk-reporting system for ICBs and providers. NHS England also worked with systems to plan ahead of the year, manage down expenditure and deliver in year efficiencies, including through the targeted Investigation and Intervention programme and strengthening financial controls in quarter 4 2024/25. Whilst significant efficiencies, other cost savings and underspends were delivered across NHS England, ICBs and many NHS providers, these did not entirely offset overspends elsewhere in the NHS providers’ sector. This meant that across the NHS budget, NHS England delivered Non-Ringfenced Resource Departmental Expenditure Limit overspend equivalent to less than 0.05% of NHS England’s budget, which the DHSC agreed to absorb within the wider group budget to ensure that once again the DHSC was able to manage spending within Parliamentary approved limits.
NHS England is now working closely with the DHSC on a finance reset in 2025/26, to strengthen financial controls and discipline across NHS systems, building on the new intervention regime, analysis of spend in the most financially challenged systems and a strengthened approach to ensure systems’ plans for 2025/26 are balanced.
Appendix 2: Meeting our Public Sector Equality Duty
In May 2024, NHS England’s Board approved and published NHS England’s equality objectives and targets for 2024/25 and for 2025/26. Progress was reviewed during 2024/25 and in May 2025, and NHS England’s Board considered a paper[9] recommending approval and publication of a review report for 2024/25.[10] The Board also approved updated equality objectives and targets for 2025/26.[11]
In developing our equality objectives and targets, we are required to focus on the Equality Act (2010)’s nine protected characteristics[12] where there is evidence of a need to take strategic action to address discrimination or other matters that are unlawful, advance equality of opportunity, or foster good relations.
The 2024/25 review report demonstrates how NHS England continued to meet our statutory requirements under the Equality Act 2010’s Public Sector Equality Duty[13] and the associated Specific Equality Duties[14] (SEDs). Central to these statutory requirements is the duty to publish equality information annually. The full 2024/25 review report is available on NHS England’s website[15] and provides a range of key equality information as of 31 March 2025, as required by the SEDs, including:
- planned changes to employment and equality legislation coming into force later in 2025/26 or 2026/27[16]
- an explanation of the changing context which will affect NHS England in the next year as the organisation will cease to exist as a separate legal entity and will integrate to the DHSC[17]
- four recommendations on what may be done in 2025/26 to balance the impact of these changes to the SEDs[18]
- a summary assessment of performance against our eight equality objectives and associated 2024/25 targets[19], along with further information[20] on work undertaken by NHS England during the reporting period.
Appendix 3: Reducing health inequalities
During 2024/25, NHS England continued to discharge its statutory, governance and delivery support responsibilities for health inequalities.
Our strategic approach to reducing healthcare inequalities
Our work across 2024/25 supported ICSs and NHS providers to take further action on the five priority areas for tackling healthcare inequalities:
Restore NHS services inclusively
Following the publication of the Delivery Plan for Recovering UEC Services[21], we now have 83% coverage of High Intensity Use services across Type 1 Emergency Departments (EDs) across England, reflecting the commitment we set out in the UEC Recovery Plan.
We facilitated the implementation of the ‘Framework for NHS action on Inclusion Health’, promoting improved healthcare access and experiences for socially excluded groups.
The framework was referenced in the 2024/25 NHS England Priorities and Planning Guidance, supporting implementation by ICBs. To support this, we developed an ICB action learning network to identify and share common success factors.
We established a Coastal Navigators Network and Accelerator programme in collaboration with Suffolk and North East Essex ICB and Breaking Barriers. Six accelerator sites co-developed transformation projects linked to their coastal locations, with interim learning published in December.[22]
We are developing a Community Languages and Translation Framework for action.
Mitigate against digital exclusion
We have held regular learning and support sessions to embed use of 2024’s Inclusive Digital Healthcare: A Framework for NHS action on digital inclusion.[23]
Ensure datasets are complete and timely
Metrics for measuring progress in reducing healthcare inequalities across all the Core20PLUS5 clinical programmes for adults have been agreed and will be available to track using the NHS England Performance Oversight Dashboard. Work to develop healthcare inequalities metrics across the Core20PLUS5 areas for children and young people, and further metrics for adults (including UEC and electives) has begun.
We have developed proposals for improving the quality of ethnicity data and intend to refine and publish these in next financial year.
Accelerate preventative programmes that proactively engage those at greatest risk of poor health outcomes
We have produced a Core20PLUS5 Handbook (which brings together best evidence and practice examples to support successful delivery of Core20PLUS5 interventions for underserved groups) for imminent circulation.
To improve quality of care and experience for Sickle Cell Disorder (SCD) and thalassaemia, seven Emergency Department Bypass Units have opened in high-prevalence areas, providing faster pain relief for patients presenting in crisis. Two community development pilots in Manchester and London will offer community nursing and post-discharge follow ups to support these. Investment has been made to improve provision and access to digital care plans for Patients with SCD, supporting healthcare professionals to rapidly access patients’ personalised care plans.
A blood group genotyping programme has been introduced, enabling detection of previously undetectable antibodies that could cause blood transfusion complications. Following the NICE’s approval of a gene therapy (Exa-cel), the NHS has confirmed funding to offer it to those with the most severe forms of SCD and Major Thalassemia.
In response to the Infected Blood Inquiry, we enhanced our Patient Participation Group to include the UK Thalassaemia Society and the Sickle Cell Society.
Strengthen leadership and accountability
We have worked with stakeholders to develop a health inequalities strategic framework to guide action on healthcare inequalities across the NHS and intend to publish this in sequence with the 10-Year Health Plan.
We have catalysed health inequalities research investment of circa £800 million from organisations including National Institute for Health Research.
We mobilised phase two of the ICB NEDs and Chairs’ Health Inequalities leadership programme with representation from 21 ICBs.
In collaboration with the NHS Confederation, we implemented a development offer for primary care health inequalities leads, including webinars to support local implementation of the Core20PLUS5 approach.
We have developed further resources to support Making Every Contact Count and health literacy, including national webinars and a Making Every Contact Count ‘How to guide’ for acute settings.
In collaboration with Healthcare Finance Management Association, we also developed resources to support finance leads to tackle health inequalities and have recruited Health Inequalities Finance Fellows.
We supported NHS Providers to developing a Board Guide to Health Inequalities.[24]
We worked with the Association of British Pharmaceutical Industries to redevelop their training curriculum and professional exams to incorporate modules on health inequalities.
In partnership with the Royal Society of Medicine, we hosted the third Annual Tackling Health Inequalities Conference with poster presentations and Awards.
Framework for action – Core20PLUS5 approach
Core20PLUS5[25] remains our national and system-level approach to help reduce healthcare inequalities. This year we successfully launched a third cohort of 670 Core20PLUS Ambassadors working across the health system and an accompanying alumni programme.
Our Core20PLUS Connectors programme supports peer-led approaches to address health inequalities. This has involved work with 120 voluntary, community, faith, and social enterprise delivery partner organisations, and local Healthwatch partners.
Finally, we have continued to support the work of NHS Race and Health Observatory and through an open market procurement secured future hosting of NHS Race and Health Observatory until 31/3/2027.
Appendix 4: Working in partnership with people and communities
In 2024/25, we continued to build NHS England’s approach to involving people and communities in our work.
The participation review undertaken in 2023/24 set the foundation for taking forward the good practice embedded in the three legacy organisations (Health Education England, NHS England and NHS Digital) on working in partnership with people and communities.
During 2024/25, we developed a new policy on working with people and communities to cover the new organisation, with the aims of:
- Setting out various approaches to involving people and communities, including online consultation, events, workshops, and the recruitment of PPV Partners
- Supporting colleagues to better understand our legal duty to involve the public (section 13Q of the NHS Act 2006 (as amended)).
The policy was approved by NHS England’s Strategy, Investment and Performance Committee and then at NHS England’s Quality Committee.
To discharge its legal duty to involve the public, NHS England has an assurance process in place for its commissioning decisions that affect the recipients of NHS services, including their carers and representatives. National and regional reporting on public involvement provides assurance that NHS England has met its legal duty.
We ran engagement sessions for the 10-Year Health Plan to support the inclusion of specific communities covered by our networks and forums. These included the Older People Sounding Board, LGBTI+ Sounding Board, Learning Disability and Autism Advisory Group, and the NHS Citizen Advisory Group.
Examples of how we involve people in our work
Peer Leadership
This year, NHS England’s Voices of People Team, in the Primary Care and Community Services directorate, continued to deliver the four Step Peer Leadership Development Programme, empowering over 6,000 people with lived experience to interact with the health and care system and have better conversations with clinicians. This year 350 people worked collaboratively with the health and care system in their local health economies and national programmes, including members of the Strategic Co-Production Group.
Other activities include:
- Publication of commissioning principles for abortion which were developed by Strategic Co-Production Group members
- Development of personas to support use of digital technology for New Hospital Programme
- Supported publication of Universal Offer for Community Services.
Research and health inequalities
At NHS England, research is an important driver of improvement in health and care and in addressing health inequalities, so it is important that our diverse communities are involved in research. In 2024/25 NHS England and the DHSC funded the ICS Research Engagement Network programme. Research Engagement Network teams aim to increase diversity in research participation by engaging with people in underserved communities around research, making research more accessible, and by embedding approaches to diverse research inclusion in how local organisations work.
Data deliberation
The Joint Digital Policy Unit (comprised of NHS England and the DHSC teams) delivered a £1.5 million programme of national public engagement on data in 2024/25. This programme comprised of three cohorts, each covering a different topic within the health and care data landscape. This included the use of data for research, a single patient record and the use of data in the GP health record for planning and research, and the opt out landscape. Each cohort includes a core deliberation, bringing together 120 people across four locations around the country. This is supported by a programme of inclusive engagement with seldom heard voices, as well as a quantitative survey. The programme has reached around 8,600 people so far and fed into the evidence base for the 10-Year Health Plan.
Cancer programme engagement
The National Cancer Programme (NCP) continues to engage with People and Communities through the PPV Forum, spanning the wide range of transformation initiatives, including Early Diagnosis, Faster Diagnosis, Innovation, Living with & Beyond Cancer, Treatment, and Experience of Care. A particular emphasis has been placed on ensuring a diversity of voices in engagement, alongside a targeted focus on reducing health inequalities. The PPV Forum was a key route of engagement in developing the National Cancer Plan, created collaboratively between NHS England and the DHSC, providing scrutiny and challenge. The National Cancer Programme supported engagement by Cancer Alliances by including requirements for engagement through the Cancer Alliance Annual Planning Pack and fostering collaboration among leads within a high-functioning Community of Practice.
Maternity and service user voice
The Maternity and Neonatal Programme works with 21 PPV Partners on its board, committees and all steering groups. This helps ensure that women, babies and families are central to any policies developed. In addition, NHS England has seven regional PPV Partners who contribute service user voice to the regional boards and co-ordinate the Maternity and Neonatal Voices Partnerships (MNVPs) across England. Maternity and Neonatal Voices Partnerships support ICBs and provider trusts to listen to the experiences of women and families, and bring together service users, staff and other stakeholders to plan, review and improve maternity and neonatal care. This influences improvements in the safety, quality, and experience of maternity and neonatal care.
Maximising the impact of NHS volunteers and the VCSE sector
Work has continued to develop volunteering based on the recommendations from the NHS Volunteering Taskforce 2023. Over the past year this has included:
- Continued development of a recruitment website[26] to facilitate an easier route for potential volunteers to find an opportunity that suits their needs. Previously in a testing phase, this platform is now being made more widely available as a single front door for NHS volunteer recruitment.
- £10 million awarded to 15 system level partnerships across England (through the Volunteering for Health programme, in partnership with NHS Charities Together and CW+) and that will use this to develop and deliver volunteer projects in their local ICS. The 15 projects are diverse, innovative and, above all, have a clear ambition to grow and strengthen volunteering in health systems so that everyone gets better healthcare.
- Culmination of the two-year funded Volunteer to Career programme2F[27], in partnership with Helpforce, supporting routes into careers, particularly clinical workforce pathways which saw 72% of participating volunteers go on to further education, training or employment.
- The NHS and Care Volunteer Responders programme has continued to provide support through micro volunteering opportunities over the past year, with 48,000 volunteers together supporting the delivery of over 100,000 tasks. This has included support through vaccination stewards, telephone companionship and transport tasks amongst other roles.
- In April 2024, the first national data collection for volunteers supporting NHS Trusts was launched, providing consistent and appropriate measures to track the number of NHS volunteers. This shows there are over 71,000 volunteers across NHS Trusts in England, collectively providing over six million hours of volunteering support.
- Maintained support for ambulance trusts through an extension to the National Ambulance Auxiliary service213F[28] with over 16,500 hours of additional capacity provided, including 881 hours of support to four acute hospitals to release ambulances back on to the road.
Work has also continued to support embedding of VCSE engagement within ICSs with dedicated Communities of Practice and Expert Networks in place for ICB and VCSE Alliance leads. Tools and resources have been co designed with these groups including the Embedding the VCSE in ICS Quality Development tool and RSM Impact Framework.
Working in partnership with carers
Work has continued on our commitment to support young carers, in recognition that young carers are more likely to have poorer health and educational outcomes. We hosted the inaugural cross-departmental Young Carers Data Summit, triangulating intelligence from the Departments of Education, Work and Pensions, and Health and Social Care along with key VCSE organisations, to inform collaborative improvements and enhance partnership working. We published a series of co-produced GP Top Tips to support identification of, and engagement with, young carers within Primary Care.
We continue to work closely with people and communities, leading widescale stakeholder engagement to inform the refresh of key national publications, including commissioning principles and GP Quality Markers. We hosted national roundtables aligned to shifts in the Darzi report, ‘Technology’ and ‘Care from Hospital to Community’, to promote the carer voice throughout the development of the Long-Term Plan and engaged with Carer entrepreneurs across both shift conversations.
The Health and Wellbeing Alliance Carers Partnership published a new resource for health and social care professionals to improve the identification and support of unpaid carers across ICSs. We continue to provide opportunities to scale and spread learning via well-established national networks and awareness campaigns, including the regional development of hospital discharge toolkits, digital products for contingency planning and supporting carers through virtual wards.
Networks and forums
Across the organisation, we run a wide range of forums, advisory groups and sounding boards, involving people from different communities and health interests. These include the NHS Youth Forum, the Older People’s Sounding Board, the LGBTI+ Sounding Board and the Adult Mental Health Advisory Network.
Many of NHS England’s forums come together as part of the NHS Citizen Advisory Group, which helps to join-up voices from across different programme areas, speaking directly to programme and policy leads. The Advisory Group champions appropriate, effective, and meaningful engagement, including identifying good practice and opportunities for improvement. A couple of example forums that are members are included below:
- NHS England’s Older People’s Sounding Board: Working in partnership with National Development Team for Inclusion, a diverse group of 25 older people have continued to engage with policy makers and clinicians to influence decision making and suggest improvements. They have influence across and beyond NHS England’s directorates; and over the last 12 months they have explored ‘living with frailty’; neighbourhood health and care; hospital discharge to care home; day-case hip, knee and orthopaedic trauma pathways; care partners; integrated care; and NHS building and estates. More recently, they have also contributed the views of older people into the ‘Change NHS’ 10-year planning and have met with the NHS RHO to consider health inequity at the intersection of age and race.
- The Learning Disability and Autism Advisory Group said goodbye and thank you to long standing members and recruited and welcomed 20 new autistic people, people with a learning disability and family carers. They include people of all ages, from different walks of life with diverse ethnicities, backgrounds and experience.
Topics during 2024/25 included co-producing ideas to:
- better meet the needs of people with disabilities when designing hospital buildings
- improve the NHS as part of the Change NHS programme
- highlight the key points to consider when launching the Reasonable Adjustment Digital Flag to people with disabilities
- better develop an autism pathway
- explore what would help people be able to live happier lives in their community, without having to have high numbers of staff surrounding them.
As well as holding meetings, different members also worked on key programmes of work across the year, helping to shape and design policy and guidance. Through the Forum, which has more than 10,000 members, we shared key national campaign information in more accessible language to widen reach, help raise awareness, explain complex messages and help improve services. We used social media and monthly update email bulletins, along with easy read and plain English versions of a co-produced newsletter.[29]
Appendix 5: Sustainability
With the conclusion of the 2021-2025 Greening Government Commitments (GGCs), we are pleased to report overall positive progress against the targets.
|
A: Mitigating climate change: working towards net zero |
Target |
Actual |
|
Reduce overall GHGs |
-44% |
-80% |
|
Reduce direct GHGs |
-20% |
-83% |
|
Reduce emissions from domestic business flights |
-30% |
-88% |
|
B: Minimising waste and resource efficiency |
|
|
|
Reduce the overall amount of waste generated |
-15% |
-92% |
|
Reduce the proportion of waste going to landfill |
5% |
1% |
|
Increase the proportion of waste being recycled |
70% |
65% |
|
Remove all items of consumer single use plastics (CSUPs) |
-100% |
245% |
|
Reduce paper use |
-50% |
96% |
|
C: Reducing water use |
|
|
|
Reduce water consumption |
-8% |
-87% |
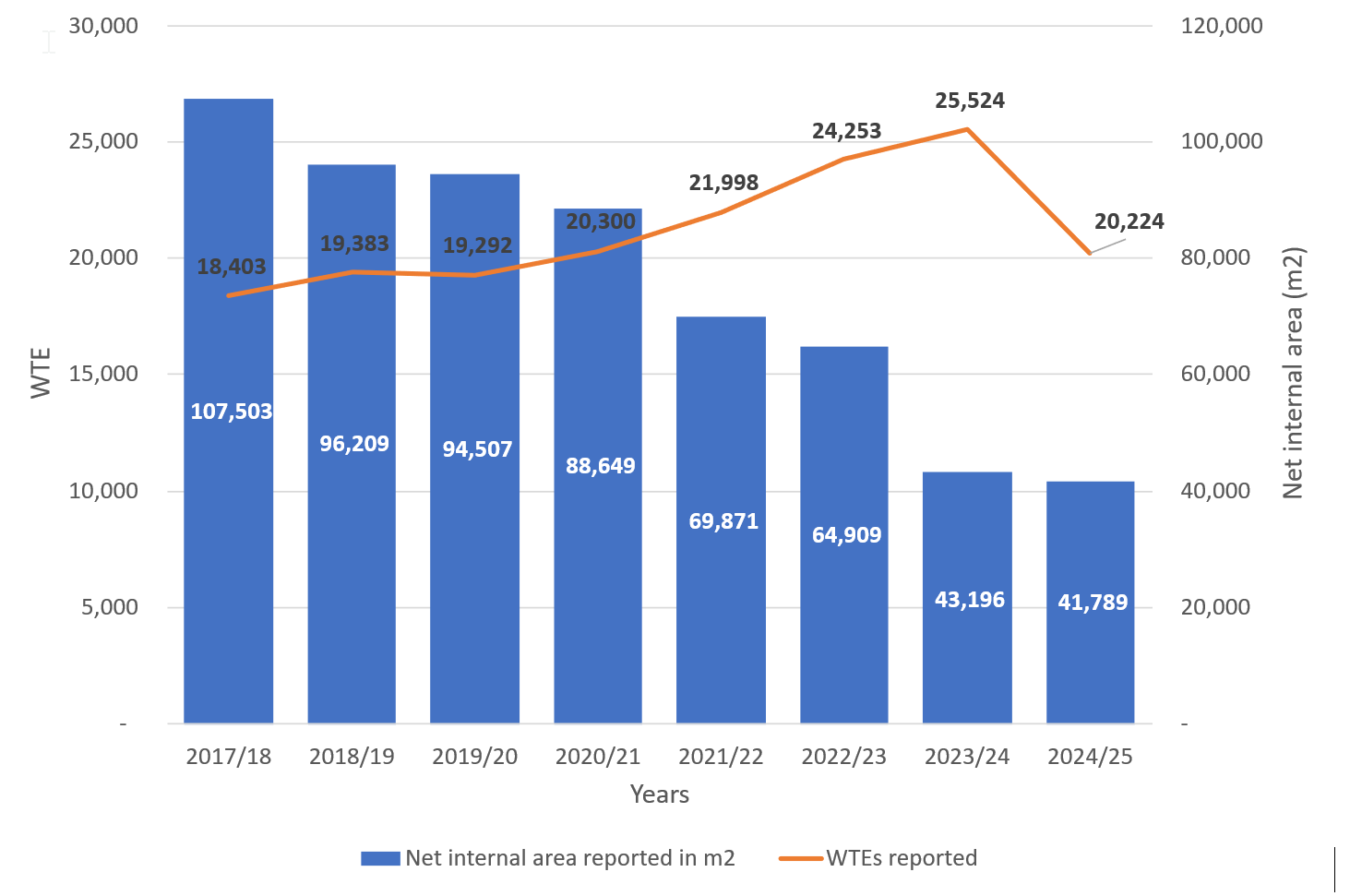
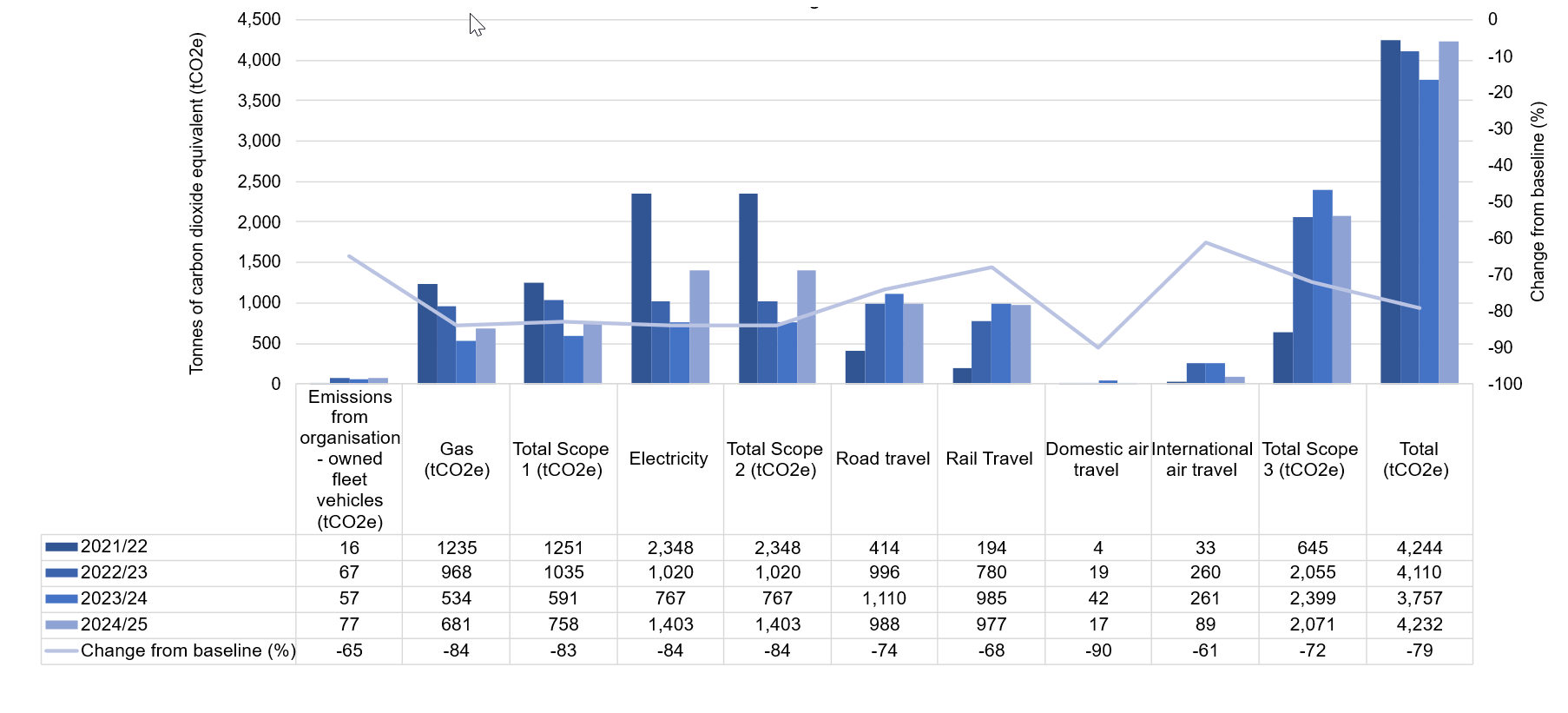
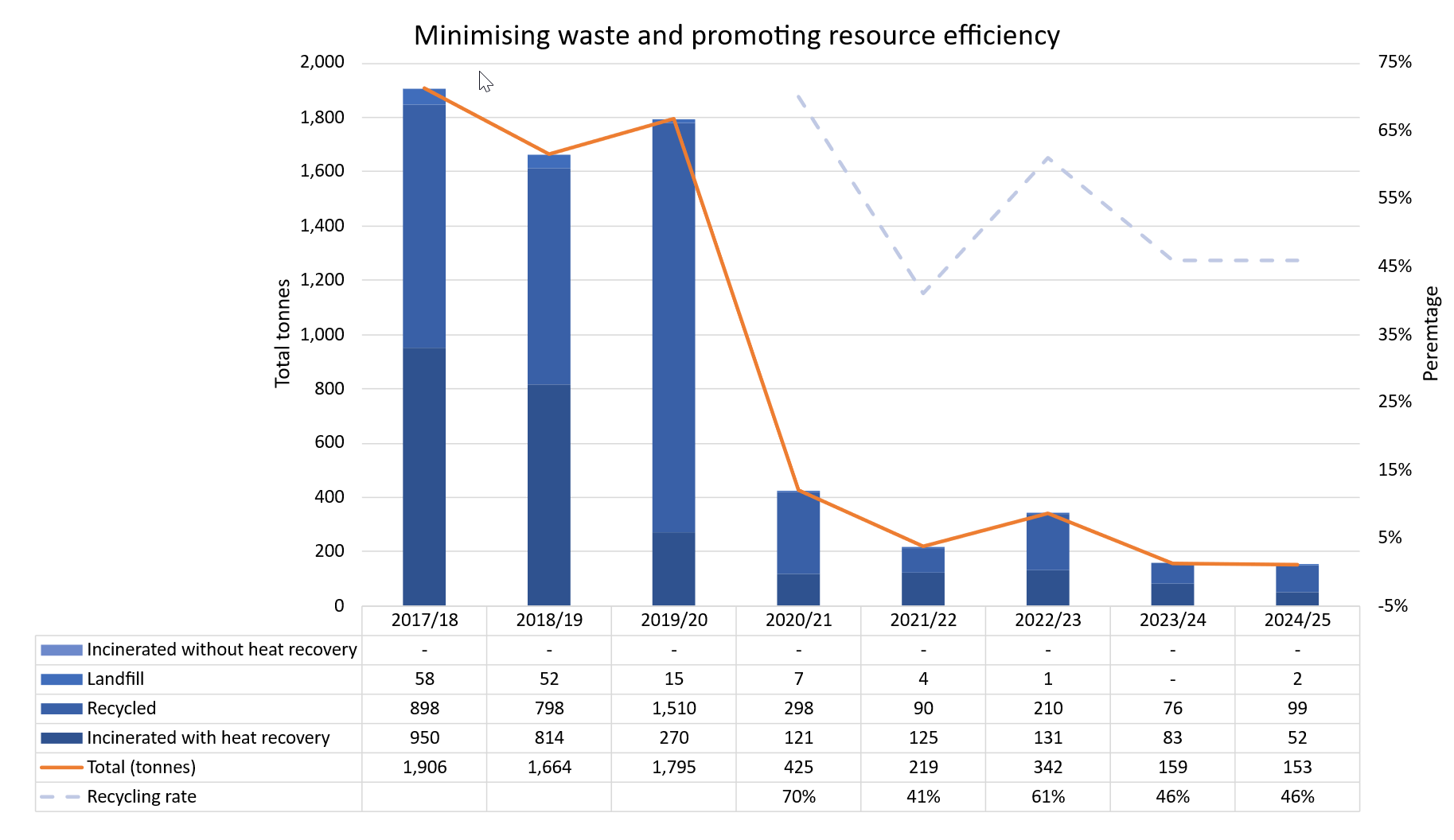
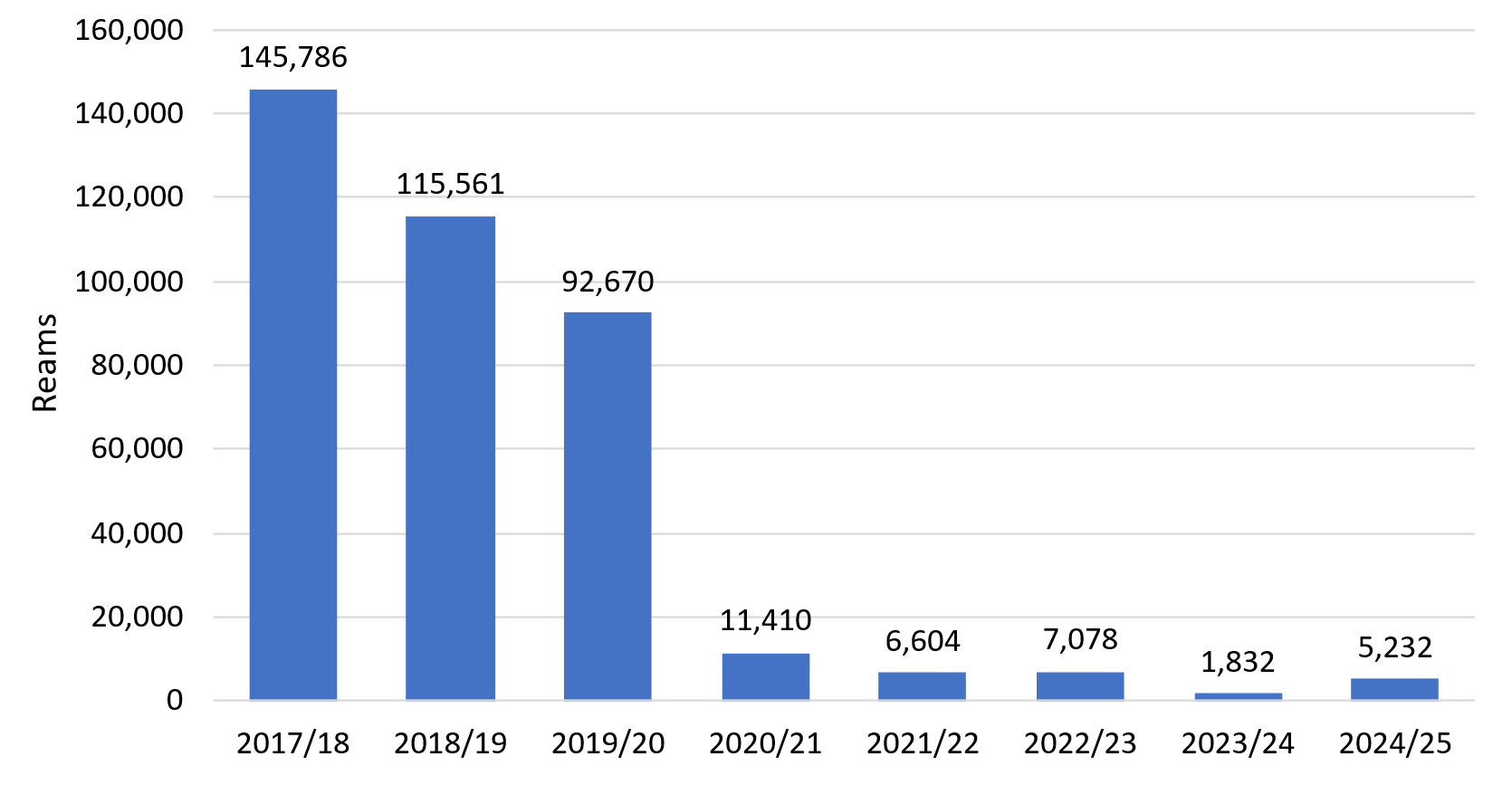
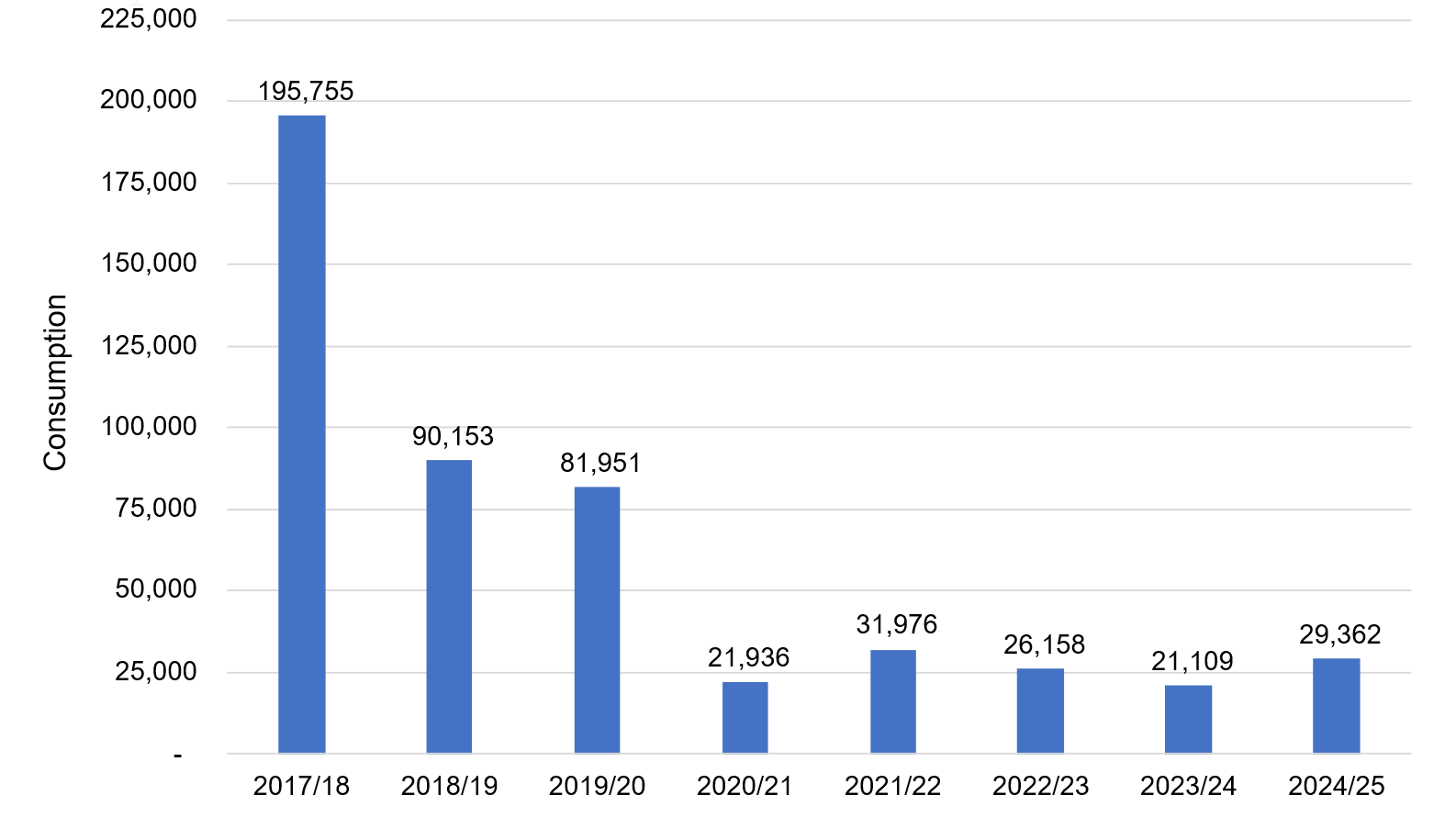
Our direct GHGs have reduced by 79% from the 2017/18 baseline year. This can largely be attributed to the size of the reportable estate more than halving, resulting in emissions from gas and electricity use reducing by 84% each. The overall volume of waste has reduced by 92% since 2017/18, against a target to achieve a 15% reduction. Emissions from domestic business flights have reduced by 88% and have reduced significantly since our Flight Approval Panel was established in May 2024.
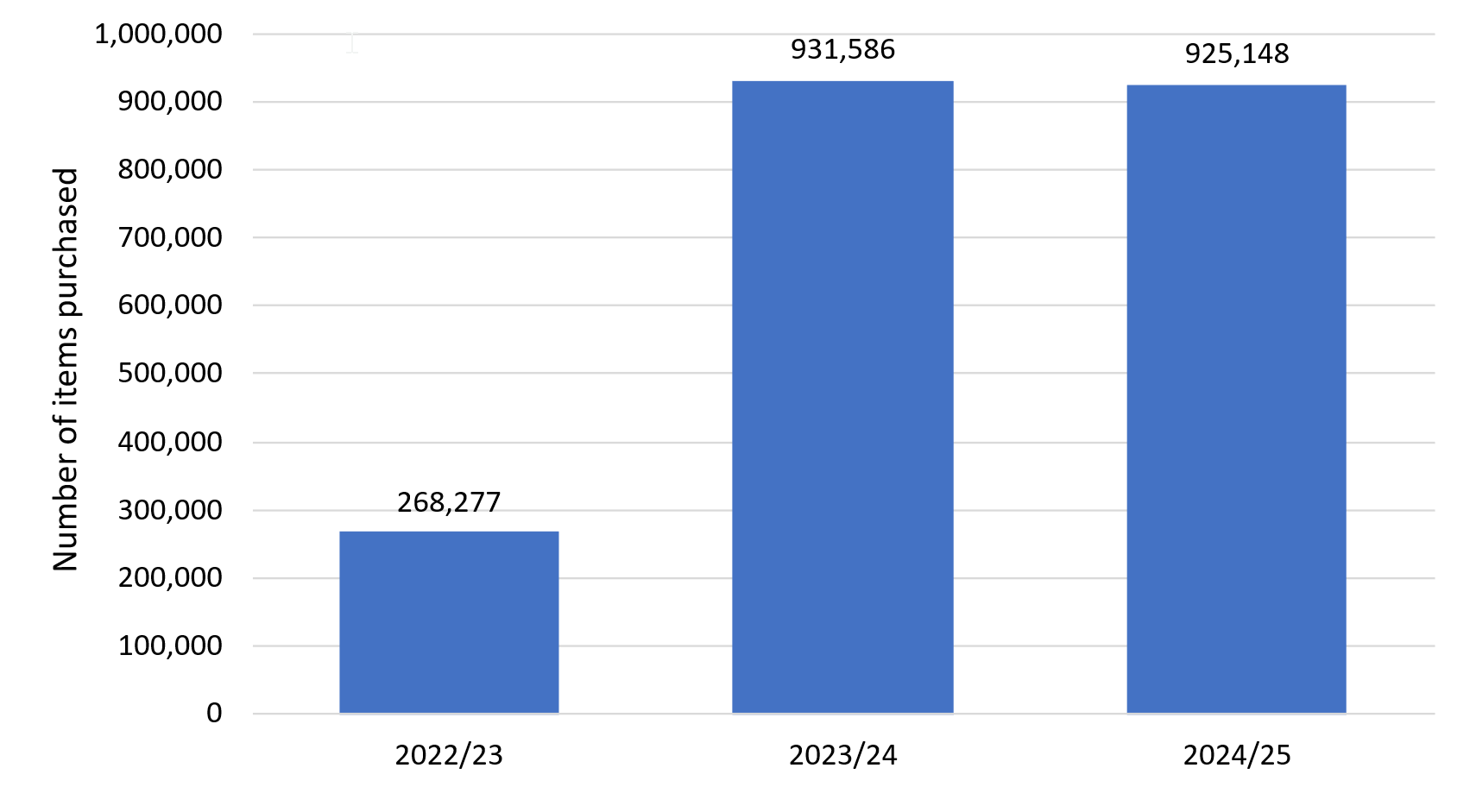
We have not had success across the board: our overall rate of recycling did not meet the 70% target, and we did not remove Consumer Single Use Plastics (CSUPs) from our estate. We continue to work with landlords, who manage facilities management services on our behalf, to improve waste management. This includes the implementation of the government’s Simpler Recycling policy, which came into effect in March 2025. The number of items of CSUPs increased with higher office utilisation after the COVID-19 pandemic. We remain committed to implementing the changes which have been agreed with our supplier to significantly reduce the number of CSUPs items purchased across our estate.
Taskforce on Climate-Related Financial Disclosures
We recognise climate change as a risk to NHS England and to delivery of services across the NHS system. For our own operations, we are dedicated to enhancing environmental impacts from government estates and operations as part of the GGCs, while promoting efficiency and optimal use of taxpayer money. We recognise climate change risks for the wider NHS through our Greener NHS programme and are committed to achieving a net zero NHS by 2040. This involves improving healthcare, reducing harmful carbon emissions, and investing in initiatives that remove GHGs from the atmosphere, acknowledging the inextricable link between climate change and human health.
Governance
Our progress against the GGCs continued to be measured and regularly reported to the Executive Corporate Group (ECG) throughout the year. Where necessary, progress can be reported to the Board via the Executive Group.
Risk Management
NHS England’s Risk Management Framework sets out the architecture within which risk management operates in NHS England. The Board and NHS England Executive own the SRR and ORR. Executive and Board committees receive strategic risks and top operational risks that fall under their remit. They assess and challenge the effectiveness of risk mitigation plans and ensure relevant actions are implemented. No risks concerning climate change and NHS England have been recorded on either the SRR or ORR during 2024/25.
Metrics and targets[30]
We are aligned to the targets set out in the GGCs. Our progress against the targets is published annually in this report.
Scope
All reporting in this section covers NHS England and the CSUs. Each trust and ICS have its own Green Plan and will report its sustainability performance separately.
Reporting for multi-occupancy sites
Where we are tenants of a government department, energy, waste, and water information for the whole building will be reported in their annual reports and published on their websites. For all other sites, we report on the proportion of the sites that we occupy. Approximately 43% of our estate is included in this reporting.
Provision of data
Where actual figures for energy, water and waste were unavailable owing to a lack of data from suppliers and landlords, we have made our best efforts to estimate using available data. Estimates are based on averages per m2 of Net Internal Area.
Contextual information
Greenhouse gas emissions[31]
Related use and cost2[32]
|
|
|
|
2021/22 |
2022/23 |
2023/24 |
2024/25 |
Change from baseline |
|
Scope 1218F[33] |
Km |
Scope 1 business travel |
99,511 |
414,563 |
699,852* |
779,279 |
-66% |
|
kWh |
Gas |
6,740,320 |
5,302,724 |
2,926,969* |
3,721,038 |
-83% | |
|
Cost |
Scope 1 business travel |
£28,565 |
£145,519 |
£217,832 |
£181,429 |
-51% | |
|
Gas |
£298,604 |
£240,222 |
£310,546 |
£284,342 |
64% | ||
|
Scope 2219F[34] |
kWh |
Electricity |
11,060,753 |
5,273,549 |
3,718,599* |
6,774,884 |
-72% |
|
Cost |
Electricity |
£1,355,197 |
£824,398 |
£1,214,235 |
£1,112,591 |
-57% | |
|
Scope 3 Related use |
Km |
Road travel |
2,475,394 |
6,192,563 |
6,990,748* |
6,416,785 |
-81% |
|
Rail Travel |
5,691,051* |
30,917,856* |
27,755,605* |
26,804,110 |
-57% | ||
|
Domestic air travel |
30,521* |
150,354* |
261,643 |
103,502 |
-91% | ||
|
International air travel |
428,159* |
911,144* |
1,184,953 |
595,477 |
-74% | ||
|
Total business miles km (scope 1 and 3) |
8,724,637* |
30,503,294* |
36,891,801* |
34,699,153 |
-66% | ||
|
Scope 3220F[35] Cost |
Road travel |
£789,775 |
£1,881,592 |
£2,287,977 |
£1,992,559 |
-67% | |
|
Rail Travel |
£1,472,414 |
£6,018,908* |
£8,551,756 |
£7,748,290 |
-53% | ||
|
Domestic air travel |
£4,807* |
£32,962* |
£63,459 |
£26,083 |
-89% | ||
|
International |
£3,164* |
£37,258* |
£116,600 |
£46,152 |
-80% | ||
|
|
Total cost of business travel |
£2,298,725* |
£8,116,240* |
£11,237,624* |
£9,994,513 |
-57% | |
|
Total cost of related use (all scopes) |
£4,239,738 |
£10,417,501 |
£12,762,405 |
£11,391,446 |
-57% | ||
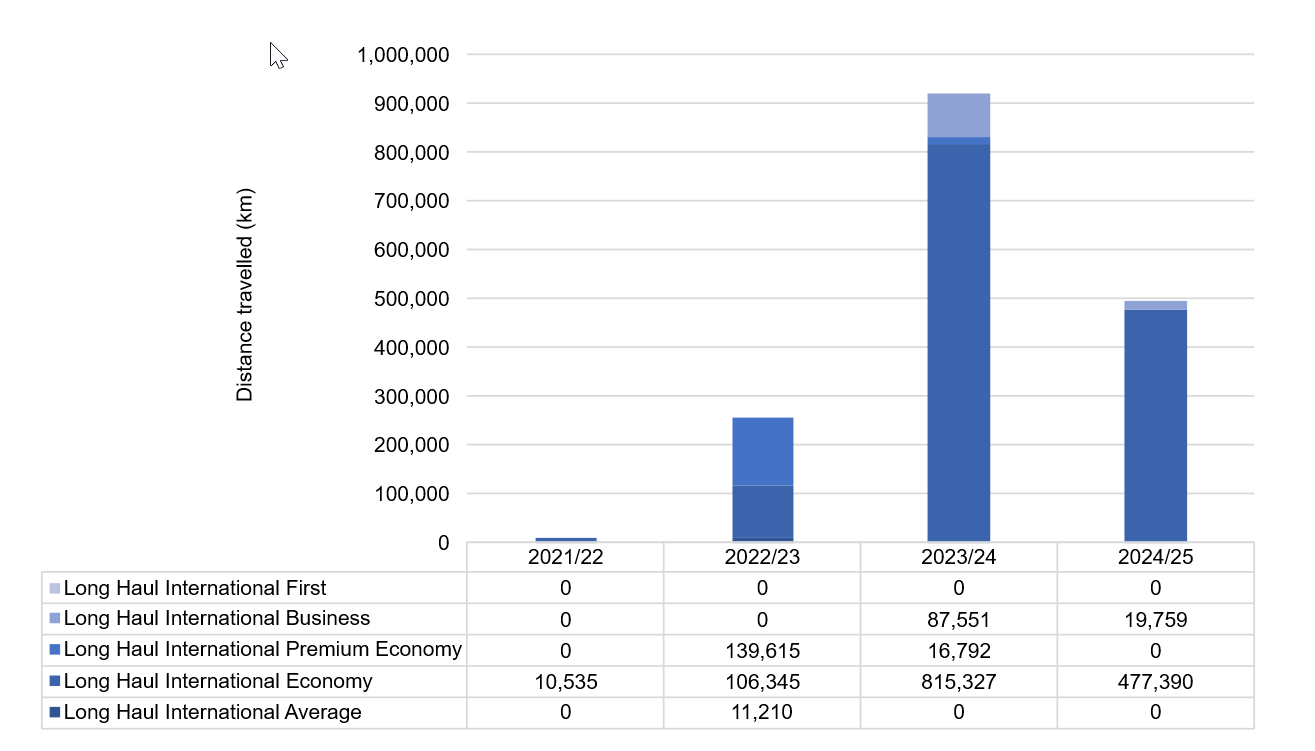
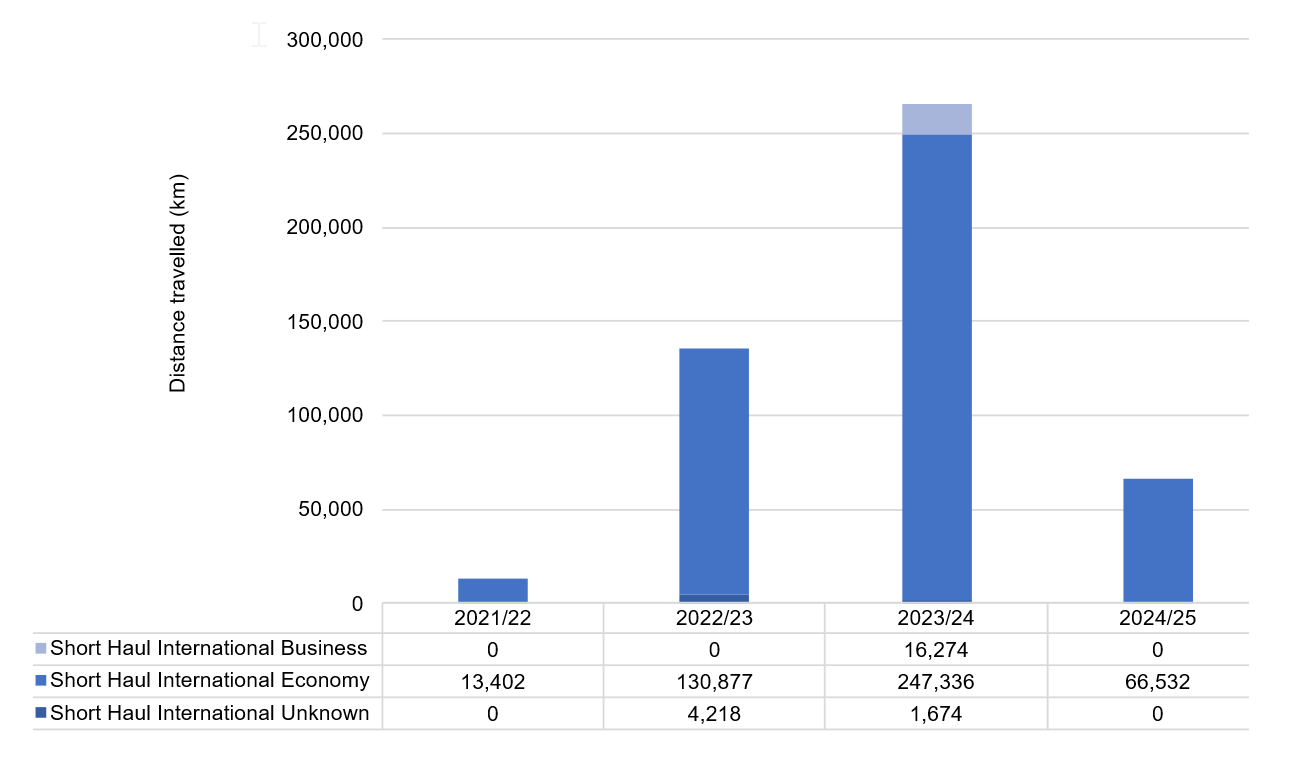
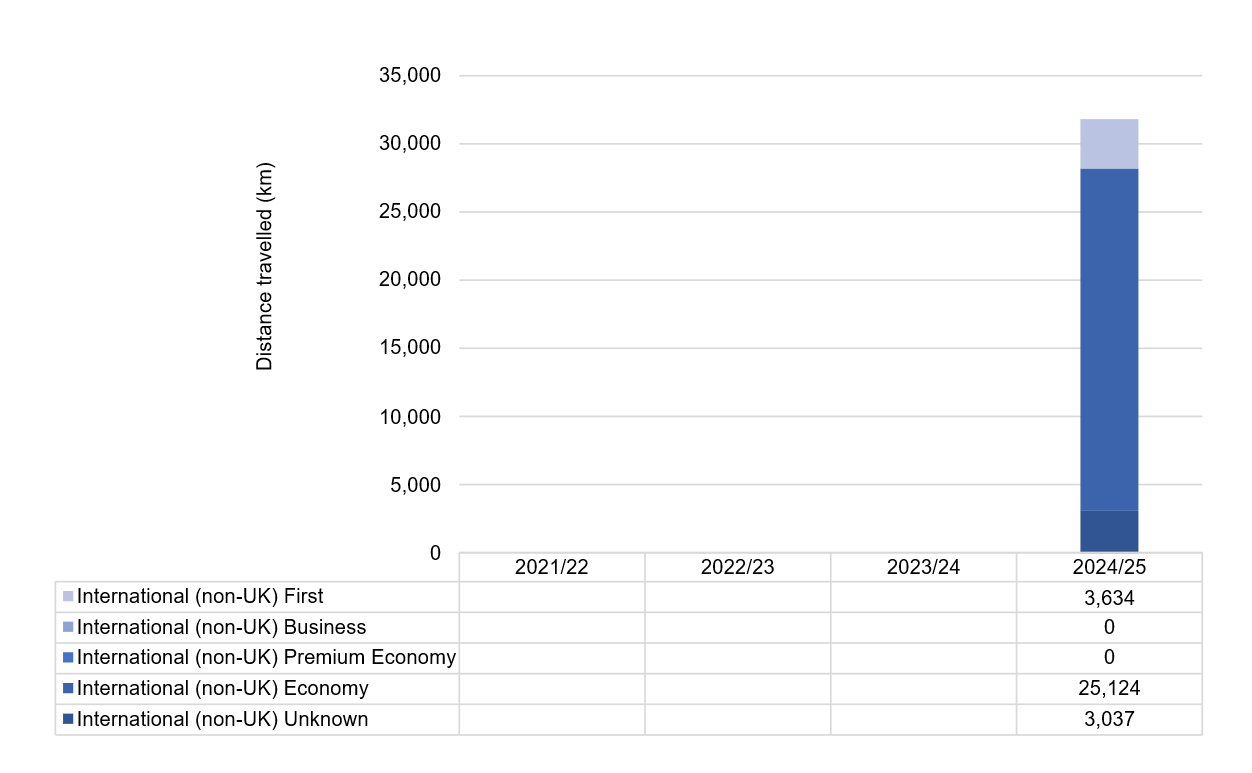
International air travel[36]
Long haul international flights
Short haul international flights
Non-UK international flights[37]
Waste
We have reduced the overall amount of waste generated by 92% since 2017/18, against a target of 15%. Our recycling rate was 65%, against a target of 70%.
Cost of waste disposal
|
|
2021/22 |
2022/23 |
2023/24 |
2024/25 |
|
Incinerated with heat recovery |
£83,931 |
£83,808 |
£14,469 |
£6,252 |
|
Cost of recycling |
£44,680 |
£100,952 |
£14,274 |
£17,996 |
|
Total |
£128,611 |
£184,761 |
£28,743 |
£24,248 |
NHS England ICT and digital waste disposal[38]
|
Waste disposal (tonnes) |
2024/25 |
|
Donating items within Government |
– |
|
Donating items to charity, schools or other NGO |
– |
|
Selling items – for commercial sale |
81 |
|
Recycling (hazardous and non-hazardous) |
145 |
|
Combustion / Energy recovery |
– |
|
Incineration without energy recovery |
– |
|
Landfill |
– |
|
Total |
226 |
We continue to maintain the use of ICT equipment for as long as possible, extending the life of user devices compared to previous years.
When items do become obsolete, we work with other organisations to process our ICT waste responsibly and sustainably. This may be through offering equipment to other public sector organisations that can still make use of them, approved authorised treatment facilities, following waste electrical and electronic equipment regulations or using corporate recycling schemes.
We have moved away from hosting our services on our own premises and we now use Crown Hosting (in mission-critical data centres providing leading environmental performance) and cloud hosting.
Reuse schemes
Surplus furniture is often reused across the public sector through the Cabinet Office reuse scheme or is donated to other public and charitable organisations locally. The surplus furniture from three office closures this year were donated to a school charity and to other public organisations through the Cabinet Office reuse scheme.
Consumer single-use plastics
Paper use
Water consumption (m3)
Sustainable procurement
Our policy is outlined in the published net zero supplier roadmap[39], supported by guidance aligned with Procurement Policy Note (PPN) 002[40] on the Social Value Model and PPN 016[41] on Carbon Reduction Plans. Additionally, our Evergreen Sustainable Supplier Assessment tool[42] helps suppliers align with our net zero and sustainability goals. We are committed to eradicating modern slavery in line with PPN 009[43] and have integrated a risk assessment tool into our e-commerce system to support this effort.
Net zero and social value buying guides have been created to aid the development of specific category strategies, incorporating Government Buying Standards where relevant.
Nature recovery and biodiversity
We do not own any natural capital or landholdings.
Adapting to climate change
Business continuity management identifies our priorities and prepares solutions to address disruptive threats, including those which may be the result of climate change and extreme weather events.
NHS emissions
As set out in the DHSC GAM, NHS bodies are not required to disclose emissions as part of the metrics and target pillar of TCFD disclosures, as NHS England provides estimates of NHS total emissions.
The breakdown of estimated 2024/25 NHS Carbon Footprint emissions into Scope 1, 2 and limited Scope 3 emissions is included below, aligning with reporting requirements for central government departments, plus additional categories that are included in the NHS Carbon Footprint definition.[44] These figures are rounded to the nearest 50 ktCO2e, are based on both actual and forecasted data as at end May 2025, and may be subject to revision as final input data is published. Updated figures for 2023/24, based on latest available 2023/24 data and methodology, are also included in the table. The intention for future reporting is to include additional Scope 3 emission categories.
NHS England is undertaking a review of emissions in the NHS footprint in line with best practice methodology, as well as progress made five years on from the ‘Delivering a Net Zero NHS’ report.
|
|
Estates |
Medicines |
Fleet and business travel |
Total (ktCO2e) |
|
Scope 1 |
Onsite combustion of fossil fuels |
Anaesthetics |
Owned and leased fleet |
|
|
Estimated NHS emissions (ktCO2e) |
1,600 |
250 |
150 |
2,000 |
|
Scope2 |
Electricity / purchased heat and steam |
– |
– |
|
|
Estimated NHS emissions (ktCO2e) |
650 |
N/A |
N/A |
650 |
|
Scope 3 |
Well to tank emissions, waste and water |
All inhalers and anaesthetic manufacturing |
Business travel |
|
|
Estimated NHS emissions (ktCO2e) |
500 |
700 |
450 |
1,700 |
|
Total 2024/25 Provisional |
2,800 |
950 |
600 |
4,350 |
|
Updated 2023/24 |
2,850 |
1,000 |
600 |
4,450 |
[1] https://www.england.nhs.uk/long-read/neighbourhood-health-guidelines-2025-26/
[2] https://www.england.nhs.uk/publication/the-insightful-icb-board/
[3] 12-month rolling average https://nhsd-ndrs.shinyapps.io/rcrd/
[4] https://www.officeforstudents.org.uk/for-providers/finance-and-funding/health-education-funding/medical-and-dental-maximum-fundable-limits/
[5] https://www.england.nhs.uk/long-read/our-new-operating-model-supporting-you-to-deliver-high-quality-care-for-patients/
[6] https://www.england.nhs.uk/wp-content/uploads/2025/03/6-the-nhs-performance-assessment-framework-annex.pdf
[7] https://www.england.nhs.uk/long-read/capital-guidance-2025-26/
[8] https://www.england.nhs.uk/leaders/vsm-pay-framework/
[9] https://www.england.nhs.uk/long-read/specific-equality-duties-review-report-as-at-29-may-2025/
[10] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/
[11] https://www.england.nhs.uk/about/equality/objectives-24-25-and-25-26/
[12] https://www.equalityhumanrights.com/equality/equality-act-2010/protected-characteristics
[13] https://www.legislation.gov.uk/ukpga/2010/15/section/149
[14] https://www.legislation.gov.uk/uksi/2017/353/contents
[15] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/
[16] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/#5-major-legislative-and-nhs-reforms-and-the-impact-on-nhs-england-s-equality-objectives-and-targets:~:text=5.1%20Recent%20and%20planned%20changes%20to%20Equality%20legislation
[17] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/#5-major-legislative-and-nhs-reforms-and-the-impact-on-nhs-england-s-equality-objectives-and-targets:~:text=5.1%20Recent%20and%20planned%20changes%20to%20Equality%20legislation
[18] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/#5-major-legislative-and-nhs-reforms-and-the-impact-on-nhs-england-s-equality-objectives-and-targets:~:text=5.3%20Recommendations%3A%20equality%20objectives%20and%20targets%20for%202025/26
[19] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/#3-progress-against-the-2024-25-equality-objectives-and-targets
[20] https://www.england.nhs.uk/long-read/review-of-progress-in-2024-25-delivering-the-equality-objectives-and-meeting-the-wider-equality-requirements/#4-meeting-our-public-sector-equality-duty-psed-our-wider-equality-information
[21] https://www.england.nhs.uk/long-read/delivery-plan-for-recovering-urgent-and-emergency-care-services-january-2023/
[22] https://bbi.uk.com/coastalnavigtorsnetwork/
[23] https://www.england.nhs.uk/long-read/inclusive-digital-healthcare-a-framework-for-nhs-action-on-digital-inclusion/
[24] Reducing health inequalities: A guide for NHS trust board members
[25] https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/
[26] https://volunteering.england.nhs.uk
[27] https://helpforce.community/back-to-health/volunteer-to-career-programme
[28] https://www.sja.org.uk/press-centre/press-releases/st-john-commissioned-as-the-nations-ambulance-auxiliary/
[29] https://www.england.nhs.uk/learning-disabilities/about/get-involved/newsletters/
[30] Unless otherwise stated, the baseline year is 2017/18
[31] Figures marked with * have been restated
[32]Figures marked as* have been restated due to more accurate and/or up-to-date figures being available.
[33] Direct emissions – These occur from sources owned or controlled by the organisation.
[34] Energy indirect emissions – As a result of electricity consumed which is supplied by another party.
[35] Other indirect emissions – All other emissions which occur as a consequence of activity in an organisation’s value chain, but which are not owned or controlled by the accounting entity.
[36] International (non-UK) flights were included in the short haul and long haul international figures in previous years.
[37] These are flights that start and end overseas (i.e. neither departing nor arriving in the UK).
[38] This is the first year we have figures available. Midlands and Lancashire CSU did not submit a return.
[39] https://www.england.nhs.uk/greenernhs/get-involved/suppliers/
[40] https://www.gov.uk/government/publications/ppn-002-taking-account-of-social-value-in-the-award-of-contracts/procurement-policy-note-002-the-social-value-model-html
[41] https://www.gov.uk/government/publications/ppn-009-tackling-modern-slavery-in-government-supply-chains/ppn-009-guidance-on-tackling-modern-slavery-in-government-supply-chains-html
[42] https://www.england.nhs.uk/nhs-commercial/central-commercial-function-ccf/evergreen/
[43] https://www.gov.uk/government/publications/ppn-009-tackling-modern-slavery-in-government-supply-chains/ppn-009-guidance-on-tackling-modern-slavery-in-government-supply-chains-html
[44] https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2022/07/B1728-delivering-a-net-zero-nhs-july-2022.pdf

