Purpose and scope
The NHS in England has been a global leader in the development of specialist services to support people affected by the long-term effects of COVID-19. There has been important innovation in service provision which should be maintained and developed further.
Future commissioning of post COVID services will be the responsibility of Integrated Care Boards (ICBs). This document presents guidance for the commissioning and oversight of post COVID services by ICBs in England for adults and children and young people (CYP) from April 2024. This document is not intended to represent a clinical guideline which is covered by the in the National Institute for Health and Care Excellence (NICE), the Scottish Intercollegiate Guidelines Network (SIGN) and the Royal College of General Practitioners (RCGP) rapid guideline on managing the long-term effects of COVID-19 (December 2020, updated November 2021).
Dedicated services should continue to be offered to support people suffering ongoing effects of COVID-19 infection. This guidance builds on learning from national commissioning, improvement, and oversight of services in England since 2020. People continue to develop long COVID, and some will have prolonged illness.
Referral rates throughout 2023, together with the significant number of patients who require follow-up services, indicate there is an ongoing need for post-COVID assessment and treatment services and rehabilitation. Early intervention is predicted to support more effective recovery and may be essential to safely exclude other causes of significant symptoms.
Learning from the long COVID model has the potential to bring transferable benefits to the management of other long-term conditions and aligns strongly with the population health approaches being adopted by ICBs.
It is acknowledged that ICBs may wish to consider whether there is benefit in aligning pathways for post-viral illnesses or similar multi-system conditions for both their local adult and CYP populations. However, such wider provision will need to be in accordance with funding available for additional conditions.
Background
The most recent publication of the Office of National Statistics (ONS) in March 2023 estimates there are around 1.56 million people in England experiencing symptoms following COVID-19 for any duration; 1.1 million of whom experiencing symptoms for over 12 months. An estimated 298,000 people in England report that long COVID is significantly impacting on their day-to-day activities.
Long COVID symptoms occur in children and young people; the latest ONS COVID infection survey data showed an estimated 62,000 people aged 2 to 16 years have self-reported long COVID of any duration in the UK.
Although evaluation of the effectiveness of post-COVID services is at an early stage, several sources are beginning to indicate benefits: the NHS long COVID registry shows high levels of healthcare use among long COVID patients, which the post-COVID service model of treatment and rehabilitation addresses.
Outcome measures soon to be reported from the Living With and ELAROS digital self-management apps have shown a serious impact of long COVID on function in working age adults. Clinical experience from existing services indicates that early and effective care addressing symptoms and improving patient outcomes is essential to provide best value for the NHS and for patients.
Post-COVID services have been commissioned according to an integrated care system (ICS) footprint with the intention that providers within an ICS would come together to provide co-ordinated multidisciplinary integrated care to people with long COVID and other sequelae of SARS-CoV-2 infection.
Elements of the pathway which have proved particularly beneficial, and which are recommended to be developed, are listed in the post-COVID service requirement section.
Clinical case definition
This guidance refers to patients who meet the clinical case definition of ongoing symptomatic COVID-19 or post-COVID-19 syndrome as described in the National Institute for Health and Care Excellence (NICE), the Scottish Intercollegiate Guidelines Network (SIGN) and the Royal College of General Practitioners (RCGP) rapid guideline on managing the long-term effects of COVID-19 (December 2020, updated November 2021).
- Ongoing symptomatic COVID-19: signs and symptoms of COVID-19 lasting from 4 to 12 weeks.
- Post-COVID-19 syndrome: signs and symptoms that develop during or after an infection consistent with COVID‑19, continue for more than 12 weeks and are not explained by an alternative diagnosis. It usually presents with clusters of symptoms, often overlapping, which can fluctuate and change over time and can affect any system in the body. Post-COVID‑19 syndrome may be considered before 12 weeks while the possibility of an alternative underlying disease is also being assessed.
A positive molecular test is not required for diagnosis in adults or CYP. Without testing, long COVID can be difficult to distinguish from other post-viral illnesses, but that need not be a barrier to referral if there is clinical need.
- The term ‘long COVID’ is commonly used to describe signs and symptoms that continue or develop after acute COVID-19 (defined as signs of COVID-19 for up to four weeks). It includes both ongoing symptomatic COVID-19 and post-COVID-19 syndrome. Given the post-COVID service pathway supports referral from four weeks, the term ‘long COVID’ is used in this document (but coding should be via the above terms, as shown in table 1 below).
Table 1: Condition coding
| Condition | Code |
| Ongoing symptomatic COVID-19 | 1325181000000106 |
| Post-COVID-19 syndrome | 1325161000000102 |
The World Health Organization has also developed a clinical case definition of post-COVID-19 condition by a Delphi consensus for children and young people (October 2021).
ICB responsibilities for post-COVID services
Commissioning of post-COVID services will transition from the long COVID national programme to ICBs by the end of March 2024. ICBs will need to consider the transition in advance of April 2024 as they will be responsible for ensuring the delivery of consistently high-quality post-COVID services.
Funding for adult long COVID services in 2024/25 is expected to be allocated based on the current (2023/24) distribution, to minimise disruption to funding flows. Adult service funding will be moved into ICB programme allocations (from the Service Development Fund [SDF]) but will be identified separately in 2024/25.
Funding for the children and young people’s services will remain in the SDF and distributed through a lead ICB. This is the same approach as in 2023/24. This section sets out the expected responsibilities.
- Establishment of an ICS-based post-COVID steering function accountable to the ICB, with a named ICB lead to oversee delivery of post-COVID services and ensure appropriate reporting, escalation, and assurance mechanisms.
- Representation of lived experience partners as part of the steering function which may be part of a wider long-term conditions (LTCs) programme of work to optimise the resource most effectively.
- Provision of strategic clinical leadership and guidance with clinicians involved in the planning, delivery, and transformation of services.
- Alignment of ICB governance for post-COVID services with population health management for people with multi-system LTCs and the consideration of opportunities for care provision for people with similar patient needs.
- Commitment to data submission to the NHS long COVID registry to allow benchmarking with other services in England and support better understanding of long COVID and its impact on population health.
- Consideration should be given for inclusion of post-COVID syndrome or long COVID in LTC dashboards where these are developed.
- Commitment to the regular review and analysis of service data and primary care coding rates to understand service quality and equity of access. Input from public health teams would be beneficial to this analysis.
- Services should monitor changes in PROMS from assessment to discharge (or longer if able to collect via a digital platform). This data should be shared with the ICB oversight group to support quality improvement work.
- Opportunities to strengthen integrated pathways through collaboration between services across the ICS and region should be explored.
- Consider any ongoing support required by individuals following treatment and discharge from the long COVID pathway.
- Development of a clinical specification for assessment, treatment, and rehabilitation which fulfils the post-COVID service requirements below. See appendix B for an exemplar specification.
- Communications plans should be developed to encourage appropriate signposting and referral to services.
- This should be shared widely with primary care teams, secondary and tertiary care clinicians, pharmacists, psychology services and other public bodies such as secure unit services, local authorities, education and the voluntary, community and social enterprise (VCSE) sector.
- All public-facing communication should be culturally competent to audiences from all backgrounds to promote equity of access to services.
NHS England regional responsibilities for post-COVID services
- Regional leads should review post-COVID assessment service activity alongside other assurance processes. Financial provision will be made for this function in 2024/25.
- NHS England regional teams should continue to support systems commissioners and providers to:
- ensure equitable access to post-COVID services including assessment, treatment and rehabilitation for adults and CYP across the region as part of ICBs’ population health management approach
- support ICB commissioning decisions relating to the provision of services that extend beyond ICS footprints or on a regional footprint in conjunction with the relevant ICBs; this will particularly apply to CYP services and where there is a need for mutual aid
- review post-COVID service activity such that data insights on demand, capacity, access, and equity can inform assurance function
- mitigate risks and support with issues that impact on the provision of post-COVID services, escalating issues to the relevant NHS England regional director where necessary
- disseminate national guidance, policy, and updates to ICS leads as and when required
- maximise opportunities to adopt best practice pathways/models of care.
Post-COVID service requirements
NICE/SIGN/RCGP guidance recommends that access to multidisciplinary services is provided (these could be ‘one-stop’ clinics) for assessing physical and mental health symptoms and carrying out further tests and investigations. They should be led by a doctor with relevant skills and experience and appropriate specialist support, considering the variety of presenting symptoms.
In summary, post-COVID services should comprise an integrated pathway of assessment, medical treatment and multifaceted rehabilitation, including psychology with direct access to required diagnostics. Referral should be via a single point of access which is managed by clinician-led triage.
Resource allocation and planning for post-COVID services should include:
- Multidisciplinary teams (MDTs) to bring specialist medical, nursing, and allied health professional (AHP) input to community-based case management without multiple separate referrals. This should include clinical leadership from a doctor with the relevant skills and experience, and care co-ordinator roles to support and advise patients through the pathway and to be a point of contact. See Appendix C for description of how the professions support the post-COVID services pathway.
- Delivery of needs/symptom-based rehabilitation by a broad multi-professional team, to include management of breathlessness and fatigue, physical rehabilitation, management of dysautonomia symptoms, management of pain, educational support for children and young people and vocational rehabilitation.
- Referral into and from specialist services, such as secondary care, mental health services, the VCSE sector as needed. Adjustment of financial flows may be needed if this represents new activity and different ways of working.
- Provision of a self-management plan on discharge and details of who to contact in the event of a relapse or development of a new symptom. Patient-initiated follow-up (PIFU) should be made available to patients in the event of future deterioration. This supports transition to self-management.
- Options for in-person and virtual support as per clinical need and patient preference. Patients need access to in-person assessments, but some care can subsequently be delivered virtually.
- Integration of peer support and social prescribing into models of care.
- Provision of high-quality self-management resources to patients for people with long lasting symptoms and a fluctuating course. This should include digital adjuncts to support self-management and rehabilitation.
- Submit data to NHS England which contributes to the long COVID registry. Aggregated data are made available in the Long COVID dashboard on the NHS National Data Platform (Foundry) for commissioners and services to monitor activity, equity of access and healthcare use, and enable benchmarking with other services.
- Regularly monitor post-COVID assessment service activity, including referrals, waiting times, assessments and equity of access, and patients’ outcomes and experience, and compare these with national benchmarks.
- Ensure involvement of lived experience partners in co-design of services and pathways.
- Provide ongoing workforce training in management of the treatable traits of the condition. Multi-professional long COVID specific e-learning training is available and supports the delivery of an integrated and personalised care approach. Services benefit most from medical, nursing and AHP leaders with significant experience of long COVID management and should belong to long COVID clinical networks or clinical societies, ideally beyond their ICS to maintain continued professional development.
- Offer training opportunities and support to other relevant multi-professional clinical teams who may identify long COVID in their patients; primary care teams, community services such as psychology, musculoskeletal, specialist services such as cardiology, neurology, rheumatology.
- Regular liaison with the national long COVID clinical society that is being developed during the autumn of 2023 for updates on clinical management, and to provide a networking platform for clinicians and service providers delivering long COVID care.
Health inequalities
Data from the NHS long COVID registry shows that there is significant unwarranted geographical variation in access to post-COVID services across the country. Analysis has also shown that those from the most deprived areas and those belonging to ethnic minorities are significantly underrepresented in many areas.
It is also clear that this inequality of access is worse among patients who were never admitted to hospital for acute COVID-19 infection. It may be more difficult for these people to access referral to post-COVID services, in contrast to patients who were admitted with acute COVID-19 infection and may be referred via secondary care.
In planning and delivering post-COVID services, ICSs should consider how they will minimise these health inequalities, including for those with a protected characteristic and under-served or marginalised communities. A proportion of long COVID services funding should be allocated to tackling health inequalities. See Appendix D for an example of good practice.
To make an objective assessment ICSs should routinely analyse socio-demographic service activity data against the local socio-demographic composition to understand equity of access. This can be supported by the Long COVID Dashboard.
- The relative risk of developing long COVID based on socio-demographic variables such as sex, ethnicity and level of deprivation should also be considered when interpreting equity of access. Early studies that provide insights into the relative risk of developing long COVID include the ONS study, REACT-2 study and the CONVALESCENCE study. These studies are based on pre-Omicron variants and have not considered vaccination status.
- Post-COVID services should be aware of diagnostic overshadowing and make reasonable adjustments as required for neuro-divergent groups, or patients with pre-existing physical and mental health conditions or other impairments such as visual or hearing loss. See Appendix D for an example of good practice.
ICBs and services should implement proactive case finding approaches and adapted referral pathways for vulnerable people experiencing long COVID. ICSs should pay particular attention to young adults who are transitioning from paediatric to adult services to ensure that their long COVID care needs are adequately catered for.
Referral
Referral routes
There are two main referral routes into post-COVID services.
A: Referral from primary care (see figure 1 below)
- Patients with new or ongoing symptoms four weeks or more after they first had suspected or confirmed acute COVID-19 symptoms can be signposted to contact their general practice team – by community pharmacy, the NHS.uk website, occupational health, the Your COVID Recovery website, VCSE sector, other community settings such as schools and churches, or following discharge from an emergency department.
- Patients who present to their general practice team should be assessed using a holistic, person-centered approach. This should include a comprehensive clinical history and appropriate examination to assess physical, cognitive, psychological symptoms, and functional abilities including impact on education and work.
- Investigations (see Appendix E) that are tailored to a person’s signs and symptoms should be offered to rule out acute or life-threatening complications and find out if symptoms are likely to be caused by ongoing symptomatic COVID-19, post-COVID-19 syndrome or a new, unrelated diagnosis, as per NICE/SIGN/RCGP COVID-19 rapid guideline NG188.
- Adults should be referred directly to post-COVID services.
- Self-referral routes may improve access particularly for vulnerable groups but there should be liaison with the primary care team to ensure adequate sharing of clinical information and appropriateness.
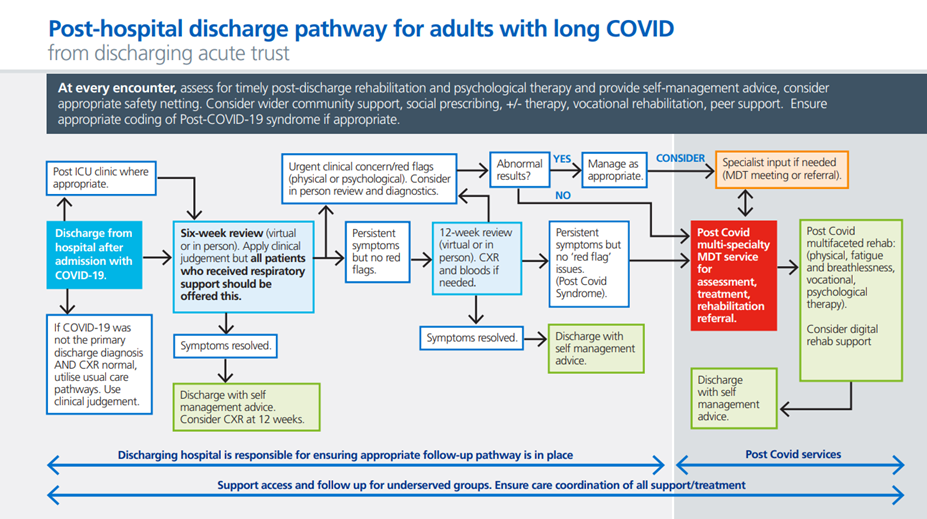
B. Post-admission with COVID-19 (see figure 2 below)
- Discharging hospitals are responsible for ensuring follow-up pathways are in place following admission with COVID-19. If COVID-19 was not the patient’s primary discharge diagnosis and they have a normal chest X-ray (CXR) at discharge, usual care pathways can be used.
- Primary care should be provided with a detailed discharge summary of the admission and ongoing related conditions and previous social care arrangements which need to be re-instated.
- Patients who required respiratory support should be reviewed at six weeks and the discharging hospital should consider a holistic review at six weeks (virtual or face-to-face) for others based on clinical judgement and patient preference.
- Patients with new or non-improving symptoms after discharge will require additional follow-up to rule out alternative diagnosis, and if no alternative diagnosis is made, the need for referral to post-COVID services should be considered.
- People who develop new or different symptoms after the 12-week review should be asked to seek help from their general practice.
- People with COVID-19 cared for in an intensive care unit (ICU)/high dependency unit (HDU) setting should undergo an MDT assessment of their rehabilitation needs at the point they are stepped down to other inpatient facilities. Inpatient rehabilitation with defined goals should begin immediately. Post ICU follow-up should occur via usual care pathways with onward referral to post-COVID services if needed.
Referral criteria
Patients with ongoing symptoms lasting for four weeks or more following confirmed or suspected COVID-19 illness should be considered for referral, particularly if the following criteria are met:
- severe presentations where symptoms are having a significant impact on normal activities of daily living, including attendance at work or, for children and young people, access to education or attendance at school
- non-improving trend
- atypical presentations where further assessment is needed to confirm the diagnosis/consider alternative diagnoses
- further assessment is needed to confirm safety and appropriateness of either self-management or supported rehabilitation
- typically, referral by primary care will not be immediate due to the need to consider alternative diagnoses and undertake relevant initial investigations before doing so. People who experience spontaneous recovery will not require referral.
Pathways of care and role of primary care
Pathways of care
Adult care pathways: Figures 1 and 2 below are designed to help services and systems plan and deliver streamlined post-COVID services to provide consistency of service delivery and patient experience. The pathway for children and young people with long COVID is given in the CYP section.
Figure 1: Primary care/community long COVID pathway for adults
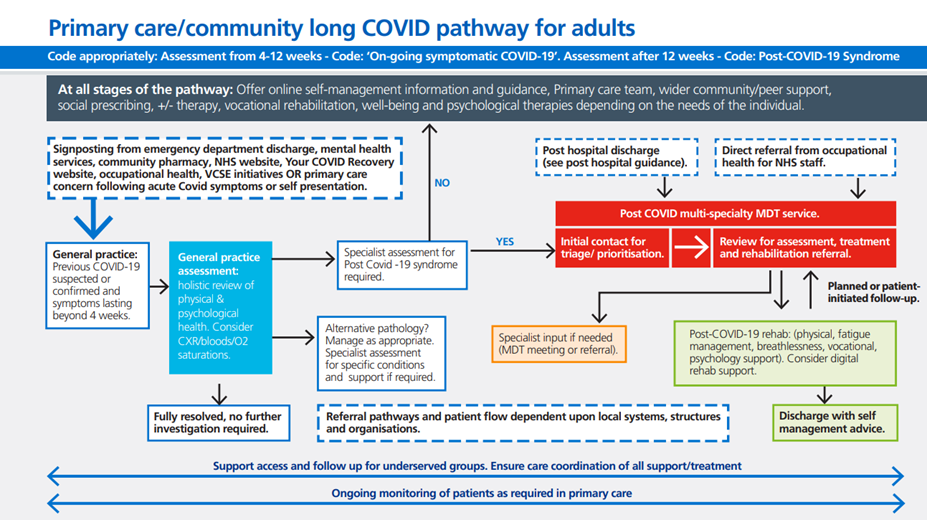
Figure 2: Post-hospital discharge pathway for adults with long COVID
Role of primary care
Primary care plays a key part in the long COVID clinical pathway:
- consider and exclude potential other causes of symptoms as per NICE/SIGN/RCGP
- determine appropriate management of symptoms and timing of onward referral to post-COVID services if appropriate
- code a diagnosis of ongoing symptomatic COVID19 or post-COVID syndrome appropriately
- signpost to self-management advice including the option of using Your COVID Recovery or other online resources
- refer to social prescribing link workers or health and wellbeing coaches as appropriate
- to provide ongoing care if needed following discharge from services/ completion of post-COVID rehabilitation and to re-refer to services if further support needed.
See Appendix E for suggested diagnostics in primary care.
Referral onwards from a post-COVID service
While some symptoms can be addressed immediately in the long COVID service, some patients will need further therapeutic input.
After a holistic assessment, clinicians should use shared decision-making to discuss and agree with the person (and their family or carers, if appropriate) what support and rehabilitation they need and how this will be provided.
This should include:
- advice on self-management (see self-management)
- initiation of treatment, rehabilitation, psychological support and vocational rehabilitation, if needed
- specialist referral for specific clinical scenarios
- transition between children’s and adult services should be supported and services should work flexibly to provide support based on the needs of the young person
- multi-faceted post-COVID rehab provision is a core requirement; services for which referral pathways should also be available or specialist input accessed include:
- respiratory services, sleep services and pulmonary rehabilitation
- cardiac services including cardiac rehabilitation
- neurology
- rheumatology
- dermatology
- ENT
- infectious disease services
- gastroenterology
- speech and language therapy services
- co-morbidity management, e.g., for diabetes or obesity
- occupational health
- Services for learning disability and autism
- dietetics and nutrition services
- pain management
- social care support services
- social prescribing link workers
- health and wellbeing coaches
- IAPT and other mental health services including cognitive management.
Principles of care for long COVID
Patients should be managed according to current clinical guidance such as that published and updated by NICE. Where possible, patients should be given access to any ongoing suitable programmes of research such as trials of treatment or rehabilitation.
Personalised care
An individual personalised care plan is one of the most important aspects of supporting recovery for people living with long COVID. Actively listening to people and asking, ‘what matters to you?’ supports planning and shared decision-making.
- Staff training can be accessed via the Personalised Care Institute (PCI) which provides a PCI-accredited eLearning website and access to accredited training providers and programmes and resources. More information can be found at NHS England » Personalised care.
Multidisciplinary support and rehabilitation
The skilled long COVID clinical multidisciplinary team should enable:
- the development of individual care plans for physical, mental, and social needs, which may include digital programmes such as Living with and ELAROS C19-YRS
- provision of the multi-faceted core rehabilitation offer
- access to clinical review and more specialist advice or rehabilitation when needed, typically via MDT case discussion meetings
- care co-ordination for streamlined care.
Supporting and enabling self-care including digital supported self-management
Individuals should be provided with information in a way that is accessible to them as digital tools may not be suitable for all. Options include these below:
- Signposting to the Your COVID Recovery website.
- Yourcovidrecovery is an NHS-supported online information platform designed for and with people with Long COVID offering information, advice, and guidance on physical, emotional, and psychological wellbeing.
- All this information can be downloaded to print and has been translated to 17 languages.
- ELAROS’ C19-YRS application offers a range of translatable educational and rehabilitation resources for adults and CYP which have been developed by its network of NHS organisations to facilitate clinical discussions alongside patient-reported outcomes collected from patients
- The Living With Covid Recovery virtual care platform is a multi-modal app for assessment, treatment, self-management and remote support and can be used for monitoring of cohorts and individual patients as their symptoms evolve.
- The app has a carer module that allows family member support, and data reports are available at clinic, ICS or regional level.
- Many services have developed written self-management material or webpage content such as short videos or recorded talks to align with their specific service model.
- Services should be encouraged to share this content through the clinical networks in place.
- Referral to social prescribing link workers based in primary care and/or in the VCSE sector.
- They connect people with activities, groups, and services in their community to meet practical, social, and emotional needs, including peer support.
- They can signpost patients to community support including financial and benefit applications.
- Referral to a health and wellbeing coach based in primary care.
- Access to peer support networks, where they exist.
Occupational health support and vocational rehabilitation
Most people experiencing long COVID are of working age, and long COVID can have a detrimental effect on their ability to work, care for others and carry out their usual activities.
Occupational health support and vocational rehabilitation are a core component of rehabilitation to support individuals with long COVID to return to work sooner and remain in work. Employers need to make reasonable adjustments for people with long COVID to allow them to return to work safely.
Post-COVID services should collect information on employment status and the impact of rehabilitation and treatment on a person’s ability to work and carry out their usual activities. They should support patients to coordinate with their employers and advocate for their needs.
Post-COVID services should be aware of any specific occupational health or human resource support available for various workforce groups especially those disproportionately affected by long COVID. For example, Guidelines for supporting our NHS people affected by Long COVID who have been noted to have a high prevalence of long COVID.
Post-COVID services should be aware of long COVID community champions and charities that provide various support for long COVID patients.
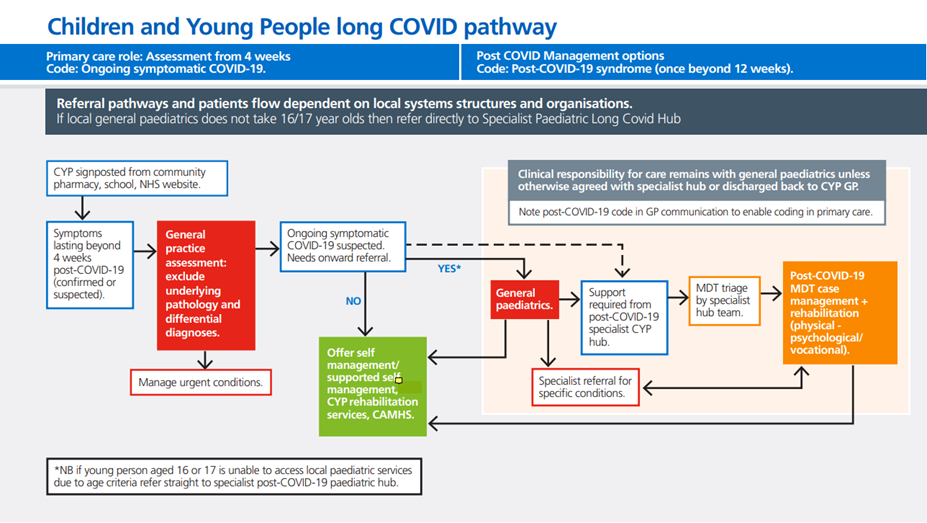
Children and young people
This guidance refers to children and young people (CYP) as those aged up to and including 17 years. People aged 18 years and over are referred to as adults.
The early assessment can be carried out by a GP, or if required, by a general paediatric service. Support should be offered where possible at the earliest opportunity to reduce symptoms and concerns and improve the quality of life.
The holistic bio-psychosocial assessment to:
- exclude other conditions
- identify co-morbidities
- identify effects on ability to undertake usual activities
- identify if a further specialist assessment is required
- offer early appropriate medical and holistic support.
The experience of existing CYP services is that most CYP with long COVID symptoms will improve or recover within 12 weeks following the acute infection, but some CYP may need to be referred for further assessment from four weeks. The timing of any onward referral should be based on clinical judgement.
CYP with suspected long COVID who are more severely affected or have complex health conditions will benefit from further multidisciplinary input, advice, and ongoing support. This cohort of patients should be referred to one of the CYP specialist post-COVID service teams established across England to provide expert advice to paediatric services.
Models of care
Access to CYP specialist post-COVID services should be made available across the region including from ICSs that do not have CYP specialist post-COVID services within their own system.
- Pathways should be in place to enable access to post-COVID services for all children up to and including 17-year-olds and may provide input for 18-year-olds still at school to provide support around exams and university transition.
Services employing a virtual consultation model should have the flexibility to offer a face-to face service depending on patient and family needs.
Principles of care (CYP)
CYP specialist post-COVID services
- Referral to specialist CYP post-COVID services should be locally agreed but may be via:
- initial primary care referral to general paediatrics in secondary care for advice, and onward referral to a specialist CYP post-COVID hub
- primary care referral directly to the specialist CYP post-COVID hub with a concurrent referral to local general paediatric services if agreed locally.
- Regular virtual MDTs to discuss referrals with the referrer should be held, including participation by the referring paediatrician and primary care team. A comprehensive letter to family and team is a useful part of the offer and should also be provided where care is transferred back to the referring team.
- Provide multidisciplinary and expert advice on the diagnosis and management of long COVID in complex cases or where there are co-existing complex conditions considering co-morbidity and patient/carer needs, and the psychosocial impact.
- Provide further assessment for impact and co-morbidities, including referrals to other specialists where necessary.
- Educate local clinicians on assessment and management of long COVID, and other relevant conditions and support the local delivery of rehabilitation and treatment.
CYP generalist management
- Children with special educational needs or neuro-disability may not be able to verbally express their symptoms, so behaviour changes and carer insights should be taken into account.
- Symptoms should be managed holistically, including medical and rehabilitative treatments, to relieve symptoms and reduce impact on daily life. Autonomic dysfunction, anxiety and low mood may need primary care management or onward referral.
- Multifaceted rehabilitation should be provided as locally as possible with access to further advice and support from the CYP specialist post-COVID services where required. Rehabilitation advice should include symptom management, and may include pacing, activity management, and pain management.
- Referral for further assessment and investigation is recommended if symptoms are not settling with simple interventions.
Assessments and treatment
- Bio-psychosocial assessment should include a comprehensive clinical history and examination to assess physical, cognitive, and psychological symptoms and functional abilities. A psychosocial screening tool such as the HEEADSSS assessment tool may be useful to identify psychosocial risks and resilience factors.
- Tests and investigations to exclude acute or life-threatening complications and establish whether symptoms are likely to be caused by ongoing symptomatic COVID-19, post-COVID-19 syndrome, or a new, unrelated diagnosis.
- Not all CYP with long COVID symptoms will need onward referral, many may be managed by the primary care team with measures including recommended investigations, advice on symptom management, general lifestyle, liaison with school, support for wellbeing, and treatment.
- As with adult services, some CYP may need further therapeutic input, rehabilitation, psychological support, specialist investigation or treatment once they have been assessed and patients should have access to relevant local services.
Recording activity and outcomes
- All CYP specialist post-COVID service teams should record and submit their specialist clinic activity as required to NHS England.
- All CYP specialist post-COVID services should record the health status of those who have accessed the service(s) at the point of new assessment (baseline) and at every six months thereafter until discharged. Health status primarily concerns symptoms (including brain fog and post exertional malaise), co-morbidities such as autonomic dysfunction, wellbeing, functioning and work/education status. CYP specialist post-COVID hubs should continue to review and log outcomes against those initially recorded to reflect the trajectory of recovery.
- Clinicians should consider recording against the core outcomes of significance for all new patients accessing the service in future.
Figure 3: Children and young people – long COVID pathway
Data and management information
There will be an ongoing need for data to inform service provision and clinical management and to reduce health inequalities. Data is used to support funding, operational decisions and research, and data quality is a key component of the commissioning for post-COVID services.
Data collection
- NHS England has set out the national data collection process for post-COVID assessment services. Guidance can be found on the NHS Futures website.
- NHS England will continue to provide updates on changes to the data collection process, to service providers as required.
- Each service provider should submit service activity as required to the post-COVID service data collection determined by NHS England.
- Each service provider should have a data lead who ensures data is submitted via established collection routes as determined by NHS England.
- Post-COVID assessment service activity should be recorded on local patient administration systems against the treatment function code for long COVID (348) and/or a specified clinic code for the post-COVID assessment service to support commissioning processes.
- Data collection supports monitoring of key indicators in relation to performance; referrals, waiting times and assessments, and health access; IMD, ethnicity, age, sex etc.
- Activity for post-COVID assessment services being submitted should be extracted from local patient administration systems using local business intelligence queries where possible to reduce the data collection burden on clinicians.
- Each service provider is encouraged to share the activity they submit to the national collection with the relevant local clinicians to ensure the accuracy of data.
- Nationally published statistics on Post-COVID Assessment Service activity will be produced monthly until April 2024, and nationally collected activity data will continue to be available through the Long COVID dashboard on the NHS National Data Platform (Foundry), accessible via request to NHS England (see guidance on NHS Futures).
Further support
Resources to support data and data collection are available on the Long COVID Network FutureNHS website. These include:
- frequently asked questions
- information on recommended codes
- data definitions.
Updates and changes to the method of data collection will be communicated to providers via NHS England and regional teams.
Key service outcomes
Adult and CYP services in primary care, secondary care and specialist services should collect and analyse patient-reported outcome measures, clinical measurements and patient reported experience measures to help monitor patient progress, facilitate communication between professionals and improve the quality of services.
Data also contributes to the evidence base on the management of long COVID efforts to reduce unwarranted variation in post-COVID services.
Outcome measures for adults with long COVID
- The 5-level EQ-5D version (EQ-5D-5L), Health-Related Quality of Life (HRQOL) measure, including the EQ Visual Analogue Scale (EQ VAS) component, should be completed for all patients on assessment, during follow-up or rehabilitation support at three or six months, depending on clinical judgement, and at discharge from treatment and/or rehabilitation. This tool allows comparison of long COVID outcomes with other health conditions.
- Additional outcome measures can also be used where clinically indicated, depending on symptom presentation, and to personalise the management or treatment approach. Disease specific tools have been validated in Long COVID such as the COVID-19 Yorkshire Rehabilitation scale, and the Symptom Based Questionnaire.
- Return to work and carer roles should be documented. This should be monitored as a measure of functional recovery. Many services have developed specific questions to document this.
- All providers are expected to collate information on patient experience in post-COVID services via the Friends and Family Test and a specific question on patient access.
- Of particular interest will be the experience of groups from underserved populations and those that experience health inequalities, as outlined in the health inequalities section. Aggregate reporting of patient experience will occur regionally and nationally.
NHS Standard Contract
Commissioners may use the NHS Standard Contract to commission post-COVID services. The service specification should be recorded in Schedule 2A of the Particulars of the Contract, where a non-mandatory model template for local determination and population is provided.
Guidance on developing the specification and populating the contract template is provided in the contract technical guidance.
Queries about using the contract can be sent to: nhscb.contractshelp@nhs.net.
Appendix A: Supporting resources.
Post-COVID-19 syndrome is a new illness, which we are learning more about every day. The following list of resources have been developed to help teams adapt to and learn about the condition.
Please note these resources, or their online location, may be updated. Please contact england.clinicalpolicy@nhs.net if you have difficulty accessing them.
Patient resources
- Patient safety learning and RCGP resource: Post COVID-19 syndrome: What support can patients expect from their GP?
- Your COVID Recovery
- How to conserve your energy: Practical advice for people during and after having COVID-19
- Home – Long Covid Support
- Long COVID SOS Charity
- Long Covid Kids | Charity | Post Covid Syndrome
- Long Covid Work – Supporting people with Long Covid to stay in, return to, or leave work well.
- Long COVID Physio
Workforce resources
- NICE/SIGN/RCGP COVID-19 rapid guideline: managing the long-term effects of COVID-19
- Long COVID network on the FutureNHS platform
- Health Education England (HEE) e-learning modules: Long COVID programme
- RCGP: Management of the long term effects of COVID-19
- Queen’s Nursing Institute: Living with COVID19 – Community and Primary Care Nursing Resource
- Managing the long-term effects of COVID-19. (Pharmaceutical Journal) Pharmacists in community and primary care should be able to provide patients with appropriate advice and support to manage their symptoms.
- NIHR resources:
- The Faculty of Occupational Medicine guidance for return to work for patients with Long-COVID: COVID-19: information for the respiratory community | British Thoracic Society | Better lung health for all (brit-thoracic.org.uk)
- NHS England: Allied health professionals’ role in rehabilitation during and after COVID-19
- The Faculty of Occupational Medicine: Guidance for return to work for patients with post-COVID syndrome
- Occupational therapy and adults with long Covid (post-COVID-19 syndrome/condition)
- Occupational therapy and children and young people with long Covid (post-COVID-19 Syndrome/Condition)
- Orthostatic tachycardia after covid-19 – PubMed (nih.gov)
Appendix B: An example of a clinical services specification developed by the London region
Assessment
1. Patients need access to in-person assessments, but some care can subsequently be delivered virtually.
2. Services must include input from a doctor with adequate expertise in the management of post-COVID syndrome. This could be a general practitioner with a special interest or a physician (but would not typically be a psychiatrist). Expertise is required in the following areas as an example:
- Investigation and management of breathlessness (ability to request chest imaging and lung function and to interpret results)
- Investigation and management of chest pain (ability to exclude cardiac causes through diagnostics when necessary)
- Investigation and management of fatigue
- Management of headache and migraine
- Management of dysautonomia
- Management of pain
- Management of sleep
- Management of anxiety and depression
3. Services should be able to access efficient input for decision making from the following specialities: respiratory, cardiology, neurology, rheumatology, ENT. Other specialty advice could be by usual routes (case discussion/A&G/referral). Ideally services would serve a hub function coordinating clinical input around the patient and avoiding multiple onward referrals and waiting times.
4. Patients benefit from early input rather than delaying to see if symptoms resolve spontaneously.
5. Assessment should generate a management and therapy plan. The core components of post-COVID rehab are fatigue management and symptom titrated exercise support, support for breathlessness/ disordered breathing pattern, integrated psychology support, and support re management of pain and dysautonomia and disturbed sleep. Vocational rehab will be needed for many (working age patient group.
Rehabilitation
1. Post-COVID rehab therapy teams need access to training in the condition. There is significant opportunity for skills transference between professions (OT/Physio/SLT/nursing/medical). There should be good integration between the medically supported post-COVID service and onward therapy input. Therapy input can be considered to have tiers of approach. At all tiers psychology input may be needed – such as via IAPT but ideally with dedicated support from a post-COVID psychologist.
- Tier 1 self-management advice, material (written and/ or video) access to peer support
- Tier 2 virtual input from an AHP for case management
- Tier 3 access to in-person support, eg for difficult disordered breathing pattern.
2. Given the multi-system nature of PCS and the range of interdisciplinary and multi-professional input care coordination is very important.
3. Outcomes should be documented regularly. Ideally via a digital platform if appropriate for the individual. The service should regularly review outcomes and compare to other benchmarks available nationally and internationally.
4. Any updates to NICE guidance re management of PCS should be noted and services will need to keep up to date via effective use of clinical networks.
Appendix C: Workforce supporting the post-COVID pathway
- NICE/SIGN/RCGP guidance recommends that access to multidisciplinary services is provided (these could be ‘one-stop’ clinics) for assessing physical and mental health symptoms and carrying out further tests and investigations. They should be led by a doctor with relevant skills and experience and appropriate specialist support, considering the variety of presenting symptoms.
- There is the opportunity for local systems to consider innovative and locally appropriate approaches to service leadership and skill mix. We recognise that different regional and geographical challenges mean that areas have different service needs and resources, so one model may not suit all areas. However, a core workforce is required within the post COVID service which includes a medical clinical lead with appropriate experience, physiotherapist provision, psychology provision and care coordinator roles. Access to other input will also be needed as listed below and the primary care team also play a central role in care provided.
- Medical input: Post COVID medicine is an emerging field and requires generalist skills with access to advice from multiple specialties. Doctors in post COVID services may have a primary care or physician background but they should have had adequate quantity, and breadth of experience of managing long COVID and dedicated sessions for this work. The medical workforce needs to stay abreast of the latest treatment and management advice and have access to appropriate training opportunities relating to post COVID medicine, management of fatigue and dysautonomia.
- Physiotherapists provide a holistic assessment to identify the specific needs of the patient and agree a personalised plan. They offer support, rehabilitation and self-management advice for patients dealing with symptoms such as breathlessness, deconditioning, fatigue, and dizziness, and can provide specific guidance on pacing, exercise, rest and recovery time.
- Speech and language therapists provide holistic assessments to identify the specific needs of the patient and agree a personalised plan with them. They support the rehabilitation and self-management of individuals with common post COVID-19 symptoms, including cognitive communication (‘brain fog’), swallowing, voice (including muscle tension dysphonia) and respiratory difficulties.
- Occupational therapists provide occupation-focused assessment of physical and mental health needs and cognition, offering self-management approaches to, for example, fatigue, brain fog, sleep disturbances, cognitive and psychological difficulties. They offer personalised advice and rehabilitation, enabling people to maintain and regain independence in daily activities, and vocational rehabilitation to support return to work and education.
- Psychologists can assess cognition and mental health. They can support patients managing persistent symptoms and can also provide access to services such as IAPT, wider health, social care and third-sector provision, and pain, fatigue and neuro-rehab services.
- Specialist nursing functions and roles such as district nursing, community nursing, mental health nursing, clinical nurse specialists, nurse consultants and general practice nurses can support holistic assessment and treatment of both the patient’s and wider family’s needs, while also supporting the co-ordination of services more widely where appropriate.
- Dietitians can support people living with long COVID in a range of ways, including advice on the impact of COVID-19 on nutritional status, and support to address malnutrition because of loss of appetite, breathlessness, swallowing difficulties or other long COVID symptoms.
- Pharmacists can support people on medication for other long-term conditions experiencing long COVID. People can be referred to pharmacy for a structured medication review (primary care) or for ‘new medicines service’ (community). They can also be signposted for self-care and over-the-counter symptomatic relief. Patients newly discharged from hospital can be referred to pharmacies for the ‘discharge medication service.’
- Care coordinators in post COVID services are support staff who have a good understanding of the post COVID pathway. They provide a point of contact for patients, advising patients about the pathway and supporting them through it, from receipt of referral to discharge.
- Social prescribing is a key component of universal personalised care and a way for local agencies to refer people to a link worker. Link workers connect people to community groups and statutory services for practical and emotional support. They can receive referrals from several professions across health, care and public services and people can self-refer.
The Primary Care Team and other community services
- Healthcare professionals working in primary care should be supported to access training and education on managing long COVID. They should have knowledge and understanding of local clinical pathways and engage in any quality improvement work to further develop the local pathways.
- Patients may also be supported by care coordinators in primary care who provide extra time, capacity, and expertise to help patients prepare for clinical conversations or follow-up discussions with primary healthcare professionals. They work closely with primary healthcare professionals to identify appropriate support for patients and their carers, ensuring that changing needs are addressed.
- Physician associates are an increasing part of the workforce within primary care, supporting the identification, referral and support of people living with long COVID.
- Social prescribing is a key component of universal personalised care and a way for local agencies to refer people to a link worker. Link workers connect people to community groups and statutory services for practical and emotional support. They can receive referrals from several professions across health, care and public services and people can self-refer.
Appendix D: Regional examples of interventions taken to tackle health inequalities
Midlands approach to post-COVID service funding allocation and health inequalities 2022/23
Background
The midlands region worked in liaison with public health colleagues and other stakeholders to develop a post-COVID service funding allocation approach which adjusts for inequalities within 11 ICSs. The methodology and rationale behind the allocation across the Midlands was informed by several perspectives among which include:
- knowledge of the differential epidemiological patterns of acute and chronic illness following COVID-19 infection
- recognition of the priority placed on addressing health inequalities and delivering the NHS CORE20PLUS5 initiative
- evidence of poorer access to, experience of and outcomes from healthcare services in more deprived areas and likely higher cost of service provision in more inaccessible places.
Methodology
Core allocation
- Divided up 90% of the funding by looking at the number of COVID-19 infections between April 2020 and November 2021 by ICS in comparison to the weighted population size of that system.
- COVID-19 infection numbers were used (as opposed to modelled estimates of post-COVID-19 syndrome cases) because of the availability and robustness of the data.
- This allowed the region to determine the relative proportion of this part of the budget that each ICS should be given.
Health inequalities allocation
- 10% of the overall Midlands post-COVID allocation was dedicated to proportionately tackling health inequalities.
- To determine the proportion of this funding each ICS should be allocated, the region considered the number of people living in the most deprived quintile (Index of Multiple Deprivation [IMD] 2019 quintile 1) to determine the size of need for enhanced support in the ‘CORE20’ population.
- This allowed determination of the relative proportion of the budget that each ICS has been allocated.
East of England’s example of proactive approach to tackling diagnostic overshadowing among patients with learning disability and autism
Background
Hertfordshire services provided by Hertfordshire Community Healthcare Trust and Central London Community Healthcare Trust, worked in collaboration with Hertfordshire County Council to improve long COVID care among patients with Learning disabilities.
Interventions
- The collaboration developed and held long COVID webinars targeted at paid carers who support people with learning disabilities. These webinars explained the symptoms of long COVID and how to recognise them in people who may be unable to express physical and mental symptoms directly.
- The webinars brought in the long COVID assessment and treatment service leads in Hertfordshire to describe the treatment being offered for people with long COVID, explain how the service works and how to access it through a GP.
Production of an easy read booklet on long COVID, so that patients with learning disabilities could have material that they could understand and use to communicate to their carers.
Appendix E: Post-COVID-19 syndrome diagnostic pathway
Investigations should be tailored to the patient’s symptoms and exclude other causes as far as possible. The list below is based on NICE guidance and feedback and learning from clinical services.
It is intended as a guide to investigations that may be required, depending on the patient’s presentation, and are not intended to be prescriptive or exhaustive.
Primary care diagnostics
Key aim: To rule out serious underlying pathology or alternative diagnosis that would prompt referral other than to post-COVID services.
Possible tests according to symptoms
General bloods:
- FBC
- U&E
- LFT
- TSH
- HbA1c
- ferritin
- vitamin D
- lipid profile
- Blood panel:
- As per primary care + D-dimer, troponin, clotting studies, CK, autoimmune profile
- Breathlessness:
- Assessment for disordered breathing pattern, Chest X-ray, oxygen saturation, full lung function including spirometry, lung volumes and gas transfer, CTPA/HRCT, FeNO, sleep studies, walk test such as 6-minute walk or shuttle walk test. Assessment for dysautonomia which can contribute to breathlessness/ exercise intolerance.
- Palpitations:
- Active Lean test, ECG, Holter, 24-h blood pressure,
- Chest pain:
- ECG, NT-BNP, echo, troponin, NT-BNP (acute medicine access), cardiac MRI if myocarditis suspected (could be via cardiology referral or discussion with cardiology)
- Fatigue:
- TSH, ferritin, ESR, testing for other viral infection- HIV, testing for adrenal insufficiency if risk factors present.,
- Abnormal LFTs:
- US abdomen, hepatitis screen, lipid profile
- Dizziness:
- Active Lean test, Holter, 24-h blood pressure, access to referral for testing for autonomic dysfunction, consider use of the adapted autonomic profile home-based testing
- Cognitive difficulties/brain fog:
- Brain imaging not typically helpful but if atypical presentation will need consideration of CT Head/ MR Head and discussion with neurology or memory services.
Long COVID service
Investigations should be directed by presenting problems, based on clinical assessment and judgement.
Post-COVID services should have direct access to, be able to interpret and act on the investigations suggested below. (These are an addition to the investigations already completed in primary care)
Blood panel: As per primary care + D-dimer, troponin, clotting studies, CK, autoimmune profile
Breathlessness: Assessment for disordered breathing pattern, Chest X-ray, oxygen saturation, full lung function including spirometry, lung volumes and gas transfer, CTPA/HRCT, FeNO, sleep studies, walk test such as 6-minute walk or shuttle walk test. Assessment for dysautonomia which can contribute to breathlessness/ exercise intolerance.
Palpitations: Active Lean test, ECG, Holter, 24-h blood pressure
Chest pain: ECG, NT-BNP, echo, troponin, NT-BNP (acute medicine access), cardiac MRI if myocarditis suspected (could be via cardiology referral or discussion with cardiology)
Fatigue: TSH, ferritin, ESR, testing for other viral infection- HIV, testing for adrenal insufficiency if risk factors present
Abnormal LFTs: US abdomen, hepatitis screen, lipid profile
Dizziness: Active Lean test, Holter, 24-h blood pressure, access to referral for testing for autonomic dysfunction, consider use of the adapted autonomic profile home-based testing
Cognitive difficulties/ Brain Fog: Brain imaging not typically helpful but if atypical presentation will need consideration of CT Head/ MR Head and discussion with neurology or memory services.
Appendix F: Coding
Primary care coding
It is important to accurately capture data on primary care activity related to long COVID, to support demand modelling, service planning and research.
Primary care should code for all the following data categories (the ‘minimum dataset’), if applicable, when delivering care for people with ongoing symptomatic COVID-19 or post-COVID-19 syndrome:
- COVID-19 diagnosis (where this has not been previously recorded)
- 1325181000000106 Ongoing symptomatic disease caused by severe acute respiratory syndrome coronavirus 2 (disorder)
- 1325161000000102 PostCOVID-19 syndrome (disorder)
- red flag symptoms/signs
- diagnostics/investigations
- management/referrals
- 1325031000000108 Referral to post-COVID assessment clinic (procedure)
- 1325021000000106 Signposting to Your COVID Recovery (procedure
- outcome measure score – EQ-5D-5L, EQVAS (where available)
Primary care clinicians are encouraged to use appropriate clinical templates to support coding.
Patients do not need to have had a positive SARS‑CoV‑2 test (PCR, antigen or antibody) or a previous COVID-19 diagnosis code for the post-COVID-19 syndrome codes to be used.
Secondary care coding
A treatment function code (TFC) for post-COVID services has been available since April 2021. It is defined as follows:
- TFC number: 348
- TFC name: post-COVID-19 syndrome service
- TFC description: multidisciplinary services for patients experiencing long-term health effects following COVID-19 infection, whether this was diagnosed at the time of acute illness, or the patient was initially asymptomatic. Post-COVID-19 syndrome has also been known as ‘long COVID’.
- Providers of post-COVID services should use the TFC for their service, which will enable tracking of service activity and associated onward diagnostic and referral activity. Services should also ensure complete demographic data (age, sex, ethnicity, postcode) is recorded for each patient.
- Community care coding.
- Post-COVID services should ensure implementation of SNOMED CT coding where compatible clinical information systems are in place. A post-COVID service coding minimum dataset to guide coding can be found on the Long COVID Network FutureNHS website. Clinics should ensure complete demographic data (age, sex, ethnicity, postcode) is recorded for each patient.
Publication reference number: PRN00488

