Introduction
Heart failure and respiratory conditions are leading causes of patient morbidity, disability, mortality and health inequalities in England, and place a significant and potentially avoidable burden on the NHS.
Patients can miss the opportunity of an early diagnosis, either because tests are not made available to them or because there are long waits for the diagnostics they need. Yet there are simple interventions and diagnostics which can be deployed in general practice to give patients a clearer picture sooner. For example, GPs should have access to spirometry in the community and while various models exist, the pandemic had an impact on the delivery of spirometry in community settings.
With an estimated 107,000 fewer new cases of asthma and 87,000 fewer new cases of chronic obstructive pulmonary disease (COPD) between March 2020 and December 2021, it is critical that action is taken to enhance GP direct access to diagnostic tests. This can be achieved by maintaining, restoring or enabling access to local services and, where service restoration is challenging, by taking the opportunities for more spirometry and fractional exhaled nitric oxide (FeNO) testing outlined in this guidance.
GPs should also have access to N-terminal pro B-type natriuretic peptide (NT-proBNP) blood tests and the corresponding phlebotomy services to refer patients with suspected heart failure. This test should be used as a triage for echocardiography (echo), however recent feedback from several echo services suggests that a significant proportion of suspected heart failure patients are referred for echo without a prior NT-proBNP test. Diagnosis of heart failure through hospital admission continues to dominate. It is associated with a significantly greater short-term risk of mortality and substantially increased long-term costs, than if first diagnosed in the community. Evidence shows that 40% of heart failure patients presenting in an emergency department for the first time had symptoms that should have triggered an earlier assessment in primary care. To address this, GPs must enable highest-risk heart failure patients to get faster access to echo testing. Data from January 2023 shows that nearly 165,000 patients were waiting for an echo test, up nearly 3% since January 2022. More than 40% of these patients were waiting over 6 weeks. Delivering these echo tests is best achieved by using NT-proBNP as a triage, as it will make detecting undetected heart failure feasible.
By enhancing GP direct access to rapid spirometry and FeNO testing, and ensuring that GP direct access to NT-proBNP provides a triage for echo, we can:
- Achieve the earlier detection and diagnosis of chronic obstructive pulmonary disease and asthma, enabling early interventions for optimal treatment, better management of the conditions and benefits to the health system. Earlier detection can also lead to a reduction in acute admissions, reduction in non-elective winter admissions, resource utilisation, improvement in quality of life and healthy life expectancy.
- Achieve the earlier detection and diagnosis of heart failure, enabling referral for specialist assessment and echo in non-acute symptomatic patients, more effective use of echo capacity and provide faster access to echo tests for acute heart failure patients.
About the guidance
This guidance supports operational planning guidance which requires systems to: “Increase GP direct access in line with the national rollout ambitions and develop plans for further expansion”.
It advises general practice, providers of respiratory diagnostics, pathology laboratories and integrated care boards on the provision of GP direct access pathways for adult patients with symptoms indicative of chronic respiratory diseases (chronic obstructive pulmonary disease [COPD] and asthma) and heart failure.
The guidance recommends that general practice teams refer patients for the following tests:
- spirometry for the diagnosis of COPD with FeNO for suspected asthma, complementing National Institute for Health and Care Excellence (NICE) guideline NG80.
- NT-proBNP for patients with suspected heart failure, prior to a referral for an echo. The results from the NT-proBNP test must be used to determine whether an echo test is required for suspected heart failure, complementing NICE guideline NG106.
To ensure that GPs receive timely test results, the guidance sets an expectation on the wait and turnaround times that respiratory diagnostic, cardiac services and pathology laboratories should adhere to for each test.
It also recommends that the post-diagnostic management of low-risk patients is balanced between primary and secondary care, while patients with urgent test findings can be referred straight to secondary care services.
This guidance is not a clinical guideline but sets out the pathways that are required to achieve the following aims:
- Increase patient access to diagnostics for COPD and asthma, so that more patients are diagnosed early enabling proven interventions to be delivered to improve outcomes.
- Effectively triage patients with suspected heart failure, so that highest-risk patients can have shorter waits for these tests.
Using the guidance
Drawing on clinical guidelines
This guidance should be delivered in line with the following National Institute for Health and Care Excellence clinical guidelines:
- Asthma: diagnosis, monitoring and chronic asthma management [NG80]
- Chronic obstructive pulmonary disease in over 16s: diagnosis and management [NG115]
- Chronic heart failure in adults: diagnosis and management [NG106]
- Pneumonia in adults: diagnosis and management [CG191]
Ensuring equity of patient access
General practice referrers, providers of respiratory diagnostics and pathology laboratories should consider the following when implementing this guidance:
- In 2020, the rate of premature mortality due to respiratory disease among people living in the most deprived quintile of areas was at least twice the average for England.
- In 2020, The rate of premature mortality due to cardiovascular disease (CVD) in the most deprived deciles was more than double that in the least deprived deciles. In that year, 5,976 people in the 10% most deprived areas of England died prematurely from CVD.
- Many people with a learning disability and severe mental illness also have chronic health problems such as heart and respiratory conditions. (Emerson E, Hatton C (2013). Health inequalities and people with intellectual disabilities).
- Older adults who are homebound are often socially isolated, have unmet care needs, suffer from high mortality and are invisible to health systems.
- Populations experiencing inequalities are more likely to experience premature frailty and those with the greatest need often also find it hardest to access and receive appropriate care and support.
- Results from a GP patient survey in 2021 show that people from the most deprived areas were less likely to report that their needs were being met, had a poorer overall experience and a worse experience of making an appointment.
- Socially excluded groups can report challenges in registering with a GP surgery when they do not have a fixed address, particularly those living in Gypsy and Traveller sites or at the roadside.
GP practices have put initiatives in place, with support from commissioners, to improve patient access and ensure that enhanced GP direct access to spirometry, FeNO and NT-proBNP are available to all local communities. These include:
- new consultation types and access hubs
- targeting access by providing consultations outside traditional care settings
- improving communications with patients and broadening the general practice skill mix to provide unique skills that can benefit patients.
Tackling inequalities in healthcare access, experience and outcomes guidance is also available to support all NHS providers.
Enhancing GP direct access to spirometry, fractional exhaled nitric oxide (FeNO) and N-terminal pro B-type natriuretic peptide (NT-proBNP)
Increasing access to tests for patients with symptoms indicative of chronic obstructive pulmonary disease (COPD) or asthma
GPs (in or out of hours) or other referrers within general practice should refer all patients presenting with symptoms indicative of COPD or asthma for spirometry and FeNO tests where no local services exist.
Symptoms include:
- exertional or nocturnal breathlessness
- a chronic cough
- regular sputum production
- frequent winter ‘bronchitis’ and/or a wheeze.
Local commissioners can use NHS England guidance for spirometry commissioning to restore their local services. Where this is challenging, the increasing availability of spirometry and FeNO testing will equip more general practice teams to refer patients using direct access. This means that GPs without existing local services can:
- Refer directly via the Electronic Referral System (e-RS) to community diagnostic centres (CDCs), which are increasingly providing these tests. Guidance is available below and on the NHS Futures platform (log in required) to support e-RS leads and CDC operational leads to put the right systems in place. A list of CDCs providing spirometry and FeNO testing is also available on the NHS Futures platform.
- Use new models for delivering quality assured spirometry, details for which are available on the NHS Futures platform..
General practice teams can refer patients with uncertain symptoms that suggest either a respiratory condition or heart failure onto breathlessness pathways that are being delivered through several CDCs (listed on the NHS Futures platform). This pathway provides a combination of tests and can support GPs to diagnose and optimise uncertain COPD, asthma, and heart failure referrals. This uncertainty can be the result of some COPD and asthma symptoms also being indicative of heart failure, including exertional or nocturnal breathlessness, a chronic cough and regular sputum production. Guidance underpinning the delivery of the breathlessness pathway is available on the NHS England website.
To ensure we can increase patient access to spirometry and FeNO, this additional provision should complement, but not be in place of, existing established models of delivery in general practice.
To support GPs to access spirometry and FeNO testing via existing local services or other provision, NHS England is:
- Guiding clinical networks to support integrated care boards to transition to new models of delivering quality assured spirometry, address backlogs and ensure diagnosis rates increase above pre-pandemic levels.
- Providing guidance and a support pack that enables systems to establish services that will increase the number of people receiving early, accurate diagnosis for respiratory disease.
- Working with the Association of Respiratory Technology and Physiology to increase the number of individuals accredited in the delivery of quality assured spirometry by making the route to certification easier to navigate and more achievable.
Increasing access to N-terminal pro B-type natriuretic peptide (NT-proBNP) as a triage for echo for patients with symptoms indicative of heart failure
GPs should refer all patients presenting to general practice with suspected heart failure for an urgent NT-proBNP blood test.
Symptoms include:
- breathlessness
- oedema indicative of heart failure
- fatigue indicative of heart failure.
Pathology laboratories can advise on which patients are appropriate for NT-proBNP measurement.
Critically, an NT-proBNP test must be used as a triage for referral to echo, in line with National Institute for Health and Care Excellence guideline NG106. This will ensure that higher-risk patients get faster access to an echo test. GPs may also want to consider the patient’s history and, where possible, an accompanying electrocardiogram.
NT-proBNP tests can be undertaken alongside routine blood tests in any phlebotomy service and the Getting It Right First Time (GIRFT) pathology team are working to ensure all NHS pathology laboratories are equipped to provide results. General practice teams can also order NT-proBNP tests via community diagnostic centres (CDCs). NT-proBNP is one of the combination of tests available on the breathlessness pathway referred to above, and GPs can use this pathway for patients with uncertain symptoms indicative of either a respiratory condition or heart failure.
Pathology laboratories should provide information or recommendations for results below or above appropriate thresholds.
The NHS England Diagnostics Transformation Programme is taking action to reduce waits for echo, by:
- increasing echo capacity via CDCs
- running annual echo improvement workshops with systems and cardiac networks
- developing and disseminating an echo systematic improvement guide
- investing in echo training pathways.
Wait and turnaround times
Providers of respiratory diagnostics and pathology laboratories should adhere to the following wait and turnaround times to ensure that patients can benefit from an early diagnosis:
Spirometry
- Time from referral to test: 3 weeks
- Time from test to acquisition of report: 2 weeks
Fractional exhaled nitric oxide (FeNO) and N-terminal pro B-type natriuretic peptide (NT-ProBNP)
- Time from referral to test: 1 week
- Time from test to acquisition of report: 48 hours
Ensuring direct booking via the Electronic Referral System (e-RS)
We recommend that general practice referrers use e-RS to book direct-to-test appointments, including when referring to community diagnostic centres (CDCs).
Trust e-RS leads should work with CDC operational leads to link both appointment slots with existing diagnostic service providers and CDCs’ patient administration system (PAS) to e-RS directly bookable services (DBS). This will enable general practice teams to book an appointment for a test before the patient leaves the consultation. If the patient wishes to book their test appointment later, the healthcare practitioner or practice can email the test request referral to the patient and they can arrange their own appointment using the online Manage your Referral Service, via the NHS App or by calling the telephone appointments line.
Further details of requirements for e-RS direct-to-test are available on the NHS Futures platform (login in required).
Balancing patient management between primary and secondary care
Pathways have been developed (see below) to ensure that the management of patients following their test results is balanced between primary and secondary care. This includes direct referral to secondary care services where the test result shows urgent findings, with a clinical specialist communicating the results to the patient and sharing these with the general practice referrer.
Where test results are normal, GPs will need to investigate other causes for the patient’s symptoms, using their detailed knowledge of the patient’s history.
Where the results are not normal but do not require an urgent referral, GPs will be provided with clear actionable next steps, including details of any further tests.
Suspected chronic obstructive pulmonary disease (COPD) and asthma pathway
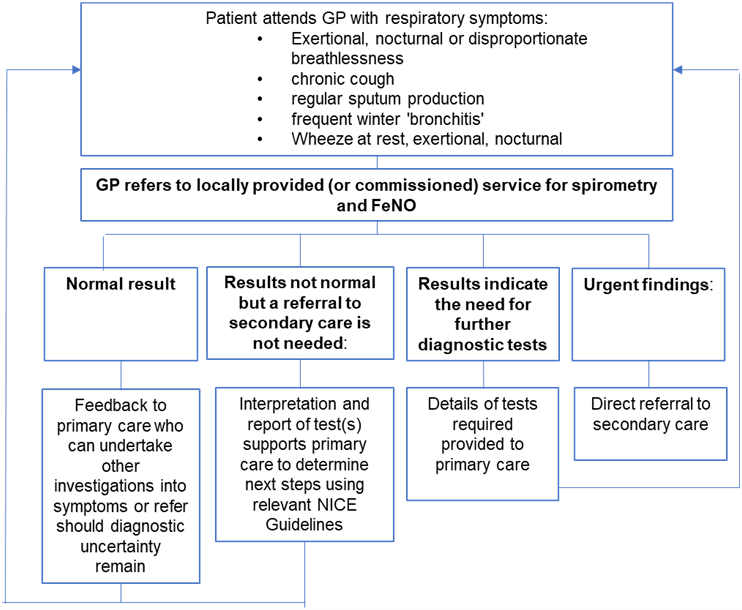
The diagram above shows the suspected COPD and asthma pathway for GP to follow post referral to locally provided (or commissioned) service for spirometry and FeNO. It shows the care escalation routes depending on the result of the spirometry and the FeNO results.
- Top of the chart begins with “patient attends GP with the following respiratory symptoms”:
- exertional, nocturnal or disproportionate breathlessness
- chronic cough
- regular sputum production
- frequent winter `bronchitis’
- wheeze at rest, exertional, nocturnal.
- If these symptoms are observed, then the GP refers to locally provided (or commissioned) service for spirometry and FeNO.
- If the results of the spirometry and FeNO are normal, the GP then feedback to primary care who can undertake other investigations into symptoms or iRefer should diagnostic uncertainty remain.
- If the results of the spirometry and FeNO are not normal but a referral to secondary care is not needed, the GP then interprets, and report of test(s) supports primary care to determine next steps using relevant National Institute for Health and Care Excellence guidelines.
- If the results of the spirometry and FeNO indicate the need for further diagnostic tests, the details of tests required provided to primary care.
- If the results of the spirometry and FeNO indicate urgent finding, then a direct referral to secondary care is made.
Suspected heart failure pathway
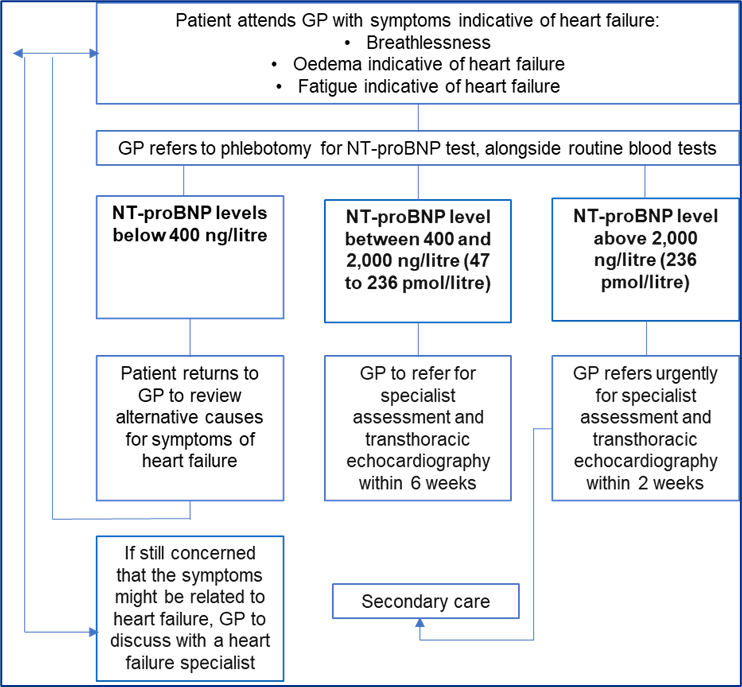
The diagram above shows the suspected heart failure pathway for GP to follow post referral to phlebotomy for NT-proBNP service. It shows the care escalation routes depending on the result of the NT-proBNP tests.
- Top of the chart begins “patient attends GP with symptoms indicative of heart failure”:
- breathlessness
- oedema indicative of heart failure
- fatigue indicative of heart failure.
- If these symptoms are observed, the GP refers to phlebotomy for NT-proBNP test, alongside routine blood tests.
- If the NT-proBNP levels are below 400 ng/litre, the patient returns to GP to review alternative causes for symptoms of heart failure.
- If still concerned that the symptoms might be related to heart failure, GP to discuss with a heart failure specialist.
- If NT-proBNP levels are between 400 and 2,000 ng/litre, the GP refers for specialist assessment and transthoracic echocardiography within 6 weeks.
- If NT-proBNP are above 2,000 ng/litre, the GP refers urgently for specialist assessment and transthoracic echocardiography within 2 weeks and care management then moves to secondary care.
Time to the echo test relates to both the acquisition and reporting of the echocardiogram.
Acknowledgements
The following contributed to the development of this guidance:
- National Specialty Advisor for Physiological Science, NHS England
- National Clinical Advisor for Heart Failure, NHS England
- Royal College of General Practitioners
- British Medical Association
- Primary Care Respiratory Society
- Association of Respiratory Technology and Physiology
- British Thoracic Society
- British Society for Heart Failure
- British Society of Echocardiography
- Asthma + Lung UK
The following were consulted on this guidance:
- Association of Respiratory Nurse Specialists
- British Cardiovascular Society
- Society for Cardiological Science and Technology
- Pumping Marvellous
- British Heart Foundation
Publication reference: PRN00809

