1. Introduction
1.1. Aim and key principles
This guidance is intended to support preparedness for and management of suspected or confirmed measles cases in healthcare settings. It sets out key infection prevention and control (IPC) principles required to prevent transmission of measles in healthcare settings and provides resources to support patient screening, triage, management (appendices 1 and 2), and assessment of risk applying the hierarchy of controls (HoC) (appendix 3). Further information and resources can be found within the National IPC Manual for England.
To support application of these principles organisations should ensure that:
- immunisation status/records are available for all staff (clinical and non-clinical) that may be exposed to a suspected or confirmed case of measles and staff are supported to ensure they are fully immunised. Satisfactory evidence of protection would include documentation of having received 2 doses of MMR or having had a positive antibody test for measles.
- patient screening, triaging and testing protocols are in place for all relevant care settings to ensure prompt isolation of suspected or confirmed cases of measles.
- a respiratory season or winter plan is in place to ensure, for example, appropriate segregation of patient cases depending on the pathogen and management of increasing case numbers where they occur.
- FFP3 respirator fit testing is completed for staff who may be required to assess or clinically care for a suspected or confirmed measles case.
- training in IPC measures is provided to all staff, including: the correct use of PPE and the correct technique for donning and doffing (putting on and removing) PPE safely.
- risk assessment(s) is undertaken for staff who may be at high risk of infection and/or complications from infection with measles.
Additional information can also be found in the:
- the national measles guidelines on GOV.UK
- the Green Book of Immunisation’s chapter on measles
- NICE’s measles diagnosis pages
A glossary of terms is available in the National Infection Prevention and Control Manual (NICPM) for England.
The UK Health Security Agency has a ‘Think Measles’ Poster for A&E, walk-in and GP centres.
1.2. Measles virus (Rubeola)
Measles is a highly infectious, notifiable, vaccine-preventable, acute viral disease.
Initial symptoms include fever, conjunctivitis, cough, runny nose and sneezing. This may be followed by small grey/white spots, called Koplik’s spots, on the inside of the mouth 1 to 2 days before rash onset, which may last for 2 to 4 days. These spots are often confused with other lesions in the mouth and so their suspected presence is an unreliable marker of measles.
Measles rash appears brown or red and blotchy on white skin but may be harder to detect on black or brown skin. The rash develops 2 to 4 days after the onset of fever and spreads from the head to the body over the next 3 to 4 days.
Measles is transmitted via airborne respiratory particles or direct contact with nasal/throat secretions of infected individuals.
It has an incubation period ranging between 7 to 21 days (mean: 10 to 12 days) and individuals are typically infectious from 4 days before and up to 4 full days after rash onset.
The exclusion period from healthcare settings, workplaces and educational settings is for the duration of the infectious period, which includes a full 4 days after onset of the rash.
Further information can be found on:
- NHS website’s measles page
- this GOV.UK factsheet on the symptoms, diagnosis, complications and treatment of measles
1.3. At-risk populations and settings
Anyone who has not had measles infection before or who has not had 2 doses of a measles containing vaccine will be susceptible to measles. Vulnerable groups include immunosuppressed individuals, infants under 1 year of age and pregnant women. These groups are more at risk of developing severe complications including pneumonia or bronchitis, convulsions, diarrhoea, meningitis or encephalitis, immune thrombocytopenic purpura (ITP) and late-onset subacute sclerosing panencephalitis (SSPE).
At-risk settings include settings where infectious patients may present for care, including GP surgeries and emergency care. They also include settings where vulnerable patient groups may be exposed, such as neonatal and paediatric units, antenatal clinics and maternity units, haematology, and oncology units.
This list is not exhaustive. If vulnerable individuals are exposed to a suspected or confirmed case of measles, a risk assessment should be undertaken to urgently consider need for post-exposure prophylaxis. Refer to the guidance in the national measles guidelines.
2. Infection prevention and control
2.1. Standard infection control precautions (SICPs) and transmission based precautions (TBPs)
All staff should be familiar with standard infection control precautions (SICPs) and transmission based precautions (TBPs) as set out in Chapters 1 and 2 of the National Infection Prevention and Control Manual (NIPCM) for England.
Staff should follow the principles of SICPs, as set out in the National Infection Prevention and Control Manual (NICPM) for all patients, whether infection is known to be present or not. This will help protect those being cared for, staff and visitors to the care environment. TBPs are applied when SICPs alone may be insufficient to prevent cross transmission of specific infectious agents. TBPs are additional infection control precautions required when caring for patients with known or suspected infections.
This guidance includes specific guidance for patient placement, personal protective equipment (PPE), durations of precautions, advice for visitors, and occupational health (OH) when managing a case of suspected or confirmed measles. Refer to the NIPCM for guidance on all other elements of SICPs and TBP.
2.2. Patient placement
Patients must be promptly assessed for infection risk on arrival at the care area (for example, inpatient or outpatient) and should be continuously reviewed throughout their stay. The assessment should influence patient placement decisions in line with clinical or care need(s). If a patient is requested to attend secondary care, or requires transfer within a secondary care facility, their infectious status should be communicated to the receiving department.
2.2.1. Patient placement in primary care or outpatient settings
If remote consultation is not possible or if, following telephone triage, a patient with suspected or confirmed measles is required or advised to attend primary care or outpatient settings, there should be separation in space and/or time between patients. Patients attending with suspected measles infection should be prioritised for assessment/treatment and isolated at the time of arrival (for example, directed to a side room). Appointments should be scheduled to reduce waiting times in reception areas (where necessary) and avoid cross-over of infectious and non-infectious patients.
If transfer from a primary care facility to a hospital is required, ambulance services should be informed of the infectious status of the patient. Patient confidentiality must be maintained.
2.2.2. Patient placement in accident and emergency departments
Patients attending without prior notification should ideally be screened and triaged at the reception or entrance.
Patients with suspected measles should not wait in communal areas or reception areas and should be placed in a segregated area (ideally a single room away from others) as soon as possible.
If patients with suspected measles arrive in A&E by ambulance, the ambulance service should pre-alert the receiving department to ensure they are admitted directly to a side room or segregated area.
This must not compromise or delay patient care.
2.2.3. Patient placement and cohorting in inpatient settings
In the hospital setting, patients with suspected or confirmed measles should, whenever possible, be placed in a negative-pressure isolation room with en-suite facilities.
If negative-pressure isolation rooms are limited, infectious patients who have conditions that could increase the risk of transmission of infection to other patients (such as an excessive cough) should be prioritised for placement in a single room, ideally with en-suite facilities. Patients should be moved to a negative-pressure isolation room as soon as one becomes available. If a single room or a negative-pressure isolation room is not available, cohort patients with confirmed measles with other patients confirmed to have the same infectious agent.
In a situation where multiple suspected and confirmed measles cases occur (for example, during an outbreak) patients with suspected infection can be cohorted together following a risk assessment. However, they should not be cohorted with confirmed measles cases. Risk assessment should consider the vaccination and disease history of suspected cases and individuals who may be exposed.
Infectious patients should only be transferred to other departments if clinically necessary. See section 2.3.2
2.2.4. Staff cohorting
As an additional infection control measure during outbreaks or incidents, consideration should be given to assigning a dedicated team of care staff to care for patients in isolation or cohort rooms and areas. This can only be implemented if there are sufficient levels of staff available (so as not to have a negative impact on non-affected patients’ care). Only staff whose vaccination status, disease history or immune status is known should be assigned to isolation or cohort rooms and areas.
2.3. Personal Protective Equipment (PPE)
Before undertaking any procedure, staff should assess any likely exposure to blood and/or other body fluids, non-intact skin or mucous membranes and wear personal protective equipment (PPE) that protects adequately against the risks associated with the procedure. Refer to the NIPCM sections 1.4, 2.4 and appendices 5b and 6 for further information of the use of PPE, including donning and doffing.
2.3.1. PPE for assessment and management of confirmed and suspected cases of measles
Staff should wear the following PPE when assessing or managing patients with confirmed or suspected measles:
- single-use, disposable gloves
- single-use, disposable apron (or gown if extensive splashing or spraying, or performing an aerosol generating procedure (AGP))
- respiratory protective equipment (RPE)
- eye/face protection (goggles or visor)
2.3.2. Surgical face masks as source control
If the patient has confirmed or suspected measles, then if possible/tolerated the patient should wear a surgical face mask (type I/II/IIR) in communal areas (for example, during transfer). The request for patients to wear a facemask must never compromise their clinical care.
Note: FFP3 respirators or powered respirator hoods must never be worn by an infectious patient.
2.3.3. Sessional use of RPE in outpatient and inpatient settings only.
Where patients are cohorted, consideration can be given to sessional use of RPE (including eye/face protection). All other items of PPE (gloves and gowns) must be changed between patients and/or after completing a procedure or task.
2.4. Duration of precautions
In general, patients should remain in isolation or cohorted, and TBPs should be applied until resolution of symptoms and/or in accordance with the exclusion period (4 full days after rash onset, where day 0 is the date of onset of rash).
The duration of TBPs may require modification as some patients with more severe illness or underlying immune problems may remain infectious for a longer period. TBPs should only be discontinued in consultation with clinicians (including microbiology/IPC team).
2.5. Advice for parents, carers, and visitors
Parents and carers should be supported to attend the care area while minimising the risk of exposure to other patients and themselves. Non-essential visitors should be minimised. Parents, carers, or visitors with symptoms (or who are a known, non-immune contact – for example, siblings) should not be permitted to enter a care area. However, if their presence is considered essential for compassionate (end of life) or other care reasons (for example, they are a parent or child) a risk assessment should be undertaken and mitigations (including source control) put in place to support attendance wherever possible.
Parents, carers, and visitors should be instructed on effective hand hygiene, be made aware of any infection risks, and offered appropriate PPE. Appropriate PPE (see section 2.3.1) should be considered for parents, carers, or visitors who are considered a non-immune contact. Parents, carers, or visitors who are considered a household contact of the infected patient do not require PPE. Powered respirator hoods are an alternative to tight-fitting FFP3 respirators (for example, when fit testing cannot be achieved) if there has been no previous exposure to the infected person or the measles virus.
Parents, carers, or visitors should not be present during AGPs on infectious patients unless they are considered essential following a risk assessment.
It may be considered appropriate to restrict visiting in the event of an outbreak of measles within the healthcare setting. This is a local outbreak management team decision.
2.6. Occupational health (OH)
If staff are uncertain of their immunisation status, they should discuss this with their occupational health provider.
In relation to childhood illnesses and use of RPE, no vaccine confers 100% protection and a small proportion of individuals acquire/become infected despite vaccination or known IgG immunity (previous infection).
It is recommended that vaccinated individuals wear RPE as detailed in the NIPCM appendix 11a, and within this guidance, to minimise any residual risk, and to promote consistency in practice across all staff groups.
2.6.1. Definition of occupational contacts
A health care worker (HCW) is considered to be ‘exposed’ and/or a contact if they have face-to-face contact of any length or spend more than 15 minutes in a small, confined area with a confirmed measles patient without wearing appropriate PPE (RPE) (see section 2.3.1).
If appropriate PPE (including RPE) is worn, the HCW is not considered exposed.
2.6.2. Exclusion of exposed HCWs from work
Health care workers who are exposed to a confirmed or suspected case of measles and do not have satisfactory evidence of protection (2 documented doses of measles containing vaccination or measles IgG positive) should be excluded from work from the 5th day after the first exposure to 21 days after the final exposure.
If health care workers are tested rapidly after exposure, they can continue to work if found to be measles IgG positive within 7 days of exposure (as this is too early to be due to infection from the recent exposure). Where MMR vaccine is given post-exposure, it is unlikely to prevent the development of measles but, if the HCW remains symptom-free for at least 14 days after MMR was given, they can return at that stage.
HCWs with satisfactory evidence of protection can continue to work normally but should be advised to report to occupational health if they develop prodromal symptoms or a fever between 7 days after the first exposure and 21 days after the last exposure. Exposed health care workers that develop fever or rash should be excluded from all work until 4 full days after onset of the rash.
Refer to the national measles guidelines for further information.
Appendix 1: Practical steps towards completing a local risk assessment for measles in healthcare settings
To support organisations, practices and employers to undertake a local risk assessment in the context of managing cases of suspected or diagnosed measles based on the measures as prioritised in the hierarchy of controls.
Download a word copy of this template: Practical steps towards completing a local risk assessment for measles in healthcare settings.
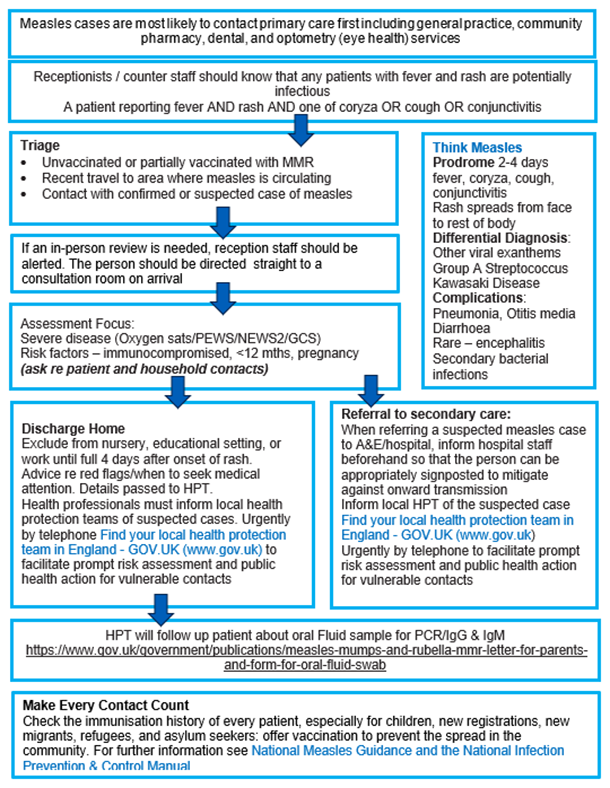
Appendix 2: Think Measles – primary care actions for screening, triage and management
Appendix 2 image text:
Face-to-face contact of any length or more than 15 minutes in a small, confined area is considered as exposure and will require follow-up.
Think Measles
Prodrome:- 2-4 days fever, coryza, cough, conjunctivitis.
- Rash spreads from face to rest of body.
- Other viral exanthems.
- Group A Streptococcus.
- Kawasaki Disease.
- Pneumonia, Otitis media Diarrhoea.
- Rare – encephalitis.
- Secondary bacterial infections.
A patient reporting fever and rash and one of coryza or cough or conjunctivitis.
Triage
- Unvaccinated or partially vaccinated with MMR.
- Recent travel to area where measles is circulating.
- Contact with confirmed or suspected case of measles.
Assessment focus
Severe disease (Oxygen sats/PEWS/NEWS2/GCS)Risk factors – immunocompromised, <12 mths, pregnancy (ask re patient and household contacts)
Discharge home
Exclude from nursery, educational setting, or work until full 4 days after onset of rash. Advice re red flags/when to seek medical attention.Details passed to HPT. Health professionals must inform local health protection teams of suspected cases.
Urgently by telephone find your local health protection team in England – GOV.UK (www.gov.uk) to facilitate prompt risk assessment and public health action for vulnerable contacts
Referral to secondary care
When referring a suspected measles case to A&E/hospital, inform hospital staff beforehand so that the person can be appropriately signposted to mitigate against onward transmission.Inform local HPT of the suspected case.
Find your local health protection team in England – GOV.UK (www.gov.uk) urgently by telephone to facilitate prompt risk assessment and public health action for vulnerable contacts.
Make every contact count
Check the immunisation history of every patient, especially for children, new registrations, new migrants, refugees, and asylum seekers: offer vaccination to prevent the spread in the community. For further information see National measles guidance and the National infection prevention and control manualAppendix 3: Think Measles – urgent and emergency care actions
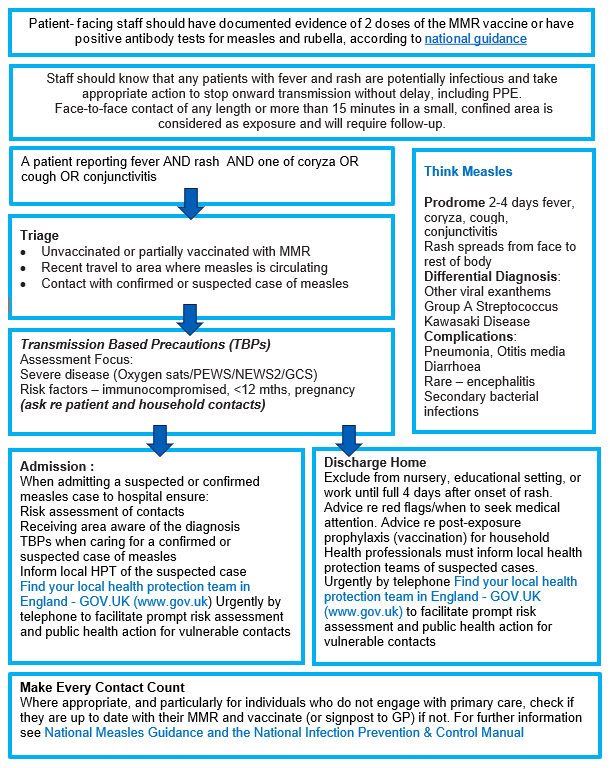
Appendix 3 image text:
Face-to-face contact of any length or more than 15 minutes in a small, confined area is considered as exposure and will require follow-up.
Think Measles
Prodrome:- 2-4 days fever, coryza, cough, conjunctivitis.
- Rash spreads from face to rest of body.
- Other viral exanthems.
- Group A Streptococcus.
- Kawasaki Disease.
- Pneumonia, Otitis media Diarrhoea.
- Rare – encephalitis.
- Secondary bacterial infections.
Triage
- Unvaccinated or partially vaccinated with MMR.
- Recent travel to area where measles is circulating.
- Contact with confirmed or suspected case of measles.
Transmission Based Precautions (TBPs)
Assessment focus:- Severe disease (Oxygen sats/PEWS/NEWS2/GCS).
- Risk factors – immunocompromised, <12 mths, pregnancy (ask re patient and household contacts).
Admission
When admitting a suspected or confirmed measles case to hospital ensure:- Risk assessment of contacts.
- Receiving area aware of the diagnosis.
- TBPs when caring for a confirmed or suspected case of measles.
- Inform local HPT of the suspected case.
- Find your local health protection team in England – GOV.UK (www.gov.uk) urgently by telephone to facilitate prompt risk assessment and public health action for vulnerable contacts.
Discharge home
Exclude from nursery, educational setting, or work until full 4 days after onset of rash. Advice re red flags/when to seek medical attention.Advice re post-exposure prophylaxis (vaccination) for household Health professionals must inform local health protection teams of suspected cases.
Urgently by telephone find your local health protection team in England – GOV.UK (www.gov.uk) to facilitate prompt risk assessment and public health action for vulnerable contacts.
Make every contact count
Where appropriate, and particularly for individuals who do not engage with primary care, check if they are up to date with their MMR and vaccinate (or signpost to GP) if not. For further information see National measles guidance and the National infection prevention and control manualPublication reference: PRN01102