Introduction
The development of virtual wards care for people with heart failure (HF) builds on the learning from virtual wards for acute respiratory infection and frailty, as healthcare systems start to expand virtual ward capacity.
They support personalised care for suitable adults with a confirmed diagnosis of HF by providing an alternative pathway to hospital admission and/or a safe early discharge pathway to receive treatment and monitoring in their usual place of residence.
The virtual ward model is underpinned by patient choice, clinical suitability and monitoring, access to timely specialist advice and guidance as required, and safe and appropriate clinical pathways and governance.
Healthcare systems that have yet to expand virtual ward capacity for people with HF should consider virtual wards on a whole integrated care board (ICB) footprint basis or in partnership with other ICBs to improve integration of specialist input for HF and other complex co-morbidities, patient care and hospital flow, and support earlier discharge where appropriate.
ICBs should work with cardiac clinical networks to understand their HF population needs, workforce skills and competencies, and existing service provision to deliver virtual ward care for their HF population and identify opportunities for system-wide efficiencies to improve the quality of patient care.
This guidance sets out the minimum requirement for the care of people with HF on a virtual ward. This requirement should supplement and integrate with existing condition specific pathways, including alternative pathways to admission.
It supports implementation led by ICBs and delivery by appropriate providers as they begin to explore and test virtual ward care as an additional or complementary service model for people with HF care needs.
This guidance should be read in conjunction with NHS England’s Supporting information for virtual wards including Hospital at Home and relevant NICE clinical guidelines, including CG187 (2014) Acute heart failure: diagnosis and management and NG106 (2018) Chronic heart failure in adults: diagnosis and management.
It has been tested with people living with HF, national representative bodies, those delivering frontline HF care, and those working at a system and national level, and their feedback taken on board.
For the definition of the terms used in this guidance, please see Appendix C.
Drivers for change
Reducing the high rates of hospital admissions and readmissions for people with HF relies on many enablers:
- early diagnosis
- optimal treatment and secondary prevention
- co-morbidity management
- cardiac rehabilitation
- personalisation and patient enablement
- early identification of frailty and those who are in the last year of life
- advance care planning.
Many people with decompensated HF will require care in a hospital setting as only that setting can meet or co-ordinate their clinical needs.
However, others, based on their clinical suitability, choice and informed consent, could have safe, effective and co-ordinated care – that is, equivalent treatment, monitoring and specialist clinical input – delivered in a hospital ambulatory setting, in the community or at home through a virtual ward.
Virtual ward care can improve a person’s quality of life at home, with care provided when they need it without having to leave their home. They can remain active at home and maintain independence, with support from their families and carers.
It reduces the risks of concomitant infection and deconditioning during hospital admission, allows earlier hospital discharge and avoids readmission, while maintaining access to timely and responsive HF specialist care and guidance.
Admission to a virtual ward is underpinned by ensuring a person is on the most appropriate pathway and virtual ward based on their needs, not reducing hospital bed occupancy. This includes:
- People on virtual wards may have multiple co-morbidities, including severe frailty, that require input from a number of specialist teams including HF specialists.
- The overall responsibility for the person should lie with the specialist team providing virtual ward care for the primary cause for admission and they should be managed by that team.
- However, input from other specialist teams should be sought as required. See Guidance on introducing or expanding Hospital at Home virtual wards for people living with frailty.
- People with HF who require advanced HF therapies or advance care planning should be assessed and referred in a timely manner, supported by face-to-face discussions with their carers and HF multidisciplinary team (MDT).
What is virtual ward care for heart failure?
Heart failure virtual ward care is a safe alternative (under the care of a HF specialist team) to inpatient hospital care for people with deteriorating signs and symptoms who could, and wish to, be cared for in their usual place of residence.
This includes supporting early discharge from hospital, typically supported by remote monitoring.
A virtual ward enabled by technology makes it possible (as a minimum) for people to measure and input, agreed health data, eg vital signs, into an app or website (this may also be done automatically, eg with wearable/Bluetooth technology).
This data feeds into a digital platform/dashboard that is reviewed remotely by a clinical team. The clinical team are alerted when a person’s data transgresses agreed parameters so they can take appropriate and timely action. More information is available on setting up technology-enabled virtual wards.
Virtual ward care should complement, and be integrated with (not replace), existing acute and community HF services and HF specialist care. The care for people with HF delivered by primary care, community services and secondary care providers continues to be essential in any integrated care system (ICS).
In some parts of the country, ‘step up’ and ‘step down’ services exist between community and secondary care providers. These could meet the criteria for a virtual ward even if they have not been known as such.
However, systems would need to review where it may be necessary to expand local HF specialist resources to support the higher and daily specialist HF input, as well as monitoring, that people on a virtual ward need.
Overview of the heart failure virtual ward
What and who
Enhanced care, monitoring (usually remote) and support under the care of a HF specialist team.
A safe alternative to inpatient hospital care for suitable adults with a confirmed HF diagnosis and deteriorating signs and symptoms of HF who could, and wish to, be cared for in their usual place of residence, and who would otherwise require admission to hospital.
This includes supporting early discharge with an extended period of patient monitoring.
Where
In the person’s home or usual place of residence with access to face-to-face care as and when required, eg attendance at ambulatory HF units or community HF units.
When
To avoid hospital admission or to support early discharge to reduce length of stay in a secondary care bed.
Why
- Improved choice and quality of life: if they wish, the person can remain under the care of HF specialists but receive care in their usual place of residence.
- Improved experience and outcomes for the person and their carers.
- Timely access to expert professionals for the person and their carers.
- Shared decision-making with the person and their carers.
- Improved hospital flow and earlier discharge.
- Reduced hospital length of stay and avoidance of non-elective readmission.
- Promotion of supported self-management.
- Improved integration across care settings within ICBs.
- Updated patient HF management plans and appropriate long-term follow-up.
How
- Recognition of the person who due to a clinical deterioration of their HF (including evidence of decompensation) would otherwise require admission to hospital.
- Joint decision-making to determine the most appropriate care plan for the person.
- Proactive daily monitoring by a HF team for a short duration (up to 14 days).
- This can be in-person and/or remotely using a technology-enabled digital platform that alerts the HF MDT when a person is showing signs and symptoms of deterioration.
Criteria for virtual ward care for people with heart failure
HF specialists (with input from the HF MDT) should develop local admission criteria that reflect the need of the local population. Importantly these should include where the person prefers to receive care.
ICS urgent and emergency care boards should review the admission criteria and whether the virtual ward is supporting the health needs of its population at a place or primary care network level.
Inclusion criteria
Virtual ward care for HF is for people with HF who:
- are ≥18 years, need acute level care and can be safely and effectively managed in the community, often with the support of digital technology
- have a confirmed HF diagnosis and who, due to clinical deterioration of their HF:
- would require admission to hospital
or - could be considered for early supported discharge following an admission to hospital and would otherwise remain in a secondary care bed.
- would require admission to hospital
- are discussed with/reviewed by a HF specialist at the time of onboarding
- are referred by the HF MDT who consider virtual ward care is the best pathway to meet their ongoing clinical needs
- can benefit from daily remote monitoring and regular clinical reassessment, and are suitable for remote treatment by a HF specialist team, including home visits where required
- have made an informed decision and consented to be on a virtual ward based on their needs and preferences, and carer support where appropriate
- are expected to be in the service in the short term (usually managed within 14 days).
Exclusion criteria
- Clinical presentations, co-morbidities or psychosocial problems that can only be investigated or treated, or the care of which co-ordinated, with hospital admission.
- Each of these exclusion criteria should be defined with HF specialists and be robustly considered by each ICB co-ordinating a virtual ward programme.
- Acute pulmonary oedema should not be an indication for HF virtual ward care unless this is to support a person as part of an end of life care at home pathway.
- Where it is not safe for a person to remain in their home or usual place of residence.
Minimum requirements for managing people with heart failure on a virtual ward
The following requirements should be included in any local design and standard operating model. Existing guidance should be read to support their implementation:
- supporting guidance on maximising the rollout of virtual wards
- supporting information on the enablers of success
- supporting clinical leadership in virtual wards
- guidance on pharmacy services and medicines use within virtual wards
- addressing palliative and end of life care needs for people living with heart failure: a revised framework for integrated care systems.
Access to HF specialist care and advice
- Those people the local HF specialist team does not already know should be made known to this team and be under the care of a senior clinician with clear lines of responsibility for their care and communication to a named HF specialist.
- Virtual wards should have the appropriate workforce, skill mix and MDT for delivery and teams have the training and tools required to deliver care.
- Patient care has MDT input, and this team has representation from generalist and specialist HF practitioners across primary, community, secondary, social care and voluntary sector services, with expertise in specialist HF prescribing, medical, nursing, the allied health professions and palliative care as a minimum.
- Consideration to be given for health and care support staff and other skill sets to support onboarding, eg telehealth co-ordinators.
- Virtual ward staff and people with HF should have access to rapid specialist advice and guidance (eg telephone, digital, video), where necessary.
- This supports clinical decision-making in real time, equitable access and equivalent inpatient priority to hospital-based investigations and treatments, and clear pathways for referrals to other specialties across virtual wards for other conditions.
Staffing and clinical oversight
- A senior clinical decision-maker should decide whether the person is admitted to a virtual ward.
- Their decision should be based on the same level of clinical assessment and decision-making as if the person were being admitted to a hospital bed, and can be made in consultation with other specialty clinicians.
- Clearly defined criteria and clinical decision-making for triaging, admission, discharge and follow-up.
- These should include personalised and shared decision-making and proactive care based on the person’s choice and needs.
- Daily virtual review with the HF team/MDT with safe and robust staffing and processes for specialist input and care, including for escalating concerns and unexpected deterioration (based on an individual’s criteria) to cardiology during virtual ward hours (eg 8am–8pm), 7 days a week.
- Robust and locally agreed plans for provision of specialist advice, including out of hours cover (usually from a member of the on-call cardiology or general medicine team, dependent on local arrangements), to maintain patient safety.
- Those facilitating out of hours care should be notified when a person is on a virtual ward and what their care plan is.
- A locally agreed approach for alignment or integration with other local services to support seamless patient care across the ICB; for example:
- access to multimorbid specialist input
- single point of access
- ambulatory care
- same day emergency care
- rapid response teams
- initiation and escalation to intravenous diuretic therapy
- specialist palliative care advice
- urgent community response
- unscheduled care across systems.
- Virtual ward plans for HF should be communicated across the local system.
- Clearly defined, safe and robust planning process (including optimisation and follow-up) for discharge to locally arranged service provision.
- When developing services, transitions of care between virtual ward services and end of life services should be a high priority.
- Care planning with clear pathways between services needs to be agreed to ensure high quality end of life care delivery in line with Addressing palliative and end of life care needs for people living with heart failure: a revised framework for integrated care systems.
Onboarding and admission
- Through shared decision-making, people with HF are informed of the benefits and risks of virtual ward care versus hospitalisation, and what being on a virtual ward means for them and their carers (based on their needs and preferences).
- People need to provide informed consent before being onboarded to a virtual ward.
- Onboarding and virtual ward admission should be supported by the HF specialists who determine the management plan.
- A hybrid approach to care – virtual and appropriate face-to-face reviews and physical examinations when required – can be taken where technology allows this (along with support for the person to use equipment and who they should contact should the technology develop faults).
- Local systems should ensure information and communication about virtual ward admission is visible to relevant services (eg at onboarding, in virtual ward round entries and in the discharge letter).
- This could also be achieved with, for example, entries in shared care records.
- Robust systems to be put in place for remote prescribing.
- This includes specifying the arrangements and responsibilities for prescribing, supplying, collecting, administering and monitoring for response.
- Consideration should be given to necessary arrangements where the person is unable to collect medication.
- Need for timely access to blood testing (with point of care blood tests considered if available).
Appendix A: Key elements in the pathway
The patient journey can be split into three stages:
Stage 1: Identifying people with heart failure
People with a confirmed diagnosis of HF may be identified as potentially suitable for virtual ward care in the following circumstances:
- During emergency department or acute medical ward assessment as part of admission avoidance.
- On or following discharge home from hospital as part of early supported discharge.
- Those at home who have deteriorating signs and symptoms of HF and who in usual circumstances would require hospital admission.
- When discussed at an MDT meeting or through more informal information sharing across organisations/teams.
- Those with severe frailty or in the last year of life who express a wish to be managed in their home environment.
Stage 2: Clinical assessment and suitability for a virtual ward
- Clinical holistic assessment and investigations (as outlined in NICE quality standards and guidelines for HF) should be carried out before admission to a virtual ward, both where a person has already been admitted to hospital or is in their usual place of residence, if appropriate against the local eligibility criteria.
- This should include consideration of medicine optimisation if the person is more suitable for other treatment and appropriate care planning for frailty and/or palliative care.
- Assessment should include a person’s wishes, their safety, their family or carers’ ability to provide support, and any mental capacity, consent and safeguarding concerns.
Stage 3: Onboarding to a virtual ward
HF specialists should discuss with the person whether a virtual ward admission is suitable for them. If it is, onboarding should ideally be done at a face-to-face appointment with support from HF specialists. This should include:
- Information on the risks and benefits of HF virtual ward care.
- Information on agreed goals, covering their condition, lifestyle and what signs of deterioration to look for.
- Assessment and provision of equipment to keep the person safe at home and support/maintain their independence.
- The person should be advised who to contact if the equipment fails or they need additional support.
- Alternative options may need to be considered for those who find it difficult to use the equipment and should be discussed as part of personalised care planning.
- Initiate discussion to review existing personalised care plans, treatment escalation plans, and emergency care and treatment plans if the person is willing and able to do so at this time.
- This should include a holistic review and management plan for those with multi-morbidities.
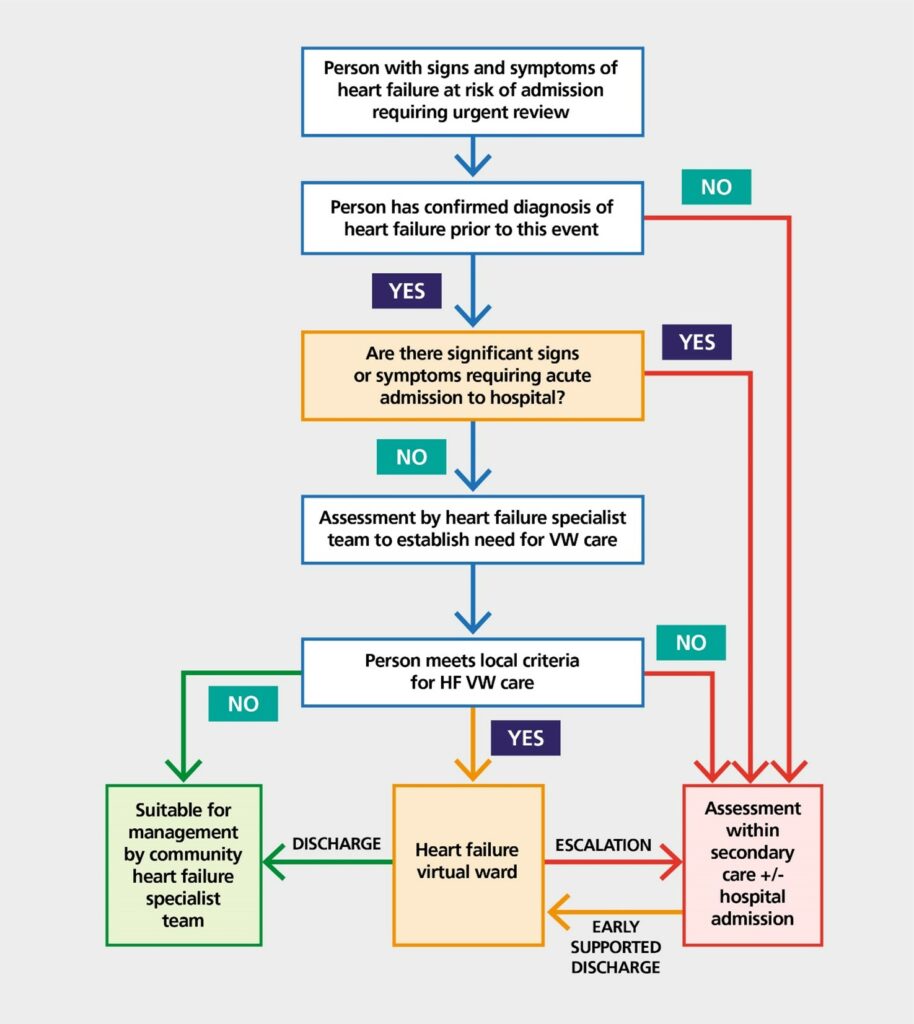
Figure 1 shows how heart failure virtual ward care fits with the wider health system.
Figure 1: Heart failure virtual ward care pathway
Stage 4: Assessments, monitoring and management
- Daily review of every person on the virtual ward and communication between the virtual ward team and the person’s specialist HF team.
- Ensure that the person and their carers are kept informed and that their information, practical and emotional needs are supported.
- Check that the virtual ward staff involved in the person’s care can recognise early signs of deterioration and fully understand the appropriate escalation processes to maintain patient safety.
- Monitor essential clinical parameters daily, based on individual and clinical needs, eg daily symptom questionnaire.
- Assessments and measures for remote and self-monitoring will be determined by local standard operating models according to an individual’s treatment plan (part of the personalised approach and shared decision-making).
- Both frequency and type of any remote monitoring or clinical tests should be agreed with the person and clearly documented in their management plan.
Stage 5: Discharge and transferring care
The need for a timely discharge should never result in an unsafe discharge – that is, without adequate support or the person not being fully informed as to the next stages of their care.
- Follow-up with a HF specialist within 2 weeks of discharge as per NICE Quality standard [QS103]: Acute heart failure.
- Robust discharge process to appropriate primary, community or secondary care providers including onward referral (eg Managing Heart Failure @home, cardiac rehabilitation) within the individual’s treatment and management plan.
- When developing services, transitions of care between virtual ward services and end of life services should be a high priority. Care planning with clear pathways between services needs to be agreed to ensure high quality end of life care delivery.
- The discharge criteria from acute level virtual wards are expected to be in line with the Hospital discharge and community support: policy and operating model, which sets out the hospital discharge model for all providers of NHS-commissioned hospital and community beds, community health services and social care in England.
Appendix B: Key considerations for heart failure services and integrated care boards
Existing guidance should be read to support implementation:
- supporting guidance on maximising the rollout of virtual wards
- supporting information on the enablers of success
- guide to setting up technology-enabled virtual wards – Key tools and information – NHS England Transformation directorate.
In planning the development of a virtual ward, the following should be considered:
- Quality improvement and sustainability
- ICBs with cardiac clinical networks to consider the funding and workforce requirements for sustaining the service if safety and effectiveness can be demonstrated, and how learning can be incorporated as the service develops.
- This includes ensuring appropriate implementation, delivery, oversight, harms reviews and complaints handling, and taking opportunities for continuous quality improvement and expansion of the virtual ward and equity of access.
- Governance.
- Responsibility, including for ensuring appropriate clinical governance, remains with the relevant provider.
- Each system should have a named person responsible for the establishment of the service in their area.
- Personalised care and holistic approaches to care, as well as considering inequalities and barriers to access.
- These approaches draw on the components of the Comprehensive model for personalised care, including:
- shared decision-making
- personalised care and support planning
- advance care planning
- supported self-management through educating the person about their condition.
- Ensuring integration and communication between different parts of the system to improve continuity of care and patient experience, across the whole patient pathway. Including: correct coding of HF, interoperability of organisational electronic systems, up-to-date management plans and treatment escalation plans.
- Completed equality and health impact assessments when developing local standard operating models for virtual ward care for people with HF.
- Identify and assess people with HF and frailty and those in the last year of life as early as possible, to guide care planning.
- Consider pre-discharge assessment of the suitability of a person’s home or usual place of residence following transfer of care.
- These approaches draw on the components of the Comprehensive model for personalised care, including:
Clinical judgement is vital, particularly for people at higher risk of serious illness, with multi-morbidity, with a learning disability or living with serious mental illness.
Suitable arrangements must be made to support communication, eg the use of interpreters, hearing aids and advocates, especially in shared decision-making.
- Digital systems, platforms and data
- Consider what technology-enabled remote monitoring platforms are being used across the ICB and how they can be organised to best support patient care within and across virtual wards with different specialty input (eg dashboards to support daily review).
- Collaborative working across all providers to make navigation easier for the person and their experience better.
- Arrangements and responsibilities specified for access to equipment, assessment, supply, collection and demonstration of use for remote monitoring.
- Systems may want to consider how these digital systems can:
- Collect routine data that demonstrates patient safety and effectiveness, and provides early indication of any unintended consequence.
- Integrate with existing digital systems across the ICB to notify other providers, where possible and necessary, when a person is on a virtual ward.
- Access route, service hours and routes of escalation.
- Whether this is through a single point of access and what arrangements are in place to ensure monitoring and access to specialist HF input during virtual ward hours and cardiology during out of hours.
- These will depend on how virtual ward care integrates with and/or becomes an extension of existing services, including hospital admission and presentation at the emergency department.
Appendix C: Definition of terms
The terms used in this guidance are defined as follows, unless the context clearly states otherwise:
Heart failure (HF) specialists
HF specialist nurses, advanced nurse practitioners, advanced clinical practitioners, consultant cardiologists, cardiology registrars, GPs with a specialist interest in HF, HF specialist pharmacists.
Supported self-management
The ways that services encourage, support and empower people to manage their health conditions themselves.
More information on supported self-management and personalised care is available.
Patient initiated follow-up (PIFU)
Patients with long or short-term conditions, including heart failure, initiate an appointment when they need one, based on their symptoms and individual circumstances.
PIFU also goes by other names (eg patient-led follow-up, supported self-managed follow-up, patient-activated care).
Read more on setting up PIFU services for HF.
Managing heart failure @home
Supports self-management by helping people with HF and those with complex co-morbidities (including frailty) to identify early signs of deterioration.
May include using digital and technology-enabled remote monitoring and/or telehealth, supported by paper resources.
Managing heart failure @home should not be considered for those who are acutely unwell and treated in hospital or a virtual ward setting.
It should though be considered for people with HF following discharge from hospital or virtual ward care, to avoid HF-associated readmissions where possible.
Services between and across acute and community HF services may already exist that could fit the criteria for managing heart failure @ home, even if they have not been known as such.
Further information on Managing heart failure @home.
Publication reference: PRN00299

