NHS England has defined interoperability as follows:
‘Interoperability, in the context of health and social care, is the capability for people involved in the provision and receipt of care to interact and complete a task across software and organisational boundaries; and use equipment, systems, or products from different vendors, which operate together in a coordinated fashion, with minimal to no human intervention.’
With new models of care emerging and evolving, there is a clear need for more effective information sharing between care settings, organisations and geographies, as well as between professionals and citizens, to optimise patient outcomes and quality of care. This is reliant on the ability of IT systems across health and care to be interoperable with one another and is key to the delivery of the future vision of care in England.
More integrated ways of working across health and care are necessary to enabling care professionals and citizens to better manage care. Lack of access to an up-to-date medical history can affect the way patients are treated. The impact on treatment, particularly in an emergency situation, can be significant.
The NHS in England is not one single organisation. It is made up of hundreds of different organisations, of differing sizes, at central, national, regional, and local levels, with separate roles and responsibilities. Staff working in these organisations are likely to be entering information in different ways on systems that are have different information models supporting different structures and different coding systems (i.e. they are ‘heterogeneous’).
Interoperability in general practice
Within general practice interoperability already exists between many of the local, national and patient-facing systems in use. All new systems in general practice must be interoperable as this is a core and mandated requirement of the Securing Excellence in Primary Care (GP) Digital Services: The Primary Care (GP) Digital Services Operating Model 2021-2023.
Consistency and Standards
Consistency and standards are key to the success of interoperability, particularly but not exclusively, in the following areas:
- developing and expanding the services provided through
- pathology results, a consistent set of interoperability standards for the sharing of a core set of pathology results
- clinical coding
- standards to support the move from paper to electronic transfers of care
- building on the successes identified by the local health and care record (LHCRE) exemplars
- the national shared care record (ShCR)
- movement of staff across organisations and operational boundaries
- ensuring that there is a consistent way to find and authenticate staff securely across multiple services
- development of standards, including for the following:
- NHS booking and referral standard
- digital social care records
- nursing documentation standard (expected 2023)
- clinical content standards from the Professional Records Standards Body (PRSB)
Standards roadmap tracking
You can follow future standards to see more information about the above, and the full range of standards currently in development including the timescales in which they are expected to be launched.
Role of IT service desks
There are many NHS IT service desks in operation, usually aligned with geographical areas. Each general practice will access support through its own service desk, commissioned by its ICB.
Service desks can be vital to the success of interoperability initiatives. They:
- provide remote technical support to practices for system or PC problems are usually the provider and maintenance option for all practice computer equipment
- provide wider support with data collection, management of data, and training solutions for new systems and staff
- may also procure new digital solutions for geographical areas, project managing the deployment, overseeing all the back-end infrastructure, and providing the necessary training for users
- manage staff access security requirements such as smartcards and NHS CIS2
How does interoperability work?
Different systems and products need to be able to access, exchange, and make use of information promptly. General practices in England do not use a single clinical system and are not expected to do so anytime in the future. The transformation of health and social care depends on the need for information in one system to be made available to authorised users within a different system, ensuring that clinical documentation integrity is preserved.
Information sharing through Application Programming Interfaces (APIs)
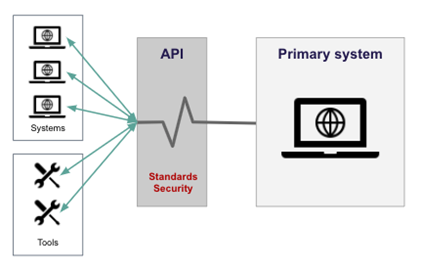
Information sharing between different systems can be enabled through a centralised point such as an application programming interface (API) mechanism. This enables two software components to communicate with each other using a set of definitions and protocols. These definitions and protocols are underpinned by the standards.
An example of an application that can be accessed securely by different organisations, is the Personal Demographics Service (PDS). The diagram below, gives a simple view of where APIs fit.
The NHS has been developing APIs for some time now, adopting, where possible, the latest technologies for any new APIs. It is, however, costly to rebuild APIs when technology changes, so the NHS uses a variety of technologies in their APIs. The health and social care system uses centrally run API services (for example Spine, Patient Demographic Service (PDS), Summary Care Record (SCR)).
Note | it is the standard that the API conforms to that is important, not the API itself.
You can learn about the different types of API here.
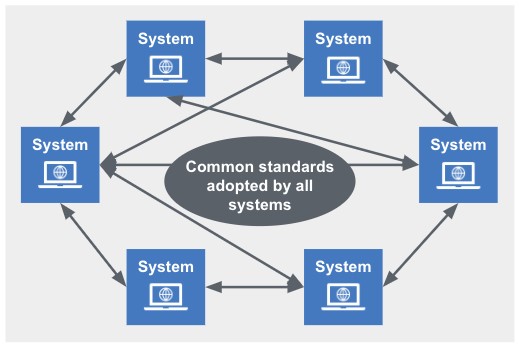
Peer-to-peer interface
A third-party system using a set of common standards allows various providers to communicate directly with one another. The diagram below, from a standards and interoperability end-to-end model, gives a simple view of the peer-to-peer approach.
Standards
The NHS uses ‘Fast healthcare interoperability resources’ (FHIR) to make integration with APIs and services easier.
NHS England has an API catalogue which details the APIs currently available or in development. The catalogue includes API services as well as API standards as defined by them.
FHIR is the global industry standard for passing healthcare data between systems. It is free, open, and is designed to be quick to learn and implement. FHIRs are part of an international family of standards developed by Health Level Seven (HL7).
Some APIs give access to sensitive or personal data. The NHS uses various techniques or ‘patterns’ to keep them secure.
Some APIs are available on the internet but not directly on the Health and Social Care Network (HSCN). All HSCN connections, however, can include internet access. Some will need the end user to be an authenticated healthcare worker. The most common ways of doing this are with an NHS smartcard or by using an NHS CIS2 service.
Information standards underpin national healthcare initiatives and provide the mechanism for introducing requirements to which the NHS, those from whom it commissions services, and its IT system suppliers, must conform. NHS England provides an Interoperability Toolkit (ITK) which is a set of national standards, frameworks and implementation guides aimed at those who develop and deploy ITK based solutions.
Compliance with the two following standards is mandatory under the Health and Social Care Act 2012:
- DCB0129 Clinical risk management: its application in the manufacture of health IT systems which sets clinical risk management requirements for manufacturers of health IT systems
- DCB0160 Clinical risk management: its application in the deployment and use of health IT systems which requires a health organisation to set up a framework within which the clinical risks associated with the deployment and implementation of a new or modified health IT system are effectively managed
The NHS has launched a Data Standards Directory, which can be used to find the nationally recognised standards for use in health and adult social care.
Benefits of interoperable systems
General benefits
Having a holistic view of patient information can provide insight to make crucial, sometimes lifesaving, clinical decisions and allow for treatment adjustment earlier in the process. The key benefits of delivering an interoperable health and care system are huge:
- improved patient safety through better and more informed decision making with access to current information, reducing the potential for errors due to limited information
- more integrated care, enabling clinicians in different settings to have current information available at the right time and place to offer patients better, joined-up care
- an innovative health sector which promotes health and tech information such as the NHS App
- patient interaction with access to some of their own information, via apps, such as the NHS App, Airmid, etc., and personalised services for booking purposes, through internet-based systems such as the electronic referral service
- patient interaction and involvement with long-term condition management through wearable devices and apps
- population health data which can be used to drive policy priorities and research
- reduction in unnecessary or duplicated tests, because clinicians will be able to see test results ordered by another care provider
- reduction in diagnosis delays
- quicker access to the right treatments
- smoother transition of care supporting easier patient movement between care settings, allowing the NHS to continue the development of specialised services in one location in a geographical area, such as specialist cancer service
Benefits for general practice
The key benefits for general practice are:
- better and more informed decision making at the point of care
- better and safer transfers of care
- relevant and consistent patient clinical information available across care boundaries and systems improving patient care and patient experience
- current up-to-date patient information available to all users involved in the patient’s care
To realise these benefits, practices need to:
- engage in data sharing where an appropriate legal basis can be identified
- ensure they follow record keeping guidance to keep accurate records which are essential to the provision of safe and effective care
- ensure staff use SNOMED-CT
- ensure staff are consistent, using the same up-to-date templates, as this will help with the achievement of the Quality and outcomes framework (QOF) and other incentives
- ensure the practice follows the NHS Records management code of practice
Risks
The principal risks are:
- managing inconsistent information across multiple sources – systems often store different pieces of data in multiple, often disparate places, such as data silos
- organisational resistance to sharing data, including unwillingness to use tools – this could be due to lack of resources and/or expertise, or poor-quality interoperability tools
- electronic requests for patient information must be validated, secure user authentication must be via NHS smartcard or NHS CIS2
- greater risk of harm to vulnerable patients with access to their own health record, including the potential for abuse, or the release of confidential information through coercion
- cybersecurity risks – patient confidentiality must be always protected – all apps linking to healthcare must meet encryption standards and have appropriate end-user verification processes
Risks relating to standards
Risks specifically relating to standards include:
- making data available between two different organisations requires coordination to make sure all suppliers of the relevant systems used in the sending and receiving organisations adopt a single, common solution for sending and receiving the information
- standards that are not supported or managed after their creation and standards that are not integrated and aligned with a broader technology strategy
- there is no effective and consistent mechanism for managing and tracking supplier and provider change activity to adopt standards
- realistic funding requirements need to be addressed by accommodating a switch from capital funding to revenue funding, with clarity about how different funding initiatives align to the different digital priorities
Related GPG content
- Clinical coding – SNOMED CT
- Shared care records
- Smartcards and access control (RBAC)
- NHS Care Identity Service 2 (CIS2)
- Personal demographic service (PDS)
- Summary care records (SCR)
- NHS App
- Coercion
- Cyber security
- Population health management
- Clinical messaging and test results
- eReferrals
- High quality patient records
Other helpful resources
- InterOpen, Introduction the Care Connect API
- NHS England, The NHS Patient Safety Strategy
- The Kings Fund, Sharing health and care data
- The Kings Fund, Interoperability and the NHS: are they incompatible?
- The Kings Fund, Understanding factors that enabled digital service change in general practice during the Covid-19 pandemic 2021
- HIMSS (non-profit international healthcare think tank), Interoperability in Healthcare