Epilepsy is one of the most common long-term conditions for children and young people (CYP), affecting approximately 112,000 children and young people within the UK.
Epilepsy can have a significant impact on the quality of life of CYP including on social, educational and future employment activity.
Epilepsy is one of the five key clinical areas within the CYP Core20PLUS5 framework.
Children and young people in the most deprived areas of England are more likely to have epilepsy than those in less deprived areas.
People with epilepsy have a higher prevalence of neuro developmental disorders (e.g. learning disabilities and autism spectrum disorder) than in the general population.
Key epilepsy metrics to identify and track areas for local improvement are included within the National Children and Young People Transformation Programme Dashboard.
This Bundle of Care covers each of the below four areas of focus:
- Variation in care: variation in the delivery of key aspects of epilepsy care continue to persist, such as access to epilepsy specialist nurses and the provision of information on Sudden Unexpected Death in Epilepsy (SUDEP).
- Mental health and wellbeing: CYP with epilepsy have a higher incidence of mental health conditions than the general population, yet screening and support within services vary.
- Tertiary care and epilepsy surgery: CYP may be missing out on, or having delayed access to, specialist neurological care and epilepsy surgery.
- Transition from paediatric to adult services: Support and pathways for patients to transition to adult services varies considerably.
This bundle contains standards of care for each of the four areas of focus, with key recommendations for systems to consider.
Executive summary
NHS England’s Children and Young People’s (CYP) Transformation Programme has established a programme of work to improve care and outcomes for CYP with epilepsy. In response to supporting systems with epilepsy quality improvement, the programme has developed key standards around the care and delivery of epilepsy services. Recommendations for integrated care boards (ICBs) to support implementing key standards have also been developed.
This Bundle of Care covers each of the four areas of focus within the CYP epilepsy programme:
- addressing variation in care between epilepsy services,
- supporting the mental health and wellbeing of CYP with epilepsy,
- improving referrals into tertiary services and the Children’s Epilepsy Surgery Service (CESS), and
- improving the transition from paediatric to adult epilepsy services.
NHS England has worked with key stakeholder organisations, as well as young people and their families, to develop this National bundle of care for CYP with epilepsy. National working groups were formed on each area of focus to inform the standards and recommendations set out within this document. In addition, supporting resources have been identified or developed by the working groups to aid implementation of the standards and recommendations made.
NHS England has used data from the national Epilepsy12 audit to inform the development of these standards and recommendations. The Epilepsy12 audit provides organisational and clinical data on care provided to CYP with epilepsy. A data-led approach has been taken to identify key areas of focus, and these recommendations build on areas of development highlighted in the audit.
The standards within each of the four areas of focus can be found in Annex 1, alongside the rationale for each of the areas of focus. These standards are aligned to guidance from NICE. Recommendations on specific standards have been developed to support systems in commissioning consistent quality epilepsy care for CYP. Implementation of these recommendations are expected to reduce overall care-costs through reducing unplanned hospital admissions, ensuring timely referrals into tertiary care, and supporting earlier identification of co-morbidities.
ICBs are encouraged to develop improvement plans in line with recommendations made within this bundle. The majority of recommendations consist of undertaking a local mapping of epilepsy services against the key standards. The National CYP Transformation Programme dashboard contains epilepsy metrics to support systems in undertaking this. In addition, supporting resources have been provided within appendices to aid local delivery of this bundle.
Background
Epilepsy is one of the most common long-term conditions among children and young people, affecting approximately 112,000 CYP within the United Kingdom. It can have a significant impact on the quality of life of CYP including on social, educational and employment activity. Epilepsy is characterised by recurrent seizures, however most individuals with active epilepsy can maintain satisfactory control of seizures through appropriate use of antiepileptic drugs. Where pharmacological management is not effective, a select group of CYP may benefit from epilepsy surgery.
Optimal management of epilepsy improves health outcomes and can reduce emergency admissions. In addition, it can also help to support mental health and wellbeing and minimise other impacts on social, educational and employment activity. For example, there is evidence of poorer education achievement in children with active epilepsy, and people with epilepsy may face a number of complex and interacting problems in finding and maintaining employment later in life.
The National Institute for Health and Care Excellence (NICE) has published guidelines on the diagnosis and management of epilepsy (NG217). There is also a quality standard for epilepsy in children and young people (QS27) which is due to be updated in December 2023. The standards developed within this document are aligned to NICE guidelines.
NHS England’s ambition is to improve the quality of care for all CYP with epilepsy. This includes working with systems to ensure they take a whole system approach to the diagnosis, management, and treatment of epilepsy. This will include mapping pathways of care, supporting the delivery of developmentally appropriate care, and sharing examples of good practice. NHS England has developed this bundle in response to requests from systems to enable greater focus on the delivery of epilepsy services.
NHS England, supported by Young Epilepsy, has worked with a range of stakeholders to develop the standards and key recommendations within this bundle. These stakeholders include NHS England national and regional programmes, paediatric and adult epilepsy clinicians, voluntary sector organisations, and CYP with epilepsy. This bundle has been approved by NHS England’s National Children and Young People Epilepsy Oversight Group and developed through national working groups.
To date, NHS England’s CYP Transformation Programme has:
- Funded the appointment of dedicated regional clinical leadership for CYP epilepsy. These posts are expected to support the delivery of key recommendations within this Bundle of Care.
- Established a National CYP Epilepsy Oversight Group, which is co-chaired by NHS England and Young Epilepsy. The Oversight Group supports the development of national policy and strategy to improve the quality of care for CYP with epilepsy, as well as mobilise key stakeholder organisations.
- Included epilepsy as one of the five key clinical areas within the CYP Core20PLUS5 framework, the national NHS England approach to support the reduction of health inequalities.
- Supported the Epilepsy12 audit programme to ensure a data-led approach towards improvement, including the reporting of data at Integrated Care Board level.
- Supported the Epilepsy Quality Improvement Programme (EQIP). This is a structured programme run by the Royal College of Paediatric and Child Health (RCPCH) to build improvement capability within selected Trusts. NHS England will share future learning and case studies to support wider scaling of specific improvement interventions from the EQIP programme. These will be in line with the recommendations and standards within this document.
- Funded a number of Epilepsy Specialist Nurses with a specific focus on integration and continuity of care for patients across organisational boundaries. These posts are due to commence in 2023/24. Learning from these roles are expected to help inform future models of care.
- Funded pilots on integrating mental health care within epilepsy services, to commence in 2023/24. These pilots aim to build an evidence base on how mental health and wellbeing support can be effectively integrated within secondary care epilepsy outpatient services.
Supporting resources have been identified or developed by the working groups to aid the implementation of the standards and recommendations made within this document. These are contained within the relevant appendices.
To support identifying local areas for improvement, and the tracking of progress made against the recommendations within this bundle, key Epilepsy12 audit metrics are included within the National CYP Transformation Programme Dashboard. This is available on the NHS England application platform.
Health inequalities
CYP living in the most deprived areas of England are more likely to have epilepsy than those in less deprived areas.
Epilepsy is one of the five key clinical areas within the Children and Young People Core20PLUS5 Core20PLUS5 is the national NHS England approach to support the reduction of health inequalities at both national and system level.
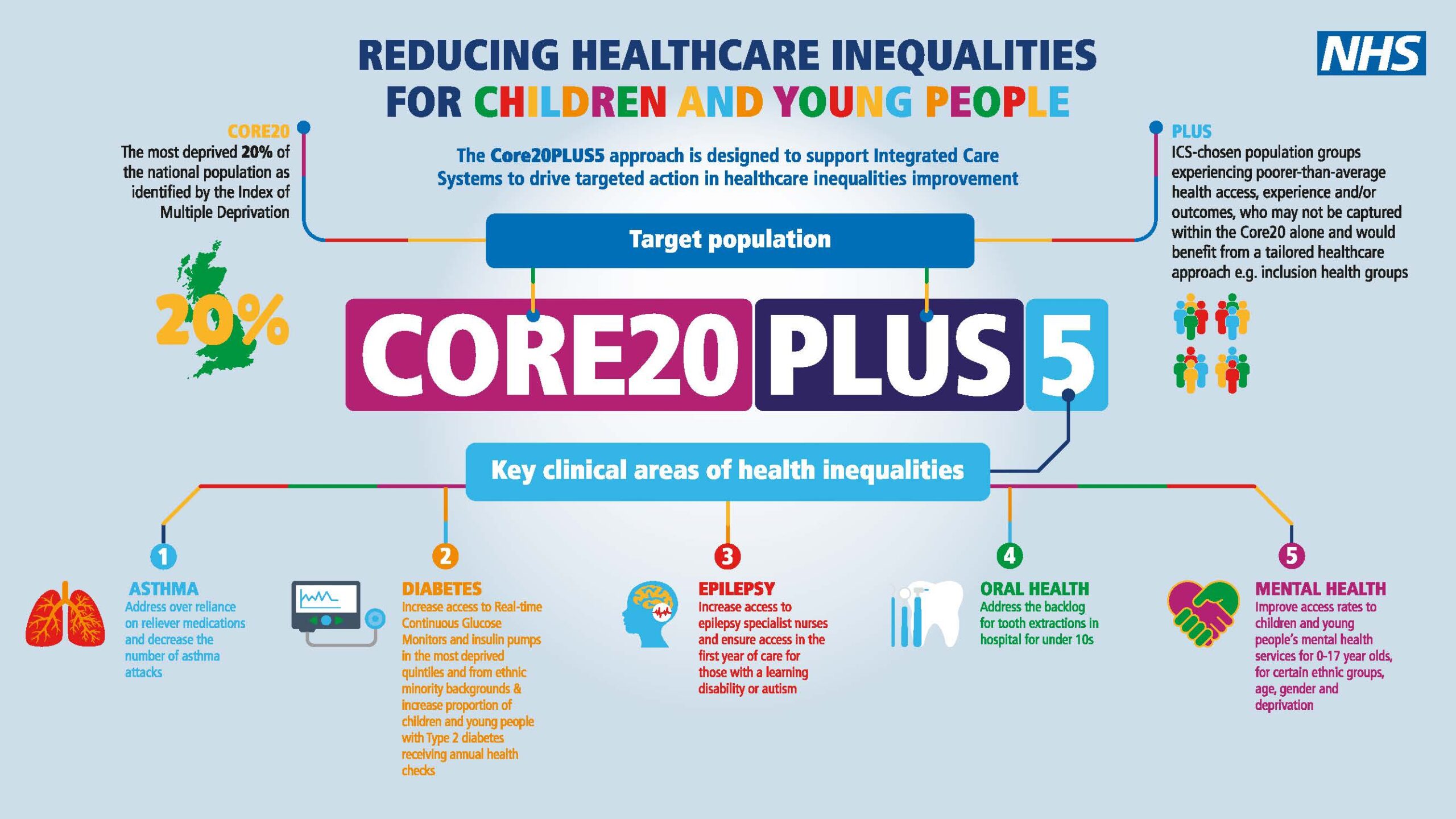
See here for an accessible version of the above CORE20PLUS5 CYP infographic.
CYP with epilepsy are more likely to have neurodevelopmental disorders. This includes a diagnosis of a learning disability, autism, and attention deficit hyperactivity disorder (ADHD).
One in five CYP with epilepsy also have a learning disability.
A recent review found that 12.1% of autistic people have epilepsy.
Annex 2 contains specific information to consider in delivering epilepsy services for autistic CYP and those with a learning disability.
According to the Learning from Lives and Deaths (LeDeR) review, epilepsy is one of the five most common causes of treatable death in CYP with a learning disability aged four to 18.
Perspective from young people living with epilepsy
This programme of work has been supported by young people who have been diagnosed with epilepsy. NHS England has worked closely with Young Epilepsy to develop this Bundle of Care. Young Epilepsy co-chairs the National CYP Epilepsy Oversight Group alongside NHS England, and Young Epilepsy’s young representatives have played a key role in informing the programme’s priorities, including sitting on the National Oversight Group and contributing to the work of the National Working Groups.
“Living with epilepsy has affected all areas of wellbeing, but the mental impact has been the hardest to deal with”
“I feel forgotten within the system and very much alone”
“Paediatric care was amazing, but there wasn’t a transition period. One day I was just handed off to a new service with no idea who I was seeing or what these people were like”
“The transition needs to be less stressful. I formed a bond with my epilepsy doctor and it was extremely confusing when I couldn’t see him anymore. At the time it felt like a massive part of my support system had been taken away”
“Care plans would be really helpful for parents and educational settings, it would reduce the amount of explaining you would have to do when attending school”
Addressing variation in care between epilepsy services
Recommendations for ICBs
Variation 1
All CYP with epilepsy should have access to an epilepsy specialist nurse (ESN) as set out in NICE guidelines (NG217, 11.1.1)
Recommendation
- ICBs to identify gaps in ESN provision and work with relevant providers to ensure plans are in place to address any variation in access.
Measures
- Epilepsy 12: Percentage of children and young people with epilepsy, with input by epilepsy specialist nurse within the first year of care.
The following may support in the delivery of this recommendation:
Variation 2
All CYP should receive timely access to appropriate electroencephalogram (EEG) and magnetic resonance imaging (MRI) investigations as per NICE guidelines (NG217, 1.2 and 1.3).
Recommendations
- ICBs to identify and map relevant neurophysiology providers and determining waiting times for EEGs. Where waiting times for routine EEGs exceed an average of 8 weeks, ICBs should work with their Regions to develop appropriate plans with clear timelines to ensure timelier access to EEG investigations.
- ICBs to map and ensure clear and consistent pathways for obtaining EEGs and MRIs are in place as part of initial investigations.
- ICBs should determine if appropriate pathways exist for CYP to access investigations under sedation/anaesthesia where appropriate. Waiting times for investigations under sedation/anaesthesia should be determined.
Measures
- Epilepsy12: Median waiting time for first EEG from time of request (Epilepsy12 Audit).
- Epilepsy12: Percentage of children with defined indications for an MRI, who had timely MRI brain within 6 weeks of request.
- Local Audit: Evidence of clear pathways in place for EEG and MRI investigations, including investigations under sedation/anaesthesia.
Variation 3
All CYP should have an agreed and comprehensive written care plan provided to them as per NICE guidelines (NG217, 2.1.7). This should be for home and education settings with evidence of involvement from the CYP and their parent/carer.
Recommendation
- ICBs to identify and work with Providers to increase comprehensive care planning completion rates where they fall below 75% based on Epilepsy12 audit data.
- The care plan should include:
- diagnosis (including seizure descriptions and any known seizure triggers),
- current medication and treatment details,
- any impact on learning and behaviour,
- parental prolonged seizures care plan,
- water safety,
- first aid,
- general participation and risk (safety and injury prevention at home and at school or work, for example road safety, heights, cooking, sleep, adherence), and
- Sudden Unexplained Death in Epilepsy (SUDEP) information
- The care plan should be a patient-held individualised document or copy of a clinic letter that includes care planning information. It should also include service contact details, have patient/carer/parent agreement and be updated when necessary. Providers should ensure care planning takes into account reasonable adjustments for CYP with a learning disability or autistic CYP. This should be reviewed at least annually, and should help inform relevant school healthcare plans.
Measures
- Epilepsy12: Percentage of children with epilepsy after 12 months where there is evidence that a) care planning includes patient held individualised epilepsy document or copy clinic letter that includes care planning information, b) there is patient/carer/parent agreement, and c) care planning has been updated when necessary.
- Epilepsy12: Percentage of children diagnosed with epilepsy with documented evidence of communication regarding core elements of care planning: parental prolonged seizures care plan, water safety, first aid, general participation and risk, SUDEP, and service contact details.
- Epilepsy12: Percentage of children and young people with epilepsy aged 5 years and above with evidence of a school individual healthcare plan by 1 year after first paediatric assessment.
The following may support in the delivery of this recommendation:
Variation 4
All CYP/parents/carers should receive personalised and developmentally appropriate information on the risks of Sudden Unexpected Death in Epilepsy (SUDEP). This should include discussions on minimising individual risks listed in NG217, 10.1. This should be documented and revisited annually as part of the care planning process.
Recommendation
- ICBs should identify and work with providers to increase provision of information on SUDEP where they fall below 75%, based on Epilepsy12 audit data.
Measures
- Epilepsy12: Percentage of CYP with evidence of provision of information on SUDEP.
The following may support in the delivery of this recommendation:
Supporting the mental health and wellbeing of CYP with epilepsy
Recommendations for ICBs
Mental Health 1
CYP over the age of five years old with epilepsy should have their mental health screened routinely within epilepsy clinics.
Recommendations
- ICBs should ensure that processes are in place for all CYP with epilepsy to be routinely screened for mental health difficulties. This should be at the point of diagnosis and in subsequent annual reviews.
- Should mental health problems be identified, the use of a validated screening tool and clear pathways for onwards referral to appropriate providers should be considered.
- ICBs should ensure that where Epilepsy12 audit data indicates mental health screening is not routinely being undertaken within epilepsy clinics, there are plans in place with clear timelines to address and rectify this.
Measures
- Epilepsy12: Percentage of children with epilepsy over five years where there is documented evidence that they have been asked about mental health either through clinical screening, or a questionnaire/measure.
The following may support in the delivery of this recommendation:
- Me and Epilepsy (Appendix 4)
Mental Health 2
CYP with epilepsy who have been identified as requiring additional support with their mental health and wellbeing should be referred to an appropriate service to manage their mental health care. Self-help resources to support wellbeing should be made available to CYP with epilepsy. Providers should have access to clear referral pathways and an up-to-date directory of local services of providers/organisations offering the appropriate level of support. This should include services within healthcare, education and Voluntary Sector and Community Enterprise (VCSE) organisations. It may include Child and Adolescent Mental Health Services (CAMHS), NHS Talking Therapies for Anxiety and Depression, Mental Health Support Teams/educational psychology, psychology support, specialist neuropsychology and neuropsychiatry services, and VCSE mental wellbeing support depending on the level of need.
In addition, CYP with identified neurodevelopmental needs (e.g. Attention Deficit Hyperactive Disorder, or Autism Spectrum Disorder) should be referred into relevant local neurodevelopmental pathways.
Recommendations
- ICBs should map provision of, and referral pathways to, relevant mental health providers and services within their system. This should include mapping appropriate providers of CAMHS, mental health support teams and educational psychology, and specialist neuropsychology, clinical psychology, and neuropsychiatry services.
- ICBs should map availability of VCSE Providers who may be able to provide support for mental wellbeing for CYP with epilepsy including through social prescribing.
- Where gaps in referral pathways are identified, ICBs should have clear plans in place to develop appropriate criteria and pathways into relevant services.
- ICBs should map provision of, and referral pathways to, relevant neurodevelopmental services within their system.
- ICBs should ensure specialist psychological advice is made available across the system to support the management of complex co-morbidities arising alongside the development of epilepsy. Where advice is not available, ICBs should develop appropriate plans to mitigate risks.
- ICBs should determine if there are appropriate local pathways in place to support specialist advice and management for CYP with non-epileptic attack disorder (NEAD). Where such pathways are not available, ICBs should develop appropriate plans to mitigate risks particularly in the context of co-occurring epilepsy syndromes and NEAD.
Measures
- Epilepsy12: Percentage of children with epilepsy and a mental health problem who have evidence of mental health support.
- Epilepsy12: Percentage of Trusts with agreed referral pathways for children with mental health concerns.
- Local Audit: evidence of the availability of specialist psychological advice and local pathways.
The following may support in the delivery of this recommendation:
- Every Mind Matters: This contains advice to enable parents and carers to look after their children’s mental wellbeing, as well as self-help resources.
Mental health 3:
Providers should aim for mental health care to be integrated within the epilepsy service. This may comprise of epilepsy clinics where mental health professionals can provide direct input into clinical care, and meetings where epilepsy and mental health professionals can discuss individual patients.
Recommendation
- ICBs to identify and map providers which have mental health care integrated within the epilepsy service. This comprises epilepsy clinics where mental health professionals can provide direct input into clinical care (for example multi-disciplinary team (MDT) meetings). Where providers do not have evidence of integrating mental health care within epilepsy services, there should be clear plans to mitigate this risk via the development of appropriate pathways into mental health services.
Measures
- Epilepsy12: Percentage of Trusts where mental health provision is facilitated within epilepsy clinics.
The following may support in the delivery of this recommendation:
- Case studies on integrated mental health care (Appendix 5)
Improving referrals into tertiary services and the Children’s Epilepsy Surgery Service (CESS)
Recommendations for ICBs
Tertiary care 1:
All CYP who meet criteria for tertiary neurology referral should have timely access to the relevant tertiary specialist with expertise in managing complex epilepsy. This should be within two to four weeks from referral depending on criteria set out in NICE guidelines (NG217, 3.1.3 and 3.1.4). Assessment will include consideration of all potential treatment modalities including an evaluation for epilepsy surgery. An initial appointment in tertiary care may be held at the tertiary centre or through a locally held paediatric neurology outreach clinics.
Recommendations
- ICBs to ensure there are agreed pathways of referral into tertiary neurology services within each secondary care epilepsy service.
- ICBs to identify and map the provision and waiting times for paediatric neurology input, including outreach clinics based in secondary care centres around the geographical region served (or ‘satellite outreach’ services). ICBs should determine if there are gaps in provision of outreach services within their system to include absence of a service or inadequate provision of the service which prevents the achievement of the standard.
- ICBs to work with their tertiary paediatric neurology centres to determine paediatric neurologist whole-time equivalent (WTE) provision within their system normalised for population.
Measures
- Epilepsy12: Percentage of Trusts that had agreed referral pathways to tertiary paediatric neurology services.
- Epilepsy12: Time in weeks from referral to neurologist input.
- Epilepsy12: Health Boards and Trusts that were hosting satellite paediatric neurology clinics.
Tertiary care 2:
All CYP meeting criteria for epilepsy surgery should be referred into a tertiary paediatric neurology service for consideration of referral to the Children’s Epilepsy Surgery Service (CESS) for an initial assessment as per NICE guidelines (NG217, 8.2).
Recommendation
- ICBs to ensure that there are clear and consistent referral pathways within their system for CESS evaluation. This pathway should involve a referral to a tertiary paediatric neurology service for consideration of referral to a children’s epilepsy service surgery centre (NG217, 8.2)
- ICBs to monitor referral rates within their population such that they are consistent with the expected rates. This will be supported through the provision of referral incidence rates data to Regions.
Measures
- Epilepsy12: Percentage of CYP meeting referral criteria for epilepsy surgery with evidence of epilepsy surgery referral.
- Epilepsy12: Number of CYP diagnosed with epilepsy that met any of the CESS referral criteria that were seen by a neurologist within four weeks of referral.
- CESS referral incidence rates.
The following may support in the delivery of this recommendation:
- Illustrative patient journey (Appendix 6)
Tertiary care 3:
There should be an defined model of shared care between tertiary and secondary care epilepsy services.
Recommendations
- ICBs should ensure that patients who are referred into tertiary neurology services are not discharged from the care of the referring secondary care services.
- CYP should retain a named secondary care paediatrician and continue to receive support from Epilepsy Specialist Nurses within secondary care regarding the day-to-day management of their epilepsy.
- Tertiary teams should provide clear treatment plans for secondary care teams. If there are implementation concerns tertiary care should be consulted.
Measures
- Local audit
Improving the transition from paediatric to adult epilepsy services
Recommendations for ICBs
Transition 1:
All CYP with epilepsy should have a designated named worker responsible for initiating and planning for transition, taking into account any co-existent conditions, as per NICE guidelines (NG43, 1.2.5).
Recommendations
- ICBs should ensure CYP with epilepsy have access to an epilepsy specialist nurse (or access to a Community Paediatric nurse if the CYP has co-morbidities managed under the community paediatric team) to support them through transition.
- The consultant paediatrician primarily responsible for managing the care of CYP with epilepsy should identify those needing transition to adult services between one and two years before proposed time of transfer.
Measures
- Local audit: see suggested proforma (Appendix 10).
Transition 2:
Transition provision and resources should include key essential components and take into account any co-existing conditions and the complexity of epilepsy. The information provided should be individually tailored to the CYP with epilepsy.
Recommendations
- ICBs should ensure that services provide developmentally appropriate information and support for CYP during transition. The Framework for Transition provides a suggested approach with key ‘essential’ components of transition for CYP with epilepsy.
- ICBs should ensure that epilepsy services provide CYP with an Individual Transition plan which takes into consideration professionals or services involved during transition. This should include agreed outcomes with the CYP to achieve before transfer to adult services and discussion about timing of transfer to adult services.
- CYP with epilepsy should be given accessible transition resources with specific components relevant to their condition to prepare them for transfer to adult services.
Measures
- Epilepsy12: Percentage of Health Boards and Trusts that were using structured resources to support transition.
- Local audit: see suggested proforma (Appendix 10).
The following may support in the delivery of this recommendation:
- Example Framework for transition (Appendix 7)
Transition 3:
During the transition period, paediatric and adult multidisciplinary teams should jointly review the person’s diagnosis and management plan as per NICE guidelines (NG217, 11.2.4) Services should involve the Young Person and their family or carers in planning and making decisions about their care.
Recommendation
- ICBs should map outpatient services consisting of both adult and paediatric professionals. Where no service exists, ICBs should work with providers to develop plans for the provision of joint clinics. This may include the development of multi-disciplinary team (MDT) case base discussions between the paediatric and adult teams.
Measures
- Epilepsy12: % of Trusts with outpatient service for epilepsy where there is a presence of both adult and paediatric professionals.
- Epilepsy12: % of Trusts where adult neurologists were routinely involved in transition to adult services.
Transition 4:
Transfer into adult services should be developmentally appropriate and at a time of ‘relative stability’ as per NICE guidelines (NG43, 1.2.3).
Recommendation
- ICBs to map current transfer policies to ensure these are developmentally appropriate, avoid rigid age thresholds and have evidence of co-production between paediatric and adult services.
- Transfer policies should include local arrangements for hospital emergency admission for those over age of admission to paediatric inpatient ward, but still under care of paediatric epilepsy services. In addition, transfer policies should include local protocols in the case of emergencies post-transfer into adult services but prior to the first appointment with the adult team.
- ICBs should determine if there is an agreed transfer destination for each service involved in supporting the CYP with epilepsy.
Measures
- Local audit: see suggested proforma (Appendix 10).
The following may support in the delivery of this recommendation:
- Who should be involved in transition (Appendix 8)
- Suggested transfer destinations (Appendix 9)
- Example local audit proforma (Appendix 10)
Publication reference: PRN00318_i

