Digital tools are changing the way primary care is delivered. By providing practices with a range of features, digital tools enable them to develop new care pathways and workflows that can enhance the delivery of healthcare.
Decision-makers within practices need to understand how they can be used in real-world scenarios. This means understanding their capabilities, appreciating their differences, and choosing digital tools that will have the highest impact. Online consultation (OC) tools have a range of features that may benefit practices and patients alike. Choosing the right OC tool to meet the needs of the practice and local population is an important decision
NHS England has published a toolkit for practices on using online consultations in general practice, which you will find helpful.
Security and confidentiality considerations are ser out in the NHS England web pages Using video conferencing and consultation tools.
Purpose
Online consultation tools allow patients to contact their practice without coming into the surgery or Online consultation tools allow patients to contact their practice without coming into the surgery or waiting on the telephone. They allow patients to provide the reason for their request and provide any clinical or admin-related information. They act as an entry point into the practice, a digital front door. In their simplest form, the tools allow online consultation requests to be directed to different services, appointment types, or consultations within the practice. Various tools are available, and they all operate in slightly different ways. The digital and online services requirements detail the minimum features OC tools must provide. As a minimum, they must allow the patient to:
- make clinical or administrative requests
- seek health advice
They use different methods to collect and analyse the information they receive from patients. They also have different feature sets which impact the experience for patients and clinicians.
OC tools use three basic methods when collecting clinical information from patients:
- questionnaire-type – collects information on predefined forms based on the presenting complaint, often allowing free text entry
- chatbot-type – collects information using a real-time chatbot that presents questions based on the answer to the previous question and the presenting complaint (free text entry is often limited)
- online messaging-type – uses online messaging (OM) tools as the entry point for patients to initiate patient-led online consultations. They allow patients to free text their information directly to the practice through a two-way communication platform
Many of the tools use a combination of the three methods listed above, for example questionnaire-based tools that have direct secure messaging built into their package.
Understanding the different features of OC tools is important when choosing the right tool for your practice. As OC tools mature, they will be able to offer more advanced features. You can find out more by visiting the Digital First Online Consultation and Video Consultation framework.
Online consultation tools | History taking style
Amongst the features on offer, important considerations include:
- the degree of free text entry
- the automation capabilities of the tool, which should be considered in the following ways:
- automated history-taking engines (chatbot style) that collect information without any free text entry
- automated processing of this patient-provided information without human intervention to direct patients into a service or care pathway, g. automatically directing a musculoskeletal-related OC request by booking them in for a telephone call by a first-contact physiotherapy practitioner
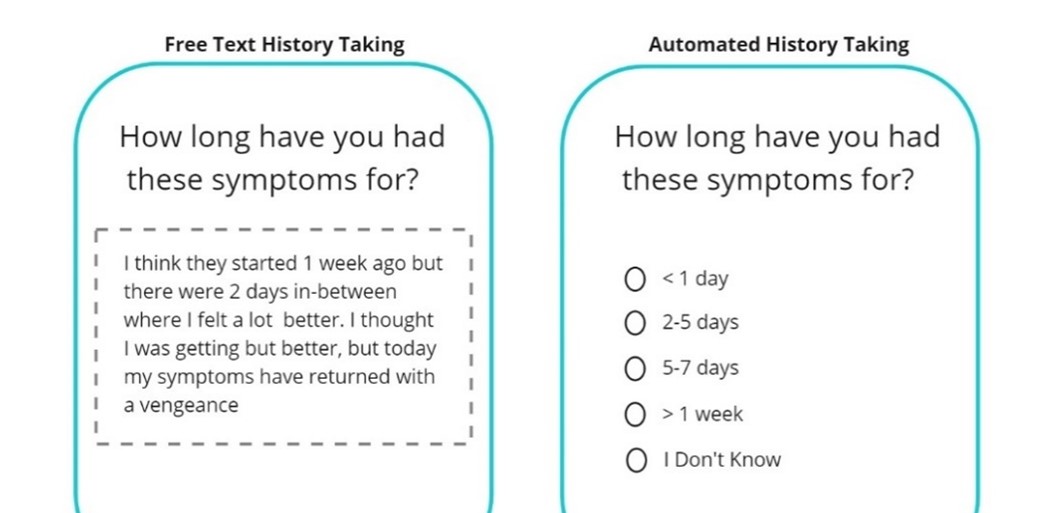
Chatbot-type OC tools typically use an automated history-taking engine. Patients respond to predefined questions from predefined pick lists or options. In most cases, patients are unable to attach clinical images or documents. Conversely, questionnaire-type history-taking allows patients to describe their symptoms in their own words and often allows patients to attach clinical images and documents.
Figure 1: Automated history-taking engine vs free-text history taking
Tools limiting free text entry have increasing capabilities to automatically process the information provided by patients without the need for human intervention. These tools do not need to understand the contextual meaning of any free text entry by patients. The technology can then process the information provided against predefined rule sets. In some cases, it means they can automatically process information (without human intervention), and direct patients into a service or care pathway.
Tools that automatically process patient information requires a Data Protection Impact Assessment (DPIA). Many OC tools now allow a combination of automated history taking and free text entry.
There are advantages and disadvantages to the different methodologies and degrees of automation.
Choosing the right tools
Picking the right OC tool for your practice can be difficult. Remember to work closely with your commissioners, suppliers and local practices and learn from each other. A ‘one size fits all’ approach will not work. You need to match the tool to the needs and wants of the practice and your local population.
Remember you are unlikely to find an OC tool that can meet all your needs. Choose one that solves your high-priority short to medium-term challenges and can grow with your long-term strategic objectives.
Online messaging tools (as a feature of the online consultation tools or as a standalone product)
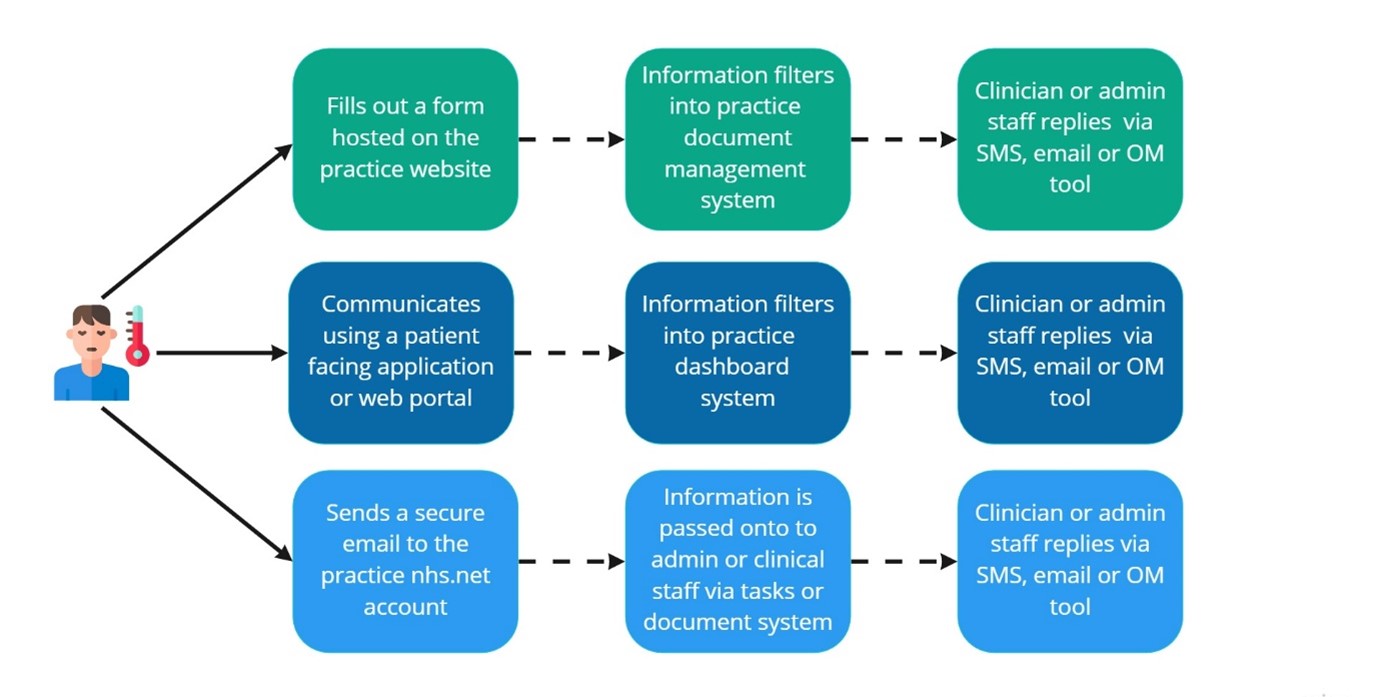
The core digital offer means patients must be able to communicate with the practice via electronic communications digitally. The diagram below shows some flows currently used for online messaging between patients and the surgery.
Figure 2: Online messaging flows in practice
Practices using NHSmail to reply to patients must remember to use the secure encryption facility when replying. To do this add the word [secure] in the subject line of a message – with the inclusion of the square brackets.
Most practices use a combination of the three methods detailed above, with many relying on OM tools either as part of their OC tool or as a standalone product to respond to patients.
OM tools have a variety of feature sets that can benefit patients and practices when compared to NHS mail or SMS. The Digital first online consultation and video consultation framework (DFOVC) covers many OM tools currently in use, as many of these tools also offer OC and video consultation (VC) functionality.
Related GPG content
- Digitally enabled triage
- Remote consulting
- Remote consulting tools – procurement, regulations, governance and transformation
- Video consultation tools
- NHSmail
- NHS App
- Cyber security
- Information governance and data protection
- Calculating Quality Reporting Service (CQRS) and Quality Outcomes Framework (QOF)
- Health equalities and inclusion
- Clinical coding – SNOMED CT
Other helpful resources
- NHS England, Dynamic Purchasing System (DPS) for digital social care record solutions
- NHS England, Online consultations in the NHS App