Patient-centred services sit at the heart of primary care, and practices are best placed to develop consultation models that serve their local communities. Creating systems that allow access to face-to-face and remote consultation methods reduces the risks of exclusion and increasing inequalities. Using remote consulting appropriately can enable faster, more convenient access whilst delivering timely face-to-face access for those that need it.
Key definitions
Remote consultation is a type of consultation between a patient and staff member(s) that involves a complete episode of care which does not need face-to-face contact.
Telephone consultations allow patients to interact with health professionals using the direct voice-to-voice function of the telephone – this includes internet telephony systems.
Video consultations allow patients to interact with clinicians using video conferencing technology.
Online ‘written’ consultations allow patients and clinicians to interact with each other using a secure two-way online messaging via SMS, secure email, or online messaging (OM) tool to complete an episode of care.
Remote consulting overview
The NHS England web pages on the Modern General Practice Model contains a helpful resources section including guides to high quality video consultations and an online consultations in primary care toolkit.
Making remote consulting a success
All consultation types have their own benefits and risks. Practices need to engage, communicate, and help patients navigate different appointment systems if they want to experience the advantages and minimise the pitfalls (Figure 1).
Getting the best out of remote consulting is a report by the Nuffield Trust (2022) that you might find helpful in making remote consulting a success.
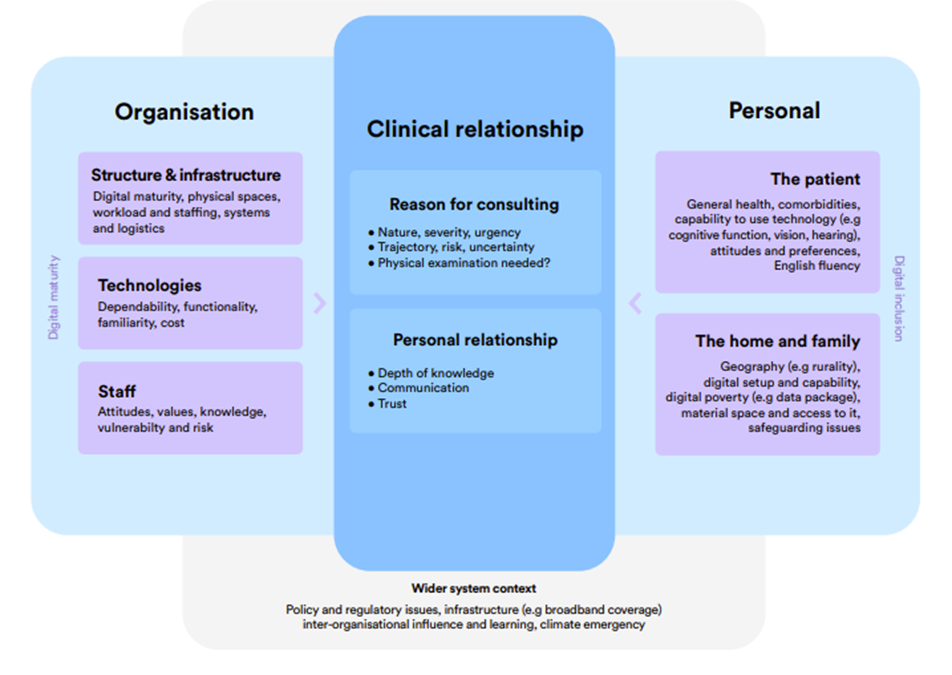
Several factors influence the overall success of remote consulting for practices (Figure 2 below). Practices need to work collaboratively with their local population and the individual needs of their patients to ensure the right clinicians are seeing the right patients in the right way.
Figure 1: Factors influencing remote consultations
The General Medical Council (GMC) has published a guide to prescribing in remote consultations which you might find useful.
Benefits and pitfalls of remote consulting
Benefits
The right use of consulting remotely can be beneficial both for patients and practices. Remote consulting can:
- save patients time, reducing the need to travel into the practice
- improve access for certain patient groups:
- the working population, who may find it difficult to take time off work
- physically housebound patients, by reducing the need to travel
- patients who are digitally literate and happy to consult remotely
- carers or relatives of patients who can use remote consulting to provide better support for their loved ones
- those living in rural/remote areas
- reduce waiting times for initial contact with a practitioner
- help patient groups experiencing difficulties with social interaction, who may prefer remote consulting
- patients may find it easier to explain their symptoms using online consultation tools or explain embarrassing problems in a remote setting
Practices can benefit by using hybrid working models that allow staff to carry out clinical care conveniently in their homes. This can be particularly powerful in terms of staff recruitment by disrupting geographical recruitment barriers.
Remote consulting can also help practices maximise the use of their estate, especially when space is at a premium.
Potential pitfalls
Without adequate training, support, and process development, staff may struggle to optimise patient care through remote means. In these circumstances remote consulting could result in:
- delayed or missed diagnoses
- over or under investigation of patients
- increasing the burden on clinicians to make judgements remotely
- reduction in the therapeutic relationship between patients and clinicians
- increase in the transactional aspect of care over personalisation, where patients experience limited interactions remotely or feel they are unable to see their doctor face-to-face
- missed opportunities to pick up subtle cues during a face-to-face consultation
- digital exclusion of certain patient groups
- increasing complexity for reception staff when booking in patients to different consultation types
Barriers to technology or simple blockers, such as a poor phone signal, can become problematic for patients being asked to consult remotely.
Challenges of remote consultation
Personalised care
Personalised care helps patients shape their own care, health, and well-being. It recognises that a one size fits all health and care system does not meet individual needs. Delivering personalised care can be challenging, even in traditional face-to-face settings.
Practices must support and train their staff to effectively provide personalised care during remote encounters.
Workload
There is no current evidence that remote consulting reduces workload in primary care. This does not mean remote consulting can’t reduce workloads in primary care, however assessing the impact of remote consulting can be difficult because practices may use remote consulting in different ways.
If triage isn’t done well remote consulting can lead to an increase in workload as a face-to-face consultation may still be needed. Practices need to be mindful when booking appointments that the most appropriate appointment type is given for the problem at hand.
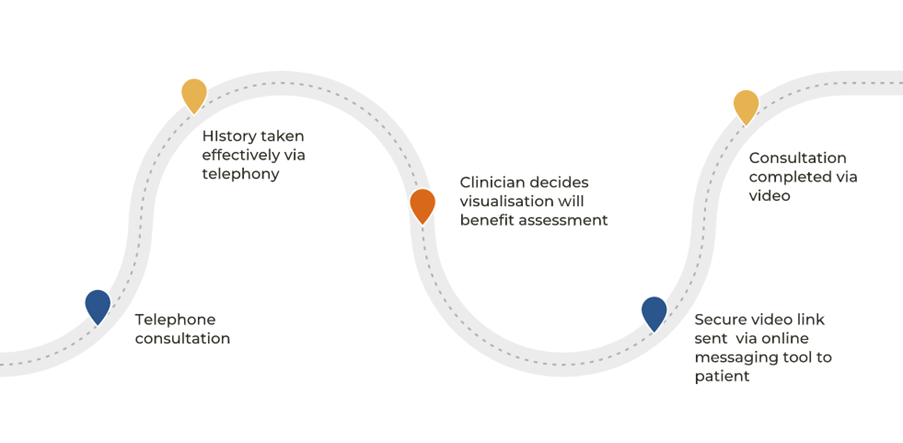
As illustrated in Figure 3, the fluid nature of consultation types in one ‘episode’ of care can also complicate the data that is being collected regarding remote consultations in primary care.
Figure 2: Multiple consultation modes in a single episode of care
Workload is only one factor when considering the impact of remote consultations. The intersection between workload, patient access, demand management, hybrid working, and patient triage needs further evaluation.
Regulatory and medico-legal considerations
Practices should ensure they are offering remote consultations appropriately. The Medical Protection Society advises the following:
‘When considering a remote consultation, you should weigh up whether you can adequately assess the patient remotely.’
Remember, the General Medical Council’s (GMC) standards of good medical practice still apply to all remote consultation types. The GMC has created a helpful flow chart reminding clinicians and practices of these expectations when delivering or providing care remotely.
Similarly, the Care Quality Commission (CQC) expect all the standards for good care to apply to remote consultations. Their myth buster is an important reminder of these requirements.
Further information can be found through guidance created by Medical Defence Union (MDU) Conducting Remote Consultations.
Preparation, policies and procedures
Many practices implemented remote consulting at speed during the COVID-19 pandemic (2020 – 2022 ). In addition to updating privacy notices and carrying out data protection impact assessments, practices must ensure their policies and procedures are updated to reflect the use of remote consulting in primary care.
Table 1 summarises a bird’s eye view of some important policies and protocols that may need updating or creating.
Table 1: Policies and procedures in remote consulting
|
Policy or Standard Operating Procedure |
Key Considerations |
|
Consent |
|
|
Confidentiality |
|
|
Capacity |
|
|
Adult and Child Safeguarding |
|
|
DNA/Was not brought policy |
|
|
Emergency management |
|
|
Clinical safety risk assessment |
|
|
Clinical images and photographs |
|
|
Intimate examinations and chaperoning |
|
|
Prescribing |
|
|
Health and safety |
|
|
Remote working |
|
|
Remote consulting |
|
|
Staff training |
|
General approaches when carrying out remote consultations
The principles of good medical practice apply to all consultations. There are, however, specific areas that need consideration when consulting remotely.
Workspace preparation
Optimising the workspace is essential when delivering remote consultations. Staff should ensure their workspace is optimised to maintain their comfort during a remote consultation. Staff should complete a display screen equipment assessment. Headphones should be comfortable and within safe sound limits.
Preparation of consulting area
Staff must ensure they are stationed at a desk in a private, quiet, confidential area, with the door closed. During video consultations the seating position should be free of pictures or distracting artwork, with lighting providing patients with a clear, unobstructed view.
Personal factors and positioning
Professional work attire applies to any remote consulting within practices or when staff are working from home. During telephone and video consultations clinicians should confirm that patients can hear and/or see them adequately. Clinicians should avoid being too close or far away from webcams during video consultations to ensure effective patient engagement.
Clinical preparation before a remote consultation
Clinicians should try to review relevant information before starting the appointment. When further review of the patient record is necessary, patients should be made aware, to explain any temporary disengagement by the consulting clinician.
Patient identity and verification
The responsibility for identity verification and authentication sits with the consulting clinician. The consulting clinician must confirm the identity of the patient and/or their delegated representatives.
Confirming location
Patients may choose to consult in a variety of environments, including those outside of their homes or places of work. Confirming the location of the patient is important in the event of an emergency.
There is an increased likelihood of patients requesting remote consultations whilst abroad. The Medical Protection Society (MPS) has created guidance regarding this. Practices and staff should contact their own indemnifier for further information.
History taking
Thorough history-taking is essential during any consultation, but even more so during a remote consultation where visual cues may be missed. Clinicians should adapt their consultation skills when consulting via video or telephony. For example, it may be helpful to convey attention through eye contact and facial expression during video calls. Clinicians may need to change how they use ‘pacing’ cues during the consultation.
When conducting written consultations, clinicians must think clearly about how they construct and convey ideas and instructions to create a shared understanding.
Examination
Examination during a remote consultation requires a modified approach. Documenting examination findings is an essential part of any consultation. During a remote video or telephone consultation, simple judgements can be made about the patient’s speech, level of distress or general engagement during the call. Carrying out more targeted examinations is possible. Clinicians must, however, ensure:
- the examination is suitable for remote consulting
- the patient can conduct any self-led examination safely
- they remember the burden it may place on certain patients
Clinical images and photo examination
Clinicians may have asked a patient to upload a photo of the affected region. Patients must be informed that uploaded images will form part of their medical records.
Clinicians or staff should only request clinical images if they feel it will aid clinical decision-making. Examination of any image that helps form a management plan or diagnosis must be documented in the notes. The MDU has detailed guidance on this subject.
Intimate examinations
It is not advisable to encourage patients to send clinical images of intimate regions or reveal or self-examine intimate areas during a remote consultation. The GMC is clear that all patients should be offered a chaperone. Patients who require an intimate examination should, therefore, be encouraged to attend for a face-to-face assessment.
If the patient insists on a remote intimate examination, staff must apply clinical judgement considering the following:
- impact of a remote examination on eventual management
- suitability of effective assessment using video or clinical images
- risks benefit approach for the patient
- risk of any coercion or safeguarding concerns
- the patient’s individual and personal circumstances
- alternative ways the patient could provide that information, e.g. taking a picture on their own phone and holding it up to the webcam
For further information, see the Care Quality Commissioner and GMC Guidance.
Closing/ending remote consultations
Summarising at the end of the remote consultation will help identify areas of misunderstanding which can arise during remote consultations. This is particularly important for video or telephony consultations when connection or lag issues can result in important information being misinterpreted. Communicating the intention to terminate the encounter is important so patients understand the consultation has been closed rather than the occurrence of an unexpected technical event.
Safeguarding
It is the responsibility of all adults to safeguard and promote the welfare of children and young people. Practices need to train and guide clinicians on identifying and escalating child and adult safeguarding concerns during a remote consultation. Patients identified as safeguarding risks should be followed up in a face-to-face setting unless doing so is not in the patient’s best interests.
Remote consulting with children and young people
A child may wish to exclude a parent from their remote consultation. This is their choice if they have the capacity to make this decision. Children under the age of 12 are unlikely to have the capacity to make this decision, and parental presence is strongly recommended. The principles of the Gillick competency and Fraser guidelines apply to remote consultation just as they do for face-to-face consultations.
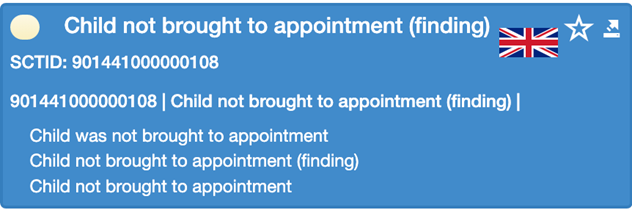
Children who fail to attend a planned remote appointment without cancellation should have the relevant SNOMED code added to their record, as is the case for face-to-face consultations.
Figure 3: SNOMED CT code
Adults of course may also fail to attend a remote consultation, and this should be coded as a ‘did not attend’. There is another article in this series on Online access for children.
Prescribing
Clinicians must satisfy themselves that they can adequately assess the patient, and only prescribe remotely when they have adequate knowledge of the patient’s health. Clinicians should consider:
- the limitations of the medium through which they are consulting with the patient
- the need for physical examination or other assessments
- level of access to the patient’s medical records
The GMC has guidance on prescribing in remote consultations.
Patient held devices and remote consultations
Patients increasingly want to share information from wellness apps, wellness devices, and medical-grade devices to monitor their health, e.g. pulse oximeters, smartwatches, blood pressure machines, etc.
Clinicians should apply caution when using this information to influence decision making, unless they are familiar with the device being used.
Online written consultations
Written consultations allow patients and clinicians to exchange information via two-way communication systems. This can be as simple as using a webform, email portal, or more sophisticated online messaging tools. These can be patient or clinician/practice initiated.
Consultations can be delivered using solely written consultation methods. For example, a patient may enter a written request through an online consultation tool, and the clinician may review, assess, respond, and close the episode of care directly via an online messaging tool.
They often form part of a dynamic consultation approach in practices as additions during a telephone or video consultation (see Figure 1).
The BMJ has a helpful article on how to conduct online written consultations in primary care.
Related GPG articles
- Digitally enabled triage
- Online consultation tools, covering the different types of tools and their important features
- Video consultation tools
- Remote consulting tools – procurement, regulations, governance and transformation
- Safeguarding
- Identity (ID) verification
- Clinical coding – SNOMED CT
- Health equalities and inclusion
Other helpful resources
- The Lancet, Remote general practitioner consultations during COVID-19 (2022)
- British Journal of General Practice (BJGP) Clinical risk in remote consultations in general practice: findings from in-COVID-19 pandemic qualitative research
- BJGP, Why do GPs rarely do video consultations? qualitative study in UK general practice
- Healthwatch, Locked out: Digitally excluded people’s experiences of remote GP appointments
- RCGP, GP consultations post-COVID should be a combination of remote and face to face, depending on patient need
- BJGP, Inequalities in general practice remote consultations: a systematic review
- National Library of Medicine, PubMed, Impact of digital first consultations on workload in General Practice: modelling study
- Remote Consultations and Personalised Care (NIHR, University of Bristol, Centre for Academic Primary Care)Medical Protection Society (MPS), Remote consultations – What are the benefits and risks?
- MPS, Providing care to patients who are abroad
- University of Bristol, Student guide to remote consulting in primary care
- BMJ, How to conduct written online consultations with patients in primary care
- NHS England, Inclusive access routes, summary evaluation report of a pilot in the Humber and North Yorkshire
- Department for Health and Social Care, General practice access routes – campaign resources including a toolkit.