Introduction: generating greater value for patients from outpatient care
This improvement guide supports clinical and operational teams to improve the outpatient care provided to patients. In 2023 the NHS worked with the Royal College of Physicians and the Patients Association to engage with people with lived experience to understand what mattered to them. In addition to the clear expectation of high quality safe care, delivered as rapidly as possible, people told us they want:
- care to be co-ordinated better, particularly for people with co-occurring conditions which bring them into contact with multiple clinical teams
- improved communication, both between healthcare professionals, and between healthcare professionals and their patients
- a more holistic approach to care – treating the whole person, focusing not just on physical but also psychosocial care needs
- greater control and choice – not just choice of hospital but of their whole end-to-end experience (including information about treatment choices; control over timing and format of appointments; more options for post treatment care)
- greater join up between services and organisations – avoiding suboptimal hand-offs of care between parts of the system, which are inefficient and clinically risky
This guide sets out the current evidence-based practice and provides a range of change ideas that can deliver improved care for patients. We encourage teams, organisations and systems to test and adapt these for their local context.
We want to understand how this guide works for you and your teams, and how we can further develop and improve it to make it as useful as possible to support local improvement programmes. Therefore, this is an interim guide – our intention is it will be refined, developed and updated as we learn what works through your teams. Please share your thoughts on the guide and your ideas to include in it – details on how to do this are at the end of this guide.
Alongside this guide, improvement analytics can be used to diagnose issues and identify opportunities to improve care and track improvement over time. The improvement metrics will evolve as data collected nationally better reflects new care models. Alone they do not give the complete picture for flow and the opportunities to improve patient outcomes across the whole cycle of care. For this, clinical and operational teams need to work together to join up local insight and intelligence to better understand and address opportunities to improve outcomes for the patient, particularly at the interface of specialties and services. Teams are encouraged to supplement the nationally available measures with locally collected insight on patient experience and pathway-related outcomes.
Overarching ambition
This driver diagram sets out the theory of change for how the change ideas in this improvement guide can lead to improved outpatient services.
Outpatient driver diagram
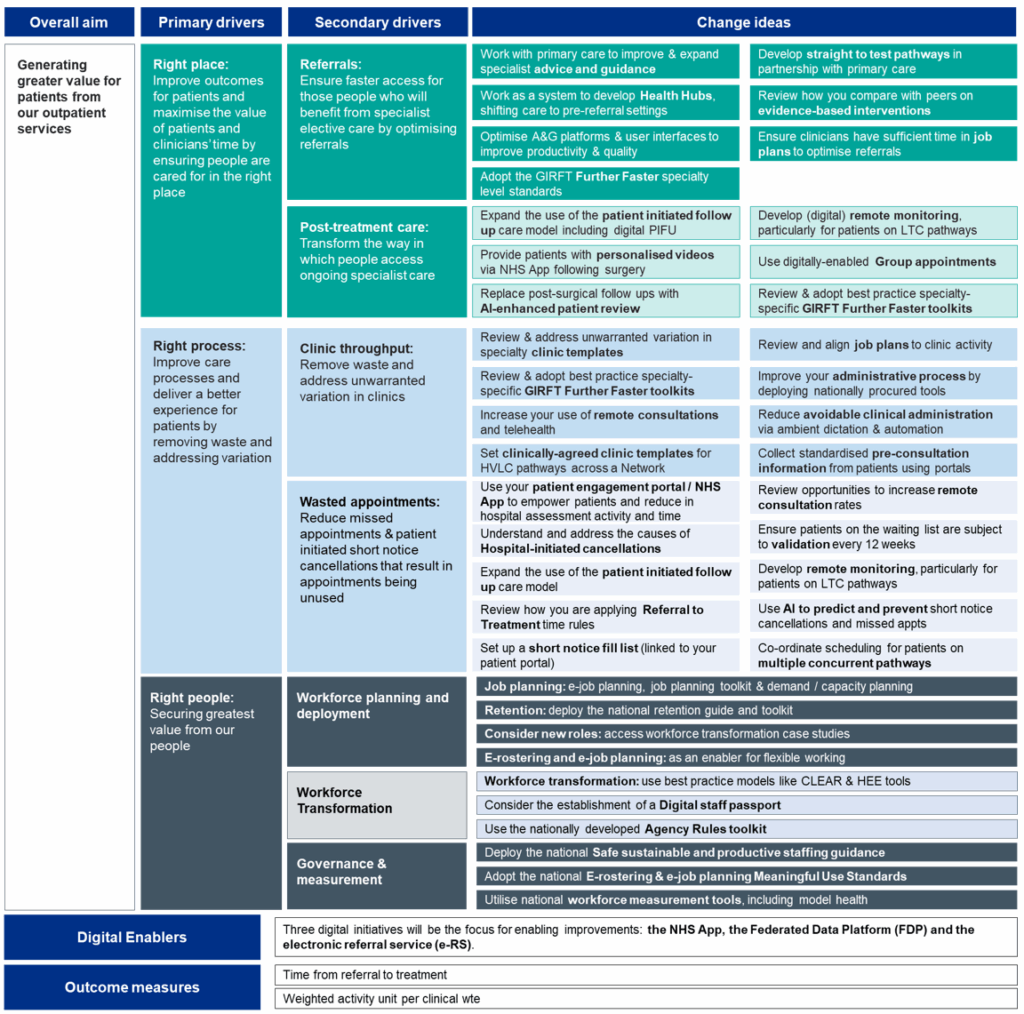
Click here to access an accessible description of the driver diagram:
Overall aim
- Generating greater value for patients from our outpatient services.
Primary drivers
- Right place: improve outcomes for patients and maximise the value of patients and clinicians’ time by ensuring people are cared for in the right place.
- Right process: improve care processes and deliver a better experience for patients by removing waste and addressing variation.
- Right people: secure the greatest value from our people.
Areas of focus
- Referrals: ensure faster access for those people who will benefit from specialist elective care by optimising referrals.
- Post-treatment care: transform the way in which people access ongoing specialist care.
- Clinic throughput: remove waste and address unwarranted variation in clinics.
- Wasted appointments: reduce missed appointments & patient initiated short notice cancellations that result in appointments being unused.
- Workforce planning and deployment.
- Workforce transformation.
- Governance and measurement.
Change ideas
- Work with primary care to improve and expand specialist advice and guidance.
- Develop straight to test pathways in partnership with primary care.
- Work as a system to develop Health Hubs, shifting care to pre-referral settings.
- Review how you compare with peers on evidence-based interventions.
- Optimise AandG platforms and user interfaces to improve productivity & quality.
- Ensure clinicians have sufficient time in job plans to optimise referrals .
- Adopt the GIRFT Further Faster specialty level standards.
- Expand the use of the patient initiated follow up care model.
- Develop remote monitoring, particularly for patients on LTC pathways.
- Provide patients with personalised videos via NHS App following surgery.
- Use digitally enabled Group appointments.
- Replace post-surgical follow ups with AI-enhanced patient review.
- Review and adopt best practice specialty-specific GIRFT Further Faster toolkits.
- Review and address unwarranted variation in specialty clinic templates.
- Review and align job plans to clinic activity.
- Review and adopt best practice specialty-specific GIRFT Further Faster toolkits.
- Improve your administrative process by deploying nationally procured tools.
- Increase your use of remote consultations and telehealth.
- Reduce avoidable clinical administration via ambient dictation & automation.
- Set clinically-agreed clinic templates for HVLC pathways across a Network.
- Collect standardised pre-consultation information from patients using portals.
- Use your patient portal to empower your patients.
- Review opportunities to increase remote consultation rates.
- Understand and address the causes of Hospital-initiated cancellations.
- Ensure patients on the waiting list are subject to validation every 12 weeks.
- Expand the use of the patient initiated follow up care model.
- Develop remote monitoring, particularly for patients on LTC pathways.
- Review how you are applying Referral to Treatment time rules.
- Use AI to predict and prevent short notice cancellations and missed appts.
- Set up a short notice fill list (linked to your patient portal).
- Co-ordinate scheduling for patients on multiple concurrent pathways.
- Job planning: e-job planning, job planning toolkit & demand / capacity planning.
- E-rostering and e-job planning: as an enabler for flexible working.
- Retention: deploy the national retention guide and toolkit.
- Consider the establishment of a digital staff passport.
- Use the nationally developed agency rules toolkit.
- Workforce transformation: use best practice models like CLEAR and HEE tools.
- Consider new roles: access workforce transformation case studies.
- Deploy the national safe sustainable and productive staffing guidance.
- Adopt the national e-rostering and e-job planning meaningful use standards.
- Utilise national workforce measurement tools, including model hospital.
Digital enablers
- Three digital initiatives will be the focus for enabling improvements: the NHS App, the Federated Data Platform (FDP)and the electronic data referral services (e-RS).
Outcome measures
- Time from referral to treatment
- Weighted activity unit per clinical for wte
Download the above diagram as a PDF file.
These ideas are key enablers for an increase in the percentage of patients waiting <18 weeks for their first appointment which is the overarching focus for elective Learning and Improvement Networks across the country. This guide is also an important resource in exploring Clinical and Operational productivity opportunities identified in planning support tools provided to finance teams during the planning round.
Right place
Improve outcomes for patients and maximise the value of patients’ and clinicians’ time by ensuring people are cared for in the right place
Optimising referrals
Ensure faster access for those people who will benefit from specialist elective care
There are several ways in which clinicians can work together at the interface between services to ensure people access the right specialist care as rapidly as possible. Key to success is consistent and constructive engagement between primary care and secondary care.
Many systems have agreed guidelines that advise primary care clinicians on the criteria and thresholds for referral to specialist care. The GIRFT programme is publishing referral and specialist advice guidance for several higher volume pathways later this year. Straight to test pathways are also now expanding beyond cancer pathways, streamlining access for patients and avoiding unnecessary appointments.
Systems are also going further and establishing walk-in and pre-appointment health hubs that bring together primary, community and secondary care to improve access to care currently delivered in hospital outpatients and to bring it closer to home.
Specialist advice (both pre and post-referral) is now a cornerstone of referral optimisation. Enabled by the e-Referral Service (e-RS), this approach helps ensure patients are managed in the most appropriate setting.
Technology is also transforming how referrals are managed. Telehealth solutions (for example, teledermatology) are enabling a step-change in the speed with which referrals can be safely reviewed by specialists, cutting waiting times for patients.
Case study: Northumbria Healthcare NHS Foundation Trust
The Northumbria gastroenterology team, led by Consultant Gastroenterologist Dr Matt Warren, treats patients with a wide range of conditions – relating to the liver, stomach and bowel – across a mix of urban and rural settings.
The challenge
The gastroenterology teams previously followed the traditional NHS Choose and Book model of the GP making a referral to the gastroenterology team and the patient then waiting a significant length of time for a face-to-face appointment in a consultant outpatient clinic. This first appointment would often then lead to further waiting for the patient who would have been referred for diagnostic tests, such as endoscopy, after the clinic. This would all add up to a considerable length of time until patients would receive necessary and effective treatment.
Making the best use of e-RS
“At Northumbria, offering support to primary care to treat their patients without delay was pivotal. Our approach was very much to encourage GPs to ‘discuss with’ rather than ‘refer to’ us – enabling appropriate patients to be managed by their GPs, and reducing the waiting times for those patients who did need hospital appointments. And this builds up confidence in primary care that their patients with urgent gastroenterological problems could be seen within 1 to 2 weeks as a result”, explains Dr Warren.
“For me, it’s really important that we use all the technologies we have available, such as e-RS and electronic patient records, to get treatment advice as quickly as possible.”
The results
Northumbria’s gastroenterology team is now seeing most elective new patients within 2 to 4 weeks of any referrals, and urgent patients within 1 to 2 weeks. Previously this had been closer to 12 to 14 weeks.
The percentage of patients being seen within the 18 weeks Referrals to Treatment (RTT) timescales has risen, Appointment Slot Issues (ASIs) have been reduced and Advice and Guidance requests have risen compared to pre-COVID figures.
The team is also now rolling out some of their ways of working to other specialties in the trust, with early results looking positive.
How to optimise your referrals
Value opportunity
If every system increased the impact of Advice and Guidance (A&G) by 15% in 2024/25, this would free up 60,000 first appointments across the country (even accounting for the time spent supporting the A&G process). If this increase in A&G impact were achieved equally across the country, the averaged sized acute hospital would be processing 48 additional A&G requests every week.
Tracking indicators
In addition to local process measures linked to your change ideas, A&G process measures are available in the Model Health System, including utilisation, turnaround time and diversion rate.
Change ideas
- Work in partnership with general practice to establish or optimise existing pre-referral specialist advice services. There is guidance on commissioning these services; support on medico-legal issues; benchmarking information on expansion opportunities; a specialist advice toolkit and a specialist advice comms toolkit, and GIRFT standardised A&G templates (FutureNHS is a member platform that requires a log in).
- Streamline and reduce variation in post-referral A&G and triage, supported by the NHS e-Referral Service (e-RS) toolkit. Optimise user interfaces to improve clinical productivity. Also consider using your patient portal to collect pre-consultation questionnaires from patients to support clinicians to enhance this post-referral assessment process.
- Work as a system to review current practice for consultant-to-consultant referrals.
- Adopt GIRFT ‘further faster’ specialty-level standards.
- Explore the use of straight to test pathways.
- Review the opportunity to improve adherence to nationally published evidence-based interventions.
Resources
Help and support: england.outpatient-transformation@nhs.net
Optimising post-treatment care
Transform how people access ongoing specialist care
There are significant opportunities to improve the experience and outcomes for elective patients following diagnosis and at the start of their treatment, particularly for those people with co-occurring conditions whose care can lack co-ordination and be difficult to navigate.
How to optimise post-treatment care
Value opportunity
If every hospital were to increase its patient initiated follow up (PIFU) utilisation rate by 1 percentage point compared to the 2023/24 baseline through the second half of 2024/25, nationally 400,000 more patients could be seen in outpatients this financial year. For an average sized hospital this would mean 60 more patients on a PIFU pathway every week.
Tracking indicators
In addition to local process measures linked to your change ideas, 2 process measures feature in the improvement analytics:
- PIFU utilisation
- proportion of all outpatient attendances that are for first appointments or follow-up appointments attracting a procedure tariff
Change ideas
- Expand the use of PIFU; there is national guidance, GIRFT specialty-level guidance and the trust-specific PIFU opportunity packs to support you. While PIFU will be appropriate for many children and young people, there are specific considerations to take into account, including the availability of alternative support for children and whether the primary care workforce is currently best placed to support children.
- Develop Care Coordination to better support all patients, but particularly the most vulnerable or those who are on complex co-occurring condition pathways.
- Develop remote monitoring protocols for patients on long-term condition pathways who require regular and routine review, leveraging patient engagement portals. Where possible automate this remote monitoring to reduce the administrative burden on staff; see Supporting care with remote monitoring. Consider using freed up clinic administrative staff to support patients to use new digital channels.
- Consider using personalised videos to inform, reassure and equip patients with the information they require to manage their care following surgery, reducing the need for follow-up appointments.
- Use forms and questionnaires delivered through your patient portal to triage post-surgical patients to determine if they require follow up care. Artificial intelligence can augment this approach, collecting, collating and presenting information to clinicians to enable them to discharge without follow-up.
- Learning from primary care models, use digitally-enabled group appointments (particularly for long term condition pathways) to increase the number of patients accessing advice and support per clinician.
- Clinic letters to be received within 5 days; meds initiated, and patients given 28-day supply; with clear accountability for trust, GP and patient and point of escalation.
Resources
Help and support: england.outpatient-transformation@nhs.net
Right process
Tackling waste and reducing variation
Increasing clinic throughput
As described above, referral initiatives can release capacity for quicker first and procedure follow-up appointments, but unwarranted variation in clinic throughput should also be addressed. The number of patients scheduled to be seen in clinic templates varies widely even within the same specialty and hospital.
In many cases, this variation is appropriate as it relates to the mix and complexity of patients, but in some it will be down to practical constraints or historical practices that would benefit from review – to deliver greater value from our existing services.
We encourage systems to focus on identifying, understanding and addressing variation in clinic throughput in 2024/25
How to increase clinic throughput
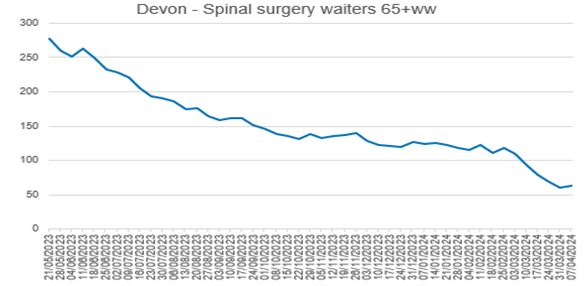
Case study: Devon Health System
Supported by GIRFT, Devon ran a pan-system improvement programme across a range of specialties including spinal. The Devon Spinal clinical lead led work to harmonise clinical pathways, standardise clinic templates and improve operational processes. This increased clinic slots within existing job plans by about 50%, providing over 1,100 additional slots per annum and delivering a significant reduction in long (65+-week) waiters.
Value opportunity
If every clinical team sees at least 1 more patient in every outpatient clinic held in the second half of 2024/25, nationally an additional 3.5 to 4.5 million more patients could be seen by the end of the financial year.
Tracking indicators
In addition to local process measures linked to your change ideas, the relevant indicator in the improvement analytics is:
- All outpatient attendances per consultant whole time equivalent.
Change ideas
- Review your current operational processes against the GIRFT best practice guidance*
- Increase your use of remote consultation and telehealth (including teledermatology) to help increase your clinic throughput. Remember children and young people have specific needs in relation to remote consultation*
- Increase the transparency of clinic throughput within and between specialties. You can benchmark your specialty throughput against the ‘further faster’ sites using GIRFT data. We are developing specialty-specific clinic templates that set minimum throughput ambitions with Royal Colleges, and these will be available later in 2024/25*
- Review clinic processes to identify where technology (for example, robotic process automation) might address operational constraints and/or where technology might be creating delays.
- Review the alignment between consultant outpatient activity and consultant job plans with a view to increasing job plan compliance – using the national job planning toolkits on the FutureNHS NHS IMPACT platform.*
- Deploy the NHS Federated Data Platform outpatient care co-ordination solution.
- Use your learning network/improvement collaboratives to identify variation in specialty or condition level clinic throughput, and develop collective improvement plans to reduce variation across the system.
* Specialty-specific best practice guidance for these change ideas is in the GIRFT ‘further faster’ handbooks and the Remote Consultation Improvement Toolkit.
Resources
Help and support: england.outpatient-transformation@nhs.net
Reducing wasted appointments
Last year patients did not attend nearly 7.5 million of the around 100 million booked outpatient appointments. Less visible, but equally impactful, are the patient cancellations too close to the time of the appointment to allow the hospital to re-use the slot. Both these events, as well as unfilled slots, waste appointments. Such waste is frustrating for patients and staff, inefficient and can contribute to inequalities in access and care.
Some clinics work on the basis that some missed appointments are to be expected and seek to mitigate this waste by overbooking the number of patients they plan to see, but this risks a poor experience for patients, and for clinical and operational teams.
We know that the rate of missed appointments varies within and between hospitals. The national rate is just above 7%, but it is over 9% for a quarter of hospitals and below 6% for another quarter. While the demographics of the population served will impact on the rate of missed appointments, there are evidence-based interventions that can improve the situation.
Understanding and addressing the causes of missed appointments and short notice cancellations is key to delivering locally focused improvement. Some will be within the hospital’s direct control. For example, there is a strong correlation between the number of times a hospital changes a patient’s appointment and the likelihood the patient will miss their appointment.
Communicating with and giving people control of their appointments reduces the number of missed appointments. The recent roll out of patient portals nationally, accessible through the NHS App, is key to achieve this. Refer to the principles for delivering personalised, patient-centred communications to patients who are waiting for planned care.
We also know there is predictability in the people most likely to miss an appointment. Several organisations have used technology, including artificial intelligence, to predict and mitigate the risk of missed appointments or short notice cancellations to good effect.
How to reduce wasted appointments
Value opportunity
If every hospital reduces the number of missed appointments by 1 percentage point through the second half of 2024/25, the NHS would be able to see an additional 120,000 patients this financial year. For an average sized hospital a 1 percentage point reduction equates to 7,500 fewer missed appointments a year.
Tracking indicators
In addition to local process measures linked to your change ideas, there are process measures in the improvement analytics for the percentage of missed appointments by specialty, type and relative level of deprivation of the area in which the patient lives.
Change ideas
- Send appointment reminders – and where possible do so using the NHS App to minimise costs. Patients are over twice as likely to cancel appointments ahead of time, rather than miss their appointment, if they receive a For those who cancel, half do so within 2 days of being sent a reminder, so the timing of reminders (>4 days) needs to anticipate when services will learn that a patient wishes to cancel and if they do, give sufficient time to allow the appointment slot to be reused. Keep a list of patients who can attend at short notice to fill last minute cancellations.
- In addition pre-appointment questionnaires could be sent to confirm patients still want/need the appointment in the weeks prior (clinical and admin appt validation), or to request they attend a diagnostic test prior to their appointment.
- We know a small percentage of patients (~5%), typically those on multiple concurrent pathways, account for almost a quarter of all missed appointments. Ensure you understand and identify how to make care more co-ordinated and appointments more convenient for patients, including by minimising their number. This might be achieved using remote consultations, remote monitoring and PIFU.
- The causes of and solutions to reducing the number of children not brought to appointments are slightly different. The ’further faster’ guide has more detail on reducing the incidence of ‘was not brought’ for children.
- Ensure national referral to treatment rules are applied if patients miss appointments – do not simply continue to send further appointments to people who miss appointments.
- Increase the number of clinic appointments that patients can manage themselves using a patient portal and NHS App appointment management functionality. There is a system target in the Operational planning guidance of at least 70% of elective appointments available in the NHS App by March 2026. Refer to the guidance on NHS Wayfinder services.
- Review which clinics the hospital regularly cancels.
- Undertake administrative validation for 90% of patients waiting over 12 weeks (and every 3 months thereafter) using WLV tools, patient portals and the NHS App for appointment messaging.
- To ensure patients are aware of what is needed from them and that they are prepared for their appointment, provision of pre-appointment information could be enabled via the patient portal and NHS App. For example, fasting, appropriate support, someone to collect them afterwards.
- In addition, sending pre-appointment questionnaires that allow clinic pre-assessment and other questions to be completed ahead of an appt, saving in clinic time, and ensuring the patient is ready for their appointment.
- Sending reminders about their appointment, letters, supporting information, questionnaires in the NHS App and/or portal to ensure the patient turns up on time in the right place for their appointment. Consider using the nationally procured NHS Federated Data Platform care co-ordination solution (using AI to predict missed appointments and short notice cancellations).
Resources
- improvement analytics
- reducing did not attends (DNAs) in outpatient services guidance
- specialty-level guidance
For help and support: england.outpatient-transformation@nhs.net
Right people
Utilising your workforce more effectively through high quality operational workforce planning and deployment will help improve staff experience and retention, support service improvement and further improve productivity by optimising the skills and capacity of your workforce.
Optimising the valuable skills and capacity of clinical workforces
Good quality workforce planning and deployment is about optimising the valuable skills and capacity of our clinical workforce, by ensuring the right people are in the right place, at the right time to deliver high quality, efficient patient care. It is about supporting the development of staff and services and providing the visibility of clinical capacity required to plan services effectively and match valuable clinical capacity to patient need.
Improvement requires targeted action on workforce planning and transformation, workforce deployment, governance and measurement.
Follow the resources on clinical workforce productivity on FutureNHS. In particular, we recommend the following resources for each of the 3 pillars of excellence, which are workforce planning and deployment; workforce transformation; and governance and measurement.
Workforce planning and deployment
Workforce planning and deployment resources
- e-job planning and e-rostering for effective planning and deployment of all staff:
- the Advancing levels of attainment handbook and related resources: help organisations establish what their e-rostering and e-job planning levels of attainment are and what is required at each level to progress, based on local need and current position
- the e-job planning toolkit and e-rostering toolkit: provide a step-by-step guide to optimising system usage and embedding effective associated processes and governance
- e-rostering as an enabler to flexible working: provides resources to support team leaders working in clinical areas to develop ways to roster their staff more flexibly, thereby improving work-life balance and experience at work for staff. The case studies showcase the innovative initiatives that are being implemented and their impacts on staff wellbeing and retention
- medical consultant job planning improvement guide
- demand and capacity planning: provides resources to support service and system-level demand and capacity planning, including modelling tools and approaches, case studies, webinars and e-learning
- digital staff passport: enables NHS employees to use their smart phone to share employment, education and training, and occupational health details with hospitals 24/7, to support their moves between those hospitals
- agency toolkit: supports organisations to reduce their agency staff bills and encourage workers back into substantive and bank roles
Retention resources
- improving staff retention guide: supports line managers and employers to consider the key areas that affect workforce retention
- international retention toolkit: actions employers can take, such as mapping skillset and qualifications and setting up pastoral support, to ensure internationally recruited staff will want to stay, thrive and build lasting careers in the NHS
- NHS Emeritus: an initiative that connects recently retired and peri-retired clinicians across England with NHS providers of acute care who need the help only experienced clinicians can offer
Workforce transformation
Workforce transformation resources
- Clinically-Led Workforce and Activity Redesign (CLEAR) programme: supports clinicians and organisations to deliver transformation and workforce redesign projects to enhance patient care, by equipping frontline staff with skills in data analysis, innovation and leadership
- Star: accelerating workforce redesign: a model and workshop for workforce transformation, enabling you to explore workforce challenges, develop bespoke action plans and use resources in the Star online directory
- roles explorer: provides resources for workforce redesign, such as introducing new roles or innovative adaptations to existing roles within a service or system
- Calderdale Framework: an evidence-based workforce transformation tool used in acute and community settings to rapidly identify skill sets required by services and their populations in acute, sub-acute and rehabilitation phases
- workforce transformation case studies: an interactive map of good workforce transformation practice, including examples from diagnostics and outpatients
Governance and measurement
Governance resources
- National Quality Board (NQB): safe sustainable and productive staffing guidance (2016): an improvement resource that builds on the NQB’s 2013 expectations and framework within which organisations and staff should make decisions about staffing that optimise productivity and efficiency while maintaining focus on improving quality
- e-rostering and e-job planning meaningful use standards: support hospitals to implement and use e-job planning and e-rostering software to its full potential, which includes the use of board reporting and metrics for improvement
Measurement resources
- Model Health System: data-driven improvement tool that enables NHS health systems and hospitals to benchmark quality and productivity
- Workforce Productivity Diagnostic Tool: supporting systems and hospitals to understand and benchmark their workforce productivity
Change ideas
- Collect workforce data to understand your workforce capacity:
- capture and review data for all staff who work in outpatients on a permanent or temporary basis. Include data from/on ESR, temporary spend, recharge, recruitment and retention rates, turnover, sickness absence, age profile and demographics
- review your consultant-level capacity (including direct clinical care and supporting professional activity time)
- Understand your retrospective and prospective activity:
- collect activity data and review any service plans that may impact on future activity levels (such as work transferring from location or changes in mode of delivery)
- this review should include key hours of operation
- Undertake a systematic review of your workforce requirements:
- map your pathway and consider which staff are required at each stage
- review the roles, skills and capacity required to meet your expected activity. Consider whether any new roles are required or would improve productivity
- review your pay spend run rates and compare these to your budget
- consider recruitment, training and retention needs, including specific equipment/ specialty training requirements
- Review national policy when building your establishment and optimising deployment:
- Developing workforce safeguards: Supporting providers to deliver high quality care through safe and effective staffing
- GIRFT guidance
- appropriate Royal College guidance
Digital enablers of improvement
Three digital initiatives will be the focus for enabling improvements: the NHS App, the Federated Data Platform and the electronic referral service (e-RS).
The NHS App is becoming the single, comprehensive and trusted digital front door to care for patients. With 36 million registered users and 85% of acute hospitals connected by March 2025, the NHS App will improve communication and shared decision-making between patients and clinicians.
The majority of outpatient elective care appointments should be available for people to view and manage through the NHS App in the coming year. Trusts should also adopt digital patient engagement portals (PEPs). These enable patients and their healthcare team to send messages and share documents, and for the NHS App to host patient questionnaires to help validate waiting lists, monitor patients remotely and gather information before an appointment. Providers need to make these digital tools available to all clinical teams within their organisations, along with the appropriate support to adopt and embed them in clinical and administrative workflows.
Patient engagement portals (PEPs) and the NHS App allow providers to provide high-response digital channels as part of admin/clinical/patient pathways to support:
- wait list validation post referral/pre-appointment (to reduce missed appointments, manage wait list)
- waiting well information for patients to look after themselves post referral and whilst waiting for an appointment
- view/manage/cancel appointment (to reduce missed appointments)
- provide patients with important “push” messages (NHS App and/or SMS)_about their appointment/treatment
- provide appointment letters and important pre-appointment supporting information (arrive on time, right place, prepared)
- request pre-appointment information from patients (arrive prepared/reduce pre-appointment clinic admin in hospital)
- provide important pre-treatment letters and supporting information (arrive on time, right place, prepared)
- request pre-treatment information from patients (arrive prepared/reduce pre-treatment clinic admin in hospital)
- support clinical/diagnostic remote monitoring and/or provide channels for patient initiated follow-up (PIFU) post treatment
- provide access to past appointments and associated data.
For any queries on the NHS App for secondary care appointment management please contact: wayfinder.comms@nhs.net , in addition please find the link for the NHS Futures site here: Wayfinder: Referrals and Appointments in the NHS App – FutureNHS Collaboration Platform
The NHS Federated Data Platform (NHS FDP) aims to enhance patient care and increase efficiency. It securely connects data, breaks down information silos, and provides insights to assist in decision-making, reduce costs, and improve patient outcomes. Staff can access the information they need in one safe and secure environment and use it to improve how they work and deliver care for patients. The NHS FDP is available for all trusts in England and is centrally funded for at least 7 years. The platform is continuously evolving with a range of innovative products and enhanced capabilities being developed to support trusts to improve quality and productivity. These will be shared on the NHS FDP Solution Exchange as they become available.
The Outpatients Care Coordination Solution is a live NHS FDP product available to all trusts now. It provides waiting list validation and data quality to teams tackling outpatient backlogs. The product flags entries in the waitlist for further investigation, based on an agreed set of criteria. This allows teams to identify which patient entries no longer need to be included, for example if the patient is deceased or there is a duplicate entry. These waiting list entries can then be safely removed from the waiting list by clinicians, ensuring that the correct patients are listed and then receive the necessary care and attention. The 14 trusts using this product, have so far in total safely requested 205,539 patients for removal from the waitlist.
To learn more about the NHS FDP products or to arrange a product demo, please contact: england.fdp@nhs.net.
NHS e-RS is a national digital platform for referring patients from primary care into elective care services and is a significant enabler of patient choice, advice and guidance. It supports effective joint clinical decision making, improving the quality of information shared between primary and secondary care through standardised referral guidelines. For further enquiries about the NHS e-RS service please contact: enquiries.ers@nhs.net
Please share your ideas and feedback with us
Thank you for engaging with this guide.
Please share your ideas and feedback with us. There are 2 ways you can do this:
- by emailing england.improvementdelivery@nhs.net
- by feeding back through your local Learning and Improvement Network. Details on the networks are on the FutureNHS platform
PRN01435_i

