Chief executive’s overview
Welcome to NHS England’s Annual Report and Accounts for 2022/23.
This report covers the performance of the organisation between April 2022 and the end of March 2023, including from 1 July 2022 onwards the legally merged constituent organisations of NHS Improvement and from 1 February 2023 onward the legally merged organisation NHS Digital.
This ongoing merger had, by April 2023, successfully integrated NHS Improvement, Health Education England, and NHS Digital into one unified organisation. The new NHS England has a shared purpose, leading the NHS in England to deliver high-quality services for all, and putting workforce, data, digital and technology at the heart of our plans to transform the NHS.
In 2022/23, and since, the NHS has continued to face considerable challenges. In addition to the continued challenge of recovery from the first waves of Covid-19 and ongoing global economic volatility, last year saw the start of unprecedented operational and financial impact from industrial action.
Throughout the now several periods of action, we have done everything in our power to support front line staff and local leaders to ensure those needing life-saving care have continued to be able to receive it. However, each strike comes at a significant cost to the NHS – both in terms of resources and in momentum on our key recovery programmes – and this is ultimately borne by patients. We have therefore been steadfast in our calls on both Government and staff unions to engage in meaningful discussions which avoid further strikes.
Despite these strong headwinds, the NHS has delivered on many of our ambitions. We virtually eliminated two-year waits for routine hospital care by the end of July, and then achieved a vast reduction in those waiting 18 months or more by the end of March 2023.
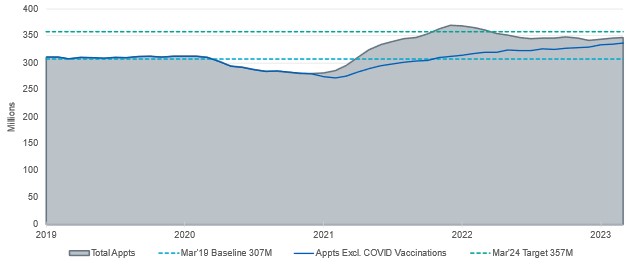
GP practices delivered 337 million appointments, on top of COVID-19 vaccinations, supported by a growing workforce able to offer more services closer to patients’ homes.
We have provided mental health support to ever more people, including fast-tracking the roll out of mental health teams in schools, and continued progress on expanding and improving support in the community for people with a learning disability and autistic people.
Record numbers of people have been checked for cancer symptoms, recovering the deficit caused by the pandemic and meaning that more people than ever before are getting diagnosed at an early stage, improving the chances of effective treatment.
We’ve achieved our NHS Long Term commitment to treat 1,000 children a year for severe complications related to their obesity.
And together, we have also shown the NHS remains at the forefront of innovation, with the introduction of several new cutting edge treatments, including the first new treatment for mesothelioma in over a decade and gene therapies for children born with ultra-rare conditions, the expansion of routine genomic testing for children seriously ill in hospital, and continued progress on frontline digitisation and the safe use of data to support better care planning and delivery.
These are just a few examples of the progress made over 2022/23 thanks to robust planning and the incredible commitment to patient care shown by NHS teams up and down the country – many more are set out in the pages that follow.
The start of 2023 marked the beginning of the health service’s 75th year. And while we cannot, and do not, ignore the fact that in too many cases patients are not currently receiving the high quality and timely care we all aspire to, it is simultaneously true that the public retain belief in the NHS, its founding principles, and those who work within, and in support of, their local services.
We don’t take that faith for granted, just as we don’t take for granted the contribution made by each and every member of staff who works every day to live up to it.
I would therefore like to take this opportunity to thank staff for their ongoing hard work and continued commitment to patients and their colleagues, during what continues to be a period of significant challenge and change.
Amanda Pritchard, NHS England Chief Executive and Accounting Officer.
Performance overview
This performance overview provides a brief summary of NHS England and its objectives, along with progress made in health inequalities and prevention of ill-health, access and outcomes, recovery of services and using taxpayers’ investment to maximum effect. Together, our work programmes encapsulate the objectives set out in the government’s mandate to the NHS for 2022/23.
About NHS England
NHS England was established by Parliament in 2012 as an independent statutory body. Its role is to lead the NHS in England to deliver high quality services for all.
NHS England shares with the Secretary of State for Health and Social Care the legal duty to promote a comprehensive health service in England, in accordance with the National Health Service Act 2006 (as amended by the Health and Social Care Act 2012 and most recently the Health and Care Act 2022). We set the national direction, allocate resources, ensure accountability, define the national strategy for supporting and developing people, mobilise expert networks, give support to drive improvement, deliver essential services including national procurement and digital services, and lead the national agenda for transformation.
Supply Chain Coordination Limited (SCCL) transferred into NHS England on 1 October 2021. 2022/23 is the first full year SCCL is part of NHS England.
On 1 July 2022, NHS England merged with NHS Improvement when the Health and Care Act 2022 became law. NHS Improvement’s constituent bodies, NHS Trust Development Authority (NHS TDA) and Monitor, were abolished and its staff, functions and resources transferred to NHS England.
On 1 February 2023, NHS England and NHS Digital legally merged. NHS England then became the custodian of national health and social care datasets and the single executive non-departmental public body with responsibility for digital technology, data and health service delivery in the NHS.
On 1 April 2023, NHS England incorporated Health Education England, the body responsible for the education and training of the health workforce.
Through ongoing delivery of the NHS Long Term Plan, we promote high quality health, care and support NHS organisations to work in partnership to deliver better outcomes for our patients and communities, at the best possible value for taxpayers.
How we operate
NHS England is governed by a Board which provides strategic leadership and accountability to the government, Parliament and the public. The Board is supported by committees which undertake detailed scrutiny in their respective areas of responsibility and provide it with regular reporting and formal assurance.
NHS England works closely with other partners at national and regional level to ensure services are safe, effective, and clinically and financially sustainable.
Our work is also supported by third party organisations including NHS Business Services Authority (NHS BSA), NHS Shared Business Services, NHS Property Services Limited (NHS PS) and Primary Care Support England (PCSE) provided by Capita. Additionally, NHS England hosts NHS Interim Management and Support and sponsors the Sustainability Unit on behalf of the NHS.
NHS England also oversees commissioning support units (CSUs). The CSU staff group are employed by NHS BSA but are formally a part of NHS England. CSU activities are included in our report and accounts except where otherwise indicated. Details on how we assure the activity of our organisation is presented in this annual report.
Services are commissioned by integrated care boards (ICBs), which replaced clinical commissioning croups (CCGs), and are overseen by NHS England on a regional and national basis. ICBs lead 42 local ICSs, which were fully established across England on a statutory basis on 1 July 2022. These are made up of NHS organisations, primary care professionals, local councils, social care providers and the community, voluntary and social enterprise sector. Our 7 regional teams support ICSs to improve the health of the population, improve the quality of care, tackle inequalities and deliver care more efficiently.
How we measure performance
The NHS Constitution sets out the rights of patients, the public and staff. We measure and monitor performance against a wide range of constitutional performance standards and publish statistics relating to these core constitutional standards on the NHS England website every month.
Performance of integrated care boards (ICBs)
Under the terms of the NHS Act 2006 (as amended), NHS England has a duty to undertake a performance assessment of each ICB with respect to each financial year. NHS England has completed its first annual assessments for 2022/23 based on an approach developed with ICBs.
The assessments specifically considered how effectively each ICB had led its system and its contribution to each of the 4 fundamental purposes of an ICS, highlighting areas of good practice as well as opportunities for improvement. The outcome of each assessment was set out in a letter from the relevant NHS England Regional Director to the ICB Chair in response to the ICB’s first annual report and accounts.
Overall, the assessments show that ICBs have made strong progress in their first year of operation to develop as new organisations and build on existing partnership arrangements, including the development of the 5-year joint forward plans.
Feedback from health and wellbeing boards considered as part of the assessment highlighted how ICBs have worked with partners to make progress on delivering the priorities set out in joint local health and wellbeing strategies. NHS England will continue to work alongside ICBs and the Care Quality Commission to evolve the approach to annual assessment for future years.
NHS England has the option of using its statutory powers, including the power to issue directions where an ICB is failing or is at risk of failing to discharge any of its duties, conferred by section 14Z61 of the National Health Service Act 2006 (as amended). There was no recorded use of these powers during 2022/23.
Overview of 2022/23 operational performance
NHS England started out 2022/2023 with significant system pressures remaining from the tail end of the COVID-19 Omicron wave, with 15k hospital beds occupied by patients with the virus and a Level 4 National Incident in effect. Resources were therefore directed at wider NHS recovery.
The 2022/23 operational planning guidance outlined 10 clear priorities to drive recovery and improvements across the year. These were:
- Invest in our workforce.
- Respond to COVID-19 ever more effectively.
- Deliver significantly more elective care to tackle the elective backlog, reduce long waits and improve performance against cancer waiting times standards.
- Improve the responsiveness of urgent and emergency care (UEC) and build community care capacity.
- Improve timely access to primary care.
- Improve mental health services and services for people with a learning disability and/or autistic people.
- Continue to develop our approach to population health management, prevent ill-health and address health inequalities.
- Exploit the potential of digital technologies to transform the delivery of care and patient outcomes.
- Make the most effective use of our resources.
- Establish ICBs and collaborative system working.
Over the course of 2022/23 we made significant progress against these areas, achieving some of the commitments made in the NHS Long Term Plan since its publication, while delivering a record number of patient contacts. We:
- delivered the target of all integrated care systems (ICSs) operating 2-hour community crisis response services in April 2022, ahead of the target date of March 2024
- delivered and exceeded the targets for patients receiving personalised care interventions, with almost 6 million recorded interventions by the end of 2022/23, against a target of 2.5 million by March 2024
- reached 1.72 million referrals to social prescribing schemes reached 1.72 million in 2022/23, against the a target of 900k by March 2024
- achieved the NHS Long Term Plan commitment of 1,000 children treated each year for severe complications related to their obesity in February 2023, a month earlier than the target date of March 2023
- achieved and exceeded the commitment of 26,000 Additional Roles Reimbursement Scheme posts in March 2023, a year earlier than the target date of March 2024, boosting capacity in primary care.
In December 2022, there were 2.3 million A&E attendances, the highest on record.
This was due to the combined impact of COVID-19, influenza and Group A Streptococcus, known as Strep A.
Ambulance services also saw unprecedented demand throughout 2022/23, with the number of the most serious ambulance callouts (category 1) up by one third on pre-pandemic levels at some points in the year.
NHS acute hospitals admitted 275,977 people with COVID-19 over the course of the year, with an average of 5,811 beds per day occupied by patients with COVID-19.
In primary care, 347.4 million appointments were delivered by General Practice teams during 2022/23, exceeding pre-pandemic levels even when excluding the 10.5 million appointments relating to COVID-19 vaccinations.
A record 2,878,267 people were seen following an urgent suspected cancer referral – 21% above pre-pandemic levels.
From December 2022 onwards, local services were impacted by industrial disputes between the Government and unions representing multiple professions (including ambulance workers, nurses, radiographers, and junior doctors). The extensive planning and intensive management that the withdrawal of labour has necessitated – focused on maintaining the safest possible care for patients requiring urgent and emergency care as well as planned treatment for time-sensitive conditions – has inevitably impacted on the ability of systems and providers to recover and improve services.
To address some of the larger challenges, NHS England published further delivery plans in quarter 4 2022/23, including:
- The ‘Delivery plan for recovering urgent and emergency care’ in January 2023, a two-year plan focused on 2 key ambitions: to achieve A&E 4-hour performance of 76% by March 2024 and improve category 2 ambulance response times to an average of 30 minutes over the next year
- the 3-year delivery plan for maternity and neonatal services in March 2023, which set out how we will make care safer, more personalised, and more equitable.
These plans sit alongside the ‘Delivery plan for tackling the COVID-19 backlog of elective care’, published in February 2022.
Performance analysis
Delegation of commissioning to ICBs
Since 1 July 2022 all 42 ICBs have had delegated responsibility for commissioning primary medical services, with 9 ICBs also taking on one or more of: dental (primary, secondary and community), general ophthalmic services and pharmaceutical services. All remaining ICBs were assigned delegated responsibility for all 4 primary care services from April 2023.
Primary and community health services
General practice
General Practice continues to demonstrate increased activity with 347.4 million appointments in the 12 months to the end of March 2023, including 10.5 million COVID-19 vaccinations. This is 13% above the March 2019 baseline. The March 2024 target of an additional 50 million appointments was met in October 2023.
Appointments in general practice
In May 2022, the Fuller stocktake report set out what is working well and how we can accelerate the implementation of integrated primary care. All ICB chief executive officers co-signed a letter committing to deliver this vision of streamlined access to urgent care, with continuity for those who would benefit the most, and a more proactive role in creating healthy communities.
In September 2022, we set out actions to boost capacity ahead of winter 2022/23.
ICBs rapidly repurposed £37 million of the Investment and Impact Fund to expand clinical capacity. 351 acute respiratory infection hubs were established over winter, delivering more than 200,000 appointments.
From 1 October 2022, primary care networks (PCNs) were required to provide a standardised service offer to patients, through the Network Contract Directed Enhanced Service, ensuring 6:30pm to 8pm evening appointments Monday to Friday and 9am to 5pm appointments on Saturday in all networks.
In 2022/23, the accelerated improvement programme supported 724 GP practices to address their immediate access pressures. As a result, 88% of practices reported a productivity gain and 99% of practice staff reported they felt better equipped to deal with their work challenges.
Primary care workforce
The wider workforce numbers continued to rise with more than 29,103 whole time equivalent (WTE) additional staff in place and an additional 1,903 WTE doctors in general practice at the end of March 2023 compared to the March 2019 baseline. This has achieved and exceeded the Additional Roles Reimbursement Scheme government commitment to deliver 26,000 additional roles in primary care by March 2024, however retention of the qualified GP workforce remains a significant issue.
Doctors in general practice
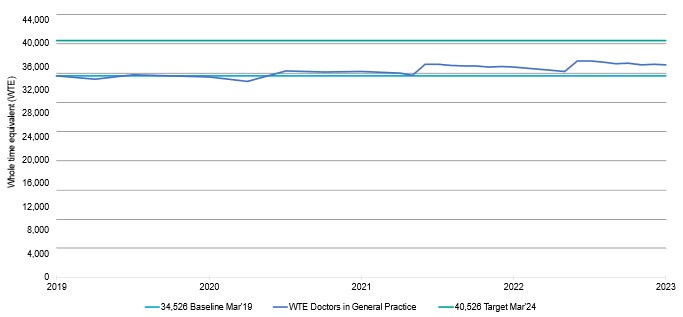
Targeted efforts are in place to retain GPs in the workforce, including working with systems to communicate and adopt the enhanced package of GP retention initiatives in ‘Investment and evolution: updates to the GP Contract 2020/21 to 2023/24’.
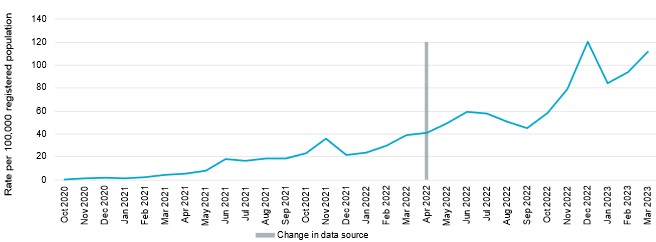
Community pharmacy
The Community Pharmacist Consultation Service (CPCS) continued to grow. During 2022/23, 2.8 million consultations were delivered in community pharmacies as part of the New Medicine Service. This included significant increases in referrals from 111 and GPs.
Completed GP referrals to CPCS per 100,000 registered population
Other key achievements include the delivery across England of:
- a community pharmacy hypertension case-finding service with a million clinical blood pressure checks and 55,000 ambulatory blood pressure checks delivered by community pharmacies in the reporting period
- a smoking cessation service for patients recently discharged from acute NHS trusts. Implementation is planned to be completed across England by the end of March 2024 as hospital smoking cessation services mobilise. Almost 4,000 community pharmacies have signed up to deliver this service to the end of March 2023
Dentistry and optometry
Primary care dental services continue to recover from the pandemic following the lifting of infection prevention control constraints in July 2022, with 78% of contracted units of dental activity delivered in 2022/23. However, approximately 101% of contracted units of dental activity were delivered in March 2023, marking an improvement in performance.
In July 2022, we announced the first dental contract amendments since 2006 to improve care for higher-needs patients and improve overall access.
Optometry services exceeded pre-COVID-19 activity levels in high street practices.
The special schools eye care service proof of concept began in May 2021 to provide sight tests to children with a learning disability and/or autism in a special educational setting. As of 28 February 2023, more than 11,000 sight tests had been undertaken and 4,700 spectacles had been dispensed.
Personalised care
We have already achieved more than double our commitment in the NHS Long Term Plan to 2.5 million people receiving personalised care, a year ahead of the target. More than 6 million people have benefitted from a personalised care intervention during the reporting period, giving patients more control of their care and alleviating pressure on GPs.
Urgent community response
Urgent community response (UCR) teams continued to provide urgent care to people in their homes, avoiding hospital admission. More than 80% of patients were seen within 2 hours of referral to UCR in January 2023, exceeding the national expectation of 70%. 88% of ICBs accepted falls referrals as part of their UCR provision from 8am to 8pm, 7 days a week, as a minimum, by February 2023.
Virtual wards
Significant progress was made in developing digitally enabled virtual wards (also known as ‘Hospital at Home’), where the number of virtual ward beds increased from 4,845 (May 2022) to 8,241 (March 2023). More than 100,000 patients were treated in a virtual ward in the reporting period.
Urgent and emergency care
Average daily A&E attendances for 2022/23 were close to 69,500 (66,800 in 2021/22), an increase of 4% against the previous year. In March 2023, 71.5% of patients were admitted, transferred or discharged from A&E within 4 hours of arrival.
Admissions to hospital through the emergency department had however decreased over the same period, averaging 4% lower compared to 2021/22. Despite this, and increases in bed numbers, bed occupancy continued to rise averaging at 93.6% across the year.
To support reducing hospital occupancy rates, we increased bed capacity by the equivalent of more than 7,000 additional general and acute beds in 2022/23, as well as through the expansion of same day emergency care and urgent treatment centres.
As part of the plan to increase resilience over winter 2023/24, system control centres were set up across all 42 ICSs. These centres operate 24/7 and are staffed with senior clinical decision makers and operational teams with expertise in dealing with capacity and demand across both primary and secondary care.
NHS 111
NHS 111 received 22.3 million calls in 2022/23 with an exceptional level of calls during December 2022 due to winter pressures, including widespread public concern about Strep A infections. The number of NHS 111 call handlers increased by 12.4% by March 2023, compared to September 2021. In terms of 111 online services, digital uptake (the percentage of online completed sessions as a proportion of total activity, including calls and online pathways) during 2022/23 was typically just under 30%. This rose to approximately 40% in December 2023, equating to just over 1.1 million completed online sessions.
Ambulance services
By the end of March 2023, we had increased the number of 999 call handlers by 15% compared to September 2021. The total of 2,376 WTE is marginally short of the 2,500 target, however the average call answer times fell to their lowest in January 2023, before increasing slightly in February and March as demand increased.
The ambulance service responded to 18% more category 1 incidents in December 2022 compared to the previous high in July 2022 and, by March 2023, performance was 8 minutes and 49 seconds. Category 2 incidents decreased by 10% in December 2022 against the same point in the previous year. However, ambulance services continued to be challenged by long handover delays that impacted the flow of patients through hospitals and response times increased to 39.3 minutes in March 2023.
In November 2022, 2 ambulance trusts trialled an intelligent digital call-routing system to reduce long waits for calls. Following a successful trial providing category 2 calls with additional clinical input in order to prioritise those calls most in need of an ambulance, this is now being rolled out to all ambulance trusts.
In January 2023, we published the UEC services recovery plan which outlined the steps we will take to ensure patients are seen in emergency departments, and that ambulances get to patients quicker.
Elective care
In February 2022, the delivery plan for tackling the COVID-19 related backlog of elective care set out clear ambitions for the next 3 years. This remains the blueprint for elective delivery.
The initial focus was on patients who were waiting 2 years or more by the end of July, with the exception of those who chose to wait longer, did not want to travel to be seen faster, or for very complex cases requiring specialist treatment. More than 22,500 people who had been waiting 2 years or more at the start of the year, and a further 51,000 who would have exceeded a 2-year wait by the end of July, were treated. The NHS met this first target by virtually eliminating waits longer than 2 years for elective care by July 2022, despite higher levels of COVID-19, with hospitals treating more than 220,000 patients with the virus since the plan was published.
The next milestone was to virtually eliminate waits of more than 18 months by the end of 2022/23 (with the exception of patients who chose to wait longer and a very small number of highly specialised areas). As of 31 March 2023, this figure was 10,718, down from a peak of 63,777 in April 2022.
While reducing the number of people waiting a very long time for treatment was the focus, the plan was clear that the total waiting list was likely to keep growing. In 31 March 2023, there were 7.3 million incomplete referral to treatment pathways (up from 6.4 million in March 2022).
Targeted Investment Fund (TIF)
This was the first year of the £1.5 billion TIF2 capital funding agreed at Spending Review 2021, ringfenced to increase elective activity. For 2022/23, £537.3 million had been drawn down against an allocation of £600 million, supporting a total of 85 schemes. We will be commencing an evaluation of the TIF schemes in 2023/24.
Mental health
The mental health programme is on track to invest an additional £2.3 billion a year in expanding services by the end of 2023/24, and there has been sustained growth in workforce and activity.
An additional 207,542 children and young people aged up to 17 received at least one contact from an NHS-funded mental health service in the 12 months up to March 2023. The programme is on course to achieve the overall access ambition to support an additional 345,000 people aged up to 25 by the end of 2023/24.
By the end of 2023, 35% of the school-age population were covered by 398 operational Mental Health Support Teams, meeting our Long Term Plan ambition a year earlier than planned.
The Early Intervention in Psychosis standard, requiring more than 60% of people who experience a first episode of psychosis begin treatment with an evidence-based care package within 2 weeks of referral, continued to be achieved in 2022/23.
Children and Young People (CYP) community eating disorder services are treating 55% more children and young people since the start of the pandemic, which is in turn affecting waiting-time standards. As of March 2023, 82.5% of routine CYP eating disorder referrals were seen within 4 weeks and 78.7% of urgent referrals were seen within 1 week, compared to a standard of 95%.
NHS Talking Therapies referral to treatment time target and the recovery standards continued to be met and, in quarter 4 of 2022/23, 320,254 people accessed services.
The new integrated model of primary and community mental health care supports adults and older adults with severe mental illnesses to access mental healthcare. In 2022/23, a record 313,022 people within this demographic received all 6 elements of the physical health checks, against an ambitious target of 346,000.
The urgent and emergency mental health pathway continues to be under significant pressure, experiencing exceptionally high bed occupancy of 95% to 97% since May 2022. According to quarter 4 2022/23 data, inappropriate out-of-area placements, which are driven by capacity limitations, totalled 58,515 days.
The estimated dementia diagnosis rate was 63% as of March 2023, against the national ambition of 66.7%. We are funding an evidence-based improvement project for 2 trusts in each region to pilot the ‘diagnosing advanced dementia mandate tool’ to improve the diagnosis of dementia in care homes.
People with a learning disability and autistic people
The number of people with a learning disability and autistic people in a mental health inpatient setting continued to reduce. During 2022/23, 1,229 adults were discharged from hospital, 444 (36%) of which had been in hospital for more than 1 year, and 147 (12%) had been in hospital for more than 5 years. The inpatient total at the end of July 2023 represented a 30% net reduction since March 2015 but there is further to go to reach the NHS Long Term Plan target.
We supported PCNs to deliver learning disability annual heath checks (AHCs). Between April 2022 and March 2023, 78.1% of people aged 14 and over on a GP learning disability register had received an AHC, meaning that we met our commitment to reaching 75% by March 2024 a year earlier than planned.
Our Learning from the Lives and Deaths of People with a Learning Disability and Autistic People programme continued to review the care of people with a learning disability and autistic people who died. Drawing from the learnings from this programme and to support improvements in care and outcomes, we have published an acute care toolkit, British Thoracic Society clinical statements on aspiration pneumonia community acquired pneumonia and a RightCare scenario on aspiration pneumonia, and Restore2 mini training via Skills for Care.
Health inequalities and prevention of ill-health
The NHS Prevention Programme delivers targeted work to tackle risk factors and their underlying causes, subsequently helping to reduce health disparities and narrow inequalities.
Since its launch in June 2021 more than 200,000 people have been referred to the NHS Digital Weight Management Programme.
By the end of 2022/23, more than a third of all inpatient trusts and around two-thirds of all maternity trusts had actively implemented new tobacco dependence treatment services. Additionally, 32 Alcohol Care Teams were optimally established in areas of the highest alcohol related harm and deprivation.
NHS Diabetes Prevention Programme
Referrals to the NHS Diabetes Prevention Programme have recovered to pre-pandemic levels. More than 1.2 million referrals have now been made into the programme, with just under 600,000 people joining. An independent evaluation has shown a 37% relative reduction in incidence of those who complete the programme and a 7% reduction in population-level incidence of type 2 diabetes. The latest independent analysis published in February 2023 showed the risk of developing type 2 diabetes is 20% lower for those referred, even if they do not complete the programme.
Non-cancer adult and young person screening
Following the pandemic, all 38 services providing the NHS abdominal aortic aneurysm screening programme to men aged 65 years or older, were restored. At quarter 4, annual surveillance (92.3%) was above efficiency threshold of 85% and both below optimal standards of 85% and 95%, respectively. Coverage for men on quarterly surveillance is 93.1%, which is also above the efficiency standard of 85%, however coverage of initial screen (72.8%) was below efficiency threshold of 75%.
The NHS diabetic eye screening programme was fully restored by September 2022, and its routine appointment uptake levels continued to perform above the required standard (75%) at 79.1% in quarter 4 2022/23.
NHS vaccinations and public seasonal flu programmes
The UK remains a world leader in uptake across many vaccination programmes and in 2022/23, the NHS achieved the second highest flu vaccination rates on record with 21.2 million people taking up the offer. A major national communications and marketing campaign ran, with a key focus on those at highest risk of serious illness and communities with the lowest uptake.
Maternity and neonatal services
We published the 3-year delivery plan for maternity and neonatal services [1] in England on 30 March 2023. This includes learning from independent reports into maternity and neonatal services in Shrewsbury and Telford, and East Kent.
We aim to halve rates of stillbirth, neonatal death, maternal death and brain injury between 2010 and 2025. We made progress towards this ambition with the stillbirth and neonatal mortality rate in 2021 being 23% and 30% lower respectively compared with 2010.
Since March 2021, we have invested an additional £165 million recurrently in maternity and neonatal services. Our additional investment enabled a substantial increase in workforce establishment for midwives (over 2,000 WTE), obstetricians (over 400 WTE), maternity support workers (340 WTE) and neonatal nurses (550 WTE).
We have continued to expand and embed specialist community perinatal mental health services; 36 maternal mental health services were established for women who experience moderate to severe or complex mental health issues directly related to a trauma or loss. Work is ongoing to ensure one is established in each of the 6 remaining ICSs.
We continued working with trusts to implement all elements of the Saving Babies’ Lives care bundle, version 2.[2] We have developed version 3 of the care bundle[3], which will roll out across all trusts in 2023/24, including the new Element 6 on managing diabetes in pregnancy.
NHS antenatal and newborn (ANNB) screening programmes
Coverage for the 3 antenatal screening programmes remained above 99% and above 98% for newborn screening programmes within the target timescales. The NHS ANNB programmes continue to deliver 2 important in-service evaluations for the UK National Screening Committee: non-invasive prenatal testing rollout within the NHS Fetal Anomaly Screening Programme[4] and severe combined immuno-deficiency within the NHS newborn blood spot screening programme.[5]
Cancer and NHS cancer screening
Our public awareness campaigns and case-finding initiatives are making a difference. GPs are referring more people for urgent cancer checks than ever before – more than 200,000 every month – meaning we have eradicated the shortfall in cancer referrals that began in the early part of the pandemic. We are diagnosing a higher proportion of cancers earlier than ever before and the number of people starting treatment is higher than ever before.
We are investing more in expanding diagnostic and treatment capacity to meet the rising demand and working with the most challenged trusts, which is showing positive results.
The number of people waiting longer than 62 days for treatment to begin from the date of referral for suspected cancer has reduced significantly. By the end of March 2023 there were 14,700 fewer people waiting more than 62 days than during the peak in September 2022, when there were over 33,900 patients.
The NHS is focusing particular attention on resolving the more challenged pathways, including interventions such as tele-dermatology for skin cancer pathways, a £2 million investment in dermatoscopes and increased use of faecal immunochemical tests for bowel cancer. More than 5,400 patients have benefited from a colon capsule endoscopy ‘pill-cam’ in 53 pilot sites, and approximately 70% have not needed a colonoscopy.
We have a comprehensive, 6-pillar strategy to diagnose more cancer types earlier, including rare and less common cancers, and others that are not assigned a staging group in the conventional way (such as some blood cancers and brain cancers). Highlights of this strategy include:
- in April 2022, we expanded the Targeted Lung Health Check programme [6] to invite people from 20 more areas, reaching 43 areas in total. By the end of March 2023, the programme had invited more than 890,000 current or former smokers from some of the most disadvantaged areas in the country. More than 2,100 people were diagnosed with lung cancer – 76% of those at stage 1 or 2 – compared with the previous overall lung cancer early diagnosis rate of 28%
- in 2022/23, we launched Community Liver Health Checks in 12 areas. Between June 2022 and March 2023, the pilots delivered more than 11,000 fibroscans and identified more than 1,200 people at increased risk of liver cancer. The programme is actively reducing health inequalities by offering mobile services to those most at risk, including homeless people, people using drug and alcohol services and people with type 2 diabetes
- by Autumn 2022, the NHS-Galleri trial [7] successfully recruited 140,000 participants. The trial will assess the impact of offering a blood test to people without symptoms, with participants having 3 blood tests over 2 years
Cervical screening programme
2022/23 data [8] shows that for the higher age cohort, coverage is just marginally under the 75% efficiency standard at 74.9%. For the younger cohort aged 25 to 49 it remains lower at 66.4%.
Breast screening programme
The NHS breast screening programme continued to recover from the pandemic with a focus on removing the backlog in screening invitations and restoring the 3-year screening interval for the eligible population. Capacity was increased through additional evening and weekend appointments, building the workforce and investing in additional mobile breast screening units.
Bowel screening programme
The NHS bowel cancer screening programme exceeded the optimal coverage standard of 60%, with latest performance measured at 72.9% in March 2023. Eligibility was extended to include 56-year-olds in 2021/22 and 58-year-olds in 2022/23.
COVID-19 vaccination deployment
As of 31 March 2023, the NHS had administered more than 144 million COVID-19 vaccinations in England with around 4.5 million spring boosters. A major national campaign ran over autumn and winter alongside the annual flu campaign, offering protection to those at greater risk of severe illness and helping reduce hospital admissions.
Mpox vaccination deployment
In July 2022, the NHS began vaccinations against Mpox (previously known as monkeypox) to those at highest risk of exposure, following the World Health Organisation’s declaration of a public health emergency of international concern. Working with sexual health services and other partners in health systems, the NHS vaccinated more than 70% of those eligible by 31 March 2023, nearly 100,000 doses in total. [9]
In March 2023, UK Health Security Agency (UKHSA) confirmed that, due to the success of this vaccination programme, a sustained reduction in case numbers meant that Mpox vaccination work could end in summer 2023.
Workforce
In 2022/23, our focus was on restoring services to full capacity following the pandemic, alongside continuing to support the delivery of innovative new ways of working, as described in the 2022/23 operational planning guidance. [10] The planning guidance set out actions to increase workforce capacity and resilience to deliver safe and high-quality services that meet health and care needs.
Over the course of the year we engaged extensively with staff groups and others over the development of the NHS Long Term Workforce Plan, published in June 2023. However, ongoing actions continued alongside this policy development to support workforce growth, redesign, improved retention and improved productivity. Achievements included:
More people:
- the NHS Hospital and Community Health Service (HCHS) workforce was 1,280,350 WTE strong in March 2023, 4.4% (53,672) more than in March 2022.
- within this, the number of professionally qualified clinical staff was 671,943 WTE by March 2023, an increase of 3.7% (24,098) against March 2022.
- we have continued to support Trusts with overseas recruitment to address domestic labour supply shortages and vacancy rates. As part of this, 15,146 additional international nurses were recruited over the year, an increase of 19.6% on the previous reporting period.
Compassionate and inclusive culture
The Staff Survey was redesigned to align with the 7 elements of the People Promise, to improve how staff experience is monitored. 2022 data shows the staff engagement score has remained stable since 2021 (6.8), though it remains lower than before the pandemic in 2018-2020 (7.0). The morale score has declined for a second consecutive year and is now 0.3 points below its peak (6.1) in 2020.
More than 5,300 managers have attended the national health and wellbeing conversation training programme, and 195 of those will become trainers.
23 People Promise exemplar sites were implemented, improving staff experience and retention. Initial insights show 14 out of the 23 sites improved their quarterly staff engagement scores from quarter 1 to quarter 2 2022/23, with the overall cohort improving by 1.1% compared to a deterioration nationally of 0.3%. The retention rate is improving faster in the exemplar cohort than for the rest of the NHS.
96% of secondary care organisations had a wellbeing guardian in post as of December 2022, and our regional teams are working with the remaining 4% of organisations to support them in appointing wellbeing guardians.
Health and justice
We achieved 100% coverage across England of mental health treatment requirements for individuals whose offence crosses the community order sentencing range.
RECONNECT services continue to be opened, supporting those leaving prison and immigration removal centres. Over the course of the reporting period, we achieved 51.4% coverage in England and are on track to deliver 100% coverage by March 2024.
3 pilot sites for Enhanced RECONNECT have been mobilised to support high risk and highly complex individuals leaving custody.
We have mobilised 7 vanguards, 1 in each of our 7 regional teams, to implement the Framework for Integrated Care (Community).
We have delivered the Private Finance Initiative programme, which transferred the healthcare commissioning of 5 private prisons to NHS England. All prisons in England now have their healthcare commissioned by NHS England.
All service specifications for healthcare services in health and justice settings have been updated. This includes further reinforcing our commitment to ‘equivalence of care’ in the much revised Service Specification 29 for NHS Section 7A (s7a) public health services for children and adults in secure and detained settings in England.
Armed forces
Work has progressed on the commitments in the document, ‘Healthcare for the Armed Forces community: a forward view’ [11], which include:
- re-procurement of Op COURAGE [12]: the Veterans Mental Health and Wellbeing Service, underpinned by an enhanced service model for a fully integrated mental healthcare pathway across each of our regions. These improved service arrangements began on 1 April 2023, to facilitate increased access to a broader range of mental health and wellbeing services for individuals due to leave the armed forces, reservists and those who have already left the military
- commissioning a new non-clinical service to improve the identification and support of veterans pre- and post-prison custody. Informed by local services across several of our regions and a robust programme of engagement, Op NOVA [13] services began on 1 April 2023, providing a single point of contact for veterans, who, following an assessment, will have a comprehensive support plan developed for them that is overseen by a care and support coordinator
- implementation of the ICB-based single point of contact service for armed forces families and community. Over the last year, 7 pilots have been launched to test and inform a dedicated service that supports improved access to and continuity of care for this patient cohort that reflects the unique circumstances of military life and the impact on the wider family
- establishment of the national Serving and Ex-Serving Women’s Health Improvement Group with members from across government departments and the armed forces charity sector
- expansion of services and support for the armed forces community through the ongoing development of:
- fully functioning clinical pathways for the veterans’ trauma network
- military maternity care pathways
- improving access to sexual assault referral centres (SARCs) for serving personnel, underpinned by a pathfinder at Catterick Garrison in North Yorkshire
- the NHS England-commissioned Royal College of General Practitioners’ veteran-friendly practice accreditation programme, with 2,000 practices accredited in-year
- the NHS England-funded Veteran Covenant Healthcare Alliance, which has 140 accredited acute NHS trusts. Plans within the New Hospital Programme for a national rehabilitation centre have been approved and construction has commenced. Once opened the Centre will benefit veterans.
Digitising, connecting and transforming health and care
Our strategy for technology in health and care is to digitise, connect and transform. [14] With the legal merger of NHS Digital and NHS England on 1 February 2023, the new NHS England became one of the largest digital and tech organisations in the country. The Transformation Directorate plays a critical role in supporting the development and spread of digital innovation by developing and deploying national products and platforms, while running many live services.
In June 2022, the data saves lives strategy [15] set out future plans for data and building on the lessons learned from COVID-19 about the power of data. The plan for digital health and social care [16] set out a vision and plan for digitally transformed health and social care services and, in March 2023, the cyber security strategy for health and social care [17] set out the approach for the sector and its suppliers to achieve cyber resilience no later than 2030.
Electronic records and digital foundations
We are committed to NHS organisations having a core level of digital maturity – specifically an electronic patient records (EPR) system – by March 2025, and 80% of Care Quality Commission (CQC) registered adult social care providers having digital records by March 2024. By March 2023, 86% of trusts had EPR, this is expected to rise to 91% by December 2023. In adult social care, 52% of providers had a digital social care record by March 2023 (up from 41% in December 2021).
Understanding, protecting and improving the health of the population
A data platform enables NHS organisations to bring together operational data stored on separate systems. In January 2023, we began procuring a federated data platform so that every trust and ICS will have its own platform that can connect and collaborate with other data platforms.
We are trialling tools locally with promising results. An elective care co-ordination pilot in East Sussex removed 16% of its waiting list by identifying errors and was made live in 36 trusts by the end of March 2023. A discharge pilot helped North Tees reduce patients staying 21 days or more to 12% over a 12-month period (the national average is 20%). This was live in 16 trusts at the end of March 2023.
Planning, evaluating and improving the delivery of services
During 2022/23, we began work to develop cross-ICS bed management systems to improve the flow of patients through hospitals and across the healthcare system.
Data for research and development
In 2022/23, we invested over £13.5 million [18], as part of a funding package of over £100 million, to catalyse the development of interoperable and multi-model sub-national secure data environments. Secure data environments will enable more rapid and efficient health research and innovation, and are designed to provide secure, transparent data access for approved researchers, without that data leaving NHS secured databases.
NHS App
The NHS App and NHS.UK was established as a digital ‘front door’ to the NHS, enabling more people to participate more in their health and care. The NHS website received more than 90 million visits per month in 2022/23, making it the UK’s most popular health website, and more than 32 million people are registered for the NHS App, making it the UK’s most popular non-commercial app.
By the end of 2022/23, each month the NHS App enabled people to undertake tasks relating to 2.1 million repeat prescription orders (saving practices 336,000 hours in administration time), 1.2 million referrals to secondary care, 300,000 primary care appointments (saving practices 12,500 hours of administration time), and 470,000 people view their secondary care appointments.
Artificial intelligence (AI)
The NHS AI Lab, set up in 2019, accelerates the development and deployment of safe, effective applications that support clinicians by informing their decisions and saving time. We have funded 7 technologies through the AI in Health and Care Award. These have been rolled out to 65 hospital sites and helped over 200,000 patients. In December 2022, one recipient of funding, ‘Brainomix’ [19], tripled the number of stroke patients recovering with no or only slight disability from 16% to 48%.
NHS DigiTrials service
The NHS DigiTrials service developed at pace and supported the NHS-Galleri early cancer detection study to recruit over 140,000 people to participate in ground-breaking research in less than a year. In November 2022, the service launched a ‘beta’ version of its feasibility self-service tool, creating more opportunities for life-saving innovations to be developed for the NHS.
Live services
Following the merger with NHS Digital, NHS England became responsible for the operation of several technology services and live services which directly support patients and staff across the NHS, ranging from core infrastructure through to data sharing and cybersecurity operations.
The NHSmail team continued to support the adoption of the centralised Microsoft tool set to build enhanced collaboration. Adoption of these technology solutions has been crucial to improving patient care and efficient service delivery. The NHSmail collaboration platform has supported more than 800,000 audio calls, 1.5 million Microsoft Teams meetings and 9 million Microsoft Teams chats per week throughout 2022/23.
The Future Connectivity programme [20] supported a series of wireless trials within NHS trusts that helped frontline staff improve services by using digital technology and provided valuable insights into how investing in advanced wireless infrastructure in the NHS can improve user experience, care and outcomes. We helped NHS organisations upgrade more than 1,000 networks to faster and more reliable fibre connectivity; supported 12 NHS organisations with upgrades to gigabit-capable connectivity; established bandwidth demand profiles for nearly half of NHS premises; and identified up to 2,000 sites eligible for funding under the Department for Digital, Culture, Media and Sport’s ‘Project Gigabit’.
Digital inclusion
Mitigating the risk that digital approaches exclude people unwilling or unable to use them is a continuing priority for action on health inequalities and, in September 2023, NHS England’s framework for NHS action on digital inclusion [21] set out plans to support ongoing learning and action.
Emergency preparedness, resilience and response
During 2022/23, the NHS Resilience team continued to provide oversight to the COVID-19 response. Following the Omicron peak of just over 17,100 inpatients in early January 2022, there were several subsequent waves of COVID-19 infection alongside the return of the normal seasonal range of infections. In May 2022, we announced the move from COVID-19 response to recovery and moving from a Level 4 to Level 3 (regional leadership) incident response. At the end of March 2023, the NHS was caring for 7,500 patients with COVID-19 in inpatient beds; most had the infection as a complication of another condition that led to their admission.
The NHS Resilience team also manages the activation process for confirmed high consequence infectious disease (HCID) cases. These are usually single cases and include setting up HCID network calls to discuss patient placement, arranging safe patient transport where required and incident management. The team have supported the response to confirmed cases of Lassa fever, Crimean-Congo haemorrhagic fever and the Mpox outbreak during 2022. The team also worked with UKHSA on plans for managing any confirmed cases of returning travellers or healthcare workers linked to an Ebola outbreak in Uganda and monitored the global situation regarding Marburg virus, Lassa fever and avian flu.
In August 2022, the team worked closely with the NHS Cybersecurity Centre (then in NHS Digital) on the response to a cyber-attack on an NHS supplier.
The Resilience team led planning for significant national events and, following the death of Her Majesty the Queen, the plan for Operation London Bridge was activated.
Over the latter part of the reporting period, staff across a range of sectors, including the NHS, took industrial action. The NHS developed an operational plan in advance of strike action, informed by clinicians’ views on risk and setting out arrangements to respond to multiple different clinical and non-clinical NHS staff groups taking industrial action across ambulance and nursing services. The NHS Resilience team, together with the nursing, UEC and people directorates, established effective relationships with trade unions to inform discussions on derogations, taking a risk-based approach.
We frequently set out key actions for trusts and ICBs to minimise disruption and support patient care. To ensure readiness, identify areas of concern and focus our support, NHS Resilience worked with clinicians to develop and issue assurance ahead of each day of proposed strike action.
Other key responses over the reporting period include:
- supporting the UK response to the conflict in Ukraine
- a Level 4 heatwave alert
- supporting the NHS Blood and Transplant amber alert triggered by low bloodstock levels
- coordinating deployment of hazardous area response teams to assist with the suspected gas explosion in St Helier, Jersey
Access to medicines
The NHS is internationally competitive in adopting innovative medicines. Industry data shows 5 treatments are available in England for every 4 in Europe, and we have access to almost a third more cancer drugs.
Throughout 2022/23, the NHS Commercial Medicines Directorate (CMD) has secured new treatment options for thousands of patients while safeguarding the sustainability of the NHS medicines budget. Our approach is set out in the NHS Commercial Framework for New Medicines [22] and is aligned to the priorities and ambitions of both the NHS Long Term Plan and the UK’s Life Sciences Vision. [23]
In June 2022, we launched the Innovative Medicines Fund (IMF), a £340 million initiative to support faster access to non-cancer drugs. Together with the existing £340 million Cancer Drugs Fund (CDF), a total of £680 million ringfenced NHS funding is now provided for innovative medicines that show clinical promise, but where there remains uncertainty around clinical and cost-effectiveness. This uncertainty is then resolved through real-world data collection in the IMF or CDF.
In July 2022, we reported a £1.2 billion saving on the NHS medicines bill over 3 years. This was in large part due to the CMD’s Commercial Medicines Unit achieving better prices for hundreds of hospital medicines. This figure also included continued savings from the adoption of biosimilar versions of adalimumab (Humira®) which was previously the health service’s most costly drug.
The CMD has continued to work closely with partners at the National Institute for Health and Care Excellence (NICE), the Medicines and Healthcare Products Regulatory Agency and in industry to reach commercial terms for innovative treatments, enabling patient access, including:
- Alpelisib (Piqray®) with fulvestrant is a life-extending drug for patients with advanced breast cancer, the 100th cancer drug fast-tracked to patients under the CDF
- Eladocagene Exuparvovec (Upstaza®) is a first and only gene therapy for children with the ultra-rare genetic condition, aromatic L-amino acid decarboxylase deficiency
- Nivolumab (Opdivo®) and Ipilimumab (Yervoy®) is a combination treatment benefiting around 1,000 people with aggressive respiratory cancer, the first new mesothelioma treatment to be approved in nearly 15 years
- Ataluren (Translarna®) – routine approval for the first licensed treatment for Duchenne muscular dystrophy that addresses the loss of dystrophin, following a period of managed access
- Darolutamide (Nubeqa®) is a life-extending treatment secured following a Project Orbis regulatory review for thousands of patients with one of the most advanced forms of prostate cancer
- Axicabtagene Ciloleucel (Yescarta®) is a pioneering CAR-T therapy which will benefit adults with an aggressive form of blood cancer
Following a 5-year medicines procurement deal for antiviral drugs and a concerted effort to identify people at risk, in December 2022 we announced that deaths from hepatitis C have fallen by 35%, keeping England on track to be the first country in the world to eliminate the virus ahead of the World Health Organisation’s 2030 goal.
National deals to expand access to treatments have resulted in England being on track to have zero new HIV infections by 2030.
In June 2022, the NHS demonstrated global leadership on antimicrobial resistance, after the CMD reached agreements with 2 pharmaceutical companies for 2 antibiotics for treating severe drug-resistant Gram-negative bacterial infections.
Medicines account for between one-fifth and one-quarter of the NHS’s carbon footprint.
In January 2023, with support from professional anaesthesia bodies, we announced that Desflurane (a volatile anaesthetic used for surgery which has a global warming potential 2,500 times greater than carbon dioxide) will be decommissioned in 2024 and used only in exceptional circumstances. This will reduce harmful emissions by around 40 kilotons of carbon per year, the annual equivalent of powering 11,000 homes.
A new framework for local health and care providers aims to reduce inappropriate prescribing of high-strength painkillers and other addiction-causing medicines. We reported in March 2023 that opioid prescriptions have fallen by over 450,000 in under 4 years.
Research and innovation
We continue to support innovation, research and life sciences to improve patient outcomes and reduce health inequalities. The Accelerated Access Collaborative (AAC) provides patients with access to proven innovations by bringing together key partners from across government, charities, the NHS and industry.
Research and innovation are more important than ever in helping address operational pressures and mitigate increased demand. Work has continued to ensure that the NHS remains a partner for research and innovation, reflecting the aims in the government’s Life Sciences Vision [24] and NHS priorities.
During the reporting period:
- more than 230,000 new patients registered their interest in participating in research via the NHS App
- we completed 24 demand-signaling projects, investing £7.7 million in mental health, learning disabilities and autism, and stroke priorities
- we exceeded the 5-year forecast for the number of patients accessing the NICE-approved sickle cell treatment (Spectra Optia) via the MedTech funding mandate policy
- we supported more than 1,000 NHS staff through the Clinical Entrepreneur Programme (CEP), a mentoring and development programme to develop innovative solutions. These NHS innovators have now raised more than £850 million for solutions they have developed for frontline challenges
- NHS trusts were supported to develop their in-house innovation implementation capability and capacity through the CEP InSites Programme. 23 innovations have already been procured or piloted in the sites, with a further 29 innovations in the initiation phase and plans to expand to more sites in 2023/24
- 1,125 innovators registered with the NHS Innovation Service, which is supporting innovators to get tailored support from AAC partners. More than 340 needs assessments have been completed with 15 innovations now available through NHS Supply Chain.
Support for providers
Provider collaboratives
Provider collaboratives play a key role in ICSs, bringing organisations together to share best practice and resources, and to transform services.
Most acute and mental health providers are now in a provider collaborative. In February 2023, we announced the 9 collaboratives – with at least one from each of the 7 NHS England regions – that we will work with under our provider collaborative innovator scheme to accelerate their development and the benefits they can deliver for patients.
We continued to work with NHS Providers on a support programme to accelerate the spread of good practice via peer learning and make resources available to develop provider collaboratives.
Supporting trust boards to collaborate as part of a system
We published an updated code of governance for NHS trusts and foundation trusts that takes account of system working and collaboration, along with an addendum to the guide on foundation trust governors’ duties and new guidance, issued under the NHS provider licence, that sets clear expectations for collaboration and the governance arrangements.
Following consultation, we modified the NHS provider licence to bring it in line with statutory and policy requirements and enable us to develop our regulatory approach.
Mergers and acquisitions
In October 2022, we published ‘Assuring and supporting complex change: statutory transactions, including mergers and acquisitions’ [25], which supersedes NHS Improvement’s guidance. It reflects the changing NHS landscape and focuses on the most important areas for successful transaction. All transaction proposals must have patient and population benefits at their core, underpinned by detailed plans for delivering them.
We offer bespoke support to trusts considering or proceeding with mergers or acquisitions and help ensure clarity about the intended benefits. Significant transactions completed during the reporting period included:
- Royal Devon and Exeter NHS Foundation Trust acquired Northern Devon Healthcare NHS Trust on 1 April 2022, with the newly enlarged trust renamed Royal Devon University Healthcare NHS Foundation Trust
- after year end, Yeovil District Hospital NHS Foundation Trust acquired Somerset NHS Foundation Trust on 1 April 2023, with the newly enlarged trust retaining the Somerset NHS Foundation Trust name
Regulating independent providers of NHS services
Since April 2014, all independent providers of NHS services have had to hold a provider licence, unless exempt, under Department of Health and Social Care (DHSC) regulations.
The licence allows us to help commissioners protect essential local services if an independent provider fails. As of 31 March 2023, 135 independent providers held licences, of which 3 are NHS-controlled providers.
Commissioners are asked to consider which of their services must continue to be provided locally should the provider fail, and therefore should be designated as commissioner requested services (CRS). Out of the 135 licensed independent providers, 34 are providers of CRS as part of the national risk assessment and financial oversight regime. In the year to 31 March 2023, no formal enforcement action was taken with any independent providers, therefore on 31 March 2023, no enforcement undertakings were in place.
During the year, we consulted on updates to the Risk Assessment Framework and Reporting Manual for Independent Sector Providers. The proposed updates set out the oversight approach for standards of quality governance at some independent sector providers.
Recovery Support Programme
Where a trust is in breach or suspected breach of the conditions of its provider license, NHS England can use its statutory powers, including legal powers of direction, to intervene in line with the NHS Enforcement Guidance. [26] At the end of the 2022/23, NHS England was providing intensive support via the Recovery Support Programme to 15 trusts, with a further 2 trusts exiting the programme by March 2023.
Chief Financial Officer’s report
Introduction
The financial statements for the year ending 31 March 2023 are presented later in this document on a going concern basis (as per note 1.5 of the accounts) and show the performance of both the consolidated group – covering the whole of the commissioning system – and NHS England as the parent of the group. The group comprises NHS England, the CCGs from 1 April 2022 to the end of 30 June 2022, and 42 ICBs from their inception on 1 July 2022.
During 2021/22 the government announced the intention to effect the legal merger of NHS Digital, Health Education England and NHS England from April 2023. In preparation for this, the organisations undertook an extensive and consultative process to design the functions and form of the new, combined organisation, alongside the necessary work to ensure continuity of vital functions.
At the request of the Secretary of State for Health and Social Care at the time, in October 2022, we further announced an accelerated timeline for merger with NHS Digital, by 1 February 2023. The NHS England group therefore included NHS Digital from this mid-year point.
NHS England is required to manage spending within a fixed revenue limit. The total revenue limit for 2022/23 was £158,521 million.
Funding and allocations
In 2022/23, the NHS saw a real-terms reduction in total funding from the previous year of 0.6%, mainly driven by lower government funding for the impacts of COVID-19 and reductions in the scope – and therefore the costs of programmes such as vaccinations and testing. Additional funding has been agreed during the year for the pay award (including the 2022/23 backdated element), the voluntary scheme for branded medicines pricing and access to the COVID-19 vaccination and testing programmes, and funding for additional flu vaccine cohorts.
In 2022/23, the temporary COVID-19 financial framework came to an end, and we began the process of transitioning back to a more sustainable financial framework and allocation approach for the NHS. This included setting fixed allocations for ICBs for the year and ending the top-up funding arrangements that operated during the pandemic. The allocations for 2022/23 also included specific funding to reduce waiting lists, through the Elective Recovery Fund.
At the start of the year, we were forced to issue additional inflation funding of £1.5 billion to cover higher energy costs, a direct impact of inflation on index-linked contracts and other inflationary pressures. This required us to reprioritise transformation funding, in particular cutting funding for digital investment and for primary care.
We have also issued additional pay funding to the NHS totalling £4.4 billion to cover the costs of the recurrent in-year pay award and the back dated non-consolidated award, for which we received additional funding from the government.
Operational pressures
While government funding for pressures related to the pandemic was reduced in 2022/23, the NHS was still experiencing the ongoing impacts of COVID-19 on costs and services.
Industrial action has also created a significant pressure on the NHS in 2022/23, with a total of 17 days of strike action by nurses and other staff groups during the year.
Throughout the year, providers have struggled to discharge medically fit patients due to a lack of capacity in social care – in particular, care homes – which has led to longer lengths of stay and much higher bed occupancy.
In November 2022, we issued additional winter surge funding to the NHS which enabled us to put in place the equivalent of 7,000 beds, including community-based virtual wards. This enabled us to manage the highest ever number of A&E attendances in a single day, and to absorb the impact of the peak infection rates for COVID-19 and seasonal flu coinciding in the same week.
In spite of these pressures, the NHS has delivered around £5 billion of savings and has made significant improvements in productivity, allowing us to improve operational performance in a number of key areas including reducing elective waiting lists, though not by as much as we had planned.
The real terms cut in core funding, combined with the high rate of inflation and operational pressures set out above, has made this a very challenging year for the NHS.
Irregular spending
As noted above, the NHS was allocated additional funding under the Elective Recovery Fund to reduce waiting lists. This money was ringfenced, to be used for this purpose only. Because elective activity was lower than planned, some of this money should have been returned to the government. However, the lower levels of elective activity were due to ongoing COVID-19 pressures and longer lengths of stay, factors for which no additional funding had been provided. Therefore, we decided to allow providers to retain the elective funding to cover these costs, which the government has now deemed to be irregular.
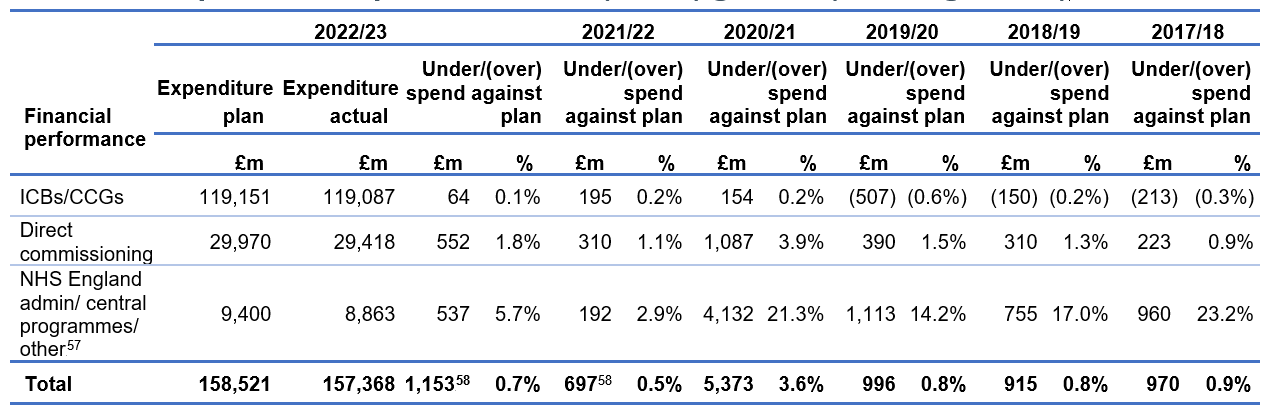
Financial performance
This year, NHS England delivered an underspend of £1,153 million against the revenue resource budget. Of this, £120 million (2021/22: £604 million) related to budgets restricted for specific purposes. The remaining £1,033 million underspend was against core funding budgets, of which around £600 million was necessary to offset overspending by NHS providers and the balance to offset the pressure caused by provider technical issues. By the end of the year, 40 out of 42 systems either broke-even or achieved the stretch target that we set for them.
Revenue Department Expenditure Limit (RDEL) general (non-ringfenced)
|
Financial performance
|
2022/23 |
2021/22 |
2020/21 |
2019/20 |
2018/19 |
2017/18 | ||||||||
|
Expenditure plan |
Expenditure actual |
Under/(over) spend against plan |
Under/(over) spend against plan |
Under/(over) spend against plan |
Under/(over) spend against plan |
Under/(over) spend against plan |
Under/(over) spend against plan | |||||||
|
£m |
£m |
£m |
% |
£m |
% |
£m |
% |
£m |
% |
£m |
% |
£m |
% | |
|
ICBs/CCGs |
119,151 |
119,087 |
64 |
0.1% |
195 |
0.2% |
154 |
0.2% |
(507) |
(0.6%) |
(150) |
(0.2%) |
(213) |
(0.3%) |
|
Direct commissioning |
29,970 |
29,418 |
552 |
1.8% |
310 |
1.1% |
1,087 |
3.9% |
390 |
1.5% |
310 |
1.3% |
223 |
0.9% |
|
NHS England admin/central programmes/ other (Supply Chain Coordination Ltd included in ‘other’) |
9,400 |
8,863 |
537 |
5.7% |
192 |
2.9% |
4,132 |
21.3% |
1,113 |
14.2% |
755 |
17.0% |
960 |
23.2% |
|
Total |
158,521 |
157,368 |
1,153* |
0.7% |
697* |
0.5% |
5,373 |
3.6% |
996 |
0.8% |
915 |
0.8% |
970 |
0.9% |
*The underspend in 2022/23 includes £120 million (2021/22: £604 million) relating to specific ringfenced budgets included in DHSC’s financial directions to NHS England with these amounts not available to support general spending.
In the mandate the DHSC sets a number of technical financial targets for the NHS England Group, including the core operational limit (general RDEL) described above. These limits are ringfenced, which means that underspends on the other revenue limits cannot be used to support core patient services covered by the general RDEL limit.
2022/23 performance against key financial performance duties
a) Revenue limits
|
Revenue limits |
Target (2022/23) |
2021/22 | ||||
|
Mandate limit £m |
Actual £m |
Underspend |
Target met |
Underspend as % of mandate |
Underspend £m | |
|
RDEL – general |
158,521 |
157,368 |
1,153 |
Yes |
0.7% |
697 |
|
RDEL – ring-fenced for depreciation and operational impairment |
288 |
259 |
29 |
Yes |
10.0% |
0 |
|
Annually Managed Expenditure limit for provision movements and other impairments |
250 |
12 |
238 |
Yes |
95.4% |
28 |
|
Technical accounting limit (e.g., for capital grants) |
200 |
(274) |
474 |
Yes |
237.2% |
199 |
|
Total revenue expenditure |
159,259 |
157,364 |
1,89558 |
1.2% |
924 | |
b) Administration costs (within overall revenue limits above)
|
Total administration costs |
2,011 |
1,832 |
179 |
Yes |
8.9% |
243 |
c) Capital limit
|
Capital expenditure contained within our capital departmental expenditure limit |
330 |
276 |
54 |
Yes |
16.5% |
46 |
Financial priorities for 2023/24
Our priorities continue to focus on making sure that the frontline of the NHS has the resources it needs to deliver on our key priorities for patients, with a focus on recovering cancer performance, maintaining emergency care services and treating as many patients who are waiting for elective care as we can.
We must also recognise the continuing efforts of NHS staff and ensure that colleagues are supported in order that they can continue to deliver their best work for patients.
For 2023/24 we will be working with ICSs to:
- ensure we have the physical and workforce capacity to manage COVID-19 in the long term
- ensure the smooth delegation of pharmaceutical services, general ophthalmic services, and dental services to ICBs
- continue to support DHSC in delivering the multi-year New Hospital Programme and invest in our wider estate
- use the specific resources we have been provided with to reduce the number of people waiting for elective procedures, and continue to increase our investment in mental health and primary care services
- continue the journey towards greater system working and integrated care budgets
- maintain spending controls and deliver care as efficiently as we can in the context of ongoing operational constraints.
Julian Kelly, Chief Financial Officer, NHS England.
References
[1] https://www.england.nhs.uk/publication/three-year-delivery-plan-for-maternity-and-neonatal-services/
[2] https://www.england.nhs.uk/publication/saving-babies-lives-version-two-a-care-bundle-for-reducing-perinatal-mortality/
[3] https://www.england.nhs.uk/publication/saving-babies-lives-version-three/
[4] https://www.gov.uk/guidance/fetal-anomaly-screening-programme-overview
[5] https://www.nhs.uk/conditions/baby/newborn-screening/blood-spot-test/
[6] https://www.nhs.uk/conditions/lung-health-checks/
[7] https://www.nhs-galleri.org/
[8] https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-programme/cervical-screening-programme-coverage-statistics-management-information
[9] https://www.england.nhs.uk/statistics/statistical-work-areas/vaccinations-for-Mpox/
[10] https://www.england.nhs.uk/publication/2022-23-priorities-and-operational-planning-guidance/
[11] https://www.england.nhs.uk/publication/healthcare-for-the-armed-forces-community-a-forward-view/
[12] https://www.nhs.uk/nhs-services/armed-forces-community/mental-health/veterans-reservists/
[13] https://www.forcesemployment.org.uk/programmes/op-nova/
[14] https://transform.england.nhs.uk/digitise-connect-transform/what-good-looks-like/what-good-looks-like-publication/
[15] https://www.gov.uk/government/publications/data-saves-lives-reshaping-health-and-social-care-with-data
[16] https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care
[17] https://www.gov.uk/government/publications/cyber-security-strategy-for-health-and-social-care-2023-to-2030
[18] https://www.england.nhs.uk/blog/investing-in-the-future-of-health-research-secure-accessible-and-life-saving/
[19] https://www.gov.uk/government/news/artificial-intelligence-revolutionising-nhs-stroke-care
[20] https://digital.nhs.uk/services/future-connectivity
[21] https://www.england.nhs.uk/long-read/inclusive-digital-healthcare-a-framework-for-nhs-action-on-digital-inclusion/
[22] https://www.england.nhs.uk/medicines-2/commercial-medicines/nhs-commercial-framework-for-new-medicines/
[23] https://www.gov.uk/government/publications/life-sciences-vision
[24] https://www.gov.uk/government/publications/life-sciences-vision
[25] https://www.england.nhs.uk/publication/statutory-transactions/
[26] https://www.england.nhs.uk/long-read/nhs-enforcement-guidance/
[27] Supply Chain Coordination Ltd included in ‘other’
[28] The underspend in 2022/23 includes £120 million (2021/22: £604 million) relating to specific ringfenced budgets included in DHSC’s financial directions to NHS England with these amounts not available to support general spending.

