Introduction and use of funding
1. NHS England provides service development funding (SDF) (also sometimes called ‘System Development Funding’) each year for ICBs, as additional programme funding on top of ICB baselines. This document provides guidance for primary care SDF for 2023/24.
This funding should be invested in initiatives which will support practices and primary care networks (PCNs) to deliver high quality primary care, and specifically in delivering the ambitions of the Delivery Plan for Recovering Access to Primary Care (referred to in this document as ‘the Delivery Plan’) and other primary care improvement programmes as outlined in this guidance.
2. In 2023/24, the key priorities for integrated care boards (ICBs) in relation to primary care (see 2023/24 planning guidance) are supporting improved access to services, particularly patient experience of contacting general practice, and supporting practices and PCNs with demand management and improving job satisfaction.
Improving access to primary care services, particularly general practice, is also one of the three overall national objectives for the NHS in 2023/24.
3. The Delivery Plan focuses on two central ambitions for patients:
- Tackling the 8am rush and reducing the number of people struggling to contact their general practice.
- For patients to know, on the day that they contact their general practice, how their request will be managed.
4. To deliver these ambitions and provide ‘modern general practice access’ as set out in the Delivery Plan, it is necessary to support practices to change and improve their operational models, and to optimise use of available staff.
It is also essential to cut bureaucracy, to reduce the workload across the interface between primary and secondary care, and to invest in recruiting, retaining and developing primary care staff. The primary care SDF provided to ICBs in 2023/24 should be allocated to support these aims.
5. Primary care SDF in 2023/24 can be thought of in three sections:
- a transformation budget to support change and improvement in primary care (and particularly general practice) including support to the workforce
- a set of specific workforce programmes continuing from previous years (including some ARRS funding) – see ‘Workforce initiatives’ section and appendix 3 for more detail.
- funding from primary care SDF to increase general practice IT (GPIT) revenue budgets (‘GPIT Infrastructure and Resilience’).
Primary care SDF 2023/24 overview
6. To support ICBs to maximise use of their primary care SDF funding and in recognition of the new statutory nature of ICBs, the number of separate primary care SDF allocations has been reduced significantly for 2023/24.
This will reduce administrative burden and allow greater local autonomy and flexibility in managing funding and addressing priorities for change. Eight previously separated allocations have been bundled together for 2023/24 into a single ‘primary care transformation’ allocation.
7. Primary care SDF funding available to systems in 2023/24 is as per the table below. For the bundled primary care transformation budget, the names of the previous funding lines that have been brought together are included for information.
The bundled primary care transformation funding should not be split into separate allocations and managed separately between these lines (apart from where necessary for coding purposes – see appendix 1). For ICB funding breakdowns see appendices 2 and 3.
8. It is for ICBs to determine how to invest the overall transformation amount to deliver the support required to general practice and PCNs set out in the Delivery Plan and in the ‘primary care transformation funding’ section below. Systems should also consider how to support and consolidate improvements in practices who have already invested in changes.
Table 1: Primary care SDF 2023/24
1. Transformation
|
Primary care transformation – includes funding that was previously split between the following schemes, but which is now bundled into one allocation to provide greater flexibility for ICBs:
|
£169.9 million |
2. Workforce programmes
|
ARRS centrally held for ICB draw-down1 |
£521.3 million |
|
General practice fellowships |
£35.7 million |
|
Supporting mentors scheme |
£8.4 million |
|
International GP recruitment |
£2.4 million |
3. GPIT
|
GPIT – infrastructure and resilience |
£13.0 million |
9. PCN funding continues for clinical directors, which is included in primary medical care allocations, (see page 2 of the Financial Implications letter) and is further supplemented by PCN leadership and development funding (£43m) included in the bundled primary care transformation amount as above.
PCNs will also receive monthly funding via the IIF Capacity and Access Support Payment to support transformation. There is also additional transformation support funding for practices available via the Delivery Plan to provide ‘transition cover’ for change.
Primary care transformation funding
10. NHS England will allocate £169.9m of primary care SDF in 23/24 to ICBs to support primary care transformation. Systems should use this funding to leverage and achieve the maximum transformation possible, in line with the Delivery Plan, alongside initiatives to recruit, retain and support primary care staff. The SDF should not be used to fund business as usual staff or other ICB costs.
11. The Delivery Plan sets out specific actions and asks of ICBs. These should be brought together through a ‘system-level access improvement plan’.
This system-level plan should set out how the ICB will meet the ambitions in the Delivery Plan to deliver modern general practice access, including how it will provide the necessary support to primary care to make improvements to service delivery, support demand and workload management, and help with staff recruitment and retention.
The overall aim of this work is to deliver an improved experience of access for patients, better continuity of care where most needed and improved job satisfaction for staff.
12. The ICB plans should bring together the actions to be taken at practice and PCN level with those required at system level taking high level direction from the Delivery Plan, and tailoring to specific local needs, challenges and context. They should also set out the work that will be done using primary care Transformation SDF funding.
Please see appendix 5 for the list of key actions for ICBs in relation to the Delivery Plan (‘the ICB checklist’), but noting that primary care Transformation SDF will be especially relevant for items 5 and 16 from the ICB checklist, as follows:
Table 2: ICB checklist actions 5 and 16
Commitment |
|
Action for ICBs |
Reporting |
Time due |
|
Modern general practice access |
5 |
Fund or provide local hands-on support to 850 practices nationally (ICBs should work with regions to determine population appropriate share of target) We would expect the level of support to be similar to the national intermediate offer, and offered alongside wider or ongoing support for practices and PCNs where required, using the outputs of the SLF to help guide specific support needs |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
31 March 2024 |
|
Enablers |
16 |
Co-ordinate system comms to support patient understanding of the new ways of working in general practice including digital access, multidisciplinary teams and wider care available. This messaging should include system specific services and DoS (Directory of local services). |
Ongoing 2023/24 |
13. In addition to the specific actions outlined in the Delivery Plan, ICBs should continue to use primary care Transformation SDF to support improvements that will enable progress of the Fuller Stocktake ambitions and support more sustainable ways of working to reduce the burden on general practice staff including:
- providing general practice with business intelligence tools to support practices and PCNs to make informed decisions based on easily accessible near real time data and to support systems to understand and help manage demand pressures
- continuing or increasing support to enable at-scale working across primary care and with other parts of the system tailored to local needs, for example:
- development of virtual hubs
- access hubs
- integrated urgent care
- community and neighbourhood working, etc.
- strengthening partnerships and communications within the system between primary care and other health and care providers to ensure patients receive consistent messages and encourage collaborative solutions
- supporting development of ICB infrastructure strategies, as per the Fuller Stocktake commitment, to enable and support an integrated service delivering care closer to home in the community (capped at £188k/ICB).
- funding automation tools to reduce burden on practices, and tools for proactive monitoring of long-term conditions to support remote monitoring and risk stratification as part of local population health approaches
- working with training hubs to consider the recruitment, training and development needs of practice and PCN teams and to carry out effective local workforce planning
- this should aim to enable new models and processes as outlined in the Delivery Plan (including call handling, care navigation and triage, and IT system training), and to develop staff skills to meet local population needs and improve staff productivity and retention
- systems should engage with practices, PCNs and training hubs to understand these needs, and identify where programmes may need to be commissioned to meet them, building on the training hub core offer.
- increasing capacity in primary care by maximising recruitment of additional roles reimbursement scheme (ARRS) roles, embedding and increasing use of digitally enabled flexible staff/locum pools, supporting local programmes focused on recruitment, retention and wellbeing of all general practice staff, and continuing work to encourage the recruitment and retention of general practice nurses.
14. ICBs are expected to report on progress in delivering the commitments in the Delivery Plan and their own system level access improvement plans, via ICB public board meetings, both in October/November 2023 and April/May 2024.
This will sit alongside existing workforce reporting requirements, including monthly updates to the national workforce reporting service (NWRS) and primary care monitoring survey (PCMS), and submission of ARRS recruitment intentions and GP retention schemes delivery plans, as well as encouraging practices and PCNs to make updates as required.
15. ICBs and NHS England regional teams will have supportive discussions over the financial year on delivery, progress, and issues to help ensure best use and impact of the funding. Where it is preferable for some primary care SDF to be held and spend to take place at NHS England regional level to achieve economies of scale, this can take place with the agreement of ICBs in that region.
Workforce initiatives
16. The second part of the primary care SDF consists of budgets and allocations supporting specific workforce programmes as set out below. Although some schemes came to an end in 2022/23 there may be costs arising in 2023/24 due to commitments carried over from previous years.
17. These initiatives should be used to grow and strengthen the primary care workforce, deliver objectives on ARRS and GP full-time equivalents (FTEs), improve services, and improve patient and staff experience as a result.
Additional roles reimbursement scheme
Overview
18. The ARRS provides funding for 26,000 additional roles for PCNs to create bespoke multidisciplinary teams. The ARRS programme also offers opportunities for practitioners to join primary care with an exciting, supported and more diverse career. Funding from the scheme can be used to reimburse roles recruited into PCNs under the Network Contract DES.
A. Available funding and method of allocation
19. £891 million for 2023/24 is included within ICBs’ baseline allocations; and £521.3 million for 2023/24 is held centrally within primary care SDF – a further £385m in total above 2022/23. Each ICB’s share of this central allocation is available for release when needed, subject to regional and national approvals. Please see appendix 3.
Expected national deliverables
20. ICBs are expected to:
- continue to increase the number of additional roles in primary care beyond 26,000 by the end of 2023/24
- ensure all PCN claims for funding are made and approved via the online portal and NWRS returns are completed by 100% of practices and PCNs
- ensure effective support is provided to PCNs to recruit, embed and retain new roles as specified in PCN DES documentation and guidance related to the scheme.
Further details on the scheme can be found on the NHS England website.
B. General practice fellowships for GPs and nurses
Overview
21. The fellowship scheme offers a two-year programme of support, available to all newly qualified GPs, newly qualified nurses and new to practice nurses working substantively in general practice – with an explicit focus on working within and across PCNs.
Participants receive mentorship (or supervision) and continuing professional development (CPD) opportunities. Plus, rotational placements within or across PCNs of up to one session per week, to develop experience and support transition into the workforce. Further details can be found on the NHS England website.
Available funding and allocation
22. £35.7 million is available nationally for 2023/24 (system shares are based on local demand for fellowships as this will vary).
23. The programme will be funded based on actual costs incurred, but with an initial fair shares allocation upfront during Q1, which will be adjusted in later quarterly allocations to reflect actual and planned spend and delivery.
Expected deliverables
24. These include that:
- fellowships are offered to 100% of GPs and nurses completing training in the preceding 12 months
- fellowships are offered to all nurses new to general practice
- there is increased conversion of newly qualified GPs into substantive roles, increased participation by newly qualified GPs and nurses, contributing to increasing the overall numbers of GP FTEs (system delivery plans are submitted outlining forecast numbers of newly qualified GPs, newly qualified nurses and new to practice nurses)
- monthly updates on actual figures are reported through the primary care monitoring survey, with ongoing evaluation and sharing of lessons learned to the national team.
C. Supporting mentors scheme overview
Overview
25. This scheme creates a portfolio working opportunity for experienced GPs to support GP colleagues through high quality mentoring. ICBs will receive funding to support the training of GP mentors and to cover reimbursement to mentors for their mentorship session costs. Further details can be found on the NHS England website.
Available funding and allocation
26. £8.4 million is available nationally for 2023/24.
27. The programme will be funded based on actual costs incurred up to the £8.4m, but with an initial fair shares allocation upfront during Q1, which will be adjusted in later quarterly allocations to reflect actual and planned spend and delivery.
Expected deliverables
28. ICBs are asked to:
- increase the number of matches between mentors and mentees from the previous year (2022/2023)
- achieve a mentor-to-mentee ratio of at least 1:4
- maintain current mentor numbers, ensuring training, ongoing peer networking and CPD activities are made available
- ensure that the scheme meets the mentoring needs of GPs on the General Practice Fellowship programme
- increase retention of experienced GPs through access to mentor training and opportunities, and increased retention of local GPs through high quality mentoring support, contributing to increasing the overall numbers GP FTEs
- submit a system delivery plan outlining forecast number of mentors, number of mentees and anticipated number of mentoring sessions
- provide monthly updates on actual figures via PCMS and share evaluations and lessons learned with the national team on an ongoing basis.
D. International GP recruitment, Return to Practice programme, International Induction programme, and visas overview
29. The International GP Recruitment (IGPR) programme and International Induction Programme (IIP) provide support to enable internationally qualified GPs to come and work in the NHS and gain the necessary entry to the medical performers list. The Return to Practice (RtP) programme provides a safe supported pathway for former GPs to return to their careers in general practice.
30. In addition, NHS England supports the retention of newly qualified GPs by funding the visas of international medical graduates (IMGs) that have completed GP training in England. These costs will be reimbursed to the GP via their employing practice.
31. The IGPR Programme has now closed to new applicants but there remain over 20 doctors recruited into the programme and undergoing training. Funding is available for those areas that were actively recruiting in the 2020/21 and 2019/20 financial years, to enable the intensive support required for these doctors to complete the programme of training.
32. The International Induction Programme remains open to new applications from international GPs. Where these GPs require visa sponsorship and employment with a practice to complete the programme, NHS England will reimburse the employing practice for salary and on-costs while they are on the programme.
33. During 2023/24 NHS England may also expand support for GPs on the Return to Practice programme and allow them to complete the programme while in employment. In such cases, NHS England will reimburse the employing practice for salary and on-costs while they are on the programme.
34. Further details of the International GP Recruitment programme can be accessed on the NHS England website. Further details of the GP Return to Practice and International Induction programmes can be found on the HEE website.
Available funding and allocation
35. Funding is provided to NHS England regional teams on a monthly drawdown basis and includes costs for salaries, visas, language training, and relocation expenses. The indicative funding envelope nationally in 2023/24 is £2.4 million. Drawdown will be monitored carefully to ensure forecasting is accurate.
As distribution of this centrally-held funding is on a drawdown basis, this is a targeted – ie demand-led programme. The envelope is based on planning assumptions of GPs still progressing through the programme.
Expected deliverables
36. To support the remaining GPs through the International GP Recruitment programme into substantive roles, GPs through the International Induction and Return to Practice programmes and the retention of GPs requiring visa sponsorship.
37. This is expected to contribute to increasing the overall numbers of GPs.
General practice IT funding
38. GPIT funding includes:
- GPIT revenue embedded as part of ICB core baselines
- funding held centrally for spend on accredited GPIT systems (including core clinical systems but also other systems)
- capital funding embedded in overall NHS England capital allocations.
39. None of this funding is primary care SDF but is mentioned here for information.
40. The total GPIT revenue for 23/24 embedded in ICB baselines is £269.9m, with indicative shares by ICB set out in Appendix 4 below. This funding is designated to deliver, as first priority, the core and mandated requirements of the GPIT operating model, for both practice and additional roles staff working with PCNs. Any remaining funding should be used to support the wider digital transformation of primary care.
41. £13 million GPIT Infrastructure and Resilience funding from primary care SDF will be allocated on a fair-shares basis to ICBs, via a single payment in Q1 of this year. This funding should be used by ICBs for investment in specific technology upgrade initiatives aligned with the requirements of the GPIT operating model.
42. Funding held centrally for spend on accredited GPIT core clinical and other systems, is provided based on a notional allocation per ICB. This funding is required to be spent on products included on the digital care services catalogue and associated frameworks.
There will be additional funding available (c.£70m) for spend on accredited systems in 2023/24 as part of the delivery plan for access recovery plan to support general practice to access improved digital tools (online consultation systems, messaging and appointment booking tools).
NHS England will work alongside systems to ensure this new funding enables additional digital capacity for practices and PCNs, and does not allow disinvestment, or replace existing digital funding.
ICBs will be expected to work with PCNs and practices to decide which tools from the catalogue will best enable them to shift to the modern general practice access model and to implement and sustain improvements as set out in appendix 4.
Appendix 1: Coding instructions
Primary care transformation coding
1. Expenditure should be coded to one of the following existing codes. These codes will be looked at in total to determine spend against the £169.9 million:
- Digital First support sub analysis A3 code 000010
- Primary care Network sub analysis A3 code 000009
- GP Transformation Support sub analysis A3 code 000030
- Estates Business Cases – sub analysis A3 code 000005
- Local GP Retention Fund – sub analysis A3 code 000013
- primary care Flexible Staffing Pools – sub analysis A3 code 000016
- Training Hubs – sub analysis A3 code 000007
- Practice resilience programme – sub analysis A3 code 000004
- Practice Nurse Measures – sub analysis A3 code 000006
- PCN Leadership and Management – this is co-commissioning expenditure and should be coded as such.
2. If none of these codes seem appropriate, please contact the primary care Finance Team: pcfinancegroup@nhs.net. These codes will be kept under review and added to if required.
Coding for workforce programmes
ARRS coding requirements
3. PCNs will need to submit claims for ARRS and ICBs will need to approve the claims through the online claims portal. Use of the portal has been mandatory since 1 April 2021 and ICBs will be eligible to draw down additional funding from primary care SDF, conditional on them providing evidence that PCNs have made claims via this process to a level above the ICB’s ARRS funding in their primary medical care allocation.
4. ARRS expenditure integrated single financial environment (ISFE) coding uses nationally defined subjective codes for each role that is recruited to. Funding transferred to PCNs will need to be coded using the appropriate PCSE codes. ICBs will need to create budgets on ISFE that reflect baseline allocations and forecast for the expected 2023/24 expenditure on individual roles.
5. National guidance for ARRS coding can be found in Section 10.3.6 on pages 40 to 46 of the Network Contract.
6. Systems should ensure that PCNs and practices are accurately recording workforce numbers in the National Workforce Reporting Service (NWRS).
General practice fellowships coding and monitoring requirements
7. Systems need to code expenditure using the sub analysis A3 code. The General Practice Fellowships allocations will have two Sub Analysis A3 codes:
- 000024 ‘Fellowships GP’ for expenditure relating to GP Fellowships and
- 000025 ‘Fellowships Nurse’ for expenditure that relates to Nurse Fellowships.
8. Systems will be required to draw together a proposal for how the scheme will be delivered, as well as supplying updates through PCMS. Validation of actual and planned spend and delivery will enable further allocations.
Supporting mentors coding and monitoring requirements
9. Expenditure should be coded to the sub analysis A3 code 000015 ‘PCT Supporting Mentors’.
10. Systems will be required to draw together a proposal for how the scheme will be delivered. Validation of actual and planned spend and delivery will enable further allocations.
International GP recruitment, International Induction programme and visa support coding and monitoring requirements
11. Expenditure should be coded to the sub analysis A3 code 000003 ‘PCT International Recruitment’.
12. ICBs will need to provide a list of the names and practices of the GPs who have signed up for these programmes.
GPIT – Infrastructure and Resilience
13. Expenditure should be coded to the sub analysis A3 code 000012 ‘PCT Infrastructure and Resilience’.
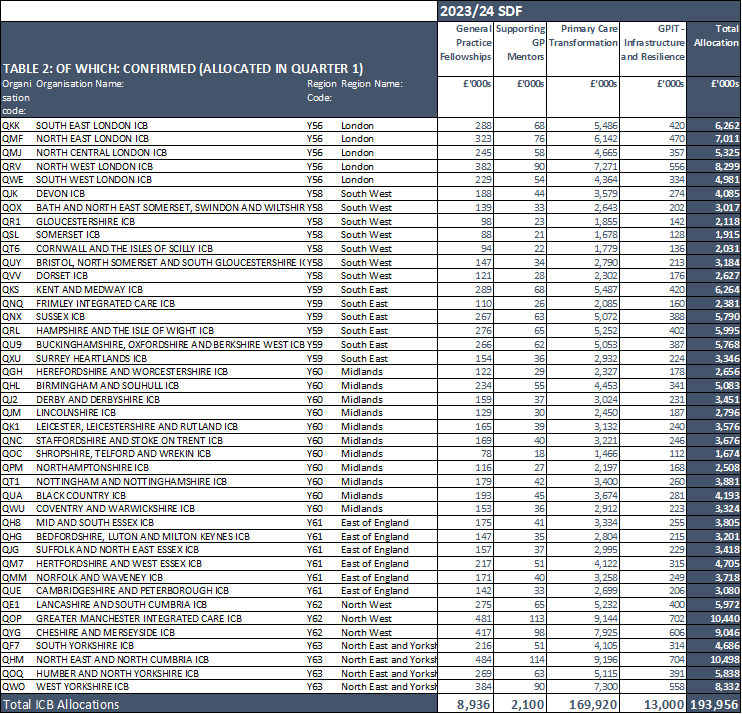
Appendix 2: ICB primary care SDF allocations
Figure 1: Total funding available
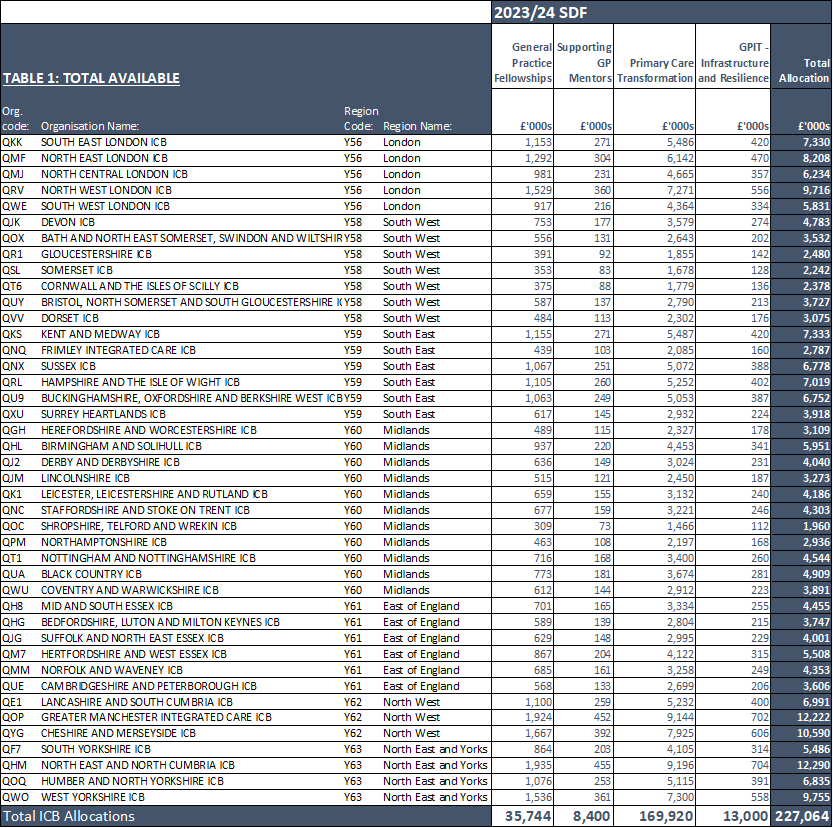
Figure 2: Confirmed funding (allocated in quarter 1)
Appendix 3: ICB ARRS funding
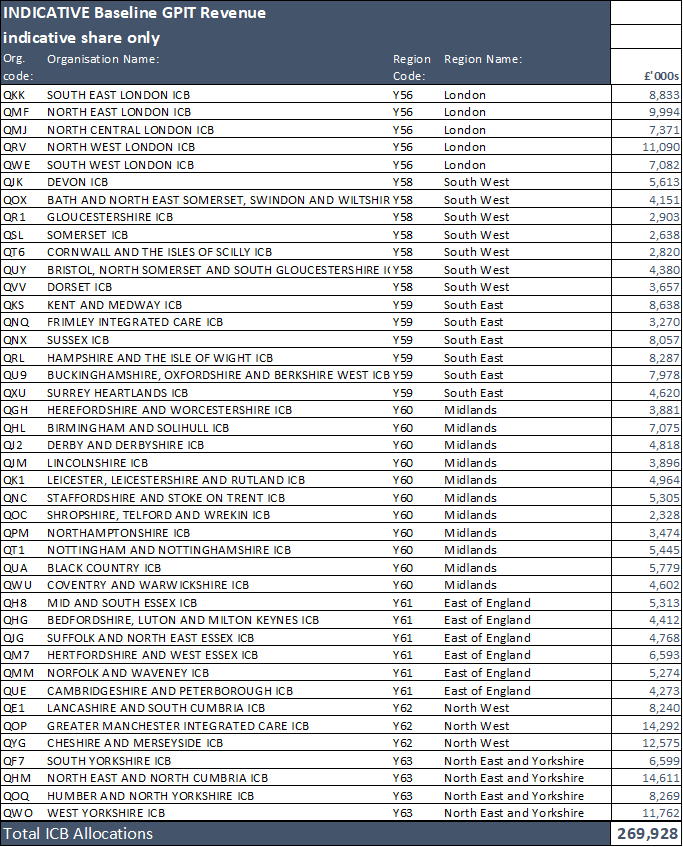
Appendix 4: GPIT – indicative funding within ICB core allocations
ICBs receive GPIT revenue funding as part of their core allocation baseline. ICBs are required to deliver the core and mandated requirements of the GPIT Operating Model, for both practice and additional roles staff working with PCNs. Any remaining funding should be used to support the wider digital transformation of primary care. The total for 23/24 is £269.9 million, with indicative shares by ICB as follows:
Appendix 5: Checklist of key ICB actions from Delivery plan for recovering access to primary care
Commitment: Empowering patients
| Action for ICBs | Reporting | Time due |
|---|---|---|
|
1. Establish all self-referral pathways (including MSK, audiology and podiatry) as set out in 2023/24 guidance, also ensure pathways are in place between community optometrists and ophthalmologists |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By 30 September 2023 |
Commitment: Modern general practice access
| Action for ICBs | Reporting | Time due |
|---|---|---|
|
2. Sign up practices ready to move from analogue to digital telephony, and co-ordinate access to specialist procurement support through NHS England’s commercial hub Determine whether ICB wants to follow scale approach to telephony (see Leeds case study on p23 in Delivery Plan for Recovering Access to primary care) Use peer networks and demonstrations with practices/PPGs/PCNs to help practices and PCNs identify and adopt digital telephony |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By 1 July 2023 for sign-up Ongoing for co-ordination |
|
3. Select digital tools from the Digital Pathway Framework lot on DCS product catalogue (published in August), using user research and preview to be published by June Determine whether ICB wants to follow scale approach to digital products Use peer networks and demonstrations with practices/PPGs/PCNs to help practices and PCNs identify and adopt the most usable software |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
31 August 2023 |
|
4. Nominate practices and PCNs for national intensive and intermediate transformation support matched to needs using the Support Level Framework where possible to understand support needs, with the aim being for all practices to have had a facilitated discussion using the SLF during the year. Prioritise practices with greatest challenges, and with data from digital telephony already in place, and nominate further practices as they implement digital telephony (ICBs should work with regions to determine population appropriate share of nominations). Phase A (Intensive) (250 practices nationally) nominated by 30 May 2023. Phase B (Intensive & intermediate) (250 and 100 practices nationally) nominated by 14 June 2023. Further phases to be nominated, in July, September and November 2023. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
ICBs nominate practices and PCNs for support through 23/24 and 24/25
|
|
5. Fund or provide local hands-on support to 850 practices nationally (ICBs should work with regions to determine population appropriate share of target). We would expect the level of support to be similar to the national intermediate offer, and offered alongside wider or ongoing support for practices and PCNs where required, using the outputs of the SLF to help guide specific support needs. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
31 March 2024 |
|
6. Agree and distribute transition cover and transformation support funding (£13.5k / qualifying practice) to support practice teams seeking to implement Modern General Practice Access model. Guidance on distribution to be published soon. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Ongoing |
|
7. Co-ordinate nominations and allocations to care navigator training, and digital and transformation PCN leads training and leadership improvement training. Cohort 1 (40 PCN D&T leads nationally) nominated by 7 June 2023. 3,250 Care Navigators nationally nominated by 31 July. ICBs should work with regions to determine population appropriate share of nominations. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
50% of 2023/24 nominations by 31 July 2023 |
|
8. Understand and sign off PCN/practice capacity and access IIF CAIP baseline using guidance and Annex B template. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By 30 June 2023
|
|
9. Agree with practice/PCN support needs (digital telephony, online tools, training, capacity backfill, intensive support, etc). |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By 15 July 2023 |
| 10. Co-develop and sign off PCN/practice access improvement plans* leveraging example practice access improvement plans published by NHS England by 9 June. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By 31 July 2023 |
|
11. Assess improvement and pay 30% CAP IIF funding at the end of year using progress against baseline and access improvement plans, as well as improvement activity across all three areas over the year as per template in guidance and further guidance to be issued by 30 June. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Instruct PCSE by 6 August 2024 To be paid by 31 August 2023 |
12. Set up process for practices to inform of diversion to 111 and monitor exceptional use when over capacity. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Ongoing 2023/24 |
| 13. Develop system level access improvement plans which include summary of practice/PCN improvement plans, challenges, wider support needs and barriers and ICB actions (including leading local improvement communities, leveraging and promoting universal support offer, and improving the quality of core digital patient journeys for patients and staff and usability of practice websites supported by the national website audit tool).
|
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By October /November board 2023 |
*As specified in Network Contract DES IIF Capacity and Access improvement payment guidance. Plan should also cover all the items in this practice/PCN checklist
Commitment: Capacity
| Action for ICBs | Reporting | Time due |
|---|---|---|
|
14. Support PCNs to use their full ARRS* budget and report accurate complement of staff using NWRS portal |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Ongoing 2023/24 |
*The ARRS scheme is highlighted in the Delivery Plan for Recovering Access to primary care. The action is therefore included here, even though it is an ongoing action for ICBs.
Commitment: Reducing bureaucracy
| Action for ICBs | Reporting | Time due |
|---|---|---|
|
15. Report in public board updates and plans for improving the primary–secondary care interface (four focus areas highlighted in the recovery plan) |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
By October/ November board 2023 |
Commitment: Enablers
| Action for ICBs | Reporting | Time due |
|---|---|---|
|
16. Co-ordinate system comms to support patient understanding of the new ways of working in general practice including digital access, multidisciplinary teams and wider care available. This messaging should include system-specific services and DoS (Director of local services). |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Ongoing 2023/24 |
|
17. Maintain an up-to-date DoS and deliver training to all practices/PCNs on DoS. |
Report progress into public Oct/Nov 2023 board and public Apr/May 2024 board |
Ongoing 2023/24 |
Publication reference: PRN00310