Introduction
This guidance contains the information requirements, costing processes and costing methods for the acute, mental health, Talking Therapies for Anxiety and Depression and community sectors. Guidance for the ambulance sector is available separately. Note that Talking Therapies was previously known as IAPT and the data feed on the extract specification will still be call IAPT for 2024 NCC.
The integrated technical document provides detailed information on the data items, terminology and the calculations of the prescribed Approved Costing Guidance. It is important to work through it with the relevant costing standard for full understanding.
The guidance also refers to supporting information on our FutureNHS platform. You can access FutureNHS if you have an NHS email address or email costing@england.nhs.uk to request access if you do not.
You will find the Costing glossary invaluable for understanding the concepts and terminology underpinning the standards.
Information requirement
Before you implement Information Requirement (IR) standard IR1: Collecting information for costing, you should read and understand:
- Costing principle: Materiality
- bring in the information feeds that cover the largest service areas first.
- Sources for national datasets: learning extension available on FutureNHS.
You should have access to the integrated technical document, in particular:
- Spreadsheet IR1.1: Patient-level feeds
- Spreadsheet IR1.2: Patient-level field requirements for costing.
IR1: Collecting information for costing
Scope
-
This standard specifies the requirement for the activity feeds as prescribed in the Approved Costing Guidance for integrated trusts: most are at patient level and some require aggregated information.
-
The information feeds described in this standard include prescribed and development feeds.
Overview
-
This standard describes the main information feeds for input into the costing system:
- master feeds (patient event information feeds): for example the admitted patient care (APC), non-admitted patient care (NAPC) and emergency department (ED) feeds
- auxiliary feeds: the patient-level activity feeds that contain the components of the care, for example the diagnostic imaging and pathology feeds
- standalone feeds: for example to provide records to be costed for services that are not costed at patient level and are not matched to any patient event, for example the cancer multidisciplinary team (MDT) meeting feed
- allocation feeds: local information sources to support relative weight values, for example the estates floor area data showing square metres per service.
-
Critical care is also a master feed but has special properties. Where the trust does not have separate episodes for critical care it will be the main feed and for others it will be an auxiliary. Other auxiliary feeds such as pathology can be matched to it. This improves the quality of the costing of critical care stays. See Critical Care feeds 6a, 6b and 6c
-
Master feed events show the unit of care that is costed – a patient event. For example, an inpatient episode or community care contact.
-
Auxiliary feeds and allocation feeds are used to provide proportional information on which patients have used a service and so will have cost from that service allocated to them. For example, which patients have used a ward or received high-cost medicines.
-
The auxiliary feeds match components of the care for a specific patient on a specific date (tests, scans and medicines,) to the patient event on the master feed.
-
Some patient-level feeds will include the specific cost of item or care provided for the patient but most will not include cost as a data item.
-
Most of the data items required for master feed patient events are available in the submission your trust makes to the national dataset for the service area. You should use the national definitions of activity from these data sources. A list of the national datasets used for costing is given in the FutureNHS Sources for national datasets: learning extension. This list is not exhaustive and other national datasets may provide extra information.
-
Spreadsheet IR1.1 provides a list of the data feeds needed to bring data into your costing system.
-
Spreadsheet IR1.2 contains the activity data fields for the feeds in spreadsheet IR1.1, following national naming conventions for the national activity datasets.
-
In the integrated technical document in spreadsheet IR1.2 state the activity data extract specification field code and field name as required by the National Cost Collection (NCC).
-
The data fields required in each information feed are for costing, collection, matching or business intelligence. The reason each field is included in a feed is given in spreadsheet IR1.2.
-
The information feeds provide four types of information to inform cost allocation:
- activities that have occurred, for example the NAPC feed itemises contacts with the patient
- the cost driver needed to allocate costs, for example ward minutes
- information to weight costs, for example the medicine cost included in the medicines dispensed feed
- information about the clinical care pathway, for example procedure codes that are used to allocate specific costs in the costing process.
-
The information feeds include data items for the NCC: for example patient information for linking PLICS across organisations and sectors, for example NHS number.
-
The information feeds also contain data items used in CP4: Matching costed activities to patients. The matching process uses a combination of data items to create a Patient Level Extract Matching Identifier (PLEMI) linking between auxiliary feeds and the master feed patient event.
-
The PLEMI may contain data items such as a unique patient identifier, service code, and the date and time of the episode but this concatenated code must be unique within the trust.
-
Work with your informatics department to understand the different types of activity captured and reported for each data feed. You may need to contact the service areas for some feeds, as they have their own data managers. For example, pharmacy departments often manage the medicines information.
-
The standards prescribe the information to be collected but not how it is collected. If you collect several of the specified feeds in one data source, continue to do so. Record the source of the data item and any local definitions for patient events or component costs in the integrated costing assurance log (ICAL) worksheet 3: Local activity definitions.
-
Where a prescribed data item is not part of national dataset and you use a local dataset, also record the source of the data item and local definitions for this activity in ICAL worksheet 3: Local activity definitions.
-
You are not required to collect a patient-level feed if your trust does not provide that activity, for example a provider with no mental health care is not required to assemble the mental health feeds.
-
If your trust provides mental health, community or maternity services, you need to identify whether the Mental Health Services Data Set (MHSDS), the Community Services Data Set (CSDS) or the Maternity Services Data Set (MSDS) submission contains special characters. For onward linkage after collection, the data items in the costing system that are used for linking, should match the submission your trust made to the national dataset. If the PLICS feeds do not match the national data submission, your NCC submission will be compromised, as it linking to the national dataset will not be possible.
-
For the MHSDS, CSDS and MSDS, to build the relevant patient-level feed, you will need to work with your service teams or informatics department to map local field names to the information feed data items in spreadsheet IR1.2.
-
Any costs not allocated by the patient-level feeds need allocation feeds. These hold the local information sources that inform relative weight values (RWVs).
-
Where you use local sources of information for costing, document them in your ICAL worksheet 2: Additional information sources.
-
If you have activity in your data feeds where the costs are reported in another provider’s accounts, report this under ‘cost and activity reconciliation items’ as described in cost groups in CP5: Reconciliation. This is so your own patient costs are not allocated to this activity, deflating the cost of your own patients.
-
For internal reporting, the patient events where costs are reported in another provider’s accounts can be reported as part of patient pathways, even though the cost to the organisation is zero.
Additional patient-level activity feeds and data fields
-
The patient-level activity feeds specified above do not cover all patient activities involved in providing healthcare services or overheads.
-
You need to decide whether you require additional patient-level feeds to meet specific and material costing needs such as:
- offsite educational awareness/promotion
- immunisation programmes (for example site visits to schools)
- services provided to prisons and other secure locations
- primary care services.
-
Future development areas should be prioritised according to the costing principles and the following three criteria:
- value of service
- volume of service
- priority of the service within the provider and the healthcare economy.
-
If your trust already collects extra patient-level activity feeds in costing, we encourage you to continue and to record them in ICAL worksheet 2: Additional information sources.
-
Overheads and areas of general ledger (GL) disaggregation will need extra information entered in your costing system to create relative weight values (RWVs), so that the prescribed allocation calculation can be based on sound data. You should ensure this data comes from an appropriate source, the source is recorded and it is updated regularly.
Approach
Patient-level information for the costing process
- This section describes each information feed, explaining:
- accompanying costing standard(s)
- data collection source
- feed detail.
-
You should read the following sections describing the feeds listed in spreadsheet IR1.1 Patient-level activity feeds required for costing, in conjunction with spreadsheet IR1.2: Patient-level field requirements for costing and the FutureNHS Sources for national datasets: learning extension.
-
Your informatics team will be able to advise how to use the activity data in your local data systems, so you are working with the data sent to the national dataset and can reconcile to the patient events in your costing system.
-
You should reconcile your activity data regularly, to reduce the burden of the year-end process.
-
Activity for NHS-funded patients, private patients, overseas visitors, non-NHS patients and patients funded by the Ministry of Defence should be included in the costing system and costed. However, it is important to understand the type of patient for some cost allocations, and for reporting. The patient’s administrative category code in spreadsheet IR1.2 will supply this information. See CM7: Private patients and other non-English NHS-funded patients.
- Where your trust does not submit data to a national dataset but this is part of your ‘own patient care’ patient events, you should still have an electronic patient record. You should bring the events into the relevant feed, so all patient events can be costed. You should:
- Ensure your PLICS steering group is aware this information is not being submitted.
- Record this data in the local activity definitions on the ICAL worksheet tab 3, Local activity definitions and in your NCC activity reconciliation.
- Inform NHS England of why no submission is made to the relevant national dataset, and there can be no reconciliation between your National Cost Collection and the national dataset for this service. You should complete this MS form. This issue should also be logged and should form part of the NCC sign-off process.
Master Feed 1a and Feed 1b: Admitted patient care (CM13 Admitted patient care)
Data source
-
This data will come from the source used at your trust for the nationally collected and mandated admitted patient care (APC) Commissioning Data Set (CDS) (Feed 1a) or Mental Health Services Data Set (MHSDS) (Feed 1b).
-
The APC feed name is shown in spreadsheet IR1.2. The fields shown in this must be contained in the APC feed as these are required for the NCC.
-
For the most accurate mapping to mental health APC data, use spreadsheet IR1.2, which shows the MHSDS unique identifier codes for Feed 1b. There is no corresponding unique ID in the acute/community CDS for Feed 1a, so the field names listed should be used as the specific identifier.
-
You should take the data from the same source as your trust’s submission to the national dataset, using the same data as sent to the PLICS team at NHS England (formerly NHS Digital). This will allow the best possible reconciliation of your costed information to the national dataset.
Feed detail
-
Scope: all admitted patient episodes (all sectors) within the costing period, including all patients discharged in the costing period and patients still in bed at midnight on the last day of the costing period. This includes regular day or night admissions.
-
Each record is:
- an episode in Feed 1a (CDS)
- a spell in Feed 1b (MHSDS).
-
Use the patient discharged flag in spreadsheet IR1.2 to identify whether a patient has been discharged. Including patients who have not been discharged as incomplete patient events reduces the amount of unmatched activity and ensures discharged patients are not allocated costs that relate to patients who have yet to be discharged. See CM2: Incomplete patient events.
-
We recognise that some patient-level information, such as clinical coding, may not be available until after a patient is discharged. However, information on ward stays and named healthcare professionals will be available and can be used in the costing process.
-
Feed 1a includes one row for ‘ICD10 – secondary and subsequent diagnosis codes’. You can repeat this row by adding a #2, #3, #4, etc, to include as many ICD10 codes, in order, as required locally. This will allow improved reporting of specific diseases or comorbidities within the costing system.
-
Acute and community patients on Feed 1a should be identified as one of the nine ‘Episode Groupings’. See CM13: Admitted patient care, spreadsheet IR1.2 and the integrated extract specification for more information.
-
This data item enables the identification of community inpatients within the same feed as the acute inpatients, and so avoids the need for another input feed or output feed. Episode groupings are for patient-level costing use only.
-
Some patients may return home for planned or trial periods while still admitted to an inpatient bed. In acute settings this may be a ‘hospital at home’ arrangement for step down care, and in mental health settings it may be ‘home leave’ designed to ensure a bed is reserved for their care. The APC feeds include this home leave to reflect the organisation’s continuing responsibility for the patient. You should review CM13: Admitted patient care when costing home leave.
-
For private patients, the designation of ‘administrative category’ may change during an episode or spell. For example, the patient may opt to change from NHS to private healthcare. In this case, the start and end dates for each new administrative category period should be recorded in the start and end date fields respectively, in spreadsheet IR1.2.
-
Where a patient has a care programme approach (CPA) meeting during a mental health admission, the date of this will be included in the field ‘care programme approach review date’. This will be used to identify a ‘contact’ with the patient. The cost will therefore not be part of the admission, it will be costed and reported separately as a patient event. See CM3: Non-admitted patient care.
Master feeds 2a and 2b: Urgent care (emergency departments/minor injury units/walk-in centres) (CM4: Emergency care attendances)
Data source
-
The data will come from the source used at your trust for the nationally collected Emergency Care Data Set (ECDS) and the emergency department (ED) Commissioning Data Set (CDS).
-
The data for some walk-in centres and other unplanned care centre attendances may need to be collected locally where not included in the ECDS. This data will need grouping to an HRG to complete the information for reporting and the NCC.
-
The ECDS is the mandated dataset for emergency care and has replaced the CDS dataset in national commissioning. However, ECDS does not include the investigation and treatment fields used to group to the HRG codes, which are still required for costing, and a manual mapping table has been provided by the National Casemix Office. You should bring sufficient information into the costing system to perform the costing process from the ECDS and the ED CDS sources.
-
For clarity, we have retained the original Feed 2 (now renamed Feed 2a) and have added Feed 2b ECDS to signal the move towards the new dataset when the HRG grouping issue has been resolved.
Feed detail
-
Scope: all emergency department (ED), minor injury unit (MIU) and walk-in centre (WIC) attendances within the costing period, including all patients discharged in the costing period and patients still in the department at midnight on the last day of the costing period.
-
The ED feed requires the same terminology as the ECDS, so SNOMED-CT codes should be brought into the costing system for the emergency care procedure field.
-
The Casemix groupers do not yet group to the emergency care HRGs from SNOMED-CT, so you should also include the investigation and treatment fields and HRG codes from the previous dataset – the A&E CDS. These can be mapped from the SNOMED-CT codes using the mapping tool supplied on the Secondary Uses Services webpage. The process of mapping from SNOMED-CT to investigation and treatment codes and grouping to HRG is used for contracting, so your local contracting/income team may have further information
-
The ED, MIU and WIC attendances are not admitted patient care. If a patient requires admission, they will have an episode which will show on Feed 1a. If the patient is admitted to a hospital bed in the ED unit, they should have a treatment function code (TFC) of 180 – these are still admissions and not ED patient events. Use the patient discharged flag in spreadsheet IR1.2 to identify if a patient has been discharged from ED (including where they are admitted to a bed in the ED unit).
Feeds 3a, 3b and 3c: Non-admitted patient care (patient events from CDS, MHSDS and CSDS) (CM3: Non admitted patient care)
Data source
-
This data will come from your patient administration system (PAS) but relates to three different national datasets. The feed should be built based on how your activity data is submitted in the mandated national data weekly/monthly submissions:
- Your trust’s outpatient appointments submitted to the nationally collected Outpatient CDS, should be included in the PLICS on Feed 3a NAPC.
- Your trust’s mental health care contacts submitted to the nationally collected MHSDS, should be included in the PLICS on Feed 3b NAPC (mental health).
- Your trust’s community care contacts submitted to the nationally collected CSDS, should be included in the PLICS on Feed 3c NAPC (community).
-
You should take the data from the same source as the national submission of the CDS, MHSDS or CSDS for Feeds 3a, 3b and 3c respectively, before the data is sent. This will allow the best possible reconciliation of your costing data to the national dataset.
Feed detail
-
Scope: all outpatient or clinic attendances, care contacts or other patient events in a non-admitted care setting or within the community within the costing period. This includes non-face-to-face contacts such as telephone calls.
-
This feed captures activity recorded on the PAS but not reported in the other master feeds, including:
- outpatient attendances and procedures – formal booked or drop-in sessions in a clinic setting
- community contacts, including those in the patient’s own residence or mutually agreed location
- telemedicine consultations, including telephone calls, video conference, text, email and online patient model
- ward attenders (outpatient attendances where the patient is seen in a ward environment but does not need an admission)
- day care (patients attending for general supportive activities throughout a day, sometimes but not necessarily including clinical therapy); patients are not admitted, but are present for far longer than a standard NAPC contact
- NAPC contacts in groups for care, education, therapy
- individuals who are well but have contacts with clinical services for example, for health promotion, preventive medicine and education
- did not attend (DNA) – note: these are included on the feed for information but are not patient events in the costing standard. See CM3: Non-admitted patient care.
-
The NAPC feeds (feeds 3a, 3b and 3c) should not include the following areas, which have different field requirements and separate feeds:
- Feed 3d: Community midwifery contacts
- Feed 3e: Home births
- Feed 16: Improving Access to Psychological Therapies
- Feed 17: Sexual health anonymised contacts
- Feed 18: Community dentistry
- Feed 19: Wheelchair service
- Feed 26: Direct access audiology.
-
We recognise not all NAPC activity is captured in the PAS. You may need to work with your informatics department and the relevant department to get the activity information at patient level and log this local information source in the ICAL worksheet 2: Additional information sources. See also the FutureNHS Managing information for costing: learning extension on FutureNHS.
Master Feed 3d: Non-admitted patient care (NAPC) (Community Midwifery) (CM3: Non-admitted patient care)
Data source
-
This data will come from the source used at your trust for the nationally collected Maternity Services Dataset (MSDS).
Feed detail
-
Scope: all community midwifery care contacts within the costing period, including antenatal and postnatal contacts.
-
This feed is separate to feeds 3a, 3b and 3c as community midwifery is not a mandatory part of submissions to CDS, MHSDS or CSDS national datasets.
Master Feed 3e: Non-admitted patient care (NAPC) (home births) (CM3 Non-admitted patient care)
Data source
-
This data will come from the source used at your trust for the nationally collected Maternity Services Dataset (MSDS).
Feed detail
-
Scope: all patients who have a home birth recorded within the costing period.
-
This feed is separate to Feed 1a as we are aware, not all home births are recorded on the submissions to the CDS national dataset due to local trust issues. The clinical record in MSDS is a separate mandated dataset. You should ensure there is no duplication of home births when setting up this feed.
-
Given the nature of the patient events, matches to this feed are unlikely.
-
All home birth patient events require a valid HRG for reporting.
Feed 4: Ward stay
Data source
-
This data will come from a local source. It will largely be relevant to acute and community providers as the required data will not be in Feed 1a: APC. (For mental health services, ward data is in the MHSDS and so Feed 1b: APC mental health may include sufficient information.)
-
If you also have the required data in your main APC feed, this feed is optional.
Feed detail
-
Scope: All patients with part or all of an admission within the costing period: both those discharged and those still in a bed at midnight on the last day of the costing period. This includes but is not limited to patients on:
- general wards
- ED observation and clinical decisions wards
- rehabilitation and other long stay wards.
-
The ward stay feed is an auxiliary feed that is matched to master feeds.
-
Each record on this feed is either a complete or an incomplete episode.
-
Use the patient discharged flag in spreadsheet IR1.2 to identify if a patient has been discharged or not.
-
The start and end dates on Feed 4 Ward stay and Feed 1a APC should match to a high tolerance level. Any anomalies will be data quality issues and should be reviewed if there is a material number.
-
Critical care patient-level information is collected in a separate feed, so you need to exclude the critical care ward stay information from Feed 4: Ward stay, to avoid costing critical care twice. See feeds 6a, 6b and 6c: Critical care.
-
The applicable types of CDS ward stays are:
- 120 – Finished birth episode
- 130 – Finished general
- 140 – Finished delivery
- 150 – Other birth event
- 160 – Other delivery event
- 170 – Detained and/or long-term psychiatric census
- 180 – Unfinished birth
- 190 – Unfinished general
- 200 – Unfinished delivery.
Master feeds 6a, 6b, 6c: Acute critical care – neonatal, paediatric and adult (CM6: Critical care)
Data source
-
This data should come from the source used at your trust for the nationally collected:
- Neonatal Critical Care Minimum Data Set (NCCMDS)
- Paediatric Critical Care Minimum Data Set (PCCMDS)
- Critical Care Minimum Data Set (CCMDS).
-
This data source should show the bed days of the critical care period separately from the patient’s episode. This information is required for the NCC.
-
You should discuss with your informatics department how to obtain the data that is submitted to the national system, so you can reconcile the bed days to the relevant national dataset.
-
We know some providers open a new episode of care when a patient is transferred to a critical care unit, whereas others do not. We do not advocate one approach over the other. You should therefore understand whether your trust holds the critical care data:
- as a discrete episode with a transfer of care to a consultant, or
- as part of a patient episode under the surgical or medical consultant, where another data item (such as the type of ward) or source (such as the CCMDS for the area) will identify the critical care.
-
Your costing system should create an identifiable record for critical care, separate from the APC record, showing each bed day (or part thereof) in critical care.
-
In adult critical care we recognise that not all episodes are recorded at bed day level. Ways to do this include:
- using the separate episode from Feed 1a: APC, as the critical care record
- creating a separate critical care period record showing the bed days where there is no separate APC episode using:
- Feed 6: Critical care, as it will show the dates the patient had a critical care period according to CCMDS (recommended option) or
- Feed 4: Ward stay, to identify the patient moving to the relevant critical care unit. Please note this option may require extra attention where dates on the ward stay feed do not match Feed 6: Critical care, which could cause problems with reconciling the costed data to the CCMDS.
-
Whichever approach your costing system uses, you need to ensure there is a critical care record to keep these costs separate from the APC data record. Consult your software supplier for more information on how your costing system creates the costed record for critical care.
Feed detail
-
Scope: All patients who had a critical care stay within the costing period, including patients still in a critical care bed at midnight on the last day of the costing period. These patient events should be recorded on the national datasets noted above.
-
This includes but is not limited to patients on:
- intensive care units, also called intensive therapy units
- specialist care units, including specialist care baby units
- high dependency units
- general wards, with a CCMDS record (see CM6: Critical care).
-
We recognise not all critical care activity is reported to national datasets. You should note in your ICAL worksheet 26: CM6: Critical care, where the data is not reported nationally.
-
Where costing processes require your APC length of stay to be adjusted to distinguish the time spent on critical care, use the prescribed matching rules on spreadsheet CP4.1 to identify the appropriate dates/times and create the net length of stay on the APC feed.
-
Spreadsheet CP4.1 also includes the matching rules for feed 4: Ward stay, if you are using that method to identify the critical care days.
Auxiliary Feed 7: Supporting contacts – mandated for selected services
Data source
- This data will be available from local systems.
Feed detail
-
Scope:
- Patients receiving specialist rehabilitation outreach supporting contacts and specialist palliative care supporting contacts. These supporting contacts will be mandatory from 2023/24.
- Patients receiving care from interventional radiology and audiology as part of an episode under a different TFC. These supporting contacts will be mandatory from 2024/25.
- Patients receiving care from critical care outreach teams while on a non-critical care ward. These supporting contacts will be mandatory from 2025/26.
- All other patients who had contacts from anyone other than the healthcare professional named on the master record within the costing period.
-
A patient often receives multiprofessional services during their patient event, but this may not be noted on the master record. Feed 7: Supporting contacts is designed to reflect the multiprofessional nature of the patient’s pathway and the costs associated with it: for example, physiotherapists working with orthopaedic patients on a ward.
-
There is no national source data for this feed:
- where data is available from the service, there may be multiple sources for the different types of supporting contact activities. For example, physiotherapy supporting contacts will be on a different feed from the critical care outreach team contacts. They should all be brought into a single feed using the feed structure in spreadsheet IR1.2
- where no electronic data is available, you should consider the materiality of the cost allocation. If you consider it to be material, work with the service and informatics to record the necessary supporting contacts.
-
An admitted patient can be expected to have contact with their named care professional during their admission as part of standard ward rounds and ward care. This does not need to be included on Feed 7 supporting contacts but can be added if it enhances the detail available to the costed record; for example, where a consultant’s medical ward round data is available at patient level.
-
Spreadsheet CP4.1 contains the prescribed matching rules for this feed.
Auxiliary Feed 8: Pathology
Data source
-
This data will be available from local systems.
Feed detail
-
Scope: All types of pathology tests undertaken by the trust or purchased for patients within the costing period.
-
Direct access tests should be identifiable from the ‘direct access flag’ field, as shown in spreadsheet IR1.2. See also CM23: Direct access.
-
Pathology tests, especially specialist tests, are often run via operational partnership agreements for provider-to-provider services. See CM8: Clinical and commercial services.
- You should ensure you can identify tests performed for other organisations, and not include them in the matched activity to your trust’s own patient care events.
- Where your trust received tests from another organisation for your own patient care, obtain the data and add it to the feed, to be matched to patient events in the same way as for your own pathology department.
-
Certain pathological tests may be purchased from highly specialist private sector organisations; for example, genetic testing or products in the research and development phase. Where these are of material cost and relate to your trusts ‘own patient events’, get the cost of these tests and match to the patient event. See also CM21: Clinical non-pay items.
Auxiliary Feed 9: Blood service products (CM28: Blood services)
Data source
-
This data will be available from local systems.
Feed detail
-
Scope:
- units of blood and blood components used in transfusion (red cells, white cells, platelets, plasma and other blood products)
- also Car-T Cell therapy, which is the patient’s own blood, collected, processed by a third party and given back to the patient.
Auxiliary Feed 10a Medicines dispensed and standalone Feed 10b: Home delivery medicines dispensed from third party (CM10: Pharmacy and medicines)
Data source
-
Feed 10a data will be available at patient level from local systems and will include the NHS Payment Scheme high cost drugs, chemotherapy drugs and the mandated drugs patient-level monitoring (DrPLCM) specification for specialised commissioning of high cost drugs. This covers approximately 70% of high cost medicines nationally, which may be extended by including locally commissioned high cost medicines.
-
Feed 10b may be used to include data from homecare medicine delivery contracts, where this data is available.
Feed detail
-
Scope: medicines dispensed in all provider locations including:
- medicines issued to the patient’s residence
- medicines attributable to individual patients (including high cost drugs, controlled medicines, medicine gases issued in bulk and discharge items)
- chemotherapy medicines
- medicines not attributable to individual patients (for example ward stock) within the costing period.
-
The medicines feeds will contain the cost of the medicine dispensed, to be used for a proportional allocation of cost. See CM10: Pharmacy and medicines.
-
FP10s are the prescriptions issued from hospitals and are out of scope of the medicines dispensed feed. You may include an FP10 feed at patient level as a superior costing method if this information is available.
Auxiliary feeds 12a, 12b, 12c: Diagnostics – imaging, maternity ultrasound and clinical physiology services
Data source
-
This data will be available from a range of clinical information systems.
- Feed 12a Diagnostic imaging data will be available from the clinical radiology information system or picture archiving and communications system (PACS) (diagnostic imaging) and other local systems. This system may also be known as radiology information system (RIS) or clinical radiology information system (CRIS).
- Feed 12b Maternity ultrasound data will be recorded in the local maternity system used to submit to the maternity services data set (MSDS).
- Feed 12c Clinical physiology will come from a range of local systems specific to the physiology service.
-
You may bring the data into the costing in a single feed containing all the information, or into multiple feeds, according to local system configuration.
-
Feed 12b should show the ultrasound scans undertaken in maternity patient events which are not recorded on the main diagnostic imaging system but should be clinically coded. It may also include other types of diagnostics if not recorded in another system. See CM24: Maternity.
Feed detail
-
Scope: all diagnostic imaging (Feed 12a) and clinical physiology (Feed 12c) scans and tests performed within the costing period, including maternity ultrasound (Feed 12b).
-
The diagnostic feeds are auxiliary feeds that are matched to master feeds.
-
Direct access tests should be identifiable from the ‘direct access flag’ field as shown in spreadsheet IR1.2.
-
You should ensure that ultrasound scans are not duplicated in both Feed 12a and Feed 12b. The pregnancy identifier is available in Feed 12b: ensure any scans relating to a maternity pathway are included in Feed 12b or elements will be missing from the maternity pathway reporting.
Auxiliary Feed 13: Theatres and specialist procedures suites (CM5 Theatres and specialist procedures suites)
Data source
-
This data will be available from local systems.
Feed detail
-
Scope: all procedures performed in theatres and specialist procedure suites within the costing period.
-
This feed should be at patient level, including time points, so the system can calculate pre-op, anaesthesia, surgical time, recovery and other relevant time sections.
-
This feed should also include session information to enable costing of staff to particular operations.
Feed 14: Cancer multidisciplinary team (MDT) meetings (CM9: Cancer MDT meetings)
Data source
-
This data will be available from local systems.
Feed detail
-
Scope: all cancer MDT meetings held within the costing period.
-
This standalone feed is not matched to master feeds and has no auxiliary feeds matched to it.
-
This feed does not have to be at patient level as the costs for MDTs are reported at specialty level rather than patient level.
Auxiliary Feed 15a: Prostheses and other high cost items and Feed 15b Homecare clinical items, personal equipment and consumables
Data source
-
This data will be available from local systems.
-
The high cost drugs and blood products listed in the integrated extract specification should be shown separately to the core patient event by inclusion on the supplementary information (SI) feed. This list has been created by combining worksheet 14b of the NHS Payment Scheme high cost drugs list, the specialised commissioning drugs taxonomy list and the specialist commissioning chemotherapy taxonomy list. Commissioning data will be available for these items.
-
A wider range of devices, consumables and personal equipment may be recorded in inventory management systems that track clinical non-pay items to the patient. Using this source of information for material non-pay items is a superior costing method.
-
If an inventory management system is not available, national programmes such as Scan4Safety or the National Joint Registry are useful sources of patient-level information for prostheses, devices and implants.
Feed detail
-
All prostheses, devices, implants and clinical non-pay items with a material cost provided to patients in clinical settings or at home, within the costing period.
-
The homecare clinical items, personal equipment and consumables feed is an auxiliary feed but is not expected to match to any master feed patient events.
-
Feed 15a is an organisation-wide feed to cover clinical non-pay items with a material cost, not just those used in theatres. Key areas to review are interventional radiology, cardiac devices inserted in catheter labs and assisted reproduction.
-
Feed 15b brings in items supplied to the patient’s home, so the costing system can report on the services vital to safe and effective care outside the hospital setting.
Master Feed 16: Improving Access to Psychological Therapies (IAPT)
Data source
-
This data will be available from local systems, in accordance with the submission of IAPT data.
Feed detail
-
This feed should contain the non-admitted contacts for IAPT services that are not recorded in the MHSDS dataset.
-
It is unlikely there will be any auxiliary feed matches.
-
As the fields available in IAPT are not the same as in the MHSDS we are treating this as a separate feed. The costing processes should be the same as those for CM3: Non-admitted patient care.
Feed 17: Sexual health
Data source
-
This data will be available from local systems.
Feed detail
-
Scope: all sexual health contacts within the costing period that are not recorded in the standard NAPC feeds.
-
This is a standalone feed and therefore should not be matched to any other feeds.
-
These may be pseudonymised contacts.
-
If used as a master feed, the sexual health feed patient events can have auxiliary feeds such as pathology matched to them, to show the testing part of the care. If the contacts are anonymised or pseudonymised, this may not be possible. See CM16: Sexual health services.
Master feed 18: Community dentistry
Data source
-
This data will be available from local systems.
-
There are three types of data for dental activity:
- in the main PAS as admission episodes (included in the APC feed, out of scope for this feed)
- in the main PAS as outpatient attendances (included in the NAPC feeds, out of scope for this feed)
- in a separate local system for community dentistry activity (in scope for this feed).
Feed detail
-
Scope: all community dentistry contacts are in scope of this feed. This may include personal dental services.
-
It is unlikely there will be any auxiliary feed matches.
-
The feed should show the unit of dental activity as this is used for costing and local reporting.
-
This feed should not contain hospital-based dentistry data already recorded as part of the CDS. This information should be in Feed 1a: APC and Feed 3a: NAPC.
Master Feed 19a Wheelchair contacts and auxiliary Feed 19b: Wheelchair equipment (CM19: Wheelchair services)
Data source
-
This data will be available from local systems.
-
There are two types of data for wheelchair activity for this feed:
- wheelchair service contacts either recorded in the main PAS or in the local wheelchair system. If PAS data is used, additional data items are required to show the currencies (see CM19: Wheelchair services)
- the value recorded against each item of equipment issued to a patient as recorded in the wheelchair system.
Master Feed 19a: Wheelchair contacts
Detail
-
Scope: wheelchair contacts within the costing period regardless of whether they are recorded on the main PAS or a separate clinical information system. You should ensure there is no duplication of data between NAPC feeds and the wheelchair feed.
-
The only anticipated match for Feed 19a would be auxiliary Feed 19b: Wheelchair equipment.
-
The feed should show the nationally defined level of patient need as this is a unit used for local reporting and national currencies – this information would normally only be included in the wheelchair system. An optional field has also been included in the data items in spreadsheet IR1.2 to record a locally defined level of need if this gives greater detail/specialisation.
-
The feed should have a patient identifier and date so analysis and reporting can show wheelchair equipment with the patient contact(s). The cost of equipment should not be absorbed into the wheelchair contact.
Auxiliary Feed 19b: Wheelchair equipment
Feed detail
-
Scope: all wheelchair equipment and accessories issued to a patient (including where a patient representative collects the items or they are delivered to the patient’s residence) within the costing period.
-
The anticipated match for Feed 19b would be Feed 19a: Wheelchair contacts, so any other matches should be reviewed.
-
The feed should include the cost of the equipment or the cost of reconditioning equipment before reissue to a patient.
-
The feed should have a patient identifier and date so analysis can show the total cost of wheelchair services for the patient but the cost should not be absorbed into the wheelchair contact(s).
- Equipment will not be issued at all contacts, and there will not necessarily be a contact with a wheelchair professional on the date equipment is issued.
Feed 25: Specialist rehabilitation (CM36: Specialist rehabilitation)
Data source
-
This data will come from the source used at your trust for the nationally collected CDS or United Kingdom Rehabilitation Outcomes Collaborative (UKROC) submission.
Feed detail
-
Scope: patients receiving specialist rehabilitation in a discrete unit.
-
This feed provides extra information to capture the rehabilitation complexity score and associated dates.
-
The patient events created as HRGs by the grouper should be brought into the PLICS as a feed so they can be costed as patient events separately from the admission:
- the feed should contain the categorisations of rehabilitation as defined by (UKROC:
- complex specialised rehabilitation services – level 1
- specialist rehabilitation services – level 2
- non-specialist rehabilitation services – level 3
- or show a null categorisation.
-
As reporting the point of delivery for these HRGs is also a requirement, a field is included for this manual allocation based on your data:
- admitted patients with overnight stay (elective and non-elective)
- day case
- regular day/night admissions
- outpatients/contacts (non-admitted)
- other – this category has been included to understand if there are any types of activity not included above.
Feed 26: Audiology contacts (CM22: Audiology services)
Data source
-
This data will be available from local systems.
-
All audiology contacts should be included in the costing system. The contacts may be loaded via Feed 26: Audiology contacts or Feed 3a: NAPC. You should ensure there is no duplication of patient events between these two feeds. Feed 26 is available to assist the reconciliation of patient events, where audiology is not included in the main PAS and CDS submissions.
Feed detail
-
Scope: all patients receiving audiology services, where they are not contained in Feed 3a: NAPC. This should include:
- direct access audiology patients (GP direct access and ongoing audiology care): these are audiology patient events
- patients having ongoing care following discharge from an acute pathway: these are audiology patient events
- patient events where the responsible clinician is in another specialty – and the audiology contact supports that service area. These are components of the patient event in the named TFC within NAPC, APC or ED. These contacts should be used in the costing system to support allocation of audiology cost as component of the other TFC, not as an audiology TFC patient event.
Feed 27: Maternity Services identifiers: mandating year 2024/25 (CM24: Maternity)
Data source
-
This data should come from the local source used for the nationally collected Maternity Services Data Set (MSDS).
Feed detail
-
Scope: maternity patient events as recorded on the MSDS including the pregnancy identifier, the antenatal appointment booking date, the maternity discharge date to identify when patient events relate to maternity services, and the discharge from delivery event date for identifying postnatal contacts following a delivery event. This feed is used for pathway reporting.
-
This feed is used to connect mother to baby, and mother/baby to pregnancy, so the whole pathway can be reported. It can be used to link feeds 1a and 3a (which do not have a pregnancy identifier) to feeds 3d, 3e and 12b. There is no costed output to patient events from this feed.
Feed 28: Radiotherapy (CM26: Radiotherapy)
Data source
-
This data should come from the source used at your trust for the nationally collected Radiotherapy Data Set (RTDS). Extra information may be required from your main PAS or other local sources.
Feed detail
-
Scope: patient events showing all radiotherapy planning HRGs and treatment attendance HRGs. There will usually be multiple treatment events for each planning event.
Feed 29: Chemotherapy (CM25: Chemotherapy)
Data source
-
Patient NAPC information will be available from local systems. APC care will be available from PAS.
-
The medicines information will be available from the local e-prescribing system, as it is mandatory to record chemotherapy and supporting medicines at patient level (see Feed 10a: Medicines dispensed).
Feed detail
-
Scope: all patient events where chemotherapy was delivered.
Master feed 30: Renal dialysis (CM37: Renal dialysis)
Data source
-
The patient information will be available from local systems. All renal dialysis patients are admitted for their treatment, but this information may not be within the main PAS or the CDS. The episodes may be loaded via Feed 30: Renal dialysis or Feed 1a: APC if the additional data items for renal dialysis are included in that feed.
-
You should ensure there is no duplication of patient events between these two feeds. Feed 30 is available to assist the reconciliation of patient events, where renal dialysis is not included in the main PAS and CDS submissions.
Feed detail
-
Scope: all patients undergoing renal dialysis within the costing period, including those still in a bed at midnight on the last day of the costing period.
Identifying hidden activity
-
Take care to identify any ‘hidden’ activity in your trust. This is activity that takes place in your trust but is not recorded on any of your trust’s main information systems, including PAS.
-
For example, a department may not record telephone activity on PAS. If this is the case, you should work with your informatics department and the service to obtain a feed containing 100% of the patient events undertaken by the department. This work is part of the NHS Long Term Plan to improve digitally enabled care, benefiting staff and patients.
-
Capturing ‘hidden’ activity is important to ensure that:
- costs incurred are not incorrectly allocated to recorded activity, thus inflating its reported cost
- patient-facing and overhead costs incurred are allocated over all activity, not just activity reported on the provider’s main system such as PAS
- income received is identified against the correct service.
Other data considerations
-
The patient-level feeds do not contain income information. You may decide to include an income feed at patient level to enhance your trust’s reporting dashboard. The standards refer to income where this makes it easier to understand both the costs and income for a particular service for cost reconciliation, local reporting, business intelligence and where there is special treatment of income for the National Cost Collection.
-
The feeds do not include description fields, for example there is a ward code field but not a ward code description field. You may ask for feeds to include description fields for ease of use; otherwise, you will need to maintain code and description look-up tables for each feed, so you can understand the cost data supplied and facilitate appropriate outputs for reporting. There should be a process for mapping and a rolling programme for revalidating the codes and descriptions with each service.
-
You may use locally generated specialty codes to report patient events locally. For example, epidermolysis bullosa will be reported under the dermatology TFC but your provider may decide to assign it a local TFC code, so this specialist activity is clearly reported.
-
If local TFC codes are used, they should still be included in the patient level feeds and in the costing process, as they need to be allocated correctly. You should maintain a table mapping the local specialty codes to the national TFCs, to ensure consistency with the information submitted nationally for reconciliation purposes.
Legally restricted sensitive data
-
Some costed records should not be reported locally or submitted to the National Cost Collection at patient level, for information governance reasons. The costing system will manage these in different ways:
- Pseudonymised records are where the patient record has had patient identifiable information removed but the system keeps a key to track back to the patient.
- Anonymised records are where the patient record has the patient identifiable data removed but without a key.
- Proxy records are where no patient record is available for costing, so a ‘record’ is created to show the cost of care.
Proxy records
-
Proxy patient event records can be created to provide patient records to attach cost where there is no other record – for example:
- where there is no patient event to attach the component costs care provided, such as homecare delivered medicines or equipment
- to provide anonymous costed records for services that need to cost ‘a’ patient not ‘the’ patient: for example, LRSD patient events.
-
You will need a suitable source of local information to create the correct number of proxy records, provide sufficient detail for the costing process, and agree this within your assurance process (see the FutureNHS Assurance of cost data: learning extension). These should conform to the same criteria as the relevant national dataset but remain clearly identifiable as proxy records.
-
You should avoid generating proxy patient records within the costing system to solve data quality issues or to create an electronic record where there is only a paper record for the patient event as this can lead to double counting of activity outputs. For example, if someone later adds a missing record and it flows through to the costing system, both the proxy record and the correct record will receive costs for the same activity. It is better practice to work with your informatics department and service teams to create the correct electronic data entry in the ‘right first time’ principle.
-
Proxy records should be noted in your ICAL worksheet 16: Proxy records. They should also appear in the activity reconciliation – as described in Standard CP5: Reconciliation – as the costed patient records will not reconcile to the in-house or national dataset.
Part cost flag
-
Where part of the patient care cost relates to different organisations, the total cost of the patient event will not show a ‘complete’ value. For example:
- where part of the care is provided by an independent sector provider, and the remaining care is provided by the NHS trust
- where two (or more) NHS trusts in an integrated care system (ICS) provide care for the same patient event, without a recharge of the cost between organisations.
-
To identify records where the cost is not complete, you should identify the patient event with a ‘part cost flag’.
Costing processes
Before you implement the costing processes (CPs), you should have access to the integrated technical document, in particular:
- spreadsheet CP3.1: Resources for patient-facing cost
- spreadsheet CP3.2: Activities for patient-facing costs
- spreadsheet CP3.3: Methods to allocate patient-facing resources, first to activities and then to patients.
CP1: Ensuring the correct cost quantum
Scope
-
This standard applies to all lines of the general ledger (GL).
Overview
-
You need the income and expenditure for costing. We refer to this as the GL output. This output needs to be at cost centre and expense code levels and is a snapshot of the general ledger at a point in time. Expense codes may also be called ‘account codes’ or ‘subjective codes’.
-
You do not require balance sheet items for costing.
-
If your charitable funds are in your general ledger, they should be identified and not included in the costing system, except where costs funded by charitable funds have been transferred to own patient care services.
-
You can bring your general ledger into your costing system, either bringing in:
- the trial balance: for audit purposes this should balance to zero, or
- only the cost and income: this should reconcile to your statement of comprehensive income.
To reduce the burden on your costing system, we recommend the second approach
-
As a minimum, you should bring the values into the costing system each quarter. This allows regular work to map the GL combinations in the costing system in a manageable way. Leaving this process to the year end will lead to more burden for both costing and wider finance teams.
-
As a superior costing method, SCM83: Loading finance data from the general ledger monthly, you can bring your financial values into the system in the cycle that is recognised by financial management teams. Loading financial values more frequently can enable swifter resolution of mapping problems and allow more accurate adjustments.
-
The general ledger is closed at the end of the period, after which it cannot be revised (although some systems may allow you to back post payroll journals and to make other changes during the external audit process). For example, if in March you discover an error in the previous January’s ledger, the correction can only be made in March’s ledger. Doing so will correct the year-to-date position, even though the January and March figures do not represent the true cost at those times: one will be overstated and the other understated. Check with other finance team colleagues to ensure only final closed periods that contain any such changes are brought into the costing system.
-
If such corrections are material, you may choose to amend the costing system GL input with a journal, ensuring an audit trail of such adjustments to ensure reconciliation.
-
The timing of reporting some costs in the general ledger may pose a challenge. For example, overtime pay for a particular month may be posted in the general ledger in the month it was paid, not the month it was worked. This highlights a limitation in the time-reporting and expense payment system. We recognise this limitation but are not currently proposing a work-around for it.
-
Discuss the GL layout and structure with the other finance team colleagues so you understand it. This will help you understand the composition of the costing output. The Financial accounting and reporting page on the NHS England website can also help you understand your GL structure.
-
Keep a record of the input of cost into your costing system for each costing period. There may be multiple loads and we recommended each load is noted in the ICAL worksheet 12: GL load record.
Approach
Obtaining the general ledger output
-
Finance team colleagues should tell you when the general ledger has been closed and give you details of any off-ledger adjustments for the period. You need to put these adjustments into your cost ledger (CL), especially if included in your trust’s financial position report, as you will need to reconcile to this.
-
Keep a record of all these adjustments in ICAL worksheet 11: Adjustments to the general ledger at each load, to reconcile back to the GL output. Take care to ensure any manual adjustments are mapped to the correct line of the cost ledger.
-
Ensure the process for extracting the GL output is documented in ICAL worksheet 8: Extracting GL output. You should extract this only after the finance team colleagues tell you they have closed the general ledger for the period.
-
You should be notified when new cost centres and expense codes have been set up in the general ledger.
-
Trusts should not rename, merge or use existing cost centres for something else without informing you, as not knowing when this has been done will cause problems for costing. Ideally, they should close a cost centre and set up a new one rather than renaming. If this is not possible, they should tell you about any changes.
-
The new GL cost centres and expense codes need to be mapped to the cost ledger. You then need to reflect these changes in the costing system.
-
‘Error suspense’ ledger codes need to be addressed so that all costs can be assigned accurately to patients. Work with your finance colleagues to determine what these codes contain so the contents are mapped to the correct lines in the cost ledger. Note: organisations may use a different name for these codes, such as ‘holding’ or ‘dump’ ledger codes.
-
You should have a rolling programme of regular meetings with your wider finance colleagues to review the general ledger and its role in costing. This can identify problems and enhance their engagement with use of the data.
-
Where income from a charitable donation appears in the general ledger it should be aligned with the cost centre and expense code where the expenditure is recorded, using the income code in spreadsheet CP2.1 to identify it. This allows compliance with both costing standards (income should be identifiable) and collections (charitable income can be netted off from the cost which it funded).
-
Where charitable cost centres are in the general ledger, the expenditure and income on the cost centre should net to zero at the end of the costing period. The income not used would normally be deferred until the next period: but you should review any negative balances on the charitable fund cost centres and ensure the costing system does not offset the income against the cost of own patient care cost group. A set of charitable fund cost centres are shown in the cost ledger as cost centre codes starting with WWW for transparency.
CP2: Clearly identifying costs
Scope
-
This standard applies to the general ledger (GL) in conjunction with the GL load described in CP1: Ensuring the correct cost quantum.
Overview
-
Costing processes should identify and consistently allocate costs to enable meaningful analysis locally and nationally.
-
A trust’s general ledger is normally set up for local requirements rather than to support the standardised cost process. This means they will vary in structure.
-
This standard aims to ensure a process is in place to take this into account when the costing process starts, ensuring costs are mapped to resources consistently. To achieve this, the Approved Costing Guidance uses a standardised cost ledger (CL).
-
The cost ledger ensures that as part of the costing process, all costs across the NHS are categorised and allocated in the same way. This process is called general ledger to cost ledger (GL to CL) mapping.
-
This standard describes a flexible approach that enables you to decide between two methods of GL mapping:
- Method 1 Essential mapping: This method will take your GL chart of accounts directly to the collection resources or overheads. In completing method 1 you should ensure you do not miss costs that need remedial action to get them in the right place to start the costing process.
- Method 2 Full mapping: This method will take your general ledger and map all the GL codes to the standardised cost ledger.
-
This standard describes the process for method 2 mapping as this is our preferred approach for most organisations. It also details how you should allocate overheads to patient-facing resources so they can be distributed to activities. See the FutureNHS Ledger mapping: learning extension on FutureNHS.
-
As part of your costing process, you may encounter elements of negative cost. The treatment of these is explained in General ledger negative costs
-
Some areas of your ledger will need specialist treatment. You should ensure you understand and implement CP5: Reconciliation and CM8: Clinical and commercial services.
Approach
The following key principles enable you to clearly identify costs and allocate them according to the prescribed methodology (see CP3: Allocating costs to activities):
- Patient-facing costs:
- relate directly to delivering patient care and are driven by patient-facing activity
- can be either pay or non-pay and should be allocated using an activity-based allocation method
- are grouped into resources for allocation and linked to costing activities in the costing process.
- Overheads do not directly relate to delivering patient care; many relate to running the organisation. For example, they may be a corporate service, such as finance, or at a service level, such as ward clerk.
- Corporate overheads such as finance and HR are allocated to all services that used them, using a code starting T1S, each with a prescribed allocation method. These costs should not be directly mapped to resources and activities in the costing process.
- Income can be clearly and transparently identified.
-
You should work with your financial management team to ensure costs are aligned to the correct location in the cost ledger, starting with the most material items.
Mapping methods
-
You may choose to implement either method 1 or method 2 change mapping to meet the needs of your trust; combine mapping methods if that better represents your trust.
-
Whichever method you choose:
- you must understand the general ledger, especially larger items, and make sure costs are mapped appropriately to resources
- ensure the costing system reconciles at resource level; otherwise, further steps will not reconcile and may prove more complex to unravel. Refer to CP5: Reconciliation and the FutureNHS Assurance of Cost data: learning extension.
-
Over time, all trusts should aim to use method 2 mapping where method 1 does not ensure consistency for national level analysis. For example, where different allocation methods are prescribed by costing resource and costing activity level but only one allocation method is possible at collection resource and collection activity level.
-
You may wish to retain some elements of method 1 mapping if that is more suitable for your environment.
-
Figure CP2.1 shows the application of the cost ledger to the trust’s general ledger in the two mapping methods.
Figure CP 2.1: Mapping methods
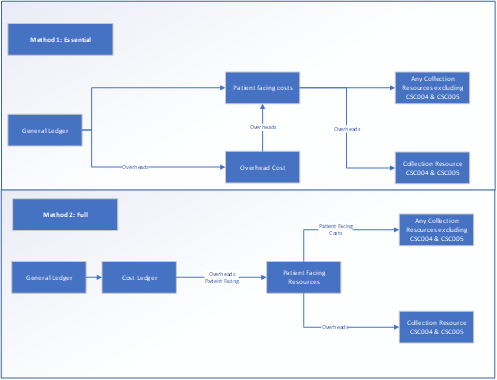
This figure outlines the two mapping methods. Essential method 1 maps costs flowing from the general ledger to overhead costs and patient facing costs and then from patient facing costs to a) any collection resources excluding CSC004 and CSC005 and b) collection resources CSC004 and CSC005. Full method 2 maps costs flowing from the general ledger via the cost ledger to patient facing resources and from there to patient facing costs (any collection resources excluding CSC004 and CSC005) and overheads (collection resources CSC004 and CSC005).
-
Complying with method 2 involves an in-depth investigation of the general ledger to understand the costs it contains.
-
You should ensure it does not become too time consuming: focus on material areas initially and plan to review other areas periodically.
-
Method 2 provides a way to get the costs into the right starting position with the appropriate label – that is, from your GL to the CL costing account codes, and then to the correct resource codes.
-
Method 1 is more straightforward and aggregates costs to collection resources. Benefits include the ability to establish a holistic view of your GL costs.
-
If you use method 1, you should retain evidence of your mapping exercise if this cannot be completed in your costing software. It should evidence that all material costs have been considered.
-
Regardless of mapping method, you should still comply with the prescribed resource and overhead allocation methods in spreadsheets CP2.2 (for overheads) and CP3.3 (for patient-facing resources). See CP3: Allocating costs to activities. You should not use locally defined allocation methods to allocate costs.
-
There is additional risk of inaccuracy if adopting method 1. Trusts should be aware of these risks and plan appropriate mitigations.
-
If as an organisation, you choose not to complete the full GL to CL exercise, it is still important to understand method 2. The FutureNHS Ledger mapping: learning extension outlines the main premises of the two mapping methods in more detail.
Implementing method 2
-
The cost ledger outlines a chart of accounts that will cover most costs in many trusts but is not exhaustive. Where it does not have a combination of cost centre and expense code required for your trust, you should refer to the resource application hierarchy (RAH) tool on FutureNHS and customise your cost ledger.
-
Although the initial GL to CL mapping is a one-off exercise when setting up your PLICS; you should review it at least once a year, in line with the refresh of the integrated technical document. This is to ensure your cost ledger remains representative of how the costs in each part of your general ledger are used for costing.
-
The process of GL to CL mapping may run incrementally or simultaneously. For ease of understanding, we describe the process in linear steps.
-
The transformation of the general ledger into the resources should occur within your costing system to ensure mappings can be traced and reconciled to your general ledger.
-
If, in your costing system, the costing process takes place at a more granular level than the prescribed costing resources, you may continue using this method. The use of local resources or cost items will require the implementation of an additional mapping process. You should log the method you use in ICAL worksheet 15: Superior costing methods.
-
Your actions should include:
- Disaggregation: Some costs may be reported in the general ledger at a level not detailed enough for patient-level costing; for example, where multiple costs are combined in a single GL code. These costs need to be disaggregated when creating the cost ledger, using an appropriate method.
- Aggregation: Some costs may be reported separately in the general ledger but can be aggregated for patient-level costing when creating the cost ledger to simplify areas with the same treatment.
- Remedial actions: If a material cost has been incorrectly recorded in the general ledger, it should be corrected at this point.
-
At the same time or following the system process to put the costs into the right starting place following the GL to CL mapping, the costing software will undertake a process called reciprocal costing. Figure CP2.2 describes the costing process from general ledger to collection resources.
Figure CP2.2 Simplified costing process
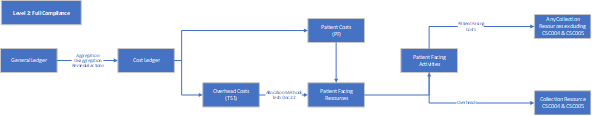
Figure CP2.2 is a flow diagram outlining a simplified costing process from general ledger to cost ledger then overhead costs and patient costs feeding into patient facing resources and from there to patient facing activities.
Treatment of overheads (including reciprocal costing)
-
Certain costs in your general ledger are not patient facing but provide support services for clinical and non-clinical areas. These are called overheads and refer to expenses associated with running a trust that cannot be directly linked to the treatment of a patient. They are incurred regardless of activity level.
-
Overheads should be allocated to the cost centre(s) which used the service using prescribed allocation methods. Once the overhead has been allocated to the cost centre(s), it should be apportioned to the expense codes within the cost centre(s).
-
Overheads are grouped into overhead titles and assigned a T1S code in spreadsheet CP2.2. Each T1S code, and its allocation method, is shown in spreadsheet CP2.2.
-
As a superior costing method, SCM84: Overhead costs (patient level), you may use an appropriate two-step allocation method which incorporates a patient event-based allocation method. See Figure CP2.3.
Figure CP2.3 Simplified GL to collection output
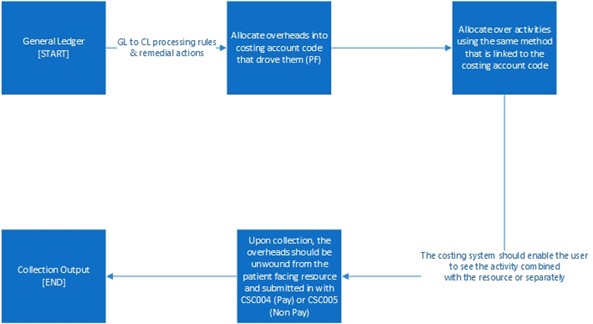
Figure CP2.3 describes the treatment of overheads from the general ledger to cost ledger to collection. Overheads that have been absorbed into patient-facing resources need to be separated for the cost collection and grouped into the two support collection resources: CSC004 (Pay) and CSC005 (Non-Pay).
-
Using an expenditure-based allocation method, some ledger areas may get a larger proportion of allocated overheads because of specific high-cost items.
-
Costs that may affect the allocation calculation include Clinical Negligence Scheme for Trusts (CNST), high cost medicines, interventional radiology/nuclear medicine consumables or prostheses. If so, investigate and correct the overheads allocation and adjust the allocation to allow for this. Any amendment to overheads should be recorded in your ICAL worksheet 13: Percentage split of allocation bases. See the FutureNHS CNST briefing paper.
Devolved and centrally held costs
-
During your GL review, it is important to identify whether a cost is centrally held or has already been devolved to the relevant cost centres in the cost ledger – for example, as part of service line reporting. You should discuss the allocation method used for devolving costs with your financial management department, so you can understand whether the devolved general ledger represents costs allocated using a method prescribed for costing.
-
Once understood, you can identify any steps needed to put the costs in the correct starting place for the costing process as follows:
- Held centrally: use the prescribed allocation method.
- Already been devolved to the cost centre that used it, using the prescribed method or a superior costing method: no action – costs are already in the correct place and you do not need to aggregate the costs.
- Already been devolved to the cost centre that used it but not using the prescribed method or a superior costing method: aggregate to a central code, so the process will use the prescribed allocation method.
Reciprocal costing
-
This standard prescribes reciprocal costing enabling allocation of overheads across patient facing and other overhead cost centres, as all those services have ‘used’ the cost of the overhead.
-
You should do this using a reciprocal allocation method, which allows all corporate support service costs to be allocated to, and received from, other corporate support services. For example, HR costs should be allocated across all cost centres that have staff, as all staff benefit from HR services.
-
Reciprocal costing must take place within the costing system.
-
A reciprocal allocation method reflects the interactions between supporting departments and therefore provides more accurate results than a hierarchical approach.
-
Overheads should not be allocated using a hierarchical method as this will only allow cost to be allocated in one direction between corporate support services. See Figure CP2.4.
Figure CP2.4 Reciprocal costing
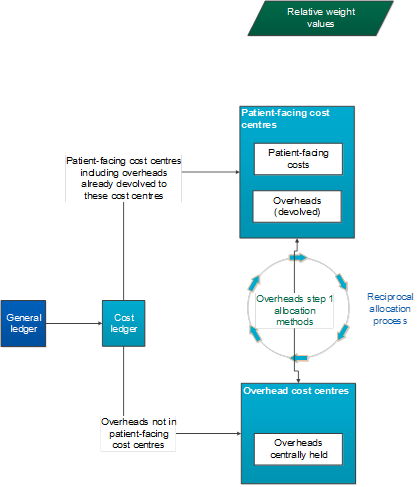
Figure CP2.4 describes reciprocal costing and the allocation of overheads across patient facing and centrally held cost centres.
-
Following this process, patient-facing costs with their allocated portion of overheads are mapped to resources.
General ledger negative costs
-
A negative cost is a balance less than zero on a costing account code that is for expenditure. This code would normally have a positive balance to show the expenditure.
-
Negative costs flowing into the costing system can cause problems in calculating an appropriate cost for a patient event, as it reduces the true cost of the care. Where a negative cost is significant, the impact may even show as patient events that have a negative cost. These are not accepted in the National Cost Collection, as this situation should not be possible.
-
When doing the final, full-year costing process for the National Cost Collection, many negative balances that show in the monthly or quarterly reporting will disappear, as the expenditure in that costing account code will be sufficient to offset them. However, you should monitor negative balances throughout the year, to ensure major issues do not occur. See the FutureNHS Negative costs: briefing paper.
Cost classification
-
Classifying costs as fixed, semi-fixed or variable is not part of the costing calculations but rather a classification showing how costs behave based on level of activity. It is therefore used for reporting purposes, based on national classification rules given here and in spreadsheet CP2.1 The standardised cost ledger.
-
This classification is important for a trust’s internal financial management and discussions about service change and developing local payment mechanisms.
-
When activity levels change, costs do not all change in the same way. Variable costs will usually change in relation to the activity change but fixed costs will remain the same over the given period.
-
You should classify each line in your cost ledger as fixed, semi-fixed or variable, based on a timeframe of 12 months. Where trusts are applying method 1 mapping and do not use the cost ledger, they should still ensure they have an appreciation of which costs are fixed, semi-fixed and variable.
Fixed costs
-
Fixed costs remain the same regardless of the level of activity.
-
Typical fixed costs include corporate costs such as rates, depreciation, CNST, financial charges and board of directors’ costs.
-
Agenda for Change (AfC) staff at band 8a and above are classed as fixed, as AfC guidelines state these grades do not qualify for overtime. Trust scale senior managers are also classified as fixed costs. This classification should be applied regardless of the role or duties.
-
Medical staff basic pay must be paid regardless of activity, so this is a fixed cost.
Semi-fixed costs
-
Semi-fixed costs remain the same until a certain level of activity is reached; the costs then increase in proportion to the level of activity or ‘step up’ to a new level where again they remain the same until the next threshold of activity is achieved.
-
Costs are defined as semi-fixed when the level of cost needed to maintain the infrastructure to deliver the contracted activity level is fixed. The costs incurred to deliver activity above that level are thus variable.
-
Staff contracted at band 7 and below are classified as semi-fixed costs, as their salary is fixed but they can work and be paid for overtime.
Variable costs
-
Variable costs increase in proportion to the level of activity. They are only incurred to deliver activity: for example, medicines, patient consumables and hire or issue of equipment and the cost will vary depending on the level of activity.
-
The costs of additional sessions that reduce waiting lists will be variable.
-
Locums, agency and bank staff also fall into this category. We understand that sometimes these staff are contracted to cover longer term absences (such as planned staff sickness) but as a general principle they should be classified as variable.
Other considerations
-
As each CL line is mapped to a classification, resources may end up containing costs of all three cost classifications, based on how overheads are allocated in the costing process. The classification of fixed/semi-fixed/variable costs will be applied at CL level. Therefore, resources will not map to a single classification.
-
Activity codes are not classified as fixed, semi-fixed or variable. Some expense codes within an activity will vary in classification according to the behaviour of the cost when the number of patient events changes.
-
The classification should be applied regardless of the role for which an individual was employed. For example: a nurse manager may have a portion of their role in a clinical setting and the rest in a management capacity. Their whole role will be considered as one classification.
CP3: Allocating costs to activities
Scope
-
This standard applies to all costs reported in the costing system and all activities undertaken by the trust.
-
It covers relative weight values (RWVs) and how to identify and use traceable costs in the trust.
Overview
-
The standardised costing process using resources and activities aims to capture cost information by reflecting how those costs are incurred.
-
After mapping from the general ledger to the cost ledger and resources, the costing process allocates resources to patients in two steps:
- Step 1: allocate resources to activities (as explained in this standard)
- Step 2: match costed activities to the correct patient event (as explained in Standard CP4: Matching costed activities to patients).
-
The allocation methods prescribed in the standards in most cases do not include an RWV for acuity or intensity. If you are using an RWV for acuity or intensity on top of the prescribed allocation method, continue to do this and record it in ICAL worksheet 15: Superior costing methods.
Approach
Resources
-
Resources are the components used to deliver activities, such as staff, equipment or consumable items. The costs of providing these resources are recorded in your general ledger, and the resource code prescribed by the standards groups these costs in themes.
-
In the standardised cost ledger (see spreadsheet CP2.1) all patient-facing lines are mapped to resources. Once you have mapped your general ledger to the standardised cost ledger, you will get a subset of resources your trust uses from the list in spreadsheet CP3.1.
-
The costs in a resource may contain overhead costs, as overheads are allocated to patient-facing resources to be allocated to activities. For example, the patient-facing nurse resource could include the costs of overheads, such as protective clothing, stationery and computer hardware purchase, HR and finance costs. See Standard CP2: Clearly identifying costs.
-
The transparency of these costs – what they are and where they come from in the general ledger – should be maintained throughout the costing process. In the National Cost Collection, overheads are identifiable as separate pay support cost and non-pay support cost collection resources.
-
Once these separated costs have been calculated, they can be aggregated to whatever level the resources have been set at, and you can be confident the costs in each resource are accurate because they are underpinned by this costing process.
-
Spreadsheet CP3.1 lists the prescribed patient-facing resources to be used for the costing process. You are expected to use the most appropriate resource and not a generic resource to aggregate costs. For example, you are expected to use the physiotherapist and speech and language therapist resources, and not report all therapists’ costs against the general therapist resource. Use the general resources only if there is no specific resource for that cost.
-
Spreadsheet CP2.1 contain the mapping from each line in the cost ledger to the patient-facing resources. Use this information to identify the two-step prescribed allocation methods in spreadsheet CP3.3.
Activities
-
Activities are the work all resources carry out to deliver the services that achieve the desired outcomes for patients; for example, a procedure in theatre, pathology tests or a psychotherapy session carried out in clinic.
-
This standard prescribes a list of activities for integrated services. See spreadsheet CP3.2.
-
Together, resources and activities form a two-dimensional view of the costs incurred to deliver services. The acceptable combinations are shown in worksheet CP3.3 PF allocations, with the prescribed allocation method.
-
You need to identify all the activities your trust performs from the prescribed list of patient-facing activities in spreadsheet CP3.2. You are expected to use the most appropriate activity. For example, audiology assessments should be reported using the ‘audiology assessment’ activity rather than the ‘outpatient care’ activity; for endoscopy use the ‘endoscopy’ activity rather than ‘outpatient procedure’ or ‘theatre care’.
-
For non-admitted patient care, the activities prescribed for the community care sector are more specific than for other sectors because of the lack of detail in community care activity data. For example, for outpatient clinic activities for diabetes in an acute hospital, ‘outpatient care’ should be used as the activity as the care provided can be seen by the treatment function code (TFC); for diabetic care in a community setting, ‘diabetic care’ should be used. These more specific activities (by specialty) are for community care only. See Standard CM3: Non-admitted patient care.
-
Some activities are informed by patient-level feeds; for example, the activity ‘ward care’ uses information from Feed 4: Ward stay, for costing (acute and community providers only; mental health trusts may have the same data in Feed 1b: Admitted patient care) and the ‘dispense all other medicine scripts’ activity uses information from Feed 10: Medicines dispensed.
-
Spreadsheet CP3.2 indicates which prescribed patient-level feed informs the activity, or if another information source is required where a patient-level feed is not prescribed.
Allocate resources to activities
-
You need to use the prescribed resource and activity combinations in Figure CP3.1 in your costing system.
Figure CP3.1: Allocation of resources to activities
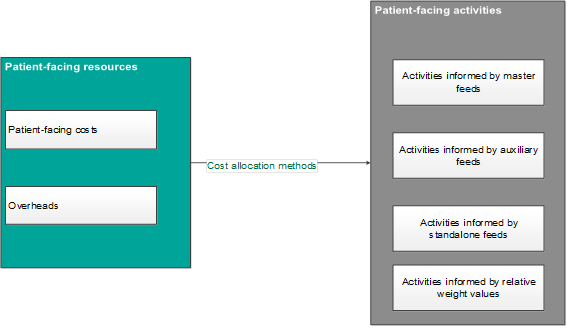
Figure CP3.1 shows the two types of patient-facing resources (patient-facing costs and overheads) allocated to four different types of source information (master feeds, auxiliary feeds, standalone feeds and relative weight values) that inform the activities.
-
Identify the resource and activity combinations used in the costing process for your trust by:
- obtaining the list of resources for your trust from mapping your general ledger to the cost ledger or mapping directly to resources (see CP2: Clearly identifying costs) and
- reviewing the prescribed list of activities to identify those performed by your trust (see spreadsheet CP3.2).
-
You must allocate resources to the activities using the methods prescribed in spreadsheet CP3.3.
-
Resources need to be allocated to activities in the correct proportion before being allocated to each unit of activity. There are three ways to do this:
- based on actual time or costs from the relevant information feed prescribed
- using RWVs created in partnership with the relevant departments
- using a local information source, such as ‘traceable costs’.
-
Where one resource needs to be apportioned to several activities, for example consultants delivering both inpatient and outpatient care, you need to determine what percentage of the cost to apportion, after discussions with clinicians and managers supported by documented evidence where available (for example medical job plans). These splits and their basis should be recorded in ICAL worksheet 13: % allocation bases. Please note this is a different process from disaggregating costs in your general ledger for mapping to the cost ledger.
-
As an example, the disaggregation of medical staffing costs to four different activities is shown in Figure CP3.2. Table CP3.1 shows how this example would look in the resource–activity matrix.
Figure CP3.2: Example of how the cost in a resource (consultant) is apportioned to activities using relative weight values
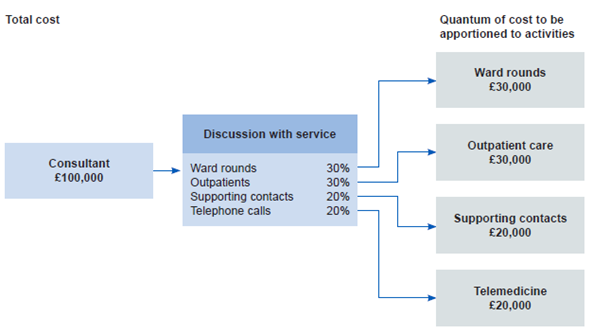
Figure CP3.2 is an example of how the cost in a resource (the consultant) is apportioned via discussion with services (ward rounds, outpatients, supporting contacts, telephone calls) to activities using relative weight values.
Table CP3.1: Example resource and activity matrix for a consultant, using the information in Figure CP3.2 for costing
| Activity | Resource |
|
|
Consultant |
|
SLA098: Ward rounds |
£30,000 |
|
SLA135: Outpatient care |
£30,000 |
|
SLA099: Supporting contacts |
£20,000 |
|
SLA149: Telemedicine |
£20,000 |
|
Total |
£100,000 |
-
Use an RWV unless there is a local reason for applying a specific traceable cost. (For more information on traceable costs see the Costing glossary). You should document the reason for using a traceable cost in the integrated costing assurance log (ICAL) worksheet 14: Local costing methods.
-
Do not apportion costs equally to all activities without clear evidence they are used in this way and do not apportion costs indiscriminately to activities.
-
Where the same cost driver is used for several calculations in the costing system, and providing the costs can be disaggregated after calculation, you can aggregate the calculations in your costing system to reduce calculation time. For example, if several costs on a ward use the cost driver length of stay, you can add them together for the cost calculation.
-
If you have a more sophisticated cost allocation method for allocating resources to their activities:
- confirm whether it is considered a superior costing method on spreadsheet CP3.5
- if it is shown on CP3.5, keep using it
- document it in ICAL worksheet 15: Superior costing methods.
-
If your method does not show on CP3.3 or CP3.5, contact our costing team on costing@england.nhs.uk. Spreadsheet CP3.5 contains the methods we have accepted as superior costing methods, developed from experiences of implementation across sectors. We would like to hear about any other methods you are using to develop costing standards based on actual experience, so if appropriate we can add them to the prescribed or superior lists.
-
Some superior costing methods require a subset of resources. See CP2: Clearly identifying costs including Figure CP2.2: Simplified costing process. For example, CM1: Medical staffing superior costing method SCM33 allocates actual payroll detail for medical staff. To do this, a resource below the standard level of resources is needed for each staff member. There is no requirement currently to adopt this method but if you are already doing it, continue to do so and log it in ICAL worksheet 15: Superior costing methods.
-
There are some cost allocation methods we do not accept as superior to the prescribed methods. These include using income or national averages to weight costs.
-
The key cost drivers, such as length of stay, which inform cost allocation methods can be obtained from the information feeds.
-
Investigate any costs not driven to an activity or any activities undertaken by your trust that have not received a cost and correct these.
Relative weight values
-
You should allocate all material costs based on actual use or consumption using the prescribed allocation method and an information feed. However, where there is no information feed, or the costs are immaterial, use a relative weight value (RWV).
-
RWVs are a method of using appropriate source information as a percentage weighting to distribute or ‘drive’ the allocation of cost. For example, see Figure CP3.2. RWVs may be used to:
- disaggregate costing account codes so the cost can flow to different resources in conjunction with the mapping to the cost ledger (see CP2: Clearly identifying costs)
- apportion overheads to resources (see CP2: Clearly identifying costs and the FutureNHS Overhead allocations: learning extension)
- apportion resources where they deliver more than one activity (see Figure CP3.2)
- allocate costs from resources to activities
- attribute costed activities to patient events.
-
One way to store the relative weight values for use in your costing system is to compile ‘statistic allocation tables’.
-
RWVs may contain information from sources such as staff job plans, HR/electronic staff record data, interviews, floorplan measurements, catalogues of laboratory supplies and consumable costs. (See also FutureNHS Overhead allocations: learning extension.)
-
RWVs may also use data from information feeds, such as actual medicine costs in Feed 10: Medicines dispensed.
-
Income values and national cost averages should not be used as RWVs.
-
You must develop and agree RWVs with the relevant service managers, healthcare and other professionals to ascertain all aspects of the costs involved and ensure these are as accurate as possible. You can also use traceable costs as RWVs.
-
Different costs will require different approaches to derive appropriate RWVs to support their allocation to patients. For example, some scans require RWVs for review time per scan and contrast required per scan.
-
The approach should not be high level; for example, the measure should not be the average time to carry out a test or investigation but should be tailored to the specific activity. To do this you need to break down the activity into its component costs and measure the drivers of these individual costs
-
RWVs should be reviewed on a rolling programme or when a significant change occurs in the relevant department.
Traceable costs
-
Where the actual costs of items are known, you can use them in the costing process as an RWV to allocate costs to the activities. These are known as traceable costs.
-
If an actual cost is applied, it is likely that costs will be over or under-recovered in the costing system, so actual traceable costs should be used as a percentage, relative weight value to allocate the costs. Table CP3.2 shows an example of traceable costs used as a relative weight value.
Table CP3.2: Using traceable costs as a relative weight value
Number of prostheses | Actual cost | Actual total cost | % weighting | Weighted spend | |
|---|---|---|---|---|---|
|
Prosthesis A |
5 |
1,000 |
5,000 |
67% |
7,333 |
|
Prosthesis B |
12 |
500 |
6,000 |
33% |
3,667 |
| Total |
1,500 |
11,000 |
100% |
11,000 |
-
Items for which a traceable cost may be available include:
- medicines, including high cost drugs
- security – patient-specific cost of escorting using an external provider
- patient appliances
- pacemakers and other cardiac devices
- hearing aids – bone-anchored, digital
- theatre consumables.
-
If the value of a traceable item is material to the cost of the patient and you want to use the actual cost, you must ensure it matches the value in the ledger. If there is under or over recovery, you must use the cost as an RWV, as outlined above.
-
Some trusts may have local departmental databases or an inventory management system that records material cost components against individual patients which can be used in a supplementary feed. These traceable costs can be used in the costing process as a weighting to allocate the costs on a costing account code. See CM21: Clinical non-pay items.
Overheads
-
The cost ledger shows the costing account codes that relate to overhead costs, by using a code starting T1S in spreadsheet CP2.1. To allocate overheads in the correct proportion, you will need to identify RWVs by obtaining the relevant information from the departments, for example RWVs for actual whole time equivalent (WTE). See FutureNHS Overhead allocations: learning extension.
Complex relative weight values
-
Some cost areas will require RWVs that have more than one facet in the calculation of the proportional split for the cost allocation. This method combines cost drivers to make a multiple-layer statistical allocation table.
Other considerations
-
If you have already undertaken a sampling exercise in which you calculated RWVs for the costing process, you can use this information. You should repeat this exercise at reasonable intervals to include technological, contractual and cost changes.
-
If your trust contracts an external organisation to provide a clinical or non-clinical service, you may not have a patient-level feed or detailed information on the components of the service, and so may need RWVs to allocate the cost. See CM8: Clinical and commercial services.
-
RWV calculations should be made within the costing system to minimise the risk of error.
CP4: Matching costed activities to patients
Please note: The PLICS extract matching identifier (PLEMI) is an identifier intended to enable data linkage across several crucial PLICS activity feed types from one trust. It is for linking not matching, therefore is not applicable to this matching process.
Scope
-
This standard applies to all costed activities.
Overview
-
Matching is integral to accurate patient-level costing. For an accurate final patient unit cost, the costed activities need to be matched to the patient event – that is the episode, attendance or contact – in which they occurred. This allows the final costed record to show the different components of cost within a patient event.
-
The costing process allocates resources to patients in two steps:
- Step 1: allocate resources to activities (explained in CP3: Allocating costs to activities)
- Step 2: match costed activities to the correct patient event.
-
Matching can be derived from the data in a master feed or an auxiliary feed.
-
Matching derived from a patient event in the master feed, uses cost allocation and matching in the same process. For example, ward care activities can be calculated using the length of stay in the admitted patient care (APC) feed (mental health services) and are already matched to the costed patient record using the patient event identifier of the record. Acute and community patients may use the auxiliary ward feed for the ward care activity as described in the next paragraph. See IR1: Collecting information for costing.
-
Matching where an auxiliary feed is matched to the patient event will cost the activity on the auxiliary feed, and then use the prescribed matching rules specified in spreadsheet CP4.1 to match the costed activity to the patient event. For example, the system will cost supporting contacts using the duration of attendance in Feed 7: Supporting contacts and then match the costed activity to the patient event using the matching rules in spreadsheet CP4.1.
Prescribed matching rules
-
The prescribed matching rules shown in spreadsheet CP4.1 ensure the relevant auxiliary information feeds can be attached to the correct patient episode, attendance or contact in the master feeds.
-
Matching rules are hierarchical (match iteratively) and should be strict enough to maximise matching accuracy, but not so rigid that any matching is impossible. Matching rules that are too lax risk false-positive matches – that is, activity matched to the wrong patient event.
-
The matching hierarchy in spreadsheet CP4.1 determines which master feed the auxiliary feed is matched to, and the order in which to identify the correct master feed.
-
Where there is a local unique identifier for patient and patient event across all types of service, this is matched first.
-
If an auxiliary feed contains the patient’s point of delivery (POD) or location, use this field to determine which master feed to match to. For example, if a patient is recorded non-admitted patient care (NAPC), their activity is first matched against master Feed 3a NAPC, then Feed 3b NAPC (mental health) then Feed 3c NAPC (community). If the POD data field is considered robust, records should be matched to the NAPC dataset only, to avoid the risk of false-positive matches.
-
As the matching patterns for data feeds differ depending on the activities they contain, each has a distinct set of matching rules. Matching rules may vary in their hierarchies, date parameters or additional data fields used in the matching criteria.
-
Unmatched records should be reviewed.
-
The accuracy of which costed activities are matched using the prescribed matching rules depends on the quality of the master and auxiliary feeds. Follow the guidance in the FutureNHS Managing information for costing: learning extension.
Approach
Using the prescribed matching rules
-
The unique identifier of patient and patient event (episode/spell/attendance/ contact) always generates the best match as it is unique to the patient and the relevant date range. If there is more than one contact on one day, the ID should include this, whereas a simple aggregation of patient identifier and date will only reflect one contact on one day.
-
In the Mental Health Services Data Set (MHSDS) for Feed 1b: APC feed, this is: ‘local patient identifier (extended)’, ‘start date (care professional admitted care episode)’ and ‘end date (care professional admitted care episode)’; and for Feed 3b: ‘care contact identifier’ and ‘care contact date’. In some trusts, the care contact identifier will include the care contact.
-
If your auxiliary data feeds are obtained from the patient administration system (PAS), and you can include the unique identifier of patient and patient event in the feeds, you should use this field to match to the master feeds. We understand some MH organisations use ‘ward stay’ data as a separate auxiliary feed. It can be used if it provides more information than the MHSDS Feed 1b: APC.
-
If your auxiliary feeds do not include the unique identifier of patient and patient event, you should use the prescribed matching rules in spreadsheet CP4.1.
-
If your matching rules are more sophisticated than the prescribed matching rules and improve the accuracy of your matching, continue to use them and record them in the integrated costing assurance log (ICAL) worksheet 29: Superior matching rules.
-
If an element of a prescribed matching rule would produce a false-positive match for a particular feed, adjust the rule to ensure a more accurate match and document this in ICAL worksheet 29: Superior matching rules.
-
Activities from non-integrated systems need to be matched to these groups of patients:
- APC patients discharged during the costing period
- APC patients not discharged and still in a bed at midnight on the last day of the costing period
- non-admitted patient care
- attendances at a minor injuries unit, emergency department of a walk-in centre
- critical care stays (adult, paediatric and neonatal).
-
Some activities from non-integrated systems should not be matched:
- those for patients not in the provider’s care, including direct access (CM23: Direct access) and services received activity (CM8: Clinical and commercial services); however, there may be instances where such activities should be matched, for example diagnostic imaging for direct access physiotherapy
- items such as replacement orthotics, homecare medicines or blood factor products for which there may be no corresponding patient event can have a proxy record created to match to (superior costing method) or be recorded as ‘reconciliation items’ (although the trust provides these, they can be issued directly to the patient for use at home)
- medicines dispensed from the pharmacy for a patient whose episode is already closed
- medicines issued by the pharmacy but sent to another trust without a patient contact, even if the patient is under a care plan with your trust
- medicines dispensed from pharmacy to patients who did not attend (DNA) or who were not brought to clinic. See CM10: Pharmacy and medicines.
-
Medicines supplied to patients at home under a homecare arrangement should be matched to a proxy patient event, using the date the medicines were dispensed. These medicines are administered at patient level, so can be included in Feed 10: Medicines dispensed. See IR1: Collecting information for costing.
-
There are no prescribed matching rules for the following master feeds:
- Feed 6d: Critical care transport
- Feed 16: Improving access to psychological therapies data set
- Feed 19b: Wheelchair equipment.
-
There are no matching rules for these feeds as these services are not anticipated to have a need for auxiliary feed matches. However, if you have information that requires matching one of these feeds, you can add them to the matching rules hierarchy.
-
Not all trusts have or need separate feeds for some activity. For example, for mental health trusts, the MHSDS APC feed contains ward information, and the Community Services Data Set (CSDS) care contacts feed contains ‘did not attend’ (DNA) information, so no matching is needed.
-
Direct access activity must be correctly identified using the direct access flag in Spreadsheet IR1.2 to avoid it being incorrectly matched to other episodes or attendances for that patient. For example, giving all direct access patients a hospital patient identifier risks the incorrect matching of activity other than own patient care to an episode, attendance or contact with the same patient identifier. An incorrect match could be made if a patient has previously been a patient at the trust and their hospital patient identifier is applied to the direct access activity.
-
Clinical services supplied activity contracted to another organisation must be correctly identified using the ‘services supplied flag’ indicator in spreadsheet IR1.2 to avoid being incorrectly matched to episodes or attendances. Note: this activity should still be costed, so that the cost of all patient care is correctly allocated.
-
The rules to identify and correctly treat direct access and services purchased from another organisation activities are included in the prescribed matching rules. See CM23: Direct access and CM8: Clinical and commercial services.
Matching hierarchy used in the prescribed matching rules
-
You only need to follow steps relevant to your trust. For example, if your trust does not provide ED services, start at the next relevant service and so on through the steps in order.
-
All the feeds with prescribed matching rules in spreadsheet CP4.1 follow the hierarchy described below. The hierarchy is adjusted slightly for each feed to reflect how the service is provided but the principle is that for all sectors the matching feed is matched first to the unique identifier and then to:
- ED attendances (including MIU and WIC, Feed 2)
- ED activity on an observation ward (APC Feed 1a: APC)
- critical care – adult (Feed 6c: Adult critical care)
- critical care – paediatrics (Feed 6b: Paediatric critical care)
- critical care – neonatal (Feed 6a: Neonatal critical care)
- APC (APC Feed 1a, Feed 1b)
- NAPC (NAPC Feed 3a, Feed 3b, Feed 3c, Feed 3d, Feed 3e)
- unmatched to the treatment function code (TFC)
- if the TFC is missing, to the providing department.
-
You should also search 24 hours before and after the exact date, and then expand the search timeframe by 24-hour increments up to 720 hours (30 days) either side of the delivery dates to increase the chance of a match.
-
The prescribed matching rules contain conditional criteria, which should be followed in the order shown in spreadsheet CP4.1 in the Matching Rule ID.
-
The matching process should then search again without the conditional criteria, incorporating the final prescribed matching elements.
-
If you have (or develop) other auxiliary feeds, these should be matched after the mandated feeds, to ensure the prescribed matching to the master feeds is completed first.
Using the prescribed cost allocation methods in matching
-
For patient-facing activities not informed by a patient-level feed, for example where relative weight values are used in cost allocation, use the prescribed cost allocation methods in spreadsheet CP3.3 to match (or allocate) the costs to the relevant patient events.
-
For costed activities informed by the standalone activity feeds, no matching rules are prescribed, and the prescribed allocation methods in spreadsheet CP3.3 should be followed as in Feed 14: Cancer multidisciplinary team (MDT) meetings.
Other considerations
-
Some costed activities will not match; either because the activity was too long before the patient event, for example a diagnostic imaging scan done more than 720 hours (30 days) before the connected NAPC contact, or because the quality of the information in the activity feed is so low. As stated above, unmatched activity should be reviewed.
-
Develop a list of ‘unlikely matches’ to be included in the matching rules for your trust, to ensure that costs for certain activities are correctly assigned to episodes. For example, medicines that are never used by certain specialties should never be assigned to episodes within those specialties, even if other matching criteria are fulfilled. Work with clinicians, the pharmacy team and other staff to identify these ‘unlikely matches’. Work with your costing software supplier to ensure regular reporting of these items and have a process to audit/amend erroneous matches.
-
Your costing system should produce a report of the matching criteria used in the system, as described in CP5: Reconciliation.
-
If costed activities are matched on the least stringent criteria, data quality needs to improve so that activity can be matched more accurately. You should have a rolling programme to review this.
Reporting unmatched activity for local business intelligence
-
Unmatched activity should be reported to the PLICS steering group. The report should identify items expected to be unmatched activity (including direct access and homecare without proxy records) and the unexpected unmatched activity.
-
Trusts have traditionally treated the cost of unexpected unmatched activity in different ways. Most commonly it was absorbed by matched activity, which could have a material impact on the cost of that matched activity, particularly when reviewing the cost at an individual patient level for benchmarking and decision-making.
-
For local reporting, we recommend you do not assign unmatched activity to other patient events but report them as reconciliation items.
-
To achieve consistent and comparable costing outputs for local reporting, unexpected unmatched activity should be treated consistently across trusts. We suggest applying the following rules:
- If the specialty that ordered the item can be identified but the item cannot be matched to a patient event, the cost sits in the specialty under unmatched items and should not be matched to the other patients in that specialty.
- If the specialty that ordered the item cannot be identified, the cost sits in the providing department under unmatched items. Likewise, the cost should not be matched to the patients within the most likely specialty. For example, if a pathology test cannot be matched to a patient event and the requesting specialty (for example cardiology) cannot be identified, the unmatched activity is reported under the pathology service line, as this is the department that provided the service. This data should be discussed with the department to improve the understanding of data quality in the feed.
-
If reported unmatched activity forms a material part of a trust’s expenditure, this is likely to be due to inadequate source data. As this will deflate the patient unit cost, it needs to be identified and steps taken to improve the quality of the source data, rather than artificially inflating the patient unit cost by allocating unmatched activity. See CM2: Incomplete patient events and the FutureNHS Managing information for costing: learning extension.
-
Tables CP4.1 and CP4.2 show examples of how unmatched activity could be reported to assist business intelligence.
Table CP4.1: Example of unmatched activity costs (in blue text) within a specialty
| Specialty: Medical oncology | |
|
Total activity |
Total resource cost |
|
Inpatient care – core episodes |
£X |
|
Critical care for oncology patients |
£X |
|
Outpatient care |
£X |
|
Cancer MDTs |
£X |
|
Unmatched activity identified as oncology but unable to match to individual patients |
£X |
|
Total |
£X |
Table CP4.2: Example of unmatched activity costs (in blue text) by providing department
| Department: Pathology | |
|
Total activity |
Total resource cost |
|
Cardiac service |
£X |
|
Medical oncology service |
£X |
|
Dermatology service |
£X |
|
Critical care service |
£X |
|
Unmatched activity unable to be allocated to a specialty or patient |
£X |
|
Total |
£X |
CP5: Reconciliation
Scope
-
This standard applies to all cost, income and activity included in the costing process.
Overview
-
All costing process outputs must reconcile to the information reported to the board, submitted to national datasets, and in the final audited accounts. This ensures a clear link between the costing outputs and the cost and activity information captured in the source data.
-
Reconciliation to an agreed tolerance is important as it allows users of cost data to use it with confidence. See the FutureNHS Assurance of cost data: learning extension. The benefits of reconciliation include assurance that:
- the data is reliable and complete
- unit costs reflect the true cost of the service, undistorted by provider-incurred costs unrelated to the trust’s own patient activity
- the true cost is more appropriate for benchmarking between peers as non-patient related costs can significantly affect cost reporting by different providers.
-
Tolerance levels: for your reconciliations you should agree the level of acceptable difference between input values and output values with your costing steering group in line with the costing principles. The tolerance level for patient events may be different percentages for the different datasets.
Approach
-
The cost and income outputs from the costing system must reconcile to the main sources of this information – the general ledger (G)L output and the trust’s reported financial position. See CP2: Clearly identifying costs for guidance on where adjustments made between the GL output and the cost ledger (CL) can be included in your reconciliation.
-
The patient event outputs should also reconcile to what has been reported nationally.
-
The submissions to national datasets will include data items that are not used for costing – for example, activity under a provider-to-provider contract. These should be noted on your local reconciliation as they will form part of the difference between the costing system outputs and the submission made by your trust.
-
To avoid any reconciliation differences due to timing, the information feeds used in the costing process and those reported by the trust should be created at the same time.
Reconciliation of cost and income
-
To demonstrate that the costing system’s outputs reconcile to the main sources of cost and income information, use the reports detailed in the four cost groups below and created from the costing system, as described in the Minimum software requirements on FutureNHS.
-
To support reconciliation and reporting, the costing model outputs should be categorised into the four cost groups: Own patient care/Activities other than patient care/Other activities/Cost and activity reconciliation items:
- Own patient care:
- National Cost Collection included services:
- incomplete patient events
- all cancer MDT meetings where your trust’s patients are discussed.
- Services performed by another NHS provider:
- clinical services received (such as capacity purchased from private inpatient organisations)
- Patient care for patients funded from outside the NHS:
- private patients, overseas visitors, non-NHS funded patients and patients funded by the Ministry of Defence.
- National Cost Collection included services:
- Activities other than patient care
- Costs relating to research and development and costs relating to education and training in the organisation.
- Other activities:
- National Cost Collection included services:
- direct access diagnostic services where the patient is referred from primary/community care for assessment only and the care remains with the GP/community organisation
- critical care transport where the patient is not brought to your trust
- external cancer MDTs where your trust’s patients are not discussed
- Services performed by another NHS provider:
- clinical services supplied, such as pharmacy services supplied to another provider
- commercial activities.
- Services where the costs are not collected in the National Cost Collection:
- local authority care
- primary care services
- national programmes such as breast screening.
- Cost and activity reconciliation items (Includes activity for which there is no corresponding cost and costs for which there is no corresponding activity):
- Services performed by another NHS provider:
- cost to provide agreed resources to an external body with no responsibility for delivering a service to a commissioner, for example a provider-to-provider service-level agreement, including national programmes
- cost to employ a staff member, such as a youth worker, for activity undertaken by the local council and the provider is unable to include it in the costing system.
- Accounting adjustments:
- grants or donations received.
- Services performed by another NHS provider:
- National Cost Collection included services:
-
To complete the reconciliation, it is also necessary to understand the income shown in the organisation’s accounts. See income groups below:
- Operating income (relates to cost group ‘own patient care’:
- National Cost Collection included services:
- income for own patient care.
- Services performed by another NHS provider:
- clinical services received (such as capacity purchased from private inpatient organisations).
- Patient care outside the NHS:
- private patients, overseas visitors, non-NHS funded patients and patients funded by the Ministry of Defence.
- National Cost Collection included services:
- Other operating income:
- This income group includes income that does not relate to own patient care:
- research and development income
- education and training income
- commercial income.
- This income group includes income that does not relate to own patient care:
- Recharges and adjustments to cost:
- This income can be netted off from the cost to reduce the value shown in the costing system:
- Consultant Excellence Awards (CEA)
- Recharges between organisations where the staff/service is provided at cost, but the employing organisation does not have all the activity that is supported (subject to a materiality decision).
- This income can be netted off from the cost to reduce the value shown in the costing system:
Reconciliation of patient events
-
You should reconcile the patient event outputs to the patient events in the source datasets, to ensure all the activity you entered in your costing system has been costed and then included in the costing output. Use the information feed log in ICAL worksheet 1: Patient-level activity feeds to record the input data. This can then be used to compare to the output data.
-
The patient events used for costing should be the same patient events sent to the relevant national dataset; for example, to the outpatient commissioning dataset.
-
Not all national datasets are at patient level, some are at aggregate level. If this applies to your dataset, you should reconcile to the aggregate value of the dataset. For example, the wheelchair national dataset is a quarterly submission of aggregate data.
-
To demonstrate that the costing system’s outputs reconcile to the main sources of activity information, use the reports listed below. The reports must be created from the costing system, as described in the Minimum software requirements on FutureNHS.
Services with sensitive/legally restricted data requirements
-
You will need to consider pseudonymising data for services with sensitive/legally restricted data. Some services have extra levels of required information governance for them because the legal data holding regulations and patient consent differ.
-
‘A’ patient rather than ‘the’ patient may need to be costed. The reconciliation of both cost and activity with other trust records will need to take this into account.
Provider-to-provider services reconciliation
-
Your trust may provide services for other NHS trusts and receive services from other NHS trusts. Standard CM8: Services supplied and services received provides more information.
-
Where your trust has the activity but no cost, as the costs are incurred by another NHS trust, you cannot cost this activity. Report this activity in the ‘cost and activity reconciliation items’ cost group, and ensure it is noted in your activity reconciliation. You must make this activity data available to the other organisation at the required contractual level. For NHS providers, the activity data should include all the prescribed information required for the Approved Costing Guidance and the National Cost Collection.
- If you have cost but no activity at patient level because the contractual detail is in the information system of another trust, you should request the patient event information from the other trust and enter it on your costing system. If there are difficulties obtaining this data, discuss the next steps with your costing steering group, and contact the NHS England costing team at costing@england.nhs.uk.
Integrated costing methods
Before you implement these costing methods (CMs), you should read and understand:
To successfully implement the costing methods, use them in conjunction with the technical document, especially the following spreadsheets:
- spreadsheet IR1.2: Field requirements for the activity feeds
- spreadsheet CP2.1: Standardised cost ledger
- spreadsheet CP3.1: Resource list
- spreadsheet CP3.2: Activity list
- spreadsheet CP3.3: Methods to allocate resources to activities and give details of resource and activity combinations.
For CM35: Education and training you will require E&T costs at cost centre/expense code level adjusted for 2022/23, 2022/23 E&T activity information, including programme schedules, and 2022/23 E&T income.
CM1: Medical staffing
Scope
-
This standard applies to all medical staffing costs. The term medical staff applies to doctors of all grades, including general practitioners and locums.
Overview
-
Medical staff form a large proportion of many trusts’ costs, and where the service is medically led, their input is essential to the patient care. In some services, they are likely to deliver a significant proportion of patient-facing activities. In others, they provide a smaller proportion of patient-facing care but are important to decision-making and clinical responsibility.
-
If clinicians are to use patient-level costing effectively to improve services, they need to be confident that their activity is costed appropriately. To enable good engagement, you should work with the lead consultant or designated medical staff member to obtain the best possible information for allocation of cost to services.
-
To accurately cost medical staff activities, you need to know which activities each medical staff group in your trust delivers, differentiating between ward rounds, ward care, outpatient clinic, appointments, contacts in community settings, care programme approach (CPA) meetings and specialist work such as theatre sessions.
-
You should allocate consultant costs to the activities to which they have contributed.
- Where they work within a team, their costs may be allocated across the team activity.
- If they work across a whole treatment function code (TFC), their costs may be allocated across all activity in that TFC.
- As a permissible substitution, where you have confidence in your data allocating patients to the named consultant or their GMC number, you can allocate the consultant costs to their own patient events.
-
You also need to understand which of the activities delivered by medical staff are patient facing, and which are ‘other’ activities including research and development (R&D) and education and training (E&T).
Approach
Information requirements
-
Information on medical staffing activities will be available from the patient administration system (PAS) data and the service area. Use both sources to understand the best source of information for allocating cost.
- PAS data will include a named consultant as responsible for each patient event, for most patient events. Other healthcare professionals may also be identified as the named person, particularly in mental health and community services. The Commissioning Data Set (CDS), Community Services Data Set (CSDS) and Mental Health Services Data Sets (MHSDS) include the consultant code (or other ID) in the ‘healthcare professional local identifier’ field to show clinical responsibility for the patient. This is built into feeds 1a and 1b Admitted patient care and feeds 3a, 3b and 3c Non-admitted patient care.
- The service area will have information on where the medical staff spend their time; for example, consultant job plans or non-consultant medical staff rotas. Use these as relative weight values (RWVs) to allocate cost to the relevant services.
-
Each patient admission may have multiple episodes of care with the TFC changing from one to the next. Each episode should have a cost for medical staff in the relevant treatment function associated with it.
-
If you are already costing medical staff activity at patient level using name or GMC number, and linking this to the individual consultant, continue to do so and document it in your integrated costing assurance log (ICAL) as this approach is a permitted substitution. However, if you are using this method, you do need to identify activity that does not incur a named consultant cost and ensure the cost of medical staffing is allocated to the patients from the relevant area.
-
You should avoid double counting the costed resources to the patient – that is, from both the named professional costing and the standard non-medical staff process.
-
GPs and junior doctors work in community wards and community hospitals, with some community providers having no consultant-led services.
Specialist cost centres and expense codes
-
Map your medical staffing costs to resources via the mapping in spreadsheet CP2.1: the standardised cost ledger, according to the service in which the staff work. See Figure CM1.1. This may be:
- within a service cost centre
- at specialty level
- a local service team category.
-
Customising your cost ledger: these cost centres are designed to show the resource mapping used for medical staff, but the mapping rows can be repeated for different service areas, changing the XXX to an identifiable local code and adding the service name.
-
You should use the expense codes for consultant and other grades of medical staff shown in spreadsheet CP2.1: The standardised cost ledger.
-
You should disaggregate the proportions of time spent in different areas to set up your customised cost ledger. Disaggregating the cost at this stage enables a streamlined flow of cost to activities.
-
Please note: consultant ‘programmed activities’ are not all patient facing. They may be for education & training, research & development, clinical leadership or other project work – called ‘special programmed activities’. The cost for these activities should be allocated across the service or other area rather than allocated to their patient-facing work.
Figure CM1.1: Identifying the correct quantum of cost to be apportioned to activities (does not include any non-patient facing or special programmed activities)
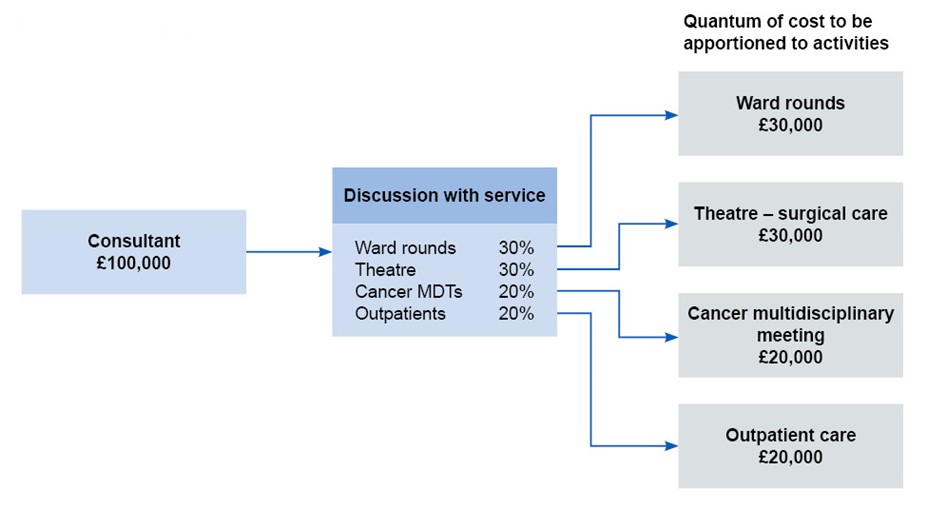
Figure CM1.1 outlines the correct quantum of cost to be apportioned from a consultant via discussion with services such as ward rounds, theatre, cancer MDTs and outpatients to activities. It does not include any non-patient facing or special programmed activities.
-
An example template for gathering this information is included in the ICAL worksheet 23: CM1 Medical Staffing % split.
-
For some consultant medical staff, the percentage split of consultant medical staffing costs by activity type may be divided further for specific groups of patients, for example orthopaedic surgeons split into hips, knees, trauma.
-
Do not apportion the same percentage split to all activity types unless evidence suggests that is appropriate. Document the rationale for the percentage split you use in ICAL worksheet 24: CM1 consultant % reasoning.
-
Do not use consultant job plans as a basis to allocate non-consultant medical staffing costs. Allocate those costs based on discussions with the lead for those staff groups and other information sources. There will usually be a consultant responsible for non-consultant medical staff, and administration support.
Resources
-
To identify the resources used for medical staffing costs you should refer to spreadsheet CP3.1: Resource list.
-
Mental health consultants (resource ID: MHR253) should be separated from other consultants (resource ID: SGR062) in the costing system as they have distinct areas of work, such as psychiatry, forensic psychology, neuropsychology.
-
This separation of mental health consultants improves reporting at integrated providers with staff from physical and mental health specialties. For example, providing physical health support for post-traumatic stress disorder in a mental health centre or child psychiatry in a physical health children’s centre.
Activities
-
Review the prescribed list of activities in spreadsheet CP3.2 and identify those your medical staff deliver (see also GP services below).
Ward rounds
-
Ward rounds are regular or planned acute consultant visits to the ward to review a range of patients sequentially. They can also involve nurses, non-consultant medical staff, social workers, care programme leads, therapists, and other staff. (Note: where material, the costs of all these staff should be identified as part of the Activity SLA098: Ward round).
-
If the clinical service deems all ward rounds to be identical, the allocation of activity to patient-level can be based on the number of patients alone. No further information is needed.
-
Superior costing method SCM49: Ward round allocations varied patient groups, enables you to allocate ward round costs to patients with different TFCs or other specific characteristics. You will need local information from medical staff for this method.
-
As a more advanced superior costing method, SCM71: Ward rounds at patient level, enables you to use patient-level data on time spent with each patient in the ward round for allocation of cost. This information can be obtained from clinical notes systems or another data source. However, you should ensure the data quality is sufficient, as we recognise the duration of time spent with a patient is not the most important thing recorded in clinical notes. Both these methods are shown in spreadsheet CP3.5: Superior and alternatives.
-
Anaesthetists may do pre-surgery ward rounds for patients due to go into theatre. Work with the anaesthetic teams to develop an RWV assigning these patients an appropriate element of anaesthetist costs.
-
Community hospital wards may have ward rounds led by non-consultant medical staff and/or the GPs responsible for the wards but these may have a less formal process. You should agree with the service whether the medical staff visits to the wards are best costed as ward rounds (that is, separate formal time spent with each patient) or the Activity SLA097: Ward care is more appropriate for the more fluid model of care.
-
Mental health medical staff may spend time with patients informally on a ward or have formal ward rounds.
Ward care
-
Where medical staff of all grades are continually interacting with the patients on a ward, this is called ‘ward care’ for costing purposes. For example, junior doctors on a surgical ward, all grades of medical staff on general medical wards, and for mental health inpatient units.
-
Community wards may have general practitioners or junior doctors operating either ward rounds or ward care.
-
Where medical staff perform minor procedures on the ward, this should be included in the ward care activity. If the procedures are of significant duration, you should obtain the patient-level information and include it in Feed 13: Theatres with any material consumable costs and in Feed 15: Prostheses and other high-cost items. See also Standard CM5: Theatres and special procedure suites and Standard CM21: Clinical non-pay items.
Supporting contacts
-
Supporting contacts are contacts with a patient outside the clinician’s main specialty.
-
For medical staff, inpatient supporting contacts would include ward visits additional to the regular ward rounds or ward care, to a ward that is not their normal area. NAPC supporting contacts would include a consultant attending specific patients at another TFC outpatient clinic.
-
Specialist palliative medicine, specialist rehabilitation and interventional radiology medical staff have been identified as providing regular and essential services to wards other than their named services. The supporting contact costs of medical staff at patient level for these services are now prescribed.
-
Use Feed 7: Supporting contacts in accordance with spreadsheet IR1.2. Spreadsheet CP3.2 showing the activities relating to supporting contacts.
-
MH CPA meetings are NAPC patient events (recorded as such even when they take place during an admission) where one patient and multiple professionals meet to agree the formal care plan usually take place annually but may be more frequent. The information for this meeting is in feed 3b NAPC (mental health) as the contact is recorded in the MHSDS, but you may need to use Feed 7: Supporting contacts to identify cost for the medical staff present at the meeting. There is a separate activity MHA261 CPA meeting in response to the need to identify them separately to other NAPC contacts.
Non-admitted patient care
-
The NAPC feeds (3a, 3b and 3c) will record these events at patient level. They can include formal booked clinics or home visits, drop-in clinics, and ad-hoc contacts. See also CM3: Non-admitted patient care.
-
Many medical staff NAPC contacts are consultations only, so you should use the Activity SLA135: Outpatient care. There are other types of NAPC contacts, especially for mental health and community services.
-
Some appointments include procedures during the NAPC contact. For example, pain management consultants give pain-relief injections. For these procedures, use Activity SLA136: Outpatient procedure and treatment room care. The procedure should be clinically coded on the outpatient record: you can use the clinical coding to identify when this activity should be applied.
-
Anaesthetists may be involved in, or run, pre-operative, pain management or critical care NAPC clinics. Work with your anaesthetists to find out if they are involved in outpatient care and if they perform procedures. Use this information to develop RWVs to assign an appropriate element of anaesthetist costs to the patients who received the care.
Telemedicine (non-face-to-face) contacts
-
Telemedicine contacts can include telephone and video consultation contacts (telemedicine), and other types of non face-to-face contacts recorded on feeds 3a, 3b, and 3c: NAPC, using the data field ‘Consultation medium used’.
-
With some widely used methods of communication, such as text and email, contacts are not always recorded. As recording protocols for these contacts are part of the patient pathway, we have included them in the standard. If your clinicians are not yet recording these contacts and this activity is material, we recommend you work with your informatics team to support the development of an appropriate recording method for the clinical teams. If the recording methods do not use the main PAS and flow to the national dataset, you should document what is counted in ICAL worksheet 3: Local activity definitions.
Emergency departments
-
Emergency departments are the 24-hour service units, providing emergency care (EC). The consultants work across the whole emergency department and have no named activity in the PAS record. Use Activity SLA121: EC – medical care for these staff, which has a different allocation method from other consultant services. EC consultants may also provide ambulatory care, which is emergency NAPC similar to an outpatient clinic.
-
If you have information on the time spent with specific patients, you may use this as superior costing method SCM72: EC patient-level acuity, as shown on spreadsheet CP3.5. For example: you can allocate additional resources to patients treated in the resuscitation room using information in the patient record to show the acuity.
Liaison
-
Where MH medical staff work with emergency departments or physical health consultants work in MH trusts, their cost should be identifiable against the activity it relates to. See CM3: Non-admitted patient care and CM4: Emergency care attendances.
-
If this activity lies in a different organisation, the cost should be shown in the reconciliation statement under ‘Other activities’ and not be allocated to your trust’s own patient care. See CM8: Clinical and commercial services.
-
Where activity is not available for this service, you should disaggregate the cost before it is entered into the cost ledger, so the cost is not allocated to your trust’s own activity.
Other considerations
Theatres
-
For information on medical staff in theatres, refer to CM5: Theatres and special procedure suites.
Critical care
-
For information on medical staff in critical care, refer to CM6: Critical care.
Pathology
-
Most pathology consultants specialise in a particular field, such as hematopathology or forensic pathology. Some will have patient consultations, but not all; therefore, allocating cost based solely on patient contact is not always relevant. You should disaggregate their costs to the appropriate part of the service, including separating patient contact time from laboratory work and post-mortems.
-
As superior costing method SCM73: Pathology – allocation by test, you can add an RWV for acuity of tests to the consultant costs – see spreadsheet CP3.5: Superior and alternatives.
-
Use spreadsheet CP3.3 to identify the pathology activities the consultant resource is linked to. Supporting documents will reference CM1: Medical staffing.
Diagnostic imaging
-
Radiologists specialise in diagnosing and treating disease and injury using medical imaging techniques such as X-rays, computed tomography (CT), magnetic resonance imaging (MRI), nuclear medicine, positron emission tomography (PET), fusion imaging and ultrasound. A significant proportion of medical staff time in diagnostic imaging is spent reporting on the imaging scans. You should understand whether variation in the reporting time is consistent or variable by type of scan and allocate cost accordingly.
-
You should work with the department to ensure radiology medical staff costs are allocated appropriately to all their activities.
-
The radiologists may also deliver interventional radiology which has named patient events recorded in PAS. These will be costed according to the APC or NAPC format.
-
Interventional radiologists also work with surgeons in theatre when the procedure is image guided.
-
As a superior costing method SCM74: Diagnostic Imaging – allocation by imaging scan, you can add an RWV for acuity of scans to the consultant costs. See spreadsheet CP3.5: Superior and alternatives.
-
Use spreadsheet CP3.3 to identify the diagnostic imaging activities the consultant resource is linked to. Supporting documents will reference CM1: Medical staffing.
Special programmed activities
-
Special programmed activities are non-clinical duties that underpin clinical care and contribute to ongoing professional development.
-
E&T activities should be costed in line with CM35: Education and training transitional method and documented in ICAL worksheet 21 Education and Training. Identify E&T using Activity SPA154: Education and training.
-
E&T activities should not be matched to patients but reported under the ‘education and training’ cost group.
-
R&D activities should be costed using your current methods and documented in ICAL worksheet 20: Research and development. Identify R&D using Activity SPA155: Research and development.
-
R&D activities should not be matched to patients but reported under the ‘research and development’ cost group.
-
Other non-clinical activities should be allocated to clinical activities using the actual cost of the clinical activity as an RWV.
CM2: Incomplete patient events
For this costing method you will also need to read and understand:
Scope
-
This standard applies to all patient events, as all patient events could start in one costing period and finish in another. It is most likely to occur in admitted patient care (APC) and is also known as ‘work in progress’.
-
It applies to all components of care brought into the costing system by an auxiliary feed, to ensure they are costed and allocated to the patient event when they took place, irrespective of whether the patient event was complete or incomplete.
Overview
-
The correct treatment of incomplete patient events is necessary to ensure:
- full reconciliation to the audited accounts
- the cost of completed events is not inflated by the costs of incomplete events
- when the multi-year events are completed, the full costs can be derived by looking at multiple years of patient-level data.
-
Users of the costed data need to understand whether the cost they are reviewing represents a complete or incomplete patient event, to use the information appropriately.
-
Costs should be applied to the patient event as they occur but with the costing model using a defined costing period some will occur outside the costing period.
-
The costs of incomplete patient events should not be used as part of decision-making so it is essential to understand and identify the difference between complete and incomplete patient events.
-
This standard defines ‘incomplete patient events’ as:
- patients not discharged at the end of the costing period and/or
- patients admitted before the beginning of the costing period.
-
This definition works in conjunction with the National Cost Collection (NCC) guidance of ‘event types’ 1, 2 and 4 – see the integrated collections guidance and the integrated extract specification.
-
Complete events are therefore where the patient event has been discharged or the event ended during the costing period. This is NCC event type 3.
-
Activities brought into the costing system on auxiliary feeds should be matched to the patient event when they occurred as in CP4: Matching. This means some costs would be matched to incomplete patient events and would need special treatment to ensure reconciliation to the cost quantum. See Figure CM2.1.
Figure CM2.1 Example incomplete event, with medicine costs
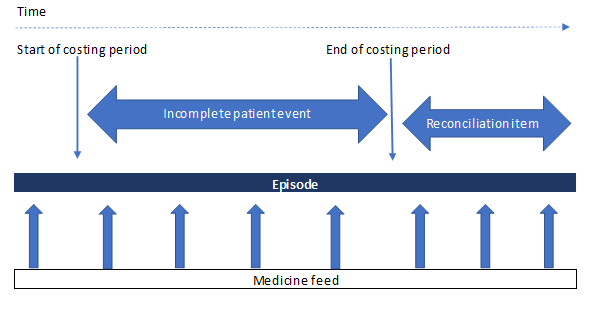
Figure CM2.1 shows an example of medicines dispensed to an incomplete patient event: the medicine cost is shown within and outside the costing period, and on the reconciliation statement.
Admitted patient care
-
An incomplete patient APC event is where the patient’s current episode or spell is ongoing – that is, they are still in a bed at midnight – on the last day of the current costing period. See the Costing glossary.
-
Costing an episode should be based on its start and end dates. This means a patient whose care started in an earlier costing period will be recognised as having costs incurred during the costing period; and patients discharged after the end of the costing period can be identified and costs allocated according to the day when they were incurred.
-
The costed patient event is an episode, and there may be several episodes within a spell. If an APC episode is incomplete, the spell will also be incomplete. A spell may have one or more complete episodes and an incomplete episode. See the Costing glossary.
-
If costs in the current costing period are allocated to discharged patients only, those yet to be discharged will not incur any cost: incomplete episodes will be under costed and the costs of complete episodes inflated.
-
Note: A change of ward does not start a new episode. See CM13: Admitted patient care.
Non-admitted patient events
-
Some NAPC events go past midnight: for example, where a community midwife is supporting a home birth. These events should have costs allocated in proportion to the duration of the event.
-
You should consider the materiality of work in this area and prioritise areas of significance.
Approach
-
To accurately cost your trust’s activities, it is important only resources consumed in delivering the event are allocated to the event. To achieve this, costs need to be allocated to all patient events on the day they were incurred, regardless of whether they are complete or incomplete at the end of the costing period.
-
Incomplete patient events are included in the financial accounts. Trusts are required to follow the principles of IAS18 in relation to revenue recognition; for example, income relating to partially completed episodes at the financial year-end should be apportioned across the financial years on a pro-rata basis. Using the same principle, the costs of care are also accumulated as they are incurred.
-
The values for work in progress in the final accounts contain additional items to just the value for incomplete patient events and therefore the values will be different. There is no requirement to reconcile them, though the incomplete patient events cost data may help future assessments of income due for annual accounts purposes.
Identifying incomplete patient events
-
Incomplete patient events need to be brought into the costing system, and the patient-level costs calculated each time you run your costing model. Work with your informatics team on a suitable way to do this with your costing software.
-
You should ensure your master feeds (for example APC, NAPC, EC) and auxiliary feeds (for example ward stay, pathology, diagnostic imaging) recognise incomplete events as valid patient records. They should not be rejected during data quality processes: for example, validation checks on the discharge date or discharge flag fields.
-
To identify APC incomplete events, use Feed 1a APC or Feed 1b APC (Mental health). There will not be a discharge date in the costing period and there will be a blank in derived field ‘patient discharge flag’ (see spreadsheet IR1.2).
-
One way to set up the calculation of the incomplete event is to put the date of the end of the costing period in the ‘discharge date’ field. You should ensure this substitute date is replaced with the actual discharge date or a revised substitute date at next calculation.
-
The APC feeds should then include information relating to patients still in a bed at midnight on the last day of the costing period.
-
To calculate incomplete events for non-APC master feeds, use the date and time information in the feeds. Where the start date (and time) is different to the end date and time, and the end date is outside the costing period, the attendance is an incomplete event.
- Feed 2a: use the field Departure date and time from emergency department to compare with the field Arrival date and time at emergency department.
- Feeds 3a and 3e: use the field Appointment end date and time to compare with the field Appointment start date and time.
- Feeds 3b, 3c and 3d: use the field Care contact date, Care contact time and Clinical contact duration of clinical contact to identify incomplete patient events.
-
To ensure costed activities receive information from auxiliary feeds, incomplete patient events should be included in the matching process. For example, medicines dispensed can be matched using the date and time. Where auxiliary feeds do not have a time stamp, the matching to the NAPC incomplete patient event should be based on the starting date.
-
You should ensure patients admitted before the start of the costing period are also included in the PLICS feeds and receive matched data from auxiliary feeds on the date the cost was incurred. See Figure CM2.2.
-
For local reporting, complete and incomplete patient events should be clearly displayed. See Table CM2.1.
Table CM2.1: Example of incomplete patient events in a local reporting dashboard
Specialty X | Cost (£) | Income (£) |
|---|---|---|
|
Patients discharged |
100 |
90 |
|
Patients not discharged |
60 |
|
|
Total costs incurred in month on delivering patient care |
160 |
|
Figure CM2.2: Parts of episodes to be costed
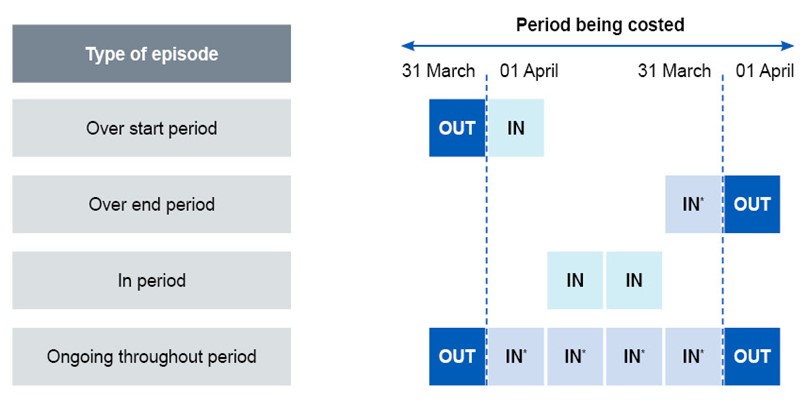
Figure CM2.2 shows the National Cost Collection treatment of incomplete patient events – episodes type 1, 2 and 4. Episode type 3 is a complete patient event, which is wholly within the costing period.
Allocating costs to year-end incomplete patient events
-
Where a prosthesis or non-pay item of material value is used in a cross-year episode, you need to use the ‘date of implant’ field in feed 15: Prostheses and other high-cost items, in spreadsheet IR1.2 to allocate this cost to the correct part of the episode.
-
For example, a patient episode starts on 26 March 2023 (financial year 2022/23) and the patient is discharged on 6 April 23 (financial year 2023/24):
- Of the 12-day admission, the first 6 days are costed in the financial year 2022/23 as the incomplete episode. The second 6 days are costed in the next financial year 2023/24. Both would have a part-cost flag.
- If a prosthesis was inserted on 27 March 2023, the prosthesis cost should be matched to the part of the episode that falls into the incomplete episode in financial year 2022/23.
-
Where you identify that costed activity is unmatched because the patient event to which it relates is in a different costing year, you should flag it as ‘unmatched – incomplete patient event’. Then report this under incomplete patient events, not unmatched. The time spent doing this should be proportional to the value of the unmatched activity for your trust, in line with the costing principles.
CM3: Non-admitted patient care
Scope
-
This standard applies to all non-admitted patient care (NAPC) activity, including:
- hospital outpatient clinic appointments
- clinical settings such as health centres or community mental health outpatient appointments, including day care
- contacts in the patient’s residence or other non-clinical locations for specialist care, community care and mental health care contacts (sometimes known as ‘domiciliary’ visits)
- attendances to a ward without admission (ward attenders)
- Talking Therapies (formerly IAPT) contacts.
-
Types of NAPC activity include consultations, talking therapies, procedures, physical therapies, telemedicine and community care contacts.
-
For further guidance on costing maternity, chemotherapy and radiotherapy NAPC contacts (hospital-based and community), please see:
- Standard CM24: Maternity services
- Standard CM25: Chemotherapy services
- Standard CM26: Radiotherapy services.
-
Emergency care attendances to a 24-hour unit (also known as accident and emergency departments or emergency department) or non-24-hour unit (including minor injury units, walk in centres, and urgent treatment centres) are out of scope of this standard. Please refer to CM4: Emergency care attendances.
Overview
-
NAPC occurs in many settings, including formal outpatient clinics held in hospitals, community or mental health centres, and the patient’s residence. Some events are booked in advance; others are ‘drop-in’.
-
The terminology for NAPC is defined by the NHS Data Dictionary. The national dataset definitions are used for costing, as all trusts that supply a service should submit to the relevant national dataset. These are described in IR1: Collecting information for costing.
-
NAPC activity should be costed based on which clinical staff are in the clinic, service team session or actual care contact
with the patient. This does not include staff present for education and training. Other relevant costs include:
- Clinical support and administration costs specific to the service. These should be allocated to all patient events in the service equally, using the appropriate cost allocation method.
- Outpatient departments that are often managed as a central team. These should be allocated to the patients who used the function, using the duration of their NAPC appointment.
- Community care contacts and procedures that take place outside the clinic setting, for example in a patient’s residence or a community clinical setting. Costs should include travel and must also be allocated using the duration of the contact which should not include time spent travelling to/from the patient. For more detail on clinical contact duration of care, see the NHS Data Dictionary.
- Non face-to-face (‘telemedicine’) contacts. These are an essential part of patient care and are increasing in number; they should therefore be included as patient events. If this activity is not recorded in or submitted to the national datasets, work with your informatics teams to progress this. Non face-to-face contacts may form a large part of ‘hidden activity’, as discussed in IR1: Collecting information for costing. It is essential to include this activity as care models change, so the cost and outcome benefits can be understood. Costs are allocated using the duration of the contact but should not be allocated the costs of support nursing, consumables or other elements of an outpatient department.
-
Duration is defined for costing as the time recorded in minutes in the patient administration system, that the patient is in the care of a clinician for non-admitted patient care. Travel to/from the patient, and preparatory-/post-contact administration time is not included. This definition is consistent with the NHS Data Dictionary definitions of Clinical contact duration of care and Expected duration of appointment.
-
The patient costs allocation using ‘duration’ of the patient event in minutes should use the duration of patient events that took place, proportionally, so all costs are allocated for the period. Empty slots, did not attends (DNAs), cancellations and cancelled clinics should not be costed.
-
Different services and clinics may use varying staffing numbers, types and professional bands across and within different sessions. Where the clinical area has materially variable staffing or other resources, you can cost the service team sessions using superior costing method SCM62 and spreadsheet CP3.5 Superior and alternatives. This will require local information on staffing detail, and then allocation of the session cost to the patients.
-
A service team session is a defined period of time where one or more care professionals see a sequential list of patients. It could be a day in the community, a four-hour session or defined as a formal clinic, depending on the sector and the available information.
Approach
Information requirements
-
Costing NAPC activities requires information from the local source that supplies the national datasets listed in Table CM3.1, in accordance with IR1: Collecting information for costing and spreadsheet IR1.2. Where there is no national dataset for the service area, local information should be used.
Table CM3.1: NAPC information feeds and the source data
|
PLICS information feeds |
Feed reference |
Source data |
|
NAPC acute and community outpatients |
3a |
Commissioning Data Set (CDS) |
|
NAPC mental health |
3b |
Mental Health Services Data Set (MHSDS) |
|
Talking Therapies (formerly known as IAPT and the dataset continues to be named IAPT) |
16 |
IAPT Data Set (IAPT) |
|
NAPC community: for community care contacts and community clinic attendances |
3c |
Community Services Data Set (CSDS) |
| NAPC community midwifery (see CM24: Maternity Services) |
3d |
Maternity Services Data Set (MSDS) |
| NAPC home births (see CM24: Maternity Services) |
3e |
Maternity Services Data Set (MSDS) |
-
You should bring all NAPC patient events into the costing system including:
- home visits
- ward attenders – where the patient attends a ward without being admitted, often for specialist nursing input but the care given can be from any clinical professional groups
- day care
- home births, as these are not admissions to a hospital (see also CM24: Maternity services)
- separate, sequential contacts recorded as part of a team clinic or ‘one-stop shop’, as long as they are recorded according to NHS Data Dictionary requirements and NHS commissioning rules
- where a therapy service has a discrete referral list and supports another service: for example, a senior physiotherapist may have their own clinics – this is a discrete service. They may also see patients in an orthopaedic clinic where they are still the only professional seeing the patient – this would not be a discrete clinic but is counted – in this case, as an orthopaedic contact.
-
The following data fields in spreadsheet IR1.2 record the duration of the patient event for costing:
- CDS (Feed 3a): field ‘expected duration of appointment’
- MHSDS (Feed 3b): field ‘clinical contact duration of care contact’
- CSDS (Feed 3c): field ‘clinical contact duration of care contact’
- IAPT dataset (Feed 16): this does not have a field for the duration of contact; you need to calculate the duration locally
- MSDS (Feed 3d): field ‘clinical contact duration of care activity’.
-
The NAPC feeds in spreadsheet IR1.2 contain the fields for each attendance/contact.
-
Duration of the NAPC patient event is an essential driver of cost and the clinical contact duration of care activity is a defined field in NHS datasets (see the NHS Data Dictionary). There are two recognised types of duration:
- ‘expected duration’: the planned or ‘booked’ slot for the appointment – usually built into the clinic/diary template. This term is used in the CDS.
- ‘actual duration’: the actual time the patient is with the clinician. This term is used in the CSDS, the MSDS and the MHSDS.
-
Acute services should use ‘expected’ or ‘booked’ duration for the allocation as they are typically standard-length appointment slots, and so will be a reasonable allocation of cost. As a superior costing method SCM59) you can use actual duration. See spreadsheet CP3.5 Superior and alternatives. This is particularly beneficial to the costs if:
- time spent with patients is materially variable across a costed session, or
- you have accurate information to allocate based on actual duration.
-
Mental health services should use actual duration because of the variability of time spent with each patient during one costed session.
-
Some NAPC patient events will go over midnight; for example, a community nurse night-sitting service. The costing system should use the start of the attendance for the costed record, to ensure it is identified with other NAPC records in the same month.
-
If your trust does not record the duration of attendance in minutes for a particular service, work with your services and informatics teams to develop this information. In the meantime, continue to use your current method for costing outpatient activity and record this in the integrated costing assurance log (ICAL) worksheet 14: Local costing methods.
Outpatient procedures
-
Outpatient procedures performed in acute and community clinics that are recorded on the CDS should be clinically coded and grouped to show the healthcare resource group (HRG).
-
Procedure coding will indicate extra cost for consumables but this may not be material. Discuss whether there are material costs with the service team and, if relevant, use relative weight values to allocate to patients. See CM21: Clinical non-pay items.
-
Where OPCS codes are used, clinical coders will apply the codes to the patient record or agree on a set template of codes for the administration team to apply to the NAPC patient record. SNOMED-CT codes will be applied to the patient record by the healthcare professional. Clinical coding of outpatient attendances is not mandatory but organisations have local arrangements to support accurate patient records and enable more appropriate reimbursement from the Payment by Results/NHS Payment System. We recognise clinical coders are not responsible for ensuring the templates are completed correctly.
Home visits
-
Home visits are identified in the information feeds (feeds 3a, 3b, 3c, 3d and 3e) using the field ‘activity type location code’.
-
There is no national definition of what a community service is. Home visits are provided by acute, mental health and community care professionals.
-
For costing purposes, we use the national dataset to which the patient events are submitted, to define whether a service is a community care contact on the Community Services Data Set (CSDS) or an acute attendance on the Commissioning Data Set (CDS). This will aid activity reconciliation during the National Cost Collection.
-
For costing, you should understand the nature of the team providing the services so the data can be built into the correct feed and costed accordingly:
- Where the trust provides consultant-led or non-consultant-led specialist/acute services in the community, this would be included in the Outpatient (CDS) and should use Feed 3a. These will be costed as part of the acute services and will include specialist acute care professionals attending the patient in their home.
- Where the patient event is part of mental health services, it will be included in the Mental Health Services Data set (MHSDS) and use Feed 3b. This will include care professionals in community mental health teams but may also include specialist mental health professionals.
- Where a trust is commissioned to provide district nursing, community allied health professionals or other care as a community service, it is expected that they will submit this data to the CSDS and use Feed 3c. This is the feed source for community care contacts.
- Where the provider (usually an acute trust) provides community midwifery home visits and manages home births, this will be included in the Maternity Services Data Set (MSDS) and brought into PLICS on Feed 3d. As the MSDS is relatively new, some trusts have built this data into the CDS. You should ensure these patient events are not duplicated in Feed 3a and Feed 3d within the costing system.
-
For example:
- a district nurse providing wound dressings as part of the community service, will be reported using the ‘activity location type code’ of ‘A01 patient’s home’ as a home visit on the CSDS (Feed 3c), and costed as a community care contact
- a specialist paediatric oncology nurse – based in hospital – would also be recorded using the ‘activity location type code’ of ‘A01 patient’s home’ as a home visit – but this should be on the CDS (Feed 3a) as specialist work that takes place in the patient’s residence, rather than a ‘community’ contact.
Ward attenders
-
Ward attenders see a clinician in the ward location without the need for admission. They are treated as ‘outpatients’ for costing and commissioning and are identified in the information feeds 3a, 3b, 3c and 3d using the ‘activity type location code’ E02 Ward (nursing and other non-medical professionals).
Day care
-
Day care facilities do not have hospital beds. Patients with a range of physical and mental health needs attend sessions for therapeutic and social benefit to their health. Patients in a specialist palliative medicine setting may also attend day care facilities. See CM38: Specialist palliative medicine.
-
The activity type location code of H01 Day Centre is the national method of identification but day care may be commissioned using other fields or local identification codes.
-
Day care should also be costed using the duration of the patient contact. As day care is typically several hours long, the duration of contact will be greater than most types of NAPC, and allocation using the duration will show the greater proportion of cost needed to operate the service.
-
Most day care is given as a group, so the cost of the session should be allocated across all the patients that attended. See CM14: Group sessions.
Data quality and hidden activity
-
The CDS, CSDS, MHSDS, IAPT and MSDS datasets require all NAPC contacts to be recorded. However, the quality and completeness of the data are variable in some areas. If fields required for PLICS are not completed fully on your NAPC information feeds (as shown in Table CM3.1), the information may be available from data not included in the main national datasets. You should use this information to guide discussions with clinical and service leads and enable you to enter local patient-level data into your NAPC feed(s). See also IR1: Collecting information for costing for how to work with missing or poor data.
-
You may need to create proxy records for services that do not keep an electronic record, as a temporary solution until an electronic patient record is in place. See the FutureNHS Managing information for costing: learning extension.
Data on staff involved
-
The CDS (Feed 3a) for acute services includes the HRG field to identify multiprofessional and multidisciplinary activity separately from single professional activity but it does not determine who was present. If the different staff types are considered material, you will need to obtain information from the service about who was present at the attendance to ensure the correct costs are allocated to the right patient.
-
The CSDS, MHSDS, IAPT and MSDS datasets do not currently contain suitable fields to identify multiprofessional and multidisciplinary activity separately from single professional activity. You may need to collect extra information about who else is present in a clinic or care contact and build this into your NAPC feeds, using the ‘multidisciplinary flag’ and ‘multiprofessional flag’ data items. Use this information to construct relative weight values (RWVs) to allocate the appropriate staff costs to contacts.
-
Be aware that a clinic may be assigned to the consultant or lead care professional with overall responsibility for it. This person is not necessarily present in the clinic or may only be physically present in some patient contacts in that clinic.
Other NAPC data sources
-
The information feeds for some discrete services in the trust may be separate from those showing contacts in the CDS, CSDS, MHSDS, IAPT and MSDS. Examples include:
- sexual health (see CM16: Sexual health services)
- dentistry (see CM17: Dental services)
- assisted reproduction/fertility
- fetal/foetal medicine
- learning disabilities
- addiction services, including drug and alcohol
- perinatal mental health services
- mental health liaison.
-
Information on what took place during these contacts will be recorded on a local electronic system or paper pro forma completed by clinical staff and entered into an electronic system by administrators. These datasets, where available, should be brought into the costing system in accordance with IR1: Collecting information for costing, and the appropriate costing method.
-
Procedures performed during these patient events should be recorded by OPCS procedure codes (hospital care) or SNOMED-CT codes SNOMED-CT is mandated for all NHS providers since April 2020). However, there may be other coding models used: for example, community dental services have separate treatment coding structures that show a course of treatment and the unit of dental activity (UDA) for commissioning purposes. See CM17: Dental services.
-
If you think the quality of the electronic data for any NAPC service is not good enough for costing, get a blank pro forma (may be known locally as a routing slip, coding form, outpatient procedure record) and use it to guide discussions with clinical and service leads about the most performed procedures. You can then identify the materiality of the cost for the clinical non-pay items and the staff involved in performing them.
Specialist cost centres and expense codes
-
Use expense codes appropriate for the staff type and band. You may need to disaggregate the costs of staff covering more than one unit or service area, to ensure the correct flow of cost to resources.
Resources
-
NAPC activities can involve a wide range of healthcare professional resources, including consultants, nurses, therapists, psychiatrists, radiographers, and clinical scientists. You should map the cost to the appropriate resource for the type of staff conducting the contact, see spreadsheet CP3.1
-
As a permitted substitution (SCM48), you can use healthcare professionals’ individual costs, identified from a payroll data source, in the costing system to calculate the staff cost per contact. See spreadsheet CP3.5: Superior and alternatives for more information.
-
Some NAPC contacts may require input from a healthcare professional who is not a member of the regular clinic staff: for example, minor surgery may require an anaesthetist or practitioner. Where material, their cost needs to be included for the relevant patient, based on the duration of the patient event. This information can be brought into the costing system using Feed 7: Supporting contacts.
Activities
-
Non-admitted care services relate to the type of care given and may include more than one activity within each contact.
-
Review the list of activities in spreadsheet CP3.2 and determine those relevant for the service. You can then identify how they may be mapped automatically using the information on your NAPC feeds. For example, activity CMA302 Community care can be identified by the ‘Service or team type referred to’ field in Feed 3c: NAPC – as code 12 District nursing.
-
As a superior costing method, community care activities can use the field ‘Community care activity type code’ to further detail the activity/activities in the patient event.
-
For detailed descriptions of NAPC patient events, see spreadsheet CP3.
Outpatient care – patient to clinician ‘consultations’
-
Activity SLA135: Outpatient care represents a discussion with a care professional – usually in a clinical setting. The term ‘outpatient’ is usually used for ‘clinics’ in a specialist, hospital-based service. There would not be material costs of consumables in these patient events.
-
Mental health interventions may include a wide range of talking therapies, patient education and management of medicines/substances, enabling the patient to manage or improve their condition. Costing such complex non-admitted mental health services needs a good understanding of the staff working in these services, and how the information recorded about them may be used to ‘count’ activity and allocate cost.
-
Community clinics in a health centre or other community setting where one care professional is visited sequentially by different patients, would not normally be called ‘outpatient care’. They would be community care contacts, in a clinical setting.
Outpatient procedures
-
These are interventions performed in an NAPC setting by specialist care professionals. For example, pain management consultants give pain relief injections, podiatrists perform surgical procedures on feet, and electroconvulsive therapy (ECT) may be administered in the mental health sector. These procedures should be identified from their clinical coding or other sources of information and will have an HRG currency. Use Activity SLA136: Outpatient procedure.
-
Outpatient procedures or interventions may occur in the consultation room (clinic) or a specialist treatment room. You need to ensure the correct department costs and clinical non-pay items are allocated to the procedure (see Standard CM21: Clinical non-pay items for more information).
-
Outpatient procedures would not normally be performed in the patient’s home. Where a community care contact includes a procedure, this will have a ‘care activity code’ on the patient’s record, and this will show in the CSDS. You should use the relevant community care activity for the procedure.
Ward attenders
-
Patients attending a ward for an NAPC contact with a nurse, therapist or medical staff are often follow-up care or for long term conditions; they have ‘open access’ to the ward but are not admitted to a hospital bed. You should use Activity SLA157: Ward attender care.
-
The ward attendance should be included on Feed 3a: NAPC feed or Feed 3c: NAPC community feed. Feed 4: Ward stay may contain some of the information used for costing these attendances, as bed spaces may be allocated to these patients (even though they are not admitted).
-
Some costs will come from the ward cost centre, as the staff from the ward will give most of the care. An outpatient department should not be included in the cost, even though the patient event is classified as NAPC.
-
You will also need to identify any additional care professionals (rather than the ward staff) involved in the ward attendance. For example, specialist nurses may see their patients on a ward in this model. As a superior costing method SCM33, they should be recorded on Feed 7: Supporting contacts and costed using the relevant Activity ID.
Day care
-
Day care is where a group of non-admitted patients benefit from care services in a group setting – usually over a few hours. A range of care professionals may provide care over the period of attendance. The activity may be recorded in the patient administration system (PAS) and reported as part of the CDS, or it may be on a standalone local system.
-
The staff involved are most likely to be nurses, therapists and other care workers but in some areas, there can be medical input. The model of care may be termed ‘social’ or ‘medical’ depending on its clinical content. There are separate cost centres in the cost ledger if you need to keep the two types of model separate. You should use Activity MHA262: Day care. Note: day care – even surgical or medical day care – is different from ‘day hospital’, which is an APC unit.
Non face-to-face (telemedicine) consultations
-
For costing, telemedicine and other non face-to-face contacts should be treated in the same way as face-to-face contacts.
-
Non face-to-face contacts are a vital part of clinical care for many patients. Most of these contacts will be by telephone but video calling is increasingly used: these are both defined as ‘telemedicine’. Use Activity SLA149: Telemedicine consultation (telephone and video consultation).
-
Other non face-to-face contacts include text conversations, email, patient-online schemes and patient letter review. They need to be separated from telemedicine as the duration of ‘patient contact’ will be the time taken to review and respond to the patient rather than the duration of the patient contact (there is no actual patient contact). Use Activity SLA102: Other non face-to-face contact.
-
Note: As there are only names for these communication methods in the NHS Data Dictionary, we apply the same guidelines as for telephone contacts. If you include these in your PLICS, we recommend you include your local policy on what constitutes the currency in ICAL worksheet 3: Local activity definitions.
-
Clinical telemedicine can be identified in the NAPC dataset using the ‘consultation medium used’ field. The NHS Data Dictionary contains the list of codes for consultation medium used.
-
These contacts should be counted and costed as they often replace the need for face-to-face contact and prevent escalation of conditions, making an effective contribution to agreed pathways. Non face-to-face contacts simply to make bookings or pass on results without advice and guidance are not countable.
-
If services record their non face-to-face calls on a separate database to the patient administration system (PAS), you should obtain a patient-level feed from this alternative source that includes all important identifiable information. If this data is not submitted to the national dataset, you will need to note this on your activity reconciliation.
-
Telemedicine and other non face-to-face contacts are often ‘hidden activity’ (see IR1: Collecting information for costing). Therefore, you may need to identify where there are gaps in your NAPC data.
-
You need to determine if the time recorded for a non face-to-face consultation is the actual call duration or if it includes preparation and write-up time. Only the duration of the phone call should be used, for consistency with other NAPC contacts. Preparation and write up time are treated as administration time not contact time, as in the NHS Data Dictionary.
-
Most telemedicine and other non face-to-face contacts are likely to involve only one staff member but multi-professional contact is possible. The appropriate resources should be attached to the activity accordingly.
Mental health outreach care
-
These are contacts outside the standard clinical setting that have required significant additional time ‘searching’ for the patient, often where the patient has not attended appointments to continue their treatment plans. The MH professional searches for the patient and holds the contact wherever possible – not necessarily in a clinical setting. Without these contacts, patients may not take medication or follow self-care plans.
-
Use Activity SLA101: MH outreach visit. Allocate this activity using the total duration of contact in accordance with the ‘clinical contact duration of care contact’ field, plus local information at the patient level for the searching time.
Home visits (including ‘domiciliary visits’)
-
Acute and mental health visits by specialist medical staff and other care professionals to the patient’s home or current place of residence should use Activity SLA135: Outpatient care, even if the location is not a traditional home setting. They can include contacts at hostels or shelters, temporary residence at a friend’s/family’s home and where a homeless person lives on the street. Consultant visits to the patient’s home are rare, and are sometimes known as ‘domiciliary visits’ because of the payments made for these to the individual in the past. In costing terms, these are still ‘outpatient care’ if the care professional is a consultant or another specialist care professional.
-
The location is identified by the ‘activity location type code’ field, so there is no need for a different activity ID code.
-
Community-specific staff visiting the patient’s residence should use the activity relevant to the care given – for example, Activity CMA301: Community care, or the detailed community team areas of care given using activity ID prefixed with ‘CMA’. These community teams can be general – such as district nurses that provide a range of services and knowledge, or more specific – such as a community diabetes service.
-
If there is not a clear division between a specialist service and a community service, you should agree with (1) the service, and (2) your PLICS steering group which type of service is provided. This decision will take into account:
- understanding the data recorded (ie consider which national dataset their patient events are reported to)
- the service or team’s understanding of whether they are a specialist service, or a community service
- if the service is commissioned as a specialist service or a community service. Traditionally, community services have been under block contract arrangements. (See your contracting team for more details.)
Group sessions
-
These occur when several patients have contact with a single or multiple care professionals simultaneously.
-
Group sessions are identified by the ‘group therapy indicator’ field in the NAPC feeds (see spreadsheet IR1.2).
-
The costing method for these is detailed in CM14: Group sessions.
Mental health care programme approach (CPA) meetings
-
Care programme approach (CPA) meetings review a patient’s mental health care plan. They must be held annually but can be more frequent; and can take place in either a non-admitted setting or while the patient is an inpatient. You should ensure the costs of these meetings are allocated to Activity MHA261: CPA meeting.
-
CPA meetings will be recorded for the MHSDS and should be brought into Feed 3b: NAPC – mental health feed if they are held in the outpatient setting. Use the field ‘care programme approach review date’ to identify these reviews separately from other NAPC contacts.
-
Please note: Activity MHA261: CPA meeting should also be used for CPA meetings during admissions, showing as a component cost of the care but remaining identifiable.
Mental health liaison service
-
Patients reporting mental health illness in an acute care setting may require assessment and/or treatment for their mental health condition as well as their physical condition. Mental health liaison teams work in acute providers; usually in emergency departments, but they can also work in other areas such as outpatient clinics, emergency wards or elderly care wards supporting patients with dementia.
-
The cost of these services will be recorded in the mental health trust’s ledger or the acute provider’s ledger.
-
Some trusts will have patient-level data for these contacts, some will have aggregate data without patient records, and some will have no patient event information at all.
-
Where there is patient-level event information, and the cost of the resources is in your trust it should be costed at patient level. However, not all trusts have patient-level information for MH liaison services, so:
- if only aggregate level activity is available, you may cost this at average cost per unit in your costing system
- if no activity information is available in your trust, you should identify any cost in your trust and record it as ‘other activities’ so it is not allocated to patients who did not receive the service
- where there is cost in your trust but no activity, you should identify the cost as MH liaison services in the ‘other activities’ cost group. This cost should not be allocated to patients who did not receive the service.
-
You should use Activity SLA153: A&E – mental health liaison care to identify this service.
Other NAPC activities
-
Other activities may include, but are not limited to, the following:
- MDA062: Audiology assessments
- SLA129: External beam radiotherapy delivery
- SLA142: Chemotherapy delivery (these activities are used for both NAPC and admitted patient care (APC) patient events. There is no expectation that costing practitioners should reclassify the point of delivery from the one shown in the PAS)
- SLA132: Endoscopy
- SLA143: Pain management care
- CLA047: Sleep studies
- CMA303: Issuing of equipment.
-
Prisons or other judicial settings: use the activity ID relating to the care given, not the location where it took place. The location is identified by the ‘activity location type code’ field, not by the activity code. For example, endoscopy can be admitted patient care or non-admitted patient care – the activity is not location specific.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to ensure the auxiliary patient-level information feeds match to the correct NAPC contact. Examples include:
- medicines dispensed (Feed 10)
- pathology (Feed 8)
- diagnostic imaging (Feed 12a).
-
Where a clinician has contact with a patient during a patient event from a different department, this can be recorded on Feed 7: Supporting contacts and matched to the NAPC patient event. For example, where a specialist palliative medicine nurse attends an outpatient oncology clinic to see specific patients only.
Other considerations
NAPC events while the patient is admitted
-
If a patient is seen by a team, not in the ward and where the costs are not within the ward care activity, they can be recorded as supporting contacts and matched to the patient episode. See Feed 7: Supporting contacts. The cost of this care is part of the patient episode.
-
The only exception to this is if a NAPC patient event was pre-booked with a different service and the appointment takes place while the patient is admitted. This can be recorded separately as an NAPC event. For example, a substance use service visiting a patient admitted to a secure unit, when they have not been admitted for substance use.
NAPC ‘did not attends’ – for guidance only
-
We do not prescribe how to cost ‘did not attends’ (DNAs) but if required for local purposes, our recommended approach is available on FutureNHS.
Submission of NAPC events
-
You should note the extract specification feed type is named as OP, but this feed type contains the required data items to be submitted for the range of possible NAPC events described in this standard.
CM4: Emergency care attendances
Scope
-
This standard applies to emergency care (EC) attendances reported under treatment function code (TFC) 180 as defined in the NHS Data Dictionary and other treatment function codes where there is a record of the patient event in the Emergency Care Data Set (ECDS) which replaced the Accident & Emergency Commissioning Data Set (CDS type 010).
-
In scope are EC attendances at adult, paediatric and mixed ED units, single specialty emergency units, urgent treatment centres, minor injury units (MIU), walk-in centres (WIC) and ambulatory care departments/clinics. We have used the term EC to describe all the emergency units and ED to identify a 24 hour service area.
-
EC attendances should include ambulatory care attendances that are recorded in the ECDS as emergency care department type 05.
-
In scope of this standard are all EC attendances within the costing period, including all patients discharged in the costing period and patients still in the unit at midnight on the last day of the costing period.
-
EC services may carry out several types of activity that are all reported under TFC 180, including follow up appointments such as fracture clinics and admissions to clinical decision units. These are not EC attendances so are out of scope of this standard.
- Inpatient episodes reported under TFC 180 on the CDS should be costed using CM13: Admitted patient care.
- NAPC clinics reported on the CDS but not on the ECDS should be costed using CM3: Non-admitted patient care.
Overview
-
Patients attend or are brought to emergency units for life-threatening emergencies, less severe injuries and the fast or severe onset of clinical conditions. Some are 24-hour units and some have fixed opening times. Some have a full range of clinical services and some are clinical specialty-specific (such as ophthalmology).
-
The time a patient spends in an emergency care setting from arrival to departure is not an appropriate relative weight value (RWV) for allocating their costs, as someone with a relatively minor injury is likely to spend a disproportionate time in the department waiting to be seen.
-
However, establishing a full set of weightings by treatment is significant work. Superior costing methods offer options for advanced costing (see spreadsheet CP3.5 Superior and alternatives).
-
For the non-24-hour units covered by this standard, and for the single-specialty units, duration of attendance can be used by specific agreement with the service team. For example – where gynaecology-specific units all have the basic investigation/treatment, time may be agreed as a valid allocation method. You should record these agreements in the ICAL worksheet 14: Local cost allocation methods.
Approach
Information requirements
-
Obtain Feed 2: Urgent care (EC/MIU/WIC), for all emergency units – including mono-specialty units, urgent treatment centres, MIU walk in centre attendances and ambulatory care as described in IR1: Collecting information for costing and spreadsheet IR1.2.
-
The feed contains data items from both CDS and ECDS. The latter have been added to show the planned move to ECDS for all services. This change has not yet been completed because HRGs cannot be calculated from the ECDS data (SNOMED-CT) and are still required for national reporting. You may update the data items in line with your local reporting needs. The new data items will have the same impact on the National Cost Collection as the old data items.
-
Note: Clinical decision unit (admitted patient care) patient events are recorded on Feed 1a: APC. Outpatient appointments will be recorded on Feed 3a: APC and should not be included in Feed 2: Urgent care (EC/MIU/WIC).
-
The superior costing method SCM58: EC – Weighted treatments costing process requires treatment/procedure codes. Either CDS or SNOMED-CT codes can be used in Feed 2: Urgent care (ED/MIU/WIC) in spreadsheet IR1.2 for the costing process but please note the HRG is a mandatory requirement. In future years, the costing process will require the SNOMED-CT codes as used in the ECDS. If the SNOMED-CT codes are used, they need to be mapped to the HRG codes using the Secondary Uses Services (SUS) mapping.
-
Where there are no treatment/procedure codes in the data to be used for costing, review the data quality with the service team. If no treatment/procedure is confirmed, use the duration of the attendance as the cost driver with minimal nursing staff and administration time agreed locally.
Specialist cost centres and expense codes
-
You should refer to spreadsheet CP2.1 standardised cost ledger to identify the cost centres for emergency care.
-
Where staff cover different parts of the emergency department, you should customise the cost ledger using local digits to replace the XXX, to disaggregate the cost of staff to the relevant patient area: for example, main EC unit, clinical decision unit, outpatient attendances, eye casualty, dental emergency department, minor injuries, ambulatory care unit.
-
You need to identify the proportion of time spent by staff in the different parts of EC. Obtain this understanding through discussion with service managers and clinical leads covering the different activities. For example, consultant A works:
- 50% of their time in EC, so 50% of their costs should be allocated to a disaggregated cost centre and attached to Feed 2: Urgent care (EC/MIU/WIC)
- 50% of their time on the clinical decision unit (admitted patients), so 50% of their costs should be allocated to a different disaggregated cost centre so the costing process can use Feed 1a: Admitted patient care (APC).
Resources
-
Identify the staff in the EC attendance from the actual or planned staffing levels and allocate to the resources for the service provided.
-
Please note – general practitioners should be separately identified, using the resource SGR077 General Practitioner – secondary care, to separately identify the cost of GP within and before the EC attendance. See the integrated collections guidance for further information about the separate identification of GP streaming services.
Activities
-
You need to identify the EC activities your trust delivers from the prescribed activity list in spreadsheet CP3.2.
-
Please note, SLA159 Streaming before emergency department attendance maps to collection activity EMC002 Streaming before emergency care department and is excluded for collection purposes on the reconciliation statement.
Costing using treatment/procedures information
-
As a superior costing method SCM58, costs for each patient event should be weighted by the treatment/procedure they receive. See Spreadsheet CP3.5 Superior and alternatives.
-
Set up relative weight values (RWVs) for each treatment/procedure type to use in the costing process. You need to develop these in conjunction with the EC clinical and service leads. Table CM4.1 shows how the statistic allocation table could look although all values are for illustrative purposes only. Your data feed may include SNOMED treatment/procedure codes, not those shown in Table CM4.1.
Table CM4.1: Example statistic allocation table per treatment/procedure
| Treatment/ procedure code (SNOMED-CT) | Procedure | Nurse (min) | HCA (min) | Consultant (min) | Non-consultant medical staff (min) | Patient- specific consumables (£) |
|
SCTID: 10849003 Removal of foreign body (procedure) |
Removal of foreign body |
60 |
30 |
10 |
20 |
10 |
|
SCTID: 15631002
|
Application of dressing (minor procedure) |
60 |
30 |
5 |
10 |
20 |
|
SCTID: 439569004
|
Resuscitation (procedure) |
120 |
30 |
60 |
60 |
75 |
|
SCTID: 284182000 |
Gluing of wound |
60 |
30 |
5 |
10 |
10 |
-
Where there is more than one treatment/procedure code, use the first code as the basis for the allocation of cost. As a superior costing method SCM47 EC using more than one treatment to weight the cost, you can use a weighting based on a combination of codes. See spreadsheet CP3.5: Superior and alternatives.
-
Clinical investigations such as scans and pathology tests should be matched to the patient event from the auxiliary feeds. However, where these investigations are not recorded on a prescribed feed, as a superior costing method SCM45: EC clinical investigation weightings you can apply additional acuity weightings to the cost allocation based on the investigations shown in the EC CDS or the Emergency Care Clinical Investigation (SNOMED CT) field. See spreadsheet CP3.5: Superior and alternatives.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to ensure the auxiliary patient-level feeds, such as diagnostics, match to the correct EC attendance, APC or NAPC patient event.
Other considerations
Major trauma patients
-
Treat major trauma patients in the same way as above; they should be allocated their own costs depending on the treatment/procedures they receive.
-
The cost of the major trauma team should be allocated across all patient events for flagged major trauma patients,
-
Use the major trauma flag in Feed 2: Urgent care (EC/MIU/WIC), in spreadsheet IR1.2 to identify these patients.
-
Most major trauma patients will have an EC attendance recorded on arrival, but some patients will be admitted without an EC attendance, for example those transferred straight to theatre. The cost of the major trauma team should be allocated across all patient events for flagged major trauma patients, including any admissions without an EC attendance.
-
You should discuss with your major trauma team the care they give once the patient has been moved from EC into an admission and build this information into the allocations to the patient for the major trauma team cost.
-
Be aware that major trauma patients will have separate data recorded and a separate funding source, so their identification will need to come from the alternative data source and be flagged in Feed 2: Urgent care (EC/MIU/WIC), to allow you to correctly allocate the costs of the major trauma team.
-
Major trauma patients may have critical care input while in EC CM6: Critical Care provides guidance on how to identify these costs. The costs of the critical care input should be included in the costs of the EC attendance. If the patient is later transferred to critical care, they will also have separate patient event(s) for critical care.
CM5: Theatres and special procedure suites
Scope
-
This standard applies to all surgical operating theatre and special procedure suites (SPS) activity.
-
For this standard, the term ‘theatre’ includes main surgical operating theatres and special procedure suites such as cardiac catheter laboratories, endoscopy and electroconvulsive therapy suites. Procedures performed in treatment rooms in a non-admitted patient care setting should be included, for example podiatry. See CM3: Non-Admitted Patient Care.
-
High-cost equipment such as robotics are included in this standard.
-
High-cost clinical implants and devices used in theatres are covered in CM21: Clinical non-pay items and are out of scope of this standard.
Overview
-
Theatre services are at the centre of the hospital system and cover a wide range of activities, whether scheduled or unscheduled, complex or more routine procedures. Such services are delivered by skilled clinicians using high value clinical infrastructure in sterile environments, and often, suites specially designed for the types of procedures.
-
Theatre costs include the cost of the patient arrival in the suite, anaesthesia, the surgery/intervention, recovery and time waiting to return to the ward or be discharged. Theatre costs must include all appropriate out-of-hours and waiting list costs.
-
Only allocate costs to patients who have attended the theatre unit for surgery/procedures during the session. If the patient attended the unit but did not have the procedure, the theatre record will show the stage the patient reached before the procedure was cancelled. Costs should still be allocated for the relevant stages.
-
There should be no separate cost event for planned or unplanned downtime; the time lost for downtime should be removed from the calculations for the costing process.
-
Superior costing methods on spreadsheet CP3.5 that can increase the accuracy of your theatre costing are:
- SCM21: Theatre set up and clean down time – allocating costs to the specific theatre and therefore the patients using that theatre
- SCM23: Unused time in theatre – allocating costs to the specific theatre and therefore the patients using that theatre
- SCM57: Procedures costed in theatres/SPS: allocating costs based on the complexity of the procedures performed, including the costs of additional staff from different services
- SCM75: Theatres/SPS – actual staff by session: allocating the actual pay costs of the staff in attendance at those sessions rather than using an average.
-
The staff in a procedure will have the specific skill mix to perform the task and will usually be consistent in a theatre for a session. You should work with your theatre manager(s) to obtain, understand and use this information for costing the patient procedure.
Approach
Information requirements
-
Obtain Feed 13: Theatres, as prescribed in IR1: Collecting information for costing and Spreadsheet IR1.2. This includes the required session and procedure information, but we appreciate there might not be as much information available for SPS as there is for theatres.
-
Special procedure suites may use the same, or different, data recording and planning system as theatres. You should identify the information and include it in Feed 13: Theatres, to provide consistent information. Where smaller service areas have different information systems, you should prioritise work programmes based on the locally agreed materiality.
-
Feed 13 includes the primary surgeon and anaesthetist for the operation. It may also identify second and subsequent surgeons, anaesthetists and other medical staff for the operation.
-
Some complex operations may require two or more surgeons, multiple anaesthetists and last many hours, making them high cost activities. It is unlikely all these staff are recorded on the standard electronic theatres data.
-
As a superior costing method SCM75: Theatres – actual staff by session, where the expected cost of these additional staff is material, review this issue with the clinical/service leads to see if alternative information can be obtained. If it can, bring this information into the costed patient record. Use the actual staffing mix of grades, although a permissible alternative is the planned staffing mix, where this data is more reliable.
-
You should understand how the data shows the different timestamps in spreadsheet IR1.2 to ensure that costs are allocated using the correct durations. Surgeons will usually be present for the time period known as ‘knife to skin’. Consultant anaesthetists will be responsible for the patient for longer, from anaesthetic start time until they are out of recovery.
-
There may be instances where two theatres share an anaesthetist at the same time. You should consider this in your allocations.
Specialist cost centres and expense codes
-
In the standardised cost ledger, you should use cost centre XXX051: Theatres/SPS. This can be customised using local digits to replace the XXX if you need to disaggregate costs for main theatres and specialist procedure suites of different types.
-
Where a provider has theatres on separate sites, you should ensure that the theatre costs are identified by site and apportioned to the theatre minutes used on that site.
-
Use the expense codes for the type of staff in the suite, as shown in spreadsheet CP2.1.
-
Theatres can include both nurses and separately trained operating department practitioners.
-
Many high-cost implants will be in the general ledger linked to theatres. You should ensure these are identified and allocated in accordance with CM21: Clinical Non-pay items.
Resources
-
The resources for theatres are shown in spreadsheets CP2.1.
-
As superior costing method SCM75, where the individual staff are recorded at patient-level in the theatre information, their actual costs, which may be identified from a general ledger or payroll data source, can be calculated at an individual level in the costing system and allocated to specific activities and on to specific patients.
-
You need to consider the cost of capital charges, lease and repair costs for high-cost equipment – for example robotics – and ensure these costs are only allocated to patients who were treated using them.
Activities
-
You need to identify the theatre activities and SPS activities your trust delivers from the prescribed activity list in spreadsheet CP3.2.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to ensure the costed theatre activity is matched to the correct patient episode.
Other considerations
Sterilisation costs
-
Sterilisation services can be within the trust or contracted in. The costs should be allocated to the department(s) that use the service using resource T1S131 Sterile services
. -
As a superior costing method SCM76: Sterile services at patient level, you can allocate the cost to patients for specific items where information on the sterilisation service provided is available at patient level.
-
As a superior costing method SCM32: Sterile services – trays by procedure, you can allocate costs using the procedure codes from the theatre record. This is not as effective a method of allocation as SCM76 but may provide improved information over the prescribed allocation method shown in spreadsheet CP2.2 Overhead allocations. Both these superior costing methods will require work with the sterile services team to establish the costing methodology.
Costing emergency and out-of-hours theatre sessions
-
Theatre timetables will include planned sessions and sessions held for emergency patient needs, such as ‘expected’ non-elective maternity theatre sessions and flexibility for trauma or other emergency surgery. Emergency theatre activity costs can be materially higher per patient due to the lower use of emergency theatre sessions. Work with the theatre leads to decide if a further weighting is appropriate for this work.
-
Theatre staff are often scheduled to work outside a nine-to-five working day. However, sessions such as overnight, weekends, bank holidays may incur additional costs that are materially higher than in-hours work due to the enhanced salaries payments.
-
Theatres will also have sessions that use staffing above the planned level, for example, for clinical need or to support capacity requirements. These sessions may require additional staff payments over the cost of standard working rates.
-
The prescribed allocation method is for these costs to be allocated to all patients who have used the theatre during the costing period, weighted by actual theatre minutes. However, you may discuss with the theatre leads and costing steering group whether higher cost weightings for emergency/out-of-hours sessions should be allocated to patients in these sessions. This issue should be discussed because the staff responsible for the operations often have no control over whether a theatre session is a normal one or unplanned.
-
Do not assume all emergency and out-of-hours costs relate to non-elective patients, as patients admitted electively may need to return to theatre out of hours or may be on waiting list initiatives. Wherever possible, use unique episode identifiers to allocate these additional costs.
CM6: Critical care
Scope
-
This standard applies to adult, paediatric and neonatal critical care and high dependency unit (HDU) activity provided by the trust including but not limited to:
- intensive care units (ICU)/intensive therapy units (ITU)
- specialist care units (SCU)
- high dependency units
- high dependency beds and critical care beds on a general ward with a Critical Care Minimum Data Set (CCMDS) record
- critical care ‘outreach’ teams working on non-critical care units (critical care outreach is a clinical/service management term. For costing, note the differences from mental health outreach, as they have different costing allocation methods)
- critical care transport and the critical care transport network.
Overview
-
Critical care units, sometimes called intensive care units or intensive therapy units, are specialist hospital wards that provide treatment and monitoring for seriously ill patients. They are staffed by specially trained healthcare professionals and contain sophisticated equipment for monitoring and treatment. They are a core part of acute admitted patient care and for costing are treated separately from the general ward stay.
-
High dependency units are critical care units but contain patients with less complex conditions than the intensive care unit patients, and will usually have a lower staff to patient ratio.
-
All critical care patients should have a nationally mandated critical care record. In this standard, for brevity we refer to the CCMDS as covering all ages.
- babies under 1 month are recorded using the Neonatal Critical Care Minimum Data set (NCCMDS) (This timeframe varies across organisations, depending on the care needs of the baby, especially where the baby is born significantly before the expected delivery date.)
- children are recorded using the Paediatric Critical Care Minimum Data Set (PCCMDS)
- adult critical care patients are recorded using the Critical Care Minimum Data Set (CCMDS).
-
Patients with a critical care record may be in designated critical care units, HDU or on other wards.
-
The critical care data is used for the costing process. Local commissioning rules may govern the treatment of critical care patients differently from these datasets, so you should understand any differences for your local reporting process.
-
Use the following audit and system-based terminology so that you can have clear conversations with service and informatics colleagues:
- Adult: CCMDS is the data recorded for patients in an adult ward and is part of a wider research and audit dataset called ICNARC (Intensive Care National Audit and Research Centre).
- Paediatric: the data sent to the PCCMDS is part of a wider research and audit dataset PICANet (Paediatric Intensive Care Audit Network).
- Neonatal: Some trusts record neonatal data on the BadgerNet system, which is used by the trust as the source data for the nationally mandated NCCMDS submission. This data is also sent to a national research database BadgerNet.
-
Ideally each bed day of a critical care or high dependency ward stay should be costed as a separate patient event. This is to show the high level of cost variability in these services by day.
-
The patient’s inpatient care will be recorded in the main PAS as an episode that forms part of the Commissioning Data Set (CDS). The HRG grouper will use ICD10 and OPCS data within the CDS data to provide a core HRG for the episode; and use the unit function code to identify the patient critical care days within the episode.
-
The critical care data items for critical care are also recorded in provider information systems. The grouper mainly uses the critical care data items to create the relevant HRGs, not the ICD10 or OPCS codes within the core HRG. See Consultant Episode (Hospital Provider) (datadictionary.nhs.uk).
-
All patients will have an underlying episode called the ‘core’. This episode will have a core HRG showing the nature of the care without the critical care.
- Some trusts create a separate, standalone episode for the time spent in critical care showing the consultant transfer of care to an intensive care consultant.
- Other trusts do not have a separate episode but identify the critical care period from the critical care data items, as part of the core episode.
-
You should find out whether critical care is shown as a standalone episode or as part of a core episode used by your trust, so a critical care patient event by day can be shown in the costing system and costed separately from the core episode.
-
You should work with your service/clinical leads to understand the costs. Costs to consider for critical care include:
- nursing
- consultants and non-consultant medical staff
- allied health professional staff (physiotherapists, pharmacists, dieticians, speech and language therapists, occupational therapists, psychologists)
- other staff (healthcare assistants, cleaners, admin staff)
- clinical support services (for example pathology, radiology)
- extracorporeal membrane oxygenation (ECMO) and extracorporeal life support (ECLS)
- enhanced recovery teams (preoperative critical care input) and perioperative and critical care teams (PACE)
- critical care outreach teams
- medical and surgical consumables and equipment
- medicines dispensed
- critical care transport.
-
You also need to consider the data for, and cost of, the following types of patients, which will not be recorded on the critical care data set:
- non-critical patients in a critical care bed
- critical care staff attending major trauma patients in emergency care or other areas
- patients involved in research studies
- critical care ‘outreach’ teams.
-
Patients in a temporary critical care bed in a general ward, recovery or other unit will only be classed as critical care for costing if recorded in the critical care data set.
-
Additional factors to consider when reviewing your costed critical care:
- There should be no cost to the core episode when the patient is within the critical care unit.
- The first day in critical care may incur more costs, including nursing and medical staff input. You should discuss this factor with the critical care service team, to set appropriate relative weight values.
- Auxiliary feeds should be matched to critical care according to the hierarchy in spreadsheet CP4.1. This will ensure the cost of any additional services such as pathology and medicines are allocated to the specific bed day when they occurred.
- Lengthy stays in critical care may incur additional costs, as long periods of critical care may impact the patient’s condition. You should include critical care ward support in allocations of therapies and professional/technical services as agreed with those services. Or you can obtain Feed 7 Supporting contacts to show the cost of patient-level contacts for each patient, by day.
- Consultants from the core episode may visit the patient while in critical care. This may be part of their ward round information (superior costing method SCM71: Ward rounds at patient level) or identified as additional visits (Supporting contacts allocated at patient level). If material, these superior costing methods enable you to include this additional cost of patient care.
-
Discuss cost and data factors with the critical care team so that you understand the issues and set costing rules accordingly. Document these rules in integrated costing assurance log (ICAL) worksheet 14: Local costing methods.
-
In addition to the service leads, the local representative of the Operational Delivery Network (ODN) for each critical care area is a useful contact.
Approach
Information requirements
-
Obtain the appropriate patient-level critical care feed (Feed 6a: Neonatal, Feed 6b: Paediatric and Feed 6c: Adult) as prescribed in IR1: Collecting information for costing and in spreadsheet IR1.2. Some trusts may need to use Feed 4: Ward stay, to identify the ward days in their APC data, and ensure they are not duplicating days in the underlying episode.
-
Ideally, all critical care records should be available in the costing system as a bed day record.
-
Once the data has been gathered from the relevant data source, all age groups are costed in the same way – cost is attached to each bed day.
-
Consult your software supplier to explain how your trust records critical care and establish the appropriate method in your costing system to create the costed critical care bed day record. This will be either:
- as a discrete episode with transfer of care to a consultant intensivist (anaesthetist)
- or the patient episode continues under the surgical or medical consultant, and feeds 6a, 6b and 6c or Feed 4: Ward stay, will show the relevant critical care unit.
-
All trusts submit data to the national Critical Care Minimum Data Sets (for example adult CCMDS, PCCMDS and NCCMDS). You should reconcile the activity submitted to this dataset and not to the ICNARC, PICANet or BadgerNet datasets as they are owned by separate trusts and they cleanse the data and apply HRG codes using the payment grouper, so the HRG may be different to that in the critical care dataset and the costing system. For example, PICANet is part of the national audit programme managed by Healthcare Quality Improvement Partnership (HQIP). Where your organisation does not submit to the national dataset you should reconcile to the local system data and record this method in the ICAL.
-
The national critical care data sets undergo data cleansing, and the data may be sent back to the provider with the expectation that the data cleansing is repeated in the local system. You should find out whether the data cleansing advised by these datasets has been used to update the local data before resubmission. This allows the closest possible reconciliation of costed data to the national dataset.
-
Other data differences between the costing system and the national dataset may include:
- Timing of data extracts: has data been updated in your local systems since the data was sent to the national dataset?
- The costing grouper adds a day for part days in the length of stay calculation, where national datasets do not.
- All patients should have a PAS episode, which should be costed if the patient does not have a critical care record. This applies even if they are on a critical care unit. For example, a well baby may be cared for on the neonatal unit because the mother is unwell. The baby may not have a critical care record but should have their main episode costed with the costs of a neonatal unit patient. These patients may not be in the national dataset.
-
Data transfers for costing between critical care, main PAS episodes and the costing system should be carefully reconciled as it is reported that this process can easily miss patients.
-
You should ensure the unit function code for your critical care patients is correct. All critical care unit function codes are used for costing and reporting. You should not manually group unit function codes based on previous years of costing guidance.
-
As the critical care record costs on a ‘by day’ basis, patients not yet discharged or moved from critical care to a general ward area are always costed in conjunction with incomplete patient events. See CM2: Incomplete patient events. The critical care data will identify when the critical care period ends for the patient.
Critical care patients on a general ward
-
Where there are critical care (ICU or HDU) beds on a general ward or recovery unit, these patients should have a critical care record in the critical care data set, and these patients should be included on the acute hospital critical care feeds (feeds 6a, 6b and 6c). This identifies them as a critical care patient and not ‘outreach’. They should also be flagged in feed 4: Ward stay, using the ‘critical care bed on a general ward’ field in spreadsheet IR1.2.
-
The critical care data set allows these patients ‘to be recorded in any location where critical care is provided’. This may differ from your local commissioning arrangements.
-
Note: paediatric and neonatal critical care patients are treated on general wards far less frequently than adults.
-
You will need to work with the ward manager to identify how – or if – the nursing ratio differs for these patients. If relevant, you will need to set up relative weight values to ensure the critical care patients receive a higher proportion of the general ward nursing costs than those in the other beds.
-
These patients will not normally receive care from the ‘critical care outreach team’ as if they have a critical care record they will be supported by the main critical care units. You should also discuss the support these patients receive from critical care staff and allocate their costs accordingly. Critical care outreach services are described later in this standard.
Non-critical patients in a critical care bed
-
In exceptional circumstances, patients who do not require critical care may be placed in a critical care bed (non-critical care patients) including where beds are flexed to accommodate step-down patients waiting for a bed in another trust. Their care needs are not as high as those for a critical care patient.
-
If material in number or cost, the allocation of cost should be discussed and agreed with the critical care team.
-
These patients should have a note on their critical care record. Flag them in feeds 6a, 6b and 6c: Critical care, using the ‘non-intensive care unit patient flag’ field in spreadsheet IR1.2. We note the end date may not be consistently recorded on the local dataset to reflect this change in care level on the unit. Please note the materiality of this work.
Specific cost centres and expense codes
-
Critical care cost centres are listed in spreadsheet CP2.1.
-
These can be customised in your local cost ledger if you have different discrete costs centres for the different unit function codes. There are separate cost centres for the critical care transport service and network so these can be allocated using different methodology to the other units.
-
Use expense codes appropriate for staff type and band. You may need to disaggregate the costs of staff covering more than one unit or service area, to ensure the correct resource is applied.
-
Adult critical care units are led by anaesthetist consultants called ‘intensivists’, as opposed to theatre-based anaesthetists. Paediatric and neonatal intensive care units are normally led by consultants who are not anaesthetists. You should use the appropriate expense code for medical staff in each unit.
-
Junior medical staff will cover both critical care and theatre-based services, but when on the rota in critical care, they should map to the resource of the medical staff role they are performing (for example, non-consultant medical staff – anaesthetists).
-
Where critical care and high dependency unit costs for multiple wards are within one cost centre, you should disaggregate the cost at the general ledger to cost ledger mapping stage. You should agree the weighting with the service lead. Here is an example of relative weight values for nursing where cost of all critical care units is contained in one cost centre:
- HDU 1: 0.5 nurse
- HDU 2: 0.5 nurse
- ICU 1: 1.0 nurse
- ICU 2 (specialist unit, for example liver): 1.5 nurse.
Resources
-
The medical and other clinical staff resources for critical care are shown in spreadsheets CP2.1 and CP3.1.
Activities
-
You need to identify what critical care activity your trust delivers and map this to the prescribed activity list in spreadsheet CP3.2.
-
These activities represent the ward care of the unit for that day’s care. There is no separation between different staff types. Patients with a critical care record should not use the activity ID SLA156 as this relates to non-critical care wards only.
-
Within one critical care unit, there may be different levels of care provided. Using superior costing method SCM77: Critical care acuity within one critical care unit you can work with the clinical team to apply weightings to beds or specific patients. Here is an example of relative weight values for patient or bed-level acuity information (locally determined) and therefore nurse/medical staff in one critical care unit:
- Patient A/Bed A: 1.0 nurse: 1 medical staff
- Patient B/Bed B: 0.5 nurse: 0.5 medical staff
- Patient C/Bed C: 1.5 nurse: 1 medical staff
-
Data fields in the critical care record that may offer data on unit or patient acuity include:
- nursing acuity care level (CCMDS)
- unit function code (CCMDS)
- acuity score (local source)
- HRG (paediatric and neonatal). In these datasets, the HRG is applied per day so acuity by day can be identified. The HRG cannot be used in this way for adults as it is the highest level of care in the critical care period.
-
As the cost is calculated for each day, you should also consider the treatment of step-down bed moves within one critical care unit. For example, where a patient has higher acuity on days 1-4 but on day 5 has improved and requires less intervention for the rest of their stay. The adult critical care HRGs do not show this variation, and the patient will still have the same HRG for all days of their critical care period within one unit.
Medical and surgical consumables and equipment
-
Use the process described in Standard CM21: Clinical non-pay items to cost medical and surgical equipment.
Matching
-
Costs such as pathology, therapies, diagnostic imaging, and other clinical support services will also be incurred in critical care. Examples include Feed 8: Pathology and Feed 12a: Diagnostic imaging (CRIS).
-
Use the prescribed matching rules in spreadsheet CP4.1 to ensure the activity and costs on auxiliary feeds are matched to the correct critical care patient bed day, not just to the APC episode. For example, pathology tests should be matched to the critical care record of that day.
-
You should not match the costs from auxiliary feeds to the core episode if the patient is in critical care. The exception to this is theatres, as surgery is deemed to be part of the core episode, not the critical care episode.
-
The only time theatres can be matched to the critical care episode is where the patient spends no time on a ward other than critical care; therefore, the critical care period is the core episode. For this reason, critical care is lower in the matching rules for Feed 13: Theatres, in spreadsheet CP4.1. You should review any patients who match to critical care, to ensure they spent no time on a general ward.
Other considerations
Extracorporeal membrane oxygenation (ECMO)/extracorporeal life support (ECLS)
-
ECMO and ECLS use an artificial lung (membrane) located outside the body (extracorporeal) to infuse blood with oxygen (oxygenation) and continuously pump this blood into and around the body.
-
ECMO is used mainly to support a failing respiratory system, whereas ECLS is used mainly to support a failing heart.
-
All ages of patient in the relevant specialist units can receive ECMO/ECLS. The cost of these techniques is significant so they should be costed at patient level. These patients are likely to report higher costs against their critical care activities than critical care patients with a lower acuity.
-
You should use resource SLR087: ECMO/ECLS equipment and the Activity SLA105: Critical Care – ECMO/ECLS to identify patients who have received ECMO/ECLS during their critical care stay. The Activity SLA105 represents the whole of the ward care given for that day, so when the patient no longer receives ECMO/ECLS care, they will move to Activity SLA159: Critical care – ward care.
-
You will need to access local data on which patients use ECMO/ECLS in your critical care units. The critical care record has a ‘critical care activity’ for ECMO but does not distinguish ECLS separately, so local information will be required.
-
You can add the information to create the ECMO/ECLS flag in each of the critical care feeds (feeds 6a, 6b and 6c) in spreadsheet IR1.2 to identify which day ECMO or ECLS has been delivered.
- Ensure these patients receive the appropriate nursing and medical staff acuity costs.
- Clinical perfusion scientists – or ‘perfusionists’ – may be involved in delivering ECMO/ECLS. They are a separate type of care professional from medical staff or nurses. As superior costing method SCM52 Perfusionist team, you can identify their work separately and match their costs to the patients they work with using Feed 7: Supporting contacts.
- Some information on ECMO/ECLS equipment and consumables may come from databases separate from the main critical care record. You should identify material costs and allocate them using information from the critical care department or the relevant specialist team.
Critical care transport
-
You should identify the cost of critical care transport separately from critical care. This is because critical care transport patients do not always have critical care episodes in the same hospital, so the cost should be identifiable in the costing system.
-
Where your trust is providing the critical care and specialist transport staff and non-pay for the critical care journeys, this is part of the ‘own patient care’ cost group.
-
Use resource SLR086: Critical care – transport fleet for the cost of the vehicles, maintenance and running costs. For staff and other non-pay, use the relevant resource or overhead code.
-
Use the prescribed cost allocation rules in spreadsheet CP3.3 for all age groups using the Activity SLA106: Critical care – journey. Paediatric and neonatal patients should have patient-level information available as there are separate HRGs for this service. For adults, the cost should be allocated based on service manager/clinical lead information according to patient acuity and/or duration of the journey made.
-
As a superior costing method SCM66, if your trust provides adult critical care transport, you can obtain patient-level Feed 6d: Critical care transport, for this as prescribed in IR1: Collecting information for costing and spreadsheet 1.2.
-
If your trust hosts the network for critical care transport, you are likely to hold the network and central administration costs for running this service. Identify these costs in the cost ledger using the resource SLA086: Critical care – transport network, and Activity SLA162: Critical care transport network which flows to collection activity SEN001 Services excluded from the National Cost Collection (via the reconciliation). This will show the costs separately. See the integrated collections guidance for further information.
Critical care outreach teams
-
Critical care outreach teams support clinical staff in managing acutely ill patients by providing closer observation of ‘at risk’ patients on non-critical care wards. These patients will not be recorded on the critical care record if just receiving contact from the critical care outreach team.
-
For care provided by nurses on critical care outreach teams use the resource SLR082: Specialist nurse and Activity SLA163: Critical care outreach on general ward.
-
Agree a local allocation method with the critical care outreach lead.
-
The critical care outreach team activity can be recorded on Feed 7: Supporting contacts and matched to the patient event.
Major trauma patients and other emergency department support
-
Some patients in the emergency department (ED), including major trauma patients, may require material critical care input. You should ensure the cost shows as a component of ED care and not as part of critical care. See CM4: Emergency care attendances (including ED, minor injury units and walk-in centres).
-
You will need to discuss and agree with the critical care team:
- how information is collected for major trauma patients (and other ED patients) who receive input from the critical care team
- how this input is measured; that is, who in the team provides the input
- a scale to weight the input; that is, how long a member of the critical care team stays with the patient. This could be a sliding scale based on patient need.
-
Supporting contacts allocated at patient level, can be entered onto Feed 7: Supporting contacts, matching to Feed 2: Urgent care (ED/MIU/WIC).
Perioperative/pre-rehabilitation and postoperative teams
-
Critical care staff in ‘enhanced recovery’ or ‘post-acute care enablement (PACE)’ teams may support patients across non-critical care wards/specialties. These will:
- pre-screen patients for treatments
- prepare them for surgery
- improve the effectiveness of patient rehabilitation
- facilitate effective discharge by co-ordinating care across specialties, disciplines and trusts.
-
Where these services are in place the critical care staff costs should be disaggregated between pre-rehabilitation/postoperative work and work on the critical care unit. Costs should be allocated to the patients who have received the different types of care.
-
You can allocate the relevant staff costs using patient-level activity on Feed 7: Supporting contacts, matched to specific patient outpatient appointments or admitted patient care episodes. Only patients who have received care from the relevant team should be allocated their costs.
Follow up contacts for critical care staff
-
In many units, medical and nursing staff will have follow-up contacts with the patient after they have left the critical care unit to support the ongoing effect of critical care. These will be recorded as clinical activity to ensure the electronic patient record is complete and should be costed according to the resources used.
-
Where these are outpatient or home visits, they should be included in Feed 3a: Non-admitted patient care and costed as a separate patient event using the data item in spreadsheet IR1.2 ‘Activity location type’ to identify where the patient event took place.
-
For contacts while the patient is on a non-critical care ward, the event can be recorded in the supporting contacts feed, and the cost attached to the core HRG, rather than to the critical care event.
Part day costs and transfers
-
Part-day costs should be applied to the critical care record as the costs are incurred. When the patient leaves critical care or dies while in critical care, the minutes of the day will form a part-day cost.
-
For patients discharged from the critical care bed to a non-critical care ward, the costs relating to the non-critical care ward should be included in the cost of the final critical care bed day.
CM7: Private patients and non-English NHS-funded patients
Scope
-
This standard applies to activities relating to all patients funded from outside English NHS commissioning, including private patients, overseas visitors and patients funded by the Ministry of Defence. For this standard, these are called CM7 patients.
-
It also applies to patients funded by English NHS commissioning of an NHS provider but managed and paid for via a third party, for example capacity purchased from a local private hospital.
Overview
-
CM7 patients should be costed regardless of whether they are on NHS wards or private/designated wards. Conversely, NHS patients on private patient wards should be costed using the costs of the ward they were on.
-
The relevant episodes, attendances and contacts must be flagged in the costing system.
-
Costed activity for these patients should be reported as ‘own patient care’, along with the corresponding income for local reporting and business intelligence purposes.
-
We recognise there may be issues with recording these patients. For example, private patient records may be held on a separate patient administration system (PAS). This should be brought into the PLICS where possible, to ensure consistency of costing across NHS providers.
-
The income for these patients should be correctly identified and aligned to the correct patient event for service line reporting, and not netted off from cost. This treatment is on the basis that all patients for whom the English NHS provides care should be costed in the same way, irrespective of the way their care is funded.
Approach
-
CM7 patients should be costed in the same way as patients funded by the English NHS, using the resources, activities, and prescribed cost allocation methods in spreadsheets CP3.1, CP3.2 and CP3.3.
-
They should also be included in the allocation of support costs
-
You can identify who funds each patient episode, attendance or contact for these patients from their ‘organisation identifier (code of commissioner)’ and their ‘administrative category code’ in spreadsheet IR1.2.
-
Cost centres for CM7 patients are included in spreadsheet CP2.1 standardised cost ledger and can be customised to show other types of CM7 patients in your local cost ledger.
-
Private patients’ administration and overseas visitor managers’ costs have been classified as an overhead cost in the standards. These costs should be allocated directly to these patients as prescribed in spreadsheet CP2.2.
-
The patient’s ‘administration category code’ may change during an APC episode. For example, the patient may opt to change from NHS to private healthcare. In this case, the start and end dates for each new administration category code should be recorded in Feed 1a: APC, so all activity for CM7 patients can be correctly identified and costed accurately.
-
Non-admitted patients cannot change status during one attendance or contact.
-
Spreadsheet 3.4 shows the resource and activity combinations for private patient administrators and overseas visitor management teams.
-
Do not include any costs in the costing process for CM7 patients where the costs incurred do not sit in the trust’s accounts. For example, where a consultant saw a patient using NHS facilities and staff but separately invoices the patient/healthcare company for their time, you should allocate the facilities and other staff cost to that patient but not the consultant time. This example presumes the patient contact was recorded on an NHS data system.
-
Therapy, medicines, diagnostic tests, critical care costs, social care and other costs should be included in the costing process for CM7 patients unless they do not sit in the trust’s accounts.
- If the patient receives a service that is additional to those received by an English NHS-funded patient, these costs should be identified and allocated to that specific patient – for example:
- private room costs
- additional catering costs
- additional clinical or holistic treatments, tests, and screening not normally available on the English NHS patient pathway
- privately or charitably funded specialist limbs/equipment, including those provided to veterans and children.
-
Private patient wards may include NHS beds where the provider’s NHS wards are facing capacity challenges. The cost of the private patient ward should be allocated to the patients occupying the beds, irrespective of how they were funded.
-
The income received for caring for private patients and other non-English, NHS-funded patients must be allocated to the correct episode, attendance, or contact. This will ensure any profit is shown against the private or other non-English, NHS-funded patient and not netted off from the English, NHS-funded patient care costs.
CM8: Clinical and commercial services supplied or received
Scope
-
This standard applies to all activities a provider performs that do not relate to the care of its own patients (services supplied).
-
This standard also applies to care provided to one trust’s patients by another organisation (services received).
-
This standard applies to where a costed patient event only shows part of the cost of care that the patient received.
-
The services can be clinical or non-clinical.
-
The services will include care provided by NHS trusts (sometimes termed ‘provider to provider’) and commercial activities that are outside standard NHS contracts (both for NHS and non-NHS organisations).
-
This standard applies to the patient events impacted, irrespective of the funding arrangements of that care.
Overview
-
Services provided by one organisation to another should have a contract in place to confirm the specification of the service provided. This document gives useful information for the costing process: it should state the remuneration agreement and include requirements for information about the service provided to be received by the receiving organisation. You should work with your contracts team to understand the services provided, and where the cost/income sits within the general ledger.
-
The detail of electronic data flows to the receiving organisation should be established in the contract.
- Where the service is for patient care activity, a patient-level clinically coded record should be received. This will be entered into the patient administration system (PAS) and flow into the costing system with the other patient events.
- Where the service is for clinical supporting items, such as medicines or diagnostic tests, the data should be received with patient identifiers for clinical safety. You can use this information to match the cost to the patient event.
- Where the service is for non-clinical services, the contract should include sufficient information to identify the service area or corporate area benefiting. For example, where maintenance is outsourced, the cleaning information should be available by ward/site/service unit.
-
If the data received by your trust is not sufficient to provide electronic patient information, you should work with the contracts team to ensure future contracts do include this information electronically. While waiting for these contract changes to take place, you may use relative weight values to allocate the costs of these services, in conjunction with the service manager responsible for managing the contract fulfilment. We do not expect costing practitioners to have to input manual patient-level information into electronic format, from invoices or other contract documents.
-
Patient care classified as ‘clinical services supplied or received’ needs to be flagged in the relevant information feeds using the clinical services supplied and clinical services received indicators in spreadsheet IR1.2.
-
All activities delivered by your trust on another organisation’s behalf should be costed in the same way as your trust’s own patient activity but reported separately so that the cost and any related patient activity are not included in your trust’s own patient care costs.
-
Work with contract managers and your finance colleagues to understand the service-level agreements for services supplied and received, as this helps you identify the nature of these activities.
-
Where activity undertaken for other organisations is in your activity feeds, you need to understand the different service users of the departments delivering this activity. See Figure CM8.1.
-
The patient-level activity feeds you obtain from the relevant departments need to contain their entire activity, not just their activity for your trust’s own patients.
Approach
Figure CM8.1: Services with different service users
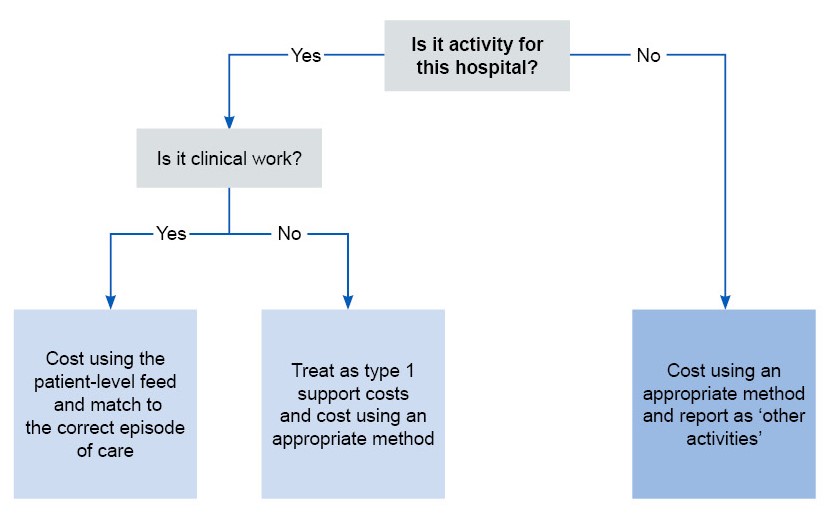
Figure CM8.1 outlines services with different service users with activity for hospital split between clinical and non clinical (type 1 support) costs and activity not for hospital to be reported as ‘other activities’.
CM9: Cancer MDT meetings
Scope
-
This standard applies to all patient-specific cancer MDT meetings hosted by your trust, whether held locally or nationally, at which the treatment of patients is reviewed. These meetings should not be recorded elsewhere, for example in Feed 3a: Non-admitted patient care (NAPC). MDT meetings that are not patient-specific are not to be costed separately.
-
This standard also applies where your trust does not host the MDT but your staff spend material amounts of time attending them.
-
Please note this standard only includes cancer-specific MDT meetings as defined in the integrated collections guidance.
Overview
-
Cancer MDT meetings are reviews by staff of available treatment options and individual responses from the patient. Patients do not attend these meetings.
-
You need to know the types of cancer MDT meetings hosted by your trust, in particular which type of cancer they relate to: for example, breast, colorectal and specialist upper gastrointestinal. You will need to identify the frequency of these meetings and who attends from your trust. See the integrated collections guidance for more information.
-
Cancer MDT meeting costs are not allocated to individual patients but are reported at specialty level. They are kept separate from other costs as they are a significant cost and involve patients from different trusts being discussed by clinical experts.
-
The costing requirement is for an average cost per patient. As a superior costing method, SCM30 Cancer MDT meetings at patient level, you can cost with more detail, including the cost of diagnostic tests if they have been ordered from the meeting.
-
Cancer MDT meetings should be reported under the ‘own patient care’ cost group. Your trust may also supply clinical experts to cancer MDT meetings hosted by another trust. These should be reported under the ‘other activities’ cost group. The trust supplying clinical experts for cancer MDT but that does not host the meetings should refer to the section on provider-to-provider adjustments in the integrated collections guidance. Also see CP5: Reconciliation.
Approach
Information requirements
-
Obtain Feed 14: Cancer MDT meetings from your trust’s MDT meeting information database as prescribed by IR1: Collecting information for costing and spreadsheet IR1.2.
-
The feed contains the number of times each MDT meeting is held during the calendar month or year. It is classified as a standalone feed so prescribed matching rules are not provided in the integrated technical document.
-
These meetings would be costed as patient events. They are not required to be matched to a non-admitted patient care (NAPC) or admitted patient care (APC) feeds.
-
Understand and gather this information and use a local feed to enter the data into the costing system.
-
The meeting duration should be recorded for each staff member present and used to allocate cost to the patient using the activity for cancer MDT meetings.
-
Patient-level information about MDT meetings may be available. Using superior costing method SCM30 you can cost the individual patient discussions and match diagnostics ordered to the specific patient event. See spreadsheet CP3.5 Superior and alternatives for further information. This information, including patient identifier and staff present, may be collected in a separate MDT database or developed from the clinical datasets.
Specialist cost centres and expense codes
-
Cancer MDTs will be run by a specific administrator or may have one administrator for each cancer type.
-
You should use cost centre XXX095 Cancer Multidisciplinary Team Meetings (CMDT) and expense code 5471 Multidisciplinary meeting co-ordinator for the administration costs.
-
The clinical costs of cancer MDTs will come from a range of staffing codes in the general ledger. You will need to disaggregate these costs to show the correct staff involved in the meetings. See column A in ICAL worksheet 27: Cancer MDT meetings for an example of the potential attendees at a cancer MDT meeting whose input may need to be costed.
-
Spreadsheet CP2.1 cost centre XXX095 Cancer Multidisciplinary Team Meetings (CMDT) can be customised to include the relevant staff groups involved in the meetings.
Resources
-
For the administration, you should use the resource ID: SLR091: Cancer MDT meeting co-ordinators. For the other staff types, use the appropriate resource for their clinical work.
Activities
-
Use Activity SLA127: Cancer multidisciplinary meeting.
-
This is the cost of your own staff attending CMDT meetings. It does not matter where this meeting was held or who hosted it. This prevents the cost being included in a costed patient event.
CM10: Pharmacy and medicines
Scope
-
This standard applies to all pharmacy and all medicine costs.
Overview
-
The cost of medicines is separate from the cost of pharmacy services.
-
Medicines are a material cost, second only to staffing for the NHS. For most providers they are a significant cost; they should therefore be costed appropriately, then matched to the correct patient event (prescribed areas) or the cost allocated across patients according to allocation rules.
-
This standard also provides guidance on how to identify the activities that pharmacy staff undertake in your trust and how to apportion their costs to these tasks.
-
If your pharmacy services are provided by an external party, your access to cost and medicine issue data may be limited but information at patient level used to support patient care and for clinical safety should be available. See CM8: Clinical and commercial services.
Approach: Medicines
-
The range of medicines provided by trusts will vary according to the services provided. You should work with your pharmacy lead and pharmacy informatics team to develop an understanding of how the different types of medicine support care, how the data on the medicines dispensed feed shows the items and how this information is used to cost medicines.
Information requirements
-
Medicines information will be provided by your trust’s pharmacy system, an outsourced partner (where the service is not delivered in-house) or via FP10HP prescriptions on ePACT2 (the system used to record FP10s, though we understand not all organisations have this information available for costing). Guidance on Feed 10: Medicines dispensed, is provided in IR1: Collecting information for costing, and spreadsheet IR1.2.
Medicines identifiable at patient level
Acute
-
A mandated monthly dataset collects data on ‘high cost drugs’ for the NHS England NHS Payment Scheme; this list covers about 70% of the highest cost medicines.
-
The medicines on the supplementary information drugs and blood products list should also be included in the patient-level data flows. DrPLCM is a mandatory data flow used to support the commissioning of services from specialised commissioning and includes chemotherapy medicines and supporting medicines for chemotherapy treatments. These medicines are not on the NHS Payment Scheme list but are now prescribed to be matched to the patient event and should show as a component cost.
-
These medicines are the minimum required in Feed 10: Medicines dispensed and should be matched to the patient event where they were prescribed; showing as a component cost at patient level. They can be identified using the ‘high cost drug (OPCS)’ and ‘chemotherapy drug flag’ fields in Feed 10: Medicines dispensed.
Mental health
-
Medicines such as the antipsychotics clozapine, paliperidone, risperidone, aripiprazole and zuclopenthixol decanoate, and methadone and melatonin – are a significant cost in an individual’s care. Information on these medicines and other controlled medicines are likely to be available at patient level and so these drugs are the minimum required in Feed 10: Medicines dispensed, for mental health services.
-
Use of Electronic Prescribing and Medicines Administration (EPMA) systems (sometimes called e-Prescribing systems) in costing medicines not normally dispensed at patient level, is a superior costing method SCM78: Inclusion of all medicines in costing at patient level, using EPMA system. This would not include the drugs on the High Cost Drugs list, as they are already prescribed to be allocated at patient level. See spreadsheet CP3.5 Superior and alternatives for more detail.
Medicines not identifiable at patient level – stock items
-
Feed 10: Medicines dispensed will also contain values for the medicines issued in bulk to wards and service units without a patient level prescription. This information is used to provide proportional calculations for the costing allocation process, across all the patients in that ward/service unit.
-
You should understand how these data items show on Feed 10, to ensure the correct costing treatment.
Negative costs in the medicines dispensed feed
-
Feed 10: Medicines dispensed may contain negative values due to products being returned to the pharmacy department: for example, it may contain the dispensing, supply and returns for a patient’s medicine within the same – or different – periods.
-
These issues and returns are not always netted off within the department’s pharmacy stock management system against the same patient. If this is the case, you need to review the medicines feed and net off the quantities and costs to ensure only what is used is costed.
-
All negative costs need to be removed, as calculations cannot be based on a negative value. The values of the returns are not a reconciliation item.
-
For reporting purposes, ensure that Feed 10: Medicines dispensed feed, includes the generic name of the medicine, not the brand name. This is for ease of reporting and discussion with users of PLICS information.
-
As part of the ‘Global Standard 1’ (GS1) project for the NHS, the expectation is that NHS trusts should have implemented the GS1 identifier (barcode) on all drugs from February 2019. This will provide more consistent information on the type and cost of items, which may improve the ability to link key items at patient level and using consistent terminology.
Specialist cost centres and expense codes
-
Use cost centre XXX038 Pharmacy to identify the pharmacy costs in the cost ledger. You can customise the cost ledger by repeating this cost centre to separate costs that need disaggregating to different sections of the pharmacy service.
-
Where medicines are delivered to patient’s home, use cost centre XXX041 Home delivery of medicines. This will include contracted services.
-
For chemotherapy home delivery use cost centre XXX042 Home Delivery of Chemotherapy Medicines. See CM25: Chemotherapy.
-
You should refer to spreadsheet CP2.1 standardised cost ledger for the expense codes for pharmacy staffing and medicines.
-
Feed 10: Medicines dispensed contains the actual cost of the medicine. These costs are used as relative weight values to allocate the costs as proportions in the cost ledger. This is so that if the total cost to the pharmacy department is £1,000 but only £900 is in the cost ledger, a negative cost is not incurred by allocating more cost using Feed 10: Medicines dispensed, than is on the cost ledger code.
Resources
-
You should refer to spreadsheet CP3.1 resource list for medicine resources.
-
You may create additional local costing resource codes to identify significant cost medicines within your costing system, ensuring they flow to the correct collection resource shown in spreadsheet CP2.1.
Activities
-
You should refer to spreadsheet CP3.2 activity list to identify the activities for medicines.
-
Where medicines are dispensed from the pharmacy in bulk rather than to specific patients – they may be called ‘ward medicines’ or ‘stock’ items. Use Activity MDA065: Dispense non patient-identifiable medicines.
-
Use the ‘Requesting location code’ data item to allocate these medicines to the ward, department, or service requesting them. Then allocate the cost to the patient events in those areas based on the allocation method shown in spreadsheet CP3.3.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to match costed medicines to the correct patient event.
-
Admitted patients often move between wards, and sometimes move between hospital sites or to ‘virtual wards’ at home. Where medicines are matched at patient level, for local reporting you should be aware the request location may not be the same as the ‘dispensed to’ location.
Homecare medicines
-
Homecare medicines issued by the trust pharmacy department will have a patient identifiable record for medicines issued directly to patients in their own homes – for safety and commissioning purposes. The patient will use the medicines over an agreed time that does not relate specifically to one patient event.
-
These medicines will be identified first in the matching process before the other matching rules for Feed 10: Medicines dispensed, using the ‘homecare flag’ so they are not incorrectly matched to patient events and are identifiable as homecare (that is, not badged as ‘unmatched’).
-
As a superior costing method SCM54: Homecare medicines or equipment (see spreadsheet CM3.5: Superior and alternatives) trusts can create a proxy record for homecare patients and the medicines match the medicines to that proxy record.
Other considerations
Treatment of FP10 costs
-
FP10 is the form used to reclaim the cost of medicines prescribed in hospital and dispensed on behalf of the NHS by community pharmacies. This prescription cost information is a useful part of the patient pathway as it shows how the medication regimen continues outside the clinical setting.
-
Where community pharmacies or the NHS Business Services Authority – NHS Prescription Services charge your provider for these medicines, you will have the costs for them in the general ledger.
-
Use resource ID: MDR063: FP10 Medicines and Activity MDA066: Dispensing non patient identifiable medicines.
-
FP10 costs are not linked to your trust’s pharmacy department, therefore they should be kept separate from other medicine costs, identified as part of the ‘other activities’ cost group. The value should be included in the matching reconciliation, not matched to patients, to ensure the cost is not spread over patients who did not receive these medicines.
-
As a superior costing method SCM79: FP10 costs at patient level, you can obtain a dataset to understand which patient prescription each cost relates to, so it can be matched to the relevant patient contact. The information can be added to Feed 10: Medicines dispensed, as shown in spreadsheet IR1.2 and matched to the patient event recorded in the feed, as described in CP4: Matching costed activities to patients. Any unmatched activity should be reported in the matching reconciliation and not allocated to other patients.
-
For the superior costing method, use Resource MDR063: FP10 Medicines and Activity MDA068: Dispensing patient level medicine scripts.
-
If your trust is in an area where community or private pharmacies that dispense medicines charge the integrated care board (ICB) directly for FP10s, the cost will not be in your trust’s accounts and there is no requirement to gather information on it.
Medicines provided by other organisations
-
Where your trust purchases its medicines – including homecare medicines – and/or pharmacy services from a different NHS provider or other external party, your trust should receive electronic information as part of the contract of services, for patient safety and invoice validation.
-
Where these medicines are in the high cost or chemotherapy groups prescribed above for costing at patient level, you should request sufficient electronic information to support Feed 10: Medicines dispensed, so the costs can be allocated to the patient event in the same way as an internal pharmacy service. This will include:
- patient-level information on medicine cost
- information on non patient-identifiable medicines which have been delivered to a trackable location from where they are issued to the required units.
-
You may need to work with your provider-to-provider contracts team to obtain sufficient and appropriate electronic information. However, if this information is not available electronically at patient level, you should allocate the costs as non patient-identifiable medicines to the relevant service area. We do not require manual entry of data from invoices into spreadsheets for a patient-level medicines feed.
Clinical trials – medicines
-
Where the medicines are part of a clinical trial, the cost may not be in the trust accounts. Where the NHS provider is supplying the staffing and facilities, the patient event should still be costed, even though there is no value available to show as a component cost of the medicines.
-
Clinical trial patients should be identified within the trust clinical information systems. For reporting purposes, this identification is helpful for users to explain the lack of medicine costs.
Technology changes in medicines
-
Some medicine costs may be significant but not yet identified at patient level in Feed 10: Medicines dispensed. Costs for such drugs may skew the cost of some patient groups. This may include:
- newly released medicines
- medicines in clinical trials within the trust general ledger.
-
Work with the pharmacy service team to understand such medicine costs and identify where they sit in the general ledger. If necessary, move material values to an appropriate place to ensure the cost sits in the correct resource and can be identified with the correct patient or clinical service.
Red book drugs
-
Some trusts have found drugs prescribed to a patient who has been discharged. This leaves the drugs unmatched with no follow-on patient events to attach the cost to.
-
These are drugs that can only be prescribed by the secondary care trust but as there is no patient event record there is nothing to match to. These drug costs should still flow as part of your National Cost Collection submission even though they are not able to be matched.
Approach: Pharmacy services
Information requirements
-
Pharmacy staff carry out significantly more activities than dispensing medicines. Pharmacy pay costs will therefore be associated with a range of services which should be understood for the most effective costed patient activity.
-
Pharmacy services have a national ‘infrastructure, governance and clinical model’. The elements are:
- patient-facing clinical services: includes prescribing, supporting patient self-care and medicine reviews
- infrastructure: includes managing supply of medicines, outsourced pharmacy service contracts, formulary development and medicines information
- governance: includes policies and procedures development, safe management of medicines, audit of clinical practice and recording information.
-
The infrastructure and governance elements (including providing the legal presence to permit medicine supply to patients, provider-wide strategy, governance and education services) should be costed separately from the clinical element of the service provided. This is to provide meaningful local information for clinical service review.
-
The cost centre will be the same as for medicines above, including XXX038 Pharmacy, and the expense codes will cover the relevant pay and non-pay items.
Resources
-
The staffing and non-pay will use the resources shown in spreadsheet CP2.1 on the Pharmacy cost centre.
-
You will need to identify which staff grades perform different tasks to identify the percentage of pharmacy staff time spent in each area. You will need to disaggregate the pharmacy cost centre to separate dispensing costs from the infrastructure and governance costs.
Activities
Clinical services
-
Clinical services include dispensing medicines, aseptic suite, and direct patient support in clinical units. These services should be allocated to patients that received the service.
-
Wards or services receiving a specific pharmacy service, with input determined by specialty, clinical need and patient turnover should have the staff/non-pay resource allocated to the appropriate ward or service area. Use Activity MDA066: Pharmacy work.
-
You should speak to your chief pharmacist to identify how many and which band of pharmacy staff work with dedicated services, and then set up relative weight values to ensure their costs are allocated only to patients using those services/wards.
-
Further things to consider when developing relative weight values for allocating clinical service pharmacy staffing costs are:
- Should there be a relative weight value division of inpatients to outpatients/community services?
- Do intensive care units require a higher percentage of pharmacy staffing costs, or is the support at a higher banding?
Aseptic unit
-
An aseptic unit is a clinical production unit for the aseptic preparation of injectables, such as chemotherapy, biological preparations/formulations and total parenteral nutrition.
-
The aseptic unit is staffed mainly by specially trained pharmacy technicians. There will also be significant costs for non-pay items, cleaning and equipment costs.
-
This is a separate pharmacy activity and should be costed separately, so the cost is allocated to the patients that use aseptic prepared items. Use Activity MDA074: Aseptic unit work.
-
Costs in an aseptic unit typically include:
- staffing (pharmacist, pharmacy technicians and assistants)
- hire/depreciation/maintenance costs of the unit
- registration and inspection to ensure the unit is fit for purpose
- quality assurance
- consumables and cleaning of the unit.
Infrastructure and governance
-
Work on infrastructure and governance should be identified and allocated to all patient events as the work is not specific to type of patient. Use the Activity MDA066: Pharmacy work.
CM13: Admitted patient care
Scope
-
This standard applies to patients receiving care in a hospital bed and individuals/patients in a hospice, long stay or care home provided by the NHS, and in virtual wards. Traditionally, some services did not use the terms ‘episode’ or ‘spell’ for inpatient stays but as they are now used in the clinical datasets, they are used throughout the Approved Costing Guidance standards.
-
This standard excludes patients in a critical care unit: defined as a patient with a record on the relevant age-related critical care minimum data set. For critical care units, refer to CM6: Critical Care.
Overview
-
Inpatient departments provide a clinical setting for patients who need to be in a hospital bed as their condition requires it. Care homes provide accommodation and personal care for individuals to meet their ongoing care needs.
-
Costs are incurred each day the patient is on the ward (or in a virtual ward). The costing process should apply costs to the patient record showing the date(s) the costs were incurred, so a timeline of costs can be viewed by bed day. This applies to acute, community and mental health services.
-
The costed patient event containing the bed days is the episode for all care sectors, whether short term, long term or residential. One care professional is clinically named responsible for the episode, even if they work as part of a team.
-
Most episodes will be completed during the costing period but some will be unfinished patient events. These should still be costed: see CM2: Incomplete patient events.
-
For costing, acute and community episodes will be classified with an Episode grouping code (see the integrated extract specification). These are costing-specific high-level currency types that group admissions. Mental health spells do not require an episode grouping.
-
Episode grouping has been developed with community providers to show the nature of the care without reliance on clinical coding.
-
Episode grouping is for all acute episodes as well as community episodes, ensuring that the National Cost Collection (NCC) does not need a separate, additional feed for community inpatients.
-
Where care is currently submitted to the NCC using HRG codes, this should continue. Acute providers will apply either episode grouping 01 Episode with costing grouper HRG (all but undefined groups) or episode grouping 09 Other episode with undefined group HRG and continue to use HRG (in the finished consultant episode HRG field). See the integrated collections guidance and IR1: Collecting information for costing for more detail.
-
Episode groupings should be based on local information, such as ward code, or using information agreed with the clinical teams.
-
The currency used to group types of care depends on the care given:
- For acute services and community hospitals performing acute-type services or procedure-based interventions (such as endoscopy), the currency is HRG code.
- For non-procedure based community admissions, the currency HRG UZ01Z is acceptable. These episodes will be identified by the episode groupings and are costing-specific currencies developed with community providers to show the nature of the care without reliance on clinical coding.
- For mental health, the currency is under development and can be found in the integrated extract specification.
- Services not in scope of PLICS for the NCC do not require an episode grouping code.
-
Wards have a range of clinical differences, depending on the level of care given. For example:
- Surgical wards provide pre-operation and post-operation care.
- Mental health wards provide a safe and therapeutic environment for patients with a range of conditions.
- Community wards will usually have patients requiring less intensity of care than acute wards, so staffing ratios and resources will be lower.
- Virtual wards are a way of recording the data for patients who are treated as admitted patient care (APC) in their homes, with clinical staff and technological input. These ward stays are usually step-down care from a hospital ward.
-
Some wards will be secured to ensure the safety of the individual and others – for example, for patients with dementia or forensic wards in mental health.
-
Wards will operate in different ways according to the needs of the patients.
- Acute hospital wards will have many clinical interventions during the patient’s episode, including pre- and post-operative care, diagnostics and treatments.
- Mental health and community/long stay wards have programmes of activities – including one-to-one medical consultation and single or group therapies such as art, cookery, exercise classes or physiotherapy and talking therapies.
- Longer-term mental health patients and individuals with learning disabilities may contribute to the ‘work’ of the ward or their place of residence, by serving meals, doing laundry or other such activities.
-
In some cases, the activities will be provided by staff from another organisation; for example, a specialist practitioner from another organisation, physical health professionals on a mental health ward, or GPs who provide community ward medical cover. Where this care is recharged to the organisation, this cost should be mapped to the patients who received the care. See CM8: Clinical and commercial services supplied or received.
Approach
Information requirements
-
The data for APC activity will come from the relevant data set as described in IR1: Collecting information for costing and spreadsheet IR1.2.
- Providers of acute hospital services admitted patient care are required to use Feed 1a: APC data, including healthcare resource groups (HRGs).
- Providers of mental health services admitted patient care are required to use Feed 1b: MH APC, including clusters.
- Providers of community hospital admitted patient care are required to use Feed 1a: APC data, and either:
- group each patient episode to HRGs where clinical coding is required to report clinical procedures (for example – endoscopy and other special procedure suites) in Feed 1a (acute APC) or
- identify community admissions with the appropriate episode groupings (see CM13: Admitted patient care and the integrated extract specification). These do not require HRGs: the mapping to these groupings should be locally defined. A record of the mappings should be referenced in the integrated costing assurance log (ICAL).
-
Where there is no national dataset – for example, in residential care run by the NHS, the data should be available from local systems. This should be brought into the costing system using Feed 1a and used for the costing process.
-
The costs allocated to ward care activity are driven by the length of stay in minutes, so the costing system needs information on the date and time on each ward, including virtual wards.
-
For acute and community services, Feed 4: Ward stay will give additional information on the time spent on a ward. This feed is required as the Commissioning Data Set (the base data for Feed 1a: APC) does not show the date and time on each ward.
-
For mental health services, Feed 1b: MH APC, is based on the mental health services data set (MHSDS), which includes ward stays, so this information can be obtained from the APC feed, and Feed 4: Ward stay, may not be required.
-
Spreadsheet IR1.2 shows the patient-level field requirements for calculating the length of stay by ward.
-
Wards may differ in their costs, so to appropriately cost an individual patient’s ‘journey’, you need to know which ward(s) the patient was on. The data field ‘ward code’ will supply information to the costing system for linking cost to patients on a physical or virtual ward.
-
Costing practitioners should understand the hierarchy of data items in the Commissioning Data Set (CDS) shown in examples below so the cost can be applied to the correct patient event as it occurs – using date and time to show the day the event happened.
-
These data items are:
- a spell (admission to discharge) (one or more episodes)
- at least one episode (an episode is a period of time during a spell under a single healthcare professional or team; an episode may have one or more wards)
- at least one ward: the longer the spell, the more likely there will be multiple wards recorded.
-
For example:
- In one spell Patient A was admitted to ward A for surgery, moved to ward B for post operation care, then transferred to a different responsible care professional for rehabilitation and moved to ward C, from where they were discharged.
- In one spell Patient B was admitted to ward B and moved to ward C from where they were discharged.
-
You should be aware that taking dates and times from different datasets may show different durations or the dates and times may not match. You should regularly review the accuracy of the data and use the ward information from the source with the best data quality.
-
For example, use the start date (ward stay) and start time (ward stay) as the indicator that the patient was on that ward, rather than trying to match the end date and time of one ward with the start date and time of the next ward.
Ward care ‘acuity’
-
‘Acuity’, as defined for costing, describes the level of resource a patient uses due to their condition; including physical and mental health, behavioural and forensic issues.
-
The standard level of acuity is understood from the type of ward – for example, those with a higher staffing ratio will accommodate patients with higher acuity.
-
Unless otherwise informed, you can expect all patients on the same ward to use resources at a similar rate.
-
For mental health, information on the level of resource expected for patients on a ward may be understood from the MHSDS fields which recognise the additional levels of acuity that can be expected from different types of ward – although you should discuss this premise with the service team.
-
For example, in the APC feed:
- Field name Ward code has description: A unique identification of a ward in a healthcare provider.
- Field name Ward setting type (MH only) has description: The type of ward setting for a mental health service’s patient during a hospital provider spell
- Field name Ward security level (MH only): The level of security for a ward.
-
You can use a superior costing method to allocate the costs of additional care provided to different patients on a ward, by using nursing acuity or ratios (SCM8 Inpatient nursing acuity), specialing/observations (SCM2 Specialing and observations) and by identifying mental health escorted home leave (SCM6 Escorted home leave). This information should relate to specific patients and can come from clinical notes or other reliable sources.
-
The CDS and MHSDS do not contain acuity information. To apply these superior cost methods for acuity, you will need to obtain this information from a local information source and use the ‘acuity level’ field in feeds 1a and 1b: APC, as shown in spreadsheet IR1.2.
Supporting contacts
-
An additional data source can be included on Feed 7: Supporting contacts, to reflect the time and grade of staff providing resources to specific patients over and above the basic ward care. See the FutureNHS Supporting contents: briefing paper.
Specialist cost centres and expense codes
-
Many types of staff can work on a ward, and their costs show in the ward cost centres in your general ledger.
-
Spreadsheet CP2.1: The standardised cost ledger shows the standardised cost centre codes for wards.
-
The cost centres should be customised for each ward using the XXX to indicate your local ward identifier. The ward costs can then be mapped to the correct patients. You may group similar wards together.
-
Ward stay data may include patients on a virtual ward: the patient is not in a hospital bed but is attended by clinical staff. The ward code should be used to identify these patients and match them with the cost of providing this care in the same way as for other wards.
-
Where the care is provided by a third party, the cost may be in the form of invoices.
-
A range of staff may work on wards, including nurses and specialist nurses, non-consultant medical staff, psychiatrists, psychologists, therapists, pharmacists, support workers and activity co-ordinators. The expense codes used should reflect the staff group and non-pay items used.
-
Staff costs are not on the ward cost centre, you should ensure their costs are identified and allocated to the area of the patients they care for. This can be done by disaggregating the cost centre where their costs are held. For example, non-consultant medical staff in a community hospital might work across three wards, so their costs should be allocated across those wards. See CM1: Medical staffing for more detail.
Resources
-
The patient will incur costs from the care given by a range of staff, the use of consumables (including medicines), and ward overheads (previously known as Type 1 Support Costs), such as ward clerk costs.
-
Use the resources for staff type and non-pay as shown in spreadsheet CP2.1: The standardised cost ledger.
Activities
Ward care
-
Admitted patients incur costs just by being on a ward. Therefore, all APC patient events should show an activity ID for ward care among the list of activities the patient uses.
-
The accommodation and care costs are allocated to the ward care activity, using the length of stay in minutes. The datasets supplying the costing system with information include date and time as required fields.
-
Use Activity SLA097: Ward care for all physical wards, unless you require greater detail for your costing system to link to the costs, for additional levels of local reporting, or if you are using a superior allocation method.
-
Use Activity SLA169: Virtual wards for admitted patients cared for at home.
-
For mental health units spreadsheet CP3.2 shows the superior costing method of ward care activities for mental health inpatient units. The activities are separately identified by the level of care, security, and service, to facilitate meaningful local reporting.
Ward rounds
Mental health care programme approach (CPA) meetings
Group sessions
-
See CM14: Group sessions.
Resource activity combinations
-
See spreadsheet CP3.3 for possible combinations of resources and activities in wards.
Matching
Non-pay items
-
For the treatment of costs for other ward consumable items and equipment, refer to CM21: Clinical non-pay items.
-
For more detail, refer to CM10: Pharmacy and medicines.
Other considerations
Ward attenders
Home leave
-
‘Home leave’ is when a patient who is admitted onto a ward, leaves for a period at home, and the hospital bed remains empty for their possible return.
-
MH patients may be escorted or unescorted during home leave; acute and community patients may also have home leave but this will mostly be unescorted.
-
MH home leave is recorded in the MHSDS data set using the fields in spreadsheet IR1.2 and is authorised for an agreed number of days. Home leave is not a discharge. The duration of the admission should not include the bed days on home leave. The patient episode continues, keeping a bed for their use.
-
Acute and community providers should use their PAS data to identify the unescorted home leave period and exclude it from the length of stay used for calculations of cost.
-
Occasionally, a patient has escorted leave, where they are under a staff member’s supervision 24/7, to ensure they do not put either their own safety or that of others, at risk, and to assess them further before discharge. The number of healthcare professionals who attend the patient on escorted leave depends on the patient’s needs. As a superior costing method, you can obtain information on the resources used during escorted leave and bring them into the costing process in Feed 7: Supporting contacts. When costing escorted home leave, use Activity MHA288: Escort during home leave.
-
Unescorted home leave does not incur cost for food, fresh linen, on-ward staffing input, ward rounds or ward work with healthcare professionals. It therefore does not require additional information or consideration of acuity.
-
There may be some costs for the facilities kept available on the ward for the patient on home leave that are not used by other patients: for example, heating their bedroom.
- We are not prescribing allocating costs to the patient for ward care, ward rounds and ward work during home leave, as doing so is beyond the level of costing required. The net length of stay on the ward is the primary cost driver for ward care and ward work after the home leave period has been subtracted.
- The exception to this is where there is a full roster of staff on the ward and agency staff have been booked to cover the escorted home leave.
Perinatal mental health services
-
Some women need to be admitted to a MH unit during pregnancy or following the birth of their child. This may be to a specific mother and baby unit, the discrete costs for which should be attributable to the correct cohort of patients.
-
Where there is no specific unit and women are admitted to other wards, ensure that the appropriate relative weight values for duration and number of observations are used. This care will need to be discussed with the service as there is no mandated field in the MHSDS for it.
-
The costed activity is for the mental health care provided to the mother only, although there may be additional nursery costs on discrete units. Ensure the nursery costs are allocated across the patients (mothers) using the unit in the period unless patient-level information is available.
CM14: Group sessions
Scope
-
This standard applies to all group sessions with two or more patients attending.
-
Group sessions can take place during a non-admitted patient care (NAPC) contact or an admitted patient care (APC) episode.
Overview
-
Group sessions are often delivered in a group-specific location, for example physiotherapy in a gymnasium.
-
A group session involves multiple patients and one or more staff members. A group contact is the activity unit recorded for a single patient within a group session.
Approach
-
Group sessions take place in all sectors. Sometime having a group discussion is the objective – as with group therapy or social enrichment sessions, and for other services, groups are a cost-effective way of providing care – as with education sessions and self-care guidance for a physical health condition.
Information requirements
-
IR1: Collecting information for costing and spreadsheet IR1.2 specify the minimum information required to cost group contacts; that is, a patient event as part of a group session.
-
Each patient contact in Feed 3b: NAPC – mental health, and Feed 3c: NAPC – community, relating to a group session should have a unique identifier in the field ‘group session identifier’ as this information comes from the Mental Health Services Data Set (MHSDS) and Community Services Data Set (CSDS) respectively. Where this field is not null, it is a group session. The ‘number of group session participants’ is available as a field to enable cost to be divided between them.
-
Feed 3b: NAPC – mental health and Feed 3c: NAPC – community should include a record of the duration of the group session against each participant, in the field ‘clinical contact duration of group session’.
-
The acute patient Commissioning Data Set (CDS) does not have a field identifying a group contact, so the ‘group session identifier’ field and the ‘number of group session participants’ field in Feed 3a: NAPC will need to be populated from local information. Local information will be needed for groups held during an APC episode (if material).
-
For acute groups, you should use Feed 3a: NAPC field ‘appointment duration’. Assume all patients spend the same amount of time in the group session (although this can vary). The recorded duration will be for the whole contact, so it should be used to allocate the cost of providing the session against all the participants.
-
To identify the service/team providing the group, you will need local information:
- for some services this may be a clinic code
- another indicator may be specialty or treatment function code
- for community services, the service/team providing the group may be identified from the field ‘service or team type referred to (community care)’.
-
If the group session fields are not routinely completed, work with your informatics department to ensure these are recorded. Without this information, the contact will be costed as though it were a single professional appointment (receiving a higher weighting of resource than was used by the patient).
-
Where a patient attends (NAPC) with family support and both are recorded as separate patient events, these should be treated as a group session.
-
There is no national dataset to record groups for admitted patients, so you will need a local data source. As a superior costing method SCM33 Supporting contacts allocated at patient level, this information should be entered onto Feed 7: Supporting contacts in accordance with IR1: Collecting information for costing and spreadsheet IR1.2, to ensure a record of the cost of the group contact is included as part of the episode cost for patients benefiting from the service – see CP2: Clearly identifying costs.
Specialist cost centres and expense codes
-
There is no specific cost centre in the standardised cost ledger (spreadsheet CP2.1) for group sessions. Use the cost centres for NAPC or APC where group sessions take place, or for the team that run the session.
-
For group sessions where activity data is not available at all, use cost centre ‘XXX584: Group Session without PAS contact’ to map your group session costs to. This would apply where clinical professionals run group sessions with no record of the individuals attending – such as school nurses running a health session in a school assembly.
Resources
Staff numbers running group sessions
-
The sources of the NAPC information feeds (CSDS, MHSDS and CDS) record only one care professional for the group, using the fields ‘care professional local identifier’ (CSDS and MHSDS) and ‘healthcare professional code’ (CDS). You should ensure the cost of the identified care professional is included in the group cost. This person is the named contact for the group session to discuss the costing process with. They will know whether additional information is required and available about the service team make-up.
-
If no further information is available or the cost of additional staff is not material, for costing purposes you can assume the group is staffed by this one care professional only.
-
Group sessions with multiple care professionals will have a different cost per patient from group sessions with a single care professional. Depending on the number and type of staff involved, the cost could be higher or lower. You need to identify the appropriate resources for each patient contact, to ensure costs are not attributed to the wrong patient event (or spread across other events).
-
Where the cost of additional staff within the group is material, the activity feed can include additional staff from a local source. The field to use is ‘second care professional local identifier’. This information will then inform relative weight values to identify the resources involved.
-
You may add further fields for subsequent care professionals if needed, in conjunction with your costing software provider.
-
Work with the relevant team/service/department and your informatics department to find a suitable method of recording each staff member’s involvement in the group activities.
Allocating non-pay costs to group sessions
-
Many group sessions will not involve equipment, medicines or patient consumables, or their item use will be negligible. However, for some activities, such as specialist sporting sessions (including trips out), identifying the costs, including travel and other non-pay costs, in a more detailed manner may be beneficial and they should be allocated to patients who benefited from the group.
-
The materiality principle should be used when developing detailed models for attributing this cost. Use the methods prescribed for consumable items in CM21: Clinical non-pay items.
Activities
-
For group sessions similar in length/nature to an outpatient appointment or community care contact, where the patients are known and have a patient administration system (PAS) record for the group – use Activity CMA308: Group contact recorded at patient level.
-
Where there is no patient recorded use Activity CMA344: Group contact without a patient-level record.
Day care
-
Day care is where a group of non-admitted patients benefit from care services in a group setting – usually over a few hours. Use Activity MHA262: Day care as this will allow better reporting of the service that runs for a longer time. A range of care professionals may provide care over the period of attendance.
-
The activity may be recorded as NAPC or it may be on a standalone local system.
-
The staff involved are most likely to be nurses/therapists but in some areas, there could be medical input. The model of care may be termed ‘social’ or ‘medical’ depending on its clinical content. You should include all relevant staff costs for the session.
-
Day care should be costed as for other group sessions, using the duration of the session divided by the number of patients present.
Groups run during admitted patient care
-
Many patients receive group therapy during admissions, for example physiotherapists running a group on a ward to maintain patient mobility.
-
Where the cost of running the group is within a service area’s budget (for example the cost of the physiotherapist is on the ward budget) and all patients on that ward have the opportunity to participate in the group, there is no requirement to separately cost a group contact. The cost will be included in the Activity SLA097: Ward care.
-
Where the cost is not in the service area, you should include it in the costing of the area that runs the group, using the Activity CMA308: Group contact recorded at patient level. This will be shown as a component of the admission cost.
-
Where not all patients on the ward receive the group service, you should apply the cost to the patients who do attend the group. You should consider the materiality of this cost differential and prioritise it accordingly.
Resource activity combinations
-
Group contacts should include the cost of the resources provided to the group, spread across the number of patients in the group as shown in Figure CM14.1.
Figure CM14.1: How multiple or single staff members are attributed to resources, activities and patients
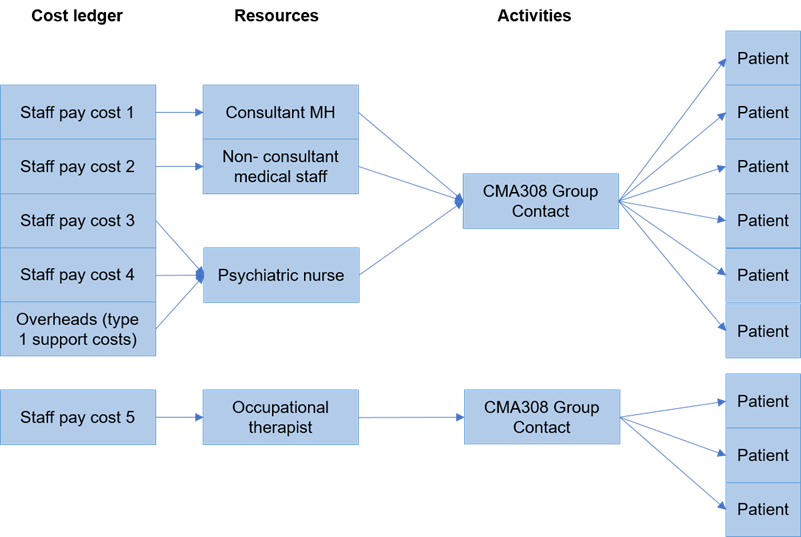
Figure CM14.1 outlines how staff pay costs and type 1 support costs are attributed to resources/roles such as consultant/psychiatric nurse/occupational therapist via activities to patients.
-
This method relies on several assumptions:
- each staff member spends the same amount of time with each patient
- patients do not leave the session early
- staff members do not leave the session early.
-
We acknowledge these assumptions do not always hold true and the method will therefore not provide a completely accurate representation of how care is delivered. As the ability to collect information improves, future versions of the standards will specify more accurate methods based on, for example, patient acuity or measuring actual time spent with specific patients.
-
If you already apply additional relative weight values to specific patients or adjust for staff presence in the relative weight values, continue to do so as this provides better information for costing. Please let us know by contacting costing@england.nhs.uk.
Matching
-
Where a group session is recorded at patient level, this can be used for allocation at a patient level and therefore there is no need for matching.
CM16: Sexual health services
Scope
-
This standard applies to all activity provided by sexual health services.
Overview
-
Sexual health services offer a range of services to those who have, may have or are at risk of sexually transmitted infections, including:
- diagnosis and treatment
- education
- family planning services
- support for sexual assault victims
- provision of surgical and medical terminations of pregnancy
- psychosexual medicine.
-
Patients can be treated in both admitted patient care (APC) and non-admitted patient care (NAPC) settings, although most of the service is in NAPC.
-
Some elements of this care will be under the formal medical specialty of genitourinary medicine (GUM).
-
Due to information governance constraints on legally restricted sensitive data (LRSD), patient information for some sexual health services will be anonymised within your trust. Therefore, we are aiming to cost a patient not the patient, accessing sexual health services. This should not mean no record of the patient’s care – such a record is important for patient safety. But the record may not be available for costing in the same way as for other NHS patients.
-
You should note that LRSD patient events are not collected at patient level in the National Cost Collection (NCC). For more information see the integrated collections guidance.
Approach
Information requirements
-
You should follow the same information requirements process for APC and NAPC contacts whether you are using patient-identifiable information or anonymised/proxy records.
-
Sexual health services may record formal medical NAPC contacts (GUM) in the outpatient Commissioning Data Set (CDS) or hold records locally in a separate data system. APC care will be in the CDS. Sexual health is not in scope of the Community Services Data Set (CSDS).
-
You will need to speak to your informatics team to determine the source of the information for sexual health. You may use Feed 17: Sexual Health or Feed 3a: NAPC to ensure the data for costing is complete and reconciles to the relevant national dataset. See IR1: Collecting information for costing and spreadsheet IR1.2.
-
Feed 17: Sexual Health includes the data item for the HIV and AIDS reporting system (HARS) required for the NCC. If you use Feed 3a for input of sexual health data, you will need to add a local data item for the HARS band.
-
If no patient-level activity is available you can create proxy records. See IR1: Collecting information for costing.
-
Patients admitted overnight or as day cases primarily for sexual health will usually be recorded under Specialty 360: Genitourinary medicine (GUM) on Feed 1a: APC. The procedures performed will be clinically coded and should be costed in the same way as for other admitted patients.
-
If a patient admitted under a specialty other than GUM receives a bedside consultation with a sexual health professional, the contact can be recorded on Feed 7: Supporting contacts and be separately identifiable as part of the patient episode.
-
Sexual health or GUM services may use theatres. See CM5: Theatres and special procedure suites and CM21: Clinical non-pay items.
Specialist cost centres and expense codes
-
The cost of sexual health services should be shown in cost centre XXX613; Sexual health/GUM care. If there are multiple services in the sexual health costs in your general ledger, you may customise the XXX in your cost ledger to ensure the cost flows to the appropriate resource for allocation. See also CP2: Clearly identifying costs.
-
There are no specific expense codes for this service. However, if the sexual health testing is purchased from another organisation, you should use expense code 7020 Contract: pathology testing – non patient specific data. If you receive this information at patient level, please use 7261 Laboratory External Tests.
Resources
-
You should map to resources as shown in spreadsheet CP2.1.
-
To note: for contracted out services you will map to:
- CLR026: Services received – pathology testing – non patient specific
- CLR031: Services received – pathology testing – patient specific.
Activities
-
Where the patient receives a consultation in non-consultant led services for sexual health only, use Activity CMA312 Sexual health/GUM care.
-
Where the patient(s) receive integrated sexual health and family planning, use Activity CMA334 Integrated sexual health and family planning care.
-
Medical staff resources for standard GUM consultations should be mapped to the Activity SLA135: Outpatient care.
-
Where a procedure is performed, use Activity SLA136: Outpatient procedure and treatment room care.
-
These activities will include the cost of taking bloods or swabs for testing and sending them to the laboratory but not the cost of the test processing in the laboratory. This is costed to the separate activity CMA306 Sexual Health Testing and then matched to the patient contact in accordance with CP4: Matching costed activities to patients.
Sexual health tests
-
A sexual health test is the pathological test or group of tests to determine type of condition or cause. This is the activity of receiving the blood test or swab sample at the relevant laboratory and processing it, and the cost of consumables, staff/machine processing time and the test. In this way, local laboratory costs can be identified separately from those of contacts and may be compared to those of an outsourced laboratory. The cost of outsourced tests will include consumable and other variable costs as well as support costs.
-
Not all patients will undergo a test during their contact. Therefore, the cost of the test should show up as a separate activity from staff time with the patient doing the swab or taking the blood.
-
The cost of taking the blood/swab sample is usually associated with the consultation with the sexual health professional, and therefore should be included as part of the activity for sexual health/GUM care, outpatient care or outpatient procedure.
-
If the test is carried out separately from the sexual health consultation – for example, in a separate laboratory clinic room by a different type of health professional such as a phlebotomist – this should be recorded as a separate activity CLA028 and matched to the sexual health patient event.
-
If your sexual health test information comes from a pathology service dataset (including outsourced) other than the main pathology lab, add its data to the Feed 8: pathology.
-
Sexual health tests may be performed by a different provider from the one where the contact took place. The information should be available to your trust at patient level, in accordance with CM8: Clinical and commercial services supplied or received. You should use Activity CMA306: Sexual health testing for outsourced laboratory tests.
Matching
-
Use the prescribed matching rules in the integrated technical document in spreadsheet CP4.1 to ensure the costed diagnostic tests, medicines and implants are matched to the correct patient event, as in CP4: Matching costed activities to patients.
CM17: Dental services
Scope
-
This standard applies to all activities provided by NHS dental services, including community and hospital dentistry, emergency and planned dental care, orthodontics and where oral surgery and maxillofacial services include dental practitioners.
-
This standard does not apply to dental emergencies treated in 24 hour emergency departments. These are included in CM4: Emergency care attendances.
Overview
-
Dental services are provided across various settings including:
- planned outpatient clinics in a hospital, health centre or prison
- non-admitted patient care (NAPC) in a domiciliary setting
- community NAPC appointments in a high street setting
- emergency dental departments: excluding dental emergencies treated in type 1 EC departments which will be recorded on the Emergency Care Data Set (ECDS) as part of ED services
- patients admitted to a ward under dentistry or another specialty for dental care.
Approach
Information requirements
-
Activity for dental patients will be recorded in provider systems in various ways:
- in the main patient administration system (PAS) as admission episodes (included in the admitted patient care (APC) feed)
- in the main PAS as outpatient attendances (included in NAPC, feeds 3a or 3c)
- in a separate local system for community dental activity.
-
The data required for Feed 18: Dentistry, as shown in spreadsheet IR1.2, is the community dental activity. It should only include dental activity not covered by the APC or NAPC feeds.
-
Where the patient has been admitted, the patient event for costing is the episode.
-
For non-admitted patients seen in hospital outpatient clinics, the patient event for costing is the outpatient attendance. If dental services are provided in the patient’s residence and recorded on the Community Services Data Set (CSDS), these should be entered into feed 3c: NAPC – community.
-
The unit of dental activity (UDA) is a unique data item for community dentistry. It is included in feed 18: Dentistry, so trusts can produce cost reports for UDA as needed for service management and commissioning. “UDAs measure the amount of work done during dental treatment. More complex dental treatments count for more UDAs than simpler ones.” NHS England (2018)
-
Where community dental contacts are not recorded in the main PAS but as UDAs in a separate clinical information system, that local data should be used to supply Feed 18: Dentistry. The patient contacts can then be costed under the costing process standards.
-
In some pathways, multiple patient contacts will relate to the same UDA. For example, the diagnostic contact will be followed by a treatment contact under the same UDA. These contacts are separate, often to enable the patient’s underlying health to improve before treatment (for example abscesses relating to the dental complaint or wider health issues) or to allow custom prostheses to be prepared. Each patient event should still be included in the costing system.
Specialist cost centres and expense codes
-
Map the general ledger to the cost ledger in accordance with the costing process standards, which will ensure the resources for dentistry are identifiable. The dental-specific cost centres in the cost ledger are XXX033 Dental services and XXX039 Dental laboratory. These can be customised in your local cost ledger where there are specific different dental services both inside and outside the hospital setting.
-
Other cost centres that may contribute to dental care will include theatres, day surgery units, outpatient departments, and community health centres.
-
Specific expense codes will include 5294: Dentist and dental nurse bands 1-9.
-
Bespoke prostheses purchased from external dental laboratories should be recorded under 7046: Other prosthesis
Resources
-
Spreadsheet CP3.1 shows resources for dental services.
-
Where dentistry services use medical and surgical consumables – including bespoke dental and orthodontic devices – in assessing and treating patients, allocate the cost to the patient according to Standard CM21: Clinical non-pay items.
Activities
-
Review the prescribed list of activities in spreadsheet CP3.2 and by working with the service team identify those your dental staff deliver.
-
With your service team, you should agree how the patient activities are identified from the data in Feed 18: Dentistry.
-
Oral health promotion takes place in many dental contacts but where the patient has a contact for oral health promotion with no other investigations or treatments, this should be recorded as Activity MDA076: Dental care.
-
Dental laboratories within your trust should use the relevant resource for the type of pay/non-pay items. Where they provide a service to your trust’s own patients, use Activity MDA075: Dental laboratory work, to allocate the cost to the patients.
-
Where this activity does not relate to your own patients, but to those of other providers, again use Activity MDA075; Dental laboratory work but treat it as commercial activity by applying the costing processes in CM8: Clinical and commercial services supplied or received.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to ensure the costed dental service activity is matched to the correct patient episode.
CM19: Wheelchair services
Scope
-
This standard applies to contacts with a patient provided by wheelchair services, including assessment, fitting, handover and review, and maintenance/repair.
-
It applies to all new and refurbished wheelchair equipment and accessories issued to the patient and the cost of maintenance, repair and refurbishment associated with the wheelchairs. Some wheelchairs and accessories/equipment are supplied by charities or other third parties. Only the cost incurred by the provider should be included in the costing information.
Overview
-
The wheelchair service issues a wide range of equipment and support to patients with a wide variety of conditions and requirements. The cost per patient will vary accordingly.
-
Most wheelchair services are provided during non-admitted patient care (NAPC) clinics in a hospital, health centre or at home. Some assessments and issues of wheelchair equipment may occur while the patient is an inpatient, for example following amputation surgery.
-
This standard supports the development of currencies and tariffs for wheelchairs.
Approach
Information requirements
-
There is no national clinical patient-level dataset submission for wheelchair services. Therefore, the costing system should include an information feed based on the patient level local data that is aggregated for submission to the quarterly collection – the National Wheelchair Data Collection.
-
Two information feeds are used: Feed 19a wheelchair contacts and Feed 19b wheelchair equipment. These enable the costing system to maintain information on the costs of wheelchair contacts separately from the equipment, repair and maintenance. See IR1: Collecting information for costing and spreadsheet IR1.2.
-
Wheelchair services are commissioned directly at patient level using the national currencies which rely on patient level information, so this information should be accessible. Your trust will record wheelchair service contacts either:
- in the main patient administration system (PAS) as outpatient attendances
- in a separate local system for wheelchair service activity.
-
Wheelchair contacts Feed 19a includes similar information to other NAPC feeds, but also includes additional data items held in wheelchair data systems not used in Feed 3a, that support the wheelchair currencies:
- level of patient need – low, medium, high, specialised
- type of attendance – assessment, fitting and handover, review (non face-to-face), repair and maintenance, or skills support
- powered or manual equipment.
-
Where the data is held in the PAS outpatient attendances, the patient events can be brought into PLICS in Feed 3a: Non-admitted patient care but this feed will require amendment for the additional wheelchair currency factors.
-
Wheelchair equipment should be brought into the costing system in Feed 19b: Wheelchair equipment, as described in Spreadsheet IR1.2. This will include the following data factors:
- wheelchair or accessory
- level of wheelchair package: low, medium, high, specialised
- manual/powered
- specialist seating
- repair and maintenance costs.
-
Costs of the wheelchair equipment issued at patient level required for Feed 19b will be recorded in a local system. This information will also identify if the equipment was issued new, following repairs/maintenance, or following refurbishment.
Specialist cost centres and expense codes
-
In the cost ledger, you should use cost centre XXX606: Wheelchair services. This can be customised using local digits to replace the XXX if you need to disaggregate costs to separate standard/specialist-complex services or adult/child services.
-
Expense codes specific to the staffing costs of the service include:
- wheelchair/rehabilitation therapists bands 6-9
- ancillary bands 1-4 for the wheelchair and rehabilitation assistants
- professions allied to medicine (PAM) or Allied Health Professionals (AHPs) expense codes bands 5-8d for the wheelchair/rehabilitation engineers/technicians.
-
Staffing can also include nurses, medical staff and specially trained administration staff. They should be identified by band in the same way as other staff and their costs allocated to the patients who use the service.
-
Wheelchair equipment should include chairs, cushions, and support equipment. You should use spreadsheet CP2.1 standardised cost ledger to identify the cost ledger expense codes.
-
Wheelchair repairs and maintenance have a separate cost from the purchase of new wheelchair equipment, and may either:
- be performed within the trust by designated staff – use the expense codes of those staff, and the components should show on cost ledger expense code: 7066 Medical and surgical equipment maintenance/repairs and components
- for items sent away to specialist companies – use the expense code: 7067 Medical and surgical equipment maintenance contracts.
-
Where there are repairs and maintenance of a wheelchair under contract from the manufacturer, there will be no cost in the ledger and therefore the repairs and maintenance do not need to be costed by the trust.
Resources
-
Spreadsheet CP3.1 lists the key resources to use for wheelchair service contacts.
-
Wheelchair equipment, excluding repairs and maintenance expense items, will map within the cost ledger to the resource ID: CMR303: Wheelchairs.
-
Repairs and maintenance expense codes map to resource ID: CMR338: Wheelchair repair/maintenance outsourced, and in-house components.
Activities
-
Activities for the wheelchair service include the contacts and issue of equipment, as shown in spreadsheet CP3.2.
-
With your service team you should agree how the patient activities are identified from the data in Feed 19a: Wheelchair contacts.
-
Activity IDs CMA305 and CMA342 should be attached to patient contacts, based on a calculation: CMA305 should have a clinical duration of up to 60 minutes and CMA342 should have a clinical duration of over 60 minutes.
Other considerations
-
Specialist wheelchair services do not require additional rules for costing, even though this area was not originally covered by the mandated national wheelchair commissioning currencies.
-
Some patients receive wheelchairs, equipment or accessories via the wheelchair services, which are not funded by NHS commissioning. The patient, charities or others will pay the trust for the equipment. The cost and income will be in the general ledger, and you should include the purchase value in the costing system. For reconciliation, the income should be in the ‘other operating income’ group. You can then show this income aligned with the patient equipment issued for reporting purposes, reflecting that the income contributes to a lower net cost to the trust.
-
Where equipment is collected from or returned by the patient for disposal, the disposal cost is included as an overhead to the wheelchair service.
Repair and maintenance
-
Repair and maintenance contacts are counted in line with the national currencies for wheelchair services.
-
Where repair and maintenance contacts are provided by the wheelchair service, they should be costed as patient events.
-
Where repair or maintenance components are delivered to the patient’s home without a contact, the issue should be recorded, and the cost identified separately to other contacts. The cost should not be allocated to patients that did not receive the items. For the National Cost Collection, these component costs can then be shown on the supporting information feed as part of the cost of wheelchair equipment.
Refurbished equipment
-
Where cost is incurred to recondition the equipment for future use, this should be identifiable on the wheelchair information system, and then included as the cost of the equipment in Feed 19b: Wheelchair equipment, when the equipment is issued to the patient.
-
Where equipment is refurbished the costs of refurbishment should be allocated across all wheelchair equipment in the costing period. This is because refurbished equipment may spend many months in the store until it is issued to the next patient, so timing for the refurbishment costs may not fall into the same costing year as the issue to a patient.
CM21: Clinical non-pay items
Scope
-
This standard applies to:
- all clinical non-pay items used in all patient care settings, including but not limited to wards, outpatient locations, community contacts, theatres and special procedure suites
- items identified as high cost devices in the NHS Payment Scheme list and MedTech innovation products
- clinical equipment that is not a capital purchase, including leased items and payments for loan equipment.
- It should be used in conjunction with the standard for the relevant area, for example
CM3: Non-admitted patient care and CM5: Theatres and special procedure suites.
-
The term clinical non-pay items for this standard includes prostheses, implants, devices, appliances, specialist dietetic foods, equipment and other clinical items. Other terminology may include ‘medical and surgical’ consumables and equipment but clinical non-pay items also include items used for mental health support, education and health promotion.
-
This standard does not apply to non-clinical use items, such as linen, uniforms, administrative items and basic food, although specialist dietetic items for patient use may be included as clinical non-pay items. It also does not cover medicines or blood and blood products, which are included in CM10: Pharmacy and medicines or wheelchairs and accessories, which are included in CM19: Wheelchair services.
Overview
-
Clinical non-pay items are an essential part of patient care and material items should be matched to the patient. The cost per item varies immensely, and therefore you should balance the materiality of the items against the amount of work required in identifying them to the patient.
-
Items that are material in cost per item should be allocated at patient level.
-
If an item is not material at a department level, you should also consider whether the unit cost or amount used of this item during a clinical event is so significant that recording and costing the item would improve the quality of the information to your trust.
-
Where the clinical items are not material to the cost of care, they should be allocated across the patients in the service area that used them.
-
The following definitions are provided for costing purposes to help with understanding the different terminology and types of items to expect in your trust (see also the Costing glossary). Please note, the definitions may overlap depending on circumstance and may differ from those used in your general ledger.
- An ‘implant’ is something intentionally left in the patient after surgery. Some implants will later be removed, and some will be permanent.
- A ‘device’ is an item ‘intended for a medical purpose, as assigned by the manufacturer’. They are usually a mechanical or electrical invention or contrivance and can be implanted in the body or used outside the body. For example, a pacemaker is implanted into the body; a circular external fixator frame is applied externally but goes into the body; and continuous positive airway pressure (CPAP) machines are applied externally.
- A ‘consumable’ is an item used once for a patient. These may also be called disposable or single use items.
- ‘Prosthetic and orthotic limbs/appliances’ are a personal item ‘worn’ by the patient to replace – or to support – a function of their body, for example a prosthetic leg, or a hearing aid. Appliance can also refer to an item of equipment used by a single patient, for example a walking frame.
- The term ‘prosthetic’ can also refer to an artificial body part implanted into the patient – such as a breast prosthesis.
- ‘Medical and surgical equipment’ includes non-capitalised items to be used by more than one patient in a clinical setting.
-
All implants and devices in the NHS Payment Scheme high cost devices list and listed procedures tab in Annex A: NHS Payment Scheme should be included in Feed15: Prostheses and other high cost items, to be costed at patient level.
-
Your trust will have cost, activity, and patient information available for these items, as this information is used to generate pass-through payment from commissioners.
-
You should also include any implants or devices your trust deems to be high cost for costing at patient level. We do not specify what constitutes ‘high cost’ for items not in the NHS Payment Scheme list. That is left for local policy.
-
Superior costing method SCM24 uses inventory management system to allocate other equipment/consumables/implants at patient level.
-
Data sources for patient level information will vary by trust. For example:
- implants within the Scan 4 Safety theatres protocol or other local tracking system. Your trust should have activity and patient information available, as this is used for patient safety
- electronic inventory management systems (IMS) that record the clinical non-pay items used at patient level, with the cost.
Approach
Information requirements
-
Obtain Feed 15 Prosthesis and other high cost items showing items of clinical non-pay to be costed at patient level. See IR1 Collecting information for costing and spreadsheet IR1.2.
-
Feed 15 allocates the cost for the item to the patient, irrespective of the location or setting of the issue. For example, a heart valve may be implanted in theatre and a prosthetic limb may be issued to the patient in an outpatient attendance.
-
You should include the following in Feed 15: Prostheses and other high cost items:
- consumable high cost items associated with specialist equipment such as perfusion or robotics
- consignment stock items actually used for the patient
- custom-made prosthetic limbs and appliances purchased from a laboratory or other manufacturer.
-
The patient-level feed will show the actual cost of the item. This will be used as a proportional weighting in the allocation of patient identifiable items in the costing account code. This allows for discounts and residual balances of cost on general ledger codes.
Specialist cost centres and expense codes
-
Clinical non-pay items are identifiable as expense codes in your general ledger to comply with the financial accounting requirements.
-
Many trusts will have clinical non-pay items in the budget of the service that uses it but others will keep the items as separate budgets. You should work with the service and your finance colleagues to understand where the cost is, to link it to the patients that used the service.
-
High cost items should be identifiable in your general ledger and have patient-level information available for safety and clinical tracking reasons. Wheelchairs and wheelchair equipment are covered in CM19: Wheelchair services.
-
The cost ledger expense codes have been set up so you can clearly identify the high cost devices and consumables in the appropriate code. The expense codes for medical and surgical consumables and equipment can then identify those not of significant cost, which will not be costed at patient level.
-
You may need to disaggregate the costs in the general ledger to separate the clinical non-pay items into patient identifiable and non-patient identifiable so they can be used for separate calculations.
-
You should identify the patient-level items first, and the rest will fall into the second group.
-
Items identified on a ‘sale or return’ or ‘consignment stock’ basis will only be in the general ledger at the point they are purchased, so no adjustment to the costing system is necessary. The patient level feed will only apply this cost to the patient when the item is issued. If the item is returned to the manufacturer the cost will be removed from the GL.
-
For clinical non-pay items that cannot be attributed directly to the patient, you should use the following categories of items and cost accordingly:
- consumables used in specific theatres, wards or service areas should be allocated to the patients in those areas based on duration of the operation in minutes
- consumables used in all theatres, wards or service areas, or where the cost is held centrally, should be allocated across all areas where the items are used to all patients.
-
The MedTech innovation devices should be identifiable in your general ledger. Not all are identifiable at patient level, but there are separate allocation methods depending on the product.
Resources
-
Clinical non-pay items should be mapped clearly from the expense codes to resources, showing whether they are patient identifiable or non-patient identifiable.
-
See spreadsheet CP3.1 for the resources using a patient-level feed.
-
Where there is no separate resource for patient-specific items, use resource ID: MDR052: Patient-specific consumables.
-
Resources for use where you are not using a patient-level feed:
- MDR046: Medical and surgical consumables – including medical gases and dressings
- MDR047: Medical and surgical equipment and maintenance – including hire.
Activities
-
Most high-cost items issued to the patient should use one of these activities:
- SGA089: Insertion of a prosthesis implant or device
- SLA160: Use of a MedTech Innovation Device
- SLA161: Use of PLGF Placental Growth Factor Test – MedTech Innovation.
- Other methods of issue are possible.
Matching
-
Use the prescribed matching rules in the integrated technical document in spreadsheet CP4.1 to ensure the costed prosthesis, implant or device is matched to the correct patient event, as in CP4: Matching costed activities to patients.
Expected costs
-
For many procedures – particularly those done in theatres and special procedure suites – the procedure would be expected to contain the cost of prostheses, devices and implants. These are often expensive, so investing time to ensure these procedures have clinical non pay items allocated to the patient event will improve the accuracy of the final patient costs.
-
Use the procedure (OPCS) field in Feed 1a: Admitted patient care in spreadsheet IR1.2 to compare the costed patient event for these procedures with the actual clinical non-pay item allocated. Where there is no item matched to the patient, this costed record may need a data quality review.
-
Review these with clinicians and service managers to ensure you are identifying and correctly allocating the appropriate costs to procedures for clinical non-pay items used. Be aware there may be timing or clinical coding issues with either the costed record or the PAS record.
-
The expected cost spreadsheet does not make any clinical statement about whether these items should have been used in this procedure. The list of prostheses, devices and implants in the expected costs spreadsheet is there to help identify missing costs in the costing outputs.
Inventory management systems
-
As part of the ‘Global Standard 1’ (GS1) project for the NHS, the expectation is that all NHS trusts have had the GS1 identifier (barcode) on all drugs (since February 2019) and medical devices (since May 2020). This provides more consistent information on the type and cost of items, which may improve the ability to link key items to patient level.
MedTech innovation products
-
The trusts that use these innovation products will have a clear funding stream from NHS England and should also have identifiable costs in the general ledger.
-
Some items are patient specific and some are technological products used across a range of products.
-
Report the cost of patient level identified devices in the Supplementary Information (SI) feed, using the patient level extract matching identifier (PLEMI) to identify the patient event where the device was used for the patient’s benefit. The placental growth factor tests do not need to be reported in the SI feed, as they are reported as a component cost using Activity SLA161.
- Where you find no patient identifiable data available for the products, you should allocate them across all patients in the service area that the products are used.
CM22: Audiology services
Scope
-
This standard applies to:
- all activities provided by audiology services, across all sectors, including purchase of equipment and patient contacts for assessment, fitting, review, maintenance and repair
- all patient hearing and balance aids, accessories and equipment provided by the audiology service, and the maintenance/repair of items for patients accessing the audiology service
- newborn hearing screening services.
Overview
-
Audiology services assess the hearing, tinnitus and balance function of referred patients, and support the associated disorders/diagnoses with various methods of rehabilitation.
-
Commissioning services for people with hearing loss involves a framework for commissioners defining the demographics, requirements and audiological pathways available to primary care. This standard explains the commissioning of audiological services supporting acute pathways, including ear, nose and throat (ENT) and complex hearing aid referrals.
-
The services may be direct access from GPs, ongoing and long-term support, or part of a broader pathway. Understanding which part of the service the cost relates to is critical to the accurate allocation of costs. The Direct Access Audiology (DAA) service “covers all patients referred to a direct access audiology service – that is a service not led by a medical or surgical consultant – regardless of where that service is provided”.
-
For costing purposes, the audiology services are broken down into the following areas:
- Audiology patient events:
Services for people with hearing loss are referred directly from primary care (direct access audiology or community audiology) or where the patient has been discharged from a primary care pathway but continues with the hearing loss/balance support element of their care – such as battery changes and repairs. The service may include complex referrals for patients with complex needs, for example learning disabilities and dementia. The audiology cost will be the main cost of this activity. - Ear, nose and throat (ENT) and other specialty support:
the audiology service provides clinical support to other specialties, including – but not exclusively – otology ENT services, which diagnose and treat diseases and disorders of the ear. The patient event will have the consultant-led specialty code.- Where the audiology support takes place in outpatient clinics or in theatres during surgical implant procedure. The cost of the audiology service will be a part of the consultant-led appointment
- the patient may alternatively attend the audiology department for specialist hearing/balance tests, but these activities are still part of the consultant-led service. The audiology will be the main cost of the event.
-
In the point above on ENT and other specialty support, audiology appointments are not separately reported for commissioning, and should not be costed separately from the main treatment function code (TFC). The location of the audiology contact with the patient does not define how it should be recorded in the activity data.
-
All patient events – including direct access audiology and audiology as a clinical support function – should be costed at patient level but note DAA is reported in the National Cost Collection at average cost per unit level in the AGG file.
-
Newborn hearing screening may be part of the audiology service or separate. You should identify how your trust structures newborn screening and ensure costs are categorised to the correct service.
Approach
Information requirements
-
Audiology services are largely provided as non-admitted patient care (NAPC) activity, so the data can be brought into PLICS via Feed 3a: NAPC.
-
Where the audiology contacts are held in a standalone system, you may use Feed 26: Audiology to load data. A standalone system may also hold other useful information about the contact.
-
Appointments for clinical support within ENT (and other specialties as relevant) may be identified by clinic codes within the patient administration system (PAS) or via the audiology system.
-
Feeds 3a NAPC and 26 audiology each have a flag in the feed to identify direct access patient events separately in your costing system.
Treatment function codes
-
You should use the appropriate TFC for costing as detailed on the data dictionary.
-
The TFC depends on the care professional who has clinical responsibility for the patient in that appointment:
- Under TFC 840 the audiologist has clinical responsibility – this is a ‘non-consultant led’ patient event.
- Where an audiologist works directly in a consultant led TFC clinic, the overall clinical responsibility for the patient in that appointment lies with the consultant. This appointment will usually be part of a wider pathway, not for hearing loss alone.
- Where an appointment is in the audiology department but is part of a consultant led pathway (ie the patient has not been discharged from the consultant) the patient event will remain under the consultant’s TFC.
- Where an audiologist or other specially trained staff member performs newborn hearing assessments, the clinical responsibility will be agreed locally. You should set up a local TFC for newborn screening to identify it separately from the other parts of audiology.
-
Adult and paediatric audio vestibular medicine are specialist services, only provided in a few trusts. You should only use this TFC if it is used in your commissioning contracts.
Currency codes
-
Audiology procedures in outpatient clinics require OPCS clinical coding to generate the outpatient procedures for reporting at HRG level – for example: using the OPCS code U243: Hearing assessment. This coding may be included in the record for ENT outpatients (or other treatment functions) to indicate audiology input.
-
Where clinical coding is not applied to the patient record but the patient has an outpatient procedure, you should agree a mapping table for the clinical codes with the clinical coders locally and apply these to generate the HRG for the patient event. There is no mandation of clinical coding for outpatients agreed by the Clinical Classifications Service. See the integrated collections guidance on audiology for more detail including the treatment of NAPC clinical support function audiology under a TFC other than 840 audiology but without clinical coding/HRG codes.
-
For direct access audiology, the patient events are not expected to have OPCS or HRG codes attached. You should work with the audiology service to apply the currency codes detailed in the integrated extract specification.
Admitted patient care
-
Most audiology services are provided during NAPC clinics but if an audiologist or other staff member attends an admitted patient, this can be recorded on Feed 7: Supporting contacts, to show the audiology component of the episode.
-
Some APC procedures – for example bone anchored hearing aids and cochlear implants – involve audiologists attending theatre sessions. You should identify sources of local information to ensure the cost of these staff is allocated to the relevant patient events.
Specialist cost centres and expense codes
-
You should use spreadsheet CP2.1 standardised cost ledger to identify the cost centres and expense codes.
-
You should customise your cost ledger to disaggregate the cost of the different parts of the audiology service to ensure the correct resource activity combination can be achieved. For example, to separate the direct access audiology from the clinical support function audiology.
-
Disaggregation may also be required for where staff provide a commercial service, services for another trust, or under ‘Any Qualified Provider’ contracts, which may need separate local monitoring.
-
Medical staff are not connected to the audiology cost centres, but if relevant, the cost ledger should have a separate cost centre to show doctors specifically in audiological medicine, for example cost centre code XXX049 Medical staffing – by specialty can be customised – for example X21049 Medical staffing – audiology.
-
Costs of the audiology equipment provided will be recorded in the local system or spreadsheet and should give the cost of the items issued per patient.
-
Where material, this information should flow to Feed 15: Prostheses and other high-cost items, to be matched to the patient appointment in accordance with CP4: Matching costed activities to patients. See CM21: Clinical non pay items. We are not specifying what is material but allowing trusts to agree locally whether this is a priority area.
Resources
-
Professional audiologists and associated staff are trained to provide the hearing, tinnitus and balance assessments, fitting and review of aids, rehabilitation with/without hearing aid provision, and ongoing long-term care.
-
Allocate audiologists and assistant technical officers pay costs using the resources MDR039: Audiologist and MDR040: Assistant technical officer (audiology).
-
Allocate audiology clinical non-pay costs such as hearing aids and implants using the resource ID: MDR041: Hearing and other audiology devices.
-
For cochlear implant or bone anchored hearing aids, the external part of the hearing aid may be applied in audiology; however, part may be implanted in a theatre or a special procedure suite. You should identify where the high cost implants sit in the GL and ensure these costs flow to the patient event where the device was implanted, in accordance with CM21: Clinical non-pay items.
Activities
-
You should identify which activities your audiology team deliver and map these to the activity list in spreadsheet CP3.2.
-
The activities will be costed using the ‘clinical contact duration of care contact’ field in Feed 3a: NAPC, in accordance with CP2: Clearly identifying costs and CP3: Allocating costs to activities.
-
With your service team, agree how the patient activities are identified from the data in Feed 3a: NAPC.
-
To ensure your local reporting shows the impact of audiology on the cost, use the Activity MDA062: Audiology assessment for all contacts where no equipment is issued.
Matching
-
The costs for material clinical non pay items should be matched to the patient for the episode or attendance where it was implanted/issued.
-
The materiality of the cost of devices should be considered locally. If a patient-level feed is not considered necessary, the cost of the devices should be allocated across all the patients who received them.
CM23: Direct access
Scope
-
This standard applies to all activity relating to direct access: this service receives direct referrals from primary care and provides diagnostic assessment and/or treatment.
-
This standard does not include direct access audiology, which is covered in CM22: Audiology.
Overview
-
A direct access service is defined as one carried out independently from an admission or attendance: for example, when a patient is referred by their GP.
-
Direct access is part of a clinical diagnostic service. The clinical responsibility for reviewing results and ongoing care of the patient remains with the GP who requested the test(s). GPs can directly access a range of diagnostic services for their patients, including pathology, phlebotomy, imaging, physiological and clinical tests.
-
In some regions, commissioners have agreed the provision of a wider range of clinical testing as direct access, including respiratory physiology (lung function testing), cardiac physiology and audiology (although audiology is covered in CM22: Audiology).
-
The cost of diagnostic or pathology services provided during admitted patient care (APC), critical care, outpatients or emergency care (EC) is included in the composite cost of those hospital patient events. They are not part of the direct access service because the clinical responsibility for reviewing results and ongoing care is with the care professional who requested the test and the provider, not the patient’s GP.
Approach
Information requirements
-
Direct access activity for imaging is identifiable in Commissioning Data Set (CDS) 6.2 through the direct access referral indicator field, and providers should report it using the relevant healthcare resource groups (HRGs). These scans can be costed at patient level.
-
For more information on pathology tests, refer to the National Laboratory Medicine Catalogue, which is designed to support consistent, standardised reporting and is available from the Technology Reference Data Update Distribution Service (TRUD).
-
Direct access should be reported under the ‘other activities’ cost group.
Resources
-
Direct access pathology costs should include the entire cost: staffing, consumable and machinery running costs and transportation of samples where appropriate.
-
The pathology service may contract some tests to external laboratories. You should identify where the cost for this is in the ledger and ensure it is allocated to the correct type of test (or group of tests).
-
The material resources most associated with direct access for pathology and phlebotomy and diagnostic imaging are:
- SGR062 Consultant
- MDR042 Medical and surgical consumables
- CLR017 Clinical scientists
- CLR015 Technician
- MDR047 Medical and surgical equipment and maintenance.
Activities
-
Use Activity SLA118: Direct access services.
-
Direct access testing will also use clinical equipment. The running costs of this equipment should be allocated across all the different uses, including hospital patient events and direct access.
Matching
-
You are not required to match direct access activity to master feeds in PLICS.
Other considerations
-
You do not need to calculate direct access activity at individual patient level. From a system perspective, multiple calculations do not need to be run if the correct costs and activities are used.
-
Direct access includes plain film X-rays and other imaging scans. You should be aware that the more expensive tests such as MRI and CT scans are lower volume. You should work with the diagnostic imaging team to understand and cost the activity to the appropriate tests.
-
Direct access pathology and phlebotomy are usually based on blood testing. The phlebotomy cost may sit in the hospital where the laboratory is based or in the community (for example where blood is taken in a GP surgery or community hospital). Therefore, for direct access the cost of phlebotomy should be separate from that for the test, to ensure the cost of the test is comparable.
CM24: Maternity
Scope
-
This standard applies to all maternity services provided by your trust, irrespective of sector. In this standard the term ‘community care’ for maternity relates to care given by any provider outside a hospital setting, including midwife-led care in GP surgeries and home births.
-
It includes care of the mother during the antenatal phase, the delivery event and the postnatal phase.
-
This standard also covers the care of the baby/babies before discharge from the maternity services, where they are not within a neonatal critical care episode or part of a paediatric care pathway.
-
This standard excludes fetal medicine although it is intended to include it in future years. We use the spelling ‘fetal’ medicine throughout.
-
This standard only applies to NHS provider staff. It excludes maternity services provided by GP primary care staff, including GPs and practice nurses.
Overview
-
The maternity service specialises in the treatment and care of women and baby/babies during a maternity episode, including pregnancy (antenatal), delivery and postpartum (mother)/postnatal care (baby).
-
The care delivered through the maternity episode starts at the ‘booking appointment’ where the pregnancy is recorded on the maternity data system. It will depend on the individual woman’s needs.
-
The care may be in a clinical setting or the patient’s home/other community location.
-
You should cost each patient event separately. This includes costing all the baby’s events, where they have a patient administration system (PAS) record.
-
Information from the auxiliary feeds should be matched to the patient events. This includes an auxiliary feed for the maternity-specific information (Feed27) sent to the Maternity Services Data Set (MSDS), which will link patient events for costing and reporting, including:
- mother to baby/babies
- patient events to the pregnancy
- and to match information not recorded in other feeds, such as ultrasound scans and screening not recorded in other auxiliary feeds. For example: some scans are done in treatment rooms by maternity medical or midwifery staff without a clinical radiology information system record but will be recorded on the MSDS.
- Maternity care should be provided in line with the National Institute for Health and Care Excellence (NICE) guidelines (select ‘topics’ then ‘service delivery, organisation and staffing’ then ‘Maternity Services’). In general, women with complex health conditions before or during pregnancy will have more contacts with the maternity service, and/or more complex care.
Antenatal care
-
Standard maternity care is usually midwifery-led. Non-admitted patient care (NAPC) activity is delivered both in hospital (Feed 3a) and in a range of non-acute settings (such as GP surgeries, health centres or the patient’s own home) (Feed 3d).
-
Consultant-led care (obstetrics) is provided for women of higher risk and complexity, in a hospital setting.
-
Mothers may be admitted for antenatal care, especially the higher risk patients, and conditions such as ectopic pregnancies and hyperemesis gravidarum (excessive nausea and sickness). Patients may also be admitted for termination of pregnancy or attend the ED or maternity unit for miscarriages. Both will end the maternity pathway. These events should be costed in the same way as other admitted patient care (APC) events. High risk mothers may have additional NAPC events, including additional scans and blood tests.
Antenatal screening
-
Screening currently comprises the combined test at 11 to 14 weeks for Down syndrome, Edward syndrome and Patau syndrome using maternal hormone levels and nuchal fold size, and assessment for structural abnormalities such as anencephaly/neural tube defects (for example spina bifida) and for completion of the abdominal cavity.
-
The screening continues with the 18 to 20 week anomaly scan to assess the fetus structural normality and determine if there are any indications for referral for a fetal medicine specialist’s opinion.
-
These screening tests should be costed and matched to the patient event when they occurred in accordance with CP4: Matching costed activities to patients. Screening attendances will mostly be NAPC events but may be a hospital NAPC contact (Feed 3a) or an NAPC community contact (Feed 3d).
Delivery phase
-
Delivery events can vary considerably depending on the type of delivery, for example caesarean section (elective or emergency), forceps, normal or multiple births. The delivery event should be costed according to the care the patient receives, including theatre time, ward care, delivery suite time, and where the cost of clinical non-pay items is material.
-
Delivery events can take place in different types of unit, including:
- hospital delivery suites
- hospital obstetric theatres
- midwife-led birthing centres
- home
- main theatres for a few very complex deliveries, including those for mothers with intensive needs and complex co-morbidities
-
The recording of home births is mandatory and must be submitted to the MSDS alongside the hospital births. Home births are not a mandatory submission to the Commissioning Data Sets (CDS)/Secondary Uses Services (SUS) data.
-
The costing system must include the HRG for all births, so the costing grouper will need to apply the HRG to all delivery events. This will show the hospital deliveries in Feed 1a APC and the home births in Feed 3e NAPC home births. There should not be a duplication of the same data item in both feeds. If there are data quality issues with this process, you should discuss the plan for improvement with informatics and maternity service colleagues.
-
The delivery event may start as a home birth and later transfer to a hospital unit. The home birth will be recorded as a distinct patient event in Feed 3e NAPC home births, and a spell will only start when the patient is admitted to hospital care in Feed 1a APC.
-
The hospital spell may contain one or more episodes, depending on whether the care transfers to another care professional or from midwife-led care to obstetrics during the admission. Figure CM24.1 illustrates the most probable scenarios, showing which treatment function code is used.
Figure CM24.1 Three patient events for delivery starting as home birth with subsequent transfer to hospital
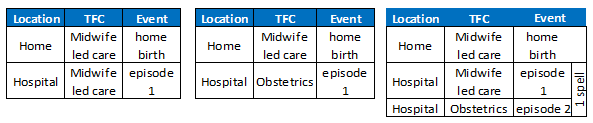
Figure CM24.1 outlines three different patient events for delivery starting as home birth and subsequent transfer to hospital all involving midwife led care at the start and then both midwife and obstetrics care.
Note: Each example would have a single pregnancy identifier but two or more data items. The home birth will be in Feed 3d and the admitted episode(s) will be in Feed 1a.
-
Costs should be applied to each separate event, showing the resources used at each stage. For example, theatre costs should only be matched to the hospital part of the care.
-
The mother delivering at home or in a birthing centre, whether an obstetric or midwifery unit, may have different care: for example, water birth, sensory stimuli and complementary therapies. Where material, the cost of the care items should be matched to the patient using Feed 15 Prosthetic and high-cost items.
-
Delivery events that result in a stillbirth should be costed in the same way as other delivery events. This outcome would close the maternity pathway so there would be no postnatal care but there might still be postpartum care for the mother. If psychological support is provided, this should be costed as part of the patient delivery event where it is given or recorded as a separate patient event for NAPC care.
-
Where the mother receives material additional care or education on feeding or care of the baby during the delivery event, this should be shown as part of the mother’s event, rather than as part of the baby’s event.
Postpartum/postnatal phase
-
Postpartum care begins once a woman is discharged from a maternity unit or birthing centre and includes postnatal care of the baby. Most postnatal care is provided in NAPC settings and may be provided in the woman’s home.
-
Use the discharge date of the delivery event to identify when the postnatal contacts begin. If there is a home birth and not a hospital birth, use the date of home birth to start the postnatal phase.
-
Postpartum/postnatal maternity care in the MSDS will generally cease to be part of the maternity service at ten days after the delivery event has completed. Longer periods of care may occur. Different datasets and clinical practice may cover different lengths of time after the delivery.
Care of the baby
-
When a baby is delivered, the baby will be recorded on the patient administration system (PAS) with their own separate clinical record, and an NHS number generated within six weeks.
-
For completeness, all babies delivered under the trust’s care should be included in the costing system so that the baby’s record can have cost attached to it when (if) the baby receives material care that can be quantified.
-
Treatment function codes (TFCs):
- If the baby has a neonatal level of care classification of one or above, they will be TFC 422 Neonatology and usually move to one of the neonatal areas.
- If the mother is discharged but the baby remains in hospital, they will be TFC 422 Neonatology and will move to a neonatal ward.
- While the mother is admitted (and well), and if the baby is considered within normal parameters of health, the baby will have TFC 424 Well Baby. A ‘Well Baby’ has a neonatal level of care classification of zero which is defined as ‘normal care’: the main care is given by the mother with medical and nursing advice if needed. See the FutureNHS Well babies: briefing paper.
- If the mother is significantly unwell but the baby is well, the baby will remain under TFC 424 Well Baby. The baby may remain on the maternity unit under the care by the maternity team or move to a neonatal unit.
-
The care of a well baby will as a minimum include:
- a first review in the national screening programme of new-born and infant physical examination (NIPE)
- a possible review by a paediatrician also
- initial and further midwife reviews
- Vitamin K injections before discharge.
-
As a superior costing method SCM80: Well babies – costed in detail, you can allocate these costs to the baby’s episode.
-
There is a risk that significant costs are not identified to the correct baby because the baby’s TFC is not always robustly applied, and TFC 424 Well Baby is not included in the National Cost Collection (NCC). You should therefore cost all babies under TFC 424 locally to identify any with significant cost. This enables local review of the baby’s episode, to ensure the treatment function code (and any clinical coding) is appropriate.
-
The babies receiving additional care should have these costs allocated to their record, and should be recorded as TFC 422 Neonatology, irrespective of the ward they are in. Care that would trigger this costing treatment includes:
- where the baby is receiving regular review from a neonatology doctor, for example on ward rounds
- babies who receive additional care or procedures (for example IV antibiotics or phototherapy)
- babies who need significant levels of monitoring (for example observations for risk of sepsis, meconium aspiration, hypoglycaemia)
- where a baby has a record on the critical care neonatal minimum data set with a neonatal level of care of 1 or above. The baby will have significant additional needs and reviews, and the critical care record and the core episode will both be costed. See CM6: Critical care and Feed 6a: Acute Hospital Critical care – neonatal.
-
The baby’s event may be recorded at birth or transfer to TFC 422 Neonatology during the episode to reflect the clinical responsibility for the additional care. Babies under TFC 422 Neonatology may remain on a hospital ward with the mother, or in the neonatal unit.
-
There should be no costs for the mother against the baby’s event.
-
The NCC guidance assumes there is no material use of resources anticipated for the care of a TFC 424 Well Baby. Local costs of the mother and baby delivery event should be added together.
-
Please note: ‘Well Baby’ is a data term. Babies are not necessarily ‘well’ or ‘unwell’ based on the TFC alone. The baby may be within a range of normal conditions for newborns but still require additional support. The accepted terminology for these babies should be agreed locally and used sensitively.
Approach
Information requirements
-
You should obtain the patient-level feeds necessary to cover all maternity services – feeds 1a, 3a, 3d, 3e, 12b and 27, as shown in IR1: Collecting information for costing and spreadsheet IR1.2. Table CM24.1 shows these feeds with names and descriptions
-
Feeds 3d, 3e, 12b and 27 may use data only reported in the MSDS. You should work with your maternity service and informatics teams to understand where the data should come from.
-
Feeds 1a and 3a will use data reported in the acute CDS. This data should also be in the MSDS. You should ensure there is no duplication in the costing system.
-
Midwives and medical staff frequently perform ultrasound scans in antenatal outpatient attendances, without requiring a sonographer. These scans should be identified from the data source that submits information to the MSDS and be brought into the costing system on Feed 12b: Diagnostic imaging maternity. Where material, the cost of equipment should also be matched to the mothers who had the scans. Scans can also be recorded on Feed 12a: Diagnostic imaging where they take place in the main diagnostic imaging department.
-
You should ensure that scans are not duplicated in feeds 12a and 12b. The pregnancy identifier is available in Feed 12b so it is preferable that any scans relating to a maternity pathway are included in Feed 12b, or elements will be missing from the maternity pathway reporting.
-
Feed 27: Maternity gives the mother and baby information to match to feeds 1a and 3a so that those patient events can show in reporting, by using the pregnancy identifier, which is already in feeds 3d, 3e and 12b. This allows a connection of mother and baby, and different patient events in the pathway. It will also be used for separating antenatal and postnatal NAPC contacts. See Table CM24.1.
Table CM24.1: Feeds for costing the maternity pathway
|
Feed no. |
Feed name |
Feed description |
Source data |
Purpose in maternity context |
Patient |
|
1a |
Admitted patient care (APC) |
Episodes for all acute services |
CDS (but should also be on MSDS) |
Any maternity admissions including delivery (excludes home births |
Adult, baby |
|
3a |
Hospital non-admitted patient care (NAPC) |
Acute outpatient contacts in hospital and other clinical settings |
CDS (but should also be on MSDS) |
Maternity outpatient contacts with all care professionals (excludes pure diagnostic appointments) |
Adult |
|
3d |
NAPC community midwifery |
Community contacts with patient – antenatal and postnatal. |
MSDS |
Home visits and GP surgery appointments which may/may not be recorded on hospital PAS |
Adult |
|
3e |
NAPC home births |
Delivery events started and completed in patient’s home, whether birth takes place there or not. |
MSDS (should not be on CDS) |
Home births are a separate patient event to a delivery in hospital and clear information is needed for accurate pathway review |
Adult |
|
12b |
Diagnostic imaging – maternity ultrasound |
Scans not recorded on main diagnostic imaging system |
MSDS |
These are usually performed during outpatients by the relevant maternity care professional (including specialist and midwife sonographers) rather than the diagnostic imaging department |
Adult |
|
27 |
Maternity services |
Pregnancy identifier and maternity pathway discharge date |
MSDS |
This allows the costing system to link the patient events to a pregnancy, connecting mother and baby, and identifies when that pathway has closed. |
Adult |
Ward attenders
-
Ward attenders see a clinician in the ward location without the need for a hospital bed admission. They are treated as ‘outpatients’ for costing and commissioning purposes and are identified in the information feeds (feeds 3a, 3b, 3c and 3d) using field ‘activity type location code’ E02 Ward (nursing and other non-medical professionals).
-
Some ward attendances will go over midnight (for example, in an early pregnancy unit but this could happen throughout a pregnancy), so the costing system should use the start of the attendance for the costed record (and for the National Cost Collection), to ensure the costed record is identified with other NAPC records in the same month. This date must be in the same month as the other submission data for the collection
Community midwifery
-
This area is known to have limited electronic data. The service should be recorded and submitted to the MSDS for clinical and safety reasons, so we recommend you work with the service and informatics team to develop consistent and robust patient-level information. We recognise costing is a secondary information use but that can be used as an extra reason to establish these information recording protocols locally.
-
We understand some trusts have been able to extend the use of their electronic neonatal systems to the whole maternity pathway, allowing real-time recording of all events whether in the hospital, the community or at home. This includes both high risk (consultant-led) and low risk (midwife-led) pregnancy pathways. It means that mothers-to-be in some trusts have access to their electronic record via applications on their smartphones or tablet, and because of this, these trusts are using such applications for their community midwifery contacts. In these instances, applications that cover all the maternity contacts (for example, BadgerNet Maternity Notes software) can provide extra data but it would still be the MSDS data items that are needed.
-
All trusts should have a digital midwife; a key contact for understanding the maternity service data (including community midwifery) and any data quality issues.
-
Where community midwifery PLICS data cannot identify the postnatal start locally, for example where the mother delivers in another trust, local technical reporting rules should be introduced to identify deliveries outside the trust. For example, if a baby record is created linked to the mother with a date of birth within nine months of a midwifery or obstetrics appointment.
-
Cross-border births are to be reviewed via matching with the MSDS after the first collection (ie not during this collection year). A field for Estimated date of delivery (EDD) has been added to Feed 27 to improve the matching of cross-border births.
Specialist cost centres and expense codes
-
You should refer to spreadsheet CP2.1 Standardised cost ledger for the cost centres and expense codes for maternity services.
-
For obstetrics medical staff, you can customise your cost ledger (CL) for cost centre XXX049 Medical Staffing – by Specialty.
-
If you require a delivery suite cost centre, you can customise your cost ledger for cost centre XXX051 Theatre/SPS.
Resources
-
Healthcare staff for maternity pathways can include the resources shown in Table CM24.2. You should ensure the mother only receives cost from the staff involved in her care.
Table 24.2: Resources for maternity by care type
|
Staff group |
Standard care / low-risk |
Complex care / high risk |
|
Midwives |
SLR085 Midwife |
SLR085 Midwife |
|
Maternity support workers |
SLR084 Healthcare assistant |
SLR084 Healthcare assistant |
|
Specialist midwives – antenatal/newborn screening and breastfeeding |
SLR082 Specialist nurse |
SLR082 Specialist nurse |
|
Sonographer within maternity department |
CLR022 Sonographer |
CLR022 Sonographer |
|
Anaesthesia team |
SGR065 Non-consultant medical staff – anaesthetist or consultant grade |
SGR065 Non-consultant medical staff – anaesthetist or consultant grade |
|
Obstetrician |
|
SGR062 Consultant |
|
Cardiologist |
|
SGR062 Consultant |
|
Psychologist |
|
SLR090 Psychologist |
|
Dietitian |
|
MDR033 Dietitian |
-
In some trusts, medical staff duties are split between obstetrics and gynaecology and this may need disaggregation to ensure appropriate cost allocation. Where a consultant works solely in either specialty, this will not be an issue.
-
Staff may be present for different lengths of time in home birth events. This should be considered when allocating cost to resources.
Medical and surgical consumables
-
You should pay particular attention to the medical and surgical consumables and equipment used during maternity procedures.
-
The unit cost of the consumables used in many maternity contacts may be negligible. But if you find these costs are material, per patient or in total, please refer to CM21: Clinical non-pay items.
-
Medical and surgical equipment such as delivery boxes used in home births should be costed and allocated to the patient who uses them, in accordance with CM21: Clinical non-pay items.
Activities
-
The main activities for the mother are shown in Table CM24.3. All admission events should be costed in the same way. See CM13: Admitted Patient Care.
Table CM24.3: Example activities for the mother in a maternity service
|
Phase of care |
Activity ID |
Activity description |
Use for: |
|
Antenatal |
SLA135 |
Outpatient care |
Hospital clinic attendances |
|
|
SLA158 |
Community maternity care |
Midwifery in community clinic settings or the patient’s home |
|
|
CLA022 |
Obstetrics Ultrasound |
Scans matched from Feed 12 Diagnostic imaging or Feed 27 maternity services |
|
Delivery (and other admissions) |
SLA097 |
Ward care |
Time on maternity wards |
|
|
SLA146 |
Birthing suite care |
Usually midwife-led deliveries |
|
|
SGA082 |
Theatre care – general |
Surgical or high risk deliveries, usually in specific obstetric theatres |
|
|
SLA147 |
Home birth |
Delivery at home |
|
Postnatal |
SLA135 |
Outpatient care |
Hospital clinic attendances |
|
|
SLA158 |
Community maternity care |
Midwifery in community clinic settings or the patient’s home |
Matching
-
Mothers and babies may receive care that is recorded on auxiliary patient-level feeds, including medicines, theatres, imaging from the main diagnostic imaging department and sonography. These component activities should be matched to the patient event in accordance with CP4: Matching costed activities to patients using the matching rules in spreadsheet CP4.1.
-
Where physiotherapy or other specialist therapies is part of the ward care budget, it should be costed as part of the ward care. However, if it is on a separate general ledger cost centre, you can include in Feed 7: Supporting contacts and match it to the patient event.
The Clinical Negligence Scheme for Trusts
-
The premium payment for the Clinical Negligence Scheme for Trusts (CNST) is calculated by NHS Resolution and is a considerable cost for maternity care See the FutureNHS CNST briefing note for more information.
-
Maternity services form the largest part of the premium – around 40% for most trusts. This is because of the impact maternity delivery can have on the long-term needs of the baby.
-
The premium will be notified to your trust in a ‘contributions letter’, with a supporting schedule, showing the value for your trust and the proportion relating specifically to maternity.
-
Follow the cost allocation method for allocating the whole CNST payment in spreadsheet CP3.3, using Resource ID SPR105: CNST payment.
-
Allocate the maternity portion to live births delivery events only.
-
Live births are identified from the secondary diagnosis code (ICD10) Z37* on the patient record. Please note: It is the mother’s delivery event that has the CNST matched against it, not the record for the new baby.
-
CNST should also be allocated to home births, using Feed 3e: NAPC to identify these patient events.
-
CNST maternity premium cost should not be allocated to admissions that are not a delivery event, outpatient attendances or community midwifery contacts.
-
As a superior costing method SCM37: CNST in maternity to use advanced weightings, you can agree to a local complexity weighting for this allocation with the local clinical team; for example, additional weightings for multiple births or where the mother has complex co-morbidities. See spreadsheet CP3.5: Superior and alternatives.
Other considerations
Early pregnancy unit
-
An early pregnancy unit (EPU) is a specialist unit that provides care for women with problems and concerns in early pregnancy. The care often centres around provision of an ultrasound scan to confirm the location and viability of a pregnancy.
-
The EPU forms part of maternity services, irrespective of when the patient is booked and which TFC the care is recorded under.
-
It can also provide treatment for women diagnosed with complications such as a miscarriage or ectopic pregnancy.
-
Some patients will attend a designated EPU in the early stages of pregnancy before a pregnancy is confirmed, as an admission, a ward attender, or an outpatient attendance. Others will attend after the pregnancy booking event, although this may occur prior to the booking date.
-
The service is usually specialist nurse, midwife or general practitioner-led care. The TFC of this service may vary, so identification of these patient events needs to be agreed locally where possible, for example by ward code.
-
Some staff will work in both the EPU and the wider maternity service. You should discuss the allocation of staff time to resources with the clinical team, to ensure the correct proportion goes to patient events in the EPU and the maternity service.
Fetal medicine
-
Fetal medicine is the specialty that encompasses the extra care required for babies in the womb, such as smaller babies or babies with complications and co-morbidities. All maternity services provide some fetal medicine care, but some services provide more specialised care for mothers and babies with particularly complex or highly specialised needs.
-
TFC 505 Fetal medicine will be applied where a specialist fetal medicine consultant is responsible for the care.
-
Some staff will work in both fetal medicine and the wider maternity service. You should discuss the allocation of staff time to resources with the clinical team, to ensure the correct proportion goes to each service type.
Parentcraft
-
Some staff will work in both parentcraft and the wider maternity service. You should discuss the allocation of staff time to resources with the clinical team, to ensure the correct proportion goes to each service type.
Safeguarding
-
As a superior costing method SCM81 Safeguarding maternity and paediatric services, where your safeguarding team can provide information on the proportion of time spent with maternity services, can be used to allocate that proportion directly to maternity, rather than allocating the costs across all patients equally as per spreadsheet CP2.2.
Transitional care
-
Transitional care means ‘in between care’ and is for babies who need a little more nursing care and monitoring than the routine care all babies receive on the maternity ward. It is offered to babies who require extra care or observations after birth and supports babies to stay with their mother rather than going to the special care baby unit (SCBU).
-
A baby may be admitted to transitional care after spending some time on the neonatal unit or may be admitted with the mother from the delivery suite. There are several reasons why a baby may be admitted to the transitional care unit. For example:
- babies who may need help to keep warm or with feeding
- babies who may need phototherapy (light treatment) for jaundice
- babies who may need treatment with antibiotics
- babies whose mother was known to have Group B streptococcus bacteria (GBS) in pregnancy
- babies born over 24 hours after the waters were broken (prolonged rupture of membranes)
- babies born between 35–37 weeks who do not require admission to the special care baby unit
- small babies suspected of having inter uterine growth restriction
- babies of diabetic mothers
- babies who were distressed at birth.
-
Each baby will be assessed by the neonatal team for admission to the transitional care pathway.
-
Transitional care facilities can form part of postnatal wards as well as being specific transitional care units.
-
To identify babies in transitional care, the activity may show on a specific transitional care unit ward, not a neonatal unit, but would normally sit under TFC 422 Neonatology.
CM25: Chemotherapy
Scope
-
This standard applies to:
- all patient events where the chemotherapy is administered, including admitted patient care (APC) and non-admitted patient care (NAPC)
- all medicines prepared and dispensed as part of a chemotherapy pathway, including medicines delivered to the patient’s home, hormone therapy, immunotherapies and supportive medicines
- the cost of preparatory services for chemotherapy, such as aseptic suites within pharmacy departments
- interoperative chemotherapy.
Overview
-
Chemotherapy is a type of cancer treatment that uses medicines to kill cancer cells. Chemotherapy agents are also used for a few other conditions such as rheumatoid arthritis.
-
The main aims of chemotherapy treatments are to:
- cure cancer – this is known as curative chemotherapy
- make other treatments more effective or reduce the risk of the cancer returning: for example, it can be combined with radiotherapy (where radiation is used to kill cancer cells) or given before surgery (see CM26: Radiotherapy)
- relieve symptoms: for example, where a cure is not possible, palliative chemotherapy may relieve symptoms
- enable surgery or radiotherapy to be easier or more effective used before (also called ‘adjuvant therapy’)
- lessen the chance of the cancer returning used post operatively/post radiotherapy.
-
It is essential to understand the chemotherapy in the context of the broader treatment plan to ensure the costs are allocated correctly and local reporting is appropriate and meaningful. For example, one plan might consist of:
- initial outpatient attendance
- multidisciplinary team (MDT) meeting to agree on the most appropriate plan of treatment (see CM9: Clinical MDT meetings)
- surgery (for solid tumours) followed by
- chemotherapy (a series of attendances, admissions, or home delivery).
-
The act of administering chemotherapy to a patient is called ‘delivery of chemotherapy medicines’ (see Activity section below). Patients receive their chemotherapy in a variety of settings, including home/community or as day-case, regular admissions or outpatients.
-
Methods of chemotherapy delivery are varied, and the most common include:
- oral (by mouth – can be a tablet, liquid or sub-lingual)
- intravenous/infusion (into the vein via cannula, peripherally inserted central catheter (PICC) line, central line or port)
- intrathecal (into the fluid around the spinal column or brain)
- ophthalmic (into the eye – usually done in the eye unit)
- intramuscular (injection into the muscle) – particularly gynaecology
- subcutaneous (injection between skin and muscle)
- a bolus injection (single large dose)
- intra-arterial
- topical
- implantable
- intraoperative, (during surgery) including peritoneal (administered into the lining of the abdomen).
-
Oral and intravenous/infusion are the most frequently used methods.
-
The different approaches may require varying admission methods and consumables.
-
Intravenous chemotherapy has various methods of administration to the patient, including:
- via a disposable cannula inserted and removed at each attendance
- a central line, PICC or implantable port that remains in place for the course of treatment. It is normally inserted under local anaesthetic at a day case or outpatient attendance before treatment begins. This procedure should be costed at the patient event when it is inserted and not included as part of the chemotherapy delivery cost.
-
If a patient has a permanent (or semi-permanent) central line or port installed, the costs of the installation or removal procedure costs should relate to the event when it was installed/removed.
-
The medicines used in this event are identified at patient level using the resource ID for medicines and separate activities for dispensing chemotherapy medicines (see Activity section below).
Approach
-
The patient event to be costed is where chemotherapy medicines are given to the patient. For many patients this will be an NAPC event, and some patients will have their medicines delivered to their home. See the section on homecare below.
-
Chemotherapy medicines should be matched to the patient event at patient level.
-
The cost of supportive medicines used alongside chemotherapy should also be allocated to the chemotherapy patients. These are used to alleviate symptoms of the chemotherapy, such as chronic sickness and fatigue. As a superior costing method SCM78, the cost of these supportive medicines can be allocated to the patient event at patient level.
-
Home delivered chemotherapy medicines should be costed at patient level using Feed 10a: Medicines dispensed and should use the prescribed resources and activities. These will not match to a patient event, as the medicines are delivered for consumption at home. The costing system should be able to report these medicines separately from the patient events in the rest of the patient’s care pathway.
Information requirements
-
The patient event data is brought into the costing system as described in IR1: Collecting information for costing.
-
Most patients who attend for delivery of chemotherapy do not stay overnight. They are recorded as a day-case, a regular day admission or an outpatient. One attendance for chemotherapy delivery is one patient event.
-
Where the patient events for chemotherapy are within the main patient administration system (PAS) and are submitted to the Commissioning Data Set CDS, use the following feeds:
- For outpatient chemotherapy use Feed 3a: Non-admitted patient care.
- For day case and regular day admissions, use Feed 1a: Admitted patient care.
- For patients receiving chemotherapy as part of a longer admitted episode, use Feed 1a: Admitted patient care but be aware there will be no chemotherapy delivery OPCS code in the patient record, as currently there is no chemotherapy delivery clinically coded for overnight admissions. The chemotherapy will be identified using Feed 10a: Medicines dispensed, which has a chemotherapy drug flag as one data item.
-
Where the chemotherapy delivery is not available in the main NAPC or APC data or does not flow to the CDS, use Feed 29: Chemotherapy delivery.
-
You should work with the cancer services or pharmacy information leads to obtain this data from a local source.
-
The costing grouper will currently generate HRG codes for chemotherapy procurement but you will not need these for the costing process in any care setting or the patient-level National Cost Collection. The chemotherapy drugs now use Feed 10: Medicines dispensed as a component part of the delivery patient event and should be identified by the drug dispensed.
-
Existing delivery HRGs cover factors such as first/subsequent attendance, simple/complex regimens and method of administration.
-
You should identify the patient events specifically for chemotherapy in your costing system.
-
Some patients admitted for chemotherapy as day case or regular day admissions will have another HRG relating to the reason for admission, because the clinical coding generates the HRG for the other elements of care. If the patient was admitted primarily for chemotherapy, you should apply the SB HRG subchapter to this patient event.
-
Many patients admitted overnight who receive chemotherapy will have another, more detailed HRG relating to the reason for admission. These should go through the national cost grouper in the same way as all other relevant patient events. They will not have chemotherapy HRG but will be identifiable by the activity codes relating to chemotherapy.
-
If the main PAS does not have sufficient data items to identify the chemotherapy delivery, other information sources can be used to contribute to the PLICS feed. For example:
- electronic prescribing systems
- local clinical information systems collecting data supplied to the Systemic Anti-Cancer Therapy (SACT) dataset
- ChemoCare data system.
-
If using these supplementary data sources, you should ensure the process is consistent and reliable, and reconciling between sources is not burdensome.
-
You will need to bring data for time spent in the aseptic unit for chemotherapy services into the costing system. This can be done using a local feed to construct the relative weight values or as superior costing method SCM67.
Specialist cost centres and expense codes
-
The main cost centre shown in spreadsheet CP2.1: Standardised cost ledger, for adult chemotherapy is XXX093 Chemotherapy unit.
-
For children and teenagers/young adults, chemotherapy will be delivered differently – for example, on designated wards. You should identify the area(s) with the service and customise your cost ledger to ensure the chemotherapy can be identified.
-
The expense codes for the staff type should be used. This will mainly include nurses and administration according to the service in which the staff work.
-
Some trusts may have additional staff (for example paediatrics) or oncology specialist nurses in different cost centres to the chemotherapy unit. You need to identify these costs in the cost ledger and ensure they are identifiably allocated to the correct resources.
-
A vital part of the chemotherapy service is the specialist pharmacists who prepare and manage the complex medicines. You should ensure any specialist pharmacists and their services, are identified as part of the work on the pharmacy services, in conjunction with CM10: Pharmacy and medicines.
-
The cost of chemotherapy preparation in the aseptic suite should be identified and allocated to the patient events where chemotherapy was received, as this is where trust pharmacists prepare the chemotherapy medicines. The cost centre is XXX096 Aseptic unit.
-
Where there is a separate pharmacy for chemotherapy, you can customise your cost ledger to include this cost centre separately from the main pharmacy cost centre.
-
Chemotherapy medicines should be recorded on the Expense code 7026: Medicines.
-
Where chemotherapy medicines are purchased already prepared for the patient, the cost of the aseptic suite is included in the purchase cost. You should identify how these medicines show in the general ledger and if a proportional split between the medicine cost and the aseptic unit cost/staff time is not available, you should report the purchase of the medicines on the Expense code 7026: Medicines.
-
As a superior costing method, where there is a proportional split available between medicines and aseptic unit/staff time, you should allocate the latter as Expense code 7021: Contract: pharmacy services (not including medicines) within the cost centre XXX096 Aseptic unit.
-
Home delivery of chemotherapy prepared in and delivered by the trust will include the cost of the pharmacy staff used to prepare and dispense the medicines, the use of the aseptic suite/unit and the costs of delivering the medicines, for example driver, vehicle costs. These costs should be separately identifiable in the cost ledger via the cost centre XXX041 Home delivery of medicines so the information can flow through the costing system.
-
If your trust buys in the home delivery of chemotherapy drugs this should also be separately identifiable in your general ledger (and therefore cost ledger) so the cost of other patient events is not inflated. You should use the cost centre XXX041 Home delivery of medicines and Expense code 7026: Medicines.
Resources
-
Map your staffing costs to resources via the mapping in spreadsheet CP2.1: Standardised cost ledger, according to their professional group. This includes staff delivering the chemotherapy and staff preparing and dispensing the specialist chemotherapy medicines.
-
All chemotherapy medicines will use the resource code MDR044 Medicines.
-
Where medicines are purchased complete, including the preparation in an aseptic suite, the drugs should use resource code MDR044 Medicines.
-
As a superior costing method, where the purchased medicines and aseptic unit costs can be separately identified, using the resource code of MDR044 Medicines (as for own trust prepared services), and the aseptic suite cost will use resource code CLR034 Services received: aseptic suite services.
Activities
-
For the staff and non-pay used in patient events specifically for delivering chemotherapy, use Activity SLA142: Chemotherapy delivery. You can also use this delivery to identify patients receiving chemotherapy as part of their overnight episode using the chemotherapy drugs dispensed to them.
-
For the medicines, use Activity MDA067: Dispensing chemotherapy medicine scripts.
-
For the pharmacy time spent in the aseptic unit preparing chemotherapy, use the Activity MDA074 Aseptic unit work.
-
Some patients may have a medical staff consultation as well as the delivery of chemotherapy to prevent them from having to make a separate trip to the clinical service. The consultation cost should be allocated to the patient event using the appropriate resource for the staff member(s) and the Activity SLA135: Outpatient care.
-
For any medicines delivered to the patient at home, use the Activity SLA126: Dispensing and delivery of homecare medicines.
Matching
-
The chemotherapy medicines should be matched from Feed 10a: Medicines dispensed to the patient event, using the hierarchical rules on spreadsheet IR1.2 (see CP4: Matching costed activities to patients).
-
As superior costing method SCM78, supporting medicines can also be matched to the patient event.
-
As superior costing method SCM67, aseptic suite work can be matched to the patient event where the drugs were given to the patient.
-
The chemotherapy preparations and aseptic suite work will usually take place before the patient event. The items are then stored until needed. The matching rules for the medicines feed should be reviewed locally to ensure sufficient time is allowed between preparation and patient event.
-
The costs of material clinical non-pay items for these procedures should be applied to the patient event where the item was used, in accordance with CM21: Clinical non-pay items. As superior costing method SCM24, the costs of the consumables for the appropriate delivery method can be allocated to the delivery event at patient level.
Other considerations
Home delivery of chemotherapy medicines
-
When the chemotherapy medicines are delivered to the patient’s home (usually oral medication) there will be no ‘delivery’ event as the patient administers their own medicines. However, it is crucial to understand the pathway including this cost. You should therefore cost the service at patient level.
-
Feed 10a: Medicines dispensed can identify homecare medicines with a flag for the delivery to a patient’s home, as pharmacy systems are required to have this for national reporting. These should not be matched when the medicines feed is matched to the patient events.
-
Where homecare medicines are provided by a third-party organisation, or from a medicine system separate from the main pharmacy system, you can use standalone Feed 10b: Homecare medicines dispensed.
-
For local reporting your costing system may need to create a ‘host’ or ‘proxy’ patient event to attach the costs to.
Telephone consultations
-
Patients cannot have chemotherapy administered by telephone but a telephone review of the pre-treatment blood tests can be discussed to agree when the patient will start/continue the self-administration of chemotherapy, or to receive supporting information from a clinical professional (for example nurse, doctor, pharmacist) about the chemotherapy they are taking at home.
-
If patients have these telemedicine consultations to discuss their chemotherapy, they should be recorded under Feed 3a: Non-admitted patient care using the relevant treatment function code (TFC). Refer to CM3: Non-admitted patient care and IR1: Collecting information for costing for further details. These are not chemotherapy delivery events.
Chemotherapy in the community
-
Specialist nurses will attend some patients to deliver chemotherapy at their home or at satellite community clinics. These should be recorded and costed in the same way as other NAPC, with the activity location type showing the setting for the delivery.
Chemotherapy waste
-
Some patients have chemotherapy dispensed to their prescription but are too unwell or do not attend to receive when the delivery time comes. This usually means the prepared medicines are wasted.
-
Where the patient has arrived for the delivery event, the cost of the medicines should still be matched to the patient event. If the patient has not attended, the medicines will remain unmatched to an event.
-
If information is available on the wasted product, this can be identified using a separate activity code SLA168 Chemotherapy wasted medicines. This will include the cost of the medicine and any cost of disposal (if identifiable).
-
If the information on waste is not available at patient level, the cost should be allocated across all patients having chemotherapy.
Clinical trials
-
Some organisations have substantial clinical trials activity for cancers, including developmental chemotherapy:
- As clinical trials funding usually covers only the costs of the medicines being tested and treatment costs over and above standard NHS treatment, this activity should be costed in the same way as regular NHS patient events, excluding any costs covered by the trial.
- Clinical coding rules for clinical trials may result in patients not having OPCS codes identifying their chemotherapy in the same way as other chemotherapy. You should liaise with your clinical coding team and chemotherapy service to understand these patient events.
CM26: Radiotherapy
Scope
-
This standard applies to:
- all patient events with radiotherapy planning and treatment, including non-admitted patient care (NAPC) and admitted patient care (APC)
- all radiotherapy, including the modalities of external beam and internal radiotherapy (including brachytherapy and molecular radiotherapy)
- the high non-pay costs of providing radiotherapy services.
Overview
-
Radiotherapy is a treatment where radiation is used to kill cancer cells. The treatment is given in specialist radiotherapy centres.
-
Most radiotherapy is delivered using external beam radiotherapy, which usually involves a series of outpatient attendances where radiotherapy is given to a carefully specified target area or areas. It is usually given using a linear accelerator or other specialist treatment machines, which may include ‘superficial treatment units’ that deliver lower voltage treatments than a linear accelerator.
-
External beam radiotherapy includes treatment techniques using photons, such as image-guided radiotherapy (IGRT), stereotactic radiotherapy (SRT/SABR) and conformal radiotherapy (including intensity-modulated radiotherapy. Volumetric modulated arc therapy is a type of intensity-modulated radiotherapy. Proton beam therapy using protons (rather than photons) is now provided by three NHS providers.
-
Medical physicists will be included in the process of planning and administering external beam therapy, including calculating the dose of radiation and verifying the quality of the treatment.
-
Internal radiotherapy is introducing radioactive material to the site of the tumour (in solid or liquid form). Some treatments can be delivered in the nuclear medicine department.
-
The costing process for radiotherapy uses the structure of healthcare resource groups (HRGs) for costing. You should therefore understand the HRGs in association with the chapter summaries (subchapter SC), which separates the radiotherapy into planning and treatment HRGs. These grouped currencies are the patient events that are costed.
-
This approach is taken so the preparation for radiotherapy (planning) can be costed separately from the treatment. Most (but not all) patients will attend the department for a planning patient event, although most of the planning will take place without the patient. As there is not necessarily a patient event, the planning HRG is created on the first patient treatment event.
-
Each treatment has a patient event, so these can be costed in their own right. There is no requirement to cost the ‘core HRG’ SC97Z.
-
The data for external beam radiotherapy costing can come from clinical coding in the patient administration system (PAS) that groups to HRGs or from information in the radiotherapy clinical information system (also called the oncology management system).
Approach
-
External beam radiotherapy and internal radiotherapy brachytherapy both have a planning phase and treatment patient events.
- For external beam radiotherapy, the HRGs for planning and treatment are the events that are costed. Where the grouper creates a ‘core HRG’, this should be ignored for costing purposes.
- For internal radiotherapy brachytherapy, the patient is usually admitted and radiotherapy planning and treatment costs are a component of that episode. Use the costing activities to identify the radiotherapy part of the care in the core HRG.
-
Molecular radiotherapy will have a treatment event but not a planning event. Some molecular radiotherapy patients will be admitted but some will be treated in an NAPC setting.
-
Radiotherapy can be delivered on linear accelerators (mega voltage units) or on a superficial treatment unit (kilo voltage). Not all departments have both facilities.
External beam radiotherapy
Information requirements
-
Radiotherapy data is collected in a radiotherapy clinical information system that contains appropriate information for the costing process and National Cost Collection. This data is submitted to the radiotherapy dataset.
-
You should bring the radiotherapy from this information system into the PLICS using the separate Feed 28: Radiotherapy. This will allow clear reconciliation to the radiotherapy dataset.
-
As an acceptable alternative, if your radiotherapy patient events are also recorded in the main PAS and submitted to the commissioning dataset (CDS), you may bring the data for radiotherapy HRGs into PLICS in Feed 3a: NAPC.
-
You should ensure there is no duplication of patient events in the costing system and the feed used contains all the information needed for the costing process and the National Cost Collection.
-
HRGs for external beam radiotherapy include one event for ‘planning’ for the prescription of each course of treatment, and a set of patient events with a separate treatment HRG being allocated for each fraction delivered. Further information about the HRGs is available in the National Casemix Office chapter summaries.
-
Feed 28a: Radiotherapy should include the HRGs for each planning and treatment event.
-
The treatment HRG and planning HRG will show in the HRG data field in either Feed 28 or Feed 3a. If Feed 3a is used, the HRG for treatment and planning should be in the HRG field.
-
The patient may attend the service area multiple times for planning reasons before the planning phase is complete to have measurements taken, masks or moulds made and tested of the area for radiotherapy, and for a CT or MRI scan. These separate attendances are not costed separately – they are part of the single planning patient event. You should identify any planning attendances from the data and use only them to support the allocation of cost.
-
The duration of the staff input may not be recorded against a patient event, so you should either:
- obtain a supporting contact feed linking the duration of the time spent to the individual patient or
- discuss an appropriate relative weight value (RWV) with the clinical team to allocate the cost to patients having radiotherapy events.
-
Most external beam radiotherapy treatment will be NAPC. However, where a patient is admitted for external beam radiotherapy or is already admitted and receives external beam radiotherapy during their episode, the clinical coders will apply the clinical codes, and the grouper will generate HRGs. If you are using the radiotherapy system as the main source of data in Feed 28, you should ignore the radiotherapy HRGs grouped as part of the APC episode as the patient event will come from the external beam radiotherapy data.
-
For local reporting, external beam radiotherapy can still be shown with the correct APC patient event.
Specialist cost centres and expense codes
-
You should refer to spreadsheet CP2.1 standardised cost ledger for the cost centres and expense codes for radiotherapy.
-
Planning events will include:
- medical physicists, dosimetrists and radiographers who contour the area to be treated and produce a treatment plan that includes the dose distribution and parameters calculating the radiation dose information
- clinical oncology medical staff who may also provide input to the planning process
- radiographers or mould room technicians who make immobilisation devices (moulds) to keep the patient still during treatment
- depreciation of the treatment planning information system, oncology patient management information system, dosimetry and IT equipment
- consumable items of the planning process (where material)
- as a superior costing method, the running costs of the specialist scanning equipment (such as CT).
-
Treatment events will include:
- radiographers who set up the patient in the treatment position according to the treatment plan and administer the radiotherapy as prescribed
- supporting nursing and other staff who manage the patient during the event
- the linear accelerator running costs and depreciation and superficial treatment unit running costs and depreciation
- consumable items for each treatment event (where material).
-
Clinical oncologists contribute to the overall service and will instigate a patient prescription, leading to the plan for treatment. They may contribute to the specific patient pathway via multidisciplinary meetings or be involved in specific patient planning. They do not see the patient during the planning or treatment but are there for clinical advice when/if needed.
Resources
-
The staff type in spreadsheet CP2.1 standardised cost ledger maps to the appropriate resources.
-
For non-pay, you should allocate the maintenance, repair and running costs of the high-cost radiotherapy equipment to patients who have treatment events, using the appropriate expense codes and the resource code MDR047: Medical and surgical equipment and maintenance.
-
Depreciation for linear accelerators and other equipment should use the expense code for the type of asset and be allocated to the overhead code T1S023: Depreciation – medical equipment. The depreciation for linear accelerators is allocated to the treatment patient events only.
-
As a superior costing method SCM55 depreciation on CT scanners and radiotherapy treatment planning systems used wholly for radiotherapy can be allocated to the planning HRG.
-
Consumable items will include items used to make moulds, and disposable parts of equipment. Cost these as in CM21: Clinical non-pay items.
Activities
-
You should refer to spreadsheet CP3.2 for the Activities relevant to radiotherapy.
Internal radiotherapy – brachytherapy or molecular radiotherapy
-
The different types of therapy will be given in different service areas and treat different conditions, so you should discuss the specifics of each type with the service team. To find these services you could liaise with the financial management team to track the high-cost radioactive items or look at the data recorded to see if the HRGs highlight the areas for specific costing work. Figure 26.1 shows a diagram of the main categories with examples.
Figure CM26.1 Types of internal radiotherapy
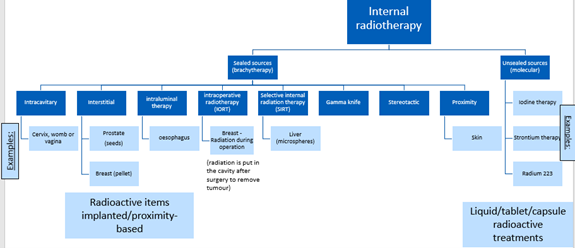
Figure CM26.1 outlines types of internal radiotherapy through sealed sources (radioactive items implanted/proximity-based) and unsealed sources(liquid/tablet/capsule radioactive treatments).
-
The method of administration will vary, including:
- A sealed radioactive source implanted into the body: types include low dose rate and high dose rate; for example, interstitial radiotherapy for prostate cancer is given by implanting seeds.
- Molecular radioactive treatments containing an unsealed source, administered via a drink, capsules, a cannula or as an injection: the radiation treatments are also known as radioisotopes or radionuclides. Types include radioactive iodine, radioactive strontium therapy and radium 223 therapy. This service may be delivered in radiotherapy or nuclear medicine departments.
-
The service is highly regulated, including licensing for the organisation and for individual practitioners, with a cost for each licence. These licences are set out by the UK Health and Safety Agency, the Health and Safety Executive and the Environment Agency.
-
The planning process for some patients will take place in a similar way to the external beam radiotherapy, with specialist professionals calculating the appropriate dosage and other staff contributing to the plan. For others, there will be no specific planning process required to be costed and reported separately.
Information requirements
-
Brachytherapy and some molecular radiotherapy treatments are delivered during an admission. The patient events are brought into the costing system using Feed 1a: APC.
-
For admitted patients, the clinical coding will identify the internal radiotherapy, so you can use this information to cost the treatment (and any planning elements) as a component part of the episode. SNOMED-CT codes are more detailed for internal radiotherapy than OPCS codes, so should be used if they are available.
-
Other types of internal radiotherapy – especially molecular radiotherapy – will be performed in a NAPC setting, as there is no hazard from the radiation once it is in the patient. Use Feed 3a to bring these into the costing system. Internal radiotherapy performed in a NAPC setting may not be clinically coded, so you will need additional information from the service.
-
The treatments will usually take place in a specially shielded procedure suite, which may be in the main radiotherapy suite, the nuclear medicine unit or another specialist service area. This information may be available on Feed 4: Ward stay or may be collected locally.
-
The radioactive items used to give the radiotherapy doses are significant in cost and need to be tracked for radiation safety, to comply with the licence regulations. Information on them will therefore be identifiable at patient level. Use Feed 15: Prostheses and other high-cost devices to bring the information into the costing system.
-
You should ensure you can identify if the information feed is at patient level or the source of radiation level: for example, where one vial of radiation is split between two different patients.
-
Removal of the sealed sources seeds/needles is a separate patient event. This will be costed separately to the radiotherapy planning or treatment.
Specialist cost centres and expense codes
-
Use cost centre XXX101 Internal radiotherapy or XXX708 Nuclear medicine unit. These can be customised by using a local code in place of the XXX where you have different treatments in one service area.
-
Use the expense codes in spreadsheet CP2.1 for the appropriate staff group.
-
Use expense code 7813 Radioactive seeds, beads, capsules, liquids for the sealed and unsealed radioactive items, whether they are prepared on site, or purchased readymade.
-
You should use CM21: Clinical non-pay items to ensure the cost of these and other non-pay items is allocated appropriately, matching cost to patients in accordance with CP4: Matching costed activities to patients and spreadsheet CP4.1.
Resources
-
Use the resources shown in spreadsheet CP2.1 including resource CLR035 Radioactive implants, liquids, and devices for the sealed and unsealed sources.
Activities
-
The patient may be radioactive for some time following some types of treatment. They may require an ensuite, shielded ward room for their care, with specialist equipment for monitoring the radiation levels of the waste. Use Activity SLA097: Ward care to show this care.
-
The patient may be admitted to the specialist procedure suite or to the ward. Where they remain on the specialist procedure suite, there will be no additional ward costs. If the patient stays in a ward separately from the specialist procedure suite pre- or post-op, use the activity ID as for other episodes.
-
Where a theatre or special procedure suite is used for the treatment, you should refer to CM5: Theatres and specialist procedure suites.
-
Where imaging is performed during or following an internal radiotherapy procedure, you should cost the scan and use the relevant activity code.
Other considerations
-
There are no consultations with medical staff about the cancer pathway included in the cost of external beam radiotherapy planning or delivery. If the patient has a consultation during their visit to the radiotherapy suite, this should be recorded separately and costed as a NAPC patient event.
-
Likewise, most patients for molecular radiotherapy will not see a consultant oncologist during the treatment event.
Radiotherapy and chemotherapy as part of a wider admission
-
In a few patient events, the patient receives chemotherapy in conjunction with the radiotherapy. Here the core HRG is likely to be an APC episode, which should be costed according to the resources used and activities undertaken, in line with CM25: Chemotherapy services.
-
The chemotherapy medicines will form a component part of the core HRG. The chemotherapy delivery cannot currently be clinically coded, so will also form part of the cost of the core HRG; but the medicines will identify that the chemotherapy has been delivered during the admission.
-
The radiotherapy planning and delivery HRGs should be costed separately.
-
There may be some overlap in staff working with the patient – for example, nursing support. Allocate this cost using information from the service.
-
If the contact is only for chemotherapy and radiotherapy treatment, there is no requirement to cost the core HRG. See also CM25: Chemotherapy services.
Proton beam therapy
-
This service is provided by three NHS organisations – The Christie Hospital, University College London Hospitals and The Clatterbridge Cancer Centre.
-
It is provided as NAPC. The cost is identified in the general ledger (GL) for these organisations, as the GL value is separately reported to the NHS England highly specialised commissioning department and reimbursed outside other commissioner contracts.
-
For local costing purposes, you should bring the patient events for this service into the costing system and cost them using the resources listed in CP3.1. It will be similar to the staffing required for radiotherapy services, with different equipment.
-
Use Activity ID SLA164 Proton beam therapy.
CM28: Blood services
Scope
-
This standard applies to blood, blood factor products and immunotherapy blood products, including CAR-T cell therapy.
Overview
-
Blood services are a significant cost in some patient pathways. The emergency department (including major trauma) and theatres may use significant volumes of blood, and blood products are used to support patients with blood disorders such as haemophilia.
-
All blood units and blood products should be tracked to the patient for clinical safety, however in some areas – such as ED units – blood may be issued for general use. For example, ‘O-negative’ blood is used in emergency circumstances when the patient’s blood type is not known.
-
Blood and blood products will be provided to your trust by NHS Blood and Transplant. Once in the trust, the items require appropriate storage and issue to service teams, along with other regulatory duties. The blood service will manage the information about the issue to departments and onwards to individual patients, and they will also have information on wastage and expired items.
- High cost blood products are defined by the NHS Data Dictionary as ‘an expensive prescribed item and represents a disproportionate cost relative to the total cost of the relevant episode in terms of volume and cost’.
- A list of the items identified as ‘high cost’ are in the NHS Payment Scheme Annex A, tab 14b HC drugs, using the group called ‘Blood-related products’.
Approach
Information requirements
-
You should work with your informatics team and blood services manager to access sufficient blood and blood product tracking information for Feed 9: Blood and blood services. See IR1: Collecting information for costing and spreadsheet IR1.2.
-
Where blood is provided for general use and there is no patient identifier provided, you will need information on the use and cost of this blood to set up a RWV allocating across all patients in this service.
-
If specialist blood items or immunotherapy services are provided by an external party, your access to data may come from different sources but information at patient level used to support patient care and for clinical safety should still be available.
Specialist cost centres and expense codes
-
Use cost centre ID XXX053 Blood service and blood products. You may customise this cost centre to show different parts of the service if needed.
-
The blood service is usually managed in conjunction with the pathology department and the staff will include clinical scientists, medical laboratory scientific officer (MLSO) and scientific professional and technical staff.
-
You should refer to spreadsheet CP2.1 for the blood service specific expense codes.
-
Blood costs will be in the general ledger using prices from NHS Blood and Transplant. You should understand how the costs relate to the patient level feed values by working with the blood services leaders.
-
The cost of the blood management team should be allocated proportionally between the patients receiving the blood and blood products, and the infrastructure and governance of the blood service. You should work with the blood services manager to agree appropriate relative weight values.
Resources
-
Use the resources for blood service staffing as identified with the blood services team.
-
You should map blood service specific non-pay items to the resources in spreadsheet CP3.1 resource list.
-
For blood issued to departments such as emergency care where the patient is not identified, the cost can be allocated across all patients in the relevant department(s).
-
For the infrastructure and governance work – allocate to all patient events.
-
The costs on Feed 9: Blood and blood services, are used as relative weight values to allocate the costs in the cost ledger, in the same way as for medicines. Negative costs should be treated in the same way as negative costs for medicines and not used as part of the allocation calculation process.
Activities
-
For the management of blood services, the transfusion of blood and injection of clotting factors/other blood products using patient information use the activities listed in spreadsheet CP3.2 activities list.
-
For the blood and blood products themselves, use the activity SGA090 Consumption of high-cost blood and factor products.
-
For the high-cost blood products, the combination is with SGA090 Consumption of high-cost blood and factor products because these products are reported on the supporting information feed in the National Cost Collection.
Matching
-
Use the prescribed matching rules in spreadsheet CP4.1 to match costed blood and blood-related products to the correct patient event.
Other considerations
CAR-T cell therapy
-
Immunotherapy for cancer is a rapidly emerging area of blood-based treatments. The most advanced of the therapies is chimeric antigen receptor T-cell (CAR-T), which involves reprogramming a patient’s immune system to target their cancer. It is specifically developed for each patient, used only for certain cancers and is available in a limited number of NHS trusts.
-
Contacts with the patient for immunotherapy should be recorded and costed as NAPC or APC patient events as relevant: this is where the patient’s blood is taken, and after the laboratory has ‘trained’ the blood to fight the cancer cells, the CAR-T blood is given back to the patient.
-
Where the patient’s blood is sent to an external laboratory, use expense code 7024 Contracts: clinical – patient specific and Resource CLR030 Services received – clinical – patient level. Match this cost to the patient event where the blood is first infused back into the patient.
-
Use Activity SLA131: CAR-T therapy delivery for the preparation costs of the CAR-T blood and match this activity to the patient event at which the therapy is given using the rules in spreadsheet CP4.1.
-
If the preparation of the patient’s blood is in the trust laboratory, use the prescribed resources for the appropriate staff and non-pay. As the treatment is inherently associated with the patient, patient level information will be available, although the detail of preparation time and consumables may vary.
Blood testing for transfusions
-
Where the patient attends for blood testing in advance of a transfusion, this should be costed as non-admitted patient care for a phlebotomy test, using the Activity CLA059: Blood transfusion testing.
CM35: Education and training
Scope
-
This standard applies to the acute, community and mental health sectors.
-
All integrated providers should net off E&T income from expenditure for their submissions of both PLICS elements and aggregated costs as part of the mandated National Cost Collection (NCC).
Overview
-
NHS England is not collecting education and training (E&T) costs in 2023/24.
-
This guidance specifies the transitional method to be used in 2023/24 for netting off E&T income from patient care costs for the National Cost Collection (NCC) as the costs of E&T are not currently part of any mandated collection. This method supports the transition from the national reference costs to the PLICS collection.
-
This guidance describes a six-step method to allocate and net off E&T income at cost centre/expense code level, for the four categories of E&T income:
- tariff postgraduate medical
- tariff undergraduate medical
- tariff non-medical
- non-tariff.
-
Refer to the Healthcare education and training tariff guidance for details of the first three NHS Payment Scheme income categories and for a list of non-NHS Payment Scheme training programmes. Funding for these programmes is based on local agreements. Their associated activity is described in the learning and development agreements (LDAs) issued by Health Education England.
-
In the ‘Reconciliation’ in the NCC, income for all categories should be included in line 2: Other Operating Income.
-
You do not need to calculate 2023/24 E&T costs to be able to apply this transitional method. When the guidance states you should use E&T costs as a weighting, use your most recently submitted cost data adjusted for changes in subsequent years.
-
When allocating E&T income to the service area that supports the students, the cost for the number of students and trainees on courses in 2023/24 should be adjusted for significant changes to the previous year. For example, if the number of students and trainees falls between 2022/23 and 2023/24, adjust your E&T costs down by the same proportion.
-
E&T costs should be adjusted where more accurate internal information has been obtained or a more accurate costing exercise has been done since the 2022/23 National Cost Collection.
-
You will need to develop local relative weight values for areas of E&T income that were not covered in 2022/23 – for example, if your trust received funding to deliver a new training programme (specialty) in 2023/24.
Approach
-
The six-step approach to allocate and net off E&T income at cost centre/expense code level, for the four income categories listed above, is described below, and summarised in Figure CM35.1.
-
E&T income is netted off at cost centre/expense code level because E&T costs are not incurred treating patients, although both patient-facing and E&T activities share the same resources. Therefore, E&T income should not be allocated and netted off at healthcare resource group or patient level. Netting off needs to happen before the costing process calculations begin – that is, at the general ledger stage. This puts the correct cost quantum in the right place.
-
E&T income should be transparent in your cost ledger so the impact of this income on the cost of patient care can be viewed locally
Figure CM35.1: Transitional method to net off E&T income
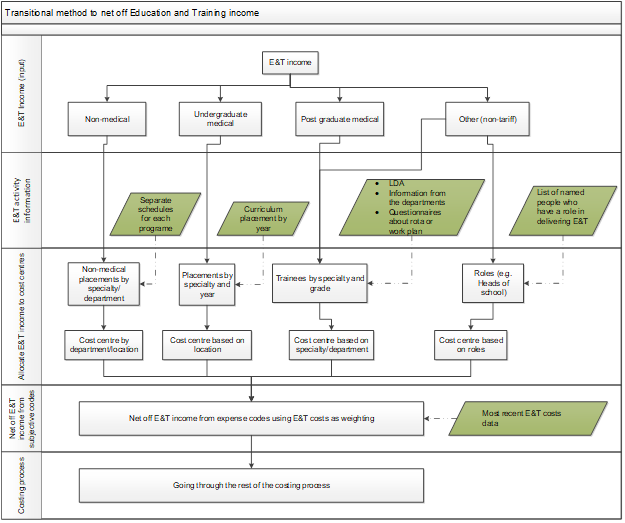
Figure CM35.1 describes the transitional method to net off E&T income following steps 1 to 4 as outlined below.
-
The four areas of E&T income are netted off, following steps 1 to 4 in any order, and the remaining cost processed as specified in standards CP1 to CP5.
Step 1: Allocate and net off non-medical income
You need to obtain the following information:
- activity and cost information:
- separate schedules for each programme
- E&T cost information at cost centre/expense code level
- income information:
- E&T income for non-medical students or trainees by schedule for each programme.
To allocate and net off the income you need to:
- allocate E&T income for NHS Payment Scheme category: non-medical to courses (departments), location or clinical pathway based on the programme schedules
- allocate the E&T income to cost centres by course or location
- allocate the income by cost centre to expense codes weighted by E&T costs
- net off the income from the cost centre/expense codes.
Step 2: Allocate and net off undergraduate medical income
You need to obtain the following information:
- activity and cost information:
- length of undergraduate medical student placement in weeks by curriculum placement year and specialty
- placement location
- E&T cost information at cost centre/expense code level
- income information:
- E&T income for undergraduate medical students.
To allocate and net off the income you need to:
- allocate E&T income by NHS Payment Scheme category: undergraduate medical to specialties (departments) by length of placement in weeks
- allocate the income to cost centres based on specialty or placement location
- allocate the income by cost centre to expense codes weighted by E&T costs
- net off the income from the cost centre/expense codes.
Step 3: Allocate and net off postgraduate medical income
You need to obtain the following information:
- activity and cost information:
- number of funded whole time equivalents (WTE) for postgraduate medical trainees by:
- course (department)
- grade
- E&T cost information at cost centre/expense code level
- deanery post schedules
- finance schedules
- income information:
- postgraduate medical E&T NHS Payment Scheme income
- NHS Payment Scheme basic salary contribution for postgraduate medical trainees
To allocate and net off the income:
- for the group 1 income group you need to:
- allocate E&T income for postgraduate medical trainees to courses (departments) weighted by the number of WTE for postgraduate medical trainees
- allocate the income to cost centres by course
- allocate the income by cost centre to expense codes weighted by E&T costs
- net off the income from the cost centre/expense codes
- allocate basic salary contribution income by trainee grade to courses (departments) weighted by the number of funded WTEs
- for the group 2 income group you need to:
- allocate the income to cost centres by course
- net off the income from the expense codes for postgraduate medical trainees’ salaries.
Step 4: Allocate and net off non-NHS Payment Scheme income
You need to obtain the following information:
- Activity and cost information:
- separate schedules for each programme
- list of named people and their specific E&T roles
- E&T cost information at cost centre/expense code level
- income information: non-tariff E&T income for undergraduate medical programmes, postgraduate medical programmes, non-medical programmes, and other regional programmes.
To allocate and net off the income you need to:
- allocate non-tariff E&T income to roles (for example heads of school) based on the schedules for each programme
- allocate non-tariff non-medical postgraduate and undergraduate medical income by following the approaches specified in steps 1, 2 and 3 respectively
- allocate E&T income for each role to cost centres and net off from the expense codes for the salaries.
Step 5: Allocate E&T specific support costs
After netting off the E&T income, some type 1 support costs that relate to E&T may still sit in your ledger – for example, library costs. If these support costs are shared between E&T and non-E&T services:
- use local judgement to categorise these support cost centres as E&T or non-E&T based on materiality; that is, if the costs in a cost centre are materially E&T support costs, categorise the cost centre as an E&T-specific support cost centre
- for those costs that are not dominantly for E&T or non-E&T services, use locally developed relative weight values to apportion them to:
- E&T-specific support costs
- non-E&T support costs.
Use locally developed relative weight values to apportion the E&T-specific support costs (either as an E&T-specific support cost centre or as an E&T-specific expense line) to:
- tariff-funded postgraduate medical E&T programmes
- tariff-funded undergraduate medical E&T programmes
- tariff-funded non-medical E&T programmes
- non-tariff programmes.
Follow the allocation methods specified in spreadsheet CP2.2 to allocate the E&T-specific support costs to relevant patient-facing and type 2 support cost centres.
Step 6: Netted off costs go through the costing process
Check the output from the five steps above – that is, all four categories of E&T income netted off at cost centre/expense code level – and adjust the output to ensure this process does not generate negative balances at the resource level (see spreadsheet CP3.1 for prescribed resources).
Put the checked output through the costing process prescribed by the healthcare costing standards for England and National Cost Collection guidance.
CM36: Specialist rehabilitation
Scope
-
This standard applies to inpatient specialist rehabilitation activity provided by the trust and defined as levels 1 and 2 by the United Kingdom Rehabilitation Outcome Collaborative (UK ROC) and level 3 and community specialist rehabilitation:
- level 1 services: complex specialised rehabilitation including hyperacute rehabilitation
- level 2 services: local specialist rehabilitation centres
- rehabilitation outreach from services at levels 1 and 2
- level 3 rehabilitation centres
- patients receiving specialist rehabilitation on a general ward
- outpatient rehabilitation assessments
- community rehabilitation.
-
The standard also applies to spinal cord injury rehabilitation for the eight national centres, and specialised burn care, pain management and brain injury.
Overview
-
Rehabilitation is a process of assessment, treatment and management by which the individual (and their family/carers) are supported to achieve their maximum potential for physical, cognitive, social and psychological function, participation in society and quality of living.
-
Patient goals for rehabilitation vary according to the recovery trajectory and stage of their condition.
-
Specialist rehabilitation is delivered by a multiprofessional team with recognised specialist training in rehabilitation, led or supported by a consultant trained and accredited in rehabilitation medicine or neuropsychiatry in the case of cognitive/behavioural rehabilitation. Services are identified based on complexity of their caseload.
-
For costing levels 1 and 2 specialist rehabilitation, we use the UK ROC levels of specialisation and the patients reported on the SCI database.
Rehabilitation: UK ROC
-
In the national clinical registry UK, most rehabilitation is categorised in levels by UK ROC as follows:
- Level 1 sub-divided into:
- level 1a: for patients with high physical dependency
- level 1b: mixed dependency
- level 1c: mainly walking wounded patients with cognitive/behavioural disabilities.
High cost/low volume services that provide for patients with highly complex rehabilitation needs that are beyond the scope of their local and district specialist services. These are normally provided in co-ordinated service networks planned over a regional population of 1 to 5 million covered by the D02 service specification.
As well as admitted patient care, level 1 services provide specialised outreach support for patients with complex needs.
- Level 2 subdivided into:
- level 2a: supra-district catchment
- level 2b: localised catchment
- hyper-acute specialist rehabilitation services: Units sited within acute care settings that take patients at a very early stage in the rehabilitation pathway when they still have medical and surgical needs requiring continued active support from the trauma, neuroscience or acute medical services.
Typically planned over a district-level population of 350K to 1 million and led or supported by a consultant trained and accredited in rehabilitation medicine, working in both hospital and community settings. The specialist multidisciplinary rehabilitation team provides advice and support for local general rehabilitation teams.
- Level 3
Local specialist rehabilitation teams providing general multiprofessional rehabilitation and therapy support for a range of conditions within the context of acute services (including stroke units), intermediate care or community services.
-
The UK ROC D02 service specification for services at levels 1 and 2 includes four programmes of care:
- Restorative rehabilitation
- Complex disability management
- PDOC evaluation and management
- Neuropalliative rehabilitation (including end of life care for patients dying with unsurvivable injuries.
-
To be defined as a level 1 or level 2 service a rehabilitation service should be:
- led or supported by a consultant trained and accredited in either rehabilitation medicine or neuropsychiatry.
- registered with and reporting data to UK ROC.
-
Specialist rehabilitation data for levels 1 and 2a services centres is submitted to UK ROC fortnightly in line with the requirements of the NHS England D02 contract. Level 2b services are not contracted to submit data for level 2b for commissioning purposes; however, units are required to submit data to UK ROC to meet the requirement of being banded a level 2b centre.
Rehabilitation complexity scale – extended (RCS-E v13)
-
Assessing the complexity of rehabilitation needs of a patient presents a challenge; however the rehabilitation complexity scale (RCS-E) provides a simple measure of the complexity of rehabilitation needs, covering basic care, specialist nursing, therapy and medical interventions and equipment.
-
There are five UK ROC weighted bands and an initial RCS-E score between 0 and 22 is applied by the patient’s multidisciplinary team. The scores and bands are shown in Table 36.1 and Table 36.2.
-
Different staff groups then calculate banding weightings using the Northwick Park Hospital Nursing Dependency Score and Northwick Park Therapy Dependency Assessment in a weighted bed day model. The weighted scores are used in the reporting of specialist rehabilitation costs.
Table 36.1: UK ROC RCS-E scoring mechanism
|
Category |
Scoring range |
|
Basic care |
0-4 |
|
Specialist nursing needs |
0-4 |
|
Therapy disciplines |
0-4 |
|
Therapy intensity |
0-4 |
|
Medical needs |
0-4 |
|
Equipment |
0-2 |
|
Total patient RCS-E |
0-22 |
Table 36.2: UK ROC weighted bands with scoring
| RCS-E band name | Scoring level |
|
Very high |
15-22 |
|
High |
11-14 |
|
Medium |
08-10 |
|
Low |
05-07 |
|
Very low |
00-04 |
-
The RCS-E is used for planning; for example, to ensure the unit has enough resource to meet the complex needs of the patients. The RCS-E score may both increase and decrease during care on the specialist rehabilitation unit.
-
It is reviewed fortnightly for each specialist rehabilitation patient, recorded at patient level and submitted to UK ROC. It does not form part of the commissioning dataset or hospital episode statistics; therefore, you should obtain this data from your rehabilitation unit.
Rehabilitation: specialist spinal cord injury
-
Spinal cord injury (SCI) is an insult to the spinal cord at any level resulting in a change, either temporary or permanent in the normal motor, sensory or autonomic function of the cord.
-
National spinal cord injury services include the services provided by the eight designated specialist spinal cord injury centres in England for adults, young people and children who have sustained a non-progressive injury to the spinal cord or cauda equina. The eight centres are: The Golden Jubilee North East Regional Spinal Injuries Centre, The London Spinal Cord Injury Centre, The Yorkshire Regional Spinal Injuries Centre, Princess Royal Spinal Injuries Centre, North West Regional Spinal Injuries Centre, Midlands Centre for Spinal Injuries, Duke of Cornwall Spinal Treatment Centre, and the National Spinal Injuries Centre.
-
The national spinal cord injury services do not submit information to UK ROC, rather they submit to the national spinal cord injury database using the three categories:
- high tetraplegic
- low tetraplegic.
-
There may be some overlap between patients submitted to UK ROC and the national database on spinal cord injury. Where an RCS-E score exists, this should supersede the fact the patient has a spinal cord injury.
-
Only the eight spinal cord injury centres should record patients under treatment function code (TFC) 323.
Approach
Information requirements
-
The data for level 1 and level 2 rehabilitation activity will come from the relevant admitted patient care (APC) dataset described in IR1: Collecting information for costing for Feed 1a: APC.
-
You will also need the RCS-E and RCS-E scoring date from the specialist rehabilitation unit for Feed 25a: Specialist Rehabilitation. The RCS-E scoring dates are used to construct the RCS-E period – which is usually two weeks – with the start of each period marked by an assessment score.
-
Patients who do not qualify for a UK ROC RCS-E score should be treated as non-specialist rehabilitation patients (see Activities below).
-
If you are a spinal cord injury centre, you will need to obtain data from the spinal cord injury rehabilitation unit so the four categories can be included in Feed 25b: Specialist spinal cord injury rehabilitation. The categories do not form part of the commissioning dataset (CDS) or Hospital Episode Statistics (HES).
-
These national datasets may undergo data cleansing, and the data may be sent back to the provider with the expectation the cleansing is repeated in the local system. You should understand if that has been done, so that your activity reconciliation includes whether data you are using for costing is the same as held in the UK ROC and national spinal cord injury dataset.
-
For level 3 and community the data for rehabilitation activity will come from Feed 1a: Admitted Patient Care as described in IR1: Collecting information for costing and spreadsheet IR1.2. Patients can be identified by TFC 314 Rehabilitation. There is no requirement to obtain additional data from your rehabilitation team as level 3 services are not required to submit data to UK ROC at this stage.
Specialist rehabilitation patients on a general ward
-
Not all NHS trusts have a designated specialist rehabilitation unit. Some patients will be given specialist rehabilitation while their care remains on an acute ward.
-
You should obtain Feed 7: Supporting contacts to identify staff working with specific patients on the rehabilitation unit and patients receiving specialist rehabilitation outreach services on a non-specialist rehabilitation ward. Where this information is available, it avoids the need to use relative weight values (RWVs) as it relates to actual patient-level resource received in more detail than an acuity RWV. (See Activities below.)
-
Patient events in this category will generate two HRGs and two lengths of stay – one for the core episode and one for the rehabilitation element of that episode. Costs may be attributable both core episode and rehabilitation element.
-
If the whole episode of care is within the rehabilitation area, all the cost should be in the rehabilitation HRG, leaving a core HRG with a zero cost.
Follow up contacts and non-admitted patient care contacts
-
In many cases, medical and nursing staff will have follow-up contacts with the patient after they have left the hospital to support the ongoing after care. Some trusts will also have outpatient assessment appointments.
-
Both types of patient event should be brought into the costing system on Feed 3a Non-admitted patient care (NAPC) as shown in spreadsheet IR1.2.
Community rehabilitation
-
Community rehabilitation should be brought into the costing system on Feed 3c NAPC (community) as shown in spreadsheet IR1.2.
Specific cost centres and expense codes
-
Specialist rehabilitation cost centres and expense codes can be found in spreadsheet CP2.1 standardised cost ledger.
-
The cost centres can be customised in your local cost ledger if you have different discrete cost centres for each of the different types of specialist rehabilitation/SCI ward.
-
You should work with your service/clinical leads to understand the costs.
-
Use expense codes appropriate for the staff type and band. You may need to disaggregate the costs of staff covering more than one unit or service area to ensure the correct resource is applied.
-
The cost of most non-pay items will not be material in the delivery of a specialist rehabilitation unit; therefore, allocate according to the methods shown in spreadsheet CP3.3 and using CM21: Clinical non pay items.
Resources
-
You should use the resources shown in spreadsheet CP2.1.
-
Specialist rehabilitation medical, nursing and therapy staff should be allocated across all patients in the unit or ward they work on.
-
You should use CM1: Medical staffing to allocate medical staff including junior doctor costs based on job plans, rotas or through discussion with clinicians and managers, at the patient level.
Activities
-
You need to identify what specialist rehabilitation activities your trust delivers and map these to the prescribed activity list in spreadsheet CP3.2.
- SLA173 Specialist rehabilitation ward care: to apply the medical and nursing weighted RCS-E score
- THA001 Therapies supporting contact: for showing the therapies staff input at patient level (where information is available)
- SLA167 Specialist rehabilitation supporting contacts: for showing the medical and specialist nursing staff input at patient level (where information is available). Includes specialist rehabilitation input to patients on a non-specialist rehabilitation ward (outreach)
- SLA174 Rehabilitation therapists care on a specialist rehabilitation ward: to apply the weighted RCS score by band name
- SLA 135 Outpatient care: where specialist rehabilitation professionals have clinic appointments for a discharged patient who has been in the unit.
- SLA097 Ward care: this should only be used where the ward does not submit data to UK ROC and so has no RCS-E score: for example level 3 rehabilitation
- CMA309 Community rehabilitation care.
-
The sections below specify how to allocate costs to rehabilitation episode, mini episodes or bed days where patient acuity/complexity has a material impact on cost. Any pay costs not described here should be costed according to the methods shown in spreadsheet CP3.3.
Patient-level weighting
-
The specialist rehabilitation unit staff will not (all) have their time recorded in this way, so the RCS-E for the patient should be used as a weighting.
Consultant medical staff and rehabilitation unit nursing staff
-
Specialist rehabilitation medical and nursing staff should be allocated across all patients in the unit they work in, based on the full RCS-E weighting. Examples by patient are shown in Table 36.3.
Table 36.3: Examples of how RCS-E totals are used to apply weightings to patients for medical staff and nursing
|
Category |
Scoring range |
Patient A |
Patient B |
Patient C |
|
Basic care |
0-4 |
1 |
3 |
2 |
|
Specialist nursing needs |
0-4 |
1 |
2 |
2 |
|
Therapy disciplines |
0-4 |
3 |
4 |
2 |
|
Therapy intensity |
0-4 |
3 |
3 |
2 |
|
Medical needs |
0-4 |
2 |
4 |
1 |
|
Equipment |
0-2 |
1 |
2 |
1 |
|
Total patient RCS-E |
0-22 |
|
|
|
|
Score (sum of the patient scores) |
39 |
11 |
18 |
10 |
|
Ratio (sum of weightings) |
|
=11/39 |
=18/39 |
=10/39 |
|
Share of cost |
£50,000 |
=(11/39)*50,000 |
=(11/39)*50,000 |
=(11/39)*50,000 |
|
Allocated cost |
|
£14,103 |
£23,077 |
£12,821 |
-
The weighting should only be applied to the staff where whole time equivalents are dedicated to the specialist rehabilitation services.
-
The acuity weighting should be applied per rehabilitation complexity RCS-E period using the date the RCS-E was scored for each day on the ward, until the next score is done.
Therapy and clinical support staff
-
Rehabilitation therapists include the following disciplines:
- physiotherapists
- occupational therapists
- speech and language therapists
- psychologists
- social workers
- dieticians
- orthotics
- rehabilitation assistants
- rehabilitation technicians
- others, such as music therapists, art therapists, activities coordinators.
-
Rehabilitation therapists have a weighting based on the band of the RCS-E score and the level of ward, and not the total score. The cost should be allocated across all patients in the unit, based on the weightings shown in Table 36.4 for each rehabilitation complexity RCS-E period.
Table 36. 4Weighting by level and RCS-E band name
|
RCS-E band name |
Level 1 weighting |
Level 2 weighting |
|
Very high |
2.053 |
1.813 |
|
High |
1.620 |
1.454 |
|
Medium |
1.000 |
1.000 |
|
Low |
0.822 |
0.801 |
|
Very low |
0.547 |
0.706 |
-
In levels 1 and 2 units, hours of therapy provision will form a significant part of the total cost of rehabilitation. There is a difference between therapy care on general wards and therapy care on specialised rehabilitation wards.
-
On general wards, the therapist input is more routine with generic contacts equating to more of the therapy service delivered whereas in specialist rehabilitation units the therapists deliver rehabilitation programmes as part of a multidisciplinary team and generic contacts form a much smaller proportion.
-
Where you have a superior patient data feed for therapy contacts, you can use this data to allocate costs to direct therapy contacts in your rehabilitation unit but all costs for therapy in rehabilitation should not be allocated solely on the information in the therapy feed.
-
You should work with your service to split rehabilitation costs between direct contacts (allocated using therapy contacts) and indirect patient care which should be allocated to patients using the banding factor shown in Table 36.5.
-
This is the preferred method of cost allocation as it provides a more accurate patient level cost. However, where you do not have a patient data feed for therapy contacts you can use the banding factor shown in Table 36.4 to allocate all therapy costs.
Patients in a level 1 or level 2 unit without an RCS-E score
-
Where a patient has recently moved into a level 1 or level 2 unit, they may not have received a first score before the end of the costing period. You should assume a mid-range score in these instances.
Patients not in a UK ROC-defined specialist rehabilitation unit
-
Patients not in a UK ROC-defined specialist rehabilitation unit will not have an RCS-E score and should use the Activity SLA097: Ward care, even if the TFC is 314 Rehabilitation.
-
You can allocate medical, nursing and therapy staff costs at the patient level to these patients, using available information on the length of time spent with the patient on Feed 7: Supporting contacts.
Spinal cord injury
-
The level of complexity of patient needs is detailed in the spinal cord injury database and shows if the patient falls into one of the four categories:
- tetraplegic
- paraplegic
- central cord syndrome
- cauda equina.
-
You should work with the service team to set relative weight values to represent the different resource intensity.
-
Patients recorded on the spinal cord injuries database as ventilated or noted with pressure ulcers will also require additional weighting to reflect additional resource intensity.
-
Paediatric spinal cord injury patients under the age of 12 will not be assigned a level of injury; therefore, a different weighting can be locally applied to the patient event.
Matching
-
Costs such as pathology, diagnostic imaging and other clinical support services will also be incurred in specialist rehabilitation care. These will be costed as part of the department that provides the service and will then be matched to the patient in the rehabilitation area.
-
Examples include Feed 8: Pathology feed, Feed 7: Supporting contacts and Feed 12: Diagnostic imaging. Feed 8 is a superior costing method.
-
Use the prescribed matching rules in the integrated technical document in spreadsheet CP4.1 to ensure the activity and costs on auxiliary feeds are matched to the correct specialist rehabilitation patient bed day.
-
You should match the costs from auxiliary feeds to the specialist rehabilitation episode.
Other considerations
Outreach
-
Rehabilitation outreach contacts support clinical staff in managing patients who may require admittance to a level 1 or level 2 unit. This could be for a patient in the community, from another specialty within the trust or from another trust. The primary duty of the outreach team is to screen patients before admittance into the specialist unit where signposting to other services may be beneficial.
-
These patients will not be recorded on the Commissioning Data Set as a rehabilitation episode as they will remain under the care of the medical or surgical consultant rather than the rehabilitation consultant. The cost of the specialist rehabilitation outreach team should be included as a component of the episode.
-
Feed 7: Supporting contacts should include information on the rehabilitation outreach team activity and this can be matched to the patient event.
-
Agree a local allocation method with the rehabilitation outreach lead if Feed 7 Supporting contacts is not available for this service.
Complex paediatric rehabilitation
-
Patients aged 16 or 17 do not get an RCS-E score even if they are in a discrete level 1 or 2 adult rehabilitation unit. They should be costed in the same way as adult specialist rehabilitation, using a mid-range weighting for the RCS-E.
Patients involved in research studies
-
If you can identify the costs associated with research and development for individual patients, allocate them to those patients using activity SPA 155 Research and development. If not, continue with your current method and document it in ICAL worksheet 20: Research and development.
CM37: Renal dialysis
Scope
-
This standard applies to all renal dialysis services whether provided in a renal specialist or non-specialist centre.
-
It includes renal dialysis for all ages.
-
It does not apply to renal transplant. See CM5: Theatres and special procedures suites and CM13: Admitted patient care.
Overview
-
Renal dialysis is a clinical procedure that filters waste products from blood. The main conditions treated are chronic kidney disease (CKD) or acute kidney injury (AKI) which has prevented the kidneys functioning correctly.
-
CKD is a long-term condition usually caused by damage to the kidneys from other conditions, most commonly diabetes and high blood pressure.
-
No cure exists for CKD, although treatment can slow or halt its progression and prevent other associated serious conditions. Many patients can be managed in primary care but if the disease progresses to kidney failure or end-stage kidney disease, patients may need dialysis or a kidney transplant.
-
AKI is where the kidneys suddenly stop working properly. It can range from minor loss of kidney function to complete kidney failure. The kidney function deteriorates very quickly, often as a complication of another serious illness. Patients with AKI may also receive dialysis.
-
All renal dialysis is provided in a specialist area in a hospital, satellite centre (a community hospital, GP surgery or separate building) or a specially prepared room at home. Patients (such as those with AKI) may also have dialysis while admitted to hospital (for example to an intensive care unit or renal ward) for a longer episode.
-
The care pathway varies according to type of treatment and trust. There are two types of renal dialysis:
- Haemodialysis which diverts blood into an external machine, where it is filtered before being returned to the body. Most patients have three sessions per week with each treatment lasting about four hours. Patients at home may have more than three sessions a week. It can be given in an acute hospital, a satellite unit or at the patient’s home.
- Peritoneal dialysis which takes place at home and pumps dialysis fluid (dialysate) into the space in the abdomen (peritoneal cavity) to draw out waste products from the blood passing through the vessels lining the abdomen, and then drains this fluid from the abdomen. There are two types:
- continuous ambulatory peritoneal dialysis (CAPD): four bag exchanges a day, seven days a week is usual
- automated peritoneal dialysis (APD): a machine filters a patient’s blood at night while they sleep; a variation is assisted APD, where a healthcare professional goes into the patient’s home to help them set this up (often necessary because of the size of the bags).
-
People may switch between treatment types (most likely from peritoneal to haemodialysis).
Approach
Information requirements
-
Discuss with clinical and service leads how the data is recorded locally, and how it will be available for the patient-level costing process. You should also discuss whether the data source for children and young people differs from that for adults.
-
You should bring Feed 30: Renal dialysis into the costing system using the source information submitted to the national renal dataset or the UK Renal Registry dataset.
-
Most renal dialysis will be an episode of one day.
-
Renal dialysis should be reported using the HRG in the LD and LE subchapters.
-
If the patient was admitted specifically for renal dialysis, they will have a core HRG code and multiple HRG codes from the LD subchapter.
-
If the patient attends solely for renal dialysis, there is no requirement to cost the core HRG of LA97A or LA97B.
-
If the patient was admitted for a reason other than dialysis, but during that episode the patient requires dialysis, they will have a HRG code from the LE subchapter and an additional HRG for their original admission reason.
-
If a patient has renal dialysis during an episode that lasts for more than one day, each intervention for dialysis will be costed as though it were a separate admission.
-
Different types of renal dialysis have different currencies and methods of counting. See Table 37.1.
Table CM37.1: Currency and method of counting
|
Dialysis type |
Renal service terminology |
Costing patient event terminology |
|
Acute kidney disease |
Per session |
Per episode |
|
Peritoneal dialysis |
Per day |
Per episode |
|
Home haemodialysis |
By week |
Per contact |
-
Proxy patient events may need to be created in the costing system to allocate the costs where activity information is not available for satellite or home patients.
-
Some haemodialysis patients go on holiday and continue their dialysis in a trust local to their holiday location. The trust providing the dialysis must identify patients seen away from their normal base (host trust). The dialysis should be costed where it is performed. The host trust may keep a record of the dialysis but this should not be costed.
Specific cost centres and expense codes
-
The cost centres for renal dialysis are in spreadsheet CP2.1.
-
They can be customised in your local cost ledger if you have discrete cost centres for each of the renal dialysis service areas.
-
Use expense codes appropriate for the staff type and band. You may need to disaggregate the costs of staff covering more than one unit or service area, to ensure the correct resource is applied:
- Medical staff may undertake sessions at main hospital and satellite sites and attend clinical multidisciplinary team meetings (MDT).
- Anaesthetic medical staff may be required at times to insert lines.
- To allocate the costs of specialist nurses, use timetables to allocate costs between outpatients, inpatients and the administration of dialysis itself, including by treatment type. You may need to ask what the average nursing input is for each type of dialysis, to determine this allocation by treatment type. Most organisations have nurses who visit patients on home dialysis. Establish the frequency of these visits and allocate the costs accordingly.
- Dialysis patients require discussion at a clinical MDT meeting. This may include but is not limited to dieticians, specialist pharmacists, social workers, psychologists and counsellors. You should discuss with the team the frequency and participants with the service and allocate the cost of relevant staff according.
-
Considerable capital costs are involved in renal dialysis, for example the cost of the dialysis machines and the cost of a water treatment plant at the main hospital site. However, the capital value should not be included in the cost of the patient dialysis.
-
Revenue costs for this equipment should be included in the cost of patient care including:
- consumable items
- maintenance costs.
-
Use the process described in CM21: Clinical non-pay items to cost medical and surgical equipment. Material items should be allocated to patients using Feed 15: Prostheses and other high-cost items.
-
For patients receiving dialysis at home, there may be revenue conversion costs, including nursing assessments, electricity and water supply, and drainage facilities. These costs should be included in the cost of home haemodialysis. Patients dialysed at home may be reimbursed for their raised utility bills.
-
The renal department will keep track of the supplies ordered for each patient having home dialysis, so patient level costs for material items, consumables and fluids should be available.
-
Be aware the consumables delivered to satellite units may have been ordered by a central unit (for example main hospital). These costs will need disaggregating between the units supplied.
-
The department will monitor maintenance and repair costs for the dialysis machines and other equipment, so you can use this information to inform the development of relative weight values.
-
A patient on home dialysis uses a single machine whereas in a centre, machines are usually shared and the running costs should be apportioned appropriately. Some hospital site patients require single or dialysis group specific use machines for infection control.
-
Where the independent sector is used, both pay and non-pay costs may be covered by the charge to the NHS provider. This should be established with the service and allocated to the patient event is recorded for clinical purposes.
-
Specialist expense codes for renal dialysis are include in the renal cost centres on spreadsheet CP2.1, and the costs should be allocated to all patients having renal dialysis, including:
- 7109 UK Renal Registry – Software Fee
- 7112 UK Renal Registry – Mandatory Capitation Fee: for all dialysis patients is payable to the UK Renal Registry.
Resources
-
Renal dialysis can involve a wide range of healthcare professional resources. You should map the cost to the appropriate resource for the type of staff using spreadsheet CP3.1 resource list.
Activities
-
You need to identify what renal activity your trust delivers and map this to the prescribed activity list in spreadsheet CP3.2.
Matching
-
Medicines costs should be matched to the correct patients using Feed 10: Medicines dispensed. Any non-patient-identifiable medicine costs used on the dialysis unit are allocated using the allocation methods in spreadsheet CP3.3.
-
Use the prescribed matching rules in the integrated technical document in spreadsheet CP4.1 to ensure the activity and costs on auxiliary feeds are matched to the correct renal patient.
-
Some medicines used for dialysis are high-cost drugs, such as erythropoiesis stimulating agents. You can use the mandated monthly dataset for NHS England’s specialised commissioning on high cost drugs to help you allocate these costs to the correct patients.
Other considerations
Dialysis facilities in critical care or on wards
-
You can use the UK Renal Registry to identify patients who received dialysis outside the renal dialysis specific units, either by directly identifying the patient or by cross-matching with ward data. Then allocate the costs to those patients using the renal dialysis activities shown above.
Patient travel
-
Patient travel to dialysis has been identified as a significant cost to providers; therefore, clear information about this is helpful. Include patient transport costs in renal dialysis patient events using expense code 7286 Patients travel exp/allowances and overhead ID: T1S405; Patient transport. This will allow patient events to be reviewed with or without the patient transport element at local level.
Patients involved in research studies
-
If you can identify the costs associated with research and development for individual patients, allocate them to those patients using activity SPA155: Research and development. If not, continue with your current method and document it in ICAL worksheet 20: Research and development.
Hub-and-spoke configuration
-
For dialysis provided by a hub-and-spoke configuration, the activity and costs should be recorded in the NHS provider contractually responsible for delivering the care, whether this is the hub or the spoke. See CM8: Clinical and commercial services supplied or received.
CM38: Specialist palliative medicine
Scope
-
This standard applies to specialist palliative medicine (SPM) activity provided by the trust and includes:
- inpatient hospice units and SPM wards
- inpatient hospital palliative care support provided on other wards (hospital SPM team)
- day care
- outpatients
- community specialist palliative medicine (including ‘hospice at home’ services).
Overview
-
Specialist palliative medicine encompasses end of life care provided in both hospital and home settings, as well as a range of other specialist care, advice and support, such as that provided by hospital SPM teams.
-
For admitted patients, costs are incurred each day the patient is admitted. The costing process should apply costs to the patient record showing the date(s) the costs were incurred, so a timeline of costs can be viewed locally. For the National Cost Collection, the cost of each bed day will be aggregated to the episode.
-
For SPM admitted patient care (APC), the patient event is the episode which will have the currency of an HRG. There is no requirement to cost the core HRG if the patient episode is under TFC 315 Palliative medicine service or TFC 240 Paediatric palliative medicine service.
-
The periods when hospice or SPM ward patients are receiving specialist palliative medicine are referred to as APC episodes regardless of whether they are short term, long term or residential. One care professional will be clinically named responsible for the ‘episode’, even if they work as part of a team.
-
Within an APC episode, the patient will incur costs from the care given by a range of staff, the use of consumables (including medicines) and ward overheads, such as ward clerk costs. You should refer to CM13: Admitted patient care for detail on costing admitted patient episodes.
-
Where a patient is on an acute ward and receives acute treatment alongside SPM support from the hospital palliative medicine team, the SPM support should be costed using the specific activity code and shown as a component of the acute episode.
-
Where patients attend SPM outpatient clinics, have SPM day care or SPM in their home, you should follow CM3: Non admitted patient care.
Approach
Information requirements
-
For admitted patients the SPM episodes should use TFC 315 Palliative medicine service or TFC 240 Paediatric palliative medicine service from the source used for the Commissioning Data Set (CDS). They will be included in Feed 1a: Admitted patient care, using the HRG code generated by the grouper. No SD subchapter HRG is required for this episode.
-
Providers should ensure:
- their clinical coding is sufficient to enable the appropriate HRGs to be created
- all patients moved to a SPM ward or separate hospice have a new episode created under TFC 315 or TFC 240.
-
Outpatient clinics should be included in Feed 3a: Non admitted patient care.
-
For hospital SPM teams, an internal data source will be required from the service team to load into the costing system as Feed 7: Supporting contacts.
-
Community SPM team activity will be available in either the CDS as non-admitted patient care (NAPC) which has an activity location of the patient’s home (or other location), or in the Community Services Data Set (CSDS) under the service or team type referred to as 07 Palliative care. Where the data is in the CDS, use Feed 3a: Non-admitted patient care. Where the data is in the CSDS, use Feed 3c: Non-admitted patient care (community).
-
There is further information on these data elements in IR1: Collecting information for costing and spreadsheet IR1.2.
Specific cost centres and expense codes
-
The SPM cost centre in spreadsheet CP2.1 is: XXX630 Palliative/respite medicine.
-
You should refer to the codes in spreadsheet CP2.1 Standardised cost ledger for SPM wards and hospices to show the different discrete costs centres.
-
Allocate staff according to the work they do, disaggregating the costs where staff work across more than one care location.
Resources
-
Allocate pay costs using spreadsheet CP3.1 resource list.
-
The unit cost of the consumables used in specialist palliative medicine may be negligible but if they are material, per patient or in total, please refer to CM21: Clinical non-pay items.
Activities
-
You need to identify what SPM activity your trust delivers and map this to the prescribed activity list in spreadsheet CP3.2.
Matching
-
Costs such as pathology, therapies, diagnostic imaging and other clinical support services will also be incurred in specialist palliative medicine. Use the appropriate auxiliary feed to match these costed activities to the patient event.
-
The hospital SPM teamwork will be shown as a component part of non-SPM episodes, therefore Feed 7: Supporting contacts is a prescribed feed for specialist palliative medicine.
Other considerations
-
Bereavement counselling should only be included as a separate cost in specialist palliative medicine in the unusual circumstance it is provided directly to the patient or, where the patient is a child or vulnerable adult, to the carer as a proxy. In all other situations, it should be treated as a support cost.

