Introduction
This guidance was amended on 9 April 2024 to correct a link in paragraph 286, 22 April 2024 to correct a link and add codes in paragraph 280, and 23 April 2024 to correct codes in paragraph 472.
-
This guidance contains National Cost Collection (NCC) reconciliation and submission information for the acute, mental health, Talking Therapies for Anxiety and Depression and community sectors. NCC guidance for the ambulance sector is available separately. Note that Talking Therapies was previously called IAPT and the data feed on the extract specification that trusts will submit will still be called IAPT for 2024 NCC.
-
Supporting information is on our FutureNHS workspace. You can access FutureNHS if you have an NHS email address or email costing@england.nhs.uk to request access if you do not, using the subject line ‘FutureNHS’.
Reconciliation and exclusions: how to obtain and record your cost quantum
Introduction
Purpose and context
-
The National Cost Collection (NCC) collects data about the costs of patient care in the NHS. This means only costs that relate to the ongoing running costs of your trust and not those that are one off.
-
Some of the costs your trust incurs are not collected, for example:
- caring for another NHS provider’s patients
- caring for non-NHS patients
- services which are funded by non-NHS bodies such as the local authority
- services for which there is no requirement to understand the costs or for which it is not possible to collect the cost
-
There are also certain types of income that offset the cost of patient care.
-
Therefore, you are required to reconcile your trust’s audited year-end accounts and the costs your trust submits in the NCC cost quantum because otherwise they will differ.
-
Completion of the reconciliation must be completed before preparing patient-level costs (PLICS) XML files to obtain your NCC cost quantum. You should not try to work backwards from your submission files to create your NCC cost quantum. Use your draft final accounts to start to prepare this reconciliation.
-
Reconciliation to your trust’s audited year-end accounts is important for assuring the quality of costing outputs. You need to understand how your trust’s cost quantum is derived from these accounts, to ensure that your cost model includes all costs and produces reliable and comparable results. As some of your trust’s audited accounts are not part of its cost quantum, a reconciliation is needed to establish the links between the two. The information included in your reconciliation is published as part of the NCC publication.
-
This section describes the reconciliation process for cost data submitted in all National Cost Collections, whether patient-level information and costing system (PLICS) or aggregate costs. It is supported by Standard CP5: Reconciliation.
Cost reconciliation
-
The reconciliation feed type in the extract specification enables you to submit the information from your trust’s audited financial accounts and any adjustments required to your total cost quantum.
-
The feed name is INTREC.
-
You must ensure the income and expenditure amounts entered in each line of the cost reconciliation feed are not duplicated on another line in the feed.
-
In 2024 the final accounts document will not be finalised until after the NCC guidance is published and therefore the FIN codes used in the reconciliation template, XML reconciliation reference data and integrated technical document will need mapping to the final accounts.
-
We will supply a mapping table to final accounts template coding on FutureNHS. This can also be useful for drafting your reconciliation in preparation for finalising your XML reconciliation.
Reconciliation process
-
We recommend you review the INTREC worksheet in the extract specification when you start preparing your annual costing submission. You must be able to accurately map the costing quantum back to your audited financial accounts right from the start of the costing process. Otherwise, reconciliation may prove more complex later.
-
You must obtain values for the operating expenses, activities other than patient care and accounting adjustments sections of the reconciliation template from the final audited accounts.
-
In 2024, when we carry out our reconciliation checks if there are material differences, you will be required to resubmit.
-
We also advise scoping all the services your organisation delivers as early as possible to give yourself adequate time to include all of those within your operating expenses that are permitted to be in your cost quantum.
-
Where one provider is acquired by another mid-year, the acquiring provider must contact us on costing@england.nhs.uk with the subject line Merger group trusts to clarify the action it needs to take for reconciliation.
-
These are the steps we recommend you take in carrying out your organisation’s reconciliation.
Financial accounting element
Step 1: Ensure the financial accounts are closed and the final version of the general ledger (GL) is available. Ask colleagues in financial accounts for the information from the final audited accounts.
Step 2: Obtain the final trial balance and/or the GL output, and ensure they agree at the detailed account code level. Familiarise yourself with which income centre each GL code is categorised into.
Step 3: Allocate the lines on the trial balance/output to the relevant lines on the cost reconciliation in partnership with your financial accountant. You can also use Spreadsheet CP2.1: Standardised cost ledger in the technical document.
Step 4: Together with your financial accountant check the figures in Step 3 agree with those in the final audited accounts spreadsheets.
Step 5: Complete the reconciliation up to the pre-costing software subtotal. Ensure your adjustments are a true and fair representation of your audited accounts. Perform a sense check at this point against last year.
The financial accounting element is now complete and you should move onto working with the costs from your costing software to finalise your cost quantum for the financial year. Your subtotal should now only relate to the costs for delivering patient care.
Finalising your cost quantum
Step 6: From the costing system outputs identify the costs of services performed for/by another NHS provider, services out of scope of the NCC and care of non-NHS patients. Adjust for these costs in the appropriate lines of the reconciliation.
Step 7: Request approval from the NHS England costing team before making any extra requirements not explicitly captured in the reconciliation. If approved, we will send you an authorisation code and you need to log this in your cost reconciliation. Adjust the lines in the cost reconciliation.
Development and quality assurance of your costing model in preparation for submission may take some weeks before you move onto Step 8 and Step 9.
Final check
Step 8: Ensure the total cost quantum for the files you are submitting for your cost collection agrees to within ±1% of the total quantum in the reconciliation.
Step 9: Perform a final check of the reconciliation against last year’s to identify any material or unexpected variations. If variations exist, investigate them and make changes as needed.
Operating expenses
-
Your operating expenses are the starting point for your reconciliation. You derive your cost quantum by adjusting the operating expenses figure but this must be done transparently using the reconciliation template and not by adjusting the operation expenses figure directly.
-
Your cost quantum should include costs incurred for any discontinued operations within the financial year. If a patient care operation is discontinued, it should be matched to the appropriate activity. If another type of activity is discontinued, it should be netted off and you need to request an agreed adjustment from us.
-
Your general ledger (GL) output will often not correlate to your final audited accounts. The basis for the NCC is that your cost quantum is derived from your trust’s final audited accounts. Therefore, you need to work closely with your financial accounting team to understand and interpret the differences between the two and derive costs that relate only to the patient care your trust is responsible for delivering.
Increase in employer’s superannuation
-
In 2019/20, the employer’s superannuation contribution increased from 14.38% to 20.68%, with the increase of 6.3% being funded centrally by NHS England. Trusts are required to account for the full cost (20.68%) in their operating expenses (TAC08) which will come from ESR allocated in line with staff cost arrangements.
-
The notional income of 6.3% should be recorded in patient income and will not affect the quantum of costs or the trust’s bottom line. If your trust has recorded this notional income in other operating income in error, please request an agreed adjustment.
-
We understand this will also be operational for 2023/24.
-
The cost of the pension increase will inflate the quantum costed by practitioners this year. As this is a recurrent cost of delivering healthcare it should be included in the quantum and allocated to patients.
-
The income, regardless of how it has been coded, should not be netted off the cost of the increased premiums as it is a cost of providing a service.
-
To apportion this cost where unable to easily link it to a specific individual via ESR information, use gross payroll as the basis of apportionment.
Other operating income
-
This details how you need to submit your trust’s other operating income in the NCC INTREC. It will ensure only the costs that relate to patient care are included in your cost quantum by reducing the operating expenditure by the value of non-patient care activities.
-
Non-patient care income categories are:
- education and training (E&T)
- research and development (R&D)
- commercial or other activities not primarily related to providing care to NHS patients.
-
You will adjust for the income your trust receives for these activities in both the NCC reconciliation and your costing model.
-
National policy is if the income received for services is more than it costs your trust to provide them, this contributes to the provision of NHS patient care. Therefore, the NCC requires you to net off all income from activities other than patient care from the appropriate cost centre within your cost ledger (CL).
-
Income from activities other than patient care should be matched to the service that generated the income, offsetting the cost of providing that service. In the INTREC, income from activities other than patient care is deducted from the total operating expenses.
-
You need to understand the different types of income recorded in the general ledger and what costs the income relates to, so the outputs from the costing system can be reconciled to the audited accounts. Income groups need to be separated into income that relates and does not relate to patient care. We recommend you familiarise yourself with which income centre each general ledger code is categorised into.
-
The INTREC requires you to deduct income from E&T and R&D activities. The totals for other operating income (all) and other operating income – not permitted, should balance with the other operating income in your organisation’s final audit accounts.
Education and training
- E&T income should be deducted from the operating expenses in other operating income.
Research and development
-
Research and development (R&D) comprise the following funding streams:
- Research: Grant funding to pay for the costs of the R&D itself (for example writing the research paper) received from the Department of Health and Social Care (DHSC) and other bodies including the National Institute for Health Research (NIHR), other government departments, charities and the Medical Research Council (MRC), and which includes funding for biomedical research centres, biomedical research units and Collaborations for Leadership in Applied Health Research and Care (CLARHC).
- NHS support: Funding from DHSC and NIHR to cover extra patient care costs associated with the research (for example extra blood tests, extra nursing time) that end when the research ends.
- Flexibility and sustainability funding: Funding from DHSC mainly to support the NIHR faculty and associated workforce.
-
Other R&D funding streams relating to patient care costs continue after the research ends. Where there is no income to match to a cost, the income must not be deducted from operating expenses. For example:
- treatment costs, including excess treatment costs: funding from normal commissioning arrangements to cover patient care costs associated with the research that would continue to be incurred after the research ends if the service in question were to continue
- subventions: exceptional funding from DHSC that contributes to the cost of very expensive excess treatment costs.
-
We are reviewing how excess treatment costs might be funded differently in future. This could have implications for the reporting of these costs in future NCCs.
-
All R&D income regardless of the accounting treatment (IFRS 15 or non-IFRS 15) and from the above funding streams should be deducted from the operating expenses in other operating income.
Apprenticeship levy
-
Expenditure in relation to the apprenticeship levy will be recorded in operating expenditure, however this should be removed as the value should not be included in the overall cost quantum.
-
Two income elements make up the apprenticeship levy balance: one from HMRC and one notional amount. Only the notional amount should be adjusted for, however, providing the balance is recorded in other operating income. This will already reduce the balance of your operating expenditure and no further adjustment is required.
-
If your notional income is within patient income, you will need to adjust for this in the reconciliation line ‘Non-patient care income recorded in patient care’. The remaining balance from HMRC should remain in your cost quantum.
Remaining operating income including clinical excellence awards
-
Income for clinical excellence awards (CEAs) should have been recorded in your organisation’s other operating income and should not be adjusted for. However, if your CEA income was included as patient income in your audited accounts, you should adjust for it in non-patient care income recorded in patient care.
-
If you discover patient income within your other operating income, you must ask NHS England for an agreed adjustment. This ensures costs are not artificially reduced. For more information see the government financial reporting manual.
-
The remaining balance in other operating income should not need to be adjusted but if you are not sure how to treat a source of income, contact the NHS England costing team on costing@england.nhs.uk.
Other operating income – not permitted
-
NHS England does not allow you to take away some income streams from your organisation’s operating expenses known as ‘other operating income – not permitted’.
-
If you have patient-related income in your other operating income, you should not take this away from your operating expenditure.
-
The income streams you are not permitted to take away are listed in the FutureNHS Adjustments to operating income: learning extension. For transparency, adjust for this income in ‘other operating income – not permitted’.
-
For assurance, the FutureNHS Other operating income: learning extension also lists the types of income that can be included appropriately as part of the total you have used in other operating income.
Non-patient care income recorded in patient care
-
If you discover non-patient care income that has been incorrectly recorded in patient care income, you must adjust for this in the NCC reconciliation line ‘non-patient care income recorded in patient care’.
-
The income for FP10 prescriptions should be within other operating income. If this income is incorrectly recorded in patient income, you should adjust for this in ‘non-patient care income recorded in patient care’.
Accounting adjustments
-
Further adjustments must be made to the ‘operating expenses’ reported in operating expenses from consolidated accounts of the reconciliation. Several non-cash items, such as donations and government grants for non-current assets, must be separately deducted from the operating expenses. Additionally, some income deducted as part of ‘other operating income’ that relates to patient care must be added back to the operating expenses.
Finance income and expenses
- Finance income is unrelated to patient care and should be deducted from the operating expenses, whereas finance expenses should be added. Finance expenses for the unwinding of discount should be treated as part of finance expenses.
Public dividends capital
-
The provider’s public dividends capital (PDC) should be added to the operating expenses.
Profits and losses
-
Profits from the sale of an asset that contributed to patient care should be deducted from the operating expenses, whereas losses should be added. The sale can be either at fair value or recycled.
-
Shares of profit from subsidiaries, associates or joint ventures (that is, from group accounts) should be deducted from the operating expenses, whereas shares of loss should be added. The net effect of profits and losses should be calculated, and the resulting adjustment made to the operating expenses, as this figure will not be reflected in your organisation’s cost quantum.
-
Any profit or loss from the sale of non-current assets in a private finance initiative (PFI) or Local Improvement Finance Trust (LIFT) deal should be deducted from the operating expenses to net off the gain or loss. Only the profit or loss from sales as part of a new PFI or LIFT scheme apply.
Impairments
-
Impairments charged through the statement of comprehensive income are not included in the NCC and must be removed. The balance of this line should be the net value of the impairment. This could be a positive or negative value.
-
Impairments should be deducted from the operating expenses, whereas reversals of impairments should be added.
-
The balance charged to revaluation of reserves does not relate to the operating expenditure for the year and should not be deducted from operating expenses.
Private finance initiative and Local Improvement Finance Trust expenditures
-
As a general principle, PFI and LIFT set-up costs include one-off revenue costs incurred in setting up a new scheme from the initial business case to financial close.
-
They include fees (consultancy, legal, financial, etc) and other costs such as planning applications. Set-up costs do not include the cost of services and other costs such as interest expenses. There a FutureNHS learning extension clarifying the treatment of PFI and LIFT costs.
Donations and government grants for non-current assets
-
The depreciation relating to donated or government-granted on current assets charged to expenditure in-year should be deducted from the operating expenses. This is because the whole cost of the purchase is recognised in the year of the purchase.
-
You will have removed the depreciation of the donated asset and therefore the whole cost of the purchase is recognised in the year of the donation.
-
Any income received in-year to fund non-current assets must be added back to the operating expenses, as it is deducted as part of other operating income.
-
Take care not to remove impairments that will already have been deducted in ‘Impairments net of (reversals)’. The income may be actual cash donated to purchase an asset or the asset value where an asset has been donated; the treatment here will be the same.
-
The treatment of the credit entry relating to donated assets is not held in reserves and is used to offset charges to expenditure. Instead, the funding element is recognised as income in-year as required by IAS 20 and as interpreted by the HM Treasury Financial Reporting Manual.
-
In the year when the asset is received, the provider will have income equal to the value of the asset and a much smaller depreciation charge to expenditure. To prevent any instability in the cost quantum caused by this large net income in the year of receipt followed by years of increased costs (that is, the depreciation charge, etc), all income and expenditure relating to donated assets must be excluded from the NCC.
- Impairments will not be an issue as these are also excluded from the NCC.
Corporation tax
- A row has been added to the extract specification AMBREC for corporation tax. Corporation tax will normally only be part of the final audited accounts if it is paid for regarding subsidiaries, associates or joint ventures. If your final audited accounts include this, then you should remove the value on this line of the reconciliation statement.
Services provided to or by another NHS provider
-
This guidance ensures you capture only the costs of caring for your organisation’s own patients in your reconciliation. It details the correct treatment in the reconciliation of services provided to or received from another NHS organisation.
-
A provider’s operating expenses minus its other operating income should typically equal its cost quantum. This may not be the case when one NHS provider performs services for another, such as elective operations for a provider that is struggling to meet its operational targets. Reconciliation adjustments are therefore needed.
Services supplied and received (provider to provider)
-
The standards refer to services provided to other organisations as ‘clinical services supplied’ and services received from other organisations as ‘clinical services received’. See Standard CM8: Clinical and commercial services supplied or received.
-
The management of patients by a third-party organisation but on behalf of an NHS commissioning body is a type of contracted service. If in doubt about this, please contact us on costing@england.nhs.uk.
-
Activity contracted out to the private sector is discussed separately in ‘Care contracted out to private providers’ in Services excluded from the NCC.
-
The trust supplying the service provides the activity but does not receive patient income as part of its integrated care board (ICB) commissioned contract; rather it receives payment from the service recipient.
-
The receiving trust is invoiced for the services provided to its patients by the supplying trust. It is therefore the final recipient of the cost of caring for the patient and responsible for reporting the activity and costs of the activity in its NCC, as if it had provided the service itself. Its operating expenses will include the payments it has made for the services it contracted out.
-
The receiving trust should include the cost of the invoice in the operating expenses. As it will then flow through to the receiving trust’s cost quantum, no adjustments in the reconciliation are necessary.
-
The trust supplying the service should not report the cost or the activity in its NCC submission. The profit or loss from supplying the service should remain in the total quantum of the supplying trust’s costs.
-
This means that instead of adjusting the cost quantum for the true cost of supplying the service, you should adjust it for the income generated by the supplied activity.
-
The way income is treated depends on where it has been coded in the general ledger:
- other operating income – no adjustment required
- patient income – adjust in clinical and support services supplied to or received from other organisations (P2P).
-
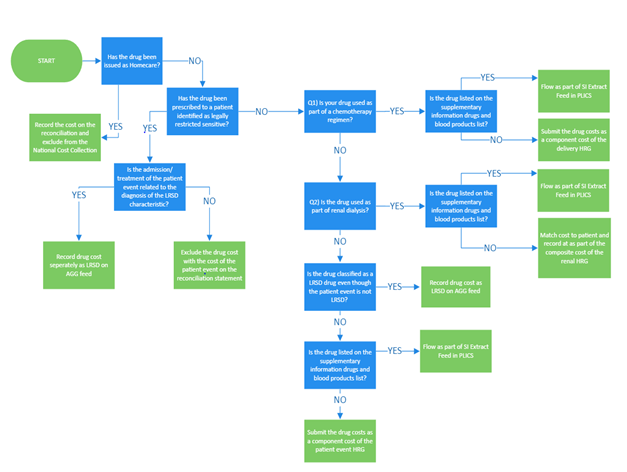
Figure 1 shows how trusts should treat the costs of contracted services in their NCC reconciliation.
-
In your activity reconciliation, you should ignore any activity in the patient activity feeds (for example diagnostic imaging and pathology) relating to services supplied; it should be reported only by the trust receiving and paying for the services.
-
Since 2022 an extra field has been added to the extract specification to flag where a trust has part costs because of some resources being provided by a supporting organisation.
-
Trusts that are a supporting organisation providing some of the resource to another organisation, should exclude the costs of the resource given in the provider-to-provider line of the reconciliation.
Figure 1: Cost and reconciliation reporting for services supplied and received
-
The INTREC should not be adjusted for any profit or loss made on these arrangements; instead profit or loss should remain as part of the cost quantum
-
Costs relating to any qualified providers should be adjusted for in clinical and support services supplied to or received from other organisations (P2P).
Services excluded from the National Cost Collection
-
This section details the services excluded from the NCC that should still be reported on the INTREC. This is required as there is still a national requirement to understand the costs of these services that are not collected at PLICs or aggregate level.
-
The main services excluded are described in Annex 1.
National screening programmes
- These are national screening programmes included in the NCC with details of where costs should be included:
- NHS Fetal Anomaly Screening Programme: included in relevant maternity outpatient and admitted patient costs.
- NHS Infectious Diseases in Pregnancy Screening Programme: Included in relevant maternity outpatient and admitted patient costs.
- NHS Linked Antenatal and Newborn Sickle Cell and Thalassaemia Screening Programme: Included in relevant maternity outpatient and admitted patient costs except for a few genetic tests that are excluded and should be funded directly by ICBs.
- NHS Newborn and Infant Physical Examination Screening Programme: Included in the cost of maternity delivery HRGs or postnatal visits.
- NHS Newborn Blood Spot Screening Programme: The cost of taking the sample is included in the cost of maternity delivery HRGs or postnatal visits. The cost of its analysis by regional newborn screening services is excluded from the NCC.
- NHS Newborn Hearing Screening Programme: Included in audiology services as neonatal screening.
- National Screening Programme for Diabetic Retinopathy: Included in diabetic retinal screening, which should be reported as a directly accessed diagnostic service against HRG WH15Z.
- NHS abdominal aortic aneurysm screening programme: Included in the AGG feed type with activity count number of tests.
- NHS breast screening programme: Included in the AGG feed type with activity count number of tests.
- NHS cervical screening programme: Included in the AGG feed type with activity count number of tests.
- NHS bowel cancer screening programme: Included in the AGG feed type with activity count number of tests.
- Several other national screening programmes are excluded from the NCC. Only those listed above should be included in the NCC.
Services excluded from the NCC in 2024
- Some services are not collected as part of the NCC because they meet one or more of the following criteria:
- no national requirement to understand the costs
- lack of clarity about the unit that could be costed
- no clear national definitions of the service
- no clearly identifiable national classification or currency
- underlying information flows do not adequately support data capture
- overlaps with social care or other funding.
-
Annex 1 gives the details of these services. Only these services may be excluded. The total cost of patient events should be excluded using full absorption costing and recorded on the INTREC.
-
This guidance ensures that in your reconciliation you only capture the costs your organisation incurs caring for patients whose care is funded by the NHS. Costs for patients not funded by the NHS in England should not flow through your NCC cost collection and instead should be included on the reconciliation.
-
Therefore, this guidance applies only if your provider is submitting these costs as part of its operating expenditure.
-
It details the correct treatment in the reconciliation for services provided by your organisation to non-NHS patients or to your patients by private providers. When following the PLICS costing process, please refer to Standard IR1: Collecting information for costing and Standard CM8: Clinical and commercial services supplied or received.
Private patients
- Deduct the costs of providing care to private patients who are funded by private medical insurers or pay for their treatment themselves.
Overseas visitors
-
Deduct the costs of providing care to overseas visitors who are not exempt from charge under the NHS (Charges to Overseas Visitors) Regulations 2011. This includes most irregular migrants, visitors from a country that the UK does not have a reciprocal agreement with and some UK citizens living overseas.
-
Where the UK has a reciprocal agreement with another country you should not deduct the costs of caring for patients from that country as it is part of NHS activity. ICBs commission the care of these patients and their costs should be included in the same way as if they were registered or resident in England.
Other non-NHS patients
- Deduct the costs of providing care to the following non-NHS patients:
- Armed forces personnel: These patients are funded by the Ministry of Defence (MoD) where the requirement varies from the standard NHS pathways in either the treatment requested or management requirements (for example fast-track care or non-standard treatment). Their attendances or episodes are identified by the code ‘XMD’ rather than the ICB code for data submission purposes. Non-standard care arrangements are normally covered in specific MoD contracts or by prior agreement with the MoD referrer. For some mental health services, MoD funding does not apply and therefore the cost of these services should be included in the quantum.
- Patients from the devolved administrations (Scotland, Wales and Northern Ireland): Parliament sets the NHS budget based on the requirements of NHS patients in England; that is, those resident in England and legally entitled to NHS care.
Care contracted out to private providers
- Deduct the costs of outsourced activity that is:
- contracted out to private providers (care contracted out to other NHS providers is discussed in Services provided to or by another NHS provider)
- patient activity rather than outsourcing of functions, for example payroll
- patient activity where the whole episode is carried out by a private provider.
-
Commissioners may pay the increased cost of these patients; if so, the only cost that can be attributed by your trust is the administration of these patients (waitlist office, informatics, etc).
-
Your organisation’s costs may include those for services it performs to facilitate the care of patients under the care of a private provider located within your organisation, for example nursing or administrative support.
Networks
-
Operational delivery networks support the regional care for specialised services. There are 14 specialised commissioning networks that should be treated as exclusions for the 2024 NCC.
-
The funding is sent to a host trust that runs the clinical leadership and administration for the network. The cost of this service is not solely for the patients in the host trust, so should not be included in ‘own patient care’ for that trust.
-
The principle of keeping this type of cost separate from the cost of own patient care has been well established in the cancer multidisciplinary team (MDT) meetings submission within the National Cost Collection.
-
Similarly, the cost of these meetings relates to patients from a wider clinical responsibility than just one trust, and so separation is needed from the cost of own patient care.
Agreed adjustments
-
All adjustments below should be agreed with NHS England before being included in the reconciliation.
-
To request an agreed adjustment please complete the MS form which can be found here.
-
Requests for an agreed adjustment must be sent to the costing team at NHS England no later than two weeks before the submission window opens.
-
Agreed adjustments requested after this date must be requested from your trust’s director of finance.
-
Any change to the approved agreed adjustment value must be detailed in the NCC sign off or the final submission board report. See the introduction to the Approved Costing Guidance for more information. If the value change is more than 10% a new agreed adjustment request must be made for the updated value.
-
Agreed adjustments must be reported with one approval reference per line. Values for multiple adjustments per trust should not be added together.
-
We monitor the entries in agreed adjustment lines throughout the submission window. If we find entries that have not been previously agreed with us and for which there is no appropriate explanation, we may contact your provider and ask for a resubmission.
-
Adjustments must be agreed on an annual basis – that is, for each collection. Do not roll over those agreed in previous years as there is no guarantee they will be agreed in subsequent years.
-
Agreed adjustments codes will not be issued without an estimated value for the adjustment.
Non patient income recorded in patient care income
-
In some instances, activities other than patient care will be miscoded to patient care income in the final audited accounts.
-
You should adjust for this in the agreed adjustments section to ensure the other operating income figure recorded in your reconciliation matches back to the final audited accounts.
Final accounts – FAQ adjustments
-
Five lines have been provided for any adjustments that need to be made because of the final accounts being released later than the costing guidance.
-
An FAQ will be published explaining any additional adjustment required and which row to be used.
Other trust-specific agreed adjustments
- Trusts may ask for additional exclusions in exceptional circumstances where including the cost would mean the costing quantum did not represent the provider costs that relate to the ongoing running costs of the trust and for NHS services.
Activity reconciliation
-
Reconciliation of submitted activity has always been a requirement of the National Cost Collection.
-
For the 2024 NCC all trusts should attempt to reconcile their activity information to the mandated dataset where possible. For HES, MHSDS and IAPT submitted activity we expect this to be with +/- 1%. Where you have a material difference you should report this on your NCC sign off.
-
It is best practice for community contacts to reconciled to CSDS and record this on their NCC sign off.
-
You should reconcile to the versions of mandated datasets shown below:
- HES: version CDS V6.3, final cut (M13), feeds APC and OP
- ECDS: version 4.0, feed EC
- MHSDS: version 5.0, feeds MHCC and MHPS
- Talking Therapies/IAPT: version V2.1, feed IAPT
- CSDS: version V1.6, feed CSCC.
-
You do not need to reconcile activity to mandated datasets for high cost drugs, high cost blood or high cost devices and unbundled imaging.
-
Historically, trusts have been asked to reconcile their activity to within 1% of the mandated dataset. However, in certain cases this may not be possible, for example due to timing differences or pilot schemes outside the remit of the mandated dataset.
-
Where activity cannot be reconciled within 1% of the mandated dataset you must record this in your NCC sign off.
-
Trusts that deliver mental health activity must consider where their activity data is submitted to complete the activity reconciliation. Mental health activity should be submitted to MHSDS; however some acute trusts with small activity levels currently submit to HES.
-
Where your costing system activity data represents a more accurate picture of your trust’s activity than HES, you should not change your costing system to reconcile. Instead, you should:
- retain the emails and/or meeting notes between yourself and your informatics department or operational colleagues as verification of the reason for the difference
- record this difference in your ICAL so it can be easily understood in the future either internally or externally
- record this difference in your NCC sign off so we can record the difference in our systems for future reference.
-
A trust’s NCC reconciliation should be retained on file for audit and assurance reasons. There is a proforma activity reconciliation template in the updated ICAL on FutureNHS.
-
Further information on how we match your submitted PLICS data to the mandatory dataset can be found in Annex 2.
National Cost Collection submission overview
Introduction
-
This section sets out the scope and governance for the 2024 National Cost Collection (NCC) and should be read by all organisations that submit data for the NCC. It gives you the information you need to participate in the mandated collection during 2024. The year 2024 here refers to the cost collection for the financial year 2023/24.
-
You should read our introduction to the Approved Costing Guidance and Reconciliation and exclusions before reading this section.
-
It is mandatory for all NHS trusts and NHS foundation trusts in existence between 1 April 2023 and 31 March 2024 to comply with the NCC guidance and the collection timetables.
-
You should read the Integrated extract specification in conjunction with this section.
-
To maintain consistency and minimise burden, we have designed a collection of minimal changes only in 2023/24. We hope this will allow the sector to work from a stable foundation of relatively unchanged guidance and collection.
-
Details of our main support contacts during the collection are also in our introduction to the Approved Costing Guidance which also contains information on how your data is used and shared.
Changing operational structures
- Several changes in a trust may affect its NCC submission:
- mergers
- acquisitions
- integrations
- major service reconfiguration.
- If any of these affect your trust for the 2024 National Cost Collection or future collections, please contact the costing team at costing@england.nhs.uk to ensure your submission is in line with the mandation.
If your trust is merging with or being acquired
- In line with the Treasury’s financial reporting manual, two or more public bodies that are combining or transferring functions should apply absorption rather than merger accounting. Your collection for 2024 may be affected by a merger or acquisition either in the financial year for which data is being submitted or in the year of collection. For example:
- date of merger 31 January 2024 – merger during financial year being submitted
- date of merger 28 April 2024 – merger during year of collection.
- As each merger is unique, please contact us at costing@england.nhs.uk with the subject line merger group trusts as early as possible so we can lead you through the process and offer targeted guidance.
Submission window for 2024
- The dates for the submission window for 2024 NCC will be shared on FutureNHS.
Our support during the collection
-
We can support you in many ways leading up to and during the submission period. For more details, see FutureNHS.
-
We will publish frequently asked questions (FAQs) on FutureNHS starting after the publication of the Approved Costing Guidance.
-
Please do not contact members of the NHS England costing team directly.
-
If you leave your trust or your trust costing practitioner changes, please let us know via costing@england.nhs.uk so we can update our communication lists.
Scope of activity and costs to be collected
-
The NCC collects data about the costs of patient care in the NHS. This means some of the costs your organisation incurs are not collected. This details the scope of activity and costs your organisation should submit.
-
You should use the 2023/24 National Costs Grouper.
Costing period
-
The costing period begins on 1 April 2023 and ends on 31 March 2024.
-
For patient-level cost collections of admitted patient care (APC) all patient episodes completed within the costing period or still open at the end of the costing period are in scope. Episodes are classified by type according to their completion status. Please see Standard IR1 in Integrated costing standards, for more detail.
-
The emergency care (EC) extract list in the extract specification details the period of expected values for arrival date, and time and date of departure from the emergency department that should be accounted for in the financial year 2023/24.
-
The specialist ward care (SWC) feed type specifies the costing period is for all occupied bed days in 2023/24.
-
All mental health provider spells (MHPS) completed within the collection year, or hospital provider episodes still open at the end of the collection year, are in scope of this collection. A spell or episode that is unfinished at the end of the financial year must be collected as part of the month 12 file.
-
All mental healthcare contacts (MHCC) completed within the collection year are in scope of this collection.
-
All IAPT care contacts attended within the collection year are in scope of this collection.
-
All community health service (CHS) care contacts within the collection year and in scope of this collection.
-
For supplementary information: high-cost drugs, high-cost blood products, high-cost excluded devices, unbundled imaging and virtual wards are in scope of this collection.
-
For aggregated costs, the type of care should be assessed and the rules noted above should be applied to their inclusion.
-
Only resources used and activities undertaken within the costing period should be included, regardless of when the patient event started or ended.
What do providers need to submit in 2024?
- Patient-level costs are collected at the level of each patient event. A patient event is:
- an attendance, episode or contact for acute activity
- a spell or care contact for mental health activity
- a care contact (attendance) for IAPT activity
- a care contact for community services
- an incident for ambulance activity.
-
For each patient event costing data is collected for resources used and activities undertaken. These are listed in the appendices to the extract specification relevant to your primary or integrated sector.
-
The extract specification spreadsheet documents the fields to be collected for each sector. If your trust provides the relevant services, the following PLICS extracts should be reported at patient level for this collection:
- admitted patient care (APC) complete and incomplete episodes, including regular day or night admissions and community inpatients
- outpatients (OP) non-admitted patient care (NAPC) attendances, including ward attenders, any community attendances reported on the commissioning dataset (CDS) and wheelchair attendances
- emergency care (EC) accident and emergency attendances, including minor injury units, urgent treatment centres and walk in centres
- specialist ward care (SWC) adult, paediatric and neonatal critical care bed days
- supplementary information (SI) high-cost drugs, blood products and devices, unbundled imaging and virtual wards
- mental health provider spells (MHPS) complete and incomplete spells: trusts that submit their inpatient mental health data to Hospital Episode Statistics (HES) should submit their costs on the APC XML extract; trusts that submit their inpatient mental health activity to MHSDS should submit costs on the MHPS XML extract
- mental health care contacts (MHCC) non-admitted patient care (NAPC)
- Talking Therapies care contact (attendances)
- community services care contacts (CSCC) contacts in a patient’s home or community setting including non-face to face contacts such as telemedicine
- aggregate (AGG) patient events that are unable to be collected at patient level due to volume or legal restrictions.
-
If you are unable to meet the requirements of the extract specifications, please complete the MS form found here.
-
Aggregated unit costs are collected for some services that cannot be collected at patient level. These costs should be submitted on the AGG feed in the extract specification.
Education and training
-
Separate education and training (E&T) costs are not part of the mandated 2024 National Cost Collection.
-
In 2024 trusts are required to net off their E&T income from patient care costs. The E&T transitional method in CM35: Education and training gives guidance on how to do this in a transparent way; organisations that provide E&T should follow this method.
-
We will not be changing the NCC process for E&T costs (where income is used as a proxy for cost) in 2024.
Sign off process
-
The trust director of finance must send sign-off to the NHS England Costing Team on the day of their trust’s final NCC submission.
-
While the trust director of finance is overall responsible for the accurate completion of the combined costs collection return the submission should be subjected to the same scrutiny and diligence as any other financial returns submitted by the provider. Therefore for 2024 NCC you are also required to obtain board level sign-off.
-
Two reports should be taken to the board:
- a pre-submission report – before the submission window opens for 2024
- a final submission report – at around the time of or following submission.
- At pre submission stage, a report should be taken to the board confirming:
- The costing process has been approved ahead of the collection.
- The return has been prepared in accordance with the Approved Costing Guidance, which includes the NCC guidance.
- Information, data and systems underpinning the combined costs collection return are reliable and accurate.
- There are proper internal controls over the collection and reporting of the information included in the combined costs collection, and these controls are subject to review to confirm that they are working effectively in practice.
- The costing team is appropriately resourced to complete the National Cost Collection return, accurately within the timescales set out in the guidance.
- Any actions from previous NHS costing assurance process (CAP) reviews of costing or data quality have been formally followed up and completed (as appropriate).
- A second report should be tabled, just prior to final submission confirming that:
- The information included in the submission – both cost and activity – has been reviewed and verified as accurate.
- All mandatory and significant non-mandatory validations have been reviewed and verified.
- Any significant areas where the trust has varied from the mandation (ie unable to submit at patient-level or issues around activity or methods of apportionment) have been agreed with NHS England and have been reported to the Board.
-
An editable version of the board assurance pro forma will be available on FutureNHS.
-
We list the checks you should make as part of your internal assurances before submitting your cost collection in a learning extension on FutureNHS but we will not collect this information.
Main changes for 2024 National Cost Collection
Mental health provider spells
-
In the 2023 NCC with the removal of clustering, mental health trusts were asked to submit mental health service or team type. Following feedback received we have been made aware that this field is not relevant for inpatient services.
-
For the 2024 NCC we want to improve this and are asking trusts to submit hospital bed type (mental health) also known as mental health admitted patient classification. This field should be populated for trusts who provide inpatient services however as it is only a required field in the mental health data set (MHSDS), some trusts may not have populated this field however we expect this to be the minority.
-
Where your trust does not have this field populated in MHSDS you should leave this field blank.
-
If you have multiple currencies or commissioners within one provider spell, you can choose to identify this in your submission by creating a duplicate record in the data feed. However, if you do this you must leave the spell dates the same for both records and the cost must be split appropriately between the multiple currencies or commissioners. You must not leave the whole spell cost in both episodes of data as this will stop your cost quantum reconciling.
Extract specification changes
-
In the aggregate data feed a legally restricted sensitive data indication has been added to flag if data is LRSD or not. As a result of this new flag being added the ACSIU field has been expanded. See the extract specification for the full list of ACSIU expected values.
-
In the EC data feed the data item Urgent and emergency care activity type has been updated to include codes 05 ‘Same Day Emergency Care’ and 06 ‘Urgent and Emergency Care Extended Care Episode’.
Developing currencies
Mental health
- The Payment Development team at NHS England have developed new currencies for mental health. These have been added to the MHPS and MHCC feed in the extract specification and we will operate dual running of these currencies in the 2024 National Cost Collection. This new data item is called ‘Mental Health Services Currencies in Development’ and the data items are:
- A000: Adult: Psychosis and Bipolar Disorders
- B000: Adult: Mood and Anxiety Disorders
- C000: Adult: Eating and Feeding Disorders
- D000: Adult: Neuro-cognitive Disorders
- E000: Adult: Personality Disorders and Complex Trauma
- F000: Children: Getting Advice
- G000: Children: Getting Help
- H000: Children: Getting More Help.
- You should refer to the extract specification for a further breakdown of the settings that can be attributed to adult currencies.
Community services
- For community care the Payment Development team have developed new currencies for frailty and end of life. These have been added to the CSCC feed in the extract specification and we will operate dual running of these currencies in the 2024 National Cost Collection. This new data item is called ‘Community Health Services PLICS Currencies in Development’, the data items are:
- FR00: Frailty Group
- LYOL00: Last Year of Life Group
- SEOC00: Single Episode of Care Group
- CYP00: Children and Young People Group
- LTC00: Long Term Conditions Group.
-
You should refer to the extract specification for a further breakdown of the categories that fall into the Frailty and Last Year of Life groups.
-
We plan to share a mapping document to these new currencies on FutureNHS.
-
If you are able to submit data for these new mental health or community currencies, it must be in addition to the existing mandatory community currencies.
Preparing PLICS files
Medicines in 2024
-
For 2024, the cost of medicines is split between the AGG feed and the patient-level collection. In the latter, medicines are identifiable in the collection resource CPF005 Drugs (including drugs on the supplementary information (SI) drugs and blood products list). More detail of high-cost drugs is given in the SI feed.
-
Annex 3 provides a diagram for how medicines should flow in the NCC.
-
In the extract specification reference tables the three types of patient-level drugs have the following prefix codes in the currency.
- PCTD – patient level chemotherapy drugs
- PHCD – patient level high-cost drugs
- PSCD – patient level specialised commissioning drugs.
- There are two drugs lists in the extract specification. One for drugs that should flow in the supplementary information (SI) feed and one for drugs that are legally restricted sensitive data (LRSD) and should flow in the AGG feed.
- Medicines for patients designated as having an LRSD characteristic, including in vitro fertilisation: collect in the AGG data feed
- Medicines for patients who have an LRSD characteristic but the attendance/ treatment is not for this characteristic: exclude on the INTREC with the patient event
- High-cost drugs and blood products (including high-cost renal drugs): SI feed (PLICS) – only high-cost drugs and blood products identified as not LRSD
- High-cost drugs and blood products (including high-cost renal drugs): AGG feed: any high-cost drugs and blood products identified as LRSD
- Chemotherapy drugs: flow as part of PLICS; should be part of the cost of the delivery HRG unless it is a drug listed on the SI drugs and blood products list, in which case it should be included in the SI feed. If you have chemotherapy drugs that do not match to a chemotherapy delivery HRG they should flow as part of the composite cost of the core HRG
- Homecare drugs: excluded – reconciling item too burdensome to collect at aggregated level or patient level. Where a drug is both chemotherapy or high-cost drugs and homecare, treat it as homecare first, so the cost of all homecare drugs is excluded from the collection
- Non high-cost renal drugs: flow as part of PLICS, should be part of the composite cost of the episode or attendance.
- Cystic fibrosis drugs: flow as part of PLICS; should be part of the cost of the episode or attendance unless it has been listed as a high-cost drug, in which case it should be included on the SI feed.
- Any other drug: flow as part of PLICS; part of the composite cost of the episode or attendance.
- Red Book drugs: flow as part of PLICS; Red Book drugs should be submitted on the SI feed where they are drugs on the high-cost drugs list in the data extract specification. There will be no patient identifiers for them as there is no patient identifiable data in the SI feed. Any Red Book drugs that are not on the high-cost drugs list would be treated as an overhead to the relevant service.
PLICS extract matching identifier
-
As defined in the costing methodologies, matching should be used to attribute support service costs in auxiliary feeds to the master feeds of the clinical event. Once the support service costs have been attributed to the master feeds, you should then link unbundled costs to the core clinical event through the generation of a PLICS extract matching identifier (PLEMI).
-
The PLEMI should enable linkage of all elements of a spell/episode/attendance/care contact/event so the total cost of the clinical event can be understood, regardless of how the elements of the unit costs are submitted in the collection. It also has the benefit of reducing the volume of data that needs to be collected.
-
For example, linking a critical care patient event to an admitted patient care (APC) patient event, the specialist ward care (SWC) PLEMI will be the same as the PLEMI in the APC patient event. Or, if a patient is given a high-cost drug during an inpatient episode, the rows for the inpatient episode will have the same unique ID as the high-cost drug.
-
We do not specify the exact structure of the PLEMI, you can create this yourself; however, it does need to be unique for each episode/attendance/ care contact/event. The identifier format is alphanumeric (including special characters) and has a maximum length of 50 characters.
-
There is a learning extension on FutureNHS giving examples of the inpatient journey using the PLEMI but this identifier can be applied to all extracts collected at PLICS level.
- The PLEMI is already established in costing systems but may have a different name. If you are unsure about this, please ask your software supplier.
Patient-level costing collection activity count
-
In the extract specification for feed types APC, EC, OP, SWC, SI, MHPS, MHCC, Talking Therapies (known as IAPT in the extract specification) and CSCC, you are required to submit the ‘activity count’. This is the number or duration of activities undertaken, for example number of tests or length of time in theatre.
-
The complete list of activity counts with the corresponding collection activity is shown in the integrated data extract specification, worksheet: Ref Data – Activities.
-
In previous years the data quality of the activity count field has been poor because of multiple pre-collection allocation drivers being assimilated into one count on the XML file. There is a learning extension on FutureNHS with worked examples of how to complete the activity count field.
Integrated extract specification
-
The data feeds remain split by the type of care being delivered. For example, APC collects APC for acute and community services (episodes), MHPS collects inpatient stays for mental health services (spells) and CSCC collects care contacts for community services (care contacts).
-
There is also a new feed for the collection of aggregate data.
-
The separately published extract specification sets out the exact structure of the CSV or XML files you need to produce for the collection: field names and formats, with valid codes for fields where applicable. CSV extract files must be converted to XML before making your NCC submission.
Part costs
-
In some cases, patient care is provided by resources supplied from two or more organisations (NHS or non-NHS) without a corresponding cost recharge. These patient events should be identified with an indicator in the extract specification, indicating that the costed patient event includes only part of the cost.
-
This indicator was introduced to ensure all patient events are costed within the NCC submission but the costs are not artificially lower because of these shared provider arrangements. The patient events flagged as part costs must still include overheads.
-
To ensure PLICS data is useful for local and national analysis it is important to identify these events so they can be excluded or included, depending on the need of the stakeholder.
-
The patient event data item should be costed and reported by the main provider organisation. The organisation supporting that patient event should identify the cost of the staff support or care provided and exclude this cost on the INTREC.
-
Examples of where a part cost indicator might be needed:
- integrated care systems (ICS), where staff from multiple trusts contribute to the care for an ICS managed pathway
- where national programmes contribute to patient care via staff or non-pay items rather than by funding the items via income
-
A part cost indicator does not have to be applied where the cost of the patient event is materially appropriate, and the cost of care provided by another organisation is negligible.
-
Only the main organisation recording the activity should use the part cost indicator. The supporting organisation should exclude the costs of the resource given in the provider-to-provider line of the INTREC.
-
From 2024 the part costs indicator is shown in all feed types, excluding EC.
-
The part costs flag should only be used where items are material to the cost quantum and without would lead to inaccurate conclusions being drawn from the costing data.
Acute, mental health and community inpatients
Collection scope
-
All inpatient episodes and hospital provider spells completed within the collection year or still open at the end of the collection year are in the scope of this collection. Further information on incomplete patient events is below.
-
An episode or spell unfinished at the end of the financial year must be collected as part of the Month 12 XML file.
-
Only include resources used and activities undertaken within the collection year, regardless of when the hospital provider spell started or ended. For example, only costed ward care bed days within the collection year should be reported.
-
The cost of these items must be reported using the appropriate collection resource and collection activities at a patient level in the PLICS XML files. Costs and activity should be submitted by episode for APC and by occupied bed day for MHPS.
-
As part of the mandation of community, admissions reported as intermediate care bed days are in the scope of the PLICS collection but should be submitted per episode, not per bed day.
Incomplete patient episodes and spells including clinical event type
-
To identify and calculate the cost of incomplete patient episodes, refer to Standard CM2: Incomplete patient events.
-
For APC, the point of delivery (POD) submitted for an incomplete episode must be that of the episode if it were complete (see example below), so that on linking type 1 to type 2 episodes, the correct POD is in both records. The data validation engine (DVE) analyses types 1 and 2 length of stay separately from type 3.
-
For example, the admission of a patient as an emergency on 31 March 2024 at 14:40 and their discharge on 10 April 2024 should be recorded as non-elective (NEL), not non-elective short stay (NELST).
-
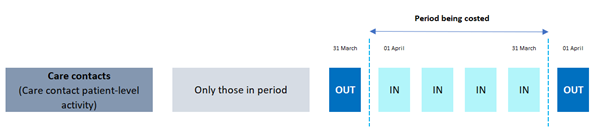
Four types of episodes or spells are collected, and should be grouped by the ‘EpType: Episode Type’ data item:
- All episodes or spells started in a previous year (over start period) and finished in the current collection year. To correctly allocate the right proportion of costs, for example ward costs, to these spells in your costing system, calculate the proportion of the episodes or spells in days falling in-year.
- All spells started in the current collection year but incomplete at year-end (over end period).
- All spells that started and finished in the period (in period). These do not require a specific calculation at year-end.
- All spells started in a previous year and incomplete at year-end (ongoing throughout the period). To cost these long-stay patients, count the number of in-year days to ensure the in-year costs only are allocated to in-year activity.
- Episodes or spells with a start date before the costing period, should flow with the actual start date of the episode or spell, so there is no change to the nationally reported episode or spell start date. You should not adjust the start date to be the start date of the costing period.
Admitted patient care episodes
- The following types of admitted patient care (APC) should form the basis of the episodes collected in the APC PLICS data feed:
- day case electives
- ordinary electives
- ordinary non-electives
- regular day or night admissions
- community inpatients.
- The 2023/24 National Costs Grouper attaches a core HRG to every finished consultant episode (FCE). Activity run through the grouper that gets attributed a core HRG will be reported in APC.
Episode grouping in APC
-
Community inpatients will be reported on the APC feed but may not include sufficient clinical coding to calculate an appropriate HRG. These community inpatients will be categorised using a new field: ‘EpGro: Episode grouping’.
-
Episode grouping is the patient care group for the episode and identifies whether a patient episode has sufficient clinical coding to have a reliable HRG in the HRG field. The episode grouping codes and description are shown below:
- 01 Episode with costing grouper HRG (all but undefined groups)
- 02 Community medical episode
- 03 Community surgical episode
- 04 Community intermediate care episode
- 05 Community neuro rehabilitation (long stay unit) episode
- 06 Other community rehabilitation episode
- 07 Community palliative care episode
- 08 Other community episode
- 09 Other episode with undefined group HRG
- 10 Mini episode for patient with rehabilitation complexity scale
- 11 Specialist rehabilitation patient at bed day level.
-
Acute trusts already submitting episode data at patient level are expected to use the episode grouping codes of 01 HRG data, or in some situations, code 09 UZ01Z HRG.
-
Providers of community inpatient services (including trusts designated as mental health for their primary sector and acute trusts with some community hospitals) will use codes 02–08, to add detail to the episode record. These community inpatient records may have an HRG attached, using the limited clinical coding information available.
-
High-cost drugs, devices and blood products are unbundled from the core HRG. The cost of these items must be reported using the appropriate collection resource and collection activity at a patient level in the SI extract (see Supplementary information in 3.13: 2024 National Cost Collection overview).
-
Adult, paediatric and neonatal critical care is unbundled from the core HRG. The cost of the days within the financial year of the collection must be reported using the appropriate collection resource and collection activity at a patient level in the SWC extract (see Specialist ward care).
-
The episode grouping data item has been expanded to provide options to flag the way you submityour trust’s specialist rehabilitation data. You must use one of the following categories:
- 01 Episode with costing grouper HRG (all but undefined groups)
- 10 Mini episode for patient with rehabilitation complexity scale
- 11 Specialist rehabilitation patient at bed day level.
Ordinary non-elective short stays and long stays
-
All ordinary non-elective activity must be separately identified as either long or short stay by completing the input fields required by the grouper for critical care, rehabilitation and specialist palliative medicine length of stays. The grouper deducts these days from the core stay when processing your APC data.
-
A short stay is one day. The grouper automatically adds one day to admissions with a zero-day length of stay. All other stays are long.
Regular day or night admissions
- Regular day or night admissions are reported in the APC collection for PLICS. Admissions for specialist palliative medicine, chemotherapy, radiotherapy or renal dialysis, should be reported against the relevant sections of the collection, not under regular day or night admissions.
Mental health provider spells
-
This section covers mental health provider spells (MHPS) and APC, which are the basis of the spells collected in the MHPS PLICS data feed.
-
Mental health trusts will submit both complete and incomplete costed spells for APC. There is a learning extension on FutureNHS with an example of trimming spell dates to match the costing period.
-
In some circumstances, a patient may:
- take home leave or mental health leave of absence for a period of 28 days or less
- have a current period of mental health absence without leave of 28 days or less which does not interrupt the hospital provider spell
- be transferred temporarily to an acute provider for treatment.
- You are not required to amend the length of stay for home leave as there is a mandatory field in the MHDS which can be matched to and adjusted if needed.
Outpatients
Collection scope
- This section covers the following types of outpatient activity and should form the basis of the activity collected in the OP PLICS data feed:
- outpatient attendances, including ward attenders
- procedure-driven HRGs in outpatients.
-
Outpatient attendances and procedures in outpatients should be reported by HRG and TFC service identifiers at patient level.
-
The grouper may attach one or more unbundled HRGs to the core HRG produced. Only core attendances should be reported on the OP extract for acute providers.
-
Unbundled imaging HRGs that unbundle from the core HRG should be reported on the SI feed.
-
Missed appointments (did not attends – DNAs) and cancelled appointments should not be recorded, and their cost should be treated as an overhead.
-
Advice and guidance should be allocated as an overhead to the service as there is currently no specified currency for them. This includes admission avoidance where advice is sought between clinicians.
General outpatients
- Outpatient attendances in HRG4+ (WF01* and WF02*), generated from mandated fields in the outpatient Commissioning Data Set (CDS), are organised by:
- first and follow-up attendance
- face-to-face and non face-to-face attendance
- single and multi professional attendance.
-
The above terms are defined in the NHS Data Model and Dictionary.
-
Where a patient sees a healthcare professional in an outpatient clinic for a consultation this counts as valid outpatient activity, regardless of whether they receive any treatment during the attendance. NHS providers offer outpatient clinics in a variety of settings, and these should all be included in the cost collection where the cost is part of your operating expenditure (see How to obtain your cost quantum).
-
For the purposes of the NCC, outpatient clinical events submitted as part of the Commissioning Data Set (CDS) should be submitted as part of the OP feed. Any clinical events submitted as part of the Community Services Data Set (CSDS) should not be submitted in the OP feed.
-
The NCC does not distinguish between attendances that are pre-booked and those that are not.
-
The patient event is recorded under the same TFC for the appointment (for example a physiotherapist assessing an orthopaedic patient) regardless of whether they see the clinician they were referred to or another healthcare professional.
Maternity non-admitted patient care
- Hospital maternity attendances should be included in the OP extract. Maternity outpatient services include:
- hospital clinics (obstetric and midwifery)
- midwifery antenatal and postnatal care undertaken by NHS providers in GP surgeries and community-based clinics
- midwifery or other maternity community care contacts with patients in their own home
- ward attenders.
- Within the appointment (regardless of whether this has included a consultation) there may be costs for:
- routine scans
- routine screens and tests.
-
Processing of maternity outpatient activity by the costing grouper may result in an outpatient procedure if the data includes the appropriate OPCS codes. Diagnostic imaging should not be unbundled from outpatient procedures: the cost should be included in the cost of the patient event and therefore not reported on the SI feed.
-
The costs of sample analysis under a separate commissioner contract (such as genetic testing, biochemistry analysis, specialist diagnostic laboratories) should not be included in the obstetrics or maternity costs.
Paediatrics
-
Providers should allocate costs and activity to paediatric TFCs in line with their NHS Data Dictionary definition: “dedicated services to children with appropriate facilities and support staff”.
-
A few patients aged 19 years and over are also cared for by specialist children’s services. Such activity, where the patient is seen by a paediatric care professional, is assumed to use resources similar to those for children rather than those for adults and should be reported under the relevant paediatric TFC.
Therapy services
-
Where patients have been referred directly to a hospital therapy service by a healthcare professional, including a GP, or have self-referred and are seen in a discrete therapy clinic solely for the purpose of receiving treatment, the attendance should be submitted as outpatients as reported on the CDS.
-
Where these services form part of an inpatient event or outpatient attendance in a different specialty, the costs form part of the composite costs of that episode or attendance and should not be reported as a therapy outpatient attendance.
Wheelchair contacts
-
Wheelchair services remain at soft implementation level for 2024.
-
The wheelchair contacts (attendances to a clinic and home visits) will be collected in the OP extract with specific data items to identify the activity instead of relying on the TFC.
-
Wheelchair categories created for the purpose of the collection have been added to the OP table in the reference data. The wheelchair contacts should use the collection activity COM003 Wheelchair contact.
-
Wheelchair equipment costs should be submitted on the AGG feed. This includes repair and maintenance.
-
Wheelchair contacts should not be submitted in the CSCC file.
Mental health and community care contacts
Collection scope
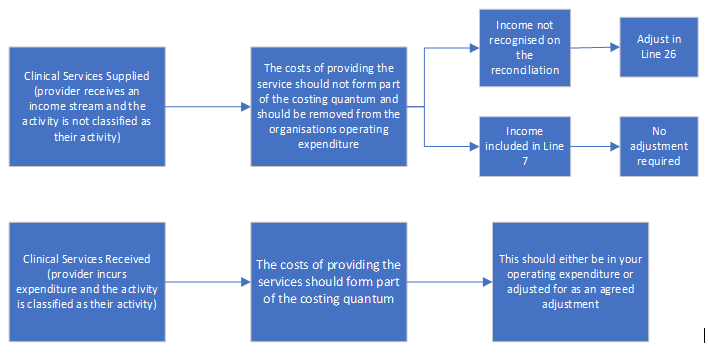
- All mental health care contacts (MHCC) and community services care contacts (CSCC) within the collection year are in scope of this collection as shown in Figure 2.
Figure 2: Scope of care contacts collected
-
Where a care contact starts in one costing period and ends in another (for example for night care), the start date determines whether it should be included in the cost collection, not the end date.
-
Missed appointments (DNAs) and cancelled care contacts should not be recorded and the cost should be treated as an overhead. Only attended care contacts are in scope for the PLICS collection.
Mental health care contacts
-
This section covers mental health non-admitted patient care contacts collected in the mental health care contact (MHCC) PLICS data feed.
-
Trusts that submit their acute services outpatient MH data to HES should submit their costs on the OP XML extract. If your MH care contacts are submitted to MHSDS, costs should be submitted on the MHCC ‘Feed Type: Patient-level costing care activity type code’.
-
Learning disabilities data that is submitted to MHSDS can be submitted in your NCC for 2024.
-
If you are unable to disaggregate learning disabilities or the data is not submitted to MHSDS then the costs can be excluded from the NCC in 2024 and should be recorded on the appropriate line of the INTREC.
Community services care contacts
-
This section focuses on community health services previously submitted at aggregate level on the CHS worksheet where the patient activity is mandated as part of the Community Services Data Set (CSDS).
-
Specialist acute non-admitted patient care activity in the community is part of the Commissioning Data Set (CDS), with a community ‘location’ and should be reported in the OP extract. The community location will be identifiable with an activity type location code that is the patient’s home or a community setting. The dataset is the method of identifying the cost collection file.
-
For the community sector in 2024 , cystic fibrosis drugs and high-cost devices remain as excluded items in the National Cost Collection and therefore should be on the XML reconciliation as an agreed adjustment. Please email the costing inbox costing@england.nhs.uk with ‘Agreed adjustment’ in the subject line.
-
Allied health professions, including podiatry, are in scope of the collection. These care contacts should be submitted to CSDS and will therefore flow in PLICS on the CSCC feed.
-
The services described in this section may be provided in various locations/settings in the community, such as a patient’s home, clinics, community hospitals, GP practices or health centres, and will include non-face-to-face contacts as recorded on the CSDS. Community rehabilitation is within scope of the patient-level collection, however the data feed for PLICS is determined by where the activity is submitted:
- Community nursing PLICS should be submitted on the CSCC feed. You should identify whether the activity is for:
- a community nurse as reported to the CSDS; for example district nurses or
- a specialist nurse who would normally be in an acute setting but is visiting a patient’s home for specialist care. These patient events may be reported on the CSDS, and if so, should be included in the CSCC file. If this specialist nursing is reported on CDS, the patient events should be included on the OP feed.
-
Daycare facilities are a community care contact and will use duration of contact to allocate the cost. They should be submitted on the CSCC feed if your trust’s activity data is submitted to CSDS. If your trust’s activity is submitted to CDS, not CSDS, the PLICS OP data feed should be used.
-
Several health services and checks are delivered in educational facilities. School-based children’s health services include all services provided in the school setting, not just school-based nurses. Community paediatricians may also contribute to these. Only NHS-funded school-based services should be included in the National Cost Collection.
Emergency care
Collection scope
- Emergency department (ED, formerly accident and emergency, A&E) attendances are categorised as:
- ‘DepTyp: Emergency care department type’:
- EDs (national code 01)
- consultant-led monospecialty A&E services, may be 24-hour or non 24-hour (national code 02)
- other types of A&E (national code 03), including minor injury units (MIUs) and urgent treatment centres (UTCs)
- NHS walk-in centres (national code 04)
- Same day emergency care attendance (national code 05)
- Urgent and emergency care extended care episode (national code 06)
- HRG subchapter VB emergency care.
Exceptions
- Emergency Care Data Set (ECDS) general practitioner (GP) streaming attendances should be costed as they form a part of the management for the emergency care department. The costs and activity of providing the service must then be excluded from the costed activity in the patient-level submission, and be reported in the reconciliation on two separate lines:
- EXC016 Emergency Care Streaming – provided by GPs only
- EXC017 Emergency Care Streaming in some fields – excluding GP costs.
- Costs and activity for minor injury units (MIUs) should be reported separately only if the MIU is:
- discrete (separate from ED) and the attendance is instead of and has not already been counted as an A&E attendance
- not discrete but sees patients independently of the main ED.
- Patients brought in dead (A&E patient group code 70 or ECDS discharge status SNOMED-CT code 63238001 Dead on arrival at hospital) should be coded, costed and submitted against HRG VB99Z Patient dead on arrival.
Implementation of the Emergency Care Data Set
-
The Emergency Care Data Set (ECDS) for urgent and emergency care is used to collect information from emergency care units across England.
-
We will continue to collect the data using the 2023/24 National Costs Grouper. This means that trusts have to map their data back to the old treatment codes for the grouper.
-
This mapping guidance helps with mapping back to the investigation and treatment codes for grouping purposes.
Cystic fibrosis
-
This section covers the cystic fibrosis (CF) year-of-care banding that adult and paediatric cystic fibrosis centres and other providers with network care arrangements should use for their NCC. Some organisations may use the term currency rather than banding.
-
We now collect CF patient events at patient level with a CF band code against each record. We no longer collect the cost in a full or part year of care format. Adult/child splits are derived centrally.
-
The Cystic Fibrosis Trust informs trusts how each patient will be categorised for the coming year. For costing purposes, this band will be applied to all patient events in that year.
-
The grouper generates cystic fibrosis specific HRGs (DZ13*, PD13*) and these patient events should be linked to a year-of-care CF banding.
-
To help improve the quality of these year-of-care costs, providers should:
- calculate the costs for each patient event against the 2024 calendar year bands, with no further local adjustment for bands
- apply the band from the Cystic Fibrosis Trust to each patient event in that year
- ensure the data from network care providers conforms with this banding before submission.
-
Under the year-of-care banding model, each patient is allocated to one of seven bands, derived from clinical information including cystic fibrosis complications and medicine requirements. Each band describes an increasingly complex year of care. See Specialised Services National Definitions Set (SSNDS) Definition No10: Cystic Fibrosis Services (all ages), 3rd edition and the Specialised commissioning section of the NHS England website more information. Providers should access their banding data from the registry through their lead clinician.
-
Band allocations are based on data from the calendar year before the next financial year and are issued each February. The 2024 calendar year bands issued by the Cystic Fibrosis Trust in February 2024 should be used for the 2024 NCC.
-
Cystic fibrosis is a chronic condition in which disease severity increases steadily over several years. Thus patients are unlikely to transfer between bands within a financial year.
Flowing cystic fibrosis in PLICS
-
The costs for all clinical events in 2023/24 should be submitted against the bands issued in February 2024.
-
Patients can be identified through:
- APC episodes with specific HRGs for cystic fibrosis – DZ13* or PD13*
- APC episodes with a primary diagnosis of cystic fibrosis although the HRGs may vary
- TFCs for adult cystic fibrosis service (TFC 343) and paediatric cystic fibrosis service (TFC 264), as described in the NHS Data Dictionary (these will mainly apply to outpatient attendances but could be applied locally to APC episodes)
- local clinic codes or wards for CF patients.
- The following costs should be included as clinical support costs to cystic fibrosis services:
- homecare support, including home intravenous antibiotics supervised by the cystic fibrosis service, home visits by the multidisciplinary team to monitor a patient’s condition (for example management of totally implantable venous access devices), collection of mid-course aminoglycoside blood levels and general support for patient and carers (there is no requirement to collect or code homecare support independently and flow as part of the PLICS extracts; any costs relating to homecare support should be treated as an overhead to APC and NAPC activity)
- annual review investigations.
-
We are aware the very few severely ill band 5 patients will have highly variable costs. Some requiring continuous intravenous antibiotics can manage their care at home with the support of the specialist team. Others may require prolonged (six months or more) hospitalisation for their administration. Such costs should nevertheless be included.
-
The following should not be included in the calculation of cystic fibrosis costs:
- the high-cost drugs, including antifungal medicines, on Annex A worksheet 14b of the NHS Payment Scheme: these should flow as part of the supplementary information (SI) feed
- unrelated care: this is assigned to the relevant HRG or TFC for example, obstetric care for a pregnant woman with cystic fibrosis, or ear, nose and throat outpatient review for nasal polyps: cystic fibrosis ICD10 codes are included in HRG complication and co-morbidity lists, and recognised in HRG4+ output
- insertion of gastrostomy devices and of totally implantable venous access devices; the associated surgical costs should be covered by the relevant separate codes
- costs associated with long-term nutritional supplementation via gastrostomy or nasogastric tube feeding: these remain within primary medical services so are an exclusion, to be reported on the EXC009 line of the reconciliation
- costs associated with all other chronic non cystic fibrosis-specific medication prescribed by GPs and funded from primary medical services (for example long-term oral antibiotics, pancreatic enzyme replacement therapy, salt tablets and vitamin supplements): these are also an exclusion, to be reported on the EXC009 line of the reconciliation
- neonates admitted with meconium ileus: they should be costed against the relevant HRG; annual banding should not be applied to the episode for which the neonate was admitted for initial surgical management
- patient transport services EXC005.
High-cost drugs for patients with cystic fibrosis
-
Funding for high-cost drugs is governed by national commissioning policies. The specialist centre initiates their prescription.
-
However, if they need to be used long term (as in bands 2A to 5), the responsible GP may be prepared to continue prescribing. Under these circumstances, and where the prescribing GP recharges the provider for the actual cost of medicines received, the provider should flow the cost of the drug into PLICS as part of the SI feed type.
Community maternity
- These attendances should be the patient events recorded in the patient administration system. The primary dataset for submitting maternity event activity is the Maternity Services Data Set (MSDS); however we are aware that in some trusts:
- the clinical event is not submitted to MSDS but to the Commissioning Data Set (CDS) or Community Services Data Set (CSDS)
- the clinical event is submitted to MSDS and submitted to either CDS or CSDS.
- The use of OP or CSCC feed type depends on where your trust submits the patient activity data:
- activity data submitted to CDS or MSDS should flow on the OP feed type
- activity data submitted to CSDS should flow on the CSCC feed type.
-
If the clinical event is duplicated across MSDS and CDS or CSDS, you should only submit the event once.
-
You still need to reconcile your submitted costed patient events to the dataset where the activity is submitted. This means you may need to reconcile to all three datasets or just one depending on how your trust is recording and submitting its activity data.
-
Providers should submit activity and costs for antenatal and postnatal contacts, home births, parentcraft sessions (usually a group event) and outpatient procedures. This care is provided mainly by midwives but other clinical professionals such as allied health professionals may record patient events under this service.
-
All community maternity contacts and home births should have an HRG code. If the record has not been clinically coded, you should submit UZ01Z. All records, where possible, for community maternity, health visitors and parentcraft contacts will also have a ‘Maternity contact type’ data currency submitted as part of the patient event.
-
Only the mother should be costed as part of OP community maternity.
-
Home birth babies are deemed to be ‘well babies’ and therefore will not have any cost. Where a baby born at home is unwell, they will be transferred immediately to a hospital neonatal unit and therefore have an admission recorded there.
-
Postnatal community maternity will normally include the cost of any review of the baby but if the contact by the community midwife is purely for the baby, the costed record should be that of the baby.
-
Health visitors also have separate contacts to review the baby. Patient events commissioned by local authorities should not be submitted as trusts are not mandated to submit patient events funded by non-NHS bodies.
-
Parentcraft contacts are usually a group session, so the cost of the session should be allocated across the mothers-to-be attending that session. The cost should not be allocated to birthing partners in attendance.
-
The costs of sample analysis taken during the community attendance (such as genetic testing, biochemistry analysis, specialist diagnostic laboratories) should be included in the midwifery costs.
-
One provider may provide all or part of the patient’s care or different providers may be involved in the patient’s maternity pathway. Each patient event should be costed separately for the patients they have seen at their organisation, irrespective of the income received for the pathway they follow.
- Payments between providers should not be netted off the cost of care.
Chemotherapy
- When the patient attendance data is run through the grouper, patients received a core HRG SB97Z and one or more extra unbundled chemotherapy HRGs, divided into two categories:
- HRGs for procurement of chemotherapy regimens according to cost band
- HRGs for the delivery of chemotherapy regimens.
-
For 2024 National Cost Collection HRG code procurement HRG codes SB01Z-SB10Z and SB16Z should not be submitted. Chemotherapy drugs should be collected from the pharmacy data as a component of the delivery patient event and reported at patient level on the SI feed type in the NCC.
-
The drug costs for chemotherapy services include cytotoxic medicines, monoclonal antibody medicines and supportive medicines as listed on the Supplementary information drugs and blood products list. The drug costs for this collection also include hormone therapies.
-
The day-case, regular day admission or outpatient attendance for delivery is the countable patient event. Where the delivery patient event is solely for the administration of chemotherapy, it will be collected on the APC extract or OP extract (according to the recorded point of delivery), with HRG code SB11-15Z or SB17Z. You should only use SB97Z where no unbundled HRG is created by the grouper.
-
Where the chemotherapy delivery is given during an overnight patient episode, there is no clinical coding in current coding guidance. This means there will be no delivery HRG and this cannot be submitted as a separate HRG in the NCC.
-
We expect most chemotherapy patient events to have only one delivery HRG although we are aware that in few circumstances, more than one delivery HRG is shown on the patient record. For the 2024 NCC you should only submit the most complex delivery HRG and all the costs of both deliveries should be shown against this patient episode or attendance.
-
If you have a core HRG that is not a chemotherapy HRG but chemotherapy did take place within the episode and therefore you have a SB HRG as well as a core HRG. You must not split and duplicate the episode as the data validation engine won’t accept duplicate episode IDs.
-
For these instances where the core HRG is not chemotherapy related you will need to submit the episode with the core HRG as generated by the grouper, but you can use the collection activity CHE001 chemotherapy to show that chemotherapy was administered and the cost will flag as a component cost of the core HRG.
Radiotherapy
-
For 2024 National Cost Collection we are collecting the planning and treatment HRG codes but not the core SC97Z HRG patient event where the treatment was delivered.
-
Radiotherapy data items counted in the costing process are split into two:
- The planning HRG generated by the grouper on the first treatment of the cycle represents all the cost spent planning for the treatment. It does not represent a patient attendance although there may be attendances for CT scans and other planning activities in the radiotherapy local system.
- The treatment HRG represents one patient attendance for the radiation to be administered.
-
Both planning and treatment HRGs are countable patient events, and both should have costs attached. These events will be shown with a HRG code in the national structure and should be submitted on the OP or APC extract depending on the point of delivery.
-
We expect one planning HRG per treatment cycle as generated by the grouper on the first treatment. If there are multiple planning HRGs you should only submit one per episode, using the most complex HRG. We do not collect the number of treatment cycles in the NCC but it is shown in the national radiotherapy dataset.
-
Whilst both the planning and treatment HRGs are countable patient events, if these occur on the same episode, we cannot accept trusts splitting planning and treatment HRGs under the same attendance identifier as the business rules will identify them as duplicate episodes and this will cause a validation failure in the data validation engine.
-
In these circumstances please only submit the treatment HRG as this would contain the majority of costs related to the patient event. Any planning costs can also be submitted under this HRG, using the collection activity radiotherapy planning to show that an element of the cost is related to planning.
-
Radiotherapy patient events are not coded by clinical coders in the same way as most services. Several years ago, as part of the systemic anti-cancer therapy (SACT) reviews, a mapping table containing clinical codes and HRG codes was agreed with the radiotherapy services and uploaded into the radiotherapy systems. This mapping table has been updated, and the radiotherapy clinical information system outputs should reflect these codes.
-
For 2024 NCC HRG code SC97Z is not required, as this core HRG does not exist in all trusts.
-
Please note: we have added depreciation to the collection resource list, as this cost has been identified as significant for the radiotherapy service. This collection resource has been added to the integrated technical document for the 2024 National Cost Collection and we would like it to be incorporated into this collection to support improved analysis of the service costs.
-
The national dataset Radiotherapy Dataset (RTDS) v6.0 is considered a more accurate source of reconciliation information than the Hospital Episode Statistics (HES) data, because not all radiotherapy data (core HRGs or unbundled HRGs) is submitted to HES. Access to draw down data may be limited, however you should be able to access the data sent to the RTDS from your local systems to populate the costing system and reconcile it to the collection files.
Renal dialysis
-
Renal dialysis on grouping, generates a core HRG and an additional HRG.
-
Where zero or minimal cost is to be allocated against the core HRG for discrete renal dialysis, you should exclude the core HRG from your PLICS return and include all costs against the renal unbundled HRG in the APC XML extract.
-
Where a patient had renal dialysis as part of a non-discrete renal admission, the core HRG must be reported on the APC feed type with the associated costs and the renal dialysis unbundled HRG with associated costs should be reported as an extra record on the APC feed type. For non-discrete renal dialysis, the renal unbundled HRG should have an adjusted length of stay of 0 days.
-
Outpatient activities associated with each dialysis modality should be separately recorded and matched to the outpatient attendance using Standard CP4: Matching costed activities to patients. For example, pathology testing or medicine prescriptions issued in clinics.
-
For dialysis using a hub-and-spoke configuration, the activity and costs should be recorded in the submission from the NHS provider with contractual responsibility for the delivery of the care.
Renal dialysis medicines
-
Renal dialysis medicines previously on the high-cost drugs list of the NHS Payment Scheme documents are now included on the Supplementary information drugs and blood products list.
-
Non high-cost drugs should be included as a component cost of the renal HRG.
-
Patients sometimes require medicines to treat associated conditions. These medicine costs should be attributed to the patient’s dialysis event when the medicines were administered. These can be identified from the medicines dispensed feed and submitted using the unbundled HRG and collection resource of medicines.
Renal patient transport services
- Patient transport services, which are a significant cost in haemodialysis services, are excluded from the NCC and therefore must be excluded from costs reported for renal dialysis services.
Specialist palliative medicine
- The specialist palliative medicine (SPM) service should be reported against the following settings:
- inpatient (ordinary elective or non-elective admissions, day cases and regular day or night admissions) on the APC feed type
- daycare on the APC feed type including regular day/night attenders
- outpatients on the OP feed type
- community:
- if the patient events are reported in the CDS, then on the OP feed type
- if the patient events are reported in the CSDS, then on the CSCC feed type.
-
Costed patient events should reconcile to those submitted to CDS/CSDS.
-
Where trusts have a SPM service partially funded by charity arrangements, the part cost flag should be used to show the patient event does not contain the full cost. If you are allocating your charity income across all patient events as it does not relate to a specific service, you should indicate part cost.
Admitted patient care – discrete specialist palliative medicine ward or hospice unit
-
A patient admitted on a discrete SPM ward should have a discrete episode under TFC 315 specialist palliative medicine service.
-
Paediatric episodes should be submitted using TFC 240 paediatric palliative medicine service.
-
Where there is a transfer of care to a new episode this represents the clinical responsibility for that patient by an SPM consultant.
-
Where no new finished consultant episode is created but a patient is transferred to a SPM ward, you should use ward activity WRD002 specialist palliative ward care and not WRD001 ward care.
-
The core HRG episode should be costed and submitted on the APC feed type: the SD HRGs should not be submitted.
Admitted patient care – non discrete specialist palliative medicine ward
- Where a patient is treated on another ward but received SPM support from the hospital SPM team, this care is called ‘non-discrete’.
- The core HRG must be reported on the APC feed type with the associated costs, under the original TFC. The costs for the SPM support should be reflected in the core HRG using collection activity OUT007 Hospital Specialist Palliative medicine supporting contacts, if recorded.
Discrete SPM outpatients including day therapy
- Outpatient attendances and day therapy under TFC 315 or 240 should be reported on the OP feed type, with the associated costs attributed to the outpatient HRGs (the subchapter of HRG codes starting with the letters WF).
Non-discrete SPM non-admitted patient care
- Outpatient attendances recorded under another TFC but with SPM support in that attendance should report in the OP feed type, the core HRG with the relevant costs, including the collection activity code OUT007 Hospital SPM supporting contact.
Specialist palliative medicine in the community
- Community SPM activity submitted to CSDS should flow on the CSCC feed type, using the currency codes starting N21 as listed in the extract specification.
Specialist rehabilitation
- For this cost collection, you should use the UK ROC level of specialist rehabilitation service. Levels 1 and 2 units are defined on the UK ROC list. All other trusts that provide rehabilitation not defined as level 1 or 2, will be a level 3 service.
Levels 1 and 2 admitted patient care
- Inpatient episodes should flow under the unbundled rehabilitation HRG, not the core HRG and should be submitted on the APC feed type as detailed in the extract specification.
- If you do not have the unbundled VC HRG subchapter then you should flow the core HRG for your APC rehabilitation.
- Inpatient activity for the Level 1 or Level 2 should be recorded as TFC 344 complex specialist rehabilitation service or TFC 345 specialist rehabilitation service.
- Four new data fields have been added to the APC extract specification as trusts must report:
- patient specialist rehabilitation complexity period status
- the rehabilitation complexity scale (RCS) scoring which is updated fortnightly by the rehabilitation service
- the start date of that RCS score or the bed day
- the end date of that RCS score or the bed day.
-
This will generate a ‘mini episode’ line per patient for every change in that patient’s RCS score.
-
The core patient event HRG should not be submitted as it should have zero cost.
-
It is best practice to submit your data at ‘mini episode’ level each time there is a change in RCS. However, if you are unable to split your activity data into ‘mini episodes’ at this level, you can submit your data as daily bed-day records in the APC feed type by submitting each day as a ‘mini-episode’.
-
If you do not have ‘mini-episode’ or bed-day level data available, you can submit the full patient episode. However, this should be avoided, if possible, as submitting in this way does not reflect a change in the use of resources in a patient’s rehabilitation episode.
-
If a patient receives non-discrete rehabilitation during an APC stay, this should be reported as a component of the core HRG using the collection activity OUT008 Specialist rehabilitation supporting contacts.
Level 1 and 2 outpatients
-
Outpatient rehabilitation assessments should be submitted under the unbundled specialist rehabilitation HRG and relevant TFC.
-
These patient events should be submitted on the OP feed type.
Spinal cord injury patients
-
National spinal cord injury services refer to the services provided by the eight designated specialist spinal cord injury centres (SCIC) in England for adults, young people and children who have sustained a non-progressive injury to the spinal cord or cauda equina.
-
National spinal cord injury services submit information to the national spinal cord injury database rather than to UK ROC.
-
Spinal cord patients will not generate a UK ROC rehabilitation complexity scale but they do get a category on the national spinal cord injury database and a new data field has been added to the APC feed in the extract specification as trusts must report the category of the spinal cord injury patient.
-
Similarly to rehab APC attendances, you can choose to submit your data at episode, mini-episode or bed day level in the NCC.
Level 3 admitted patient care (including community inpatients)
-
Inpatient episodes should flow in PLICS under the rehabilitation HRG, not the core HRG.
-
Most inpatient episodes will get TFC 314; however, other TFCs can be used for rehabilitation patients.
-
The core HRG should not be submitted.
-
If a patient receives non-discrete rehabilitation during an APC stay and that contact is captured on your patient data feed but does not result in an unbundled VC subchapter HRG, this should be reported as a component of the core HRG using the collection activity OUT008 Specialist rehabilitation supporting contacts.
-
Level 3 patient events do not get a UK ROC rehabilitation complexity scale so there is no requirement to submit this data field for level 3 patients.
Level 3 outpatients and community
-
Outpatient rehabilitation should be submitted under the specialist rehabilitation VC sub-chapter HRG and TFC 314 rehabilitation medicine service. The core WF HRG should not be submitted. These patient events should be submitted on the OP feed type.
-
For community rehabilitation the requirements for submission depend on where the activity data is submitted in your trust:
- If community rehabilitation activity is submitted to CSDS (Information Standard DAPB1069), the costs should flow on the CSCC feed type.
- If community rehabilitation activity is submitted to CDS (Information Standard DAPB0092), the costs should flow on the OP feed type.
- The currency codes for the community rehabilitation team are SCRT, NCRT, MCCRT and OSCCRT.
Complex paediatric rehabilitation
- You should record paediatric rehabilitation patient events as ‘Patient assessed but onward treatment not assigned a specialist rehabilitation complexity score’ for submission purposes.
Specialist ward care
Flowing adult, paediatric and neonatal critical care in PLICS
-
Adult, paediatric and neonatal critical care submitted via the specialist ward care (SWC) feed is now mandatory for providers already mandated for their APC patient events.
-
The SWC feed type requires all costs to be submitted on a calendar bed-day basis within the costing period.
-
Patients admitted to any critical care facility as defined by the NHS Data Dictionary must, in addition to their APC record, have a Critical Care Minimum Data Set (CCMDS) for adults, Paediatric Critical Care Minimum Dataset (PCCMDS) or Neonatal Critical Care Minimum Data Set (NCCMDS) record. The records are captured in the critical care mandated dataset as follows:
- CCMDS – per period
- PCCMDS or NCCMDS – per bed day.
- The grouper produces an unbundled critical care HRG regardless of the mandated dataset it is submitted to:
- For adults, the HRG shows the highest level of care for that patient during the CCMDS period. For the adult critical care cost collection, this HRG will be shown on each submitted day of critical care.
- For paediatric and neonatal, the grouper calculates a separate HRG for each bed day. These patient bed days may therefore show a different HRG on each submitted day of the critical care period and you do not have to submit the number of organs supported for those bed days.
-
A patient of any age admitted to hospital will have an APC dataset record for their hospital admission, and this produces a core HRG. If the patient’s stay includes a period of critical care, this produces an unbundled critical care HRG per critical care bed day.
-
All critical care submitted via SWC is linked to APC using the PLEMI. Where the patient spent their whole admission in the critical care unit, the result of unbundling cost is an episode with zero or minimal cost allocation against a core HRG. Providers should exclude the core HRG and include all costs against the unbundled HRGs collected within the SWC feed.
-
In 2024 all critical care periods should be costed per day of the critical care period against the unbundled critical care HRG, and each day should have a separate record submitted in the SWC.
-
Part day costs can be applied to the critical care HRG if the patient is discharged directly from critical care or dies while in critical care. For patients discharged from the critical care bed to a non-critical care ward, the costs relating to the non-critical care ward should be bundled into the cost of the critical care bed day. Please refer to Standards IR1 and CM6, for details of how a critical care record should be created and costed.
-
Critical care units may be discrete or in a specific area on a general ward, defined in the CCMDS, PCCMDS or NCCMDS as non-standard location using a ward area. The unit function code determines the type of ward. It is important to use the full range of unit function codes to ensure the data is accurate and comparable.
-
Where a patient is moved from a critical care area to a general ward area (or vice versa), the day of the move should be classified as a critical care bed day, in the same way as the part of a calendar day is included in the critical care period for the CCMDS, PCCMDS and NCCMDS. In terms of length of stay, the day of transfer from critical care should be counted as a critical care bed day. All trusts must comply with this even if submitting aggregate critical care costs.
-
All collection resources and activities (including the general ward costs) should be linked to the SWC feed. The costs should be attached to the day they occurred during the critical care episode. On the day of discharge, transfer or death, all costs relating to that patient (even if outside critical care) should be linked to the critical care bed day that started at midnight of the day of discharge, transfer or death.
-
The admission or discharge date of the critical care period should be ignored if it is outside the costing period. Only the days of the critical care period within the financial year should be submitted. See Figure 3 below.
Figure 3: Critical care bed days to be reported
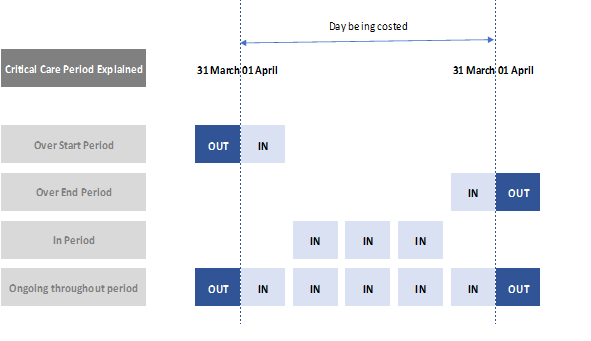
-
The critical care period is calculated by including the critical care local identifier. Therefore, the critical care length of stay (number of bed days) does not need to be calculated and submitted separately. It is calculated after submission by counting the number of rows per critical care local identifier submitted on the SWC feed.
-
The costs of any theatre time must be reported against the core HRG and not the unbundled critical care HRG.
- If a patient’s TFC changes on their admission to a critical care unit, a new finished consultant episode (FCE) will begin; theatre costs will be part of the previous FCE and will not form part of the cost for the critical care service
- If a new finished consultant episode does not start for a patient on admission to critical care or a patient is wholly under a critical care consultant from admission to discharge, theatre costs should still be excluded from critical care and reported against the core HRG.
-
The costs of relevant high-cost drugs or high-cost blood products should be included in the SI feed only.
-
Costs for critical care periods, or part thereof, that produce an unbundled HRG of UZ01Z should be reported against UZ01Z and not apportioned elsewhere.
-
The costs of adult critical care transport network services are excluded from the NCC and should be reported on EXC015.
Adult critical care
- For the 2024 National Cost Collection, adult critical care costs should be submitted at patient level for mandated acute trusts, in accordance with the PLICS data extract. These costs should include those for:
- critical care units
- high dependency units.
-
The grouper will only output one adult critical care HRG code per critical care period. Adult critical care HRG codes reflect the number of organs supported over the critical care period.
-
For 2024, providers should submit the HRG calculated by the grouper for the period, against each bed day record in the SWC feed. Providers should submit the number of organs supported per day in field ‘OrgsSupp: Number of organ systems supported’.
-
Adult critical care outreach teams who operate outside the parameters of the adult critical care unit should be reported as a cost component of the core HRG of the patient, and not be reported as a separate total cost or as part of critical care. These patients will not have a CCMDS record.
-
Example patient journey scenarios illustrating the treatment of adult critical care in 2024 are shown in a learning extension on FutureNHS.
Paediatric critical care
-
The Paediatric Critical Care Minimum Data Set (PCCMDS) version 2.0 must be used to inform the reporting of costs against the unbundled HRGs XB01Z to XB09Z.
-
Paediatric critical care HRGs are each grouped to show the cost of a single bed day.
-
For 2024 the costs per bed day per patient should be submitted in the SWC feed.
Neonatal critical care
-
Data supplied to the Neonatal Critical Care Minimum Data Set (NCCMDS) version 2.0 (2016 release) must be used to inform the reporting of costs against the unbundled HRGs XA01Z to XA05Z.
-
Neonatal critical care HRGs are each grouped to show the cost of a single bed day.
-
For 2024 the costs per bed day per patient should be submitted in the SWC feed.
-
HRG XA06Z relates to neonatal critical care transport and should be submitted in the AGG feed with the total cost and activity of patient journeys.
-
The HRGs are based on the British Association of Perinatal Medicine’s categories of care 2011 standards and use minimum required staffing levels to differentiate the anticipated resource intensiveness of the care delivered. These estimated proportional cost relationships were updated in 2021 by the Neonatal expert working group with the National Casemix Office and the NHS England costing team.
-
We have adjusted the information for costing use and if you have no more detailed information from your clinical teams, you should use the following weightings as a guide to the proportions of each HRG. The cost of medical and nursing staff costs, equipment and drug costs associated with the intensity of care required for a patient will be:
- XA01Z is at least four times that of XA03Z
- XA02Z is at least twice that of XA03Z
- XA03Z and XA04Z are similar
- XA05Z is less than that of XA03Z/XA04Z but not less than that of providing a standard paediatric/neonatal bed day.
- Diagnostics and supporting contacts from other services should be matched to the patient bed day, and not included in these weightings.
Supplementary information
- The supplementary information (SI) feed captures the costs of elements that go alongside the package of care. It should therefore include:
- high-cost drugs and blood products, including chemotherapy drugs and hormone therapies
- high-cost devices (formerly excluded devices)
- unbundled diagnostic imaging
- virtual wards.
-
High-cost drugs, high-cost blood products, high-cost devices and virtual wards are only submitted in the SI feed: they should not be included in the cost of the patient event. This means no high-cost items are in any other PLICS feed.
-
Diagnostic imaging should be included as a component cost in the core episode, attendance or period, except when occurring as an outpatient attendance. In the latter setting, the scan will have been unbundled from the core event and should be reported on the SI feed. For further detail, see NCC extract specification, worksheet ‘Reference data – HRGs’.
-
The currencies for high-cost drugs and blood products, high-cost devices and unbundled diagnostic imaging are mandated in the extract specification, so the alternative types of currency can be flowed as one extract without risking the lines of data being submitted without currency information. However, the data validation engine will test that the currency is included in the SI record to ensure the mapping of the currencies is accurate.
High-cost drugs and blood products (CSIU 01)
- This section covers the submission of the following drug elements:
- high-cost drugs
- high-cost blood products.
-
The SI drugs and blood products list in the data extract specification should be shown separately to the core patient event by inclusion on the SI feed. This list has been created from combining worksheet 14b of the NHS Payment Scheme high-cost drugs list, the specialised commissioning drugs list and the specialist commissioning chemotherapy taxonomy list.
-
The cost of these high-cost drugs and blood products should be submitted on the SI feed in the NCC using the following collection activities:
- BLD003 Transfusion of high-cost blood products
- PHA008 Consumption of high-cost drugs.
-
Chemotherapy drugs should be included in activity PHA008.
-
There are three ways drugs are reported in the NCC: patient-level high-cost drugs (PHCD), high-cost drugs (HCD) and patient-level specialised commissioning drugs (PSCD). These initials prefix the ‘drug code’ in the extract specification tab ‘Ref data – currency codes’
-
Using your organisation’s local pharmacy system, you need to collect the detail of the drug or blood products issued and map it to the PLEMI as per the extract specification, recording each issue as a separate row in the SI feed.
-
You should not include the cost of high-cost drugs and blood products in core patient events in the Emergency Care, Admitted Patient Care, Outpatient, Specialist Ward Care, Mental Health Provider Spells, Mental Health Care Contact, IAPT or Community Services Care Contacts feeds.
-
Where a high-cost drug cannot be administered without the addition of a non high-cost drug, then the non high-cost drug element of cost should also be counted with the cost of the high-cost drug. This includes on-costs such as dispensing.
High-cost devices (CSIU 02)
-
High-cost devices are expensive and are paid for on top of the national price (NHS Payment Scheme) for the procedure in which they are used. Relatively few centres procure the devices, and we recognise the costs would not be reimbursed fairly if they were funded through the NHS payment scheme alone.
-
Providers have three methods for procuring NHS Payment Scheme high-cost devices:
- transactional model introduced in 2016 and operated by NHS Supply Chain: orders are made by suppliers as zero cost. Rather than each provider paying for the devices and being reimbursed by NHS England as before, providers place orders with NHS Supply Chain at zero cost to them. NHS Supply Chain then places the order with suppliers and invoices NHS England
- local procurement model used by trusts: the purchase value to the provider is invoiced to the commissioner
- MedTech innovation devices – the provider purchases the device and is reimbursed by local commissioners.
- If used at your organisation, you should also include the cost of the three MedTech innovation funded devices on the SI feed:
- gammaCore
- HeartFlow
- subcutaneous engineered stabilisation device.
-
To ensure all providers cost the inpatient HRG in the same way, high-cost devices and MedTech innovation devices should be excluded from the HRG costs and flowed as part of the SI feed.
-
The list of devices is defined in the NHS Payment Scheme and the MedTech funding mandate.
-
Each item should have a separate record and the number issued (activity count) should be included in the extract under the relevant XML field.
-
If you are unable to separately identify and map the costs of these high-cost devices, please e-mail costing@england.nhs.uk.
-
Where zero or minimal cost is to be allocated against a core HRG as a result of unbundling costs in PLICS, you should exclude the core HRG from your PLICS return and include all costs against the unbundled HRGs in the SI feed.
High-cost devices – exceptions
-
Cardiology loop recorders are not on the SI drugs and blood products list. This has been queried by providers during the submission process. Loop recorders are implantable, single use devices and their cost should be matched to the patients who had one fitted. Therefore, loop recorders should be mapped to the patients who had HRG EY12A or EY12B and not included in the SI feed.
-
Cochlear implant devices are also not on the SI drugs and blood products list, and should be included in the NCC, matched at patient level to the patients who received them, using the collection resource of medical devices, and not included on the SI feed. This will allow users of the NCC data to view the cost of the episode or spell with or without the cost of the implant.
Unbundled diagnostic imaging (CSIU 03)
- Diagnostic imaging is unbundled from the attendance cost and should be reported separately when occurring in the following settings:
- outpatients first/follow-up attendances
- direct access
-
The costing process in the standards requires diagnostic imaging costs to be matched to the patient attendance or episode using the diagnostic imaging collection activities.
-
On collection, however, the cost of the unbundled HRG for outpatient attendances must flow as part of the SI feed.
-
Diagnostic imaging should not be reported separately when occurring in APC or MHPS, as part of an emergency care or outpatient procedure attendance or as part of an MHCC or IAPT contact. The costs should be included within the core episode, and you should ignore any unbundled diagnostic imaging HRGs produced by the grouper. Similarly, the costs of diagnostic imaging in critical care, rehabilitation or specialist palliative medicine should be included in the unbundled critical care, rehabilitation or specialist palliative medicine HRG. It is unlikely diagnostic imaging scans would be part of the cost of a community care contact, but if they are matched to this patient event they should be shown as a component cost of the care contact.
-
Some diagnostic imaging is not coded in a way that generates an unbundled diagnostic imaging HRG. For example, a correctly coded obstetric ultrasound in maternity outpatients is likely to group to one of the obstetric/maternity core HRGs. Costs and activity for these scans should not be unbundled but reported within the generated core HRG.
-
Plain film X-rays have no unbundled HRG. When occurring in APC, MHPS, OP, CSCC, MHCC or IAPT settings, their costs should be included in the core attendance. If the patient has an X-ray as a result of a direct access referral, the costs should be reported separately in the AGG feed.
-
Diagnostic imaging linked to an outpatient event should be linked to the outpatient event in which the imaging was requested using the PLEMI.
-
If you are unable to accurately assign a PLEMI, the cost should be treated as unmatched and recorded in the AGG feed.
-
The unit cost is per examination.
Wheelchair services (CSIU 04)
-
Wheelchair equipment should be submitted via the AGG feed in 2024 NCC.
-
Wheelchair equipment consists of repair and maintenance components without a contact. This will include the costs of the chairs, adaptations, seating, batteries and accessories, which are part of the service package of care.
-
The CSIU 04 has been left in the extract specification as a place holder for future use in PLICS.
-
The wheelchair equipment categories in the AGG feed are based on the national currencies for wheelchair equipment. Each item of equipment issued to the patient should be reported as a separate record with the corresponding Wheelchair Equipment Currency code (UnCur) included in the extract under the relevant XML field. The list of available currency codes is available in the extract specification.
-
Only the cost of the equipment issued should be recorded in the AGG feed. Any cost or activity related to the clinicians issuing or fitting the wheelchair should be separately recorded in the OP feed.
- There may be some wheelchair equipment on the AGG feed that has no corresponding OP record. This is because some wheelchair equipment is issued to the patient/carer without a corresponding appointment.
Virtual wards (CSIU 05)
-
Virtual wards allow patients to get the care they need at home safely and conveniently, rather than in hospital. The NHS is increasingly introducing virtual wards to support people at the place they call home, including care homes.
-
In a virtual ward, support can include remote monitoring using apps, technology platforms, wearables and medical devices such as pulse oximeters.
-
As the patient’s finished consultant episode doesn’t end, we want to identify which patients’ costs may be affected by not being in a hospital bed.
-
To collect these costs, you should submit the virtual ward episode via the SI feed and this activity can then be linked via the PLEMI.
-
For more information about virtual wards see our briefing paper on FutureNHS.
Talking Therapies for Anxiety and Depression
-
All Talking Therapies care contacts (attendances) should be submitted in the PLICS files as noted below. All attended Talking Therapies appointments within the collection year are in scope of this collection. Data for long term care/ Talking Therapies integrated services pilots is not in scope.
-
All Talking Therapies activity recorded through the IAPT dataset v2.1 should be reported on the IAPT feed. Talking Therapies care contacts (attendances) use the same cluster definitions as other mental health contacts, but we expect most Talking Therapies patients to fall into clusters 01 to 08.
-
All attendances within the collection year are in scope of this collection. To separate the data extract into appropriately sized files, it must be split into 12 monthly files which cover the reporting period, using the ‘Care Contact Date’ field (see Submitting PLICS files for further details).
-
All costs open referrals in the collection year must be reported, regardless of whether they relate to patients whose referrals have not started or have not been completed within the collection year. In addition, referrals that have started and finished in a previous reporting period and have follow-up attendances in the current collection year should also flow.
-
The number of attendances relates to contacts with the patient only – face-to-face, by telephone (where it replaces a face-to-face contact), or through other methods such as email where recorded in the IAPT dataset.
-
Only attendances with staff members within the IAPT dataset and your cost quantum should be counted.
-
Missed attendances (DNAs) and cancelled attendances should not be recorded, and the cost should be treated as an overhead.
Aggregate data
- In costing, some clinical events should not be submitted at patient level because:
- volume of data for little cost is prohibitive
- the activity cannot be matched to the core clinical event or
- the patient should not be identified due to the nature of their procedure or diagnosis (legally restricted sensitive data).
-
Aggregate data is submitted by currency at a higher level than the patient level feeds. It is high-level data acquired by combining and then summing individual lower-level data in a single average cost per unit per currency.
-
To submit aggregate data, the service should be costed in the costing system, and then the total cost and total number count of events aggregated to the currency level. There is no requirement to submit individual patient events, a breakdown of the resources used or a breakdown of the activities undertaken.
-
A new feed type ‘AGG’ has been added to the extract specification for aggregate data to be collected in an XML format.
-
Fields in the AGG feed type are mostly consistent with the other feed types. However, four new fields have been added:
- Aggregated currency scheme in use
- Aggregated currency
- Total aggregate cost
- Total aggregate volume (activity).
- The AGG (aggregate) feed type should be used to submit:
- direct access diagnostic services
- direct access plain film x-ray
- direct access pathology services
- unmatched support services
- legally restricted sensitive data (LRSD)
- high-cost drugs and blood products for HIV, AIDS and sexually transmitted disease (STD)
- reproductive medicine
- gender reassignment
- cancer MDT
- direct access audiology
- critical care transport
- national screening programmes
- community dental services.
- The part cost flag should be used in the AGG feed type to show any currencies events that do not represent the full cost of the service because other providers are providing some of the resource. This means you may submit some currencies twice.
Direct access
-
Diagnostic and pathology services undertaken during APC, OP, CSCC or EC are are included in the composite cost of those patient events, unless they are unbundled imaging which should be flowed into PLICS in the SI feed type.
-
Where these services have been requested directly from a GP, they should be submitted on the AGG feed type under Aggregated currency scheme in use = 01, 02 or 03.
-
Costs and activity for the direct access services should be submitted based on the total number of tests in each currency.
You may submit pathology costs against integrated blood sciences (PATH03) or separately against clinical biochemistry (PATH04), haematology (PATH05) and immunology (PATH06), but not both.
Unmatched support service costs
-
All unmatched pathology, drugs, blood and imaging should follow the process outlined in Standard CP4: Matching costed activities to patients where it states that you should identify it as ‘unmatched’ and not allocate the cost or items to other patient events.
-
All unmatched support costs should be submitted on the AGG feed type under Aggregated currency scheme in use = 04.
-
For radiology:
- Use the TFC from the diagnostic imaging feed and the appropriate radiology currency including plain film.
- Only use TFC 812 diagnostic imaging service where no TFC exists on the imaging feed.
- You should submit the activity count based on the total number of tests in the reporting period.
- For pathology:
- You should submit pathology by lab type.
- Use TFC 999 unknown.
- You should submit the activity count based on the total number of tests in the reporting period.
- For unmatched high-cost drugs, blood and devices:
- You should submit the unmatched issues currency code for the products dispensed.
- You should submit the activity count based on the total number of issues per product.
Legally restricted sensitive high-cost drugs, devices and blood products
-
Where a product cannot be submitted with patient-level detail because their procedure or diagnosis is legally restricted and/or sensitive, you will have to submit these costs at aggregate level.
-
The list of excluded local specialty codes, HRGs, OPCS and ICD10 codes can be found in a learning extension on patient-level costing collection activity on FutureNHS.
-
It may be the product itself is classed as legally restricted and/or sensitive or it may have been issued to a patient whose diagnosis or procedure has been classified as legally restricted and/or sensitive.
-
Both conditions noted above should be submitted on the aggregate feed type (AGG) under Aggregated Currency Scheme in Use = 05.
Legally restricted sensitive patient event data including in vitro fertilisation
-
Trusts cannot submit data at patient level for patients receiving services or treatments for which data is clinically coded as LRSD.
-
LRSD covers specific treatment and diagnosis categories. These can be found in a learning extension on FutureNHS and should be submitted as follows:
- HIV, AIDS and STD should be submitted on the aggregate feed type (AGG) under Aggregated currency scheme in use = 06
- gender reassignment should be submitted on the aggregate feed type (AGG) under Aggregated currency scheme in use = 08
- reproductive medicine should be submitted on the aggregate feed type (AGG) under Aggregated currency scheme in use = 07.
-
Only patients who have a primary diagnosis resulting in a LRSD HRG code should be submitted.
-
Where patients have a HRG code that is not on the LRSD list on the extract specification reference data under Aggregated currency scheme in use 06, 07 or 08, but have a secondary or subsequent diagnosis which meets the LRSD requirement, these patients should be submitted in the AGG feed type using the relevant ACSIU and the legally restricted sensitive data indicator.
-
The total activity count should be submitted as follows:
- APC: total number of episodes per reporting period per currency
- OP: total number of attendances per reporting period per currency.
- Where a patient has a legally restricted sensitive characteristic, but they are admitted/treated for a diagnosis that is not for treatment of the LRSD characteristic, these patients should be submitted in the AGG feed type using the relevant ACSIU and the legally restricted sensitive data indicator.
Cancer multidisciplinary meetings
-
The National Institute for Health and Care Excellence (NICE) considers cancer multidisciplinary teams (MDTs) essential to the delivery of high-quality cancer care.
-
For acute PLICS, these costs should be allocated to the cancer MDT activity and submitted on the AGG feed, submitted as part of the OP or other patient-level submission.
-
Providers should submit data against six categories of cancer MDT:
- breast
- colorectal
- local gynaecological
- specialist gynaecological
- specialist upper gastrointestinal
- other cancers: to include lung, haematological, brain.
-
Cancer MDT meetings bring together representatives from different healthcare disciplines on a formal timetable to discuss cancer patients. The purpose of these meetings is to review individual patients and agree individual treatment plans for initial and ongoing treatment. The core role of the cancer MDT is to resolve difficulties in diagnosis and staging, and to agree a management plan.
-
Cancer MDT meetings are additional to, not instead of, outpatient activity. Cancer outpatient clinics are often multidisciplinary and, similarly, cancer MDTs can address one type of cancer or a group of different cancers.
-
We are aware that cancer MDTs may no longer discuss outpatients exclusively. We will continue to collect activity and costs for all patients discussed in cancer MDTs in the defined groups (above) in 2024.
-
The unit cost is per individual patient treatment plan discussed. Cancer MDTs always have a defined consultant lead who chairs the meeting and ensures treatment decisions are recorded.
-
Include consultant costs based on job plans, preparation for peer review, support staff costs and administration costs, such as arranging cancer MDT-initiated investigations and follow-up clinics. Exclude costs for follow-up actions such as communicating the cancer MDT outcome by phone to the patient.
- Although the members of a cancer MDT may be drawn from several NHS providers, only the organisation hosting the meeting must report the costs, including its own team and support costs.
Direct access audiology
-
Direct access audiology, where the care does not have a grouped HRG code, should be reported in the AGG feed, using the audiology department data item.
-
Audiology attendances with a grouped HRG can be submitted in the OP file at patient level.
Neonatal and Paediatric Critical care transport
- The Critical care aggregate currency scheme in use (ACSIU) captures the costs and activity of neonatal and paediatric specialist transport for critically ill children and babies. In 2024 this data will be captured at an aggregate level via the AGG feed of the integrated extract specification using ACSIU 11 and the appropriate HRGs (XA06Z for Neonatal and XB08Z for Paediatric).
National screening programmes
- The cost and activity of five of the national screening programmes will be captured separately via the AGG feed of the integrated extract specification in 2024. The full list of screening programmes can be found here – NHS screening – NHS (www.nhs.uk) – but for the 2024 NCC the programmes to be submitted via the AGG feed are as follows:
- NHS abdominal aortic aneurysm screening programme
- NHS breast screening programme
- NHS cervical screening programme
- NHS bowel cancer screening programme.
- They will be submitted in the AGG feed using ACSIU 12 and the relevant currency for the specific screening programme, the activity count will be number of screening appointments carried out.
Community dental services
- Community dental services are for patients who have difficulty getting treatment in their ‘high street’ dental practice and need to be referred for treatment. The currencies are:
- Community dental services: community dentistry for patients who are unable to access NHS dentistry locally, require specialist intervention or need a home visit. Include here the costs and activity of face-to-face dental officer activity in clinics and the screening contacts that these officers carry out in schools (each screened child constitutes a contact since each requires one-to-one activity). The unit cost is per care contact.
- General dental services: some community providers provide a full range of
- NHS dental treatment for patients in a high street setting. The unit cost is per attendance.
- Emergency dental services: also known as dental access services. The unit cost is per attendance.
- In each case the countable event is per care contact – regardless of the units of dental activity (UDA) that may be counted in that contact. The list below covers the activity count for each item to be submitted in the AGG data feed plus ACSIU code and definition:
- 01 Direct access diagnostic services: number of tests
- 02 Direct access plain film x-ray: number of tests
- 03 Direct access pathology services: number of tests
- 04 Unmatched support services: number of tests/issues
- 05 Legally restricted/sensitive high-cost drugs and blood products: number of issues
- 06 HIV, AIDS and STD: number of attendances/episodes/contacts
- 07 Reproductive medicine: number of attendances/episodes
- 08 Gender reassignment: number of attendances/episodes
- 09 Cancer MDT: number of patient treatment plans discussed
- 10 Direct access audiology: number of attendances/hearing aids fitted
- 11 Critical care transport: number of patients transported
- 12 National screening programmes: number of tests
- 13 Community dental services: number of attendances/contacts
- 14 Community diagnostic centres: number of tests
- 15 Aggregate Wheelchair Equipment: number of issues
- 16 Admitted patient care: number of episodes
- 17 Outpatient care: number of attendances
- 18 Emergency care: number of attendances
- 19 Mental health provider spells: number of spells
- 20 Mental health care contacts: number of contacts
- 21 IAPT: number of contacts
- 22 Community care contacts: number of contacts
- 23 Community maternity: number of contacts
- 24 Critical Care: number of bed days
Other considerations
Unmatched pathology, drugs, devices, blood and radiology data
-
All unmatched pathology, drugs, blood and imaging should follow the process outlined in Standard CP4: Matching costed activities to patients and allocate any remaining unmatched activity to ‘unmatched’.
-
For radiology, pathology and drugs on the Supplementary information drugs and blood products list – submit the costs under Aggregated Currency Scheme In Use code 04 – unmatched support services. The POD can be left blank for unmatched support services and TFC 999 should be used if there is not a more appropriate option available in the data.
-
Unmatched drugs that are not listed on the SI drugs and blood products list should be absorbed as an overhead to the relevant service.
Miscellaneous scenarios – excluded TFCs
- The costs relating to TFC 424 (well baby service) should be reported under TFC 501 (obstetrics service) or TFC 560 (midwifery service). The activity should be excluded.
Zero cost HRGs in PLICS
-
Zero cost HRGs are clinical events that are counted in the absence of cost because their cost is linked to an unbundled HRG.
-
Activity relating to the same patient episode is linked through the core EC/APC/OP PLICS activity records.
-
The flow of the activity records for these zero cost HRGs enables the demographic information to be taken from HES data, as shown below:
- PB03Z Healthy baby: The costs relating to TFC 424 (well baby service) should be reported under the mothers TFC 501 (obstetrics service) or TFC 560 (midwifery service). The activity for well babies should be excluded.
- RD97Z Diagnostic imaging core HRG: Costs should be reported under the unbundled radiology HRG. It should be flowed within the relevant OP extract as a count of the clinical event activity.
- RN97Z Nuclear medicine core HRG: Costs should be reported under the unbundled HRG. It should be flowed within the relevant OP extract as a count of the clinical event activity.
Data validation engine for XML files
- You must only use the NHS England data validation engine (DVE). All the essential information about the DVE is on FutureNHS.
Annex 1: Excluded services
| Excluded service | Definition or description | Why is the service excluded? |
Hosted services (CM23) | Services hosted by one provider but providing benefit for the patients of other providers. The specified services are:
| There is no patient event to which costs can be allocated. The host provider is fully funded, and there is no recharge to other providers. |
| Limb fitting services (formerly discrete external aids and appliances) | This exclusion is intended for discrete services such as artificial limbs or eyes, and covers the costs of both the services and the appliances. It is not intended for aids such as synthetic wigs, custom footwear or orthoses that are an integral part of the care plan for services such as podiatry and that are provided during an admitted patient episode or outpatient attendance. | No suitable currencies exist. |
| Health promotion programmes | Health promotion programmes are delivered to groups rather than individuals and directed towards particular functions (such as parenthood), conditions (such as pre-diabetes) and aspects of behaviour (such as drug misuse). | We are considering suitable activity measures with a view to collecting unit costs in future cost collections. |
| Home delivery of medicines and supplies: administration and associated costs and drugs, supplies and associated costs | This exclusion includes all costs of home delivery, even those classified as high cost. This includes home ventilation devices. Providers incur costs in delivering drugs, oxygen, blood products or supplies directly to patient’s homes, without any associated clinical activity at the time of delivery. On this line, providers should include the administration and associated costs relating to home delivery of drugs and supplies, including:
| There is currently no national requirement to understand the unit costs of providing this service. Where the medicine is on the high-cost drugs list or a chemotherapy drug but is also delivered as homecare. You should exclude as homecare. |
Hospital travel costs scheme (HTCS) and Patient transport services (PTS) | A scheme offering financial help with the cost of travel to and from hospitals and other NHS centres. Note that overnight stays are not part of the HTCS. However, the HTCS guidance states: “Where an overnight stay away from home is unavoidable, either because of the time of the appointment or length of travel required, and the patient is to meet the cost of this stay, the expense should be treated as part of treatment costs or met through non-Exchequer funds. This should be discussed with the relevant ICB before the overnight stay occurs”. Providers should therefore include overnight stays as a support cost in their submission. All costs associated with services run by ambulance trusts and other PTS providers offering transportation of patients to and from their place of residence, premises providing NHS healthcare and/or between NHS healthcare providers for people who have a medical need. Where one trust provides a PTS for another trust, this is a commercial activity. The cost will be excluded from the submission, but the income should not be netted off in the presentation of the cost of PTS in the reconciliation. Please note: patients transported between an organisation’s own sites are a support cost to the admission. | The HTCS scheme makes fixed payments to eligible NHS patients, there is no requirement to understand or benchmark provider unit costs. PTS were included in reference costs between 2006/07 and 2009/10, and excluded from 2010/11. Consultation with the sector suggests that collection of this data would be very complex. |
| Learning disabilities | Learning disabilities data that is submitted to MHSDS can be submitted in your NCC for 2024. If you are unable to disaggregate learning disabilities or the data is not submitted to MHSDS then the costs can be excluded from the NCC in 2024 and should be recorded on the appropriate line of the INTREC. | Under consideration for further inclusion in future collections. |
| Specified services: mental health providers | The following services delivered by mental health providers:
| No suitable currencies exist. |
| Specified services: named providers | The following services are excluded:
| These are unusual services, each provided by one or two named providers, for which there is currently no requirement to submit costs for benchmarking or any other purpose. |
| NHS continuing healthcare, NHS-funded nursing care and excluded intermediate care for individuals – adults and children | NHS continuing healthcare means a package of ongoing care arranged and funded solely by the NHS where the individual has been found to have a ‘primary health need’ as set out in guidance. Such care is provided to an individual adult or child to meet needs that have arisen as a result of disability, accident or illness. It can be provided in any setting including, but not limited to, a care home, a hospice or a patient’s home. NHS-funded nursing care is care provided by a registered nurse for people who live in a care home. This also includes the Electronic Assistive Technology Service (EATS) and augmentative and alternative communication (AAC) services. |
Lack of robust activity data. |
| Non NHS Funded services – pooled or unified budgets, social care services, primary medical services and prison services, or services funded by local authorities | As a general principle, costs and activity are excluded for services jointly provided under pooled or unified budget arrangements with agencies outside the NHS, such as social services, housing, employment, education (for example Sure Start), home equipment loans or community equipment stores. This also includes: Services provided under a primary medical services contract: general medical services (GMS), personal medical services (PMS), alternative provider medical services (APMS) and specialist medical provider services (SPMS). Includes GP-provided open access services and GP out-of-hours services. | Services provided by bodies outside the NHS, such as local government, are outside the scope of PLICS. Primary medical services are subject to separate funding arrangements and are outside the scope of reference costs. Availability of prison health activity data has been an issue with prison health services. However, some costs and activity are included in reference costs (prison health and mental health specialist teams), and we will consider whether other costs and activity should be included in future. |
| Adult Critical care transport network |
| There is no national currency for these arrangements. Other transport services are also excluded. |
| Emergency care streaming services
|
| Request from NHS England Primary Care directorate to separately identify the cost of GP streaming to ED. As this service does not always have a data entry in the same format as the provider data entry, an exclusion is the method of achieving a total cost value. |
Annex 2: PLICS to activity dataset matching for financial year 2023/24 data
Information about the PLICS feed types which are matched to national activity datasets and information about key data items in those feed types, used for matching processes can be found below. This information will support further understanding of the matching processes and through that improve the quality and use of the PLICS data submitted.
APC, EC and OP PLICS feed types
The data for the PLICS feed types for APC, EC and OP is matched to Hospital Episode Statistics (HES) for the same financial year (CDS V6.3 and ECDS V4.0). The HES data used to match to the PLICS data is a fixed dataset for the financial year.
Key data items used for matching PLICS data for APC, EC and OP to HES are:
- Organisation Identifier (Code of provider)
- CDS Unique Identifier
Note: If any data for the APC, EC and OP feed types fails to match on these key data items in the first instance, then fields other than CDS Unique Identifier are used to attempt to match the record to HES (including for example the fields NHS Number, Postcode and Date of Birth).
MHPS and MHCC PLICS feed types
The data for the PLICS Feed Types of MHPS and MHCC is matched to the Mental Health Services Dataset (MHSDS) for the same financial year (V5.0). The MHSDS data used to match to the PLICS data is a fixed dataset for the financial year as set out in the submission timetable.
There are three key data items for each PLICS feed type that are vital for matching PLICS mental health data to MHSDS data for the same financial year. These are:
- Organisation Identifier (Code of provider) (MHPS and MHCC)
- Service Request Identifier and Hospital Provider Spell Identifier (for MHPS)
- Service Request Identifier and Care Contact Identifier (for MHCC).
As we use exact matching your organisation identifier must match the number of digits submitted to the national dataset.
IAPT PLICS feed type
The data for the PLICS Feed Type of IAPT is matched to Improving Access to Psychological Therapies Data Set (IAPT) for the same financial year (V2.1). The IAPT data used to match to the PLICS data is a fixed dataset for the financial year as set out in the submission timetable.
There are two key data items that are vital for matching PLICS IAPT data to IAPT, which are:
- Organisation Identifier (Code of provider)
- Care Contact Identifier.
CSCC PLICS feed type
The data for the PLICS Feed Type of CSCC is matched to Community Services Data Set (CSDS) for the same financial year (V1.6). The CSDS data used to match to the PLICS data is a fixed dataset for the financial year as set out in the submission timetable.
There are two key data items that are vital for matching PLICS Community Care Contacts data to CSDS, which are:
- Organisation Identifier (Code of provider)
- Care Contact Identifier
Additional guidance for submitting key data items
When submitting PLICS data, it is important that trusts submit the above data items using the exact SAME values and in the SAME format as submitted in the corresponding national activity dataset for the data items listed above.
Trusts should ensure the accuracy of these key data items to ensure good matching rates of their PLICS data to the corresponding national activity dataset.
Failure to adhere to the above principle may result in your PLICS data being reported as not matched (when attempts are made to link to the corresponding national activity dataset). For example, if a key data item contained special characters in the national submission of activity data (ie submitted MHSDS records contained values prefixed with a colon (A:123), but the PLICS data is submitted without a colon (A123), this will result in a non-match.
Trusts should also ensure the values are not truncated or reformatted for any of the above key data items.
The above reflects the current implementation and design of PLICS to activity data matching logic for FY23/24 data. This may change over time, for example as PLICS datasets change or requirements for use of the data change.