The accountability report sets out how NHS England meets key accountability requirements to Parliament and is comprised of 3 key sections:
The corporate governance report sets out how the organisation was governed during 2022/23, including membership and organisation of our governance structures and how they support achievement of our objectives. The report includes:
- directors’ report
- statement of Accounting Officer’s responsibility
- governance statement
The remuneration and staff report sets out our remuneration policies for executive and non-executive directors and how these policies have been implemented for the reporting period, including salary information and pension liabilities. The report provides further detail on remuneration and staff.
The parliamentary accountability and audit report brings together key information to support accountability to Parliament, including a summary of fees and charges, contingent liabilities and the Certificate and Report of the Comptroller and Auditor General to the Houses of Parliament.
Corporate governance report
Directors’ report
The key responsibility of the Board is to support strategic leadership to the organisation, including:
- setting the overall direction of NHS England, within the context of the NHS Mandate from government
- approving the business plan, which is designed to support achievement of our strategic objectives and monitor our performance against it
- holding the NHS Executive to account for this performance and for the proper running of the organisation (including operating in accordance with legal and government requirements)
- determining which decisions, it will make and which it will delegate to the Executive or committee or sub-committee, via the Scheme of Delegation
- ensuring high standards of corporate governance and personal conduct
- monitoring the performance of the group against core financial and operational objectives
- providing effective financial stewardship
- promoting effective dialogue between NHS England, its partners, ICBs and providers of healthcare and communities served by the commissioning system.
The Board
The Board comprises the Chair, at least 5 non-executive directors and 5 executive directors including the Chief Executive. The number of executive members must be less than the number of non-executive members.
Appointments
The Chair and non-executive directors are appointed by the Secretary of State for Health and Social Care and executive directors are appointed by the chair and non-executive directors. The appointment of the Chief Executive is subject to the Secretary of State for Health and Social Care’s consent.
On 1 July 2022, Sir Andrew Morris joined as Deputy Chair, having previously served as Chair of NHS Improvement. Sir David Behan joined the Board on 1 September 2022, having served as Associate Non-Executive Director on the NHS Improvement Board.
On 30 June 2022, Lord Ara Darzi’s non-executive directorship tenure ended.
The Secretary of State for Health and Social Care approved the appointment of Baroness Mary Watkins, Professor Sir Simon Wessely and Professor Sir Mark Walport as non-executive directors as of 27 January 2023.
As noted beneath the table below, various members temporarily transferred between the boards of NHS England and NHS Improvement to ensure that the boards of the organisations were appropriately constituted ahead of the legislative changes to the organisations in 2022.
Board members
Directors who served on the NHS England Board during the year are listed in the table below, along with their attendance.[1]
|
Members |
Role |
Term ends/notes |
Number of eligible Board meetings attended |
|
Richard Meddings CBE |
Chair |
24 March 2026 |
6/6 |
|
Wol Kolade |
Deputy Chair |
24 March 2025 |
6/6 |
| Sir Andrew Morris[2] |
Deputy Chair |
24 March 2025 |
5/5 |
| Sir David Behan[3] |
Non-Executive Director |
31 August 2024 |
5/5 |
|
Michael Coupe |
Non-Executive Director |
31 December 2026 |
5/6 |
| Rakesh Kapoor[4] |
Non-Executive Director |
31 December 2023 |
4/6 |
|
Susan Kilsby |
Non-Executive Director |
31 December 2023 |
5/6 |
| Jeremy Townsend[5] |
Non-Executive Director |
30 September 2026 |
5/6 |
|
Laura Wade-Gery |
Non-Executive Director |
30 June 2023 |
5/6 |
| Baroness Mary Watkins[6] |
Non-Executive Director |
26 January 2026 |
2/2 |
| Professor Sir Mark Walport[7] |
Non-Executive Director |
26 January 2026 |
2/2 |
| Professor Sir Simon Wessely[8] |
Non-Executive Director |
26 January 2026 |
2/2 |
|
Amanda Pritchard |
Chief Executive Officer |
|
6/6 |
|
Julian Kelly66F[9] |
Chief Financial Officer |
|
6/6 |
|
Dame Ruth May |
Chief Nursing Officer |
|
5/6 |
|
Professor Sir Stephen Powis |
National Medical Director |
|
5/6 |
|
Sir David Sloman |
Chief Operating Officer |
|
6/6 |
|
Former members |
Role |
Term ends/notes |
Number of eligible Board meetings attended |
|
Professor Lord Ara Darzi |
Non-Executive Director |
Left on 30 June 2022 |
1/1 |
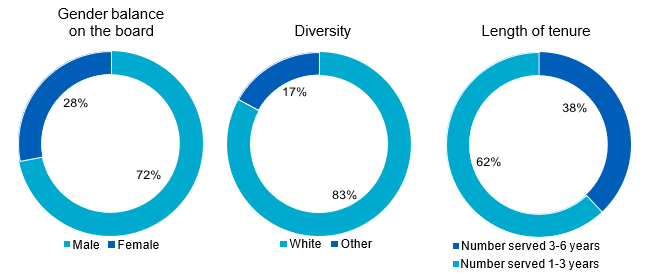
Board diversity
The charts below show the composition of the Board members by gender, diversity and tenure as of 31 March 2023.
The governance structure
Prior to the legal merger on 1 July 2022, NHS England and NHS Improvement could not legally have a joint board or joint board committees. Each organisation retained its given statutory functions and NHS England could not delegate its functions to NHS Improvement, or vice versa.
Nevertheless, the organisations operated as one, with the boards and their committees meeting in common during the year on shared business while having separate membership and the ability to take their own decisions. The governance framework included established procedures for dealing with situations in which a director may find they have a direct or indirect functional, operational or personal interest that conflicts with that of either organisation. Further detail on the Separation of Functions and Conflicts of Interest policy can be found below.
Following the legal merger on 1 July 2022, a new Board committee structure was established:
- the People, Remuneration and Nominations Committee was superseded by the People and Remuneration Committee and Nominations Committee
- the Quality & Innovation Committee was superseded by the Quality Committee
- Digital Committee was superseded by the Data, Digital and Technology Advisory Group
- the New NHS England Committee was established
- the Audit and Risk Assurance Committee’s membership was updated
- the System Oversight Committee transitioned to a subcommittee of the NHS Executive but with formal delegated duties from the Board
Further changes were implemented to the Board committee structure from 1 February 2023 when NHS England merged with NHS Digital. Namely, the Cyber Security and Risk Subcommittee was established as a subcommittee of the Audit and Risk Assurance Committee, and the Data, Digital and Technology Advisory Group was replaced with the
Data, Digital and Technology Committee. 3 former NHS Digital non-executive directors were appointed as non-executive committee members of the Data, Digital and Technology Committee, and 2 were appointed as non-executive committee members of the Cyber Security and Risk Sub-Committee.
An overview of the Board governance framework is shown below and individual Board committee reports can be found below. A report detailing the business considered by the Board committees is provided to each Board meeting.
NHS England Board governance framework and committees
- Audit and Risk Assurance Committee: Provides assurance to the Board that NHS England’s governance, internal controls and risk managing systems are effective and monitors the integrity of the financial statements.
- People and Remuneration Committee: Oversees the delivery of the overall workforce strategy for the NHS, ensures there is a single coherent remuneration policy for NHS England and approves remuneration for senior executives, as well as overseeing appointment and remuneration matters for Integrated Care Boards and trusts.
- Nominations Committee: Oversees succession plans for the Board and senior management, Board composition and Board evaluation.
- Data, Digital and Technology Committee: Considers and makes recommendations on digital and technology strategy (including cyber strategy) to the NHS England Board and oversees implementation. It advises on development of data and technology architecture and assures the Board on discharge of data functions.
- The New NHS England Committee: Time-limited, to provide leadership and strategic oversight of the delivery of the New NHS England Programme, including the safe transfer of staff and functions from NHS Digital and Health Education England.
- Quality Committee: Provides assurance to the Board that NHS England ensures continued improvements in quality of services and outcomes in relation to the safety of services, patient care and experience
- Cyber Security and Risk Sub-Committee: Provides assurance to the Board, through Audit Risk and Assurance Committee, on cyber security and insider threats.
- Executive HR Group and Regional Appointments and Approvals Committees:
- Executive HR Group – Internal recruitment and remuneration; establishment control; internal HR practices and policies.
- Regional Appointments and Approvals Committees – Appointment and remuneration matters for ICBs and NHS trusts.
- Chief Financial Officer Advisory Group: An advisory group which oversees and provides advice to the Board on the financial position across the NHS, including financial performance and efficiencies, the financial framework and NHS capital schemes.
Board activity and administration
The Board held 1 scheduled Board meeting in common with NHS Improvement, and 6 NHS England Board meetings during the year. Each had a public and a private session.
Members of the public can observe the public sessions. The option for members of the public to attend in person was available from the September 2022 meeting.
The agenda, papers and minutes for the public sessions are also published on our website.67F[10]
Additionally, the Board held 1 strategy session and a number of topic-specific deep-dive sessions during the reporting period. There were also a number of Board calls where the non-executive directors were updated on operational pressures across the NHS.
Key items considered by the Board during the year were:
Strategy
- establishment of ICBs and delegation of commissioning functions
- development of the medium-term strategy for the NHS
- strategic opportunities and challenges facing the NHS
- accelerating digitally enabled transformation in the NHS, including the Federated Data Platform commercial strategy for the NHS
- NHS Capital Strategy
- NHS England productivity and efficiency
- approved the 2023/24 business plan for Supply Chain Co-ordination Limited
- NHS Long Term Workforce Plan
Performance
- updates on the continued management of COVID-19 and the associated recovery and restoration of NHS services
- operational, quality, and financial performance of NHS providers
- approved the planning guidance and priorities for 2023/24
- approved NHS England’s 3-year delivery plan for maternity and neonatal services
- updates on mental health services
- considered the primary care access recovery plan
- updates on winter planning and development and implementation of the delivery plan for recovering urgent and emergency care services
- updates on elective recovery leadership and people
- considered progress and received reports on tackling inequalities in the NHS
- considered progress in NHS England’s internal Freedom to Speak Up
Governance and risk
- approved changes to the Board governance framework
- received updates on the Health and Care Act 2022
- merger of NHS England and NHS Improvement, and the merger of Health Education England, NHS Digital and NHSX with NHS England
Review of Board effectiveness and performance evaluation
An internal review of the effectiveness of NHS England’s Board, including Chair effectiveness and Board leadership, commenced in February 2023. The findings of the review and recommendations for improvement will be considered by the Board and implemented in 2023/24. We will therefore report on this in the 2023/24 annual report, by which time we will be better placed to describe the outcomes and reflect on delivery of the resulting actions.
Board committees
Audit and Risk Assurance Committee
Role of the committee
The committee’s primary role is to provide assurance to the Board that NHS England’s governance, internal controls and risk-managing systems are effective and monitor the integrity of the financial statements. The committee met in common with NHS Improvement’s Audit and Risk Assurance Committee (ARAC) until NHS Improvement’s abolition on 30 June 2022, from which time there was a single committee for NHS England.
Committee members
The committee met 6 times and the following table details membership, and the number of meetings attended by each member during the year:
|
Members |
Number of eligible meetings attended |
Comment |
| Jeremy Townsend[11] |
6/6 |
Non-Executive Director, Chair from 1 July 2022 |
| Wol Kolade[12] |
6/6 |
Non-Executive Director, Chair until 30 June 2022 |
|
Mike Coupe |
2/4 |
Non-Executive Director, Member from 1 July 2022 |
|
Rakesh Kapoor |
3/4 |
Non-Executive Director, Member from 1 July 2022 |
|
Susan Kilsby |
5/6 |
Non-Executive Director |
|
Gerry Murphy |
6/6 |
Non-executive Chair of DHSC’s Audit Committee (non-voting member) |
Wol Kolade was Chair of the NHS England Committee, until the 30 June 2022, when Jeremy Townsend took over as Chair. Jeremy Townsend is a qualified accountant and has considerable experience in chairing audit committees in other organisations. Wol Kolade is the managing partner of a private equity firm with valuable and recent financial experience.
Good governance provides that an ARAC should consist of 3 independent non-executive directors. Until 30 June 2022, the committee considered mainly joint organisation business and met in common with NHS Improvement’s committee. It was agreed and supported by the internal auditors, that the committee should comprise 2 non-executive directors because together there are 4 non-executive directors involved in deliberations. This was a time-limited arrangement and pre-legislative change until the merger of NHS England and NHS Improvement on 1 July. The committee has a good balance of skills and knowledge covering accounting and finance, audit committee best practice and clinical services.
Attendees
Additional attendees are invited to attend meetings to assist with committee business. For 2022/23 these included, among others, the Chief Executive Officer, the Chief Financial Officer, the Director of Governance, Legal and Inquiry, the Director of Financial Control, as well as representatives from the external auditors the National Audit Office (NAO), the internal auditors Deloitte LLP and DHSC. The committee can meet with the internal and external auditors without management when required, and the auditors have full access to the organisations.
Principal activities during the year
As part of ensuring the integrity of the organisation’s financial statements, systems of internal control and risk management processes, the committee:
- approved the internal audit plan and considered regular progress reports from the internal auditors and the annual Head of Internal Audit Opinion
- reviewed NHS England’s Corporate Risk Register
- considered several risk deep dives, including data and analytics, maternity, workforce, and integrated care systems
- received updates on information security and cyber risks
- approved changes in accounting policies and reviewed areas of significant estimation or judgement
- assessed the integrity of NHS England’s financial reporting
- approved NHS England’s 2021/22 Annual Report and Accounts
- received updates on delivery of the objectives set out in the Economic crime strategy – tackling fraud, bribery, and corruption
- approved governance manual changes for 2022/23, including approval of the standing financial instructions
- considered NAO reports and management letters and received an update on the status of the NAO Value for Money Programme.
External audit
During the year, ARAC has worked constructively with the NAO Director responsible for the NHS England audit and their team. The work of external audit sits outside our governance arrangements but independently informs our consideration of control, compliance, governance, and risk. The work of external audit is monitored by the Audit and Risk Assurance Committee through regular progress reports. These include summaries of the value for money work that is either directly relevant to our work or may provide useful insights to the committee.
Data, Digital and Technology Committee
The committee was established on 1 February 2023 to support the safe transfer and continued robust oversight of functions from NHS Digital. The committee’s role is to consider and make recommendations on digital and technology strategy (including cyber strategy) to the NHS England Board and oversee implementation. It advises on development of data and technology architecture and assures the Board on discharge of data functions, including overseeing and scrutinising how the functions are exercised and the steps taken by NHS England to follow the statutory guidance and protect confidential information.
Committee members
The committee did not meet in 2022/23 and held its first meeting on 6 April 2023.
|
Members |
Number of eligible meetings attended |
Comment |
|
Richard Meddings |
0/0 |
Chair of NHS England |
|
Laura Wade-Gery (Chair) |
0/0 |
Non-Executive Director |
|
Rakesh Kapoor |
0/0 |
Non-Executive Director |
|
Mark Walport |
0/0 |
Non-Executive Director |
| Daniel Benton[13] |
0/0 |
Non-Executive Committee Member |
| John Noble[14] |
0/0 |
Non-Executive Committee Member |
| Steve Woodford[15] |
0/0 |
Non-Executive Committee Member |
Attendees
Additional attendees will be invited to attend meetings to assist with committee business, including the National Director of Transformation, Interim Chief Information Officer, Chief Operating Officer, Chief Strategy Officer, Head of the NHS England/DHSC Digital Policy Unit, Chief Delivery Officer, Director of Privacy, Transparency and Ethics, and the Chief Data and Analytics Officer.
People, Remuneration and Nominations Committee
Role of the committee
The committee’s role is to oversee the delivery of the overall workforce strategy for the NHS and provide the Board with assurance and oversight of all aspects of strategic people management and organisational development.
The committee is also responsible for people and organisational development policies and ways of working designed to ensure NHS England’s workforce is appropriately engaged and motivated. This includes reviewing the organisation’s gender pay gap and ensuring NHS England develops policies and actions to reduce it, reviewing progress in increasing black and minority ethnic representation at senior levels in the organisation and initiatives relating to diversity and inclusion.
The committee ensures that NHS England has a single formal, robust and transparent remuneration policy that is in line with DHSC Executive and Senior Manager Pay Framework for arm’s length bodies (ALBs). The committee considers and approves remuneration, benefits, and terms of service for senior executives covered by this pay framework before submission to DHSC for approval. The committee’s role also involves employee remuneration and engagement matters.
The committee has delegated certain functions to the Executive HR Group and to the Regional Appointments and Approvals Committee.The committee receives regular reports from the group and the committees on cases considered and approved.
Committee members
The committee met 5 times and the following table details membership and attendance:
|
Members |
Number of eligible |
Comment |
|
Sir David Behan (Chair) |
5/5 |
Non-Executive Director |
| Susan Kilsby[16] |
2/4 |
Non-Executive Director |
| Richard Meddings[17] |
3/4 |
Chair of NHS England |
|
Sir Andrew Morris |
5/5 |
Non-Executive Director |
| Jeremy Townsend[18] |
2/4 |
Non-Executive Director |
|
Laura Wade-Gery |
5/5 |
Non-Executive Director |
Committee attendees
Additional attendees are invited to meetings to assist with committee business. For 2022/23 these included the Chief Workforce Officer, Chief Delivery Officer, National Director for People and the Director of Human Resources and Organisation Development.
Principal activities during the year
Matters considered by the committee included:
- development of the Long Term Workforce Plan
- the approach to improving equality, diversity, and inclusion within NHS England and across the NHS
- updates on the integration of NHS England, Health Education England, and NHS Digital
- the developing approach to management and leadership development in the NHS
- updates on the ‘The future of NHS human resources and organisational development’ report and delivery of the national priority actions
- updates on NHS England’s workforce, including recruitment, staff absence and diversity
- internal NHS England Freedom to Speak Up arrangements, and themes from staff feedback
- NHS England staff survey results and actions to address areas for improvement
- recommended revision of the NHS Very Senior Managers Pay Framework, for agreement through DHSC and HM Treasury
- approved, in line with DHSC pay framework, the remuneration and appointment of several senior executives
- approved, in line with DHSC recommendation, annual salary increases for executive senior managers and medical colleagues on local pay arrangements
During the year, the committee stood down 1 of its subcommittees, the Appointments and Approvals Committee. The subcommittee’s duties in relation to the appointment, remuneration, suspension and termination of trust and ICB chairs were reassumed by the People and Remuneration Committee, and its remaining duties delegated to the Executive Human Resources Group and the Regional Appointments and Approvals Committees.
Nominations Committee
The committee oversees the succession plans for the Board and senior management, Board composition and Board evaluation.
Committee members
The committee was established on 1 July 2022 and met 3 times. The following table details membership, and the number of meetings attended by each member during the year:
|
Members |
Number of eligible meetings attended |
Comment |
|
Richard Meddings (Chair) |
3/3 |
Chair of NHS England |
|
Sir Andrew Morris |
2/3 |
Deputy Chair, NHS England |
|
Wol Kolade |
3/3 |
Deputy Chair, NHS England |
|
Michael Coupe |
3/3 |
Non-Executive Director |
|
Amanda Pritchard |
2/3 |
Chief Executive Officer |
Committee attendees
The Director of Human Resources and Organisational Development is invited to attend meetings to assist with committee business.
Principal activities during the year
Matters considered by the committee included:
- succession plans for national directors
- updates on non-executive director recruitment
- approving the appointment of the Chief Financial Officer as the Deputy Chief Executive
on 14 December 2022
Quality and Innovation Committee and Quality Committee
The committee’s primary role is to support the Board in ensuring that areas concerning patient safety, the quality of care provided to patients and patient experience are continuing to improve and develop to meet the needs of patients in England. In doing so, the committee will ensure strategies are continually improving quality, safety, and experience of care. The committee met in common with NHS Improvement’s Quality and Innovation Committee and met once during the reporting period. The Quality and Innovation Committee was superseded by the Quality Committee, following the merger of NHS England and NHS Improvement and the Quality Committee met 3 times in the reporting period.
Quality Committee
The committee met 3 times and the following table details membership and attendance:
|
Members |
Number of eligible meetings attended |
Comment |
|
Sir Munir Pirmohamed (Chair) |
3/3 |
Non-Executive Director |
|
Dr Aidan Fowler |
3/3 |
National Director of Patient Safety |
|
Sir David Sloman |
2/3 |
Chief Operating Officer |
|
Sir Andrew Morris |
2/3 |
Non-Executive Director |
|
Mike Coupe |
2/3 |
Non-Executive Director |
|
Simon Wessely |
1/1 |
Non-Executive Director |
|
Dame Ruth May |
3/3 |
Chief Nursing officer |
|
Professor Sir Stephen Powis |
3/3 |
National Medical Director |
|
Amanda Doyle |
3/3 |
National Director for Primary Care and Community Services |
|
Vinod Diwakar |
1/2 |
Medical Director for Secondary Care and Transformation |
|
Charlotte McArdle |
2/2 |
Deputy Chief Nursing Officer |
|
Patient and Public Voice members |
1/1 |
|
Committee attendees
Additional attendees are invited to attend meetings to assist with committee business. For 2022/23 these included the Director of Health Inequalities, Director for Experience, Participation and Equalities, and the Head of Quality Strategy.
Principal activities during the year
A large part of the committee’s remit is to monitor and determine whether the NHS is maintaining and improving the quality of patient care and health outcomes. In doing this, matters considered by the committee included:
- proposals for strategic oversight of NHS quality issues and performance
- updates on the implementation of the NHS Patient Safety Strategy and related systems
- patient safety improvements
- updates on palliative and end of life care
- updates on children and young people’s care
- the development of the Quality Framework
- the delivery plan for recovering access to primary care
- reviewing the quality risks and associated mitigations
Other items considered included:
- escalations from the Quality and Performance Committee data relating to quality of services and how this can best be presented to the Committee
- patient experience, from hearing personal accounts
The Quality Committee also held 3 informal roundtables to bring the clinical and service user voice into our board governance, and the outcomes of these roundtables were reported to the committee. The roundtables were held on:
- urgent and emergency care
- maternity and neonatal services
- the model of care for patients with long-term mental health conditions.
Quality and Innovation Committee
The committee met once and the following table details membership and attendance:
|
Members |
Number of eligible meetings attended |
Comment |
|
Sir Munir Pirmohamed (Chair) |
1/1 |
Non-Executive Director |
|
Dr Aidan Fowler |
1/1 |
National Director of Patient Safety |
|
Dr Timothy Ferris |
0/1 |
National Director of Transformation |
|
Rakesh Kapoor |
0/1 |
Non-Executive Director |
|
Mike Coupe |
1/1 |
Non-Executive Director |
|
Dame Ruth May |
1/1 |
Chief Nursing officer |
|
Professor Sir Stephen Powis |
1/1 |
National Medical Director/NHS Improvement Chief Executive |
|
Patient and Public Voice members |
1/1 |
|
The New NHS England Committee
Role of the committee
The New NHS England Committee is a time-limited committee, to provide leadership and strategic oversight of the delivery of the Creating the New NHS England Programme.
Committee members
The committee met 12 times and the following table details membership, and the number of meetings attended by each member during the year:
|
Members |
Number of eligible meetings attended |
Comment |
|
Wol Kolade (Chair) |
12/12 |
Deputy Chair, NHS England |
|
Richard Meddings |
8/12 |
Chair of NHS England |
|
Sir Andrew Morris |
12/12 |
Deputy Chair, NHS England |
|
Laura Wade-Gery |
12/12 |
Non-Executive Director |
|
Sir David Behan |
9/12 |
Non-Executive Director |
|
Amanda Pritchard |
8/12 |
Chief Executive Officer |
|
Julian Kelly |
10/12 |
Chief Financial Officer |
|
Mark Cubbon76F[19] |
12/12 |
Chief Delivery Officer |
Committee attendees
Additional attendees are invited to attend meetings to assist with committee business. For 2022/23 this included the Director of Human Resources and Organisational Development, the Programme Director, the Integration Director and the Clinical Integration Director for the Creating the New NHS England Programme, and the National Director of Vaccinations and Screening, who took up the post of Chief Delivery Officer from 30 March 2023.
Principal activities during the year
Matters considered by the committee included:
- agreeing the overall approach to and overseeing delivery of the Creating the New NHS England Programme
- advising on the culture of the new NHS England, including the organisational purpose
- overseeing the high-level organisational design and priorities for the new NHS England, including the associated consultation and implementation approach
- considering, approving, and receiving updates on the voluntary redundancy scheme
- overseeing and scrutinising Day 1 readiness ahead of the mergers between NHS England and NHS Digital, and NHS England and Health Education England.
System Oversight Committee
The System Oversight Committee transitioned to a sub-committee of the NHS Executive but with formal delegated duties from the Board. Its duties from 1 September 2022 were assigned to the Quality and Performance Committee and the Strategy, Planning and Investment Committee. The System Oversight Committee met in common with NHS Improvement’s System Oversight Committee. Together they ensured a consistent approach to oversight of ICSs and their constituent organisations, including determining appropriate support where required to organisations and systems for them to improve population health outcomes and address health inequalities. This assisted the Board with their formal intervention powers, including deciding on entry into and exit from the Recovery Support Programme and segment 4 of the System Oversight Framework. It also provided strategic oversight of transactions and investments involving clinical commissioning groups and their system partners.
Committee members
The committee met 4 times in the reporting period and the following table details membership and attendance:
|
Members |
Number of eligible meetings attended |
Comment |
|
Professor Sir Stephen Powis (Chair) |
4/4 |
National Medical Director/Chief Executive of NHS Improvement |
|
Ronke Akerele |
3/4 |
Director of Culture Transformation (deputising for Chief People Officer) |
|
Mark Cubbon |
3/4 |
Chief Delivery Officer (interim Chief Operating Officer from August 2021 to Dec 2021) |
|
Miranda Carter |
4/4 |
Director of Provider Development |
|
Ian Dodge |
0/2 |
National Director Strategy and Innovation |
|
Iain Eaves |
3/4 |
Director of Planning and Oversight |
|
Dr Timothy Ferris |
2/4 |
National Director of Transformation |
|
Sue Holden |
2/2 |
National Director of Improvement/Director of Intensive Support for Challenged Systems |
|
Julian Kelly |
0/4 |
Chief Financial Officer |
|
Alex Kirkpatrick |
1/4 |
Interim Director of Provider Development |
|
Matthew Neligan |
4/4 |
Director of System Transformation |
|
Peter Ridley |
2/4 |
Deputy Chief Financial Officer – Operational Finance |
|
Simon Rogers |
2/4 |
Deputy Director of Legal (non-voting) |
|
Sir David Sloman |
0/4 |
Chief Operating Officer |
|
Seven Regional Directors of Strategy and Transformation |
|
|
Committee attendees
In addition, the Executive Director of Performance and Deputy Chief Financial Officer (Strategic Finance), were also invited to attend these meetings.
Principal activities during the period
Matters considered by the committee included:
- updates on the implementation of the NHS Oversight Framework for 2022/23, including segmentation
- approval for several organisations and systems to enter or exit the Recovery Support Programme on recommendations made by the regions
- updates on the implementation of the Maternity Safety Support Programme and its alignment with the Recovery Support Programme
- oversight of and support levers for independent providers of NHS services, including quality governance and finance, sustainability of services, and financial oversight of commissioner requested services
- development of the NHS Oversight Framework for 2023/24
- the approach to Use of Resources assessments for 2023/24 and for the future, linking to the Care Quality Commission’s rating approach
- revised guidance on assuring and supporting complex change: statutory and other transactions, and complex provider governance arrangements.
Board disclosures
From 1 April to 30 June 2022, NHS England and NHS Improvement operated joint working arrangements involving the exercise of statutory functions of the organisations’ constituent bodies in an aligned way under a single operating model. Directorates and teams within the structure performed both NHS England and NHS Improvement functions. During this period, however, NHS England, Monitor and NHS TDA remained separate bodies with distinct statutory roles and responsibilities. In some cases, the functions and decision-making of those bodies had to remain independent and separate, to ensure compliance with the bodies’ respective statutory functions and/or to avoid inherent conflicts of interest that would arise if the functions were exercised by the same part of the organisation (‘functional conflicts’).
To manage this, the bodies had in place a separation of functions and conflicts of interest policy, separate from management of personal interests, which provided guidance for staff on managing functional and operational conflicts.
On 1 July 2022, Monitor and NHS TDA were abolished, and their functions transferred to NHS England, under changes made by the Health and Care Act 2022. NHS England continues to maintain a policy on conflicts between functions, to comply with its duty under new section 13SB of the National Health Service Act 2006 (inserted by section 34 of the Health and Care Act 2022) to make arrangements to minimise the risk of conflicts between the exercise of the former Monitor regulatory functions and NHS England’s other functions, and to manage any conflicts that arise.
Register of Board members’ interests
Personal interests held by Board and committee members are managed in accordance with the NHS England Standing Orders and the Standards of Business Conduct policy. The organisation also maintains a register of members’ interests to ensure that potential conflicts of interests can be identified and addressed before Board and committee discussions. Board members and executives are also required at the beginning of each Board and committee meeting to declare any personal interest they might have in any business on the agenda and abstain from relevant Board or committee discussion as required. Where potential conflicts arise, they are recorded in the Board and committee minutes along with any appropriate action to address them. A copy of the register of interest is available on our website.
Details of related party transactions, where NHS England has transacted with other organisations during the year to which a Board or an executive is connected, are set out in Note 19.
Disclosure of personal data-related incidents
NHS England follows the NHS Digital Data Security and Protection incident reporting process guidance in the reporting of incidents. This is in line with data protection legislation, UK General Data Protection Regulation (UKGDPR).
The guidance[20] sets out the reporting requirements for NHS organisations where a potential or an actual incident may lead to a personal data breach defined under the Data Protection Act 2018 and UK General Data Protection Regulation. The scoring criteria references the circumstances where notification to the Information Commissioner’s Office (ICO) may not be necessary and has resulted in a reduction in the number of incidents classified as notifiable over recent years. As of 31 March 2023, no notifiable incidents had occurred relating to the loss of personal data.
Directors’ third-party indemnity provisions
NHS England has appropriate directors’ and officers’ liability indemnification in place for legal action against, among others, its executive and non-executive directors. There is 1 ongoing legal claim brought against NHS England in respect of the conduct of 1 NHS England director in 2022/23.
Directors’ responsibility statement
The Annual Report and Accounts have been reviewed in detail by NHS England’s ARAC and Board. At each point it has been confirmed that the Annual Report and Accounts, taken as a whole, are considered to be fair, balanced and understandable. They provide the information necessary for NHS England’s stakeholders to assess the business model, performance and strategy.
Human rights
NHS England supports the government’s objectives to eradicate modern slavery and human trafficking. An NHS England Slavery and Human Trafficking Statement for the financial year ending 31 March 2023 will be published in October 2023. The statement for 2021/22, published in March 2022, is available on our website.[21] Our strategy on tackling fraud, bribery and corruption can be found on our website.[22]
Events after the reporting period
On 1 April 2023, NHS England and Health Education England merged. As part of this, the NHS England Board approved a revised Board governance framework, including the establishment of a Workforce, Training and Education Committee. The details of the new framework will be provided in the 2023/24 Annual Report and Accounts.
Statement of Accounting Officer’s responsibilities
Under the National Health Service Act 2006 (as amended), the Secretary of State for Health and Social Care (with the consent of HM Treasury) has directed NHS England to prepare, for each financial year, a statement of accounts in the form and on the basis set out in the Accounts Direction. The accounts are prepared on an accruals basis and must give a true and fair view of the state of affairs of NHS England and of its income and expenditure, statement of financial position and cash flows for the financial year. In preparing the accounts, the Accounting Officer is required to comply with the requirements of the Government Financial Reporting Manual (HM Treasury, December 2022)[23] and in particular to:
- observe the Accounts Direction issued by DHSC, including the relevant accounting and disclosure requirements, and apply suitable accounting policies on a consistent basis
- make judgements and estimates on a reasonable basis
- state whether applicable accounting standards, as set out in the Government Financial Reporting Manual, have been followed and disclose and explain any material departures in the financial statements
- prepare the financial statements on a going concern basis
- confirm that the Annual Report and Accounts are fair, balanced, and understandable, and take personal responsibility for the Annual Report and Accounts and the judgements required for determining that they are fair, balanced, and understandable.
The National Health Service Act 2006 (as amended) schedule A1 paragraph 15(4) states that the Chief Executive shall be the Accounting Officer of NHS England. The responsibilities of the Accounting Officer, including responsibilities for the propriety and regularity of the public finances for which the Accounting Officer is answerable, for keeping proper records and for safeguarding NHS England’s assets, are set out in Managing Public Money (HM Treasury, July 2013, as amended May 2023).[24]
As the Accounting Officer for NHS England, I have taken the steps that I ought to have taken to make myself aware of any relevant audit information and to establish that NHS England’s auditors are aware of that information. So far as I am aware, there is no relevant audit information of which the auditors are unaware.
Governance statement
This governance statement covers NHS England, its system leadership role of the NHS, directly commissioned health services, and oversight and assurance of the commissioning system.
As Accounting Officer, I have responsibility for the system of internal controls supporting and enabling the achievement of NHS England’s aims and objectives, while safeguarding the public funds and assets for which I am personally responsible in accordance with Managing Public Money and as set out in my Accounting Officer appointment letter. This includes assurance of several organisations which are part of the wider commissioning system, including those organisations hosted by NHS England. My responsibilities in relation to the oversight of ICBs.
Board arrangements
Information on our Board and its committees is set out below.
Freedom to Speak Up
Our report on whistleblowing disclosures made by NHS workers is published on our website.[25]
Government functional standards
Functional standards[26] set out what needs to be done, and why, for different types of functional work. They were mandated for use in departments and their arm’s length bodies from the end of March 2022. The extent to which these standards are adopted across NHS England varies, and certain elements of the standards are not applicable to the organisation.
Governance arrangements and effectiveness
Governance framework
The Governance Manual brings together all key strands of governance and assurance, including Standing Orders, Standing Financial Instructions (SFI), Scheme of Delegation, Standards of Business Conduct Policy, Risk Management Framework and the 3 lines of defence model. Separate operating frameworks exist for each CSU.
Assessment against the Corporate Governance in Central Governance Departments: Code of Good Practice 2017 Compliance Checklist
As part of implementing best practice, an assessment is undertaken each year against this checklist from HM Treasury. NHS England is compliant[27] against the provisions of the code, with the following exceptions:
|
Ref |
Code provision |
Exception |
|
4.7 |
Through the Board Secretariat, the Department provides the necessary resources for developing the knowledge and capabilities of Board members, including access to its operations and staff. |
This responsibility is shared between the Chair, the Chief Executive’s private office and Board Secretary. |
|
4.11 |
The Board Secretary’s responsibilities include arranging induction and professional development of Board Members. |
This responsibility is shared between the Chair, Chief Executive’s office and the Board Secretary. |
|
5.5 |
The Head of Internal Audit is periodically invited to attend Board meetings, where key issues are discussed relating to governance, risk management, or control issues across the department and its ALBs. |
The Head of Internal Audit routinely attends ARAC meetings. |
|
5.9 |
The Board and Accounting Officer should be supported by an ARAC, comprising at least 3 members. |
ARAC comprises at least 2 non-executive board members. The committee met in common with NHS Improvement’s ARAC, until NHS Improvement was abolished in June 2022, and consequently there were in total 4 non-executive directors involved in deliberations. |
Corporate assurance
The NHS corporate assurance framework, set out below, provides for continuous and reliable assurance on organisational stewardship and the management of significant risks to organisational success and the delivery of improved, cost-effective public services.
|
Assurance activity |
How does it add value? |
|
Organisational change framework |
The framework provides a consistent approach to thinking about the impact of organisational change, including on people, infrastructure, financial and legal issues. |
|
Risk management framework |
The framework enables a consistent approach to be taken across the organisation, allowing identification of cross-directorate risks and challenges. It provides a mechanism for managers to identify risks with a route of escalation to those accountable. |
|
SFIs, Scheme of Delegation and |
Together, these documents ensure that our financial transactions, accountabilities and responsibilities are carried out in accordance with the law and government policy in order to achieve probity, accuracy, economy, efficiency and effectiveness. |
|
Programme management framework |
Provides staff with a framework to manage, control and deliver projects and programmes. Provides the organisation with consistency of reporting and monitoring, confidence of delivery of outcomes to enable decision-making and better resource control. |
|
Third-party assurance framework |
Ensures directorates responsible for major contracts assign a contract manager and put arrangements in place to monitor supplier performance. Obtains assurance over the services provided. |
|
Corporate policy framework |
Provides an approach to help ensure policy documents are not developed in isolation, so they are balanced against the priorities of the organisation. |
We work with the support of both our internal and external auditors to strengthen and embed our assurance framework. Each directorate and region have designated leads with responsibility for ensuring that risk management, implementation of internal audit actions and other key assurance activities are carried out and approved by the relevant senior director, including appropriate regular reporting and exception escalation processes. The leads link with the governance, audit and risk teams to provide increased focus, accountability and improved communication at operating level across the organisation.
During 2022/23, the corporate governance and compliance team worked with teams across the organisation to embed controls and underpin processes including by:
- ensuring that officers undertook staff declarations in line with the standards of business conduct policy[28]
- targeted interventions with teams to ensure the timely completion of actions arising from internal audit reviews.
Management assurance
Throughout 2022/23, the Board has been provided with regular performance updates on the implementation of the priorities and programmes committed to in the NHS Long Term Plan.
The report integrates performance against constitutional standards, NHS Long Term Plan commitments and workforce and quality metrics.
Individual programme boards and oversight groups meet frequently, with representatives from national and regional teams, each with responsibility for delivery of their programme.
Risk governance
The Board is responsible for defining NHS England’s strategy within the context of the NHS Mandate. It ensures the effective running of the organisation, approving the internal business plan, which is designed to support achievement of NHS England’s strategic objectives.
ARAC is responsible for reviewing the establishment and maintenance of an effective system of governance, risk management and internal control covering NHS England’s activities.
The committee considers the key risks faced by the organisation on a quarterly basis and reports its conclusions directly to the Board.
The internal audit team provides regular reports to ARAC based on their work programme.
The Board discusses the most significant risks and actions identified to mitigate their likelihood and impact. Each year, ARAC evaluates the effectiveness of the risk management framework and approves the annual internal audit plan for the following year.
The transfer of NHS Digital’s functions to NHS England on 1 February 2023 brought a change to the overall organisational risk profile. To ensure robust oversight of transferred key risks,
a Cyber Committee has been established as a subcommittee of the Board. This committee provides assurance on the effectiveness of cyber threat protection and risk management.
The Chief Executive Officer, supported by senior management, provides leadership, and articulates their continued commitment to risk management through the organisational risk management framework.
The Chief Risk Officer is appointed by the Chief Executive Officer to lead NHS England’s overall approach to risk management. In 2022/23, the position of Chief Risk Officer was delivered by the Chief Delivery Officer.
The executive team owns the corporate risk register (CRR) and nominates a responsible officer for each of the risks that are included within it. This approach is supported by the NHS England risk management framework, which underpins the monitoring and management of risk.
The Executive Risk Group is responsible for assuring ARAC about how risks across the organisation are being managed. This group reviews the risks escalated to it and considers which risks should be managed through the CRR and associated processes. ARAC oversees implementation of NHS England’s risk management framework. The NHS Executive also periodically reviews the CRR and, when appropriate, undertakes in-depth review.
Our executives are responsible for managing risk at a directorate/regional level (that is, at the project delivery and day-to-day operational level). Each directorate therefore also holds its own risk register and reviews its risks on a regular basis.
The risk management framework mirrors the three lines of defence of our overarching assurance framework.
Risk and control framework
In 2022/23, NHS England continued to embed its risk management framework to ensure that employees follow a single process for identifying and managing risks that may threaten delivery of services and achievement of objectives. This framework aligns with the main principles of HM Treasury’s Orange Book[29] and is informed by ISO 31000 Risk management principles and guidelines, and the UK Corporate Governance Code.[30]
Our risk appetite by category of risk
|
Category of risk |
|
Risk appetite |
|
Patient safety and quality of care |
|
Very low |
|
Operational performance (across the system) |
|
Medium |
|
Innovation |
|
High |
|
Financial |
|
Low |
|
Compliance and regulatory |
|
Medium |
|
Reputation |
|
Low |
|
Operational delivery across NHS England |
|
Medium |
Principal risks
The CRR considers a full cross-section of risks to the organisation. NHS England’s most significant principal risks in 2022/23, including strategic, reputational, financial and operational risks, and risks to the achievement of the organisations’ objectives and external threats, were:
|
Risk |
Key mitigations in place |
|
Demand and capacity: |
Urgent and emergency care recovery plan was published in January 2023 and targeted improving performance over a 2-year period through a variety of interventions, including: additional capacity for general and acute beds, virtual wards, ambulance hours on the road and community care. As part of this £1 billion was allocated to systems for 2023/24, building on the £500m allocated last year.ective recovery programme’s focus is on reducing long-wait lists. |
|
Workforce capacity: |
Additional staff were recruited into the substantive and contingent workforce with a focus on shortage areas, including nurses, healthcare support workers, with key targets for 2022/23. GP numbers: an additional 1,903 within primary care. 16,964 more international nurses and new funding for maternity services, with an increase of more than 2,000 WTE midwives. We are promoting an inclusive culture by developing an equality, diversity and inclusion plan to improve equality in the NHS, including high impact actions for all protected characteristics. Ongoing health and wellbeing interventions including health and wellbeing guardians, embedding health and wellbeing conversations and psychological support via growing occupational health. |
|
Quality of care: |
Publication of cross-system quality oversight and governance guidance through the National Quality Board (NQB). Maternity Support Programme and CQC maternity service inspection regime. |
|
Data and digital security: There is a risk that malicious cyber actors deploy widespread, catastrophic cyber-attacks against the NHS leading to patient harm and/or data misuse causing knock-on reputational and financial consequences for NHS England. |
The Data Security and Protection Toolkit (DSPT) is an online self-assessment tool that provides guidance for and measures compliance with cyber security best practice across the NHS. It is refreshed on an annual basis allowing us to increase the standard year-on-year. £12 million capital was allocated to address critical infrastructure weakness such as outdated equipment in trusts. |
NHS Oversight Framework
The NHS Oversight Framework[31] describes how NHS England oversees ICBs, NHS trusts and foundation trusts. Under the framework, organisations’ support needs are regularly assessed, and each organisation is allocated into 1 of 4 support segments; from segment 1, for those with no specific support needs, to segment 4 where intensive support is provided through the national Recovery Support Programme. Decisions on which support segment organisations are allocated to are routinely reviewed and updated throughout the year and published on our website.
NHS England has met regularly with each CCG/ICB to review performance and the support needs of each NHS organisation across their ICS footprint. At the end of 2022/23 NHS England was providing intensive support via the Recovery Support Programme to 4 ICBs, 1 ICB was successfully supported to exit the Recovery Support Programme.
NHS England is committed to ensuring that the model of oversight remains relevant and effective. During 2023/24, we will complete a full review of our approach to oversight and consult on an updated Oversight Framework that is fully aligned with the NHS England Operating Framework.
Quality oversight and assurance
NHS England has a statutory duty to act with a view to securing continuous improvements in care quality. NHS England, as co-chair of the NQB, uses the definition of quality as care that is safe, effective, provides a personalised experience, is well-led, sustainable and equitable. NHS England’s approach to managing quality is based on the quadruple aim, recognising the interoperability of quality, cost, staff experience and outcomes, and a quality management system approach (combining quality planning, improvement and control activities).
All NHS organisations have responsibility for the quality of services, and both ICBs and NHS England have a statutory duty to act with a view to securing continuous improvement in quality. NHS England, as co-chair of the NQB, uses the definition of quality as care that is safe, effective, provides a personalised experience, is well-led, sustainable and equitable.
NHS England’s approach to managing quality is based on the quadruple aim, recognising the interoperability of quality, cost, staff experience and outcomes, and a quality management system approach that combines quality planning, improvement and control activities.
Governance
From 1 July 2022, the NHS England Board has a Quality Committee to support the duties and powers of the Board in respect of quality. The committee’s duties are to:
- ensure NHS England has clear priorities for improving quality and a strategy to deliver them
- gain assurance that NHS England is delivering its functions, initiatives and policies in a way that secures continuous improvement in the quality of services and outcomes
- gain assurance that NHS England is effectively identifying, mitigating, and managing quality concerns and risks as appropriate, including through intelligence-sharing with ICSs, regulators, and wider partners.
Reporting to the Quality Committee, the NHS England Executive has a Quality and Performance Committee (QPC) to scrutinise quality, performance, workforce and finance issues, and an Executive Quality Group (EQG) to provide oversight and scrutiny of care quality across regions and receives regional quality insight from ICBs and providers.
NHS England also hosts the NQB which champions the importance of quality and drives system alignment across key health and care ALBs (NHS England, CQC, UKHSA, NICE, the Office for Health Improvement and Disparities, DHSC, and Healthwatch England). NQB discussions are also shared at the EQG and QPC.
The EQG provides an executive-level forum through which quality early warning signs, concerns and risks are shared, discussed, managed and escalated. The EQG is co-chaired by the National Medical Director and Chief Nursing Officer and brings together regional medical directors, regional chief nurses, directors of clinical quality and senior national colleagues, including the directors for patient safety, clinical effectiveness, patient experience and quality.
Assurance of the commissioning system
Specialised services
Specialised services support people with a range of rare and complex conditions. They often involve innovative treatments for patients with rare cancers, genetic disorders, complex medical conditions or surgical needs.
The specialised commissioning allocation was £23 billion at the end of 2022/23. Most of this allocation is held across seven regional teams for commissioning specialised services, with the balance held centrally to fund national budgets such as the CDF and other national programmes.
During 2022/23, the 2 major governance groups were established to set the strategic direction for specialised commissioning. In line with the ambition to delegate those specialised services which are suitable and ready for greater local leadership[32], the Delegated Commissioning Group for Specialised Services was established to provide strategic direction for such services. Correspondingly, the National Commissioning Group (NCG) for Specialised, Health and Justice Armed Forces Services was established to set strategic direction and oversee commissioning of services still to be commissioned by NHS England. The Clinical Priorities Advisory Group made formal recommendations on the commissioning position of treatments and interventions for adoption.
Health and justice and sexual assault services
NHS England commissions healthcare for 112 adult prisons, immigration removal centres and the children and young people’s secure estate. NHS England is also responsible for co-commissioning 47 SARCs to support victims and survivors of sexual assault and abuse. While the strategic direction for these services is set at a national level via the NCG, commissioning responsibilities are discharged regionally. The Health and Justice Delivery and Oversight Group and Health and Justice Clinical Reference Group were set up to oversee and join up health and justice commissioning.
The NHS England domestic abuse and sexual violence programme was established to transform the way the NHS in England responds to domestic abuse and sexual violence for both patients and staff. The programme worked with systems, regions and national and local partners to help with the implementation of the ‘Serious Violence Duty.’[33] The duty came into force on 31 January 2023, requiring specified organisations, including ICBs, to collaborate locally to prevent and reduce ‘serious violence’, which includes domestic abuse and sexual offences.
In November 2022, we published the ‘Health and Justice Framework for Integration 2022-2025: Improving lives – reducing inequality’.[34] This sets a strategic vision for the delivery of health and justice services and provides a framework for NHS commissioners, service providers, those with lived experience and cross-departmental partners to work collaboratively to improve patients’ health and wellbeing outcomes.
We published renewed national partnership agreements (NPA) to ensure a joined-up approach for all patients in health and justice. This includes the adult prisons NPA, health and justice children programme NPA and an NPA for immigration removal centres.
Armed forces health
NHS England directly commissions all secondary care health services for serving personnel and families registered with Defence Medical Services and specific specialised services for veterans that, by law, we must provide access to for those distinct populations across England.
The services directly commissioned by NHS England with providers of secondary and specialised services include:
- all secondary healthcare services
- specialised veterans’ mental health service – Op COURAGE
- prosthetics
NHS England sets policy, national clinical and governance standards and service specifications, which providers are contracted to deliver against.
The 42 ICBs commission healthcare for armed forces veterans and the families of veterans who are either currently serving or registered with an NHS GP practice. ICBs are required to give due regard to the health and social care needs of the armed forces community in planning and commissioning services.
During 2022/23, assurance to the NHS England Commissioning Group was through the Armed Forces Oversight Group on quality, performance and value for money.
The Armed Forces Clinical Reference Group and the Patient and Public Voice Advisory Group made formal recommendations on commissioning services based on strong evidence and lived experience.
We published a renewed national partnership agreement with the Ministry of Defence, which sets out the strategic intent and commitment for us to work together to commission health services for the armed forces community.
Delegation of primary care services
Since 1 July 2022, all ICBs have had delegated responsibility for commissioning primary medical services, which represented a transfer of responsibilities previously delegated to CCGs. However, 9 ICBs also took on delegated responsibility for 1 or more of dental (primary, secondary and community), general ophthalmic and pharmaceutical services. Delegation to ICBs was enabled by the Health and Social Care Act 2022. All remaining ICBs took on delegated responsibility for all four primary care services from 1 April 2023.
Delegation has been at the forefront of our vision to support more integrated care by ensuring local health and care leaders take collective responsibility for system performance and the transformation of care to improve population health, including primary care.
Where NHS England delegates its functions to ICBs it obtains assurances that these functions are being discharged effectively through the Primary Care Assurance Framework. The framework covers issues such as providing information to NHS England on the running of this function and where it can be improved, which in turn provides aggregate information to support assurance and facilitate support for improvement where needed. The Primary Care Assurance Framework has been developed specifically to cover all delegated activity across primary care services and replaces the previous framework that covered only primary medical services that were delegated to CCGs.
Vaccinations and screening – governance and the Section 7A agreement
Our Vaccinations and Screening Directorate commissions 11 screening programmes, around 20 routine immunisation programmes including the public seasonal influenza programme, and the COVID-19 vaccination deployment programme. The annual NHS Section 7A public health functions agreement between NHS England and DHSC sets out the arrangements under which the Secretary of State delegates responsibility to the NHS England Board for commissioning certain NHS public health services, including in 2022/23:
- NHS national cancer and non-cancer screening services
- NHS national routine immunisation services in general practice and school-age delivery
- Child Health Information Service (CHIS) including the Red Book
- NHS SARCs (led by Health and Justice Commissioning)
- NHS public health services for people in secure and detained settings (led by Health and Justice Commissioning)
- provision of an effective screening quality assurance service
- promotion of healthcare public health
- seasonal flu vaccinations
- COVID-19 vaccinations
Internal assurance in 2022/23 was provided through the quarterly NHS England Public Health Oversight Group. These were informed by programme-specific boards for each screening, vaccinations, flu and the CHIS programmes.
Integrated care systems
ICS development
The Health and Care Act 2022 placed ICSs on a statutory footing by creating ICBs as new NHS bodies on 1 July 2022. CCGs were simultaneously closed down, with NHS England overseeing the safe transfer of functions and staff to ICBs, which now lead strategic planning with their system partners, manage NHS resources and oversee and support NHS providers locally.
CCG and ICB annual reports
ICBs produced 2022/23 reports and accounts for each legacy CCG from within the ICB footprint (covering April to June 2022), and separate reports were published for each new ICB (accounting for the period 1 July 2022 to 31 March 2023). These annual reports were published on their individual websites. A list of ICBs, along with links to their websites, can be found on the NHS England website.92F[35]
A review of the ICB governance statements found that issues identified by internal auditors over the year (covering CCGs for months 1-3 and ICBs for months 4-12), primarily focused on ‘quality and performance’ and ‘finance, governance and control’. The majority of control issues raised related to service capacity, referral to treatment times, finance and procurement for CCGs and ICBs. Additionally, CCGs additionally raised issues relating to governing body arrangements. These closely align with the issues highlighted by ICBs in their exception reports.
The NHS England group account has been prepared using unaudited information for four CCGs (NHS Birmingham and Solihull CCG, NHS Herefordshire and Worcestershire CCG, NHS West Essex CCG and NHS North West London) and five ICBs (NHS Birmingham and Solihull ICB, NHS Hereford and Worcestershire ICB, NHS Hertfordshire and West Essex ICB, NHS North West London ICB and NHS Suffolk and North East Essex ICB), as their audit reports remain outstanding at the time of finalising this account due the auditors not completing the local audits. More information is provided in note 1.3 to the consolidated financial statements.
Timeliness of local accounts
In preparing the consolidated NHS England account we use financial information extracted centrally from the single integrated financial environment and other information from schedules submitted to us by group bodies. This is assured based on audited annual reports and accounts provided to us by each CCG and ICB, other than the nine entities listed above.
We and the Department of Health and Social Care issue directions to NHS commissioners (CCGs and ICBs for the year ended 31 March 2023) on the timing by which these should be submitted.
The vast majority of NHS commissioners and their auditors continued to meet the deadline set for submission of audited accounts in 2022/23 and we recognise the significant efforts by commissioners and audit firms made to achieve this. The compliance rate was similar in percentage terms to 2021/22 but the number significantly late in 2022/23 is worse than 2021/22. This small but significant number of CCG and ICB audited accounts that were significantly late has delayed the preparation of these consolidated accounts.
There are many reasons why a set of audited accounts may go beyond the deadline: for example, this may reflect illness in the preparer finance team or audit team, or a significant issue may be encountered that takes time to resolve, which may reflect weaknesses in a commissioner’s preparation of its accounts. It is important that auditors can complete their work independently of outside influence and take the necessary time to ensure their audit opinion is the right one and supported by appropriate audit evidence. However, standing back from the level of individual engagements, it is clear that success in enabling commissioners to achieve the audited accounts deadline, to which all firms sign up collaboratively, varies significantly between audit firms. For example, of the sixteen NHS commissioners audited by one audit firm, only three had submitted audited accounts by 31 August, two months after the deadline.
NHS England continues to work to improve timeliness in financial reporting including:
- encouraging auditors to give clear reporting to audit committees where the preparer’s quality of draft accounts or working papers needs to improve
- working closely with commissioners to ensure they appoint external auditors in good time, which helps increase the likelihood of deadlines being achieved
- regular engagement with partners including the Department of Levelling Up, Housing and Communities and the Financial Reporting Council on policy matters affecting the broader local audit system: we believe strongly that firms having sufficient capacity across their wider portfolio of work to enable effective interim audits at NHS bodies is important for success
- working with commissioners where financial reporting issues arise to ensure they can address findings effectively
- regular engagement with the audit firms and responding to their feedback to continue to strengthen the NHS financial reporting landscape, and working with partners to make sure training and guidance is available for preparers
We acknowledge that 2022/23 was a complex year for financial reporting and audit in the NHS, in particular the implementation of IFRS 16, the mid-year transition from CCGs to ICBs meaning there was an increased number of bodies in 2022/23 requiring audit, and the growing backlog of audits in local government putting pressure on audit teams. We will continue to take the steps including those outlined above to improve overall timeliness in NHS financial reporting. The Department of Health and Social Care has an ambition to return to laying the main national consolidated accounts (being the DHSC group, NHS England group and consolidated provider accounts) before Parliament in advance of the summer Parliamentary recess in July. Significant improvements in overall timeliness of NHS financial reporting and audit would be required if this is to be achievable in the years ahead.
Commissioning support units
4 NHS CSUs operate across the whole country, providing essential support to a number of organisations including ICSs, ICBs, trusts, national organisations, local authorities and non-NHS bodies. With a workforce of 7,000 people, CSUs deliver a range of support services that have been independently assessed to ensure the NHS receives the benefits derived from working at scale.
CSUs rely on income for services delivered, creating an incentive for them to offer services of quality and value to other parts of the NHS. This ensures CSU services remain value for money as well as being responsive to the needs of their local health system and national priorities. They develop innovative solutions to areas of support, including managing waiting times, ICT services, data analytics, cyber security and transformation of local health systems. CSUs work closely together to ensure integration of service offerings and benefit from expertise, regardless of geographical location.
As an integral part of the NHS, CSUs operate in accordance with good governance principles. Each CSU is led by a managing director accountable to NHS England for their CSU’s performance and delivery. This includes regular monitoring of CSU activity and the delivery of a monthly assurance statement to NHS England confirming adherence to appropriate governance processes and policies.
In 2022/23, CSUs supported development of the new NHS England and again achieved their financial targets.
Supply Chain Coordination Limited (SCCL)
SCCL ownership and responsibility for oversight of SCCL was transferred to NHS England from DHSC on 1 October 2021, to strengthen NHS England’s ability to deliver savings in procurement, as committed in the NHS Long Term Plan. SCCL is a UK incorporated company and their Articles of Association include a range of matters reserved for shareholder decision. NHS England has established a governance framework with regard to its shareholdings. In addition to controls set out in the company’s Articles of Association, NHS England sits on the Board of SCCL and holds quarterly accountability meetings to review performance against key performance indicators (KPIs) and financial targets, both of which are agreed by the NHS England board annually.
Additionally, NHS England sits on SCCL’s ARAC as shareholder director, and ensures the appropriate Senior Finance representation.
In addition to controls set out in the company’s Articles of Association, NHS England is represented on the SCCL Board and ARAC by a shareholder director. NHS England holds quarterly accountability meetings to review performance against KPIs and financial targets, both of which are agreed by the NHS England Board annually.
Other assurance
Information governance
The corporate information governance (IG) department is led by the Head of Corporate Information Governance who is also NHS England’s Data Protection Officer. 4 workstreams make up the IG service: data governance, IG delivery, IG assurance and records management, supported by a business support office responsible for communication and engagement, project support and a central IG support desk which handles thousands of enquiries a year.
The corporate IG team supports the Data Protection Officer to ensure compliance with data protection legislation, common law, IG standards, best practice and NHS England policies and procedures.
Data Security and Protection Toolkit (DSPT)
A key achievement during 2022/23 was compliance with the DSPT, which requires all organisations that handle NHS data to measure their performance against the National Data Guardian’s 10 data security standards every year. Achieving this standard provides assurance to the Board that good data security is in place and personal information is being handled correctly.
The Corporate Records Management team
The Corporate Records Management team completed a detailed analysis of the inventories for our legacy primary care services records (more than 324,600 boxes), including application of disposition and action date. IG and records management mandatory and statutory training achieved over 95% and 86% compliance respectively, with the required number of nominated records and information management co-ordinators (RIMCs) increasing to 30% by March 2023, representing over a quarter of all internal teams having two trained RIMCs.
The Data Governance team
The Data Governance team provided vital advice, direction and support to ensure adequate technical and organisational measures were in place to meet legal obligations and provided critical IG support to high profile programmes including:
- Vaccination Programme
- Get It Right First Time
- Model Health System
- Federated Data Platform
- OpenSafely COVID-19 Research Platform
- Data Management Information Services
- Clinical and medical device registries.
The Data Governance team supported the Model Health programme team to amend the data collection for Theatres Productivity, enabling the collection of the NHS number to enable data linkage (once de-identified). The Data Governance team also reviewed access controls for all major platforms, apps and dashboards and helped the organisation meet its obligations.
The IG Assurance team
The assurance service oversees IG assurance of internal directorates and functions, as well as externally hosted bodies, high-risk data processors, CSUs and PCSE to minimise information risk to NHS England. Ensuring information assets are identified and managed is another key indicator of good IG and records management. The percentage of information assets compliant with their annual review increased to over 84% in-year, demonstrating how internal asset management controls have strengthened.
The IG Delivery team
To ensure the organisation is meeting its data protection accountability obligations, the IG Delivery team oversaw and managed a privacy-by-design approach for many new projects. The team supported several hundred data protection impact assessments, maintained IG policies and procedures, and provided communication and awareness materials to the public to meet transparency obligations with the ongoing publication of privacy notices.
During the year, NHS England received 169 subject rights requests, and compliance against the statutory response times was 83.4% (141/169). Of those subject rights requests handled, there were 33 internal review requests and data protection complaints made to the ICO requiring a response. The data protection officer team and the assurance team handle data protection complaints and responded to 100% of data protection concerns within the required timeframe since August 2022 (21/21), with 88% performance over the year (29/33).
There were 327 data breach incidents/near-misses reported internally during the year requiring investigation. 1 data breach incident required reporting to the ICO via the data security and protection incident reporting portal. This consisted of a cyber security incident on 4 August, which affected the Advance and Adastra systems. An emergency response team, which included representatives from NHS Digital and NHS England, helped to manage the incident. However, NHS England was not a data controller for the data but voluntarily reported the incident to follow NHS IG policy team guidance for all other NHS and social care organisations relating to the lack of availability of systems such as Adastra.
The number of notices served on an organisation by the UK’s supervisory authority, the ICO, demonstrates a level of assurance in its information governance controls. During 2022/23, NHS England did not have any notices issued to it by the ICO.
This provides significant assurance to the data protection officer, the senior information risk owner and the Board of the organisation’s compliance with data protection legislation, common law, IG standards, best practice and policies and procedures.
Business critical models
We operate a register of business-critical models and audit of the quality assurance strategy associated with them, overseen by a committee of experienced analysts. In 2022/23, this register was developed to work on a rolling basis, supporting a continuous improvement approach to our system of quality assurance. To date all relevant NHS England models in the register have passed.
Service auditor reporting and third-party assurances
NHS England relies on a number of third-party providers (such as NHS SBS, NHS BSA and Capita) to provide a range of transactional processing services ranging from finance to data processing. Our requirements for the assurance provided by these organisations are reviewed every year. Appropriate formal assurances are obtained to supplement routine customer/supplier performance oversight arrangements. During 2022/23, service auditor reports were specifically commissioned to provide assurance over the operation of our control environment and we are working, where appropriate, with our suppliers to implement International Standard on Assurance Engagements (ISAE) 3402 or similar standards to make sure that the relevant internal controls and control procedures operated by our service organisations have operated effectively. Service providers are requested to address any control weaknesses identified during the ISAE 3402 reporting process within an appropriate timescale. The service auditor reports commissioned for 2022/23 have been reviewed and where necessary action plans are being agreed to address any control issues identified. There are a limited number of other issues which service auditors have referred to in their opinion and these are being addressed by services providers as a matter of priority. The issues identified are not considered to have a significant impact on the overall NHS England control environment.
Control issues
Managing third-party contracts
We have continued to roll out our approach to third-party contract management, based on government commercial function guidance and methodologies for clarity of responsibility and accountability. The central commercial team now has overall responsibility for 886 contracts worth £3 billion.[36] All members of the central Contract Management team have government commercial function contract management accreditation. In line with the government’s transparency agenda, we publish quarterly KPI data for our gold/strategic contracts.
Primary Care Support England performance management
Primary care support services are administration and payment services for the effective running of primary care. They are delivered by partner organisations: Capita Business Services Ltd and three CSUs.
The services:
- support more than 40,000 GP practices, dentists, opticians, and pharmacists
- pay more than £10 billion each year to primary care providers for NHS services
- invite more than 4.5 million women each year for NHS cervical screening
- process registrations for more than six million patients joining or changing GP
- move 5.8 million patient medical records each year between GPs
The PCSE contract saves the NHS more than £30 million each year compared to the previous in-house arrangement. The services have been assured throughout 2022/23 by regularly monitoring performance and quality indicators and a year-end assessment against International Audit Standard ISAE3402.
A project to assure the quality of historical GP pensions data, held by PCSE and NHS Pensions, continued to make progress including the pilot of a complex queries service. Other system and service improvements included supporting NHS Digital to build replacement software systems for the NHS cervical screening programme and patient registration function; continuing to improve the transfer of electronic records between GP practices and development of infrastructure to enable future development of an electronic only service. The programme to determine the future delivery of primary care support services began in 2022/23 to ensure continued delivery of these services from 2025 onwards.
Capita cyber incident
NHS England reported a data breach to the ICO following a cyber incident involving Capita, at the end of March 2023. Capita are contracted to provide primary care support services on behalf of NHS England. Capita informed NHS England that a document containing limited optometry information for 2 patients was accessed. Capita wrote to the 2 individuals to notify them and offer support.
Capita also informed us that 2 files containing names and NHS numbers of deceased and de-registered patients were suspected of being accessed. The files identified archived records that related to individuals who had died more than 10 years ago, or who have not been registered with a GP in England for more than 10 years. Capita informed us that no health data or other patient data was included in the lists or accessed as a result of the incident. NHS England published a statement on its website on the 5 June 2023 to publicly disclose the nature of the incident.[37]
An independent cyber security company, appointed by Capita, has not found any evidence that the information had been made available more widely. Capita continues to further investigate and undertake diagnostic analysis on data that may have been exfiltrated from its systems.
The cyber incident did cause some short-term limited interruption to the operation of PCSE services. NHS England worked with Capita to implement its business continuity plan to mitigate any impacts for primary care.
Overpayments to medical practitioners
If a medical practitioner is suspended, they may be entitled to receive payments under the statutory regulations if the qualifying criteria is met. During the reporting period, NHS England identified payments to 12 medical practitioners (2 of which have been recovered) that did not meet the qualifying criteria when subsequently reviewed. Some of these include where circumstances had changed, and the practitioner was no longer eligible but continued to receive payments and also incorrect amounts calculated due to incorrect application of the guidance. This resulted in overpayments equating to £1.3 million, as noted in the losses and special payment disclosures.
This was an issue that was first identified in 2021/22. To ensure the issue was contained, NHS England commissioned a review of all suspension payments by internal audit to ensure that NHS England understood the full scope of any problems.
To strengthen the controls on this NHS England is implementing changes to how these payments are administered and suspensions are monitored to ensure a standardised approach. This will avoid variability in judgements around applying the guidance with improved oversight from the Professional Standards national team.
NHS England is seeking to recover all overpayments subject to legal advice.
Review of economy, efficiency and effective use of resources
Allocations
NHS England has responsibility for allocating the NHS funding agreed with DHSC as part of our mandate. Please see the Chief Financial Officer’s Report, for information on allocations.
Financial performance monitoring
July 2022 saw the establishment of ICBs, so the financial position for 2022/23 includes 3 months of CCG reporting and 9 months of ICB reporting.
The financial position across the commissioning system was reported monthly using the Integrated Single Financial Environment system and supporting information collections. From July these collections included key elements of provider reporting which facilitated the focus on overall system reporting. Alongside this, NHS providers continued to report their full data using the Provider Financial Monitoring System. This reporting has enabled a detail monthly review by regional and national finance leadership teams and the Chief Financial Officer.
Individual CCG, ICB, direct commissioning and provider financial performance is monitored against KPIs including balance sheet indicators, performance against efficiency plans and specific categories of COVID-19 expenditure, in addition to the reported forecast and year-to-date position.
The financial position of commissioners is consolidated and reported in the overall NHS England accounts. The provider positions, NHS trusts and foundation trusts, are not recorded in the accounts of NHS Improvement or NHS England: these are treated as separate consolidations.
Cabinet Office efficiency controls
As part of the government’s control of expenditure, we are subject to specified expenditure controls. These controls cover a range of expenditure categories and require proposed expenditure to be approved to secure best value for money and ensure efficiency is being maximised. For expenditure above certain thresholds in specified categories (including professional services and consultancy), onward approval is also sought from DHSC and for some cases this also requires approval from the Minister, Cabinet Office and/or HM Treasury.
There were a number of cases during 2022/23 where, predominately because of the operational need to continue services or to deliver Ministerial priorities, some spend was incurred before business cases were fully approved and before the relevant expenditure controls were completed. In some cases, the DHSC declined to provide retrospective approval, and therefore this expenditure is deemed to be irregular. NHS England has continued to work within the organisation to ensure that everyone is aware of the need to pre-approve activity and have worked with the Department to ensure that any urgent cases are reviewed promptly. This has helped reduce the value and instances of irregular spend.
Counter fraud
NHS England has a dedicated counter-fraud team which ensures that appropriate counter-fraud arrangements are in place. This includes proactive activities to prevent and detect fraud, as well as the reactive investigation of allegations of fraud related to our functions.
The Director of Financial Control has day-to-day operational responsibility for the function, and the Chief Financial Officer provides executive support and direction.
We continued to work collaboratively with key partners in both proactive and reactive areas. These include DHSC, NHS Counter Fraud Agency, NHS Business Service Authority, NHS Digital (pre-merger) and others, including law enforcement agencies.
In preparation for the merger, to form the new NHS England a number of key tasks were completed in 2022/23. These included the creation of a new counter-fraud strategy 2023-26, counter-fraud policy and counter-fraud response plan.
Ministerial directions
On 1 February 2023, the statutory functions of NHS Digital transferred to NHS England under the Health and Social Care Information Centre (Transfer of Functions, Abolition and Transitional Provisions) Regulations 2023 (Transfer Regulations).
Under the Transfer Regulations, all previous directions to NHS Digital to establish and operate systems for the collection or analysis of health and social care information (information systems) or to exercise functions in relation to the development or operation of information or communication systems in connection with health or adult social care (system delivery functions), whether given by the Secretary of State or NHS England, and which were in effect on 1 February 2023 are now treated as directions made by the Secretary of State to NHS England. The one exception is for system delivery directions issued by NHS England to NHS Digital – as these relate to NHS England system delivery functions, the directions are no longer required.
There are also the Secretary of State’s financial directions.[38] There were routine financial directions issued every year – but in addition this year (and for subsequent years), they set out NHS England’s budgets, as these no longer appear in the mandate to NHS England (following changes made by the Health and Care Act 2022).
Head of Internal Audit opinion
Internal audit’s opinion is based on a programme of work designed to address the specific assurance requirements of the NHS England Board and focused on areas of risk identified by management. Results of internal audit work, including remedial actions agreed with management, have been regularly reported to management and ARAC.
In the context of the overall environment for NHS England for 2022/23, the opinion of internal audit is that the design of the governance and risk management framework at the year-end is effective and provides the foundation of a framework to take the organisation forward during 2023/24.
The organisation has been under significant operational pressure and subject to large scale change as a result of several factors including recovery from the pandemic and re-establishing business as usual processes, establishment of ICBs and navigating the new landscape NHS England operates in, and the mergers with NHS Improvement, NHS Digital and Health Education England.
Partly as a result of these factors, internal audit has found that while control frameworks are largely defined, there are weaknesses in compliance with those frameworks in a number of areas. In some cases, this has been driven by processes to identify non-compliance being paused to support the pandemic response and not yet fully re-established.
Internal audit has concluded that limited assurance can be provided over the effectiveness and efficiency of the internal control framework.
The limited assurance opinion has in part been driven by the risk-based approach to identifying audit topics and management’s desire to focus on areas where there were known or suspected issues. As a result, internal audit’s findings in these areas are not necessarily an indicator of broader issues across the organisation.
Actions have been agreed to address the issues identified by internal audit. Implementing actions in a timely manner has been challenging in the context of the ongoing organisational change programme and operational pressures, and management continues to focus on this. Management is also implementing a more holistic response to the identified compliance issues through a programme of work to further embed the corporate assurance framework, and as part of developing NHS England’s culture following the organisational mergers. This will include re-establishing processes paused to support the pandemic response where appropriate.
Some of the weaknesses in internal controls for core processes were assessed as being fundamental to the system of controls. Management actions have been agreed to address these observations, not all of which have been completed by year end given their nature. Where possible, interim solutions have been put in place.
There remains significant reliance on third party providers of core services, such as payroll processing, and there remains a requirement to further embed the contract management framework to obtain assurance over the delivery of services.
Remuneration and staff report
Our people
Our NHS People Plan[39] ambitions and values drive our workforce strategy, which aims for more staff working flexibly in a compassionate and inclusive culture. Alongside our People Plan, our NHS People Promise[40] sets out our pledge to one another of how we want to improve the experience of working in the NHS for everyone.
Staff numbers
On 31 March 2023, NHS England directly employed 15,172 staff (14,392 full time equivalents). Of these, 13,333 were permanently employed, and 1,839 were employed on payroll on fixed term contracts of employment. A further 914 individuals were engaged in an off-payroll capacity which includes agency staff and secondees.
All staff by grade
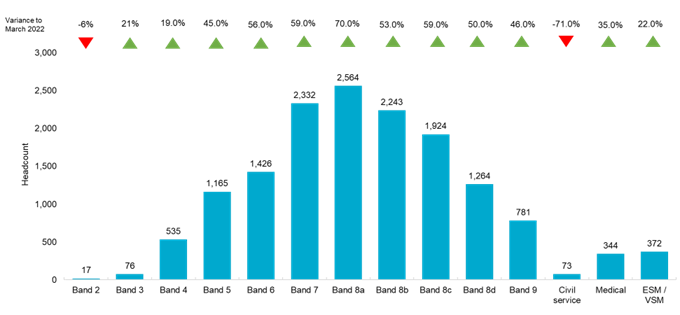
Detail on staff numbers and costs for NHS England and the consolidated group, including CSUs. The chart above shows the headcount by pay band on 31 March 2023.
The headcount of permanent and fixed term staff in NHS England increased by 50% since 31 March 2022. The growth in headcount can be largely attributed to NHS Improvement legally merging with NHS England on 1 July 2022 and NHS Digital transferring to NHS England on 1 February 2023. In preparing to safely receive staff and functions from NHS Digital into NHS England in January 2023, and to be ready to receive Health Education England staff and functions on 1 April 23, NHS England commenced the New NHS England Programme to integrate and restructure all three organisations, to create the new NHS England. In January 2023, a voluntary redundancy scheme was made available for all eligible staff.
Staff turnover
Turnover increased in 2022/23 compared to 2021/22. Both the headcount and the number of people leaving the organisation also increased.
Staff turnover (%)
|
|
April 2018 to March 2019 |
April 2019 to March 2020 |
April 2020 to March 2021 |
April 2021 to March 2022 |
April 2022 to March 2023 |
|
NHS England |
14.0% |
13.2% |
4.88% |
9.65% |
11.01% |
|
NHS TDA |
14.9% |
15.2% |
4.65% |
7.30% |
8.10% |
|
Monitor |
19.4% |
29.5% |
4.13% |
11.58% |
2.21% |
|
NHS Digital |
|
|
|
11.79% |
10.17% |
|
Total |
14.7% |
14.0% |
4.85% |
10.00% |
10.90% |
NHS Digital and Health Education England merger with NHS England
On 22 November 2021, the Secretary of State announced[41] that NHS Digital and Health Education England would merge with NHS England. The NHS England Board committed to reducing the size of the combined organisations by 30% to 40%. On 15 July 2022, recruitment controls were introduced to make the most of our internal talent and maintain staffing levels. Our aim is to come together as an effective organisation with the right vision, values and culture to deliver the best for patients, communities and people.
Our commitment to equality, diversity and inclusion (EDI) will be integral to creating our new culture, drawing on the strengths of all our existing cultures. As a first step, we put EDI at the centre of our work by building on initial engagement activity in 2022, held workshops in February 2023 designed to hear colleagues’ views and further shape our new culture and development of our new behaviour framework. To support the change programme, 135 design leads and team members were trained in the Equality Impact Assessment (EQIA) process, and over 140 EQIA panel members were trained in reviewing EQIA submissions from October to December 2022. EQIA panels are made up of volunteers from across the organisations who bring a wide range of lived experience and expertise, with individual review panels selected to be as balanced and representative as possible. Staff Networks are a key partner in advancing EDI and supporting our people through the organisational change.
Employment policies
Our priorities for 2022/23 included:
- in partnership with trade unions, the continued development and endorsement of new and harmonised human resources policies following the merger of NHS England, NHS TDA and Monitor on 1 July 2022, and the review of the temporary policy changes that were made in response to the pandemic
- identifying the employment policies that would apply to all staff transferring into NHS England from NHS Digital and Health Education England on 1 February and 1 April 2023 respectively
- committing to and beginning engagement with key stakeholders to agree an approach to harmonise of key employment policies which reflect the culture of the new NHS England
Partnership working
Trade unions make a vital contribution to representing the interests of colleagues and our organisations. Partnership work includes consulting on organisational change, a legal requirement, as well as developing and refining our policies and discussing and negotiating on a wide range of issues affecting people and the organisation. We have a National Partnership Forum, which meets regularly and provides strategic direction for other important subgroups which focus on specific issues, including policy, organisational change, equality and diversity and the Local Negotiating Committee. In addition, we have regional and corporate engagement forums to address any local issues, which can be escalated to the national partnership structure(s) if necessary.
To facilitate partnership working between NHS England, NHS Digital and Health Education England ahead of the merger, we set up a trilateral partnership forum, which consisted of management and trade union representatives from across all 3 organisations. This is the forum where we formally consult on all matters relating to the ‘Creating the new NHS England’ change programmes, including organisational change consultations arising from this.
In recognition of the increasing number of medical staff that we employ, especially following the transfer of staff from Public Health England into NHS England in 2021, we set up a Local Negotiating Committee, as a subgroup to the National Partnership Forum. This forum deals with all employment-related issues concerning medical staff’s terms and conditions.
Equality, diversity, and inclusion
Workforce Disability Equality Standard
We have an action plan to improve working conditions for people with disabilities, drawing on the Workforce Disability Equality Standard.[42]
The first priority has been to increase the disability declaration level in the Electronic Staff Record (ESR), as there is a large disparity between those who declare their disability status in ESR, and the disability data collected as part of the annual NHS Staff Survey.
Since April 2020, the organisation has noticed a positive trend in colleagues declaring their disability from 5.6% to 8% in December 2022. However, the staff survey showed the disability declaration rate of 20%, which indicates that there is more to be done on creating trust in the ESR system to support colleagues in making their personal declarations.
The graphs below show the reporting of staff disability/long-term conditions in ESR, in addition to the percentage of senior managers, which is noted as 5%.
Declared disabilities or long term conditions
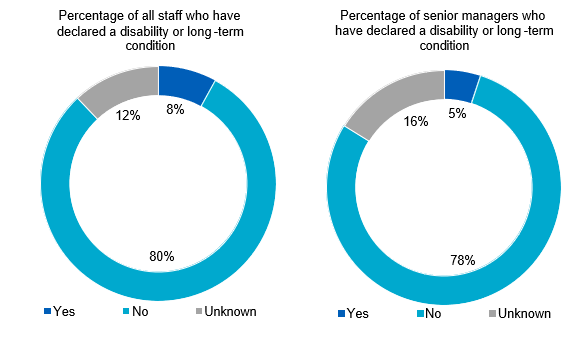
Stonewall Workplace Equality Index
We are committed to building a diverse workforce and that includes creating a safe and inclusive place to work for all our LGB colleagues. NHS England submitted the Stonewall Workplace Equality Index100F[43], which was developed in partnership with our internal LGB Staff Network. We were informed in February 2023 we continued to maintain a position within the top 100 employers in the UK for the second year running; we are currently in the 68th position.
Sexual orientation of staff and senior managers
The percentage of staff who disclose their identity as lesbian, gay and bisexual is 5% as of March 2023. The breakdown of sexual orientation declaration is detailed below, including an overview of senior managers who have declared as LGB in ESR (5%).
Staff and managers by sexual orientation
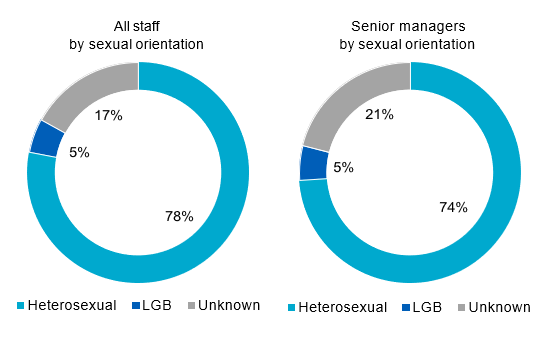
Gender of all staff and senior managers
The female gender profile of the total NHS England ‘on payroll’ workforce decreased by 5.3% between 31 March 2022 and 31 March 2023. There has been a 3.1% increase in the number of female senior managers to 54.7%. The gender diversity of Board members is set out below. The graphs below highlight gender reporting in ESR:
All staff and senior managers by gender
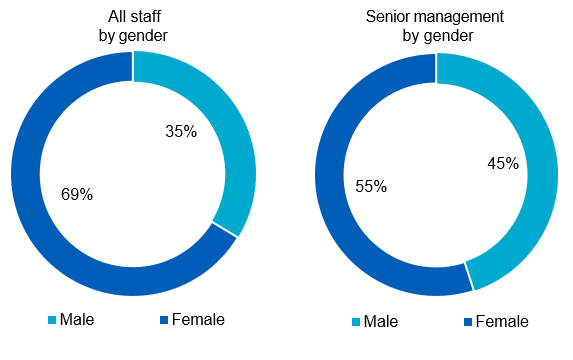
Gender pay gap
Based on the government’s methodology, the mean gender pay gap across NHS England was 14.7%, showing a positive downward trend since 2018 and a 1.5% improvement from the previous year.
|
Year |
Mean gender pay gap |
|
2022 |
14.7% |
|
2021 |
16.2% |
|
2020 |
16.7% |
|
2019 |
18.3% |
|
2018 |
19.5% |
Pay quartiles by gender in NHS England
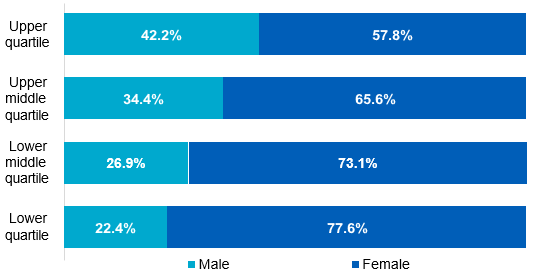
The proportion of males and females in each pay quartile is detailed above, as of 31 March 2022. Women represent the majority of staff in the upper pay quartile of the organisation, which is an increase of 1.5% from the previous year.
Working in partnership with our recognised trade unions and our Women’s Network, we continue to progress initiatives with the aim of addressing gender equality in our workforce.
Our Gender Pay Action Plan includes specific priorities around recruitment practice, reward and recognition, flexible working, developing talent pipelines and intersectionality.
The Gender Pay Gap Report is available on our website.[44]
Ethnicity of all staff and senior managers
19% black and minority ethnic aspirational target across all pay bands
In March 2020, we set an aspirational target to achieve 19% black and minority ethnic representation across all pay bands in the organisation by 2025.
Since the target was set, there has been steady progress as highlighted below, recognising there is more work to be done to build representation across all grades.
Figures below show the overall percentage of black and minority ethnic staff and the change over the last 2 years:
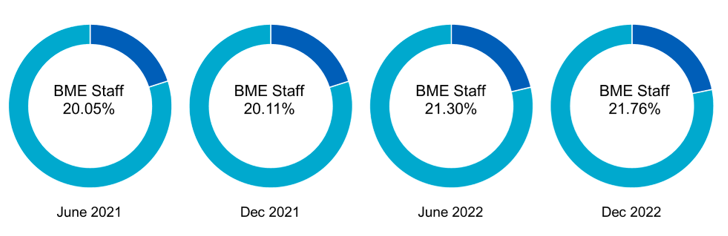
Our focus on black and minority ethnic talent is evidenced through proportionally more black and minority ethnic staff (14.94%) than white staff (11.29%) being promoted between April 2022 and March 2023.
The proportion of people employed by NHS England who consider themselves to be from a black or minority ethnic heritage has remained the same with 20.7% for both 2021/22 and 2022/23. The proportion of senior managers who identify as black or minority ethnic has decreased from 17.0% in 2021/22 to 16.4% in 2022/23.
See the below graphs reflecting the ethnicity reporting in ESR.
All staff and senior managers by ethnicity
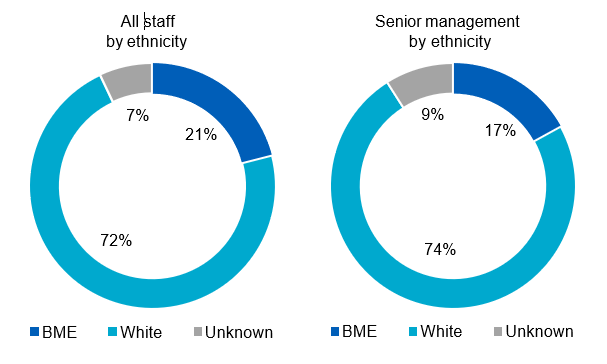
Talent management and development
As we transition to the new NHS England, we have made it our priority to support talent development as we bring teams together across NHS England, NHS Digital and Health Education England. We implemented the recruitment assurance process across all three organisations, ensuring that existing internal talent is harnessed, and business-critical vacancies continue to be filled during the change programme. Our internal recruitment process continues to drive talent progression, creating opportunities for talent growth within our organisation.
We enhanced the organisational development offers available to all colleagues to support internal talent during the change programme. Our ‘Me and My Brand’ workshop series and ‘Supporting You through Change’ webinar series focused on helping colleagues identify their key strengths and development areas, improve application writing and interview skills and tackle imposter syndrome, ensuring internal talent can flourish in the new NHS England. Our Learning Development Hub brings together key learning and development interventions, including our coaching and mentoring offer and our leadership and management development programme which continues to support new and experienced managers to develop their skills, underpinned by health and wellbeing as a core principle.
Our approach to apprenticeships continues to make progress with more than 100 apprentices currently in training. We have partnered with NHS organisations in Leeds to create a cohort of data analyst apprentices who will be able to share experience and skills, creating a future talent pool of individuals with highly sought-after skillsets. We have 44 data analysts in training with the remaining apprentices focused on leadership and management disciplines.
Staff engagement and feedback
We carried out a full staff survey on 3 October 2022 for 8 weeks, closing on 25 November 2022, with a response rate of 63%, with 7,611 staff completing the survey.
Sickness absence
Sickness absence for the period 1 April 2022 to 31 March 2023 was as follows:
|
|
Whole time equivalent days available |
|
Whole time equivalent days lost to sickness absence |
|
Sickness absence rate | |
|
NHS England |
|
5,279,191 |
|
124,442 |
|
2.38% |
|
CSU |
|
2,332,095 |
|
65,004 |
|
2.79% |
|
Total |
|
7,635,084 |
|
182,172 |
|
2.39% |
Trade union facility time disclosures
We will fulfil our obligations under the Trade Union (Facility Time Publication Requirements) Regulations 2017 for 2022/23 by reporting the information to form part of the government’s public sector trade union facility time data, which has to be submitted by July 2023. Below is last year’s submission, which is published on the gov.uk website in August each year.[45] Please note that this includes NHS Digital and NHS England data for 2022/23.
Trade union representatives – the total number of employees who were trade union representatives during the relevant period:
|
Number of employees who were relevant union officials during the relevant period |
|
WTE employee number |
|
45 |
|
44.4 |
Percentage of time spent on facility time (duties and activities):
|
Percentage of time |
|
Number of employees |
|
0% |
|
24 |
|
1-50% |
|
20 |
|
51-99% |
|
0 |
|
100% |
|
1 |
Percentage of pay bill spent on facility time – the figures requested in the first column of the table below will determine the percentage of the total pay bill spent on paying employees who were trade union representatives for facility time during the relevant period:
|
Description |
|
Figures |
|
Provide the total cost of facility time |
|
£81,042.79 |
|
Provide the total pay bill |
| £1,032,277,344[46] |
|
Provide the percentage of the total pay bill spent on facility time, calculated as: (total cost of facility time – total pay bill) x 100 |
| 0.02%[47] |
Employee benefits and staff numbers (subject to audit)
Detail on staff numbers and costs for NHS England and the consolidated group, including CSUs, are presented in the following tables:
Average number of people employed
|
Parent 2022/23 |
| Permanently employed number[48] |
|
CSU employed number |
|
Other number |
|
CSU other number |
|
Total number |
|
Total |
|
13,293 |
|
7,150 |
|
1,956 |
|
252 |
|
22,651 |
|
Of the above: |
|
|
|
|
|
|
|
|
|
|
|
Number of whole time equivalent people engaged on capital projects |
|
245 |
|
– |
|
24 |
|
– |
|
269 |
|
Parent 2021/22 |
|
Permanently employed number |
|
CSU employed number |
|
Other number |
|
CSU other number |
|
Total number |
|
Total |
|
7,754 |
|
6,897 |
|
844 |
|
430 |
|
15,925 |
|
Of the above: |
|
|
|
|
|
|
|
|
|
|
|
Number of whole time equivalent people engaged on capital projects |
|
– |
|
– |
|
– |
|
– |
|
– |
|
Consolidated group 2022/23 |
|
Permanently employed number |
|
CSU employed number |
|
Other number |
|
CSU other number |
|
Total number |
|
Total |
|
35,383 |
|
7,150 |
|
4,122 |
|
252 |
|
46,907 |
|
Of the above: |
|
|
|
|
|
|
|
|
|
|
|
Number of whole time equivalent people engaged on capital projects |
|
245 |
|
– |
|
24 |
|
– |
|
269 |
|
Consolidated group 2021/22 |
|
Permanently employed number |
|
CSU employed number |
|
Other number |
|
CSU other number |
|
Total number |
|
Total |
|
27,777 |
|
6,897 |
|
2,814 |
|
430 |
|
37,918 |
|
Of the above: |
|
|
|
|
| |||||
|
Number of whole time equivalent people engaged on capital projects |
|
– |
|
– |
|
– |
|
– |
|
– |
Employee benefits
|
Parent group 2022/23 |
Permanently employed |
Permanent CSU employees |
Other |
CSU |
Total |
|
Employee benefits |
|
|
|
|
|
|
Salaries and wages |
738,631 |
301,482 |
104,581 |
19,410 |
1,164,104 |
|
Social security costs |
85,414 |
32,521 |
– |
– |
117,935 |
|
Employer contributions to NHS Pension Scheme |
122,765 |
52,001 |
– |
– |
174,766 |
|
Other pension costs |
11 |
– |
– |
– |
11 |
|
Apprenticeship Levy |
3,343 |
1,502 |
– |
– |
4,845 |
|
Other post-employment benefits |
– |
– |
– |
– |
– |
|
Termination benefits |
78,945 |
(86) |
– |
– |
78,859 |
|
Gross employee benefits expenditure |
1,029,807 |
387,420 |
104,581 |
19,410 |
1,540,520 |
|
Less: Employee costs capitalised |
(3,302) |
– |
(754) |
– |
(4,056) |
|
Net employee benefits excluding capitalised costs |
1,025,807 |
387,420 |
103,827 |
19,410 |
1,536,464 |
|
Less recoveries in respect of employee benefits |
124 |
– |
(75) |
– |
49 |
|
Total net employee benefits |
1,025,931 |
387,420 |
103,752 |
19,410 |
1,536,513 |
|
Parent group 2021/22 |
Permanently employed |
Permanent CSU employees |
Other |
CSU |
Total |
|
Employee benefits |
|
|
|
|
|
|
Salaries and wages |
491,283 |
301,959 |
61,913 |
22,514 |
877,669 |
|
Social security costs |
56,417 |
32,803 |
– |
5 |
89,225 |
|
Employer contributions to NHS Pension Scheme |
90,413 |
55,335 |
– |
– |
145,748 |
|
Other pension costs |
– |
7 |
– |
– |
7 |
|
Apprenticeship Levy |
2,447 |
2,858 |
– |
– |
5,305 |
|
Other post-employment benefits |
– |
154 |
– |
– |
154 |
|
Termination benefits |
542 |
705 |
– |
– |
1,247 |
|
Gross employee benefits expenditure |
641,102 |
393,821 |
61,913 |
22,519 |
1,119,355 |
|
Less: Employee costs capitalised |
– |
– |
– |
– |
– |
|
Net employee benefits excluding capitalised costs |
641,102 |
393,821 |
61,913 |
22,519 |
1,119,355 |
|
Less recoveries in respect of employee benefits |
(274) |
– |
(32) |
– |
(306) |
|
Total net employee benefits |
640,828 |
393,821 |
61,881 |
22,519 |
1,119,049 |
|
Consolidated group 2022/23 |
Permanently employed |
Permanent CSU employees |
Other |
CSU |
Total |
|
Employee benefits |
|
|
|
|
|
|
Salaries and wages |
1,938,829 |
301,482 |
261,003 |
19,410 |
2,520,724 |
|
Social security costs |
223,186 |
32,521 |
681 |
– |
256,388 |
|
Employer contributions to NHS Pension Scheme |
327,632 |
52,001 |
701 |
– |
380,334 |
|
Other pension costs |
2,941 |
– |
– |
– |
2,941 |
|
Apprenticeship Levy |
8,162 |
1,502 |
– |
– |
9,664 |
|
Other post-employment benefits |
– |
– |
– |
– |
– |
|
Termination benefits |
91,304 |
(86) |
– |
– |
91,218 |
|
Gross employee benefits expenditure |
2,592,054 |
387,420 |
262, 385 |
19,410 |
3,261,269 |
|
Less: Employee costs capitalised |
(3,302) |
– |
(754) |
– |
(4,056) |
|
Net employee benefits excluding capitalised costs |
2,588,752 |
387,420 |
261,631 |
19,410 |
3,257,213 |
|
Less recoveries in respect of employee benefits |
(9,118) |
– |
(75) |
– |
(9,193) |
|
Total net employee benefits |
2,579,634 |
387,420 |
261,556 |
19,410 |
3,248,020 |
|
Consolidated group 2021/22 |
Permanently employed |
Permanent CSU employees |
Other |
CSU other |
Total |
|
Employee benefits |
|
|
|
|
|
|
Salaries and wages |
1,485,366 |
301,959 |
195,976 |
22,514 |
2,005,815 |
|
Social security costs |
167,266 |
32,803 |
547 |
5 |
200,621 |
|
Employer contributions to NHS Pension Scheme |
272,369 |
55,335 |
453 |
– |
328,157 |
|
Other pension costs |
1,147 |
7 |
– |
– |
1,154 |
|
Apprenticeship Levy |
6,017 |
2,858 |
– |
– |
8,875 |
|
Other post-employment benefits |
– |
154 |
– |
– |
154 |
|
Termination benefits |
3,814 |
705 |
– |
– |
4,519 |
|
Gross employee benefits expenditure |
1,935,979 |
393,821 |
196,976 |
22,519 |
2,549,295 |
|
Less: Employee costs capitalised |
– |
– |
– |
– |
– |
|
Net employee benefits excluding capitalised costs |
1,935,979 |
393,821 |
196,976 |
22,519 |
2,549,295 |
|
Less recoveries in respect of employee benefits |
(11,810) |
– |
(32) |
– |
(11,842) |
|
Total net employee benefits |
1,924,169 |
393,821 |
196,944 |
22,519 |
2,537,453 |
CSUs are part of NHS England and provide services to CCGs/ICBs.
The employment contracts or secondment agreements of almost all these staff are held for NHS England on a ‘hosted basis’ by the NHS BSA.
SCCL provided for 6 months of 2021/22.
Exit packages, severance payments and off-payroll engagements
Expenditure on consultancy and contingent labour
Expenditure on consultancy is detailed in the Annual Accounts under Note 4: Operating expenses. NHS England and CSUs procured consultancy services worth £17.3 million during the financial year, a decrease of £16.6 million since previous year (2021/22: £33.9 million).
Across the group, there was a total spend of £51.1 million on consultancy services during the period, against £75.7 million the previous year.
Expenditure on contingent labour, including agency staff and secondees, is given in the employee benefits table below, under the ‘other’ column.
Net expenditure for NHS England and CSUs in this area was £124 million in 2022/23, against £84.4 million in 2021/22. Across the group, there was a total spend of £281.8 million on contingent labour during the year, against £219.5 million the previous year. The increase in these 2 figures are due to legacy NHS Digital contingent labour costs, along with a full year of SCCL costs (2021/22 only accounted for 6 months of SCCL costs).
Further detail on efficiency controls, and steps we have taken to improve procurement practices and compliance within NHS England during the year, can be found in our governance statement below.
|
Contingent labour |
|
2022/23 |
|
2021/22 |
|
(Increase) / Decrease |
|
Parent Inc CSU Other |
|
123,991 |
|
84,432 |
|
(39,559) |
|
CSU Other |
|
19,410 |
|
22,519 |
|
3,109 |
|
Group Other |
|
262,385 |
|
196,976 |
|
(65,409) |
|
Total group contingent labour |
|
281,795 |
|
219,495 |
|
|
|
Consultancy |
|
2022/23 |
|
2021/22 |
|
(Increase) / Decrease £000 |
|
Parent consultancy |
|
17,290 |
|
33,899 |
|
16,609 |
|
Group consultancy |
|
51,147 |
|
75,764 |
|
24,617 |
Off-payroll engagements
NHS England is committed to employing a capable, talented, and diverse on-payroll workforce to support the delivery of its business. It is recognised that in some specific circumstances the use of off-payroll workers, working alongside our on-payroll workforce, can be helpful. For some of our time-limited programmes, short-term contracts are appropriate. The following tables identify off-payroll workers engaged by NHS England at March 2023. Off-payroll workers engaged by ICBs are reported in ICB annual reports and published on their websites.[49]
Off-payroll engagements longer than 6 months
Off-payroll engagements on 31 March 2023, covering those earning more than £245[50] per day and staying longer than 6 months are as follows:
|
Off-payroll engagements longer than 6 months | NHS England[51] (number) |
CSUs (number) |
SCCL (number) |
Total (number) |
|
Number of existing engagements as of 31 March 2023 |
420 |
107 |
0 |
527 |
|
Of which, the number that have existed: |
|
|
|
|
|
for less than 1 year at the time of reporting |
80 |
96 |
0 |
176 |
|
for between 1 and 2 years at the time of reporting |
164 |
10 |
0 |
174 |
|
for between 2 and 3 years at the time of reporting |
87 |
1 |
0 |
88 |
|
for between 3 and 4 years at the time of reporting |
45 |
0 |
0 |
45 |
|
for 4 or more years at the time of reporting |
44 |
0 |
0 |
44 |
Most off-payroll workers who provide services to NHS England are clinical medical staff. All existing off-payroll engagements, outlined above, were subject to a risk-based assessment as to whether assurance was required that the individual was paying the right amount of tax and, where necessary, assurance has been sought.
New off-payroll engagements
New off-payroll engagements or those that reached 6 months in duration, between 1 April 2022 and 31 March 2023, for more than £245[52] per day and that last longer than 6 months are as follows:
|
New off-payroll engagements |
NHS England110F[53] (number) |
CSUs (number) |
SCCL (number) |
Total (number) |
|
Number of off-payroll workers engaged during the year ended 31 March 2023 |
142 |
205 |
0 |
347 |
|
Of which: |
|
|
|
|
| Number not subject to off-payroll legislation[54] |
115 |
0 |
0 |
115 |
| Number subject to off-payroll legislation and determined as in-scope of IR35 |
24 |
205 |
0 |
229 |
| Number subject to off-payroll legislation and determined as out of scope of IR35 |
3 |
0 |
0 |
3 |
|
Number of engagements reassessed for compliance or assurance purposes during the year |
0 |
0 |
0 |
0 |
|
Of which: |
|
|
|
|
|
Number of engagements that saw a change to IR35 status following review |
0 |
0 |
0 |
0 |
Off-payroll board member/senior official engagement
Off-payroll engagements of Board members and/or senior officials with significant financial responsibility between 1 April 2022 and 31 March 2023 are shown in the table below:
|
Off-payroll board member/senior official engagement | NHS England[55] (number) |
CSUs (number) |
SCCL (number) |
Total (number) |
|
Number of off-payroll engagements of Board members and/or senior officers with significant financial responsibility, during the financial year |
0 |
0 |
0 |
0 |
|
Total number of individuals on-payroll and off-payroll who have been deemed ‘Board members and/or senior officials with significant financial responsibility’ during the financial year |
365 |
31 |
0 |
396 |
Senior officials are defined as those at pay grade executive senior manager (ESM) 1 and ESM2.
Details of exit packages agreed over the year are detailed in the following tables. All contractual severance payments were subject to full external oversight by DHSC.
Exit packages agreed during the year (subject to audit)
|
Parent |
2022/23 |
2021/22 | ||||
|
Compulsory redundancies |
Other agreed departures |
Total |
Compulsory redundancies |
Other agreed departures |
Total | |
|
Less than £10,000 |
1 |
25 |
26 |
1 |
1 |
2 |
|
£10,001 to £25,000 |
2 |
124 |
126 |
1 |
– |
1 |
|
£25,001 to £50,000 |
3 |
220 |
223 |
2 |
– |
2 |
|
£50,001 to £100,000 |
1 |
261 |
262 |
3 |
– |
3 |
|
£100,001 to £150,000 |
1 |
216 |
217 |
1 |
– |
1 |
|
£150,001 to £200,000 |
3 |
106 |
109 |
1 |
– |
1 |
|
Over £200,001 |
– |
– |
– |
– |
– |
– |
|
Total |
11 |
952 |
963 |
9 |
1 |
10 |
|
Total cost (£000) |
837 |
74,704 |
75,541 |
601 |
5 |
606 |
|
Parent |
2022/23 |
2021/22 | ||
|
Departures where special payments have been made |
Departures where special payments have been made |
Departures where special payments have been made |
Departures where special payments have been made | |
|
Less than £10,000 |
– |
– |
1 |
5,256 |
|
Total |
– |
– |
1 |
5,256 |
|
Consolidated group |
2022/23 |
2021/22 | ||||
|
Compulsory redundancies |
Other agreed departures |
Total |
Compulsory redundancies |
Other agreed departures |
Total | |
|
Less than £10,000 |
54 |
51 |
105 |
7 |
12 |
19 |
|
£10,001 to £25,000 |
30 |
156 |
186 |
7 |
10 |
17 |
|
£25,001 to £50,000 |
18 |
256 |
274 |
11 |
5 |
16 |
|
£50,001 to £100,000 |
17 |
289 |
306 |
4 |
4 |
8 |
|
£100,001 to £150,000 |
7 |
217 |
224 |
11 |
– |
11 |
|
£150,001 to £200,000 |
37 |
108 |
145 |
7 |
4 |
11 |
|
Over £200,001 |
– |
– |
– |
– |
– |
– |
|
Total |
163 |
1,077 |
1,240 |
47 |
35 |
82 |
|
Total cost (£000) |
9,352 |
78,996 |
88,348 |
3,319 |
1,424 |
4,743 |
|
Consolidated group |
2022/23 |
2021/22 | ||
|
Departures where special payments have been made |
Departures where special payments have been made |
Departures where special payments have been made |
Departures where special payments have been made | |
|
Less than £10,000 |
– |
– |
3 |
19,902 |
|
£10,001 to £25,000 |
1 |
20,000 |
2 |
35,251 |
|
£25,001 to £50,000 |
1 |
30,000 |
2 |
61,128 |
|
£50,001 to £100,000 |
– |
– |
2 |
137,152 |
|
Total |
2 |
50,000 |
9 |
253,433 |
Analysis of other agreed departures (subject to audit)
|
Parent |
2022/23 |
2021/22 | ||
|
Other agreed departures |
Other agreed departures |
Other agreed departures |
Other agreed departures | |
|
Voluntary redundancies including early retirement contractual costs |
951 |
74,696 |
– |
– |
|
Mutually agreed resignations (MARS) contractual costs |
– |
– |
– |
– |
|
Contractual payments in lieu of notice |
1 |
8 |
– |
– |
|
Exit payments following Employment Tribunals or court orders |
– |
– |
– |
– |
|
Non-contractual payments requiring HM Treasury approval |
– |
– |
1 |
5 |
|
Total |
952 |
74,704 |
1 |
5 |
|
Consolidated group |
2022/23 |
2021/22 | ||
|
Other agreed departures |
Other agreed departures |
Other agreed departures |
Other agreed departures | |
|
Voluntary redundancies including early retirement contractual costs |
955 |
75,251 |
7 |
805 |
|
MARS contractual costs |
91 |
3,115 |
1 |
90 |
|
Early retirements in the efficiency of the service contractual costs |
1 |
8 |
– |
– |
|
Contractual payments in lieu of notice |
29 |
572 |
19 |
276 |
|
Exit payments following Employment Tribunals or court orders |
– |
– |
1 |
13 |
|
Non-contractual payments requiring HM Treasury approval |
2 |
50 |
8 |
241 |
|
Total |
1,078 |
78,996 |
36 |
1,425 |
The level of voluntary redundancies has increased significantly in the parent, compared to prior year. In this financial year NHS England underwent a significant restructure to reduce the size of the organisation by between 30% to 40%. This was to reflect the merger of NHS England with NHS Digital in January 2023 and Health Education England from April 2023 and the need to resize the organisation post the Covid 19 pandemic.
As a single exit package can be made up of several components, each of which will be counted separately in this table, the total number of exit packages will not necessarily match the total number in the table above.
These tables report the number and value of exit packages agreed in the financial year. The expense associated with these departures may have been recognised in part or in full in a previous period.
Redundancy and other departure costs have been paid in accordance with the provisions of NHS England.
Exit costs are accounted for in accordance with relevant accounting standards and, at the latest, in full in the year of departure.
Where NHS England and CCGs and ICBs have agreed early retirements, the additional costs are met by NHS England or the CCG or the ICB and not by the NHS Pension Scheme and are included in the tables. Ill-health retirement costs are met by the NHS Pension Scheme and are not included in the tables.
The Remuneration report includes the disclosure of exit payments payable to individuals named in that report.
Remuneration report
People, Remuneration and Nominations Committee
Detail on the role and activity of the Strategic HR and Remuneration Committee is given in our Directors’ Report.
Percentage change in remuneration of highest paid director (subject to audit)
|
Percentage change in remuneration of highest paid director |
|
Salary and allowances |
|
Performance pay and bonuses |
|
The percentage change from the previous financial year in respect of the highest paid director |
|
0% |
|
0% |
|
The average percentage change from the previous financial year in respect of employees of the entity, taken as a whole |
|
3.00% |
|
2,423.19% |
The large average percentage increase in performance pay and bonuses across NHS England can be explained by the retrospectively agreed Governments’ Agenda for Change (AfC 2022/23 Non-Consolidated Pay Award that consisted of 2 one off non-consolidated awards on top of the 2022/23 consolidated award agreed earlier in the year. Employees received a non-consolidated award worth 2%, in addition to a one-off NHS backlog bonus worth an additional 4% of the AfC pay bill to recognise the sustained pressure facing the NHS following the COVID-19 pandemic.
Pay ratio information (subject to audit)
Reporting bodies are required to disclose the relationship between the total remuneration of the highest-paid director/member in their organisation against the 25th percentile, median and 75th percentile of remuneration of the organisation’s workforce. Total remuneration of the employee at the 25th percentile, median and 75th percentile is further broken down to disclose the salary component.
The banded remuneration of the highest paid director/member in NHS England in the financial year 2022/23 was £255,000 to £260,000 (2021/22: £255,000-£260,000). The relationship to the remuneration of the organisation’s workforce is disclosed in the below table.
|
2022/23 |
|
25th percentile |
|
Median |
|
75th percentile |
|
Total remuneration (£) |
|
37,633 |
|
50,847 |
|
69,855 |
|
Salary component of total remuneration (£) |
|
35,572 |
|
48,526 |
|
67,064 |
|
Pay ratio information |
|
6.84:1 |
|
5.06:1 |
|
3.69:1 |
|
2021/22 |
|
25th percentile |
|
Median |
|
75th percentile |
|
Total remuneration (£) |
|
32,306 |
|
47,126 |
|
63,862 |
|
Salary component of total remuneration (£) |
|
32,306 |
|
47,126 |
|
63,862 |
|
Pay ratio information |
|
7.97:1 |
|
5.46:1 |
|
4.03:1 |
The pay ratio information for the 2022/23 financial year is consistent with the pay, reward and progression policies for the employees taken as a whole, due to applying all nationally mandated Pay Awards where applicable and adhering to the relevant pay progression principles. The increased total remuneration at the 25th, median and 75th percentiles versus the salary component of total remuneration at the 25th, median and 75th percentiles were attributable to the AfC 2022/23 Non-Consolidated Pay Award, as referenced above.
In 2022/23, no employees received remuneration in excess of the highest-paid director/ member (2021/22: none). Remuneration ranged from £7,883 to £260,000 (2021/22: £7,883 to £260,000).
Total remuneration includes salary, non-consolidated performance-related pay (PRP), benefits-in-kind, but not severance payments. It does not include employer pension contributions and the cash equivalent transfer value of pensions.
Policy on remuneration of senior managers
The framework for the remuneration of executive directors is set by DHSC through the ESM pay framework for ALBs.
It is NHS England’s policy to pay salaries that are appropriate to recruit senior managers with the necessary skills, capability and experience for the effective running of a more than £158 billion organisation, while recognising the importance of demonstrating pay restraint at a time of considerable pressure on NHS finances. Recommending appropriate remuneration for executive directors is undertaken by the People, Remuneration and Nominations Committees. Final decisions are made by the DHSC ALB Remuneration Committee and HM Treasury, where appropriate.
Performance-related pay
The PRP arrangements for national (executive) directors are set out in the ESM pay framework for ALBs. They follow guidance prescribed by DHSC and are in line with HM Treasury requirements. As a local policy decision, NHS England does not currently allocate any funding for PRP non-consolidated bonus payments. In recognition of the current economic climate and the need to provide effective system leadership for the NHS, the decision was taken by the Strategic HR and Remuneration Committee and Nomination and Remuneration Committee not to allocate funds for PRP non-consolidated bonus payments for 2022/23. Secondees are subject to the terms and conditions of their employing organisation.
Policy on senior managers’ contracts
Contracts of employment for senior managers are open-ended and recurrent, unless otherwise specified. Notice periods follow the provisions of the ESM contract of employment, as applied by NHS England, of 6 months’ contractual notice. Termination payments can only be authorised where they are contractual and, subject to the value involved, may still require further approval from the DHSC Governance and Assurance Committee. Any proposed non-contractual special severance payment requires formal approval from DHSC and HM Treasury.
Payments for loss of office (subject to audit)
A payment was made to 1 senior manager to compensate for loss of office during 2022/23, and details of this payment are included in the senior manager salary and pension entitlement table.
Payments to past directors (subject to audit)
No payments have been made to past directors and no compensation has been paid on early retirement. This is subject to audit.
Senior managers’ service contracts
|
Name and title |
Date of appointment |
Notice period |
Provisions for compensation for |
Other details |
|
Amanda Pritchard Chief Executive Officer |
1 August 2021 |
6 months |
Option to provide taxable pay in lieu
|
|
|
Sir David Sloman Chief Operating Officer – Joint |
14 December 2021 |
6 months |
| |
|
Mark Cubbon Chief Delivery Officer – Joint |
14 December 2021 |
6 months |
Left NHS England 2 April 2023 | |
|
Ian Dodge |
7 July 2014 |
6 months |
Left NHS England 30 June 2022 | |
|
Jacqueline Rock |
1 January 2022 |
6 months |
| |
|
Professor Sir Stephen Powis National Medical Director – Joint |
1 March 2018 |
6 months |
| |
|
Julian Kelly CB Chief Financial Officer – Joint |
1 April 2019 |
6 months |
| |
|
Dame Ruth May Chief Nursing Officer – Joint |
7 January 2019 |
6 months |
| |
|
Prerana Issar Chief People Officer – Joint |
1 April 2019 |
6 months |
Left NHS England 4 October 2022 | |
|
Dr Tim Ferris National Director of Transformation – Joint |
10 May 2021 |
6 months |
| |
|
Christopher Hopson Chief Strategy Officer – Joint |
13 June 2022 |
6 months |
| |
|
Dr Navina Evans Chief Workforce Officer |
1 July 2022 |
6 months |
|
The senior managers indicated as ‘joint’ in the above table were jointly appointed across NHS England and NHS Improvement (consisting of NHS TDA and Monitor) until 30 June 2022. Full salary disclosures are included within the Remuneration Reports of all 3 entities and the costs are split equally between NHS England and NHS Improvement, with NHS Improvement costs being split at a ratio of 2:1 NHS TDA-to-Monitor.
Remuneration (salary, benefits in kind and pensions) 2022/23
(subject to audit)
|
Name and title |
(a) Salary (bands of £5,000) |
(b) |
(c) Performance pay and bonuses (bands of £5,000) |
(d) Long-term performance pay and bonuses |
(e) Pension-related benefits |
(f) Total |
|
Amanda Pritchard |
255-260 |
0 |
0 |
0 |
70-72.5 |
325-330 |
|
Sir David Sloman |
235-240 |
3,900 |
0 |
0 |
0 |
245-250 |
|
Mark Cubbon |
220-225 |
1,900 |
0 |
0 |
50-52.5 |
270-275 |
|
Ian Dodge |
200-205 |
0 |
0 |
0 |
0 |
200-205 |
|
Jacqueline Rock |
230-235 |
0 |
0 |
0 |
50-52.5 |
280-285 |
|
Professor Stephen Powis |
235-240 |
0 |
0 |
0 |
0 |
235-240 |
|
Julian Kelly CB Chief Financial Officer |
210-215 |
0 |
0 |
0 |
50-52.5 |
260-265 |
|
Dame Ruth May Chief Nursing Officer117F[60] |
175-180 |
0 |
0 |
0 |
0 |
175-180 |
|
Prerana Issar Chief People Officer118F[61] |
150-155 |
0 |
0 |
0 |
92.5-95 |
245-250 |
|
Dr Tim Ferris National Director of Transformation119F[62] |
190-195 |
0 |
0 |
0 |
0 |
190-195 |
|
Christopher Hopson Chief Strategy Officer120F[63] |
165-170 |
0 |
0 |
0 |
37.5-40 |
205-210 |
|
Navina Evans |
75-80 |
0 |
0 |
0 |
0 |
75-80 |
Remuneration (salary, benefits in kind and pensions) 2021/22
(subject to audit)
|
Name and title |
(a) Salary (bands of £5,000) |
(b) Benefits in kind (taxable) to nearest £000 |
(c) Performance pay and bonuses (bands of £5,000) |
(d) Long-term performance pay and bonuses (bands of £5,000) |
(e) |
(f) Total (a to e) (bands of £5,000) |
|
Sir Simon Stevens |
65-70 |
0 |
0 |
0 |
0 |
65-70 |
|
Amanda Pritchard |
255-260 |
0 |
0 |
0 |
74 |
330-335 |
|
Mark Cubbon |
80-85 |
300 |
0 |
0 |
16 |
95-100 |
|
Sir David Sloman |
65-70 |
1300 |
0 |
0 |
0 |
65-70 |
|
Ian Dodge |
170-175 |
0 |
0 |
0 |
0 |
170-175 |
|
Dr Emily Lawson |
65-70 |
0 |
0 |
0 |
0 |
65-70 |
|
Blake Dark |
75-80 |
0 |
0 |
0 |
19 |
95-100 |
|
Jacqueline Rock |
55-60 |
0 |
0 |
0 |
13 |
70-75 |
|
Professor Sir Stephen Powis |
225-230 |
0 |
0 |
0 |
0 |
225-230 |
|
Julian Kelly CB |
205-210 |
0 |
0 |
0 |
50 |
255-260 |
|
Dame Ruth May |
180-185 |
0 |
0 |
0 |
33 |
210-215 |
|
Prerana Issar |
230-235 |
0 |
0 |
0 |
54 |
280-285 |
|
Matthew Gould CMG MBE |
100-105 |
0 |
0 |
0 |
21 |
120-125 |
|
Dr Tim Ferris |
170-175 |
0 |
0 |
0 |
0 |
170-175 |
Pension benefits (subject to audit)
|
Name and title |
Real increase in pension at pension age (bands of £2,500) |
Real increase in pension lump sum at pension age (bands of £2,500) |
Total accrued pension at pension age on 31 March 2023 (bands of £5,000) |
Lump sum at pension age related to accrued pension on 31 March 2023 (bands of £5,000) |
Cash Equivalent Transfer Value on 31 March 2022132F[75] |
Real Increase in Cash Equivalent Transfer Value |
Cash Equivalent Transfer Value on 31 March 2023 |
Employer’s contribution to partnership pension |
|
Amanda Pritchard |
5-7.5 |
(2.5)-0 |
90-95 |
135-140 |
1,229 |
56 |
1,340 |
0 |
|
Mark Cubbon |
2.5-5 |
(2.5)-0 |
65-70 |
110-115 |
1,025 |
43 |
1,129 |
0 |
|
Sir David Sloman |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Ian Dodge |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Jacqueline Rock |
2.5-5 |
N/A |
5-10 |
N/A |
14 |
26 |
72 |
0 |
|
Professor Sir Stephen Powis |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Julian Kelly |
2.5-5 |
N/A |
15-20 |
N/A |
152 |
26 |
211 |
0 |
|
Dame Ruth May |
(15)-(12.5) |
65-67.5 |
65-70 |
310-315 |
1,763 |
0 |
43 |
0 |
|
Prerana Issar |
5-7.5 |
N/A |
15-20 |
N/A |
151 |
50 |
228 |
0 |
|
Dr Tim Ferris National Director of Transformation[80] |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Christopher Hopson |
2.5-5 |
N/A |
0-5 |
N/A |
0 |
23 |
46 |
0 |
|
Dr Navina Evans |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
Cash equivalent transfer values (CETV) (subject to audit)
A CETV is the actuarially assessed capital value of the pension scheme benefits accrued by a member at a particular point in time.
The benefits valued are the member’s accrued benefits and any contingent spouse’s (or other allowable beneficiary’s) pension payable from the scheme.
A CETV is a payment made by a pension scheme or arrangement to secure pension benefits in another pension scheme or arrangement when the member leaves a scheme and chooses to transfer the benefits accrued in their former scheme.
The pension figures shown relate to the benefits that the individual has accrued as a consequence of their total membership of the pension scheme, not just their service in a senior capacity to which disclosure applies.
The CETV figures and the other pension details include the value of any pension benefits in another scheme or arrangement which the individual has transferred into the NHS Pension Scheme. They also include any additional pension benefit accrued to the member as a result of their purchasing additional years of pension service in the scheme at their own cost. CETVs are calculated within the guidelines and framework prescribed by the Institute and Faculty of Actuaries.
Real increase in CETV
This reflects the increase in CETV effectively funded by the employer. It does not include the increase in accrued pension due to inflation or contributions paid by the employee (including the value of any benefits transferred from another scheme or arrangement) and uses common market valuation factors for the start and end of the period.
Policy on remuneration of non-executive directors
The remuneration of non-executive directors is set by DHSC on appointment and is non-pensionable. All non-executive directors are paid the same amount, except the Chair, Vice Chair and Chair of ARAC, to reflect the equal time commitment expected from each non-executive director. The Chair, Vice Chair and Chair of ARAC are entitled to higher amounts to reflect the increased time commitment associated with their respective roles.
Some non-executive directors, including the Vice Chair, have opted to waive their contractual remuneration. Non-executive directors do not receive PRP or pensionable remuneration.
|
Name and title |
Date of appointment |
Unexpired term at |
Notice period |
Provisions for compensation for early termination |
Other details |
|
Richard Meddings CBE Chair |
25 March 2022 |
36 months |
3 months |
None |
|
|
Wol Kolade Vice Chair |
25 March 2022 |
24 months |
3 months |
None |
Waived entitlement to remuneration |
|
Professor Lord Ara Darzi Non-Executive Director |
1 April 2020 |
0 months |
3 months |
None |
Left NHS England on 30 |
|
Jeremy Townsend Non-Executive Director Chair of ARAC |
1 October 2020 |
42 months |
3 months |
None |
Returned from temporary transfer to NHS Improvement on 1 July 2022 |
|
Laura Wade-Gery Non-Executive Director |
6 November 2020 |
4 months |
3 months |
None |
Left on 30 June 2023 |
|
Rakesh Kapoor Non-Executive Director |
1 January 2021 |
9 months |
3 months |
None |
Returned from temporary transfer to NHS Improvement on 1 April 2022 |
|
Susan Kilsby Non-Executive Director |
1 January 2021 |
9 months |
3 months |
None |
|
|
Michael Coupe Non-Executive Director |
1 January 2021 |
45 months |
3 months |
None |
|
|
Professor Sir Munir Pirmohamed Non-Executive Director |
1 July 2022 |
9 months |
3 months |
None |
|
|
Sir Andrew Morris Non-Executive Director |
1 July 2022 |
24 months |
3 months |
None |
|
|
Sir David Behan Non-Executive Director |
1 September 2022 |
17 months |
3 months |
None |
Chair of Health Education England |
|
Baroness Mary Watkins Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
|
Professor Sir Simon Wessely Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
|
Sir Mark Walport Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
Non-executive director service contracts
|
Name and title |
Date of appointment |
Unexpired term at 31 March 2023 |
Notice period |
Provisions for compensation for early termination |
Other details |
|
Richard Meddings CBE Chair |
25 March 2022 |
36 months |
3 months |
None |
|
|
Wol Kolade Vice Chair |
25 March 2022 |
24 months |
3 months |
None |
Waived entitlement to remuneration |
|
Professor Lord Ara Darzi Non-Executive Director |
1 April 2020 |
0 months |
3 months |
None |
Left NHS England on 30 June 2022 |
|
Jeremy Townsend Non-Executive Director Chair of ARAC |
1 October 2020 |
42 months |
3 months |
None |
Returned from temporary transfer to NHS Improvement on 1 July 2022 |
|
Laura Wade-Gery Non-Executive Director |
6 November 2020 |
4 months |
3 months |
None |
Left on 30 June 2023 |
|
Rakesh Kapoor Non-Executive Director |
1 January 2021 |
9 months |
3 months |
None |
Returned from temporary transfer to NHS Improvement on 1 April 2022 |
|
Susan Kilsby Non-Executive Director |
1 January 2021 |
9 months |
3 months |
None |
|
|
Michael Coupe Non-Executive Director |
1 January 2021 |
45 months |
3 months |
None |
|
|
Professor Sir Munir Pirmohamed Non-Executive Director |
1 July 2022 |
9 months |
3 months |
None |
|
|
Sir Andrew Morris Non-Executive Director |
1 July 2022 |
24 months |
3 months |
None |
|
|
Sir David Behan Non-Executive Director |
1 September 2022 |
17 months |
3 months |
None |
Chair of Health Education England |
|
Baroness Mary Watkins Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
|
Professor Sir Simon Wessely Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
|
Sir Mark Walport Non-Executive Director |
27 January 2023 |
34 months |
3 months |
None |
|
Non-executive director remuneration (including salary entitlements)
Salaries and allowances 2022/23 (subject to audit)
|
Name of non-executive director |
(a) Salary (bands of £5,000) |
(b) Benefits in |
(c) Performance |
(d) Long-term performance |
(e) Pension-related benefits to |
(f) |
|
Richard Meddings CBE[84] |
60-65 |
0 |
0 |
0 |
N/A |
60-65 |
|
Wol Kolade[85] |
0 |
0 |
0 |
0 |
N/A |
0 |
|
Professor Lord Ara Darzi[86] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Jeremy Townsend[87] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Laura Wade-Gery |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Rakesh Kapoor |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Susan Kilsby |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Michael Coupe |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Professor Sir Munir Pirmohamed[88] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir Andrew Morris[89] |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Sir David Behan[90] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Baroness Mary Watkins[91] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Professor Sir Simon Wessely[92] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
Sir Mark Walport[93] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
Salaries and allowances 2021/22 (subject to audit)
|
Name of non-executive director |
(a) Salary (bands of £5,000) |
(b) Benefits in |
(c) Performance |
(d) Long-term performance |
(e) Pension-related benefits to |
(f) |
|
Lord David Prior[95] |
60-65 |
0 |
0 |
0 |
N/A |
60-65 |
|
Richard Meddings CBE[96] |
0-5 |
0 |
0 |
0 |
N/A |
0-5 |
|
David Roberts CBE[97] |
0 |
0 |
0 |
0 |
N/A |
0 |
|
Wol Kolade[98] |
0 |
0 |
0 |
0 |
N/A |
0 |
|
Professor Lord Ara Darzi |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Jeremy Townsend |
10-15 |
0 |
0 |
0 |
N/A |
10-15 |
|
Laura Wade-Gery |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Rakesh Kapoor |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Susan Kilsby |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
|
Michael Coupe |
5-10 |
0 |
0 |
0 |
N/A |
5-10 |
Parliamentary accountability and audit report
All elements of this report are subject to audit.
Remote contingent liabilities
There were no remote contingent liabilities.
Notation of gifts over £300,000
NHS England made no political or charitable donations of gifts during the 2022/23 financial year.
Regularity of expenditure: Losses and special payments
Losses and special payments are items that Parliament would not have contemplated when it agreed funds for the NHS or passed legislation. By their nature they are items that ideally should not arise and are therefore subject to special control procedures compared to the generality of payments. They are divided into different categories, which govern the way that individual cases are handled.
Details of any losses and special payments relating to CCGs and ICBs can be found within individual CCGs and ICBs annual reports which are published on ICB websites. A list of CCGs and ICBs, along with links to their websites, can be found on the NHS England website.
Losses
The total number of NHS England losses cases, and their total value, was as follows:
|
|
Parent |
Consolidated group | ||||||
|
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases | |
|
Administrative write-offs |
– |
– |
41 |
82 |
131 |
580 |
555 |
2,875 |
|
Fruitless payments |
214 |
192 |
188 |
24,206 |
232 |
2,472 |
195 |
26,373 |
|
Stores losses |
25,060 |
1,098 |
– |
– |
303,711 |
2,322 |
3 |
4 |
|
Bookkeeping losses |
62 |
17 |
43 |
21 |
72 |
58 |
44 |
23 |
|
Constructive loss |
7 |
5,902 |
1 |
383 |
7 |
5,902 |
2 |
384 |
|
Cash losses |
11 |
1,647 |
22 |
22,033 |
17 |
1,685 |
28 |
22,065 |
|
Claims abandoned |
361 |
3,000 |
2 |
395 |
364 |
3,011 |
96 |
4,746 |
|
Total |
25,715 |
11,856 |
297 |
47,120 |
304,534 |
16,030 |
923 |
56,470 |
2022/23 Disclosure: Fruitless payments
£0.6 million. NHS Gloucestershire ICB have agreed and paid a legal settlement agreement granted by the court in financial year 2022/23. The ICB settled a court order agreement in breach of the Public Contracts Regulations 2015 in their award of the contract for advice and guidance services in 2022/23.
£0.9 million. NHS Bath and North East Somerset, Swindon and Wiltshire ICB have agreed and paid a legal settlement agreement granted by the court in financial year 2022/23. The ICB settled a court order agreement in breach of the Public Contracts Regulations 2015 in their award of the contract for advice and guidance services in 2022/23.
2022/23 Disclosure: Store losses
£1.10 million. This case relates to various stock items that cannot be utilised in healthcare facilities as the stock has reached the manufacturers expiry date and therefore requires writing off.
2022/23 Disclosure: Constructive losses
£1.102 million. This case relates to six vaporisers which support the provision of oxygen to patients. The vaporisers were purchased in March 2020 by NHS England for the London Nightingale Hospital at the ExCeL. Following decommissioning of the facility, the vaporisers were placed into storage to be available if ever required. As many hospital facilities have since been upgraded, these vaporisers are too big to be used in any other existing facility and are therefore excess to requirements.
£4.80 million. This case relates to stock that was procured as part of the Vaccine Deployment Programme in response to the COVID-19 pandemic. The stock was procured in extreme urgency and considerable uncertainty in supply chains and demand. The stock is now deemed as surplus to requirement and retaining the stock in storage will not equate to value for money when compared to the running cost of storage.
2022/23 Disclosure: Cash losses
Total cash losses for 2022/2023 amount to £1.6 million. £1.3 million of this total relates to the overpayment of suspension payments made to 10 medical practitioners. As per the reporting requirement, the overpaid suspension payments that exceed £300k are disclosed below:
£421k. This loss relates to the overpayment of suspension payments to a medical practitioner between March 2020 and June 2022 equating to a sum of £420,588. The overpayment is due to the medical practitioners qualifying entitlement ceasing, meaning that they would not have been eligible for the suspension payment as per the Secretary of States Payment Determination Guidance.
£305k. This loss relates to the overpayment of suspension payments to a medical practitioner between May 2019 and March 2022 equating to a sum of £305,000. The overpayment is due to the medical practitioners qualifying entitlement ceasing, meaning that they would not have been eligible for the suspension payment as per the Secretary of States Payment Determination Guidance.
£378k. This loss relates to the overpayment of suspension payments to a medical practitioner between June 2018 and October 2023 equating to a sum of £377,590. The overpayment is as a result of the medical practitioner continuing to receive payment at a rate higher than that which they were eligible as per the Secretary of States Payment Determination Guidance, following the cessation of one of their qualifying relationships.
£311k. The remaining cash loss relates to non-delivery of contractual dental units of activity as part of the General Dental Service. The registered performer failed to deliver the contractual agreed units of Dental and orthodontic activities for the financial years 2016 to 2022. In addition, as part of the new procedure requirements issued by NHS England during the pandemic, the registered performer did not comply with new contractual obligations to provide urgent face to face dental care. The sum being reported represents the totality of payments made where there has been no benefit to NHS England or patients.
2022/23 Disclosure: Claims abandoned
£2.83 million. This case relates to the request to write off a grant awarded to the sum of £1,749,500 and the subsequent capital gain on the property equating to £1,080,000. The funded asset was utilised for the provision of mental health care within Trust grounds by a charitable organisation. A decision was taken to dispose the funded asset to the Trust as part of a modernisation programme for mental health inpatient facilities. The capital grant agreement included a legal charge in favour of the Secretary of State for the receipts in the event that the applicant disposes the funded asset. NHS England is the successor of Health Authorities and PCTs for the purposes of this capital grant agreement.
2021/22 Disclosure: Fruitless payments
£2.1 million. This case relates to a procurement challenge as a result of a breach of Procurement Contract regulations 2015. The breach is in relation to NHS England’s incorrect application of a framework agreement which has resulted in a claim for damages for loss of a chance to provide services and legal costs incurred. The case was settled in favour of the claimant and is therefore reported to reflect the court outcome.
£17.8 million. This cost relates to a contractual amount to be paid by NHS England to exit a long-term contract for a university medical school where no future value to the entity is expected. The total represents the sum to be paid from 2023 to 2029. The cost represents a stream of funding for medical schools funding which began in 1988 when it was provided by the Regional Health Authority as part of a national policy to fund clinical academic posts. The funding and governance have passed through numerous organisations and oversight committees across the period as the NHS evolved through regular structural changes. The accrual of £17.8 million is representative of an unpaid discounted future cost that is payable to the universities, however, any final settlement will need to be approved by Treasury.
£6.2 million. This sum represents a payment to be made by NHS England to HMRC for back taxes, national insurance and related interest for the historical treatment of a cohort of clinical workers who have been paid in an off-payroll capacity. The workers should have been paid as “employed” for tax purposes. This sum is in the process of being settled by NHS England.
2021/2022 Disclosure: Constructive losses
£0.3 million included in the parent figure for NHS England relates to provision of enemas to support the Bowel Scope Screening programme. The manufacturer of the enema products decided to cease manufacturing the enema product as it was not one of their main areas of business. It was agreed to bulk order 2 years’ worth of the enema product to give time for either another product to be sourced or a decision to be made on the future of the Bowel Scope programme in light of the bowel screening age extension. Due to the bulk order in 2019, there was a large element of unused enema products that were out of date and not required due to the impact of COVID-19 on activity and decommissioning of the bowel scope service.
2021/22 Disclosure: Cash losses
£4.2 million. This relates to the review of the GP Contract Vaccinations and Immunisations (V&I) programmes within NHS England. The outcome of the review confirmed that some contractors could not meet the vaccination targets that were set in relation to routine childhood vaccination and immunisation, therefore, resulted in an overpayment. The V&I repayment mechanism is intended to limit financial gain by practices with lower levels of performance.
Having reviewed a large volume of commissioner and practice queries, it became apparent that practices were struggling to meet the performance threshold. The main reasons for this are issues outside of a practice’s control, such as increased vaccine hesitancy, people either not coming forward when invited or declining, less ability to opportunistically offer vaccination when children are present in practice for another reason, and the impacts of the COVID-19 pandemic on practice capacity.
£15.7 million relates to pharmacy cash advances paid by NHS England. At the start of the COVID-19 pandemic, community pharmacies faced significant and unexpected cash flow pressures. These were caused by several issues, including a sharp increase in prescription items in March and April 2020, higher drug prices, delayed payments for the Pharmacy Quality Scheme and extra COVID-19 related costs. It was agreed to provide an urgent uplift to the normal advance payments to support pharmacies with their cash flow pressures and to help them stay open to continue to provide vital NHS pharmaceutical services. The cash advances were made on the basis that payments would be recovered from pharmacies in 2020/21, however, a significant number of pharmacy contractors closed down between April 2020 and March 2022 making recovery of the advanced sum not feasible.
£964,000. This relates to 2 suspended GPs within NHS England that had salary overpayments, 1 due to be being ineligible for suspension payments and 1 due to being paid more than they were entitled to. Recovery of £473,000 of the £964,000 is being pursued as part of an ongoing criminal investigation, the remainder is not able to be recovered due to legal advice that estoppel would be applicable. New management processes with regard to suspension payments helped to identify these payments. These new processes have improved controls and are intended to prevent recurrence of such cases. Actions such as a new payment mechanism and authorisation procedures have been implemented along with training on application of the suspension payment rules.
£1 million relates to overpayment made on a contract with an independent sector service provider in response to the COVID-19 pandemic. NHS England has reached an agreement to recover the full amount in due course. Having made this agreement, the service provider made a repayment of £82.5k and went into administration by October 2022. Measures have been implemented within NHS England to prevent recurrence of such cases.
2021/22 Disclosure: Claims abandoned
£0.3 million relates to Dentaris (a dental provider) who went into liquidation on 21 April 2020. The provider owed money relating to 2017/18 and 2018/19 underperformance of activity on the contract. The company was dissolved at Companies House on 21 April 2021, and no creditor will receive any dividend in respect of monies owed from Dentaris. The practice closed without prior notification to NHS England. Until the closure, the practice and NHS England had agreed a repayment plan, for the moneys owing, which had been agreed to support the practice to remain open and therefore supportive of patients continuing to receive care.
Special payments
The total number of NHS England special payments cases, and their total value, was as follows:
|
|
Parent |
Consolidated group | ||||||
|
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases |
Total number of cases |
Total value of cases | |
|
Compensation payments |
7 |
159 |
1,008 |
311 |
15 |
199 |
1,013 |
353 |
|
Compensation payments Treasury approved |
– |
– |
– |
– |
– |
– |
1 |
32 |
|
Extra contractual payments |
1 |
80 |
|
|
2 |
190 |
1 |
1 |
|
Ex gratia payments |
6 |
30 |
475 |
314 |
18 |
87 |
488 |
409 |
|
Ex gratia payments Treasury approved |
– |
– |
– |
– |
19 |
55 |
1 |
18 |
|
Extra statutory extra regulatory payments |
– |
– |
– |
– |
– |
– |
– |
– |
|
Special severance payments Treasury approved |
– |
– |
– |
– |
– |
– |
1 |
57 |
|
Special severance payments |
– |
– |
1 |
5 |
2 |
50 |
6 |
167 |
|
Total |
14 |
269 |
1,484 |
630 |
56 |
581 |
1,511 |
1,037 |
All cases classified as special severance payments are subject to HM Treasury approval.
2022/23 Special severance payments
During 2022/23 SCCL paid two special severance payments for £30,000 and £20,000 respectively. The payment of £30,000 relates to a non-contractual amount to terminate employment and the payment of £20,000 relates to a non-contractual payment in relation to a dispute settlement. These payments were not approved by NHS England and are therefore irregular.
2021/22 Disclosure: Ex gratia payment
During the year 3 CSUs paid ex gratia payments to current and former employees in relation to monies received from NHS Fleet Solutions relating to refunds of VAT obtained as a result of the decision in the Northumbria Healthcare NHS Foundation Trust v HMRC on salary sacrifice lease cars of £314,000.
2021/22 Special severance payments
There was 1 Treasury approved special severance payments as follows:
NHS Surrey Heartlands CCG
During 2021/22, the CCG has paid 1 special severance payments recorded in their accounts for £56,416.75. The CCG sought approval from NHS England and HM Treasury prior to agreement and payment and approval was granted.
There were 6 special severance payments that do not have HMT approval, as follows:
NHS North of England CSU: During 2021/22, the CSU has paid 1 special severance payment in the parent account for £5,256. It relates to a non-contractual payment in lieu of notice (PILON) payment made to the individual. This payment was not approved by NHS England and is therefore irregular.
NHS Kernow CCG: During 2021/22, the CCG has paid 3 special severance payments recorded in their accounts for £22,751, £24,497 and £28,800 respectively. They relate to non-contractual PILON payments made to the individuals. This payment should have been submitted to NHS England and HMT for review and approval prior to being paid. This approval was not in place prior to making the payment. The CCG sought retrospective approval, but this was not granted and therefore the payments are considered irregular.
NHS North East Essex CCG, NHS Ipswich and East Suffolk CCG and NHS West Suffolk CCG: The 3 CCGs recorded a special severance payment in their accounts totalling £81,000 in June 2022, under a settlement agreement with a former senior employee. This payment should have been submitted to NHS England for review and approval prior to being paid. The CCG sought retrospective approval from NHS England which was granted. However, HM Treasury did not approve the payment and, as this was not granted, the payment is irregular.
NHS Bristol, North Somerset and South Gloucestershire CCG: During 2021/22, a non-contractual special severance payment of £5,389 was made by the CCG. This required approval from NHS England and the CCG has sought retrospective approval.
The payments noted above are also included in the Exit Packages disclosures.
Cost allocation and setting of charges
NHS England certifies that it has complied with the HM Treasury guidance on cost allocation and the setting of charges. The following table provides details of income generation activities whose full cost exceeded £1 million or was otherwise material:
|
2022/23 |
Note |
Parent |
Consolidated group | ||||
|
Income £000 |
Full cost £000 |
Surplus/ (deficit) £000 |
Income £000 |
Full cost £000 |
Surplus/ (deficit) £000 | ||
|
Dental |
2 & 4 |
631,415 |
(2,593,407) |
(1,961,992) |
746,642 |
(3,023,228) |
(2,276,586) |
|
Prescription |
2 & 4 |
519,753 |
(1,728,499) |
(1,208,746) |
670,324 |
(11,904,187) |
(11,233,863) |
|
Total fees and charges |
|
1,151,168 |
(4,321,906) |
(3,170,738) |
1,416,966 |
(14,927,415) |
(13,510,449) |
|
2021/22 |
Note |
Parent |
Consolidated group | ||||
|
Income £000 |
Full cost £000 |
Surplus/ (deficit) £000 |
Income £000 |
Full cost £000 |
Surplus/ (deficit) £000 | ||
|
Dental |
2 & 4 |
633,809 |
(3,099,805) |
(2,465,996) |
633,847 |
(3,099,805) |
(2,465,958) |
|
Prescription |
2 & 4 |
641,033 |
(2,351,608) |
(1,710,575) |
651,964 |
(11,430,430) |
(10,778,466) |
|
Total fees and charges |
1,274,842 |
(5,451,413) |
(4,176,571) |
1,285,811 |
(14,530,235) |
(13,244,424) | |
The fees and charges information in this note is provided in accordance with section 3.2.12 of the Government Financial Reporting Manual. It is provided for fees and charges purposes and not for International Financial Reporting Standards (IFRS) 8 purposes.
The financial objective of prescription and dental charges is to collect charges only from those patients that are eligible to pay.
Prescription charges[99] are a contribution to the cost of pharmaceutical services including the supply of drugs. In 2022/23, the NHS prescription charge for each medicine or appliance dispensed was £9.35. However, around 90% of prescription items[100] are dispensed free each year where patients are exempt from charges. In addition, patients who were eligible to pay charges could purchase pre-payment certificates at £30.25 for 3 months or £108.10 for a year. A number of other charges were payable for wigs and fabric supports.
Those who are not eligible for exemption are required to pay NHS dental charges[101] which fall into 3 bands depending on the level and complexity of care provided. In 2022/23, the charge for Band 1 treatments was £23.80, for Band 2 was £65.20 and for Band 3 was £282.80. Dental patient charges have not changed since 14 December 2020.
Accountability to Parliament and the Public
During 2022/23, NHS England has continued to work closely with the National Audit Office in their work to test whether public bodies are delivering value for money. During this period, the Chief Executive and other senior leaders gave evidence to Public Accounts Committee hearings on ‘Managing NHS backlogs and waiting times’ and ‘Introducing Integrated Care Systems’ and the NAO published reports on Introducing Integrated Care Systems[102], Managing NHS backlogs and waiting times in England[103], Progress in improving mental health services in England[104] and Alcohol Treatment Services.[105]
In response to the Public Accounts Committee’s recommendations, NHS England has:
- Continued to offer targeted support to the providers with the greatest performance challenges, including weekly or fortnightly oversight meetings, on-site diagnostic visits from the Intensive Support Team and national support to improve, which between July 2022 and July 2023 delivered a greater reduction in patients waiting over 78 weeks than in better performing providers; (Letter from Amanda to Public Accounts Committee Chair on Backlogs and Waiting times).[106]
- Investing in a Federated Data Platform, which by linking data will help Integrated Care Systems to better coordinate care across health and social care providers; and
- Supported Integrated Care Systems to accelerate and embed adoption of population health management across systems and places through the Population Health Management Academy, supporting the development of effective place-based partnerships. (both of the latter two from a letter from Sir Chris to PAC Chair on Implementing ICSs).[107]
The certificate of the Comptroller and Auditor General to the Houses of Parliament
Opinion on financial statements
I certify that I have audited the financial statements of NHS England and its group for the year ended 31 March 2023 under the National Health Service Act 2006 and the Health and Social Care Act 2012.
The financial statements comprise NHS England and its group’s:
- Statement of Financial Position as at 31 March 2023;
- Statement of Comprehensive Net Expenditure, Statement of Cash Flows and Statement of Changes in Taxpayers’ Equity for the year then ended; and
- the related notes including the significant accounting policies.
The financial reporting framework that has been applied in the preparation of the group financial statements is applicable law and UK adopted International Accounting Standards.
In my opinion, the financial statements:
- give a true and fair view of the state of NHS England and its group’s affairs as at 31 March 2023 and their total net expenditure for the year then ended; and
- have been properly prepared in accordance with the National Health Service Act 2006 and the Health and Social Care Act 2012 and Secretary of State directions issued thereunder.
Qualified opinion on regularity
In my opinion, except for the effects of the matters described in the Basis for qualified opinion on regularity section below, in all material respects, the income and expenditure recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
Basis for qualified opinion on regularity
I have qualified my opinion on regularity because of ineligible payments made to suspended medical practitioners, where the transactions do not conform to the relevant statutory regulations specifying entitlement to such payments. The expenditure is therefore irregular.
12 suspended medical practitioners received suspension payments of £1,335,626 during the financial years 2017-18 to 2022-23 (of which £156,429 relating to eight suspended medical practitioners was paid in 2022-23) to which they were not entitled. Such payments were not made in accordance with statutory regulations governing entitlement to suspension payments to suspended medical practitioners and therefore, in my opinion, the payments are irregular. I also do not have assurance over the completeness of the population of irregular suspension payments disclosed.
In respect of these payments, I consider that insufficient regard has been paid to the framework of authorities and use of public funds. These payments are therefore material by virtue of their nature. Further detail can be found in my report.
Basis for opinions
I conducted my audit in accordance with International Standards on Auditing (UK) (ISAs UK), applicable law and Practice Note 10 Audit of Financial Statements and Regularity of Public Sector Bodies in the United Kingdom (2022). My responsibilities under those standards are further described in the Auditor’s responsibilities for the audit of the financial statements section of my certificate.
Those standards require me and my staff to comply with the Financial Reporting Council’s Revised Ethical Standard 2019. I am independent of NHS England and its group in accordance with the ethical requirements that are relevant to my audit of the financial statements in the UK. My staff and I have fulfilled our other ethical responsibilities in accordance with these requirements.
I believe that the audit evidence I have obtained is sufficient and appropriate to provide a basis for my opinion.
Conclusions relating to going concern
In auditing the financial statements, I have concluded that NHS England and its group’s use of the going concern basis of accounting in the preparation of the financial statements is appropriate.
Based on the work I have performed, I have not identified any material uncertainties relating to events or conditions that, individually or collectively, may cast significant doubt on NHS England and its group’s ability to continue as a going concern for a period of at least twelve months from when the financial statements are authorised for issue.
My responsibilities and the responsibilities of the Board and the Accounting Officer with respect to going concern are described in the relevant sections of this certificate.
The going concern basis of accounting for NHS England and its group is adopted in consideration of the requirements set out in HM Treasury’s Government Financial Reporting Manual, which require entities to adopt the going concern basis of accounting in the preparation of the financial statements where it is anticipated that the services which they provide will continue into the future.
Other information
The other information comprises the information included in the Annual Report but does not include the financial statements nor my auditor’s certificate and report. The Board and Accounting Officer is responsible for the other information.
My opinion on the financial statements does not cover the other information and, except to the extent otherwise explicitly stated in my certificate, I do not express any form of assurance conclusion thereon.
My responsibility is to read the other information and, in doing so, consider whether the other information is materially inconsistent with the financial statements, or my knowledge obtained in the audit, or otherwise appears to be materially misstated.
If I identify such material inconsistencies or apparent material misstatements, I am required to determine whether this gives rise to a material misstatement in the financial statements themselves. If, based on the work I have performed, I conclude that there is a material misstatement of this other information, I am required to report that fact.
I have nothing to report in this regard.
Opinion on other matters
In my opinion the part of the Remuneration and Staff Report to be audited has been properly prepared in accordance with Secretary of State directions issued under the National Health Service Act 2006 and the Health and Social Care Act 2012.
In my opinion, based on the work undertaken in the course of the audit:
- the parts of the Accountability Report subject to audit have been properly prepared in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012; and
- the information given in the Performance and Accountability Reports for the financial year for which the financial statements are prepared is consistent with the financial statements and is in accordance with the applicable legal requirements.
Matters on which I report by exception
In the light of the knowledge and understanding of NHS England and its group, and its environment obtained in the course of the audit, I have not identified material misstatements in the Performance and Accountability Reports.
I have nothing to report in respect of the following matters which I report to you if, in my opinion:
- adequate accounting records have not been kept by NHS England and its group or returns adequate for my audit have not been received from branches not visited by my staff; or
- I have not received all of the information and explanations I require for my audit; or
- the financial statements and the parts of the Accountability Report subject to audit are not in agreement with the accounting records and returns; or
- certain disclosures of remuneration specified by HM Treasury’s Government Financial Reporting Manual have not been made or parts of the Remuneration and Staff Report to be audited is not in agreement with the accounting records and returns; or
- the Governance Statement does not reflect compliance with HM Treasury’s guidance.
Responsibilities of the Board and Accounting Officer for the financial statements
As explained more fully in the Statement of Accounting Officer’s Responsibilities, the board and Accounting Officer are responsible for:
- maintaining proper accounting records;
- providing the C&AG with access to all information of which management is aware that is relevant to the preparation of the financial statements such as records, documentation and other matters;
- providing the C&AG with additional information and explanations needed for his audit;
- providing the C&AG with unrestricted access to persons within NHS England and its group from whom the auditor determines it necessary to obtain audit evidence;
- ensuring such internal controls are in place as deemed necessary to enable the preparation of financial statement to be free from material misstatement, whether due to fraud or error;
- ensuring that the financial statements give a true and fair view and are prepared in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012;
- ensuring that the annual report, which includes the Remuneration and Staff Report, is prepared in accordance with Secretary of State directions made under the National Health Service Act 2006 and the Health and Social Care Act 2012; and
- assessing NHS England and its Group’s ability to continue as a going concern, disclosing, as applicable, matters related to going concern and using the going concern basis of accounting unless the Accounting Officer anticipates that the services provided by NHS England and its group will not continue to be provided in the future.
Auditor’s responsibilities for the audit of the financial statements
My responsibility is to audit, certify and report on the financial statements in accordance with the National Health Service Act 2006 and the Health and Social Care Act 2012.
My objectives are to obtain reasonable assurance about whether the financial statements as a whole are free from material misstatement, whether due to fraud or error, and to issue a certificate that includes my opinion. Reasonable assurance is a high level of assurance but is not a guarantee that an audit conducted in accordance with ISAs (UK) will always detect a material misstatement when it exists. Misstatements can arise from fraud or error and are considered material if, individually or in the aggregate, they could reasonably be expected to influence the economic decisions of users taken on the basis of these financial statements.
Extent to which the audit was considered capable of detecting non-compliance with laws and regulations including fraud
I design procedures in line with my responsibilities, outlined above, to detect material misstatements in respect of non-compliance with laws and regulations, including fraud. The extent to which my procedures are capable of detecting non-compliance with laws and regulations, including fraud is detailed below.
Identifying and assessing potential risks related to non-compliance with laws and regulations, including fraud
In identifying and assessing risks of material misstatement in respect of non-compliance with laws and regulations, including fraud, I:
- considered the nature of the sector, control environment and operational performance including the design of NHS England and its group’s accounting policies, key performance indicators and performance incentives.
- inquired of management, NHS England’s head of internal audit and those charged with governance, including obtaining and reviewing supporting documentation relating to NHS England and its group’s policies and procedures on:
- identifying, evaluating and complying with laws and regulations;
- detecting and responding to the risks of fraud; and
- the internal controls established to mitigate risks related to fraud or non-compliance with laws and regulations including NHS England and its group’s controls relating to NHS England’s compliance with the National Health Service Act 2006 and the Health and Social Care Act 2012 and Managing Public Money.
- inquired of management, NHS England’s head of internal audit and those charged with governance whether:
- they were aware of any instances of non-compliance with laws and regulations; and
- they had knowledge of any actual, suspected, or alleged fraud;
- discussed with the engagement team regarding how and where fraud might occur in the financial statements and any potential indicators of fraud.
As a result of these procedures, I considered the opportunities and incentives that may exist within NHS England and its group for fraud and identified the greatest potential for fraud in the following areas: revenue recognition, posting of unusual journals, complex transactions, and bias in management estimates. In common with all audits under ISAs (UK), I am also required to perform specific procedures to respond to the risk of management override.
I obtained an understanding of NHS England and its group’s framework of authority and other legal and regulatory frameworks in which NHS England and its group operate. I focused on those laws and regulations that had a direct effect on material amounts and disclosures in the financial statements or that had a fundamental effect on the operations of NHS England and its group. The key laws and regulations I considered in this context included the National Health Service Act 2006, Health and Social Care Act 2012, Health and Care Act 2022, Managing Public Money, employment law, or tax legislation, relevant legislation relating to fees charged by the NHS England, and regulations relating to suspension payments to suspended medical practitioners.
In addition, I considered regulations and regularity relating to exit packages and, in particular, special severance payments, as I identified the completeness and regularity of exits packages as a significant risk.
Audit response to identified risk
To respond to the identified risks resulting from the above procedures:
- I reviewed the financial statement disclosures and testing to supporting documentation to assess compliance with provisions of relevant laws and regulations described above as having direct effect on the financial statements;
- I enquired of management, the Audit and Risk Assurance Committee and in-house legal counsel concerning actual and potential litigation and claims;
- I reviewed minutes of meetings of those charged with governance and the board and internal audit reports;
- in addressing the risk of fraud through management override of controls, I tested the appropriateness of journal entries and other adjustments; assessed whether the judgements on estimates are indicative of a potential bias; and evaluated the business rationale of any significant transactions that are unusual or outside the normal course of business; and
- substantive testing of exit packages disclosed within the NHS England’s Remuneration and Staff Report and review of all special severance payments included in the NHS England’s group Remuneration and Staff Report.
I communicated relevant identified laws and regulations and potential risks of fraud to all engagement team members and remained alert to any indications of fraud or non-compliance with laws and regulations throughout the audit.
A further description of my responsibilities for the audit of the financial statements is located on the Financial Reporting Council’s website at: www.frc.org.uk/auditorsresponsibilities.
This description forms part of my certificate.
Other auditor’s responsibilities
I am required to obtain evidence sufficient to give reasonable assurance that the expenditure and income recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
I communicate with those charged with governance regarding, among other matters, the planned scope and timing of the audit and significant audit findings, including any significant deficiencies in internal control I identify during my audit.
Gareth Davies, Comptroller and Auditor General
National Audit Office, 157-197 Buckingham Palace Road, Victoria, London SW1W 9SP
22 January 2024
The report of the Comptroller and Auditor General to the Houses of Parliament
Introduction
- The National Health Service Act 2006 and the Health and Social Care Act 2012 requires NHS England to prepare consolidated annual accounts for each financial year. The consolidated accounts must contain NHS England’s annual accounts and a consolidation of NHS England’s annual accounts, the annual accounts of each Clinical Commissioning Group (CCG), Integrated Care Board (ICB) and the accounts of the Supply Chain Coordination Limited (SCCL).165F[108] NHS England’s consolidated accounts are in turn consolidated in the accounts of the Department of Health and Social Care (DHSC). I consider NHS England to be a significant component of DHSC and my audit of NHS England must be complete before I complete my audit of DHSC.
- I am required to examine, certify, and report on NHS England’s consolidated accounts. I provide an opinion on whether the consolidated accounts give a “true and fair” view of NHS England’s finances for the year. I also provide an opinion on whether the transactions recorded in NHS England’s consolidated accounts have been applied to the purposes intended by Parliament and whether they conform to the authorities which govern them (“regularity”).
- In this report, I explain why I have qualified my regularity opinion on NHS England’s 2022-23 consolidated accounts, with regards to ineligible suspension payments made to suspended medical practitioners.166F[109] I also set out my observations on the performance of CCGs and ICBs (“Commissioners”) in delivering accounts to support the timely production of NHS England’s consolidated accounts.
- This is the second consecutive year I have qualified my regularity opinion on NHS England’s consolidated accounts for ineligible suspension payments to suspended medical practitioners. Details of the prior year qualification are provided in the NHS England annual report and accounts 2021-22.[110]
Qualification of regularity opinion due to irregular suspension payments to suspended medical practitioners
- Under certain qualifying circumstances NHS England can make suspension payments to medical practitioners who have been suspended as set out in relevant statutory regulations. Under statutory regulations issued by the Secretary of State for Health and Social Care, NHS England may suspend a medical practitioner, when satisfied that it is necessary to do so for the protection of patients or members of the public or that it is otherwise in the public interest. A suspended medical practitioner may be entitled to receive suspension payments if the medical practitioner meets certain qualifying conditions. If the medical practitioner qualifies for suspension payments, such payments may continue until a relevant tribunal has considered the suspension and either ends the suspension or removes the medical practitioner from the medical register. For example, the General Medical Council (GMC) maintains a medical register of doctors licensed to practice medicine. The GMC considers suspensions concerning doctors. The General Dental Council and General Optical Council perform a similar role for dentists and opticians, respectively.
- In 2022/23 it was identified, by NHS England and my staff, that 12 medical practitioners had received ineligible suspension payments over the 2017/18 to 2022/23 financial years. As NHS England has set out in its governance statement, during 2022-23, 12 medical practitioners were identified in 2022-23 as having received ineligible suspension payments over the 2017-18 to 2022-23 financial years. Total payments to these 12 medical practitioners over the 2017-18 to 2022-23 financial years was £1,335,626. Of this £156,429 was paid in 2022-23 to eight medical practitioners. These cases are in addition to the two medical practitioners, who received ineligible suspension payments over the 2017-18 to 2021-22 financial years, which led me to qualify my regularity opinion in 2021-22.
- NHS England failed to establish a system of control to ensure suspension payments were only paid to medical practitioners who met the qualifying criteria and that these suspension payments were stopped promptly once the qualifying period ended. There were various reasons the 12 medical practitioners were paid ineligible suspension payments. In most cases NHS England continued making suspension payments to GPs after they had resigned their partnership in a GP practice. The regulations are clear that suspension payments should cease when the medical practitioner’s employment is terminated, which includes a GP resigning from a GP partnership. In most of these cases the GPs had informed NHS England that they had resigned their partnership, but NHS England continued to make the suspension payments; in one case for over four years, after being notified. Other ineligible suspension payments happened because NHS England had erroneously interpretated the regulations and made payments when the medical practitioner did not qualify for suspension payments.
- I have qualified my regularity opinion in relation to these ineligible suspension payments. As the suspension payments I refer to in paragraph 6 were made contrary to the statutory regulations governing such payments, I consider them to be irregular. The circumstances that led to these irregular payments being made are such that I consider that insufficient regard has been paid to the framework of authorities and use of public funds and that the payments are therefore material by virtue of their nature. Additionally, suspension of a medical practitioner often involves serious misconduct and I consider payment of ineligible suspension payments in those circumstances to be contentious. NHS England should have had checks in place to prevent or detect such payments. I have therefore qualified my regularity opinion on the consolidated accounts.
- NHS England has not recovered most of the ineligible suspension payments it made. Ineligible suspension payments made to two of the 12 medical practitioners have been recovered in full by NHS England. These recoveries amount to £32,747. The remaining £1,302,879 has not been recovered. NHS England is taking legal advice regarding recovery.
Audit completion delays of NHS England group entities
- NHS England group entities are audited by a number of different audit firms. Commissioners are free to appoint their external auditors (“local auditors”). Local auditors must comply with the Code of Audit Practice (“the Code”).[111] Under the Local Audit and Accountability Act 2014, I am responsible for the preparation, publication, and maintenance of the Code. The Code sets out what local auditors are required to do to fulfil their statutory responsibilities under the Local Audit and Accountability Act 2014. For 2022-23 the commissioner audits were undertaken by six audit firms.
- The Code stresses the need for local auditors to report on a timely basis. Section 1.19 of the Code requires local auditors to report on a timely basis. Timely reporting includes producing audit reports in time, insofar as the auditor can do so under auditing standards, to allow local bodies to comply with the requirements placed on them to publish their audited financial statements. It also means ensuring that when matters of concern arise during the audit, the auditor raises them promptly with the body and considers whether the matter needs to be brought to public attention at the appropriate time.
- The timetable set by NHS England and DHSC for the 2022-23 group accounts required Commissioners to have their statutory audits complete by 30 June 2023.[112] The statutory deadline, under the Government Resources and Accounts Act 2000, requires government departments to lay their annual reports and accounts in Parliament by 31 January, ten months after the financial year end. Although NHS England does not have a statutory deadline for laying its annual report and accounts in Parliament, as NHS England is a significant component of the DHSC group, the accounts of NHS England must be completed to the same timetable as DHSC.
- DHSC committed to laying its 2022-23 annual report and accounts before the end of 2023. At a Public Accounts Committee hearing[113] on 20 March 2023, regarding the timeliness of the DHSC annual report and accounts 2021-22, DHSC committed to aiming to lay its 2022-23 accounts before the 2023 Parliamentary Christmas recess and then to gradually improve the timeliness in future years. DHSC’s stated aim was to bring forward the laying date by two months each year to eventually enable laying before the Parliamentary summer recess. Before the Covid-19 pandemic, DHSC and NHS England routinely laid their annual reports and accounts in Parliament before the Parliamentary summer recess. The last time this happened was for the 2018-19 annual report and accounts. For the 2022-23 accounts, NHS England, DHSC and my staff agreed a target date of 30 November 2023 for audit certification, to enable laying before the 2023 Parliamentary Christmas recess.
- Delays in the enactment of the Health and Care Act 2022 increased the complexity of the NHS England group for 2022-23. NHS England is a large group account which consolidates the local commissioning bodies in England. In 2022-23 the Health and Care Act 2022 abolished the 106 CCGs and replaced them with 42 ICBs. It was originally planned that CCGs would be abolished on 31 March 2022 and replaced by ICBs on 1 April 2022. However, delays in the enactment of the Health and Care Act 2022 meant the abolition of CCGs was delayed by three months. This delay complicated the NHS England group structure for 2022-23, resulting in 149 group entities (106 CCGs producing three month accounts, 42 ICBs producing nine month accounts, and SCCL. If ICBs had been established on 1 April 2022, only 43 group entities would have been required to produce audited accounts.
- Of the 148 Commissioner 2022-23 annual report and accounts, 117 were audited by 30 June 2023. 117 Commissioner audits were completed by 30 June 2023, meaning just under four fifths of bodies achieved the target date set by NHS England. By 31 July 2023, 131 (88.5%) Commissioner audits were completed, with 134 (90.5%) Commissioner audits completed by 31 October 2023. This was the latest practical date to enable certification of the NHS England and DHSC annual report and accounts by 30 November 2023.
- At the point NHS England finalised its accounts, nine Commissioner audits remained outstanding, and these entities account for material transactions and balances in the NHS England group accounts. By Christmas 2023, 139 Commissioner audits were completed, with the remaining nine audits outstanding as the accounts were finalised. NHS England has had to perform alternative procedures to obtain sufficient assurance that the material transactions streams in the outstanding Commissioners are not materially misstated, in the context of the NHS England group accounts. My staff have reviewed the procedures performed by NHS England and are content that in the context of the NHS England group accounts, the results provide sufficient and appropriate assurance to my audit. I have therefore issued a clean “true and fair” audit opinion in respect of the NHS England annual report and accounts 2022-23. Note 1.3 to the accounts provides details of the transactions and balances relating to these nine Commissioners.
- NHS England clearly recognises the risks that late auditor reporting can represent and has been proactive in using its influence to support Commissioners and local auditors with timely delivery. As set out in its governance statement, NHS England demonstrates a clear understanding of the risks around late auditor reporting including the delays this has caused to the laying of its own annual report and accounts. NHS England has set out the range of interventions it has used to support Commissioners and local auditors to try and accelerate the audit of Commissioners’ accounts and it is critical this work continues for 2023-24.
- In 2023-24 the NHS England group has fewer entities and NHS England should continue its role in proactively monitoring audit progress of Commissioner accounts. In 2023-24 the NHS England group consists of the NHS England parent, 42 ICBs and SCCL. There are fewer Commissioners to consolidate but on average ICBs are significantly larger than CCGs. NHS England has been proactive in 2022-23 in monitoring the progress of late Commissioner accounts, including engaging with the local auditors, my staff, HM Treasury and the Financial Reporting Council (which regulates local audit firms). NHS England remains concerned about the capacity of local auditors to bring forward certification to enable NHS England, and hence DHSC, to lay their annual reports and accounts in Parliament significantly earlier than has happened over the last four financial years.
- I also have concerns given the wider local audit challenges, as set out in my report, Timeliness of local auditor reporting on local government in England.[114] Whilst the number of Commissioner audits in 2023-24 has reduced to 42, there could still be some risk in the delivery of NHS local audits due to the wider local audit system issues and significant delays in local government audits as the auditors work to clear this backlog.
Gareth Davies, Comptroller and Auditor General
National Audit Office, 157-197 Buckingham Palace Road, Victoria, London SW1W 9SP
22 January 2024
References
[1] Biographical details may be viewed on our website https://www.england.nhs.uk/about/board/nhs-england-board/members/
[2] Sir Andrew Morris was appointed to the NHS England Board from the NHS Improvement Board following the merger on 1 July 2022.
[3] Sir David Behan was appointed to the NHS England Board as a Non-Executive Director on 1 September 2022, having previously served as an Associate Non-Executive Director.
[4] Rakesh Kapoor’s directorship was temporarily transferred to NHS Improvement from 1 May 2021 to 31 March 2022, returning on 1 April 2022 as a Non-Executive Director of NHS England.
[5] Jeremy Townsend’s directorship was temporarily transferred to NHS Improvement on 24 March 2022, returning 1 July as a Non-Executive Director of NHS England.
[6] Baroness Mary Watkins was appointed as Non-Executive Director to the NHS England Board on 27 January 2023.
[7] Professor Sir Mark Walport was appointed as Non-Executive Director to the NHS England Board on 27 January 2023.
[8] Professor Sir Simon Wessely was appointed as Non-Executive Director to the NHS England Board on 27 January 2023.
[9] Julian Kelly was appointed as deputy chief executive by the nominations committee on 14 December 2022.
[10] https://www.england.nhs.uk/about/nhs-england-board/meetings/
[11] Jeremy Townsend’s directorship was temporarily transferred to NHS Improvement on 25 March 2022, and he took over the chair of NHS Improvement’s Audit and Risk Assurance Committee.
[12] Wol Kolade’s directorship was transferred from NHS Improvement to NHS England on 25 March 2022 and he took over the chair of the Audit and Risk Assurance Committee.
[13] Daniel Benton was previously a Non-Executive Director of NHS Digital until 31 January 2023 and was appointed as a Non-Executive Committee Member of the Data, Digital and Technology Committee as of 1 February 2023.
[14] John Noble was previously a Non-Executive Director of NHS Digital until 31 January 2023 and was appointed as a Non-Executive Committee Member of the Data, Digital and Technology Committee as of 1 February 2023.
[15] Steve Woodford was previously a Non-Executive Director of NHS Digital until 31 January 2023 and was appointed as a Non-Executive Committee Member of the Data, Digital and Technology Committee as of 1 February 2023.
[16] Susan Kilsby was appointed as a member of the People and Remuneration Committee on 1 July 2022.
[17] Richard Meddings was appointed as a member of the People and Remuneration Committee on 1 July 2022.
[18] Jeremy Townsend was appointed as a member of the People and Remuneration Committee on 1 July 2022.
[19] Mark Cubbon left the organisation on 2 April 2023. Steve Russell was appointed as Chief Delivery Officer from 30 March 2023, undertaking this role jointly with his role as National Director of Vaccinations and Screening.
[23] https://www.gov.uk/government/publications/government-financial-reporting-manual-2022-23
[24] https://www.gov.uk/government/publications/managing-public-money
[25] https://www.england.nhs.uk/ourwork/freedom-to-speak-up/whistleblowing-disclosures/
[27] It should be noted that the following provisions in the code do not apply to NHS England: Sections 1, 2.3, 2.11, 3.3a, 3.3b, 3.3c, 3.6e, 3.7, 3.8, 3.9, 3.14, 3.19, 4.9, 4.12, 4.13, 4.14, 5.7, 5.8 and 6.
[28] https://www.england.nhs.uk/publication/standards-of-business-conduct-policy/
[29] https://www.gov.uk/government/publications/orange-book
[30] https://www.frc.org.uk/directors/corporate-governance/uk-corporate-governance-code
[33] https://www.gov.uk/government/publications/serious-violence-duty
[35] https://www.england.nhs.uk/publication/integrated-care-boards-in-england/
[36] The number and value of contracts does not include NHS Digital due to separate accounts being submitted for 2022/23
[37] https://www.england.nhs.uk/2023/06/nhs-england-statement-on-capita-cyber-incident/
[38] https://www.gov.uk/government/publications/2023-to-2024-financial-directions-to-nhs-england
[39] https://www.england.nhs.uk/ournhspeople/
[40] https://www.england.nhs.uk/ournhspeople/online-version/lfaop/our-nhs-people-promise/
[42] https://www.england.nhs.uk/about/equality/equality-hub/workforce-equality-data-standards/wdes/
[43] https://www.stonewall.org.uk/full-list-top-100-employers-2022
[44] https://www.england.nhs.uk/long-read/gender-pay-gap-report-2022/
[45] https://www.gov.uk/guidance/report-trade-union-facility-time-data
[46] NHS England and NHS Digital’s 2022/23 wage bill combined.
[47] This figure is rounded up using Cabinet office’s reporting criteria.
[48] The most significant increase in staffing is including the transfer of staff from Monitor and Trust Development Authority at 1st July 2022 plus 2 months of NHS digital from 1 February 2023
[49] https://www.england.nhs.uk/publication/integrated-care-boards-in-england/
[50] The £245 threshold is set to approximate the minimum point of the pay scale for a Senior Civil Servant.
[51] Includes NHS Digital from 1 February 2023.
[52] The £245 threshold is set to approximate the minimum point of the pay scale for a Senior Civil Servant.
[53] Includes NHS Digital from 1 February 2023.
[54] A worker that provides their services through their own limited company or another type of intermediary to the client will be subject to off-payroll legislation and the Department must undertake an assessment to determine whether that worker is in-scope of Intermediaries legislation (IR35) or out-of-scope for tax purposes.
[55] Includes NHS Digital from 1 February 2023.
[56] The value of pension benefits accrued during the year is calculated as the real increase in pension multiplied by 20, less the contributions made by the individual. The real increase excludes increases due to inflation or any increase or decrease due to a transfer of pension rights. This value derived does not represent an amount that will be received by the individual. It is a calculation that is intended to provide an estimation of the potential benefit of being a member of the pension scheme.
[57] Sir David Sloman’s salary was recharged to NHS England from the Royal Free London NHS Foundation Trust where he was also formally employed and retained a post.
[58] Mark Cubbon’s salary was recharged to NHS England from Portsmouth Hospitals NHS Trust where he was also formally employed and retained a post. Mark Cubbon left NHS England on 2 April 2023.
[59] Ian Dodge left NHS England and NHS Improvement on 30 June 2022 and was paid a redundancy payment in the salary range of £160,000-£165,000 in July 2022 as compensation for loss of office; this is included in the salary band disclosed within the table. The full-year equivalent salary is £175,000-£180,000.
[60] Dame Ruth May retired on 16 June 2022 to access NHS Pension benefits and returned to post 18 June 2022 following the required 24 hours’ break in service. The full-year equivalent salary is £180,000-£185,000.
[61] Prerana Issar left NHS England on 04 October 2022. The full year equivalent salary is £230,000-£235,000.
[62] 80% of the salary costs for Dr Tim Ferris are recharged to NHS England and NHS Improvement from Mass General Brigham Inc. where is he is also formally employed and retains a post, with NHS England and NHS Improvement directly funding the remaining 20%. The full year equivalent salary is £190,000-£195,000. NHS England and NHS Improvement also paid Mass General Brigham Inc. a retirement contribution of $35,000-$40,000. Incorrect enrolment into the NHS Pension Scheme on commencement resulted in an underpayment of salary during 2021/22 due to pension contributions being deducted from his salary in error and these contributions were refunded during 2022/23.
[63] Christopher Hopson commenced in post on 13 June 2022. The full year equivalent salary is £205,000-£210,000.
[64] Navina Evans commenced in post on 01 July 2022 and 50% of the salary costs are recharged to NHS England from Health Education England where she was also formally employed and retained a post during 2022/23. As such, the above figures disclose 50% of salary, with Health Education England disclosing the remaining 50%. Dr Evans also received a payment for unused annual leave of £10-£15k, however Health Education England absorbed this full cost and 50% was not re-charged to NHS England. The full year equivalent salary is £205,000-£210,000.
[65] The value of pension benefits accrued during the year is calculated as the real increase in pension multiplied by 20, less the contributions made by the individual. The real increase excludes increases due to inflation or any increase or decrease due to a transfer of pension rights. This value derived does not represent an amount that will be received by the individual. It is a calculation that is intended to provide an estimation of the potential benefit of being a member of the pension scheme.
[66] On joining NHS England on 1 April 2014, Sir Simon Stevens voluntarily reduced his pay by 10% from the substantive rate of pay for the post of Chief Executive, which would normally be within the range £215,000–£220,000. He continued with this voluntary reduction in pay during 2021/22 and until he left NHS England on 31 July 2021. The full-year equivalent salary is £195,000-£200,000.
[67] During the period 1 April 2021 to 31 July 2021 the salary for Amanda Pritchard was recharged to NHS England and NHS Improvement from Guy’s and St Thomas’ NHS Foundation Trust where she was also formally employed and retained a post. From 1 August 2021 Ms Pritchard replaced Sir Simon Stevens as Chief Executive Officer for NHS England.
[68] Mark Cubbon replaced Amanda Pritchard as Interim Chief Operating Officer for the period 1 August 2021 to 13 December 2021. His salary was recharged to NHS England and NHS Improvement from Portsmouth Hospitals NHS Trust, where he was also formally employed and retained a post. The full-year equivalent salary is £225,000-£230,000.
[69] Sir David Sloman replaced Mark Cubbon as Chief Operating Officer on 14 December 2021. His salary was recharged to NHS England and NHS Improvement from Royal Free London NHS Foundation Trust, where he was also formally employed and retained a post. The full-year equivalent salary is £230,000-£235,000.
[70] Dr Emily Lawson left the position of Chief Commercial Officer on 18 July 2021. The full-year equivalent salary is £230,000-£235,000.
[71] Blake Dark replaced Dr Emily Lawson as Interim Chief Commercial Officer for the period 1 August 2021 to 31 December 2021. The full-year equivalent salary is £190,000-£195,000.
[72] Jacqueline Rock replaced Blake Dark as Chief Commercial Officer on 1 January 2022. The full-year equivalent salary is £230,000-£235,000.
[73] 80% of the salary costs for Matthew Gould are recharged to NHS England and NHS Improvement from DHSC where he is also formally employed and retains a post. As such, the above figures disclose 80% of salary and pension benefits, with DHSC disclosing the remaining 20%. The full-year equivalent salary is £125,000-£130,000.
[74] Dr Tim Ferris started in the joint post on 10 May 2021. 80% of the salary costs are recharged to NHS England and NHS Improvement from Mass General Brigham Inc where is he is also formally employed and retains a post, with NHS England and Improvement directly funding the remaining 20%. The full-year equivalent salary is £190,000-£195,000. Incorrect enrolment into the NHS Pension Scheme on starting resulted in underpayment of salary during 2021/22 due to pension contributions being deducted from his salary in error.
[75] As per previous submissions, the column Cash Equivalent Transfer Value on 31 March 2021 is the uninflated value whereas the real increase in CETV is the employer-funded increase.
[76] Sir David Sloman chose not to be covered by the NHS Pension arrangements during the reporting period.
[77] Ian Dodge chose not to be covered by the NHS Pension arrangements during the reporting period.
[78] Professor Sir Stephen Powis chose not to be covered by the NHS Pension arrangements during the reporting period.
[79] Dame Ruth May accessed NHS 1995 Pension Scheme benefits on 16 June 2022. This is the reason for the large decrease in CETV from 31 March 2022 to 31 March 2023.
[80] Dr Tim Ferris was not eligible to be covered by NHS Pension arrangements during the reporting period.
[81] Christopher Hopson commenced in post on 13 June 2022.
[82] Dr Navina Evans commenced in post on 1 July 2022 and chose not to be covered by the NHS Pension arrangements during the reporting period.
[83] Non-executive directors do not receive pensionable remuneration and therefore have no pension-related benefits
[84] Richard Meddings donated his non-executive director remuneration to charity via NHS England’s Give As You Earn scheme.
[85] Wol Kolade waived his entitlement to non-executive director remuneration.
[86] Professor Lord Ara Darzi left NHS England on 30 June 2022. The full-year equivalent salary is £5,000-£10,000.
[87] Jeremy Townsend returned from a temporary transfer to NHS Improvement in the same role and salary of Non-Executive Director and Chair of ARAC on 1 July 2022. The full-year equivalent salary is £10,000-£15,000.
[88] Professor Sir Munir Pirmohamed transferred from NHS Improvement to NHS England in the same role and salary of Non-Executive Director on 1 July 2022. The full-year equivalent salary is £5,000-£10,000.
[89] Sir Andrew Morris transferred from NHS Improvement where he held the role of Interim Chair at a salary of £60,000-65,000 to NHS England as a Non-Executive Director on 1 July 2022. The full-year equivalent salary is £5,000-£10,000.
[90] Sir David Behan joined NHS England on 1 September 2022 and waived entitlement to non-executive director remuneration due to also being the Chair of Health Education England. The full-year equivalent salary is £5,000-£10,000.
[91] Baroness Mary Watkins joined NHS England on 27 January 2023. The full-year equivalent salary is £5,000-£10,000.
[92] Professor Sir Simon Wessely joined NHS England on 27 January 2023. The full-year equivalent salary is £5,000-£10,000.
[93] Sir Mark Walport joined NHS England on 27 January 2023. The full-year equivalent salary is £5,000-£10,000.
[94] Non-executive directors do not receive pensionable remuneration and therefore have no pension-related benefits.
[95] Lord David Prior left NHS England on 24 March 2022. The full-year equivalent salary remains at £60,000-£65,000.
[96] Richard Meddings CBE joined NHS England on 25 March 2022 and waived his entitlement to non-executive director remuneration. The full-year equivalent salary is £60,000-£65,000.
[97] David Roberts CBE waived his entitlement to non-executive director remuneration and left NHS England on 30 June 2021.
[98] Wol Kolade joined NHS England on 25 March 2022 and waived his entitlement to non-executive director remuneration.
[99] https://www.legislation.gov.uk/uksi/2021/178/made
[101] https://questions-statements.parliament.uk/written-statements/detail/2020-11-23/hcws593
[103] https://www.nao.org.uk/reports/managing-nhs-backlogs-and-waiting-times-in-england/
[104] https://www.nao.org.uk/reports/progress-in-improving-mental-health-services-in-england/
[105] https://www.nao.org.uk/reports/alcohol-treatment-services/
[106] https://committees.parliament.uk/publications/41823/documents/207410/default/
[107] https://committees.parliament.uk/publications/41370/documents/203376/default/
[108] There were 106 CCGs until 30 June 2022. CCGs were then replaced with 42 ICBs from 1 July 2022.
[109] A medical practitioner could be a doctor, dentist or optician.
[111] https://www.nao.org.uk/wp-content/uploads/sites/29/2020/01/Code_of_audit_practice_2020.pdf
[113] https://committees.parliament.uk/publications/40738/documents/198470/default/

