1. Introduction
This guidance supports the planning and commissioning of local mental health rehabilitation inpatient services as part of a whole pathway, to meet the identified need of local populations. Standardising the approach to the commissioning of these services should identify and reduce inequalities and improve quality, ensuring services are safe, effective, evidence based and informed.
This is based on the premise that ‘all means all’. Services will be commissioned so that everyone who presents with a mental health rehabilitation need requiring an inpatient service should be able to access this locally, when they need it and in a way that is flexible and responsive to their needs.
Mental health rehabilitation inpatient services provide care and treatment for adults and older adults who have an identified mental health rehabilitation need. This includes people who may also have a learning disability, who are autistic or who have been given a diagnosis of personality disorder. People may be detained under the Mental Health Act (MHA), and some may be restricted under section 37/41 (MHA) (HM Prison and Probation Service, 2011). The decision to admit will be based on a comprehensive clinical assessment.
These inpatient services assess and treat mental ill health, with the core objective of providing hope, maximising quality of life and social inclusion, promoting independence and supporting the development of skills, so that people can return to live in the community (Killaspy et el, 2005).
A number of the quality failings in both NHS and independent sector hospitals have occurred in services that were described as mental health rehabilitation inpatient services of some kind. The Care Quality Commission (CQC) has highlighted specific concerns in relation to ‘locked rehabilitation’ services (CQC, 2017). Commonly, these are often spot purchased by multiple commissioners, with people from different geographic areas, with additional and varied diagnoses and needs, disconnected from local pathways, all in one service.
This commissioner guidance is underpinned by the overarching commissioning framework for mental health inpatient services. It draws on the following learning, standards and guidance, corroborated and developed through workshops and visits to mental health inpatient rehabilitation services.
- GIRFT (2022) Mental health – rehabilitation national report
- NICE (2020) NICE guideline [NG181] Rehabilitation for adults with complex psychosis
- Royal College of Psychiatrists (2022) Standards for inpatient mental health rehabilitation services, 4th edition
- Royal College of Psychiatrists (2023) Standards for mental health inpatient rehabilitation services for adults with a learning disability
- NHS England (2019) Community mental health framework for adults and older adults
In developing this guidance, we spoke to over 100 people from a variety of stakeholder groups, including experts by experience (patients, families and carers), commissioners, mental health providers, operational managers, clinicians (NHS and independent sector), the Care Quality Commission (CQC), the Voluntary and Community, Faith and Social Enterprise (VCFSE) sector, and national and regional teams from NHS England.
This guidance is for those who have commissioning responsibility for the mental health needs of their local population, recognising that commissioning can be carried out by different individuals and organisations, separately and collaboratively, and it can be delegated depending on local arrangements. The commissioner of mental health rehabilitation inpatient services could be:
- an integrated care board (ICB)
- a provider collaborative
- an NHS-led provider collaborative
The guidance also has relevance for mental health providers, professionals and partnership organisations across integrated care systems (ICSs), including:
- local authority commissioners
- commissioners of specialised mental health, learning disability and autism services, and health and justice services
- mental health community and hospital healthcare providers, both NHS and independent sector
- VFCSE
- People who use services, their families and carers, and the organisations that advocate for, and represent them.
2. Scope
The scope of this guidance is mental health rehabilitation inpatient services for all adults and older adults; that is people aged 18 years and over. This includes anyone who has additional diagnoses and/or needs; for example, people who also have a learning disability or who are autistic, and people who have been given a diagnosis of personality disorder. Also included are those who may transition from children and young people’s (CYP) mental health inpatient services. It incorporates people detained under the MHA, including those detained under section 37/41 of the MHA.
Community mental health transformation is at the heart of the NHS Long Term Plan for Mental Health. All areas are expected to develop dedicated adult community mental health rehabilitation services as part of their transformation of community mental health provision, reducing the reliance on inpatient care and to support people in the least restrictive setting.
Wherever possible mental health rehabilitation needs should be met in the community. However, where someone’s needs exceed what can be safely and effectively treated in the community, admission to a mental health rehabilitation inpatient service may be required. This should always be local and consider the least restrictive option, which should be kept under review.
Whilst the scope of this commissioning guidance focusses on mental health rehabilitation inpatient services, it is important to recognise the interfaces between these services and other mental health services, the most common are:
- acute inpatient mental health care for adults and older adults
- acute mental health inpatient services specifically for adults with a learning disability and autistic adults
- adult medium, low secure inpatient and specialist community forensic services (NHS England, 2018 and NHS England, 2018)
- community mental health services, including early intervention in psychosis (EIP) teams
- community learning disability and autism teams
- CYP mental health inpatient and community services.
Policy context relevant to all mental health inpatient services, including adult rehabilitation, is described in the overarching commissioning framework for mental health inpatient services.
3. Key messages
3.1 Language and terminology – describing mental health rehabilitation inpatient services
The variation in the language and terminology used to describe mental health rehabilitation inpatient services is confusing and persists despite previous attempts to tackle it. Stakeholders identified this as the most important issue to address in this guidance, the GIRFT report on mental health rehabilitation supports the need for clarification and ‘standardisation of rehabilitation care’.
Mental health rehabilitation inpatient services should be commissioned and described as:
Level 1 mental health rehabilitation inpatient services
Level 1 services have many of the characteristics of inpatient services described elsewhere/previously as ‘community rehabilitation units’ (RCPsych, 2019).
- These services are needs led and locally based, serving a local population.
- These services exist to meet the needs of people who have a mental health rehabilitation need that can only be treated within an inpatient environment.
- Level 1 services are normally accessed via an adult acute mental health inpatient service, including those specifically for adults with a learning disability, or who are autistic.
- As with adult acute mental health services, the default position for autistic people and those who have a learning disability, with a mental health need, would be to access mainstream mental health rehabilitation inpatient services. However, it is recognised that some people’s needs cannot be met well in a mainstream service, even with reasonable adjustments. Commissioned services may include mental health inpatient rehabilitation services that are specifically for people with a learning disability, or who are autistic.
- Level 1 services are part of a clear, agreed pathway that includes community mental health rehabilitation teams and wider general and specialist teams, such as primary care, community learning disability, autism or mental health
- They are staffed by a multidisciplinary team that have the appropriate training, skills and knowledge in mental health rehabilitation and should meet specialist need as required, for example, drug and alcohol support.
- These services should be firmly connected to the wider resources and agencies within the community, for example, employment support, housing and welfare.
Level 2 mental health rehabilitation inpatient services (higher support needs)
Level 2 services have many of the characteristics of services described elsewhere/previously as ‘high dependency rehabilitation units’ (RCPsych, 2019).
- All the points above for level 1 services apply to level 2 services.
- Level 2 services neither support nor encompass inpatient provision that may be described as ‘locked rehabilitation’, and they are not long-term placements, continuing care, or a ‘home’ by default.
- The key difference between level 1 and level 2 mental health rehabilitation inpatient services is that a level 2 service can offer more intensive support to people to meet their needs; this may be relational and/or adapted environments and procedures.
- Commissioning arrangements for level 2 services will be locally determined and will depend on the size and assessed need of the population in each ICS footprint.
- Level 2 services are part of the same pathway of care as level 1 services and may on occasion be accessed via a level 1 service.
- Level 2 services may accept people who need their mental health rehabilitation needs met at a pace that is individually and clinically appropriate for them. These services should be commissioned to do this while ensuring that lengths of stay are appropriate and reviewed regularly, to avoid stays in hospital that are longer than absolutely necessary.
Commissioners must be clear, based on their population needs’ assessment, what services they need to commission and plan accordingly using this two-level approach for all mental health rehabilitation inpatient services. They should commission the right types of service to meet agreed local need. Section 7: The service; provides more information to underpin this key message.
3.2 Local services
Mental health rehabilitation inpatient services must be commissioned as locally as possible. The GIRFT national report for mental health rehabilitation reported in 2022, that half the 3,500 people who used inpatient mental health rehabilitation beds in England were placed out of their local area, mainly in independent sector mental health providers.
Accessing mental health rehabilitation inpatient services that are at a distance from a person’s home makes it harder for people to reconnect with their communities, receive visits from family and friends, and access support networks. This makes it more challenging for the inpatient clinical team to deliver critical aspects of the care and treatment required for mental health rehabilitation. The person’s community team cannot engage as easily, and commissioners cannot fulfil their responsibility effectively. Length of stay is generally longer and discharge planning more complicated for all involved.
Where mental health rehabilitation inpatient services admit people from different geographical areas, the inpatient clinical team cannot work efficiently. Despite best efforts the team will not have the local knowledge of and connections to all these areas.
“I felt like I had been put somewhere and left, forgotten about, only when I started to get well that my home team got involved, but it was too late.”
“Yes, I’ve got community leave, but this isn’t my community.”
“I’m going to have to do all this again when I’m discharged as this isn’t where I’m going to live when I leave hospital.”
“Try to do something, but your team aren’t in the area so can’t come to meetings, or they won’t help because they’re not in the area.”
“I have been in and out of services since I was 10 years old. This recent admission has seen me in 6 placements in 11 months.”
People currently accessing mental health rehabilitation inpatient services.
3.3 Data for mental health rehabilitation inpatient services
GIRFT national report for mental health rehabilitation has identified the need for “accurately and consistently coded” data about the use of mental health rehabilitation inpatient services. Commissioners need data about everyone who requires access to a mental health rehabilitation inpatient service, including waiting times and outcomes. Increasing the oversight and awareness of where people are placed is critical in tackling the quality and safety challenges within mental health inpatient settings; this is particularly true for people accessing rehabilitation services.
Commissioners need to have the same level of visibility and scrutiny of activity, cost, and outcomes for mental health rehabilitation inpatient services as they do for all other inpatient settings. These services are a crucial part of the mental health pathway, so accurate and reliable data that is universally understood is critical. This will support planning (NHS England, 2023), escalation of delays and issues related to throughput and flow. Commissioners must ensure that mental health providers are supported to develop rehabilitation data dashboards to improve inpatient services and their related pathways where needed.
3.4 Purpose of admission
The purpose of admission to a mental health rehabilitation inpatient service must always be collaboratively agreed and articulated. Commissioners need to be assured that the purpose of admission is understood by everyone involved and that there is a clear description of how this will be achieved. This is important for staff in the inpatient service, the community team, commissioners, and particularly so for the person accessing the service, their families and carers.
“In the past rehabilitation inpatient services have been seen to do everything, but not been able to do a lot.”
“There must be a shift from patients going to rehabilitation inpatient services because nothing else has worked… and these services being expected to mop up gaps elsewhere in the pathway.”
“Rehabilitation inpatient services are not a last resort .. admission should be a positive decision.”
Clinicians working in mental health rehabilitation inpatient services.
4. Specific considerations
4.1 All means all
To ensure all those with mental health rehabilitation needs that require an inpatient admission can access an appropriate service, services must be planned and commissioned with everyone in mind and the ‘all means all’ principle as described in the commissioning framework for mental health inpatient services applies (see section 5 of the framework). Local commissioning plans must ensure that the services commissioned meet the assessed needs of the total population and can deliver the care and treatment required. It is not appropriate for people to be placed out of area because local services have not been planned with them in mind.
Commissioners of mental health rehabilitation inpatient services need to take a systematic approach to knowing their local communities, to understand who is over and underrepresented in these services, and who has poorer experiences and outcomes. They should work with relevant stakeholders to address identified local discrimination and inequalities within these services.
Mental health rehabilitation inpatient services should not develop exclusion criteria that would prevent some patients from accessing the treatment they need.
Where people have additional diagnoses or needs, expertise and support should be sought from relevant specialists who should work alongside the mental health rehabilitation inpatient team, offering interventions, advice and support as required.
4.2 Supporting people with a learning disability or who are autistic
Mainstream mental health rehabilitation inpatient services should make necessary reasonable adjustments (Equality Act 2010) based on identified needs. These will vary but may include:
- environmental sensory adaptations
- availability of different communication tools and materials
- staff with relevant training to support people who are autistic or have a learning disability, and to champion this support on the wards
- an advocacy service with relevant skills.
Where people are clinically assessed as requiring more than reasonable adjustments, mental health rehabilitation inpatient services that can provide specifically for people who also have a learning disability or who are autistic should be commissioned. Commissioning guidance for acute mental health inpatient services for adults with a learning disability and autistic adults differentiates between mainstream and more specific services. The same principles would apply when considering mental health rehabilitation inpatient services. The standards developed for mental health rehabilitation inpatient services for adults with a learning disability (RCPsych, 2023) should be included, where applicable, in contracts with mental health providers and monitored.
In summary, commissioners should ensure that for all mental health rehabilitation inpatient services that provide specifically for people who have a learning disability or who are autistic:
- the workforce is appropriately qualified and knowledgeable to provide the right support
- training is offered to ensure clinical teams have the right values, skills and capabilities
- policies relevant to these inpatient services and pathways are implemented; for example, in respect of Care (Education) and Treatment Reviews (C(E)TRs) and Dynamic Support Registers (DSR), discharge planning, personalised care and support plans
- therapeutic interventions are tailored to specific needs
- the appropriateness of the physical environment is considered.
Exactly how these specific mental health rehabilitation services are commissioned for each ICS population will depend on the local geography, numbers involved and how frequently these services are required.
4.3 Considerations for people who have a diagnosis of personality disorder
It is important to note that there are currently some mental health inpatient services registered with CQC as ‘rehabilitation’ services, which are commissioned for people who have received a diagnosis of personality disorder, specifically a diagnosis of borderline personality disorder. The provision of such services is not in line with NICE guidelines for the care and treatment of people who have received this diagnosis and as per the recommendations of GIRFT national report for mental health rehabilitation, should not be described or commissioned as such. This misuse of the term ‘rehabilitation’ is unhelpful and confusing for everyone but particularly for the people themselves, their families and carers.
The needs of this group who are currently being admitted to these types of services should be met locally, through co-produced alternative, community services which provide therapeutic, least restrictive and trauma informed care and support. Commissioners will want to consider the development of trauma-specific services to meet the needs of people who are currently admitted to these inpatient services given the majority of them will have experienced significant trauma and adversity.
However, the additional diagnostic label of personality disorder should not preclude admission where there is an identified mental health rehabilitation need. During stakeholder engagement, people accessing services and staff working in them explained that mental health rehabilitation inpatient services for people who have received diagnosis of personality disorder should deliver specific evidence-based treatment, with the whole inpatient team trained and able to deliver this approach collaboratively and consistently. These commissioned services should not be overly restrictive and should focus on relational approaches to safety as the most effective way to keep the person safe.
“It is important that I feel people haven’t forgotten about me, and I am still valued.”
“Sometimes you just need someone to sit and talk to you, not just take away your stuff.”
“…that feels like punishment, when you’re already punishing yourself.”
People currently accessing a mental health rehabilitation inpatient service.
Again, how these services are commissioned in each area will depend on the number of people who require access, efficiency of whole pathways and level of need. These specific services may need to be commissioned for more than one ICS, across neighbouring ICS footprints.
4.4 Considerations for people with other additional needs
Each person is an individual and there may be other needs to consider in addition to the assessed mental health rehabilitation need. These may be relating to physical health, degenerative neurological conditions or acquired brain injuries for example. Commissioners should make commissioning decisions based on analysis of their local population need, size of population, historical activity, geography and accessibility.
5. Commissioning arrangements
Mental health rehabilitation inpatient services should be commissioned locally for populations in a planned and proactive way, with a move away from spot purchasing from multiple mental health rehabilitation inpatient services across the country, or commissioning on a cost per case basis.
The configuration of mental health rehabilitation inpatient services for each ICS population should be articulated in a way that everyone can understand, particularly those who may access services, their families and carers.
Where numbers across a large geography are particularly small, commissioning services across more than one ICS footprint may be the right strategy. Robust systems must be in place to ensure commissioners and relevant community teams can work closely with people who access these services, their families and carers, and the inpatient multi-disciplinary team (MDT) .
The contract should be held by one commissioner, normally the host commissioner, and placing commissioners should use this contract to commission the respective mental health rehabilitation inpatient service for their population. All mental health rehabilitation inpatient services should have an identified host commissioner.
The placing commissioner will continue to be responsible for individual placement oversight and ensuring the pathway is being managed effectively, regardless of the geographical distance from the person’s local area. Plans should always be made for commissioners to visit services in person on a regular basis; exclusive use of virtual meetings is not acceptable as part of the oversight for anyone placed outside the ICS footprint.
“No one had an overview. I was the only one keeping tabs on what was happening…it shouldn’t have been me doing it.” Family member of relative placed out of area.
“I don’t see my case manager or commissioner in person. If I do see them, it is usually a meeting on the screen.”
Person placed out of area in a mental health rehabilitation inpatient service.
The host commissioner for each mental health rehabilitation inpatient services should fulfil the commissioning requirements in terms of assuring quality and safety for the service. This function should be undertaken whenever possible face to face and never exclusively virtually.
There must be robust and established lines of communication between the placing and host commissioner prior to and during any admission and placement. Commissioners need to assure themselves they are not commissioning services that by their very nature are at an increased risk of delivering unsafe and poor quality care.
6. Care pathway and interdependencies
6.1 Whole pathway approach
Commissioners should ensure that a whole pathway approach is taken so that services work collaboratively, transitions are kept to a minimum and movement across the pathway is seamless and efficient. ICBs should describe the pathway between related services in the commissioning strategy for their population.
Good practice principles should be considered when transition is required from a CYP mental health community or inpatient service to an adult mental health rehabilitation inpatient service.
6.2 Community mental health, learning disability and autism teams
Local care co-ordinator or named key worker
It is the responsibility of the identified community mental health, learning disability, or autism team to remain engaged throughout the whole mental health rehabilitation inpatient stay. This maintains local relationships and also means the inpatient clinical team will be aware of what is available locally for each person.
This is usually the responsibility of the local care co-ordinator or named key worker, and wherever possible their role should be consistent and relevant to the person’s presenting need. Their visits or attendance at reviews should be in person, face to face. While this may not be as easy when someone is placed away from their local area, it is in these instances even more important. These visits support active discharge planning and where appropriate ensure that repatriation is being considered and pursued.
“When planning discharge constant changes in staff members from the community team made it difficult.”
A family member.
Community mental health rehabilitation teams
The NHS Long Term Plan for Mental Health states that all systems should provide support for people with severe mental illness, with the development of new and integrated models of primary and community mental health care. This includes care, support and treatment for individuals with specific needs, including mental health rehabilitation needs.
Stakeholders reported positive experiences where there was a dedicated community mental health rehabilitation team, able to work closely with the inpatient clinical team and particularly where this was an integrated team. The elements that work well are:
- the assertive and flexible approach
- consistency of clinical team members
- reduction in transitions
- connection to the community.
6.3 Interdependencies
Commissioners need to work with providers of mental health rehabilitation inpatient services and other stakeholders to ensure that local partnerships are developed and supported. Key interdependencies with mental health rehabilitation inpatient services include, but are not limited to:
- VFCSE
- independent sector providers
- local authorities
- housing and accommodation providers
- Mental Health Case Work Section (MHCS) – His Majesty’s Prison and Probation Service (HMPPS).
7. The service
7.1 What should the service feel like?
People who use services, their families and carers were clear about what mental health rehabilitation inpatient services should feel like.
- hopeful
- empathic
- respectful
- compassionate
- safe
- community facing
- diverse
- inclusive
- person centred
- caring
- equality focused
- local
- trauma informed
- empowering
- kind
- recovery focused
7.2 Mental health rehabilitation services are not ‘locked rehab’.
“A high number of wards continued to identify as locked rehabilitation – this is against the least restrictive principle and potentially represents a breach of human rights.” CQC, 2020.
As described in section 3: Key messages, the different descriptions used for mental health rehabilitation inpatient services are confusing and can be misleading:
- ‘locked rehabilitation’ (not recognised but still used)
- ‘high dependency rehabilitation’
- ‘longer term high dependency rehabilitation’
- ‘highly specialist high dependency rehabilitation’
- ‘complex care rehabilitation’
- ‘longer stay rehabilitation’.
The case for change in relation to ‘locked rehabilitation’ services is clear and in future the commissioning of services described as such should cease.
Mental health rehabilitation inpatient services should not be ‘locked’ so that every person is prevented from leaving. Services can operate a controlled access and egress system, for example, use of programmed fobs. The appropriate level of access for each person should be determined based on an individual clinical assessment, and there should be a robust process in place to ensure that this is regularly reviewed.
Mental health rehabilitation inpatient services are not adult secure services, which have a specific function that is described in service specifications (NHS England, 2018 and NHS England, 2018). Adult medium and low secure services are commissioned to ‘prevent’ and ‘impede’ escape from hospital, due to the risk of harm to others. Mental health rehabilitation inpatient services should not be commissioned on this basis.
A definitive description of mental health rehabilitation inpatient services is needed, and all such services should use the same language to describe themselves. Section 3, Key messages, describes the two-level approach which should be used.
The impact of moving to this approach for the commissioning of mental health rehabilitation inpatient services will need to be assessed locally, and collaboratively planned and managed with relevant stakeholders. For example, in some areas this will need to include NHS-led provider collaboratives of adult secure services where ‘locked rehabilitation’ may for some people be accessed as part of a forensic pathway, or where an access assessment recommends it as an alternative to admission to a secure service.
7.3 How should the service work?
Commissioners should ensure that the standards for mental health rehabilitation inpatient services, including those for services specifically for people with a learning disability and people who are autistic, are reflected in service specifications within the contracts they hold with providers.
Stakeholders described what they felt were the most important components of the inpatient service. These are described under the stages of the inpatient pathway; they are included here to support commissioners and strengthen the existing published standards.
Assessment and admission
Referrals to the service should state the reason for admission and the identified mental health rehabilitation needs, to support an appropriate assessment by the inpatient clinical team. Admissions should be planned, and pre-admission visits are considered good practice.
“Our son was admitted with 1 days’ notice from an acute MH ward. This was the first time we knew that a MH rehabilitation ward was being considered.”
Parents of someone accessing a mental health rehabilitation inpatient service.
The purpose of admission should describe the specific assessments and interventions required, anticipated length of stay and estimated date of discharge. These should be agreed collaboratively at the earliest opportunity with the person accessing the service, their families and carers, the inpatient MDT, community team and commissioner. This information should be clearly articulated to make explicit what is expected from the admission.
Care and treatment
All MDT reviews, ward rounds, care programme approach meetings and C(E)TRs must centre around the person. People in services should be supported and empowered to attend throughout and where possible to lead their reviews.
“We use a dialogical model. During MDT reviews the conversation stops when the patient is no longer in the room.
Everything is discussed with the patient including risk issues.” Ward manager in a mental health rehabilitation inpatient service.
“I have had a good experience of reviews; the language used should be human, not clinical and not rushed.”
Family member of someone accessing a mental health rehabilitation inpatient service.
The purpose of admission, specific interventions required, anticipated length of stay and estimated date of discharge should be regularly reviewed, and any changes to the original position should be documented with reasons for the changes.
All therapeutic interventions and activities should focus on relationships; they should be holistic, needs led, trauma-informed and diverse.
Activities and leave from the ward should be planned individually for each person. Structured activity programmes should be co-designed with people on the ward to ensure they reflect the activities they request, and feel will be helpful. Co-facilitation of activities and groups by people accessing services and staff are described positively by those leading sessions and those attending. Activities should happen in line with NICE guidelines and be available 7 days a week and not restricted, for example, to 9am to 5pm.
“The focus of the service and staff should be on independence, rather than dependence and on fixing people.”
“One to ones with staff who work with me all the time and know me well are the most important thing. I’d support more of these.”
“I had never cooked for myself before; I have been in hospital a long time. I started with one meal a week and now I’m building up a list of things I can cook for myself.”
“When thinking about activities remember it’s okay to have fun. Children can have fun, why can’t adults?”
People accessing mental health inpatient rehabilitation services.
Vocational and employment opportunities are important to help people think about options, with an emphasis on appropriately knowledgeable and skilled staff providing education and support. Returning to their previous occupation is not an option for many people and therefore to help their recovery they will need to be supported to think about what transferrable skills they have.
“See everyone in their own context. This leads to thinking about their individual goals.”
Clinician in a mental health rehabilitation inpatient service.
Peer support should be encouraged; making friends in services is really important to people, their families and carers.
“Friends are a big part of my recovery, making friends with other patients mustn’t be seen as a bad thing.”
“Support from my peers on the ward is a big thing.”
People accessing mental health rehabilitation inpatient services.
Appropriate and accessible support for substance misuse while an inpatient needs to be available.
Physical exercise options need to be individually planned and varied These need to be available on and off the ward, accessible opportunities in the community is positive.
Primary and secondary physical health needs should be understood and met. People described a sense that not all staff were confident in this area and needed more appropriate training. Support while in hospital and a better understanding of how to self-manage physical health in the community is valued by people accessing these services.
Adaptation of the ‘red to green days’ approach, a tool developed for emergency care settings, has been suggested for mental health rehabilitation inpatient services; its adaption for mental health inpatient services is recommended in the adult acute mental health inpatient guidance.
Discharge and transition
Early person-centred discharge planning is crucial. Discussions about the purpose of admission, interventions required, length of stay and estimated date of discharge should inform this from the point of admission. In some instances, this may be considered earlier, at the point of the pre-admission assessment to inform the admission.
NICE guidance emphasises the need for people and their social networks to be actively involved in discharge planning, with good information provided about available support. Transitions are difficult times for people, their family and carers; multiple transitions can be particularly problematic. Those accessing services feel it is important to maintain continuity by being able to work with some members of the MDT on an ongoing basis, from the inpatient service to the community. They also view contact with their community team, ideally a community mental health rehabilitation team, throughout admission as crucial to supporting and facilitating earlier and more collaborative discharge planning.
People want gradual discharge planning and don’t want to feel rushed as this can be a particularly anxious time. NICE guidance recommends appropriately paced discharge planning and periods of phased leave with a gradual move to independence.
“If the pathway works well it should be easy in and easy out.”
“I need support to prepare. How will the world see me after being detained for so long?”
“Don’t just say – ‘now you are fine’; structure it, discharge needs lots of planning.” People in mental health rehabilitation inpatient services.
“Transitions are bumpy at best, traumatic at worst.” Family member.
“Early visible in and outreach with good discharge planning avoids readmission.”
Clinician working in a mental health rehabilitation inpatient service.
7.4 Physical environment
The commissioned service needs to be delivered in a physical environment that is conducive to mental health rehabilitation. It should be clean and well maintained, light and homely, not too clinical or sterile. While we recognise that access to capital can be limited, where care and attention has been paid to the co-design, co-production and physical condition of wards, these environments feel better for people accessing them and staff working in them. People view the opportunity with the right resource to be creative and personalise bedrooms and communal areas as important.
“If ward surroundings resemble penal institutions, it must be really difficult for inpatients not to feel that they are being punished for being ill.” Family member.
“In poor physical environments how can individuals be expected to feel that they are valued or believe that society cares about them?”
Family member.
Mental health rehabilitation inpatient services should have appropriate signage, soft furnishings and flooring, and be sensory friendly to meet the diverse needs of the people who access the services, including those who may be older, have physical and/or sensory impairments, or have a learning disability or are autistic.
Some rooms and areas within mental health rehabilitation inpatient services have a specific emphasis and requirement, for example:
- Activity space inside and outside – while people will be accessing activities off the ward in the community, facilities are also needed on the ward for flexible use
- Kitchens – need to support different levels of self-catering and risk management
- Treatment rooms – need to support progression to self-medication
- Physically and procedurally access to and egress from the ward should be facilitated easily, especially as it is expected that people are able to move off the ward frequently to access the community.
Access to reliable Wi-Fi in hospital is essential, particularly for people engaging in rehabilitation activities. If Wi-Fi connections on wards are unreliable people have to use their own mobile phones and personal data, this is unaffordable for many and creates inequalities.
“If ward surroundings resemble penal institutions, it must be really difficult for inpatients not to feel that they are being punished for being ill.” Family member.
“In poor physical environments how can individuals be expected to feel that they are valued or believe that society cares about them?”
Family member.
The shared experience of someone in a mental health rehabilitation inpatient service
What makes things work well?
How everyone treats you with respect. They are people that want to help you. When you explain what has happened to you they do their best to understand and create a plan catered to you so you can get the best experience.
Having staff to talk to you and remind and help you with basic needs, to take medication, personal hygiene, food and fluids, engage with you, get you back on your feet.
Psychology gives me different views from a different perspective to understand myself better, helps with confidence.
OT amazing, they are there to engage with you all the time. They know how to talk with people to make them feel relaxed.
When you have a troubling time you can always go to the doctors and talk with them.
Everyone on the ward has their own personal space.
The staff always encourage you to complain when you are dissatisfied with something and try to troubleshoot so other people don’t have to face the issue.
Enjoy how clean the facilities are, cleaners come every day.
What doesn’t work quite so well?
When there are not enough staff so it is difficult for them to engage with you, eg activities or having a small chat.
When there’s not much to do on the ward.
Some staff members work just to get paid, not bothered about whether people get better or not. Even when you try to get help they give you a vague answer so they can do paperwork and go home; don’t feel as supported then.
Patients sometimes feel a bit too uncomfortable with how much is taken away from them. Restricts your growth as coming out of hospital you learn from your mistakes because there is always going to be hazards.
The internet is really, really bad.
What would improve things?
Most of us stay in our rooms which gets us into a cycle of just thinking, getting out more would improve our mental state… more facilities to keep patients busy.
Not a fan of division between males and females because on the outside we are going to be mixed anyway.
Exercise classes – a lot of hoops to get a simple thing done, got to go to management, risk assessment, it would take at least a month to get a small activity in.
It can get really hot, there is no real way to turn the heating off. Put some time into updating the building into a modern standard.
Furniture could be improved, it’s uncomfortable, never find myself sitting comfortably, always slouching.
Would like the food to be a bit better, meets the nutrients standards, but sometimes it doesn’t look appetising. Not much variety, not much flavour. It would be nice if staff could eat with the patients… would like to listen to music or watch TV when we eat, you can just hear cutlery.
8. Involvement, co-production and advocacy
This section describes the aspects of involvement and co-production that commissioners should consider in the contracts for mental health rehabilitation inpatient services.
Everyone accessing these services should be supported to have a voice in their care. Valuing lived experience and respecting people’s perspectives is crucial. People in services, their families and carers need to be supported to make shared decisions about their care (NICE, 2021).
Families and carers describe varying levels of involvement in the care of their relative. It is important to ensure that both the right support and appropriate feedback mechanisms are in place not only from members of the mental health rehabilitation inpatient clinical team but also other interfaces, e.g., community teams. Families talk about wanting support from the MDT to feel hopeful about their relative’s recovery and pathway out of inpatient services. Cited examples of good practice are family/carer champions on mental health rehabilitation wards and family engagement workers as part of the inpatient MDT.
People, their families and carers (with appropriate consent) should be present, empowered and involved. Increased access to members of the inpatient MDT is highlighted as important, and this access should be as flexible as possible, such that contact can be made in the evening and at weekends if required.
It is vital that mental health rehabilitation inpatient services are part of a local pathway of care that promotes inclusion, strengthens individual’s rights, and is orientated towards citizenship. Inpatient mental health rehabilitation inpatient services provide for many people who may face discrimination in their daily lives, because of their race, class, gender or sexuality. Efforts should be made to address disparities and improve outcomes by seeking to understand local populations, assess trends and act on over and under representation of certain communities of people. For this it is essential that people, families and carers from racialised, ethnically and culturally diverse communities have increased opportunities for shared decision-making (NHS England, 2023).
Mental health rehabilitation inpatient services vary considerably in the extent to which they consult those with lived experience and involve them in co-production, as well as remuneration for this experience and expertise. It is essential that mental health rehabilitation inpatient services should be commissioned to recognise these contributions by making consistent and appropriate payments.
Mental health rehabilitation inpatient services must be commissioned to ensure that people, irrespective of their legal status, have access to and are supported to meet with independent advocates who are culturally appropriate and aware, and have the right skills and experience.
A recent review of advocacy for people with a learning disability and autistic people who are inpatients in mental health hospitals found that:
“The behaviour, culture and values of the hospital can undermine or strengthen advocacy, dependent on whether advocacy is genuinely welcomed and seen as an integral part of upholding rights, inclusion of the person and ensuring patient safety, or whether it is treated with suspicion, or not prioritised as a right to be supported. There was evidence of some hospital settings welcoming advocacy support and working hard to proactively facilitate people’s access to advocacy and other instances where hospitals created barriers to effective advocacy support being available to the person. For example, the reviewers heard of instances where, by not ensuring information was shared with the person in a timely way, people didn’t get the support they needed to prepare for and attend meetings about their care, treatment or discharge. Reviewers heard many examples where advocacy was not welcomed or valued by the hospital. There is concern that this perpetuates the occurrence of closed cultures within institutional settings.”
There is also evidence that advocacy works well when there is a culture that values the inclusion of people’s voices, and champions person-led approaches. This provides important learning and should be considered for all commissioned mental health rehabilitation inpatient services.
9. Workforce
The GIRFT (2022) Mental health – rehabilitation national report highlights the need for good MDT working and the value of different roles as part of, and working with mental health rehabilitation inpatient clinical teams. It recognises the importance of investing in an appropriately skilled workforce, with a core rehabilitation training offer that includes trauma informed care.
Of the essential roles within this inpatient workforce, specific mental health rehabilitation training is currently only offered for psychiatrists and occupational therapists. All staff who work in mental health rehabilitation inpatient services require appropriate training, they need to be skilled and motivated, with a recovery focused approach embedded in their culture and values, including through diversity training.
Stakeholders describe positively experiences of different disciplines undertaking the role of the responsible clinician. For example, where a social worker is the responsible clinician, the approach is led with a social prescribing model. This contributes to enhanced personalisation as people engage in more community-based interventions that increase their social functioning and test relapse plans while having full access and support from the clinical team.
Stakeholders view experiences positively where the MDT includes or has access to skilled staff who deliver creative outlets including art and drama.
“I was studying art at university before becoming unwell. I am able to attend art and drama therapy which I find really helpful for me.”
Person in a mental health rehabilitation inpatient service.
Working towards a more competency-based workforce who recognise the value and benefits of substance misuse expertise, and housing and financial support is also seen as vital.
People, their families, carers and staff working in services describe the benefit of peer support workers who are part of the MDT. They highlight that this approach offers a unique type of support and that there should be more opportunities for people with lived experience to take on such roles. .
Some providers of mental health rehabilitation inpatient services partner with a VCFSE organisation to provide a varied and diverse inpatient MDT in terms of skills and experience. Roles undertaken by, or in partnership with VCFSE include peer support workers, pathway managers, family engagement workers, and housing and accommodation support workers. This approach is described positively, enabling shared learning and increased opportunities.
For a mental health rehabilitation inpatient service to thrive, stakeholders feel staff need to better know and understand the area they have chosen to work in. Equally staff should be representative of the local community. The GIRFT Mental health – rehabilitation national report states that mental health rehabilitation inpatient services should have the necessary numbers of permanent staff with the right experience, skills, training and development opportunities to support people sensitively and effectively.
“Staff who are redeployed to rehab wards because they might be injured, they don’t have the right skills.”
“We should have experienced staff who work in rehab all the time.”
“Staff can hold you back if they don’t know what is available in the community.”
People in mental health rehabilitation inpatient services.
10. Quality
The Commissioning framework for mental health inpatient services describes how services should be commissioned to achieve high quality, safe and effective mental health inpatient services. The ‘I and We’ statements from the framework, referenced in appendix 1, provide a ‘scaffold’ for the commissioning of all mental health inpatient services.
Fundamentally commissioners need to understand and recognise what good looks like for mental health rehabilitation inpatient services. This must be informed locally by people who access services, their families and carers, and those who work within and interface with these services. Ensuring this has been achieved and areas of improvement appropriately identified must be undertaken collaboratively with those who have direct, current and relevant experience of mental health rehabilitation inpatient services. This can be done by co-producing specific mental health rehabilitation patient, family and carer reported outcome and experience measures.
Applying specific local, co-produced standards and outcomes that relate directly to mental health rehabilitation inpatient services to the principles described in the overarching commissioning framework will enable these services to be commissioned safely and effectively.
Specific measures should include, for example, recording of progress against:
- the articulated purpose of admission
- estimated date of discharge and related length of stay
- access to the service, including waiting times for admission and discharge, and the reasons for any delays.
As explained in Section 3: Key messages of this guidance, robust data collection that is universally understood by all is vital to understanding mental health rehabilitation inpatient activity and flow. Commissioners must use data to drive up quality and improve outcomes for those who use services, their families and carers.
Commissioners should use existing levers and tools within contracts to support performance management and quality improvement; for example, compliance with mental health rehabilitation inpatient service specifications and adherence to nationally mandated standards. Commissioners should access and use all available information to understand the services that they commission and ensure they are safe, compliant, and provide high quality care and treatment. This information should include, but not be limited to:
- RCPsych relevant Quality Network peer review visits, reports and provider action plans
- CQC inspections and reports of organisations and specifically the mental health rehabilitation inpatient services, and provider action plans
- specifically for services where people are placed who have a mental health rehabilitation need and a learning disability or who are autistic, C(E)TR themes, and information collated through ‘sit and see’ 8-week visits (NHS England, 2023).
Appendix 1: ‘I and we’ statements
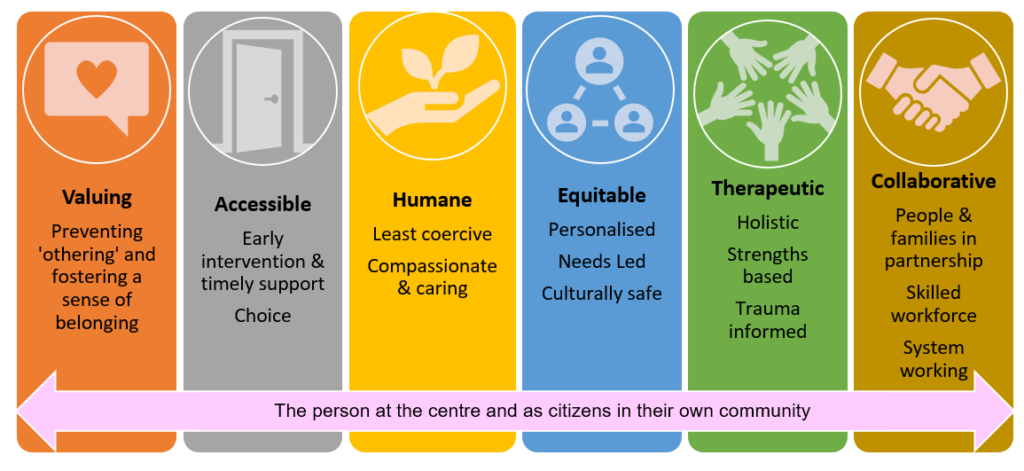
Image text:
- Valuing: preventing ‘othering’ and fostering a sense of belonging
- Accessible: early intervention and timely support. Choice
- Humane: Least coercive. Compassionate and caring
- Equitable: Personalised. Needs led. Culturally safe
- Therapeutic: Holistic. Strengths based. Trauma informed
- Collaborative: People and families in partnership. Skilled workforce. System working.
The person at the centre and as citizens in their own communities.
Valuing
I Statements
- I am valued as a person, and my individual needs and wishes are respected.
- I feel listened to and that my voice is heard.
- I have a sense of belonging and feel part of my own community.
We Statements
- We will ensure that the people who experience inpatient services and the staff who work within them, feel valued and cared for, benefitting from a culture that lives its values.
- We will work to ensure we can hear the voice of people who may need to call on mental health services and their families, we employ a range of communication methods to reflect individual preferences and needs.
- We will commission and provide services that are part of a local pathway of care which promotes inclusion, strengthens individuals’ rights, and is orientated towards citizenship.
- We will work with people in ways that prevent othering, foster a sense of belonging, reduce stigma, and enable people to maintain their social ties.
- We respect people as citizens and valued members of their community. We are here for all our people when they need us, irrespective of where they live, their background, age, ethnicity, sex, gender, sexuality, disability, or health conditions.
Accessible
I Statements
- I can access services based on my need and I do not feel excluded or stigmatised by my diagnosis.
We Statements
- We provide services that are needs led, accessible to all who need them, and are proactive in facilitating choice.
- We will ensure that admissions are appropriate, purposeful, therapeutic, and timely.
- We will employ interventions designed to avoid unnecessary admission to hospital, but when inpatient care is appropriate, it will not be impeded, nor regarded as the ‘last resort’.
Humane
I Statements
- I am first and foremost treated as a human being.
- I am cared for in an environment that is considerate of my individual strengths and needs.
- I am supported by staff who talk with me, not to me, using a way of communication that is preferred by me.
- I am supported to plan and prepare for important changes such as transitions between services, or discharge home.
We Statements
- We are unwavering in our commitment to commission inpatient services that are least restrictive and where people are not confined in conditions of greater security than required.
- We will plan discharge with each person at the very start of their admission, mitigating the risk of delays and ensuring that transitions between services are carefully considered.
- We are person-centred in our approach and staff are supported to respond to people’s distress with compassion.
- We will pay attention to our hospital environment and the impact it has on the wellbeing of people experiencing inpatient services and the staff working within them.
Equitable
I Statements
- I feel valued and respected for who I am.
- I can be myself around peers and staff.
- I am not discriminated against for who I am and the choices I make.
- I feel difference is understood, respected, and celebrated.
- I feel that my cultural needs and preferences are respected by all the staff who support me.
We Statements
- We will commission and deliver services where everyone counts, are treated with dignity and are safe. Where a person’s identity is not contested, their individuality is recognised and who they are and what they need is respected.
- We will work with people (and those who know and love them) to identify ‘what matters to them’ and make sure that the care they receive is personalised, needs led and respects their human rights.
- We will work with people to make sure we share decision making, acknowledging that even when people are acutely unwell, they are experts in their own lives and have valuable contributions to make about the support they need.
- We will be relentless in our pursuit to identify and address inequalities that exist within our local pathway. We are committed to ensuring everyone is valued irrespective of where they live, their background, age, ethnicity, sex, gender, sexuality, disability, or health conditions.
- We will strive to achieve parity of esteem, valuing mental health equally to physical heath, enabling people living with a mental health condition to have an equal chance of a long and fulfilling life.
- We ensure our environments are inclusive and accessible for everyone. We are thoughtful about people’s cultural needs and people with disabilities. We pay close attention to people’s individual sensory needs, particularly for autistic people and trauma survivors.
Therapeutic
I Statements
- I will be able to access a range of support that meets my need.
- I feel I have the time and space to form trusting relationships with the people involved in my care.
We Statements
- We know that therapeutic relationships are the strongest predictor of good clinical outcomes, so we will support staff to prioritise building relationships with people and enable continuity of care.
- We recognise that many people who are admitted to inpatient services will have experienced trauma at some point in their lives. Therefore, we will place emphasis on creating physical and emotional environments that promote feelings of safety and therapeutic relationships that are based on trust, respect, and compassion.
- We will invest in inpatient services that demonstrate a holistic, strengths based, integrated approach to care and make sure that mental and physical health conditions are considered, managed, and monitored.
- We will undertake assessments, interventions, and treatments that are evidence-based and delivered in a timely way.
- We are committed to delivering services that demonstrate therapeutic benefit. This includes continuous improvement of the inpatient pathway, co-producing service developments, making best use of data and using quality improvement methodology.
- We will develop a workforce that is in line with national workforce profiles and has the right skills and knowledge to ensure people have access to a full range of multi-disciplinary interventions and treatments.
Collaborative
I Statements
- I have a voice and I feel my views and choices are respected.
- I am able access independent advocacy if I want to.
- I can make use of peer support as I wish.
We Statements
- We respect the views and advanced choices of the people we serve and the contribution of people who know and care for them.
- We will invest in peer support and facilitate easy access to independent advocacy.
- We understand that safe and high quality inpatient mental health care relies on staff being able to ‘be with’ and work in partnership with people in a high state of distress. We will provide support for our staff to enable them to do this compassionately, safely, and respectfully.
- We are committed to providing the right resources for all our staff to ensure their time is protected to care, and that they can respond appropriately to the therapeutic aspects of their work.
- We will work in partnership across our system to ensure that locally, there is a range of services to support people within their local communities.
- We are committed to the working together so that no-one is inappropriately admitted to hospital or experiences a delayed discharge.
Support people as citizens
I Statements
- I am supported to access the things that matter to me.
- I feel my hopes, dreams, and plans for the future, are heard.
- I have a sense of belonging with the community I identify with.
We Statements
- We will actively work to promote the social inclusion of adults, children, and young people with mental health need.
- We will ensure that mental health services, by their design and activities, support the active participation of people in their local community.
- We respect everyone’s rights and responsibilities as citizens, supporting them to make real their hopes and aspirations, to contribute and to lead fulfilling lives.
Appendix 2: key resources
- Care Quality Commission (2017; updated May 2022) The state of care in mental health services 2014-201
- Department of Health and Social Care and Department for Education (2021) The national strategy for autistic children, young people and adults: 2021-2026
- Getting It Right First Time (2022) Mental health – Rehabilitation
- NHS England (2023) Acute inpatient mental health care for adults and older adults
- NHS England (2020) Advancing mental health equalities strategy
- NHS England (2019) The community mental health framework for adults and older adults
- NHS England (2018) Service specification: low secure mental health services
- NHS England (2018) Service specification: medium secure mental health services
- NHS England (2019) NHS Long Term Plan
- NHS England (2021) Monitoring the quality of care and safety for people with a learning disability and/ or autism
- NHS England (2022) 2023/24 Priorities and operational planning guidance
- NHS England (date) Commissioning framework for mental health inpatient services
- NHS England Rapid improvement guide: red to green bed days
- NICE (2020) NICE guideline [NG181] Rehabilitation for adults with complex psychosis
- NICE (2021) NICE guideline [NG197] Shared decision making
- RCPsych Mental health inpatient rehabilitation services typology table
- RCPsych Learning disability inpatient rehabilitation services
- RCPsych Rehabilitation services
- NHS England Care, Education and Treatment Reviews (CETRs)
- NHS England Personalised care and support planning
- NHS England (2023) Learning disability and autism – host commissioner guidance
- HM Prison and Probation Service (2011; last updated March 2023) Working with restricted patients
- Equality Act 2010
Appendix 3: acknowledgements
The input of stakeholders in many different ways has been considerable. The commitment and investment of time from those who commission, work in or with mental health rehabilitation inpatient services has been invaluable.
Particular acknowledgement must be given to the people in services, their families and carers who contributed, sharing their experiences, thoughts and ideas so openly and honestly.
The Mental Health Rehabilitation Inpatient Task and Finish Group has steered the development of the guidance:
Adult Mental Health Rehabilitation Inpatient Task and Finish Group Membership
- Sri Kalidindi (co-chair) – GIRFT and South London and Maudsley NHS Foundation Trust
- Louise Davies (co-chair) – Independent Expert Advisor – Commissioning
- Deb Moore – Mental Health, Learning Disability and Autism Quality Transformation Team, NHS England
- Tonita Whittier – Mental Health, Learning Disability and Autism Quality Transformation Team, NHS England
- Hirila Rose – Certitude London
- Jo Lomani – Mental Health, Learning Disability & Autism Quality Transformation Team, NHS England
- Di Domenico – Independent Expert Advisor – Commissioning
- Emily Williams – National Learning Disability and Autism Team, NHS England
- Roger Banks – National Learning Disability and Autism Team, NHS England
- Geoff Heyes – National Mental Health Team, NHS England
- Tristan Batten – Leeds and York Partnership NHS Foundation Trust
- Su Pashley – Norfolk and Suffolk NHS Foundation Trust
- Kate Oldfield – Rotherham, Doncaster, and South Humber NHS Foundation Trust
- Clair Haydon – Cheshire and Wirral Partnership NHS Foundation Trust
- Victoria Burns – Devon Partnership NHS Trust
- Keir Shillaker – West Yorkshire Health and Care Partnership ICB
- Dean Howells – Black Country Healthcare NHS Foundation Trust
- Mayura Deshpande – NHS England and Southern Health NHS Foundation Trust
- Kelly Fenton – Leicestershire Partnership NHS Trust
- Jenny Wilkes – Care Quality Commission
- Becs Daddow – National MH Specialised Commissioning Team, NHS England
- Thelma Goddard – National Learning Disability and Autism Team, NHS England
- Sheridan McKiniry – National Learning Disability and Autism Team, NHS England
- Ruth Davies – National Mental Health Team NHS
- EIan Davidson – GIRFT and Cheshire and Wirral Partnership NHS Foundation Trust
- Helen Souter – Mental Health Casework Section, His Majesty’s Prison and Probation Service
- Kathryn Nichols – Mental Health Casework Section, His Majesty’s Prison and Probation Service
Publication reference: PRN00771

