Summary
In 2019, the NHS Long Term Plan was published, together with the NHS Mental Health Implementation Plan, which set out ambitious, funded plans, to transform mental health services. Shortly after this, the COVID-19 pandemic began, which had a major impact across the health system, including mental health services. As a result of pandemic pressures and the increases in cost of living currently facing households, inpatient mental health services have experienced sustained rises in demand and acuity, which have been particularly challenging due to the current workforce pressures across the NHS.
While adult and older adult acute inpatient mental health teams continue to work hard to deliver high quality care in line with the commitments set out in the NHS Long Term Plan and NHS Mental Health Implementation Plan, feedback from those who work in and access these services indicates that while some people have positive experiences, others can experience issues accessing care that truly meets their needs and supports their recovery. This can include delays to accessing inpatient care and to being discharged, people being placed out of area where it can be challenging for friends and family to visit and disproportionate use of restrictive interventions. Furthermore, issues with the quality of care disproportionately affect certain groups of people, including people from ethnic minorities, people who have a learning disability, and autistic people.
It is vital that every person who needs acute inpatient mental health care receives timely access to high quality, therapeutic inpatient care, close to home and in the least restrictive setting possible. To support this, NHS England has produced this guidance to set out its vision for effective care in adult and older adult acute inpatient mental health services, together with resources and suggestions to support delivery. In this vision:
- Care is personalised to people’s individual needs, and mental health professionals work in partnership with people to provide choices about their care and treatment, and to reach shared decisions.
- Admissions are timely and purposeful – When a person requires care and treatment that can only be provided in a mental health inpatient setting and cannot be provided in the community, they receive prompt access to the best hospital provision available for their needs, which is close to home, so that they can maintain their support networks and community links. The purpose of the admission is clear to the person, their carers, the inpatient team and any supporting services.
- Hospital stays are therapeutic – People receive timely access to the assessments, interventions and treatments that they need, so that their time in hospital delivers therapeutic benefit. Care should be delivered in a therapeutic environment and in a way that is trauma-informed, working with people to understand any traumatic experiences they have had, and how these can be supported in hospital, in a way that minimises retraumatisation.
- Discharge is timely and effective – People are discharged to a less restrictive setting as soon as their purpose of admission is met and they no longer require care and treatment that can only be provided in hospital. For this to happen, there needs to be discharge planning from the very start of a person’s admission. There also needs to be a range of community support available and supported living options which meet different needs and enable people to maintain their wellbeing and live as independently as possible after discharge.
- Care is joined up across the health and care system – inpatient services work in a cohesive way with partner organisations, at admission, during a person’s inpatient stay and to support an effective discharge, so that people are supported to stay well when they leave hospital.
- Services actively identify and address inequalities that exist within their local inpatient pathway, in partnership with people from affected groups and communities. This must include ensuring that people are not prevented from accessing or receiving good quality acute mental health inpatient care simply because of a disability, diagnostic label or any other protected characteristic.
- Services grow and develop the acute inpatient mental health workforce in line with national workforce profiles, so that inpatient services can offer a full range of multi-disciplinary interventions and treatment. Staff wellbeing, training and development should be supported, so that inpatient services are a great place to work and staff are enabled to offer compassionate, high quality care.
- There is continuous improvement of the inpatient pathway – services strive to improve by making the best use of data, regularly developing, testing and refining change ideas using quality improvement methodology, and ensuring that service improvements are co-produced with people with experience of inpatient services and their carers.
We know that across the country there are services already delivering care that meets a number of these aims. With both the substantial investment in mental health services as part of the NHS Long Term Plan, the Government setting out its intention to reform the Mental Health Act (MHA) in the draft Mental Health Bill, and the recent establishment of NHS England’s Mental Health, Learning Disability and Autism Inpatient Quality Transformation Programme, now presents a significant opportunity to ensure that across all elements of this guidance, services are delivering care that is of a standard that we would all be proud of, and always puts people accessing services and those close to them at its heart.
Some perspectives on what good quality care means to people who have personal experience of acute mental health inpatient care, either directly or as a carer, are illustrated by these quotes:
“I would like to have staff on the ward who are compassionate and engaged, who understand my whole holistic and individual needs, and provide therapies and various activities that are meaningful, helpful, are of interest to me, and which feel comfortable for me to do. They should also help me to get better and plan my aftercare so that I can manage when I leave hospital.”
“For me, ideal inpatient care is when staff are willing to meet me and my loved ones where we are at each day, without expectations or demands. It’s about the service understanding how the small and large decisions that they make can impact my relative and her wider network, and the service being willing to work with us to identify and achieve the best outcomes for my relative, understanding that her needs change and fluctuate.”
“Co-production needs to be at the heart of inpatient care. I want to see clinicians and professionals working with me and my carers as equal partners, to develop, deliver and keep under review the best possible inpatient care for my needs. I want to see mental health inequality addressed, through people with lived experience supporting services to meet the needs of people from diverse communities.”
“If I need to be admitted, I would like inpatient care that is person-centred and provided in a recovery-focused environment. My admission should be as short as possible so as to not cause unnecessary trauma and there need to be more places that I can go to if I can’t go straight home when I’m ready to leave hospital. The power structures in inpatient settings also have to change, so that power is shared with people on the ward, particularly when they are from a marginalised group.”
Purpose of this guidance
This is the first time that NHS England has published national policy guidance outlining its vision for inpatient mental health care for adults and older adults, including people who also have dementia, an alcohol or drug problem, a learning disability, autism and any other individual needs. The guidance is intended to support integrated care systems (ICSs) and providers of mental health acute wards and psychiatric intensive care units (PICUs) to meet the ambitions for acute mental health care set out in the NHS Long Term Plan and NHS Mental Health Implementation Plan, alongside existing legislation and acute mental health standards (see Appendix 1).
It is hoped that this document will support partnership working between inpatient mental health services and crisis resolution home treatment teams (CRHTTs), community-based mental health and learning disability teams, and other services, including social care providers, local authorities, independent sector providers and voluntary, community and social enterprise (VCSE) sector organisations.
The guidance has been developed in partnership with frontline clinicians and people who have lived experience of accessing inpatient services, either directly or as a carer (see contributors to this guidance).
Key NHS Long Term Plan commitments for adult acute mental health inpatient services:
- Eliminate all inappropriate adult acute mental health out of area placements (a definition of these can be found on the FutureNHS platform (requires login).
- Improve the therapeutic offer from inpatient mental health services by enhancing access to therapeutic interventions and activities.
- Increase the level and mix of staff on acute mental health inpatient wards, including improving access to peer support workers, psychologists, occupational therapists, social workers, housing experts and other relevant professionals during admission.
- Reduce avoidable long lengths of stay in adult acute mental health inpatient settings (including for people with a learning disability and autism), so that people are not staying in hospital any longer than necessary.
- Reduce the number of people with a learning disability and autistic people in mental health inpatient settings, so that by March 2024, there are no more than 30 adults with a learning disability and/or autism in an inpatient setting, per one million adults.
- Ensure that all inpatient care commissioned by the NHS meets the Learning Disability Improvement Standards.
- Further information on several of these commitments can be found in the NHS Mental Health Implementation Plan 2019/20 – 2023/24. Across the delivery of all of these commitments, consideration must be given to reducing the associated inequalities, involving people in decisions about their care and adapting interventions and activities to meet individual needs and preferences.
Key elements of the inpatient pathway
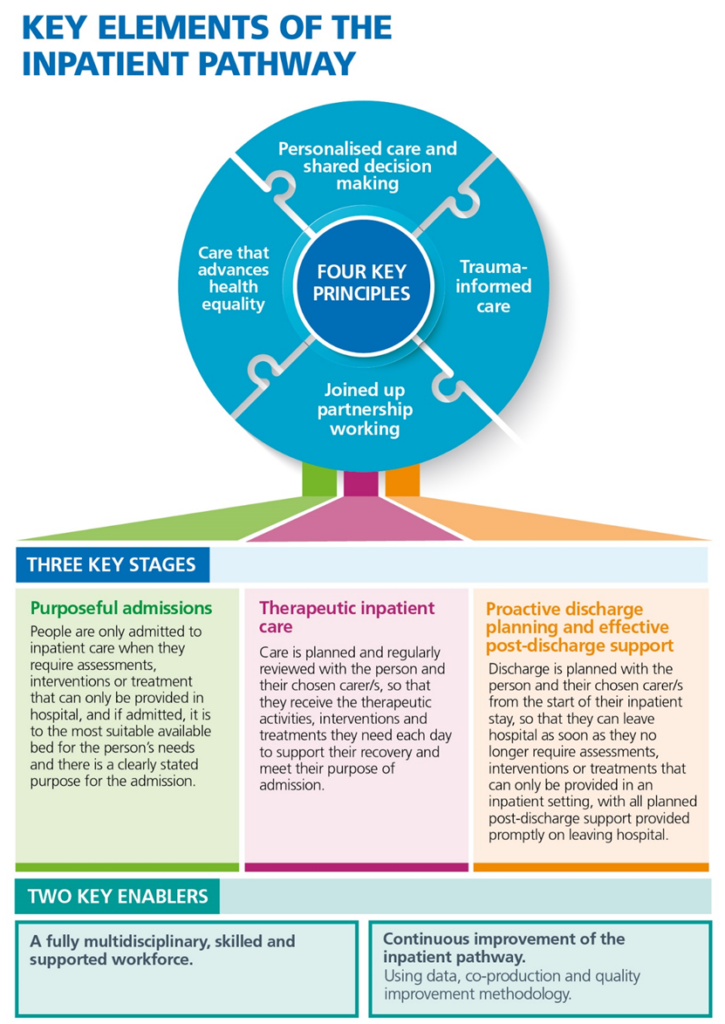
The diagram on the following page illustrates the key elements that underpin effective acute mental health inpatient care. It is made up of four key principles, three key stages and two key enablers.
The three key stages relate to pre-admission, during the hospital stay and discharge, while the four key principles and the two key enablers apply across the inpatient pathway. Below this diagram, there is also a brief memorandum of the key actions that need to be taken within 72 hours of a person’s admission to hospital. Further detail on each of the components of the diagram can be found in the sections of the guidance that follow; a summary is also provided in Appendix 2.
Key actions that need to have taken place within 72 hours of admission:
- Person’s electronic patient record (EPR) reviewed (including identifying any recorded advance choices and reasonable adjustments required); checking back key information from the person’s EPR with them and their chosen carer/s and noting any changes/updates.
- Holistic assessment completed and uploaded to the person’s EPR.
- Purpose of admission statement and estimated discharge date (EDD) agreed with the person and their chosen carer/s and uploaded to the person’s EPR.
- Interventions and treatment for physical and mental health conditions commenced/maintained, and a physical health check completed.
- Formulation review completed and care planning begun.
- Discharge planning begun – identifying what needs to happen for discharge to occur.
Please note, the term chosen carer/s is used throughout this guidance to indicate that the person should be able to choose who to involve in their care, which may include friends as well as family, and could change over time. For people detained under the MHA, there are additional processes related to a person’s Nearest Relative, which must be followed. (NB this may change if and when the draft Mental Health Bill is passed into law, including the term changing to Nominated Person.)
Principles of effective inpatient care
This section explains the four key principles that are at the heart of good inpatient care. These principles should underpin the delivery of care across a person’s entire experience of the inpatient pathway, which begins pre-admission and includes the planning and facilitation of access to effective post-discharge support. In addition to these principles, all services need to be delivered in line with other guidelines, care standards and legislation (see Appendix 1 for details), including the, Equality Act (2010), Human Rights Act (1998), Mental Health Units (Use of Force) Act (2018), the Mental Health Act (1983) (MHA) and the Mental Capacity Act (2005) (MCA).
Personalised care, including shared decision-making
Personalised care involves supporting a person in a way that takes account of their preferences, meets individual needs (including any reasonable adjustments required), enables the person to realise their aspirations, and draws on the person’s strengths. NHS England’s model for personalised care can be accessed on the NHS England website.
Delivering personalised care requires those providing inpatient mental health care to work as equal partners with the person and their chosen carer/s to reach shared decisions about the next steps in the person’s care. It also involves recognising that even when in crisis or acutely unwell, people are experts in their own lives and have valuable contributions to make about the support that they need both before, during and after their hospital stay. This approach to personalised care is illustrated in the extract below, which was developed by lived experience members of NHS England’s Adult Mental Health Advisory Network:
“…if we are going to truly change things for the better, we need to think about people as a whole – what makes up their lives, and their needs, wants and ambitions…These varied and personal needs must be reflected in the support and treatment we receive from public services too.
Here we should be striving for needs based, not diagnosis-based care and treatment…we also need to empower and enable clinicians to work with us to understand our needs as a whole person before agreeing a course of actions to keep us well. We need choice and to practice shared decision-making.” Published in the Department of Health and Social Care’s Mental Health and Wellbeing Plan: Discussion Paper.
Here are some steps that can be taken to support every person in inpatient settings to receive personalised care, which empowers them to make choices about their care and aids their recovery:
- Ensure that the assessment and care planning process is holistic (see further information in the care planning section and Appendix 3) and covers the person’s needs, strengths and aspirations. Assumptions about a person’s needs, preferences or abilities should not be made based on a disability, diagnostic label or protected characteristic.
- As far as possible, follow any advance choices that a person has made, which outline their preferences for future care and treatment. Any deviations from a person’s advance choices need to be clearly explained to the person and/or their chosen carer/s, and recorded.
- Ask the person who is best placed to act as their chosen carer/s and to contribute to discussions about their needs, wishes and aspirations – bearing in mind this may not always be a relative.
- Explore and record the person’s preferences as to what aspects of their care they would like their chosen carer/s involved and the types of information they would like to be shared with their chosen carer/s (and explain the circumstances in which their preferences may not be followed – see pages 78-82 of the MHA Code of Practice for further information (which includes information on confidentiality whether people are or are not detained in hospital)
- Check with the person’s chosen carer/s that they are comfortable taking on this role and provide them with information about sources of support for carers.
- In cases where a person does not want certain individuals (eg family members) involved in their care, or for information to be shared with them, this must be respected (within the limits of legislation – see link to the code of practice above for further information). However, these family members should still be given general information about what to expect from inpatient care and the opportunity to discuss their views about the person’s needs.
- Ask the person and their chosen carer/s about their communication preferences and identify how these preferences will be met while the person is in hospital, to ensure that people fully understand their rights (including rights under the MHA) and are able to play an active role in their care and discharge planning. For example, this may involve providing access to interpreters, providing information in a range of formats (eg in translation, large print, Braille and Easy Read format, using Augmentative and Alternative Communication, and using video clips and visual diagrams to aid understanding.
- Further information on the requirements for organisations providing NHS care and/or publicly-funded adult social care to make health and social care information accessible, can be found here: Accessible Information Standard.
- Make it part of ward practice to ask people their preferences, offer them choices about their care and treatment, and regularly check with the person about whether their current care plan is working for them. If the person says that further support is needed to help them to recover, take active steps to put this support in place. Where a person is detained under the MHA or lacks mental capacity to make specific decisions according to the MCA, it may be necessary to make some decisions on the person’s behalf, following processes in the relevant legislation. However, there should continue to be a focus on seeking to elicit people’s wishes and preferences and giving people as much choice as possible about their care and treatment.
- Make sure people have access to and are supported to meet with independent advocates (including as required under the MHA/MCA) and peer support workers/lived experience practitioners, with a diverse range of experiences and appropriate cultural competency. Ensure that people are aware that they can speak to advocates/peer support workers/lived experience practitioners to gain more information about their rights, how the mental health system works, and for support with communicating their needs, wishes and aspirations.
- Do not use blanket restrictions – rules that are applied to everyone regardless of individual risk. Decisions should be made on an individual basis as far as possible. Where there are limits imposed by national restrictions, organisational policy or individual risk assessments, staff members should creatively explore ways of meeting the person’s needs and wishes, while still adhering to policies and risk assessments.
The National Institute for Clinical Excellence (NICE) has produced useful guidance on shared decision-making and advocacy.
Care that advances health equality
The NHS is committed to ensuring that everyone receives high quality health care, regardless of their background. There is also a legal duty to advance equality, diversity and inclusion for everyone accessing health services, as laid out in the Equality Act, including meeting reasonable adjustments. NHS England has set out its plan to deliver more equitable access, experience and outcomes in mental health services in its Advancing Mental Health Equalities Strategy. As part of this, a Patient and Carer Race Equality Framework (PCREF), to improve experiences of mental health services among racialised and ethnically and culturally diverse communities, has been developed and is beingrolled out for implementation in 2023.
At present, there are significant health inequalities experienced by people in terms of their access to, experience of, and outcomes from acute inpatient mental health services and it is vital that action is taken at all levels to protect and advance health equality. A wide range of groups may experience inequalities in inpatient mental health services. ICSs and providers of inpatient mental health services are expected to use data and intelligence (including national data sets such as the National Mental Health, Dementia and Neurology Intelligence Network and the dashboards linked in this guidance, as well as local intelligence from people with lived experience and complaints data) to identify and monitor groups within their local population who have poorer access, experience, and outcomes from care. A co-production approach should be used to work with these communities to make tangible progress in reducing identified health inequalities.
To support progress in advancing health equality, the following sections provide some ideas on how to enhance the support that is provided to specific groups. These groups have been given additional focus in this guidance based on national-level evidence about the inequalities that they face and information available about some of the actions that can be taken to support these groups in inpatient mental health services. NHS England is however committed to developing further resources to support systems to address the wider inequalities that exist.
When reading the following information, it is important to recognise that people’s identities and experiences are multifaceted, and that being a member of multiple groups that experience inequalities may compound poorer experiences of care. Group-level considerations should therefore always be applied in the context of seeing and treating people as individuals, and working with people to put in place personalised care.
People from racialised and ethnic minority communities
People from racialised and ethnic minority backgrounds experience systemic barriers to accessing care and receiving inpatient support that meets their needs. In developing some suggestions to improve the care offered to people from racialised and ethnic minority communities, it is acknowledged that this term encompasses a wide range of people with very different cultural backgrounds and identities. These suggestions are therefore general, with the underpinning aim to centre care on people’s individual needs in relation to their race, ethnicity and culture:
- At admission, ask people and their chosen carer/s about how they understand their mental health condition, and plan with them how their cultural, religious, and spiritual needs (including associated dietary preferences) can be best supported while they are in hospital. Check in regularly to find out if these needs are being met.
- Provide key information in different languages and ensure ready access to independent interpreters (instead of relying on family members to translate).
- Provide access to culturally appropriate advocates and peer support workers/lived experience practitioners that reflect racialised and ethnic minority communities, as well as specialist input from VCSE sector organisations and faith-based groups.
- Ensure there are clear routes for reporting racism and discrimination, originating either other people on the ward or staff, as well as for accessing support when racist or discriminatory behaviour is experienced.
- Provide training to support staff to develop their cultural competency and the skills needed to plan and deliver care in a way that is culturally appropriate and does not make assumptions about people’s needs based on their appearance or characteristics.
- Monitor key metrics (eg length of stay, rates of detention) by ethnicity and collect feedback on people’s experiences of care and use this information to inform action to improve the cultural appropriateness of care.
- Embed the changes outlined in the Patient and Carer Race Equality Framework (PCREF) across all aspects of policy, procedure and practice.
People with a learning disability and autistic people
People with a learning disability and autistic people may experience inpatient care that is not adjusted to their needs and they are also disproportionately more likely to experience restrictive interventions while in hospital. For these reasons, the NHS Long Term Plan made a commitment to reduce the number of people with a learning disability and autistic people in mental health inpatient settings by the end of 2023/24 and work is also underway to reduce long-term segregation and restrictive practice.
To improve the support that people with a learning disability and autistic people receive:
- Ensure that people who are at risk of admission are included on local Dynamic Support Registers and that they have a Care (Education) and Treatment Review (C(E)TR) in the community pre-admission (or if this is not possible, within 28 days of admission) and that the findings of the C(E)TR inform care planning and delivery.
- Work with the person and their chosen carer/s to understand the person’s individual needs and traits, including those relating to communication, interaction, routine, repetition, predictability, food, the sensory environment and any activities or objects that will help their wellbeing. Identify and action the reasonable adjustments that are needed (working with specialist learning disability and autism professionals and other duly qualified professionals, as required) and record key preferences as an alert on the person’s EPR. If someone has a Hospital Passport, this should also be used to inform communication with the person and the support they are offered.
- (Particularly for autistic people) Make adaptations to the ward environment to create low sensory areas (eg using quiet door closers, replacing overhead fluorescent lights and fitting dimmer switches). See this resource pack from NHS England and these principles from the National Development Team for Inclusion (NDTi) for more information.
- Ensure that for all people aged up to 25 who have an Education, Health and Care (EHC) Plan, it is followed as far as possible during the person’s hospital admission and as part of discharge planning, and updated where necessary.
- Ensure all staff working in services registered with the CQC have attended mandatory training on learning disability and autism that is appropriate to their role, in line with the Health and Care Act (2022).
- (Particularly for autistic people) Use the Green Light Toolkit to regularly audit the service and use the toolkit’s resources to improve care for autistic people.
Useful resources include:
- NHS England’s Learning Disability Improvement Standards which support NHS trusts to measure and improve the quality of care they provide to people with a learning disability and autistic people.
- The Health Equality Framework, which supports services to measure their effectiveness in terms of addressing the inequalities experienced by people with a learning disability.
- The national service model for people with a learning disability and autistic people who display behaviour that challenges and guidance to support the implementation of the model.
People with a co-occurring alcohol and/or drug problem
Alcohol and drug dependence are common among people with mental health problems and are a significant factor in admission and prolonged length of hospital stay. In addition, people with co-occurring mental health and alcohol or drug use problems often experience poor health and earlier death. From 2009 to 2019, 47% of people in the UK who died by suicide and were in contact with mental health services, also had issues with alcohol dependency, and 37% with drug addiction. Services should act on the principles of ‘no wrong door’ and ‘everybody’s job’ so that people can access holistic care for both their mental health and alcohol/drug use problems, delivered by staff working in inpatient settings and/or in partnership with specialist addiction services. Here are some suggestions to support this:
- Work in partnership with community alcohol and drug treatment services to provide coordinated care and discharge planning. This may include embedding drug and alcohol workers and peer support workers/lived experience practitioners that have experience of alcohol and drug problems within inpatient teams.
- Screen all people for alcohol and drug use, using a recognised screening tool such as ASSIST-Lite.
- Train all ward staff in how to screen for drug and alcohol use, and to assess and identify alcohol and drug dependence, withdrawal symptoms, and associated acute health needs and risks, including increased risk of suicide.
- Where required, provide medically assisted withdrawal for alcohol or drug dependence and medication to avoid drug withdrawal (eg opioid substitution therapy), delivered promptly by staff with specialist addiction competencies.
- Deliver harm reduction interventions, including take home naloxone to reduce risk of overdose and referral for transient elastography to detect liver disease, to people who need them.
- Safely manage and monitor people who are acutely intoxicated on the ward, being cognisant of the increased risks of intoxication, while at the same time ensuring the person is not excluded.
- Ensure that all people with co-occurring alcohol and drug problems are able to access care in line with relevant clinical guidelines, including those from the NICE and Public Health England.
LGBT+ communities
LGBT+ people are more likely to develop mental health problems than non-LGBT+ people, including being more likely to develop depression and anxiety and being at higher risk of experiencing suicidal thoughts and engaging in suicidal behaviour and self-harm. The reasons why there are higher rates of mental health problems are complex, but one contributory factor is that LGBT+ people often experience prejudice and discrimination, which can also occur when they are in hospital. Some things that can improve the care that LGBT+ people receive in inpatient settings, include:
- Having clear posters and signage within services to show that they are LGBT+ friendly, to help create an open environment.
- Using inclusive language and not making assumptions about people’s relationships and gender (including assuming that the gender recorded in their medical record is correct). At admission, it is good practice to sensitively ask people about their sexual orientation and gender identity, and record their preferences (including what pronouns the person uses, which may vary depending on whether they are with family members, friends, with staff members or other people on the ward). The person’s name and pronouns should be respected, including managing this with other people on the ward.
- Identifying what support the person needs in relation to their sexual orientation and gender identity during their hospital stay. For example, this could include having access to peer support workers/lived experience practitioners that are LGBT+, linking people in to support from VCSE sector organisations, and ensuring continued access to gender affirming care (eg hormone replacement therapy, access to appropriate clothes and prostheses).
- Allocating trans individuals to the appropriate ward, in line with guidance on same-sex accommodation.
- Providing appropriate privacy for personal care and being aware of why this might be specifically important if the person is trans/non-binary/gender fluid.
- Being trauma-informed and aware of how someone’s sexual orientation or gender identity may have impacted on their mental health.
- Having clear procedures for responding appropriately to any reports of homophobic or transphobic abuse or sexual safety incidents.
- Providing training (eg ally training), which helps the inpatient team to understand the challenges that people who are LGBT+ experience within healthcare and society and how to ensure inpatient care is inclusive of LGBT+ people’s needs.
- Further information for healthcare professionals on providing inclusive care for LGBT+ individuals can be found in the ABC of LGBT+ Inclusive Communication.
Older adults and people with dementia
Older adults and people with dementia are particularly vulnerable to delirium, falls, poor nutrition and functional decline while in hospital, all of which can result in increased length of stay. This can be exacerbated by difficulties in identifying the required community-based support to enable timely discharge. For example, in 2021/22, length of hospital stay in older adult acute inpatient mental health services was around 80 days nationally compared to around 40 days in general adult acute services.
To support older adults and people with dementia effectively, ensure that there is:
- Engagement with the person’s chosen carer/s on admission and in all discussions about the person’s care and discharge. Carers can bring helpful insights about the person’s needs, for example, in relation to their daily routine, communication preferences, sensory needs, food preferences, and any activities or objects that will help the person’s wellbeing.
- A process in place to ensure that older adults with dementia arrive and leave hospital with their ‘This is me’ form; and that older adults living in a care home arrive and are discharged with their Red Bag; and that the information contained within these resources is used to tailor the person’s care to their needs.
- Access to all the items the person needs to improve their communication and independence, eg glasses, working hearing aids and walking aids.
- Specific focus placed on strengths, life goals and aspirations (including employment) when planning and delivering care, as these can be overlooked for older adults.
- Regular review of physical health conditions and medications, to ensure that the person’s physical health needs are met and are not impacting negatively on their mental health, and to check that any physical health medications are not interacting with the person’s mental state and with any psychotropic medications that the person is taking.
- Access to interventions and activities that take into account any physical or cognitive needs, including dementia.
- Early discussion about the intended discharge location with the person and their chosen carer/s. Online and printed information should be provided to support decision making if someone requires new accommodation or a placement, and proactive action taken to put this in place. For people with dementia, in particular, it can help if they are able to visit the intended discharge location prior to discharge if it is new to them, and discharges late in the day should be avoided, as this can increase disorientation.
- Access to specialist advice and support, eg geriatricians, palliative care, occupational therapists and physiotherapists (to aid rehabilitation), and social care staff (who can help to facilitate complex discharges).
- Appropriate signage, lighting, soft furnishings and flooring on the ward, to maximise independence for people with dementia. In addition, curtains should be closed in the evening as reflections in windows can be misinterpreted and cause distress.
There may be occasions, based on clinical judgement, when it is appropriate to admit an older adult to a general adult ward (eg because they are well known to staff there) or to admit a younger adult to an older adult ward (eg because of physical health issues such as incontinence issues that would be best managed there). Where an older adult is admitted to a general adult ward, their frailty and acuity should be considered in the risk assessment, and reasonable adjustments made. Adjustments should also be made when a younger adult is admitted to an older adult ward, to ensure the person receives care that is appropriate for their needs.
People who are given a diagnosis of ‘personality disorder’
People who are given a diagnosis of personality disorder have particularly poor experiences of inpatient care, including facing prejudices and assumptions about what is driving their distress, and potentially unsafe exclusionary practices. Some people given this diagnosis think that the personality disorder construct is inappropriately applied and feel that it overshadows and invalidates the real issues leading to distress, self-harm and suicidal ideation, and therefore the construct in itself causes further harm.
Some actions that can be taken to improve the care for people given a diagnosis of personality disorder are:
- Listening to how people describe and understand their distress, mirroring their language and offering care based around their mental health needs rather than diagnostic labels, in recognition that some people who are given a diagnosis of personality disorder do not agree with the construct.
- Recognising the role that trauma may have played in a person’s life and their current mental health needs, and seeking to understand how to support them best while they are in hospital, in a way that minimises triggers and retraumatisation. This will involve building therapeutic relationships, offering validating, compassionate support, and working with the person to understand their triggers and how to increase their sense of safety and control while in hospital. See the trauma-informed care section for further detail.
- Emphasising to people that they have a choice over the treatments and interventions they receive and that they can decline treatments if they do not want them (within the limits set out in the MHA and MCA).
- Ensuring staff working in inpatient settings have received training on personality disorders, co-delivered with people with lived experience of the diagnosis.
- Arranging for a trauma specialist and peer support worker/lived experience practitioner to meet people currently experiencing long hospital stays to identify what additional support the person needs to return home and stay well in the community.
- Ensuring that all care is delivered in line with NICE guidelines and quality standards, and that members of inpatient teams attend and apply Knowledge and Understanding Framework (KUF) training on the ward.
People admitted out of area
People that are placed in an inpatient service outside their local area have longer lengths of stay on average, poorer clinical outcomes (including increased risk of suicide) and poorer experience of care. This is often due to the negative impact of being out of area on the continuity of their care and reduced contact with people in their support network. When someone is placed out of area, the care they receive should be as close as possible to the care they would have received locally. This includes:
- The person’s named key worker staying in contact with the person and visiting the person in hospital as regularly as they would have if the person was in hospital in their local trust.
- The person receiving support to maintain regular contact with their chosen carer/s and support network. This must include funding the costs of transport and accommodation to facilitate visits, as well as supporting the use of technology to aid remote communication.
- Supporting the person, as far as possible, to engage in their usual activities and to maintain their responsibilities (eg the upkeep of their home).
- Peer support workers/lived experience practitioners from the person’s local trust keeping in regular contact (minimum weekly).
- The local hospital team maintaining involvement with the person’s care, with the aim of returning the person to their local hospital as soon as a bed becomes available, unless this would be disruptive and unhelpful to the person’s recovery.
When a person is admitted out of area, data must be flowed about the admission by the sending and receiving provider. Further information about how to do this can be found in this webinar. In addition, the FutureNHS platform (requires login) provides access to webinars held with NHS trusts that have had success in reducing the number of people placed of area, as well as the definition of an out of area placement, and details of continuity of care principles. ICSs are expected to monitor compliance with these principles where there is out of area bed use.
Trauma-informed care
Many adults and older adults accessing mental health services and particularly people requiring an inpatient admission, will have experienced trauma at some point in their lives. Furthermore, when people are admitted to hospital, and particularly when a person is detained under the MHA or is subject to a restrictive intervention, it is often accompanied by feelings of loss of power and control, and can be traumatic. It is therefore important that services work to ensure that the support that is offered in hospital is underpinned by a trauma-informed approach, both in terms of the way that care pathways are organised and how care is delivered.
Trauma-informed care first involves recognising that many people in contact with mental health services will have experienced trauma. Staff should talk to the person and their chosen carer/s to understand the role that trauma has played in a person’s life and how it is currently impacting their life and wellbeing. In discussing people’s life experiences and traumas with them, it is important to remember that for some people, asking them to recount their personal story and traumatic experiences, can in itself be retraumatising. Therefore, it is important to make use of what is already known and recorded about a person (eg in their EPR) and give the person choice about whether they wish to discuss these aspects of their life again.
To help restore feelings of control, active efforts should be made to give the person as much choice as possible while they are in hospital, and to work in close collaboration with the person, so that they are at the centre of their care planning. This should include gaining an understanding of how to support the person in a way that reduces the likelihood that they will be triggered or further traumatised by being in hospital, as well as coming to shared decisions with the person about whether they need specific support to help them process any traumatic experiences that they have had.
The physical and emotional environment on the ward should also promote feelings of safety and recovery and members of the inpatient team should work to build therapeutic relationships with people that are based on trust, respect and compassion. For this to happen, it is essential that there is a positive ward culture, where the use of restrictive interventions, including restraint and seclusion, is not seen as standard practice, and where restrictive interventions are used, it is as a last resort, proportionate to the situation and for the minimum time necessary. Managers should undertake regular reviews of practice, to ensure that where restrictive interventions are used, it is absolutely necessary and is applied proportionately.
Furthermore, in order that members of the inpatient team are able to promote positive ward cultures and build therapeutic relationships that keep individual stories at the heart of care delivery, it is essential that their own wellbeing is supported. Services should have processes in place, including reflective practice and supervision, which help team members to process their own thoughts, feelings and reactions to situations that have occurred on the ward, as well as any traumatic experiences they have had outside work (see the workforce section for further details).
The following links provide information to support services to transform the culture of inpatient wards to make them trauma-informed, both in terms of supporting people in a way that recognises and is responsive to the trauma that they may have previously experienced, and in terms of helping to ensure that inpatient care does not itself unintentionally lead to people experiencing new traumas (for example, as a result of inappropriate and disproportionate use of a restrictive intervention):
- Central and North West London NHS Foundation Trust’s webpages on trauma-informed approaches.
- The Power Threat Meaning Framework, developed by a network within the Division of Clinical Psychology at the British Psychological Society, which can be used to support a trauma-informed understanding of human distress.
- The Centre for Mental Health and the Mental Health Foundation’s guide to providing effective trauma-informed care for women.
- Surrey and Borders NHS Foundation Trust’s trauma-informed care toolkit for carers, which has a specific focus on people with a learning disability, as well as these webpages from The Challenging Behaviour Foundation on trauma support for people with a learning disability.
- The Reducing Restrictive Practice Collaborative, Restraint Reduction Network and Safewards project (see also Safewards Victoria) webpages, which provide practical information on interventions that can support reductions in conflict and restrictive practice on wards.
- NHS England’s webpages on reducing long term segregation and restrictive practice for people with a learning disability and autistic people, who disproportionately experience these practices. This details information on a number of initiatives including Independent Care (Education) and Treatment Reviews, the HOPE(S) model and the Senior Intervenors Project.
- The Sexual Safety Collaborative – includes guidance and ideas for changing practice to improve sexual safety in inpatient mental health settings.
- Guidance from the Department of Health and Social Care setting out the measures that NHS hospitals and independent hospital providing NHS-funded care must take as part of the Mental Health (Use of Force) Act (2018) to prevent inappropriate use of force in mental health units, including training requirements for staff.
Joined up partnership working
Inpatient services that work closely with a range of other services (see box below for examples) in a collaborative and coordinated way, are more likely to meet people’s varied needs, contributing to improved experiences and outcomes from care and reducing avoidable time spent in hospital. It is particularly important that where someone is transferred from another service, for example, children and young people’s mental health services, that there is strong coordination of care, so that the transition is as supportive as possible.
As part of the initial assessment and admissions process, it is important to read the person’s EPR to identify who they currently receive support from and which services they are in contact with, and to check this back with the person and their chosen carer/s. Resources such as the Circles of Support can be used to help identify the key individuals, communities and services in a person’s life.
It is also important to find out and record people’s preferences about what types of information is shared with the people and services that support them and how they would like them involved in their inpatient care and discharge. The circumstances in which these preferences may not be followed should be explained (see pages 78-82 of the MHA Code of Practice (which includes information on confidentiality whether people are or are not detained in hospital). Where people require reasonable adjustments or have additional needs that fall outside the remit of inpatient mental health services, expertise may need to be sought from specialist services (eg learning disability, autism, drug and alcohol teams). Commissioning arrangements should enable easy referral and responsive input from such teams.
Many people who are admitted to hospital will already be in contact with a community-based mental health or learning disability team and have a named key worker. On admission, anyone without a named key worker should be assigned one within 72 hours, wherever possible. Key workers should maintain contact with the person while they are in hospital and pass on any information that is useful for the person’s care, to help avoid the person having to undergo repeat assessments and retell their story, which can be frustrating and trigger past traumas. The key worker should also work closely with the inpatient team, CRHTT, and any other key services or parties, to identify and put in place the support that the person will need to be discharged and to maintain their wellbeing in the community (including working with local authorities to plan Section 117 aftercare, where applicable). It is important that this is done early and in partnership with other services so that the person’s discharge from hospital to the community is as smooth as possible.
Here are some actions that can be taken to embed effective partnership working:
- Ensure there are clear pathways between services (eg between physical health and mental health services) and joint working arrangements are agreed with partner organisations, which include information on the management of transitions (eg from children and young people’s inpatient services to adult inpatient services).
- Review the inpatient mental health pathway to understand how partnership working is currently functioning and how to strengthen it. For example, this could involve senior system partners and lived experience practitioners coming together on a quarterly basis to review performance data and local intelligence, assess where there are pressures across the pathway and identify actions to drive improvement.
- Integrate members of key partners organisations, for example, social workers and housing officers, as part of the ward team’s staffing establishment.
- Ensure cross-service attendance at key meetings (eg care planning and discharge meetings, and other reviews). This should include representatives from the local CRHTT, the person’s named key worker from the community-based mental health or learning disability team and any other key partners in the person’s care (see box below for examples), as well as anyone that the person and their chosen carer/s feel it would be helpful to have in these meetings.
- Hold joint training between services that work with one another, where relevant, to understand the types of expertise that different services and professionals offer, as well as to reflect on and improve joint working processes. As an example, this could be used to share reflections about what more could be done to avoid escalation to admission, or to identify situations in which people are better cared for in the community.
- Develop clear escalation protocols with cross-agency partners, which set out when and how to raise issues to senior managers – the protocols should clearly identify where senior responsibility sits along with contact details to enable timely escalation to occur. Escalation protocols should exist for occasions when there are long waits in A&E, challenges in locating inpatient provision for urgent admissions, and delayed discharges from hospital. These protocols should be developed and maintained by the ICS, with input and agreement from NHS mental health providers and relevant partners included in the box below, who are key to the operation of the local pathway. More information about Section 140 compliant escalation protocols is set out in this section of the guidance.
Key services for effective partnership working in inpatient mental health care
Please note, this is not intended to be exhaustive.
- CRHTTs
- Community-based mental health teams
- A&E, psychiatric liaison and diversion services
- Primary care
- Pharmacy services
- Services addressing sexual health and physical health needs (including community health, intermediate care and frailty services for older adults)
- Children and young people’s mental health services
- Community learning disability services and specialist autism services
- Gender identity services
- Drug and alcohol services
- Specialist trauma services
- Local authorities, in particular, Approved Mental Health Professional (AMHP) services, expert housing teams, and children and adult social care teams, including safeguarding specialists and those responsible for conducting needs assessments and arranging Section 117 aftercare (in partnership with integrated care boards (ICBs)
- Housing services (offering home adaptations and short- and long-term housing options)
- Rehabilitation services providing advice and specialist intervention
- Carers support services
- Financial support services providing advice on benefits and funding of ongoing care
- Employment support services
- Education services – including schools and further and higher education providers
- Criminal justice agencies, including probation and the police
- Independent sector providers (especially where people are placed in a non-NHS inpatient service)
- VCSE sector organisations providing advocacy services, peer support, community crisis alternatives, and in-reach services for specific groups, including people from racialised and ethnic minority communities.
Effective care across the inpatient pathway
For people to have the best recovery possible, they need to receive effective care from pre-admission, during their hospital stay and after discharge. This includes ensuring:
- Admissions are purposeful – people are only admitted to inpatient care when they require assessments, interventions or treatment that can only be provided in hospital, and if admitted, it is to the most suitable inpatient service provision available for the person’s needs and there is a clearly stated purpose for the admission.
- Their inpatient care delivers therapeutic benefit – care is planned and regularly reviewed with the person and their chosen carer/s, so that they receive the therapeutic activities, interventions and treatments they need each day to support their recovery and meet their purpose of admission.
- Their discharge is proactively planned and effective – the person’s discharge is planned with them and their chosen carer/s from the start of their inpatient stay, so that they can leave hospital as soon as they no longer require assessments, interventions or treatments that can only be provided in an inpatient setting, with all planned post-discharge support provided promptly on leaving hospital.
The sub-sections that follow explain each of these stages of the inpatient journey in more detail.
Purposeful admissions
Ensuring that people are only admitted to inpatient care when they require assessments, interventions or treatment that can only be provided in hospital, and if admitted, it is to the most suitable available inpatient service provision for the person’s needs, and there is a clearly stated purpose for the admission.
Deciding whether an inpatient admission is required, or the person could be supported through a less restrictive community-based acute care model
When people are in crisis, they require prompt access to the right support, in the best setting for their needs. For people with a learning disability and autistic people, a C(E)TR should normally take place pre-admission, in line with current policy, to understand the person’s needs and determine if they could be met in the community or whether they require an inpatient admission. For people who do not have a learning disability or autism, a holistic face-to-face assessment (see Appendix 3) should be conducted to understand the person’s care needs and preferences in relation to treatment.
This assessment should include identifying who the person’s chosen carer/s are and what their views are about the person’s care. To avoid the person needing to retell their story, the person’s EPR should be reviewed at the earliest opportunity, ideally prior to their initial assessment, to gather information from any prior assessments and care plans and to identify any advance choices. This information should be checked back with the person and their chosen carer/s in case there have been changes.
Based on the assessment and taking the person’s wishes into consideration as far as possible, a decision should be made about whether it would be better for the person to be admitted to hospital (including admission under the MHA) or whether it would be better for the person to be supported in the community. This may through support from a community-based acute mental health service, such as a CRHTT, acute day service or crisis house, or an intensive support team, for people with a learning disability (examples of community-based alternatives to inpatient care can be found in the case studies section on the FutureNHS platform (requires login). Given that long lengths of stay in hospital can in themselves be harmful, decision-making needs to explicitly consider whether a hospital admission is essential because the person requires assessments, interventions and/or treatment that can only be provided in hospital and could not be delivered through community-based acute services.
Though it will not always be the case, often receiving care and treatment at home or in a less restrictive community setting can lead to a better experience of care because it means that the person can more easily maintain existing routines, access to their usual support network and can stay in a more familiar location. This is illustrated in the extract below from someone who experienced a mental health crisis:
“Fortunately, one nurse who was caring for me went above and beyond to see that I was not admitted. He talked to my wife, who deemed it would be better for me to be cared for at home. No one else did this or took it upon themselves to find out my background and what happened that brought me to this point. The nurse was persistent with their encouragement and support and fought long and hard to ensure the wrong decisions were not made. I even remember him challenging the doctor who wanted to admit me… All these things had a huge impact on my recovery and eventually helped me to start caring for myself again.”
There are two main models used by providers to assess whether an inpatient admission is required, or the person could be supported through a community-based acute model:
- CRHTTs conducting all assessments for acute care, because of their expertise in knowing the care and treatment options available locally, including community-based acute care and inpatient care.
- A trusted assessor model in which CRHTTs are responsible for conducting most acute care assessments (eg those that come in via referrals to the CRHTT or the single point of access), but other teams, eg psychiatric liaison and community-based mental health teams, may complete assessments and CRHTTs then base decision-making about the most appropriate care option on this assessment and do not have to see the person face-to-face.
Regardless of which model is used, it is important that:
- Repeat assessments by different services are reduced wherever possible, as well as the need for people to wait for teams to arrive to conduct assessments.
- CRHTT clinicians are empowered to lead decision-making, working in close partnership with the person and their chosen carer/s and partner services, whose expertise may be useful to reach decisions about the most appropriate care setting. For example, involving AMHPs early on in the assessment process can support consideration of less restrictive alternatives to detaining people under the MHA. To help partnership working in relation to deciding the most appropriate care setting:
- There should be a policy setting out roles and responsibilities in relation to crisis and acute assessments, which provides details of inpatient and community-based acute services available locally, together with key referral information.
- There should be regular reviews of need versus capacity across the different inpatient and community-based acute services available locally, to ensure the system is set up to meet the current population need.
- CRHTTs, psychiatric liaison teams, inpatient teams and AMHP services should aim to operate as part of one wider team, communicating regularly in relation to team capacity and presentations in the community and A&E. This helps to build relationships and trust and enables more informed decision-making around the most appropriate care setting.
- Where someone needs to be assessed under the MHA, there should be clear protocols in place locally for securing the necessary input from Section 12 approved doctors and an AMHP in a timely way, and ensuring all key information is communicated to support the assessment.
- All services involved in conducting assessments (including CRHTTs, psychiatric liaison services and AMHPs) that feed into decisions around admission, meet regularly to share feedback and to address issues, so that all parties have confidence that admission decisions are being made appropriately, consistently and in people’s best interests.
- There is senior clinical oversight to check that there is clarity and consistency around decision-making in relation to whether people receive community-based acute care or are admitted to hospital.
Agreeing a purpose of admission
When it is judged that an inpatient admission is required, the reasons identified for this should be formalised in a purpose of admission statement, which clearly articulates why an inpatient stay is needed and the aims of the admission (see box below for example statements). Evidence from local quality improvement initiatives has shown that when a purpose of admission is recorded, it reduces the risk of people staying in hospital longer than needed. Furthermore, the intended reforms to the MHA, outlined in the draft Mental Health Bill, include new detention criteria requiring admissions to provide therapeutic benefit. By recording a purpose of admission, it helps to ensure that the inpatient team is clear on the therapeutic benefit that an admission should achieve and can work with the person, their chosen carer/s and any relevant partner services to achieve it.
Formalising a purpose of admission should be done for each person admitted to hospital, regardless of the time of day or who is doing the assessment, and should follow a consistent process that is established by the provider (eg incorporating it into initial assessment forms). It should be uploaded to the person’s EPR, together with an EDD. The purpose of admission and the EDD should also be shared with the person, and where appropriate, with their chosen carer/s and relevant partner services.
| Examples of good (*) and poor quality (×) purpose of admission statements |
| * Ayele, who is being supported by the Early Intervention in Psychosis service, is having a relapse in the community following a breakup with her partner, and has stopped taking her clozapine medication. It is known that re-starting Ayele on medication at home will not be successful and therefore hospital admission will be used to identify why she stopped taking the clozapine medication, including whether any aspects of her care plan need changing to address the reasons identified. One thing that Ayele mentioned at admission was feeling lonely so her ongoing care plan will need to include support in helping her to address this. EDD: 14 days. * Krish has been receiving treatment for a diagnosis of bipolar disorder from a community mental health team, alongside support from his local drug treatment service. He was doing well with managing his bipolar and drug use, until the death of his uncle. On Friday, he attended the local A&E, having made a serious attempt to take his own life. He had not taken his daily medication for more than four days. An admission is required to re-establish his medication and to understand what would help him to manage his bereavement. This support will then be put in place as part of his ongoing care plan. EDD: 21 days. * Reggie has recently become homeless and has been brought to a health-based place of safety by the police, because he was displaying a high level of mental distress in public. He is not known to mental health services. Reggie has been assessed as requiring admission under Section 2 of the MHA. Admission will be used to assess his mental state and identify his strengths, needs and aspirations, including how he usually manages in his day to day life, why he became homeless and what factors contributed to his mental health crisis. This will inform his ongoing care plan, including setting out which pharmacological, psychological, social and practical interventions are required to support Reggie’s recovery in the community. EDD: 21 days. × Mike required admission under Section 3 of the MHA. EDD: unknown. × Aarvi has been admitted to maintain their safety. EDD: Will be discharged once risk assessment shows it is safe to discharge Aarvi. |
Arranging prompt access to the most suitable hospital provision for the person’s needs
It is expected that when someone requires an admission, they will receive prompt access to the most suitable inpatient service that is available for their needs and begin receiving inpatient support as swiftly as possible. If someone is experiencing an unacceptably long wait for an inpatient bed and this has not been resolved through routine processes such as bed management meetings, then system-wide escalation protocols should be followed. These escalation protocols should be developed and shared with multi-agency partners (eg local authority, police and A&E departments) and must be compliant with Section 140 of the MHA, which is a duty on local NHS commissioning bodies to provide every local social service authority with a list of hospitals that can receive urgent mental health admissions, and enable applications under the MHA, if necessary. On a regular basis, including after an escalation protocol has been activated, multi-agency reviews should take place to help identify what more can be done to unlock capacity across the system and help ensure that people can access inpatient mental health services in a timely way when they need them.
Other than in exceptional circumstances, it is usually best for people to be admitted to their local acute inpatient mental health service, so that they can more easily maintain contact with friends, family and local community care teams. There are a small number of circumstances in which it is appropriate to admit someone out of area who requires a non-specialist acute mental health admission. These are:
- personal choice
- an emergency admission (eg where someone is visiting or on holiday in another area of the country)
- safeguarding concerns if the person was to be placed in their local hospital
- the person being a member of staff at the local trust.
Where one of these reasons applies, admission to a non-local hospital should be facilitated.
Where someone is admitted out of area and none of these reasons apply (ie it is an inappropriate out of area admission), this should be communicated to the senior responsible clinicians within the local provided, and the good practice suggestions provided earlier in this document should be followed. Furthermore, as soon as clinically appropriate, the person should be transferred back to their local hospital, unless there is a good reason not to (eg it will disrupt the person’s continuity of care, or the person wants to remain in the current hospital setting).
Therapeutic inpatient care
Care is planned and regularly reviewed with the person and their chosen carer/s so that they receive the therapeutic activities, interventions and treatments they need each day to support their recovery and meet their purpose of admission. Purposeful care in a therapeutic environment supports people to get better more quickly and reduces avoidable time spent in hospital.
Once a person has been admitted to hospital, they should receive care that delivers therapeutic benefit throughout their inpatient stay. This section of the guidance covers some of the key areas that acute mental health services should focus on to deliver high quality, therapeutic inpatient care.
Care formulation and planning
To understand and plan the support and interventions that an individual needs to meet their purpose of admission and to receive therapeutic inpatient care, a formulation review should take place within 72 hours of admission. The purpose of this formulation review is to build on information from the person’s EPR, including any prior assessments, existing care plans and recorded advance choices, to develop a holistic and compassionate understanding of the individual. This includes their current experiences and difficulties, what led to their admission and the reasons behind why they are showing signs of mental distress (including any current or past trauma). The formulation review should also look at the person’s treatment and support preferences, what they want their recovery to look like, their strengths, and any protective factors (eg supportive relationships, activities, and routines) that will help them to get better.
Building on the formulation process, a care plan should be co-produced with the person and their chosen carer/s (please note, it will be a statutory requirement for people detained under the MHA to have a Care and Treatment Plan, if and when the draft Mental Health Bill is passed into law). The care plan should include information on the assessments, interventions and activities that will be delivered while the person is in hospital and any considerations in terms of the way that the support is delivered. As part of early discharge planning, the care plan should also include information on what support will be needed after discharge (including housing and social care) to support the person’s recovery and maintain and improve their longer-term wellbeing. See the Discharge section for further details.
To ensure that everyone is clear on the actions that will support the person’s recovery and their role in delivering this, the written care plan should be uploaded to the person’s EPR and shared with the person, and where appropriate, their chosen carer/s and any other relevant parties. The copy that is shared should be in a format that is accessible (eg free of acronyms and jargon), and where required, provided in alternative formats, such as in translation.
Both formulation and care planning work best when it is a collaborative process between the person, their chosen carer/s, the inpatient multi-disciplinary team (MDT) and representatives from partner services who know the person well and are involved in supporting the person (eg the person’s named key worker, housing officer or advocate). An atmosphere of shared learning should be created, with equal value placed on the perspectives of each person involved. For some services, co-producing care plans will involve a shift in the way that teams usually work, to one in which the power to make decisions is shared with the person and their chosen carer/s.
In some cases, the person may not be ready or able to be fully involved in co-producing their formulation review or care plan, particularly at the start of their admission. In these instances, it is still important that the inpatient team listens to the person, offers the person choices and seeks to find out their needs and preferences, drawing on information including from their chosen carer/s, named key worker and EPR. As soon as it is possible, it is vital that the inpatient team engages the person fully in co-producing and refining their care plan. Where there are reasons that care cannot be delivered in line with the person or their chosen carer/s preferences, this should be clearly explained to them, recorded in the person’s EPR and revisited at a later stage, wherever possible.
Delivering therapeutic activities and interventions
In line with their purpose of admission and care plan, each person should receive access to the assessments, activities, interventions and treatment that they need, which aid their recovery and improve their ability to respond to future crises. The additional funding allocated to therapeutic inpatient care through the NHS Long Term Plan is intended to support providers to achieve this, particularly through increasing the number of therapeutic staff in inpatient settings, including occupational therapists, peer support workers and psychologists, who can support the delivery of a range of activities and interventions.
Interventions
As part of person-centred care planning, the evidence-based interventions that the person will receive in hospital should be agreed with the person and their chosen carer/s. These interventions should meet the person’s holistic needs (pharmacological, psychological, social and practical), and be delivered in a way that is culturally appropriate and adjusted to meet individual needs. For example, for people with a learning disability and autistic people, this could include providing one-to-one support to enable participation.
The range of interventions that should be offered on wards, and delivered to people based on their individual needs and care plans, includes:
- Physical health support
- On admission, any known physical health conditions should be identified, and any existing treatment/management plan should be continued in hospital (appropriate advice should be sought if any changes are needed).
- A physical health check should be completed within 72 hours of admission. This should consider height and weight, heart rate and blood pressure, blood glucose and lipid profile, the physical effects of medication, sexual health, use of cigarettes, alcohol and drugs, and any other areas depending on clinical need (without rescreening for conditions that are already known and which the person is receiving treatment for). Assessments should be optional (except where clinically necessary), the reasons for doing them clearly explained, and they should be conducted sensitively to avoid discomfort and distress.
- A physical health plan should be developed with the person and their chosen carer/s based on the physical health check. This may cover diet and exercise, treatment to manage long-term conditions (eg diabetes, cardiovascular disease), sexual health, smoking cessation, and alcohol and drug use (including detox and managing withdrawal).
- Psychotherapy – people’s need for psychology input, including ongoing therapy when the person leaves hospital, should be assessed as part of care and discharge planning. This guide from the Association of Clinical Psychologists and the British Psychological Society provides useful information on psychology input across the acute mental health pathway, while this quality statement from NICE provides specific information in relation to psychological interventions for people with a learning disability.
- Relapse prevention – individual or group support, particularly for people who are approaching discharge, to help establish strategies for managing their physical and mental health after leaving hospital (including identifying individual triggers and early warning signs of worsening mental health, and how to manage these) as well as to plan their daily routine and identify personal goals for after discharge.
- Medication – regular medication reviews (every 2-3 days) should take place throughout a person’s admission, which involve working collaboratively with the person to consider medication type, dosage, interactions and side effects. These resources from NHS England on STOMP (Stopping over medication of people with psychotropic medications) can help services to reduce the overuse of psychotropic medication for people with a learning disability and autistic people.
- Peer/lived experience support – group or individual support, provided by peer support workers/lived experience practitioners, with a diverse range of experiences (eg in terms of cultural background, age, diagnosis).
- Education and employment support – considering support to access training, higher and further education, apprenticeships and paid and voluntary work.
- Financial support – including use of the Breathing Space debt relief scheme and guidance on benefits and funding of ongoing care.
- Housing support – for example, this could involve meeting with an in-reach housing officer to discuss accommodation options post-discharge, if the person is not able to return to where they were living pre-admission.
- Specialist support and interventions to meet individual needs, particularly for groups that experience inequalities within the local acute pathway. These may be delivered through VCSE sector services.
Activities
To supplement these interventions, there should be a programme of activities and groups that help to improve people’s physical and mental wellbeing. These activities and groups should run daily on each ward, including at weekends and in the evenings.
The types of activities and groups available should be co-produced with people who are currently on the ward and people who have used inpatient services, to suit a variety of interests and needs. There should be age-appropriate and single sex activities offered, and a focus on ensuring that activities are culturally appropriate and appropriately adapted to meet the needs of groups that are identified as experiencing health inequalities. Providers may wish to commission VCSE sector services to support these aims.
It is important that while encouraging participation in activities and interventions, individuals are both given the choice to decline taking part, based on their interests and what they think will be of therapeutic benefit to them. Equally, people should not be denied access to therapeutic activities and interventions based on a disability, diagnostic label or another protected characteristic, including inappropriate judgements about the likely effectiveness of an intervention based on any characteristic.
Examples of the types of activities and groups that may be offered are as follows (this is not intended to be exhaustive):
- Daily ward meetings that are run in partnership with people on the ward and allow people to share their ideas and input into decisions about the running of the ward.
- Daily exercise, fitness classes and other activities that keep people active, eg dance, walking groups, yoga.
- Gardening groups and other activities providing access to the outdoors.
- Life skills groups, which may cover areas such as communication skills, developing positive relationships, diet and healthy eating, money management, sleep hygiene, stress management, and using digital technology.
- Creative activities, eg arts and crafts, music.
- Contact with animals, eg bringing pets onto wards.
- Religious or spiritual groups, including opportunities for prayer and to celebrate festivals.
- Relaxation groups, eg aromatherapy, massage, reflexology.
The Star Wards website contains additional information about many of these and other therapeutic activities, and how to deliver them.
In addition to the activities and interventions above, each person should receive support to help stay connected to friends and family and regular one-to-one contact with a named contact within the inpatient team (or another member of the inpatient team that they have developed rapport with). This helps to ensure that there is a consistent person on the ward that the person can share their feelings and experiences with.
Systems should also ensure that special consideration is given to supporting any dependants under 18 years old and that there is good provision of support for carers, including access to group psychoeducation (see NICE guidance) and support for their wellbeing and wider needs. This may be offered through local carers’ support services, and where needed, through arranging a carer’s assessment. Further information about good practice in terms of involving carers in a person’s support can be found in The Triangle of Care Guide to Best Practice in Mental Health Care in England. This resource includes a self-assessment tool, which services can use to assess how well they are working with carers and where improvements could be made.
Using the Red to Green approach
The Red to Green approach is a helpful tool that can be used to support the allocation of tasks that are needed to deliver a person’s care plan (including ensuring that people receive the activities and interventions they need to recover), and to facilitate a timely and successful discharge from hospital. Under this approach, a ‘red day’ is recorded when a person receives little or no value-adding care, while a ‘green day’ is recorded where a person receives purposeful care that progresses their recovery and path to leaving hospital. Further detail on what constitutes a red and green day is as follows:
- A red day should be recorded if any of the following criteria are met:
- The person is receiving care that could be provided in a non-acute inpatient setting.
- There are delays to discharging someone or transferring their care to a more appropriate service.
- The person does not receive active care or treatment that day.
- Requested or planned assessments, interventions or treatments are not delivered.
- The person is on leave without a clear timeframe or rationale for what the leave is intended to achieve.
- A green day does not mean the person is ready for discharge, it means that they are receiving the care and treatment that they need to progress their recovery and there are no barriers or delays to them accessing this support. A green day can only be recorded if all of these criteria are met.
- The person is receiving care that can only be provided in an acute inpatient setting.
- The person receives value-adding care that day, eg assessments, interventions or treatment that supports their recovery and path towards discharge.
- All care that is planned or requested is completed by the end of the day.
The Red to Green approach is centred around daily MDT board rounds, in which the status of each person on the ward is rapidly reviewed and tasks assigned that will support the person’s recovery and path towards discharge. An example of the steps that may be followed as part of the Red to Green approach can be found in Appendix 4.
Where the Red to Green approach is used, a central database should be kept of the number of red days and the causes of these red days, including delays to receiving therapeutic treatment and being discharged. This information should be reviewed regularly and openly, including by members of senior management, to understand and address common causes of red days. While external delays tend to be well recorded, this process can help to identify the source of internal delays, which local clinical and operational teams can address through escalating internally and through co-production and quality improvement projects.
Details about how Cheshire and Wirral Partnership NHS Foundation Trust have used the Red to Green approach to improve patient flow, can be found in this poster and video.
Reviewing and updating care plans
As well as daily reviews as part of the Red to Green approach, there should also be frequent care plan reviews with the person and their chosen carer/s, with input from relevant members of the MDT and partner services. The focus of these reviews should be to find out how the person and their chosen carer/s feel about the support that is being provided, ensure that the person is receiving purposeful and therapeutic care (ie the assessments, interventions and treatment they need) and if not, to update the person’s care plan and ensure the right support is put in place. Where care has not progressed as agreed, it is important to acknowledge this and explain the actions that are being taken to address this.
These reviews are also a good opportunity to check and update the person’s purpose of admission and discuss when the person is expected to leave hospital (their EDD), including checking with the person and their chosen carer/s about whether there have been any changes in the support that the person needs in order to be practically and emotionally ready to leave hospital.
In addition, for people with a learning disability and autistic people, commissioners are required to undertake regular face-to-face monitoring visits every eight weeks for adults that are in an inpatient setting, and on a six weekly basis for young adults aged up to 25, who have an EHC Plan.
Meeting the purpose of admission
If a Red to Green or care planning review shows that the purpose of admission is close to being met and/or the person will soon no longer need care that can only be provided in hospital (for example, they could leave hospital with support from a CRHTT), additional focus should be given to planning their discharge and post-discharge support.
The therapeutic environment
The final aspect of therapeutic inpatient care is ensuring that the environment in which care is delivered is conducive to recovery. By making the ward environment feel safe, inviting and accessible, including to people who require reasonable adjustments, for example as a result of a physical disability, learning disability and autism, it helps people to feel cared about and to have a better experience of being in hospital, which in turn enables recovery.
The suggestions given below for improving the inpatient environment draw on work undertaken by the Mental Health Team at NHS England, the Star Wards project, the work of the NDTi, who developed ten principles for ‘Sensory Friendly Wards’, and the Autism Team at NHS England who developed this Sensory-Friendly Resource Pack. As some of the work on sensory friendly wards has the potential to improve the experience of people in inpatient settings, regardless of whether they have sensory differences or not, they have been adapted for inclusion here. Please note, the points below should be read in conjunction with the Health Building Note for adult acute mental health units.
Involvement
- Involve people (both current inpatients and people with recent experience of inpatient care) in reviewing the ward environment and work with them using a co-production approach to improve the therapeutic spaces. This should involve reviewing the kitchen areas, canteen and the quality of food provision, including whether it meets dietary requirements and cultural and sensory needs. Information to support reviews of the environment can be found on the Patient-Led Assessment of the Care Environment website.
- Identify, as part of care planning, what will help the person feel as comfortable as possible during their hospital stay. This may include having access to their favourite possessions, and items that help the person to relax or engage with their hobbies (as well as a safe place, such as a locker, to store their belongings). It is important to conduct risk assessments around personal items, but all requests should be considered on an individual basis and blanket bans (eg due to fire regulations or infection control) should be avoided as far as possible.
Meeting sensory and cognitive needs
- Change fluorescent lighting for alternatives, such as halogen or ‘warm white’ light emitting diodes (LEDs), and make sure lighting does not buzz or flicker. See these resources from NDTi for further information on sensory friendly LED lighting.
- Identify ways to reduce noise on the ward, for example by using soft furnishings, acoustic vinyl flooring, sound absorbing panels and soft door closers and giving people access to noise cancelling headphones. Ward alarms can be swapped for ‘silent’ alarms that significantly reduce noise on the ward, while still alerting staff.
- Neutralise smells where possible, for example, from cleaning and laundry products, other people and food. Ways to do this include using unscented cleaning products, supporting people to choose their own laundry products, masking unwanted smells using preferred scents and shutting doors around mealtimes. However, for people with dementia, it can be helpful to have food smells on the ward as it acts as a cue that it is mealtime; decisions around how to manage this need to consider and balance the varied needs of people on a ward.
- Ensure there is clear signage on wards, eg using contrasting colours, clear typeface and incorporating visual cues or symbols, that aids comprehension among people with varied needs. Examples of clear signage developed for people with dementia can be found on the Alzheimer’s Society website.
Attractive and engaging shared spaces
- Provide information and leaflets about the ward and local and national resources, for example via a resource table or wall.
- Ensure everyone has access to quiet space (eg a relaxation or sensory room), space for prayer, and outdoor space, at all times of day. Other spaces that can enhance the inpatient environment include sensory gardens, gyms, music rooms, computer rooms and libraries, and having spaces where people can cook or prepare their own food.
- Make sure there are comfortable seats and dining chairs for all people on the ward to use.
- Address any damage to the ward environment (eg graffiti, broken windows) and repair or replace any damaged items promptly (ideally within days, wherever possible).
- Make the environment as homely as possible, for example by providing board games, televisions (more than one so that there is a choice of programmes), laptops, books and magazines (in different languages), and by playing soft music (or making headphones available) to people on the ward.
- Consider how the décor could be improved using artwork, cushions, indoor plants and by painting the walls.
- Make the visitor room inviting, for example using artwork and having games and magazines available.
Ensuring privacy, dignity and safety
- NHS England has made a national commitment to end the use of dormitories in mental health facilitates, supported by capital funding that will continue in 2023/24. This will mean that soon all people in inpatient settings will have access to their own bedroom and many more people will have access to their own ensuite.
- Ensure that there are suitable facilities for people in line with NHS England’s guidance on same-sex accommodation.
- Address all safety issues that pose immediate risks to people, including ligature points and other infrastructure concerns. To support this, capital funding was made available in 2022/23 to support urgent safety projects.
- Use the practices and interventions developed as part of the Reducing Restrictive Practice Collaborative and Safewards project (see also Safewards Victoria), and resources from the Restraint Reduction Network to support reductions in conflict and restrictive practice on wards.
- Use the guidance and resources that the National Collaborating Centre for Mental Health developed as part of the Sexual Safety Collaborative to improve sexual safety on wards.
It should also be noted that all NHS mental health trusts are now smoke-free environments. While there are challenges with implementing this in inpatient mental health settings, smoking is one of the biggest drivers of years of life lost in people with mental health needs. Therefore, reducing the amount that people smoke while on the ward, preventing people from taking up smoking and inhaling secondhand smoke, and supporting people to give up smoking while in inpatient services, has the potential to deliver significant health benefits.
Currently, tobacco dependency treatment services are being rolled out to inpatient mental health settings, with an ambition that everyone who smokes and is admitted to hospital overnight will be able to access treatment for their tobacco dependence. Systems are targeting services to those with the greatest need, which is anticipated to encompass all mental health inpatient services. Where services are commissioned, this should also include step down care post-discharge, which could include commissioned services in specialist community mental health settings. Providers should also reach a position on the use of vaping devices on hospital premises, noting that an evidence review published by the Office for Health Improvement and Disparities found that vaping devices are effective in supporting people to stop smoking, but are not completely harm-free. People who have never smoked should be discouraged from using them.
Effective discharge planning and post-discharge support
The person’s discharge is planned with the person and their chosen carer/s from the start of their inpatient stay, so that they can leave hospital as soon as they no longer require assessments, interventions or treatments that can only be provided in an inpatient setting, with all planned post-discharge support provided promptly on leaving hospital.
There has been a significant focus on timely and effective discharges from acute inpatient mental health settings in recent years. The is because staying in hospital for longer than necessary can be harmful for people, so the aim is for people to only spend as long in hospital as needed to receive the therapeutic interventions and treatment that they require. For this model to work, there needs to be an active focus on delivering therapeutic care in inpatient settings (as outlined in the previous section) and on identifying what needs to be put in place for a person to be practically and psychologically ready for discharge. There also needs to be a range of community support services and housing provision available that can facilitate discharge and support people to continue their recovery, meet their personal goals and maintain their wellbeing once they leave hospital.
Some people with lived experience and their carers have said that they do not like the term ‘discharge’ as it conveys a sudden ending, and one in which they feel they may be left without the support they need. This may lead to some people feeling reluctant about being discharged from hospital. As the term discharge is used widely across the health sector, it is used throughout the guidance. However, the expectation in this guidance is that when someone is discharged from inpatient mental health services, they will receive a follow-up within 72 hours of leaving hospital, they may receive support from the local CRHTT to leave hospital, and they will receive ongoing support from a community-based mental health or learning disability team and potentially other support services (further information is provided in this section). To ensure the right support is in place when the person is ready to leave hospital and the transition from hospital to home is smooth and coordinated, the person’s discharge plan should be developed with the person and their chosen carer/s from the start of their inpatient stay.
When to discharge someone
In this section a distinction is made between the point at which a person is ‘clinically ready for discharge’ (CRFD) and the actual point at which it is possible to discharge the person (ie when the ongoing care and treatment that they need in the community or less restrictive setting is also available).
Clinically ready for discharge
The point at which someone is CRFD is reached when: the MDT conclude that the person does not require any further assessments, interventions and/or treatments, which can only be provided in an inpatient setting.
There are three key criteria, which need to be met, before the MDT can make this decision:
- There must be a clear plan for the ongoing care and support that the person requires after discharge, which covers their pharmacological, psychological, physical health, social, cultural, housing and financial needs, and any other individual needs or wishes.
- The MDT must have explicitly considered the person and their chosen carer/s’ views and needs about discharge and involved them in co-developing a discharge plan.
- The MDT must have involved any services external to the provider in their decision-making, where these services will play a key role in the person’s ongoing care, eg social care teams and housing teams.
A webinar providing further information on the definition of CRFD can be found on the FutureNHS platform (requires login).
There may be occasions where the MDT are not able to reach a consensus that someone is CRFD or partner services may not agree with the MDT’s decision. All providers should have a rapid escalation process in place that can be followed in such cases. There may also be situations where the person or their chosen carer/s do not think the person is ready for discharge. In these cases, it is important to take the time to understand the reasons for this, identify alternative solutions and take any further steps needed to make sure the person feels ready for discharge. For example, this could include visiting the proposed discharge location and meeting the staff there. If not resolved, the rapid escalation process should be followed and this process should be clearly explained to the person and their chosen carer/s.
The point at which it is possible to discharge
Once the CRFD definition is met, it should be recorded as such in EPR systems. However, it does not necessarily mean the person can be discharged, for example, if the right support is not available in the community at that time.
The point at which it is possible to discharge someone is reached when the person is considered CRFD and the ongoing care and support agreed in the person’s discharge plan can be delivered according to the agreed timescales following discharge. To make this decision, the person’s discharge plan needs to have been reviewed and updated with the person and their chosen carer/s, and the role of each party in providing post-discharge support clearly articulated. For example, it should be clear what assessments, interventions and support will be provided by the CRHTT, community-based mental health or learning disability team and other services, and when; and what the person and their chosen carer/s are responsible for, checking in particular that the person’s chosen carer/s feel able to take on these responsibilities.
In situations where someone is deemed CRFD, but it is not possible to discharge them, the person must continue receiving interventions, activities and other support in hospital, so that they remain CRFD and can be discharged as soon as the appropriate support has been put in place for them.
Once the final decision has been made that it is possible to discharge someone:
- At least 48 hours’ notice of this discharge date should be given to the person, their chosen carer/s and any services (both NHS and non-NHS services) that will be involved in the person’s ongoing care.
- Their risk assessment should be updated, to include information on how any risks to self or others will be managed in the community or less restrictive discharge location. In line with NICE guidance on self-harm, risk assessment tools and scales should not be used to predict future suicide or repetition of self-harm, or to decide who should be discharged. Instead, person-centered approaches to safety planning should be used that involve the person and their nominated carer/s and consider individual needs, risks and contexts and personal feelings of safety. Once updated, the risk assessment should be uploaded to a clearly accessible place on the person’s EPR.
- A face-to-face follow-up meeting should be arranged for within 72 hours of discharge (see details below).
- The person should be given clear information about how to access crisis support after discharge, both during and outside standard working hours. This should include providing direct contact details for the CRHTT.
- Relevant information relating to the person’s discharge, which may include a copy of their discharge plan, should be shared with services that will be involved with the person’s ongoing care and treatment after discharge. The person’s discharge summary should also be shared with the person’s GP and other relevant parties, where appropriate, within a week of discharge.
Support after discharge
When someone leaves adult acute mental health inpatient care, they should receive:
1. A follow-up within 72 hours of discharge
Every person discharged from an adult mental health inpatient service (excluding specialised services commissioned by NHS England) should be followed-up by a CRHTT or community-based mental health team within 72 hours. This is because the National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) has found that there is an increased risk of dying by suicide within three days of discharge from hospital. Follow-ups should be arranged pre-discharge (including providing written details of when, where and who the follow-up will take place with) and should take place face-to-face wherever possible. If the follow-up indicates that the person needs additional support, action should be taken promptly to put this in place. Resources to support effective 72 hour follow-ups can be found on the FutureNHS platform (requires login).
2. Prompt access to planned support
In the majority of cases, people are expected to return to their home or alternative accommodation in the community when they are discharged from hospital, with any further assessments and ongoing, interventions, treatment and support that they require provided in their home or local community. Services need to work together to make the transition from hospital to home as joined up as possible, with the support outlined in the person’s discharge plan provided according to agreed timelines.
Support from NHS mental health services
When a person is discharged, they may receive short-term intensive home treatment from a CRHTT to facilitate discharge, and it is expected that they will receive ongoing support from a community-based mental health team. Support should commence within the timescales stated in the person’s discharge plan (in the case of discharge supported by a CRHTT, a first visit should happen within 24 hours of discharge).
If not already included in a person’s discharge plan or EPR, the CRHTT and/or the community-based mental health team are expected to support the person to:
- Develop advance choices, which set out any preferences that the person has for their care and treatment, should they be admitted to an inpatient mental health setting again. This may involve signposting the person to access additional support from an advocate or a VCSE organisation, which can help with the development of advance choices. Advance choices should be recorded and uploaded to a clearly accessible place in the person’s EPR.
- Create a crisis plan that is uploaded to the person’s EPR, containing information about the signs that the person is experiencing or approaching a crisis, where and how they can seek help (including outside standard working hours), and information on their support and treatment preferences.
- Access other support that will help maintain the person’s wellbeing and prevent future crises, such as psychoeducation and peer support.
Support from other services
According to people’s needs, as agreed in a person’s discharge plan, some people may receive additional support from services such as drug and alcohol services, community learning disability teams, palliative care, housing services, social care services, specialist autism services and VCSE sector services.
Funded packages of care
A smaller proportion of people may require and be entitled to a funded care package, in order that they can access:
- Support for social care needs (including domiciliary care).
- Community-based rehabilitation.
- A short-term placement in a step-down service or supported accommodation.
- A longer-term/permanent placement in a supported accommodation or residential care home.
This may be funded via:
- Section 117 aftercare – available to people who have been detained under section 3, 37, 47, 48 or 45A, or have been placed on a community treatment order (CTO) or conditional discharge. If someone is entitled to Section 117 aftercare, notification of their admission should be made to the local authority.
- The Better Care Fund
- Personal budgets (which are local authority funded), personal health budgets (which are NHS funded) and integrated personal budgets and personal health budgets (which include funding from both a local authority and the NHS). These budgets are intended to give people greater choice and flexibility in organising and managing their own care, in line with an agreed care plan. Please note, people eligible for after care services under Section 117 of the MHA have a right to a personal health budget; further details can be found in NHS England’s Personal Health Budget Quality Framework. It is important that those eligible are informed of this right.
- NHS Continuing Healthcare
- NHS trust discharge initiatives – which may fund home adaptations, equipment and short-term placements.
Members of inpatient teams and independent advocates should make people aware of the different options for funding ongoing care (including personal budgets), and where there are different options available, individuals and their chosen carer/s should be supported to understand how the different options work, so that they can make the best choice for their circumstances (particularly where a person will be self-funding their care).
Local protocols should be developed and agreed between NHS organisations, local authorities and other relevant partners, which detail the escalation process that should be followed where there are difficulties reaching an agreement about funding ongoing care. These escalation protocols should include information on arrangements for putting in place interim funding to enable people to leave hospital when clinically ready, and details of the procedures for agreeing longer-term funding, which ensure that no one is left without the support at the end of the interim funding period. Where local escalation protocols are activated, this should be clearly communicated to the person and their chosen carer/s and they should be involved in conversations about progress to resolve the situation and next steps.
Considerations for an effective discharge
The following can support effective discharges from hospital:
1. Commission robust community and housing support
NHS bodies and local authorities need to commission effectively so that there is the required housing and health and social care support available in the community to meet the needs of the local community and enable people to be discharged. This includes commissioning step-down services, which provide a bridge between inpatient care and living independently in the community, and services that meet the needs of specific populations that experience health inequalities within the local pathway.
Resources to support this include:
- this resource pack (requires login) produced by NHS England and partners, including the Local Government Association and the Association of Directors of Adult Social Services (ADASS). The pack includes information on funding opportunities and good practice examples relating to mental health accommodation-based support.
- the national Building the Right Support plan to develop community services and close inpatient facilities for people with a learning disability and/or autistic people who display behaviour that challenges, and the accompanying Building the Right Home guidance for commissioners.
2. Plan early and throughout a person’s inpatient stay
Discharge planning should begin at the start of a person’s admission, or a soon as practically possible afterwards. In line with Section 91 of the Health and Care Act (2022), discharge planning should involve the person and their chosen carer/s. It should also involve any services that may be involved in a person’s care after discharge, including social care. As part of discharge planning, it is important to identify early what needs to happen for the person to feel practically and psychologically ready for discharge (while recognising that this may change over the course of the person’s time in hospital). The person and their chosen carer/s should be given information about their discharge options, the opportunity to ask questions about these options and should be involved in co-developing a discharge plan.
Some key areas that should be proactively considered and addressed as part of discharge planning, include:
- Understanding what the person’s chosen carer/s are able and willing to do once the person they care for is discharged (eg whether they are happy for the person to live with them) and what support the chosen carer/s needs to be able to fulfil this role. This is particularly important when considering young carers and people with other caring responsibilities. Where a carer’s assessment is needed, this should be organised with the relevant local authority in a timely way so as to not delay discharge. Alternatively, the assessment may be completed after discharge, as long as it is not a new caring duty or there are increased care needs.
- Housing – assessing whether the person can return to the place they lived before they were admitted to hospital, and if so, what steps need to take place to make this possible (eg securing their tenancy, making any repairs or adaptations). If it is no longer possible or suitable for the person to live there, then prompt contact and referral should be made to the local authority housing services (including the homelessness team if the person is homeless or at risk of homelessness) and proactive action taken to secure a suitable home that meets the person’s individual needs (including preferences in terms of location). In some cases, step-down accommodation may be arranged ahead of permanent accommodation being identified.
- Funded packages of care – identifying any care needs that may require ongoing support within the home, in sheltered accommodation or a care home. This is particularly relevant in relation to older adults, who have longer lengths of hospital stay on average, which can be the result of delays in securing appropriate social care. Once ongoing care and support needs are identified, referral should be made promptly to the relevant agency (eg the local authority) and assessments should be arranged early, so that funding can be agreed and a package of support can be put in place as soon as the person is ready to leave hospital. Where someone is entitled to Section 117 aftercare, there should be early liaison with the local authority to begin planning the aftercare that is needed.
- Mental capacity and liberty protection safeguards for people who lack mental capacity and meet the criteria for being deprived of liberty.
- Medicines and equipment – some medicines, eg opiate substitutes, need to be arranged well in advance of discharge to avoid delays to discharge.
- Travel home/to the discharge location – especially if this is in a rural location. Travel may be through a carer picking the person up, a VCSE sector service, or where relevant eligibility criteria are met, via non-emergency patient transport services. Consideration should also be given to whether a person needs to be accompanied and who can do this, if a carer is not available.
- Immediate needs at the point of discharge, eg completing deep cleans of the person’s home, having keys to gain access, food, electricity and gas, and any other ‘settle in’ support required.
For people with a learning disability and autistic people, the 12-point discharge plan, which can be found in Appendix 7 of the Dynamic Support Register and Care (Education) and Treatment Review policy should be used to ensure appropriate steps are in place to support a timely discharge. Systems are expected to use this plan, and this will be monitored via the Assuring Transformation dataset.
3. Develop strong partnerships locally
Strong partnerships should be built between inpatient services and NHS and non-NHS services that need to be routinely involved in discharge planning, decision-making and providing post-discharge support. This includes CRHTTs, community-based mental health and learning disability teams, social services (who can provide expertise about people’s longer-term care needs and options and support shared decision-making by making sure that people and their chosen carer/s are aware of the implications of the options), housing services and VCSE organisations (who may provide discharge support services such as settle in support or peer support). Examples of other services that will need to be a key part of discharge processes, depending on individual circumstances and needs, can be found in this section.
To support partnership working, there should be policies outlining roles and responsibilities in relation to discharge planning discharge decision-making and providing post-discharge support, which include a named person responsible for discharge process in each organisation.
4. Arrange leave to prepare people for discharge
Arranging leave (including Section 17 leave for people detained under the MHA) can help the person and the inpatient team decide if the person is ready for discharge and gives the person the opportunity to make any preparations needed for leaving hospital (eg preparing their home). The period of leave should be short-term, and if it goes well, discharge should be promptly facilitated.
5. Keep a consistent focus on inpatient flow
Providers that have had success in ensuring timely discharges, consistently report that executive or senior leadership oversight of patient flow along the inpatient pathway has been key to this success. Some of the actions taken to support patient flow and discharge from hospital include:
- Using the Red to Green approach – see this section for details.
- Enabling discharge seven days a week, by having consultant cover at weekends or using criteria-led/nurse-led discharge.
- Holding operational meetings multiple times a week to look across the system at who is expected to be admitted, and discharged and planning for this accordingly. This should include regular meetings (weekly or more frequently) with system partners to unblock delays to discharge.
- Focusing on people who have been in hospital for more than 60 days to identify what needs to happen to discharge them. Some providers have ‘long stay’ or discharge teams who specifically look at this.
- Using Multi-Agency Discharge Events where there are complex discharges requiring agreement across multiple partners, and also following locally agreed escalation procedures where there are concerns about delayed discharges. Where escalation has been required, this should be reviewed to understand what could have been done differently.
- Using hospital performance data, eg length of hospital stay, number of people CRFD who have not been discharged, reasons for delayed discharges and reasons for readmission within six months, in order to monitor the effectiveness of local discharge arrangements and identify improvements.
Key enablers of effective inpatient care
There are a wide range of enablers operating both within and outside the hospital setting that can help to support the delivery of good quality inpatient care. The enablers included in this section are:
- having a fully multi-disciplinary, skilled and supported workforce, and
- continual improvement of the inpatient pathway through using data, co-production and quality improvement methodology.
These were selected as they are both key to facilitating the delivery of care in line with the principles and stages included in this guidance.
A fully multi-disciplinary, skilled and supported workforce
For people accessing acute mental health services to receive caring and compassionate support, which meets people’s holistic needs and delivers therapeutic benefit, it is essential that inpatient teams are appropriately skilled are well supported, and include staff from a range of different professional groups. Additional funding has been made available as part of the NHS Long Term Plan to improve staffing levels and skills mix in adult acute inpatient mental health settings, though workforce submissions show that at a national-level, this has not resulted in the expected workforce growth. Though there are currently significant workforce pressures, particularly in mental health, it is vital that efforts are made to strengthen the inpatient workforce. The subsections that follow provide guidance to support this, and should guide decisions about how the NHS Long Term Plan funding for acute inpatient mental health services is used.
Staffing levels
Staffing levels have a critical impact on people’s experience of inpatient care, for example, affecting the activities and interventions that are on offer and whether people can leave the hospital grounds. It is therefore crucial that inpatient services have sufficient staffing levels and there is not an over-reliance on temporary staff, which impacts on the ability for people to build up a relationship with the inpatient staffing team. Recommended full-time equivalents (FTEs) for different staffing groups are not included in this guidance, because determining the right staffing model for a given population involves assessing a range of local factors and no single model will be applicable to all areas. However, in line with the fundamental safer staffing principles set out in the National Quality Board’s guidance, and Developing Workforce Safeguards Guidance, all staffing establishments should be reviewed biannually using a triangulated approach, utilising evidence-based workforce planning tools, professional judgement of the clinical team, review of quality and safety outcomes, and benchmarking with peers. The validated, evidence-based workforce planning tool for inpatient mental health services is the Mental Health Optimal Staffing Tool. The tool is free for NHS trusts in England to use and can be licensed via https://www.innovahealthtec.com. Further resources from NHS England on safe staffing in mental health services can be accessed on the NHS England website.
Multi-disciplinary inpatient teams
There is growing evidence of the importance of having inpatient teams made up of varied staffing groups. For example, analysis by NHS Benchmarking has indicated that there may be a relationship between therapeutic staffing mix and length of stay on wards.
Using the funding made available for acute inpatient mental care as part of the NHS Long Term Plan, there is a real opportunity to increase the variety of roles represented in ward teams or with dedicated ward time. This includes, but is not limited to, roles such as occupational therapists, peer support workers/lived experience practitioners, psychology professionals (including clinical associates), activity coordinators, housing officers and social workers.
Providers should work with people and carers of people who have used local inpatient services, and members of inpatient teams, to identify which staffing models will best meet the needs of the local community. This may include looking at how to ensure the NHS Workforce Race Equality Standard is being met and that the workforce is representative of the population it serves, and how to increase the representation of therapeutic roles on wards in the evenings and at weekends. In seeking to achieve this second aim, it should be recognised that this may take long-term planning and require innovative approaches, such as employing people to work across inpatient and community settings and recruiting to new roles like clinical associate psychologists.
For a team to be truly multi-disciplinary, it is critical for a culture to be created where the value of different professions and perspectives is recognised, and the sharing of skills and expertise is actively encouraged. People in leadership roles are particularly important for setting this culture. They can do this through prioritising training or reflective practice that promotes a shared understanding of different roles, ensuring all key decision-making meetings are multi-disciplinary, and facilitating interactions in a way that demonstrates that different opinions and expertise are valued. In particular, supporting non-medical professionals (including lived experience practitioners/peer support workers) to take up leadership positions can help to embed a truly multi-disciplinary approach. This includes supporting non-medical professionals to take up roles as Responsible Clinicians and consultants, as well as senior leadership positions within providers.
Details of the additional workforce required by each ICS to deliver the NHS Long Term Plan ambitions for therapeutic inpatient care, as well as the funding allocated to each clinical commissioning group (CCG)/ICS between 2019/20 and 2023/24 to support this, can be found on the FutureNHS platform (requires login). Any skill mix change or introduction of new roles must be supported by a Quality Impact Assessment (QIA) to assess and mitigate against any potential impact on quality. This should be signed off by the Chief Nurse and Medical Director and include clear monitoring arrangements.
Skills and competencies
This guidance does not aim to offer a comprehensive list of skills and competencies for staff working in acute inpatient mental health settings, as these will vary across professional groups and depend on seniority. There are however a number of skills highlighted in this guidance, including cultural competency, that all staff should demonstrate in their daily practice. A compilation of these skills and competencies can be found in Appendix 5.
Opportunities should be made available to staff for skill development, through training, mentoring and shadowing. People in leadership positions have an important role to play in terms of enabling this to happen and for creating a culture that embraces learning and feedback. This may include forging links with other services, eg learning disability and autism teams, who can support the inpatient team to develop competencies for responding to individual needs. For nursing staff, development may be supported by Professional Nurse Educators, who are specifically employed to develop and deliver clinical practice education.
Staff wellbeing and psychological safety
It can be highly challenging to support people who are experiencing acute levels of mental distress. For staff members to be able to respond consistently with compassion and understanding and offer the best levels of therapeutic care, they need to be well supported, both on an individual and team level. Where staff are valued and well supported, there is also likely to be lower turnover, fewer vacancies and less reliance on bank and agency staff.
Those in leadership positions have an important role to play in terms of developing and maintaining a team dynamic that is valuing, respectful and empowering for all, and for creating an open culture in which team members feel able to ask questions and receive guidance on what is and is not good practice. This open culture must also include ensuring that team members understand how to raise concerns about poor practice (eg through having clear whistleblowing policies and putting in place Freedom to Speak up Guardians) and feel comfortable to do so. Where concerns are raised, team members should feel confident that they will be taken seriously by management and swift action taken to address identified issues.
Leaders also have a key role to play in ensuring each team member receives regular supervision and reflective practice. Team members should receive clinical restorative supervision at least monthly, which includes reflection on their own practice and that of the wider service, as well as their wellbeing and any challenging situations that they have encountered. There should also be regular group reflective practice within teams, led by an appropriately qualified mental health clinician, such as a therapist or Professional Nurse Advocate. The Professional Nurse Advocate (PNA) programme is training thousands of nurses to facilitate restorative supervision to their colleagues within and outside nursing, including one PNA in every adult inpatient mental health setting. By having regular team supervision and space for reflection, it helps to build supportive relationships between staff members, allows differing perspectives and approaches to be shared, and enables improvements to practice to be identified and put in place.
There may be occasions where staff require additional support for their own wellbeing. Colleagues, managers and other staff support services, such as occupational health and HR, should be aware of the support services that they can signpost people to in such cases.
Workforce resources
Resources that can support effective staffing in mental health settings, include:
- This webinar (requires login) hosted by NHS England providing an update on the NHS Long Term Plan ambition and funding available to improve acute inpatient staffing.
- NHS England e-learning on Fundamentals of Safer Staffing
- University College London (UCL)’s competency framework for adult and older adult acute mental health inpatient care
- The Mental Health Core Skills Education and Training Framework
- The Mental Health Nurse’s Handbook
- The Royal College of Occupational Therapists’ Informed View on Mental Health Rehabilitation
- Peer Support Worker Competency Framework
- The British Psychological Society and Association of Clinical Psychologists’ guidelines for psychological services within the acute adult mental health care pathway, which includes information on workforce development.
- The National Collaborating Centre for Mental Health and the Positive Practice in Mental Health Collaborative’s report covering workforce wellbeing, recruitment and retention in mental health services
- The NICE guideline on mental wellbeing at work.
Continuous improvement of the inpatient pathway
Some of the most effective inpatient mental health services are those that embrace change, where there is a culture of continuous learning and development, to identify what more can be done to improve the inpatient pathway. Three key mechanisms that can promote continuous improvement are: co-production, quality improvement methodology, and using data to inform service provision.
Co-production
Co-production should be at the heart of all aspects of how the inpatient pathway is designed, delivered and monitored. To ensure that the inpatient pathway meets the needs of people accessing inpatient services, it is vital that people who have used inpatient services and people that care for them, are involved and able to influence the development and improvement of the pathway. This should include representation from people belonging to groups that experience health inequalities and who may not traditionally become involved in co-production activities, and people who have experienced transitions between services in order to strengthen these pathways.
For co-production to be genuine and meaningful, it requires people who have used inpatient services, their carers, and people involved in delivering services, to come together as equal, reciprocal partners, from the very start of a piece of work to its conclusion. Everyone involved should be enabled and empowered to use their unique and diverse experiences and skills to shape the delivery of inpatient services, with decision-making power shared across the group. Providers should appropriately reward people’s time, put in place reasonable adjustments that enable people to participate fully, and have mechanisms for reviewing whether co-production is taking place across all aspects of inpatient policy, provision and practice. Providers should also consider having lived experience roles at all levels within their organisations (including senior management level), in line with NICE guidance on shared decision making, in order to build capacity for embedding co-production across services.
Some resources to support the use of co-production throughout the design and delivery of inpatient services include:
- This article from the Lancet Psychiatry – From Preproduction to Coproduction: COVID-19, whiteness, and making black mental health matter
- NHS England’s resources on involving people with a learning disability and autistic people in the design and development of services.
- NDTi’s practical guide to Progressing Transformative Co-production in Mental Health
- The New Economics Foundation’s publications, including: Public Services Inside Out.
- The Point of Care Foundation’s experience-based co-design toolkit
- The Royal College of Psychiatrist’s Working Well Together resource
- The Social Care Institute for Excellence’s guide and practical examples of how to do co-production.
- Think Local Act Personal’s information about co-production and links to practical examples, ladder of co-production and top 10 tips for co-production.
Quality improvement
Quality improvement methodology is increasingly used in mental health settings. One of the key features of quality improvement is the use of Plan-Do-Study-Act (PDSA) cycles, which involve developing change ideas, testing these changes and using data to review their impact and decide next steps (eg refining the idea and re-testing on the ward, testing a successful change in a larger number of services, or not proceeding with the change idea). It is important to note that not all change ideas will lead to a demonstrable improvement, however, they will still generate valuable learning to inform future quality improvement work.
Quality improvement works most effectively where there is buy-in for the process at a senior level, but it is frontline teams, together with service users and carers, who lead the process of change. This helps to ensure team-wide buy-in for implementation, and also helps to improve teams’ motivation and engagement.
Useful resources to support providers to embed use of quality improvement across the inpatient mental health pathway include:
- NHS England’s quality improvement resources.
- The King’s Fund’s resources on quality improvement in mental health
- Royal College of Psychiatrists’ quality improvement guide for trainees and trainers
- East London Foundation Trust’s quality improvement webpages
In addition, the Royal College of Psychiatrist’s Centre for Quality Improvement offers a number of relevant accreditation schemes and quality networks that support services to carry out regular peer- and self-review of the quality of care, which may inform quality improvement initiatives.
Using data to inform service provision
Data is key to understanding how the inpatient pathway is working and for identifying changes that could be made to improve the pathway and being able to demonstrate whether any changes made have led to a measurable improvement. One of the key recommendations from the Getting It Right First Time (GIRFT) report for adult crisis and acute care was that services regularly analyse their routine data and share the findings, in order to target and develop improvement work.
The data collected should include measures of how inpatient services and the wider acute pathway is operating, as well as information on the experiences and outcomes of people who have received inpatient care, including both clinician and patient reported outcome measures. There should also be a focus on data that looks at inequalities across the pathway (see this guide from NHS Digital on improving reporting of data related to equalities). Frontline teams, people who have used inpatient services, their carers and senior management should all be regularly involved in reviewing data and using it to shape delivery decisions, which drive improvements in access, capacity and flow, care quality, experience and outcomes.
At a national-level, NHS England is working to improve the use of data in acute mental health services and monitors indicators including:
- Number of inappropriate out of area placements.
- Number and percentage of admissions involving people not known to services.
- Number of mental health related A&E attendances, and the percentage of A&E waits lasting over 12 hours.
- Percentage of people on community mental health team caseloads who are admitted to hospital.
- Percentage of admissions involving detention under the MHA.
- Percentage of available adult and older adult acute beds that are occupied at any one time.
- Occupied adult and older adult acute bed days per 100,000 weighted mental health population.
- Average acute mental health length of hospital stay, and the rate of admissions per 100,000 weighted mental health population lasting over 60 days for working age adults and 90 days for older adults.
- Number of people who are CRFD who are occupying inpatient beds.
- Percentage of 72 hour follow-ups completed for people leaving acute inpatient care.
- Number of FTE staff members belonging to different professional groups per inpatient bed.
More details on the rationale for monitoring these metrics is set out in Appendix 6. As part of the drive to improve data quality, NHS England has also produced several dashboards which report data at national, regional, ICS and provider level, with several metrics broken down by demographic indicators, such as age, deprivation and ethnicity. The dashboards are frequently updated, and are accessible to those with an NHS login via the FutureNHS platform. Some of the indicators in the dashboards are included to support improvements in data quality, but the aim is that in future they may be published and used to better understand activity and performance.
Appendix 1: Legal obligations and inpatient mental health standards
As well as implementing the components of good quality acute inpatient care included in this guidance, each person who is accessing inpatient mental health care should have their legal rights respected, regardless of their background, social status or mental health presentation. The obligations that should be adhered to include:
- the Care Act 2014
- the Data Protection Act 2018
- the Equality Act 2010
- the Human Rights Act 1998
- the Mental Capacity Act 2005
- the Mental Capacity Act 2005: Code of Practice
- the Mental Health Act 1983
- the Mental Health Act 1983: Code of Practice
- the Mental Health Units (Use of Force) Act 2018
- the UK General Data Protection Regulation (GDPR) 2021
- the Common Law Duty of Confidentiality
- the Accessible Information Standard
- Duty of Care and Safeguarding responsibilities
Please note, as part of plans to reform the Mental Health Act, the Department of Health and Social Care and the Ministry of Justice has published a draft Mental Health Bill setting out proposed reforms to the Mental Health Act (1983). Although these reforms are not yet in statue, preparatory work should begin now to ensure that services are in a position to comply with the legal changes that are due to be introduced in the coming years.
All inpatient mental health care should also be delivered in line with key quality standards and guidance, including:
- The Caldicott Principles
- Royal College of Psychiatry Standards for:
- NICE guidance on:
-
- Advocacy services for adults with health and social care needs
- Coexisting severe mental illness and substance misuse: assessment and management in healthcare settings
- Self-harm: assessment, management and preventing recurrence
- Service user experience in adult mental health: improving the experiences of care for people using adult NHS mental health services
- Shared decision making
- Transition between inpatient mental health settings and community or care home settings
- Public Health England guidance on:
- NHS England’s
Appendix 2: Summary of key actions that need to take place across a person’s inpatient journey
As well as the key actions listed below, if someone is detained under the MHA, then Mental Health Act legislation and the accompanying Code of Practice should be followed. If someone is deemed to not have mental capacity to make specific decisions, then the Mental Capacity Act and accompanying Code of Practice should be followed. All other relevant legislation and guidelines should also be followed.
From the point of presentation to within 72 hours of admission
- Holistic assessment conducted to understand the person’s needs. This assessment should build on information contained within the person’s EPR, including any recorded advance choices and reasonable adjustments.
- Decision reached, considering as fully as possible the person’s preferences (including any ACDs), those of their chosen carer/s, and the views of relevant partner services, that the person’s needs can only be met in an inpatient setting and cannot be supported in the community. For people with a learning disability and autistic people, a C(E)TR should take place pre-admission to support this decision (or if this is not possible, within 28 days of admission).
- Purpose of admission discussed and agreed with the person and their chosen carer/s and uploaded to the person’s EPR.
- Prompt access facilitated to the most suitable hospital provision available for the person’s needs.
- Formulation review completed to gain an in-depth understanding of the person, the circumstances leading up to their admission and what will help them to recover. This, together with recorded ACDs and the findings of C(E)TRs (for people with a learning disability and autistic people), should be used as the basis to co-develop a personalised care plan with the person and their chosen carer/s, which should then be uploaded to the person’s EPR.
- Discharge planning begun with person and their chosen carer/s, including identifying any factors that could delay discharge (eg housing, social care), agreeing an EDD and an intended discharge destination, and uploading these to the person’s EPR.
- Interventions and treatment for physical and mental health conditions commenced or maintained, and a physical health check completed.
During the hospital stay
- Daily reviews (eg using the Red to Green approach) completed to check the person is receiving prompt access to the assessments, interventions and treatment they require, in line with their purpose of admission and care plan. Assessments, interventions and treatments should be adapted to meet reasonable adjustments and the needs of people from groups who experience health inequalities.
- Purpose of admission, care plan, discharge plan and EDD reviewed and updated regularly with the person and their chosen carer/s. If the purpose of admission is close to being met, additional focus should be given to discharge planning.
- Any factors that could delay discharge (eg need for step-down provision, home adaptations, housing, supported living or care home placement), reviewed every two to three days and proactively addressed with partner services.
- Monitoring visits completed by commissioners every eight weeks for adults with a learning disability and autistic people, and every six weeks for young adults aged up to 25, who have an EHC Plan.
At and following discharge
- Person-centred discharge plan refined with the person and their chosen carer/s. The plan should set out who is responsible for providing the assessments, interventions and treatments that the person will receive after leaving hospital and when the person can expect to receive this support.
- Discharge facilitated promptly once a decision is reached that the person is CRFD (ie the person does not require any further assessments, interventions and/or treatments, which can only be provided in the current inpatient setting), and that it is possible to discharge them (ie because the planned post-discharge support is available at that time). If a person is CRFD, but it is not possible to discharge them, they should continue receiving the interventions, activities and other support that they need in hospital to remain CRFD, so that they can be discharged as soon as planned discharge support is in place.
- At least 48 hours’ notice of the decision to discharge given to the person, their chosen carer/s and any services (eg community-based mental health and learning disability teams, CRHTTs, housing services, social services) that will be involved in the person’s ongoing care.
- Risk assessment updated and uploaded to the person’s EPR which includes information on how any risks to self or others will be managed once the person is discharged.
- Follow-up meeting arranged pre-discharge, including providing written details of when, where and who the follow-up will take place with.
- Clear information provided to the person and their chosen carer/s about how to access crisis support after discharge (including direct contact details for the CRHTT).
- Prompt access provided to all planned post-discharge support included in the person’s discharge plan. The person should also be supported to develop ACDs and a crisis plan, if they were not developed ahead of discharge.
- Follow-up completed (face-to-face wherever possible) within 72 hours of discharge for all adults discharged from an inpatient mental health service, excluding specialised services commissioned by NHS England. (NB this has been included in the NHS Standard Contract since 2020/21.) If the follow-up indicates additional support is required, action is taken promptly to put this in place.
- Relevant information relating to a person’s discharge (which may include a copy of the person’s discharge plan) shared with services involved in the person’s ongoing care and treatment. Discharge summary shared with the person’s GP and other relevant parties, where appropriate, within a week of discharge.
- Multi-Agency Discharge Events used where there are complex discharges requiring agreement across multiple partners, and follow locally agreed escalation procedures where there are concerns about delayed discharges.
Appendix 3: Holistic assessments
During the assessment and formulation process (completed within 72 hours of admission), the inpatient team should work with the person, their chosen carer/s and representatives from partner services to gather information on the areas listed below. Information contained in the person’s EPR should also be reviewed at the earliest opportunity, in order to build on their existing care plan and avoid duplication of information gathering, while at the same time recognising that the EPR may not be fully up-to-date or reflective of their current needs, and therefore information should be checked with the person and/or their chosen carer/s.
The areas that should be covered as part of a holistic assessment process, in a way that meets individual needs, include:
- Mental health symptoms and experiences, and the meaning of these for the person.
- The reasons/circumstances leading to the person presenting to services, including any previous experiences of traumatic and adverse events, and any additional support that could have helped to prevent their mental health worsening.
- Treatment preferences – what the person thinks may help them now and what has helped them and not been helpful in the past, considering a range of intervention types as well as the way in which support is delivered.
- The person’s skills, strengths and aspirations, and any protective factors and coping strategies that they use to manage their mental health.
- The person’s usual routine and ability to carry out daily living activities.
- Current medication for physical and mental health conditions, and their experience of these medications.
- Use of drugs and alcohol, assessed using a ecognized screening tool, such as ASSIST-Lite. The Clinical Institute Withdrawal Assessment Alcohol Scale Revised (CIWA-Ar) and the Clinical Opiate Withdrawal Scale (COWS) may be used to assess severity of alcohol/opiate withdrawal.
- Sleeping pattern.
- Diet and dietary requirements, including those relating to cultural or sensory needs.
- Physical health conditions and disabilities, including details of the person’s current treatment/management plan, and any aids or reasonable adjustments needed.
- Cognitive impairment, and any aids or adjustments needed.
- Sensory preferences and any aids or adjustments needed.
- Communication preferences and any aids or adjustments needed.
- Social and family relationships – who is important in the person’s life, who they would like to keep in contact with and see while in hospital and what support arrangements need to be put in place (eg for any pets and dependents).
- Support services – which health, social care and other services the person is already in contact with, what information they would like shared with these services and how they would like these services involved in their inpatient care and plans for discharge.
- Housing and financial circumstances. This may include making use of the Breathing Space debt relief scheme and making any arrangements needed to secure their home and ensure bills are paid while the person is in hospital.
- Employment, training and education, and any information that needs to be shared with employers or education/training providers while in hospital.
- Interests and hobbies, and how these can be supported while in hospital.
- Culture, race, ethnicity and how this can be supported while in hospital.
- Religion and spirituality, and how this can be supported while in hospital.
- Sexual orientation and gender identity and how LGBT+ people can be supported while in hospital.
- The person’s preferences as to who they would like involved in their care (their chosen carer/s), what types of information are routinely shared with their chosen carer/s, what aspects of their care they would usually like their chosen carer/s involved in (eg care planning), and whether their chosen carer/s have any support needs.
- Any belongings they would like with them in hospital (eg books, music, or sensory items).
- Any safeguarding or risk issues, including risk to self and others. Following NICE guidance on self-harm, risk assessment tools and scales should not be used to predict future suicide or repetition of self-harm, to decide who should be offered treatment, or to decide who should be discharged. Instead, person-centered approaches to safety planning should be used that involve the person and their nominated carer/s and take into account individual needs, risks and contexts and personal feelings of safety.
Appendix 4: Example steps as part of the Red to Green approach
Step 1
At the start of each day, record each person on the ward as having a red day.
Step 2
At the morning board round, rapidly review each person’s purpose of admission and EDD:
- If the purpose of admission has been met and the person could be effective cared for in the community, identify what steps need to occur to facilitate their discharge.
- If the purpose of admission has not been met and the person still requires inpatient treatment, identify what support the person needs (assessments, interventions, treatment), to progress their recovery.
Step 3
Agree and allocate the actions that members of the MDT will complete that day. Record the allocated actions during the board round, together with information on discharge readiness and any barriers to discharge or delays to treatment.
Step 4
Following the board round, the ward administrator sends round the agreed actions to the person who is responsible for completing them (which may include people outside the inpatient team).
Step 5
Following the afternoon board round, review whether the actions allocated have been completed, and if not, what has caused the delays, and determine whether the person is having a red or green day. Record the red and green statuses during the board round, together with information on discharge readiness and any barriers to discharge or delays to treatment.
Step 6
If someone has been recorded as on a red day for 72 hours or more and the MDT cannot resolve the problems that are causing this, then it should be escalated in line with agreed procedures.
Appendix 5: Skills and competencies for the inpatient workforce
This list of skills and competencies for delivering high quality acute inpatient mental health care has been compiled from the contents of this guidance. It is therefore not exhaustive and does not include profession or discipline specific skills.
- Understanding of good practice in relation to legal obligations, eg the Equality Act, Human Rights Act, MCA, MHA and the Mental Health Units (Use of Force) Act and safeguarding. In relation to the Mental Health Units (Use of Force) Act, this includes the ability to apply techniques for avoiding or reducing the use of force and restrictive practice and the impact of these practices when used (see further details from the Department of Health and Social Care). In terms of safeguarding responsibilities, this includes the ability to identify and respond appropriately to safeguarding concerns (including disclosures of historical or recent sexual abuse) and follow agreed reporting procedures.
- Understanding of good practice in relation to legal obligations, eg the Equality Act, Human Rights Act, MCA, MHA and the Mental Health Units (Use of Force) Act and safeguarding. In relation to the Mental Health Units (Use of Force) Act, this includes the ability to apply techniques for avoiding or reducing the use of force and restrictive practice and the impact of these practices when used (see further details from the Department of Health and Social Care). In terms of safeguarding responsibilities, this includes the ability to identify and respond appropriately to safeguarding concerns (including disclosures of historical or recent sexual abuse) and follow agreed reporting procedures.
- Understanding of data protection legislation and the common law duty of confidentiality, and in particular their application to situations involving the use and disclosure of information about adults and older adults in acute inpatient mental health settings.
- Understanding of when hospital-based acute care is most appropriate for an individual and when community-based acute care would be the most suitable option (including to facilitate discharge).
- Able to write clear purpose of admission statements and use these to inform care and discharge planning.
- Able to work in partnership with people and their chosen carer/s to ensure that they receive personalised support. This includes the ability to work with people to understand their individual circumstances and needs, and to co-develop care and discharge plans, which consider a range of therapeutic activities, interventions and treatments.
- Able to deliver activities and interventions that can support people’s recovery (with appropriate training), for example, brief physical health interventions and techniques from psychological approaches.
- Understanding of trauma and the impact it can have on people’s lives, and the ability to apply trauma-informed approaches to care.
- Able to talk to people about how their cultural needs can be best met while in hospital, and the cultural competency to work with people to deliver care in a way that meets these needs.
- Skilled at engaging and working with people with specific needs, including young adults, older adults, people with dementia, people with alcohol and drug problems, people with a learning disability and autistic people , and an awareness of when and how to access additional support from specialist services, when required. Please note, staff working in services registered with the CQC need to attend mandatory training on learning disability and autism, in line with the Health and Care Act (2022).
- Awareness of a variety of local NHS and non-NHS services (including VCSE sector organisations), what these services offer, and how to work in partnership with them to carry out assessments, develop care and discharge plans, and deliver support in a coordinated way.
- Understanding of local discharge pathways, what the challenges can be to timely and effective discharge and how these can be proactively addressed.
- Able to reflect on own emotional responses and use supervision to continuously learn and develop own practice.
- Able to respond appropriately where concerns or complaints are raised by people on the ward, their carers, the public or other members of staff, and to take action to address these concerns or complaints. This may include escalating issues to more senior managers.
- Able to work with people who have used services or cared for people who have used services to improve the delivery of acute mental health care.
- Able to understand and interpret data that is routinely collected in acute services and use this to guide service improvement.
- Understanding of quality improvement methodology and how to use this to improve acute inpatient services.
- Understanding of data protection legislation and the common law duty of confidentiality, and in particular their application to situations involving the use and disclosure of information about adults and older adults in acute inpatient mental health settings.
- Understanding of when hospital-based acute care is most appropriate for an individual and when community-based acute care would be the most suitable option (including to facilitate discharge).
- Able to write clear purpose of admission statements and use these to inform care and discharge planning.
- Able to work in partnership with people and their chosen carer/s to ensure that they receive personalised support. This includes the ability to work with people to understand their individual circumstances and needs, and to co-develop care and discharge plans, which consider a range of therapeutic activities, interventions and treatments.
- Able to deliver activities and interventions that can support people’s recovery (with appropriate training), for example, brief physical health interventions and techniques from psychological approaches.
- Understanding of trauma and the impact it can have on people’s lives, and the ability to apply trauma-informed approaches to care.
- Able to talk to people about how their cultural needs can be best met while in hospital, and the cultural competency to work with people to deliver care in a way that meets these needs.
- Skilled at engaging and working with people with specific needs, including young adults, older adults, people with dementia, people with alcohol and drug problems, people with a learning disability and autistic people , and an awareness of when and how to access additional support from specialist services, when required. Please note, staff working in services registered with the CQC need to attend mandatory training on learning disability and autism, in line with the Health and Care Act (2022).
- Awareness of a variety of local NHS and non-NHS services (including VCSE sector organisations), what these services offer, and how to work in partnership with them to carry out assessments, develop care and discharge plans, and deliver support in a coordinated way.
- Understanding of local discharge pathways, what the challenges can be to timely and effective discharge and how these can be proactively addressed.
- Able to reflect on own emotional responses and use supervision to continuously learn and develop own practice.
- Able to respond appropriately where concerns or complaints are raised by people on the ward, their carers, the public or other members of staff, and to take action to address these concerns or complaints. This may include escalating issues to more senior managers.
- Able to work with people who have used services or cared for people who have used services to improve the delivery of acute mental health care.
- Able to understand and interpret data that is routinely collected in acute services and use this to guide service improvement.
- Understanding of quality improvement methodology and how to use this to improve acute inpatient services.
Appendix 6: Indicators monitored at a national level to measure the effectiveness of adult acute mental health pathways
NHS England has a number of data dashboards that report many of the metrics listed below at national, regional, ICS and provider level, with several broken down by demographic indicators such as age, deprivation and ethnicity. These dashboards are frequently updated and can be accessed by those with an NHS login via the FutureNHS platform.
The rationale for monitoring these indicators is as follows:
- Number of inappropriate out of area placements: Inappropriate out of area placements occur when inpatient provision is not available locally. This usually occurs when the local acute mental health pathway is under too much pressure due to a combination of high admissions, long hospital stays, and delayed discharges. Being treated out of area can negatively impact people’s experience of and outcomes from care, while also being more expensive.
- Number and percentage of admissions involving people not known to services: If the first time people are encountering mental health services is at the point of admission, this may indicate that improvements are needed in primary care and community-based mental health services, to avoid escalation to the point that an admission is required. This is also used as an equality measure, as currently a higher percentage of people from racialised and ethnic minority communities have their first contact with mental health services at the point of admission.
- Number of mental health related A&E attendances, and the percentage of A&E waits lasting over 12 hours: A greater proportion of admissions coming in via A&E indicates that community-based crisis services may not be operating optimally, while long waits in A&E indicate difficulties accessing inpatient provision. Through people accessing mental health care through A&E, it may compound pressures on inpatient services, because once in A&E, consistent anecdote suggests that people are more likely to be admitted without community-based crisis alternatives being considered as fully.
- Percentage of people on community mental health team caseloads who are admitted to hospital: If a high percentage of people on community mental health team caseloads are admitted, this may indicate that improvements can be made within the community mental health team to identify when people’s needs may be at risk of escalating, and to intervene earlier and more proactively to prevent admissions. However, it is important that when admission is needed, the person is admitted to the right inpatient service provision in a timely manner.
- Percentage of admissions involving detention under the MHA: Detention status can sometimes be a helpful indication of acuity. If a large proportion of people admitted to an acute ward are detained under the MHA, it may indicate high levels of need for inpatient services locally. A higher than average proportion of admission involving the MHA is not necessarily a problem however, as it may reflect higher uptake of crisis alternatives for people who would otherwise be admitted to hospital on a voluntary basis.
- Number of adults with a learning disability and autistic people in a mental health hospital: The NHS Long Term Plan sets out that by March 2024, there should no more than 30 adults with a learning disability and/or autism in a mental health inpatient setting, per one million adults. Therefore, it is important to monitor this metric, using data from the Assuring Transformation dataset, to determine whether alternatives to hospital are being utilised (where this is the best option for the person), in order to support this commitment.
- Percentage of available adult and older adult acute beds that are occupied at any one time: Very high levels of bed occupancy (above 90%) can indicate significant pressure on the acute pathway and inpatient services in particular.
- Occupied adult and older adult acute bed days per 100,000 weighted mental health population: How reliant the local area is on inpatient care compared to other areas. Occupied bed days is used as this takes into account number of admissions as well as length of hospital stay.
- Average acute mental health length of hospital stay, and the rate of admissions per 100,000 weighted mental health population lasting over 60 days for working age adults and 90 days for older adults: People’s experience of care, their outcomes and service pressures all benefit if people do not spend a day longer than is necessary in restrictive hospital environments. A focus on reducing length of hospital stay (where appropriate) is also key to unlocking inpatient capacity and eliminating out of area placements. To understand true length of stay, it is important to look at the full length of stay in hospital (which may include a number of consecutive ward stays), rather than the length of individual stays on a ward. Monitoring the number of very long lengths of stay (as well as the average), helps to highlight where people are getting stuck in hospital for a very long time, which can be indicative of an admission that is not therapeutic or purposeful, or where there are barriers to discharge that need addressing.
- Number of people who are CRFD who are occupying inpatient beds: People are considered CRFD when no further assessments, interventions and/or treatments are needed that can only be provided in the current inpatient setting. Monitoring the number of people in an inpatient mental health service who are CRFD, and the reasons for this, sheds light on the barriers that need to be addressed to facilitate timely discharge.
- Percentage of 72 hour follow-ups completed for people leaving acute inpatient care: NCISH has found that there is an increased risk of dying by suicide on days 2-3 following discharge from hospital. As such, timely follow-up is key, and NHS England introduced a national standard from April 2020 that requires everyone who is discharged from an adult mental health inpatient service to be followed-up within 72 hours of discharge (excluding specialised services commissioned by NHS England).
- Number of FTE staff members belonging to different professional groups per inpatient bed: Higher numbers of FTE staff per inpatient bed is associated with a shorter length of hospital stay. This is particularly where there is a good therapeutic skill mix, eg higher numbers of psychologists and occupational therapists.
List of abbreviations
- ADASS: Association of Directors of Adult Social Services
- AMHP: Approved Mental Health Professional
- CCG: Clinical Commissioning Group
- CQC: Care Quality Commission
- C(E)TR: Care (Education) and Treatment Review
- CIWA-Ar: Clinical Institute Withdrawal Assessment Alcohol Scale Revised
- COWS: Clinical Opiate Withdrawal Scale
- CRFD: Clinically Ready for Discharge
- CRHTT: Crisis Resolution Home Treatment Team
- CTO: Community Treatment Order
- EDD: Estimated Discharge Date
- EHC: Education Health and Care plan
- EPR: Electronic Patient Record
- FTE: Full-Time Equivalent
- GDPR: General Data Protection Regulation
- GIRFT: Getting It Right First Time programme
- ICB: Integrated care board
- ICS: Integrated care system
- IMCA: Independent Mental Capacity Advocate
- IMHA: Independent Mental Health Advocate
- LGBT+: Lesbian, Gay, Bisexual and Transgender. The plus indicates that this term is inclusive of a wide range of sexual orientations and gender identities.
- LED: Light emitting diode
- MCA: Mental Capacity Act
- MDT: Multi-Disciplinary Team
- MHA: Mental Health Act
- NCISH: National Confidential Inquiry into Suicide and Safety In Mental Health
- NDTi: National Development Team for Inclusion
- NICE: National Institute for Clinical Excellence
- PCREF: Patient And Carer Race Equality Framework
- PDSA: Plan-Do-Study-Act cycle
- PICU: Psychiatric Intensive Care Unit
- UCL: University College London
- VCSE: Voluntary, Community and Social Enterprise organisations
Contributors to this guidance
In addition to the people named here, the guidance has built on broader engagement and learning through local, regional and national networks over the NHS Long Term Plan delivery period.
- Amanda Thompsell -National Speciality Advisor for Older People’s Mental Health, NHS England
- Bobby Pratap – Deputy Head of Mental Health, Adult Crisis and Acute Mental Health Programmes, NHS England
- Cassandra Lovelock – Expert Advisor, Adult Mental Health Programme, NHS England
- Charli Clement – Expert Advisor, Adult Mental Health Programme, NHS England
- Clair Haydon – Clinical Advisor (Occupational Therapy), Adult Acute Mental Health Programme, NHS England
- Colin King -Expert Advisor,Adult Mental Health Programme, NHS England
- Dwayne Smith – Expert Advisor, Adult Mental Health Programme, NHS England
- Dylan Kerr -Programme Manager, Alcohol and Drug Treatment and Recovery Team, Office for Health Improvement and Disparities, the Department of Health and Social Care
- Ellie Walsh -Assistant Director, Acute Mental Health Services, NAViGO
- Emma Wadey – Deputy Director, Mental Health Nursing, NHS England
- Fabida Aria – Consultant Psychiatrist and Associate Medical Director, Leicestershire Partnership NHS Trust
- Hazel Jordan -Programme Manager, Alcohol and Drug Treatment and Recovery Team, Office for Health Improvement and Disparities, the Department of Health and Social Care
- Husnara Malik – Programme Manager, Advancing Mental Health Equalities and PCREF, NHS England
- Ian Davidson -National Clinical Lead, GIRFT programme: Crisis and Acute Mental Health, NHS England
- Jason Brandon – Mental Health Social Work Lead, Office of Chief Social Worker, Department of Health and Social Care
- Johanna Frerichs - Senior Project Manager, Adult Acute Mental Health Programme, NHS England
- Kate Oldfield – Clinical Advisor (Clinical Psychology), Adult Acute Mental Health Programme, NHS England
- Kirsty Hart -Head of Adult Inpatient Mental Health Services, Northamptonshire Healthcare NHS Foundation Trust
- Laura Henry – Programme Manager, Adult Acute Mental Health Programme, NHS England
- Mark Farmer – Expert Advisor, Adult Mental Health Programme, NHS England
- Michael Kelleher -National Clinical Advisor for Alcohol and Drug Treatment, Office for Health Improvement and Disparities, the Department of Health and Social Care
- Naheen Ali – Expert Advisor, Adult Mental Health Programme, NHS England
- Richard Seager -Business Support Officer, Adult Crisis and Acute Mental Health Programmes, NHS England
- Roger Banks – National Clinical Director for Learning Disabilities and Autism, NHS England, and Christine Bakewell, Head of Strategic Commissioning, Learning Disability and Autism, NHS England, together with other members of the NHS England Learning Disability and Autism programme.
- Ruth Davies – Senior Programme Manager, Adult Acute Mental Health Programme, NHS England
- Sarah Rae – Independent Expert by Experience
- Saskya Falope – Deputy Head of Nursing, Urgent Care Pathway, Leicestershire Partnership NHS Trust
Publication reference: PR00033

