Introduction
Following publication of the Delivery plan for the recovery of urgent and emergency care services and the commitment in the NHS Long Term Plan for an acute frailty service/same day emergency care service (AFS) to be in place across every hospital with a Type I emergency department (ED) for 70 hours a week, this FRAIL strategy supports wider healthcare systems to deliver and improve acute frailty services across England by setting out a practical approach. This will mean more older people living with frailty can be safely discharged on the same day they arrive, avoiding admission overnight.
A self-assessment tool that summarises the recommendations is given in Appendix 1.
Acute frailty services routinely and systematically assess frailty in older people who present acutely to urgent and emergency care (UEC) services, with the aim of doing this within 30 minutes of a person’s arrival. These services consider the personalised needs of individuals living with frailty, evaluating their grade of frailty and degree of illness, supported by clear reliable pathways into and out of hospitals, aligned to the grade of frailty identified.
The development of acute frailty services is crucial for our ageing population. According to the Office for National Statistics UK 2021 census, over one-sixth (18.6%, 11.1 million) of the population were aged 65 years and over and this is estimated to increase to 25% of the population in the next 20 years.
To further support frailty within the acute sector a Commissioning for Quality and Innovation (CQUIN) indicator was developed to increase the identification of frailty within EDs. This CQUIN runs from the 1 April 2023 for 12 months as an incentive to identify frailty in a person early and for them subsequently to be seen at the right time by the right team as well as early identification of their needs.
The Same Day Emergency Care Community Space offers a full range of useful resources.
We are keen to continue to develop and improve the strategy for system leaders to better meet the needs of patients and the public. Please send your comments to england.sdec@nhs.net.
Frailty is everyone’s business
A person who is defined as frail is at high risk of adverse outcomes such as falls, immobility, delirium, incontinence, side effects of medication – and admission to hospital or the need for long-term care.
People with frailty can be vulnerable to dramatic and sudden changes in their health due to, for example, infection, medication change or a new environment.
While this strategy focuses on acute frailty services/SDEC and the key priorities in establishing or improving their provision, other services also support the avoidance of attendance at ED and/or admission including for older people; for example, urgent community response (UCR) services and virtual wards.
As all these services develop, it is important to reflect that frailty is everyone’s business, and to ensure a patient receives the right care, in the right place at the right time; that a mechanism is needed to support a clinical discussion.
Figure 1 shows how an older patient in the community could be supported to receive the right intervention and the central role of clinical discussion in the process.
Figure 1: Frailty is everyone’s business
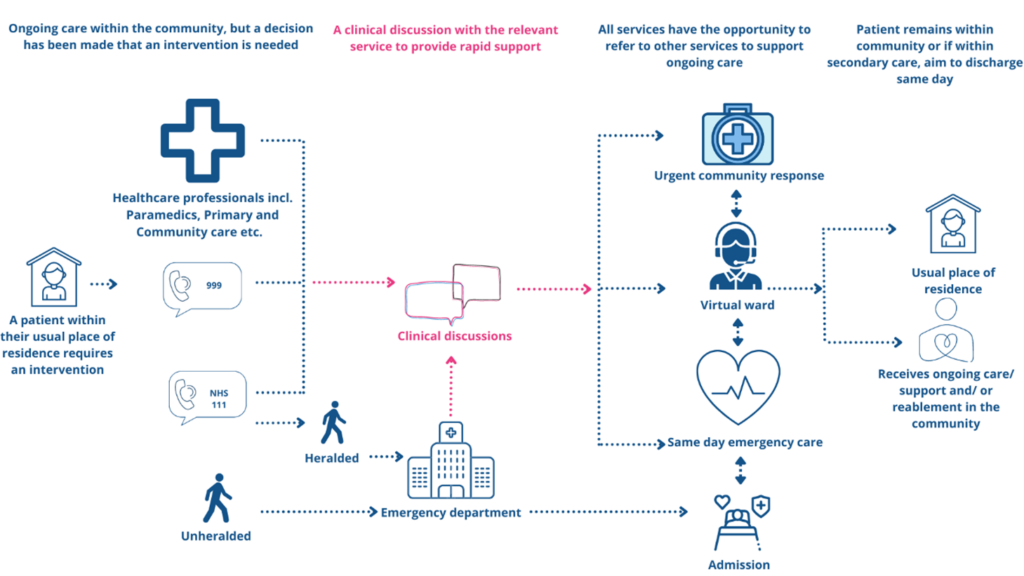
The above figure shows the clinical pathway when someone receiving ongoing care in the community needs an intervention. Referral routes can be by a paramedic, primary or community care, 999, NHS 111 or someone who presents unheralded at the emergency department. Through clinical discussion with the relevant service the patient is provided with the appropriate rapid response – urgent community response, virtual ward or SDEC, or admission. All services can refer to each other to support ongoing care, and always with the aim that where appropriate the patient remains in the community or is discharged from secondary care on the same day.
FRAIL
FRAIL is a mneumonic for the 5 key principles of an acute frailty service:
- Focus on the acute problem:
- assess patients on arrival and treat the acute condition they have presented with
- complete a clinical frailty assessment within 30 minutes of arrival
- Refer:
- refer to the multidisciplinary acute frailty service if needed
- liaise with other key services to support same day discharge
- Assess:
- initiate a Comprehensive Geriatric Assessment (CGA) to further assess the patient
- Identify needs:
- aim to personalise needs and support a patient-centred approach
- Leave:
- discharge the patient on the same day, with a discharge summary that links the patient into other key services for ongoing care
FRAIL is not independent from the SAMEDAY strategy. They should be used together to support the implementation or review of SDEC services in totality.
The 5 priorities are described further below, with the action providers and integrated care systems (ICSs) should take for each.
Principle 1 – Focus on the acute problem
- Patients should be assessed on arrival at acute settings and treated for the acute condition they have presented with; remembering frailty can co-exist with the presenting acute complaint
- While frailty tends to be seen in older people, anyone can have frailty markers regardless of their age
- Assessment for the identification of frailty and initial assessment of the acute problem based on clinical guidance in both the NHS England guidance for emergency department initial assessment and British Geriatric Society (Silver Book):
- National Early Warning Score (NEWS) 2
- Clinical Frailty Score (CFS) assessment (for patients aged 65+) – within 30 minutes of arrival
- 4AT (rapid clinical test for delirium)
Actions at provider level
- Develop protocols to implement a SDEC-by-default approach
- The acute frailty service should support front door assessment of appropriate patients. This could be provided by an advanced clinical practitioner and a physiotherapist as long as they can seek advice from other members of the acute frailty service team
- Promote a fit to sit approach at the front door
Actions at ICS level
- Work with system partners to advocate clinical frailty assessment in the community. Completing this within the patient’s own surroundings rather than a secondary care setting is often easier, quicker and more reflective
- Shared records across health and social care are vital to support the initial assessment
Principle 2 – Refer
- All healthcare professionals, including those in primary and community care, NHS 111 and 999 services, and paramedics on scene should have access to acute frailty services. This should also include UCR services
- A multidisciplinary team (MDT) is required to provide a holistic assessment and meet the needs of the patient
- The MDT should be available for a minimum of 10 hours a day (ideally 12 hours), 7 days a week
- A senior decision-maker should be available to accept the patient into the acute frailty service and offer onward advice to enable same day care
- Referrals should be made to other services that support the patient in their usual place of residence. These include but are not limited to:
- virtual ward monitoring, for example heart failure
- Hospital at Home, for example IV antibiotics
- third sector/voluntary sector organisations, for example British Red Cross, Age UK and other local organisations
- social care (including to resume care after an admission)
Actions at provider level
- Training for advanced level practitioners (ALPs) so they are confident and comfortable in being part of the senior decision-making team
- The acute frailty service should have a ‘pull’ mechanism to ensure patients are rapidly assessed
Actions at ICS level
- Open access routes to acute frailty services with clarity on who can refer – that is, all healthcare professionals including ambulance technicians
- Referral routes to other services should be available to support a same day approach, and they should be clearly mapped across the ICS to support decision-making
- Development of ICS workforce plans across community settings to enable delivery of care at home
Principle 3 – Assess
- The acute frailty team should have the skills and equipment to undertake a CGA while the ongoing acute problem is being managed
- Frailty is everyone’s responsibility. As such, dedicated acute frailty units are not always required. The service can instead be co-located with other services (such as medical) to improve collaboration and increase the identification of frailty
- Where it has not been possible to implement a frailty unit, developing a front door frailty model is an effective and credible alternative. This model allows members of the MDT to operate a peripatetic/roving model across the UEC pathway. An established model from South Tees Hospitals NHS Foundation Trust was highlighted in the Delivery plan for the recovery of urgent and emergency care services
- Community SDEC models are another way to embed an acute frailty service to support patients
- Rapid access to diagnostics is vital to ensure a same day approach can be achieved
- Point of care testing devices can support immediate patient review, assessment and treatment
Actions at provider level
- Every patient who has a CFS score ≥6 should have a CGA. This threshold has been agreed with the British Geriatric Society for EDs initiating the CGA
- Consider where the frailty service should be sited in the organisation
- Determine the senior decision-maker in the acute frailty service to facilitate contact by primary and community care, ambulance services, etc
Actions at ICS level
- Completed CGAs should be made available to all relevant decision-makers to reduce duplication and inform prioritisation within treatment plans
Principle 4 – Identify needs
- Patients should be supported to:
- understand the care, treatment and support options available and the risks, benefits and consequences of those options
- decide a course of action, based on their personal preferences and, where relevant, using legal rights to choose
- Using the personalised care model patients have proactive, personalised conversations that focus on what matters to them
- Patients who have a CFS of ≥7 should be supported with advanced care planning (ACP)
- Patient experience should be used to continually assess the service and identify where improvements should be made
- Patients should not stay in the acute frailty service and/or SDEC service longer than 8 hours
- Patients should be assessed as a fit to sit patient
Actions at provider level
- Work with voluntary, community and social enterprise (VCSE) organisations and liaise with social services to support patients’ and their carers’ needs and reduce admissions for social reasons
- Advocate for other specialised teams to be involved in the patient’s management at this stage, for example diabetes, oncology and tissue viability
- Advocate for staff training with the Personalised Care Institute
Actions at ICS level
- Work with primary care and community teams to ensure that patients with cancer or who are at end of life and receiving palliative care are aware of how to access appropriate services when they have an acute problem
Principle 5 – Leave
- The SDEC service should provide a summary of the attendance within 24 hours of discharge so that the patient’s primary and community care providers become actively involved in the ongoing care needs
- SDEC services need to consider patient transport. Where needed, transport should be provided to enable a patient to return to their place of residence on the same day
- Discharge planning should start at initial assessment by the frailty service and include practicalities such as whether the patient has access to their home
Actions at provider level
- Consider having a role in the service who links into primary and community services (such as by having access to GP records) to help with assessment and discharge planning
- Consider how success is measured, for example patient and staff experience
- Work with commissioners to address any patient transport concerns that may obstruct the same day approach
Actions at ICS level
- The acute frailty service should work with its ICS to ensure that services are integrated, for example UCR/virtual ward services and the acute frailty service
- Ensure that the reablement offer is consistent for all patients
- ICSs should work with nursing and residential homes to help patients return to their setting as quickly as possible, including out of hours (at night and over weekends)
Appendix 1: FRAILTY self-assessment tool
| Principle | Minimum requirement to be met for SDEC service audit tool | Met? Yes/No |
| F – Focus on the acute problem |
Develop protocols to implement a SDEC-by-default approach. |
|
|
The acute frailty service should support front door assessment of appropriate patients – this could be provided by an advanced clinical practitioner and a physiotherapist as long as they can seek advice from others in the acute frailty service. |
| |
|
Promote a fit to sit approach at the front door. |
| |
|
Work with system partners to advocate clinical frailty assessment in the community. Completing this within the patient’s own surroundings rather than a secondary care setting is often easier, quicker and more reflective. |
| |
|
Shared records across health and social care are vital to support the initial assessment. |
| |
| R – Refer |
Training for advanced level practitioners (ALPs) so they are confident and comfortable in being part of the senior decision-making team. |
|
|
The acute frailty service should have a ‘pull’ mechanism to ensure patients are rapidly assessed. |
| |
|
To ensure its success, the acute frailty service must have both clinical and executive sponsorship. |
| |
|
Open access routes to acute frailty services with clarity on who can refer – that is, all healthcare professionals including ambulance technicians. |
| |
|
Referral routes to other services should be available to support a same day approach, and they should be clearly mapped across the ICS to support decision-making. |
| |
|
Development of ICS workforce plans across community settings to enable delivery of care at home. |
| |
| A – Assess |
Every patient who has a CFS score ≥6 should have a CGA. |
|
|
Ensure that SDEC services have the same diagnostic turnaround times as the ED. |
| |
|
Consider where the acute frailty service should be sited in the organisation. |
| |
|
Determine the senior decision-maker in the acute frailty service to facilitate contact by primary and community care, ambulance services, etc. |
| |
|
Completed CGAs should be made available to all to reduce duplication and inform prioritisation within treatment plans. |
| |
| I – Identify needs |
Work with voluntary, community and social enterprise (VCSE) organisations and liaise with social services to support patients’ and their carers’ needs and reduce admissions for social reasons. |
|
|
Advocate that other specialised teams should be involved in the patient’s management at this stage, for example diabetes, oncology and tissue viability. |
| |
|
Advocate staff training with the Personalised Care Institute. |
| |
|
Work with primary care and community teams to ensure that patients with cancer or who are at end of life and receiving palliative care are aware of how to access appropriate services when they have an acute problem. |
| |
| L – Leave |
Consider having a role in the service who links into primary and community services (such as by having access to GP records) to help with assessment and discharge planning. |
|
|
Consider how success is measured, for example patient and staff experience. |
| |
|
Work with commissioners to address any patient transport concerns that may obstruct the same day approach. |
| |
|
The acute frailty service should work with its ICS to ensure that services are integrated, for example with UCR/virtual ward services. |
| |
|
Ensure that the reablement offer is consistent for all patients. |
| |
|
ICSs should work with nursing and residential homes to help patients return to their setting as quickly as possible, including out of hours (at night and over weekends). |
|
Publication reference: PRN00449

