1. Our call to action
1.1 Our professional call to action
Now is the time to act to invest in and grow our occupational health and wellbeing services in the NHS. This strategy represents a collaborative direction of travel for our entire healthcare system to fully realise the value that our occupational health and wellbeing professional services contribute to our NHS.
Recent years have placed an enormous demand on our NHS workforce. The massive impact of the pandemic, and the future burden of underdiagnosed disease and long-term conditions, for both the wider population and NHS staff, make it essential that our NHS workforce get access to, and reassurance from, the very best occupational health and wellbeing support. This will enable them to be safe, healthy, and protected in their roles.
There have been multiple expert-led reviews concluding that the health and wellbeing of NHS staff impacts quality of patient care, organisational efficiency, and ability to deliver regulatory targets. Simply put, looking after the health and wellbeing of our NHS people enables them to pass on good quality care to our patients.
We not only commend this strategy to our healthcare leaders and fellow occupational health and wellbeing professionals, but we urge you to take action to make this happen.
Dame Carol Black, Chair, NHS Health and Wellbeing Expert Advisory Group
Dr Steven Boorman, Chair, NHS Growing Occupational Health and Wellbeing Steering Group
1.2 Our strategic call to action
Our occupational health and wellbeing (OHWB) professionals are vital in ensuring that our NHS people are safe and healthy. During the pandemic, OHWB rapidly responded to the challenge of keeping our NHS people safe and well and demonstrated the value that they bring. Yet, this also identified variation and an inequality of OHWB provision across our NHS.
The Growing occupational health and wellbeing together strategy is a united vision and call to action to invest in and grow our OHWB services and multidisciplinary family of OHWB professionals.
We want to recognise and thank the many people – OHWB professionals, senior healthcare leaders, and national strategic partners – who have helped to co-design this strategy, and who are also fully committed to working together to deliver it and realise our collective ambitions.
NHS England is committed to working in partnership with the OHWB community to realise the vision outlined within Growing occupational health and wellbeing together. The work outlined in this strategy directly supports our NHS people promise and especially ‘we are safe and healthy’. It forms part of our wider health and wellbeing programme of work, directly supporting the ongoing delivery of the strategic themes set out in the NHS people plan through the commitment of looking after our NHS people, with quality OHWB services.
Growing occupational health and wellbeing together is a collaborative strategy, as we know that growing OHWB requires investment, championing, and action in a variety of different needs-driven ways to realise our united vision. We encourage our senior healthcare leaders to join us in realising the ambition within this strategy, with your OHWB professionals in the driving seat and empowered to take action flexibly, based on the health and wellbeing needs of your local NHS people. We encourage our valued OHWB community to join with us as we work together to put this strategy in place to grow and strengthen our OHWB services, in a way that is right for the diversity of the NHS people that we care for.
As we emerge from the pandemic, and the innovation and learning it has prompted, this is a key moment for us to grow our OHWB services and OHWB people. We recognise the crucial role they play to create a culture of wellbeing where all our NHS people feel valued and cared for, which ultimately leads to higher quality and more compassionate patient care.
Em Wilkinson-Brice, National Director for People ,NHS England
John Drew, Director of Staff Experience and Engagement, NHS England
1.3 Acknowledging our supportive community
We would like to thank everyone who has supported the co-design of Growing occupational health and wellbeing together.
We want to thank the members of our multiprofessional occupational health and wellbeing (OHWB) community who shared their knowledge, experience, and passion for making a positive difference to the health and wellbeing of our NHS people. We also want to thank our NHS employees and managers who are our service users of OHWB, organisational leaders, strategic system leaders, experts, and national bodies. Your collective contributions were essential in understanding the complexity, challenges, opportunities, best practice, and innovations when developing this strategy that take us from where we are now, to where we want to be collectively, in realising the future potential of our OHWB services.
Growing occupational health and wellbeing together has been commended by Dr Steve Boorman and Dame Carol Black, endorsed by the NHS national Growing Occupational Health and Wellbeing Steering Group and is supported by the national NHS Health and Wellbeing Expert Advisory Group. Key national bodies have united behind Growing occupational health and wellbeing together and are committed to working together to realise the vision within this strategy, including NHS England, NHS Health at Work Network, the Society for Occupational Medicine (SOM), the Faculty of Occupational Medicine (FOM), the Chartered Institute of Personnel and Development (CIPD), Health Education England (HEE), NHS Employers, the Social Partnership Forum (SPF), NHS Trade Unions and the Council for Work and Health. We are also grateful for the Department of Health and Social Care (DHSC) and the Department for Work and Pensions (DWP) engagement as part of their work and health activity.
2. Introducing Growing occupational health and wellbeing together
2.1 Purpose
Growing occupational health and wellbeing together provides a strategic and long-term roadmap that enables us to fully realise the value that our occupational health and wellbeing (OHWB) services and our multiprofessional family of OHWB people bring to enabling the wellbeing of our NHS people, which in turn leads to better patient care.
It has been purposefully designed as a collaborative and action-oriented strategy to cover the entire English NHS system, acknowledging that we all have a part to play in growing OHWB. It achieves this by:
- Outlining a roadmap for healthcare organisations and system leaders in England to flexibly work toward when articulating their localised vision and steering their investment in OHWB services over the next five years.
- Empowering and uniting our diverse family of OHWB professionals around a common vision when developing services and improving the health and wellbeing of our NHS people.
- Enabling collaborative action between OHWB stakeholders, NHS organisations and systems, and strategic partners to drive action to grow our OHWB services, our OHWB people, and enhance their impact.
2.2 Introducing our vision and collaborative action areas
Growing occupational health and wellbeing (OHWB) together centres around a united vision for OHWB in the NHS, four strategic drivers, and corresponding areas for collaborative action.
Driver 1: Growing the strategic identity of occupational health and wellbeing
1.1 Integrated occupational health and wellbeing
1.2 Strategic voice of occupational health and wellbeing
1.3 A trusted and proactive brand
1.4 Collaborative action and visible investment in occupational health and wellbeing
Driver 2: Growing our occupational health and wellbeing services across systems
2.1 Inclusive, needs-driven, and well-resourced occupational health and wellbeing
2.2 Integrated service user pathways
2.3 Common service development framework
2.4 Service innovation
2.5 Quality improvement
2.6 Maximising technology and digital
2.7 Integrated care system collaboration
2.8 Improving access to occupational health and wellbeing for smaller healthcare organisations and primary care
Driver 3: Growing our occupational health and wellbeing people
3.1 Multidisciplinary occupational health and wellbeing workforce planning
3.2 Attractive career pathways and talent management for occupational health and wellbeing professionals
3.3 Credible and accessible occupational health and wellbeing education and training
3.4 Empowered occupational health and wellbeing leaders
3.5 Empowered occupational health and wellbeing workforce
3.6 Developing all NHS managers in supporting employee health and wellbeing
Driver 4: Growing our occupational health and wellbeing impact and evidence-based practice
4.1 Using data to demonstrate the impact of occupational health and wellbeing
4.2 Driving occupational health and wellbeing practice
4.3 Demonstrating the value of occupational health and wellbeing
4.4 Driving the occupational health and wellbeing market
4.5 Demonstrating the impact of this strategy
2.3 Co-creating Growing occupational health and wellbeing together
This strategy represents the united voices of a breadth and depth of people, including our NHS employees and managers who are our occupational health and wellbeing (OHWB) service users, senior healthcare leaders, OHWB experts, and our OHWB professional community.
This is inclusive of all healthcare service areas (for example, primary, secondary, tertiary and commissioning services) and at various levels (i.e. from frontline delivery, through to system and national working) covered by the English NHS system.
We all must work together to realise the value of OHWB in improving and sustaining the health and wellbeing of our NHS people, to enable them to pass this wellbeing on to our patients. No one person, group, or organisation can achieve the transformational change we need alone, and we must unite to grow our OHWB services and people together. This is why collaborative action sits at the heart of our strategy.
The pandemic represented a ‘moment of truth’ for our OHWB professionals. They demonstrated their value in improving the health and wellbeing of our NHS people by their ability to innovate and work flexibly and collaboratively to achieve this.
We identified outstanding practice that not only informed this strategy, but also demonstrated that growing OHWB is already being effectively achieved in many areas. We learnt how OHWB services have transformed to meet the needs of their organisational workforce around integrated pathways, how integrated care systems and their organisations have united to maximise economies of scale to create integrated and accessible approaches and how high quality OHWB services are adapting and meeting the needs of their entire local workforce population.
We also identified the following core enablers that sit at the heart of this collaborative strategy:
- Organisation and system leaders need to empower and invest in OHWB services to realise their true potential and maximise their value in employee OHWB and ultimately patient care.
- Our family of OHWB professionals need to be in the driving seat and working as an integrated service and united team to collaboratively develop their services in a joined-up way to inclusively meet the health and wellbeing needs of our healthcare people.
- Strategic bodies, influential partners and national OHWB stakeholders need to unite behind our common vision to fully realise the strategic and transformational change needed in OHWB.
This strategy synthesises the exemplary practice that we identified with the breadth and depth of stakeholder voices, who jointly articulated what we need from future facing OHWB services.
2.4 Our definition of occupational health and wellbeing
This strategy unites occupational health and wellbeing (OHWB) as a multiprofessional family of job roles and services that collaborate to improve the health and wellbeing of our NHS workforce.
When co-creating this strategy, we heard how developing a ‘positive brand and identity’ for OHWB was a key driver. We also heard how integration was an underpinning driver and that OHWB needed to unite as a family of professional services that collectively improves the health and wellbeing of our workforce. We were also motivated by the holistic definition of health from the World Health Organization and by how many of our healthcare organisations and integrated care systems have already started to integrate the family of OHWB professions under one umbrella service. These drivers helped us to create our integrated definition of OHWB as a family of professional services that unite to improve the health and wellbeing of our NHS workforce.
2.5 Working collaboratively to make it happen
This strategy provides a united roadmap for all parts of our healthcare system to collaboratively develop our occupational health and wellbeing (OHWB) services, our OHWB people, and enhance their impact in creating a culture of wellbeing for our NHS workforce, which ultimately leads to quality patient care.
This strategy is designed to enable everyone reading it to relate to our united vision and inspire them to identify ways that they can take action to grow OHWB. This includes our OHWB professionals in their services, through to our organisation and system leaders and national OHWB strategic partners. We appreciate that ‘one size, does not fit all’ and we encourage local translation of this strategy, to lead to local action that will support the realisation of our joint vision, improvement drivers and areas for collaborative action.
The following outlines our main target audience for this strategy, and ways they can use it:
Multiprofessional OHWB community
This strategy provides a unified voice for you as our OHWB community. It is a ‘call to action’ to collaborate as a multi-professional family to grow your services and grow together as a community. It empowers you with a direction of travel and offers strategic leverage to influence others to support you on your journey to grow OHWB services that keep our NHS people well, so that they can continue to deliver high quality patient care.
Organisational leaders
This strategy provides a strategic roadmap and ‘call to action’ to ensure that organisations are prioritising, investing in, and leading the development of OHWB services. It offers direction to ensure that your OHWB services are integrated, innovative, add value, and are meeting the health and wellbeing needs of your diverse workforce. It provides collaborative action areas that can be flexibly interpreted in your local context, appreciating that every organisation is at a different stage of your growing OHWB journey.
Integrated care system leaders
This strategy outlines areas for collaborative action across integrated care systems and your organisations to maximise the value of OHWB as part of your strategic people plan. It encourages system leaders to think about how you can collaboratively grow OHWB services and your OHWB workforce to meet your local workforce population needs. It poses questions about ensuring equity of access across all healthcare organisations (for example, provider, commissioning, community and primary care) and how you can work collaboratively to maximise OHWB expertise, resources, and economies of scale when empowering future-focused OHWB services.
Wellbeing guardians and people directors
This strategy enables you to hold your organisations to account to ensure that the value of OHWB services is maximised, they are being adequately invested in, and are empowered to meet the health and wellbeing needs of your healthcare workforce.
National leaders and national bodies
This strategy connects our national leaders and national bodies in a unified way. It provides a roadmap for national partnership working through tangible collaborative areas to grow OHWB people and services. It provides action areas to focus national long-term investment and transformational change activity, and a framework for identification and sharing of best practice.
NHS people, as our occupational health and wellbeing service users
This strategy gives all of our NHS people and managers, as the service users of OHWB, a united voice by articulating how OHWB services need to grow and develop to keep you healthy and well, to enable you to pass this wellness on to those that you care for. It outlines how OHWB is everyone’s business and champions all NHS managers in developing skills in looking after the health and wellbeing of your teams.
The remainder of this strategy:
- Brings the vision, improvement drivers and areas of collaborative action to life by offering more detail, inspiring healthcare leaders and our OHWB community to take action to realise this vision.
- Summarises the evidence that informs this strategy and shares the voices of those who contributed to its design, using inspirational quotes and case studies that demonstrate how growing OHWB can be, and already is being, done.
- Offers next steps for how this strategy forms part of a five-year and longer-term programme to grow our OHWB services, our OHWB people, and the impact of OHWB.
3. Drivers and collaborative action areas
Caring for our NHS people enables them to pass that care on to our patients. This strategy is driven by this and our united vision to improve the health and wellbeing of our NHS people by growing our occupational health and wellbeing (OHWB) services and people to be trusted, strategic and integrated partners. Four drivers for improvement and accompanying areas for collaborative action have been created to outline how we can work together to bring this vision to life over the next five years.
Our four drivers and underpinning areas for collaborative action are designed to be:
- Collaborative and empowering – as we know that the change needed to grow OHWB in the NHS cannot be achieved alone, and we must unite to achieve the ambitions in this strategy where everyone reading this strategy feels empowered to take action.
- Future focused – as we want this strategy to move us forward in a united way towards the vision that our variety of healthcare stakeholders have inclusively helped us to co-create.
- Flexibly interpreted – as we know that the NHS is a complex system where ‘one size does not fit all’, and our OHWB professionals, organisational and system leaders will need to flexibly interpret and support the ambitions of this strategy in their own context when developing local actions for growth.
The following section outlines our drivers and underpinning areas for collaborative action in detail and explains why these are important. We have included case studies from OHWB services to demonstrate that these areas for collaborative action are not only the future we want to work towards, they are also achievable.
3.1 Driver 1: Growing the strategic identity of occupational health and wellbeing
1.1 Integrated occupational health and wellbeing (OHWB): OHWB is experienced by service users as one integrated service and multiprofessional family who are working towards the shared goal of improving the health and wellbeing of our NHS people.
1.2 Strategic voice of OHWB: OHWB has a strong voice in all organisation and system-wide decisions that impact the health and wellbeing of our healthcare workforce. This is supported by a comprehensive OHWB strategy.
1.3 A trusted and proactive brand: NHS employees and managers are the service users of OHWB. They experience OHWB positively as a trusted service that helps them to proactively prevent ill health, improve their personal health and wellbeing, and the health and wellbeing of their teams.
1.4 Collaborative action and visible investment in OHWB: All stakeholders at national, system and organisational level are united around the Growing occupational health and wellbeing together strategy. They are working collaboratively to realise the vision, improvement drivers, and demonstrate the positive impact of OHWB in the NHS.
We have an opportunity to evolve the identity of OHWB to be a proactive, strategic and integrated service at the heart of improving the health and wellbeing of our NHS people, to enable them to pass care and wellbeing on to our patients and wider population.
To achieve this, we need to enable OHWB to be a fully integrated service. We must breakdown any silo working and unite the professionals, services and interventions offered into one complete package so that our NHS employees and managers experience OHWB as one service, united by clear and accessible service pathways. This will require not only change to the way our OHWB services operate and are configured, but also cultural change to support OHWB professionals to work collaboratively in this interconnected way.
OHWB people are the experts in improving the health and wellbeing of our NHS people in the workplace. We must empower OHWB to have a strategic voice to help senior organisational and system leaders to consider the health and wellbeing needs of our NHS people in every decision they make. This will ensure that any strategic or operational decisions made will also positively support the wellbeing of our NHS people. The wellbeing guardian will have a role to play in helping to realise the strategic voice of OHWB at board and senior leadership level. The NHS health and wellbeing framework will support this and enable the creation of organisational and integrated care system OHWB strategy.
To maximise the contribution and impact of our OHWB services, we must also ensure that they are seen and experienced as a positive and proactive brand. We need to move away from OHWB services that are seen as a transactional service to go to when things go wrong, and move toward OHWB as proactive and preventative services that actively helps our NHS people to improve their health and wellbeing. To achieve this, we need to give OHWB the capacity to maximise their value in this preventative space. We also need to support OHWB services to develop in a way that inspires trust from our NHS people, and a brand that is experienced as supportive, compassionate, and inclusive.
To maximise the value and grow a positive identity of OHWB, we will require collaborative action. We need our OHWB people to unite behind this strategy as a ‘call to action’ to achieve our shared ambitions. We need our NHS leaders to unite to position OHWB as a strategic voice and invest in its development as an integrated, proactive, and partnership service. This will be supported by our national NHS organisations and OHWB professional bodies, uniting behind this strategy and working together to achieve this unified vision.
Case Study: Cambridge University Hospital’s occupational health and wellbeing brand and proactive, preventative approach
Occupational health services at Cambridge University Hospitals NHS Foundation Trust (CUH) are on a long-term journey to ensure their services provide not just services at point of need, but also pre-empt staff needs in a proactive and preventative way. This underpins the way the whole service operates.
Developing a trusted brand
As part of their proactive, preventative approach, CUH Occupational Health and Wellbeing (OHWB) team wanted to develop their interactions with their 11,500 staff population. An independent sub-brand ‘Oh’ was created to offer the health and wellbeing service through its own website and communications to support targeted groups of workers with health and wellbeing initiatives and resources. As a recognisable sub-brand within CUH corporate communications, ‘Oh’ was able to effectively communicate all health and wellbeing services and offers in a consistent way. The branding and how it is used has made a strong contribution to staff feeling cared about and trusting the OHWB services provided.
Musculoskeletal (MSK) conditions
The OHWB team have tried a number of different approaches to support staff with MSK conditions in recent years. Having the aim of keeping staff well so they can continue to care for patients, a fast access physiotherapy service for staff was developed, regardless of whether they were injured at work or outside work. Demand has remained high for the service since it was inaugurated. More recently, the physiotherapy team experimented with preventative outreach education sessions for staff, targeting areas where MSK referrals were notably high, as well as receiving requests from areas and giving staff the tools to support their own MSK health. While the outreach education sessions were running, lower levels of staff absence for back related MSK issues and positive feedback via the staff survey were observed, and the sessions were felt to have played a part in this.
Staff mental health
A pilot, which brought a liaison psychiatrist into the trust on a sessional basis to work alongside OH team members, combined with another pilot project instigated by the area’s mental health trust gave rise to the current staff mental health service provision across Cambridge and Peterborough. CUH were one of the first trusts to pilot this approach, finding the benefits for fast assessment and fast access to specialist advice and treatment for staff, and additional support for OH team members, of great benefit to the OH service. There were additional benefits in terms of peer-to-peer learning for the OH team, as well as adding an extra layer of surety and safety to OH clinical practice. The sessional liaison model and collaboration between OH and Cambridgeshire and Peterborough Foundation Trust gave rise to a comprehensive staff mental health service commissioned by Cambridge and Peterborough Integrated Care System. There have been benefits seen in outcomes as a result of interventions, and better, swifter support for staff with mental health needs.
Case Study: Using the NHS health and wellbeing framework to strategically develop organisational occupational health and wellbeing strategy and priorities at East Lancashire Hospitals NHS Trust
East Lancashire Hospitals recognises that caring for colleagues is essential to enable them to pass that care on to their patients. They used the NHS health and wellbeing framework to create a clear and holistic action plan for improvement and investment, underpinned by a needs-driven and holistic evidence base that supports their employees to feel well, happy, and healthy through high-quality occupational health and wellbeing (OHWB) support for all.
They used multiple sources of information to inform their diagnostic phase using the NHS health and wellbeing framework seven elements model and toolkit. This included staff survey data, occupational health data, usage trends, attendance data, health needs assessment surveys, and wider workforce data. They complemented this by directly engaging their people, staff groups and trade unions to develop their needs-driven and inclusive approach.
This approach enabled them to identify the OHWB needs of their workforce. They were then able to build their OHWB plan and services around the seven elements in the NHS health and wellbeing framework and identified 70 smart actions for investment as part of this plan. This enabled them to drive forward a holistic OHWB approach that was inclusive, proactive, and preventative, and reactive and restorative. It enabled them to demonstrate visible investment and action to their NHS people that brought their OHWB strategy to life, delivering on their People plan and People promise.
3.2 Driver 2: Growing our occupational health and wellbeing services across systems
2.1 Inclusive, needs-driven, and well-resourced occupational health and wellbeing (OHWB): All healthcare organisations can articulate their OHWB requirements strategically and operationally, inclusive of their entire workforce health and wellbeing needs. OHWB services and solutions are well-resourced and fully supported by senior/board-level leaders. This is consolidated within each organisation’s OHWB strategy.
2.2 Integrated service user pathways: All OHWB services are working in an integrated way to improve the health and wellbeing of our NHS people. Services and interventions are inclusive of the entire OHWB clinical and employee support pathway, that holistically encompasses surveillance, proactive, preventative, diagnostic and treatment services, and interventions.
2.3 Common service development framework: There is an established maturity framework that describes core delivery, through to transformative and exemplary levels of OHWB service. This is actively used to drive up standards for both internally delivered, externally procured, and hybrid models of service delivery.
2.4 Service innovation: OHWB professionals are actively engaged in work that supports service innovation. They are empowered to lead innovative initiatives and are supported to work collaboratively to realise these opportunities to advance practice.
2.5 Quality improvement: All OHWB services demonstrate a commitment to continual quality improvement by maximising the use of accredited quality management standards and service development tools.
2.6 Maximising technology and digital: The benefits of integrated and innovative OHWB digital technology are maximised. This is reducing demand on OHWB services, increasing OHWB service capacity, and widening access to OHWB services for all our NHS people.
2.7 Integrated care system (ICS) collaboration: ICSs have OHWB as a core part of their people strategy. They are collaborating around OHWB service delivery to maximise their combined OHWB expertise and resources, economies of scale, standardisation of services, increased equity of access, and improved quality of OHWB across all their healthcare organisations – inclusive of all healthcare providers, commissioners, and primary care.
2.8 Improving access to OHWB for smaller healthcare organisations and primary care: There is improved and equitable access to the benefits of OHWB services and interventions in smaller healthcare organisations, including primary care.
We have an opportunity to grow OHWB services to inclusively meet the needs of our NHS people across our diversity of healthcare organisations. This will mean empowering OHWB with the same service improvement tools and resources that our external patient facing services have been encouraged to use for some time. The key difference being that our NHS people are the service user or ‘patient’ in the eyes of OHWB.
Health and wellbeing is different, to different people, needing different things, at different times. To maximise the impact of OHWB, we need to grow needs driven OHWB services that inclusively support the diversity of our workforce, in their local context, and deliver this in a compassionate way. This will involve equipping OHWB professionals and services to work in a unified way across integrated service user pathways. This must cover the health surveillance, preventative, and proactive elements of improving health and wellbeing, through to supportive diagnostic, treatment services, and employee assistance programmes, when our NHS people present themselves with periods of ill health or long-term conditions that require adjustments to enable them to return to work and keep working. Population health management approaches will support the strategic planning and delivery of services that address the needs and desired health outcomes of our NHS people, including addressing health inequalities, underpinned by improved data driven decision making.
To achieve this, all NHS organisations must be able to clearly articulate the needs of their workforce, whether they are smaller primary care practices, healthcare commissioning functions, large healthcare provider organisations, through to collaborative organisations across ICSs. This will require maximising the use of strategic health and welling service improvement tools such as the NHS health and wellbeing framework to help organisations and ICSs to develop their localised OHWB strategies, their service delivery plan, and inform investment requirements. To help grow OHWB services in a forward-thinking way, we will need to develop new service improvement tools, such as a common OHWB service development framework that flexibly outlines what ‘good to great’ looks like in service delivery and unites OHWB services in how we develop and transform services. To drive up the quality of our OHWB services, we must also maximise the use of accreditations and quality improvement tools such as Safe Effective Quality Occupational Health Service (SEQOHS). This will ensure that internally delivered, externally produced, and hybrid models of OHWB service delivery are of high quality.
Technology and digital is a significant enabler for OHWB. We have opportunities for ‘quick wins’, such as improving access through video consultations that became increasingly popular throughout the pandemic. We also have the opportunity to improve the clinical aspects of digital OHWB, such as improving usability and integration of OHWB workflow and patient database systems so that these better support health surveillance, diverse workforce needs, and the investment in preventative OHWB interventions. We can better use the capacity of our OHWB people by making these systems easier to use while also empowering OHWB with usable data that demonstrates the impact of their services and informs decisions around health and wellbeing. There is also potential to further invest in digital OHWB services such as ‘apps’ that better support our NHS people in improving and managing their own health and wellbeing. This, in turn, further improves the capacity of OHWB to work more strategically and focus on complex health needs. This will require further work to understand the potential for digital and technology in the OHWB space, build on what is working well already, and collaboratively influence the OHWB technology and digital market to better serve our NHS.
Collaborative OHWB service development work across ICSs is also essential. ICS leaders will need to work with their OHWB people across all their organisations to ensure that they to truly understand the needs of their entire workforce. They will need to ensure that these needs are represented in their system-wide people strategy, and then work collaboratively to resource, develop and/or commission services that achieve these needs across their system. Working across a system geography empowers OHWB professionals to work collaboratively and explore opportunities for truly integrated working across systems that maximise the contribution of their collective skillsets. It also provides the benefits from economies of scale to get better quality and value from locally delivered and/or jointly commissioned services, to ‘go once, go together, and go well’. Having a system-wide approach to OHWB services also enables a collaborative approach to driving up equitable access to quality OHWB services across all local healthcare organisations and provides a more streamlined experience for NHS managers and NHS people accessing these services. While every system will need to do what is right for their local organisations and workforce, this is likely to require collaboration, strong leadership, empowered service development, integrated and multidisciplinary models of service delivery, investment and resourcing, and cultural change.
We need to better support equity of access for smaller healthcare organisations such as those in primary care. This will require further work to explore potential OHWB service models for smaller healthcare organisations, demonstrate the value of OHWB, and encourage resourcing and investment. There is also potential to maximise the opportunities to grow OHWB in smaller organisations that have been put forward within Health is everyone’s business and alignment to wider national work in this area across all sectors.
Above all, our multidisciplinary family of OHWB professionals must be in the ‘driving seat’ and empowered by supportive healthcare leaders to drive the development of our OHWB services so that they are delivering what is needed for their local healthcare workforce.
Case Study: Developing a consolidated occupational health service across North Central London Integrated Care System
In 2019, North Central London Integrated Care System (NCL ICS) set itself an ambition of establishing a single, consolidated, clinically excellent occupational health (OH) service that consistently delivers high-quality, cost-effective services to all NHS staff working across the ICS. The aims of this were to:
- Move from a reactive, medicalised model to a proactive biopsychosocial model of care.
- Explore the use of other staffing groups and skill mix to help manage demand.
- Improve career pathways for occupational health and wellbeing (OHWB) professionals.
- Automate transactional administrative processes, to free up clinical and development time.
- Improve resilience of OHWB services.
- Provide equity of access to a broader range of services for all employees within the ICS, including psychology and musculoskeletal provision.
Collaborative leadership, shared resources, and putting OHWB professionals in the driving seat enabled this aspiration to become a success. Leaders worked together across the ICS and jointly prioritised funding from existing budgets for OH service development. The project involved eight partner organisations, with a collaborative of 40 OH professionals. The vision for a shared service and supporting clinical and operational models were co-designed by leaders from within these services.
NCL ICS successfully launched the new consolidated OH shared service in May 2022, as part of its corporate services partnership – North London Partners Shared Services. The integration of a single clinical OH IT system for use across the ICS will continue throughout 2022. As the new service grows, the aspiration is to share the benefits with other partners within the ICS including primary care, and other NHS organisations outside of North Central London.
Case Study: Developing a collaborative approach to delivering occupational health and wellbeing (OHWB) services in Hampshire and Isle of Wight Integrated Care System
Working across one of the biggest integrated care systems (ICSs) in England, occupational health and wellbeing (OHWB) leaders in Hampshire and Isle of Wight (HIOW) saw the opportunity to expand their programme of strategic and operational development that had been launched to respond to the NHS people plan, to include growing OHWB services. The groundwork was already in place, thanks to a strong history of local NHS organisations working together collaboratively and existing trusted strategic relationships. Leaders were keen to incorporate an OHWB workstream into the ICS Health and Wellbeing programme, recognising the greater impact that could be realised by aligning services and taking a high-level holistic view of services, staff, and provision.
The ICS team began by undertaking a comprehensive gap analysis to identify best practice, the opportunities to improve, and gaps to fill. There was a particular focus on ‘quick wins’ as well as cost-neutral solutions to build in sustainability into the programme plans. Nine areas of collaborative action emerged from the gap analysis, including:
- ‘Quick wins’ to standardise documents across the ICS and develop an occupational health (OH) passporting process for extra efficiency in intra-ICS organisation transfers.
- The development of a business case to secure funding to set up a connection between one OH IT data management system and ESR (the NHS HR system).
- Developing local education opportunities for aspiring and existing OHWB staff with a local higher education provider partner.
Within the first year of the Growing OHWB programme across the ICS, the following successes were achieved:
- Additional resources were channelled into supporting staff with musculoskeletal (MSK) conditions, with expanded teams in local areas. The focus was expanded to include treating people close to their home, having gained an understanding that for some people to access physiotherapy services where they work involves a long journey that may exacerbate underlying MSK conditions.
- OH teams in HIOW ICS were able to make referrals for additional care for MSK directly, with joint benefits for the individual who gets speedier care, and primary care which has seen a corresponding reduction in demand from NHS people.
- A strong focus on keeping people well and in work in the NHS, with the development of new OHWB services, including a menopause clinic; funding directed into burnout support for senior managers and clinicians; and the development of a new neurodiversity and disability advice service in OH to better support staff and their managers.
These successes enabled funding to be secured for further year’s development of the programme across the ICS.
Case Study: Developing a collaborative occupational health shared service across North West London Integrated Care System
As the North West London Integrated Care System (ICS) began to take shape, the four acute, two community and one mental health trusts within the ICS, with support from the North West London Clinical Commissioning Group (now part of the ICS) identified that their staff would be best served by a single occupational health (OH) provision. This model also had potential for the 360 GP practices in the area and eight local authorities to join in the future.
The development of OH services for the North West London region had been explored by the ICS pre-pandemic, however the onset of the pandemic drew focus to the pivotal role played by OH services and strengthened the strategic opportunity. A shared services option was identified as the best approach, and the vision of a three-tiered OHWB service model agreed. This was designed to meet the needs and complexities of the circa 60,000 North West London NHS people and delivering Safe Effective Quality Occupational Health Service (SEQOHS) quality standard OH using one common OH IT system.
The core model delivers shared practice and expertise across the ICS and enables sufficient commonality to work at scale, for example, using the same processes, documentation, clinical systems, and standardised reporting. The model also consolidates the existing collaboration across ICS organisations, as well as delivering economies of scale and the buying power to afford the best innovative OHWB solutions. These could include wellbeing apps and physio digital triage self-assessment.
Launching in 2021, the team worked with four ‘prototype’ partners forming a ‘mini shared service’ to align documentation, working practices, policies and procedures, and to ensure all were working to SEQOHS service quality standards. Alongside this, parallel workstreams were working with software developers on a common OH IT platform, carrying out a strategic estates review, and scoping the staffing needs required. Successes for this shared service model include:
- Launching a digital self-triage pilot for musculoskeletal issues experienced by staff.
- A well-received peer support and coaching offer for specialist clinical staff to engage them in shaping the future of OHWB services in North-West London.
- Stronger partnership working across the ICS, with a shared focus on keeping staff and patients safe.
The pilot is scalable, and it is anticipated that by the end of 2022 other partners across the ICS will join the initial prototype partners in the shared service, leading to the formation of a wider shared service model in 2023.
Case Study: Providing occupational health services for GPs and their staff in Leicester and Leicestershire
University Hospitals of Leicester (UHL) has been providing an occupational health (OH) service for GPs in the city of Leicester and Leicestershire for 20 years. This was a pioneering approach at the time and is still in the vanguard of innovative OHWB service provision. From the outset, one of the key drivers has been to provide GPs and practice staff with the same access to OH services as staff working in larger NHS organisations.
When initially set up, senior OH nurses from the service visited the 150 practices across the city and the borough to carry out assessments for staff, to work with the GP practices to understand workplace risk, and support the process of risk assessment for all staff working in the practice. This approach has been sustained, despite changes in national specifications and commissioning arrangements, with funding prioritised by the local clinical commissioning group (now the local integrated care system) to respond to local demand. From the outset, the service has been valued amongst the local primary care community, with high levels of demand via self and management referral, and very low-levels of ‘opt-out’ from the service contract. UHL OH service have also been local partners in working with the practitioner health programme for primary care, promoting the correlation between workplace factors and performance and assisting practitioners to remain in practice
The benefits of this approach became even clearer during the pandemic. At the start of pandemic, the UHL OH team’s remit to urgently develop and support the risk assessment process naturally included those in primary care. This provided a unique whole-system view of staff at higher risk across Leicester and Leicestershire and their insight proved vital to the national work developing a national risk reduction framework for NHS staff at risk of Covid-19 infection. Bespoke advice and information were also provided to those local practices with staff at higher risk.
The UHL team tracked the impact of the provision of OH services to GPs over nearly 20 years, noting and sharing some of the unique OHWB challenges faced by primary care providers, as well as common causes of workplace risk, across the wider NHS knowledge base. As well as ensuring GP staff are kept well and safe, there has been significant skills transfer between OH professionals and the primary care community in Leicester and Leicestershire. This has taken the form of more practices feeling confident to carry out workplace risk assessments, reflecting a wider understanding of OH and workplace risk factors. Research has also shown that there are key benefits provided by extended OH consultations by general practitioners, which can achieve positive self-reported outcomes for patients in employment. The GPs of Leicester and Leicestershire, with a deeper understanding of OH, have fostered years of collaborative working with the UHL OH team and have been pioneers in this area.
Case Study: Driving up service quality by using the safe effective quality occupational health service accreditation across North East and North Cumbria Integrated Care System
The North East and North Cumbria (NENC) Integrated Care System (ICS) recognised the need to improve the quality of future occupational health (OH) services in four of its provider trusts through achievement of the national Safe Effective Quality Occupational Health Service (SEQOHS) accreditation. A key objective of their programme was to improve communication and collaboration between the trusts and in turn enable the standardisation of best occupational health and wellbeing (OHWB) practice across the region. One of the key strands was to develop a collaborative approach between the trusts, working with key stakeholders to support each other with the SEQOSH accreditation process. A gap analysis tool was used to identify where learning could be shared.
The benefit of this approach has led to a reduction in time spent by OH professionals on the accreditation process and released capacity to deliver a wide range of OHWB services to their patient group (ie NHS employees). In addition, the project has supported the development and promotion of OHWB at a strategic level within the wider health and care system.
3.3 Driver 3: Growing our occupational health and wellbeing people
3.1 Multidisciplinary occupational health and wellbeing (OHWB) workforce planning: A new, national OHWB workforce development plan is in place and representative of the multi-professional OHWB family of roles that collectively contribute to improving the health and wellbeing of our NHS people. This plan includes growing capacity and capability of existing professional roles (for example, occupational health (OH) physicians and OH nurses), growing newer roles (for example, wellbeing leads, OH allied health professionals, wellbeing guardians, and wellbeing champions) and innovating in new roles (for example, chief OHWB officer, health business partner, OH apprentices). National NHS bodies and partners are working in a united way to deliver this workforce plan.
3.2 Attractive career pathways and talent management for OHWB professionals: The family of OHWB professions in the NHS is seen as a valued and attractive vocation. Career pathways in OHWB are clear, accessible, and inclusive of a variety of professional entry routes, both clinical and managerial. A talent management approach is used to ensure that there are sustainable talent pipelines, and we are growing our OHWB talent to maximise their potential. This is considered at organisational, integrated care system (ICS), and national levels.
3.3 Credible and accessible OHWB education and training: Credible professional training and education enables entry into the OHWB family of roles through a variety of flexible pathways. Higher education partners and expert OHWB bodies are working collaboratively to develop the family of OHWB professional vocational roles in the NHS.
3.4 Empowered OHWB leaders: Through professional development and peer learning, OHWB leaders are enabled to effectively lead their teams, develop their services, and enable innovation in OHWB.
3.5 Empowered OHWB workforce: The multiprofessional OHWB community are enabled to collaboratively develop their skills, capabilities, and specialised practice through a combination of personal development and peer development opportunities.
3.6 Developing all NHS managers in supporting employee health and wellbeing: All NHS managers are supported to look after their own health and wellbeing and are empowered to pass this wellbeing on to their teams. They are trained in basic health and wellbeing skills, are confident to engage in good wellbeing conversations with their employees, and are actively signposting and supporting interventions that improve their employees’ wellbeing.
We have an opportunity to grow our multiprofessional family of OHWB practitioners, with the skills, quantity/increased capacity, and ability to rise to the opportunities set out in this strategy. By OHWB family of practitioners, we are referring to anyone who contributes to improving the health and wellbeing of our NHS workforce. This includes:
- established OHWB roles such as OH physicians and OH nurses
- emerging OHWB roles such as wellbeing leads, OH physiotherapists, OH mental health professionals and OH apprentices
- wider allied health professionals who are increasingly becoming part of the OHWB family
- newer roles such as the wellbeing guardian advocating the strategic organisational value of OHWB
- wellbeing champions supporting and improving the wellbeing of their team and colleagues in their local workplace.
Health and wellbeing is everyone’s business, and this strategy ambitiously includes developing all of our NHS people to feel empowered to take control of improving their health and wellbeing in the workplace and developing our NHS managers in basic OHWB competencies to compassionately and inclusively support the needs of their team members. To achieve this, we will require long-term workforce planning, investment, and making the OHWB multiprofessional family of roles attractive to work in. It will also require cultural change, as we market OHWB as a multiprofessional family of roles, maximise inter-disciplinary working, and create integrated services and pathways.
Developing a new national, long-term, and multiprofessional OHWB workforce development plan will support national NHS bodies to collaborate in strategically growing our OHWB people and empower local growth in OHWB professions. This ambition will, for the first time, unite OHWB as a family of professions working toward a common goal of looking after the health and wellbeing of our NHS people. It will better enable us to target investment to increase and sustain the numbers of OHWB professionals we need to meet the current and future health and wellbeing needs of our NHS people at local, regional and national level.
However, we also know that currently there are not enough professionals working in this field to meet demand, that we are competing with the private sector for OHWB professionals as a scarce resource, and OHWB is not a well-known, well defined, or easy profession to get into and navigate. To address this, we need to maximise the potential of our existing OHWB workforce utilising a talent management approach to identify people with high potential, develop them to advance their practice, while ensuring that they are in roles that maximise their skills, contribution, and ambition. We must also make OHWB in the NHS an attractive place to work by marketing the benefits of working in the profession. In addition to the values-based benefits of caring for colleagues who go on to care for patients, we can also maximise the inclusive and multiprofessional nature of working in OHWB. We need to develop career pathways that consider the multiprofessional routes into the OHWB profession, inclusive of clinical (for example, OH physicians, nurses and allied health professionals) and managerial pathways (for example, human resource and organisational development wellbeing professionals, as represented in the NHS future of human resource and organisational development report 2021). We can also raise the profile of OHWB as a multispecialty and flexible career. For example, profiling how medical professionals are already working across OH, general practice and public health in flexible careers, and how mental health, physiotherapy practitioners and wider allied health professionals work across OHWB supporting internal NHS employees, as well as external patient facing practice. We must also maximise the positive impact and raised profile of OHWB resulting from the pandemic and how OHWB welcomed a variety of multidisciplinary professionals to join the profession to support increased capacity. This has raised awareness of careers in the field, increased focus on multiprofessional career pathways, and demonstrated that it is possible to join OHWB from a variety of professional backgrounds.
Working with higher education providers and those who lead formal qualifications and training pathways in OHWB is essential, from clinical training such as the National School of Occupational Health and Health Education England, through to managerial and human resources and organisational development pathways such as Chartered Institute of Personnel Development. In addition to finding resources and ways to invest in the existing OHWB workforce, we must also leverage creative ways to grow the profession, such as maximising the use of apprentices. This will ensure that there is adequate and high-quality training available to support this workforce strategy and support professionals wishing to enter and advance their career in OHWB. We must also ensure that our OHWB workforce has opportunities to continually develop their skills and knowledge and to keep their practice contemporary, through wider training and development opportunities. We can connect our community to enable peer support, inter-disciplinary learning, and development across the wide family of OHWB professions.
OHWB leaders must also be supported in their development to be capable and confident to rise to the opportunities outlined within Growing occupational health and wellbeing together and to effectively develop their services. We should develop leaders at all levels of OHWB practice, from future emerging leaders, through to our established leaders.
Developing new and emerging roles is important to widen the reach of OHWB to support creating a culture of wellbeing across our NHS. Developing our new community of wellbeing guardians will ensure that wellbeing is a strategic priority for senior leaders and boards, championing the strategic voice of OHWB. Encouraging all NHS organisations to develop wellbeing champions in each team and service area will provide an additional layer of wellbeing support for our NHS people. We can also explore the development of more strategic level OHWB roles to help raise the strategic voice of OHWB, such as health business partners at organisational level, through to accredited specialists, and strategic OHWB officers at system and national levels.
Finally, we need to develop our entire NHS workforce in basic wellbeing competencies, including supporting managers in being confident to have wellbeing conversations with their teams. This includes the knowledge of how to support each individual’s diverse needs in a preventative and compassionate way, and how to effectively refer them on to specialist OHWB support when needed. This will support us in creating a culture of wellbeing that prioritises a preventative approach, improving the day-to-day wellbeing of our NHS people. This will also support reducing demand on specialist OHWB services, which will increase the capacity of OHWB professionals to maximise the use of their expert skills and release time to focus on the new opportunities outlined within Growing occupational health and wellbeing together.
Case Study: Growing occupational health and wellbeing competencies in North East and North Cumbria Integrated Care System
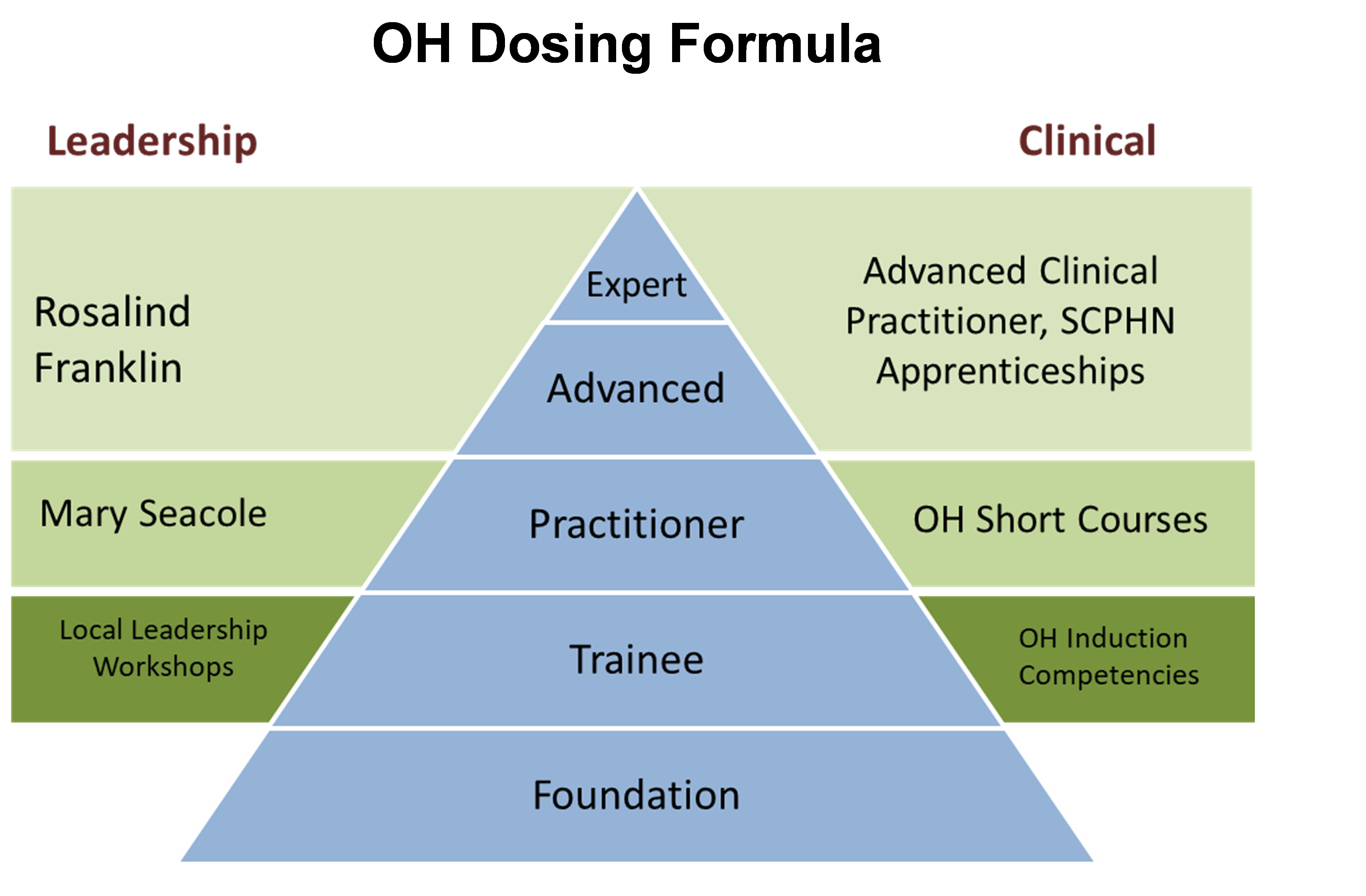
North East and North Cumbria (NENC) Integrated Care System (ICS) has developed a ‘dosing formula’ strategy to develop occupational health and wellbeing (OHWB) skills across four NHS trusts in their central and southern integrated care partnerships.
This approach is underpinned by all employees in each NHS trust being developed to have a foundation of OHWB skills, which creates a culture of wellbeing by empowering each employee to take control of their health. It includes knowing what services are offered, how they can refer and what health promotion materials are available so they can self-manage their health and wellbeing.
The multi-professional OHWB service team are also being developed through career pathways, which also attracts more people into the profession. Those entering OHWB as ‘trainees’, undergo a competency-based induction which is overseen by an advanced member of the clinical team. For those who have completed their competencies, they can access OHWB short courses such as in the areas of physiotherapy, mental health training, health surveillance and vaccination. Advanced members of the OHWB team are able to undergo apprenticeships through links with universities. This is being enabled through developing supportive relationships with local higher education providers and utilisation of the range of available apprenticeships and the development of bespoke short courses in OHWB.
Case Study: Developing all employees and managers in health and wellbeing at Manchester University NHS Foundation Trust
Employee health and wellbeing (EHW) services at Manchester University NHS Foundation Trust (MFT) are working to create a culture that enables open and honest conversations around mental and physical health. They have developed a comprehensive training package for staff and managers to develop their skills and confidence in health and wellbeing, which acts as an enabler to this cultural change, and helps to raise awareness of the wide range of services available to support them. There are a wide range of courses available, including decompressing after a critical/traumatic incident in the workplace, mental health conversation training, and a new dedicated health and wellbeing leadership course.
This leadership course equips managers with the necessary training and resources to develop their skills and confidence to support the physical and mental health of their staff, especially when their wellbeing is impacting their work. In only several months, over 250 managers engaged with this training, and there is an extensive waiting list based on its popularity. Feedback is positive, such as:
Employees are also encouraged to become part of the Mental Health First Aid (MHFAs) and Wellbeing Champion programme to help influence and reduce the stigma in talking about health and wellbeing, and to create a positive culture that supports the mental and physical health of MFT employees.
The EHW service are also providing further training and professional development for specialists within internal EHW services. EHW physiotherapists can access upskilling courses provided by the Association of Chartered Physiotherapists in Occupational Health and Ergonomics to ensure they meet the criteria for delivering an EHW service. Rehabilitation specialists are supported to attend a vocational rehabilitation course accredited by the Health and Care Professions Council and the Vocational Rehabilitation Association.
3.4 Driver 4: Growing occupational health and wellbeing impact and evidence-based practice
4.1 Using data to demonstrate the impact of occupational health and wellbeing (OHWB): OHWB services are using common quantitative and qualitative output-focused metrics, data, and service evaluation methodologies to demonstrate their impact. This routinely forms part of organisational and integrated care system (ICS)/system-level board discussions, where wellbeing guardians (or equivalent assurance roles) actively hold organisations to account for improving the health and wellbeing of their NHS people.
4.2 Driving OHWB practice: The NHS is recognised for driving best practice in OHWB. OHWB research and innovation is supported, and best practice that advances OHWB is captured, shared, scaled, and spread.
4.3 Demonstrating the value of OHWB: Impact data is continually built upon to clearly demonstrate the value proposition for OHWB in keeping our NHS people well and delivering quality patient care, as part of a wider integrated people strategy.
4.4 Driving the OHWB market: The united and collaborative voice of OHWB in the NHS is driving up service standards in the OHWB market. This is enabling higher quality, needs-driven, value for money, and impactful OHWB services, interventions and support (both internally delivered, and externally procured) that benefits NHS organisations and NHS people.
4.5 Demonstrating the impact of this strategy: The Growing occupational health and wellbeing together strategy is regularly reviewed to establish how all healthcare organisations, systems and strategic partners are supporting realisation of the vision and to oversee progress across all areas for collaborative action.
We have an opportunity to demonstrate the value and impact that OHWB has on creating a culture of wellbeing by supporting our NHS people, and the value chain in delivering quality patient care. Demonstrating the value and return on investment in OHWB in this way, will support the case for continued investment in the service. While OHWB is a common service across all industries and sectors, being the NHS and health being our primary business, we have an opportunity and duty to ‘lead the way’ in OHWB practice.
To achieve this, we will need to maximise how we collect, analyse, and strategically use OHWB data. A standardised approach to using data will enable a common way for all healthcare organisations to demonstrate the day-to-day value of OHWB services. We will need to outline common metrics and key performance indicators for how OHWB contributes to a well running healthcare organisation. We should leverage both quantitative (ie statistical) and qualitative (ie stories and case studies) as sources of data that contribute to this, to ensure a rounded view of the service. While input measures are useful (for example, number of referrals, appointments, waiting times, caseload) we must also focus on output measures if we are to demonstrate the true impact and value of our OHWB services (for example, outcomes of treatment, successful return to work, management of long-term conditions, satisfaction rates with the service, stories from service users, how preventative interventions have improved health and wellbeing, health surveillance data).
We must take a population health management and health surveillance approach to support the strategic planning, decision making, resourcing, and development of OHWB services. Different people need different things at different times. We have the opportunity to empower OHWB to be a needs-driven service, flexibly addressing the diverse needs of our NHS people, addressing health inequalities, and encouraging a preventative and proactive approach to improving health and wellbeing.
Identifying and sharing excellent practice and learning from testing new ideas is important in supporting OHWB practitioners to take a strategic approach to growing practice and continually improving quality of services. This needs to be encouraged through informal routes, such as peer networking and development opportunities, through to more formal routes where practice is identified and shared in a centralised, wide reaching, and national scale. We should also encourage formal research studies into OHWB practice. This will increase our formal and academic evidence base, to drive up practice quality and innovation.
Our NHS is complex and there is no ‘one size fits all’ model to delivering OHWB services. While larger NHS organisations will likely have some form of internal provision, many healthcare organisations will likely procure OHWB services. By using a data driven approach, having established service standards, and growing OHWB practice, this will empower healthcare organisations to make better informed decisions when commissioning OHWB services to support their NHS people. This will support the NHS to drive the market for OHWB, increasing the quality and value of provision.
We must also evaluate the impact of this strategy to understand the difference it is making to growing our OHWB services, OHWB people and OHWB practice. We need to understand how it is driving a culture of wellbeing for our NHS people, and ultimately the difference this is contributing to patient care. This will require NHS England, working with its strategic partners as part of the national OHWB Steering Group, to oversee progress and work together and actively monitor and report on the impact of this strategy over time.
Case Study: Using occupational health and wellbeing data to design new multiprofessional services that support and retain staff with the menopause in London North West Healthcare Trust
Occupational health and wellbeing (OHWB) and workforce data in the London North West Healthcare Trust identified a steady rise in the number of female staff being referred to OHWB services with menopausal symptoms. In extreme cases, female staff were also leaving the workforce in their 40s and 50s, citing that they were unable to manage and continue to work while in menopause. With 40% of the trust’s female workforce over 50 years of age, the impact on staff retention and ability to work was a significant issue.
The OHWB team developed a new service to support this, facilitated within existing OHWB team resources and expert networks. They ran regular women’s health sessions, with topics including managing menopause symptoms and the positive impact that nutrition and exercise has. Following the success of this, the trust then provided additional support for anyone wanting to self-refer to the menopause clinic, regardless of previous medical care offered. This service is run by a menopause specialist pharmacist, who was able to prescribe and link in with GP services with a summary of the advice.
Feedback from staff was very positive, and that the support has improved their quality of life inside and outside of work. This approach is keeping staff with high levels of skill and experience in the NHS and reducing staff taking early retirement due to feeling the menopause is unmanageable. One member of staff shared:
Case Study: The Centre for Work and Health in London
The London Centre for Work and Health (LCWH) recently launched as an NHS based partnership with colleagues at King’s College London, University College London, and Imperial College London. Their mission is to formally bring together researchers and academic physicians from complementary medical specialties with policy makers and employee and employer representatives. Their collective strengths will be harnessed and resourced to lead on a long-term and sustainable programme of high quality and impactful research, with outputs that inform government policy and the health outcomes of the working age population. LCWH will form strategic partnerships with funding bodies to enable the delivery of OH research in the UK in the future. The LCWH positioned themselves to provide expert advice and functional support to central and local government bodies and be closely aligned with the future implementation and benefit realisation of growing occupational health and wellbeing.
4. Our evidence base for change
When developing this strategy, we explored the existing and extensive evidence base that informs the future of occupational health and wellbeing (OHWB) services, while also extensively consulting with our stakeholders to co-design our vision and areas for collaborative action together. This section provides a high-level overview of key learning from our co-design work that took place between October 2021 and March 2022.
4.1 The voice of our NHS people
Developing this strategy involved an extensive approach to consultation and co-design over a six-month period. We wanted everyone to have a voice and to feel heard within this strategy and we wish to thank everyone who supported the development of Growing occupational health and wellbeing together.
With the help of national occupational health and wellbeing (OHWB) experts, using the existing evidence base, and led by Dr Steve Boorman, we initially developed Growing a healthier tomorrow as a discussion document to engage our diverse stakeholders, explore their needs, challenges, best practice, and opportunities. Extensive stakeholder engagement and co-design work then followed which helped us to iteratively design, test and enhance the vision and collaborative areas for action within this strategy. We achieved this through focus groups, workshops, surveys, attending network events, collaborative design meetings, and with the support of our expert Growing Occupational Health and Wellbeing Steering Group, who sit under the national NHS Health and Wellbeing Expert Advisory Group.
Stakeholders that we engaged with included: OHWB professionals, wellbeing guardians, human resources and organisational development professionals, executive leaders, NHS managers, NHS employees, NHS trade unions, national OHWB experts and expert bodies. We also examined what was working in practice through engagement with over 60% of integrated care systems (ICSs) who were enhancing their approach to health and wellbeing, and through the support of several ICS ‘trailblazers’ who were doing extensive work in developing a united and collaborative approach to growing OHWB services and professionals across their system organisations.
The following represents a sample of the voices we heard, mapped to our vision and four key improvement drivers:
Vision: Improving the health and wellbeing of our NHS people by growing our occupational health and wellbeing services and people to be trusted, strategic and integrated partners
Driver 1: Growing the strategic identity of occupational health and wellbeing
Driver 2: Growing our occupational health and wellbeing services across systems
Driver 3: Growing our occupational health and wellbeing people
Driver 4: Growing occupational health and wellbeing OHWB impact and evidence-based practice
4.2 The evidence base and strategic national drivers
4.2.1 Demonstrating the value of occupational health and wellbeing
Key benefits provided by occupational health and wellbeing (OHWB) services (adapted from Society of Occupational Medicine, OH Value Proposition, 2022)
NHS Employees
- improved health
- maintain workability
- maintain earnings.
Workforce
- improved attendance
- reduced presenteeism
- improved productivity.
Employers
- improved performance
- lower costs
- increased profits (value).
NHS patients
- improved experience
- improved access
- improved care
- improved health outcomes.
Economy
- reduced cost of healthcare and benefits
- improved gross domestic product.
Investment in occupational health and wellbeing (OHWB0 adds value beyond a financial return on investment, through reduced costs associated with the prevention of ill health, improved health and wellbeing outcomes, improved productivity, and a range of other intangible benefits (Society of Occupational Medicine – Occupational health value proposition, 2022). This includes wider benefits to society as a whole, where having a job is considered one of the most important factors linked with societal wellbeing, and where being in a ‘high quality’ job where an individual’s health and wellbeing is supported at work is even more important (HM Treasury – Wellbeing guidance for appraisal, 2021). While the evidence base for the contribution and value of OHWB is ever-evolving, it is clear that when we care for our NHS people, this positively impacts patient care (NHS England, 2018).
4.2.2 Aligning to national strategy and policy
Growing occupational health and wellbeing together is informed by a variety of national drivers. The NHS of the future will look very different to the service we see today. The NHS Long Term Plan sets out ambitions for new models of care including those that are digitally enabled, the breaking down of organisational boundaries through the establishment of integrated care systems (ICSs) and a shift to focusing on the changing needs and expectations of our populations, including preventive care, and reducing health inequalities. These ambitions should apply not only to future service for the populations we care for, but likewise for future OHWB services for our NHS people. The NHS ‘quadruple aim’ references the need to equally improve NHS employee experience and health and wellbeing, in addition to the historic ‘triple aim’ which focuses on patient experience, improved population health, and increased value/reduced costs.
Health, work and wellbeing is a cross-government initiative to protect and improve the health and well-being of working age people. The impact of employees’ health and wellbeing on performance and productivity has been well documented over the past two decades. It gathered momentum with the publication of Dame Carol Black’s report Working for a healthier tomorrow in 2008 in reviewing the health of working age population, followed by Dr Steve Boorman’s report on NHS staff health and wellbeing in 2009. The initiative was supported by the National Institute for Health and Care Excellence public health guidance for the workplace (Mental wellbeing at work 2009, Workplace health 2015) and the Public Health Responsibility Deal (2012). In 2015, the chief executive of NHS England highlighted the health and wellbeing of NHS staff as a key enabler in moving towards a different NHS.
Health is everyone’s business (2021) sets out a national way that the government is seeking to improve the health and wellbeing of those in work and prevent ill-health related job loss. As part of this policy, the need to realise the benefits of OHWB in the workplace is identified, particularly the need to improve access to OHWB in small to medium-sized enterprises (SMEs). These drivers outline the need to increase the OHWB workforce, better use the multidisciplinary team, embrace new OHWB roles, better use OHWB technology, and encourage innovation, to drive up quality of services, and to provide guidance that supports better purchasing of OHWB services. It also acknowledges that more needs to be done to demonstrate the value and benefits of high-quality OHWB services to encourage investment in them across all sectors.
This is a message that is replicated in the NHS people plan which emphasises the need to ensure we are looking after our NHS people with quality health and wellbeing support for everyone, and this is directly supported through NHS people promise driver of ‘we are safe and healthy’. The NHS health and wellbeing framework supports this, as a national toolkit that demonstrates seven essential elements for organisations to address to create a culture of wellbeing.
The seven elements are:
- improving personal health and wellbeing
- relationships
- fulfilment at work
- managers and leaders
- environment
- data insights
- professional wellbeing support.
It supports healthcare organisations to undertake a needs analysis, create their OHWB strategies, prioritise investment in their OHWB services and interventions, and evaluate the impact of this. Most importantly, it advocates that health and wellbeing is different, to different people, at different times. Therefore, it encourages healthcare organisations to understand the diverse needs of their workforce and build OHWB services and supportive interventions around these needs.
Developing and expanding OHWB as a multiprofessional workforce is also a key strategic driver. This is endorsed by the work of Society of Occupational Medicine, The Faculty of Occupational Medicine and the Future of NHS human resources and organisational development report by NHS England, which outline the need to grow OHWB professionals as a multidisciplinary community, spanning both clinical and managerial professional routes. The Faculty of Occupational Medicine has been in the vanguard of this work, championing core qualifications for OH specialist doctors, nurses and allied health professionals, developing ethical guidelines for occupational health (OH), and providing regular briefings to the OH community on new and emerging clinical needs, including more recently the impact of long Covid. Describing and determining the value of new OHWB roles in the NHS has been the recent focus of publications by the Society of Occupational Medicine and Faculty of Occupational Medicine including work such as defining the value of accredited OH specialists.
4.2.3 The impact of the pandemic
When developing this strategy, we unanimously heard how the pandemic highlighted the importance, value, and impact of good OHWB support for our NHS people. However, it also exposed gaps and inconsistencies in OHWB service provision across our healthcare system, the health inequalities of our NHS workforce, and the strategic imperative to address this. This is supported in the evidence, for example in describing OH as the ‘thin line protecting the front line’ in the Journal of Occupational Medicine which articulates the significant increase in the workload of OH, driven by the pandemic.
NHS organisations working collaboratively across ICSs responded with empathy and agility to the challenges of the pandemic, with OHWB teams developing innovative and integrated ways to support their colleagues. One element, for example, has been the dynamic risk reduction approach in NHS settings, informed by the work of many NHS OH services during the pandemic, with a focus on vulnerable staff groups. This demonstrates how many aspects in this strategy are already being achieved, yet there is still a need to continue to capture, scale and spread innovation and practice arising from the pandemic so that it is not done in isolation.
We also heard the need to maximise the opportunity to harness the increased visibility and understanding of the value of OHWB services following the pandemic. This is especially true for our senior NHS leaders, who have been more involved than ever in actively improving the health and wellbeing of our workforce, and empowering OHWB services to achieve this. As we move through the recovery phase, there is a need to build on this focus and momentum, to ensure that the needs of a healthy, sustainable workforce continue to be met proactively in the future so that the NHS is able to deliver a sustainable recovery of services for our patients.
4.2.4 The evolving needs of our NHS workforce
Improving access to integrated data and increasing capability in the use of population health management approaches has provided us with greater insight into the changing demographics and associated health and wellbeing needs of the NHS workforce. This approach supports our ability to take a strategic, proactive, and preventive approach to the health and wellbeing of our NHS workforce, including addressing the wider determinants of health and reducing health inequalities amongst our workforce in the future.
When writing this strategy, mental health and musculoskeletal challenges continue to be at the forefront of the reasons for poor workplace health. However, there are other evolving challenges that are becoming prevalent, such as the increasing need to address financial wellbeing and its added impact on wider personal wellbeing, and more recently the impact of long Covid. There are also issues that have culturally taken time to address, such as becoming more supportive to women’s health including menopause, appreciating that women make up the majority of our valued NHS workforce. We have seen how people in our communities who have protected characteristics, such as those from ethnic minority backgrounds, LGBTQ+ people, and people with disabilities, have different needs and we need to ensure we are providing tailored health and wellbeing interventions to our diverse healthcare people, rather than blanket approaches.
The way we work is also changing, as are expectations of employers. Digital technology and remote care interventions are evolving, and certain tasks are being automated through use of robotics and artificial intelligence. Greater numbers of employees are working in an agile way because of the pandemic combined with rapid advances in technology. They expect proactive support to maintain more flexible working arrangements and a healthy and sustainable work-life balance. There are also opportunities to explore wider roles and multidisciplinary support for OHWB outside of the traditional workplace, such as the documented benefit of extended OH consultations by general practitioners in achieving positive self-reported outcomes for patients in employment.
Ultimately, the clear message we heard when co-designing this strategy is that we are not working in a ‘one size fits all’ environment. We need flexibility in how we locally improve the health and wellbeing of all our NHS people across the diversity of our healthcare organisations. It is important that NHS leaders take a localised approach to understanding the health needs of their local workforce and respond in a needs-driven way, supporting the investment in and development of needs-driven OHWB services.
5. What next?
Growing occupational health and wellbeing together is a dynamic and long-term strategy. Our ambition is that this first edition of the strategy will cover growth of our NHS occupational health and wellbeing (OHWB) services and people over the next five years. It represents the great work that has already begun in this space, and our collaboratively designed future direction of travel. We see Growing occupational health and wellbeing together as a continuing journey, and each year we will evaluate the impact of our collaborative work to track progress and inform future investment as part of this journey.
Everyone has a part to play in this strategy. This section outlines suggested next steps relevant to our key audience of this strategy, including:
- OHWB professionals
- NHS integrated care system (ICS) and NHS organisation senior leaders
- national bodies.
5.1 Our occupational health and wellbeing professionals call to action
Now is the time to work as a multidisciplinary team of occupational health and wellbeing (OHWB) professionals to unite behind this strategy. Your work in improving the health and wellbeing of our healthcare people is not only valued, but also of vital importance in ensuring that our NHS has a healthy workforce who are empowered to deliver quality patient care.
We encourage you to grow as individuals, as teams, and as a community, to grow your OHWB services to meet the local needs of your NHS people and use this national strategy as your lever to create change. We know that everyone will be at a different part of this journey, and we encourage you to do what is right for you, your service, and the diversity of people that you care for.
NHS England and our partners are committed to helping you on your journey with flexible resources and support. We are also committed to working with senior leaders to champion increased investment in growing OHWB. To get you started on your journey, we encourage you to:
- Use this strategy as a lever to create change that is right for you, your organisation, and your service users.
- Work collaboratively with your senior leaders to ensure there is a clear OHWB strategy and investment plan for your organisation and that this forms part of regular discussions at senior leadership levels. Use the NHS health and wellbeing framework to help you to create this, and leverage the relationship with your wellbeing guardian and/or senior leaders responsible for OHWB at executive level to help give you a voice at a strategic organisational level. Use a variety of data to evidence your direction of travel. Help your organisation to create a preventative culture where wellbeing champions are supporting the wellbeing of their teams, and managers are engaging in supportive wellbeing conversations with each of their team members. Claim your space in leading the creation of a culture of wellbeing.
- Explore ways to unite as a multidisciplinary professional service – if you do not already work in this way. Work together to build an integrated service pathway and interventions to ensure that you have a good balance of preventative, diagnostic, and treatment services based on your local workforce needs. Use service development tools and quality improvement standards to help you to continually grow your services.
- Consider your own development needs when growing the service, your service improvement skills, leadership skills, professional competencies, and career ambitions. Take advantage of the development offers presented to help you grow. Take a talent management approach to maximising your potential, developing yourself and your peers. Build upon your networks and increasingly find ways to work as a community of practice to grow OHWB. Seek out and connect with each other, especially if you are a solo practitioner in your organisation. We are stronger together.
- Act as professional ambassadors for OHWB, helping to build the positive OHWB identity and demonstrate the value and impact that a strong, multidisciplinary OHWB service offers and the value chain in supporting our NHS people, to improve their health and wellbeing, to care for our service users and public. Use data and success measures to support you to demonstrate your value and impact to encourage continued investment in our OHWB services. Share your successes and best practice, to help others to learn from you.
- Work with us nationally and engage in the collaborative work and resources associated with the launch and long-term journey of Growing occupational health and wellbeing together. NHS England and our partners will offer a variety of opportunities to help you to continue to shape the programme of work associated with this strategy, and ways to bring the OHWB community together to work on common opportunities and develop supportive resources to help collaboratively realise the vision in this strategy.
5.2 Our NHS system and organisation leaders’ call to action
We acknowledge that many of our NHS organisations and integrated care systems (ICSs) are already on their journey of growing occupational health and wellbeing (OHWB) and have driven the ambitions within this strategy. We also appreciate that there are many who will be starting out on their journey. NHS England is committed to supporting our healthcare organisations and ICSs throughout this dynamic journey in a collaborative way, and more resources and support will become available throughout the lifetime of this strategy.
At the time of publishing this strategy and being at the start of our growing OHWB journey, we encourage our ICS and organisational boards and senior leaders to consider their position in relation to this strategy, and how they can respond to this ‘call to action’ to invest in and grow our OHWB services and people, with consideration toward the following:
- Understanding the OHWB needs of your workforce: The NHS health and wellbeing framework – diagnostic tool can support you in seeking out data to understand the OHWB needs of your workforce against the seven elements of health and wellbeing.
- Creating a OHWB strategy and investment plan: Following your diagnostic phase, the NHS health and wellbeing framework – toolkit and implementation guide offers a suite of tools to help you to create your OHWB strategy and investment plan. This will help you to identify how to grow your OHWB services, people, and interventions to meet your needs.
- Having a wellbeing guardian in place: A wellbeing guardian is essential to hold your senior leaders to account for improving the OHWB of the workforce, and also is a key role to bring the voice of OHWB to the board and senior leadership team as a key part of the OHWB vision.
- NHS organisations enabling strategic, well-resourced, integrated, high-quality and impactful OHWB services: Every organisation is different, will be at a different stage of their journey and need different things. Some will internally deliver OHWB services, and others will use externally procured OHWB services with varying levels of integration and investment. We encourage organisational leaders to do what is right for your organisation and workforce. In the short term, we encourage all NHS board and senior leaders to work with and empower their OHWB team of professionals, united under this strategy, to work as a multi-professional and integrated team to develop your local ambition for growing your OHWB services, to meet your workforce health and wellbeing needs. If your OHWB service is delivered internally, Safe Effective Quality Occupational Health Service may be a useful accreditation to ensure services are delivered to a good level of quality. More resources and support will be developed over the coming year to support organisational leaders with developing services that are right for their local context and workforce needs.
- ICSs having OHWB as part of their people plan strategy and investment plans: We encourage ICS leaders to work together to understand the OHWB needs of their entire workforce across their healthcare organisations and ensure that they are investing in OHWB as part of their people plan. While developing this strategy and working with ‘trailblazer’ ICSs who are already working toward growing OHWB, in addition to supporting over 60% of ICSs in enhancing their approaches to improved employee wellbeing, we identified many benefits to enabling system-wide and collaborative approaches to delivering OHWB. For example, sharing professional skills and expertise, consistent levels of service, increased/equality of access, and economies of scale. Key learning from this work is that ICS leaders who engage in collaborative approaches are more likely to improve the health and wellbeing of their entire healthcare workforce. We encourage ICS leaders to enable system-wide opportunities to invest in and grow OHWB services, in a way that benefits all partner organisations, and ultimately improves the health and wellbeing of their diverse local healthcare workforce population.
5.3 Our national call to action
NHS England is committed to working collaboratively to realise the vision within this strategy. We are working with our strategic partners as part of a newly formed national Growing Occupational Health and Wellbeing (OHWB) Steering Group chaired by Dr Steve Boorman to collaboratively realise the vision within this strategy. Partners include NHS England, NHS Health at Work Network, the Society for Occupational Medicine, the Faculty of Occupational Medicine, Chartered Institute of Personnel and Development, Health Education England, NHS Employers, the Social Partnership Forum and trade unions, and the Council for Work and Health. We are also grateful for the Department of Health and Social Care and the Department for Work and Pensions engagement as part of their work and health activity. We appreciate the partnership and commitment at this national level, knowing that each of our partners has a unique part to play to realise the ambitions within Growing occupational health and wellbeing together, and supporting our OHWB community and NHS leaders to flexibly realise this vision in their local organisations and systems.
We have created a programme plan for 2022-23 that accompanies this strategy and supports collaborative action for how we are supporting growing our OHWB people, OHWB services, and OHWB impact. Several areas of immediate investment within this plan will include:
- Enabling organisations and systems to create their OHWB strategies and investment plans using the NHS health and wellbeing framework.
- Investing in and developing our OHWB multi-professional workforce and leaders.
- Supporting OHWB service development through a community of practice approach and the co-design of a service development framework to support this, with consideration to internally delivered and externally procured services.
- Creating task groups to work with us to design and enable initiatives that support the realisation of new areas of work to support implementation of this strategy. For example, the effective use of OHWB technology and improving access to OHWB in primary care and smaller healthcare organisations.
- Capturing best practice, case studies, impact data and sharing this to drive up innovation in OHWB practice.
- Working with national strategic partners to align our contributions and ability to support implementation of this strategy and support NHS leaders and OHWB professionals to grow their services.
Growing occupational health and wellbeing together represents a long-term and collaborative journey. We invite everyone reading this strategy to join us on this journey, as the evidence is clear: when we care for the health and wellbeing of our healthcare people, this enables them to pass that wellbeing on to our patients.
Publication approval reference: B1407

