1. Introduction
Personalising outpatients can reduce unnecessary follow-up appointments by enabling patients to have more control of their care.
This guide supports systems and trusts in setting up formalised personalised follow-up in their renal services for kidney transplant recipients (KTRs), and focuses on how remote monitoring (RM) and patient initiated follow-up (PIFU) can be implemented as part of their routine outpatient follow-up care. It supplements the generic Implementing PIFU: guidance for local health and care systems and aims to bring consistency in the delivery of personalised follow-up for KTRs across England.
We estimate about 20–25% of stable KTRs could benefit from personalised follow-up interventions (RM and PIFU), but which patients use them will depend on clinical judgement and shared decision-making (SDM).
This guide aligns with the priorities of the NHS Long Term Plan and the Renal Services Transformation Programme (RSTP), and with the recommendations in the Getting It Right First Time (GIRFT) review of renal services, specifically new methods for delivering outpatient care to reduce inconvenience to patients and pressure on renal services.
It was developed by the Outpatient Recovery and Transformation Programme and the RSTP, with the involvement of stakeholders including nephrologists, renal nurse specialists, primary care clinicians, renal patient charity representatives, patients and implementation managers from renal services and organisations, such as Kidney Care UK, UK Kidney Association (previously the Renal Association and the British Renal Society) and the British Transplantation Society (BTS).
2. National context
Each year in England around 5,500 people start treatment for kidney failure, and around 54,000 are currently receiving renal replacement therapy (RRT) (Getting It Right First Time (GIRFT), 2021), a number that is increasing by 30% a year. About half of these patients will have had a kidney transplant, and this RRT group has steadily increased in size over the past decade (NHS Blood and Transplant, 2019).
As with many specialties, the COVID-19 pandemic has affected both patients and the workforce: KTRs (along with other renal patients) have experienced high COVID-19 mortality, backlogs have built up with the reduction in non-COVID-19 activity and COVID-19-related capacity constraints, including the restriction of kidney transplant programmes, and training of the renal workforce has been disrupted (Hurst et al, 2020).
3. What is personalised follow-up?
Personalised follow-up is follow-up care tailored to a patient’s individual clinical need, circumstances and preferences. It can include interventions such as RM, PIFU and timed care reviews/follow-up (when appointments are planned with the interval between them dependent on the individual patient’s needs).
These interventions can be used individually or in combination to help reduce face-to-face outpatient follow-up appointments for patients when they do not need them for the management of their condition. However, for KTRs they must not replace their routine follow-up regimen, and regular diagnostics and care reviews must continue.
3.1 Remote monitoring
By monitoring a patient remotely (using medical devices, applications, clinical investigation results or assessment tools) a healthcare professional can initiate an outpatient appointment when the patient needs this for the management of their condition. RM can also enable and enhance a patient-centred personalised approach by offering the patient greater involvement in their care and regular diagnostics, as well as reducing their need to travel to hospital to receive diagnostic results. The latter is particularly relevant for patients who need regular diagnostics as part of their follow-up regimen, such as KTRs.
3.2 Patient initiated follow-up
PIFU enables a patient who is under the care of a service, or their carer, to access support when they need it by initiating a follow-up appointment themselves, eg when their symptoms or circumstances change. This may reduce face-to-face routine review appointments where the patient does not need these because their condition is stable; however, for KTRs, routine diagnostic monitoring and timed care reviews will need to be consistent and embedded for PIFU to work as part of a wider personalised follow-up approach.
PIFU is not a new concept in renal services and commonly goes by other names, including open appointments, direct access or patient activated care. The principle, however, is the same. PIFU is the formalised version of these approaches, and more information can be found in the Implementing PIFU guidance for local health and care systems.
4. Why use personalised follow-up in kidney transplant?
Reducing the need to attend follow-up appointments can be particularly beneficial for this patient group who require regular, ongoing outpatient care.
4.1 Benefits of personalised follow-up appointments
Patients and carers:
- saves patients travel and appointment time, parking and travel costs, and also has environmental benefits
- avoids the need to arrange time off work and lost income
- avoids having to arrange and pay for childcare and alternative arrangements to support caring responsibilities while attending the appointment
- reduces anxiety for patients
- empowers and enables patients to book appointments when they need them (PIFU)
- enables self-management by monitoring their health, and increasing their knowledge, skills and confidence in managing their condition (RM/PIFU)
- supports shared decision-making
- diagnostics can be undertaken closer to home (such as those delivered in a community setting or through a diagnostic hub/centre).
Clinicians and service:
- can reduce their caseloads and waiting times
- reduces overcrowding in outpatient waiting areas, due to a net reduction in follow-up appointments
- reduces service costs
- reduces ‘did not attends’ (DNAs)
- improves the use of clinical resources
- delivers the NHS Long Term Plan’s aim of reducing unnecessary face-to-face outpatient appointments where appropriate
- supports recovery as outlined in the 2022/23 priorities and operational planning guidance.
5. Which patients could benefit?
5.1 Remote monitoring
This is not an exhaustive list and any decision to use RM with a patient should be based on clinical judgement and risk assessment.
KTRs who could benefit from RM include those who:
- have access to the required technology for RM (eg a smart phone, or laptop or tablet with internet connection) and the digital literacy and understanding to engage with a healthcare app, website or online platform
- adhere to their transplant medication and treatment plan
- can initiate contact with the service in a timely way – either themselves or through their carer/representative
- have the health literacy and knowledge, skills and confidence to self-manage their follow-up care (eg finding, understanding and using the relevant information), referred to as ‘patient activation’; if they do not, the patient may benefit from support to improve these areas in line with personalised care.
KTRs who require careful consideration for RM (in the context of potential mitigations) include those:
- for whom the healthcare professional has health literacy or digital literacy concerns
- who may not be activated and able to engage with RM
- who cannot easily access the required technology.
KTRs who are unsuitable for RM include those:
- for whom the healthcare professional has safeguarding, consent or capacity concerns
- who cannot access the required technology easily and for whom support to improve these areas will not sufficiently mitigate this risk
- who do not have the knowledge, skills and confidence (referred to as ‘patient activation’) in managing their own wellbeing, and cannot identify when they may need to engage with RM, where support to improve these areas cannot sufficiently mitigate this risk.
- Patient initiated follow-up
Non-condition specific criteria for selecting patients for PIFU are given in Implementing patient initiated follow-up guidance.
KTRs who could benefit from PIFU include those who:
- are stable and at a low risk of urgent follow-up care
- generally are 12+ months post transplant (based on clinical judgement KTRs <12 months post transplant may also be appropriate for PIFU)
- adhere to their transplant medication and treatment plan
- have a good understanding of the clinical indicators that should initiate a PIFU appointment
- can initiate contact with the service in a timely way – either themselves or through their carer/representative
- have the health literacy and knowledge, skills and confidence to self-manage their follow-up care (eg finding, understanding and using the relevant information; referred to as ‘patient activation’); if they do not, the patient may benefit from support to improve these areas in line with personalised care.
This is not an exhaustive list and any decision to place a patient on a PIFU pathway should be personalised using shared decision-making and be based on clinical judgement and risk assessment.
KTRs who require careful consideration for placement on a PIFU pathway (in the context of potential mitigations) include those:
- for whom the healthcare professional has health literacy concerns
- who may not be activated and able to identify when they may need to initiate a PIFU appointment
- who cannot easily contact the service.
KTRs who are unsuitable for PIFU include those:
- who are clinically unstable
- whose regular diagnostic tests (eg blood tests, blood pressure, urine), either before or during a PIFU pathway, indicate they are becoming clinically unstable
- for whom the healthcare professional has safeguarding, consent or capacity concerns
- who would be unable to contact the service in a timely way and for whom any support with this would not be sufficient to mitigate this risk
- who do not have the knowledge, skills and confidence (referred to as ‘patient activation’) to manage their wellbeing and identify when they may need to initiate a PIFU appointment, and for whom support with this would not be sufficient to mitigate risk.
6. Designing a personalised follow-up model for KTR
We recommend that organisations adopt a consistent approach to personalised follow-up interventions, but one that can be tailored to each specialty’s needs and service’s casemix. For KTRs regular diagnostics and care reviews must continue where needed as part of this follow-up care, irrespective of the use of RM or PIFU interventions.
The renal clinical team should have overall responsibility for the development of clear clinical guidance, risk stratification protocols and standard operating procedures (SOP) for the implementation and safe and effective delivery of personalised follow-up interventions (RM and PIFU) in their service. Providers should also ensure high quality education for patients and clinical teams on optimal use of RM and/or PIFU.
Decisions around the clinical appropriateness of personalised follow-up for a particular patient lies with the clinician responsible for their care. The use of a SDM approach is an essential part of this process. The use of shared care agreements (Responsibility for prescribing between primary and secondary/tertiary care, NHS England, 2018) supports the monitoring of patients who may need to be seen face to face. Providers will need to consider their existing infrastructure and ensure appropriate safety-netting procedures are in place to implement personalised follow-up safely.
NHS England regional teams may be able to connect you with organisations that have already rolled out RM and/or PIFU.
6.1 Remote monitoring
Patient-facing digital platforms are already used for self-management and care planning in renal care (see the case studies in Section 10). As with traditional follow-up, the frequency of monitoring should be decided based on clinical judgement and the relevant clinical guidelines.
RM digital maturity
A digital RM system can be a standalone system designed for RM purposes (such as an application or website) or a RM system module integrated into the trust’s main electronic system.
Providers will need to decide which, if any, digital RM solution is most appropriate and feasible to implement. For this, they should review their existing infrastructure, including the digital maturity and ability to access diagnostic results, to determine if it is sufficient or needs to be enhanced to deliver RM locally. Where existing infrastructure needs to be enhanced or a digital RM solution procured, they will need to identify available funding for this.
Advice around procurement can be obtained from your local procurement experts and the National Commercial and Procurement Hub.
RM digital standards
The effective and efficient implementation of digitally enabled healthcare, in this case RM, is underpinned by standards set by the Department of Health and Social Care, NHS England, NHS Digital and the Care Quality Commission:
- Data Coordination Board standards (mandatory under the Health and Social Care Act 2012): clinical risk management in the manufacture of health IT systems and the use of health IT systems
- NHS Digital service manual and NHS service standard
- UK Service Standard and Technology Code of Practice.
Further resources to support the use of RM include:
- Supporting care with remote monitoring, which includes case studies
- UK Kidney Association and BTS’s Clinical practice guideline post-operative care in the kidney transplant recipient, in particular guideline 1.3 – kidney transplant recipients: Patient access.
- Patient initiated follow-up
Resources to support implementation can be found on the PIFU FutureNHS page, such as SOPs and guidance. When considering the use of PIFU for KTRs, any required regular diagnostics and care reviews will need to continue as part of follow-up where needed.
Clear processes and procedures should be in place for patients to initiate PIFU appointments, with this information conveyed clearly to patients and, where appropriate, their carers. Patients must be given the number or email address to use and a personalised summary of when to initiate a PIFU appointment, and services must diligently communicate any changes to this information to all patients on a PIFU pathway.
PIFU: Triage and target response times
- Waiting time between a patient activating a PIFU appointment and review of the PIFU request by a clinician should be no longer than 2 working days.
- If a PIFU appointment is appropriate, the wait time between initiation of the PIFU appointment and the appointment itself should be determined by an appropriate clinician, but it should be a maximum of 48 hours (urgent) or 7 days (not urgent).
When a patient initiates a PIFU appointment, the contact should be triaged; for example:
- Does the reason for contact meet red flag criteria?
- Does the reason for contact fall within the remit of a PIFU appointment?
- Does the patient need to be seen face-to-face or would a remote appointment be appropriate?
Associated response times for any red flag symptoms should be in line with the trust’s guidance on response times.
PIFU: Timescales
- A patient will be moved to a PIFU pathway for a defined period, potentially spanning multiple years, or on a continuous basis, depending on clinical judgement.
The timescales attached to PIFU must be clinically relevant and, ideally, personalised to each patient, although we recognise that truly personalised timescales can be challenging to implement. Where longer timescale (eg multiple years) are implemented, a clinical review may be used to assess if a PIFU pathways remains suitable.
Generally, PIFU uses both:
- fixed-term pathways – where PIFU is offered as a service for a predetermined length of time, eg 2 years
- continuous pathways – where a patient with a long-term condition has ongoing access to a specialist team when they feel they need it.
The type can be agreed with the patient through a SDM process at the point they are placed on the pathway, and this must be clearly documented.
Timescales for PIFU pathways should be decided at a local level, as appropriate for the service and patient, enhancing the existing regular diagnostic monitoring and timed care reviews.
PIFU: Action at the end of the timescale or during reviews
When a patient reaches the end of a fixed-term PIFU pathway, the clinician will decide the appropriate action based on the agreed PIFU plan. For patients on either fixed-term or continuous PIFU pathways, during any follow-up appointment the clinician should review the appropriateness of the PIFU pathway with the patient, and any shared decisions about ongoing follow-up will be added to the clinical outcome form and clinical records, and the GP notified. The patient or carer should receive confirmation of any decision through their preferred communication route.
7. Implementing a KTR personalised follow-up model
7.1 Timed care reviews
The UK Kidney Association and BTS’s Clinical practice guidelines for post-operative care in the KTR recommends patient-centred care reviews for KTRs. These should include:
- consideration of bone health
- a full assessment of the skin
- addressing concerns in medical, social, psychological and sexual domains
- access or referral to a renal dietitian, social worker, specialist renal pharmacist and psychologist or counsellor (and these should be readily available)
- other matters affecting the patient’s health.
7.2 Personalised care – shared decision-making
Personalised care approaches operated through personalised follow-up can effectively empower and enable patients to better manage their condition. Organisations should be able to show evidence of SDM, such as by documenting the discussion as described in NICE’s SDM guidelines.
When offering a patient RM or PIFU, there should be a SDM conversation about whether this is an acceptable option for them, and the patient reassured that they can decline without this decision affecting their ongoing care. Even where the clinician and patient agree that RM or PIFU is a good option, the patient should be able to return to a traditional follow-up pathway at any time if RM or PIFU no longer works for them due to a change in their condition or circumstances.
The SDM conversation needs to be holistic and include:
- why the KTR is suitable (or unsuitable) for RM and/or PIFU
- details of the pathway (eg the pathway timeframes if applicable, what happens at the end of any timeframes, details of any platforms or procedures that may need to be used)
- any mitigations to support the patient to use the RM and/or PIFU intervention.
The patient should have the opportunity to ask questions and raise concerns.
The Personalised Care Institute’s eLearning resources include case studies and an SDM readiness assessment.
The agreed plan should be recorded in the patient’s medical records and a copy given to them or their carer. When a personalised follow-up pathway has been confirmed, the clinician will need to record this on the trust clinical outcome form (COF), identifying that the patient is now on a personalised follow-up pathway (RM and/or PIFU) and describing all relevant details of the pathway.
7.3 Remote consultations
The decision around the clinical appropriateness of remote consultation for a particular patient appointment lies with the clinician responsible for that patient’s care.
Remote consultations (telephone and/or video) offer the patient, clinician and organisation a range of benefits, including greater flexibility in the provision of care; however, there may not be savings in terms of clinician time (GIRFT, 2021). These gives KTRs greater choice in the way they are cared for, as well as the opportunity to reduce trips to hospital. Also, patients are less likely to cancel or not attend remote appointments compared to face to face (The Strategy Unit, 2018).
Clear written protocols, SOPs, patient information and risk assessments are needed to support the safe and effective use of remote consultations.
Further resources to support the use of remote consultations (telephone and/or video) include:
- The UK Kidney Association’s remote working in nephrology review of the London kidney teams’ response to COVID-19
- Video consultations for NHS secondary care providers (FutureNHS page)
- A guide to video consultations for providers
- Illustrated guide for clinicians and for patients
- Video consultation one week implementation guide (FutureNHS page)
- Choosing how to meet your patients: a quick guide to remote consulting in secondary care (FutureNHS page).
7.4 Engagement with patients and patient groups
KTRs must be involved in the development of any local KTR personalised follow-up guidance, SOPs or patient information leaflets, to ensure a patient voice is present in these materials. This can be obtained through initiatives such as patient groups, direct patient involvement, co-production of materials and stakeholder engagement at patient representative organisations. NHS England has produced guidance on patient and public participation for all commissioners of health services.
8. Risks and mitigations
Safety net information can be found in Ensuring high quality of care when using PIFU.
Identified risks and associated mitigations for RM and PIFU include:
Patients on a personalised follow-up pathway may become lost to follow-up if they do not contact the service, resulting in worse clinical outcomes. This could also result in non-compliance with GMC good practice guidance in terms of prescribing without adequate supervision.
Actions:
- Build in safety nets: if patients do not contact the service within a certain timeframe, or do not attend for their regular diagnostics, a review is activated.
- A process should be in place to ensure that any required regular tests (eg blood tests, etc) are reviewed in a timely way.
- Ensure GPs are aware their patient is on a personalised follow-up pathway and that they can trigger an appointment if necessary.
Some patients may not recognise when they need to seek specialist help and advice, and their condition deteriorates as a result.
Actions:
- Careful patient selection and education.
- Good patient education and information about their condition and relevant self-management strategies at the outset.
- Signpost patients to available help and support in the voluntary sector.
- Provide clear patient guidance on how and when to contact the service.
Some patients may be reluctant to contact the service to seek help and advice despite being aware that their condition is deteriorating.
Actions:
- Careful patient selection and education.
- Ensure GPs are aware when their patient is on a personalised follow-up pathway and that they can trigger an appointment if necessary.
If patients contacting the service do not access specialist help and advice in a timely manner they may lose trust in the system.
Actions:
- Ringfence capacity for personalised follow-up (RM and/or PIFU).
- Ensure appropriate administrative and clinical capacity from the outset.
- Start small with a carefully defined group and gradually build up.
With regards to PIFU, some patients may access the service too frequently, resulting in reduced capacity for others and increased pressure on clinics and staff.
Actions:
- Careful patient selection and education.
- Good patient education and information about their condition and relevant self-management strategies at the outset.
- Clear patient guidance on how and when to contact the service.
- Discussion with patients about why they have initiated contact and their concerns, with signposting to voluntary sector support.
- Offer other personalised care interventions, eg peer support and social prescribing.
- Ensure that agreed access times are maintained, and a triage system is in place – otherwise patients may book unnecessary appointments ‘just in case’.
With regards to PIFU, staff burnout due to seeing more complex patients, as PIFU appointments are initiated when there is a problem or concern.
Actions:
- Adjust clinic templates to accommodate PIFU appointments.
- Change job plans to accommodate PIFU.
Reduced contact with the service in the traditional way may result in some people feeling disconnected from that service, or needing extra support to feel comfortable and confident in managing their condition.
Action:
- Ensure access or referral to extra support such as from a social worker, psychologist or counsellor (as appropriate) is readily available.
Lack of consistent and embedded diagnostic monitoring may make it difficult to implement the necessary safety nets effectively and safely for personalised follow-up.
Action:
- A process should be in place to ensure that any required regular tests (eg blood tests) are accessible and can be reviewed in a timely way.
Increased personalised follow-up relies on the patient’s ability and awareness to report their health accurately.
Actions:
- Careful patient selection and education.
- Good patient education and information about their condition and relevant self-management strategies at the outset.
8.1 Equalities and health inequalities
Trusts have a legal responsibility to complete their own equality and health inequalities impact assessment (EHIA) for the personalised follow-up services they offer. This will help them understand any inequalities that could emerge and interventions to address them. Personalised follow-up may not be right for everyone, but it is important to consider whether the service design excludes particular groups or individuals and how to address this.
Providers should consider three areas in particular, based on identified key areas of kidney health inequality:
- Impact of race and ethnicity as some groups are particularly disadvantaged in terms of kidney disease, for instance South Asian and Black people are more likely to have a longer wait for a kidney transplant and to require dialysis.
- Impact of social deprivation on developing a kidney condition; people experiencing social deprivation are often diagnosed at a later stage of disease.
- Impact of digital communication and remote appointments (telephone or video) for multiple groups on widening health inequalities if not mitigated. This is particularly relevant when considering the use of RM, where access to and understanding how to use a smart phone, a healthcare app, website or online platform are needed.
9. Evaluating personalised follow-up for KTR services
Tracking patients at all stages of the pathway helps ensure a safe service and good patient experience, as well as forecast impact on demand for services. Implementing RM or PIFU may create challenges for recording and reporting activity, and how to do this needs to be discussed early on.
For RM, implementation of local reporting measures that provide insight into the following (this is not an exhaustive list) would be of value:
- number of people on RM and their diagnosis at any one time
- number of patients moved onto RM in the last month
- number of people who revert from RM to regular follow-up RM (and reasons)
- number of people and their diagnosis who decline RM (and reasons)
- patient experience and feedback
- clinician and administrative staff experience and feedback
- estimation of proportion of patients in the service for whom RM could be used
- potential impact on demand for services.
All providers of outpatient services are required to submit monthly PIFU data to the Provider Elective Recovery Outpatient Collection (EROC) via the NHS England Data Collection Framework. The Recording and reporting PIFU guidance, Provider elective recovery outpatient collection recordings and FAQs support providers in reporting PIFU as part of their submission to the Outpatient Commissioning Data Set. For PIFU, in addition to the data collected through EROC, local reporting measures that provide insight into the following (this is not an exhaustive list) would be of value:
- patient experience and feedback
- clinician and administrative staff experience and feedback
- estimate of future demand on administrative services, eg booking follow-up appointments
- estimate of proportion of patients in the service for whom PIFU could be used
- potential impact on demand for services.
Consider resources that support evaluation such as The Model Health System and NHS England’s quality dashboards; the renal dashboard includes five renal metrics.
For evaluation of equality of access to services, consider linking demographic and protected characteristics data where possible. Patient experience data should also be analysed to highlight any inequalities, support service improvements and contribute to research on patient outcomes.
Organisations should also audit evidence of SDM in follow-up.
- consider using the patient activation measure
- patient reported outcome measures (PROMs) and patient reported experience measures (PREMs) such as the UK Kidney Association’s Annual survey of patient reported experience measure
- staff experience and other workforce productivity measures.
10. Innovation and good practice
There are many examples of how good practice personalised follow-up could look in renal services including:
- Patient initiated follow-up (PIFU) using MyRenalCare remote technology
- PatientKnowsBest case studies
Ongoing pilots (at time of writing) with a focus on renal outpatient care and personalised follow-up are:
- Reducing unnecessary outpatient appointments in kidney care – at Barts Health NHS Trust
- PIFU pilot in a renal population using DrDoctor;.
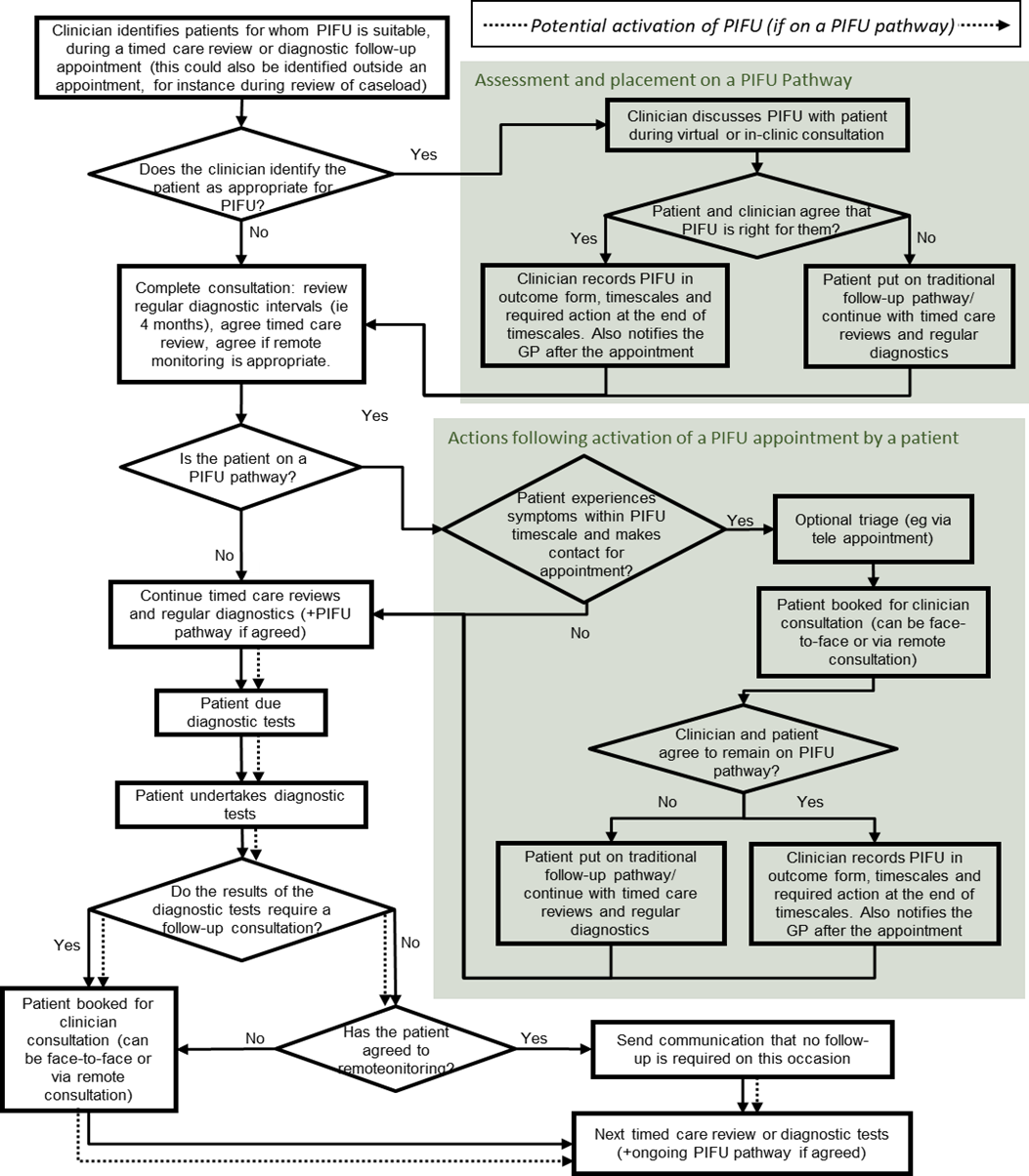
Appendix 1: Example personalised follow-up process for KTR, including regular diagnostics, PIFU and annual reviews
Note: patients can opt-out of RM/PIFU at any point in the process and return to traditional follow-up alongside their care reviews and regular diagnostics. Dotted arrows show where patients placed on a PIFU pathway can activate a PIFU appointment where needed.
Publication reference: PR1213_i

