Foreword
Dear colleague,
Today (24 October) we are publishing the Medium Term Planning Framework – delivering change together 2026/27 to 2028/29 – marking the beginning of a new way of working in the NHS.
It signals the end of the short-termism that has held the local NHS back for so long, providing local leadership teams and boards with the opportunity to break the cycle of ‘just about managing’ by creating the environment and headroom to fix the fundamental problems we face, while in parallel improving care in the immediate term.
It further closes the gap between the national centre and service: the fact that much of what is contained within this document has been co-produced with hundreds of leaders from primary care, acute, mental health, ambulance and community services is testimony to the collective desire to genuinely embrace the change the public told us all they wanted, and drive improvement in every part of the country.
But most importantly, it marks the return of locally-led ambition in the NHS – creating the platform for NHS boards and leaders to truly listen to their communities and drive the change they want and need.
And we’re already seeing the early impact that new-found ambition is having: for the first time in years, elective waiting lists have started to fall, access to primary care is improving with more people saying it’s easier to contact their GP than a year ago, corridor care incidents have fallen sharply and 12 hour waits are down year-on-year for the first time since the pandemic. We’ve even seen a sharper uptake in flu vaccinations across staff and the public in the early part of this year’s campaign.
The same commitment to accelerating improvement is going to need to be seen right across the NHS as we go into the next few months: we need to deliver a strong and safe winter, continue our drive to improve elective performance and maintain our firm grip on the money as this is what unlocks future freedoms.
Just a few short months ago we published the 10 Year Health Plan: today’s publication shows how that reform agenda will drive faster delivery of care now while creating a platform for sustained improvement in the future. It completely rewires how the NHS works, setting out how a new operating model and financial regime will rightly return freedom and innovation to the frontline of the NHS.
Resetting these foundations will enable the NHS to accelerate the delivery of neighbourhood health services, radically transform its approach to quality, and finally embrace the opportunities of digital health to drive improvements in every aspect of its work.
All of this means that the NHS is now able to commit to even more ambitious delivery targets across cancer, urgent care, waiting times, access to primary and community care, mental health, learning disabilities and autism, and dentistry. At the same time, the Planning Framework sees a return to some of the basics that have taken a back seat over the last decade: ensuring providers take the time to better understand what their patients and staff are telling them, and making sure they take action when they fall short.
In short, this is the most ambitious plan the NHS has published in a generation. Over the next 3 years it will return the NHS to much better health – with waiting times dramatically reduced, access to local care restored to the level patients and communities expect, and unnecessary bureaucracy slashed so that savings are poured back into frontline services and staff.
None of what is set out in this Framework is going to be easy to deliver – but the emerging energy for change generated through the 10 Year Health Plan has started to create new optimism in the NHS.
We will continue to challenge ourselves when we fall short of what patients and communities need. Equally, we give you a clear commitment to break down any unnecessary barriers in your way – as we hope we have started to demonstrate over the course of this year.
Our collective challenge goes well beyond improving the care we provide our patients – it’s about ensuring we are the community of staff and leaders that seize the opportunity to put the NHS on a sustainable footing: safeguarding it for generations to come, winning back the public’s faith, and most importantly saving, extending and improving many more lives.
Thank you to all of you who have committed time and effort this year – either through contributing to the 10 Year Health Plan or helping shape this new approach to delivery. Keep up the hard work – it’s very much appreciated.
Rt Hon Wes Streeting MP, Secretary of State for Health and Social Care
Sir James Mackey, Chief Executive, NHS England
Introduction
The NHS is undergoing the biggest change process since its inception: moving away from an era where unparalleled levels of bureaucracy, complicated rules and unnecessary processes have constrained and restricted transformation to a new way of working where local leaders are empowered to drive the change their patients, communities and staff want, and need, to see.
6 months ago, despite a £22 billion injection of additional funding made available through the Autumn Statement, the NHS was predicting a deficit of £6.6 billion for the current financial year, the Public Attitudes Survey showed record-low public confidence in the NHS, staff surveys reflected worrying levels of dissatisfaction among our workforce, and the variation gap between the best and worst performers in the NHS had never been bigger.
In short, service confidence to deliver the commitments the NHS has made to improve access to care and reduce waiting times during this parliament was at an all-time low: due, in part, to a growing disconnect between the centre and the service and an operating model that had become overly bureaucratic and that stifled local innovation and change.
Yet, given the opportunity to contribute to the development of the 10 Year Health Plan, local health and care staff and NHS leaders talked with genuine optimism about what the future could look like – but only if we dramatically changed course on how the NHS is run: empowering local leaders to take more control and moving away from the annual cycle of short-term, centrally directed planning and finance that made it hard to drive real change over the medium and long term.
The 3 strategic shifts and wider transformation areas of the 10 Year Health Plan offer a blueprint for reimagining services, unlocking productivity and redirecting resources to where they can deliver the greatest impact. By embracing this approach, systems and trusts can cut waiting times, improve performance against constitutional standards, and deliver better outcomes for individuals.
The proposed abolition of NHS England is already helping to fundamentally reset the relationship between the centre and the service, so that local NHS leaders can be more supported and empowered to drive accelerated change and improvement on behalf of their patients and staff.
Reviving an ambitious NHS
The early response from local NHS leaders has been fantastic. There’s been a significant, system-wide and disciplined effort to get a better grip of the money, meaning we could start the financial year with plans that projected balance – collectively recognising some of the challenges that lie ahead in fulfilling that ambition. So far this year, these plans are being held in aggregate and for most of the NHS.
The leadership community has also stepped up to the opportunity to shape the way in which we operate in future: integrated care board (ICB) leaders have collectively drafted the Model ICB and have redrawn the map of ICBs to create the platform through which we can do much more effective strategic commissioning going forward, drive greater productivity and better target our resources.
The broader leadership community from acute, mental health, ambulance, community and primary care has worked together throughout the summer developing plans that will see us accelerate delivery of the 10 Year Health Plan. That work forms the basis of many of the commitments set out in this document.
At the same time as more effectively planning for the broader changes we need to see, the NHS has delivered overall improvements in the rate of elective recovery on both referral to treatment waiting times and reducing waiting lists, significant reductions in spending on inefficient use of agency staff, and improvements in access to primary care.
That early progress gives us the foundation to accelerate the pace of reform. The 3-year revenue and 4-year capital Spending Review 2025 (SR25) settlement gives us both the opportunity to move away from annual financial and delivery planning cycles and a real terms increase in funding. Revenue funding will increase by 3% in real-terms over the SR25 period up to £226 billion in 2028/29, and capital spending will increase from £13.6 billion in 2025/26 to £14.6 billion in 2029/30 – equivalent to a 3.2% average real-terms growth across the full SR25 period. This represents a 31.4% and 50% real-terms funding growth in revenue and capital, respectively, since 2019/20.
Regaining public confidence in the NHS is dependent on delivering change that local communities can see and experience – better access to urgent care when they need it; reduced waiting times for elective care; and more convenient access to primary care – all of which can only be delivered and accelerated if we manage our finances well.
But it goes beyond winning back the confidence of the public: improving access to care and reducing waiting has a clear impact on future economic growth. Improving population health and tackling sickness in a more productive way directly impacts on reducing the drivers of health related inactivity, which in turn can make us more productive as a nation. It’s from that economic growth that future investments in the NHS will come. On a macro scale, we can also act as a catalyst for stimulating demand for innovative health technologies, creating a robust market for UK life sciences businesses, and supporting research and development that accelerate product development and commercialisation.
The NHS has signed up to some challenging delivery commitments between now and the end of 2028/29, including:
Elective, cancer and diagnostics
- Elective (including diagnostic) reform and activity to deliver 92% 18-week referral to treatment by the end of 2028/29.
- Improve performance against key cancer standards: Maintaining performance against the 28-day Faster Diagnosis Standard (FDS) at 80% and improving 31 and 62 day standards to 96% and 85% respectively.
- Improve performance for diagnostic waiting times so that the rate of those waiting over 6 weeks is 1% (DM01 measure).
Urgent and emergency care
- Improve A&E waiting times, so that 85% of patients wait no more than 4 hours, as well as reducing the number who wait over 12 hours.
- Improve Ambulance Category 2 performance to an average of 18 minutes.
Primary care and community services
- Improve access to primary care, including reducing unwarranted variation in access. Ensure 90% of clinically urgent patients are seen on the same We will consult with the profession on this new ambition and approach.
- Maintain the additional 700,000 urgent dental appointments per year.
- At least 80% of community health service activity occurring within 18 weeks.
- Community pharmacy: maximise pharmacy first and roll out new services (emergency contraceptives and HPV vaccination).
Mental health, learning disabilities and autism
- 73,500 people accessing individual placement and support and providing 915,000 courses of NHS Talking Therapies treatment.
- 94% coverage of mental health support teams in schools and colleges, reaching 100% by 2029.
- Reduce the number of inappropriate out of area placements.
- Reduce reliance on mental health inpatient care for people with a learning disability and autistic people, delivering a minimum 10% reduction year-on-year.
Delivering all these priorities between now and 2028/29 will only be achievable if we change the way we work together.
This document sets out how we are moving to a new operating model, resetting the financial framework and creating much greater opportunity for local autonomy through the new neighbourhood health approach, a new foundation trust model and the creation of integrated health organisations. It also sets out the early progress being made on reforming our approach to quality, workforce and neighbourhood health, while setting the scene for embracing a crucial new principle that services should be delivered digitally as the default wherever possible. All the work to date has been supported and developed by leaders from across the NHS and much of it is being published in draft this autumn so that the broader health and care leadership community can contribute to these important policy developments.
Using the reform agenda to fix today while building a more sustainable future
For too long, the delivery and reform agendas have been seen as separate conversations in the NHS.
The lack of progress in recovering delivery since the pandemic and the urgent need to dramatically change the NHS operating model to return freedoms and innovation back to local NHS organisations means our central leadership challenge over the next 3 years is how we use the reform agenda to accelerate delivery in the short-term while creating new ways of working that provide the platform for much more sustainable, locally- driven improvement in the future.
The Medium Term Planning Framework provides us with the road-map to achieving this. The reforms to the financial regime set out in this document can help us to accelerate the long-overdue changes to the delivery of outpatient care. Taken together, they can have a substantial impact on waiting lists in the immediate and medium term.
The changes we have set out to reform the NHS App will improve direct communication with patients who are waiting for their care – helping us to reduce ‘did not attend’ rates, which can have a big impact on reducing waiting lists.
Similarly, embracing interoperable technology supports better communication between acute and primary care providers – enhancing how we can use Advice and Guidance, which allows us to provide more appropriate care and reduce waiting times for our patients.
Accelerating the delivery of neighbourhood services – supported in this document by changes to the operating model and the financial regime – can have a dramatic impact on urgent and emergency care performance, simply by reducing the number of frail patients that require hospital beds, freeing up more capacity and increasing the amount of elective work we can deliver.
To support this, the Medium Term Planning Framework sets out the priority deliverables and the reform opportunities that ICBs and providers need to deliver for the next 3 years and the broader strategic aims that will need to be reflected in 5-year plans developed by each organisation.
The priorities in this document are deliberately high-level. We are setting a clear direction on the top priorities the NHS needs to deliver, while allowing local autonomy to meet the needs of local populations. Strategic aims are set out in section 2. Headline targets and multi-year performance expectations are set out in section 3. Supporting publications will provide further detail on the key actions and interventions.
To support a shared understanding of the expected pace of progress, ICBs and providers must develop robust and realistic 5-year plans that outline improvement against these priorities, based on the principles outlined in this guidance.
1. Incentivising delivery and creating the conditions to transform care
1.1 Financial context and discipline
The multi-year settlement provides the foundation on which we can move away from annual to medium-term financial and delivery planning cycles.
Provider and system finance directors and CEOs have been working with the national finance team to develop a new approach that enables:
- better alignment of incentives to enable more robust delivery – payment schemes, best-practice tariffs, deconstructing fixed payment and urgent and emergency care (UEC) payment model
- a move to fairer distribution of funding across the NHS – ICB allocations will move toward the fair sharing of resources and reflect funding streams established in recent years to cover deficits and pay for additional elective activity. Careful consideration will be given to the pace with which we achieve this move. In parallel, a review is underway of components of the broader NHS funding formula to identify any improvements that can further enhance the calculation of fair funding. A review of the Carr-Hill formula for general practice is also under way
- longer-term planning – to support more robust delivery and improved decision-making locally
- a new approach to capital – maximising value from increased public and private capital through a reformed capital regime
This new approach will be underpinned by far greater transparency of increasingly granular financial data – with NHS England committing to publish trust-level productivity statistics on a routine basis to provide transparency on performance. Costing dashboards will also be made available to drill down into provider costs to better understand cost variation.
NHS England will bring together existing tools (including, Patient-Level Information and Costing Systems (PLICS) dashboards, Model Health System, and Health Expenditure Benchmarking), so they are more consistent and coherent.
This will increase and simplify the information available, enabling providers and others to interrogate more granular cost data and support more informed spending decisions.
Existing measures of productivity recognise technical efficiency gains (unit cost reductions, shorter lengths of stay, and increased activity per whole-time equivalent (WTE)). We are also designing a different approach that identifies and incentivises left shift, prevention, and the use of technology to ensure that productivity measures do not penalise trusts for moving lower-complexity activity into more appropriate settings.
In support of better alignment of incentives and to enable more robust delivery, we plan to dismantle block contracts and are proposing to:
- introduce a new UEC payment model for 2026/27, comprising a fixed element (based on price x activity) and a 20% variable payment
- develop an incentive element of the UEC payment model with clinical, financial and operational groups
Findings from the dismantling block contracts work will inform future planning requirements, including the pace of change.
New best practice tariffs will be proposed as part of the 2026/27 Payment Scheme to incentivise a shift to day cases, outpatients, and more efficient ways of working, including the use of technology and alignment with the GIRFT ‘Right Procedure, Right Place’ approach. A consultation on these proposals will take place later this autumn.
The proposed new payment model for UEC is also designed to help unlock funding for neighbourhood health as demand for acute services reduces. A financial/incentive model is currently being developed with pilot sites, available for adoption in 2026/27.
A review of the broader funding formula for the NHS is underway to ensure funding is allocated fairly across the system. The use of funding streams such as deficit support funding and elective recovery funding have become so widespread over the last few years that careful consideration needs to be given to the pace with which we achieve the move to a fair shares model. The conclusions of this work will be detailed in the financial allocations and supporting technical guidance.
Allocations for capital will also be released this autumn, alongside updated guidance on new delegated limits. Business case templates will also be made available through NHS England regional teams to support planning and delivery.
Full details of changes to the financial framework, including multi-year revenue and capital allocations, and updated assumptions will be set out in the accompanying technical guidance published as part of the Medium Term Planning Framework package.
ICBs and providers must now take responsibility for implementation of these changes as part of their work to develop multi-year plans. All ICBs and providers will be expected to deliver a balanced or surplus financial position in all years of the planning period. Plans should incorporate:
- delivery of the 2% annual productivity ambition, as a minimum
- delivery of a break-even financial position without deficit support funding by the end of this planning horizon, other than where, exceptionally, a different expectation is agreed with NHS England
- adherence to other requirements, including guidance on managing provider/commissioner funding changes and a new board risk assessment process
Where deficit support funding (DSF) is in place, non-DSF financial positions should be reported transparently to boards.
Taken together, these measures represent the biggest shake-up of the NHS financial regime in more than a decade – with the aim of significantly strengthening local decision-making, enabling boards to plan much more effectively, and providing local leaders with a rules based transparent framework to drive transformation, not only in their own organisations but as part of their broader system.
1.2 Productivity
In 2024/25, acute hospital productivity grew by 2.7%, and this positive trend has continued into 2025/26, with 2.4% growth in Q1. Despite this, productivity is still below pre-COVID levels. Since 2019/20, the NHS workforce has grown much faster than activity, highlighting the need to decouple workforce growth from service delivery growth. Reversing this trend is essential for long- term sustainability.
While recent productivity gains are encouraging, significant inefficiencies and unwarranted variation persist across the system. There must now be sustained and targeted action to drive further improvements in productivity throughout the remainder of this financial year and over the next 3 years.
This effort has 2 components. First, we must get the basics right – reducing inpatient length of stay, improving theatre productivity, and returning to pre-COVID levels of activity per whole-time equivalent (WTE). Second, we must seize the major opportunities offered by technology, service transformation, and tackling unwarranted cost variation. This includes accelerating the shift to a digital-by-default approach and embedding more efficient models of care across the NHS.
This focus must extend across all parts of the NHS, including acute, community, mental health, learning disabilities and autism services, and primary care, to ensure we deliver maximum value for every pound spent.
SR25’s revenue settlement locks in a requirement to deliver a sustained 2% year-on-year improvement in productivity over the next 3 years. Achieving this as a minimum target is essential to restoring the NHS to its pre-pandemic productivity levels and is a prerequisite for financial sustainability and future efficiency gains.
To support delivery, NHS England will share improved and updated productivity and efficiency opportunity packs, with analysis of these opportunities for all NHS providers. NHS providers and commissioners should use this analysis to identify the local improvement actions they can take over the full planning horizon.
Trust-level productivity measures will also be published monthly as official statistics in development and will be incorporated into the NHS Oversight Framework, supporting transparency and accountability.
Delivering the productivity transformation at scale is fundamental to the plan. It will enable the NHS to reform and respond to growing demand, improve patient outcomes, and maintain long-term financial sustainability.
As part of the wider productivity and transformation agenda, systems are expected to make demonstrable progress on 2 long-term shifts in the models:
1. UEC: transition to digital-first and clinically prioritised access
ICBs and providers should accelerate the shift to a more structured, digital-first UEC model, using clinical prioritisation and scheduling to improve patient experience and reduce avoidable demand.
This shift involves moving away from traditional walk-in demand to models that support patients to access the right care, in the right setting, at the right time, based on clinical urgency and individual need.
This includes:
- expanding digital and telephony-based triage and booking mechanisms
- increasing access to same-day or next- day scheduled care where clinically appropriate
This will help protect emergency departments for the most unwell patients and address crowding – one of the greatest safety risks in UEC.
Organisations should set out in their plans how these approaches will be scaled during 2026/27, including through collaboration with primary care, 111, and community urgent care providers.
2. Outpatients: shift to a digital-first, patient- led model
ICBs and providers must continue to progress towards a digitally enabled, patient-led outpatient model that improves access, efficiency, and patient experience. Priorities include:
- expanding the use of Advice and Guidance and digital triage tools
- empowering patients with greater choice and control over their follow-up care – including access to patient initiated follow up (PIFU), remote consultations and digital monitoring
This transformation should result in a sustained reduction in unnecessary outpatient follow-up activity (OPFU), freeing up capacity to reduce long waits.
Given the variation in baseline position, a uniform national target will not apply.
Instead, providers and commissioners must:
- model the level of OPFU opportunity and compare it against the reduction required locally to accelerate delivery of referral to treatment and long-wait recovery objectives
- develop plans that reflect local opportunity and ambition, aligned to the scale of change required
Plans are expected to be suitably ambitious and progress will be assessed as part of routine oversight arrangements, specifically recognising the evidence that a significant proportion of follow-ups may be clinically unnecessary or avoidable through better use of digital tools and pathways.
2. Resetting the foundations: a new operating model
Over the course of the last few months, we have created the foundations of a radically different way of working: a clearer operating model, a consistent set of rules, and a service more confident in its ability to deliver reform.
The 10 Year Health Plan provides the vision: a system in which care should happen as locally as it can, be digital by default, and be in a patient’s home if possible, in a neighbourhood health centre when needed, or in a hospital if necessary. The operating model now being embedded provides the vehicle to get there.
This new approach is rooted in simplicity and discipline: the NHS is moving to a rules-based system where everyone knows what is expected and what follows.
Success will be rewarded with greater freedom; challenge will be met with real support; and persistent failure will be confronted fairly but firmly. By replacing duplication with clarity and bureaucracy with guardrails, we want to enable leaders to act with ambition and staff to focus on what matters most: better care for patients and communities.
Every part of the system has a clear role:
- the Centre sets national outcomes, codifies standards, builds shared platforms once and well, and removes barriers
- regions are the leadership interface, with a single line of sight across performance, finance, workforce and quality, responsible both for grip and for support
- ICBs are becoming strategic commissioners, moving resources into prevention and community capacity, tackling inequalities and commissioning for value (quality of care and optimal efficient cost)
- providers, through a revitalised foundation trust process, are responsible for collaboration, productivity and quality, with earned freedoms for those who deliver and proportionate intervention where standards slip
- where integration adds most value, integrated health organisation contracts will enable end-to-end redesigning of pathways, with efficiencies reinvested into better and more effective ways of working
- at the frontline, neighbourhood teams will be established to support our communities. Working with social care colleagues, they will deliver proactive support for people with frailty and long-term conditions. They will provide urgent and acute community services, rehabilitation and prevention – and support improved access to care, especially general practice. Their work will be enabled by digital tools and shared care records
The NHS Oversight Framework is the backbone of this system. It will bring fairness, proportionality, consistency, transparency and predictability, measuring access, quality, finance, people, productivity and delivery of the 3 shifts: presenting this information clearly in league tables to ensure that everyone – including for the first time the public – can see how organisations are performing relative to their peers, and what comes next. Boards will be expected to use this to drive improvement.
This model will be supported and enabled at all levels by service transformation through technology, with a default preference that patients interact with services digitally, wherever possible and clinically appropriate.
A suite of documents will sit alongside the Medium Term Planning Framework to bring this to life and to support ICBs and providers to develop 5-year plans that will allow them to transform their services. They are designed to create the conditions for the NHS to start implementing the ambitions of the 10 Year Health Plan.
- Model Region and ICB blueprints are now published, with the Model Neighbourhood Framework expected in November.
- The Strategic Commissioning Framework, which will be shared in October, builds on the Model ICB blueprint to provide commissioners a clear scope for their evolved role.
- A draft foundation trust framework, which will be published for consultation in November as well as a system archetypes blueprint explaining the interplay of the new contract models set out in the 10 Year Health Plan (integrated health organisations, multi- neighbourhood provider contracts and single neighbourhood provider contracts) and a draft integrated health organisation blueprint.
The new Strategic Commissioning Framework will enable the NHS – led by the ICBs – to create a much greater focus on outcomes and to incentivise systems and providers to prioritise investment where the impact on patients’ lives has the greatest potential to be transformative.
Working with ICBs, we will commit to developing a shadow set of outcome measures for 2026/27 building on the NHS Outcomes Framework and international best practice, supporting ICBs to drive better patient outcomes in their commissioning of both internal and commercial contracts.
The NHS Oversight Framework will continue to bring consistency and transparency to performance management and will be updated to include a comprehensive set of metrics to account for different organisations.
Commissioning responsibility for vaccination and screening will move to ICBs – likely from April 2027, subject to the passage of legislation. In 2026/27, NHS England will continue to develop the commissioning and contracting framework that will support ICBs with their new responsibilities for vaccinations and will expand our digital service systems to other providers and vaccinations, in line with the 10 Year Health Plan. Furthermore, subject to consultation on changes to the Human Medicines Regulations, NHS England will enable community pharmacy to deliver vaccinations off-premises, where commissioned.
Providers must continue to deliver regional public health programmes in 2026/27, in line with programme standards, guidance, service specifications and quality assurance requirements.
2.1 Unleashing local potential – a foundation trust framework; integrated health organisations; and oversight of trusts and system models
The publication of the 10 Year Health Plan has unleashed real enthusiasm for re-empowering boards, with early design work on the new foundation trust model being based on excellent governance, organisational self-awareness and transparency: where providers must demonstrate how they will deliver high-quality, efficient services and provide evidence of being good at participating within collaboratives as well as leading their own organisation.
A draft foundation trust framework will be published for consultation in November.
A draft system archetypes document will be published in the same timeframe, setting out how integrated health organisations (IHOs) will be a contract-based delivery method, not a new organisational form, and will explain how IHO contracts work alongside multi-neighbourhood and single-neighbourhood contracts. IHOs will work with the wider provider landscape to deliver high-quality care efficiently, including through sub-contracting arrangements and, where appropriate, delegation of commissioning. We will issue further detailed guidance in a Model IHO blueprint document later this year.
While the draft model is still being designed, early consideration is being given to how:
- NHS England will assess provider capability to take on an IHO contract, with contracts commissioned by ICBs
- IHO contract holders will work to deliver the shift of resources from hospital to community through an integrated and preventative delivery model aligned to neighbourhood health working
- IHO contracts will be responsible for a defined population, building on existing working to improve population health outcomes, allocative efficiency, access and quality. More detail will be given in the model system archetypes publication expected in the autumn
These draft models are being developed in tandem with the design of new oversight arrangements, including reviewing the current oversight model, metrics and provider capability.
The new approach to oversight is being driven by 3 core principles:
- oversight should drive improvement, not bureaucracy
- peer support and tailored interventions, which are sufficiently aspirational and valued, especially when organisations acknowledge their own challenges
- oversight metrics must reflect system- minded behaviours, including addressing inequalities and left shift
We will continue to work with providers and ICBs to refine the NHS Oversight Framework so that it genuinely supports improvement. We will also amend the NHS Oversight Framework to expand to a more comprehensive set of metrics and to account for new models for provision of services, in addition to governance and transaction adjustments for 2026/27, while ensuring alignment with the Care Quality Commission on provider capability.
2.2 Delivering neighbourhood health at pace
Delivering neighbourhood health at pace is central to returning patient and community trust in the NHS, breaking down siloed working among our staff and finally getting control of improving urgent care by providing more convenient and appropriate services in every neighbourhood in the country.
An NHS that isn’t consumed by a near continuous cycle of ‘just about managing’ to deliver urgent care services is realisable – but only if we put our collective leadership effort into making neighbourhood care a reality. The impact on patient and staff morale will be exponential. The delivery of neighbourhood care has to be a priority for every leader in the NHS because it will create more space to do elective work, reduce waiting times, improve the quality of care and make headroom for leaders to focus on innovation.
Most care is already delivered in our communities and neighbourhoods, and many community-based services will continue as they are today. But for those patients that are using multiple services – or are referred from one service to another – we can make a big difference to the individual, as well as to staff, quality of care and productivity, if we can join up or integrate services and teams better. There are also opportunities to improve care through the provision of digital services, empowering patients to manage their own care or to receive digitally-enabled treatment in their own home, complementing community-based services.
The impact we can have by organising ourselves better around the patient on priority long-term conditions such as cardiovascular disease and diabetes won’t just transform how patients get their care, it will dramatically improve productivity in how we deliver services going forward.
This is not just about NHS services working more closely together but also about improved joining up of care across NHS, local authority and voluntary and charitable sector services. By doing this, we will keep more care in people’s neighbourhoods and use our hospitals only for patients who truly need to be treated in them.
There are examples of neighbourhood health working across the country and in every ICB. The evidence from these examples shows they have a significant impact, not just on making services more convenient to access, but supporting improvements in urgent and emergency care, access to primary care and improving patients’ satisfaction. Starting now and accelerating over the next 3 years, we want to deliver even more care in our neighbourhoods, providing more joined up care for high-priority cohorts through integrated neighbourhood teams (INTs), and make a material difference to patient experience and hospital demand.
In implementing neighbourhood health, the immediate focus must be on:
- improving and tackling unwarranted variation in GP access for the whole population
- reducing unnecessary non-elective admissions and bed days from high priority cohorts – people who have moderate to severe frailty, people living in a care home, people who are housebound or at the end of life
- enabling patients requiring planned care to receive specialised support closer to home
Starting this year, we will bring forward a roadmap for the delivery of the NHS App functions as described in the 10 Year Health Plan.
High-functioning systems will want to go further and faster and should be looking to set up integrated teams and services for other cohorts, in areas such as children and young people and mental health and learning disability, autism and ADHD.
To support moving at pace, we will produce:
- a draft model neighbourhood framework, which will set out the definitions, goals and scope of neighbourhood health, along with priority actions for 2026/27
- a national neighbourhood health planning framework, co-produced with the Local Government Association and local authority colleagues, setting out how the NHS, working in active partnership with local authorities and others, can plan for the delivery of the broader set of neighbourhood goals
- model system archetypes, which will outline different archetypes for the commissioning and provision of neighbourhood health services, including the 3 new contract types: single and multi-neighbourhood provider contracts, and integrated health organisation contracts
- model neighbourhood health centres archetypes, which will describe different archetypes of provision of neighbourhood health services that can be used to inform the better utilisation and enhancement of existing estates, together with new-build solutions, where appropriate
From April 2026, ICBs and relevant NHS providers should:
- identify GP practices where demand is above capacity and create a plan to help decompress or support to improve access and reduce unwarranted variation
- ensure an understanding of current and projected total service utilisation and costs for high priority cohorts of those with moderate to severe frailty, living in care homes, housebound or at the end of life
- create an overall plan to more effectively manage the needs of these high priority cohorts and significantly reduce avoidable unplanned These plans should be consistent with national standards for urgent community response services, which require 7-day availability and rapid response. Systems should ensure funding and commissioning covers a minimum 12 hour ‘community urgent care’ offer, supervised by senior clinical decision-makers and operating at a multi-neighbourhood level. Local ICBs must confirm how this will be resourced and delivered
Plans should also include establishing integrated neighbourhood teams, ideally contract-based, working with local authorities and starting in areas of highest need. Further details will be set out in the Model Neighbourhood Framework.
However, providers and systems should not wait for guidance to be finalised where there are local opportunities to rapidly create an approach to neighbourhood delivery that will improve delivery of services this winter. Local leaders are strongly encouraged to work collaboratively to identify these opportunities where they are confident of delivering immediate impact – supporting improved access to urgent and emergency care now.
2.3 Shifting from sickness to prevention
The 10 Year Health Plan is clear that we need to shift from an NHS that focuses on treating patients to one that improves the lives of the population by preventing ill health or slowing the exacerbation of ill health. This approach will improve the outcomes and experiences of patients and improve the management of demand for general practice and acute care services.
ICBs must ensure their 5-year plans support the following preventative goals:
- a significant focus on tackling. Specifically:
- in 2026/27, to be making demonstrable progress in delivery of new obesity service models to improve advice and support, access to treatment, and effective management of obesity, including providing access to weight loss medications and strengthening specialist provision, including complications of excess weight clinics for children and young people
- by the end of June 2028, to have provided access to National Institute for Health and Care Excellence (NICE) approved weight loss treatments for an initial eligible cohort of around 220,000 adults
- by the end of March 2029, to be making 250,000 referrals to the NHS Digital Weight Management Programme a year
- supporting the target of a 25% reduction in cardiovascular disease (CVD)-related premature mortality over the next 10 years, including working in partnership with local authorities to test the new NHS Health Check online service and to scale it across the country
- implementing opt-out models of tobacco dependence in routine care
- reducing exposure to antibiotics to meet thresholds set in recent guidance and addressing problematic polypharmacy to reduce avoidable harm
- demonstrating how they will reduce health inequalities in the exercise of their functions
Further detail on emerging national standards and legislation related to prevention will follow.
2.4 Doing digital differently
The 10 Year Health Plan sets out how we will take the NHS from the 20th century technological laggard it is today to the 21st century leader it has the potential to be.
The health service must become one that is digital- by-default, a principle widely established across government and private services worldwide, but one the NHS has not embraced. A core element of this is giving patients a ‘doctor in their pocket’, available through the NHS App.
Starting this year, we will bring forward a roadmap for the delivery of the NHS App functions as described in the 10 Year Health Plan:
- Delivering My NHS GP – using AI-assisted triage models and data-driven pathways to guide people to the service they need quickly and provide those who need an appointment with the ability to book one.
- Transforming Planned Care – putting patients in control of their treatment pathways by giving them one place to manage all their appointments, referrals and interactions – while bringing efficiencies that reduce referral-to-treatment times.
- Managing My Health – empowering people to manage their health and the health of their dependants by giving them targeted access to prevention services – helping to reduce future demand before sickness develops or worsens.
Through these features, the NHS App has the potential to transform how NHS services are delivered and unlock a range of benefits, including:
- reducing future demand by intervening before sickness develops or worsens
- getting patients to the right service, first time
- reducing the cost of delivering NHS services
- streamlining patient journeys to deliver better outcomes with fewer interactions
- meeting patient needs as efficiently as possible through automation and effective capacity management
- improving the experience of NHS services
Getting this right doesn’t just mean making appointments and other transactional services available online. It means fundamentally rethinking our care models to make the best possible use of technology and innovation and to deliver a high- quality care model at scale accessed through the NHS App, wherever possible.
But we will need to go further, looking beyond the digitisation of transactional and administrative services and more fundamentally rethink care pathways. Modern technology and innovation provide new opportunities to empower patients to manage their own care and receive treatment digitally, rather than face-to-face, wherever clinically safe and accessible for the patient. This enables better care, better health outcomes, a better patient experience and lower cost. We will set out the implementation of this approach through the modern service frameworks, ensuring the clinically- led design of ambitious, affordable and clinically safe digital-first pathways. This shift will free up capacity for those who need it, while making a material contribution to financial sustainability.
To expand the range of options available to patients, work will continue to establish NHS Online – a new ‘online hospital’ to digitally connect patients to expert clinicians anywhere in England from 2027. Using the NHS App, patients will have the option of being referred to the online hospital for their specialist care following a GP appointment. This new model of care will enhance patient choice and control, while helping to reduce patient waiting times.
Those providers leaning heavily into the digital agenda are already achieving substantial performance improvements and cash-releasing productivity benefits. For example, acute trusts leveraging the NHS Federated Data Platform have achieved an average increase of 114 elective surgeries per month per trust and a 35% reduction in delayed discharge days.
Providers and commissioners must therefore prioritise adopting and embedding a modern infrastructure to continue realising these benefits. From April 2026, the NHS must begin to:
- fully adopt all existing NHS App capabilities as a priority, including making at least 95% of appointments available after appropriate triage via the NHS App across all care settings. More widely, providers should ensure full coverage of patients’ abilities to manage their medicines, to view waiting times and contact information, to receive and complete pre- and post-appointment questionnaires, and to implement digital PIFU in line with GIRFT guidance. This should be in place no later than the end of 2028/29
- ensure all providers in acute, community, and mental health sectors are onboarded to the NHS Federated Data Platform (FDP) and using its core products to support elective recovery, cancer, and Trusts should use the FDP for data warehousing and implement the canonical data model. ICBs should use the population health management suite of tools from the FDP for strategic commissioning and adopt the FDP System Coordination Centre and other performance management tools. This should be achieved by 2028/29
- move all direct-to-patient communication services to NHS Notify, terminating local arrangements, and exploit NHS App-based ‘push’ notifications as the preferred method of Transitions should start in 2026/27, with providers completing migration by the end of 2028/29
- move to a unified access model, using AI-assisted triage, that can effectively guide patients to self-care or to the appropriate care setting, through a single user interface delivered via the NHS App but with an integrated telephony and in-person offering
- achieve full compliance with the minimum standards set out in the Digital Capabilities Framework, including ensuring 100% coverage of electronic patient record systems as soon as possible
- implement all core national products and services specified in the forthcoming national product adoption dashboard by the end of 2027/28, prioritising: deploying the Electronic Prescription Service; deploying the Electronic Referral Service APIs; consolidating NHS.Net Connect into the national collaboration service; and integrating all existing NHS App capabilities. This applies to acute, community and mental health providers
- providers should deploy ambient voice technology (AVT) at pace, with due regard to the national AVT registry, and adopt the latest in digital therapeutics for both supportive and wrap-around care (and for direct clinical delivery where services have the appropriate regulatory approvals – typically Class IIa)
2.5 Transforming our approach to quality
The publication of the 10 Year Health Plan ushered in a new era of transparency, driving higher quality care across the NHS. Over the summer, we have worked with system leaders to develop plans to deliver some of the core commitments within the plan, including:
- developing the purpose and scope for a new National Quality Board (NQB) Quality Strategy to be published by the end of March 2026. Following initial discussion with the NQB, wider stakeholder engagement is now taking place to inform the vision and implementation approach that the strategy will set out
- establishing the approach to introducing modern service frameworks (MSFs), which will support more consistent delivery of high- quality, evidence-based, digital-by-default care in conditions where there is potential for rapid and significant improvements in both quality and productivity. The criteria and methodology are being tested through the development of a first set of 3 MSFs, focused on CVD, serious mental illness and sepsis, with further MSFs on dementia and frailty to follow. Task and finish groups are being set up for each, and the frameworks will be co-designed in partnership with clinicians, people with lived experience and system partners
We are also progressing a set of immediate priorities to improve care quality:
- National Care Delivery Standards are currently being developed to ensure the consistent delivery of high-quality and equitable care every day of the week. In November, we will confirm the scope of the new standards and publish them in March 2026
- the Emergency Department Paediatric Early Warning System (PEWS) will be launched in 2026. All hospitals will be expected to ensure a change plan is in place to add PEWs to their transition and complete this transition by April 2028
- a Single National Formulary will be introduced within the next 2 years
All ICBs and providers must continue to implement the NHS Patient Safety Strategy, including embedding the Patient Safety Incident Response Framework to support a systems-based approach to safety and ensuring patient safety specialists are appointed and trained and that patient safety partners contribute to safety-related governance committees. It also involves ensuring full implementation of all 3 components of Martha’s Rule in all acute inpatient settings, as set out in the new NHS Standard Contract requirement.
From April 2026, and as guidance is published, ICBs and providers are also expected to:
- use the new NQB quality strategy to guide local action to improve the quality of care in the highest priority areas for their population and service users
- implement modern service frameworks as they are launched
- implement the National Care Delivery Standards to ensure consistent high-quality care across the week
- plan for the introduction of a Single National Formulary, prioritising the following efficiency savings in 2026/27 to create headroom for adopting innovations: use of best value Direct Acting Oral Anticoagulants, SGLT-2 medicines and the wet AMD Medical Retinal Treatment Pathway
- continue to focus on improving the quality and efficiency of all-age continuing care (AACC) services, addressing unwarranted variation while meeting statutory NHS Continuing Healthcare ICBs should prepare for full transition to AACC Data Set v2.0 and its digital infrastructure by March 2027, replacing the current quarterly collection to improve monitoring
- undertake local process and workflow re- engineering to make sure all colleagues are using digital systems and to remove duplicate paper-based processes, ensuring maximal use of the NHS Federated Data Platform
- for all hospitals with a paediatric inpatient setting, implement the Paediatric Early Warning System by April 2027
Improving the quality of our maternity services
In June 2025, the Secretary of State announced an independent investigation into maternity and neonatal care and a taskforce to agree and oversee the resulting action plan.
Ahead of the action plan being finalised, all ICBs and providers are expected to take immediate action to improve care and ensure women are listened to. This includes:
- implementing best practice resources as they are launched, such as the forthcoming maternal care bundle, new approaches to avoiding brain injury in childbirth, the specification for maternity triage, and the Sands National Bereavement Care Pathway for stillbirth and neonatal death
- using the national Maternity and Neonatal Inequalities Data Dashboard to identify variation in practice and put in place interventions for improvement
- participating in the Perinatal Equity and Anti-Discrimination Programme to support leadership teams to improve culture and practice
The Maternity Outcomes Signal System (MOSS) will be implemented across all NHS trusts by November 2025, enabling the use of near real-time data to monitor key safety indicators such as stillbirth, neonatal death, and brain injury rates. Signals in MOSS prompt a local safety check to prevent further harm and maintain high quality care.
This near real-time data, the maternity and neonatal performance dashboard and the new inequalities dashboard mentioned above, alongside gathering patient experience information and active staff engagement, gives teams, leadership and boards vital insight into the quality of their services. They should stay continuously curious, actively using this information to understand how their services are performing and whether they are meeting the expectations of the women and families they serve. Where there are incidents or things go wrong, they should engage proactively with families, be honest and open, seeking to learn and to implement changes quickly to prevent incidents in future.
2.6 Understanding and improving the patient experience
The British Social Attitudes survey published early this year showed that satisfaction rates are at a record low and continuing to drop. We all have a collective responsibility to address this with absolute urgency.
The progress we’re making in improving access and reducing waits – providing care in a faster and more convenient way – will help with this, but there’s more we can be doing now to better understand why some patients are dissatisfied with the service they receive.
A number of NHS organisations already run inpatient surveys and capture patient experiences in real time. This helps boards better understand the issues patients face and helps local teams identify the changes they need to make to improve the experience of care.
Between now and the end of 2025/26, all NHS trusts will be expected to:
- complete at least one full survey cycle to capture the experience of people waiting for care: Have they had cancellations? Has anyone been in touch? What do they think has got worse since they have been on the waiting list? What information do they need to manage their condition well? This should support delivery teams to improve the experience of waiting and, where necessary, re-prioritise patients who may need to be treated faster
- capture near real time experiences with a renewed focus on ensuring effective discharge processes. Trusts should triangulate inpatient survey results, relevant Friends and Family Test feedback and PALS complaints data to identify areas where improvement is needed. A resource pack will be published on NHS England’s website in November to support organisations to do this
Improving experience of care will be a central feature of the Quality Strategy, due to be published in 2026. This will include cross-cutting improvement priorities which will enhance everyone’s outcomes and experiences.
2.7 Reconnecting with our workforce, and renewing and strengthening leadership and management
Delivering the 10 Year Health Plan will require an engaged and empowered workforce. Creating that means truly listening to what our staff tell us are the barriers they face and acting to address those concerns.
Earlier this year we published a 10 Point Plan to improve the working lives of resident doctors: tackling those non-pay issues that we’ve long since known about but not committed to fully resolving.
It sets a new standard: we need to be unwavering in our commitment to understanding the challenges our local staff face and to fixing those issues.
The annual Staff Survey provides a rich source of data for every organisation, but too often the findings it generates don’t elicit the organisational response our staff and teams want and need.
Over the course of the last few years, the use of national pulse surveys alongside annual staff surveys has sometimes created a confused picture of what staff are trying to tell us. We will commit to working with staff experience leads from the NHS to revise our approach to how we use these tools to better support local boards to be more innovative in how they measure and improve staff experience. We will conclude this ahead of the publication of the latest staff survey results.
In the meantime, every NHS board will be expected to use the 2025/26 staff survey findings to commit to:
- a full and detailed analysis of all free text comments generated through their staff survey
- identifying, as a minimum, 3 areas where the data shows the greatest staff dissatisfaction, generating a detailed analysis where those issues impact most within their organisation and developing detailed action plans to resolve those issues within year wherever possible
Calling out all forms of discrimination
Discrimination, racism, antisemitism, Islamophobia and aggression have no place in the NHS: during the race riots of 2024, local NHS organisations acted as beacons of hope in their local communities – supporting staff in taking an active stand against racism.
The current climate in some of our communities means we need to redouble our efforts to create workplaces where our staff and patients alike feel safe and welcome, and in particular where racism, antisemitism, Islamophobia and discrimination are not tolerated.
We also expect organisations to continue to tackle sexual misconduct, including regularly assessing progress on the Sexual Safety Charter, in line with the letter of 20 August.
Leadership
Successive reports – most recently from General Sir Gordon Messenger and Dame Linda Pollard – have made clear the vital role of high quality leadership in the NHS, and this has never been more important than it will be in the coming years.
While leadership is everyone’s responsibility, our very senior leaders (chairs, CEOs and executive directors) carry specific accountabilities and impact. They must set the tone, standards, and direction that enable colleagues across the health and care system to lead and deliver effectively, improve how services are delivered, and support the vision of the 3 shifts.
The reforms to the NHS operating model set out in Chapter 2 are designed to create the space for leaders to lead, incentivise those who do it well, and support those who need it.
The regulation of managers – widely welcomed across the NHS leadership community – will, when enacted, provide additional clarity on the standards expected and accountability for upholding them, just as is in place for clinicians and other professionals within the NHS.
But the high expectations we rightly have of our leaders must come with the tools and support needed for success – something which has been severely lacking in recent years.
As a first step, we will publish the new Management and Leadership Framework during the autumn, setting a code of practice and standards and competencies for clinical and non-clinical leaders and managers at 5 levels, from entry level to board. ICBs and providers should embed this Framework into recruitment and appraisal practices, with all leaders and managers self-assessing against the Code and standards and senior leaders obtaining 360 degree feedback. Digital tools will be provided during 2026/27 to facilitate this.
Going further, over 2026/27 we will continue progress to establish a new College of Executive and Clinical Leadership. A national curriculum and interactive online modules will be published in 2026/27, offering time-efficient leadership and management development at each level.
National leadership programmes will also be updated, and ICBs and providers should incorporate these national offers as part of personalised development pathways for leaders and managers, linked to agreed development needs and career plans and our new appraisal system.
This new consistent and standards-based approach will help the leaders of today both improve their own practice, and identify and support the leaders of tomorrow.
Finally, it is vital that the benefits of excellent leadership are retained within, and well-spread across, the NHS. Regional teams will work with national colleagues to develop a talent database of our strongest leaders to guide challenged systems and organisations.
2.8 Genomics, life sciences and research
Research in the NHS is vital for generating the next generation of treatments and improving health outcomes, and clinical trials can provide a significant benefit to participating patients by giving early access to new treatments and technologies.
All NHS providers must meet the site-specific timeframes of the government’s 150 day clinical trial set-up target. To support embedding research as part of everyday care, research activity and income should be reported to boards on a 6-monthly basis. This should include details of study set-up performance, how they are meeting the terms of research contracts outside the NHS HM Treasury allocations, commercial research income and how capacity building elements of commercial contract income are used, as set out in the research finance guidance.
From April 2026:
- ICBs should ensure clinical trials are proactively supported, including by reducing the time they take to set up, by following standards and guidance set out in Managing research finance in the NHS
- providers are expected to deliver services in line with the NHS Genomic Medicine Service service specification, including the delivery of genomic testing services and testing strategies as well as clinical functions for cancer, rare disease and population health and the new genomics population health service
3. Trajectories for operational performance and transformation
As outlined earlier, 2026/27 marks the beginning of a new method of planning, with priority targets set for the SR25 period and ambitions covering the first 5 years of the 10 Year Health Plan. Achieving these targets is the bedrock of delivering the shifts outlined in this framework. Without progress, we will fail to realise the ambitions in the 10 Year Health Plan and lose any progress we have made in stabilising the NHS for the future.
Alongside meeting these key targets, the NHS must develop plans that enable systems to deliver healthcare that follows best practice standards and meets the needs of local populations. The NHS Oversight Framework will allow monitoring of performance against plans, while also tracking delivery across a broader range of standards.
Performance improvement has slowed in 2025/26, but we cannot allow this to continue if we are going to capitalise on the opportunity the 10 Year Health Plan and SR25 has created. These targets will be supplemented with appendices on the key actions and interventions that will drive our success.
3.1 Elective, cancer and diagnostics
We are committed to returning to the constitutional standard of 92% of people waiting less than 18 weeks for treatment, and to continuing to improve performance against the 3 cancer standards for 28-day diagnosis, 31-day treatment and 62-day referral to treatment. We have made significant progress over the past year and need to build on this momentum, driving further radical transformation, including introducing a new model for planned care that meets the 10 Year Health Plan commitment of “ending outpatient care as we know it”.
This plan is rightly ambitious and will require a significant shift in the way trusts work, but also how ICBs, trusts and primary care work together to change the way most patients access planned care in the future. Our aim is for patients to receive more specialised support closer to home – that means working with GPs, community and neighbourhood teams and being digitally enabled where appropriate.
The key priorities will be:
- general practice is asked to continue prioritising the use of Advice and Guidance prior to, or instead of, a planned care referral where clinically appropriate (excluding referrals for urgent suspected cancer). There should be a move to all referrals going via Advice and Guidance for the 10 specialties at provider level which have the most potential for this model to be effective. We expect ICBs to support this, and bring it to life, through their strategic commissioning for 2026/27
- to support this increased use of Advice and Guidance, we encourage systems to ensure all referrals receive appropriate clinical triage, which we expect to flow through a single point of access. This will ensure more patients wait less time to receive a diagnosis and start an appropriate form of treatment
- to move toward the e-Referral Service (e-RS) being used for all Advice and Guidance requests from primary care, with effect from July 2026, where these requests are managed within the e-RS user interface, and from October 2026 where a third-party service is used. We will work with regions and providers to ensure rapid but manageable roll-out supported by appropriate platforms, including improvements to the functionality of e-RS
- to start to plan with ICBs and primary care how greater access to specialist advice and direct access to diagnostics for specific specialties, when aligned to neighbourhoods, could support GPs to manage more patients without the need for referral. Further details will be set out in the Model Neighbourhood Framework
Further details on how ICBs, trusts and general practice should work together to plan for this new neighbourhood health approach for elective pathways will be set out in the model neighbourhood framework.
For those patients who do require specialist outpatient care, we expect providers to continue identifying and acting on opportunities to improve productivity and ensure timely access. This includes:
- significantly reducing the number of routine, clinically low-value follow-up appointments. This will be supported by GIRFT’s specialty-level good practice guides and the first group of these will be available in December, with other pathways to follow. We are exploring whether further changes are required to the payment for follow-up activity and will advise of this in due course. Where there is greatest variation in the management of follow-ups, there will be rigorous performance management. By releasing capacity from clinically low-value follow ups, we will allow new patients to be seen and diagnosed
- conducting comprehensive reviews of clinic templates and standardising these in line with GIRFT’s specialty-level good practice and job planning guides
- expanding ‘straight to test’ pathways and one-stop clinics where clinically appropriate, starting with the 10 largest specialties by volume and expanding, with the aim of including all clinically appropriate specialties by March 2029
Further guidance in productivity opportunities relating to outpatient care are set out in the productivity section of this document. Delivering improved referral to treatment performance is closely correlated with reducing waiting lists at national and provider level. Nationally, we expect to see the waiting list reduce during 2026/27 and while the local requirement will vary by provider, reductions in waiting list sizes will be expected at all trusts.
As well as ensuring patients are treated in order of clinical priority, providers and ICBs should appropriately manage their waiting lists, including through thorough validation and the application of referral to treatment guidance and local access policies to assure themselves of their data quality. This is particularly important in carefully managing any service changes that may affect reporting, such as EPR installations and upgrades. There is a growing range of digital tools available to support data quality and address other issues, and all providers will be expected to use the NHS Federated Data Platform or equivalent technology to deliver these improvements.
Children and young people (CYP) continue to face longer waiting times for planned care, despite the disproportionate impact of long waits on their development and longer-term outcomes. Systems and providers are required to put in place targeted actions to increase activity and improve performance for their CYP population.
This should include developing ringfenced CYP capacity within the ICB footprint using existing NHS estate by running regular dedicated paediatric surgery days in either a day surgery or hub setting, with an aim to increase CYP activity delivered through surgical hubs.
Management attention needs to be maintained on meeting cancer standards and securing further improvements to early diagnosis. This should include the continued prioritisation of diagnostic (including CDC) and treatment capacity for urgent suspected cancer (USC) pathways, stratifying referrals in primary care, identifying alternative pathways to the USC pathway and diverting lower- risk people to more appropriate access routes for their condition. Cancer alliances will continue to be a source of expert performance improvement advice and support to providers, ICBs and wider system partners. Regions will continue to encourage close working and co-ordinated support across alliances and diagnostic networks to tackle the key performance challenges across their areas.
Diagnostic activity will need to increase to support delivery of both planned care and cancer standards. All systems have already been provided with activity and performance targets that need to be achieved by March 2029, and significant progress is expected in 2026/27. To support this, CDC capacity should be fully utilised and operating hours extended where possible to deliver the activity that has been commissioned, and – as neighbourhood health teams mature – organisations should consider how CDC capacity can be made available to neighbourhood teams as well as providers. Systems should ensure that these targets are achieved through a mix of capital-funded capacity increases, improved productivity (digital and services throughput) and demand optimisation that reduces the use of tests with limited patient benefit. This should include implementation of decision support tools like i-Refer-CDS. To support demand optimisation, NHS England and the royal colleges are launching a campaign this autumn – Right Test, Right Time – which encourages clinicians to focus on test referrals that add most value to patient care.
Working with local providers, ICBs will continue to hold responsibility for commissioning levels of activity for providers to deliver the performance requirements set out in this guidance. They will need to take steps in-year to mitigate demand growth in excess of agreed growth assumptions. This will require close working between primary and secondary care, with neighbourhood health teams playing an increasing role over time.
Given the interdependence between referral to treatment and diagnostic performance, we are taking a consistent approach in setting individual targets at provider level (for example, a percentage improvement as well as a performance floor). This will support planning locally by giving a clear and consistent message about performance improvement requirements on a like-for-like basis across delivery areas.
| Success measure | 2026/27 target | 2028/29 target |
|---|---|---|
| Improve the percentage of patients waiting no longer than 18 weeks for treatment | Every trust delivering a minimum 7% improvement in 18-week performance or a minimum of 65%, whichever is greater (to deliver national performance target of 70%) | Achieving the standard that at least 92% of patients are waiting 18 weeks or less for treatment |
| Improve performance against cancer constitutional standards | Maintain performance against the 28-day cancer Faster Diagnosis Standard at the new threshold of 80% | |
| Every trust delivering 94% performance for 31-day and 80% performance for 62-day standards by March 2027 | Maintain performance against the 31-day standard at 96% and 62-day standard at 85% | |
| Improve performance against the DM01 diagnostics 6-week wait standard | Every system delivering a minimum 3% improvement in performance or performance of 20% or better, whichever level of improvement is greater (to achieve national performance of no more than 14% of patients waiting over 6 weeks for a test) | Achieving the standard that no more than 1% of patients are waiting over 6 weeks for a test |
3.2 Urgent and emergency care
It has been over 5 years since the 18-minute response to Category 2 ambulance calls standard was met and over a decade since the service delivered the standard for 95% of patients waiting 4 hours or less to be seen, treated and discharged from A&E.
During that time, in parts of the NHS, we have normalised asking our staff to deliver sub-optimal care, and some of our patients have all but given up hope of expecting a reliable service in urgent care.
This document sets out expectations for next year and beyond, but we are also taking immediate steps to improve performance and service quality throughout this winter. This will include a major focus on reducing crowding in our emergency departments, ensuring that patients unlikely to require admission are seen in urgent treatment centres (UTCs), same day emergency care and other suitable points of delivery and that children are seen within 4 hours. This will allow our emergency departments to start focusing on the sickest patients and reduce the risks associated with crowding that have become normalised in recent years.
Throughout 2026/27, this will result in a service that is UTC-first and by default for patients who are less likely to require admission, and pathways for children that support more rapid assessment and treatment, with the aim that these cohorts of patients are treated within the 95% standard again. We will work with NHS providers and the relevant professional bodies (RCEM, RCPH, RCP etc) to develop this approach over the coming weeks and ask how we can best improve standards of care for the sickest and most unwell patients.
The priority will then be to improve core operational performance against constitutional standards each year by developing services and pathways that align with the neighbourhood health model, while continuing to improve clinical and operational processes inside hospitals. This will allow acute emergency care to be safeguarded for those who will benefit from it most, while unified and more efficient urgent care can be delivered in the community.
To achieve this:
- ICBs and providers must ensure patients are directed or conveyed to the most appropriate care for their urgent or emergency care needs, reducing avoidable ambulance conveyances to hospital. This will require fully utilising core services such as 111 and increasing the rate of impactful interventions such as ‘hear and treat’
- ICBs and providers must deliver more urgent care in the community by expanding neighbourhood health services, aiming to reduce total non-elective admissions and bed days, with a specific focus on frail older people, given rising demand pressures. ICBs and providers must have robust ways to measure the impact of neighbourhood health, and take remedial action if non-elective demand in this population group continues to increase
- ICBs should specifically assess total resources spent on those living with frailty and shift a proportion of those resources to better community provision, to ensure safe and effective care away from an acute hospital setting wherever possible, and to short-stay frailty attuned care when people do require admission
- ambulance services must continue to be planned in accordance with the published ambulance service specification. This includes acute trusts and ambulance services working collaboratively to reduce ambulance handover times toward the 15-minute standard
- acute trusts should embrace new standards and guidance on how to achieve our ambitious 4-hour performance target and use these to drive the necessary step-change, aligning with the soon to be published Model Emergency Department and clinical operational standards for the first 72 hours in hospital
- providers must have a renewed and rigorous focus on ensuring that patients who are less likely to require admission are directed to a UTC by default, and that there are agreed clinical and operational processes for non-admitted patients to be seen, treated and discharged within 4 hours to reduce overcrowding in departments and improve safety
- to improve our ability to respond to patients in mental health crisis and ensure the needs of mental health patients are met in an appropriate environment, we will establish mental health emergency centres in Type 1 emergency departments
- we need a whole-system effort to continue to reduce discharge delays. This should include improving in-hospital discharge processes, making best use of community beds, and increasing home-based intermediate care capacity
- ICBs and providers must ensure early action to improve flu vaccination uptake among staff and the public, helping to keep patients and colleagues safe
- systems should accelerate the transition towards a more structured, digital-first UEC model, with appointments and scheduling according to clinical prioritisation and ultimately a better patient experience (see section on productivity)
| Success measure | 2026/27 target | 2028/29 target |
|---|---|---|
| 4-hour A&E performance | Every trust to maintain or improve to 82% by March 2027 | National target of 85% as the average for the year |
| 12-hour A&E performance | Higher % of patients admitted, discharged and transferred from ED within 12 hours across 2026/27 compared to 2025/26 | Year-on-year % increases in patients admitted, discharged and transferred from ED within 12 hours |
| Category 2 response times | Improve upon 2025/26 standard to reach an average response time of 25 minutes | Further improvement so that by the end of 2028/29 the average response time is 18 minutes, with 90% of calls responded to within 40 minutes |
3.3 Primary care
Central to the broader reforms we are delivering is continuing to focus on improving access to general practice – this is critical to not only managing wider system pressures but also rebuilding the public’s faith in its NHS. Building on existing general practice action plans, in 2026/27 all ICBs must:
- ensure practices are delivering the 2025/26 GP contract (including recent 1 October changes) and the 2026/27 GP contract from April, including improving and providing good access whether by phone, online or walk in throughout core This includes all patients knowing on the day how their request will be managed, and increasing the number of people who can see their preferred healthcare professional
- put in place action plans to continue to improve contract oversight, commissioning and transformation for primary care, and tackle unwarranted variation, including identifying and planning how to support those struggling to deliver access or other elements of the GP contract
- ensure additional capacity is commissioned to meet demand out-of-hours and over surge periods including bank holidays and weekends
- support primary care providers to deploy ambient voice technologies, ensuring the time freed up is used to see additional patients
| Success measure | Target for all years 2026/27 to 2028/29 |
|---|---|
| Same-day appointments for all clinically urgent patients (face to face, phone or online) | 90% We will consult with the profession on this new ambition |
| Improved patient experience of access to general practice (ONS Health Insights Survey) | Year-on-year improvement |
To support primary care access and increase the role of community pharmacy, ICBs must:
- embed pharmacy-first approaches, ensuring that local commissioning discussions utilise available pharmacy capacity to support primary care pressures
- continue developing the relationships between general practice and community pharmacy to support access to pharmacy services
- introduce prescribing-based services into community pharmacies during 2026/27
- expand access to emergency contraception through community pharmacies
- maximise use of the Discharge Medicines Service to reduce medicines harm and reduce readmissions
- make HPV vaccination available at pharmacies for women and young people who missed out on vaccination at school
- ensure all community pharmacies have fully enabled the capability for patients to track their prescription status using the NHS App
- ensure all primary care services enable patients to request and manage their medicines online
- transition all messaging to NHS Notify, using NHS App-based ‘push’ notifications as the default option
For dental services, the government has set out a manifesto commitment to deliver 700,000 additional urgent care dental appointments against a pre-election baseline in every year of the parliament. Additional capacity has been put in place in 2025/26 to ensure an urgent care safety net is in place. ICBs will be asked to continue to secure necessary capacity, including working to implement dental contract reforms that are expected to be taken forward from April 2026 following consultation in summer 2025. In 2026/27, all ICBs must:
- deliver their contribution to the government’s commitment to deliver an additional 700,000 urgent dental appointments in England against the July 2023 to June 2024 baseline period
- successfully implement dental reforms to ensure the additional manifesto target is incorporated into contractual activity (subject to consultation)
- implement locally driven quality improvement approaches for dentistry, ensuring clinical leadership and communities of practice are in place to support improved access and the introduction of new pathways for high needs and complex patients
| Success measure | Target for all years 2026/27 to 2028/29 |
|---|---|
| Deliver 700,000 additional urgent dental appointments against the July 2023 to June 2024 baseline period | Each ICB to deliver their share of the urgent dental appointment target every year (2026/27 to 2028/29) |
3.4 Community health services
Timely and effective community health services will be critical to shifting care out of hospital and into the community to deliver our ambitions for neighbourhood health. Community health services deliver both planned and reactive provision, often for the most complex patients. Variation in capacity, provision and long waiting times have existed for too long in community health services.
In 2026/27, all ICBs and community health services providers must:
- increase community health service capacity to meet growth in demand, expected to be approximately 3% nationally per year
- actively manage long waits for community health services, reducing the proportion of waits over 18 weeks and developing a plan to eliminate all 52-week waits
- identify and act on productivity opportunities, including ensuring teams have the digital tools and equipment they need to connect remotely to health systems and patients, and expanding point-of-care testing in the community. To support this, community health service productivity metrics will be published later this financial year
- continue to standardise core service provision as defined in Standardising community health service
- consider where digital therapeutics, such as for MSK treatment, could be deployed at pace where those therapeutics have appropriate regulatory approval
| Success measure | 2026/27 target | 2028/29 target |
|---|---|---|
| Address long waiting times for community health services | At least 78% of community health service activity occurring within 18 weeks | At least 80% of community health service activity occurring within 18 weeks |
3.5 Mental health
Mental health care isn’t just important to the service users who rely on care and support being available when they need it; it is critical to the smooth running of health economies right across the NHS.
We all accept that more must be done to improve the mental health of the nation. The quality of mental health services and the ability to access them – especially for those in crisis and children and young people – must improve to address current unmet needs and reduce the risk of future harm.
There are also significant opportunities to improve quality and productivity in mental health services. There is unwarranted variation in the direct and indirect contacts per whole time equivalent hours worked within children and young people’s community mental health services and this contributes to long waiting times. We must also reduce average lengths of stay in adult acute mental health beds and complete the job on 3-year plans to localise care, reduce out-of- area placements and end the commissioning of locked rehabilitation inpatient services.
Achieving these improvements will take leadership at every level. Nationally, we will commit to working with local NHS mental health providers to set a new approach for mental health in 2026, including through the upcoming MSF for serious mental illness, led by a new national lead for mental health alongside the mental health NHS leadership community.
In 2026/27, all ICBs and mental health providers must:
- continue to expand coverage of mental health support teams in schools and colleges ahead of the ask for full national coverage by 2029
- develop a plan for delivering their local approach to establishing mental health emergency departments co-located with or close to at least half of Type 1 emergency departments by 2029
- use ring-fenced funding to support the delivery of effective courses of treatment within NHS Talking Therapies and reduce ill-health related inactivity through access to Individual Placement and Support for people with severe mental illness
- reduce inappropriate out-of-area placements and locked rehabilitation inpatient services. From 2027/28 onwards, ICBs should only commission mental health inpatient services for adults and older adults that align with the NHS Commissioning Framework
- reduce longest waits for CYP community mental health services by improving productivity, and reducing local inequalities and unwarranted variation in access
- identify and act on productivity opportunities including, in children and young people’s community mental health services, increasing the number of direct and indirect contacts per whole time equivalent hours worked, and reducing the average length of stay in adult acute mental health beds
- ensure mental health practitioners across all providers undertake training and deliver care in line with the Staying safe from suicide guidance, which sets out the latest evidence in understanding and managing suicide
| Success measure | 2026/27 target | 2028/29 target |
|---|---|---|
| Expand coverage of mental health support teams (MHSTs) in schools and colleges (including teams in training) | 77% coverage of operational mental health support teams and teams in training | 94% coverage, reaching 100% by 2029 (operational mental health support teams and teams in training) |
| Meet the existing commitments to expand NHS Talking Therapies and Individual Placement and Support | 63,500 accessing Individual Placement and Support by the end of 2026/27 805,000 courses of NHS Talking Therapies by the end of 2026/27 with 51% reliable recovery rate and 69% reliable improvement rate | 73,500 accessing Individual Placement and Support by the end of 2028/29 915,000 courses of NHS Talking Therapies by the end of 2028/29 with 53% reliable recovery rate and 71% reliable improvement rate |
| Eliminating inappropriate out-of-area placements | Reducing the number of inappropriate out of area placements by end of March 2027 | Reducing or maintaining at zero the number of inappropriate out of area placements |
3.6 Learning disabilities, autism and ADHD
People with a learning disability and autistic people too often experience avoidable health inequalities and can also be inappropriately admitted to mental health hospitals for long periods. To improve health outcomes and access to and experience of care, in 2026/27 all ICBs and providers must:
- reduce the very longest lengths of stay in mental health hospitals
- reduce admission rates to mental health hospitals for people with a learning disability and autistic people
- optimise existing resources to reduce long waits for autism and ADHD assessments and improve the quality of assessments by implementing existing and new guidance, as published
The government will publish plans for the reform of SEND in due course. We expect ICBs and providers to work with NHS England and the Department of Health and Social Care to respond to those reform plans once published, and to continue to meet their statutory duties in the meantime.
| Success measure | 2028/29 target |
|---|---|
| Reduce reliance on mental health inpatient care for people with a learning disability and autistic people | Deliver a minimum 10% reduction year-on-year |
3.7 Workforce
The ambitions outlined in the 10 Year Health Plan will require a fundamental shift in the way the NHS deploys, retains and trains its workforce. The forthcoming 10 Year Workforce Plan will set out how. In advance of this, providers’ plans should set out the workforce assumptions to deliver the shifts from hospital to community and sickness to prevention, while taking full advantage of productivity improvements, for example, from the shift from analogue to digital. Workforce plans must triangulate with finance and activity plans. Providers must also:
- fully implement the 10 Point Plan to improve resident doctors’ working lives, with action plans informed by feedback and national survey results, and progress reported publicly
- demonstrate progress in reducing sickness absence rates, which are higher in the NHS (5.1%) than in other industries and are a significant driver of expensive temporary staffing use. Providers must set out how they intend to support the 10 Year Health Plan ambition to reduce sickness absence rates to the lowest recorded national average level (approximately 4.1%)
- continue to reduce agency staffing usage in support of the ambition to eliminate this by August 2029
- implement the reformed statutory/mandatory training framework due for publication in March 2026, alongside a new approach to staff safety management
- implement the reforms to consultant job- planning to improve productivity and staff satisfaction (specifically, a trust-wide process for demand and capacity planning linked into service-level activity plans). Effective service- level job planning is essential to delivering innovation, education and training because it ensures clinical capacity is aligned to both service and education and training needs, providing transparency for funding allocation. Providers must:
- for each year, ensure that 95% of medical job plans are signed-off in line with the business cycle, underpinned by service- level demand and capacity planning
- by the end of 2026/27, ensure a system for monitoring and assurance is in place for tracking job planned activity
- by the end of 2027/28, achieve tracking of job planned activity for the full year
- by the end of 2028/29, ensure multiprofessional service level activity and job planning are in place
| Success measure | 2026/27 target | 2028/29 target |
| Reduce use of bank and agency staffing | Trusts to reduce agency and bank use in-line with individual trust limits, as set out in planning templates, working towards zero spend on agency by 2029/30 Annual limits will be set individually for trusts, based on a national target of a 30% reduction in agency use in 2026/27, and a 10% year-on-year reduction in spend on bank staffing | |
4. Next steps and plan submission
The 10 Year Health Plan stipulates that organisations should develop 5-year strategic plans that set out how they will deliver the 3 shifts and improve productivity of their services. These 5-year plans will need to be supported by 3-year numerical returns that describe what the organisation will deliver from 2026 to 2029. This timetable sets out the key outputs expected from the NHS and describes the planning process across the 3 phases.
The planning timetable – expectations for phase 2
Organisations will be expected to submit their 3 year plans as part of their first submission. This will be reviewed and assured by NHS England regional teams. Regional teams will provide feedback on the plans, and organisations will resubmit, alongside their 5-year strategic plans.
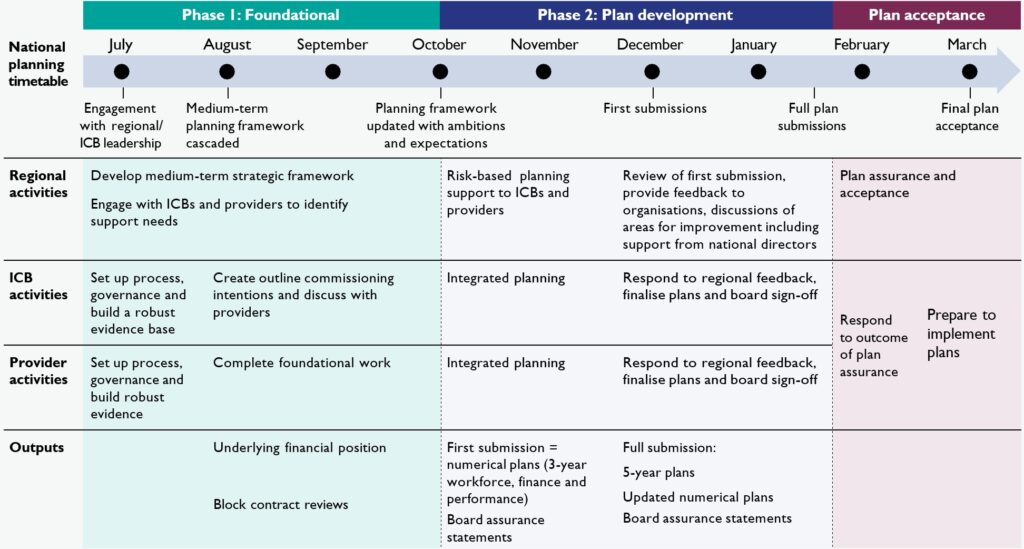
The above planning timetable can also be downloaded as a PDF.
The following tables provide a plain text version of the planning timetable:
Phase 1: Foundational (July – October)
| Category | July | August | September | October |
|---|---|---|---|---|
| National planning | Engagement with regional/ICB leadership | Medium-term planning framework cascaded | – | Planning framework updated with ambitions and expectations |
| Regional activities | Develop medium-term strategic framework Engage with ICBs and providers to identify support needs | – | ||
| ICB activities | Set up process, governance and build a robust evidence base | Create outline commissioning intentions and discuss with providers | – | |
| Provider activities | Set up process, governance and build robust evidence | Complete foundational work | – | |
| Outputs | – | Underlying financial position Block contract reviews | – | |
Phase 2: Plan development (November – January)
| Category | October | November | December | Mid January |
|---|---|---|---|---|
| National planning | – | – | First submissions | Full plan submissions |
| Regional activities | Risk-based planning support to ICBs and providers | Review of first submission, feedback, improvement discussions | ||
| ICB activities | Integrated planning | Respond to regional feedback, finalise plans and board sign-off | ||
| Provider activities | Integrated planning | Respond to regional feedback, finalise plans and board sign-off | ||
| Outputs | First submission = numerical plans (3-year workforce, finance, performance) Board assurance statements | Full submission: – 5-year plans – Updated numerical plans – Board assurance statements | ||
Plan acceptance (February – March)
| Category | Mid January | February | March |
|---|---|---|---|
| National planning | – | – | Final plan acceptance |
| Regional activities | Plan assurance and acceptance | ||
| ICB activities | – | Respond to outcome of plan assurance | Prepare to implement plans |
| Provider activities | – | ||
| Outputs | – | – | – |
Providers and ICBs will be expected to return the following plans to NHS England:
| Submission | Requirement |
|---|---|
| First submission | – 3-year revenue and 4-year capital plan return – 3-year workforce return – 3-year operational performance and activity return – integrated planning template showing triangulation and alignment of plans – board assurance statements confirming oversight of process |
| Full plan submission | – updated 3-year revenue and 4-year capital plan return – updated 3-year workforce return – updated 3-year operational performance and activity return – integrated planning template showing triangulation and alignment of plans5-year narrative plan – board assurance statements confirming oversight and endorsement of the totality of the plans |
The phase 2 planning process
Each NHS organisation is expected to develop their own integrated plans that set out:
- their strategic ambitions
- how they will meet their local population health Plans should reflect the needs of all age groups and explicitly children and young people
- their transformation ambitions, demonstrating how they will implement the 3 shifts set out in the 10 Year Health Plan while improving productivity
- evidence of partnership working and co-operation with other NHS organisations, local authorities and the voluntary, community, faith and social enterprise sector
- how they will meet the standards set out in this document
These plans should be developed in collaboration with their NHS partners and in discussion with NHS England regional teams. Although system plans are no longer required, it is still important that plans are based on cooperation and partnership-working.
Organisations’ boards should be engaged in the development of plans and are expected to complete board assurance statements demonstrating that they are satisfied that plans are robust and deliverable. Organisations will be required to demonstrate a comprehensive understanding of financial risk and an agreed approach to managing and mitigating risks in-year, which must be assured by the board as part of the final plan submission process. To support the management of in-year risk, NHS providers and commissioners should identify specific and timely actions that could be taken to reprioritise existing budgets to address unforeseen pressures, guided by the principles in HM Treasury’s ‘Consolidated Budgeting Guidance’.
We will ask for the first submission of plans before Christmas. This will include the 3-year numerical plans covering workforce, finance and performance trajectories, as well as board assurance statements. This first submission does not include the narrative plans. Final plans will be expected in early February, including refreshed numerical plans, 5-year plans and updated board assurance statements. Neighbourhood health plan requirements will be set out in the Neighbourhood Health Framework and these will not need to be submitted to NHS England as part of this planning round.
Plans will be assured by NHS England regional teams who will provide specific support to those organisations who face the biggest challenges in meeting our collective ambitions. NHS England national programme teams will also provide support where required and ensure that transformation expertise is targeted and aligned.
We will share further guidance on what should be included within the 5-year narrative plans. ICBs should ensure that their 5-year strategic commissioning plans encompass the statutory requirement for joint forward plans (JFPs) agreed by the ICB and their partner trusts.

