1. Meeting our Public Sector Equality Duty (PSED): our equality objectives
1.1 Creating the new NHS England
2022/23 has been a year of significant change for the NHS in England with the passage and commencement of the Health and Care Act 2022 which formally created the new NHS England and Integrated Care Boards (ICBs). These changes extensively impact on NHS England’s reporting requirements under the Equality Act 2010’s Public Sector Equality Duty (PSED) and the Specific Equality Duties (SEDs). This report reflects on the creation of the new NHS England and mergers with four other national NHS statutory bodies and NHSX.
In April 2022, the Health and Care Act 2022 received Royal Assent and set out major changes for NHS England, including formally changing NHS England’s statutory name from the NHS Commissioning Board to NHS England. In July 2022, NHS Improvement (NHSI), made up of the NHS Trust Development Authority and Monitor, ceased to exist and merged into NHS England.
Among its many provisions, the Health and Care Act 2022 also required NHS England to take on key functions from NHSI, NHS Digital (NHSD) and Health Education England (HEE). NHSD merged with NHS England on 31 January 2023 and HEE merged with NHS England on 1 April 2023. These mergers impact on the activities/roles /functions of NHS England and therefore on the development of our equality objectives and the publication of equality information. The publication of equality objectives and equality information are key reporting requirements under the SEDs covered in this Review Report.
In July 2022, NHS England announced plans to reduce the number of posts across the three organisations, by the end of the merger and transformation process in 2023/24, by a minimum of 30%, and up to 40%.
From July 2022, ICBs took on core roles and functions from Clinical Commissioning Groups (CCGs) and NHS England. ICBs have or will also jointly manage, and eventually take over, important functions from the new NHS England with respect to primary care commissioning and specialised commissioning. The 2022 Act also significantly strengthened the statutory framework for reducing health inequalities, placing new and stronger requirements on ICBs and other NHS organisations including on: outcomes in relation to quality, safety, service effectiveness; performance management; and annual reporting. The 2022 legislation also requires NHS England to issue guidance and information to the NHS (see Appendix 2).
In October 2022, NHS England published the Operating framework, which set out how we will give systems the space to lead and we will focus on what we are uniquely placed to do at a national and regional level.
During 2022/23, the mergers profoundly impacted on the role of the new NHS England and our purpose, responsibilities and structures. As the transformation programme and process of reducing the headcount by up to 40% was ongoing, this necessarily impacted on the work delivered by NHS England and on the delivery of some equality targets during 2022/23.
1.2 The SEDs’ reporting requirements
During 2022/23, NHS England and NHSI were both subject to the Public Sector Equality Duty (PSED). The general Equality Duty is set out in primary legislation as part of the Equality Act 2010 (see Appendix 1). The general Equality Duty is supported by Specific Equality Duties (SEDs), secondary legislation in the form of statutory regulations (see Appendix 1). These statutory duties, also placed on NHS England and NHSI, require the publication of equality information annually and the publication of equality objectives at least every four years.
This report meets the SED requirement to publish equality information annually. It includes information on progress against our eight equality objectives and targets set for 2022/23. Prior to 2022/23, NHS England and NHSI worked as a single organisation, fully merging in July 2022, and we published joint equality objectives and reported jointly on PSED/SED compliance. This report addresses the PSED and SED reporting requirements for NHS England as at March 2023. It also addresses the SED reporting requirements placed on NHSI between April and June 2022 before its dissolution.
This report does not address the 2022/23 PSED/SED reporting requirements for either NHSD or HEE. In the case of NHSD, the merger with NHSD came too late in 2022/23 to allow for meaningful reporting. With respect to HEE, although there was close working between the new NHS England and HEE, the statutory merger took place after 2022/23 on 1 April 2023.
1.3 The purpose of this report
Equality objectives and reporting provide an important improvement tool. They provide a strategic focus for change and help to drive systematic and demonstrable improvements in equality framed by the Equality Act 2010’s nine protected characteristics and the PSED’s three equality aims (see Appendix 1). This review informed the revision of our equality objectives and targets for 2023/24 and 2024/25 [See the Future report]. This report demonstrates NHS England’s continued compliance with the PSED more broadly and with the SED’s requirements to publish equality information annually. This report:
- explains the changing context within which NHS England is now functioning and what reporting is covered by this report (part 1)
- provides a summary assessment of our performance against our eight equality objectives and the associated targets set for 2022/23 (part 2)
- provides broader equality information looking at NHS England’s 2022/23 business plan priorities and key national equality programmes (part 3)
- provides key employment statistics for 2022/23 for NHS England looking at the protected characteristics on which employment data is gathered on the NHS Electronic Staff Record (ESR) (part 4)
- provides key employment statistics for April to June 2022 for NHSI looking at the protected characteristics on which employment data is gathered on ESR (part 5).
With respect to the employment data in parts four and five, it is important to note that the mergers and the planned staff reductions mean that comparisons between the employment data for 2022/23 and 2021/22 are difficult; key implications and caveats are cited in parts four and five of this report.
1.4 The amended health inequalities duties
The health inequalities duties placed on NHS England and the wider system are provided by the National Health Service Act 2006 and are a separate legislative framework to the Equality Act 2010, the PSED and SEDs. This separate legislative framework, primarily directed at the NHS, was significantly amended and enhanced by the Health and Care Act 2022 (see Appendix 2). NHS England’s Healthcare Inequalities Improvement Programme is accountable for the consistent application of the health inequalities duties.
Under provisions introduced by the Health and Care Act 2022, NHS England has wide ranging duties, powers and responsibilities in relation to the enhanced health inequalities duties. These include issuing guidance on monitoring, annual reporting and performance assessment by ICBs and other NHS organisations. NHS England also has to assess the performance of ICBs and other NHS organisations in a number of areas including health inequalities. By contrast, the Equality Act 2010, together with the PSED and SEDs, impose important but separate legal obligations and the Equality and Human Rights Commission (EHRC) is the regulatory body and has important regulatory enforcement powers.
NHS England is developing strategic approaches to address the health inequalities duties and some of these are also making a positive contribution to addressing the PSED’s requirements. This report only considers health inequalities where these are directly related to one or more of the nine protected characteristics and/or address one or more of the PSED’s three equality aims. The link between the health inequalities duties and the PSED and SEDs was raised in 2021/22 and 2022/23 so is addressed in this review report, the Engagement Report and the report on NHS England’s Equality objectives and targets for 2023/24 and 2024/25.
During 2022/23, NHS England started to review guidance to support the wider NHS to comply with the strengthened health inequalities duties including new reporting requirements. This review considered how to ensure compliance with the PSED’s requirements and separate SED reporting requirements. It was therefore not possible, or appropriate, to bring together the reporting requirements for the health inequalities duties, being developed under the 2022 Act and the separate statutory reporting requirements under the PSED and the SEDs.
1.5 The equality objectives and targets for 2022/23
We set eight equality objectives (EOs) for 2022/23 and 2023/24. Each EO was supported by equality targets to be delivered in 2022/23. Progress made during 2022/23 is reported against our eight EOs and associated targets:
- EO1 [COVID-19]
- EO2 [Capability]
- EO3 [Information]
- EO4 [Internal workforce]
- EO5 [Patient access and communication]
- EO6 [System workforce]
- EO7 [Integrated Care Boards]
- EO8 [System landscape]
Where it might be helpful, links to relevant reports and more detailed equality information is provided. In some cases, unsurprisingly key equality focused initiatives, which have informed the achievement of one or more of the eight equality objectives and their associated targets, were launched prior to 2022/23. Where it is important to understand these policy commitments, due to be delivered over a number of years, this is noted.
1.6 Meeting the SEDs and the PSED
This report demonstrates that NHS England has made progress. However, further work and a continued focus on advancing equality will be required over future years. [see the Future Report].
2. Progress against the 2022/23 equality objectives and targets
2.1 Context
This part reviews progress made towards the eight equality objectives and targets in the year to 31 March 2023. Where the target has not been achieved a brief explanation has been provided. This has normally resulted in the target being rolled over into 2023/24 unless a more fundamental issue has arisen or another more fundamental solution is required [See the Future Report]. In relation particularly to EO1 and EO5, we have explained when key actions taken to address health inequalities also address inequalities by reference to one or more protected characteristics.
2.2 Equality objective 1 [COVID-19]
EO1 To ensure that the equality and health inequality impacts of COVID-19 and key lessons learnt are fully considered and that clear strategies are developed and implemented for the NHS workforce and patients of all ages as the NHS moves into and beyond the recovery phase. To ensure that patient and workforce focused strategies reflect this and make an effective contribution to advancing equality for people of all ages by reference to protected characteristics and to reducing associated health inequalities.
Progress against EO1T1 To ensure that operational, planning and associated guidance to systems considers how to address and reduce the adverse equality impacts of COVID-19 and provides strategic guidance to the NHS.
Progress against EO1T2 To work to ensure that key NHS England and NHS Improvement patient and workforce strategies consider the lessons learned from COVID-19 and how to address and reduce the adverse equality impacts of COVID- 19.
This assessment reports on progress against the first two targets. Progress in relation to workforce strategies is generally reported under EO6 unless it made more sense to report it under these targets. The 2022/23 priorities and operational planning guidance, like the 2021/22 guidance, addressed both equality and health inequality considerations. Two of the four strategic purposes for ICBs were identified as being to: Improve outcomes in population health and healthcare; and tackle inequalities in outcomes, experience and access. Moreover, another strategic purpose, ‘supporting broader social and economic development’ had the potential to have significant and positive equality impacts. The guidance stated that ICBs would be expected to undertake preparatory work through 2022/23 to ensure that their five-year system plans ‘match the ambition for their ICS’, including delivering specific objectives under four purposes to: improve outcomes in population health and healthcare; tackle inequalities in outcomes, experience and access; enhance productivity and value for money; support broader social and economic development.
Five of the ten priorities for systems, in the 2022/23 Guidance – A, B, F, G and J – addressed equalities and health inequalities either directly or indirectly.2 The 2022/23 guidance restated that ‘across all these areas we would maintain our focus on preventing ill-health and tackling health inequalities by redoubling our efforts on the five priority areas for tackling health inequalities set out in guidance in March 2021’. The guidance also sought to ensure that all priorities made a contribution to addressing equalities and health inequalities. It explicitly recommitted to the expectation that ICBs and ICSs would take a lead role in tackling health inequalities, building on the Core20PLUS5 approach introduced in 2021/22 to support the reduction of health inequalities experienced by adults, children and young people, at both the national and system level. Part 4 of the 2021/22 implementation guidance required systems and providers to focus on recovering elective services inclusively and build on the health inequalities priorities announced in 2021.
The 2023/24 priorities and operational planning guidance reconfirmed the ongoing need to recover our core services and improve productivity, make progress in delivering the key NHS Long Term Plan ambitions and continue to transform the NHS. The formula, identified in the 2023/24 guidance, included an adjustment to weight resources to areas with higher avoidable mortality and the £200 million of additional funding allocated for health inequalities in 2022/23 was made recurrent for 2023/24.
Progress against EO1T3 To continue to develop and implement strategies in elective recovery including people of all ages to reduce the adverse equality impacts of COVID-19 as the NHS moves into the recovery phase.
In February 2022, NHS England published the Delivery plan for tackling the COVID- 19 backlog of elective care. This set out a progressive agenda for how the NHS would recover elective care over the next three years and it explicitly renewed the commitment to ‘tackling inequality by ensuring the wellbeing offer is accessible to all staff’ including tailored support for staff. It also identified that work was planned to increase minority ethnic representation at senior levels across the NHS and to overhaul recruitment and promotion practices.
The plan committed to understanding and addressing inequalities and putting reducing inequalities at the core of recovery plans and performance monitoring. It stated that systems ‘will be expected to analyse their waiting list data by relevant characteristics, including age, deprivation and ethnicity, and by specialty.’ The plan committed to:
- ensuring a ‘fair recovery’ is at the core of our approach
- embedding a focus on health inequalities in how we hold systems to account for delivery
- focusing particularly on equity of access, experience and outcomes for the most deprived 20% of the population and the five clinical areas of focus in ‘Core20PLUS5’ where we know we can make the greatest difference (maternity, severe mental illness, chronic respiratory disease, cancer and hypertension case-finding).
The Elective Recovery Programme established a Health Inequalities Working Group following the publication of the Elective Recovery Delivery Plan in February 2022. The Group established a clear governance approach and senior accountability and began to develop a set of health inequality project plans covering the performance, delivery and transformation of the Elective Recovery Programme.
In April 2022, the 2022/23 priorities and operational planning guidance: Elective recovery planning supporting guidance was published. This guidance built on the delivery plan and set out the key ambitions for 2022/23 to 2024/25. Addressing health inequalities remained a key element of elective recovery. A number of specific commitments were also required as part of assurance on how health inequality data would be used locally. In addition, an equality and health inequalities impact assessment had to be completed for elective recovery plans locally.
In January 2023, NHS England published the delivery plan for recovering urgent and emergency care services. This identified the need for a sustained focus on 5 areas: increasing capacity; growing the workforce; improving discharge; expanding and better joining up health and care outside hospital; and making it easier to access the right care.
2.3 Equality objective 2 [Capability]
EO2 To improve the capability of NHS England’s and NHS Improvement’s teams to understand and address the PSED’s legal obligations and the separate health inequalities duties and associated requirements as they develop.
Progress against EO2T1 To improve and develop the in-house capability programme for NHS England and NHS Improvement staff.
A programme of work was delivered during 2022/23 as part of the in-house capability programme for NHS England staff. This work included:
- The creation of an eBook as an addition to NHS England’s onboarding process for new employees
- Equality and Health Inequalities Impact Assessment (EHIA) guidance
- An Equality Library and Evidence Repository: a library of completed EHIAs to support staff to develop EHIAs and an evidence repository was added to during 2022/23
- Bespoke training was made available to teams on request, covering the PSED, the EHIA template and process and a recorded training session was made available
- We continued to support our Engagement and Equality Champions for each region and directorate within NHS England
Progress against EO2T2 To respond to the priorities identified by NHS England’s and NHS Improvement’s Boards to address patient equalities and associated health inequalities
In May 2022, NHS England’s Board agreed the publication of our reports on compliance with the PSED and SEDs. The reports included an assessment of progress against our equality objectives. We also published a revised set of objectives and targets for 2022/23 and 2023/24. In October 2022, NHS England’s Board reviewed progress and the impact of the Healthcare Inequalities
Improvement Programme (HiQiP) and future plans to support systems to address healthcare inequalities in a systematic way. The Board agreed a range of commitments relating to delivery in 2022/23 that would help address health inequalities and improve outcomes and experience for those with a range of protected characteristics.
To support NHS England teams to ensure that key strategic initiatives considered and addressed the requirements of the PSED, additional customised support was provided where appropriate. Examples of this included a number of programmes and initiatives: The Children and Young People Cancer Experience Survey (Under 16 CPES gender question); NHS Equality, Diversity and Inclusion (EDI) improvement plan; Equalities input into Guidance on the Health Inequalities Duty Statutory Guidance; and the NHS payment and finance schemes for 2022/23 and 2023/24.
2.4 Equality objective 3 [Information]
EO3 To improve the mapping, quality and extent of equality information to better facilitate compliance with the PSED in relation to patients and NHS service-users of all ages, NHS service delivery, and the NHS workforce.
Progress against EO3 T1 To establish a Unified Information Standard for Protected Characteristics (UISPC) Publication Steering Group to identify which of the UISPC’s recommendations should be taken forward.
Progress against EO3 T2 To work with the UISPC Publications Steering Group to identify how best to carry forward and oversee the work of the UISPC Project.
Progress against the first two targets has been taken together because target 2 depended on the conclusion of target 1. The Unified Information Standard for Protected Characteristics scoping project (UISPC) is a DHSC commissioned initiative designed to provide recommendations on the collection of improved equality data on patients and employees around protected characteristics. It is an NHS wide initiative. Once implemented, the UISPC should enable NHS organisations to improve care and employment approaches and to better respond to their legal duties around equalities by reference to protected characteristics under the Equality Act 2010. It is intended to enable DHSC and the wider NHS to identify viable options for improving the consistency, detail and quantity of equality data in major NHS information systems and to allow the development of a unified Information Standard or Standards for this data.
Following a commission from DHSC in late 2021/22, a UISPC Publication Steering Group (UISPC PSG) was established. This was a technical steering group with representatives from cross-government agencies and NHS system partners including NHS England (including teams formerly part of NHS Digital); NHS Business Services Authority and the Care Quality Commission.
During 2022/23, the UISPC PSG reviewed the content of the two comprehensive literature and evidence reviews produced in late 2020 during the first phase of the project and the detailed recommendations within them. The PSG also considered whether and how the material produced to date should be updated to incorporate learning from the later stages of the COVID-19 pandemic and the changes to the health and care system.
Progress against EO3T3 To identify what options there are for the UISPC programme to inform how to undertake mapping by reference to health inequalities.
During 2022/23, there were discussions to explore how the UISPC could inform how to undertake mapping by reference to health inequalities. These identified that the primary areas of intersection with the UISPC programme were likely to be around the protected characteristics of age, disability, ethnicity and sex. However, it was also agreed that until more progress had been made on the UISPC, limited progress could be made with on this target.
2.5 Equality objective 4 [Internal workforce]
EO4 To improve, by reference to protected characteristics, the recruitment, retention, progression, development, and experience of the people employed by NHS England and NHS Improvement to enable the organisations to become inclusive employers of choice.
Progress against EO4T1 To maintain the 19% aspirational target of BME representation at all levels of our organisation.
In March 2020, we set an aspirational target to achieve 19% BME representation across all levels in the organisation by 2025. Good progress was made between 2020 to 2021 as highlighted below. Between March 2020 and September 2021, overall BME staff representation increased from 16% to 20%. At ESM level, between March 2020 and March 2023, BME representation increased from 7.2% to 16%. However, in July 2022, a recruitment freeze was introduced across NHS England, HEE and NHS Digital. This naturally constrained progress towards our 19% target although comparing April 2022 and December 2022, we saw an overall 18% increase in BME staff, this equated to 400+ additional BME staff.
During 2022/23, and before, regional and national directors scrutinised senior level recruitment outcomes from 8c to ESM level to hold directors to account. Between April 2022 and December 2022, the number of BME employees in Band 8c increased by 21.1% although the percentage increases at Band 8d, Band 9 and MDL were lower. During 2022/23, we analysed the BME representation across NHS England, NHS Improvement, NHS Digital and Health Education England. This identified that the incoming organisations had less diverse BME representation than NHS England. We therefore recognised the need to take appropriate and lawful proactive measures to reduce the potential adverse impact on BME representation in the new NHS England.
These lawful and proactive measures placed Equality, Diversity and Inclusion at the heart of our design principles for organisational change. This messaging was, and continues to be, reinforced by the Chief Executive, Amanda Pritchard and Executive leaders. The Executive Team committed to maintaining our diversity as a workforce with a view to improving levels of diversity in the new NHS England.
We established the EDI Advisory Group in September 2022, a new forum for Staff Network Chairs across HEE, NHS Digital and NHS England to meet with senior leaders directly. This EDI Advisory Group has helped to ensure that all voices are heard. The Advisory Group also sought assurances on EDI commitments and maintaining our diversity as part of the organisational change programme. A new Equality Impact Assessment (EQIA) framework was established in December 2022 to provide check and challenge on the design structure proposals. From October to December 2022, 135 design leads and team members were trained in this EQIA process, and over 140 EQIA panel members were trained in reviewing EQIA submissions. Between January 2023 and early March 2023, 19 EQIA panels met to provide scrutiny on the organisational design structure and more met before the end of March 2023. This process led to greater assurance and rigour in our design processes and ensured that inclusive practices, to support and maintain the diversity of our workforce, were properly embedded.
Progress against EO4T2 To continue increasing declaration rates of under- represented groups in our workforce including disabled colleagues.
We published regular communications in our staff newsletter, leaders and line managers communications, all staff briefings and on the intranet to encourage colleagues to update their ESR record. Staff were specifically encouraged to make any necessary declarations about their protected characteristics. We created a ‘How to video’ to help colleagues to update their ESR records.
Between February 2022 and January 2023, we saw increases in diversity declarations across our teams including BME colleagues (20.7% to 22%); Disability (7.7% to 8.4%) and LGB declarations (4.7% to 4.9%). Female representation remained the same throughout this year at 69.1%.
In Disability History Month, we shared staff stories encouraging colleagues to explore how to support each other. There was a particular focus on colleagues with a disability and on reinforcing the importance of updating personal details and declarations on ESR. Our Executive Sponsor for the Disability and Wellbeing Network (DAWN), Julian Kelly, Chief Finance Officer, concluded the month by providing his insights and reflections for the year ahead.
These initiatives raised awareness and visibility by presenting personal stories. For example, Ruth May, Chief Nursing Officer declared her Dyslexia as part of the focus on ‘Hidden Disabilities’. Ruth presented her story on dealing with her disability and her journey to becoming the Chief Nursing Officer for NHS England. This presentation encouraged colleagues to share their stories and promoted a more open culture with respect to disability. Ruth is also an Executive Sponsor for our DAWN network.
Disability representation continued to increase year-on-year since March 2020, with a 1.1% increase from 2021/22. As of 31 March 2022, 7% of staff had declared a disability. This increase correlated to more colleagues declaring their disability on ESR. Furthermore through recruitment, this increase has been seen at Bands 3, 4, 5, 8c, Medical grades and senior grades. There was an increase of 2.4% in declarations in senior grades (ESM) from the previous year (2020/21).
Progress against EO4T3 To undertake a change programme on our recruitment and promotion, further enabling the organisation to become an employer of choice and a workforce that reflects the communities we serve.
There were continuous improvements in recruitment outcomes for disabled colleagues, which was potentially enhanced by greater flexibility in work-base options.
In Quarter 2 2022/23, recruitment data indicated that applicants who declared a disability had a 6.5% higher chance of being shortlisted than non-disabled applicants. The recruitment data for this period also indicated that applicants who declared a disability had a 4.3% higher chance of being appointed in comparison to non-disabled applicants. The September 2022 position showed the organisational ratio of 1:1.08 for disabled applicants, indicating a greater success rate for disabled applicants in comparison to non-disabled applicants.
Moving to a deployment first model
We built on successes made during our response to COVID-19 in mobilising the workforce fluidly and at pace by moving to a deployment-first model. The Deployment First Model placed employees in timebound programme delivery placements. This enabled us to support opportunities to deploy our existing workforce where and when they were needed. Benefits of adopting this approach included avoiding lengthy, expensive and formal recruitment processes, removing potential biases and barriers to opportunities for our employees, maximising our internal talent, and embedding talent agility across our organisation.
We also made significant improvements to our internal recruitment processes; we managed this in-house end-to-end, simplified the candidate experience, and made it more accessible as a result. Improvements included streamlining processes to enable vacancies to be advertised more quickly; better search functions for candidates to find suitable matches; and an automated process to quickly republish advertisements for roles which had not been filled. During 2022/23, we continued to test and build on this approach to harness the diversity of internal talent while looking to develop a new recruitment and promotion model that supports the organisation’s aims.
Progress against EO4T4 To reset our EDI strategy, for the new NHS England, creating opportunities to refresh our targets to ensure they are reflective of our EDI values, local labour markets and accommodating the rapid growth of a merged workforce.
In resetting our EDI strategy, we established a cross-organisational working model in April 2022 comprising of EDI and other senior leaders from across HEE, NHS Digital and NHS England. We undertook a number of initiatives to develop understanding, prioritisation and planning to achieve impact. This also required building organisational capability and resilience to deliver on EDI during the transition and going forward.
Our strategic initiatives during 2022/23, included cross-organisational benchmarking to understand EDI strengths and legacies across the three organisations as well as areas of vulnerability, particularly in workforce representation and staff experiences. We had a major focus on ensuring our staff networks were well supported and part of the conversation about organisational change.
We also established new forums including the EDI Advisory Group as well as the collective of staff networks. Staff network chairs had a direct dialogue with senior leaders to hear directly from them and to feed back their concerns, priorities and experiences to inform the change programme and future priorities. We delivered additional engagement workshops with an independent facilitator for our networks to explore how they come together and collaborate and how they wish to be supported in the new organisation. Finally, we built, and continued to build, on the insights from the Equality Impact Assessment process. Some of these insights had and have wider implications, including asking the organisation to better embed effective governance, scrutiny and accountability in delivering outcomes while building capability in the new organisation. This work laid the foundation for the full strategy due to be launched in 2023/24.
2.6 Equality objective 5 [Patient access and communication]
EO5 To improve access and reduce communication barriers experienced by individuals and groups of people of all ages, by reference to protected characteristics, who need NHS services.
Progress against EO5T1 To complete the review of the Accessible Information Standard (AIS) and publish the revised standard together with guidance to support compliance.
In June 2022, the NHS England-commissioned review report on AIS implementation across the NHS and adult social care was completed. This work involved engagement with people with lived experience and voluntary sector organisations who represent and work with people with disabilities. This work assessed the challenges that people with disabilities and specific communication needs face and made 14 recommendations to support the redrafting of the AIS. These recommendations fell into the following categories: the Standard itself; roles and responsibilities; training and education; patient awareness; digital; implementation; complaints; regulation; and assurance.
The work engaged with four ‘coalition groups’ of people with lived experience to ensure that their feedback was heard and contributed to the work. The groups represented those: with sensory loss; with mental health problems; people with learning disabilities and autistic people and people with other communication needs.
The work was used to support and inform the redrafting of the AIS. The redrafting was also informed by surveys undertaken and reports published by Healthwatch England, Sign Health and other partners. These reports provided further information on the challenges faced by people with disabilities, specific communication needs and concerns about the uneven implementation of the AIS across the NHS.
During 2022/23, there were regular meetings with the AIS Programme Board. This Board, made up of stakeholders and organisations representing those with lived experience including Healthwatch, CQC, DHSC, local authority providers of care and VCSE organisations, advised and fed back on the work to redraft the AIS.
Alongside this work there was engagement with relevant NHS England teams and colleagues in NHS Digital to inform the work and ensure that the AIS was aligned with relevant internal processes, policy and programmes of work. The updated AIS documentation was completed in March 2023 with publication planned for the first half of 2023/24.
Progress against EO5T2 To ensure that the expectations placed on key stakeholders are clear and processes are in place to assure compliance with the AIS at a local and provider level
In line with one of the key recommendations of the AIS Review, a task and finish group was set up to work on the development of a ‘self-assessment framework’. The purpose of this was to enable ICBs, local providers and local authorities to demonstrate assurance and compliance with the recommendations of the AIS. Work was also initiated to consider how the self-assessment framework could be incorporated in CQC’s regulatory framework.
During 2022/23, work continued with Sense, through the VCSE Health and Wellbeing Alliance, to produce a detailed Communication and Engagement plan to set out arrangements for ensuring that organisations are aware of, and informed about the AIS, both pre and post launch and are effectively engaged.
The broader AIS programme identified ongoing challenges for people with disabilities who have specific communication needs. However, our assessment was that some of these challenges are less about the content of the AIS and much more about the extent to which it is implemented (or not) at a local and service level. The work identified that providers and healthcare professionals are frequently unaware of their responsibilities to provide accessible information to individuals.
The work also identified that better training for the healthcare workforce on their legal responsibilities and the importance of providing information and communications in accessible formats (and the negative impact on individuals of not doing so).
Progress against EO5T3 To ensure relevant NHS England and NHS Improvement policies use language that is inclusive of LGBT+ people.
During 2022/23, the NHS England LGBT Health Team worked with colleagues across NHS England to agree a recommended approach to take in terms of inclusive language for LGBT+ people in relevant policy and clinical areas across the organisation. This work was informed by research undertaken by NHS Digital during 2022. NHS Digital engaged with a range of people to test which approach to language was best understood. The research found that a ‘partially additive’ approach to language used had the highest levels of comprehension, including among those with low literacy. This approach is in line with the inclusivity statement jointly issued by the Royal College of Obstetricians and Gynaecologists (RCOG) and the Royal College of Midwives and Government guidance. The guidance recommends that to achieve both clarity and inclusivity an additive approach to language is employed.
The LGBT Health team undertook a literature review on the use of gender inclusive language (and the impact of not doing so) and built on that with engagement work with relevant NHS England policy teams. The aim was to develop a proposal for NHS England to consider in terms of using language that both retains current language and is also inclusive of trans and non-binary people.
2.7 Equality objective 6 [System workforce]
EO6 To improve, by reference to protected characteristics, the recruitment, retention, progression, development and experience of staff in the NHS workforce.
Progress against EO6T1 To increase the proportion of staff in senior leadership roles who a) are from a BME background b) are women c) disabled, in line with the NHS Long Term Plan commitments.
In February 2023, the NHS Workforce Race Equality Standard showed that BME staff made up almost a quarter of the workforce overall (24.2% or 383,706 staff) – an increase of 27,500 people since 2021 (22.4% of staff). The analysis also showed more than two fifths (42%) of doctors, dentists and consultants, and almost a third (29.2%) of our nurses, midwives, and health visitors were from BME backgrounds. Similarly, the figures also showed an increase in representation at board level – including executive board roles. The number of BME members across all NHS trusts had increased to 13.2% in 2022, up from 12.6% the year before, and almost double what it was in 2017 (7%). In the 12 months from 2021 to 2022, BME very senior managers increased from 9.2% to 10.3% (an increase of 51 – from 290 in 2021 to 341 in 2022)*.
*New figures show NHS workforce most diverse it has ever been, NHS England, 22 February 2023.
The disability declaration rate in NHS trusts and foundation trusts overall was 3.7% in 2021, and this increased to 4.2% in 2022. This meant that in 2022, the disability declaration rate among Board members was higher than the overall workforce declaration rate for the first time since the beginning of WDES data records.
Progress against EO6T3 To increase the representation of disabled people on NHS trust and NHS foundation trust boards, in line with the NHS Long Term Plan commitments.
The percentage of NHS trust and foundation trust board members who declared a disability on ESR as at 31 March 2021 was 3.7%, and this had increased to 4.6% as at 31 March 2022.
Note: As at May 2023, this was the latest data collection of WDES data.
For comparison, the disability declaration rate in NHS trusts and foundation trusts overall was 3.7% (equal to the Board declaration rate) as at 31 March 2021. The declaration rate increased to 4.2% as at 31 March 2022. In 2022, the disability declaration rate among Board members was higher than the overall workforce declaration rate for the first time since the beginning of WDES data records.
Progress against EO6T2 To publish a workforce EDI strategy for NHS staff, including LGBT+ staff, aimed at establishing areas of focus for systems and organisations to improve the experience of LGBT+ staff in their workplace.
Progress against EO6T4 To continue the rollout of the six high impact actions to progress inclusive recruitment and promotion practices across the NHS.
Progress against targets 2 and 4 has been assessed together. In Q2 and Q3 2022/23, the national EDI team undertook a wide engagement exercise to ensure that the NHS EDI Improvement plan, in development during 2022/23, reflected the lived experience and lessons from staff across all protected characteristics, as well as covering intersectionality and social mobility. The team had multiple sessions with Chairs, Chief Executives and NEDs from the service as part of the Equality Advisory Group, the national workforce plan Reference Group and the national HRD/ People Leaders webinars. The EDI team also held sessions with HRD networks across all regions, Shelford Group trusts, ICS CPO networks in collaboration with NHS Providers and NHS Confederation as well as key external stakeholders such as the NHS Race and Health Observatory (RHO), Rainbow Badge project and EHRC.
To ensure that staff lived experience was reflected throughout, the team engaged closely with staff networks, EDI leads and subject matter experts (SMEs) across all protected characteristics. Over 30 engagement events were completed, and over 150+ responses from staff surveys were incorporated into the NHS EDI Improvement plan. The NHS EDI Improvement plan is expected to be published in early 2023/24, and the national team continued to socialise the plan with key internal and external stakeholders during 2022/23.
In addition to stakeholder engagement, the team undertook a synthesis of the available evidence to ensure that, in addition to the moral case, the business case for greater diversity within the NHS workforce was clearly understood. Using the evidence, the theory of change underpinning the EDI plans links improvements in staff experience with improved patient outcomes and better organisational productivity.
The empirical evidence and the themes from the engagement informed the High Impact Actions (HIAs) outlined in the plan. The plan identifies that all systems and employers will be expected to implement the HIAs to have a demonstrable impact on equality and diversity within their workforce. The latest draft of the HIAs is set out in section 3.4 of this report. A key aim of engagement was for system leaders who helped to develop the NHS EDI Improvement plan to become advocates for it to support its successful implementation.
Progress against EO6T5 To launch 38 new supported internship programmes during 2022/23 and 2023/24 with NHS organisations offering between 304 to 380 new supported internship places for young people aged 18 to 24 as part of the DFN Project SEARCH programme funded by NHS England and NHS Improvement and Health Education England.
The Pan-London Supported Employment Board was launched by NHS England London region in partnership with London Councils and held its inaugural meeting in June 2022. This Board brings together a range of partners from local authorities, NHS organisations, government, education and social services and experts by experience. The Board aims to develop a strategic action plan to create sustainable employment routes for this group of disadvantaged young people in London.
As part of our work to deliver real change in the capital, we commissioned a report that considered lessons learnt from the West London Alliance. The draft report, ‘Making Change Happen’ by Profession Richard Griffin, set an ambitious ask for leaders to implement evidence-based interventions to transform the lives of young people through work. The draft report was considered by the Pan London Supported Employment Board in November 2022.
The work with DFN Project SEARCH, a national provider of supported internships, continued. 24 new programmes, funded by NHS England and HEE, were rolled out in 2022/23. In total 28 programmes, funded by NHS England and HEE were running across England by the end of 2022/23.
The DfE-funded initiative, Internships Work was launched in Q2 2022/23 to expand NHS funded supported internship programmes in England. In Q4 2022/23, we commissioned the development of some tools and resources to enable NHS organisations to access this.
Progress against EO6T6 To implement a framework for monitoring the number of volunteers across the NHS by reference to protected characteristics and any other relevant characteristics.
Work was undertaken to develop a mandatory national data collection to capture the number of NHS volunteers. Subject to, and informed by, what is already collected locally, it is intended that this will include demographic information including protected characteristics. To support the approval process for a new mandatory data collection, an optional annual voluntary survey of volunteer service managers in secondary care NHS trusts was developed which helped to determine how and where to start with this ambition. This survey was last conducted in September 2022.
This survey had a response rate of 39% (with 79 out of 213 trusts sending in a return). Of those that replied, 91% of trusts collected some background information on their volunteers. However, this survey identified variable collection levels across the protected characteristics with the highest collection levels on age (87%), gender (84%), ethnicity (79%), disability (79%), religion/beliefs (62%) and sexual orientation (59%). The lowest collection levels were on pregnancy and maternity (15%) and gender reassignment (21%).
Work commenced again in Q3 2022/23 to establish an engagement and consultation process with NHS trusts to identify evidence regarding data collection and if there were any elements of the ambition that could be collected without creating an unnecessary burden. Key preparatory work to develop a framework was undertaken during 2022/23.
2.8 Equality objective 7 [Integrated Care Boards]
EO7 To work with Integrated Care Boards (ICBs) to support their, and their systems, compliance with the Equality Act 2010’s Public Sector Equality Duty (PSED) and the associated Specific Equality Duties (SEDs)
Progress against EO7T1 To publish guidance on compliance with the PSED and the SEDs.
The revised SEDs were published in July 2022, following the passage of the Health and Care Act 2022. However, there were no transitional arrangements, which meant that it was not clear exactly how the gender pay gap provisions and annual reporting requirements would apply to ICBs. To clarify matters detailed discussions were held with the EHRC focused on how the SEDs would apply to ICBs. As the statutory body with enforcement and regulatory powers in relation to both the SEDs and the PSED, only the EHRC could formally clarify the position.
In February 2023, the EHRC wrote to all ICB Chief Executives to set out their advice and expectations as the regulatory and enforcement body with respect to the SEDs. NHS England ensured this information was circulated to relevant teams within NHS England. Until we received the clarity provided by the EHRC, NHS England could not address how best to provide guidance to ICBs on the PSED and the health inequalities duties. The letter from the EHRC raised important regulatory issues for ICBs and had implications for the support that NHS England might need to provide. These issues informed the development of the equality objectives and targets for NHS England in 2023/24 and 2024/25.
Consideration was given to various options for providing guidance on the interface between the requirements of the amended health inequalities duty (13G of the National Health Service Act 2006) and the Public Sector Equality Duty (section 149 of the Equality Act 2010). These have also informed the 2023/24 and 2024/25 equality objectives and targets report.
Progress against EO7T2 Working in partnership with the National Healthcare Inequalities Improvement Team to identify a named Executive Board level lead with oversight for meeting the requirements of the PSED and the SEDs.
During 2022/23, the process of identifying named Executive Board Level Senior Reporting Officers (SROs) for health inequalities in regions, ICS and providers continued. However, consideration of their role in relation to the PSED/SEDs was deferred until 2023/24.
Progress against EO7T3 To deliver a programme for ICBs to support PSED compliance using the Equality Delivery System and other relevant tools, as part of a wider offer from NHS England and NHS Improvement.
In 2022/23, NHS England concluded a thorough revision of the Equality Delivery System (EDS). The EDS is a system that helps NHS organisations to improve the services they provide for their local communities and to provide a better working environment for those who work in the NHS while meeting the requirements of the Equality Act 2010. The new EDS2022 was published in August 2022 together with supporting guidance, the EDS Technical Guidance and the NHS Equality Delivery System 2022: EDS Ratings and Score Card Guidance. To support implementation and delivery, a virtual network was developed and maintained on the FutureNHS platform.
2.9 Equality objective 8 [System landscape]
EO8 To ensure that the equality objectives for NHS England and NHS Improvement address the relevant statutory functions, duties, powers and responsibilities of NHS England created by the Health and Care Act 2022.
Progress against EO8T1 To identify the existing arrangements within HEE and NHS Digital for securing compliance with the PSED and the SEDs and agree how to harmonise the differing arrangements.
Progress against EO8T2 To establish a process for reviewing whether the equality objectives developed for NHS England and NHS Improvement for 2022/23 and 2023/24 appropriately address the overall statutory functions of the new NHS England.
Targets 1 and 2 have been assessed together. The transformation programme meant that limited progress was made against these targets. We identified and reviewed the equality objectives and some published equality information for NHS Digital and HEE.
Some of the preparatory work and planning undertaken during 2022/23 informed our thinking about the approach to the new targets for 2023/24 and 2024/25. However, the complexity of the transformation programme and the need to understand the final new NHS England structure, which will not emerge until sometime during 2023/24, meant that it was not possible to make substantive progress with respect to either target.
3. Meeting our Public Sector Equality Duty (PSED): our equality information
3.1 NHS England’s business plan for 2022/23 and specific equalities focused commitments
Our business plan published in July 2022 set out ‘our work in leading and supporting the NHS to respond to the challenges of the last two years as well as the opportunities to transform the delivery of care and health outcomes through collaborative system working, and the use of data and digital technologies.’ Addressing equalities and reducing health inequalities were embedded in the 10 priorities set out in the plan with a focus on: inclusive culture; the COVID-19 response; improving mental health services and services for people with a learning disability and/or autistic people; improving the cancer backlog; delivering improvements in maternity care; preventing ill health and tackling health inequalities; and reducing unwanted variation.
Most of the health inequalities initiatives addressed health inequalities by reference to one or more protected characteristics as well as wider factors. Key equalities and health inequalities focused commitments included developing person-centred and age-appropriate care for mental and physical health needs rather than a transition to adult services based on age. These commitments also included developing and delivering the Cervical Screening Programme strategy to better understand and support improvements to address health inequalities.
3.2 Patient Equalities and LGBT Health Team
The team provided a strategic focus for change and helped to drive systematic and demonstrable improvements in equality. During 2022/23, key priorities to address patient equalities included:
- co-ordinating the review and development of NHS England’s equality objectives for 2022/23 and 2023/24 and targets for 2022/23
- co-ordinating the review of NHS England’s equality objectives and targets for 2023/24 and 2024/25
- ensuring the Equality and Delivery System (EDS) was reflective of changes to the NHS system architecture
- providing guidance and advice to support the capability of staff to support delivery of our equalities and health inequalities legal duties
- seeking to reduce barriers to information and care associated with a disability by reviewing the Accessible Information Standard (AIS)
- identifying how to improve equality information and continuing to ensure that the COVID-19 response effectively considered the Public Sector Equality Duty (PSED), equality considerations and associated health.
During 2022/23, the National Advisor for LGBT Health and his team continued to work on a number of priority areas to reduce health inequalities for LGBT+ people. We expanded the commissioning of ‘Phase 2’ of the Rainbow Badge project to support a further 45 NHS trusts in their work to address LGBT+ health inequalities and to ensure an inclusive workplace for their LGBT+ staff. We also developed a detailed evaluation framework for the project to measure its impact.
The LGBT Health team set up the NHS England LGBT+ Sounding Board. The group is made up of 20 volunteers who have lived experience of being LGBT+ and knowledge of the health inequalities faced by their communities. The group served as a resource for NHS England policy teams to better support feedback, engagement, co-production and consultation on areas of relevance to LGBT+ people. In 2022/23 four priority topics were identified: mental health, trans and non- binary people’s health, primary care and young LGBT+ people’s access to services.
The learning from the ‘Improving Trans and non-binary people’s Experience of Maternity Services’ (ITEMS) project was used to support the development and delivery of a training and support package for perinatal services to better address inequalities in experience and outcomes for trans and non-binary people accessing maternity services. We worked with colleagues across NHS England to propose a recommended approach to LGBT+ inclusive language across the organisation.
3.3 Healthcare inequalities improvement programme
The national Healthcare Inequalities Improvement Programme undertook a range of work in 2022/23 to reduce health inequalities. There was a particular emphasis on efforts across the system. In October 2022, we reported to the NHS England Board in our Annual report on NHS England’s work on healthcare inequalities, to improve access, experience and outcomes for all. This report provided examples of work
that had implications for groups that share protected characteristics. This report, drew on the Health Profile for England, 2021 published by Public Health England. That report and the annual report acknowledged that the COVID-19 pandemic had highlighted stark health inequalities across England, exacerbated existing inequalities and had had an unequal impact across ethnic groups.
In July 2022, the NHS England Board agreed to support the ongoing work provided by the NHS Race and Health Observatory (RHO) to the NHS and the wider health system to tackle health inequalities related to the protected characteristic of race.
COVID-19 was identified as one of the five core priorities for the RHO. In November 2022, working in partnership with three universities, the RHO published a report, REACH-OUT: Caring for the healthcare workforce post-COVID-19. This report was part of a longitudinal study looking at the impacts of long-COVID on the physical and mental health of healthcare workers, and the broader impacts on their working, social and family lives.
3.4 Workforce Equality Diversity Inclusion (EDI) programme
The Equality and Inclusion team has a mandate to develop a national strategy to make the NHS future-proofed in equality, diversity and inclusion (EDI) where everyone counts and experiences a sense of belonging – part of our NHS constitutional values.
The team developed a practical plan that would provide systems and employers with a ‘compendium of actions’ for improving equality and diversity within their workforce. Key work, undertaken during 2022/23, focused on how to distil lived experience and research evidence into 6 High Impact Actions (HIAs). These HIAs formed the basis of the NHS EDI Improvement Plan. In addition, to developing the NHS EDI Improvement plan, the team also contributed to the development of resources and guides to the system in response to recommendations from the Messenger Review. The 6 High Impact Actions notified to the system were:
- HIA1 Chief executives, chairs and board members will have specific and measurable EDI objectives to which they will be individually and collectively
- HIA2 All organisations must embed fair and inclusive recruitment processes and talent management strategies that target under-representation and lack of diversity.
- HIA3 Every organisation should develop and deliver an improvement plan to eliminate pay gaps.
- HIA4 Every organisation should develop and deliver an improvement plan to address health inequalities within their workforce.
- HIA5 NHS organisations must develop and deliver a comprehensive induction, onboarding and development programme for internationally recruited staff.
- HIA6 NHS organisations will create an environment which eliminates the conditions in which bullying, discrimination, harassment and physical violence at work occurs.
3.5 The Workforce Disability Equality Standard
The Workforce Disability Equality Standard (WDES) is a mandated standard that provides a strategic direction for disability equality. A WDES national data collection takes place annually. Trusts collect, report and publish data against a collection of ten metrics that compare the workplace experiences of Disabled and non-disabled staff as at 31 March of each year. A national WDES report is published annually with an analysis of trends, recommended actions and key findings. The WDES is mandated for NHS trusts and NHS foundation trusts and, on a voluntary basis, covers arm’s-length bodies (ALBs). The purpose of the WDES is to identify and close the gaps in experience between disabled and non-disabled staff.
In May 2022, NHS England published, the Workforce Disability Equality Standard: 2021 data analysis report for NHS trusts and foundation trusts, together with an Easy read version of this report and the Excel file, setting out key data. This report provided an analysis of the WDES data returns from NHS trust and foundation trusts from 2019 to 2021. It provided the second opportunity to compare year on year progress into the career and workplace experiences of NHS disabled staff.
During 2022/23, the WDES team worked on the collection of data for the 2022/23 report. A set of resources were developed or updated to help prepare and support NHS Trusts and Foundation Trusts.
Published in March 2022, the NHS Disabled staff experience during COVID-19 report contained 9 recommendations on learning from the pandemic to improve experience of disabled staff. Working in conjunction with NHS Employers, the WDES team conducted research into the experiences of Disabled staff in Wave 1 of the Covid-19 pandemic. During 2022/23 guidance, including on areas such as flexible working policies, was given to the system.
During 2022/23, the WDES implementation team used qualitative data from past WDES data collections to create evidence-based information on effective interventions. These were shared and added to a growing repository available to NHS staff. The WDES implementation team completed focused work on ambulance trusts, leadership development and the experiences of staff who are deaf or hard of hearing. The WDES Innovation Fund continued to support trusts to develop and share good practice across key areas such as reasonable adjustments, neurodivergence, digital empowerment passports and testing new technology.
3.6 The Workforce Race Equality Standard
The Workforce Race Equality Standard (WRES) supports organisations involved in NHS service delivery to identify and evidence progress and close gaps in experience between BME and White staff. WRES reports since 2015 have shown year-on-year improvements across some WRES indicators.
In 2022, the work programme focused on translating data by providing bespoke improvement actions within trusts. Specific interventions to improve race equality were incorporated in the NHS EDI Improvement plan to provide further focus on leadership accountability, provider responsibility and strategies to deliver sustainable, evidence-based and future-focused advancement of race equality across all professional groups and hierarchies. This included areas such as embedding ethnicity pay gap reporting across all organisations, further implementation of the International Medical Graduates onboarding programme and the development of the International Educated Nurses induction programme.
The NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts, alongside the raw data, was published in February 2023 (this data was at 31 March 2022 and is the latest data available as at May 2023).
3.7 Clinical areas and equalities
This section provides equality information focusing on the clinical priority areas identified in NHS England Business Plan for 2022/23. Where major equality focused initiatives were developed prior to 2022/23, an explanation of the initiative and the year in which it was launched has been provided to set the work undertaken in 2022/23 in context.
3.7.1 Cancer
During 2022/23, making improvements across different cancer types continued to be critical to help achieve the NHS Long-Term Plan ambition of diagnosing 75% of patients at an early stage (stage 1 and 2) by 2028 and reducing inequalities in cancer survival. The Core20PLUS5 approach to reducing health inequalities continued to include early cancer diagnosis as a core objective. We continued to recognise the particular challenges for a number of different population groups and directly targeted our activity at areas we knew would make a difference, including:
- Awareness raising campaigns: The NHS ‘Help Us, Help You’ (HUHY) cancer campaigns aimed to increase awareness of cancer symptoms, address barriers and encourage people to get checked. Some campaigns focused on specific symptoms, including those linked to common (lung cancer) and rare and less common cancers (such as our HUHY abdominal and urological symptoms campaign), while others focused on fear as a barrier to help-seeking, relevant across all cancer types. The key target audiences for these campaigns were people aged 50 and over living in more deprived areas, as well as groups who may have particular risk factors such as people from Black and South Asian communities.
- Targeted lung health checks: We continued to deliver targeted lung health checks to people aged 55-74 who have ever smoked in areas with high lung cancer mortality rates and high levels of deprivation. In 2022/23, an additional 23 sites went live, taking the total number of live sites to 43 by the end of the year. Over the lifespan of this project, a total of 1,625 lung cancers have been diagnosed, 76% of those at stage 1 or 2.
- Our approach to innovation: A cross-England trial of the Galleri blood test, which could be used to detect a range of cancers, continued during 2022/23 to see how well the test works in the NHS. The trial recruited a representative sample from minority ethnic groups. A call for innovations also embedded equality and health inequality impact assessments into the submission and implementation process.
- Understanding and improving experience: The second National Under 16 Cancer Patient Experience Survey (U16 CPES) results were published in November 2022. The survey was developed with the support of children with cancer, parents/carers of children with cancer, NHS staff, charities and other While the results were extremely positive, with parents/carers giving a mean rating of 9.01 out of 10 for overall experience of their child’s care, we confirmed our ambition to continuously improve. This led to the development of a Cancer Experience of Care Improvement Collaborative with providers and partners in a number of areas across the country focusing on key themes of communications and information, facilities and home comforts, and emotional support as areas to improve experience for children and families. The Collaborative continued its work during 2022/23.
3.7.2 Learning Disability and Autism
The Operational and Planning Guidance, published in December 2022, set out a number of key actions to address the needs of people with a learning disability and autistic people including:
- Continuing to improve the accuracy and increase the size of GP Learning Disability registers
- Increase the rate of annual health checks for people aged 14 and over on a GP learning disability register, working towards the 75% ambition in 2023/24
- Reducing reliance on mental health inpatient care for adults and children with a learning disability and autistic people and to develop community services to support admission avoidance and timely discharge
- Developing integrated, workforce plans for the learning disability and autism workforce to support delivery of the NHS Long Term Plan objectives,
The NHS made good progress in increasing the number of annual health checks (AHC) for people aged 14 and over on a GP learning disability register. In the 10- month period between April 2022 and January 2023, 57% of people had received an AHC, an improvement of 26% on the equivalent period in the previous year.
Work continued to improve the accuracy of GP learning disability registers in relation to the identification and coding of patients, particularly for underrepresented groups such as children and young people (CYP) and ethnic minorities.
The LeDeR (Learning from the Lives and Deaths of People with a Learning Disability and Autistic People) programme continued to work to improve care and reduce health inequalities for people with a learning disability and autistic people and prevent people with a learning disability and autistic people from early deaths. The programme rolled out intersectionality training to the LeDeR workforce through December 2022 which considered people’s overlapping identities and experiences (such as race and gender) to understand the complexity of prejudices they face.
People from minority ethnic communities and autistic adults continued to receive a focused LeDeR review.
In line with the NHS Long Term Plan commitment, that staff across the NHS will improve their understanding of the needs of people with a learning disability and autistic people, the Oliver McGowan mandatory training on learning disability and autism launched in November 2022. The training programme, which has been co- produced with people with lived experience, has been trialled with over 8,300 health and care staff.
Reducing reliance on mental health inpatient care for people with a learning disability and autistic people remained a key priority for the NHS. At the end of January 2023, the number of people with a learning disability and autistic people in a mental health inpatient setting was 2,020. This represented a decrease of 30% since March 2015. We have further to go to achieve the ambition set out in the NHS Long Term Plan of a reduction of 50% by March 2024. Work continued to support local areas to develop community services as alternatives to mental health inpatient care. In 2022/23, NHS Long Term Plan investment in community services including Children and Young Peoples keyworkers was £75 million.
As at July 2022, there were just over 125,000 people waiting for an autism diagnostic assessment, of which over 105,000 had waited longer than 13 weeks (the NICE standard). This represented a 33% increase since October 2021. In 2022/23, NHS England published Sensory Environments Resource Pack and a autism research strategy and developed an all-age autism assessment guidance framework for commissioners, providers, and clinicians, as well as supporting data quality improvements across systems.
3.7.3 Maternity
In September 2021, NHS England published robust, coproduced Equity and Equality guidance for Local Maternity and Neonatal Systems (LMNS). The purpose of the guidance was to ensure that women and babies, no matter what their ethnic background or where they live, get safe, compassionate care that meets their needs. The guidance set out 22 interventions for LMNS to implement locally along with the support that is on offer for them to do this. The NHS approach to improving equity (Core20PLUS5) involves implementing midwifery continuity of carer, particularly for women from minority ethnic communities and from the most deprived areas; this should be in line with the principles around safe staffing that NHS England set out in September 2022. In addition, NHS England began to pilot and evaluate a new service model – enhanced midwifery continuity of care – designed to reduce inequalities in the 10% most deprived neighbourhoods nationally. Enhanced Midwifery Continuity of Carer (MCoC) teams work in the same way as standard MCoC teams, but additional funding is provided to provide more holistic support that reduces midwives’ workload and releases additional time for midwives to care for women who are more likely to experience poorer maternity outcomes.
The guidance asked LMNS to publish equity and equality action plans by 30 September 2022. Every LMNS produced a plan and every plan was reviewed by NHS England. The review identified good practice and what further support was needed to improve equity and equality. Most LMNS published their equity and equality action plan in 2022/23; NHS England’s regional teams will continue to work with the remaining systems to ensure their plans are published.
The aims of the guidance are to improve: equity for mothers and babies from Black, Asian and Mixed ethnic groups and those living in the most deprived areas; and race equality for staff. Based on the five health inequalities priorities in the 2021/22 Implementation Guidance*, the guidance was designed to help LMNS align their equality and equality action plans with Integrated Care Systems’ health inequalities work. The guidance included an analysis of the evidence, interventions to improve equity and equality, resources, indicators and metrics. It set out interventions under each of the 5 health inequalities priorities previously referenced.
*21/22 Priorities and Operational Planning Guidance: Implementation guidance, NHS England, March 2021. Five priorities: Priority 1: Restore NHS services inclusively; Priority 2: Mitigate against digital exclusion; Priority 3: Ensure datasets are complete and timely; Priority 4: Accelerate preventative programmes that proactively engage those at greatest risk of poor health outcomes; Priority 5: Strengthen leadership and accountability.
Alongside this guidance NHS England published four pledges to improve equity for mothers and babies and race equality for staff. The four pledges are intended to help create a shared understanding of why work on equity and equality is needed, and the aims and outcomes of this work. The four pledges may be used in co- production work – where women and their families and NHS staff work in partnership to design, improve and evaluate services (NHS pledges to improve equity for mothers and babies and race equality for staff, NHS England, September 2021). Pledge 4 includes a focus on mortality rates for babies from Black, Asian and mixed ethnic groups and maternal mortality rates by ethnicity*.
*Pledge 4: The NHS will measure progress towards the equity aims. The NHS will track the outcome of its plans. The NHS will continue to track: the mortality rates for babies from Black, Asian and mixed ethnic groups; the mortality rates for babies born to mothers living in the most deprived areas; maternal mortality rates by ethnicity; maternal mortality rates for women living in the most deprived areas.
An evaluation of the Equity and Equality Guidance commenced in February 2023.
In March 2022, the Women and Equalities Committee (WEC) launched a short inquiry to bring together the different work by a number of committees on black maternal health, improve scrutiny and make recommendations to Government. In addition to the WEC, the committees were the Petitions Committee, Health and Social Care Committee and the Joint Committee on Human Rights (JCHR).
Following an evidence session in March 2022, NHS England’s National Clinical Director for Maternity and Women’s Health gave evidence to the Committee on 13 July 2022. In a letter, dated 3 November 2022, from NHS England’s Chief Midwifery Officer and National Maternity Safety Champion, we provided additional evidence on the following matters: the disparities in health outcomes; equity and its priority in the NHS; culturally sensitive care and addressing bias, microaggressions and racism; Midwifery continuity of carer (MCoC) implementation; investment in the maternity services workforce; the feasibility of setting targets for reducing maternal health disparities; and the Maternity Disparities Taskforce.
In December 2022, a report to NHS England’s Board about services covered the protected characteristic of maternity and pregnancy. This report noted that outcomes were good for most babies born to women with a Covid-19 infection, but that higher COVID-19 infection rates and higher mortality rates in pregnant women with COVID-19 had contributed to the increase in stillbirth rate and there was some evidence of an increase in neonatal mortality rate. Subsequently, the ONS has published data confirming this in Child and infant mortality in England and Wales – Office for National Statistics (ons.gov.uk).
3.7.4 Mental Health
In July 2019, the five-year NHS Mental Health Implementation Plan 2019/20 – 2023/24 was published. This plan was underpinned by a clear commitment to advance equalities in mental health. In 2019, alongside the strategy, NHS England commissioned the development of a toolkit which provides advice on how to set up and deliver local, data-driven actions to reduce inequalities in access, experience, and outcomes within mental health services. In October 2020, the Advancing mental health equalities strategy was published which summarised the core actions needed to bridge the gaps for communities fairing worse than others in mental health services. It was also an important element of the overall NHS plans to accelerate action to address health inequalities in the next stage of responding to COVID-19.
It remained an expectation that the strategy and toolkit would be used when systems develop and deliver their plans. The Core20PLUS5 approach to reducing health inequalities continued to include a focus on reducing avoidable mortality in people with serious mental illness through focused implementation of the annual physical health checks and appropriate follow-up interventions for people with severe mental illness. Other relevant pieces of work NHS England undertook during 2022/23 to advance mental health equalities included:
- introducing four specific metrics relating to outcomes, access and experience. All four metrics are now routinely part of the quarterly monitoring and assurance reporting at regional and national These are:
- NHS Talking Therapies Recovery rates for Black, Asian and minority ethnic communities completing treatment
- The proportion of Black, Asian and minority ethnic people admitted as an adult acute mental health inpatient who had no contact with community mental health services in the prior year
- NHS Talking Therapies access to older adults (65+) population
- Acute inpatient length of stay – adult and older adult (18-64, and 65+) population
- NHS England developed a data dashboard that provides a breakdown of the ethnic background of people detained under different sections of the Mental Health Act (MHA). The dashboard reports data at national, regional, ICS and provider level, enabling systems and providers to more easily identify inequalities in terms of who is detained locally. It therefore enabled and enables NHS England to take targeted action to address this.
- Data quality and data availability present a significant limitation at a national level, which is why improving data quality and flow to national datasets is an ‘urgent action’ to advance equalities in mental health. However, the range of data available, during 2022/23, has been and is steadily improving thanks to the ongoing work to deliver the recommendations of the Mental Health Act review.
- In January 2023, NHS England commissioned a two-year quality improvement programme to improve the care that people receive in hospital when detained, with a focus on addressing inequalities in outcome and experience for people from an ethnic minority background and people with a learning disability and autistic people.
- A key way of addressing inequalities around MHA detention is to provide people with tailored mental health support earlier, in their communities. NHS England continued to expand access to new integrated models of primary and community mental health care. The transformation of community services focused on co-producing models of care with service users, families and carers, as well as close partnership working with the VCSE sector.
- NHS England introduced a metric to monitor the disparity in admissions with no prior contact between service users from a White British background and service users from an ethnic minority National data indicates that service users from an ethnic minority background have had a consistently higher rate of admissions to hospital with no prior contact with community mental health services. (In Q1 2022/23, 16% of admissions had no prior contact for those from an ethnic minority background compared to 12% for those from a White British background.
- The NHS Long Term Plan committed to provide physical health checks for people with severe mental illness (SMI). NHS England continued to work on a range of activities to close this gap particularly by increasing the number of people with SMI receiving an annual physical health check in the last 12 months to 390,000 by 2023/24 (in the 12 months to Quarter 3: 2022/23, 256,000 people received a physical health check). The annual physical health check focuses on early identification of preventable physical illnesses that are likely to affect people with SMI, and should be followed up with appropriate follow-up interventions. To expand on improving SMI physical health checks, a range of prevention programmes were and are offered, including, specialist mental health smoking cessation support to inpatients and in communities, while the flagship CORE20PLUS5 approach to tackling health inequalities – which covers both SMI physical health checks and smoking cessation – continued to be embedded across all ICBs as a matter of priority.
- NHS England published the draft Patient and Carer Race EqualityFramework (PCREF), one of the recommendations from the Independent Review of the Mental Health Act.
- The PCREF was co-produced with experts by experience, along with four PCREF pilot trusts, in partnership with their ethnic minority-led VCSE organisations, ethnic minority communities, patients and carers.
- The PCREF aims to improve access to care for people from ethnic minorities and the experiences and outcomes of care received from mental health services. This covers inpatient services, and community and crisis mental health services, who need to play a vital role in reaching and supporting people from ethnic minorities, so that their mental health does not reach a point that they require an admission under the MHA.
- NHS England aims to publish the PCREF by 2023/24.
- Culturally appropriate advocacy pilots – DHSC commissioned and oversaw the piloting of different models of culturally appropriate advocacy for people from ethnic minority groups between November 2021 and June 2022. This followed a commitment in the Government’s Reforming the Mental Health Act White Paper to taking forward such pilots, to build understanding of how culturally appropriate advocacy services might be deployed in the future to address racial disparities in the application of the Mental Health Act, given the particularly stark inequalities in detention rates. During 2022/23, DHSC said it planned to commission a second phase of pilots.
Priority F of the 2022/23 priorities and operational planning guidance specifically focused on improving mental health services and services for people with a learning disability and/or autistic people – maintaining continued growth in mental health investment to transform and expand community health services and improve access. The 2023/24 priorities and planning guidance set out specific commitments on recovery and mental health. The guidance set out expectations in relation to mental health services under the banner of delivering the key NHS Long Term Plan ambitions. It focused on transforming the NHS by improving ‘mental health data to evidence the expansion and transformation of mental health services, and the impact on population health, with a focus on activity, timeliness of access, equality, quality, and outcomes data’ (Planning Guidance 2022/23: Section 2A).
The objectives in relation to mental health are to:
- Improve access to mental health support for children and young people in line with the national ambition for 345,000 additional individuals aged 0-25 accessing NHS funded services (compared to 2019)
- Increase the number of adults and older adults accessing NHS Talking Therapies
- Achieve a 5% year on year increase in the number of adults and older adults supported by community mental health services
- Work towards eliminating inappropriate adult acute out of area placements
- Recover the dementia diagnosis rate to 7%
4. Meeting our Public Sector Equality Duty (PSED): employment reporting and information for NHS England staff
4.1 Context
The information in this part of the report is the employment data for NHS England staff as at 31 December 2022. This data is impacted by the merger of NHS Improvement into NHS England, which took place on 1 July 2022. This report references the Combined Gender Pay Gap Report for NHS England and NHS Improvement published on 30 March 2023, which looked at employment data as at 31 March 2022.
The employment data is likely to have been impacted by: the external recruitment freeze from 1 July 2022, which continues to apply; the transformation programme; the merger of NHS Improvement into NHS England; and the decision to seek a reduction in staff numbers of up to 40% across the new NHS England.
In these circumstances, any meaningful comparisons in employment data from 31 March 2022 to 31 December 2022 is difficult. Similarly, it is difficult to compare the data in the Combined Gender Pay Gap Report for 2022 with the Combined Gender Pay Gap Report for 2021.
4.2 Gender of staff and senior managers
The percentage of the total ‘on payroll’ workforce who were women decreased by 1%, to 69%, from March 2022 to December 2022. There was a 2% decrease in the number of female senior managers to 56% over the same period and 44% of senior managers identified as male. 69% of staff identified as female and 31% identified as male.
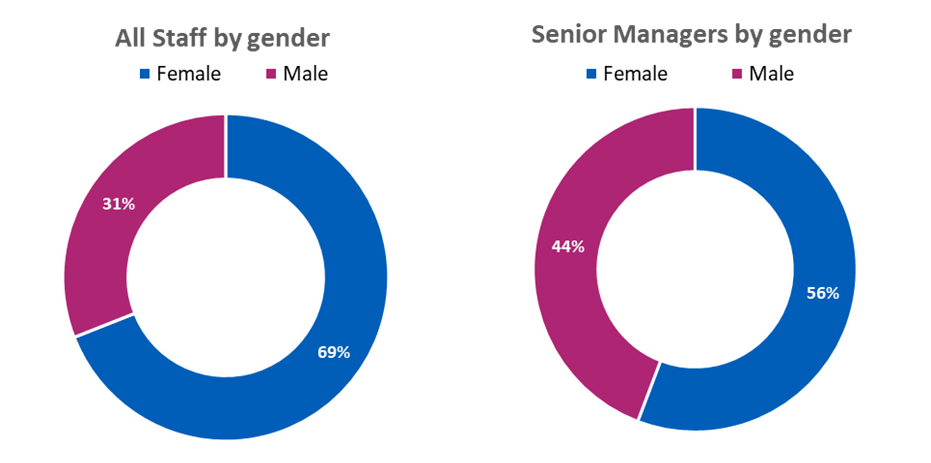
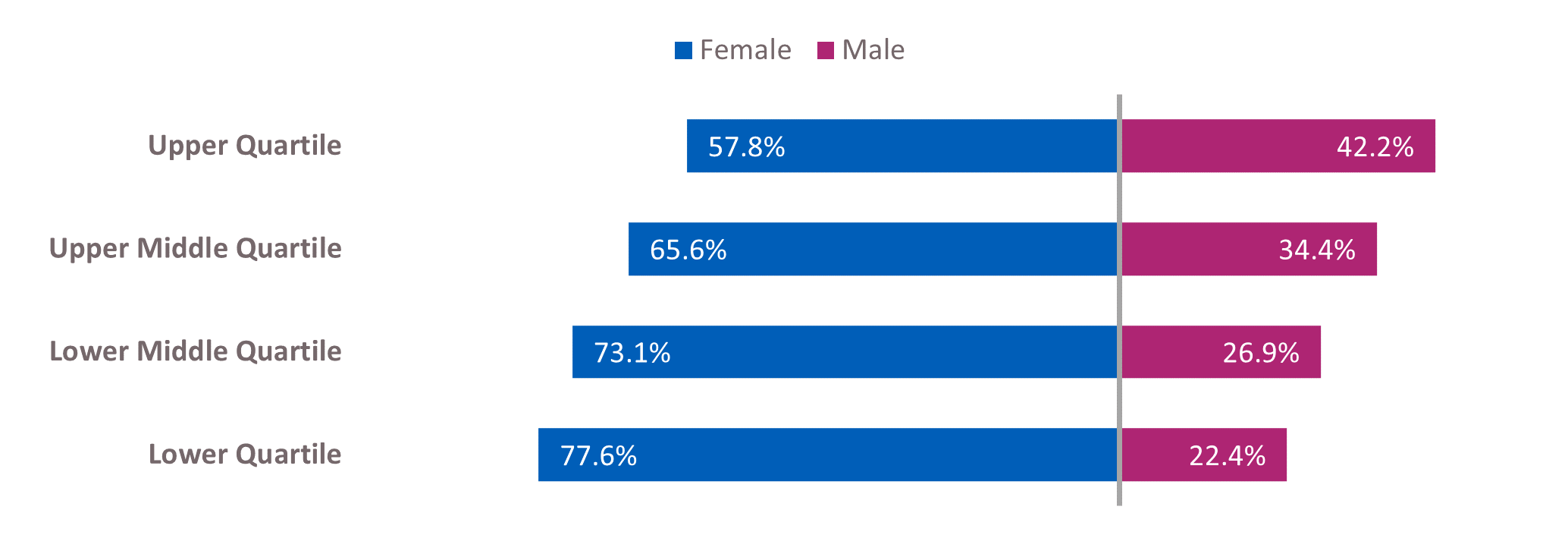
|
|
Female |
Male |
|
|
Upper Quartile |
57.8% |
|
42.2% |
|
Upper Middle Quartile |
65.6% |
|
34.4% |
|
Lower Middle Quartile |
73.1% |
|
26.9% |
|
Lower Quartile |
77.6% |
|
22.4% |
Working in partnership with our recognised trade unions and our Women’s Network, we continued to progress initiatives to address gender inequality in our workforce.
Our Gender Pay Action Plan, published on 30 March 2023, included specific priorities around recruitment practice, reward and recognition, flexible working, developing talent pipelines and intersectionality. The Gender Pay Gap Report is a combined report for NHS England and NHS Improvement and the quartile data, provided above, is drawn from this report.
4.3 Ethnicity of staff and senior managers
The proportion of people employed by NHS England who considered themselves to be from a BME heritage increased from 21% (March 2022) to 22% (December 2022). The proportion of senior managers who considered themselves to be from a BME heritage decreased from 17% to 16%. 71% of staff identified as White, 22% identified as BME and 7% did not identify their ethnicity. 74% of senior managers identified as white, 16% identified as BME and 10% did not identify their ethnicity.
We continued to use the annual publication of the WRES data as a driver for improving the working lives of BME staff. NHS England continued to pursue the target that by 2025 at least 19% of all senior staff will be from BME backgrounds.
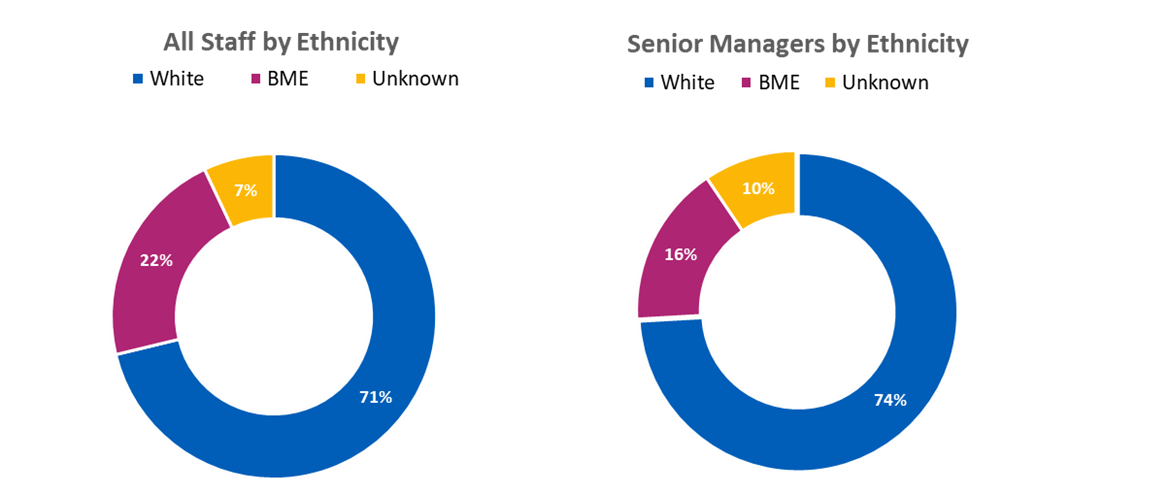
4.4. Declarations of disability or long term conditions
We continued to work with our Disability and Wellbeing Network (DAWN) to support employees within the workplace and sought to ensure that decisions relating to employment practices were objective, free from bias and based solely on work criteria and individual merit. These principles are reinforced in our joint Recruitment and Selection and our Equality, Diversity and Inclusion in the Workplace policies.
The percentage of staff who declared a disability or long term condition is in the charts below.
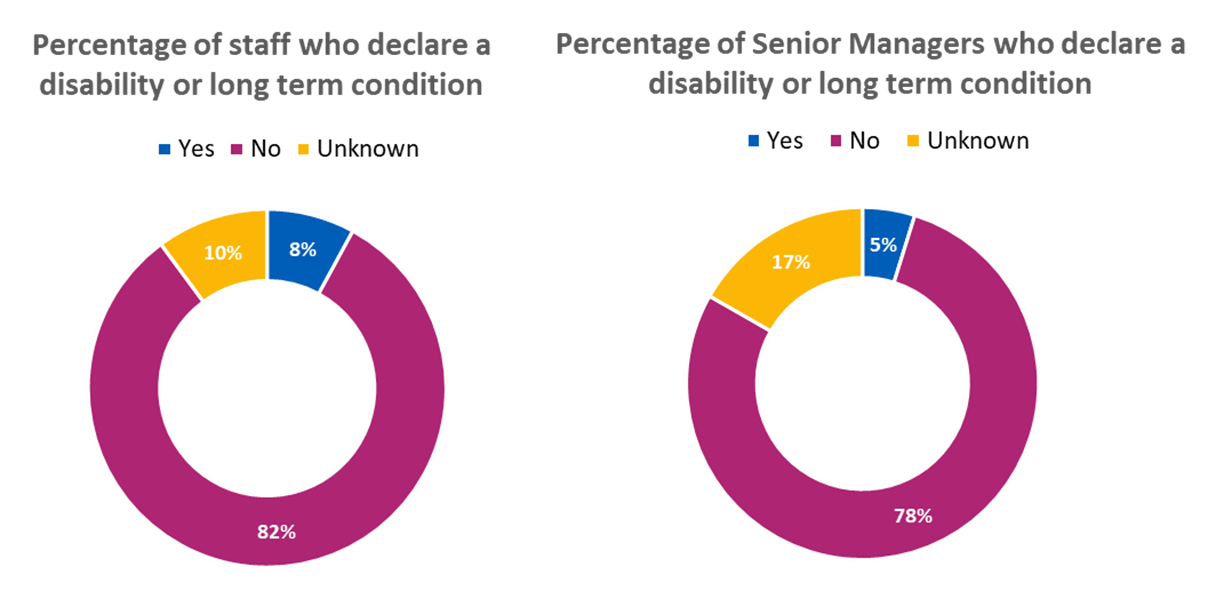
82% of staff declared they did not have a disability or long term condition, 8% did declare a disability and 10% did not declare whether or not they had a disability (unknown). 78% of senior managers declared they did not have a disability or long term condition, 5% did declare a disability and 17% did not declare whether or not they had a disability (unknown).
As a Disability Confident Employer, recognised by the Department for Work and Pensions, we continued to fulfil our commitments to employ more disabled staff, and support disabled staff to work, develop and progress. We also recognised the need to increase the level of reporting and improve the unknown numbers.
4.5 Sexual orientation of staff and senior managers
80% of staff identified as heterosexual, 5% identified as lesbian, gay or bisexual (LGB) and 15% did not identify their sexual orientation (unknown). 74% of senior staff identified as heterosexual, 4% identified as LGB and 22% did not declare their sexual orientation (unknown).
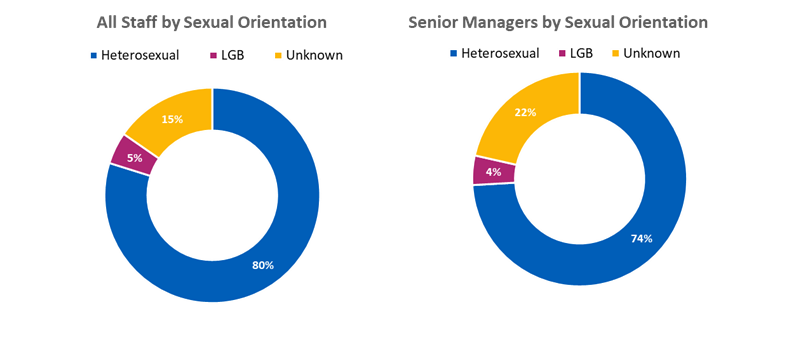
5. Meeting our Public Sector Equality Duty (PSED): employment reporting and information for NHS Improvement staff
5.1 Context
NHS Improvement (formally Monitor and the NHS Trust Development Authority) still existed from April 2022 to the end of June 2022. NHS Improvement merged into NHS England on 1 July 2022. This report references the Combined Gender Pay Gap Report for NHS England and NHS Improvement published on 30 March 2023, which looked at employment data as at 31 March 2022. It is difficult to compare the data in the Combined Gender Pay Gap Report for 2022 with the Combined Gender Pay Gap Report for 2021. Similarly, comparing employment data as at 30 June 2022 with the data as at 31 March 2022 presents similar difficulties.
5.2 Gender of staff and senior managers
63% of staff identified as female and 37% identified as male. 52% of senior managers identified as female and 48% identified as male.
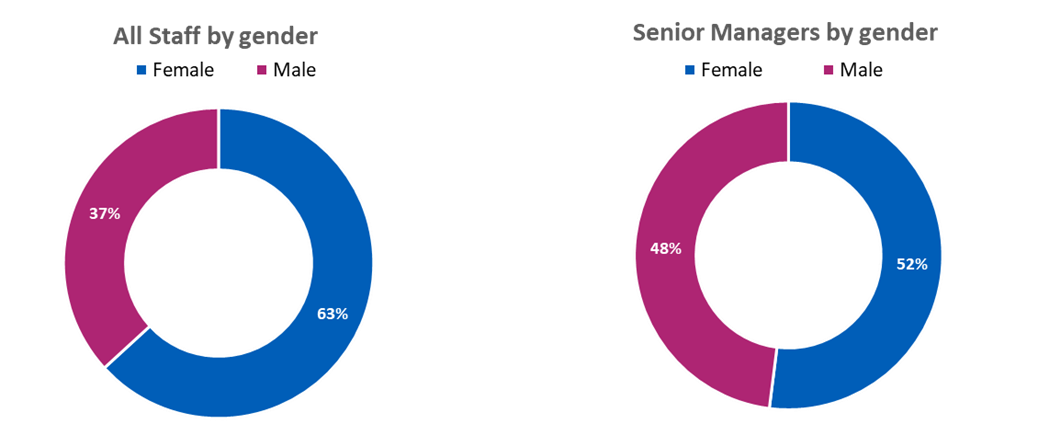
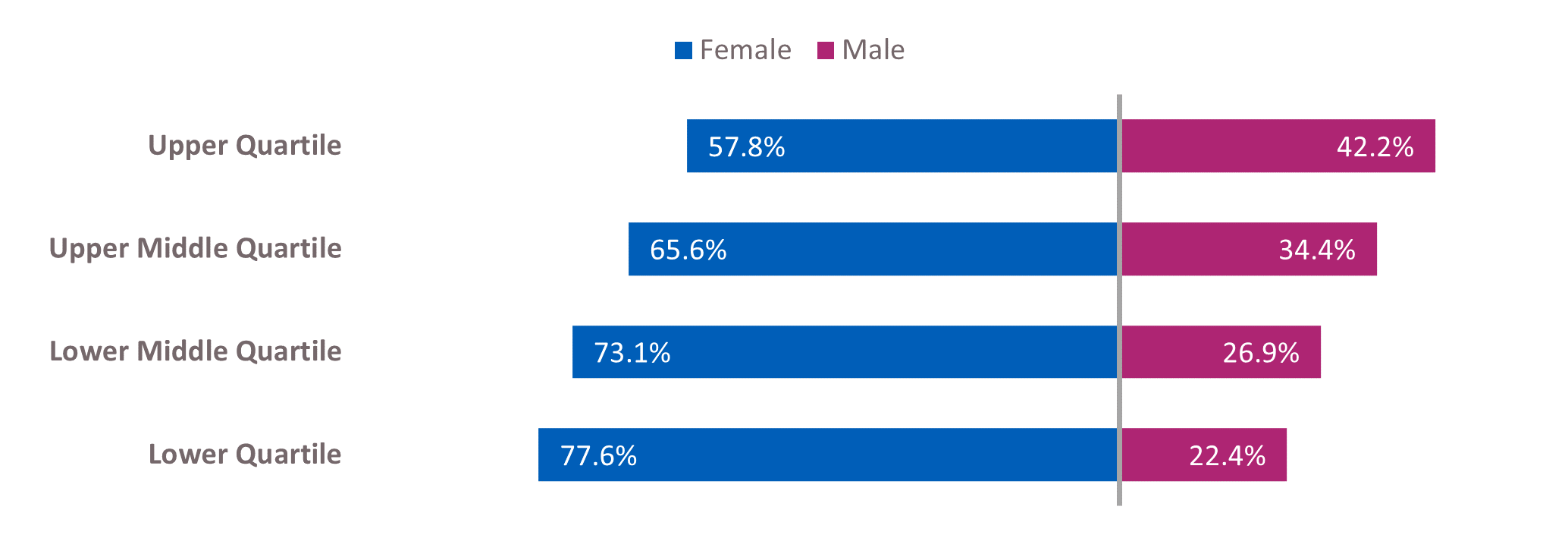
|
|
Female |
Male |
|
|
Upper Quartile |
57.8% |
|
42.2% |
|
Upper Middle Quartile |
65.6% |
|
34.4% |
|
Lower Middle Quartile |
73.1% |
|
26.9% |
|
Lower Quartile |
77.6% |
|
22.4% |
Working in partnership with our recognised trade unions and our Women’s Network, we continued to progress initiatives to address gender inequality in our workforce.
The Gender Pay Gap Report was published on 30 March 2023. This report included gender pay gap data for NHS Improvement as at 31 March 2022. The quartile data, provided above, is drawn from this report.
5.3 Ethnicity of staff and senior managers
As at 30 June 2022, 75% of staff identified as white, 20% identified as BME and 5% did not identify their ethnicity (unknown). 82% of senior managers identified as white, 12% identified as BME and 6% did not identify their ethnicity (unknown). We continued to use the annual publication of the WRES data as a driver for improving the working lives of BME staff. Until the dissolution of NHS Improvement, NHS England and NHS Improvement continued to work together to pursue the target that by 2025 at least 19% of all senior staff would be from BME backgrounds.
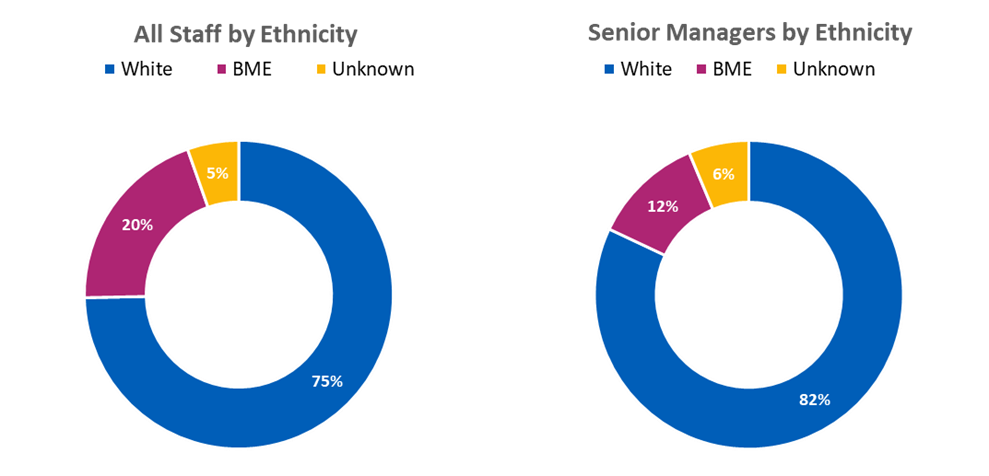
5.4 Declarations of disability or long term conditions
We continued to work with our Disability and Wellbeing Network (DAWN) to support employees within the workplace and sought to ensure that decisions relating to employment practices were objective, free from bias and based solely on work criteria and individual merit. These principles are reinforced in our Recruitment and Selection and our Equality, Diversity and Inclusion in the Workplace policies. The percentage of staff who declared a disability or long term condition is in the charts below.
78% of staff declared they did not have a disability or long term condition, 6% did declare a disability and 16% did not declare whether or not they had a disability (unknown). 75% of senior managers declared they did not have a disability or long term condition, 5% did declare a disability and 20% did not declare whether or not they had a disability (unknown).
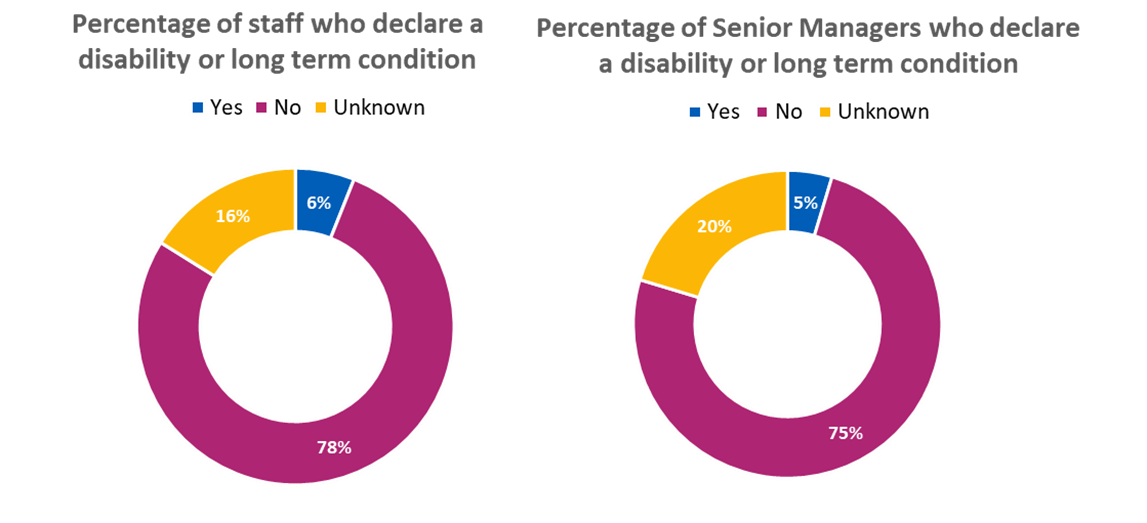
As a Disability Confident Employer, recognised by the Department for Work and Pensions, we continued fulfil our commitments to employ more disabled staff, and to support disabled staff to work, develop and progress.
5.5 Sexual orientation of staff and senior managers
74% of staff identified as heterosexual, 4% identified as lesbian, gay or bisexual (LGB) and 22% did not identify their sexual orientation (unknown). 70% of senior managers identified as heterosexual, 3% identified as LGB and 27% did not identify their sexual orientation (unknown).
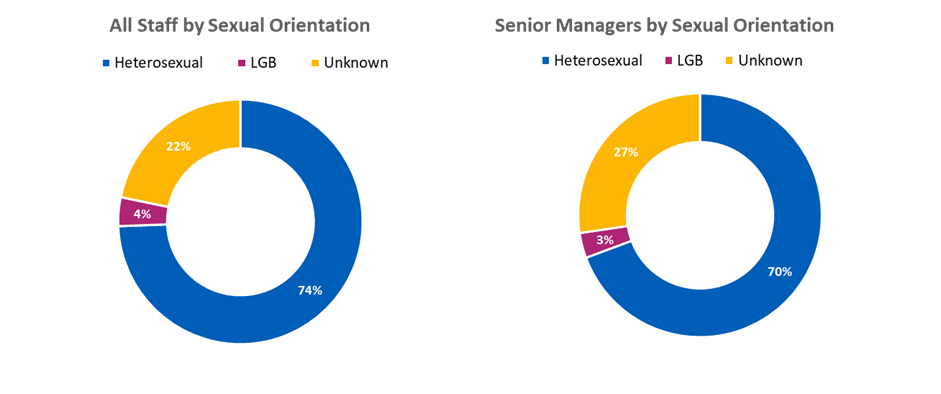
Appendix 1: Introduction to the general and specific public sector equality duties
The public sector equality duty
The Public Sector Equality Duty (PSED) consists of the general equality duty, and the statutory regulations, the Specific Equality Duties (SEDs).
Understanding the general equality duty
Section 149 (1) of the Equality Act 2010, requires a public body (such as NHS England), in the exercise of its functions, to have due regard to the need to address three equality aims:
- to eliminate discrimination, harassment, victimisation and any other conduct that is prohibited by or under this Act
- to advance equality of opportunity between persons who share a relevant protected characteristic and persons who do not share it
- to foster good relations between persons who share a relevant protected characteristic and persons who do not share it.
The Equality and Human Rights Commission (EHRC) has responsibility for the promotion and enforcement of the Equality Act 2010 and the Specific Equality Duties. The Equality Act 2010 lists the relevant protected characteristics which the three equality aims apply to as:
- age
- disability
- gender reassignment
- pregnancy and maternity
- race (including: colour, nationality, and ethnic or national origins),
- religion or belief
- sex
- sexual orientation
Marriage and civil partnership, also a protected characteristic under the Equality Act 2010, is partially covered by the general equality duty. For this protected characteristic, the first equality aim (elimination of discrimination, harassment, victimisation, and any other conduct prohibited by the Equality Act 2010) applies but only in relation to work as other functions covered by the Act do not apply.
The general equality duty means that a public body must properly consider all three equality aims in all the activities that it undertakes, including: employing staff, commissioning, procurement, planning services, and fulfilling statutory and legal obligations.
Understanding the specific equality duties
The Equality Act 2010 provided Ministers with the power to ‘impose’ Specific Equality Duties (SEDs) to enable ‘the better performance’ of the general Equality Duty’s three equality aims. The first SEDs were agreed in parliament and published in 2011. The current regulations were published in 2017. These statutory regulations were updated in July 2022 following the passage of the Health and Care Act 2022. The changes in July 2022 made the ‘new’ NHS England, ICBs and other NHS organisations cited in the 2022 Act subject to the SEDs.
These provisions apply to most public bodies, including the new NHS England and other organisations that exercise public functions. The key statutory regulations placed on listed bodies including NHS England are:
- Gender pay gap reporting [ 3]
- Publication of information to demonstrate compliance with one or more of the 3 equality aims and people who share a relevant protected characteristic who are NHS England’s employees [ 4(3a)]
- Publication of information to demonstrate compliance with one or more of the 3 equality aims and people who share a relevant protected characteristic who are affected by NHS England’s policies and practices [ 4(3b)]
- Publication of one or more equality objectives that it thinks it should do to achieve one or more of the Equality Duty’s equality aims [ 5]
- Manner of publication: The information should be accessible to the public but information can be published within other documents [ 6]
The purpose of the SEDS
- Equality aims: Are to meet 1 or more of the 3 general duties’ equality aims (SEDs 2017, reg 5)
- Measurable: To be specific and measurable (SEDs 2017, reg 5).
- Proportionate: At least one equality objective (EO). ‘There is no upper limit, but it will need to adopt a proportionate approach, depending on the relevance of its functions and their size.’ [EHRC Technical Guidance (TechGuid): England, 6.36]
- Evidence: To consider properly its choice of published objectives, a listed authority should have sufficient evidence of the impact of its policies, practices and functions on people with different protected characteristics. This will enable the authority to have a clear understanding of the equality issues it faces. [EHRC TechGuid: England, 6.37]
- Impact: Listed authorities will need to prioritise which of these equality issues are the most pressing and so should form the subject matter of equality objectives. [EHRC TechGuid: England, 6.37]
- PSED still applies where no EO: ‘A listed authority that chooses not to publish an equality objective in respect of any protected characteristic will not be free to ignore that protected characteristic in the exercise of its functions. It will still have to comply with all the requirements of the general duty, regardless of whether it has set objectives in respect of all the relevant protected characteristics.’ [EHRC TechGuid: England, 6.38]
- Frequency of publication/revision and progress reports: Authorities can revise and publish objectives more regularly than every four A review of progress against the preceding objectives likely to help an authority’s selection of its subsequent objectives. [EHRC TechGuid: England, 6.43]
- Manner of publication: An authority ‘must publish its equality information and equality objectives in a manner which is accessible to the public and may publish this information within another published document.’ [EHRC TechGuid: England, 6.45]
Appendix 2: The Health Inequalities general duty and new health inequalities reporting requirements
The general duty
Duty as to reducing health inequalities – National Health Service Act 2006, section 13G as amended
NHS England must, in the exercise of its functions, have regard to the need to:
- reduce inequalities between persons with respect to their ability to access health services, and
- reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services (including the outcomes described in section 13E(3))
Note 1: The outcomes that must be considered in relation to 13G (b) are set out in section 13E (3).
Note 2: An equivalent general health inequalities duty is placed on the Boards of ICBs and some other bodies
Note 3: The Health and Care Act 2022 introduced or amended a range of other duties in relation to health inequalities
Note 4: Requirements placed on ICBs and others, introduced by the Health and Care Act 2022, require consideration of how the health inequalities duties have been addressed in annual reports and performance assessment.
13E Duty as to improvement in quality of services
1. NHS England must exercise its functions with a view to securing continuous improvement in the quality of services provided to individuals for or in connection with:
- the prevention, diagnosis or treatment of illness, or
- the protection or improvement of public
2. In discharging its duty under subsection (1) {NHS England] must, in particular, act with a view to securing continuous improvement in the outcomes that are achieved from the provision of the services.
3. The outcomes relevant for the purposes of subsection (2) include, in particular, outcomes which show:
- the effectiveness of the services,
- the safety of the services, and
- the quality of the experience undergone by patients.
4. In discharging its duty under subsection (1), NHS England must have regard to:
- any document published by the Secretary of State for the purposes of this section, and
- the quality standards prepared by NICE under section 234 of the Health and Social Care Act 2012.
Health inequalities duties and the Health and Care Act 2022
|
2022 Act |
2006 Act |
Placed on |
Impacts |
|
Section 6 & 25: Duties as to reducing inequalities |
13G and 14Z35 |
NHS England and ICBs |
Wider NHS |
|
Section 8, 25, 52, 67: Duty to have regard to wider effect of decisions |
13NA (2), 14Z43, 26A, 63A |
NHS England and ICBs, NHS, FTs, NHS Ts |
NHS England, ICBs, NHS Trusts and Public Benefit Corporations (s 11) |
|
Section 11: Information about inequalities |
13SA, Schs 4, 7 |
NHS England | |
|
Section 25: Duty to promote integration |
14Z42 |
ICBs | |
|
Section 25: Performance assessment of integrated care boards |
14Z59 |
NHS England and ICBs |
Wider NHS |
|
Section 76: Wider effect of decisions: licensing of health care providers |
|
NHS England and ICBs, NHS, FTs, NHS Ts |
Health care providers |
|
[Note: Unamended by the 2022 Act] |
Duty as to reducing inequalities: Section 2C |
Secretary of State |
Wider NHS |
Appendix 3: Acronyms used in this report
- AIS – Accessible Information Standard
- ALBs – Arm’s Length Bodies
- BME – Black and Minority Ethnic
- BAME – Black, Asian and Minority Ethnic
- BSL – British Sign Language
- CCG – Clinical Commissioning Groups (CCGs ceased to exist as separate legal entities on 1/7/22)
- CPO – Chief People Officer
- CQC – Care Quality Commission
- DAWN – Disability and Wellbeing Network
- DHSC – Department of Health and Social Care
- EDI – Equality, Diversity and Inclusion
- EHIA – Equality and Health Inequalities Impact Assessment
- EHIN – Equality and Health Inequalities Network
- EHRC – Equality and Human Rights Commission
- EO – Equality Objective
- ESR – Electronic staff record
- GEO – Government Equalities Office
- GP – General Practitioner (family doctor)
- HEE – Health Education England (HEE ceased to exist as a separate legal entity on 1/4/23)
- HIA – High Impact Action
- HR – Human Resources
- HRD – Human Resource Development
- ICS – Integrated care systems
- ICB – Integrated care board (ICBs became formal legal entities on 1/7/22)
- LDEP – Learning Disability Employment Programme
- LeDeR – Learning Disabilities Mortality Review
- LGB – Lesbian, Gay and Bisexual
- LGBT – Lesbian, Gay, Bisexual and Transgender
- LGBT+ – Lesbian, Gay, Bisexual and Transgender plus (LGBT+: LGBT stands for lesbian, gay, bisexual and transgender/transsexual people. However, it is recognised that those four letters do not necessarily include all those whose sexuality is not heterosexual, or whose gender identity is not based on a traditional gender binary (Council of Europe definition))
- NECS – North of England Commissioning Unit
- NHS – National Health Service
- NHS CAG – NHS Citizen Advisory Group
- NHSD – NHS Digital (NHS Digital ceased to exist as a separate legal entity on 1/2/23)
- NHS EDC – NHS Equality and Diversity Council
- NT – New Target
- OD – Organisational Development
- PET – Patient Equalities Team
- PSED – Public Sector Equality Duty
- RT – Revised Target
- SED – Specific Equality Duty
- SEND – Special Educational Needs and Disability
- SME – Subject Matter Expert
- SMI – Serious Mental Illness
- SOP – Standard Operating Procedure
- UISPC – Unified Information Standard for Protected Characteristics
- UISPC PSG – UISPC Publication Steering Group
- VCSE HWA – Voluntary Community and Social Enterprise Health and Wellbeing Alliance
- WDES – Workforce Disability Equality Standard
- WRES – Workforce Race Equality Standard
Publications reference: PRN00344
See also:

