1. Purpose and scope
1.1 This framework provides good practice principles and guidance for undertaking quality impact assessments (QIAs) as part of the decision-making process for planning, approving and implementing changes to health and care services or when commissioning new ones.
1.2 This framework updates the 2012 National Quality Board’s (NQB) how-to guide Quality Impact Assess Provider Cost Improvement Plans. The previous NQB guidance focused on using QIAs for cost improvement planning. This framework recognises the need for QIAs to be carried out in a wider range of circumstances when any service change is proposed, not just those focused on financial efficiencies.
1.3 QIAs ensure quality of care considerations, and not solely financial considerations, are central to decision-making for the design and delivery of health and care services. Quality care is defined in accordance with the NQB Shared Commitment that care is safe, effective, provides a personalised experience, is well led, sustainable and equitable (addresses inequalities).
1.4 This framework is intended for use by commissioners and providers of health and care services to support them develop organisational policy and processes for undertaking QIAs. This may include NHS providers, independent sector providers, integrated care board (ICBs) and local authorities.
2. Background
2.1 The 2025/26 NHS priorities and operational planning guidance asks ICBs to embed a robust quality and equality impact assessment (QEIA) process into financial and operational decision-making. The guidance also called for ICB boards and providers to produce quality impact assessments (QIAs), test all changes with boards and consider the appropriate involvement by public, service users, staff, local authorities and wider stakeholders.
2.2 The 2025/26 NHS priorities and operational planning guidance refers to QEIAs. QIAs are a contractual requirement and are recommended in the NHS Act 2006 (section 13NA as amended, known as the Triple Aim duty) to be undertaken when considering health and care service changes. Equality impact assessments (EIAs) enable organisations to show compliance with the requirements of the Equality Act (2010) and the Public Sector Equality Duties (PSED) general Equality Duty section 149.
2.3 Although QIAs and EIAs are closely linked, organisations can determine whether they combine them into a single QEIA process. This publication focuses on QIAs only.
2.4 This framework should be considered alongside other published guidance including:
- NQB National Guidance of Quality Risk Response and Escalation in Integrated Care Systems
- NQB Principles for Assessing and Managing Risks Across ICSs
- NHS 2025/26 priorities and operational planning guidance
- Allocations
- NHS Payment Scheme
3. When to use a quality impact assessment (QIA)
3.1 QIAs need to be carried out in a wide range of circumstances when any service change is proposed, not just those focused on financial efficiencies.
3.2 The QIA process includes considering which changes require stakeholder engagement and involvement, whether by consultation or otherwise, with the public, people using services, staff, local authorities and wider stakeholders.
3.3 QIAs are a tool to understand the likely impact of change and decision-making within organisations on the quality of care. Such changes can include:
- service redesign and major service change, including changes to eligibility criteria or access to services
- system prioritisation of services and pathway delivery
- commissioning and procurement of new services
- decommissioning of existing services or contracts
- temporary and urgent service changes, including during emergency preparedness, resilience and responses (EPRR)
- when piloting new ways of working as part of quality improvement
- organisational policy changes which may affect the staff, such as management of change processes or changes to workforce policies
- cost improvement plans (CIPs) or efficiency savings programmes, including the effect of cumulative CIPs within a service over time
- business case proposals and investments
- mergers and acquisitions
- changes in leadership models, such as shared executive leadership arrangements
- changes to workforce in response to pressures or the introduction of new roles
3.4 QIAs should be viewed a continuous, iterative process with documents remaining live and updated as circumstances change. Completion of QIAs tools and consideration of service change impact should be repeated at every stage of a proposal or project, not just at the start or end.
3.5 The frequency of reviewing and updating QIAs should be proportionate to the proposed change and the implementation timeframe, following a risk stratification approach.
3.6 QIAs should still be carried out in urgent situations, such as EPRR situations, although time pressures may mean an expedited process is followed to meet the key principles and to identify associated impacts and risks.
4. Key principles
4.1 The following key principles ensure a robust approach to undertaking QIAs:
- Board commitment and oversight ensuring any decisions made about service changes have an associated QIA.
- Collective oversight to consider the impact of changes more widely than at the individual provider.
- Multidisciplinary engagement, oversight and review, which includes input from clinical leaders and people using services.
- A dynamic process, which sets out an iterative approach to the completion and ongoing review of QIAs.
- A standardised tool that allows for the assessment of impact against the NQB’s definition of quality.
- An ability to monitor and review the impact captured in QIAs on decisions made.
5. Principle 1 – Board commitment and oversight
5.1 Ensure a shared understanding of the role and value of QIAs to support strategic commissioning, drive high-quality experience and outcomes, and support sustainable, value-led care (including reducing waste). Align QIA use with competency domains in the NHS leadership competency framework for board members to enable the setting of strategy and delivery of long-term transformation.
5.2 Organisations, including single providers, ensure that QIAs are completed for all changes processes as part of operational and financial decision-making.
5.3 Use QIAs as a mechanism to consider what changes require involvement, whether by consultation or otherwise, with the public, people using services, staff groups and local authorities.
5.4 Use QIAs to identify agreed arrangements for escalation and risk management and align to governance and risk management arrangements. Use cross-system governance arrangements, such as System Quality Groups, where collaboration at a system level is required.
5.5 Ensure high-quality data and insight intelligence underpins decision-making as set out in the Insightful board guidance.
6. Principle 2 – Collective oversight
6.1 All interested parties should work collaboratively to complete a QIA where there are multiple commissioners, providers and agencies involved (including NHS providers; independent providers; voluntary, community and social enterprise sector; primary care; ambulance trusts and local authorities).
6.2 A lead may be nominated to complete the QIA on behalf of all parties.
6.3 The RASCI tool (appendix A) can be used to clarify roles and responsibilities. This is particularly useful when proposed changes affect more than 1 system or a combination of systems, cross regional boundaries or that involve multiple health and care service providers.
6.4 Align efforts to improve quality. Quality concerns and identified risks affecting multiple ICBs should be managed in accordance with National Quality Board principles for assessing and managing risks across integrated care systems.
7. Principle 3 – Multidisciplinary engagement oversight and review
7.1 Ensure a multidisciplinary approach to engagement, oversight and review, through existing business change, programme office and transformation arrangements, or using a dedicated QIA panel to enable a fair and balanced review of the proposal’s impact on quality.
7.2 A multidisciplinary team approach allows both clinical and non-clinical input to review evidence of impact and decide if all likely impacts on quality have been identified and recognises the chief medical officer and chief nursing officer roles and responsibilities for quality.
7.3 Ensure stakeholder involvement has been included so evidence of impact is properly considered in oversight and review. A need for further stakeholder engagement may be identified as part of subsequent mitigations and action plans. Working in partnership with people and communities: statutory guidance supports effective partnership working to improve services.
7.4 Seek specialist advice and input where necessary. This should be aligned and proportionate to severity and proximity of impacts and associated identified risks.
7.5 Multidisciplinary team members may include:
- medical director or chief medical officer (CMO)
- nursing director or chief nursing officer (CNO)
- other relevant clinical and care professionals, such as, allied health professionals
- director of quality or governance (head of regulation)
- director of operations
- health inequalities lead
- quality improvement (or equivalent) team member
- experience of care lead
- finance lead
- commissioning lead
- project management office lead
- workforce lead
- performance lead
- patient safety lead
- sustainability lead
- medicines or prescribing lead
- strategic lived experience partner
- Mental Health Act team member
- infection prevention lead
- social care lead
- Freedom to Speak up Guardian
Organisational ownership, roles and responsibilities
7.6 The responsibility for completing a QIA and subsequent ownership of the risks and impacts should be clear within an organisation. Allocation of responsibility will depend on the proposed change and arrangements for commissioning and service delivery. The RASCI tool (appendix A) can be used to clarify roles and responsibilities. For examples of how this may work in practice, see appendix B.
8. Principle 4 – Dynamic quality impact assessment process
8.1 Use a clearly described dynamic QIA process and policy that sets out a transparent and iterative approach to the ongoing review and monitoring.
8.2 QIAs are reassessed and updated at every stage a proposal, not just at the start or end, as part of a continuous improvement approach supported by high quality data and intelligence.
8.3 Frequency of updates are proportionate to the proposed change, the implementation timeframe and informed by the severity of identified impacts and associated mitigation plans.
8.4 The stages within the QIA process will depend on the number and complexity of proposals, the speed at which decisions are required and if there is a dedicated team to support the QIA process. (An example QIA process is shown in appendix C).
8.5 Stages may include:
- identification of need – if a change or proposal will impact how a health and social care service or pathway is delivered or provided, a QIA is required
- completion of QIA documentation – the team leading the proposed change complete the QIA template and submit to multidisciplinary group for review
- triage – this step may be undertaken by nominated staff within an organisation to ensure the QIA template has been fully completed and if needed additional information is requested
- stage 1 (optional) – a nominated team apply screening criteria to QIA to determine level of sign off required
- some QIAs assessed as having a neutral impact on quality domains signed off under stage 1, and do not progress to a stage 2 assessment, depending on locally agreed arrangements
- screening criteria may include considering the level of identified risk (linked to the organisations risk appetite) if the proposal aligns to a national priority programme, the change increases the opportunity for risk within the care pathway or the QIA author has requested panel review due to high profile nature of change proposal
- stage 2 – QIA is reviewed by the multidisciplinary group to determine whether the impact of change has been accurately assessed
8.6 When deciding to use a multistage process, it is important to ensure that those who apply screening criteria are trained in and understand the purpose of undertaking a robust QIA process. Organisations should ensure that an expedited stage 1 process does not risk the rigour of the assessment.
9. Principle 5 – A standardised quality impact assessment tool
9.1 Include an evidence-based impact assessment in all QIAs, using the NQB Shared Commitment defined domains of quality (safe, effective, provides personalised experience of care, well led, sustainable and addresses inequalities).
9.2 Whenever possible, structure QIA tools to include a summary of the proposal, the assessment of impact on quality (and EIA if included), a summary of screening and assessment and an assessment review section (see appendix D for further detail).
9.3 Model QIA templates can be downloaded for use and adaptation by organisations.
Assessing the impact on quality
9.4 Undertake a comprehensive evidence-based assessment of the likely impact the proposed changes will have on quality of care and outcomes, assessed using NQB quality of care definition.
9.5 Classify impact on quality and outcomes as positive, neutral or negative. Negative impacts can be further risk scored, managed and reported on in line with the organisation’s risk management processes, if risk scoring is part of the organisation’s QIA process. See table 2 for example impacts by quality domains.
9.6 If risk scoring is used, set a risk threshold for escalation to the organisation’s quality committee (or equivalent) for further consideration and approval.
NQB principles for assessing and managing risks across integrated care systems outlines key principles to support assessments and discussions about risk in fast-changing, multi-factorial environments where system approaches are required.
Example impacts on quality domains
Safe
- Positive – improves patient flow through emergency department.
- Negative – leads to increased likelihood of avoidable readmissions.
Effective
- Positive – implementation of latest best practice guidance or standards.
- Negative – patients less likely to receive treatment within recommended timeframe.
Provides a personalised experience
- Positive – increases opportunity for patient choice in the care pathway.
- Negative – reduces the ability for care to be provided closer to home.
Well-led
- Positive – supports improved staff wellbeing.
- Negative – permanent recruitment and retention will be reduced and service will rely on bank or agency staff.
Sustainable
- Positive – reduces the environmental impact associated with maintaining and heating the existing older estate.
- Negative – leads to increased costs to deliver service over time.
Addresses inequalities
- Positive – move to a new site increases accessibility for those with a physical disability.
- Negative – predominantly digital ways of accessing the service increases risk of digital exclusion.
9.8 QIAs should also be used to consider the impact of proposals on additional areas of operational planning, such as:
- workforce – staff and volunteers health and wellbeing, workforce and education training needs, including provision of workforce training placements linked to service delivery, and the impacts on recruitment and retention of staff.
- performance – the impact on the services ability to meet national and local performance metrics and standards
- strategic objectives – assessment of the impact against the organisation’s key strategic objectives
Evidencing impact on quality
9.9 There should be clear evidence that quantitative and qualitative data and intelligence has been reviewed, triangulated and included within the relevant QIA. Data and intelligence is crucial to demonstrate the impact of the proposals and determine if mitigations are appropriate.
9.10 Sources of data and intelligence can include locally and nationally reported quality and performance data (including professional clinical insight). Sources of data and useful products include: Model health system, Insightful board series, outcomes frameworks, specialised services quality dashboards (SSQD), quality frameworks, patient safety intelligence (including incident reporting data) and patient safety incident response plans, national and local survey data, complaints data, compliments, Patient Advice and Liaison Service (PALs), Friends and Family Test (FFT), insights from focus groups, reports from HealthWatch.
9.11 Data gaps that prevent impact from being evidenced should be highlighted, with an action plan to address them.
Mitigations and key performance indicators (KPIs)
9.12 Actionable mitigations should be identified and documented for every identified negative impact. Mitigations should use SMART methodology (specific, measurable, actionable, realistic and time-bound) and include named leads and clear deadlines, with linked key performance indicators (KPIs) that can be reliably used to demonstrate achievement.
Training and support
9.13 Organisations should ensure staff completing and contributing to QIAs receive training on the process and purpose of these assessments.
9.14 Organisations may consider publishing local FAQs and how-to guides for staff and provide opportunities to access advice and guidance when completing QIAs. This could take the form of a quality buddy being assigned to a proposal lead to support QIA completion.
Principle 6 – Monitoring and reviewing the impact of quality impact assessments
10.1 Keep records of approved QIAs, and a log of associated risks and mitigations, in line with the organisations governance and risk management processes.
10.2 Report outcomes from approved QIAs to internal quality committees or groups who provide quality oversight and decision-making on behalf of the organisation’s board.
10.3 Publicly publish completed QIAs to enable openness, transparency and further learning.
10.4 Produce regular reports to monitor progress (quarterly or 6 monthly), allowing QIAs mitigations and actions to be reported to the relevant multidisciplinary team groups where decisions are taken.
10.5 Ideally, review and update QIAs every 6 months for large scale changes and at least at project initiation, mid-point and close-down or implementation.
10.6 Organisations should review the impact of completed QIA as part of monitoring and reporting arrangements. This will help support QIA use by highlighting best practice.
10.7 As part of the review and monitoring arrangements, organisations should also ensure a longer-term process for escalation and raising concerns is in place following the change project implementation. This should make use of existing governance structures and risk management arrangements.
Appendix A: Template for RASCI
Introduction
The downloadable template is to be used when undertaking a RASCI assessment to clarify roles and responsibilities in the delivery of quality care.
RASCI stands for: Responsible, Accountable, Support, Consulted, Informed.
The template can be used flexibly. It could be used to support care delivery to individuals, or across a team, service, organisation or pathway.
How to use the RASCI tool
Those using the RASCI tool should take the following steps:
- Undertake an initial diagnostic to understand what the issues are.
- Agree which people and stakeholders need to be involved.
- Agree key tasks and functions.
- Collectively discuss and agree roles and responsibilities.
- Agree any actions and mitigations.
- Continue to monitor and review progress, re-doing the RASCI as required.
Those using RASCI should also draw on good practice, as set out in the tool, including:
- focusing first-and-foremost on people using services and staff
- using the tool as a communication tool, to gather views and agree responsibilities across all key stakeholders
- ensuring that any actions and mitigations informed by using the RASCI are SMART (specific, measurable, actionable, realistic and time-bound)
The RASCI assessment tool can be accessed and downloaded from the NHS England website.
Appendix B: Example roles and responsibilities for quality impact assessment completion and oversight
Example 1
System commissions service or pathway and is leading the change proposal, for example, a new procurement or decommissioning of existing service.
Who leads QIA process?
ICB as lead commissioner, working in collaboration with any providers who are already delivering the services.
Who completes QIA documentation?
ICB staff who are involved in making decisions about the design, delivery and quality assurance of the services (such as, ICB patient safety specialist, director of quality).
This may include contracting and commissioning team members, service transformation team members, associated clinical leads and experience of care lead.
Who oversees and monitors QIA process?
ICB staff working within a business change or transformation team support the completion and monitoring of QIA.
Who signs off QIA?
Project management, business change or transformation team or dedicated QIA panel.
ICB board members have final responsibility for decisions which impact on services for their local population and should ensure that QIAs have been effectively completed and considered as part of that decision-making process.
Example 2
Provider proposing service change or making changes relating to the internal organisation of the service or pathway they deliver.
Who leads QIA process?
Provider, involving internal clinical or care delivery teams, directorates and working in collaboration with the commissioner of service or pathway.
Who completes QIA documentation?
Staff within provider organisations, such as service leads, directorate managers, care group leads, patient safety leads, experience of care leads, transformation and improvement leads.
Who oversees and monitors QIA process?
Clinical quality and governance teams or PMO support the completion and monitoring of QIA and facilitate the management of the QIA panel or equivalent.
Who signs off QIA?
Business change panel, project management office or dedicated QIA panel.
The final decision-making on proposed changes progression sits with the providers internal governance arrangements, for example, the provider quality committee or board.
Appendix C: Example quality impact assessment process diagram
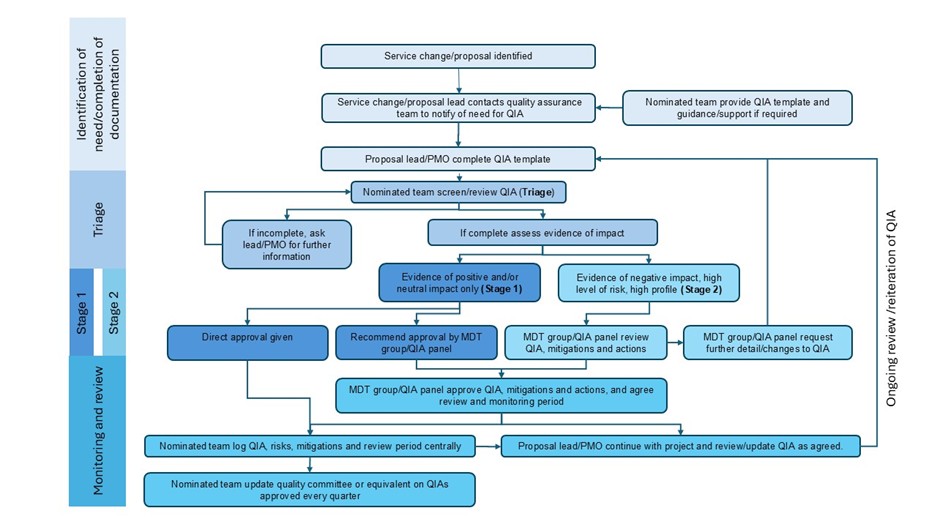
Flowchart shows the quality impact assessment (QIA) process for service changes.
It starts with identifying a proposal, completing a QIA template and a nominated team then completing a triage review.
Based on impact evidence, proposals follow either a Stage 1 (low risk) or Stage 2 (high risk) approval path.
Approved QIAs are logged, risks monitored and updates reported quarterly. The process includes ongoing review and updates.
Appendix D: Key sections and content to include in quality impact assessment tools
Proposal summary
This should include:
- contact details of leads
- version control information and date
- outline of service areas affected
- any identified stakeholders
- funding requirements
- engagement work planned or completed
Completed by:
- either or both the project lead or directorate project management office
Assessment of impact on quality
An evidence-based assessment of the proposed change against the NQB definition of care quality (safe, effective, experience, well led, sustainable, inequalities). This should include:
- whether a positive, neutral or negative impact is expected for each domain
- a clear description of the impact
- identified evidence to support that assessment
- risk score assigned (if impact is risk assessed)
- clearly described mitigations and balancing measures
- KPIs (which will demonstrate achievement) and monitoring plan
- expected revised risk score once mitigations are actioned (if impact is risk assessed)
Completed by:
- either or both the project lead and directorate project management office
- clinical service lead
- lived experience partner
- quality representatives (patient safety, experience, outcomes)
Assessment of impact of equality duties
If the QIA and EIA have been combined into a QEIA, it will also include an impact assessment on the 9 protected characteristics.
Completed by:
- either or both the project lead and directorate project management office
- clinical service lead
- lived experience partner
- health inequalities lead
Summary of assessment and screening tool
Once the impact of the proposal on the quality domains of quality has been assessed, it is helpful for an impact summary, initial assessment and revised assessment to be noted alongside whether there are any gaps in evidence.
A summary of this information is helpful if a screening or triage step has been built into the QIA process.
Summary completed by:
- either or both the project lead and directorate project management office
Screening completed by:
- nominated team
Assessment review
Once a QIA has been completed and triaged it will be reviewed to determine:
- whether the mitigations and KPIs are appropriate
- if further information and evidence is required
- whether the proposal QIA is approved
- whether the proposed change should be amended to reduce an expected negative impact on the quality of care
- whether they recommend the proposal should be allowed to proceed
If stage 1, completed by:
- nominated team, such as quality assurance team, or equivalent
If stage 2, completed by:
- multidisciplinary team group, project management office, business change or transformation team, or dedicated QIA panel
Publication reference: PRN01920_i

