Classification: Official
Publication reference: PR1329
Published 1 November 2022, Version 1
Glossary
|
Term |
Definition |
|
Early menopause |
Menopause happening between the ages of 40 and up to 45. |
|
Menopause |
Menopause is when periods stop due to lower hormone levels. This usually happens between the ages of 45 and 55 but for some it can be earlier or later. Family history, surgery and medical conditions can affect the age menopause occurs. Menopause is reached when there has not been a period for 12 consecutive months. |
|
Perimenopause |
The time leading up to menopause when ovulation cycles and periods can be irregular, continuing until 12 months after the final period. Perimenopause usually begins during the mid-40s, although it can start earlier and extends until 12 months after the final period. |
|
Post menopause |
This is the time after menopause (12 consecutive months without a period). Symptoms of menopause may continue and may require ongoing support. |
|
Premature menopause |
When menopause occurs under the age of 40, it is termed premature menopause or premature ovarian insufficiency (POI). |
|
Menopause transition |
Refers to the stages: perimenopause, menopause and post-menopause |
Menopause – NHS (www.nhs.uk)
Menopause (who.int)
22-Menopause-factsheet.pdf (selfcareforum.org)
Introduction: why this matters
The NHS employs over 1.3 million people and around 1 million of these people are women. This is over 75% of the entire workforce. Women between the ages of 45 and 54 alone make up a fifth of all NHS employees, and so up to a fifth of our workforce could be experiencing menopausal symptoms.
Six out of every 10 women experiencing menopausal symptoms say it has a negative impact on their work. With the right support, women do not need to press pause, struggle through, or leave their careers during this natural transition. Many women will continue to suffer in silence unless we break the taboo and start talking openly about the menopause at work.
Good menopause care has both direct and indirect impacts on workforce retention, productivity, presenteeism and absenteeism. Ensuring staff get the support they need is an important part of retaining experienced talent and skills. The right support would also reduce the impact of a person’s symptoms on their health and wellbeing, their effectiveness at work personal life and relationships.
Looking after our NHS people and supporting them is a critical priority. We need to ensure the NHS is the best possible place to work where its people can fulfil their potential. The NHS Menopause Improvement Programme is a key pillar of this work, supporting delivery of our NHS People Promise. This work will also align with the first Women’s Health Strategy for England, which the Government has launched.
As part of our commitment to supporting colleagues going through the menopause, NHS England recently signed the Wellbeing of Women Menopause pledge.
What is the purpose of this guidance?
This guidance helps NHS organisations, line managers, and those working in the NHS understand more about the menopause, how they can support colleagues at work and those experiencing menopause symptoms.
It includes advice on HR aspects such as how to record menopause-related absence, as well as practical tips for line managers on the benefits of having regular health and wellbeing conversations with their teams, and it supports them to consider any reasonable adjustments they may want to implement to support colleagues who are experiencing menopause symptoms.
This guidance has been developed in collaboration with a number of task and finish groups including external members such as NHS Employers and the Chartered Institute of Personnel and Development, as well as colleagues from relevant teams within NHS England.
We will review this guidance regularly to ensure the advice is continuously updated and in line with evidence-based practice. If you have any questions or comments about this guidance, please email england.lookingafterourpeople@nhs.net.
We know that many NHS organisations are already working hard to support colleagues experiencing menopause in work, so this guidance will serve to enhance your efforts. However, we would encourage all our NHS people to read this guidance to ensure:
- they have a better understanding of what menopause is
- they have key information on how to support people to have open and receptive conversations
- they are much better equipped to support staff managing the effects of the menopause transition at work.
Organisations may choose to develop a specific guidance or policy to support their colleagues and/or they may wish to use this guidance as a support tool to inform their current policies and procedures.
Case study: East Midlands Ambulance Service
Created menopause guidance for employees and line managers to support staff who are experiencing issues, creating an environment where staff feel confident to raise concerns, instigate conversations and ask for reasonable adjustments in the workplace.
Case study: Nottingham University Hospitals NHS Trust
Developed a staff menopause policy, have menopause advocates, and have hosted a range of wellbeing sessions centred on the menopause, such as mindfulness, pelvic health and eating well so that staff receive a holistic approach to the topic. This work was recognised on a national level as it was nominated for a Healthcare People Management Association award for partnership work with unions.
How can menopause symptoms impact work?
The body can be affected by menopause in numerous ways, causing a myriad of symptoms The duration and severity of these symptoms varies across individuals, with some likely to experience severe and/or bothersome symptoms. The impact of these symptoms on self-confidence, mental health, and relationships with others, will clearly have an impact not only on their life outside work but also their working life. It is therefore important for managers and colleagues to be aware of these symptoms so that they can appreciate the full extent of how some workers experience the menopause and its impact on work.
Symptoms usually start a few months or years before periods stop (perimenopause) and can continue for some time afterwards. Symptoms of the perimenopause and menopause are wide ranging and can impact women both physically and psychologically.
Some of the common symptoms include the following:
- change in periods – irregular periods, lighter or heavier periods
- headaches and migraines that are worse than usual
- muscle aches and joint pains
- hot flushes – short, sudden feelings of heat or cold, usually in the face, neck and chest
- night sweats
- mood changes/ swings
- difficulty sleeping which makes people feel tired and irritable during the day
- anxiety
- problems with memory or concentration (often referred to as ‘brain fog’).
Find out more about menopause symptoms on the NHS website.
Women’s experience at work
The law and menopause
While menopause is not a specific protected characteristic under the Equality Act 2010, in accordance with the Advisory, Conciliation and Arbitration Service (ACAS), “if an employee is disadvantaged and treated less favourably in any way because of their menopause symptoms this could be viewed as discrimination if related to a protected characteristic, for example, age, disability, gender reassignment or sex”.
The following legislation is key to note:
- Equality Act 2010: legally protects people from discrimination in the workplace and in wider society.
- Health and safety at Work Act 1974: which states, “An employer must, where reasonably practical, ensure everyone’s health, safety and welfare at work”.
Further information regarding menopause and the law can be found on the ACAS website: Menopause and the law: Menopause at work.
Transgender, non-binary and intersex staff and the menopause
The NHS recognises and values its diversity and trans inclusive culture. We are aware people of diverse gender expressions and identities experience menopause, and it is therefore not just an issue for female colleagues.
Transgender, non-binary and intersex staff may experience the menopause, either due to age-related hormonal changes or hormone treatments and surgeries. It is important to acknowledge some trans, non-binary and intersex staff may not wish to disclose their menopausal symptoms as this may mean disclosing their trans or intersex status. It can therefore be particularly difficult for these employees to access support and/or ask for adjustments. Within each of these groups, people’s needs will be different and so it is crucial to listen to people on an individual basis and allow them to take the lead on their conversations and required adjustments.
Guidance on menopause and the workplace makes specific reference to trans people and is a useful reference to help understand the impact of menopause in different communities. Appendix 3 also provides more information to consider on this topic.
Supporting line managers and colleagues experiencing menopause
Menopause can have indirect effects on other people such as spouses, significant others and close family members or friends of individuals going through the menopause, which can put additional pressures and changes on relationships. As an employer, it is therefore important to foster an open and inclusive culture where colleagues experiencing symptoms of the menopause feel they can talk openly about their experiences and receive or be signposted to the support they need.
Line managers and leaders: If you are supporting someone who is experiencing symptoms of the menopause, we would encourage you to:
- Normalise asking for help and reassure colleagues that it is ok to ask for help even when their symptoms are not too bad.
- Increase your own and your team’s knowledge and awareness about the menopause: Menopause – NHS.
- Link in with local occupational health and wellbeing services and employee assistance programmes (where available) to understand how they can support you and your colleagues.
- Share details of the wellbeing support available to colleagues, including local NHS services and the national support offer.
- Encourage attendance at organisational menopause support groups and peer networks (where available) to meet others who are experiencing similar symptoms.
- Link with organisational health and wellbeing champions to hear about any local support being offered to staff affected by the menopause. Find details here about support for colleagues affected by the menopause.
- Access free training to learn how to have safe and effective wellbeing conversations and offer regular health and wellbeing conversations to check in and see how colleagues are feeling. Here is a link to the national wellbeing conversations offer.
- Use these health and wellbeing conversations to discuss whether it would be helpful to consider any reasonable adjustments to their working pattern: for example, asking if working flexibly would support them in the workplace.
- Consider flexible working as one of the measures to help colleagues cope with symptoms.
- Read the guidance produced by the NHS Staff Council’s Health, Safety and Wellbeing Partnership Group to consider best practice in supporting colleagues experiencing menopause, as well as the guidance published by CIPD aimed at managers and employers.
Case study: Belfast Health and Social Care Trust
Created an information leaflet for staff which directly links into its overall health and wellbeing strategy and improving working lives policies. Its Let’s Talk Menopause page provides useful links and toolkits. The trust has also created videos to further support staff and managers with the menopause in the workplace. Take a look at the guide for managers video and the guide for employees video.
How should I record menopause-related absences?
By recording menopause-related absences accurately, organisations can gain a better understanding of the impact menopause is having on their colleagues and put in place the necessary support.
There is now guidance available on recording menopause-related absence. The guidance includes step-by-step instructions on how to record menopause-related absence.
For organisations that do not use electronic staff records (ESR), including the primary care sector, a more bespoke approach is required, and you will need to determine how you capture this information. It is recommended that each practice includes the recording of menopause-related absence when reviewing practice-based sickness levels.
Case study: Sherwood Forest Hospital NHS Foundation Trust
Senior nurses at the trust recognised that the wisdom and expertise of older nurses and other healthcare workers could be retained and put to best use by providing a structured and supportive working environment that champions their wellbeing and counteracts age-related issues such as menopause. Over 12 months, the organisation carried out a research intervention study which included expertise from menopause clinical colleagues to develop action plans to educate line managers, to raise awareness and understanding of the effects of menopause at work, to destigmatise the taboo associated with talking openly about menopause and to train managers to make reasonable adjustments for those struggling with menopausal symptoms. This led to improved clinical assessments and referrals for staff and a change in organisational culture around the menopause.
Employee experience: menopause champions
“Having a menopause or wellbeing champion at work could help people affected by the menopause. The champion could be a point of contact if staff need advice, or someone to initially talk to if they are not comfortable talking to their managers.” (TUC ToolKit – All employee experience examples.)
How can your organisation be menopause friendly?
The following checklist provides guidance for employers to promote menopause awareness and ensure staff get the support they need.
Is there a menopause guidance document or policy in place?
- Is it clear from this document how the organisation supports those affected by the menopause?
- Is it accessible, regularly shared and reviewed?
Is there an open and receptive culture around the menopause?
- Can menopause be talked about openly?
- Are there opportunities/forums for shared stories/experiences?
- Are there menopause events in your organisation?
Is the right menopause training and support available?
- Employee training?
- Line manager training?
- Human resource director and occupational health training?
Is other support available?
- Is occupational health support available and accessible?
- Is there an employee assistance programme? (Does it include menopause?)
Is menopause-friendly uniform/workwear available?
- Are uniforms in suitable, breathable fabrics?
- Are there extra uniforms/garments available if needed?
- Can uniforms/garments be adapted (eg for layering of clothes if needed)?
Are workplace facilities menopause-friendly?
- Can workplace temperatures be adjusted or is there access to desk fans for employees who need them?
- Is there access to cold water, washrooms and toilets?
- Can people have access to restrooms for breaks/is there a breakout space available if they are patient/customer-facing?
Adapted from: menopauseintheworkplace.co.uk.
Menopause support and services available to NHS colleagues
The NHS has a range of support offers and services available to colleagues to support their overall health and wellbeing, which includes:
National Menopause Programme
- Here are the National Menopause Programme support offers:
- Access to a range of health and wellbeing offers through the national health and wellbeing support programme, including free access to health and wellbeing apps and coaching and counselling offers. The range on offer is available to all and in particular colleagues are encouraged to sign up to the Unmind app to access their two dedicated series on menopause – Menopause 101 and Let’s talk Menopause.
- Many colleagues working across the NHS will also have access to occupational health and wellbeing services and local employee assistance programmes (EAPs) through their employing organisations. It is likely that referral into occupational health and wellbeing services will need to be via a line manager, but access to EAPs is often direct.
(The delivery of occupational health and wellbeing services and local EAP services will vary for those working within primary care, and line managers and leaders within primary care are encouraged to check with their local integrated care board or primary care network clinical director to understand what is available.)
Workplace union representatives can also provide support to their members who are experiencing difficulties and signpost to union guidance and advice.
A helpful webinar from NHS Employers focusing on how to support colleagues with menopause in the workplace can be found on NHS Employers website.
Useful links
NHS links
- The NHS ESR team has worked with NHS England to develop a guide on recording menopause related sickness. The guidance includes step-by-step instructions on how to record menopause-related absence to help HR colleagues and ESR users.
- The NHS menopause webpages includes advice on symptoms and treatment.
- Supporting our NHS People – Helping colleagues look after their own health and wellbeing while looking after others.
- As set out in the NHS People Plan, we want all of our NHS people to have the chance to work flexibly, regardless of role, grade, reason or circumstance. It also reinforced the importance of looking after our own health and wellbeing. We know that for those colleagues going through the menopause, flexible working is one of the measures that can help them to cope with symptoms.
- National Retention Programme: Improving staff retention: a guide for line managers and Nursing and midwifery retention self-assessment tool are also useful resources for colleagues and managers.
- NHS Employers includes information on how menopause can affect people at work and provides practical guidance for employers on how to improve workplace environments.
- The NHS Staff Council’s Health, Safety and Wellbeing Partnership Group has developed this guidance to support NHS organisations to improve the way they address menopause and work. This is complemented by principles for line managers and staff.
Other links
- The Chartered Institute of Personnel and Development (CIPD) has published helpful people manager resource.
- The Faculty of Occupational Medicine has produced guidance on menopause and the workplace, and an accompanying infographic offering advice, tips and stats.
- ACAS has published support documents for organisations on the menopause at work.
- British Menopause Society educates, guides, and informs healthcare professionals on all aspects of the menopause.
- The government’s vision for the Women’s Health Strategy informed by the call for evidence.
Appendix 1a: Checklist for managers
Appendix 1a Checklist for managers is available as a word document.
Appendix 1b: Wellbeing action plan
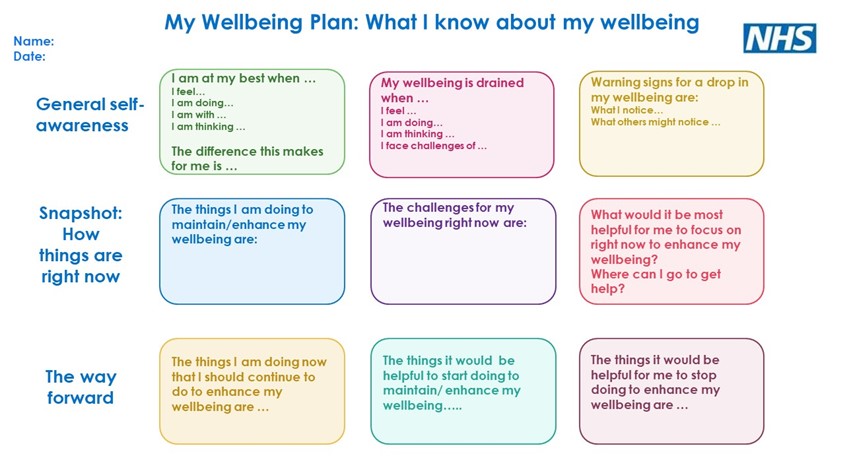
Appendix 1b Wellbeing action plan is available as a word document.
Appendix 2: Resources
- NHS Website – Menopause
- Menopause self-care factsheet
- Health and wellbeing hub for lifestyle and other wellbeing considerations
- British Menopause Society
- Women’s Health Concern
- Daisy Network – Charity for those with Premature Ovarian Insufficiency POI
- Rock My Menopause primary care women’s health forum
- https://www.queermenopause.com/ – particularly for people in the LGBTQIA+ community
Appendix 3 – Menopause in transgender, non-binary, and intersex colleagues
Trans women (women who were assigned male at birth) undertaking hormone therapy are likely to take this for life. They may experience menopausal-like symptoms, especially if their hormone therapy is interrupted or unstable.
Trans men (men who were assigned female at birth) will experience an age-related menopause process if they do not undertake hormone therapy and retain their ovaries. If trans men have their ovaries and uterus removed, they may experience a premature menopause. These symptoms are also affected by hormone therapies – for example, taking testosterone. This is important to remember as trans men may more commonly experience the menopause at an earlier age, which can add another barrier to seeking care and adjustment.
Non-binary people may also experience menopause, and these experiences will depend on a variety of factors including their sex assigned at birth and their medical treatments. While it is not appropriate to ask about these things, it is important to be aware of them and allow space for the individual to take the lead on the support and adjustments they may require.
Intersex people may also experience menopause, depending on a variety of factors including their sex assigned at birth and their medical treatments. While it is not appropriate to ask about these things, it is important to be aware of them and allow space for the individual to take the lead on the support and adjustments they may require.
Menopausal symptoms will be related to the individual’s age and the time in their life that they have undergone transition-related treatments. The menopause may also induce dysphoria for trans individuals (dysphoria is when a person experiences discomfort or distress because there is a mismatch between their sex assigned at birth and their gender. This may be so intense it can lead to depression and anxiety and have a harmful impact on daily life). This should be considered when talking to trans and non-binary people about the menopause. If a trans, non-binary or intersex person does disclose their menopausal symptoms and their trans or intersex status, it is important that this information is not passed on to others without their consent. For trans people who have a gender recognition certificate it is illegal to disclose their trans status without consent.
The menopause in the workplace: A toolkit for trade unionists, Wales TUC Cymru
Gender dysphoria
Appendix 4: Understanding people and data
Understanding workforce data should be at the centre of an effective strategy to support our workforce. Collecting and analysing data and identifying trends allows trusts and systems to determine the impact of any menopause support programme initiated. It is important to understand the profile of your workforce affected by menopause and assess and address any issues affecting particular groups. You may want to consider who in your trust or system you will need to work with to better understand your data.
Some options to consider would be:
- ensure that menopause-related sickness ESR reporting takes place within the organisation
- encourage and support attendance at menopause support sessions
- identify how many staff of perimenopause/menopausal age are taking up flexible working options
- evaluate your leaver data and identify how many staff of perimenopause/menopause age are leaving your organisation
- analyse and act on feedback from your employee assistance programme services if available
- analyse and act upon feedback from wellbeing/menopause champions in your organisation and employee surveys/polls.
To support the above activities, some of the data you may want to review includes:
Internal data sources:
- locally designed surveys
- workforce information from ESR
- staff turnover and stability rates
- exit surveys and exit interviews
- conversations with existing staff.
External data sources:
- NHS Staff Survey.
Research shows that the morale and engagement theme scores from the NHS Staff Survey have a strong correlation and statistical significance with retention. You can also use specific questions within the NHS Staff Survey to understand staff feedback on whether people are thinking of leaving and various elements of the People Promise, such as flexible working or health and wellbeing support.
The National Quarterly Pulse Survey
NHS People Pulse
National Quarterly Pulse Survey (NQPS)
The Model Health System
Retention compartment and data from national organisations such as NHS Digital can all provide useful insights into retention and related indicators of staff experience by age and gender.
For further information please visit NHS England » Understanding your data.
If you have any questions or comments about this guidance, please send an email to england.lookingafterourpeople@nhs.net.

