This updated statutory guidance is issued in accordance with s12ZB(4) of the National Health Service Act 2006. In accordance with s12ZB(5) of that Act, NHS England, integrated care boards (ICBs), NHS trusts, NHS foundation trusts, local authorities and combined authorities (relevant authorities and each one a relevant authority) must have regard to this guidance when arranging services in scope of the Provider Selection Regime (PSR), as set out in the Health Care Services (Provider Selection Regime) Regulations 2023 (the Regulations), which came into force on 1 January 2024. Where a relevant authority departs from this guidance it should be able to explain the reasons for doing so and keep appropriate records of its decision-making to do so.
This guidance replaces the PSR statutory guidance that NHS England issued on 18 October 2023. The changes are:
- in response to feedback, redrafted throughout for easier comprehension and navigation
- in particular, the guidance on the most suitable provider process now better explains how it is distinct from the competitive process, in accordance with the Regulations
- amendments arising from the Procurement Act 2023 coming into force on 24 February 2025; in addition to replacing references to the Public Contracts Regulations 2015, the guidance explains how the PSR will draw on the provisions of the Procurement Act relating to the exclusion and debarment of providers
None of these updates represents a major change in policy and none is expected to disrupt processes underway.
Summary
The Health Care Services (Provider Selection Regime) Regulations 2023 were made under s12ZB of the National Health Service Act 2006 (the 2006 Act), replacing The National Health Service (Procurement, Patient Choice and Competition) (No 2) Regulations 2013 (the PPCCR) and removing healthcare services from the scope of the Public Contracts Regulations 2015 (the PCR). On 24 February 2025 the PCR were repealed by the Procurement Act 2023 (the Procurement Act), and Regulation 20 of the PSR was updated to reflect exclusion criteria and reporting of exclusions that align with the Procurement Act.
From 1 January 2024, relevant authorities, namely NHS England, ICBs, NHS trusts, NHS foundation trusts, local authorities and combined authorities have been required to follow the PSR when contracting for healthcare services that are in scope of the PSR.
Actions that relevant authorities must take
The regulations require that, when arranging healthcare services, relevant authorities adhere to the procurement principles and identify which 1 of 5 selection processes to follow:
- direct award processes A – must be used where there is an existing provider for the service and that provider is the only one capable of providing the service
- direct award process B – must be used where there is unrestricted patient choice of provider for a service
- direct award process C – can be used where an existing provider is satisfying its contract and the new contract will not be materially different from the current contract
- most suitable provider process – can be used where the relevant authority cannot or does not wish to use direct award process C but is of the view that it can identify the most suitable provider
- competitive process – can be used where the relevant authority cannot or does not wish to use direct award process C or the most suitable provider process
There are also specific provisions dealing with: modifications of existing contracts; frameworks and contracts awarded under them; and urgent awards or modifications.
Relevant authorities must consider 5 key criteria when following direct award process C, the most suitable provider process or the competitive process.
The flexibility in decision-making processes given to relevant authorities under the PSR is balanced by mandatory transparency requirements. These requirements on relevant authorities enable them to be scrutinised and held to account for their decisions. They include:
- for all PSR processes – keeping records of their decisions and publishing transparency notices confirming these decisions
- when following the most suitable provider process or the competitive process, publishing transparency notices making their intentions to use these processes clear in advance
- when following direct award process C, the most suitable provider process or the competitive process: keeping records of their decisions on the relative importance of each of the key criteria and providers that were assessed against them; observing a standstill period during which representations can be made; and responding to any representations received before confirming their decision and awarding a contract to the selected provider
Relevant authorities are expected to develop and maintain sufficiently detailed knowledge of the provider landscape. This will help them to put in place services that best meet the needs of their population and to select the appropriate award process. Relevant authorities are expected to develop and maintain sufficiently detailed knowledge of the provider landscape. This will help them to put in place services that best meet the needs of their population and to select the appropriate award process.
Relevant authorities must publish an annual summary of the procurements they have arranged under the PSR. They must monitor their compliance with the Regulations and publish annually the results from this (this may be integrated into other annual reporting requirements, as appropriate), including processes, decisions made under the PSR, contract modifications, and declaration and management of conflicts of interests.
If the relevant authority finds instance(s) of non-compliance, it must put in place actions to address the issue and to improve adherence with the regime.
Using this guidance
This guidance is published under s12ZB of the 2006 Act, which requires NHS England to publish guidance on compliance with the requirements imposed by the Regulations.
In this guidance ‘healthcare services’ means ‘relevant healthcare services’ in scope of the Regulations, and the ‘arranging of healthcare services’ refers to when a relevant authority procures relevant healthcare services under the PSR.
It sets out the scope of the PSR and how relevant authorities must follow the PSR and must be followed by relevant authorities. It also details the scope of the PSR and how to meet requirements for considering the key criteria, complying with transparency requirements and managing conflicts of interest.
Relevant authorities must apply the Regulations, must have regard to this guidance and are expected to read this guidance alongside its annexes. The annexes detail the application of the PSR and the transitional arrangements in place now that the PSR is in force. Organisations may use the toolkit that accompanies this guidance in arranging the provision of healthcare services.
When exercising their functions so as to comply with the PSR, relevant authorities must continue to comply with their other legal obligations where applicable, for example under the:
- National Health Service Act 2006
- Local Government and Public Involvement in Health Act 2007
- Equality Act 2010
- Modern Slavery Act 2015
- Local Authorities (Executive Arrangements) (Meetings and Access to Information) (England) Regulations 2012
- Subsidy Control Act 2022
- Transfer of Undertakings (Protection of Employment) Regulations 2006.
This guidance does not specify how to comply with these other legal obligations.
Relevant authorities are advised to also be aware of other requirements and duties not set out in legislation. For example, NHS England, ICBs, NHS trusts and NHS foundation trusts are expected to adhere to NHS England’s net zero emissions requirements, the application of net zero and NHS social value and the carbon reduction plan requirements in the procurement of NHS goods and services.
A reference in this guidance to legislation or a legislative provision is a reference to it as amended, extended or re-enacted from time to time.
Introduction
The Health and Care Act 2022 (the 2022 Act) amended the 2006 Act and sets an expectation that all those involved in planning, purchasing and delivering health and care services work together to agree and address shared objectives, and makes it easier for them to do so. As part of these legislative changes, under s12ZB of the 2006 Act, the Health Care Services (Provider Selection Regime) Regulations 2023 (the Regulations) introduced a new regime for arranging healthcare services for the NHS and local authorities – the Provider Selection Regime (the PSR or the regime).
The Regulations replaced the National Health Service (Procurement, Patient Choice and Competition) (No 2) Regulations 2013 (the PPCCR) and removed procurement of healthcare services, when procured by relevant authorities under the PSR, from the scope of the Public Contracts Regulations 2015 (the PCR) and now of the Procurement Act 2023. Engagement with the healthcare system on the design of the PSR identified that the PCR and PPCCR could create barriers to integrating care, as their focus on competition made development of stable collaborations and new models of care harder and at times resulted in complex procurement processes.
The PSR provides:
- a flexible and proportionate process for selecting providers of healthcare services so that all decisions can be made with a view to securing the needs of the people who use the services, improving the quality of the services and improving the efficiency of service provision
- the capability for greater integration and collaboration across the system, while ensuring that all decisions about how healthcare is arranged are made transparently
- opportunities to reduce bureaucracy and cost associated with the previous rules
These benefits can be realised through the selection and administration of the appropriate PSR process. Where there is an existing provider and the contract has come to an end, the regime allows for new contracts to be awarded through direct award processes A, B or C in specific circumstances. Where the service is changing considerably or a new provider for it is sought, the regime offers the most suitable provider process and the full competitive process.
Scope of the PSR
The scope of the PSR is set out in Regulation 3(1).
Relevant authorities are defined in s12ZB(7) of the 2006 Act.
The health service is defined in s275(1) of the 2006 Act.
Healthcare services are defined in s150(1) of the Health and Social Care Act 2012. The common procurement vocabulary (CPV) codes for use under the PSR are defined in Schedule 1.
Relevant authorities
This guidance applies to the following relevant authorities in England, which under s12ZB of the 2006 Act are required to comply with the Regulations:
- NHS England
- integrated care boards (ICBs)
- NHS trusts and foundation trusts
- local authorities or combined authorities
These relevant authorities must follow the PSR for arranging healthcare services, even when contracting with another relevant authority. Other authorities, including the Secretary of State for Health and Social Care or executive agencies of the Department of Health and Social Care (DHSC), such as the UK Health Security Agency (UKHSA), must not use the PSR to arrange healthcare services directly, but may commission relevant authorities that must follow the PSR when acting on their behalf to arrange or provide healthcare services. Wholly owned subsidiaries of relevant authorities cannot use the PSR but may provide administrative support to a relevant authority awarding a contract.
Procurements in scope of the PSR
A service is in scope when a relevant authority is commissioning or subcontracting a service that:
- is provided as part of the health service, whether NHS or public health
- consists of the provision of healthcare to individuals or groups of individuals; and
- falls within one or more of the specified CPV codes listed in Annex A, and at least the general ‘health services’ code
There is no minimum threshold for application of the regime, including where mixed procurements fall under the PSR. When applying this regime, relevant authorities are expected to take a proportionate approach that ensures their implementation of this regime does not create disproportionate burden relative to the benefits that will be achieved.
The healthcare services subject to this regime are those that provide healthcare (whether treatment, diagnosis or prevention of physical or mental health conditions) to individuals (that is, patients or service users) or groups of individuals (that is, where treatment is delivered to a group).
In broad terms, these are services arranged by the NHS, such as hospital, community, mental health, primary healthcare, palliative care, ambulance and patient transport services, and for which the provider requires Care Quality Commission (CQC) registration, as well as those services arranged by local authorities that focus on preventative public health provision to individuals, such as substance misuse, sexual and reproductive health, and health visits.
Unless goods and non-healthcare services fall within the definition of a mixed procurement set out in this regime, they are not in scope and must be arranged under the rules governing wider public procurement.
Examples of services not in scope of this regime are:
- goods (for example, medicines and medical equipment)
- social care services
- patient transport services that do not require CQC registration
- non-healthcare services or health-adjacent services that do not provide healthcare to an individual (for example, capital works, business consultancy, catering, hospital administrative services, hospital bedding services or public health marketing campaigns)
- community pharmacy essential services arranged under the National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013, and advanced and enhanced community pharmacy services arranged under The Pharmaceutical Services (Advanced and Enhanced Services) (England) Directions 2013 (where all providers on the pharmaceutical list within the area for the relevant authority making the arrangements may apply to provide these services)
If a procurement exercise for healthcare services started under the PCR or the PPCCR, then it must be completed under those rules. This applies even if the process is ongoing and completed after the PSR took effect on 1 January 2024. The PSR does not have any retrospective effect on contracts or framework agreements that were entered into before 1 January 2024. However, from 1 January 2024 any changes to contracts or framework agreements awarded or established before 1 January 2024 for services in scope of the regime must be carried out in accordance with the contract modifications section of the PSR.
Mixed procurement
Mixed procurement is defined in Regulation 3.
The PSR must not be used for the procurement of goods or non-healthcare services alone. However, when a contract comprises a mix of in-scope healthcare services and out-of-scope goods or services, relevant authorities may only use the PSR to arrange those services when:
- the main subject matter of the contract is in-scope healthcare services; and
- the relevant authority is of the view that the out-of-scope goods or services could not reasonably be supplied under a separate contract (that is, where procuring goods or services separately would likely prevent the relevant authority from meeting its duty to act in accordance with the procurement principles)
The main subject of the contract is determined by which of these 2 components is higher:
- the estimated lifetime value of the in-scope healthcare services
- the estimated lifetime value of the out-of-scope goods or services
Relevant authorities must keep an internal record of the rationale for their decision (see Annex B: transparency).
Examples of services that can be arranged under the PSR but may require some mixed procurement of healthcare and non-healthcare services to achieve their core objectives include but are not limited to:
- healthcare and social care services arranged under a single contract
- healthcare and social care services under a section 75 (National Health Service Act 2006) partnership arrangement
- patient transport for healthcare services (for which the provider requires CQC registration) and non-healthcare services (where no CQC registration is required)
- packages arranged under the Better Care Fund
- discharge to assess services
- mental health aftercare services, such as support services arranged under s117 of the Mental Health Act 1983
- prison services that include healthcare services
- asylum seeker services that include healthcare services
- veteran services that include healthcare services
Procurement principles
Relevant authorities must make decisions in the best interests of people who use the service. To do this, they must act with a view to all of the following:
- securing the needs of the people who use the services
- improving the quality of the services
- improving the efficiency of service provision.
Relevant authorities must also act transparently, fairly and proportionately when procuring healthcare services.
Relevant authorities may consider the value of providing services in an integrated way, including with other healthcare services, health-related services or social care services, when acting in accordance with the procurement principles.
The PSR processes
See in PSR toolkit: Getting to the right decision flowchart
Relevant authorities are expected to identify which provider selection process applies to their procurement, including where they choose to modify an existing contract. They should do this sufficiently in advance of a contract coming to an end.
If the criteria are met to follow direct award process A or B, then these processes must be followed to award the contract. A competitive process must be used to award a framework agreement. In all other circumstances, each relevant authority must identify which provider selection process is appropriate for the particular situation and ensures best outcomes for their patients.
If a relevant authority has previously used a specific provider selection process to award a contract for a healthcare service, it is not bound to use that process again when next selecting a provider for that service (unless a specific provider selection process must be used in the circumstances). Where a provider has an existing contract covering multiple services, relevant authorities may keep all services under a single contract, determining which single provider selection process is the most appropriate for the entire contract.
The Regulations allow the award of a contract to more than 1 provider, either jointly or otherwise. It should be noted that the NHS Standard Contract does not allow multi-provider contracting (that is, the award of a single contract to more than one provider). However, the NHS Standard Contract can be used as a ‘lead’ or ‘prime’ contract. Under this model, the relevant authority enters into a contract with a single lead or prime provider and the lead or prime provider then subcontracts the delivery of some or all of the services to the other providers (that is, the subcontractors).
The NHS Standard Contract can also be used in an alliance agreement approach, under which multiple providers are bound together to pursue shared aims and objectives.
For more information on the lead or prime provider model and subcontracting, and the alliance agreement model, please see the NHS Standard Contract technical guidance.
Direct award process A
The process that must be followed when awarding a contract under direct award process A is set out in Regulations 6(3) and 7.
See in PSR toolkit: Direct award process A end-to-end process map
Direct award process A must be used when all the following apply:
- there is an existing provider of the healthcare services to which the proposed contracting arrangements relate
- the relevant authority is satisfied that the healthcare services to which the proposed contracting arrangements relate can only be provided by the existing provider (or group of providers) due to the nature of the healthcare services
- the type of service means there is no realistic alternative to the current provider
Direct award process A must not be used to award contracts when establishing a new service or to establish or conclude a framework agreement.
Services may include but are not limited to:
- Type 1 and 2 urgent and emergency services and associated emergency inpatient services
- 999 emergency ambulance services
- NHS urgent mental health crisis services
- services established as commissioner requested services (CRS)*
- a service that is interdependent with and cannot realistically be provided separately from another service that only that provider can realistically provide (for example, because of a need for cross-specialty or cross-service working).
* A service is established as a CRS by following the processes set out in the provider licence (for NHS trusts, foundation trusts or certain independent sector providers). Relevant authorities are expected to periodically review CRS designations, in line with the Guidance for commissioners on ensuring the continuity of healthcare services, as markets and alternative provision may evolve. Providers that have been designated to provide CRS can still be replaced if the relevant authority considers this to be appropriate.
Relevant authorities must consider the exclusions in Regulations 20 and 20A and whether a provider is an excluded or excludable provider, and act accordingly.
Transparency
When awarding a contract under direct award process A, relevant authorities must:
- keep accurate records of their decision-making
- publish a confirmation of award notice within 30 days of the contract award date (see Annex B: transparency.). There is no requirement to apply a standstill period
Direct award process B
The process that must be followed when awarding a contract under direct award process B is set out in Regulations 6(4) and 8.
See in PSR toolkit: Direct award process B end-to-end process map
Direct award process B must be used when all the following apply:
- the proposed contracting arrangements relate to healthcare services in respect of which a patient is offered a choice of provider and team
- the number of providers is not or cannot be restricted by the relevant authority
- the relevant authority will offer contracts to all providers to which an award can be made when they meet all requirements in relation to the provision of the healthcare services to patients
- the relevant authority has arrangements in place to enable providers to express an interest in providing the healthcare services
Direct award process B must not be used to conclude a framework agreement.
The updated NHS Standing Rules (Part 8) set out the minimum qualification criteria in Regulation 42C against which providers should be assessed to become a ‘qualified’ provider for services where patients have the legal right to choose a provider and team, and for services where the relevant authority has decided not to restrict the number of providers patients can choose from.
Therefore, services arranged using direct award process B may include but are not limited to:
- elective services led by a consultant or mental health care professional where the ICB or NHS England has a legal duty to provide patients with a choice of provider [as set out in Part 8 of the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012 (as amended)]
- other elective services for which patients do not have a legal right to choice but relevant authorities, including local authorities and NHS trusts, can voluntarily offer them a choice of providers, and where the number of providers is not restricted by the relevant authority through provider selection (for example, mandatory eye health services, audiology, podiatry services, NHS continuing healthcare services, and public health services such as over-40 health checks).
The qualification criteria (which must be applied by ICBs and NHS England) sit outside the PSR decision-making processes. They are set out in the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012 (as amended) and are further explained in NHS England’s patient choice guidance, under the heading Patient choice and qualification of providers.
Relevant authorities must consider the exclusions in Regulations 20 and 20A and whether a provider or subcontractor is an excluded or excludable provider, and act accordingly.
If relevant authorities are seeking to voluntarily establish other pools of providers from which patients can choose (that is, for services where there is no legal right to choice) and they intend to select a limited number of providers to be available, they must use the most suitable provider process or the competitive process to make their selection.
Example: NHS continuing health care services
NHS continuing health care (CHC) services can be within scope of the regime, but how the regime applies may depend on the way relevant authorities are managing their CHC services.
For example, relevant authorities can voluntarily establish a pool of providers that individuals can choose to receive care from. Providers can apply to be part of this contractual pool of NHS CHC providers assessed by the relevant authority. Once an individual is assessed as eligible for NHS CHC, a placement for that individual is brokered between the individual, the relevant authority, and the provider. In this case, where relevant authorities decide to limit the number of eligible providers in the contractual pool, and so are selecting between providers, then they must not use direct award process B and instead must follow the approach for the most suitable provider process or the competitive process.
There may be cases where the relevant authority does not select and limit the number of providers in the contractual pool, and an eligible individual can choose any provider from the CHC contractual pool capable of meeting their assessed needs as defined in a care and support plan (assuming the provider has capacity and is willing to take them on). In such instances, the existing providers of CHC services can be awarded contracts under direct award process B of the regime. This is because the relevant authority does not decide which providers the eligible individual can choose from.
Transparency
When awarding a contract under direct award process B, relevant authorities must:
- keep accurate records of their decision-making
- publish a confirmation of award notice within 30 days of the contract award date (see Annex B: transparency). There is no requirement to apply a standstill period
Direct award process C
The process that must be followed when awarding a contract under the direct award process C is set out in Regulations 6(5) and 9.
See in PSR toolkit: Direct award process C end-to-end process map
Direct award process C may be used when all the following apply:
- the relevant authority is not required to follow direct award processes A or B
- the term of an existing contract is due to expire and the relevant authority proposes a new contract to replace that existing contract at the end of its term
- the proposed contracting arrangements are not changing considerably from the existing contracting arrangements
- the relevant authority is of the view that the existing provider (or group of providers) is satisfying the existing contract and will likely satisfy the proposed contract to a sufficient standard
Direct award process C must not be used to establish a framework agreement.
Even where a relevant authority can use direct award process C, it may choose instead to follow the most suitable provider process because it believes it can identify a better placed provider or the competitive process because it wishes to test the market.
Relevant authorities must consider the exclusions in Regulations 20 and 20A and whether a provider or subcontractor is an excluded or excludable provider, and act accordingly.
Establishing that the proposed contracting arrangements are not changing considerably from the existing contract
To use direct award process C, the relevant authority must be satisfied that the arrangements in the proposed contract for the provision of healthcare services are not changing considerably from the existing contract. In practice, this means the changes do not meet the considerable change threshold as set out in Regulation 6(10) or they fall within one of the exceptions in Regulations 6(11) and 6(12).
If the considerable change threshold is met, the proposed arrangements will be a considerable change and direct award process C must not be used.
What constitutes a considerable change?
For the purposes of the PSR, the considerable change threshold is met where one or both of the following tests are satisfied:
- the proposed arrangements are materially different in character to the existing contract when the existing contract was entered into (unless the corporate changes exception below applies)
or
- the change meets all 3 of the following criteria:
- the proposed change to the contracting arrangements (as compared to the existing contract) is attributable to (or the result of) a decision made by the relevant authority
- the lifetime value of the proposed new contract is at least £500,000 higher than the lifetime value of the existing contract when it was entered into (that is, the increase in value is equal to or greater than £500,000)
- the lifetime value of the proposed new contract is at least 25% higher than the original lifetime value of the existing contract when it was entered into (that is, the lifetime value of the new contract exceeds that of the original contract by 25% or more)
(unless the external factors exception below applies)
Lifetime value of a contract for the purpose of calculating the considerable change threshold
Lifetime value of a contract means the total value of the contract over the full length of the contract. If the contract explicitly states there is an option to extend, then the value of the extension should also be considered in the lifetime value. For example, where a contract may be worth £1 million per year and is for a duration of 3 years, its lifetime value when it was entered into would be £3 million. If there was an option to extend for an additional 2 years, worth £1 million per year, then the lifetime value of the contract when it was entered into would be £5 million. Unplanned modifications to the contract during its term are not to be included in this calculation.
Corporate changes exception [Regulation 6(11)]
If the relevant authority is making a change to an existing contract solely because the provider’s identity is changing due to succession into the position of provider following corporate changes, including takeover, merger, acquisition or insolvency, this will not meet the considerable change threshold (that is, it is permissible), provided that the requirements of part (b) above are not met.
The relevant authority must also be satisfied that the provider meets the basic selection criteria.
External factors exception [Regulation 6(12)]
There is also an exception to the general threshold on considerable change if a relevant authority is making changes to an existing contract in response to external factors beyond its control. These may be changes in patient or service user volume or in prices in accordance with a formula provided for in the contract, for example.
To note, this exception cannot be used if the changes result in a contract materially different in character to the existing contract when that was entered into. This exception may be useful, for example, where a relevant authority needs to commission higher volumes of the same services owing to factors it has no control over.
Example: change that is considerable
A relevant authority holds a contract with an original contract value of £3 million. The contract is coming to an end and the relevant authority wants (so attributable to a decision made by the relevant authority) to continue with the current provider but add £1 million to the contract. The contract is not going to be materially different in character.
The change in the value of the contract represents 33% of the original contract value, which is over the 25% threshold. It would also be over £500,000. Therefore, the relevant authority must not continue the contract under direct award process C and instead must follow the most suitable provider process or the competitive process.
Example: change that is not considerable
A relevant authority holds a contract with an original contract value of £1 million. It has made a contract modification that increases the value of the contract by £400,000 and wishes to reflect this in the new contract (so attributable to a decision made by the relevant authority) at the point of re-contracting. The lifetime value of the proposed new contract will therefore be £1.4 million. The contract is not going to be materially different in character.
The £400,000 change is 40% of the lifetime value of the existing contract when it was entered into, which is over the 25% threshold. However, the change is under £500,000 and so is not a considerable change. The relevant authority can proceed with direct award process C.
Example: change that renders the contract materially different in character
An existing contract to provide physical health assessments for patients receiving care for severe mental illness is coming to an end and the relevant authority wants to add a new service to this contract to provide physical health assessments for patients with eating disorders. The original contract was valued at £1 million and the service the relevant authority wants to add is valued at £450,000, making the value of the future contract £1.45 million.
Although the change in the value of the contract would be lower than the considerable change threshold, the addition of the new service for a patient group with different needs constitutes a material change in the character of the contract. Therefore, the relevant authority must not continue the contract under direct award process C and instead must follow the most suitable provider process or the competitive process.
Establishing that the existing provider is satisfying the existing contract, and is likely able to satisfy the new contract to a sufficient standard
Once the relevant authority has established that the proposed contracting arrangements are not changing considerably, it must assess whether the existing provider is both:
- satisfying the existing contract to a sufficient standard, according to the detail outlined in the existing contract, including the key criteria and basic selection criteria used
- will likely satisfy the new contract to a sufficient standard, according to the detail outlined in the new contract, including any changes to the application of the key criteria and the basic selection criteria
The relevant authority must decide the relative importance of each of the key criteria for the service in question, before assessing the existing provider against the key criteria.
If direct award process C is not applicable because the proposed contracting arrangements are changing considerably, the existing provider is not satisfying the existing contract or is unlikely to satisfy the new contract, then the relevant authority must follow the most suitable provider process or the competitive process.
The most suitable provider process
The process that must be followed when awarding a contract under the most suitable provider process is defined in Regulations 6(6) and 10.
See in PSR toolkit: Most suitable provider end-to-end process map
The most suitable provider process is designed to allow relevant authorities to assess which provider (or group of providers) is most suitable for delivering the proposed contracting arrangements, based on consideration of the key criteria and the basic selection criteria, and to award a contract without running a competitive exercise.
The relevant authority decides the weighting it gives to each of the key criteria – quality and innovation; value; integration, collaboration and service sustainability; improving access, reducing health inequalities and facilitating choice; and social value – or indeed whether to make a criterion assessment one that is passed or failed, and how to assess them. Weightings will reflect the importance the relevant authority places on each of these criteria given its ambitions for the service.
The decisions that a relevant authority makes on weighting and whether any criteria assessments are passed or failed might mean that only a few providers, or even one, can meet its key criteria required of a suitable provider. Relevant authorities should make their requirements clear in the notice of their intention to follow the most suitable provider process, so only providers that have a realistic prospect of being a suitable provider invest time in making themselves known.
The most suitable provider process may be used when all the following apply:
- the relevant authority is not required to follow direct award processes A or B
- the relevant authority cannot or does not wish to follow direct award process C
- the relevant authority is of the view that it is likely to be able to identify the most suitable provider (without running a competitive process) – considering its ambitions for the service for which it is contracting (as reflected in the weight it is giving to each of the key criteria) and all relevant information available to the relevant authority at the time
The most suitable provider process can be used to arrange new or existing services but must not be used to establish a framework agreement.
The fundamental difference between the most suitable provider process and the competitive process is that:
- in the competitive process each interested provider must submit a bid that is evaluated by the relevant authority to determine which is successful, whereas
- in the most suitable provider process the relevant authority makes a judgement on the suitability of the provider (or group of providers) based on its knowledge of the market
Therefore, the most suitable provider process may be an attractive option where the relevant authority’s familiarity with likely suitable providers for the service it is procuring leads it to believe it can identify the most suitable provider.
The relevant authority’s ongoing market research (see provider landscape) beyond its own system will influence its familiarity with potential suitable providers. However, the nature of the contract that the relevant authority plans to award will normally be the biggest influence on how familiar it is with potential suitable providers and whether the most suitable provider process is the most appropriate option.
For example, if the relevant authority is planning to let a contract for which successful delivery and achievement of value for money will depend on integration with other local services – such as with primary care, local voluntary, community and social enterprise (VCSE) organisations, the partner local authorities and existing local service provision – it may judge that only providers that have existing local relationships and services would be able to meet its requirements, particularly those against the integration, collaboration and service sustainability key criterion. The duty on the relevant authority to issue a notice stating that it intends to follow the most suitable provider process tests whether its analysis that it is familiar with the potential suitable providers is correct: if a suitable but unfamiliar provider comes forward in response to the notice, the relevant authority may decide that it should undertake a competitive process instead.
Process and transparency
Where a relevant authority follows the most suitable provider process:
- The relevant authority must keep robust records of its decision-making throughout the process. Suitable providers may have an existing relationship with the relevant authority, including potentially sharing membership of partnership forums, and so it is particularly important that management of conflicts of interest is transparent and recorded.
- The relevant authority decides its process for choosing the most suitable provider, taking into account the key criteria and the weighting it has given to each criterion.
- The relevant authority publishes an intention to follow the most suitable provider process and must wait at least 14 days after the day on which the notice of intention is submitted for publication before proceeding. Relevant authorities must be able to demonstrate that they have considered whether an alternative provider that makes itself known in writing following publication of the notice would be suitable given the key criteria as weighted by it and having followed the procurement principles – the work involved for this is not expected to make a disproportionate administrative burden on any party. If the relevant authority judges that any providers unfamiliar to it would be suitable, it should consider whether the competitive process would be more suitable.
- Having identified the suitable providers, the relevant authority assesses their relative suitability by considering the key criteria it has weighted and applying the basic selection criteria in a fair way across them (that is, on the same basis), and chooses the most suitable provider or group of providers to which to make an award.
- The relevant authority must publish an intent to award notice detailing the chosen provider and observe the standstill period of 8 working days, calculated from the day after the notice is published. The relevant authority and the most suitable provider may agree further details, including financial, of the service to be delivered before or after the relevant authority issues the intent to award notice.
- The relevant authority may then enter into a contract with the chosen provider after the standstill period has ended.
- The relevant authority must publish a notice confirming the award of the contract within 30 days of the contract being awarded.
Relevant authorities may approach providers and ask for information at any point in the process as necessary but must take a fair and proportionate approach.
If despite these requests for information, the relevant authority has insufficient information to award the contract under the most suitable provider process or it cannot identify which is the most suitable provider, it may wish to undertake either a new most suitable provider process with its requirements more fully and clearly articulated (ensuring its weighting of key requirements are matched) or a competitive process where doing so would be proportionate to the benefits expected from running a competitive process.
If the relevant authority decides to switch provider selection approach after publishing its intended approach notice, then it must abandon the selection process before switching.
Relevant authorities must consider the exclusions in Regulations 20 and 20A and whether a provider or subcontractor is an excluded or excludable provider, and act accordingly.
The competitive process
Regulations 6(7) and 11 set out the process that relevant authorities must follow when awarding a contract under the competitive process.
See in PSR toolkit: Competitive process end-to-end process map
Relevant authorities may design and run the competitive process in any way they choose so long as this complies with the procurement principles of the PSR and with the steps outlined below.
The competitive process must be used when both of the following apply:
- the relevant authority is not required to follow direct award processes A or B
- the relevant authority cannot or does not wish to follow direct award process C or the most suitable provider process
The competitive process must be used if the relevant authority wishes to conclude a framework agreement.
Process and transparency
The steps outlined in the Regulations and the transparency requirements must be adhered to.
When following the competitive process, relevant authorities:
- Must develop a service specification setting out its requirements for the service. In doing so, relevant authorities may consider undertaking a pre-market engagement exercise.
- Must determine the contract or framework award criteria for the service in question, taking into account the key criteria and applying the basic selection criteria and any other elements of the contract or framework award.
- Must formally advertise the opportunity to bid (see Annex B: transparency) and ensure providers are given a reasonable timeframe in which to respond. The advertisement must include information on how bids will be assessed, including whether the different award criteria will be assessed in stages.
- Must assess any bids received by following the assessment process – that is, against the award criteria and the exclusion criteria set out in Regulations 20 and 20A, in a fair way across all bids (that is, on the same basis). Relevant authorities may assess criteria in stages, in accordance with step 3 above. For example, a provider that does not meet the basic selection criteria may be discounted without further assessment.
- Must keep robust records of the procedure followed, how each bid scored and the rationale for selecting the successful provider.
- Must identify the successful provider (or group of providers).
- Must inform the successful provider (or group of providers) in writing of its intention to award a contract or conclude a framework agreement, and also each unsuccessful provider that its bid has been unsuccessful.
- Must publish a notice of its intention to award the contract to or conclude a framework agreement with the chosen provider (or group of providers) and observe the 8 working day standstill period.
- May enter into a contract or conclude a framework agreement with the chosen provider (or group of providers) after the standstill period has concluded.
- Must publish a notice confirming the award of the contract within 30 days of the contract being awarded.
Relevant authorities may engage in dialogue or negotiate with all bidders or shortlisted bidders prior to determining which provider it will award a contract to or conclude a framework agreement with. This will be with a view to improving on initial offers, providing they do so in a fair and proportionate way and treat all bidders equally.
Framework agreements
Framework agreements for the purposes of this regime are agreements between a relevant authority (or relevant authorities) and provider(s) that set out the terms and conditions for how the provider will enter into one or more contracts to provide healthcare services in scope of the PSR, for as long as the framework agreement is in place.
The terms and conditions of a framework agreement may be modified in line with the requirements for contract modification for this regime.
Establishing a framework agreement
When concluding a framework agreement, relevant authorities must use the competitive process to select provider(s) to be party to the framework agreement.
Providers may be added to a framework agreement during its term, but relevant authorities must use the competitive process to do so and are advised to set out how and when this might be done in the terms and conditions of the framework agreement. Relevant authorities are advised to use the same award criteria as they did when setting up the original framework agreement.
When concluding a framework agreement, relevant authorities are expected to set out:
- the terms for awarding a contract based on the framework agreement including which relevant authorities can award contracts
- the duration of the agreement. This must not exceed 4 years, other than in exceptional cases where the relevant authority is satisfied that the subject of the framework agreement justifies a longer term
- how the framework agreement will operate
- how the call-off procedures will operate (see below)
- how new providers or relevant authorities can be added to the framework agreement at a later date (if applicable)
Relevant authorities must consider whether a provider or subcontractor is an excluded or excludable provider as set out in Regulations 20 and 20A, and act accordingly. Relevant authorities are advised to set out in the terms and conditions of their framework agreement that they may remove a provider if that provider meets the exclusion criteria.
Awarding contracts based on a framework agreement
The processes that must be followed when awarding a contract based on a framework agreement are defined in Regulation 18.
Only relevant authorities identified as able to award contracts under the framework agreement may award contracts to providers that are party to that same framework agreement. Relevant authorities may decide that the award criteria for awarding contracts under a framework agreement differ from those for concluding the framework.
Relevant authorities must award a contract under a framework agreement in accordance with the terms and conditions of that framework agreement.
Relevant authorities may award a contract under a framework agreement in one of the following ways:
- without competition if the framework agreement only includes 1 provider
- if the framework agreement includes more than 1 provider, either:
- without a further competition
- by following the competitive process (via a ‘mini-competition’)
In all these scenarios, relevant authorities must make decisions in accordance with the framework agreement.
Transparency for awards of a contract without competition
Relevant authorities must:
- publish a notice confirming the decision within 30 days of the contract being awarded
Process and transparency for award of a contract following a competitive process
Relevant authorities must:
- follow the process for the competitive process, substituting step 3 (the step advertising the opportunity to the market) with ‘invite providers party to the framework to submit an offer’
- follow the terms and conditions of the framework agreement, including how competitions must run when awarding a contract based on that framework agreement (if this is set out)
- publish an intent to award notice and observe the standstill period for 8 working days before awarding the contract
- publish a notice confirming the decision within 30 days of the contract being awarded.
When awarding a contract under a framework agreement, the term of the contract may exceed the length of the framework agreement provided that the contract is awarded while the framework agreement is live.
Contracts awarded from a framework agreement are expected to not exceed the total value of the framework agreement.
Transitional arrangements for framework agreements arranged under the PCR
Where relevant authorities wish to award contracts based on existing framework agreements and dynamic purchasing systems (DPS) from 1 January 2024, then they must use the PSR. However, the awarding of contracts from a framework agreement or DPS must be in line with the terms and conditions of the framework or DPS agreement, which may restrict which approach can be used.
From 1 January 2024, if a relevant authority wishes to modify contracts awarded under a DPS or framework agreement that was established under PCR regulations, the modification must be made by following the PSR process detailed in the contract modifications section.
Urgent awards or contract modifications
The requirements for an urgent award or contract modification are detailed in Regulations 14(1), 14(2) and 14(4).
See in PSR toolkit: Urgent circumstances end-to-end process map
There are limited circumstances where relevant authorities may need to urgently award or modify contracts to address immediate risks to patient or public safety.
These circumstances include where:
- a new service needs to be arranged rapidly in an unforeseen emergency or local, regional or national crisis (for example, a pandemic)
- urgent quality or safety concerns pose risks to patients or the public and necessitate rapid changes
- an existing provider is suddenly unable to provide services under an existing contract (for example, it becomes insolvent or suddenly lacks critical workforce) and a new provider needs to be found
In urgent situations, relevant authorities may make the following decisions without following the steps required under this regime:
- re-award contracts held by the existing provider(s)
- award contract(s) for new services
- award contract(s) for considerably changed services
- make contract modifications (without limitation)
An urgent award or modification must only be made by a relevant authority when all the below apply:
- the award or modification must be made urgently
- the reason for the urgency was not foreseeable by and is not attributable to the relevant authority
- delaying the award of the contract to conduct a full application of the regime would likely pose a risk to patient or public safety
Relevant authorities must not use the urgent award or contract modification provisions in this regime if the urgency is attributable to the relevant authority not leaving sufficient time to make procurement decisions and run a provider selection process – poor planning is not an acceptable reason for using these provisions.
In these urgent circumstances, relevant authorities:
- are expected to limit the contract term or contract modification term to that which is strictly necessary. This is advised to be long enough to address the urgent situation and to conduct a full application of the PSR for that service at the earliest feasible opportunity. Contracts awarded under Regulation 14 are anticipated to be for no longer than 12 months and, if longer relevant authorities must justify and record this decision
- must keep records of their decision-making, including the justification for using an urgent award
- must be transparent about their decision through issuing an urgent award notice or urgent modification notice
Relevant authorities may also make specific urgent modifications to extend the term of an existing contract during the standstill period if they are seeking advice from the Independent Patient Choice and Procurement Panel, in accordance with Regulation 14(3).
Modification of contracts and framework agreements during their term
The requirements for the modification of contracts or framework agreements during their term are detailed in Regulation 13.
See in PSR toolkit: Contract modification end-to-end process map and Contract modification flowchart
There will be situations where contracts or framework agreements need to be modified within their term to reflect or account for changes to services or circumstances. This regime allows for certain modifications to be made to contracts or framework agreements during their term without following a new provider selection process, but in some cases will require the publication of transparency notices.
Relevant authorities are expected to consider this section in conjunction with the modifications (variations) provisions of the relevant contract or subcontract (for example, General Condition 13 of the NHS Standard Contract). Guidance on varying an NHS Standard Contract is available on the NHS Standard Contract webpage.
Modifications that materially change the character an existing contract or framework agreement are not permitted under the regime; a new provider selection process is required to be undertaken. Further information on which modifications are permitted is given below.
The provisions in this section must only be used for modification of contracts during their term and not to circumvent the Regulations when a contract ends and a new one needs to be awarded.
Permitted modifications
Under this regime, some modifications to contracts are permitted during their term and so do not require a new selection process.
Calculating the change in the lifetime value of a contract for the purpose of modifications
Lifetime value of a contract means the total value of the contract over the full length of the contract (including any extensions of duration or scope provided for in the contract).
When calculating the cumulative change in the lifetime value of a contract, relevant authorities must include all modifications to the contract since it was awarded regardless of the reason, except those that were provided for in the original contract (for example, extensions provided for in the original contract).
Modifications to contracts originally awarded under direct award process A or B
Modifications are permitted where the original contract was awarded under direct award process A or B and the modification does not materially alter the character of the contract.
If that modification is attributable to a decision of the relevant authority and the cumulative change in the lifetime value of the contract since it was entered into is £500,000 or more, the modification is still permitted but the relevant authority must publish a transparency notice.
Modifications to contracts originally awarded under direct award process C, the most suitable provider process or the competitive process, or to contracts that were originally awarded under the Public Contracts Regulations 2015
Such modifications are permitted during the term of the contract in the following instances:
- the modification is unambiguously provided for in the contract or framework agreement documents (that is, the scope and nature of the potential change are detailed in the existing contract)
- the modification is solely a change in the provider’s identity due to succession into the position of provider following corporate changes, including takeover, merger, acquisition or insolvency, and where the relevant authority is satisfied that the provider meets the basic selection criteria
- the modification is made in response to external factors beyond the control of the relevant authority and provider, including but not limited to changes in:
- patient or service user volume
- prices in accordance with a formula provided for in the contract documents (for example, pay uplifts, uplifts in prices published in the NHS Payment Scheme or index linking) that do not render the contract or framework agreement materially different in character
- the modification is attributable to a decision of the relevant authority and does not materially alter the character of the contract or framework agreement, and the cumulative change in the lifetime value of the contract or framework agreement, compared to its value when it was entered into, is under £500,000 or under 25%
If the relevant authority makes a permitted modification (to a contract that was originally awarded under direct award process C, the most suitable provider process or the competitive process, or where the contract was originally awarded under the Public Contracts Regulations 2015), it must publish a transparency notice where both the below apply:
- the modification is attributable to a decision of the relevant authority
- the cumulative change in the lifetime value of the contract or framework agreement is £500,000 or more
To note, contracts entered into before the PSR came into force must be modified in line with this section.
Calculating the change in the lifetime value of a contract for the purpose of modifications examples
1. A contract valued at a total of £100,000 is awarded for 3 years. 1 year into the contract the relevant authority modifies the contract to incorporate a nationally mandated uplift valued at £10,000 for staff pay increases. In the third year, the relevant authority wishes to add 6 months to the contract valued at £15,000.
This would be a permitted modification under the PSR because, although the total cumulative value of the changes (£25,000) equals 25% of the lifetime value of the original contract, it is below the £500,000 threshold. A transparency notice is not required.
2. A contract is awarded for 3 years with an optional extension of 2 years. The original contract value is £5 million (including the extension). The relevant authority uses the 2-year extension (worth £2 million). Prior to the contract’s end the relevant authority decides to increase the value of the contract, adding £500,000.
This would be a permitted modification under the PSR because, although the cumulative value of the modifications to the contract over its lifetime are not below £500,000, it is lower than 25% of the lifetime value of the original contract. In accordance with Regulation 13(4), the relevant authority would have to publish a notice in relation to this modification.
Contract modifications in urgent situations
Contract modifications may need to be made urgently. In these circumstances relevant authorities must still be transparent about their decision-making. Details of what needs to be published and when can be found in the urgent awards or contract modifications section above.
Planning and running PSR processes
Planning
To apply this regime effectively, relevant authorities are expected to have a clear understanding of the services they want to arrange and the outcomes they intend the services to deliver.
The relevant authority’s intentions are prerequisites to any decision about selecting a provider and they are expected to be clearly established in good time via the routine planning activity that takes place across a system. Relevant authorities are expected to reflect these intentions in their pipeline of healthcare and non-healthcare procurements, and decisions taken under this regime are also expected to serve and reflect these intentions.
The regime also sets out how to deal with unplanned urgent situations (see urgent award or contract modifications).
Provider landscape
Relevant authorities are expected to develop and maintain sufficiently detailed knowledge of potential suitable providers; that is, including an understanding of their ability to deliver services to their (local, regional or national) populations, varying actual or potential approaches to delivering services, and capabilities, limitations and connections with other parts of the system. Relevant authorities may wish to consider undertaking pre-market engagement to update or maintain their provider landscape knowledge.
This knowledge is expected to go beyond that of existing providers and to be a general feature of planning and engagement work, developed as part of the commissioning or subcontracting process rather than only at the point of contracting. Without this knowledge, relevant authorities may not have enough evidence to confirm the existing provider is performing to the best quality and value, may miss opportunities to improve services and identify valuable innovations and ultimately lead providers to make representations (see standstill period).
Relevant authorities are expected not to treat providers from VCSE and independent sectors differently from NHS trusts and foundation trusts or local authorities based solely on their status.
Governance
Relevant authorities are expected to establish how best to follow this regime within their wider structural and governance arrangements. This regime does not require relevant authorities to structure their decision-making arrangements in any specific way or for provider selection decisions to be taken by particular committees or at a particular level within an organisation or system. Relevant authorities are expected to ensure that their internal governance supports the effective application of this regime.
Keeping records of decision-making
The relevant information requirements are detailed in Regulation 24.
Relevant authorities must make and keep clear records detailing their decision-making process and rationale. This must be done for all provider selection processes detailed in this guidance including those abandoned or where the relevant authority decided to return to an earlier step in the process.
Records must include:
- name of the provider to which the contract has been awarded or the name of any provider that is a party to a framework agreement, and the address of its registered office or principal place of business
- the decision-making process followed to select a provider(s), including details of the procedure used when the competitive process is followed
- the reasons for the decisions taken
- details of the individual(s) making the decision (this may be the name of a committee or job titles of individuals making the decision, as appropriate)
- any declared or potential conflicts of interest for individuals involved in decision-making and how these were managed
- where a procurement is abandoned, the date on which it was abandoned
Records are expected to be kept when contracting for mixed procurements, including how the procurement meets the requirements for mixed procurements under this regime.
When following direct award process C or the most suitable provider process, records must also include:
- a description of how the key criteria (e.g. weighting, hierarchy, or more informal description of importance) were taken into account and the basic selection criteria were assessed when making decisions. This description is expected to cover the relative importance of the key criteria that the relevant authority used to make a decision, the rationale for this relative importance and the rationale for choosing the provider with reference to the key criteria
When following the competitive process (including when concluding a framework agreement or when awarding a contract based on a framework agreement following the competitive process), records must also include:
- a description of how the key criteria were considered, the basic selection criteria were assessed and contract or framework award criteria were evaluated when making a decision. This description is expected to cover the relative importance the relevant authority attributed to the key criteria, the rationale for this relative importance and the rationale for choosing the provider with reference to the key criteria
When concluding a framework agreement, records are expected to include the terms and conditions the framework agreement will lay down and which relevant authorities are part of the framework agreement.
When awarding a contract from a framework agreement, records are expected to include which framework agreement the contract is being awarded under.
Relevant authorities must be aware that they may need to disclose the rationale for their decision-making under the Regulations if a representation is made (see standstill period). Relevant authorities are expected to keep their records for a period of time that is in line with their organisation’s record keeping policies and any applicable legislation.
In urgent circumstances
When awarding or modifying a contract in an urgent circumstance, relevant authorities must make and keep clear records detailing their decision-making process and rationale.
Records must include:
- justification for using the urgent circumstances exemption
- name of the provider(s) to which the contract has been awarded and the address of its registered office or principal place of business
- the approach taken to select a provider and the decision-making process followed (that is, urgent circumstance)
- details of the individual(s) making the decision
- any declared or potential conflicts of interest of individuals making the decision (not including individual names) and how these were managed
Conflicts of interest
The conflicts of interest requirements are detailed in Regulation 21.
The routine declaration and management of conflicts of interest is a key aspect of good governance, and critical in maintaining public confidence in decision-making and in protecting staff, board members, councillors and trustees from allegations that they have acted inappropriately.
Relevant authorities must take appropriate measures to prevent, identify and remedy conflicts of interest arising during the application of the PSR. Their governance arrangements for making provider selection decisions must be able to manage conflicts that arise. Relevant authorities may wish to give board committees or non-executive directors (or other senior persons independent of the decision-making process) a role in managing and resolving conflicts of interest relating to provider selection decisions.
The way in which conflicts of interest are managed needs to be sympathetic to the vision for integrated care systems (ICSs) of collaboration and joint working, the procurement principles of the regime and the policy intent of the 2022 Act in relation to bringing NHS organisations and local authorities together to collaborate in making decisions about care provision. Therefore, relevant authorities are expected to follow and have regard to that vision and policy when managing conflicts of interest around provider selection decisions.
Conflict of interest is defined in Regulation 21(2)(a) as any situation:
“where an individual has, directly or indirectly, a financial, economic or other personal interest which might be perceived to compromise their impartiality and independence in the context of the procurement process”.
Any such individual is required to recuse themselves from the procurement decision-making process.
This section should be read in conjunction with other relevant regulations and statutory guidance, including Managing conflicts of interest in the NHS, as applicable to relevant authorities.
Principles of management
The management of conflicts of interest is expected to be based on the following principles:
1. All decisions made under this regime must be clearly and objectively directed towards meeting the statutory functions and duties of relevant authorities or, for local authorities only, directed towards the delivery of a service that the local authority has power to provide. Individuals involved in decisions relating to these functions are expected to act clearly in service of those functions and duties, rather than furthering (their own) direct or indirect financial, economic or other personal, professional or organisational interests.
2. ICBs have been created with the intention of giving statutory NHS provider, local authority and primary medical services (general practice) nominees a role in decision-making. These individuals are expected to act in accordance with the first principle and, while the Regulations allow for the fact that an ICB member may also be an employee, director, partner or otherwise hold a position with one of these organisations, the possibility will remain of actual and perceived conflicts of interest arising. In addition, any member who is an employee, director, partner or otherwise holds a position in a provider taking part in a procurement process must recuse themselves from the decision-making process. For all PSR decisions, ICBs must carefully consider whether an individual’s role in another organisation may result in actual or perceived conflicts of interest and if so whether that possibility outweighs the value of the knowledge they bring to the process.
3. The personal and professional interests of all individuals involved in decisions about provider selection need to be declared, recorded and managed appropriately, following the relevant authority’s established conflicts of interest arrangements. This includes being clear and specific about the nature of any interest and of any conflict that may arise with regard to a particular decision, and how any conflicts are managed for each decision. To fulfil the transparency requirements under this regime, relevant authorities must keep internal records of individuals’ conflicts of interest and how these were managed (see record keeping).
4. Any conflicts of interests and how they were managed must be published alongside the confirmation of the decision to select a provider (see Annex B: transparency). When the decision is made by a committee or group, it is advised that any potential conflicts of interests of the committee or group as a whole are declared and not the names of individuals within it to whom they relate. When the decision is made by an individual, it is advised that conflicts of interest are declared against the individual’s job title rather than their name.
5. Actions to mitigate conflicts of interest when making procurement decisions are expected to be proportionate and to seek to preserve the spirit of collective decision-making wherever possible. Mitigating actions are expected to account for a range of factors, including the impact the perception of an unsound decision might have, and the risks and benefits of having a particular individual involved in making the decision. Mitigations may include:
- excluding a conflicted person from both the discussion and the decision-making
- excluding a conflicted individual and securing technical or local expertise from an alternative, unconflicted source
- arranging decision-making structures so a range of views and perspectives are represented, to avoid potentially conflicted individuals being in the majority
- convening a committee without the conflicted individual present (for example, when dealing with particularly difficult or complex decisions where members may not be able to agree, or to prevent an unsound decision being taken or the perception of bias)
6. Relevant authorities are expected to clearly distinguish between those individuals involved in formal decision-making and those whose input informs decisions but are not involved in the decision-making itself (such as through shaping the relevant authority’s understanding of how best to meet patients’ needs and deliver care for its population). The way conflicts of interest are managed is expected to reflect this distinction. For example, where independent providers (including those in the VCSE sector) hold contracts for services, it would be appropriate and reasonable for the relevant authority to involve them in discussions about pathway design and service delivery, particularly at place level. However, this would be clearly distinct from any considerations around contracting and commissioning, from which they would be excluded.
7. Where decisions are being taken under the competitive process, any individual associated with an organisation that has a vested interest in the procurement must recuse themselves from decision-making during that provider selection process. This includes ICB members who are also employees, directors, partners or otherwise hold a position in a provider that intends to take part in the procurement process.
8. The way conflicts of interest are declared and managed is expected to contribute to a culture of transparency about how decisions are made.
Abandoning a provider selection process
The process that must be followed when abandoning a provider selection process is set out in Regulation 15.
Relevant authorities may decide to abandon the process of provider selection at any time before an award is made (and not award a contract or conclude a framework under that provider selection process), providing this decision is transparent, fair and proportionate.
After deciding to abandon a provider selection process, relevant authorities are expected to notify providers that are aware they were being considered for the award of a contract or framework agreement (for example, in response to a tender under the competitive process). Relevant authorities must also submit for publication a notice of their decision on the Find a Tender Service (FTS) or the Central Digital Platform (see Annex B). This notice must be submitted within 30 days of the decision to abandon a provider selection process or if the decision was made during the standstill period, then within 30 days after the end of the standstill period. Where the decision to abandon a provider selection process is made during the standstill period, relevant authorities must follow the steps set out in Regulation 12 (see the standstill period).
Relevant authorities must also keep a record of their reasoning for abandoning a provider selection process (see record keeping).
Repeating a step in a provider selection process
When following direct award process C, the most suitable provider process or the competitive process, relevant authorities may decide to return to an earlier step in a decision process to rectify an issue in its application of that process. All providers that have previously been notified that they are being considered for the award of a contract, or to be a party to a framework agreement, must be informed in writing that the relevant authority is returning to an earlier stage in the provider selection process, including the step and any changes to timeframes. Where the decision to return to an earlier step is made during the standstill period, relevant authorities must follow the necessary steps set out in Regulation 12. For the avoidance of doubt, if the relevant authority is repeating a step as a response to a representation received during the standstill period, it does not need to communicate this decision twice (see standstill period).
Relevant authorities should not use the option to return to an earlier step as an opportunity to modify the selection parameters (that is, to modify the key criteria or change the service specifications). If relevant authorities need to modify the selection parameters, then they should abandon the provider selection process (in accordance with the Regulations) and start a new one.
Contract management
The requirements for termination of contracts are detailed in Regulation 22.
The decision-making process set out in this regime is part of a wider set of activities that together help ensure that NHS services are arranged in the best interests of the people who use them.
Once decisions have been made about which providers should provide services under this regime, the contract or subcontract awarded and associated contract management arrangements must reflect the desired outcomes. These are expected to take into consideration any relevant local and national policies on contract management.
Relevant authorities are expected to have appropriate mechanisms in place to periodically assess whether the anticipated benefits to patients, taxpayers and the population are still being realised, and where they are not to vary or end contracts or subcontracts, in accordance with the processes set out in them.
Relevant authorities are advised to ensure the duration of contracts and subcontracts is appropriate to the service in question and, where appropriate, that contracts and subcontracts include clear review provisions and options to terminate (as the NHS Standard Contract and subcontract templates do; see General Condition 17).
It is advised that contracts and subcontracts, where possible, set expectations about the possibility that they may need specific modifications during their term and about the potential for extension when the initial term ends (see General Condition 13 of the NHS Standard Contract and subcontract templates).
Subcontracting
Some healthcare services are purchased by provider organisations by means of a subcontract. Where an NHS provider (NHS trust or NHS foundation trust) is planning to subcontract to another provider for the provision of a service that is in scope of the regime, then this regime must be followed to select an appropriate subcontractor (as well as meeting any provisions governing subcontracting contained in that NHS provider’s own contract).
Where subcontractors are to be named in a contract award, the awarding relevant authority must gather information about which subcontractors a provider plans to include and ensure that subcontractors are not excluded or excludable under Regulation 20A. Where a relevant authority finds a planned subcontractor is excluded, they should (unless for reasons of national security) inform the lead contractor that is planning to use this subcontractor and give them an opportunity to find an alternative. Where the lead contractor does not agree to change the subcontractor, the provider should be excluded from the procurement.
Likewise, where the contract allows for subcontracting after the contract award, the relevant authority must ensure the contract requires the provider to seek the relevant authority’s consent to approve the identity of the subcontractor. Relevant authorities must ensure that no excluded or excludable provider is appointed as a subcontractor, subject to Regulation 20(1A).
If a provider that is not a relevant authority has been awarded a contract under this regime, and then sets out to subcontract any elements of that service, that subcontracting will not be governed by this regime. This makes it particularly important that the relevant authority that awarded the initial contract holds such a provider accountable via its contract for any subcontracting it undertakes and exercises its right to approve subcontracts and subcontractors (see General Condition 12 of the NHS Standard Contract).
Relevant authorities may consider it necessary to specify any limits or conditions to subcontracting in the contract (for example, services that may not be subcontracted under any circumstances).
Where subcontracting has taken place, the ongoing contract management of both the lead contractor by the relevant authority and of the subcontractors by the lead contractor is important, to ensure that the service in place is achieving the desired outcome.
Good information sharing between the original relevant authority and lead contractor about the arrangements with other providers will be an important means of assurance for both the relevant authority and the lead contractor.
The NHS subcontract published by NHS England is suitable for use for subcontracts entered into under the NHS Standard Contract. See the NHS Standard Contract webpage for more information.
Termination of contracts
The requirements for contract terminations are set out in Regulation 22.
Relevant authorities must ensure that each contract awarded contains provisions enabling its termination by the relevant authority if:
- the contract has been subject to modifications that are not permitted under the regime (see contract modifications) without following a new provider selection process
- the provider, at the time of the contract award, should have been excluded from the procurement process in line with the exclusion criteria set out in Regulation 20 or 20A
The provisions allowing the termination of a contract may address how such terminations would take place (for example, by setting out a notice for terminations and by addressing any consequential matters that may arise from that termination). If the contract does not contain specific provisions allowing the relevant authority to terminate on the grounds specified above, there is an implied term of any contract awarded under the PSR that the relevant authority may do so by giving reasonable notice.
Due diligence
When applying this regime, relevant authorities are expected to undertake reasonable and proportionate due diligence on providers. They are expected to consider whether the organisation(s) they enter into a contract with have the legal and financial capacities and the technical and professional abilities to deliver the contract.
Basic selection criteria
The basic selection criteria are set out in Regulation 19 and in Schedule 16.
For direct award process C, the most suitable provider process and the competitive process (including when establishing a framework agreement), relevant authorities must assess if providers are considered suitable to provide a service by applying the basic selection criteria as outlined in Schedule 16. Relevant authorities are not expected to use the Crown Commercial Services Standard Selection Questionnaire (SSQ); however, all basic selection criteria requirements must be related and proportionate to the subject of the contract or framework agreement.
The basic selection criteria may relate to the provider’s:
- suitability to pursue a particular activity. Where a provider is required to possess a particular authorisation or be a member of a particular organisation to perform the required services in the contract, the relevant authority may require the provider to prove that it holds such authorisation or membership
- economic and financial standing. The relevant authority may impose requirements ensuring that the provider possesses the necessary economic and financial capacity to deliver the contract
- technical and professional ability. The relevant authority may impose requirements ensuring that the provider possesses the necessary human and technical resources and experience to deliver the contract to an appropriate quality standard
Relevant authorities are not required to apply the basic selection criteria when following direct award processes A or B, or when awarding a contract based on a framework agreement.
The rules on provider exclusions are set out in Regulation 20 to 20C. Reporting of excluded providers to the debarment list is set out in Regulation 20D.
- Regulation 20 and 20A set out the provisions determining when a provider or a subcontractor must be excluded, as well as situations where a provider or a sub-contractor may be deemed excludable.
- Unless Regulation 20(1A) applies, relevant authorities must not award a contract to an excluded provider or select an excluded provider to be party to a framework agreement, and must exclude a provider from any of the PSR processes, if the provider or their subcontractor meets the exclusion criteria detailed in Regulation 20 and 20A. A provider may offer evidence that it has taken measures to demonstrate its reliability despite meeting a criterion for exclusion; if the relevant authority considers these measures to be sufficient, they must not exclude the provider. If the relevant authority does not consider the measures to be sufficient, they must respond to the provider with a statement of the reasons for this decision.
- If a provider or a subcontractor is excludable, the provider or subcontractor may be excluded by a relevant authority.
- On an exceptional basis, relevant authorities may award a contract to a provider that is excluded where there is no other choice of provider and there are overriding reasons relating to the public interest, including public health.
- Where a provider wishes to use an excluded provider as a subcontractor for some or all of the services in a procurement, the relevant authority must exclude the provider and the subcontractor from the procurement. Before excluding the provider, unless the exclusion is for reasons of a threat to national security, the relevant authority must inform the provider that it plans to exclude it and give the provider an opportunity to identify an alternative subcontractor. Where there are national security concerns, the relevant authority must seek agreement from the National Security Unit for Procurement prior to excluding the provider.
- Relevant authorities must report certain exclusions to the Procurement Review Unit which will consider whether to add the provider to the debarment list. This is where both:
- a provider is excluded from a procurement on the grounds that they are an excluded provider
- the relevant authority considers that the circumstances giving rise to this exclusion will continue
Key criteria
Five key criteria must be considered when making decisions about provider selection under direct award process C, the most suitable provider process and the competitive process. These criteria are:
- quality and innovation
- value
- integration, collaboration and service sustainability
- improving access, reducing health inequalities and facilitating choice
- social value
Application of key criteria
Relevant authorities must be able to justify their decisions in relation to the key criteria when following a provider selection process and keep a record of this (see record keeping).
Relevant authorities are expected to be aware of wider requirements or duties when considering procurement decisions. These include equalities duties in the Equality Act 2010, including the Public Sector Equality Duty, which are relevant to all criteria and due regard to these requirements must be given when considering each criterion.
How relevant authorities assess providers against the key criteria, including what evidence they consider, may vary according to the service they want to procure. The regime does not specify how relevant authorities must balance the key criteria. No key criteria are expected to be discounted, and relevant authorities should consider the weightings and their consequences against how the service will be delivered before beginning a provider selection process. A relevant authority may wish to address specific priorities; these are expected to be described as part of the key criteria and can be considered when deciding the relative importance of the key criteria.
Criterion 1: Quality and innovation
This addresses the need to ensure good quality services and to support the potential for the development of new – or significantly improved – services or processes that strengthen healthcare or health outcomes.
Quality
The NHS National Quality Board defines high quality healthcare as care that is:
- Safe: delivered in a way that minimises things going wrong and maximises things going right; continuously reduces risk, empowers, supports and enables people to make safe choices and protects people from harm, neglect, abuse and breaches of their human rights.
- Effective: informed by consistent and up-to-date high-quality training, guidelines and evidence; designed to improve the health and wellbeing of a population and address inequalities through prevention and by addressing the wider determinants of health; delivered in a way that enables continuous quality improvements based on research, evidence, benchmarking and clinical audit.
- Provides a positive experience:
- Responsive and personalised: shaped by what matters to people, their preferences and strengths; empowers people to make informed decisions and design their own care; co-ordinated; inclusive and equitable.
- Caring: delivered with compassion, dignity, and mutual respect.
- Well-led: driven by collective and compassionate leadership, which champions a shared vision, values and learning; delivered by accountable organisations and systems with proportionate governance; driven by continual promotion of a just and inclusive culture, allowing organisations to learn rather than blame.
- Sustainably resourced: focused on delivering optimum outcomes within financial envelopes, reduces impact on public health and the environment.
- Equitable: everybody should have access to high quality care and outcomes, and those working in systems must be committed to understanding and reducing variation and inequalities.
Relevant authorities are advised to consider relevant local and national information on the quality of the service provided, where available.
Relevant authorities are advised to consider the extent to which the desired outcomes in terms of quality will be maintained or improved because of the provider or arrangements being considered.
Where a new or innovative service is being considered and no data on quality is available, relevant authorities are advised to weigh the potential value of the innovation or new service against the risk that the service does not deliver the anticipated quality, and understand how performance will be assessed, risks managed and the service evaluated.
The selection process for any new or innovative service provider should include an assessment of how the service will provide information or data on the quality of service provision and monitor safety of operations (given it will not be able to rely on existing methods or indicators).
Relevant authorities are advised to consider the provider’s willingness or ability to identify, monitor and mitigate risks on an ongoing basis, engage with clinical governance processes and involve service users in service planning and oversight.
Assessing the evidence on quality and innovation
Assessing the quality of a provider’s services is complex and requires a good understanding of the context in which those services are to be provided. It also requires an understanding of which evidence sources are available as well as which best provide evidence in relation to the provider in question.
Sources of information may include but are not limited to:
- provider service model
- all recent regulator inspection reports, including any issues related to quality they describe, overall quality ratings and data on innovation adoption (for example, inspection reports from the CQC or General Pharmaceutical Council)
- CQC insight
- NHS England’s new NHS Oversight and Assessment Framework metrics at provider level
- Model Health System data
- where commissioning a specialised service, all national clinical audits or outcome reviews relevant to that service (see Healthcare Quality Improvement Partnership)
- contract management data
- key performance indicator (KPI) data, including data on equalities and health inequalities
- commissioner and lead provider satisfaction with quality delivered in previous contracts or subcontracts (where applicable)
- evidence that patients and unpaid carers with relevant lived experience are engaged as partners in improving experience and quality
- feedback about service delivery from patients and unpaid carers, including survey results, and action being taken in response
- data relating to the uptake of proven innovation
- progress reports on adopting innovative products
Innovation
Relevant authorities must ensure they assess the extent to which an arrangement with a provider may generate and maximise the promotion and adoption of proven innovations in care delivery.
When assessing innovation, relevant authorities are advised to give due consideration to any particular innovative approaches offered by providers that may help deliver better health outcomes.
Relevant authorities are expected to consider how their decisions may improve or limit the longer-term ability of the NHS to continue to innovate and meet health needs. They are expected to take into account whether an arrangement with a provider may stifle the development and adoption of innovations, and how their decisions may affect the ability of the provider market to support access to, or the development of, new or innovative services for patients in future.
Relevant authorities are expected to:
- consider how their decisions may improve or exacerbate inequalities in access to, experience of or outcomes from healthcare services
- operate with a view to securing quality improvement of services in connection with the prevention, diagnosis and treatment of illness
- consider when entering into an agreement with a provider the impact on reducing inequalities in the accessibility of healthcare services, and the quality of outcomes achieved for all eligible persons through the provision of healthcare services
Relevant authorities are advised to consider providers’ ability and willingness to engage with and undertake health research, and to make arrangements that promote and support clinical research and use of research evidence on matters relevant to the health service.
Duties related to quality and innovation
Section 14Z34 of the 2006 Act (as amended) places a duty on ICBs to exercise functions with a view to securing continuous improvement in service quality. ICBs must in particular act with a view to securing continuous improvement in the outcomes achieved from the provision of services. The relevant outcomes include the effectiveness of the services; the safety of the services; and the quality of the experience for patients.
Section 14Z39 places a duty on ICBs to promote innovation in the provision of health services (including innovation in the arrangements made for their provision).
Section 14Z40 places a duty on ICBs to facilitate or otherwise promote research on matters relevant to the health service and the health service’s use of evidence obtained from research.
Criterion 2: Value
This refers to the need to achieve good value in terms of the balance of costs, overall benefits and the financial implications of a proposed contracting arrangement. Relevant authorities must give due consideration to this need.
When assessing the value of a service or arrangement with a provider, relevant authorities are expected to consider:
- the benefits of the arrangement with a provider. Benefits may be evaluated in relation to the other criteria in the regime and may relate to patients (in terms of outcomes or experience), the population (in terms of improved health and wellbeing) and to taxpayers (by reducing the cost burden of ill-health over the whole life of the arrangement within the resources available)
- the costs (or likely costs) of the arrangement, including but not limited to the efficiency of the service, the cost over the length of contract, value for money, the historical market valuation of certain services and any benchmarking of costs against other similar services
- any relevant local/national financial goals
When judging value, relevant authorities are expected to consider both the costs and the benefits of an arrangement with a provider over the expected contractual term, including fluctuations in external trends and the potential variation of the value of the service over the length of the contract.
Relevant authorities are advised to consider whether a particular arrangement with a provider may positively or negatively impact the costs or benefits of other related services, or other commissioning priorities.
Relevant authorities are advised to consider the costs to the provider of changing existing arrangements or establishing new ones, alongside the anticipated cost of the contract itself, when assessing value. For example, arranging a service with a new provider may offer a financial saving to the relevant authority over a relatively long contract duration, but if the anticipated cost of switching to a new provider, including any start-up funding required, outweighs the savings the new provider offers, then consideration needs to be given as to whether such an arrangement is still in the best interests of taxpayers.
Relevant authorities may:
- use published data (such as that from the Spend Comparison Service and the Model Health System, which draws on data from trusts’ patient-level costing systems) to benchmark costs
- ask providers for the information needed to establish the value they offer (for example, a cost breakdown)
- use the competitive process to establish the value available providers offer (see the competitive process)
Duties related to value
Section 223M of the 2006 Act (as amended) places a duty on each ICB and its partner NHS trusts and NHS foundation trusts to exercise their functions with a view to ensuring that, in each financial year, they do not exceed the capital and revenue resource limits set by NHS England.
Section 223C places a duty on NHS England to exercise its functions with a view to ensuring that the expenditure incurred by NHS England and ICBs in a financial year (taken together) does not exceed the aggregate of any sums they receive in a financial year. Section 223D places a duty on NHS England to exercise its functions with a view to ensuring that, in respect of each financial year, relevant NHS bodies (NHS England, ICBs, NHS trusts and foundation trusts) do not exceed the total capital and total revenue resource limits set by the Secretary of State.
The triple aim duty – which applies to NHS England, ICBs, NHS trusts and NHS foundation trusts through the 2006 Act (as amended) – obliges those bodies to have regard to all likely effects of their decisions in relation to matters, including “efficiency and sustainability in relation to the use of resources by relevant bodies for the purposes of the health service in England”’.
Paragraph 2(1) of Schedule 5 of the 2006 Act places a duty on NHS trusts to break even “taking one financial year with another”; defined in statutory guidance as expenditure being covered by income over a 3-year period.
Section 63 of the 2006 Act obliges NHS foundation trusts to exercise functions “effectively, efficiently and economically”.
Criterion 3: Integration, collaboration and service sustainability
This is the extent to which services can improve health outcomes by being provided in:
- an integrated way (including with other healthcare services, health-related services or social care services)
- a collaborative way (including with providers and with persons providing health-related services or social care services)
- a sustainable way (which includes the stability of good quality healthcare services or service continuity of healthcare services)
Integration and collaboration
Relevant authorities must consider the extent to which the services can be provided in an integrated and collaborative way – including with other healthcare services, health-related services or social care services, and their providers.
Relevant authorities are advised to ensure that their decisions are consistent with local and national plans around integrating care and joining up services for patients.
When assessing this criterion, relevant authorities are expected to consider the extent to which the provider under consideration will be able to integrate with other related services in a way that improves care (recognising that integrating services does not necessarily mean all those services have to be delivered by the same provider).
What are integrated services?
Integrated services are services delivered in a seamless and co-ordinated way, viewed from the patient’s perspective, regardless of whether they are provided by different professionals within an organisation or different organisations altogether.
Services may be integrated over different geographical footprints (for example, neighbourhood, place or system level).
Relevant authorities are expected to consider whether a decision may improve or adversely impact the care pathways and patient journeys of other related services as well as the service being considered, and seek to avoid unnecessary disruption or fragmentation of services where possible.
Relevant authorities are expected to consider whether integration may:
- improve the quality of those services (including the outcomes from their provision)
- reduce inequalities between persons with respect to their ability to access those services
- reduce inequalities in outcomes from the provision of those services
Relevant authorities are advised to also consider the extent to which a provider is willing and able to be involved in existing integrated care plans and joint working approaches locally. For example, if a provider can clearly demonstrate that the services it provides will sufficiently integrate into the existing infrastructure and patient pathway, but at a cost slightly higher than by others, an argument may be made for still pursuing delivery by that provider due to the additional benefits outweighing the additional costs.
When considering the potential benefits of joined-up working, relevant authorities are advised to consider any existing relationships between the providers under consideration and connected organisations, and whether these are likely to improve sufficiently to lead to tangible benefits for patients and service users.
Relevant authorities are expected to consider:
- whether the flow of patient data will be improved or impeded by the decision
- whether the respective working practices, culture, infrastructure and systems of the providers involved across linked services are likely to enable better integration
- the location of services proposed by providers and whether this may impact on the providers’ ability to integrate
Duties related to integration and collaboration
The triple aim duty – which applies to NHS England, ICBs, NHS trusts and foundation trusts through the 2006 Act (as amended) – obliges those bodies to consider the effects of their decisions on: the health and wellbeing of the people of England; the quality of services provided by both themselves and other relevant bodies; and the sustainable and efficient use of resources by both themselves and other relevant bodies.
Section 14Z42 of the 2006 Act (as amended) places a duty on ICBs to promote integration, where the ICB considers this would improve service quality (including outcomes) or reduce inequalities with respect to patients’ ability to access services or the outcomes achieved for them; s13N places the same duty on NHS England.
Service sustainability
Relevant authorities must consider whether and how the decisions they make about which providers should provide services might impact on the stability and sustainability of the NHS locally.
When assessing service sustainability, relevant authorities are expected to consider several factors, including but not limited to the:
- financial impact on other services
- impacts on continuity of other related services
- potential impact on quality of other related or dependent services (including those arranged by other bodies)
- stability and sustainability of other providers in the short, medium and long term
- impact on the ability of the wider market to provide required services in the future
Relevant authorities are expected to consider whether and how the decisions they make about which providers should provide services might have a sustained and material impact on the local healthcare workforce, including but not limited to:
- the retention of a skilled local workforce
- the ongoing availability of relevant training opportunities for the local workforce (for example, apprenticeships, training structures, clinical placements)
- the impact on well-established teams
- whether the models of employment used by providers are consistent with current NHS workforce policy priorities
Relevant authorities are expected to avoid destabilising providers through their decision-making. If the proposals are likely to have a negative impact on the stability, viability or quality of other good quality services immediately or over time, relevant authorities are advised to consider whether this is justified by the wider benefits of the proposal.
Criterion 4: Improving access, reducing health inequalities and facilitating choice
This concerns ensuring accessibility to services and treatments for all eligible patients, improving health inequalities and ensuring that patients have choice in respect of their healthcare.
Improving access
Relevant authorities must consider the extent to which a particular arrangement with a provider furthers the pledges set out in the NHS Constitution in relation to patient and public rights, including to:
- access NHS services and not be refused access on unreasonable grounds
- expect the NHS to assess the health requirements of the local community and to arrange and put in place the services to meet those needs as considered necessary, and in the case of public health services arranged by local authorities, to take steps to improve the health of the local community
- not be unlawfully discriminated against in the provision of NHS services, including on grounds of gender, race, disability, age, sexual orientation, religion, belief, gender reassignment, pregnancy and maternity or marital or civil partnership status
Relevant authorities are expected to consider the extent to which the arrangements with a provider may support local population health needs, and ensure services are as easy to access as possible for all patient groups.
Relevant authorities are advised to consider how providers may best be able to:
- meet needs of local groups who experience poorer than average access
- improve the access to services and patient experience and outcomes for deprived and vulnerable groups and groups with protected characteristics
- relate to and understand the populations they are seeking to serve
- expand access to services via their delivery models
- address digital exclusion
- provide services at locations accessible for patients
Reducing health inequalities and disparities
Tackling inequalities in outcomes, experience and access is one of the 4 aims of ICSs. The legal duty in relation to health inequalities requires ICBs to have due regard to the need to reduce inequalities between persons in access to health services and the outcomes achieved, including for patient experience.
Relevant authorities are expected to consider how the arrangement with a provider will impact on health inequalities, and in arranging services seek to reduce health inequalities and disparities. For example, some population groups may require additional support to exercise choice and this support is expected to be proactively offered and provided.
What are health inequalities?
Health inequalities are unfair and avoidable differences in health across the population, and between different groups within society. These include how long people are likely to live, the health conditions they may experience and the care that is available to them. They arise because of the conditions in which we are born, grow, live, work and age. These conditions influence how we think, feel and act, and can impact on both our physical and mental health and wellbeing. Within this wider context, healthcare inequalities are about the access people have to health services and their experience and outcomes.
The wider determinants of health are often interlinked and include but are not limited to:
- socio-economic status and deprivation – for example, unemployed, low income, people living in deprived areas (such as poor housing, poor education or unemployment)
- protected characteristics: age, disability, gender reassignment, marriage or civil partnership, pregnancy and maternity, race, religion or belief, sex and sexual orientation
- vulnerable groups or ‘inclusion health’ groups – for example, vulnerable migrants; Gypsy, Roma and traveller communities; rough sleepers and homeless people; and sex workers
- geography – for example, urban, rural
Duties related to reducing health inequalities and disparities
Section 14Z35 of the 2006 Act (as amended) places a duty on ICBs to have regard to the need to reduce inequalities between persons in access to health services, experience and outcomes.
The triple aim duties on NHS England, ICBs, NHS trusts and NHS foundation trusts includes a need to have regard to the effects of a decision in relation to health inequalities, and inequalities in the benefits individuals can obtain from health services.
The Public Sector Equality Duty (s149) and the wider obligations in the Equality Act 2010 require public authorities, in the exercise of their functions, to have due regard to the need to eliminate discrimination, harassment and victimisation, and to advance equality of opportunity and foster good relations between those with a relevant protected characteristic and those who do not share it.
Facilitating choice
When assessing potential providers against this criterion, relevant authorities must consider the extent to which the arrangements with a provider may impact on patient choice of provider and about their treatment and personalisation of care. Relevant authorities must not limit choice where patients have a legal right to choose the provider of their first outpatient appointment from any clinically appropriate provider in England that is contracted to work with the NHS.
Different types of choice are available to patients:
- legal right to choice of provider and team of elective services led by a consultant or mental healthcare professional
- choice of provider for other non-consultant led elective services where commissioners have decided to offer choice of provider (for example, where commissioners have established a list of providers that patients can choose from)
- choice about treatment and the personalisation of care
Relevant authorities are expected to:
- consider the extent to which a particular decision may expand or reduce the choice of providers available to patients
- consider that some population groups may require additional support to exercise choice
- proactively offer and provide any additional support, as required
For services where there is no legal right to choice and there is risk that the relevant authority’s plans may limit the services and treatments that patients can choose from, the relevant authority is expected to consider whether this risk is sufficiently offset by the wider benefits of its proposal, and whether other forms of choice may be included in the arrangement (for example, choice of treatment).
Relevant authorities are advised to consider the range of options a provider can offer for the services, treatments and modes of access they provide, and how well these match the needs and wishes of the population (including the needs of different subgroups or populations).
Relevant authorities should consider where giving patients a choice of provider would benefit all patients by enabling them to access services that best meet their needs (where this is not already a legal requirement) – for example, by establishing a list of providers that patients can choose from.
Criterion 5: Social value
This is whether a proposed contracting arrangement might improve economic, social and environmental wellbeing in the relevant geographical area.
Relevant authorities must seek to ensure that their decisions about which providers should provide services will contribute to improvements in social, economic and environmental conditions aligned to local priorities.
In assessing social value, relevant authorities are expected to think about how the arrangements with providers under consideration impact on:
- environmental issues and sustainable development, including addressing climate change, making and meeting commitments around reducing emissions, air pollution, consumption and waste, through promoting circular economy principles as well as enhancing the natural and built environment, as applicable
- inclusive and ‘good’ employment that increases equality of opportunity in the workplace and supports a diverse workforce, designs in equity, provides fair terms and conditions and supports staff wellbeing, physical and mental health, supports opportunities for local people or population groups experiencing health or other inequalities, and eliminates modern slavery
- local inclusive and sustainable economies that decrease economic inequality and poverty, including through employment as an economic and health intervention and payment of a living wage
- community cohesion and the wider health and wellbeing of the population, including by helping communities to manage and recover from the impact of COVID-19
- social determinants of health (for example, employment, income, housing, local environment, food, transport, community, safety)
Relevant authorities are advised to consider the extent to which providers have themselves acted to increase social value, and how social value improvements can improvements health outcomes.
Relevant authorities are advised to consider social value in relation to the other criteria in this regime. For example:
- a better integrated service that leads to fewer patient journeys may also enable environmental gains to be made
- a service that leads to improved air quality may contribute to better health outcomes over time and hence savings
Relevant authorities are advised to consider how a provider’s policies and practices align with:
- moving towards net zero and delivering social value in the procurement of goods and services
- increasing the impact of organisations providing health services as anchor institutions, particularly in their role as significant local employers, and partners in place
- supporting broader social, environmental and economic development
- eliminating modern slavery in the supply chain; providers should conduct due diligence on their own supply chains, identify any risk of abuse of labour standards and put in place mitigation to reduce this risk
Relevant authorities are expected not to make arrangements with providers that stifle the potential for development and adoption of sustainability within the services or may not be able to support the development of new or sustainable services for patients in the future.
Relevant authorities are advised to be aware of other requirements and duties not set out in legislation.
Duties and guidance related to social value
- Social Value Model
- Delivering a Net Zero National Health Service
- NHS net zero supplier roadmap
- NHS England guidance on Applying net zero and social value in the procurement of NHS goods and services
- The Health and Care Act 2022 places a duty on NHS organisations to have regard to compliance with the net zero emission target and adapt to the impacts of climate change
Balancing the key criteria
The relative importance of the key criteria is not predetermined by the Regulations or this guidance and there is no prescribed hierarchy or weighting for each criterion. Relevant authorities must decide their relative importance for each decision they make under this regime, based on the proposed contracting arrangements and what they are seeking to achieve from them ort he services, including for scenarios where a particular criterion is ‘pass or fail’ or certain key criteria are equally important. Relevant authorities are expected to use information and evidence from a range of sources, as well as their knowledge and experience of working with providers. They can ask providers for further information to assist with this assessment if they wish. When following the competitive process, relevant authorities must only use the information given in the bid to assess the bid.
Relevant authorities are expected to be aware of wider requirements or statutory duties when considering procurement decisions. The flexibilities offered by the regime do not mean that relevant authorities are exempt from complying with their other obligations.
For provider selection processes with higher contract values, it is advised that greater focus is given to value for money and the quality and efficiency of the services to be provided, unless this means the service does not best meet the needs of the population it is serving.
Relevant authorities may state in their tender documents that a provider’s wilful misrepresentation of a bid will result in its exclusion from the provider selection process.
Relevant authorities must justify and record how they have ranked the importance of the key criteria for the service they are arranging (see record keeping).
Reviewing decisions during the standstill period
The standstill period requirements, including for review of decisions, are detailed in Regulations 12 and 14(3). Provision for independent expert advice is set out in Regulation 23, including how the Independent Patient Choice and Procurement Panel may provide advice during the standstill period (see the section below on the Independent Patient Choice and Procurement Panel).
See in PSR toolkit: Reviewing decisions during the standstill period flowchart
The standstill period must be observed once a notice of intention to make an award to a provider under direct award process C, the most suitable provider process or the competitive process has been published. This includes when concluding a framework agreement or awarding a contract based on a framework agreement following a mini-competition.
Calculating the standstill period
The standstill period follows a decision to select a provider and must end before the contract can be awarded. It gives time for any provider that might otherwise have been a provider of the services to which the contract relates to make representations; and for relevant authorities to consider those representations and respond as appropriate. See the section below on receiving representations for further details.
The standstill period must last for a minimum period of eight working days and begins on the day after the notice of intention to award or conclude is published (this can occur on a non working day) and, unless a written representation is made, ends at midnight of the eighth working day after the day the standstill period begins (see worked examples below).
The standstill period will end at midnight on the 8th working day after the day the standstill period begins if:
- no representations are received by midnight on the 8th working day; or
- representations do not meet the required conditions (set out below)
Where representations meeting the required conditions are received, the standstill period continues until the relevant authority:
- completes its review
- communicates its further decision (with reasons) to the provider(s) that submitted the representations and the provider to which it intended at the beginning of the standstill period to award the contract to
- concludes it is ready to award the contract or that it wishes to return to an earlier step in the process or abandon the process
The end of the standstill period must be at least five working days after the relevant authority has communicated its decision to the provider. The minimum five working days’ notice allows for providers that remain unsatisfied about the response given by a relevant authority to their representations to seek the involvement of the Independent Patient Choice and Procurement Panel (see Independent Patient Choice and Procurement Panel. Where the relevant authority’s decision is to award the contract (rather than return to an earlier step in the process or abandon the process), the standstill period should end when there has been at least five working days since the relevant authority communicated its further decision. Other providers cannot use this time to make their own representations. Where within 5 working days of receiving the relevant authority’s further decision, a provider requests an independent review from the Independent Patient Choice and Procurement Panel, the standstill period should continue, other than in exceptional circumstances.
If the Independent Patient Choice and Procurement Panel accepts the request, the standstill period should not end until the relevant authority makes a further decision having considered the advice provided by the panel. The relevant authority must again give at least 5 working days’ notice of its further decision before the standstill period can end and the relevant authority takes forward its further decision.
The standstill period must end before a contract is awarded and confirmation of the decision is published (or before returning to an earlier step in the process or abandoning a process). The transition of services must only take place after the standstill period has ended and the contract has been awarded.
Receiving representations
The purpose of making a representation is to seek a review of the decision made, to determine whether a relevant authority has applied the regime correctly and made an appropriate provider selection decision.
Relevant authorities are only obliged, to respond to representations that meet all the following conditions, however they may choose to respond if they wish:
- The representation is received within the first 8 working days following the start of the standstill period
- the representation comes from a provider that might otherwise have been a provider of the services to which the contract relates
- the provider is aggrieved by the decision of the relevant authority
- the provider believes that the relevant authority has failed to apply the regime correctly and sets out reasonable grounds to support its belief
- the representation is submitted in writing (which includes electronically) to the relevant authority within eight working days of the start of the standstill period.
When awarding a contract based on a framework agreement, only providers that were party to the framework agreement and then either excluded from or unsuccessful in the call off from the framework may make a representation to the relevant authority.
Relevant authorities must follow the relevant transparency requirements for the approach they take and must keep internal records of their decision-making (see transparency).
Example of calculating the minimum length of the standstill period during which representations can be made
Example A
The intention to award a contract notice is published on Thursday 11 January 2024. The standstill period begins the following day. Representations can be made for up to eight working days after the day the standstill period begins. Therefore, the standstill period would end at midnight on Wednesday 24 January 2024.
Example B
The intention to award a contract notice is published on Friday 12 January 2024. The standstill period begins the following day. Representations can be made for up to eight working days after the day the standstill period begins. Therefore, the standstill period would end at midnight on Wednesday 24 January 2024.
Example C
The intention to award a contract notice is published on Tuesday 16 January 2024. The standstill period begins the following day. Representations can be made for up to eight working days after the day the standstill period begins. Therefore, the standstill period would end at midnight on Monday 29 January 2024.
Considering representations
Relevant authorities should ensure that appropriate internal governance mechanisms are in place to deal with representations made against provider selection decisions. To this end, relevant authorities should, where possible, ensure that decisions are reviewed by individuals not involved in the original decision. Where this is not possible, relevant authorities should ensure that at least one individual not involved in the original decision is included in the review process.
If the relevant authority is considering representations on the same issue from multiple providers, it may consider these together if appropriate.
Where a representation is received within the eight working days, the relevant authority:
1. Must ensure that the provider is afforded an opportunity to explain or clarify its representation(s) if these are not clear.
2. Is expected to provide an indicative timeframe for when the representation might be considered by, and when the provider might reasonably expect a decision to be made.
3. Must provide any information requested by the provider that the relevant authority is required to keep under the regime (see record keeping) as soon as possible, except where this:
- would prejudice the legitimate commercial interests of any person, including the relevant authority
- might prejudice fair competition between providers
- would otherwise be contrary to the public interest.
4. Must review the evidence and information used to make the original decision, taking into account the representations made.
5. Must consider whether the representation has merit (e.g., it identifies that the process has not been correctly followed or brings to light information that has a bearing on the decision reached).
The provider that made the representations is expected to respond promptly and concisely to questions from the relevant authority about the points it has made, and if it cannot respond within a reasonable timeframe then it is expected to provide a justification.
We expect the relevant authority to allow sufficient time and opportunity for the provider that made the representations to respond to questions from the relevant authority. In the event that the provider fails to respond/communicate, then it is for the relevant authority to decide whether to complete its assessment of the representations and communicate their decision to the provider.
Outcome of representations
Where the relevant authority finds that a representation has merit (e.g., it identifies that the process has not been followed correctly or brings to light information that has a bearing on the decision reached), it must further consider whether this impacts on the intention to award a contract to the selected provider. It must then decide whether to:
- enter into a contract or conclude the framework agreement as intended
- go back to an earlier step in the selection process, either to the start of the process or to where a flaw was identified, rectify this, and repeat that step and subsequent steps (see repeating a step)
- abandon the provider selection process (see abandoning a process).
The relevant authority must communicate the decision described above promptly and in writing, to:
- the provider that made the representation
- the provider to which the relevant authority intended at the beginning of the standstill period to award the contract, or all providers with which the relevant authority intended at the beginning of the standstill period to conclude the framework agreement.
The standstill period can only end once the relevant authority has reviewed its decision, shared its conclusion (in writing) with the relevant providers, and concluded that it is ready to award the contract, or that it’s going to return to an earlier step in the process, or abandon the process.
The relevant authority must allow at least five working days following the day on which they sent their response to the provider, before the standstill period comes to an end. This time allows the provider to consider the response of the relevant authority, seek further clarifications, and to consider whether to request a further review by the Independent Patient Choice and Procurement Panel. This time also allows the relevant authority to reconsider their decision and make any subsequent decisions if necessary. The relevant authority must communicate any such further decision in writing to the provider (as outlined above).
If a panel review is requested and accepted, then the standstill period would usually continue until after the Independent Patient Choice and Procurement Panel has given its advice and relevant authority has made its further decision in light of that advice.
Independent Patient Choice and Procurement Panel
NHS England has established the Independent Patient Choice and Procurement Panel to provide independent expert advice to relevant authorities with respect to the review of PSR decisions during the standstill period, and separately to support reviewing decisions with respect to the application of the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012 (as amended).
The panel may consider whether the relevant authority complied with the Regulations and may provide advice to the relevant authority. The relevant authority should then make a further decision about how to proceed.
Further detail on how the Independent Patient Choice and Procurement Panel operates, their acceptance criteria and published findings can be found on the Independent Patient Choice and Procurement Panel website.
Urgent contract modifications during the standstill period
Where the relevant authority is awaiting the advice of the panel during the standstill period, the relevant authority may urgently modify the existing contract in accordance with Regulation 14(3), subject to all the below applying:
- there is an existing contract for the healthcare services to which the proposed contracting arrangement relates, and the relevant authority considers that the term of the existing contract is likely to expire before the end of the standstill period
- the relevant authority considers it necessary or expedient to modify the existing contract prior to the new contract taking effect in order to ensure continuity between the existing contract and proposed award of a new contract
- the relevant authority considers that it is not possible to satisfy the requirements of Regulations 6 to 13 before the term of the existing contract expires
The relevant authority may only extend the length of the existing contract and must not otherwise modify the contract. The relevant authority is expected to only extend the contract for as long as necessary to ensure continuity between the existing and the new contract.
Outcome of panel review
Once the relevant authority has considered the advice of the panel, it may make a further decision, to be its final decision, replacing the previous one, to either:
- enter into a contract or conclude the framework agreement as intended
- go back to the start of the selection process or to the step where a flaw was identified, and repeat that step and subsequent steps (see repeating a step in a provider selection process), or
- abandon the procurement (see abandoning a provider selection process).
The relevant authority must share this further decision promptly, in writing, and with reasons, with the provider who made a representation and the provider to which the relevant authority intended, at the beginning of the standstill period, to award the contract. The relevant authority must set out the outcome and a full and transparent justification for their decision, and it is expected that this will include whether they changed their original decision as a result of the advice of the panel. The relevant authority must wait at least five working days before concluding it is ready to award the contract and bring the standstill period to an end, or before it returns to an earlier step in the process, or before it abandons a process.
In exceptional circumstances, the relevant authority may conclude that it is necessary to enter into a new contract before the panel can complete its review and share its advice. In those circumstances, the relevant authority is expected to note the advice of the panel for the next time they use the PSR to arrange healthcare services.
Annual summary
The annual summary requirements are set out in Regulation 25.
Relevant authorities must publish a summary of their application of the PSR annually online (e.g. via the relevant authority’s annual reports or annual governance statement). We expect the first annual summary to relate to contracts awarded using the PSR between 1 January 2024 – 31 March 2025, and we expect this to be published no later than six months following the end of 2024/2025 financial year. Following the first annual summary, all other annual summaries must be published no later than six months following the end of the financial year it relates to.
This must include, in the year to which the summary relates, the:
- number of contracts directly awarded under direct award processes A, B or C
- number of contracts awarded under the most suitable provider process
- number of contracts awarded under the competitive process
- number of framework agreements concluded
- number of contracts awarded based on a framework agreement
- number of urgent contracts awarded and urgent modifications
- number of new providers awarded contracts
- number of providers who ceased to hold any contracts with the relevant authority
- details of representations received, including:
- the number of representations received in writing and during the standstill period in accordance with Regulation 12(3)
- summary of the outcome of all representations received and of the nature and impact of those representations.
In addition, relevant authorities are expected to publish:
- total number of providers the relevant authority is currently contracted with
- details of any reviews by the Independent Patient Choice and Procurement Panel:
- number of requests for consideration received by the Independent Patient Choice and Procurement Panel
- number of requests accepted and rejected by the Independent Patient Choice and Procurement Panel for consideration
- number of times where the Independent Patient Choice and Procurement Panel advised the relevant authority to re-run or go back to an earlier step in a provider selection process under the PSR, and the number of times the advice was followed.
Monitoring requirements
The monitoring requirements are set out in Regulation 26.
Relevant authorities must monitor their compliance with the Regulations. The results of the monitoring must be published online annually (and may be integrated into other annual reporting requirements) and include processes, decisions made under the PSR, contract modifications, and declaration and management of conflicts of interests. Relevant authorities may use internal auditors to fulfil these requirements.
If a compliance report finds instance(s) of non-compliance, relevant authorities must put in place actions to address this issue and to improve adherence with the regime.
Annex A: Common procurement vocabulary (CPV) codes
The CPV codes adopted by the PSR were defined by Regulation (EC) No 2195/2002 of the European Parliament and of the Council, as amended from time to time. Healthcare services in scope of the regime must fall within one or more of the adopted CPV codes.
The list below of CPV codes corresponds to services covered by the regime. This list must be used by relevant authorities to support decisions around scope. Relevant authorities must use the most specific CPV code they can, rather than an overarching one. For example, where relevant authorities are commissioning cycles for in vitro fertilisation, relevant authorities must use the CPV code for ‘in vitro fertilisation’ rather than one for ‘gynaecologic or obstetric services’. However, as the list of CPV codes does not cover all types of healthcare services, relevant authorities may in some situations use the overarching parent code for ‘health services’ when a more detailed CPV code is not available. If a more detailed CPV code is available, but not included in the list below, then the service is out of scope of the PSR and must be arranged using the Procurement Act or, where transitional arrangements apply, the PCR.
| CPV code | Description |
| 85100000-0 | Health services |
| 85110000-3 | Hospital and related services |
| 85111000-0 | Hospital services |
| 85111100-1 | Surgical hospital services |
85111200-2 | Medical hospital services |
| 85111300-3 | Gynaecological hospital services |
| 85111310-6 | In vitro fertilisation services |
| 85111320-9 | Obstetrical hospital services |
| 85111400-4 | Rehabilitation hospital services |
| 85111500-5 | Psychiatric hospital services |
| 85111600-6 | Orthotic services |
| 85111700-7 | Oxygen-therapy services |
| 85111800-8 | Pathology services |
| 85111810-1 | Blood analysis services |
| 85111820-4 | Bacteriological analysis services |
| 85111900-9 | Hospital dialysis services |
| 85112200-9 | Outpatient care services |
| 85120000-6 | Medical practice and related services |
| 85121000-3 | Medical practice services |
| 85121100-4 | General-practitioner services |
| 85121200-5 | Medical specialist services |
| 85121210-8 | Gynaecologic or obstetric services |
| 85121220-1 | Nephrology or nervous system specialist services |
| 85121230-4 | Cardiology services or pulmonary specialist services |
| 85121231-1 | Cardiology services |
| 85121232-8 | Pulmonary specialists services |
| 85121240-7 | ENT or audiologist services |
| 85121250-0 | Gastroenterologist and geriatric services |
| 85121251-7 | Gastroenterologist services |
| 85121252-4 | Geriatric services |
| 85121270-6 | Psychiatrist or psychologist services |
| 85121271-3 | Home for the psychologically disturbed services |
| 85121280-9 | Ophthalmologist, dermatology or orthopaedics services |
| 85121281-6 | Ophthalmologist services |
| 85121282-3 | Dermatology services |
| 85121283-0 | Orthopaedic services |
| 85121290-2 | Paediatric or urologist services |
| 85121291-9 | Paediatric services |
| 85121292-6 | Urologist services |
| 85121300-6 | Surgical specialist services |
| 85130000-9 | Dental practice and related services |
| 85131000-6 | Dental-practice services |
| 85131100-7 | Orthodontic services |
| 85131110-0 | Orthodontic-surgery services |
| 85140000-2 | Miscellaneous health services |
| 85141000-9 | Services provided by medical personnel |
| 85141100-0 | Services provided by midwives |
| 85141200-1 | Services provided by nurses |
| 85141210-4 | Home medical treatment services |
| 85141211-1 | Dialysis home medical treatment services |
| 85141220-7 | Advisory services provided by nurses |
| 85142000-6 | Paramedical services |
| 85142100-7 | Physiotherapy services |
| 85143000-3 | Ambulance services |
| 85144000-0 | Residential health facilities services |
| 85144100-1 | Residential nursing care services |
| 85145000-7 | Services provided by medical laboratories |
| 85146000-4 | Services provided by blood banks |
| 85146100-5 | Services provided by sperm banks |
| 85146200-6 | Services provided by transplant organ banks |
| 85148000-8 | Medical analysis services |
| 85149000-5 | Pharmacy services, but not including community pharmacy services that are arranged under the National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013 |
| 85150000-5 | Medical imaging services |
| 85160000-8 | Optician services |
| 85323000-9 | Community health services, but only in respect of community health services which are delivered to individuals |
| 85312330-1 | Family-planning services, but only insofar as such services are provided to individuals to support sexual and reproductive health |
| 85312500-4 | Rehabilitation services, but only insofar as such services are provided to individuals to tackle substance misuse or for the rehabilitation of the mental or physical health of individuals |
Annex B: Transparency
See in toolkit: Find a Tender Service supplementary guide
Table 1: Transparency notices that require publication under PSR processes
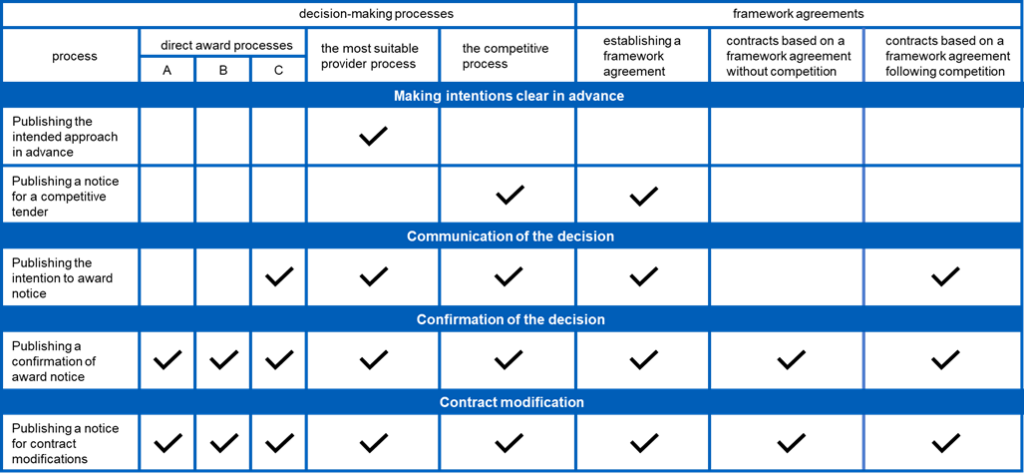
Where, following a particular provider selection process, multiple providers are awarded a contract for the same service, then a single transparency notice – which lists all successful providers – would suffice. The selection process must be the same.
Where relevant authorities come together to commission a service and use a lead authority, it is acceptable for that lead authority to publish transparency notices on behalf of the others. All transparency notices must name the associated relevant authorities.
Transparency notice contents
Intention to follow the most suitable provider process
The content of the intention to follow the most suitable provider process notice is set out in Schedule 5.
After the relevant authority has decided to follow the approach for the most suitable provider process, it must publish its intention to follow this approach. The intention to use this approach is expected to be published using Find a Tender Service websiteas a prior information notice, and this notice must include:
- statement that the relevant authority is intending to follow the most suitable provider process
- contract title and reference
- description of the services intended to be provided, including the most relevant CPV code
- details of individual(s) making the award decision (this may be the name of a committee or job titles of individuals making the decision, where appropriate).
The prior information notice for the most suitable provider process is not expected to include details of which provider(s) are under consideration as suitable providers.
The relevant authority must not proceed to assess providers until at least 14 days after the day on which the notice of intention is submitted for publication, so that providers are aware of the approach the relevant authority is taking to choose a provider.
Inviting Offers (the Competitive Process and when establishing a framework agreement)
The content of the notice inviting bids are detailed in Schedule 8.
When the relevant authority has decided to follow the competitive process (including the establishment of a framework agreement), it must publish a notice that will initiate the competitive tender.
It may also publish a prior information notice (PIN) in advance of the notice of a competitive tender opportunity. If publishing a PIN, relevant authorities are advised to include details of the service required, the proposed contract length and any proposed provision for extension or early termination, and any other matters (known or anticipated) that are likely to be of interest to prospective providers.
The invitation to offer bids in a competitive tender is expected to be published using Find a Tender Service website as a contract notice. The contract notice, or the documents provided in the content of the notice (e.g. tendering documents), must include:
- contract or framework agreement title and reference
- description of services required to be provided, including the most relevant CPV code
- intended or estimated dates between which the services must be provided and the duration of the contract (including potential extensions beyond the initial term) or of the term of the framework agreement
- approximate lifetime value of the contract or framework agreement
- contract or framework award criteria
- where the notice relates to establishing a framework agreement, the relevant authorities that will be able to use the agreement
- instructions on how to submit offers (bids), which must be by electronic means
- explanation of how offers (bids) will be assessed, including whether the assessment will be in stages.
Inviting offers (when awarding a contract based on a framework agreement following the competitive process)
The content of the notice inviting bids are detailed in Schedule 15.
When awarding a contract based on a framework agreement following the competitive process, the relevant authority must invite all providers that are part of the framework agreement to submit an offer (bid). This invitation does not have to be published.
The invitation must include:
- description of the services to which the contract relates, including the most relevant CPV code
- contract award criteria
- intended or estimated dates between which the services must be provided and the duration of the contract (including potential extensions beyond the initial term)
- approximate lifetime contract value.
Communication to unsuccessful providers
The content of communications to unsuccessful providers is set out in Schedule 9.
After having identified the winning bid, relevant authorities must communicate their decision in writing to unsuccessful providers before publishing the intention to award notice. Relevant authorities must provide unsuccessful providers with written information on why their bid was unsuccessful. This must include:
- contract or framework agreement title and reference
- contract or framework award criteria against which bids were evaluated
- reasons why the successful provider was successful (this may include the score of the successful provider)
- reasons why the unsuccessful provider was unsuccessful (this may include the score of the unsuccessful provider)
- start and end dates for the period during which written representations may be made.
We advise that an address to which written complaints should be sent is also provided in the communication (which may be an email address).
Relevant authorities may also choose to give feedback to unsuccessful providers on what they did well and what they could have done to improve their bid.
The publication of the intention to award notice marks the start of the standstill period. When awarding a contract based on a framework agreement, following a mini-competition, only providers that were party to the framework agreement and i) took part in the mini-competition but were unsuccessful, or ii) were excluded from the mini-competition, may make a representation to the relevant authority.
Intention to award notice
The content of the intention to award notice is set out in Schedule 3 for direct award C, Schedule 6 for the Most Suitable Provider process and Schedule 10 for the competitive process.
Where the relevant authority must then publish a notice setting out its intention to award a contract this is expected to be published using FTS as a contract award notice and must include:
- statement that this is an intention to award the contract and which award process has been used
- the dates between which the services are intended to be provided, if known, and for the most suitable provider and competitive processes the details of whether this is a new or existing provider and/or service
- contract title and reference
- name of the provider to which the contract is intended to be awarded and the address of its registered office or principal place of business
- description of the services intended to be provided, including the most relevant CPV code
- approximate lifetime contract value
- details of the individual(s) making the award decision (this may be the name of a committee or job titles of individuals making the decision, where appropriate)
- statement explaining the relevant authority’s reasons for selecting the provider with reference to the key criteria
- any declared or potential conflicts of interest (COIs) of individuals making the decision (not including individual names) and how these were managed.
For framework agreements:
- where the notice relates to establishing a framework agreement, the duration of the agreement and the relevant authorities that will be party to the framework agreement
- Where the notice relates to a contract awarded under a framework agreement the notice should state that this is the case.
Confirmation of award
The content of the contract award notice is set out in Schedule 2 for direct award processes A and B and for contracts based on framework agreements without competition, in Schedule 4 for direct award C, in Schedule 7 for MSP, and in Schedule 10 for the competitive process and framework agreements with competition.
The relevant authority must publish a notice of the award within 30 days of the contract award. The notice of award is expected to be published using the Find a Tender Service (FTS) website, as a contract award notice.
Notices for all award processes must include:
- statement that an award has been made and which PSR process has been used, where urgent circumstances have been used this must include a statement that the circumstances were urgent.
- contract title and reference
- name of the provider to which the contract is to be awarded and the address of its registered office or principal place of business
- description of the services to which the contract relates to, including the most relevant CPV code
- the lifetime value of the contract or, where this is not known, the amounts payable to the provider under the contract
- dates between which the services are to be provided, except for the competitive process
- details of the individual(s) making the award decision (this may be the name of a committee or job titles of individuals making the decision, where appropriate)
- any declared or potential conflicts of interest (COIs) of individuals making the decision (not including individual names) and how these were managed.
Additionally, we expect the notice to also include, except for direct award process C and the most suitable provider process, whether:
- this is a new or existing service
- this is a new or existing provider.
Where the notice relates to establishing a framework agreement:
- the duration of the framework agreement the relevant authorities that will be able to use the agreement
- The lifetime value of the framework agreement
For urgent awards (see schedule 13 of the regulations):
- A justification for the length of the contract if over 12 months
- A justification for the urgent award
Transparency requirements for abandoning a provider selection process
Where relevant authorities are abandoning a provider selection process, the following transparency requirements apply:
- a confirmation of the decision to abandon the provider selection process and not to award a contract.
- The confirmation is expected to be published using FTS as a corrigendum to the last notice published within 30 days of the decision; for example, after the relevant authority publishes its intended approach notice when following the most suitable provider process, or when it cannot or does not wish to award a contract, following representations made during the standstill period.
Transparency requirements for contract or framework agreement modifications
The content of a contract or framework agreement modification notice is detailed in Schedule 12.
Where relevant authorities are making a contract modification permitted under this regime that requires transparency, the requirements below must be observed.
Confirmation of modification
The relevant authority must publish a confirmation of the modification within 30 days of the contract modification. The confirmation of modification is expected to be published using FTS as a modification notice, and must include:
- contract or framework agreement title and reference
- description of the services to which the contract or framework agreement relates, including the most relevant CPV code
- effective date of the modification
- brief description of the modification
- any change in lifetime value of the contract or framework agreement (expressed also as a proportion of the cumulative lifetime value of the contract)
- any change in length of the contract or framework agreement
- details of the individual(s) making the decision (this may be the name of a committee or job titles of individuals making the decision, where appropriate)
- any declared or potential conflicts of interest (COIs) of individuals making the decision (not including individual names) and how these were managed.
Confirmation of modification in urgent circumstances
The content of an urgent modification notice is detailed in Schedule 14.
In urgent circumstances, relevant authorities must publish a confirmation of their decision to make a modification to a contract within 30 days of the contract modification being made (unless the modification is a permitted modification without transparency; see contract modifications). The confirmation of modification is expected to be published using FTS as a modification notice, and must include:
- a statement that in the view of the relevant authority the modification was urgent
- contract title and reference
- description of the services to which the contract relates, including the most relevant CPV code
- effective date of the modification
- nature of the modification, including any change in contract value or length of contract
- details of the individual(s) making the decision (this may be the name of a committee or job titles of individuals making the decision, where appropriate)
- any declared or potential conflicts of interest (COIs) of individuals making the decision (not including individual names) and how these were managed
- justification for why the modification was urgent (i.e. why Regulation 14 was applied).

