Classification: Official
Publication reference: PRN01472
To:
- integrated care boards (ICBs):
- chair
- chief executives
- medical directors
- chief AHPs
- chief nurses
- pharmacy leads
- lead healthcare scientists
- primary care leads
- social care leads
- trusts:
- chair
- chief executives
- medical directors
- chief AHPs
- chief nurses
- chief pharmacists
- lead healthcare scientists
- IPC leads
- all GP practices, dental practices and pharmacies in England
cc:
- regional:
- directors
- directors of primary care and public health
- lead healthcare scientists
Dear colleague,
World AMR Awareness Week (WAAW) 18 to 24 November 2024 – Educate. Advocate. Act now.
Thank you for your ongoing commitment to confronting antimicrobial resistance (AMR). We are writing to invite you to join us in taking urgent action to prevent AMR across all sectors of the healthcare system.
Infection is a common cause of death in the UK population, associated with over 87,000 deaths annually – similar to the number of deaths from ischaemic heart disease. In the UK in 2019, there were 7,600 deaths attributable to AMR and 35,200 deaths associated with AMR (Confronting antimicrobial resistance 2024 to 2029 – GOV.UK).
The additional burden of AMR on the NHS includes increased primary care appointments, hospital admissions, bed occupancy, and length of stay (OECD).
In May 2024, the UK’s second 5-year action plan for AMR was published. This plan sets out ambitions and measures of success to ensure progress towards the UK’s 20-year vision for addressing AMR. Key NAP outcomes and corresponding human health targets are set out in the table below:
AMR National Action Plan 2024-29 strategic outcomes | Human health targets by 2029 |
|---|---|
Renewed focus on infection prevention and management Strengthened surveillance of infections | 1a. Prevent any increase in drug-resistant infections 1b. Prevent any increase in Gram-negative bloodstream infections |
Enhanced public engagement and education Development of the AMR workforce | 2a. Increase UK public and healthcare professionals’ knowledge of AMR |
Improved antimicrobial stewardship and disposal | 4a. Reduce total antibiotic use in human populations by 5% 4b. Achieve 70% of total antibiotic use from the WHO “Access” category |
Addressing health disparities and health inequalities | All human health targets apply |
These outcomes require an integrated approach across healthcare systems. Integrated care boards and their partners should focus on the actions that each of them will take, and how they can most effectively work together to reduce the incidence of infections. Doing this will reduce the need for antibiotics and other antimicrobials, and so reduce the pressure for resistance to develop and spread further.
Infections are the most common reason for emergency department presentations, hospital and intensive care admissions, and death, and continue to increase as a proportion of total activity. It is vital that organisations at all levels, encourage collaboration among those working in infection-related fields and adopt initiatives that optimise infection management. This includes improving community healthcare access for patients with infection symptoms, ensuring clarity of pathways and criteria for services to support the management of infection such as acute infection hubs, and standardising clinical pathways for common infections.
Please share this letter and appendices with your teams and consider, together with your AMR lead, the following immediate actions:
Action 1 – optimise antimicrobial prescribing
- Advocate shorter courses: Support prescribers to prescribe the shortest effective course of antibiotics, following NICE guidelines. Advise patients to complete the course as prescribed, not to save them for later or share them, and return unused antibiotics to community pharmacies for safe disposal. Reducing course length of antimicrobial prescribing is one of 16 national medicines optimisation opportunities for integrated care boards (ICBs). ICB performance reports for course length are available from PrescQIPP, ePACT2 and from the AMR Policy Priority area of NHS Model Health System.
- Promote timely intravenous-to-oral switch of antibiotics: Research confirms timely switching could reduce hospital length-of-stay, release up to 5 million bed days per year in England, release 20 minutes of nursing time per dose avoided, and reduce the NHS’s carbon footprint. Switching intravenous antibiotics to oral is another one of 16 national medicines optimisation opportunities for ICBs. National criteria for IV-to-oral switch for adults and children are now available on the gov.uk website. Your local acute trust performance is visible in Fingertips.
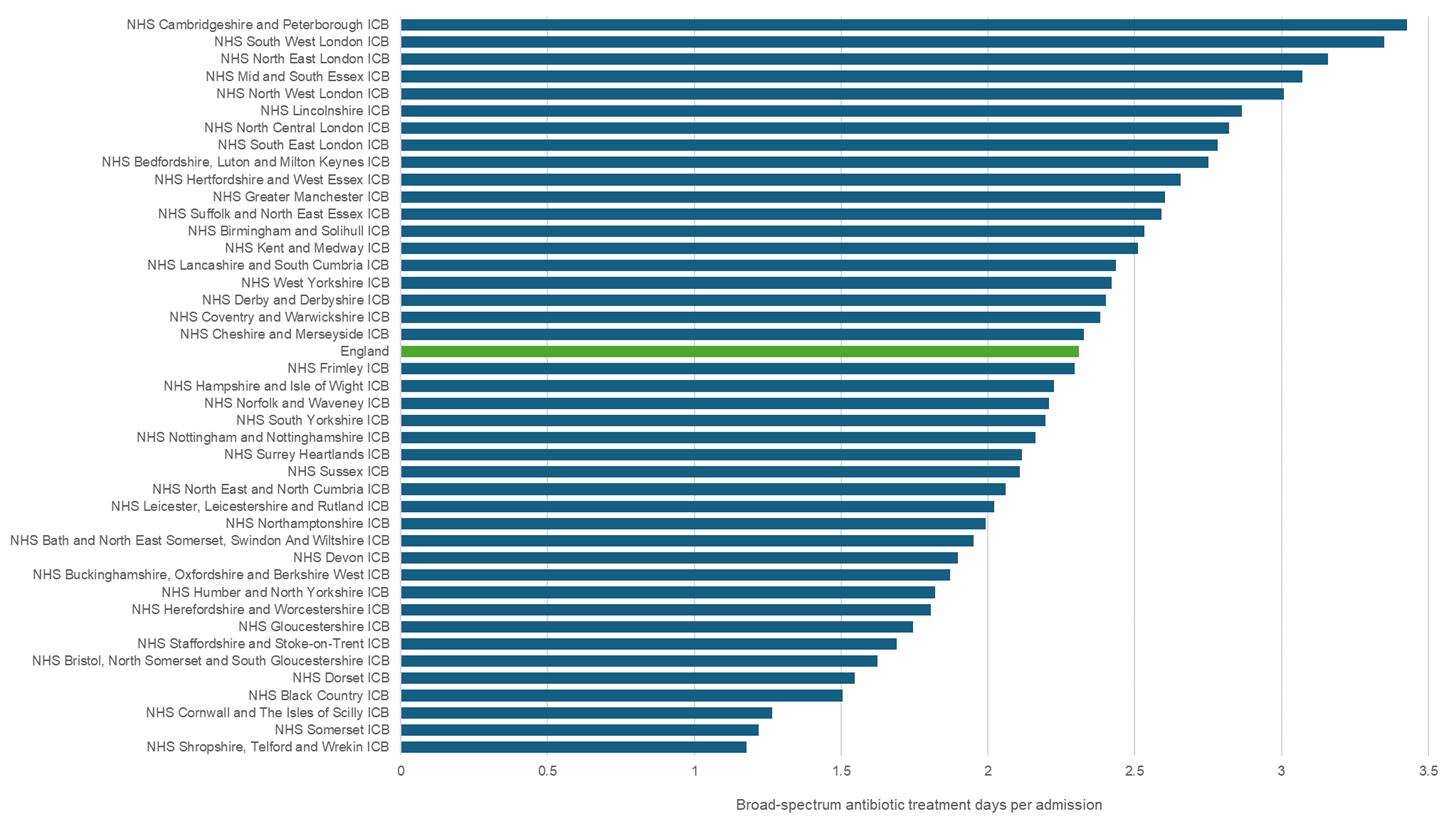
- Reduce patient exposure to broad-spectrum antibiotics: The UK AMR National Action Plan includes an ambition to reduce inpatient exposure to high-priority critically important antibiotics from the “watch” and “reserve” categories of the World Health Organisation’s AWaRe Classification. This ambition is reflected in the NHS Oversight Framework and the NHS Standard Contract for 2024/25. Your ICB performance is visible in Appendix 3 and on Fingertips. In the absence of septic shock, there is time to order tests and review the patient. It is therefore paramount that organisations adopt and promote the updated 2024 national sepsis guidance from NICE (NG51) that emphasises using physiological acuity and clinical judgement to guide the urgency of administering antimicrobials and spectrum of treatment.
- Improve appropriate antibiotic prescribing in dentistry: Alert general dental practitioners to the updated 2020 Evidence-based good practice guidelines from the Faculty of General Dental Practice (UK) and the Faculty of Dental Surgery and the National dental antimicrobial stewardship toolkit.
Action 2 – Confirm progress with implementation of the National infection prevention and control manual (NIPCM)
Infection prevention and control (IPC) is the most effective approach to controlling the spread of AMR. Every infection prevented is an antibiotic avoided (World Health Organization). The reliable application of IPC measures results in improved patient and clinical outcomes and prevents the spread of AMR in the healthcare environment.
Improving and maintaining hygiene standards in healthcare facilities, including the promotion of hand hygiene, is the most cost-effective IPC intervention. The prevention of infection enables the most sustainable delivery of care as it reduces the need for PPE, and associated waste, and reduces the risk and impact of biocide/disinfectant resistance in the healthcare environment.
Implementing the IPC measures detailed in the evidence-based NIPCM can reduce unnecessary antibiotics by preventing infections and decreasing transmission risks. This ultimately improves patient outcomes and helps standardise practice across care settings in England. The Board Assurance Framework (BAF) is available for use by organisations to provide assurance with IPC standards.
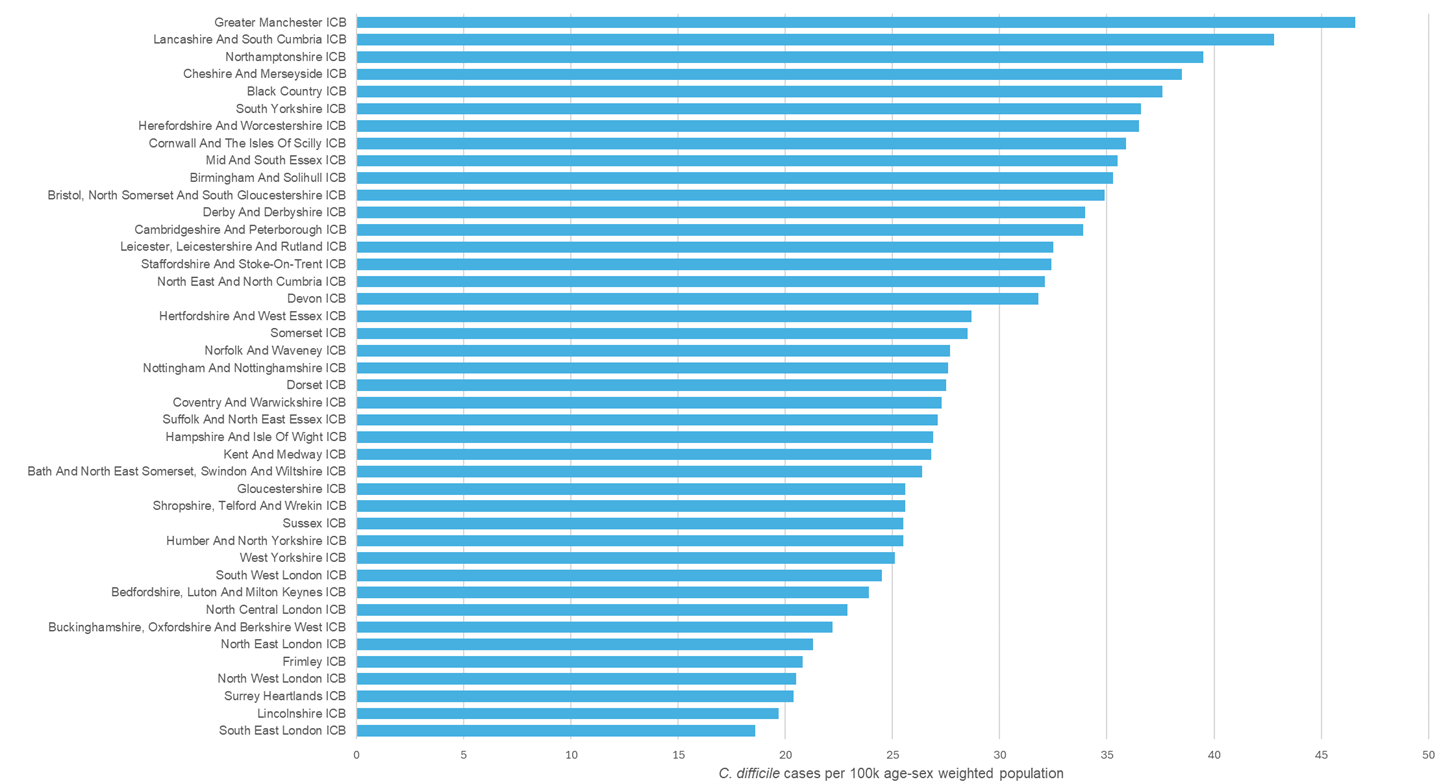
Following a 15-year declining trend, C. difficile infections are now increasing – your ICB performance is visible in Appendix 3. The Health and Social Care Act 2008: code of practice for infection prevention and control, was updated in December 2022. This outlines what registered providers in England should do to comply with the registration requirement at Regulation 12(2)(h), which includes ‘assessing the risk of, and preventing, detecting and controlling the spread of infections including those that are healthcare associated’, as well as optimising antimicrobial use and reducing AMR.
Action 3 – Audit blood culture pathway compliance
Blood cultures are critical diagnostic tests for guiding effective treatment for patients with sepsis. NHS trusts are encouraged to review and apply the findings of the improving blood culture pathway report and evaluate current performance.
An audit tool is available on the Office of the Chief Scientific Officer’s FutureNHS workspace to facilitate assurance of compliance.
A range of resources for tackling AMR during World AMR Awareness Week 2024 and beyond is detailed in appendices 1 and 2. Please share and promote these within your organisation.
If you have any queries about the above actions, please contact england.prevention-amr@nhs.net, your ICB AMR lead, or your NHS England regional antimicrobial stewardship lead at england.amrprescribingworkstream@nhs.net.
For broader World AMR Awareness Week queries, please contact the World AMR Awareness Week and Antibiotic Guardian National Lead, Professor Diane Ashiru-Oredope diane.ashiru-oredope@ukhsa.gov.uk
Yours sincerely,
Professor Sir Stephen Powis, National Medical Director, NHS England
Dr Jason Wong, Chief Dental Officer, NHS England
David Webb, Chief Pharmaceutical Officer, NHS England
Professor Dame Sue Hill, Chief Scientific Officer, NHS England
Duncan Burton, Chief Nursing Officer, NHS England
Dr Claire Fuller, National Medical Director for Primary Care, NHS England
Professor Suzanne Rastrick, Chief Allied Health Professions Officer, NHS England
Professor Susan Hopkins, Chief Medical Advisor, UK Health Security Agency
Appendix 1: Further actions to consider for World AMR Awareness Week 2024
As part of your activities for the awareness week health and care professionals are invited to encourage colleagues to take and/or lead others to take the following simple actions:
- Choose their Antibiotic Guardian pledge and encourage colleagues, family members and friends to do the same. The pledges were reviewed, and the website was updated in 2024. You may wish to share your pledge on social media platforms to encourage others to join you also. Please include #AntibioticGuardian, #KeepAntibioticsWorking and #WAAW in social media.
- Register your organisation’s AMR awareness activities by using the online registration form (this will take less than 5 minutes). Following registration, you will receive an email with a certificate for your organisation which can be displayed.
- Access the WAAW toolkit and digital resources for health and care workers that can be used and shared during WAAW. These resources build on those produced for previous campaigns, including digital notes, images, and social media messages.
- Visit the FutureNHS AMR Programme website for access to key national guidance, updates and content available relating to infection prevention and management as well as antimicrobial resistance. FutureNHS is also a mechanism to share knowledge and to network with other colleagues across the country.
- Use social media and community networks to engage with diverse population groups to promote key messages on AMR throughout the winter season using #AntibioticGuardian and/or #KeepAntibioticsWorking. Ready-to-use social media images and messages are available via the WAAW digital resources folder.
- Encourage staff to engage with the latest training resources around infections.
Appendix 2: key antimicrobial resistance resources that can support your actions to tackle AMR
A range of tools and resources are available for healthcare professionals to help you contribute to achieving the ambitions of the UK AMR National Action Plan through the collaborative work of NHS England, NHS England Workforce, Training and Education (previously Health Education England), the National Institute for Health and Care Excellence (NICE) and the UK Health Security Agency (UKHSA).
National policy and guidance
- UK Government 5-year national action plan – confronting antimicrobial resistance 2024 to 2029
- NHS long term plan
- NHS England operational planning and contracting guidance
- NHS England oversight framework
- NICE infection guidance
- UKHSA English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) annual report
- UKHSA World AMR Awareness Week (WAAW) toolkit
- WHO AWaRe list
Infection prevention and control (IPC)
- National infection prevention and control manual for England
- Infection prevention and control education framework
- Healthcare-associated infections
- COVID-19 infection prevention and control: every action counts
- National IPC manual
- DHSC Fingertips public health profiles: vaccination
Antimicrobial stewardship (AMS)
- National medicines optimisation opportunities
- UKHSA start smart then focus (SSTF) antimicrobial stewardship toolkit (refreshed in September 2023) for inpatient settings
- UKHSA Intravenous-to-oral switch (IVOS) national guidance for adults and children
- Royal Pharmaceutical Society antimicrobial resistance and stewardship: pharmacy guide
Dental stewardship
- Antimicrobial prescribing in dentistry: good practice guidelines (3rd Edition, 2020) from The Faculty of General Dental Practice UK (FGDP) and the Faculty of Dental Surgery of the Royal College of Surgeons of England (FDS). Also available from the College of General Dentistry website.
- The dental AMS toolkit from UKHSA provides a set of resources to help primary care practitioners promote the appropriate use of antibiotics in dental care.
- Additional resources are available via the British Dental Association’s antimicrobial resistance website.
Diagnostics for AMR
- Diagnosing sepsis and serious infections
- Improving the blood culture pathway: executive summary
- Improving the blood culture pathway FutureNHS (login required)
- UKHSA UK standards for microbiology investigations
Education and training
- Antibiotic Guardian website resources
- UKHSA and Royal College of General Practitioners the TARGET antibiotics toolkit for primary care includes a range of resources specific for general practice and community pharmacy
- Workforce, training and education (previously Health Education England) AMR resources
- Workforce, training and education indicative curriculum for AMR/AMS for pharmacy undergraduate and Foundation year
- BSAC Infection Learning Hub: Blood culture pathway modules
Data Sources
- Model Health System: AMR policy priority area
- Fingertips Public Health Profiles: AMR local indicators – produced by the UKHSA provides a range of Trust and ICB sub-location level datasets on antimicrobial resistance, healthcare-associated infections, antibiotic prescribing, infection prevention and antimicrobial stewardship. Fingertips also reports the number of Antibiotic Guardians at sub-ICB level
- NHS England AMR Dashboard: NHS Federated Data Platform
- PrescQIPP antimicrobial stewardship webkit provides antibiotic prescribing data visualisations for primary care in England, Wales and Northern Ireland, including prescription duration data
- OpenPrescribing, from the Bennett Institute for Applied Data Science at the University of Oxford, provides prescribing data visualisations for primary care in England and a new OpenPrescribing Improvement Radar was introduced recently to support improvement at sub-ICB location level
Healthcare students
Healthcare students are encouraged to learn more about and raise awareness of antimicrobial resistance with peers especially non-healthcare students during World Antibiotics Awareness Week and become antibiotic guardian champions.
Students can also:
- Complete on of the short e-learning AMR modules developed by NHS England Workforce Training and Education (formerly Health Education England)
- Register for access to the Antibiotic Guardian Healthcare Student Conference Module Learning Course
Schoolchildren and families
E-Bug – resources and materials for school children and their families are available via e-Bug (operated by UKHSA), including the Antibiotic Guardian Youth Badge, which educate on infection prevention and control as well as microbes, their spread and use of antibiotics with schools.
Healthcare workers, scientists and public health professionals can also sign up to become antibiotic guardian schools ambassadors.
Healthier Together web resources and Caring for children and babies with coughs leaflet via TARGET website.
Appendix 3: Antibiotic prescribing and infection metrics
Metrics included
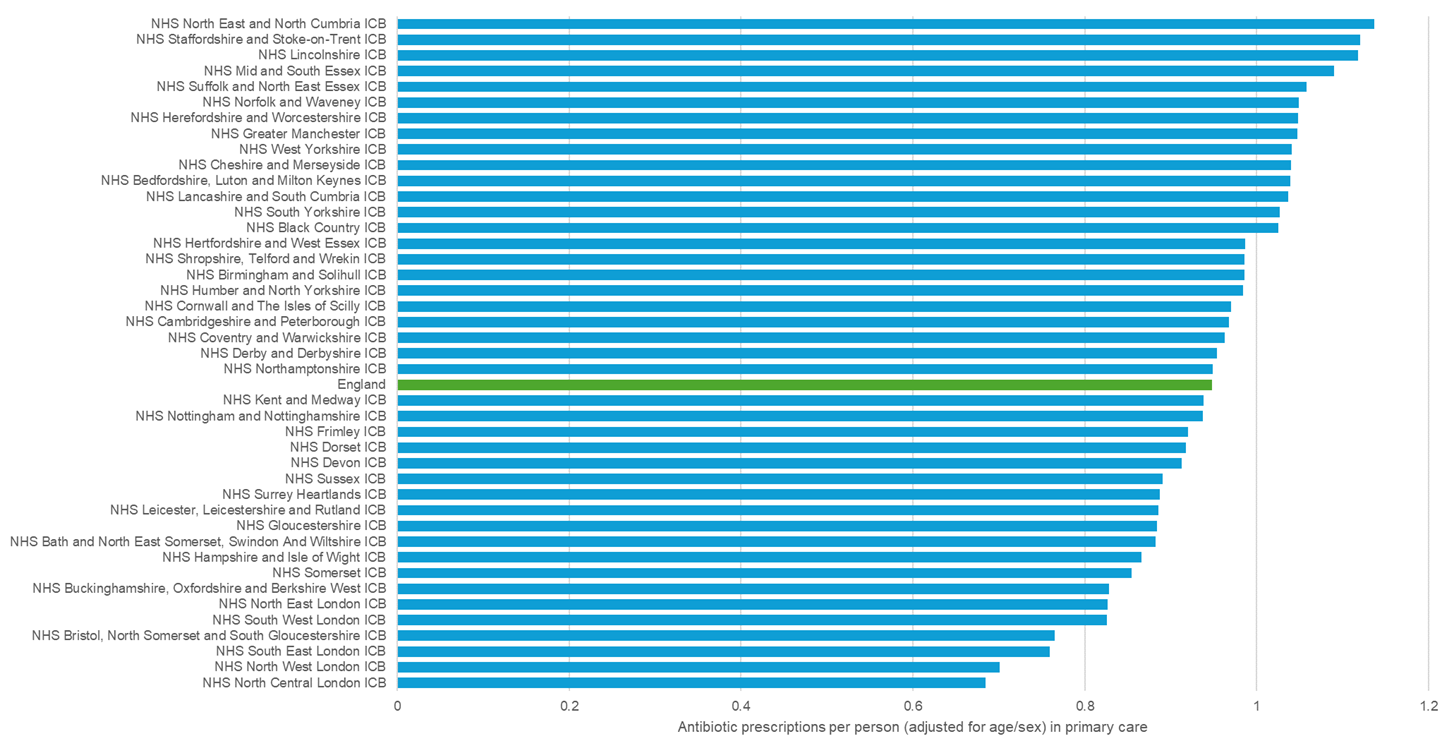
1. Antibiotic prescriptions per person (adjusted for age/sex) in primary care
Source: NHS Oversights Framework Antibiotic Dashboard (NHSBSA)
View metric – Antibacterial items per STAR-PU (12 months to month end) – Model Health System
2. Broad-spectrum antibiotic treatment days per admission
Source: Standard Contract report (UKHSA) [Published on FutureNHS only]
View metric* – Antibiotic prescribing from the “Watch” and “Reserve” categories of the WHO Essential Medicines List AWaRe index; DDDs per 1,000 admissions – Model Health System
*Data on Model Health System is quarterly whereas 12 monthly data is shown in these slides
3. C. difficile cases per 100k population
Source (origin UKHSA mandatory data capture system): View metric – Rate of C.difficile infection per 100,000 age-sex weighted population (12 months rolling to quarter end) – Model Health System
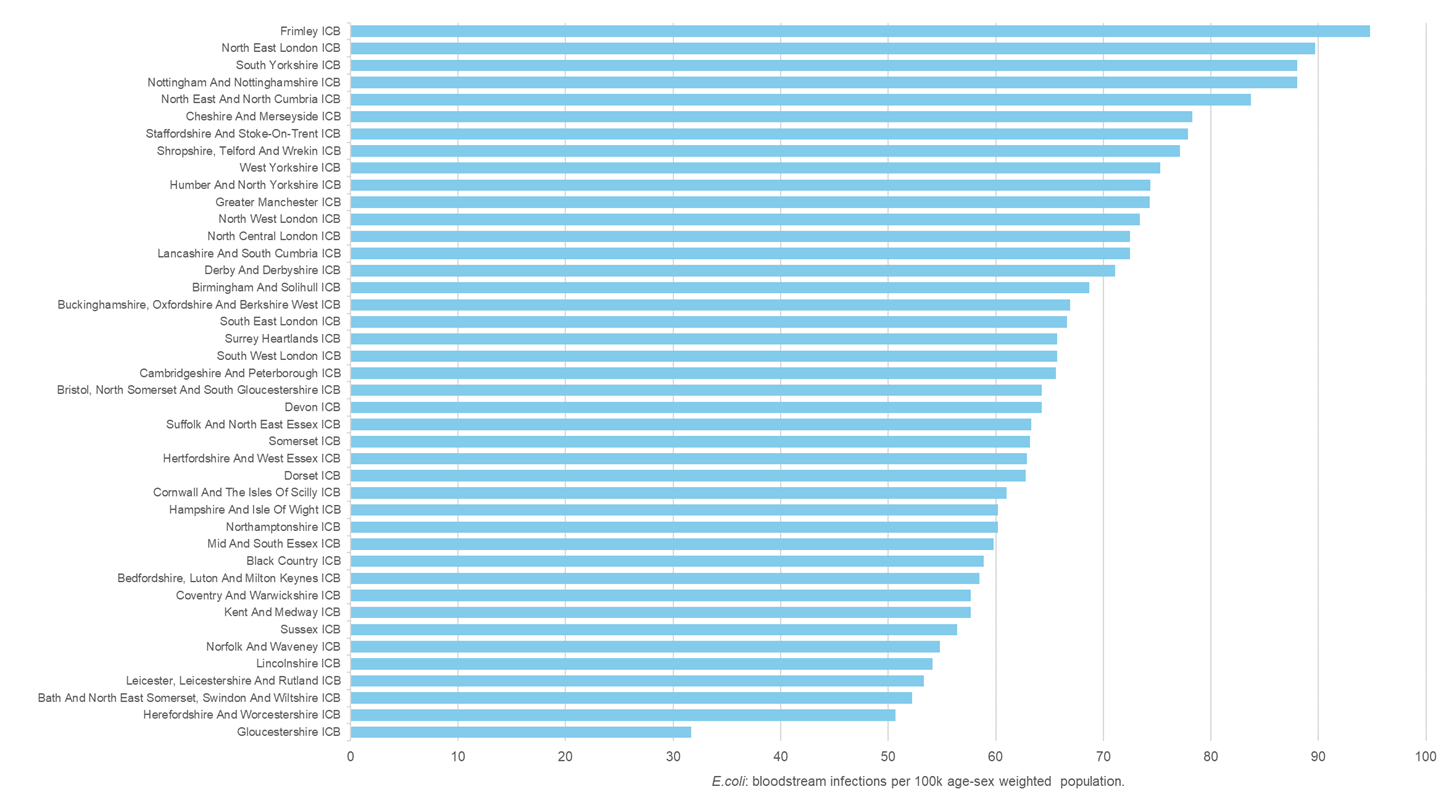
4. E.coli bloodstream infections per 100k population
Source (origin UKHSA mandatory data capture system): View metric – Rate of E.coli bacteraemia per 100,000 age-sex weighted population (12 months to quarter end) – Model Health System
Official published metrics for C. difficile and E. coli are available on Fingertips (not age-sex standardised):
Other useful resources
AMR Federated Data Platform Dashboard: Antimicrobial Resistance – Antimicrobial Resistance