These FAQs support integrated care boards and providers to deliver urgent treatment centres that meet the refreshed standards for the service.
Urgent treatment centres: frequently asked questions to support implementation of the standards and principles
General: designation
The UTC designation form can be found on the Urgent Treatment Centres Future NHS site which will support integrated care boards (ICBs) and facilities through the designation process; local areas can choose to use this form or their own process.
National assurance is not required, but the region must notify the national team of any change in service status.
This is a locally managed process. Urgent treatment centres should notify their local Care Quality Commission (CQC) teams when they have been designated, informing them of any change of function/new service, name or service opening hours. The process for registration for new services/change of function can be found on the CQC website.
It is for integrated care boards (ICBs)/local systems to determine the right service for their local population. We are not prescriptive about the type of alternative service sites may become, for example, extended access hubs and alternative non-urgent community services (for example, community mental health), and do not provide a specification for a non-urgent treatment service. However, we would not expect non-urgent treatment services to offer a walk-in option for urgent needs.
Commissioners must follow the guidelines in Planning, assuring and delivering service change for sites that are closing/changing, including public consultation as necessary.
There will be some instances where a local decision is taken to change the function of a designated urgent treatment centre (UTC) site, for example, where the UTC is part of a wider system reconfiguration of UEC services.
For any service change, commissioners should follow the guidelines in Planning, assuring and delivering service change. Local systems must have fully considered the impact on patients, involved local services and patient groups in decision-making, and clearly communicated the service change.
This change must be approved through the appropriate integrated care board (ICB) governance process. The following process is recommended for adoption relating to any change, but local systems may use alternative processes:
- a removal of designation status form is completed along with any further information to support decision-making.
- ICBs, in conjunction with NHS England regional teams, review and agree any changes to UTCs.
Like the designation process, this should be locally led in collaboration with regional teams and national sign-off is not required.
All Type 3 and Type 4 emergency department (ED) services that have yet to determine their future function must have robust plans, including timescales, to be designated an urgent treatment centre (UTC) or an alternative service by March 2024. Where a site is to be designated a UTC, the service must be operating to the standards by March 2024 or sooner. Any exemption to the timescales must be agreed between integrated care board (ICB) leads and regional leads. Regional teams should notify the national team of all decisions made.
Alignment with other urgent care services
Mental health must be considered a fundamental part of urgent care services, and pathways to support those in crisis must be included within the urgent treatment centre (UTC) service. Depending on a local needs assessment, this support may be provided by liaison mental health services or community-based crisis services, as well as signposting to other services such as places of safety.
Operational: standards
Each local system should review all appropriate information and agree any KPI measures relating to ‘average time in department’. Feedback from urgent treatment centre (UTC) site visits has indicated that many UTCs aim to complete a patient’s episode of care once initial assessment has been completed in approximately 2 hours. This differs across UTCs and localities and is dependent on the UTC case mix and access to investigations/diagnostics.
The urgent treatment centre (UTC) standards and principles are the minimum expectation that all UTCs, whether co-located or standalone, must achieve, and we encourage UTCs to go beyond the standards where that benefits local patients or the local system. For example, UTCs could consider extending their opening hours beyond 12 hours, 7 days a week to meet local demand; this is particularly relevant for those UTCs co-located with a Type 1 emergency department (ED), to maximise the diversion of appropriate activity.
Operational: estates
A paediatric waiting area should be considered ‘good practice’ but it is unrealistic to expect this to be the norm. Every service developing new facilities or altering existing facilities will be expected to consider the inclusion of a paediatric waiting room based on the volume of children who present to the service, but it will not be an expected standard for urgent treatment centre designation. Any estates adaption for paediatric requirements should be considered in line with need.
A mental health assessment room/bay should be considered ‘good practice’ in terms of providing a supportive environment for mental health patients, but it is unrealistic to expect this to be the norm. Every service developing new facilities or altering existing facilities will be expected to consider the inclusion of a mental health assessment room/bay based on the volume of patients with mental health conditions who present to the service, but it will not be an expected standard for urgent treatment centre designation.
Operational: communications
Urgent treatment centres (UTCs) should be described in a nationally consistent way to avoid public confusion about the services available and how people should access them. Good communication strategies help patients understand their options and which they should use first.
Communications should be organised locally, supported by NHS England regional teams. Where a UTC is in place, local comms should:
- promote UTCs as an increasingly common, easily accessible alternative to ED for all patients with urgent care needs
- encourage the public to use the NHS 111 service (telephone and online) when they have an urgent unexpected healthcare need
- explain that NHS 111 directs patients to the most appropriate service; this may be an urgent or same day appointment at a UTC, rather than emergency department (ED).
Integrated care boards should ensure that key local stakeholders and frontline staff – GPs, ED doctors, primary care nurses, NHS 111 providers and ambulance trusts – are kept informed about the role of the UTC in their patch.
Operational: standard operating procedures – patients
Urgent treatment centres (UTCs) must see individuals of all ages, including children under 2, for minor injuries and minor ailments.
A UTC patient is typically:
- ambulatory or mobile
- in need of same day treatment
- not in need of constant monitoring, though may need investigative tests to be undertaken
- requiring ‘urgent primary care’ level of investigations.
According to the Emergency Care Data Set (ECDS), patients spent on average 124 minutes in a UTC in May 2023; This reflects the acuity of the patients being seen in UTC settings. The most cited chief complaints of UTC patients, as recorded by 134 UTCs on ECDS in May 2023, are as below:
| Chief Complaint |
| Injury of upper extremity (disorder) |
| Injury of lower extremity (disorder) |
| Abdominal pain (finding) |
| Pain in lower limb (finding) |
| Skin problem (finding) |
| Eruption of skin (disorder) |
| Sore throat symptom (finding) |
| Pain in upper limb (finding) |
| Earache symptom (finding) |
| Cough (finding) |
| Chest pain (finding) |
| Fever (finding) |
| Laceration – injury (disorder) |
| Injury of head (disorder) |
| Wound care (regime/therapy) |
| Backache (finding) |
| Asthenia (finding) |
| Headache (finding) |
| Dysuria (finding) |
| Bite – wound (disorder) |
The list below is not exhaustive but shows some of the presentations a UTC can typically expect and should be able to treat.
Adapted from the North Tyneside Urgent Care Business Case – North Tyneside deep dive information available on FutureNHS.
Typical urgent treatment centre presentations
Minor injuries:
- superficial cuts including wound closure (suturing, stapling, gluing, steri-strips)
- bruises
- ear injury
- minor eye conditions/injuries – removal of superficial foreign bodies
- injury of severity not amenable to simple domestic first aid
- trauma (minor) to hands, limbs or feet
- minor burns and scalds
- insect, animal or human bites
- risk of tetanus
- minor head injuries without loss of consciousness
- potential fractures and foreign bodies (X-ray required)
- muscle and joint injury
- sprains and strains
- back pain and tendonitis.
Minor ailments:
- high temperature
- abscesses
- headaches
- headaches and dizziness
- coughs, colds, and flu-like symptoms
- hay fever/allergies
- ear, nose, and throat infections
- minor eye conditions/infections – conjunctivitis, eye inflammation, styes
- abdominal pain, indigestion, constipation, vomiting and diarrhoea
- dermatological and skin complaints, for example, rashes, minor allergic reactions, burns, scabies, head lice, sunburn
- genito-urinary problems, for example, urinary infections, thrush and menstrual problems
- falls in patients of any age without history of dizziness or blackout
- breathing problems, for example, asthma
- chest infections.
Operational: Standard operating procedures – appointments
Urgent treatment centres (UTCs) are expected to offer booked appointments, with patients booked direct from NHS 111/111 online, the ambulance service or their GP practice. UTCs must have a standard operating procedure for handling booked appointments alongside one for walk-ins. This should include appointments from front door streaming (for example, the urgent care self service product – streaming and redirection) whether this is available at the UTC or emergency department (ED).
The urgent treatment centre (UTC) standards continue to require UTCs to offer patients the ability to walk-in and book an appointment. Walk-in patients may be asked to book an appointment and return later if this is appropriate to their level of clinical need. Integrated care boards must provide strong justification, including with consideration of local health inequalities, for reducing or removing walk-in access, and NHS England regional assurance will be required.
While patients must be able to walk-in to a UTC, local communication should emphasise NHS 111 as the preferred option to access the service and all opportunities to illustrate the benefits of booked appointments to patients and the public should be made.
Patients contacting NHS 111 (telephone and online) or 999 will be given appropriate advice tailored to the nature of their complaint and local availability of alternative services. They may be booked an appointment with their GP or at the urgent treatment centre for the next day, booked an appointment at an enhanced access service, offered self-care advice or, if acuity warrants it, advised to attend emergency department (ED).
There must be clear signage advising patients who walk up during closing hours to phone NHS 111 or contact NHS 111 online (or 999 in an emergency).
Operational: standard operating procedures – assessment, streaming and referral
Urgent treatment centres (UTCs) should not duplicate any assessment where a record of this has been received via the appropriate messaging standard, or if the patient is conveyed where a handover is completed.
Referral from urgent treatment centres (UTCs) will depend on the patient’s condition. Patients could be referred to emergency departments (EDs), ambulatory or same day emergency care (SDEC) services, specialist services, GPs, community pharmacy (pharmacist: Community Pharmacist Consultation Service), dental, primary and community services or discharged with or without treatment. Where referral rates from UTCs into local EDs are high, integrated care boards should review relevant care pathways across UEC to maximise use of UTCs where clinically appropriate. This should form part of the ongoing review of ED case mix and re-attendance.
Where the capability exists, we expect patients to be booked an appointment at the appropriate onward service. Commissioners should work with local services to set up effective and efficient onwards referral pathways.
When making a referral, the referring service (ie NHS 111) should routinely consider the potential impact of non-attendance – given patients are generally assumed to have capacity, many problems get better on their own and it will have given appropriate worsening advice. If the patient’s attendance at the service to which they have been referred is considered essential, then it is the referring service’s responsibility either to ensure the patient has been seen as arranged, or to make alternative arrangements to ensure the patient receives appropriate onward care.
Responsibility should be considered to lie as follows:
- with the referring service (ie 111) for the correct assessment, worsening advice, and appropriate onward referral/advice
- with the patient (or guardian) to follow such advice
- with the receiving service (ie urgent treatment centre/emergency department/other face-to-face setting):
- for timely management of the patient on their presentation to the service
- on receipt of a referral message (for example, interoperability toolkit) or other message, for calling the patient back, following an agreed method for this.
All services should follow any agreed processes relating to non-attendance at booked appointments in line with their DNA procedures. In all cases the patient’s GP should be informed, but this does not imply that the GP is responsible for acting when a patient does not attend a booked appointment.
Urgent treatment centres (UTCs) can formally refer patients to community pharmacists for the treatment of low acuity minor illnesses and the supply of urgent repeat medication requests through the NHS Community Pharmacy Consultation Service (CPCS), taking advantage of the 2022 pilots of referral to this service from UTCs and EDs.
The NHS CPCS is a digital referral service to community pharmacists for the treatment of low acuity minor illnesses and urgent repeat medication requests. It has been in operation for NHS 111 services since 2019, and for general practice since 2020 (low acuity minor illness referrals only).
The service gives patients the opportunity to be seen by a community pharmacist for the treatment of their condition as an alternative to a clinician in the UTC. It supports the UTC with capacity management both at the time of the patient’s visit and for future visits through awareness of and education about the services local community pharmacies provide; and for patients can save them considerable time and improve their care experience.
Operational: standard operating procedures – coding
Patients must be coded against the location where they are seen and receive their care. If the urgent treatment centre (UTC) is co-located with a Type 1 emergency department (ED) and patients come through one main door, they will be streamed to the most appropriate place (ED or UTC) and must be coded against that place. Refer to question 21 for supporting information.
Currently, patients who miss appointments, in line with the standard operating procedure timescales (see urgent treatment centre (UTC) standards 4 and 5), must be coded as a walk-in.
It is important that UTCs continue to capture as much data as possible, to give us the best understanding of activity through the system, and help local systems describe how they are supporting patients to access urgent care conveniently and in the best setting to meet their health needs.
All urgent treatment centres (UTCs) are Type 3 services. As part of the implementation of Emergency Care Data Set (ECDS) and in line with the UTC standards and principles, all UTCs are required to report as a Type 3 service under their own organisation data service (ODS) code, including those co-located with a Type 1 emergency department (ED) and/or led by an ED consultant.
The UEC recovery plan set out the ambition to improve to 76% of patients being admitted, transferred, or discharged within four hours by March 2024. This ambition relates to an aggregated position across ‘All Types’ (Types 1, 2, and 3) performance. Systems can code against Type 1, Type 2 and Type 3 and aggregate as appropriate to report the ‘All Types’ position via ECDS and MSitAE (monthly trust situation reports).
Operational: standard operating procedures – service name and branding/signage
Services operating as urgent treatment centres are expected to call themselves an ‘urgent treatment centre’, including in road and on-site signage. Alternative names must not be used to avoid creating confusion for patients and the public.
- For urgent treatment centre based at hospital sites
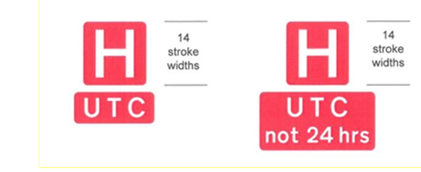
The Department for Transport (DfT) authorised the first urgent treatment centre (UTC) traffic symbol for signs in October 2018, in Wakefield Council’s jurisdiction, and designed appropriate symbols (see below) for UTCs based on hospital sites, which must not be varied locally.
The white ‘H’ on a red background is a well-recognised symbol for directing road users to hospitals with urgent medical facilities. A ‘UTC’ or ‘UTC not 24 hrs’ plate sits underneath or alongside the ‘H’ symbol to indicate a UTC facility is present at the hospital; this plate must not be used without the ‘H’ symbol and again the lettering is white on a red background.
To update signs with this new symbol, local authorities must follow the established DfT traffic sign authorisation application process to receive local consent to the new symbol’s use (see question 33 below).
Where a UTC is co-located on a hospital site with an emergency department (ED), the H/ED symbols are sufficient to signpost drivers to the hospital and only these should be used.
- For urgent treatment centres at non-hospital sites
Signs to urgent treatment centres (UTCs) based at non-hospital sites must be text based. The generic ‘urgent treatment centre’ must be used. These signs do not require DfT authorisation.
- Costs
The local authority is responsible for paying for road signs on their roads; however, it may pass this cost onto the locality. Arrangements should be agreed locally for changing signage between the integrated care board and the local authority/trust.
Local authorities are responsible for erecting traffic signs on their roads and for contacting the Department for Transport (DfT) to authorise any new traffic sign that is not prescribed by regulations (The Traffic Signs Regulations and General Directions 2016).
Each local authority will follow its own decision-making processes and is ultimately responsible for approving or rejecting proposals to signpost to a urgent treatment centre (UTC) facility. We advise that the locality contacts the local authority early in the designation process, to establish requirements for road signage, application process and cost.
The integrated care board (ICB) should advise the local authority what signage it prefers before the local authority makes a request to the DfT (although this is not compulsory or required); and for a UTC based at a hospital site, we recommend this request is for red road signage.
Local areas will need to manage the implementation process. The process for applying for UTC road signage is:
- to begin the process, NHS trusts moving from provision of an ED service to a UTC must inform their local authority
- for UTCs on hospital sites, the local authority takes responsibility for informing the DfT and raising the signage request directly with it through a formal application process, which can take up to 12 weeks; where necessary, interim arrangements can be put in place, for example, on a legacy ‘H’ and ‘A & E’ plate, the ‘A & E’ plate can be covered until a longer-term solution is agreed locally.
If the urgent treatment centre (UTC) is run by an NHS trust or foundation trust, then under the NHS identity guidelines it must be branded with the trust’s logo – and all the trust’s services will carry this logo. Trusts must not create service-specific logos for different services, the only exception being where a trust delivers a UTC service outside its usual geography.
For further information:
- identity guidelines – organisational logos
- branding services outside our usual geography
- guidelines for third-party providers of UTC services (ie private companies), and as illustrated in this example.
Tariffs
Under the NHS Payment System for 2023/2025, all NHS provider and commissioner relationships with a total annual value of £30 million or more need to use the aligned payment and incentive approach. This involves setting a fixed payment to fund all the services the provider delivers for the commissioner’s population. Most urgent treatment centre activity should fall into this category, and fixed payments will be determined locally between provider and commissioner.
The provider should have contracts with those bordering integrated care systems/integrated care boards for which it has been agreed their patients can use the urgent treatment centre as part of their fixed payment arrangements.
Health inequalities
Yes. All urgent treatment centres (UTCs) need to comply with the duty to refer rules. The Homelessness Reduction Act 2017 introduced a duty on certain public authorities to refer service users who they think may be homeless or threatened with homelessness to a housing authority. The service user must give consent and can choose which authority they are referred to, as described in the Homelessness code of guidance for local authorities.
A Urgent and emergency care (UEC) homelessness and rough sleeping pathway checklist and toolkit has been developed to support UEC services to meet the duty to refer rules.
The NHS website details how to find a GP practice, and the registration form (GMS1) can be downloaded from it. Importantly, this guidance states that “anyone in England can register with a GP surgery. It’s free to register”, and “you do not need proof of address or immigration status, ID or an NHS number”.
Clinical and workforce (including safeguarding and prescribing)
All urgent treatment centres (UTCs) should have a named senior clinical lead who is a core member of the senior team and takes responsibility for general oversight, governance, audit, training, and the strategic development of the service. It is entirely acceptable for one lead to be involved in the leadership of more than one UTC.
In the multidisciplinary team (MDT) model there must be appropriate clinical oversight of decision-making around patient care throughout the UTC’s opening hours, whether provided on or off site (or via a mixed model). Off-site arrangements may be integrated with the Clinical Assessment Service whereby identified clinicians provide the support/leadership to the UTC with appropriate access protocols in place.
Urgent treatment centres are no longer required to be GP led and while senior clinical leadership will in most cases be provided by a named GP, emergency department (ED) consultant or a combination of the two, the role can be fulfilled by a senior, non-medical clinical member of staff, for example, an advanced clinical practitioner or advanced nurse practitioner, where appropriate. Access to clinical advice and guidance from an ED must be available to the senior clinical lead and multidisciplinary team (MDT). If required necessary supervisory arrangements should be implemented to support a non-medical senior clinical lead.
The senior clinical lead must in all cases be supported on site by an appropriate MDT that have the skills to treat patients of all ages with minor injury and minor illness throughout opening hours.
No. We understand this will not always be desirable or practical. The full scope of the urgent treatment centre service, in-line with the standards, must be provided throughout the opening hours, even when the senior clinical lead is not on-site, as remote access may be adopted. Local governance arrangements should be implemented to support.
Access to remote clinical advice from clinicians in a local emergency department (ED) helps minimise avoidable onward referral of urgent treatment centre (UTC) patients into EDs, streamlining the patient’s experience of care. Systems may wish to consider the benefits of broadening the access to clinical advice, for example, to include clinicians in same day emergency care departments or surgical specialties, where this is appropriate to local demand and capacity.
Where UTCs are co-located with a Type 1 ED, we understand clinical advice from the co-located ED can already be accessed in many cases, either remotely or directly through ED consultants in the UTC workforce. In these cases, no further action will be required.
Where remote clinical advice is provided by another service, clinical responsibility for the patient remains with the UTC until the patient is discharged or, if required, referred onto another service.
Urgent treatment centre (UTCs) are required to have the capability to prescribe medication during their opening hours, potentially involving remote clinicians. Prescribers may use paper or NHS Electronic Prescription Service prescriptions may be generated.
Commissioners must consider a multidisciplinary model that ensures all urgent treatment centres (UTCs) have the capability to treat patients of all ages with minor injuries and minor illnesses, according to local need. This may include emergency department clinicians, GPs, nurse practitioners, paramedics, district nurses, paediatric or geriatric specialists, mental health practitioners, social care, physiotherapists, community mental health, allied health professionals and advanced clinical Practitioners.
We expect UTCs to consider workforce development and support for local education and training in collaboration with local integrated care boards.
We recommend that the level of training gained is advanced life support; basic life support would be considered insufficient. Annual immediate life support training may be suitable for smaller units where the need for resuscitation is infrequent.
The Resuscitation Council UK provides one-day adult and paediatric immediate life support training.
Investigation and diagnosis
Clear protocols must be in place to manage clinical risk in booking patients in for X-ray or referring them off site. Some examples of access protocols are for urgent treatment centres to have:
- an agreed arrangement for where and at what times the X-ray service is provided at an alternative site,
- access via a co-located service, for example, via a diagnostic hub,
- direct referral to X-ray at another site (not via emergency department), for example, on an appointment basis. The patient may then conclude their treatment at the site to which they have been referred if appropriate.
Patients referred off site should not have to ‘start again’ in a new setting; they should be given a booked slot or referred direct to the appropriate facility without further triage at a secondary service, for example, emergency department.
IT and digital
Urgent treatment centres will be expected to have a clinical workflow system that can as a minimum:
- send and receive patient transfers and referrals
- access key patient information, such as the local healthcare record, summary care record, care/crisis plans and key patient flags
- issue electronic prescriptions via the EPS
- access the Child Protection-Information Sharing service (CP-IS)
- submit data daily to the Emergency Care Data Set (ECDS) as a Type 3 emergency department, in line with the applicable information standard.
IT and digital: Emergency Care Data Set
As per the Emergency Care Data Set (ECDS) v4 user guide only urgent treatment centres (UTCs) should report as Type 3 emergency department services. Alternative facilities, such as out of hours GP appointments, GP streaming services, minor injury services and walk-in centres are excluded from data collection via ECDS from July 2024.
IT and digital: Booking and Referral Standard
The Booking and Referral Standard (BaRS) is an interoperability standard for healthcare IT systems that enables booking and referral information to be sent between NHS services quickly, safely and in a format that is useful to clinicians. It is being rolled out across all care settings.
Please direct questions about this standard to the national team at bookingandreferralstandard@nhs.net.
NHS 111 (telephone and online) should use Booking and Referral Standard (BaRS) to book appointments into urgent treatment centres. Full rollout of BaRS is planned for 2023/24.
Check this list of supplier status to find out the status of your supplier. If they are not on the list, your supplier has yet to engage with NHS England’s BaRS programme and they should contact the national team at bookingandreferralstandard@nhs.net.
No, this does not need to change. BaRS is digitalising the existing patient’s journey and not redirecting patients to different services.