Complications from Excess Weight (CEW) clinics for children
Obesity affects one in four children in the UK and can increase the likelihood of a child developing serious health issues such as Type 2 diabetes, liver conditions and early heart disease.
Children living with obesity can also develop difficulties such as breathing problems, sleep issues and mental health problems, which can dramatically impact their quality of life. However early action can prevent the onset of these long-term health problems which is beneficial for the health outcomes of patients and the sustainability of the NHS.
The number of children living with obesity almost doubles from the start of primary school to the end of primary school. The latest data shows one in four children aged 10-11 are obese in England. Two and a half million children in England are affected by excess weight or obesity, with 1.22 million significantly obese and eligible for treatment according to NICE guidance.
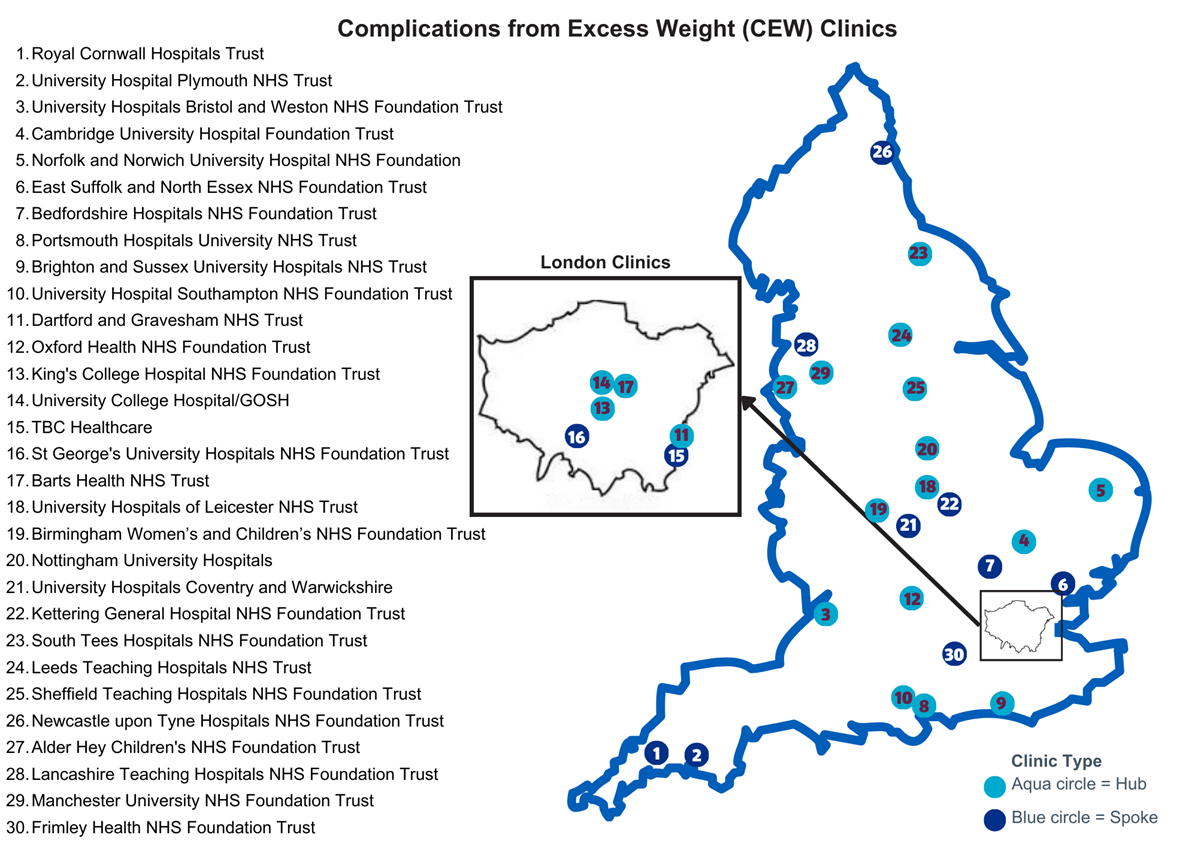
Complications from Excess Weight (CEW) clinics use a holistic approach to treating conditions related to obesity in children and young people (CYP). Thirty clinics are now open and care is being delivered by a multidisciplinary team (MDT), linked to a specialist children’s hospital.
The three aims of the service are to:
- Identify the factors involved in the development of severe obesity. Assessment should be holistic with equal consideration for mental health, physical health and social needs.
- Treat complications associated with severe obesity and coordinate / refer onto other services where required.
- Consider an individualised holistic plan. This may include interventions such as family-based therapy, behavioural coaching, dietary strategies, and mental health support. This aims to address health inequalities by considering culturally appropriate factors and a personalised approach.
Children will receive holistic treatment and person-centred care packages developed with their family, which could include mental health treatment, coaching and advice around a healthy diet.
The rollout of the pilot delivers on the NHS Long Term Plan ambition to treat children for severe complications related to their obesity, avoiding the need for more invasive treatment. One thousand children a year, who are aged between two and 18 and experiencing health complications related to severe obesity, will be supported through the new services.
There are currently 30 active sites based across the country in the following locations:
Complications from Excess Weight (CEW) clinics
South West
- University Hospitals Bristol and Weston NHS Foundation Trust (clinic type: hub)
- Royal Cornwall Hospitals Trust (clinic type: spoke)
- University Hospital Plymouth NHS Trust (clinic type: spoke)
South East
- Brighton and Sussex NHS Foundation trust (clinic type: hub)
- Dartford and Gravesham NHS Trust (clinic type: hub)
- Frimley Health NHS Foundation Trust (clinic type: spoke)
- Oxford Health NHS Foundation Trust (clinic type: hub)
- Portsmouth Hospitals University NHS Trust (clinic type: hub)
- University Hospital Southampton NHS Foundation Trust (clinic type: hub)
London
- King’s College Hospital NHS Foundation Trust (clinic type: hub)
- Barts Health NHS Trust (clinic type: hub)
- St George’s University Hospitals NHS Foundation Trust (clinic type: spoke)
- TBC Healthcare (clinic type: spoke)
- University College Hospital/Great Ormand Street Hospital (GOSH)/Tavistock (clinic type: hub)
East of England
- Cambridge University Hospital Foundation Trust (clinic type: hub)
- East Suffolk and North Essex NHS Foundation Trust (clinic type: spoke)
- Bedfordshire Hospitals NHS Foundation Trust (clinic type: spoke)
- Norfolk and Norwich University Hospital NHS Foundation (clinic type: hub)
Midlands
- Birmingham Women’s and Children’s NHS Foundation Trust (clinic type: hub)
- University Hospitals Coventry and Warwickshire NHS Trust (clinic type: spoke)
- University Hospitals of Leicester NHS Trust (clinic type: hub)
- Kettering General Hospital NHS Foundation Trust (clinic type: spoke)
- Nottingham University Hospitals NHS Trust (clinic type: hub)
North East and Yorkshire
- Leeds Teaching Hospitals NHS Trust (clinic type: hub)
- Newcastle upon Tyne Hospitals NHS Foundation Trust (clinic type: hub)
- Sheffield Teaching Hospitals NHS Foundation Trust (clinic type: hub)
- South Tees Hospitals NHS Foundation Trust (clinic type: hub)
North West
- Lancashire Teaching Hospitals NHS Foundation Trust (clinic type: hub)
- Manchester University NHS Foundation Trust (clinic type: hub)
- Alder Hey Children’s NHS Foundation Trust (clinic type: hub)
How will people be able to get an appointment and what are the criteria for referral?
Children and young people will be able to access CEW clinics following a referral from secondary or tertiary paediatrician following referral by a range of clinicians including:
- community paediatrician
- general practitioners from primary care
- from another clinical speciality (i.e. CYP mental health services) or secondary care paediatrician
- community paediatrician
- general practitioners from primary care; and
- from another clinical speciality (i.e. CYP mental health services) or secondary care paediatrician
Referral to the specialist obesity clinic should be based on (i) the degree of obesity and (ii) presence of comorbidities. It is suggested some blood tests could be conducted on referral. It is acknowledged each local system may need to adapt its referral criteria according to local demand and within the context of existing. Referrals should be considered based on need.
If you would like more information on the obesity programme please contact the CYP Transformation Programme team at: england.cyptransformation@nhs.net – please note this is a national team inbox and not appropriate for patient enquiries.