1. Introduction
In transforming mental health services, the NHS has a clear focus on strengthening community and neighbourhood care to shift care from hospital to community.
It is also committed to improving prevention and early intervention, for which access to evidence-based community mental health rehabilitation is vital for people with severe mental illness.
Commissioning good local community rehabilitation services will enable people with complex psychosis or other severe mental illness to live close to home and in the least restricted way, to be supported to manage their symptoms in a way that promotes their autonomy and to recover as defined by them.
This guidance supports the commissioning of those services. While the way in which community mental health rehabilitation services are commissioned can vary according to the needs of the local population and who holds delegated responsibility for commissioning these services, the central principle is place-based multidisciplinary provision aligned with primary care networks.
Access to these services should be premised on the needs of the individual and an ‘all means all’ approach.
All elements of the mental health rehabilitation pathway, including tertiary community rehabilitation – that is, local rehabilitation that is essential and cannot reasonably be done in universal, primary and core secondary services – should be delivered in a way that meets local population needs and makes sense for the system.
This guidance has been informed by visits to community rehabilitation services and focused discussions with groups and individuals representing commissioners, frontline staff, people currently using services and their families and carers.
It draws on key policy, evidence, standards and guidance pertinent to mental health rehabilitation such as:
- Getting It Right First Time (GIRFT) Programme National Specialty Report for mental health rehabilitation
- National Institute for Health and Clinical Excellence (NICE) guideline [NG181]: Rehabilitation for adults with complex psychosis
- Royal College of Psychiatrists: Standards for community mental health rehabilitation services
A Task and Finish Group (see Appendix 1) made up of experts by experience, commissioners, operational managers, clinicians and representatives from mental health providers, the Care Quality Commission (CQC) and the voluntary and community, faith and social enterprise (VCFSE) sector have informed its development.
Our other publications concerned with the commissioning and delivery of mental health services are:
- Commissioning framework for mental health inpatient services
- Commissioner guidance for adult mental health rehabilitation inpatient services
- Acute inpatient mental health care for adults and older adults
- Community mental health framework for adults and older adults
- National guidance to support integrated care boards to commission acute mental health inpatient services for adults with a learning disability and autistic adults
2. Scope
The scope of this guidance is community mental health rehabilitation services predominantly for adults and older adults, but commissioners should also consider young people transitioning into adult services.
References in this guidance to adult mental health services include those for older adults.
However, as commissioned services should be needs-based, services specifically for older adults should be used where particular expertise is required to support an older adult experiencing poor mental health; namely those who have specific needs because of co-morbid physical and mental health conditions, frailty, cognitive issues or end of life, acknowledging the cumulative impacts of earlier life experiences and specific stressors related to ageing.
This guidance recognises the importance of supporting all people to regain skills they have lost or learn those they have not acquired due to severe mental illness, including those receiving treatment under the Mental Capacity Act 2005 or the Mental Health Act 1983.
Where a person has received treatment under the Mental Health Act, they may be eligible for Section 117 aftercare, which includes community rehabilitation services that support them to regain, enhance or learn new skills, as referred to in Discharge from mental health inpatient settings.
The guidance also recognises that alignment and effective transitions, between community mental health rehabilitation services and other community provision and inpatient mental health services, are critical to a robust and seamless offer for people using services and their families.
Community services include, but are not limited to, community mental health services such as early intervention in psychosis, assertive or intensive outreach provision, specialist forensic services, community services for people with a learning disability and specialist autism services.
A proportion of people with rehabilitation needs will require tertiary mental health rehabilitation in the community.
Commissioners should ensure that there is dedicated capacity and specialist resource to provide this, and that these services should have seamless links to Level 1 and 2 adult mental health rehabilitation inpatient services.
Most NHS mental health trusts in England have dedicated tertiary community mental health rehabilitation services that can provide specialist intervention, advice and consultation to the wider system; scaffolding and supporting core community mental health services.
Any person with a mental health rehabilitation need who requires the level of intensity and specialism provided by the local tertiary offer should be able to access this; however, it is acknowledged that much of this demand will come from people with complex psychosis who are in hospital or who are at risk of admission to hospital.
This includes people with treatment-resistant positive symptoms (that is, hallucinations, delusions or both that have not responded to usual treatments), severe negative symptoms or specific cognitive impairments associated with psychosis that impair motivation and organisational skills, and co-occurring mental and physical health conditions.
3. Key messages
Community mental health rehabilitation is a core element in a whole pathway that supports people with severe mental illness to recover and live well, as equal citizens in their community.
The healthcare element of rehabilitation is one component of the pathway; good community mental health rehabilitation also requires a place to live, something to do and social networks.
3.1 Providing collaborative holistic support and promoting citizenship
Commissioners need to ensure that the rehabilitation pathway is holistic, meeting the medical, social, emotional and practical needs of people with a severe mental illness.
This will require strong collaboration within localities across a range of partners, including health and social care, housing and support providers and local services for specific issues such as substance misuse.
Many of these partners will be in the VCFSE sector and can be responsive to cultural and local nuances, providing care and support that is respectful and relevant to the person’s background and experiences.
The full range of local resources and expertise should be harnessed as required to ‘wrap around’ the person, supporting their recovery and wellbeing, promoting inclusion, reducing stigma and preserving their sense of belonging.
This focus on citizenship and belonging is particularly pertinent for individuals who have experienced, or are at risk of, being admitted to inpatient rehabilitation services at distance from home.
Commissioning community-based mental health rehabilitation in line with this guidance will support people to have a better quality of life, maintain their daily routines, stay connected with family and friends, and participate in their community.
These are all essential for facilitating recovery.
3.2 Reducing reliance on mental health inpatient care
“This team are ‘in depth’ – never experienced input on this scale before when I need it… it’s planned around me.” (a person accessing community mental health rehabilitation)
Commissioning community mental health rehabilitation services that can respond in a timely, flexible way (increasing or reducing the intensity of support offered) can be expected to reduce reliance on mental health inpatient services – both in terms of number of admissions and length of stay, although evidence for this has yet to be established.
Where this rehabilitation has not been developed or commissioned, people living in those areas are unable to have their rehabilitation needs met in the community.
This negatively impacts on access to early rehabilitation intervention that prevents rehabilitation needs worsening to a point they can only be addressed in an inpatient setting.
This gap may also prolong hospital stays as there is no provision for continued mental health rehabilitation post discharge.
The commissioning, development and delivery of community mental health rehabilitation services should consider the requirements of all local people who need them, including those who may be local but are currently placed in inpatient provision that is outside of the local pathway of care.
3.3 Strengths-based intervention, care and support
“…they make me feel like my mental illness is not going to define me and the rest of my life…” (a person talking about their community mental health rehabilitation service)
Strengths-based community mental health rehabilitation supports people to achieve their personalised rehabilitation goals, optimum functioning, and the skills and confidence to manage their own health and wellbeing.
This independence is vital for long-term recovery and promoting people’s citizenship.
Community mental health rehabilitation services must be specifically commissioned to provide rehabilitation interventions.
Therefore, measurement, analysis and reporting of the impact of these interventions are key.
Embedding and reporting on patient-reported outcome measures (PROMs) is important to ensure the service offer is effective.
DIALOG, recovering quality of life – 10-item scale (ReQoL-10) and goal-based outcomes (GBOs) are the recommended suite for community mental health services.
The National Collaborating Centre for Mental Health provides implementation guidance: Patient-reported outcome measures (PROMs) for people with severe mental illness in community mental health settings.
Community mental health rehabilitation services need to reference the purpose of their support for an individual. Using goal-based outcomes can enable progress to be flexibly reviewed and measured.
Individualised goals will change over time. Recording and celebrating success is important, as well as building on the person’s strengths and demonstrating progress.
This is vital for the person and those who love and care about them; but also for the workforce more generally as a demonstration of their value as a service.
Commissioners should ensure that people can access local community rehabilitation support that is collaborative in determining how they identify, gain, develop and maintain the skills that are important to them.
If there is no requirement (or it is not feasible) for a person to make progress in any rehabilitation domain, the key worker will need to work with them and those who know and care about them to ensure that their needs are met by the appropriate community provision.
Commissioners should also ensure that people can receive ongoing support and have good transitions between teams and providers as appropriate.
3.4 Dynamic strategic commissioning
“Hospital was the only option for my son, he spent most of his adult life as an inpatient because the housing and support in the community wouldn’t meet his needs.” (mother of someone now being supported by community mental health rehabilitation service in the community)
The commissioning of community mental health rehabilitation services requires a detailed assessment and analysis of local population needs and health inequalities.
This will only be possible through the collection and review of relevant, reliable data and other available evidence.
It involves mapping current demand and capacity for inpatient and community mental health rehabilitation and identifying which needs can be met through existing community services (including community mental health, learning disability and autism services) and what additional capacity may need to be commissioned to reduce reliance on inpatient care in the future.
Commissioners of community mental health rehabilitation services will need to collaborate with those of interfacing and related services – for example, housing and social care – to ensure the whole pathway is considered and the landscape of relevant provision and support for people who have mental health rehabilitation needs is planned for in a joined-up way.
The importance of this approach is described in more detail in the next section.
4. Commissioning arrangements
“We need less therapeutic communities, and more communities that are therapeutic.” (clinician working in mental health services)
The commissioning of community mental health rehabilitation services should be based on the assessed needs of local populations and their identified health inequalities.
Services should focus on improving access for underserved groups and those over-represented within mental health inpatient care, especially those receiving long-term treatment under the Mental Health Act 1983. The Patient and carer race equality framework is a resource to help support this. This mandatory framework will support trusts and providers to co-produce and implement actions to reduce racial inequalities within their services.
In any locality a range of providers will make up the landscape of mental health rehabilitation provision. This will include clinical teams, adult social care, VCFSE organisations, and housing and support providers.
Commissioners will need to consider how best to harness these assets and encourage collaboration and partnerships across them.
Commissioners across health and social care will also need to work together to achieve joined-up, efficient and effective service provision.
Robust collaborative, strategic commissioning across systems makes good fiscal sense and ensures that disputes and barriers can be resolved promptly, without causing unintended interruptions or negative consequences to the care and support for the person.
Where required, reference should be made to the appropriate guidance for identifying the responsible commissioner (see NHS England’s Who pays? guidance).
An integrated pathway across health, social care and housing is critical for effective community rehabilitation provision.
The commissioning approach that best fits with local architecture, pathways and provision should be considered and employed – such as community alliances, provider collaboratives or pooled budgets.
Many localities lack available – or cannot offer choice in – appropriate housing and support, a situation that often delays discharge from or leads to inappropriate admission to hospital.
Commissioners will need to engage their commissioned services in understanding current need and predicting future demand for housing and support, by harnessing available data and informing local strategies.
“…after being in hospital for 18 years I was told I was ready for discharge, but then I had to wait for 3 months for discharge assessments to be completed and another 10 months after that to find accommodation… that made me more unwell, I was losing all hope of ever moving out of hospital.” (person who was discharged from an inpatient mental health rehabilitation unit)
Personal health budgets (PHBs) increase choice in and control over how people with mental health needs access services and support for their needs, leading to improved outcomes.
They should be offered to those who have a legal right to them, including adults eligible to receive NHS continuing healthcare and people subject to Section 117 of the Mental Health Act 1983, with clear policies and processes in place to support access, such as brokerage support and advocacy.
Consideration should be given to offering people with severe mental illness access to one-off payments to facilitate discharge or avoid admission to hospital. PHB payments can also be made to carers.
Meaningful and informed commissioning of community mental health rehabilitation services should help to address issues such as hospital admission without a clear purpose or ‘spot purchased or cost per case’ placements outside a local pathway.
These placements have inherent risks, including dislocation of care, longer lengths of stay and increased costs.
Reinvestment of potential savings from delivering care close to home will strengthen community mental health rehabilitation services to meet the intensity and severity of needs outside hospital.
5. Community mental health rehabilitation services
“If community mental health rehabilitation was available for me, I would have saved years of my life lost in hospital.” (person who had been in an inpatient rehabilitation unit)
Killaspy et al (2009) describe mental health rehabilitation as:
“A whole system approach to recovery from mental ill health which maximises an individual’s quality of life and social inclusion by encouraging their skills, promoting independence and autonomy in order to give them hope for the future and which leads to successful community living through appropriate support.”
People who experience severe mental illness may find that they fail to acquire or lose the skills and confidence required to live as independently as they would wish.
Extended admissions to inpatient services compound this situation and make it more difficult for people to transition out of a mental health hospital and back into the community. This can in turn impact on their sense of belonging and recognition as local citizens.
For some people, the reduction of distressing symptoms may be all they need to enable them to regain their skills and confidence.
However, many others will also need specific and skilled rehabilitation support and intervention.
Robust community-based mental health rehabilitation services can positively impact on the distress and disruption experienced by individuals and their families.
All people with severe mental illness who need community mental health rehabilitation should be able to access effective early and preventative intervention, so that fewer of them need inpatient care or stay in hospital longer than is necessary.
Community mental health rehabilitation services should be commissioned to wrap around the person, their loved ones and the wider services that are providing support, to ensure continuity of care and prevent risks associated with taking a siloed approach to care delivery.
5.1 Access to appropriate services and support
“…the service believed in me, I didn’t feel other teams did. I was given a chance. I really appreciate it as I’d still be in hospital now if not.” (person accessing community mental health rehabilitation service)
Commissioners should ensure that the community mental health rehabilitation offer is clear and well communicated: what is available, from whom, where and when.
Services should be available in a variety of locations, and in settings that are culturally appropriate and accessible for the population they serve.
Commissioners should have a clear understanding of what services and support are already available locally to people with a mental health rehabilitation need, and what services, based on their local population needs’ assessment, they need to commission.
Their local needs assessment should consider the past, current and projected needs of people to understand how extensive commissioned packages of care in the community could support them to live more independently or in a less restrictive environment, and how they can be made as easily accessible to people as possible.
This should include people with:
- identified mental health rehabilitation needs in Level 1 and 2 inpatient rehabilitation services within and outside the locally commissioned pathways
- complex psychosis or other severe mental illness who require frequent admissions to mental health inpatient services or may get ‘stranded’ in mental health acute inpatient care, including the specific needs of autistic people, people with a learning disability and those described as being in ‘locked rehab’
Identifying and tackling potential barriers to easy access for people, such as complex referral processes, internal referral forms and discriminatory criteria, is essential; people and families must not be expected to navigate to or find alternative services on their own or left without an appropriate offer of support.
Where it is determined that community mental health rehabilitation services are not best placed to meet an individual’s needs, the reason should be clearly articulated and appropriate support and signposting provided.
There are 4 ‘layers’ of support in the community:
- At the centre or starting point for commissioners and providers is collaborating with people who need mental health rehabilitation support to increase their choice and control and identify the strengths and talents that they and those who know and love them bring.
- The range of community assets across the system that people with mental health rehabilitation needs can draw on. Resources are often provided by the VCFSE sector and include support with employment, housing and supported living, social prescribing and benefits advice. These provide a ‘foundation’ for all citizens and complement those services provided by primary care and social care. It is therefore important that community rehabilitation services reach out to these services to ensure they are accessible to people who have rehabilitation needs.
- Mental health rehabilitation interventions commissioned by integrated care boards (ICBs) as part of the core business of all community mental health, learning disability and autism teams and services. These should include access to skilled multi-agency practitioners that help people meet their individualised goals by recovering the skills, functions or confidence they may have lost or failed to acquire due to the impacts of severe mental illness.
- Beyond this is tertiary community mental health rehabilitation provided as an integral part of a local rehabilitation pathway where a person’s needs can be met outside hospital. This should include specific rehabilitation intervention, in-reach into mental health rehabilitation and acute inpatient care (including for autistic people and people with a learning disability), and the offer of rehabilitation formulation should be followed by advice to and consultation with the wider system. This level of support has the particular benefits of reducing transitions, facilitating early discharge and providing a link to the community.
No one type of community mental health rehabilitation support is mutually exclusive of another.
As people’s needs change, they may require mental health rehabilitation delivered in different ways and at a different intensity.
It is important that people have access to the right intervention, at the right time and in the right place.
Offers of support and provision must work together seamlessly to avoid interruptions across the pathway or gaps that disadvantage people.
5.2 Assessment and planning
Commissioners need to ensure that all community mental health rehabilitation services use a broad range of assessments to identify a person’s strengths, needs and aspirations and inform a personalised, strengths-based, recovery orientated and trauma-informed intervention plan.
Tertiary community rehabilitation services should be able to support the use of rehabilitation assessments in the wider system.
If a person requires an assessment that can only be provided by a tertiary service, the intervention it links to should have a clear purpose in optimising functioning, wellbeing and time spent in the community.
Rehabilitation assessments may include:
- daily living skills
- social functioning or participation in relationships with friends and family
- communication
- cognition
- sensory needs
- primary needs, including housing, finances or debt, safety
- vocational skills and aspirations
- symptoms or psychological needs
- hope, identity, meaning and empowerment
- substance misuse
- physical health
- physical activity
- side effects of medication
- specific risks
PROMs should be used to support shared decision-making and provide people with opportunities to explain how they are feeling, focus on what matters most to them and identify the progress they are making. Where appropriate, the views of carers should also be sought.
Statutory assessments should also be used, where appropriate, to help determine needs and support requirements, including capacity assessments under the Mental Capacity Act 2005, carer assessments under the Care Act 2014 and social care needs assessments for those eligible for Section 117 aftercare under the Mental Health Act 1983.
Commissioners should ensure that the rehabilitation offer reflects these assessments, harnesses existing information – for example, the electronic patient record, professional and multi-agency discussions – and, importantly, the views of the person and their family and/or carers.
The purpose of the intervention, when it is anticipated that it will be achieved, and who is responsible for delivery should be clear to all parties.
“The service is really clear about timescales…realistic about how long things might take, this is really helpful.” (a person being supported by a community mental health rehabilitation service)
5.3 Interventions
“They helped me look at a college course…did it alongside me…it’s good to have a friendly face to help me do these things.” (a person being supported by a community mental health rehabilitation service)
Community mental health rehabilitation services should be commissioned to provide a range of interventions that provide, but are not limited to, early intervention to prevent inappropriate admission to hospital for a rehabilitation need and support discharge from inpatient services in a timely manner.
These include psychopharmacological interventions, including antipsychotic medication management for people with complex psychosis, and skill development and strategies to improve a person’s functioning and wellbeing, such as the development of daily living skills, symptom or distress management, psychological therapies and family interventions.
Mental health community rehabilitation can also support a person to access and engage with physical healthcare services, education, employment, benefits and welfare support, and meaningful leisure activities and relationships, including via support from individual placement support (IPS) services and recovery colleges.
People with severe mental illness are more vulnerable to physical health conditions, and for them the promotion of self-care, health management and physical activity is essential to narrow any health inequalities (see Core20PLUS5 (adults) – an approach to reducing healthcare inequalities).
Based on identified local population health needs, commissioners should ensure that tertiary community mental health rehabilitation services have the skills and expertise to offer more intensive interventions, including peer support, social work, nursing, occupational therapy, psychology, psychiatry and pharmacy across a range of seniority and competency levels.
Consideration should also be given to offering services from other allied health professionals, especially for people with mental health rehabilitation needs and co-occurring conditions, such as those with a learning disability: physiotherapy, speech and language therapy, arts therapies and dietetics along with the full range of evidence-based psychological therapies.
5.4 Advice and liaison
Commissioners should ensure that tertiary community mental health rehabilitation provision has the capacity and capability to support and provide advice and consultation to wider services.
This should include in-reaching to mental health inpatient services for adults, autistic people and people with a learning disability.
This can enable people to leave hospital as soon as their rehabilitation needs can be met within a community setting. This in turn improves whole system flow, ensures least restrictive care and maximises the ability of local pathways to provide positive outcomes for people needing rehabilitation.
Advice and liaison should also be provided to housing, support and VCFSE providers to strengthen and scaffold existing community services.
5.5 Working collaboratively
Community mental health rehabilitation services should be commissioned to work collaboratively with health and adult social care commissioners, local authorities, housing and support providers.
This type of collaboration will help prevent any potential deterioration in a person’s mental health, respond in a timely manner to concerns and potentially avoid a breakdown in their living arrangements.
It also enables the identification of gaps in provision to facilitate discharge from hospital, or the need for a step up to prevent an admission to hospital as a result of a rehabilitation need.
“I don’t ask for help unless I really need it, but these professionals can read between the lines.” (a person who was being supported by a community mental health rehabilitation service)
Tertiary community mental health rehabilitation services should have oversight of people across the whole rehabilitation pathway and mechanisms for ensuring the person is receiving good quality care that meets their needs and, if there is a change in need or concerns expressed, that this can be addressed quickly.
They are key in providing intervention, consultation and support to help people continue to receive rehabilitation so they can stay where they live or move onto more independent living, if they can or wish to.
This not only improves the flow through supported placements, including residential care, but also through mental health inpatient services.
The lack of appropriate housing and support is regularly reported as the main barrier to discharge from hospital for people with mental health rehabilitation needs.
Increased flow through the whole rehabilitation pathway frees up local capacity so that more people can receive the right level of care and mental health rehabilitation for their needs, closer to home.
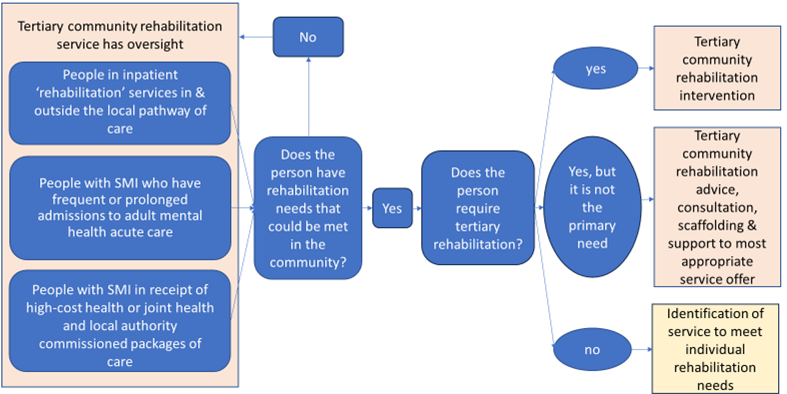
Tertiary community rehabilitation service oversight
Commissioners should consider how tertiary community rehabilitation services have oversight of:
- all people in inpatient ‘rehabilitation’ services in and outside the local pathway of care
- all people with severe mental illness who have frequent or prolonged admissions to acute adult mental health care
- all people with severe mental illness in receipt of high-cost health or joint health and local authority commissioned packages of care
For those among these who have rehabilitation needs that could be met in the community, the next consideration is whether they require tertiary rehabilitation and if they do whether this is the person’s primary need, with tertiary community rehabilitation intervention offered to those for whom it is and tertiary community rehabilitation advice, consultation, scaffolding and support offered to those for whom it is not.
For people who do not need tertiary community rehabilitation, the service that best meets their individual needs should be identified.
This consideration pathway is also shown diagrammatically below.
6. Principles for community mental health rehabilitation
6.1 ‘All means all’
“Everyone can progress, everyone should be given opportunities.” (person with experience of mental health rehabilitation)
Community mental health rehabilitation services should be accessible for all people with a mental health rehabilitation need, at every level of intensity.
No person with such a need should be excluded from community mental health rehabilitation services due to their protected characteristics or the diagnosis they have been given.
They should be commissioned with all people in mind so that all people who present with a need for mental health rehabilitation are considered fairly regardless of diagnosis, socio-economic status, gender, race or other protected characteristic.
This includes people with a learning disability, autistic people and people with complex trauma who may have been given a diagnosis of personality disorder or complex emotional and relational needs, and for whom mental health rehabilitation is the primary need.
6.2 Purposeful intervention
The purpose of intervention for each person supported by commissioned community mental health rehabilitation services must be clear and recorded.
This ensures the joint identification and prioritisation of rehabilitation needs with the person and their family and carers, and supports identification of the best evidence-based treatments and interventions for the person and their intensity.
To make best use of available resource and ensure commissioned community mental health rehabilitation is timely and responsive for people who need it, mechanisms must be in place to for regularly review the purpose of intervention and recognise when its intensity can be lowered or it can be stopped.
6.3 Data-informed community rehabilitation and system oversight
Commissioners should commission mental health community rehabilitation services based on available data and evidence, and these services should be designed and delivered based on local population needs and demographics, including ethnic background (see the Patient and carer race equality framework).
Services should proactively identify and implement findings from emerging research and identify gaps in data or research for further work through professional, clinical and improvement networks.
Where the filling of data gaps is crucial for the development of robust commissioning plans and strategies, these gaps should be highlighted locally via the relevant ICB governance structure and with system partners, regional and national NHS England colleagues.
Services should monitor the effectiveness of their service provision to prioritise areas for quality improvement and commissioners should use this data to determine the local demand and capacity needed, informing current and future commissioning.
Robust mechanisms that ensure the visibility of people with severe mental illness and mental health rehabilitation needs are essential for equitable allocation of resources and identification of opportunities with system partners to commission alternative models of care that could make better use of resources.
The ICB requirement to have oversight of all mental health inpatient activity within and outside a local pathway of care means the local demand for mental health rehabilitation will be recognised.
Commissioned services need to meet these needs, with commissioners leading and supporting their evaluation, redesign and quality improvement as and where indicated.
The inclusion of all mental health rehabilitation activity, outcome and financial data in ICB reporting structures enables financial and strategic planning to shift resource from inpatient rehabilitation to an alternative community rehabilitation offer as described in this guidance, where the need for this is indicated locally.
7. Specific considerations
People who have had lengthy admissions in mental health inpatient services due to their mental health, emotional or rehabilitation needs are likely to need an intensive support offer on discharge and some rehabilitation to readjust to community living.
7.3 People with complex psychosis
“…this service sees me weekly now and it’s with the same staff I know…that is the difference.”
(person comparing the community mental health rehabilitation service to their previous community mental health team)
Commissioners should ensure that the model of mental health community rehabilitation has a specific focus on people with severe symptoms of psychosis and functional impairment.
The service offer should align with national guidance, including the NICE clinical guideline [CG178] Psychosis and schizophrenia in adults: prevention and management and the GIRFT Programme National Specialty Report for mental health rehabilitation.
The GIRFT report identifies the potential rehabilitation needs for people with complex psychosis (including schizophrenia, bipolar affective disorder, psychotic depression, delusional disorders and schizoaffective disorder) and co-occurring conditions.
These people may also have needs relating to cognitive impairment, substance misuse, neurodevelopmental conditions, trauma, a diagnosis of personality disorder and physical health conditions.
Combined these needs can result in people requiring frequent or lengthy admissions to hospital and signficant support to live in the community; any community mental health rehabilitation service should be commissioned to meet their specific needs.
The tertiary community mental health rehabilitation service has an essential role in providing intensive intervention and specialist clinical expertise.
This along with housing and support offers can help people with complex psychosis to leave hospital at the earliest opportunity and maximise their independence and time spent in the community.
7.2 People who have experienced trauma or received a diagnosis of personality disorder
Commissioners should ensure that people who have experienced complex trauma, complex post-traumatic stress disorder or received a diagnosis of ‘personality disorder’ have equitable access to all available mental health provision as required, to meet their individual need.
There are 2 critical considerations for this:
- the provision of trauma-specific support
- an underpinning trauma-informed approach for all community mental health rehabilitation services
Commissioners should have a local clear and well-communicated plan for how a person can access evidence-based trauma-specific support, including psychological therapies, care and treatment, and whether this will be provided through the community rehabilitation service or access to talking therapies or dedicated complex trauma services.
Peer support may also be effective in minimising the impacts of trauma or emotional needs on the person’s functioning, promoting citizenship and hope.
Care must seamlessly wrap around the person, and there should be formal arrangements for and a clear service specification detailing the specific interventions, including processes for cross-service working.
All commissioned mental health community rehabilitation services, including how care and support are organised and delivered, should be underpinned by a trauma-informed approach.
This underpinning trauma-informed approach creates compassionate recovery environments for staff, survivors, their friends and allies and recognises the importance of relationships.
It acknowledges that all demographics of society experience trauma and that these experience impact not only on people using services, but also staff, allies, families and others.
7.3 Reasonable adjustments
“Communication works well and is planned around me.” (person being supported by a community mental health rehabilitation service)
To optimise access to and engagement with commissioned community mental health rehabilitation for all, commissioned services should identify a person’s needs and preferences and provide reasonable adjustments as required.
Careful consideration should be given to the physical and sensory environments where interventions are delivered, how the right level of information is communicated to meet individual needs, and how interventions and support are planned for and organised.
For people with requirements that are beyond what can be addressed with reasonable adjustments, services delivered by staff with the necessary skills and expertise may need to be commissioned.
7.4 People with a learning disability and autistic people
When commissioning community mental health rehabilitation services to meet the needs of autistic people, autistic people with a learning disability and people with a learning disability with severe mental illness, commissioners should stipulate that providers:
- use an existing health passport, written summary or reasonable adjustment checklist to inform the care and support plan and how services should communicate with the person
- in the absence of this information, work with the person and their chosen carer(s) to identify individual needs or differences relating to communication, interaction, routine, repetition, predictability and the sensory environment, and record these on the person’s electronic patient record and share with other agencies involved in the person’s care
- use NDTi’s Green Light Toolkit to audit and improve community mental health rehabilitation services so that they are effective in supporting autistic people and people with a learning disability
- for people aged up to 25 who have an education, health and care (EHC) plan, ensure this informs the community mental health rehabilitation plan
- confirm that people in the community and at risk of admission to a mental health hospital are included on local dynamic support registers and have a Care, Education and Treatment Review (CETR) in the community before any admission (or if this is not possible, within 28 days of admission), to inform care planning and delivery
- ensure that all staff working in these services have attended mandatory training on learning disability and autism appropriate to their role, in line with the Health and Care Act (2022) and including The Oliver McGowan Mandatory Training on Learning Disability and Autism
Commissioners should also consult the Royal College of Psychiatrists’ Quality network for community learning disability services standards.
8. Care pathway and interdependencies
8.1 Commissioning continuous care and ensuring seamless transitions
“We have access to a good resource and can get through to someone quickly if we need to.” (family member of a person being supported by a community mental health rehabilitation services)
A whole pathway approach to commissioning community mental health rehabilitation services is needed to ensure that transitions are kept to a minimum and there is continuity of care.
Commissioners should ensure that services work collaboratively, people can have their individual needs met flexibly and that pathways of care and support are efficient and clearly described in the commissioning strategy for their population.
Strong links and relationships between the commissioned community mental health rehabilitation service and key stakeholders are essential for maximising positive outcomes. These stakeholders include:
- the person receiving mental health rehabilitation and their family and carers
- primary care and any physical health services involved in the person’s care
- inpatient mental health, learning disability and autism and community services
- local authorities and adult social care services
- community provision – for example, forensic services, complex emotional needs services, early intervention in psychosis services, services providing assertive outreach or intensive support
- wider community provision, including housing and support providers, VCFSE organisations and individual placement support services
- children and young people’s inpatient and community services for those young people transitioning to adult mental health community rehabilitation services
8.2 Joint working
Commissioners should ensure that the service specification in the contract describes the requirement for joint working.
The standard operating procedures (SOPs) providers develop from this specification should detail how relevant services will work together and how universal support offers in the community will be identified and used to support people in their recovery journey.
SOPs should also cover how the provider maintains relationships, shares information, evaluates the effectiveness of community mental health rehabilitation services, and identifies risks, mitigations and areas for quality improvement.
Commissioners should be assured that the service specification is operationalised appropriately, through contract review meetings.
Commissioned services should have routes for escalation and system support and define the process for a person to access the right intensity of community mental health rehabilitation at the right time for them.
All people who access community mental health rehabilitation must have a key worker with the required competencies to co-ordinate their care in line with the community mental health framework.
Commissioners should be clear that the key worker role needs to be allocated to a nominated person who will maximise continuity of care and escalate any issues. This person can be external to the intensive community mental health rehabilitation provision.
Commissioners should ensure that tertiary community mental health rehabilitation services are consulted on all referrals to inpatient rehabilitation units, to ascertain if the person’s mental health rehabilitation needs could be met in the community and to inform the purpose of admission if the person does have a need that can only be addressed in hospital.
By remaining involved in the regular review of the person’s purpose of admission, the tertiary community mental health rehabilitation service can help identify and resolve any barriers to discharge to facilitate this at the earliest opportunity.
Community mental health rehabilitation services should also work with adult mental health inpatient services, including those for autistic people and people with a learning disability, to develop a viable aftercare plan for each person being discharged.
They should also be involved in multi-agency discharge events (MADE meetings) to provide mental health rehabilitation advice and liaison.
This collaborative approach supports efficient flow through services, maximising local mental health inpatient capacity for those who need it.
9. Involvement, co-production and advocacy
Commissioners should have a clear and transparent plan for consulting and engaging people with lived and living experience and their families, to ensure they take a consistent approach in maximising and facilitating the co-production of how services are commissioned and delivered.
This includes creating appropriate structures to ensure that lived and living experience, including that from compliments, complaints and informal feedback, informs service reviews, developments and improvements.
Commissioners need to ensure the services they commission do not inadvertently marginalise any groups due to factors such as social deprivation, digital poverty, cognitive functioning, ethnicity or living in a rural community.
Employing a range of approaches and locations to communicate with and listen to the voice of people and families is key in mitigating this risk, along with providing appropriate reward, recognition and reimbursement, as described in the NICE guideline [NG44] Community engagement: improving health and wellbeing and reducing health inequalities.
Service specifications for community mental health rehabilitation services and support should clearly articulate access to commissioned independent advocacy services.
Additionally, some people who meet certain criteria under the Mental Health Act 1983, Mental Capacity Act 2005 or Care Act 2014 may also be entitled to support from a social care advocate.
10. Workforce
10.1 Skilled and competent workforce
“Ensuring the right workforce with the right training, and hence skill set, can support improved patient care, treatment, and outcomes.” (GIRFT report on mental health rehabilitation)
Services need to be commissioned in a way that ensures they can provide people with the right intensity of support to meet their needs.
This means having the appropriate expertise and competencies available, including access to health and social care professionals to deliver evidence-based interventions, practitioners to provide housing and financial support, and people with lived and living experience delivering peer support.
Commissioned services will be expected to have robust workforce training and development plans in place and, as a minimum, these should cover:
- motivational interviewing
- understanding and responding to substance misuse
- psycho-social intervention, where available
- cognitive behavioural therapy (CBT)
- family interventions
All staff working in commissioned tertiary community mental health rehabilitation should be able to access the training and supervision that enables them to work with people with complex and co-occurring needs, fluctuating capacity, and relapsing and remitting mental health conditions, and to use trauma-informed and recovery orientated approaches.
Where gaps exist in specialist training for staff working in tertiary community rehabilitation services, a training needs analysis should be undertaken to understand and address them.
10.2 A diverse multidisciplinary team
Commissioned services require a workforce that comprises a range of disciplines with the experience to deliver the core and specialist skills and knowledge required.
The diversity of teams should reflect the community they service and harness the talent and expertise from the range of partner agencies and organisations within the system.
The tertiary community mental health rehabilitation workforce should include a range of multidisciplinary and multi-agency staff based on population need, including but not limited to:
- peer support workers
- occupational therapists
- psychiatrists
- nurses
- social workers
- psychologists
- pharmacists
- housing and benefit support workers
- physical health promotion practitioners
VCFSE organisations are key in ensuring connection to the community and promoting belonging and citizenship.
Commissioners should refer to the work of professional bodies, royal colleges and other relevant organisations in defining the different roles within community mental health rehabilitation services. For example, the Royal College of Occupational Therapists’ informed view of the role of occupational therapists and the joint NHS and National Collaborating Centre for Mental Health community mental health framework for adults and older adults.
10.3 Workforce challenges
Workforce challenges include the recruitment and retention of staff, and their wellbeing.
To mitigate their potential impact on the capacity and delivery of commissioned mental health rehabilitation services, commissioners should ensure that providers support their staff, including peer support workers, to access appropriate clinical, professional and managerial supervision, acknowledging that supervision structures may need to extend beyond specific services or organisations.
Mental health rehabilitation practitioners also benefit from access to peer support and professional and clinical networks at a system, regional or national level, to drive quality and share emerging research findings and best practice.
Commissioners should be confident that the services they commission have identified routes for career progression, including through the use of apprenticeships, advanced clinical practice and the development of non-medical approved clinician, responsible clinician and consultant roles.
10.4 Peer support workers
“…being a peer support worker is my passion, it brings me unmeasurable joy… I share my own experience of rehabilitation… instil hope and show that there’s a light at the end of the tunnel…. I let people know that mental illness is not a life sentence.” (peer support worker with lived experience of mental health inpatient rehabilitation)
Peer support workers are an essential part of the community mental health rehabilitation workforce.
They help instil hope of recovery in people receiving community rehabilitation, increasing their sense of identity, belonging and social inclusion in the community.
Peer support workers should have a well-defined and clearly communicated role within the service offer, one that differs from that of volunteers or self-advocates.
Commissioners need to be clear that the staffing establishment for commissioned services includes peer support workers and these workers have the infrastructure for them to flourish, including a salary commensurate with their expertise, training and career development opportunities (such as formal professional training through apprenticeships or developmental posts) and peer support networks.
11. Quality
Commissioners should have oversight and assure themselves of the suitability and quality of placements and rehabilitation services.
For this they will need to collaborate with social care commissioners, especially where services may be jointly commissioned.
Contracts for mental health community rehabilitation services should include clear key performance indicators that enable commissioners to monitor quality and effectiveness.
These indicators should include metrics relating to workforce, such as staff wellbeing, vacancies and sickness absence.
Where appropriate, service specifications in contracts should align with the Commissioning framework for mental health inpatient services and consider the mental health community framework roadmap (on the FutureNHS Collaboration Platform; login required) and relevant NICE guidance.
Commissioners should have mechanisms in place for assuring the safety, quality and compliance of community mental health rehabilitation services against the commissioned specification.
These should include review of all available information, including CQC inspection reports and action plans.
In relation to services as part of the community mental health rehabilitation pathway, commissioners should be aware that the CQC only inspects the care of people receiving regulated activities.
Supported living placements registered with the CQC will often only provide regulated activities to some of their residents.
The CQC inspection findings and ratings for their service will then only be representative of the quality of the service for people receiving regulated activities and not the whole service.
Commissioners should ensure that commissioned services embed the use of PROMs in routine care. As well as to track a person’s progress, these are key enablers for providing person-centred purposeful intervention and evaluation of the service offer.
The ‘I ‘statements from the ‘I and We’ statements in the commissioning framework for mental health inpatient services are equally applicable to community mental health services.
They should be embedded in commissioned community mental health rehabilitation services to ensure people accessing services are asked whether their individual experience tallies with these statements.
Providers should collate and regularly report this service user feedback to commissioners, alongside compliments, complaints, incidents and any quality concerns, and commissioners should use this information to inform the commissioning of community mental health rehabilitation to provide personalised, high quality and least restrictive care and support.
Commissioners need to work with providers to improve the data reporting for people accessing community mental health rehabilitation.
Good quality community service data can identify any unwarranted variance in or unintended consequences from the community mental health rehabilitation services and whether:
- numbers of people receiving rehabilitation in the community are increasing
- numbers of people moving to more independent living are increasing
- fewer people with rehabilitation needs are having to move home after an admission to hospital
- more people in the community are achieving their identified purpose of community rehabilitation intervention
Viewed against mental health inpatient data, it should be possible to determine the impact of community mental health rehabilitation services are having in:
- reducing reliance on inpatient care (adult mental health, learning disability and rehabilitation)
- reducing time spent in hospital for people with rehabilitation needs through fewer admissions or shorter length of stay
- eliminating the commissioning of outdated models of inpatient care or inpatient services that sit outside the locally commissioned pathway of care
- reducing over-represented groups defined by protected characteristic within mental health inpatient services
Appendix: Task and Finish Group Membership and acknowledgements
We would like to acknowledge the essential support of the Task and Finish Group in developing this guidance:
- Clair Haydon (Co-Chair) Cheshire and Wirral Partnership NHS Foundation Trust
- Debra Moore (Co-Chair) Mental Health, Learning Disability and Autism Quality Transformation Team, NHS England
- Dr Sheraz Ahmad East London NHS Foundation Trust
- Tristan Batten Expert by experience, Leeds and York Partnership NHS Foundation Trust
- Jon Bell Expert by experience
- Jason Brandon Department of Health and Social Care
- Ian Davidson GIRFT and Cheshire and Wirral Partnership NHS Foundation Trust
- Louise Davies Independent expert advisor – commissioning
- Russell Dunmore Midlands Region Mental Health Team, NHS England
- Conor-Eldred Earl Expert by experience, Mental Health, Learning Disability and Autism Quality Transformation Team, NHS England
- Kelly Fenton Leicestershire Partnership NHS Trust
- Joe Gavin Expert by experience
- Dr Sri Kalidindi GIRFT and South London and Maudsley NHS Foundation Trust
- Jo Kirk Midlands Region Mental Health Team, NHS England
- Clare Mayo Greater Manchester Integrated Care Board
- Jacqui Mowbray-Gould Mental Health, Learning Disability and Neurodiversity (MHLDN) Provider Collaborative
- Dr Asha Praseedom Royal College of Psychiatrists
- Kathy Roberts Association of Mental Health Providers
- Dr Amrith Shetty Cheshire and Wirral Partnership NHS Foundation Trust
- Clare Smyth Adult Mental Health Team, NHS England
- Paula Swift Tees, Esk and Wear Valleys NHS Foundation Trust
- Sam Whitewood Southern Health NHS Foundation Trust
- Tonita Whittier Mental Health, Learning Disability and Autism Quality Transformation Team, NHS England
- Emma Whittingham-Berry Care Quality Commission
- Emily Williams National Learning Disability and Autism Team, NHS England
In addition, the guidance has built on broader engagement through workshops, stakeholder groups and visits to community mental health rehabilitation services across the country, and we thank all the people involved in these.
We are particularly grateful to the people with lived experience of mental health services and their families who gave their time and shared their stories, insights and expertise so generously.
Publication reference: PRN01190

