Equality and health inequalities statement
Promoting equality and addressing health inequalities are at the heart of NHS England’s
values. Throughout the development of this strategy, the project team have:
- Given due regard to the need to eliminate discrimination and harassment, to advance equity of opportunity, and to foster good relations between people who share relevant protected characteristics (as cited in the Equality Act, 2010)
- Given regard to the need to reduce inequalities between patients in the access to, and outcomes from healthcare services and to ensure services are appropriate, meaningful, responsive and are provided in an integrated way where this might reduce health inequalities.
Foreword
Our inaugural allied health professions strategy for England AHPs into Action (2016/2017–
2020/2021) underlined the key role the AHP community plays in enabling people to live full,
active lives within their family, community and workplaces. It also articulated how AHPs could
be deployed to transform health, care and wellbeing.
So much has changed in the last five years. We know we face challenges within health and
care in striving to deliver quality care to all people and communities. We also know that the
pandemic has highlighted – and even widened – the health inequalities experienced by those
the AHP community works with and alongside. During this unprecedented time, the AHP
community has been innovative across a variety of settings – the NHS, social care, education,
academia, research, voluntary and private sectors.
Our strategy for the next five years, The AHP Strategy for England: AHPs Deliver, captures
the voices of diverse people and communities. This is intentional: they are central to
everything the AHP community plans and delivers, and we continued our co-production
commitment through to the final drafting of the strategy. We have again creatively used
crowdsourcing to generate collective insight and layered this with focused activities with
groups who may experience digital exclusion. To every person and group who has been part
of this process I express my sincere gratitude. We have included quotes from some of you
throughout this document.
This strategy is a catalyst for change. Wherever you work, every member of our AHP
community has a part in realising our collective ambitions through its delivery. I therefore
encourage you to take a moment to consider how the AHP community can enable the
change required to deliver future care today.
Suzanne Rastrick OBE
Chief Allied Health Professions Officer (England)
Summary
Collectively, allied health professionals (AHPs) are the third largest clinical workforce in the
NHS: 185,000 allied health professionals (AHPs) in 14 professions are working across the
spectrum of health and care, education (including early years), academia, research, criminal
justice system, voluntary and private sectors. From prevention to specialist care provision,
AHPs deliver care to individuals, groups and, in some cases, specific populations of children
and older adults. In 2016 NHS England published the first AHP strategy, AHPs into Action
(2016/2017–2020/2021), a framework demonstrating the transformative potential of this
workforce in supporting the NHS. The strategy set out the collective commitments and
priorities for AHPs to deliver significant improvements for people who access services, their
carers, and communities, evidenced in 53 case studies.
The NHS Long Term Plan acknowledges the essential role for AHPs in supporting the NHS to
meet demand. As instructed by this plan (p82, section 4.20), The AHP Strategy for England:
AHPs Deliver builds on its predecessor, accentuating the impact AHPs have on delivering
excellence in health and care.
This new strategy is for the whole AHP community: support workers, assistant practitioners,
registered professionals, pre-registration apprentices and students. It is inclusive and reflects
how AHPs work in multidisciplinary teams, so that those who identify as part of the AHP
community working in a variety of health and care sectors can use it to continually improve
and redesign services.
We have scrutinised the experience and impact of COVID-19 on our diverse AHP workforce
and people who access services in the development of the strategy, embracing all
opportunities for learning.
We have co-designed the strategy with these groups, receiving over 21,000 contributions
from people who access services, carers, the public and health and care staff, including
AHPs, to a digital platform (crowdsourcing) and running workshops with groups who may
experience digital exclusion, including underrepresented communities. Appendix 1 lists the
other data and evidence we have used in formulating the strategy.
Impactful, inclusive leadership at every level (national, regional, system and provider) and
down to every individual AHP community member is crucial for AHPs to continuously improve
their contribution to high-quality health and care services.
Building on the legacy of AHPs into Action, this strategy for the next five years, gives the AHP
community at a system, team and individual level permission and authority to act and fully
realise their transformative potential.
Introduction
The context
Allied health professions (AHPs) form the third largest clinical workforce in the NHS and are professionally autonomous practitioners educated to at least degree level standard. They comprise of 14 distinct occupations: art therapists, dietitians, drama-therapists, music therapists, occupational therapists, operating department practitioners, orthoptists, osteopaths, paramedics, physiotherapists, podiatrists, prosthetists and orthotists, diagnostic and therapeutic radiographers, and speech and language therapists. (NHS England (2022) Allied Health Professions (AHPs))
AHPs provide system-wide care: they are involved in assessing, treating, diagnosing and discharging patients across health, social care, housing, education, early years, schools, the criminal justice system, independent and voluntary sectors. Through adopting a holistic approach to health and care, AHPs can support and manage people’s care from birth to end of life. They focus on the prevention of ill-health alongside improving health and wellbeing to maximise the potential for people to live full and active lives within their family circles, social networks, education/training settings and the workplace.
Strategy purpose
The Allied Health Professions (AHP) Strategy for England: AHPs Deliver, has been developed to provide strategic direction to the AHP community across England, to help the AHP community and those they work with maximise their contribution to the aim of improving health outcomes for all, providing better quality care, and improving sustainability of health and care services. During the lifecycle of the strategy it will be important that the AHP community continue to build on the innovation demonstrated throughout the pandemic and apply this learning to the challenges services now face in recovering.
Overview of the four sections of this strategy
Section 1: The strategy principles of anti-racism and co-production
This strategy makes an overarching commitment that the AHP community will be anti-discriminatory and anti-racist in its approaches, using co-production to ensure actions are inclusive.
Section 2: Reflecting on the achievements of AHPs into Action
Through our wide engagement we know AHPs into Action has had impact – many of the transformations it has achieved are now considered to be business as usual; others have scope for further growth.
Section 3: Four enhanced foundations
The four priorities – described as ‘enhanced foundations’ – remain the same as in the first strategy but they have been further refined and are supported by updated frameworks and policies.
Section 4: Five areas of focus
Five ‘areas of focus’ have been identified for the next five years, each complemented by a set of ambitions.
Implementation
The AHP Strategy for England: AHPs Deliver is underpinned by an implementation framework that adopts an appreciative inquiry approach to support individuals, providers, systems and regions to map where they are in 2022, where they need to focus their activities during the term of this strategy, and how improvement will be measured and celebrated. This will support the central teams in NHS England, Health Education England and the Office for Health Improvement and Disparities (OHID) regional and local teams to identify where the strategy links with their respective workstreams, work priorities and activities.
Language and terminology
This strategy acknowledges the complexity of the concepts, meaning and terminology used when describing patient, public involvement and engagement. There is no universal term to describe those who engage with health, social and wider care organisations, and systems. As advised by consultation feedback and specific work with underrepresented groups and communities, we refer to ‘people’ and ‘people and communities’ throughout this strategy, not ‘citizens’.
“I don’t like the use of the term, citizen. It can have lots of different meanings and can feel excluding.”
Anon, February 2021. Quote: Contributed to Underrepresented Community workshop one.
“Citizen has the wrong connotation, this makes it sound like only British citizens should have a say. As a woman who was not born in the UK but has worked in the NHS for 12 years, this reads poorly.”
Anon, June 2021. Quote: Contributed to online conversation three.
This strategy also adopts the NHS Race and Health Observatory five principles for writing about race and ethnicity: no acronyms, specific, context, transparency and adaptability. We use the terms ‘ethnic minority’ and ‘people who experience ethnic health inequalities’ to refer to those who identify as ‘non-white British’ but acknowledge homogenous terms cannot capture the multitude of experiences and cultures. Language evolves and our phrasing may not be acceptable over the life of the strategy; this is something the office for the Chief AHP Officer (England) will keep under review.
Section 1. AHPs Deliver: Overarching principles
The NHS Constitution states that the NHS is for everyone and the NHS will not treat anyone unfairly. In accordance with the Equality Act (2010), which includes the Public Sector Equality Duty (PSED), it is a responsibility for everyone who works in the NHS to respect the human rights of individuals. The NHS also has a wider social duty to promote equality through the services it provides, paying particular attention to sections of society where improvements in health and life expectancy are not keeping pace with the rest of the population.
A strong theme from consultation feedback indicated that the AHP community must deliver services in a non-discriminatory way. The Chief AHP Officer is committed to ensuring that all services are delivered in a fair and equitable manner, taking into account the protected characteristics and intersectionality of all individuals concerned. Over the life of the strategy we will undertake focused activities to understand the particular needs of those with protected characteristics and use this work to take focused action.
This section focuses on being anti-racist. This is our starting point and in addressing racism we should help develop a culture where nobody with another protected characteristic faces discrimination.
Committing to being anti-racist
Racial inequality exists. The pandemic has further highlighted the social injustices faced by people and communities who experience ethnic health inequalities.
Addressing these inequalities – both in the community and within the AHP workforce – will be fundamental to achieving the triple aim of improving health outcomes for all, delivering safe and high-quality services, and doing so in a sustainable way.
AHPs recognise that they must play an active role in addressing societal, systemic and everyday racism within health and care. AHPs need to tackle racism in all its forms – for all those we care for and our colleagues, to create a fair and inclusive workplace that values each team member and allows everyone to succeed.
Within our AHP community we see racial inequality in the underrepresentation of minority ethnicities in our AHP workforce, particularly in decision-making and leadership positions, (13% of AHP are from an ethnic minority background, with their representation ranging from 6.8% to 23.5% for the individual allied health professions.) At senior levels representation is as follows: Band 8c: 8%; Band 8d:12%; Band 9: 17% (August, 2021) as well as educational attainment gaps for AHP students.
The AHP community is committed to achieve real and lasting change for ethnic minority AHPs, communities and people, through proactive challenge, advocacy and collaboration. The anti-racism statement in this section sends a clear and consistent message that racism will not be tolerated. Those who sign up to it commit to being anti-racist by:
- Not tolerating racist behaviour and calling out racism including micro-aggressions
- Educating people on what being anti-racist means
- Addressing racial inequality, improving opportunity plus access to services and employment progression for underrepresented groups in the AHP community
- Being an ally by realising privilege exists, being proactive in their own education and taking action to amplify the voices of under-represented people and communities.
“To stop recycling racial inequity and hence health inequality the workforce has to widen its knowledge and evidence gathering further than the global north. We need to do this because the western centric ideas have done little to change the experiences of black and minority ethnic, LGBTQIA+, disabled and gypsy/traveller/Roma population’s health and social determinants outcomes.”
Anon, June 2021. Quote: contributed to online conversation three.
“We serve a diverse population which bring unique challenges, in order to address these challenges effectively we need the decision-making table to represent the community it services.”
Anon, June 2021. Quote: contributed to online conversation three.
Co-production
Co-production of services is much more than consulting people; they have an equal part in service conception, design, steering and management. Capturing the voice of people and communities who access health and care in England has been a commitment throughout the development of The AHP Strategy for England: AHPs Deliver (see Appendix 1).
We used co-production right from when we started developing the strategy to ensure diverse voices, including those of underrepresented communities, were represented, e.g. those who have experienced homelessness, those who have experienced the criminal justice system, travelling communities, refugees. It is their insights that have shaped the strategy.
Just as the strategy development ensured co-planning and co-design, the implementation of this work will require co-implementation and co-evaluation between people, the AHP community and wider health and care professional groups. For this we will use the model proposed by Roper, Grey and Cadogan, (Coproduction putting principles into practice) which defines co-production as the intersection between co-planning, co-design, co-implementation and co-evaluation.
That this strategy has been co-produced will ensure health and care stakeholders are involved in leading the design and delivery of solutions to meet the changing needs of health and care, evaluating the outcome at all levels. We will ensure that AHPs remain connected to the strategy’s progress and their continued involvement in co-implementation and co-evaluation using a variety of ways to communicate with them across systems, regions and nationally; these will also encourage networking and sharing of best co-production practice.
“This is a visionary project. The way you are ensuring a wide range of people and community voices are captured is to be applauded. Thank you AHPs.”
Anon, March 2021. Quote: Older People Sounding Board Focus Group.
“Thank you for including us from the start of this work. Often, we are an afterthought despite being considered underrepresented communities.”
Anon, July 2021. Quote: Underrepresented Communities’ workshop.
Section 2. AHPs into Action and the 2021 Consultation
AHPs into Action set out our collective priorities and commitments to improve outcomes for people, carers, communities, and populations. It provided a blueprint to support system leaders to decide how AHPs can most effectively deliver their services.
Our priorities to meet the challenges of changing care needs:
- AHPs can lead change
- AHP skills can be further developed
- AHPs evaluate, improve, and evidence the impact of their contribution
- AHPs can use information and technology.
Our commitments to the way services are delivered:
- Commitment to the individual
- Commitment to keep care close to home
- Commitment to health and wellbeing of populations
- Commitment to care for those who care.
Our impact on the effectiveness and efficiency of service delivery:
- Improve the health and wellbeing of individuals and populations
- Support and provide solutions to general practice and urgent and emergency services to address demand
- Support integration, overcoming the barrier of historical service boundaries to reduce duplication and fragmentation
- Deliver evidence-based/informed practice to address unexplained variances in service quality and efficiency.
The 2021 consultation
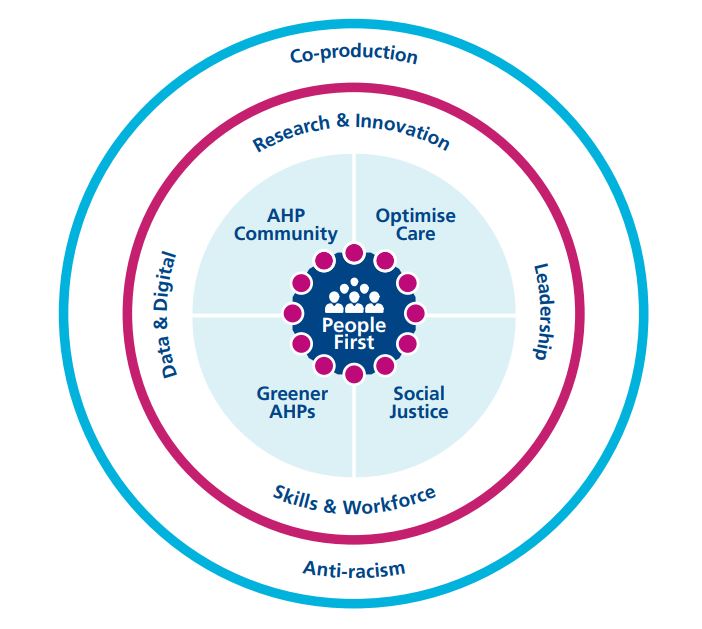
The consultation for AHPs Deliver captured the successes between 2016 and 2021 (see Appendix 2). Contributions to the online and virtual workshops emphasised that the current priorities remain relevant but with scope for expansion. These ‘enhanced foundations’ are retained in this strategy, but are reshaped as:
- AHPs champion and promote diverse and inclusive leadership
- AHPs in the right place, at the right time, with the right skills
- AHPs commit to research, innovation, and evaluation
- AHPs further harness digital technology and innovation through data.
The ‘enhanced foundations’ are the key enablers to achieving the five ‘areas of focus’ as set out in section four:
- People first
- Optimising care
- Social justice, addressing health and care inequalities
- Environmental sustainability: Greener AHP
- Strengthening and promoting the AHP community
The rationale for each of the ‘enhanced foundations’ and ‘areas of focus’ – and the corresponding actions – are covered in the following sections.
Section 3. AHPs Deliver: Enhanced foundations
The retained but reshaped ‘enhanced foundations’ are the critical enablers to achieving the new five ‘areas of focus’:
- AHPs champion and promote diverse and inclusive leadership
- AHPs in the right place, at the right time, with the right skills
- AHPs commit to research, innovation, and evaluation
- AHPs further harness digital technology and innovation through data.
1. AHPs champion diverse and inclusive leadership
Evidence suggests that diverse board and senior teams will increase the likelihood the NHS Long Term Plan ambitions are achieved.(Clinical leadership framework) AHPs have made great strides in demonstrating how their strategic leadership has impacted on workforce transformation, change/improvement activity and staff engagement – at local, regional and national levels.(Investing in Chief Allied Health Professions leadership) We can go further. As committed to in the NHS People Plan, AHPs will continue to champion diverse and inclusive leadership, improving representation from those with protected characteristics and all our different professions, by gathering the evidence and working with the system to realise the workforce’s potential. It is crucial that AHPs build the diversity of their leadership, step into these roles and are representative of the people and communities they work alongside.
Diverse AHP leadership can transform an organisation and system by focusing the engaged, productive and visible AHP workforce on trust, local authority and system priorities. It is essential that providers recognise the sustained cultural shift needed to remove outdated practices that prevent AHPs from harnessing their leadership ability. By thinking differently about how leadership is developed and managed, systems and providers will maximise the contribution of the NHS’s third largest clinical workforce.(Developing AHP leaders, Principal Occupational Therapists in Adult Social Care services) This starts with AHPs at all leadership levels.
In 2018 the appointment of substantive strategic AHP leaders within provider organisations and systems was recommended to realise the full potential of the AHP community. The evidence now demonstrates that having a Chief AHP role in an organisation is crucial to the delivery of quality care.
“A non-diverse leadership team is not inspiring for the younger generation.”
Anon, July 2021. Quote: contributed to regional workshops.
2. AHPs in the right place, at the right time, with the right skills
An effective supply of new AHPs and retaining existing staff across professions and geography are imperative for robust deployment and development to ensure the system has the right workforce, with the right skills, in the right place to deliver high -quality care. The visions and priorities for AHPs to achieve this are:
- Securing the future supply through stimulating demand for AHP careers and responding to this with more places on AHP courses
- Bridging the gap between education and work by optimising the confidence and capability of students and new registrants and securing robust foundations for professional development
- Enabling the workforce to deliver and grow through AHP deployment that recognises the needs of the system and the population. To realise this, AHPs must be supported and retained, including by supporting the development of all staff, developing talent pipelines, addressing discrimination and mitigating grievances and disciplinaries. Career development can be championed through advancing practice(Advanced practice multi-professional framework for advanced clinical practice in England) and new roles, including medicines management, education, digital, technology, informatics and leadership
The AHP support workforce and assistant practitioners provide a crucial contribution to the provision of high-quality, life changing care across a range of providers. Developing the AHP support workforce sets out the ambitions to realise this: ensuring people have access to skilled support workers who have defined roles; support workers have access to development structures that give them opportunities to follow a rewarding career pathway; services address the current variation in support worker roles; support worker roles are at the heart of improvements in service delivery and transformation, including new models of care.
Finally, the deployment of the AHP community during the pandemic demonstrated the flexibility of AHP skills and highlighted the untapped potential within and capabilities of this group. Through the pandemic, AHPs advanced their skills and new innovative roles developed. There is a unique opportunity now to capture and further develop their expertise.
“AHPs have proven to be successful boundary pushers and innovators for the benefits of patients in many different ways. Advancing practice, consultant practice, collaborative working, research, new pathways.”
Anon, June 2021. Quote: contributed to online conversation three.
3. AHPs research, innovate and evaluate
Innovation is critical to achieving the ambitions set out in the NHS Long Term Plan. That AHPs are innovators has been demonstrated through the pandemic. Research is key to ensuring safe evidenced-based practice to support patients and patient pathways. It is also important to strengthening the evidence base, to inform service design, clinical reasoning and shared decision-making with the people and communities we work alongside.The co-produced Allied Health Professions Research and Innovation Strategy makes the following vision statements, which align with the priority agendas in national health, care and wellbeing strategies:
- Transformation of AHP professional identities, culture and roles
- Delivery of excellence in evidence – based AHP practice
- National strategic research agendas and priorities explicitly inclusive of allied health research and innovation
This strategy provides a framework to drive AHP research and innovation, enhancing its visibility, reputation, influence and impact on services. This includes research with and alongside diverse communities to understand the need for and potential impact of AHPs.
The strategy encompasses building capacity and capability, including by engaging with third-sector organisations to understand people and community needs, and addresses the significance of context and culture. These four aspects are inter-dependent, and each is essential to achieve transformational impact and sustainable change.
“Research needs to be built up from grass roots, from undergraduate experience onward and role models developed who can support staff. Roles do not have to be research only. Research needs to be embedded in portfolio roles which also include clinical work, education and leadership. AHP research opportunities and culture need to be developed and spread across all organisations.”
Anon, June 2021. Quote: contributed to online conversation three.
4. AHPs can further harness digital technology and innovate with data
Digital technology and data are critical for the transformation of care. In 2019, the Topol Review stated that the UK had the potential to become a world leader in healthcare technologies and anticipated how technology innovation would impact the roles and functions of health and care staff over the next 20 years. Published in the same year, A digital framework for allied health professionals, as well as focusing on the AHP workforce also sought to support local services and AHPs to work towards services that are paper-free at the point of care and well-connected to other services and systems. The framework outlined three core ambitions for AHP services that support the development and implementation of local digital roadmaps and use of digital maturity assessments:
- Creating digitally ready AHP services: focusing on digital leadership, digitally ready AHPs and AHPs in clinical informatics addressing the use of digital capabilities, integration, interoperability and digitally – enabled AHP services
- Developing digitally mature AHP services: calling on AHPs to ensure that the adoption of new technologies and processes, and the services data from these, leads to improvements
- Supporting data – enabled AHP services.
Over the next five years, the AHP community must advance the implementation of the AHP digital framework. AHP community expertise must be engaged when developing digital platforms and digitising services to deliver connectivity across the system, and AHP communities need to be supporte1d to successfully implement digital tools that optimise workforce capacity.
When considering this enhanced foundation, it will be important to think about the support people and communities who experience digital exclusion require. Digital exclusion describes people and communities who do not have the access, skills and confidence to use the internet and benefit fully from digital technology in everyday life. Any digital advances need to appraise the health inequality challenges presented by digital exclusion.
“We need to have the right digital enablers which allow AHPs to communicate across systems and with populations. AHPs have fabulous ideas around this but are not always in the right place to innovate.”
Anon, June 2021. Quote: contributed to online conversation three.
Section 4. AHPs Deliver: Areas of focus
While the enhanced foundations are the enablers for the new five-year strategy, the Chief AHP Officer is committed to five areas of focus identified in its co-production:
- People first
- Optimising care
- Social justice: addressing health and care inequalities
- Environmental sustainability
- Strengthening and promoting the AHP community.
The implementation framework for this strategy identifies how improvements in these areas will be delivered at individual, local, systems and regional levels.
Focus 1: People first
At the centre of AHPs Deliver are the people and communities who access health, care and wellbeing services. AHPs will continue asking “what matters to you?” at both individual and community level, and the AHP community will work with other health and care colleagues and beyond traditional boundaries to ensure AHP approaches are always person and community centred.
“There could be a stronger focus on collecting and utilising a range of patient experience measures, quantitative and qualitative, and really using this information to improve care.”
Anon, June 2021. Quote: contributed to online conversation three.
“I think we ought to take great care in using virtual appointments and ask people if this is what they want rather than this being the default position.”
Anon, June 2021. Quote: contributed to online conversation three.
Person-centred care is one of the seven core principles of the Constitution. Personalised care means putting people and their families at the centre of decisions and seeing them as experts, working alongside professionals to achieve the best outcome. To be person-centred, services need to be more flexible to meet people’s needs in the way that is best for them. The AHP community, by the nature of their work, have many examples of how they follow this approach. Nevertheless, there is room for further development.
Personalised care gives people and communities the same choice and control over their mental and physical health as they have come to expect in every other aspect of their life. Universal personalised care: Implementing the comprehensive model confirms how AHPs will do this. The model builds on the success of six individual, evidence – based, but previously separate components:
- Shared decision making
- Personalised care and support planning
- Enabling choice, including legal rights to choose
- Social prescribing and community-based support
- Supported self-management
- Personal health budgets and integrated personal budgets.
In addition to providing personalised care for those who need health and care services, AHPs have an important role in preventing people from becoming ill and are recognised as an integral part of the wider public health workforce. Public health approaches prioritise prevention to help the population live more years in good health, and to lessen the burden on health and social care resources, and for precisely these reasons the NHS Long Term Plan places a focus on the need for wider action on prevention. The COVID-19 pandemic has highlighted the need to embed public health approaches into everything we do.
Yet, AHP skills are often underutilised in enhancing the public health and prevention agendas. AHPs’ contribution to the reduction of health inequalities should be considered in the redesign of patient care pathways. The AHP community already works across the life cycle using their skills to enable people to thrive.
Key approaches underpinning public health include:
- Taking a population approach
- Using data and evidence to inform decisions
- Focusing on prevention
- Considering the wider, societal determinants of health and wellbeing, and focusing on reducing inequalities.
The AHP community will work with partners across systems to design pathways that emphasise prevention and early intervention to improve and protect the health and wellbeing of all communities.
The ‘people first’ ambitions are to:
- Improve the quality of and access to services
- Help people and communities get the care they need when they need it
- Ensure this care considers people’s values, family situations, social circumstances, and lifestyles; seeing the person as an individual and working with them to develop appropriate solutions through shared decision-making
- Help people, communities and populations to look after themselves (self-care), thus reducing some of the pressure on health and social services
Focus 2: Optimising care
The AHP community is committed to having the right AHPs, with the right skills, in the right place, at the right time. This needs to be underpinned by supporting and enabling AHPs to make full use of their skills and deliver consistently great care across England in partnership with those with lived and learned experience and members of the wider health and care team.
“AHPs need to be open and ready to work with other social and care agencies providing organisations in order to achieve the optimal care delivery.”
Anon, June 2021. Quote: contributed to online conversation three.
“Optimising care means that people see the right professional with the right skills at the right time, implementing new ways of working that also consider sustainability, and supporting people with prevention and self-care.”
Anon, June 2021. Quote: contributed to online conversation three.
The NHS Long Term Plan describes the predicted increase in population demands on health and care services. This, coupled with workforce growth not keeping up with need, calls for new and innovative ways of working.
As key members of the multidisciplinary team, the AHP community is ideally placed to support the development, redesign and optimisation of patient pathways for the seven programme areas outlined in the NHS Long Term Plan: maternity, children and young people (CYP); primary, social and community care; urgent and emergency care; mental health; cancer; hospital care; and healthy communities and prevention.
AHPs can contribute to innovation that realises better care for the major health conditions outlined in the NHS Long Term Plan: musculoskeletal disorders, dementia, cancer, diabetes, cardiovascular disease, stroke, respiratory disease and adult mental ill-health.
AHPs contribute across services for CYP: learning disability and autism, mental health and supporting CYP with cancer, as well as maternity and neonatal care.
The AHP community can support health and care systems recover from the pandemic with innovative solutions in key areas such as elective recovery, diagnostics, pre-rehabilitation and rehabilitation.
Any system’s resources are finite and the AHP community needs to ensure that the use of available resources is maximised to ensure high-quality, effective and efficient services, with balanced resources, high staff satisfaction and good retention. This includes embedding e-rostering and e-job planning to maximise available workforce capacity, drive effective workforce deployment and inform establishment setting, in line with the NHS Long Term Plan ambition to have evidence-based establishment setting in place by 2023. This approach will support services to identify the clinical workforce required to meet the needs of the local population. Implementation of the AHP Quality Dashboard will support workforce planning and deployment. It provides a framework to track, interrogate and respond to data on
four ambitions:
- Delivering quality care: AHPs deliver high-quality care and fully contribute their skills and experience to patient pathways
- Supporting staff: Staff are fully engaged, well-led and retained
- Optimising the workforce: The workforce has the right skill mix and capacity and is deployed to deliver maximum impact
- Improving productivity: Productivity is monitored; unwarranted variation and opportunities for improvement are identified
Focus 3: Social justice: addressing health and care inequalities
The AHP community must focus on the needs of their local communities, represent their local populations, and be vested in reducing health inequalities and improving outcomes for all. Everyone has a part to play in this – as individuals and as a collective.
“Please ensure the socially excluded and disengaged people have as much of a voice as those already empowered.”
Anon, June 2021. Quote: contributed to online conversation three.
“This crosses over both health promotion/public health, equality and diversity and patient and public participation – all of which are key and in which AHPs have valuable skills and experience to contribute. It would be good to see these being a greater part of AHP training but also opportunities for AHPs being created within these areas, as well as within their clinical practice.”
Anon, June 2021. Quote: contributed to online conversation three.
The NHS was established on the principles of social justice and equity, yet it is acknowledged that social justice is a complex concept. The Oxford Dictionary (The Oxford Dictionary for English) defines social justice as “The objective of creating a fair and equal society in which each individual matters, their rights are recognised and protected, and decisions are made in ways that are fair and honest”.
AHPs Deliver takes social justice as a starting point for exploring health inequalities and setting out the AHP community’s ambitions and contributions.
COVID-19 has increased social and health inequalities; it has had a disproportionate impact on some communities such as ethnic minorities, older people, people living with obesity and people with a disability or long-term condition. (The Marmot Review 10 Years On) It has also highlighted the important, and often invisible, carer roles people, social care and AHPs undertake. This list is not exhaustive.
AHPs have a substantial part to play in addressing inequalities through specific targeted interventions, more equitable access to routine care and/or supporting the social determinants of health such as access to housing and welfare. The AHP’s commitment – both individually and as a community – to addressing health inequalities is demonstrated in AHPs My role in tackling Health Inequalities: A Framework for Allied Health Professionals. Each section of this framework gives examples of AHP-led work to tackle health inequalities across England.
A 2021 review of the impact of AHPs on health inequalities (Rapid Review of the Impact of Allied Health Professionals on Health Inequalities) identified two system-level themes:
- Ensuring equitable distribution of workforce in underserved areas and allocation of funding proportionate to need
- Better representation of minority groups, such as gender minorities, in clinical guidelines.
The ambitions for addressing health and care inequalities are:
- Supporting more equitable access to AHP services for lower socioeconomic groups, ethnic minority groups, people living in rural areas and other specific disadvantaged groups, and people with mental health problems
- Providing high-quality care and patient experience in terms of avoiding bias in decision-making, having culturally appropriate services and meeting clinical standards
- Addressing the social determinants of health through supporting employment and housing
- Supporting mental wellbeing with specific AHP services as well as incorporating mental wellbeing considerations in routine AHP services
- Engaging and empowering communities to support the co-design and delivery of culturally relevant services.
Delivering on these ambitions will also support the NHS England Core20PLUS5 approach to reducing health inequalities.
Focus 4: Environmental sustainability
The climate emergency is a health emergency. Tackling climate change through reducing harmful carbon emissions will improve health and save lives, which is why the NHS has set the ambition of reaching net zero emissions for the care we provide by 2040. Urgent collective action from all AHPs is crucial in helping to realise this ambition.
“Many of the AHPs by their very nature offer sustainable healthcare, through increasing independence and reducing the need for care, equipment, and surgery.”
Anon, June 2021. Quote: online conversation three.
“This needs to be integral to everything we do. We need to lead by example across all our areas.”
Anon, June 2021. Quote: online conversation three.
In October 2020, the NHS became the world’s first national health system to commit to net zero emissions in response to the health threat posed by the climate emergency. AHPs must act now to reduce the environmental impact of our services and deliver care in environmentally sustainable ways. Launched in October 2021, the Greener Allied Health Professional Hub highlights opportunities for sustainable practice and prioritises high impact actions for AHPs in a variety of environments.
Delivering a Net Zero NHS reports the high carbon footprint of healthcare delivery, especially acute care. Implementing ‘low carbon models of care’ at scale will be at the heart of a net zero future. (Greener NHS (england.nhs.uk)) The report also acknowledges that the drivers of climate change are also the drivers of ill health and health inequalities.
Many existing AHP practices already follow the principles of low carbon care; however, there is much more to do across service delivery – from sustainable equipment provision and more effective treatment pathways to highlighting the sustainability benefits of preventative and person-centred approaches. Helping people stay well through sustainable and healthy eating, personalised care and self-management decreases the severity and burden of disease, reducing their need for acute services. These practices are not only better for patients, they also reduce cost and the carbon emissions associated with a care episode.
Sources of carbon emissions vary widely across AHP practice in community, primary, secondary and tertiary settings. Opportunities to reduce these will develop quickly over the next five years.
The ambitions for environmental sustainability are:
- Workforce: Embedding new ways of working by building net zero into everything we do. To achieve this, all AHPs will need a good understanding of the net zero agenda, and it will form a crucial part of our competencies
- Models of care: Including net zero as a fundamental design principle in our models of care
- Resource use: Actively considering and reducing the environmental impact of the things we procure and prescribe as part of our practice.
Contributions to the Greener Allied Health Professional Hub demonstrate that AHPs embrace the net zero agenda. Action from the entire AHP community will ensure we collectively achieve the ambitions set out in this strategy, and bring the triple win of improving health, saving money and preserving the planet.
Focus 5: Strengthening and promoting the AHP community
Progress has been made in raising the profile of the AHP community, the third largest clinical workforce in the NHS, but there is still work to do. For the skills and capability of the 14 allied health professions to be fully realised, people accessing, and commissioning services need to understand each profession and the collective offer of the whole AHP community.
“I know some but not all of the allied health professions. The ones I have worked with are excellent and it is great to be able to advocate for a particular profession or service when discussing care plans. I would be interested to educate myself on all of the professions so I can make informed care choices.”
Anon, March 2021. Quote: Contributed to Older People Sounding Board Focus group.
“Increase the profile of the AHP support workforce. Recognise they have a unique contribution to the professional work and patient care. Enable them to feel valued in their roles or progress into registered practice if appropriate.”
Anon, June 2021. Quote: Contributed to online conversation three.
The AHP community comprises pre-registration students and apprentices, AHP support workers, assistant practitioners, those returning to practice (RtP) and registered AHPs. It is the third largest clinical workforce within the NHS, with AHPs also working across the community, education (including early years, schools), housing, justice, local authority care and voluntary sectors.
People accessing health and care need to know who AHPs are – as a collective and as individual professions with unique skills. They are then empowered to make informed personalised care decisions when choosing which profession to work with. AHPs need to articulate their offer to people, communities and other health and care professions through accessible means, and the profile of all 14 professions needs to be raised, particularly the smaller ones whose offer may not be well-known. This will also support recruitment into the professions.
AHPs into Action committed to care for those who care so they are healthy and happy. How we need to look after our people is also articulated in the NHS People Plan. This pledge has even more weight as AHPs move out of the COVID-19 pandemic. Recognising, supporting and valuing people who provide care to care is vital to the delivery of a quality and efficient care no matter their role, paid or unpaid.
Finally, AHPs must understand, encourage and celebrate diversity in all its forms. Discrimination, violence and bullying have no place and the AHP community will continue to implement the Workforce Race Equality Standard and the Workforce Disability Equality Standard. Section 1 affirms the AHP community’s anti-racist stance alongside acknowledging the ongoing work required to understand the needs of those with protected characteristics. This is particularly important for all protected characteristics that do not have standards in place, e.g. the LGBTQIA+ community.
The ambitions for the AHP community are:
- Raising awareness of AHPs: For care to be personalised, and for people to be able to make choices on how their needs can be best supported, people and communities need to know who the AHP community are. This includes understanding the expertise the 14 professions collectively provide, alongside the unique skills of each one
- Caring for those who care: As we emerge from the COVID-19 pandemic, ensuring the health and wellbeing of the AHP community will be critical for the months and years ahead. Learning from the pandemic, as individuals, organisations and systems, will drive improvement in staff experience. Staff wellbeing links to feeling valued and belonging and can be enhanced with flexible work options to support work/life balance. It is also important to identify AHPs who act as carers and support them accordingly
- Equality, diversity, inclusion and belonging: A sense of belonging ensures people bring their very best to work and provide the best for those they care for. There is a clear ethical, moral, and social case for equality, diversity, inclusion and belonging. Where standards are in place these will be used to monitor progress. Where standards do not exist, we will work to better understand the needs of these groups.
Appendix 1. AHP Strategy for England (2022-2027): Consultation methods
Strategy development was paused in 2020, owing to the COVID-19 pandemic, but resumed in early 2021 with engagement moving to a wholly virtual space.
The strategy has been co-created with people, the AHP community, and other health and care professionals in three engagement phases. Through an online conversation (crowdsourcing), hosted by Clever Together Lab Ltd, three separate workshops were open 24 hours a day, seven days a week. Those engaging could add ideas, write comments on the ideas and/or vote on the comments and ideas submitted. Contributions were completely anonymous.
| Phase | 2021 Dates | Engagement Activity (Called AHPs Listen) |
| One | February- March | An online conversation (crowdsourcing) with people and communities to gain their views and ideas about how they would like to receive and experience health and social care. |
| Two | May | An online conversation (crowdsourcing) with the AHP community to respond to the citizen voice of people and communities and have their say in how health and social care services should be delivered. This conversation included the registered AHP workforce, the AHP support workforce and AHP students across the 14 professions. |
| Three (Final) | June- July | An online conversation (crowdsourcing) with people communities, the AHP community and other health and social care professionals, discussing the final themes and findings for a ‘check and challenge’ before contributions from all three conversations were used to support the writing of the next AHP strategy for England. |
Over 3,200 registrants in 500 English postcodes made 21,000 contributions (ideas, comments, votes) across the three online conversations. These were thematically coded to identify the key themes and sentiment of the conversation. Votes and comments were also analysed to understand which ideas have strongest support (adjusting for the length of time a contribution has been visible for). The data was then triangulated with national policy and strategy to produce the final strategy.
At the time of writing, the crowdsourcing approach we adopted to support public consultation is considered the first of its kind in health and care strategy development in the UK.
For the online activities:
- 1,200 individuals identified as individuals who are accessing health and social care
- 10% identified as disabled
- 17% (3,200) identified as non-white British, and every ethnic category was represented
- All age groups and staff pay bands up to senior manager were represented
- 7% identified as non-heterosexual.
We heard from all 14 AHP professional groups, as well as other health and social care professionals (including nurses, dentists, social workers, medical doctors and psychologists) with data saturation achieved during the analysis phase.
The consultation and the strategy development team were supported by a peer leader via the NHS England and NHS Improvement personalised care team. The Peer Leadership Academy is a personal development programme that aims to build people’s knowledge, skills and confidence to play an active role in personalised care programmes and co-production at a national and regional level.
To ensure the project team did not exacerbate health inequalities and miss the voice of key groups, additional measures were taken to ensure inclusion and to support access. Three separate workshops were carried out in partnership with the organisation Working with Everyone (WE) to ensure the voice of underrepresented communities was captured during each consultation phase. WE are a not-for-profit company that prides itself on being independent. All WE directors, employees and volunteers have lived experience of social harms and marginalisation. WE members are selected for their personal, professional knowledge and expertise.
The project team also worked with the following NHS England and NHS Improvement teams and groups on various aspects of the consultation:
- Personalised Care Strategic Co-Production group
- Patient and Public Participation team
- Age UK Older People Sounding Board
- Learning Disability and Autism advisory group
- Voluntary; Charity and Third Sector Partnership team
- Children and Young People forum.
During the final online conversation, AHPs across England hosted several ad-hoc local events with local people and communities.
The NHS Assembly was asked to comment on the consultation work in September 2021.
The strategy development team appreciate the generous constructive feedback from many individuals representing a wide range of organisations across a variety of sectors during the strategy document drafting phases.
Appendix 2. Repository of ‘AHPs into Action’ outputs
- A digital framework for Allied Health Professions (AHPs).
- Allied Health Professions career guidance
- Allied Health Professions ‘AHPs Deliver’ implementation framework
- AHP job planning: A best practice guide
- Allied Health Professions leadership in trusts: what exists and what matters
- Allied Health Professions in primary care
- Allied Health Professions non-medical prescribing
- Allied Health Professions in Quality Improvement (QI)
- Allied Health Professionals supporting wellbeing and recovery in mental health – AHP North
- West (ahpnw.nhs.uk)
- Allied Health Professionals transforming health, care and wellbeing for autistic people and
- people with a learning disability – AHP North West (ahpnw.nhs.uk)
- Allied Health Professions making an impact in cardiovascular and respiratory disease – AHP
- North West (ahpnw.nhs.uk)
- Allied Health Professions within Integrated Care Systems (ICS)
- A rapid review and expert identification of the AHPs’ interventions as a contribution to
- public health outcomes.
- Chief AHP handbook
- Clinical academic careers
- Clinical leadership — a framework for action
- Commissioning for AHP services
- COVID-19: Caring for those who care – information and resources for Allied Health
- Professionals – December 2020
- COVID-19: Caring for those who care – information and resources for AHPs in Mental
- Health Awareness Week – update 4
- COVID-19: Caring for those who care – information and resources for Allied Health
- Professionals – update 3
- COVID-19: Caring for those who care – information and resources for Allied Health
- Professionals – update 2
- COVID-19: Caring for those who care – information and resources for Allied Health
- Professionals – update 1
- COVID-19: current changes in learning and development for the AHPs
- COVID-19 AHP students
- COVID related outputs can be found here: COVID-19: AHPs – AHP North
- West (ahpnw.nhs.uk)
- Developing Allied Health Professional (AHP) leaders
- Developing Allied Health Professional (AHP) leaders guide
- Digitally enabled services COVID-19: information and resources for Allied Health
- Professionals (AHPs)
- Greener Allied Health Professions (AHP) hub
- Health Education England (HEE) AHP faculties
- HEE AHP leadership in academia: Skills and attributes
- HEE AHP pre-registration student practice-based learning programme
- HEE AHP research and innovation strategy
- HEE developing practice-based learning in Mental Health and Learning Disability settings
- for the Allied Health Professions (AHPs)
- HEE developing the role of the support workforce
- HEE future proofing the podiatry workforce
- HEE increasing capacity in practice placements: challenges and solutions
- HEE practice placements: Challenges and solutions
- HEE AHP Return to Practice (RtP)
- HEE supporting the development of placements for AHP students in public health settings
- Improvement fundamentals
- Improving rehabilitation services
- Investing in Chief AHPs: Insights from trust executives
- Leadership of allied health professions in trusts: what exists and what matters
- Musculoskeletal (MSK) core capabilities
- Multiprofessional framework for advanced clinical practice in England
- National Institute of Clinical Excellence (NICE) into Action webinar series
- NHS electronic staff record: How to ensure Allied Health Professions (AHPs) are
- coded correctly
- Non-medical prescribing and Allied Health Professions (AHPs)
- Prevention of Suicide in the Ambulance Service: What we know
- Promoting Allied Health Professions (AHP) careers
- Quick guide: AHPs enhancing health for people in care homes
- Quick guide: AHPs supporting patient flow
- Quick guide: The role of AHPs in supporting people to live well with and beyond cancer
- Rapid review of the impact of allied health professionals on health inequalities
- The King’s Fund (2021) AHPs. My role in tackling health inequalities framework
- UK AHP Public Health strategic framework (2019-2024)
- Working together to prevent suicide in the ambulance service: National consensus
- Working together to prevent suicide in the ambulance service: Next steps

